User login
Staff Perspectives on the VISN 20 Tele-Neuropsychology Program
Staff Perspectives on the VISN 20 Tele-Neuropsychology Program
There are 2.7 million (48%) rural veterans enrolled in the Veterans Health Administration (VHA).1 Many VHA-enrolled rural veterans are aged ≥ 65 years (54%), a medically complex population that requires more extensive health care.1 These veterans may live far from US Department of Veterans Affairs (VA) medical centers (VAMCs) and often receive most of their care at rural community-based outpatient clinics (CBOCs). In addition to face-to-face (F2F) services provided at these clinics, many patient care needs may be met using telehealth technology, which can connect veterans at CBOCs with remote health care practitioners (HCPs).
This technology is used across medical specialties throughout the VA and has expanded into neuropsychology services to improve access amid the shortage of rural neuropsychologists. Prior research suggests that access to neuropsychology services improves the functional outcomes of people with diverse medical conditions, including dementia, brain injury, and epilepsy, and reduces emergency department visits, hospitalization duration, and health care costs.2-6 Given that veterans unable to access neuropsychology services may be at risk for poorer outcomes, identifying ways to improve access is a priority. Tele-neuropsychology (teleNP) has been used to expand access for rural veterans in need of these services.7,8
TeleNP is the application of audiovisual technologies to enable remote clinical encounters for neuropsychological assessments.9 TeleNP has been shown to be generally equivalent to F2F care, without significant differences compared with in-person visits.10-13 TeleNP was increasingly implemented following the COVID-19 pandemic and remains an enduring and expanding feature of neuropsychology care delivery.8,14-18 TeleNP services can increase access to care, especially for rural veterans and those with limited transportation.
Research in non-VA samples suggests a high level of clinician satisfaction with teleNP.16 In VA samples, research has found high levels of patient satisfaction with teleNP both within Veterans Integrated Services Network (VISN) 20 and in a VA health care system outside VISN 20.7,19 Investigating staff perceptions of these services and their utility compared with non-VA F2F visits is pertinent to the overall feasibility and effectiveness of teleNP.
TELE-NEUROPSYCHOLOGY PROGRAM
A clinical resource hub (CRH) is a VISN-governed program that provides veteran health care when local VHA facilities have service gaps.20,21 CRH 20 serves several Pacific Northwest VISN 20 health care systems and began providing teleNP in 2015. The CRH 20 teleNP service serves older adults in rural settings with > 570 teleNP evaluations completed over a recent 12-month period (May 2023 to May 2024). In the CRH 20 teleNP program, veterans are offered services by CRH 20 neuropsychologists via telehealth to a patient’s local VAMC, larger health care clinic, CBOC, or via Veterans Video Connect to the home.
Referral pathways to the CRH 20 teleNP program differ across sites. For VISN 20 sites that do not have any in-house neuropsychology services, referrals are initiated by HCPs from any discipline. At 2 sites with in-house neuropsychology programs, CRH 20 teleNP referrals typically are forwarded from the inhouse service whenever the veteran prefers to be seen at an outlying clinic. All sites, including the CBOCs, are equipped fully for testing, and the HCP encounters veterans in a private office via video-based telehealth technology after a telehealth technician orients them to the space. The private office minimizes environmental disruptions and uses standardized technology to ensure valid results. A limited number of evaluations are offered at home (< 5% of the evaluations) if the veteran is unable to come to a VHA facility, has access to reliable internet, and a minimally distracting home setting.
In VISN 20, teleNP is a routine practice for delivering services to rural sites, most of which lack neuropsychologists. However, there is limited information about the extent to which the referral sources find the service useful. This quality improvement (QI) project aimed to better understand how well-established teleNP services were received by referral sources/stakeholders and how services could be improved. Prior to the advent of the CRH 20 teleNP program, staff had the option of referring for F2F evaluations in the local community (outside the VA) at some sites, an option that remains. This QI project examined staff perspectives on the usefulness of CRH 20 teleNP services compared with non-VA F2F services. We administered an anonymous, confidential survey examining these factors to VISN 20 staff within 4 VA health care systems.
METHODS
This QI project used a mixed quantitative and qualitative descriptive survey design to elicit feedback. The authors (3 neuropsychologists, 1 geropsychologist, and 1 research coordinator) developed the survey questions. The 13-question survey was voluntary, anonymous, and confidential, and respondents were given an opportunity to ask questions, with the first author serving as the point of contact.
The survey ascertained information about respondents and their work setting (ie, facility type, specific work setting and location, profession, and rurality of patients). First respondents were asked whether they have referred patients to neuropsychology services in the past year. Those who had not referred patients during the past year were asked about reasons for nonreferral with an option to provide an open-ended response. Respondents who did refer were asked how they refer for neuropsychology services and about the usefulness and timeliness of both teleNP and non-VA F2F services. Respondents were asked to respond with their preference for teleNP vs non-VA F2F with an open-ended prompt. Finally, respondents were invited to share any feedback for improvement regarding teleNP services.
A link to the survey, hosted on the VA Research Electronic Data Capture system, was emailed to facility and service line leaders at the 4 VISN 20 health care systems for distribution to the staff. All staff were included because in many of the facilities, particularly those that are highly rural with low staffing, it is not uncommon for technicians, nurses, and other support staff to assist with placing consults. In particular, VISN 20 nurses often have an optimal understanding of referral pathways to care for patients and are positioned to give and receive feedback about the utility of neuropsychological evaluations. The Research and Development Committee at the Boise VA Medical Center determined this project to be QI and exempt from institutional review board oversight. The VISN 20 employee labor relations HR supervisor approved this survey, with union awareness. Responses were anonymous.
Data were imported into Microsoft Excel and IBM SPSS Statistics for further analysis. Data were summarized using descriptive statistics, frequencies, and percentages. Nonparametric χ2 and Wilcoxon signed-rank tests were used to test for differences. An inductive approach to develop codes was used for the 3 open-ended questions. Two authors (CC, CEG) independently coded the responses and reviewed discrepancies. Final code applications were based on consensus.
RESULTS
The survey was deployed for 1 month between February 7, 2024, and June 15, 2024, at each of the 4 health care systems. Thirty-three staff members responded; of these, 1 person did not respond to an item on whether they referred for neuropsychology services. Eighteen of 33 respondents reported referring patients to teleNP or F2F neuropsychology services in the past year. Fourteen of the 33 respondents stated they did not refer; of these, 2 were unfamiliar with the teleNP service and 12 provided other reasons (eg, new to VA, not in their professional scope to order consults, did not have patients needing services).
The analysis focused on the 18 respondents who referred for neuropsychology services. Thirteen were within health care system A, and 5 were within health care system B (which had no nearby non-VA contracted neuropsychology services) and none were in the other 2 health care systems. Ten of 18 respondents (56%) stated they practiced primarily in a rural setting. Five respondents worked in a CBOC, 12 in a main VA facility, 9 in a primary care setting, 8 in a mental health setting, and 3 in other settings (eg, domiciliary). Participants could select > 1 setting. The 18 respondents who referred to neuropsychology services included 7 psychologists, 1 nurse, 2 social workers, 1 social services assistant, 4 nurse practitioners, 2 physicians, and 1 unknown HCP.
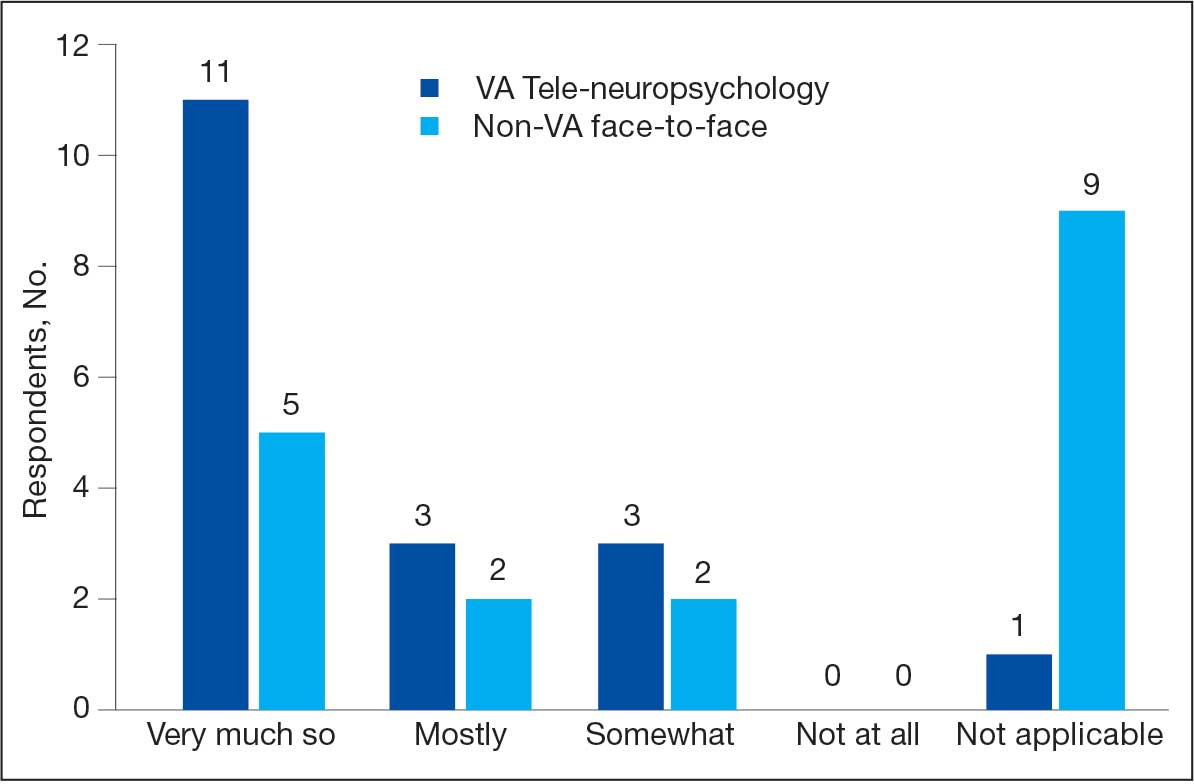
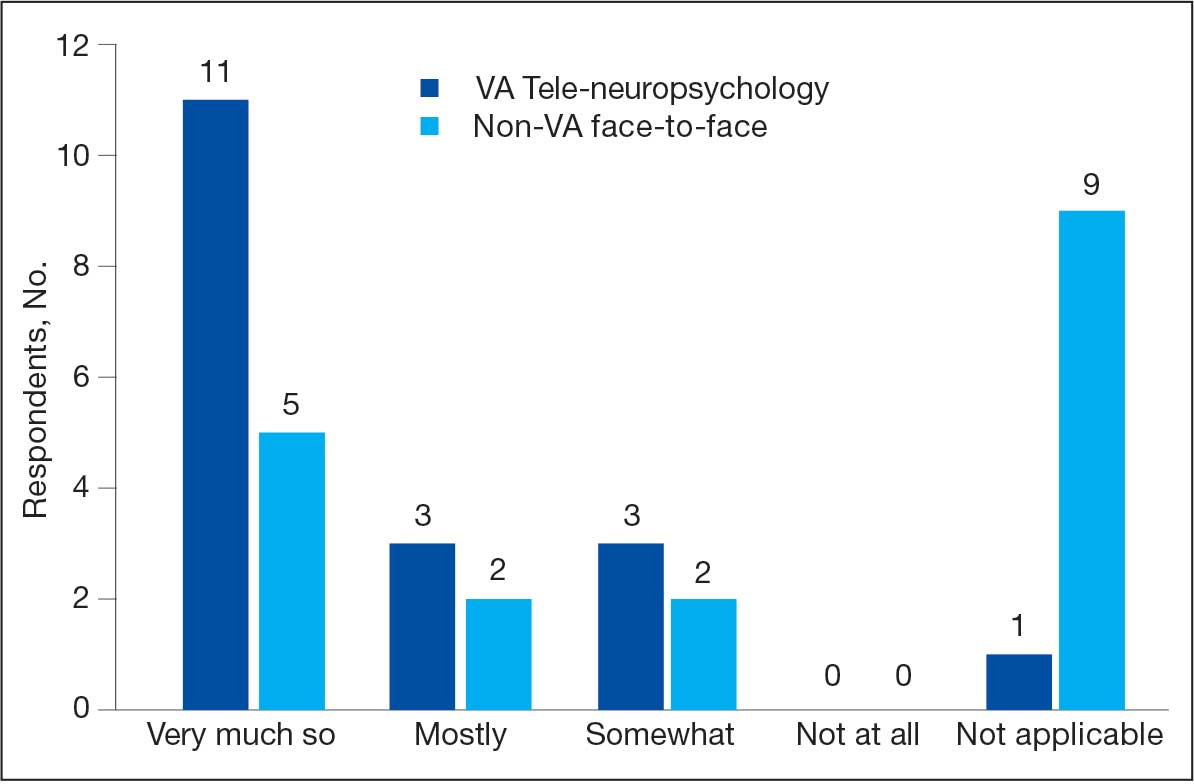
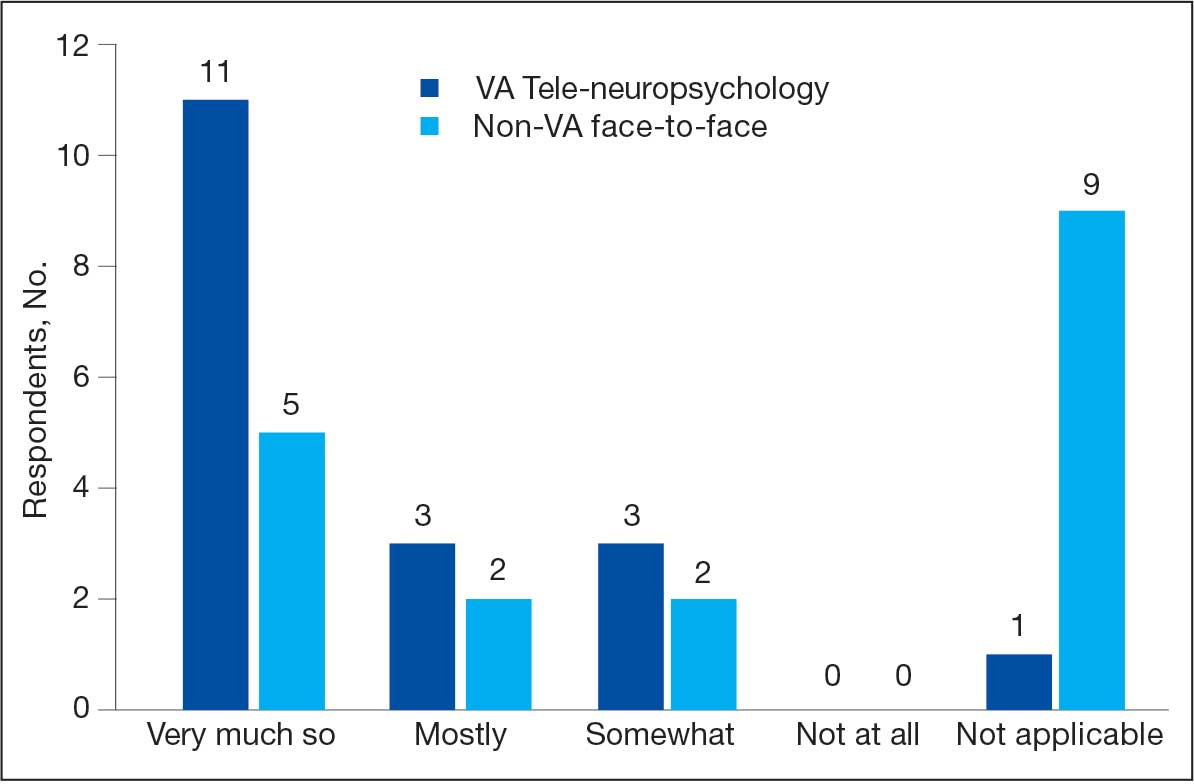
When asked to categorize the usefulness of services, more respondents characterized teleNP as very much so (1 on a 5-point scale) than F2F referrals (Figure). The mean (SD) of 1.5 (0.8) for teleNP usefulness fell between very much so and mostly and 1 respondent indicated not applicable. Similarly, the mean (SD) for non-VA F2F usefulness was 1.7 (0.9); 9 respondents rated this item as not applicable. A Wilcoxon signed-rank test of related samples indicated no significant differences between the pairs of ratings (Z = 1.50; P = .41).
Respondents with rural patients were more likely to refer them to teleNP services compared with respondents with nonrural patients (χ2 = 5.7; P = .02). However, ratings of teleNP usefulness did not significantly differ for those serving rural vs with nonrural patients (χ2 = 1.4; P = .49). Mean (SD) rating of teleNP usefulness was 1.3 (0.7) for the 9 rural subgroup respondents (between very much so and mostly) vs 1.8 (0.9) for the 8 nonrural subgroup respondents (between very much so and mostly). The mean (SD) rating for non-VA F2F usefulness was 1.8 (1.0) for the 4 rural subgroup respondents and 1.6 (0.8) for the 5 nonrural subgroup, between very much so and mostly for both groups.
Most respondents had no preference between teleNP or F2F. Notably, the responses underlying this group were multifaceted and corresponded to multiple codes (ie, access, preference for in-person services, technology, space and logistics, and service boundaries and requirements). According to 1 respondent, “the logistics of scheduling/room availability, technological challenges, and client behavioral issues that are likely to occur could possibly be more easily addressed via in-person sessions for some clients and providers.”
Six of 18 respondents preferred teleNP, citing timeliness, ease of access, and evaluation quality. One respondent noted that the “majority of my veterans live in extremely remote areas” and may need to take a plane for their visit. The 3 respondents who preferred in-person neuropsychology services cited veterans’ preference for in-person services.
Open-Ended Feedback
Thirteen respondents offered feedback on what is working well with teleNP services. Reasons mentioned were related to the service (ie, timeliness, access, quality) and the neuropsychologist (ie, communication and HCP skills). One respondent described the service and neuropsychologists positively, stating that they were “responsive, notes are readily available, clear assessments and recommendations, being available by [Microsoft] Teams/email.”
Ten respondents provided suggestions for improvement. Suggestions focused on expanding services, such as to “all veterans with cognitive/memory concerns that desire testing,” individuals with attention-deficit/hyperactivity disorder and co-occurring mental health concerns, and those in residential programs. Suggestions included hiring psychology technicians or more staff and providing education at local clinics.
DISCUSSION
This QI project examines VA staff perspectives on the usefulness of CRH 20 teleNP services and non-VA F2F services. While the small sample size limits generalizability, this preliminary study suggests that VA teleNP evaluations were similar to those conducted F2F in non-VA settings. While ratings of teleNP usefulness did not differ significantly for those serving rural vs nonrural veterans, respondents serving rural patients were more likely to refer patients to teleNP, suggesting that teleNP may increase access in rural settings, consistent with other studies.7,8,13 This article also presents qualitative suggestions for improving teleNP delivery within the VHA. This is the first known initiative to report on VHA staff satisfaction with a teleNP service and expands the limited literature to date on satisfaction with teleNP services. The findings provide initial support for continued use and, potentially, expansion of teleNP services within this CRH remote hub-and-spoke model.
Limitations
A significant limitation of the current work is the small sample size of survey respondents. In particular, while teleNP turnaround time was perceived as faster than non-VA F2F care, only 8 respondents reported on timeliness of F2F evaluation results, which renders it difficult to draw conclusions. Interestingly, not all respondents reported referring to neuropsychology services within the previous year; the most common reasons reflect the perception that referral to neuropsychology was outside of that staff member’s role or not clinically indicated.
One additional possible explanation for the absence of reporting on utility of teleNP specifically is that respondents did not track whether their patient was seen by teleNP or F2F services, based on how the referral process varies at each health care system. For example, in health care system C, a large number of referrals are forwarded to the service by local VA F2F neuropsychologists. This may speak to the seamlessness of the teleNP process, such that local staff and/or referring HCPs are unaware of the modality over which neuropsychology is being conducted. It is plausible that the reason behind this smaller response rate in health care systems B and C relates to how neuropsychology consults are processed at these local VAMCs. We suspect that in these settings, the HCPs referring for neuropsychological evaluations (eg, primary care, mental health) may be unaware that their referrals are being triaged to neuropsychologists in a different program (CRH 20 teleNP). Therefore, they would not necessarily know that they used teleNP and didn’t complete the survey.
The referral process for these 2 sites contrasts with the process for other VISN 20 sites where there is no local neuropsychology program triaging. In these settings, referrals from local HCPs come directly to teleNP; thus, it is more likely that these HCPs are aware of teleNP services. There were only 2 physicians who completed the survey, which may relate to their workload and a workflow where other staff have been increasingly requested to order the consults for the physician. This type of workflow results in an increase in the number of VHA staff involved in patient care. Ratings of usefulness were highest in health care system B, which does not have neuropsychology services at the facility or in the community; this may relate to elevated teleNP satisfaction ratings.
Further work may help identify which aspects of a teleNP service make it more useful than F2F care for this population or determine whether there were HCPor setting-specific factors that influenced the ratings (ie, preference for VA care or comparison of favorability ratings for the HCPs who conduct teleNP and F2F within the same system). The latter comparisons could not be drawn in the current systems due to the absence of HCPs who provide both teleNP and F2F modalities within VISN 20. Another consideration for future work would be to use a previously published/validated survey measure and piloting of questions with a naive sample before implementation.
CONCLUSIONS
This analysis provides initial support for feasibility and acceptability of teleNP as an alternative to traditional in-person neuropsychological evaluations. The small number of survey respondents may reflect the multiple pathways through which consults are forwarded to CRH 20, which includes both direct HCP referrals and forwarded consults from local neuropsychology services. CRH 20 has completed > 570 teleNP evaluations within 1 year, suggesting that lack of awareness may not be hindering veteran access to the service. Replication with a larger sample that is more broadly representative of key stakeholders in veteran care, identification of populations that would benefit most from teleNP services, and dissemination studies of the expansion of teleNP services are all important directions for future work. The robustness and longevity of the VISN 20 teleNP program, coupled with the preliminary positive findings from this project, demonstrate support for further assessment of the potential impact of telehealth on neuropsychological care within the VHA and show that barriers associated with access to health care services in remote settings may be mitigated through teleNP service delivery.
- US Department of Veterans Affairs, Office of Rural Health. Rural veterans. Updated March 10, 2025. Accessed July 7, 2025. https://www.ruralhealth.va.gov/aboutus/ruralvets.asp
- Braun M, Tupper D, Kaufmann P, et al. Neuropsychological assessment: a valuable tool in the diagnosis and management of neurological, neurodevelopmental, medical, and psychiatric disorders. Cogn Behav Neurol. 2011;24(3):107-114. doi:10.1097/wnn.0b013e3182351289
- Donders J. The incremental value of neuropsychological assessment: a critical review. Clin Neuropsychol. 2020;34(1):56-87. doi:10.1080/13854046.2019.1575471
- Williams MW, Rapport LJ, Hanks RA, et al. Incremental value of neuropsychological evaluations to computed tomography in predicting long-term outcomes after traumatic brain injury. Clin Neuropsychol. 2013;27(3):356-375. doi:10.1080/13854046.2013.765507
- Sieg E, Mai Q, Mosti C, Brook M. The utility of neuropsychological consultation in identifying medical inpatients with suspected cognitive impairment at risk for greater hospital utilization. Clin Neuropsychol. 2019;33(1):75-89. doi:10.1080/13854046.2018.1465124
- Vankirk KM, Horner MD, Turner TH, et al. CE hospital service utilization is reduced following neuropsychological evaluation in a sample of U.S. veterans. Clin Neuropsychol. 2013;27(5):750-761. doi:10.1080/13854046.2013.783122
- Appleman ER, O’Connor MK, Boucher SJ, et al. Teleneuropsychology clinic development and patient satisfaction. Clin Neuropsychol. 2021;35(4):819-837. doi:10.1080/13854046.2020.1871515
- Stelmokas J, Ratcliffe LN, Lengu K, et al. Evaluation of teleneuropsychology services in veterans during COVID-19. Psychol Serv. 2024;21(1):65-72. doi:10.1037/ser0000810
- Bilder R Postal KS, Barisa M, et al. Inter Organizational Practice Committee recommendations/guidance for teleneuropsychology in response to the COVID-19 pandemic. Arch Clin Neuropsychol. 2020;35(6):647-659. doi:10.1093/arclin/acaa046
- Brearly TW, Shura RD, Martindale SL, et al. Neuropsychological test administration by videoconference: a systematic review and meta-analysis. Neuropsychol Rev. 2017;27(2):174-186. doi:10.1007/s11065-017-9349-1
- Brown AD, Kelso W, Eratne D, et al. Investigating equivalence of in-person and telehealth-based neuropsychological assessment performance for individuals being investigated for younger onset dementia. Arch Clin Neuropsychol. 2024;39(5):594-607. doi:10.1093/arclin/acad108
- Chapman JE, Ponsford J, Bagot KL, et al. The use of videoconferencing in clinical neuropsychology practice: a mixed methods evaluation of neuropsychologists’ experiences and views. Aust Psychol. 2020;55(6):618-633. doi:10.1111/ap.12471
- Marra DE, Hamlet KM, Bauer RM, et al. Validity of teleneuropsychology for older adults in response to COVID-19: a systematic and critical review. Clin Neuropsychol. 2020;34:1411-1452. doi:10.1080/13854046.2020.1769192
- Hammers DB, Stolwyk R, Harder L, et al. A survey of international clinical teleneuropsychology service provision prior to COVID-19. Clin Neuropsychol. 2020;34(7-8):1267- 1283. doi:10.1080/13854046.2020.1810323
- Marra DE, Hoelzle JB, Davis JJ, et al. Initial changes in neuropsychologists’ clinical practice during the COVID-19 pandemic: a survey study. Clin Neuropsychol. 2020;34(7- 8):1251-1266. doi:10.1080/13854046.2020.1800098
- Parsons MW, Gardner MM, Sherman, JC et al. Feasibility and acceptance of direct-to-home teleneuropsychology services during the COVID-19 pandemic. J Int Neuropsychol Soc. 2022;28(2):210-215. doi:10.1017/s1355617721000436
- Rochette AD, Rahman-Filipiak A, Spencer RJ, et al. Teleneuropsychology practice survey during COVID-19 within the United States. Appl Neuropsychol Adult. 2022;29(6):1312- 1322. doi:10.1080/23279095.2021.1872576
- Messler AC, Hargrave DD, Trittschuh EH, et al. National survey of telehealth neuropsychology practices: current attitudes, practices, and relevance of tele-neuropsychology three years after the onset of COVID-19. Clin Neuropsychol. 2023;39:1017-1036. doi:10.1080/13854046.2023.2192422
- Rautman L, Sordahl JA. Veteran satisfaction with tele-neuropsychology services. Clin Neuropsychol. 2018;32:1453949. doi:10.1080/13854046.2018.1453949
- US Department of Veterans Affairs. Patient care services: clinical resource hubs. Updated March 20, 2024. Accessed August 4, 2025. https://www.patientcare .va.gov/primarycare/CRH.asp
- Burnett K, Stockdale SE, Yoon J, et al. The Clinical Resource Hub initiative: first-year implementation of the Veterans Health Administration regional telehealth contingency staffing program. Ambul Care Manage. 2023;46(3):228-239. doi:10.1097/JAC.0000000000000468
There are 2.7 million (48%) rural veterans enrolled in the Veterans Health Administration (VHA).1 Many VHA-enrolled rural veterans are aged ≥ 65 years (54%), a medically complex population that requires more extensive health care.1 These veterans may live far from US Department of Veterans Affairs (VA) medical centers (VAMCs) and often receive most of their care at rural community-based outpatient clinics (CBOCs). In addition to face-to-face (F2F) services provided at these clinics, many patient care needs may be met using telehealth technology, which can connect veterans at CBOCs with remote health care practitioners (HCPs).
This technology is used across medical specialties throughout the VA and has expanded into neuropsychology services to improve access amid the shortage of rural neuropsychologists. Prior research suggests that access to neuropsychology services improves the functional outcomes of people with diverse medical conditions, including dementia, brain injury, and epilepsy, and reduces emergency department visits, hospitalization duration, and health care costs.2-6 Given that veterans unable to access neuropsychology services may be at risk for poorer outcomes, identifying ways to improve access is a priority. Tele-neuropsychology (teleNP) has been used to expand access for rural veterans in need of these services.7,8
TeleNP is the application of audiovisual technologies to enable remote clinical encounters for neuropsychological assessments.9 TeleNP has been shown to be generally equivalent to F2F care, without significant differences compared with in-person visits.10-13 TeleNP was increasingly implemented following the COVID-19 pandemic and remains an enduring and expanding feature of neuropsychology care delivery.8,14-18 TeleNP services can increase access to care, especially for rural veterans and those with limited transportation.
Research in non-VA samples suggests a high level of clinician satisfaction with teleNP.16 In VA samples, research has found high levels of patient satisfaction with teleNP both within Veterans Integrated Services Network (VISN) 20 and in a VA health care system outside VISN 20.7,19 Investigating staff perceptions of these services and their utility compared with non-VA F2F visits is pertinent to the overall feasibility and effectiveness of teleNP.
TELE-NEUROPSYCHOLOGY PROGRAM
A clinical resource hub (CRH) is a VISN-governed program that provides veteran health care when local VHA facilities have service gaps.20,21 CRH 20 serves several Pacific Northwest VISN 20 health care systems and began providing teleNP in 2015. The CRH 20 teleNP service serves older adults in rural settings with > 570 teleNP evaluations completed over a recent 12-month period (May 2023 to May 2024). In the CRH 20 teleNP program, veterans are offered services by CRH 20 neuropsychologists via telehealth to a patient’s local VAMC, larger health care clinic, CBOC, or via Veterans Video Connect to the home.
Referral pathways to the CRH 20 teleNP program differ across sites. For VISN 20 sites that do not have any in-house neuropsychology services, referrals are initiated by HCPs from any discipline. At 2 sites with in-house neuropsychology programs, CRH 20 teleNP referrals typically are forwarded from the inhouse service whenever the veteran prefers to be seen at an outlying clinic. All sites, including the CBOCs, are equipped fully for testing, and the HCP encounters veterans in a private office via video-based telehealth technology after a telehealth technician orients them to the space. The private office minimizes environmental disruptions and uses standardized technology to ensure valid results. A limited number of evaluations are offered at home (< 5% of the evaluations) if the veteran is unable to come to a VHA facility, has access to reliable internet, and a minimally distracting home setting.
In VISN 20, teleNP is a routine practice for delivering services to rural sites, most of which lack neuropsychologists. However, there is limited information about the extent to which the referral sources find the service useful. This quality improvement (QI) project aimed to better understand how well-established teleNP services were received by referral sources/stakeholders and how services could be improved. Prior to the advent of the CRH 20 teleNP program, staff had the option of referring for F2F evaluations in the local community (outside the VA) at some sites, an option that remains. This QI project examined staff perspectives on the usefulness of CRH 20 teleNP services compared with non-VA F2F services. We administered an anonymous, confidential survey examining these factors to VISN 20 staff within 4 VA health care systems.
METHODS
This QI project used a mixed quantitative and qualitative descriptive survey design to elicit feedback. The authors (3 neuropsychologists, 1 geropsychologist, and 1 research coordinator) developed the survey questions. The 13-question survey was voluntary, anonymous, and confidential, and respondents were given an opportunity to ask questions, with the first author serving as the point of contact.
The survey ascertained information about respondents and their work setting (ie, facility type, specific work setting and location, profession, and rurality of patients). First respondents were asked whether they have referred patients to neuropsychology services in the past year. Those who had not referred patients during the past year were asked about reasons for nonreferral with an option to provide an open-ended response. Respondents who did refer were asked how they refer for neuropsychology services and about the usefulness and timeliness of both teleNP and non-VA F2F services. Respondents were asked to respond with their preference for teleNP vs non-VA F2F with an open-ended prompt. Finally, respondents were invited to share any feedback for improvement regarding teleNP services.
A link to the survey, hosted on the VA Research Electronic Data Capture system, was emailed to facility and service line leaders at the 4 VISN 20 health care systems for distribution to the staff. All staff were included because in many of the facilities, particularly those that are highly rural with low staffing, it is not uncommon for technicians, nurses, and other support staff to assist with placing consults. In particular, VISN 20 nurses often have an optimal understanding of referral pathways to care for patients and are positioned to give and receive feedback about the utility of neuropsychological evaluations. The Research and Development Committee at the Boise VA Medical Center determined this project to be QI and exempt from institutional review board oversight. The VISN 20 employee labor relations HR supervisor approved this survey, with union awareness. Responses were anonymous.
Data were imported into Microsoft Excel and IBM SPSS Statistics for further analysis. Data were summarized using descriptive statistics, frequencies, and percentages. Nonparametric χ2 and Wilcoxon signed-rank tests were used to test for differences. An inductive approach to develop codes was used for the 3 open-ended questions. Two authors (CC, CEG) independently coded the responses and reviewed discrepancies. Final code applications were based on consensus.
RESULTS
The survey was deployed for 1 month between February 7, 2024, and June 15, 2024, at each of the 4 health care systems. Thirty-three staff members responded; of these, 1 person did not respond to an item on whether they referred for neuropsychology services. Eighteen of 33 respondents reported referring patients to teleNP or F2F neuropsychology services in the past year. Fourteen of the 33 respondents stated they did not refer; of these, 2 were unfamiliar with the teleNP service and 12 provided other reasons (eg, new to VA, not in their professional scope to order consults, did not have patients needing services).
The analysis focused on the 18 respondents who referred for neuropsychology services. Thirteen were within health care system A, and 5 were within health care system B (which had no nearby non-VA contracted neuropsychology services) and none were in the other 2 health care systems. Ten of 18 respondents (56%) stated they practiced primarily in a rural setting. Five respondents worked in a CBOC, 12 in a main VA facility, 9 in a primary care setting, 8 in a mental health setting, and 3 in other settings (eg, domiciliary). Participants could select > 1 setting. The 18 respondents who referred to neuropsychology services included 7 psychologists, 1 nurse, 2 social workers, 1 social services assistant, 4 nurse practitioners, 2 physicians, and 1 unknown HCP.
When asked to categorize the usefulness of services, more respondents characterized teleNP as very much so (1 on a 5-point scale) than F2F referrals (Figure). The mean (SD) of 1.5 (0.8) for teleNP usefulness fell between very much so and mostly and 1 respondent indicated not applicable. Similarly, the mean (SD) for non-VA F2F usefulness was 1.7 (0.9); 9 respondents rated this item as not applicable. A Wilcoxon signed-rank test of related samples indicated no significant differences between the pairs of ratings (Z = 1.50; P = .41).
Respondents with rural patients were more likely to refer them to teleNP services compared with respondents with nonrural patients (χ2 = 5.7; P = .02). However, ratings of teleNP usefulness did not significantly differ for those serving rural vs with nonrural patients (χ2 = 1.4; P = .49). Mean (SD) rating of teleNP usefulness was 1.3 (0.7) for the 9 rural subgroup respondents (between very much so and mostly) vs 1.8 (0.9) for the 8 nonrural subgroup respondents (between very much so and mostly). The mean (SD) rating for non-VA F2F usefulness was 1.8 (1.0) for the 4 rural subgroup respondents and 1.6 (0.8) for the 5 nonrural subgroup, between very much so and mostly for both groups.
Most respondents had no preference between teleNP or F2F. Notably, the responses underlying this group were multifaceted and corresponded to multiple codes (ie, access, preference for in-person services, technology, space and logistics, and service boundaries and requirements). According to 1 respondent, “the logistics of scheduling/room availability, technological challenges, and client behavioral issues that are likely to occur could possibly be more easily addressed via in-person sessions for some clients and providers.”
Six of 18 respondents preferred teleNP, citing timeliness, ease of access, and evaluation quality. One respondent noted that the “majority of my veterans live in extremely remote areas” and may need to take a plane for their visit. The 3 respondents who preferred in-person neuropsychology services cited veterans’ preference for in-person services.
Open-Ended Feedback
Thirteen respondents offered feedback on what is working well with teleNP services. Reasons mentioned were related to the service (ie, timeliness, access, quality) and the neuropsychologist (ie, communication and HCP skills). One respondent described the service and neuropsychologists positively, stating that they were “responsive, notes are readily available, clear assessments and recommendations, being available by [Microsoft] Teams/email.”
Ten respondents provided suggestions for improvement. Suggestions focused on expanding services, such as to “all veterans with cognitive/memory concerns that desire testing,” individuals with attention-deficit/hyperactivity disorder and co-occurring mental health concerns, and those in residential programs. Suggestions included hiring psychology technicians or more staff and providing education at local clinics.
DISCUSSION
This QI project examines VA staff perspectives on the usefulness of CRH 20 teleNP services and non-VA F2F services. While the small sample size limits generalizability, this preliminary study suggests that VA teleNP evaluations were similar to those conducted F2F in non-VA settings. While ratings of teleNP usefulness did not differ significantly for those serving rural vs nonrural veterans, respondents serving rural patients were more likely to refer patients to teleNP, suggesting that teleNP may increase access in rural settings, consistent with other studies.7,8,13 This article also presents qualitative suggestions for improving teleNP delivery within the VHA. This is the first known initiative to report on VHA staff satisfaction with a teleNP service and expands the limited literature to date on satisfaction with teleNP services. The findings provide initial support for continued use and, potentially, expansion of teleNP services within this CRH remote hub-and-spoke model.
Limitations
A significant limitation of the current work is the small sample size of survey respondents. In particular, while teleNP turnaround time was perceived as faster than non-VA F2F care, only 8 respondents reported on timeliness of F2F evaluation results, which renders it difficult to draw conclusions. Interestingly, not all respondents reported referring to neuropsychology services within the previous year; the most common reasons reflect the perception that referral to neuropsychology was outside of that staff member’s role or not clinically indicated.
One additional possible explanation for the absence of reporting on utility of teleNP specifically is that respondents did not track whether their patient was seen by teleNP or F2F services, based on how the referral process varies at each health care system. For example, in health care system C, a large number of referrals are forwarded to the service by local VA F2F neuropsychologists. This may speak to the seamlessness of the teleNP process, such that local staff and/or referring HCPs are unaware of the modality over which neuropsychology is being conducted. It is plausible that the reason behind this smaller response rate in health care systems B and C relates to how neuropsychology consults are processed at these local VAMCs. We suspect that in these settings, the HCPs referring for neuropsychological evaluations (eg, primary care, mental health) may be unaware that their referrals are being triaged to neuropsychologists in a different program (CRH 20 teleNP). Therefore, they would not necessarily know that they used teleNP and didn’t complete the survey.
The referral process for these 2 sites contrasts with the process for other VISN 20 sites where there is no local neuropsychology program triaging. In these settings, referrals from local HCPs come directly to teleNP; thus, it is more likely that these HCPs are aware of teleNP services. There were only 2 physicians who completed the survey, which may relate to their workload and a workflow where other staff have been increasingly requested to order the consults for the physician. This type of workflow results in an increase in the number of VHA staff involved in patient care. Ratings of usefulness were highest in health care system B, which does not have neuropsychology services at the facility or in the community; this may relate to elevated teleNP satisfaction ratings.
Further work may help identify which aspects of a teleNP service make it more useful than F2F care for this population or determine whether there were HCPor setting-specific factors that influenced the ratings (ie, preference for VA care or comparison of favorability ratings for the HCPs who conduct teleNP and F2F within the same system). The latter comparisons could not be drawn in the current systems due to the absence of HCPs who provide both teleNP and F2F modalities within VISN 20. Another consideration for future work would be to use a previously published/validated survey measure and piloting of questions with a naive sample before implementation.
CONCLUSIONS
This analysis provides initial support for feasibility and acceptability of teleNP as an alternative to traditional in-person neuropsychological evaluations. The small number of survey respondents may reflect the multiple pathways through which consults are forwarded to CRH 20, which includes both direct HCP referrals and forwarded consults from local neuropsychology services. CRH 20 has completed > 570 teleNP evaluations within 1 year, suggesting that lack of awareness may not be hindering veteran access to the service. Replication with a larger sample that is more broadly representative of key stakeholders in veteran care, identification of populations that would benefit most from teleNP services, and dissemination studies of the expansion of teleNP services are all important directions for future work. The robustness and longevity of the VISN 20 teleNP program, coupled with the preliminary positive findings from this project, demonstrate support for further assessment of the potential impact of telehealth on neuropsychological care within the VHA and show that barriers associated with access to health care services in remote settings may be mitigated through teleNP service delivery.
There are 2.7 million (48%) rural veterans enrolled in the Veterans Health Administration (VHA).1 Many VHA-enrolled rural veterans are aged ≥ 65 years (54%), a medically complex population that requires more extensive health care.1 These veterans may live far from US Department of Veterans Affairs (VA) medical centers (VAMCs) and often receive most of their care at rural community-based outpatient clinics (CBOCs). In addition to face-to-face (F2F) services provided at these clinics, many patient care needs may be met using telehealth technology, which can connect veterans at CBOCs with remote health care practitioners (HCPs).
This technology is used across medical specialties throughout the VA and has expanded into neuropsychology services to improve access amid the shortage of rural neuropsychologists. Prior research suggests that access to neuropsychology services improves the functional outcomes of people with diverse medical conditions, including dementia, brain injury, and epilepsy, and reduces emergency department visits, hospitalization duration, and health care costs.2-6 Given that veterans unable to access neuropsychology services may be at risk for poorer outcomes, identifying ways to improve access is a priority. Tele-neuropsychology (teleNP) has been used to expand access for rural veterans in need of these services.7,8
TeleNP is the application of audiovisual technologies to enable remote clinical encounters for neuropsychological assessments.9 TeleNP has been shown to be generally equivalent to F2F care, without significant differences compared with in-person visits.10-13 TeleNP was increasingly implemented following the COVID-19 pandemic and remains an enduring and expanding feature of neuropsychology care delivery.8,14-18 TeleNP services can increase access to care, especially for rural veterans and those with limited transportation.
Research in non-VA samples suggests a high level of clinician satisfaction with teleNP.16 In VA samples, research has found high levels of patient satisfaction with teleNP both within Veterans Integrated Services Network (VISN) 20 and in a VA health care system outside VISN 20.7,19 Investigating staff perceptions of these services and their utility compared with non-VA F2F visits is pertinent to the overall feasibility and effectiveness of teleNP.
TELE-NEUROPSYCHOLOGY PROGRAM
A clinical resource hub (CRH) is a VISN-governed program that provides veteran health care when local VHA facilities have service gaps.20,21 CRH 20 serves several Pacific Northwest VISN 20 health care systems and began providing teleNP in 2015. The CRH 20 teleNP service serves older adults in rural settings with > 570 teleNP evaluations completed over a recent 12-month period (May 2023 to May 2024). In the CRH 20 teleNP program, veterans are offered services by CRH 20 neuropsychologists via telehealth to a patient’s local VAMC, larger health care clinic, CBOC, or via Veterans Video Connect to the home.
Referral pathways to the CRH 20 teleNP program differ across sites. For VISN 20 sites that do not have any in-house neuropsychology services, referrals are initiated by HCPs from any discipline. At 2 sites with in-house neuropsychology programs, CRH 20 teleNP referrals typically are forwarded from the inhouse service whenever the veteran prefers to be seen at an outlying clinic. All sites, including the CBOCs, are equipped fully for testing, and the HCP encounters veterans in a private office via video-based telehealth technology after a telehealth technician orients them to the space. The private office minimizes environmental disruptions and uses standardized technology to ensure valid results. A limited number of evaluations are offered at home (< 5% of the evaluations) if the veteran is unable to come to a VHA facility, has access to reliable internet, and a minimally distracting home setting.
In VISN 20, teleNP is a routine practice for delivering services to rural sites, most of which lack neuropsychologists. However, there is limited information about the extent to which the referral sources find the service useful. This quality improvement (QI) project aimed to better understand how well-established teleNP services were received by referral sources/stakeholders and how services could be improved. Prior to the advent of the CRH 20 teleNP program, staff had the option of referring for F2F evaluations in the local community (outside the VA) at some sites, an option that remains. This QI project examined staff perspectives on the usefulness of CRH 20 teleNP services compared with non-VA F2F services. We administered an anonymous, confidential survey examining these factors to VISN 20 staff within 4 VA health care systems.
METHODS
This QI project used a mixed quantitative and qualitative descriptive survey design to elicit feedback. The authors (3 neuropsychologists, 1 geropsychologist, and 1 research coordinator) developed the survey questions. The 13-question survey was voluntary, anonymous, and confidential, and respondents were given an opportunity to ask questions, with the first author serving as the point of contact.
The survey ascertained information about respondents and their work setting (ie, facility type, specific work setting and location, profession, and rurality of patients). First respondents were asked whether they have referred patients to neuropsychology services in the past year. Those who had not referred patients during the past year were asked about reasons for nonreferral with an option to provide an open-ended response. Respondents who did refer were asked how they refer for neuropsychology services and about the usefulness and timeliness of both teleNP and non-VA F2F services. Respondents were asked to respond with their preference for teleNP vs non-VA F2F with an open-ended prompt. Finally, respondents were invited to share any feedback for improvement regarding teleNP services.
A link to the survey, hosted on the VA Research Electronic Data Capture system, was emailed to facility and service line leaders at the 4 VISN 20 health care systems for distribution to the staff. All staff were included because in many of the facilities, particularly those that are highly rural with low staffing, it is not uncommon for technicians, nurses, and other support staff to assist with placing consults. In particular, VISN 20 nurses often have an optimal understanding of referral pathways to care for patients and are positioned to give and receive feedback about the utility of neuropsychological evaluations. The Research and Development Committee at the Boise VA Medical Center determined this project to be QI and exempt from institutional review board oversight. The VISN 20 employee labor relations HR supervisor approved this survey, with union awareness. Responses were anonymous.
Data were imported into Microsoft Excel and IBM SPSS Statistics for further analysis. Data were summarized using descriptive statistics, frequencies, and percentages. Nonparametric χ2 and Wilcoxon signed-rank tests were used to test for differences. An inductive approach to develop codes was used for the 3 open-ended questions. Two authors (CC, CEG) independently coded the responses and reviewed discrepancies. Final code applications were based on consensus.
RESULTS
The survey was deployed for 1 month between February 7, 2024, and June 15, 2024, at each of the 4 health care systems. Thirty-three staff members responded; of these, 1 person did not respond to an item on whether they referred for neuropsychology services. Eighteen of 33 respondents reported referring patients to teleNP or F2F neuropsychology services in the past year. Fourteen of the 33 respondents stated they did not refer; of these, 2 were unfamiliar with the teleNP service and 12 provided other reasons (eg, new to VA, not in their professional scope to order consults, did not have patients needing services).
The analysis focused on the 18 respondents who referred for neuropsychology services. Thirteen were within health care system A, and 5 were within health care system B (which had no nearby non-VA contracted neuropsychology services) and none were in the other 2 health care systems. Ten of 18 respondents (56%) stated they practiced primarily in a rural setting. Five respondents worked in a CBOC, 12 in a main VA facility, 9 in a primary care setting, 8 in a mental health setting, and 3 in other settings (eg, domiciliary). Participants could select > 1 setting. The 18 respondents who referred to neuropsychology services included 7 psychologists, 1 nurse, 2 social workers, 1 social services assistant, 4 nurse practitioners, 2 physicians, and 1 unknown HCP.
When asked to categorize the usefulness of services, more respondents characterized teleNP as very much so (1 on a 5-point scale) than F2F referrals (Figure). The mean (SD) of 1.5 (0.8) for teleNP usefulness fell between very much so and mostly and 1 respondent indicated not applicable. Similarly, the mean (SD) for non-VA F2F usefulness was 1.7 (0.9); 9 respondents rated this item as not applicable. A Wilcoxon signed-rank test of related samples indicated no significant differences between the pairs of ratings (Z = 1.50; P = .41).
Respondents with rural patients were more likely to refer them to teleNP services compared with respondents with nonrural patients (χ2 = 5.7; P = .02). However, ratings of teleNP usefulness did not significantly differ for those serving rural vs with nonrural patients (χ2 = 1.4; P = .49). Mean (SD) rating of teleNP usefulness was 1.3 (0.7) for the 9 rural subgroup respondents (between very much so and mostly) vs 1.8 (0.9) for the 8 nonrural subgroup respondents (between very much so and mostly). The mean (SD) rating for non-VA F2F usefulness was 1.8 (1.0) for the 4 rural subgroup respondents and 1.6 (0.8) for the 5 nonrural subgroup, between very much so and mostly for both groups.
Most respondents had no preference between teleNP or F2F. Notably, the responses underlying this group were multifaceted and corresponded to multiple codes (ie, access, preference for in-person services, technology, space and logistics, and service boundaries and requirements). According to 1 respondent, “the logistics of scheduling/room availability, technological challenges, and client behavioral issues that are likely to occur could possibly be more easily addressed via in-person sessions for some clients and providers.”
Six of 18 respondents preferred teleNP, citing timeliness, ease of access, and evaluation quality. One respondent noted that the “majority of my veterans live in extremely remote areas” and may need to take a plane for their visit. The 3 respondents who preferred in-person neuropsychology services cited veterans’ preference for in-person services.
Open-Ended Feedback
Thirteen respondents offered feedback on what is working well with teleNP services. Reasons mentioned were related to the service (ie, timeliness, access, quality) and the neuropsychologist (ie, communication and HCP skills). One respondent described the service and neuropsychologists positively, stating that they were “responsive, notes are readily available, clear assessments and recommendations, being available by [Microsoft] Teams/email.”
Ten respondents provided suggestions for improvement. Suggestions focused on expanding services, such as to “all veterans with cognitive/memory concerns that desire testing,” individuals with attention-deficit/hyperactivity disorder and co-occurring mental health concerns, and those in residential programs. Suggestions included hiring psychology technicians or more staff and providing education at local clinics.
DISCUSSION
This QI project examines VA staff perspectives on the usefulness of CRH 20 teleNP services and non-VA F2F services. While the small sample size limits generalizability, this preliminary study suggests that VA teleNP evaluations were similar to those conducted F2F in non-VA settings. While ratings of teleNP usefulness did not differ significantly for those serving rural vs nonrural veterans, respondents serving rural patients were more likely to refer patients to teleNP, suggesting that teleNP may increase access in rural settings, consistent with other studies.7,8,13 This article also presents qualitative suggestions for improving teleNP delivery within the VHA. This is the first known initiative to report on VHA staff satisfaction with a teleNP service and expands the limited literature to date on satisfaction with teleNP services. The findings provide initial support for continued use and, potentially, expansion of teleNP services within this CRH remote hub-and-spoke model.
Limitations
A significant limitation of the current work is the small sample size of survey respondents. In particular, while teleNP turnaround time was perceived as faster than non-VA F2F care, only 8 respondents reported on timeliness of F2F evaluation results, which renders it difficult to draw conclusions. Interestingly, not all respondents reported referring to neuropsychology services within the previous year; the most common reasons reflect the perception that referral to neuropsychology was outside of that staff member’s role or not clinically indicated.
One additional possible explanation for the absence of reporting on utility of teleNP specifically is that respondents did not track whether their patient was seen by teleNP or F2F services, based on how the referral process varies at each health care system. For example, in health care system C, a large number of referrals are forwarded to the service by local VA F2F neuropsychologists. This may speak to the seamlessness of the teleNP process, such that local staff and/or referring HCPs are unaware of the modality over which neuropsychology is being conducted. It is plausible that the reason behind this smaller response rate in health care systems B and C relates to how neuropsychology consults are processed at these local VAMCs. We suspect that in these settings, the HCPs referring for neuropsychological evaluations (eg, primary care, mental health) may be unaware that their referrals are being triaged to neuropsychologists in a different program (CRH 20 teleNP). Therefore, they would not necessarily know that they used teleNP and didn’t complete the survey.
The referral process for these 2 sites contrasts with the process for other VISN 20 sites where there is no local neuropsychology program triaging. In these settings, referrals from local HCPs come directly to teleNP; thus, it is more likely that these HCPs are aware of teleNP services. There were only 2 physicians who completed the survey, which may relate to their workload and a workflow where other staff have been increasingly requested to order the consults for the physician. This type of workflow results in an increase in the number of VHA staff involved in patient care. Ratings of usefulness were highest in health care system B, which does not have neuropsychology services at the facility or in the community; this may relate to elevated teleNP satisfaction ratings.
Further work may help identify which aspects of a teleNP service make it more useful than F2F care for this population or determine whether there were HCPor setting-specific factors that influenced the ratings (ie, preference for VA care or comparison of favorability ratings for the HCPs who conduct teleNP and F2F within the same system). The latter comparisons could not be drawn in the current systems due to the absence of HCPs who provide both teleNP and F2F modalities within VISN 20. Another consideration for future work would be to use a previously published/validated survey measure and piloting of questions with a naive sample before implementation.
CONCLUSIONS
This analysis provides initial support for feasibility and acceptability of teleNP as an alternative to traditional in-person neuropsychological evaluations. The small number of survey respondents may reflect the multiple pathways through which consults are forwarded to CRH 20, which includes both direct HCP referrals and forwarded consults from local neuropsychology services. CRH 20 has completed > 570 teleNP evaluations within 1 year, suggesting that lack of awareness may not be hindering veteran access to the service. Replication with a larger sample that is more broadly representative of key stakeholders in veteran care, identification of populations that would benefit most from teleNP services, and dissemination studies of the expansion of teleNP services are all important directions for future work. The robustness and longevity of the VISN 20 teleNP program, coupled with the preliminary positive findings from this project, demonstrate support for further assessment of the potential impact of telehealth on neuropsychological care within the VHA and show that barriers associated with access to health care services in remote settings may be mitigated through teleNP service delivery.
- US Department of Veterans Affairs, Office of Rural Health. Rural veterans. Updated March 10, 2025. Accessed July 7, 2025. https://www.ruralhealth.va.gov/aboutus/ruralvets.asp
- Braun M, Tupper D, Kaufmann P, et al. Neuropsychological assessment: a valuable tool in the diagnosis and management of neurological, neurodevelopmental, medical, and psychiatric disorders. Cogn Behav Neurol. 2011;24(3):107-114. doi:10.1097/wnn.0b013e3182351289
- Donders J. The incremental value of neuropsychological assessment: a critical review. Clin Neuropsychol. 2020;34(1):56-87. doi:10.1080/13854046.2019.1575471
- Williams MW, Rapport LJ, Hanks RA, et al. Incremental value of neuropsychological evaluations to computed tomography in predicting long-term outcomes after traumatic brain injury. Clin Neuropsychol. 2013;27(3):356-375. doi:10.1080/13854046.2013.765507
- Sieg E, Mai Q, Mosti C, Brook M. The utility of neuropsychological consultation in identifying medical inpatients with suspected cognitive impairment at risk for greater hospital utilization. Clin Neuropsychol. 2019;33(1):75-89. doi:10.1080/13854046.2018.1465124
- Vankirk KM, Horner MD, Turner TH, et al. CE hospital service utilization is reduced following neuropsychological evaluation in a sample of U.S. veterans. Clin Neuropsychol. 2013;27(5):750-761. doi:10.1080/13854046.2013.783122
- Appleman ER, O’Connor MK, Boucher SJ, et al. Teleneuropsychology clinic development and patient satisfaction. Clin Neuropsychol. 2021;35(4):819-837. doi:10.1080/13854046.2020.1871515
- Stelmokas J, Ratcliffe LN, Lengu K, et al. Evaluation of teleneuropsychology services in veterans during COVID-19. Psychol Serv. 2024;21(1):65-72. doi:10.1037/ser0000810
- Bilder R Postal KS, Barisa M, et al. Inter Organizational Practice Committee recommendations/guidance for teleneuropsychology in response to the COVID-19 pandemic. Arch Clin Neuropsychol. 2020;35(6):647-659. doi:10.1093/arclin/acaa046
- Brearly TW, Shura RD, Martindale SL, et al. Neuropsychological test administration by videoconference: a systematic review and meta-analysis. Neuropsychol Rev. 2017;27(2):174-186. doi:10.1007/s11065-017-9349-1
- Brown AD, Kelso W, Eratne D, et al. Investigating equivalence of in-person and telehealth-based neuropsychological assessment performance for individuals being investigated for younger onset dementia. Arch Clin Neuropsychol. 2024;39(5):594-607. doi:10.1093/arclin/acad108
- Chapman JE, Ponsford J, Bagot KL, et al. The use of videoconferencing in clinical neuropsychology practice: a mixed methods evaluation of neuropsychologists’ experiences and views. Aust Psychol. 2020;55(6):618-633. doi:10.1111/ap.12471
- Marra DE, Hamlet KM, Bauer RM, et al. Validity of teleneuropsychology for older adults in response to COVID-19: a systematic and critical review. Clin Neuropsychol. 2020;34:1411-1452. doi:10.1080/13854046.2020.1769192
- Hammers DB, Stolwyk R, Harder L, et al. A survey of international clinical teleneuropsychology service provision prior to COVID-19. Clin Neuropsychol. 2020;34(7-8):1267- 1283. doi:10.1080/13854046.2020.1810323
- Marra DE, Hoelzle JB, Davis JJ, et al. Initial changes in neuropsychologists’ clinical practice during the COVID-19 pandemic: a survey study. Clin Neuropsychol. 2020;34(7- 8):1251-1266. doi:10.1080/13854046.2020.1800098
- Parsons MW, Gardner MM, Sherman, JC et al. Feasibility and acceptance of direct-to-home teleneuropsychology services during the COVID-19 pandemic. J Int Neuropsychol Soc. 2022;28(2):210-215. doi:10.1017/s1355617721000436
- Rochette AD, Rahman-Filipiak A, Spencer RJ, et al. Teleneuropsychology practice survey during COVID-19 within the United States. Appl Neuropsychol Adult. 2022;29(6):1312- 1322. doi:10.1080/23279095.2021.1872576
- Messler AC, Hargrave DD, Trittschuh EH, et al. National survey of telehealth neuropsychology practices: current attitudes, practices, and relevance of tele-neuropsychology three years after the onset of COVID-19. Clin Neuropsychol. 2023;39:1017-1036. doi:10.1080/13854046.2023.2192422
- Rautman L, Sordahl JA. Veteran satisfaction with tele-neuropsychology services. Clin Neuropsychol. 2018;32:1453949. doi:10.1080/13854046.2018.1453949
- US Department of Veterans Affairs. Patient care services: clinical resource hubs. Updated March 20, 2024. Accessed August 4, 2025. https://www.patientcare .va.gov/primarycare/CRH.asp
- Burnett K, Stockdale SE, Yoon J, et al. The Clinical Resource Hub initiative: first-year implementation of the Veterans Health Administration regional telehealth contingency staffing program. Ambul Care Manage. 2023;46(3):228-239. doi:10.1097/JAC.0000000000000468
- US Department of Veterans Affairs, Office of Rural Health. Rural veterans. Updated March 10, 2025. Accessed July 7, 2025. https://www.ruralhealth.va.gov/aboutus/ruralvets.asp
- Braun M, Tupper D, Kaufmann P, et al. Neuropsychological assessment: a valuable tool in the diagnosis and management of neurological, neurodevelopmental, medical, and psychiatric disorders. Cogn Behav Neurol. 2011;24(3):107-114. doi:10.1097/wnn.0b013e3182351289
- Donders J. The incremental value of neuropsychological assessment: a critical review. Clin Neuropsychol. 2020;34(1):56-87. doi:10.1080/13854046.2019.1575471
- Williams MW, Rapport LJ, Hanks RA, et al. Incremental value of neuropsychological evaluations to computed tomography in predicting long-term outcomes after traumatic brain injury. Clin Neuropsychol. 2013;27(3):356-375. doi:10.1080/13854046.2013.765507
- Sieg E, Mai Q, Mosti C, Brook M. The utility of neuropsychological consultation in identifying medical inpatients with suspected cognitive impairment at risk for greater hospital utilization. Clin Neuropsychol. 2019;33(1):75-89. doi:10.1080/13854046.2018.1465124
- Vankirk KM, Horner MD, Turner TH, et al. CE hospital service utilization is reduced following neuropsychological evaluation in a sample of U.S. veterans. Clin Neuropsychol. 2013;27(5):750-761. doi:10.1080/13854046.2013.783122
- Appleman ER, O’Connor MK, Boucher SJ, et al. Teleneuropsychology clinic development and patient satisfaction. Clin Neuropsychol. 2021;35(4):819-837. doi:10.1080/13854046.2020.1871515
- Stelmokas J, Ratcliffe LN, Lengu K, et al. Evaluation of teleneuropsychology services in veterans during COVID-19. Psychol Serv. 2024;21(1):65-72. doi:10.1037/ser0000810
- Bilder R Postal KS, Barisa M, et al. Inter Organizational Practice Committee recommendations/guidance for teleneuropsychology in response to the COVID-19 pandemic. Arch Clin Neuropsychol. 2020;35(6):647-659. doi:10.1093/arclin/acaa046
- Brearly TW, Shura RD, Martindale SL, et al. Neuropsychological test administration by videoconference: a systematic review and meta-analysis. Neuropsychol Rev. 2017;27(2):174-186. doi:10.1007/s11065-017-9349-1
- Brown AD, Kelso W, Eratne D, et al. Investigating equivalence of in-person and telehealth-based neuropsychological assessment performance for individuals being investigated for younger onset dementia. Arch Clin Neuropsychol. 2024;39(5):594-607. doi:10.1093/arclin/acad108
- Chapman JE, Ponsford J, Bagot KL, et al. The use of videoconferencing in clinical neuropsychology practice: a mixed methods evaluation of neuropsychologists’ experiences and views. Aust Psychol. 2020;55(6):618-633. doi:10.1111/ap.12471
- Marra DE, Hamlet KM, Bauer RM, et al. Validity of teleneuropsychology for older adults in response to COVID-19: a systematic and critical review. Clin Neuropsychol. 2020;34:1411-1452. doi:10.1080/13854046.2020.1769192
- Hammers DB, Stolwyk R, Harder L, et al. A survey of international clinical teleneuropsychology service provision prior to COVID-19. Clin Neuropsychol. 2020;34(7-8):1267- 1283. doi:10.1080/13854046.2020.1810323
- Marra DE, Hoelzle JB, Davis JJ, et al. Initial changes in neuropsychologists’ clinical practice during the COVID-19 pandemic: a survey study. Clin Neuropsychol. 2020;34(7- 8):1251-1266. doi:10.1080/13854046.2020.1800098
- Parsons MW, Gardner MM, Sherman, JC et al. Feasibility and acceptance of direct-to-home teleneuropsychology services during the COVID-19 pandemic. J Int Neuropsychol Soc. 2022;28(2):210-215. doi:10.1017/s1355617721000436
- Rochette AD, Rahman-Filipiak A, Spencer RJ, et al. Teleneuropsychology practice survey during COVID-19 within the United States. Appl Neuropsychol Adult. 2022;29(6):1312- 1322. doi:10.1080/23279095.2021.1872576
- Messler AC, Hargrave DD, Trittschuh EH, et al. National survey of telehealth neuropsychology practices: current attitudes, practices, and relevance of tele-neuropsychology three years after the onset of COVID-19. Clin Neuropsychol. 2023;39:1017-1036. doi:10.1080/13854046.2023.2192422
- Rautman L, Sordahl JA. Veteran satisfaction with tele-neuropsychology services. Clin Neuropsychol. 2018;32:1453949. doi:10.1080/13854046.2018.1453949
- US Department of Veterans Affairs. Patient care services: clinical resource hubs. Updated March 20, 2024. Accessed August 4, 2025. https://www.patientcare .va.gov/primarycare/CRH.asp
- Burnett K, Stockdale SE, Yoon J, et al. The Clinical Resource Hub initiative: first-year implementation of the Veterans Health Administration regional telehealth contingency staffing program. Ambul Care Manage. 2023;46(3):228-239. doi:10.1097/JAC.0000000000000468
Staff Perspectives on the VISN 20 Tele-Neuropsychology Program
Staff Perspectives on the VISN 20 Tele-Neuropsychology Program
U.S. health care policy: What lies ahead?
The New Year brings new leadership in the United States, with President-elect Donald Trump taking office later this month. With a Republican-controlled Congress, party leaders have the opportunity to shape the nation’s policies around conservative ideals. This includes health care.
Since the Affordable Care Act (ACA) was passed in 2010, Republicans have vowed to repeal and replace it. This could be their opportunity.
However, “there is no clear coalescence around specific policy reforms that would replace the Affordable Care Act,” says Christine Eibner, PhD, a senior economist at Rand and a professor at the Pardee Rand Graduate School.
As a candidate, Trump did little to advance policy ideas around health care. Meanwhile, House Speaker Paul Ryan (R-Wis.) and others have, over the years, proposed reforms with which Trump may or may not agree.
“The Republicans now have a hard issue in their hands,” says Allison Hoffman, JD, professor of law at UCLA School of Law and an expert on health care law and policy. “It was hard before the Affordable Care Act, and it will be hard after. There is not an easy solution.”
By 2016, the ACA had expanded health coverage to 20 million people through Medicaid and private insurance on health care marketplaces. It extended the solvency of the Medicare Hospital Insurance Trust Fund. It accelerated the pace of delivery system and payment reform through creation of the Center for Medicare & Medicaid Innovation.
The law, however, has not been without its challenges.
“It was a strong achievement to get 20 million people insured, but it’s not clear that it bent the cost curve,” says Dr. Eibner. “There are high premiums on the individual market and still 31 million people without coverage. There is still opportunity to improve.”
Where we stand January 2017
Whether the Republicans can or will repeal the ACA in its entirety and improve it remains unknown. But, the experts say, the landmark law has left its mark on the American health care system.
“Everyone is complaining about the uncertainty created by the election, but we have been dealing with a highly uncertain environment for many years,” says Ron Greeno, MD, FCCP, MHM, senior advisor for medical affairs at TeamHealth, chair of the SHM Public Policy Committee, and SHM president-elect. “There will be changes, but things were going to change no matter the outcome of the election. It continues to require tolerance for change and tolerance for uncertainty.”
In an analysis for the Commonwealth Fund, Dr. Eibner investigated the economic implications of aspects of Trump’s plans as a candidate. Using a computer model that incorporates economic theory and data to simulate the effects of health policy changes, Dr. Eibner found that Trump’s plans (full repeal alone or repeal with tax deductions for health care premiums, Medicaid block grants, or selling health insurance across state lines) would increase the number of uninsured people by 16 million to 25 million, disproportionately impact low-income and sicker patients, expose individual market enrollees to higher out-of-pocket costs, and increase the federal deficit by $0.5 billion to $41 billion.1 The Congressional Budget Office (CBO) estimates full repeal could increase the federal deficit by $137 billion to $353 billion by 2025.2 Rep. Ryan’s plan, A Better Way, proposes providing people more control over their health care, giving tax credits instead of subsidies for premiums, capping the employer-sponsored health insurance tax exclusion, and expanding use of health savings accounts.3 However, Rep. Ryan’s plan “doesn’t reduce the cost of health care. It puts more onus on individuals, and their costs go up,” Ms. Hoffman says. “The weight of that will be more on people who have preexisting conditions.”
Joshua Lenchus, DO, RPh, FACP, SFHM, a member of SHM’s Public Policy Committee and hospitalist at the University of Miami/Jackson Memorial Hospital in Florida, is no fan of entitlement programs like Medicaid but says, “The safety-net hospital where I work would rather have people covered with something than nothing.”
Dr. Lenchus is optimistic that economic reforms under Trump will lead to more jobs, increasing the number of people covered by employer plans. “The economy drives health care reform,” he says. “He has to up his ante now and show people that he can stimulate job growth in this country so we don’t have this middle class that is continuously squeezed.”
Dr. Greeno and Ms. Hoffman, who is also a faculty associate at the UCLA Center for Health Policy Research and vice chair of the Insurance Law Section of the Association of American Law Schools, suggest hospitalists get involved as rules are being shaped and written.
“We want to help reform the delivery system, and we want it to be done right and to be done fairly. We want to have say in how our patients are treated,” Dr. Greeno says.
Key provisions: A delicate balance
Many people equate the ACA with the individual mandate, which requires nearly all Americans to purchase health insurance or pay a fine. The federal government provides subsidies to enrollees between 138% and 400% of the federal poverty level so their out-of-pocket costs never exceed a defined threshold even if premiums go up. These could be on the chopping block.
“The last bill Congress passed to repeal the Affordable Care Act, which Obama vetoed, repealed the individual mandate and subsidies for people to buy insurance,” Ms. Hoffman says. “If they do repeal it, private insurance through the exchanges will crumble.”
Mr. Trump’s tax deductions to offset premium costs are based on income, making them more generous for higher-income earners than low-income ones, Hoffman adds.
As a result, she says, people may choose high-deductible plans and face high out-of-pocket costs if they do seek care.
“It’s asking individuals to save by deciding how they’re going to ration care, where someone says they’re not going to go to the doctor today or fill a prescription drug they need,” Ms. Hoffman says.
Meanwhile, Mr. Trump has said he would like to keep the provision of the ACA that bans insurers from denying individuals with preexisting conditions. This, experts agree, may not be possible if other parts of the law are repealed and not replaced with similar protections for insurers.
“If you try to keep the rules about not including preexisting conditions and get rid of subsidies and the individual mandate, it just won’t work,” Ms. Hoffman says. “You end up with extraordinarily expensive health insurance.”
Rep. Ryan’s plan would prohibit insurers from denying patients with preexisting conditions but only if patients maintain continuous coverage, with a single open-enrollment period. He has promised to provide at least $25 billion in federal funding for state high-risk pools.
Prior to the passage of the ACA, 35 states offered high-risk pools to people excluded from the individual market. The Kaiser Family Foundation shows the net annual losses in these states averaged $5,510 per enrollee in 2011. Premiums ranged from 100% to 200% higher than non–high-risk group coverage. Government subsidies to cover losses amounted to $1 billion in each state.4
Meanwhile, both Mr. Trump and Rep. Ryan have proposed profound changes for Medicaid. Dr. Greeno calls this a “massive political challenge” unless they can provide an alternative way to cover people who currently rely on the federal-state entitlement, as well as those who gained coverage through ACA expansion. Currently, 70 million people are enrolled in Medicaid and the Children’s Health Insurance Program.5 Through Mr. Trump’s suggested block grants, states would receive a fixed amount of money to administer their program with increased flexibility. Rep. Ryan’s plan calls for enrollment caps that would distribute a dollar amount to each participant in the program with no limit on the number of enrollees. Either would be adjusted for inflation.
States could implement work requirements for beneficiaries or ask them to pay a small amount toward their premiums. Expansion states could also lower the Medicaid threshold below 138%.
Some states will struggle to provide for all their enrollees, Ms. Hoffman says, particularly since health spending generally outpaces inflation. Dr. Lenchus is more optimistic. “I believe states that didn’t expand Medicaid, one way or another, will figure out a way to deal with that population,” he says.
And … Medicare
The other entitlement program facing abrupt change is Medicare, typically considered the third rail of American politics.
“This is the hot political moment,” Ms. Hoffman says. “This is the point where the Republicans think they can tick off their wish list. For many Republicans, this kind of entitlement program is the opposite of what they believe in.”
Though Mr. Trump has said before he would not alter Medicare, he remained quiet on this point in the aftermath of the election. Repealing the ACA would affect Medicare by potentially reopening the Part D prescription drug doughnut hole and eliminating some of the savings provisions in the law. In fact, the CBO estimates Medicare’s direct spending would increase $802 billion between 2016 and 2025.1 Rep. Ryan has talked about privatizing Medicare by offering seniors who rely on it vouchers to apply toward private insurance.
“At the highest level, it’s moving Medicare from a defined benefit to a defined contribution program,” Ms. Hoffman says. “It shifts financial risk from the federal government onto beneficiaries. If Medicare spending continues to grow faster than the rest of the economy, Medicare beneficiaries will pay more and more.”
Seniors may also find themselves rationing or skimping on care.
Despite Rep. Ryan’s statements to the contrary, Medicare is not broken because of the ACA, Ms. Hoffman says. Its solvency has been prolonged, and though the reasons are not clear, Medicare spending has slowed since the passage of the ACA.6
MACRA launch
Another key factor in the health care policy landscape is MACRA, the Medicare Access and CHIP Reauthorization Act, which fundamentally shifts the way the government administrates and reimburses physicians for health care. MACRA begins in 2017. Dr. Greeno is concerned that changes to the ACA will impact the testing of payment models CMS is testing.
“There are hundreds of hospitals and thousands of physicians already invested in different models, so I don’t expect anybody has any desire to pull the rug from under physicians who are testing alternative payment models [APMs],” he says. “MACRA was passed on a strong bipartisan vote, and it created an APM track. Obviously, Congress intended APM models to continue to expand.”
Dr. Greeno says hospitalists are helping “shape these models,” working with the CMS and the Physician-Focused Payment Model Technical Advisory Committee (PTAC) “to ensure physicians participate in APMs and feel engaged rather than being a worker in a model someone else controls.”
On the campaign trail, Mr. Trump spoke of importing pharmaceuticals from overseas in an effort to control high prices. This policy is no longer part of his online plan. He also proposes allowing the sale of health insurance across state lines.
“It would be giving enrollees in states with stricter regulations the opportunity to circumvent to a looser state, which undermines the state with the stricter regulations,” Dr. Eibner says. “That would really create winners and losers. People who are healthy can buy a policy in a state with looser regulations, and their costs would likely fall. But someone sicker and older, it would be harder.”
Ms. Hoffman defines such a plan as a “race to the bottom.” Without well-established networks of physicians and hospitals, startup costs in new states are prohibitive, and many insurers may not wish to compete across state lines, she adds.
Repeal of the ACA could also limit some of the health benefits it required of plans on the individual market. For example, policymakers might be allowed to strip the contraceptive coverage regulation, which provides for free birth control.
“The reality is a lot of things changing in health care now were changing before the Affordable Care Act passed – PQRS, value-based purchasing, hospital-acquired infections,” Dr. Greeno says. “MACRA will continue the journey away from fee-for-service toward outcome-based models.”
At such a pivotal time, he strongly encourages hospitalists to join SHM if they are not already members and to get involved in SHM’s Grassroots Network.
“For a society of our age – young – and size, we’ve been tremendously impactful in helping with delivery system reform,” Dr. Greeno says. “I think it’s because we’re supporting change, not trying to stop it. We just want it to be intelligent change.”
He also is “convinced” hospitalists will be “critical to the redesign of the health care system. Since we are going to be taking care of the majority of hospitalized adult patients in hospitals, hospitalists want to have our say.”
Kelly April Tyrrell is a freelance writer in Madison, Wis.
References
1. Eibner C. Donald Trump’s health care reform proposals: Anticipated effects on insurance coverage, out-of-pocket costs, and the federal deficit. The Commonweath Fund website. Available at: http://www.commonwealthfund.org/publications/issue-briefs/2016/sep/trump-presidential-health-care-proposal. Accessed Nov. 17, 2016.
2. Budgetary and economic effects of repealing the Affordable Care Act. Congressional Budget Office website. Available at: https://www.cbo.gov/sites/default/files/114th-congress-2015-2016/reports/50252-Effects_of_ACA_Repeal.pdf. Accessed Nov. 15, 2016.
3. Our vision for a confident America. A Better Way website. Available at: http://abetterway.speaker.gov. Accessed Nov. 17, 2016.
4. Pollitz K. High-risk pools for uninsurable individuals. Kaiser Family Foundation website. Available at: http://kff.org/health-reform/issue-brief/high-risk-pools-for-uninsurable-individuals/. Accessed Nov. 17, 2016.
5. How accessible is individual health insurance for consumers in less-than-ideal health? Kaiser Family Foundation website. Available at: https://kaiserfamilyfoundation.files.wordpress.com/2013/01/how-accessible-is-individual-health-insurance-for-consumer-in-less-than-perfect-health-report.pdf. Accessed Nov. 17, 2016.
6. The Affordable Care Act and Medicare. The Commonwealth Fund website. Available at: http://www.commonwealthfund.org/publications/fund-reports/2015/jun/medicare-affordable-care-act Accessed Nov. 17, 2016.
The New Year brings new leadership in the United States, with President-elect Donald Trump taking office later this month. With a Republican-controlled Congress, party leaders have the opportunity to shape the nation’s policies around conservative ideals. This includes health care.
Since the Affordable Care Act (ACA) was passed in 2010, Republicans have vowed to repeal and replace it. This could be their opportunity.
However, “there is no clear coalescence around specific policy reforms that would replace the Affordable Care Act,” says Christine Eibner, PhD, a senior economist at Rand and a professor at the Pardee Rand Graduate School.
As a candidate, Trump did little to advance policy ideas around health care. Meanwhile, House Speaker Paul Ryan (R-Wis.) and others have, over the years, proposed reforms with which Trump may or may not agree.
“The Republicans now have a hard issue in their hands,” says Allison Hoffman, JD, professor of law at UCLA School of Law and an expert on health care law and policy. “It was hard before the Affordable Care Act, and it will be hard after. There is not an easy solution.”
By 2016, the ACA had expanded health coverage to 20 million people through Medicaid and private insurance on health care marketplaces. It extended the solvency of the Medicare Hospital Insurance Trust Fund. It accelerated the pace of delivery system and payment reform through creation of the Center for Medicare & Medicaid Innovation.
The law, however, has not been without its challenges.
“It was a strong achievement to get 20 million people insured, but it’s not clear that it bent the cost curve,” says Dr. Eibner. “There are high premiums on the individual market and still 31 million people without coverage. There is still opportunity to improve.”
Where we stand January 2017
Whether the Republicans can or will repeal the ACA in its entirety and improve it remains unknown. But, the experts say, the landmark law has left its mark on the American health care system.
“Everyone is complaining about the uncertainty created by the election, but we have been dealing with a highly uncertain environment for many years,” says Ron Greeno, MD, FCCP, MHM, senior advisor for medical affairs at TeamHealth, chair of the SHM Public Policy Committee, and SHM president-elect. “There will be changes, but things were going to change no matter the outcome of the election. It continues to require tolerance for change and tolerance for uncertainty.”
In an analysis for the Commonwealth Fund, Dr. Eibner investigated the economic implications of aspects of Trump’s plans as a candidate. Using a computer model that incorporates economic theory and data to simulate the effects of health policy changes, Dr. Eibner found that Trump’s plans (full repeal alone or repeal with tax deductions for health care premiums, Medicaid block grants, or selling health insurance across state lines) would increase the number of uninsured people by 16 million to 25 million, disproportionately impact low-income and sicker patients, expose individual market enrollees to higher out-of-pocket costs, and increase the federal deficit by $0.5 billion to $41 billion.1 The Congressional Budget Office (CBO) estimates full repeal could increase the federal deficit by $137 billion to $353 billion by 2025.2 Rep. Ryan’s plan, A Better Way, proposes providing people more control over their health care, giving tax credits instead of subsidies for premiums, capping the employer-sponsored health insurance tax exclusion, and expanding use of health savings accounts.3 However, Rep. Ryan’s plan “doesn’t reduce the cost of health care. It puts more onus on individuals, and their costs go up,” Ms. Hoffman says. “The weight of that will be more on people who have preexisting conditions.”
Joshua Lenchus, DO, RPh, FACP, SFHM, a member of SHM’s Public Policy Committee and hospitalist at the University of Miami/Jackson Memorial Hospital in Florida, is no fan of entitlement programs like Medicaid but says, “The safety-net hospital where I work would rather have people covered with something than nothing.”
Dr. Lenchus is optimistic that economic reforms under Trump will lead to more jobs, increasing the number of people covered by employer plans. “The economy drives health care reform,” he says. “He has to up his ante now and show people that he can stimulate job growth in this country so we don’t have this middle class that is continuously squeezed.”
Dr. Greeno and Ms. Hoffman, who is also a faculty associate at the UCLA Center for Health Policy Research and vice chair of the Insurance Law Section of the Association of American Law Schools, suggest hospitalists get involved as rules are being shaped and written.
“We want to help reform the delivery system, and we want it to be done right and to be done fairly. We want to have say in how our patients are treated,” Dr. Greeno says.
Key provisions: A delicate balance
Many people equate the ACA with the individual mandate, which requires nearly all Americans to purchase health insurance or pay a fine. The federal government provides subsidies to enrollees between 138% and 400% of the federal poverty level so their out-of-pocket costs never exceed a defined threshold even if premiums go up. These could be on the chopping block.
“The last bill Congress passed to repeal the Affordable Care Act, which Obama vetoed, repealed the individual mandate and subsidies for people to buy insurance,” Ms. Hoffman says. “If they do repeal it, private insurance through the exchanges will crumble.”
Mr. Trump’s tax deductions to offset premium costs are based on income, making them more generous for higher-income earners than low-income ones, Hoffman adds.
As a result, she says, people may choose high-deductible plans and face high out-of-pocket costs if they do seek care.
“It’s asking individuals to save by deciding how they’re going to ration care, where someone says they’re not going to go to the doctor today or fill a prescription drug they need,” Ms. Hoffman says.
Meanwhile, Mr. Trump has said he would like to keep the provision of the ACA that bans insurers from denying individuals with preexisting conditions. This, experts agree, may not be possible if other parts of the law are repealed and not replaced with similar protections for insurers.
“If you try to keep the rules about not including preexisting conditions and get rid of subsidies and the individual mandate, it just won’t work,” Ms. Hoffman says. “You end up with extraordinarily expensive health insurance.”
Rep. Ryan’s plan would prohibit insurers from denying patients with preexisting conditions but only if patients maintain continuous coverage, with a single open-enrollment period. He has promised to provide at least $25 billion in federal funding for state high-risk pools.
Prior to the passage of the ACA, 35 states offered high-risk pools to people excluded from the individual market. The Kaiser Family Foundation shows the net annual losses in these states averaged $5,510 per enrollee in 2011. Premiums ranged from 100% to 200% higher than non–high-risk group coverage. Government subsidies to cover losses amounted to $1 billion in each state.4
Meanwhile, both Mr. Trump and Rep. Ryan have proposed profound changes for Medicaid. Dr. Greeno calls this a “massive political challenge” unless they can provide an alternative way to cover people who currently rely on the federal-state entitlement, as well as those who gained coverage through ACA expansion. Currently, 70 million people are enrolled in Medicaid and the Children’s Health Insurance Program.5 Through Mr. Trump’s suggested block grants, states would receive a fixed amount of money to administer their program with increased flexibility. Rep. Ryan’s plan calls for enrollment caps that would distribute a dollar amount to each participant in the program with no limit on the number of enrollees. Either would be adjusted for inflation.
States could implement work requirements for beneficiaries or ask them to pay a small amount toward their premiums. Expansion states could also lower the Medicaid threshold below 138%.
Some states will struggle to provide for all their enrollees, Ms. Hoffman says, particularly since health spending generally outpaces inflation. Dr. Lenchus is more optimistic. “I believe states that didn’t expand Medicaid, one way or another, will figure out a way to deal with that population,” he says.
And … Medicare
The other entitlement program facing abrupt change is Medicare, typically considered the third rail of American politics.
“This is the hot political moment,” Ms. Hoffman says. “This is the point where the Republicans think they can tick off their wish list. For many Republicans, this kind of entitlement program is the opposite of what they believe in.”
Though Mr. Trump has said before he would not alter Medicare, he remained quiet on this point in the aftermath of the election. Repealing the ACA would affect Medicare by potentially reopening the Part D prescription drug doughnut hole and eliminating some of the savings provisions in the law. In fact, the CBO estimates Medicare’s direct spending would increase $802 billion between 2016 and 2025.1 Rep. Ryan has talked about privatizing Medicare by offering seniors who rely on it vouchers to apply toward private insurance.
“At the highest level, it’s moving Medicare from a defined benefit to a defined contribution program,” Ms. Hoffman says. “It shifts financial risk from the federal government onto beneficiaries. If Medicare spending continues to grow faster than the rest of the economy, Medicare beneficiaries will pay more and more.”
Seniors may also find themselves rationing or skimping on care.
Despite Rep. Ryan’s statements to the contrary, Medicare is not broken because of the ACA, Ms. Hoffman says. Its solvency has been prolonged, and though the reasons are not clear, Medicare spending has slowed since the passage of the ACA.6
MACRA launch
Another key factor in the health care policy landscape is MACRA, the Medicare Access and CHIP Reauthorization Act, which fundamentally shifts the way the government administrates and reimburses physicians for health care. MACRA begins in 2017. Dr. Greeno is concerned that changes to the ACA will impact the testing of payment models CMS is testing.
“There are hundreds of hospitals and thousands of physicians already invested in different models, so I don’t expect anybody has any desire to pull the rug from under physicians who are testing alternative payment models [APMs],” he says. “MACRA was passed on a strong bipartisan vote, and it created an APM track. Obviously, Congress intended APM models to continue to expand.”
Dr. Greeno says hospitalists are helping “shape these models,” working with the CMS and the Physician-Focused Payment Model Technical Advisory Committee (PTAC) “to ensure physicians participate in APMs and feel engaged rather than being a worker in a model someone else controls.”
On the campaign trail, Mr. Trump spoke of importing pharmaceuticals from overseas in an effort to control high prices. This policy is no longer part of his online plan. He also proposes allowing the sale of health insurance across state lines.
“It would be giving enrollees in states with stricter regulations the opportunity to circumvent to a looser state, which undermines the state with the stricter regulations,” Dr. Eibner says. “That would really create winners and losers. People who are healthy can buy a policy in a state with looser regulations, and their costs would likely fall. But someone sicker and older, it would be harder.”
Ms. Hoffman defines such a plan as a “race to the bottom.” Without well-established networks of physicians and hospitals, startup costs in new states are prohibitive, and many insurers may not wish to compete across state lines, she adds.
Repeal of the ACA could also limit some of the health benefits it required of plans on the individual market. For example, policymakers might be allowed to strip the contraceptive coverage regulation, which provides for free birth control.
“The reality is a lot of things changing in health care now were changing before the Affordable Care Act passed – PQRS, value-based purchasing, hospital-acquired infections,” Dr. Greeno says. “MACRA will continue the journey away from fee-for-service toward outcome-based models.”
At such a pivotal time, he strongly encourages hospitalists to join SHM if they are not already members and to get involved in SHM’s Grassroots Network.
“For a society of our age – young – and size, we’ve been tremendously impactful in helping with delivery system reform,” Dr. Greeno says. “I think it’s because we’re supporting change, not trying to stop it. We just want it to be intelligent change.”
He also is “convinced” hospitalists will be “critical to the redesign of the health care system. Since we are going to be taking care of the majority of hospitalized adult patients in hospitals, hospitalists want to have our say.”
Kelly April Tyrrell is a freelance writer in Madison, Wis.
References
1. Eibner C. Donald Trump’s health care reform proposals: Anticipated effects on insurance coverage, out-of-pocket costs, and the federal deficit. The Commonweath Fund website. Available at: http://www.commonwealthfund.org/publications/issue-briefs/2016/sep/trump-presidential-health-care-proposal. Accessed Nov. 17, 2016.
2. Budgetary and economic effects of repealing the Affordable Care Act. Congressional Budget Office website. Available at: https://www.cbo.gov/sites/default/files/114th-congress-2015-2016/reports/50252-Effects_of_ACA_Repeal.pdf. Accessed Nov. 15, 2016.
3. Our vision for a confident America. A Better Way website. Available at: http://abetterway.speaker.gov. Accessed Nov. 17, 2016.
4. Pollitz K. High-risk pools for uninsurable individuals. Kaiser Family Foundation website. Available at: http://kff.org/health-reform/issue-brief/high-risk-pools-for-uninsurable-individuals/. Accessed Nov. 17, 2016.
5. How accessible is individual health insurance for consumers in less-than-ideal health? Kaiser Family Foundation website. Available at: https://kaiserfamilyfoundation.files.wordpress.com/2013/01/how-accessible-is-individual-health-insurance-for-consumer-in-less-than-perfect-health-report.pdf. Accessed Nov. 17, 2016.
6. The Affordable Care Act and Medicare. The Commonwealth Fund website. Available at: http://www.commonwealthfund.org/publications/fund-reports/2015/jun/medicare-affordable-care-act Accessed Nov. 17, 2016.
The New Year brings new leadership in the United States, with President-elect Donald Trump taking office later this month. With a Republican-controlled Congress, party leaders have the opportunity to shape the nation’s policies around conservative ideals. This includes health care.
Since the Affordable Care Act (ACA) was passed in 2010, Republicans have vowed to repeal and replace it. This could be their opportunity.
However, “there is no clear coalescence around specific policy reforms that would replace the Affordable Care Act,” says Christine Eibner, PhD, a senior economist at Rand and a professor at the Pardee Rand Graduate School.
As a candidate, Trump did little to advance policy ideas around health care. Meanwhile, House Speaker Paul Ryan (R-Wis.) and others have, over the years, proposed reforms with which Trump may or may not agree.
“The Republicans now have a hard issue in their hands,” says Allison Hoffman, JD, professor of law at UCLA School of Law and an expert on health care law and policy. “It was hard before the Affordable Care Act, and it will be hard after. There is not an easy solution.”
By 2016, the ACA had expanded health coverage to 20 million people through Medicaid and private insurance on health care marketplaces. It extended the solvency of the Medicare Hospital Insurance Trust Fund. It accelerated the pace of delivery system and payment reform through creation of the Center for Medicare & Medicaid Innovation.
The law, however, has not been without its challenges.
“It was a strong achievement to get 20 million people insured, but it’s not clear that it bent the cost curve,” says Dr. Eibner. “There are high premiums on the individual market and still 31 million people without coverage. There is still opportunity to improve.”
Where we stand January 2017
Whether the Republicans can or will repeal the ACA in its entirety and improve it remains unknown. But, the experts say, the landmark law has left its mark on the American health care system.
“Everyone is complaining about the uncertainty created by the election, but we have been dealing with a highly uncertain environment for many years,” says Ron Greeno, MD, FCCP, MHM, senior advisor for medical affairs at TeamHealth, chair of the SHM Public Policy Committee, and SHM president-elect. “There will be changes, but things were going to change no matter the outcome of the election. It continues to require tolerance for change and tolerance for uncertainty.”
In an analysis for the Commonwealth Fund, Dr. Eibner investigated the economic implications of aspects of Trump’s plans as a candidate. Using a computer model that incorporates economic theory and data to simulate the effects of health policy changes, Dr. Eibner found that Trump’s plans (full repeal alone or repeal with tax deductions for health care premiums, Medicaid block grants, or selling health insurance across state lines) would increase the number of uninsured people by 16 million to 25 million, disproportionately impact low-income and sicker patients, expose individual market enrollees to higher out-of-pocket costs, and increase the federal deficit by $0.5 billion to $41 billion.1 The Congressional Budget Office (CBO) estimates full repeal could increase the federal deficit by $137 billion to $353 billion by 2025.2 Rep. Ryan’s plan, A Better Way, proposes providing people more control over their health care, giving tax credits instead of subsidies for premiums, capping the employer-sponsored health insurance tax exclusion, and expanding use of health savings accounts.3 However, Rep. Ryan’s plan “doesn’t reduce the cost of health care. It puts more onus on individuals, and their costs go up,” Ms. Hoffman says. “The weight of that will be more on people who have preexisting conditions.”
Joshua Lenchus, DO, RPh, FACP, SFHM, a member of SHM’s Public Policy Committee and hospitalist at the University of Miami/Jackson Memorial Hospital in Florida, is no fan of entitlement programs like Medicaid but says, “The safety-net hospital where I work would rather have people covered with something than nothing.”
Dr. Lenchus is optimistic that economic reforms under Trump will lead to more jobs, increasing the number of people covered by employer plans. “The economy drives health care reform,” he says. “He has to up his ante now and show people that he can stimulate job growth in this country so we don’t have this middle class that is continuously squeezed.”
Dr. Greeno and Ms. Hoffman, who is also a faculty associate at the UCLA Center for Health Policy Research and vice chair of the Insurance Law Section of the Association of American Law Schools, suggest hospitalists get involved as rules are being shaped and written.
“We want to help reform the delivery system, and we want it to be done right and to be done fairly. We want to have say in how our patients are treated,” Dr. Greeno says.
Key provisions: A delicate balance
Many people equate the ACA with the individual mandate, which requires nearly all Americans to purchase health insurance or pay a fine. The federal government provides subsidies to enrollees between 138% and 400% of the federal poverty level so their out-of-pocket costs never exceed a defined threshold even if premiums go up. These could be on the chopping block.
“The last bill Congress passed to repeal the Affordable Care Act, which Obama vetoed, repealed the individual mandate and subsidies for people to buy insurance,” Ms. Hoffman says. “If they do repeal it, private insurance through the exchanges will crumble.”
Mr. Trump’s tax deductions to offset premium costs are based on income, making them more generous for higher-income earners than low-income ones, Hoffman adds.
As a result, she says, people may choose high-deductible plans and face high out-of-pocket costs if they do seek care.
“It’s asking individuals to save by deciding how they’re going to ration care, where someone says they’re not going to go to the doctor today or fill a prescription drug they need,” Ms. Hoffman says.
Meanwhile, Mr. Trump has said he would like to keep the provision of the ACA that bans insurers from denying individuals with preexisting conditions. This, experts agree, may not be possible if other parts of the law are repealed and not replaced with similar protections for insurers.
“If you try to keep the rules about not including preexisting conditions and get rid of subsidies and the individual mandate, it just won’t work,” Ms. Hoffman says. “You end up with extraordinarily expensive health insurance.”
Rep. Ryan’s plan would prohibit insurers from denying patients with preexisting conditions but only if patients maintain continuous coverage, with a single open-enrollment period. He has promised to provide at least $25 billion in federal funding for state high-risk pools.
Prior to the passage of the ACA, 35 states offered high-risk pools to people excluded from the individual market. The Kaiser Family Foundation shows the net annual losses in these states averaged $5,510 per enrollee in 2011. Premiums ranged from 100% to 200% higher than non–high-risk group coverage. Government subsidies to cover losses amounted to $1 billion in each state.4
Meanwhile, both Mr. Trump and Rep. Ryan have proposed profound changes for Medicaid. Dr. Greeno calls this a “massive political challenge” unless they can provide an alternative way to cover people who currently rely on the federal-state entitlement, as well as those who gained coverage through ACA expansion. Currently, 70 million people are enrolled in Medicaid and the Children’s Health Insurance Program.5 Through Mr. Trump’s suggested block grants, states would receive a fixed amount of money to administer their program with increased flexibility. Rep. Ryan’s plan calls for enrollment caps that would distribute a dollar amount to each participant in the program with no limit on the number of enrollees. Either would be adjusted for inflation.
States could implement work requirements for beneficiaries or ask them to pay a small amount toward their premiums. Expansion states could also lower the Medicaid threshold below 138%.
Some states will struggle to provide for all their enrollees, Ms. Hoffman says, particularly since health spending generally outpaces inflation. Dr. Lenchus is more optimistic. “I believe states that didn’t expand Medicaid, one way or another, will figure out a way to deal with that population,” he says.
And … Medicare
The other entitlement program facing abrupt change is Medicare, typically considered the third rail of American politics.
“This is the hot political moment,” Ms. Hoffman says. “This is the point where the Republicans think they can tick off their wish list. For many Republicans, this kind of entitlement program is the opposite of what they believe in.”
Though Mr. Trump has said before he would not alter Medicare, he remained quiet on this point in the aftermath of the election. Repealing the ACA would affect Medicare by potentially reopening the Part D prescription drug doughnut hole and eliminating some of the savings provisions in the law. In fact, the CBO estimates Medicare’s direct spending would increase $802 billion between 2016 and 2025.1 Rep. Ryan has talked about privatizing Medicare by offering seniors who rely on it vouchers to apply toward private insurance.
“At the highest level, it’s moving Medicare from a defined benefit to a defined contribution program,” Ms. Hoffman says. “It shifts financial risk from the federal government onto beneficiaries. If Medicare spending continues to grow faster than the rest of the economy, Medicare beneficiaries will pay more and more.”
Seniors may also find themselves rationing or skimping on care.
Despite Rep. Ryan’s statements to the contrary, Medicare is not broken because of the ACA, Ms. Hoffman says. Its solvency has been prolonged, and though the reasons are not clear, Medicare spending has slowed since the passage of the ACA.6
MACRA launch
Another key factor in the health care policy landscape is MACRA, the Medicare Access and CHIP Reauthorization Act, which fundamentally shifts the way the government administrates and reimburses physicians for health care. MACRA begins in 2017. Dr. Greeno is concerned that changes to the ACA will impact the testing of payment models CMS is testing.
“There are hundreds of hospitals and thousands of physicians already invested in different models, so I don’t expect anybody has any desire to pull the rug from under physicians who are testing alternative payment models [APMs],” he says. “MACRA was passed on a strong bipartisan vote, and it created an APM track. Obviously, Congress intended APM models to continue to expand.”
Dr. Greeno says hospitalists are helping “shape these models,” working with the CMS and the Physician-Focused Payment Model Technical Advisory Committee (PTAC) “to ensure physicians participate in APMs and feel engaged rather than being a worker in a model someone else controls.”
On the campaign trail, Mr. Trump spoke of importing pharmaceuticals from overseas in an effort to control high prices. This policy is no longer part of his online plan. He also proposes allowing the sale of health insurance across state lines.
“It would be giving enrollees in states with stricter regulations the opportunity to circumvent to a looser state, which undermines the state with the stricter regulations,” Dr. Eibner says. “That would really create winners and losers. People who are healthy can buy a policy in a state with looser regulations, and their costs would likely fall. But someone sicker and older, it would be harder.”
Ms. Hoffman defines such a plan as a “race to the bottom.” Without well-established networks of physicians and hospitals, startup costs in new states are prohibitive, and many insurers may not wish to compete across state lines, she adds.
Repeal of the ACA could also limit some of the health benefits it required of plans on the individual market. For example, policymakers might be allowed to strip the contraceptive coverage regulation, which provides for free birth control.
“The reality is a lot of things changing in health care now were changing before the Affordable Care Act passed – PQRS, value-based purchasing, hospital-acquired infections,” Dr. Greeno says. “MACRA will continue the journey away from fee-for-service toward outcome-based models.”
At such a pivotal time, he strongly encourages hospitalists to join SHM if they are not already members and to get involved in SHM’s Grassroots Network.
“For a society of our age – young – and size, we’ve been tremendously impactful in helping with delivery system reform,” Dr. Greeno says. “I think it’s because we’re supporting change, not trying to stop it. We just want it to be intelligent change.”
He also is “convinced” hospitalists will be “critical to the redesign of the health care system. Since we are going to be taking care of the majority of hospitalized adult patients in hospitals, hospitalists want to have our say.”
Kelly April Tyrrell is a freelance writer in Madison, Wis.
References
1. Eibner C. Donald Trump’s health care reform proposals: Anticipated effects on insurance coverage, out-of-pocket costs, and the federal deficit. The Commonweath Fund website. Available at: http://www.commonwealthfund.org/publications/issue-briefs/2016/sep/trump-presidential-health-care-proposal. Accessed Nov. 17, 2016.
2. Budgetary and economic effects of repealing the Affordable Care Act. Congressional Budget Office website. Available at: https://www.cbo.gov/sites/default/files/114th-congress-2015-2016/reports/50252-Effects_of_ACA_Repeal.pdf. Accessed Nov. 15, 2016.
3. Our vision for a confident America. A Better Way website. Available at: http://abetterway.speaker.gov. Accessed Nov. 17, 2016.
4. Pollitz K. High-risk pools for uninsurable individuals. Kaiser Family Foundation website. Available at: http://kff.org/health-reform/issue-brief/high-risk-pools-for-uninsurable-individuals/. Accessed Nov. 17, 2016.
5. How accessible is individual health insurance for consumers in less-than-ideal health? Kaiser Family Foundation website. Available at: https://kaiserfamilyfoundation.files.wordpress.com/2013/01/how-accessible-is-individual-health-insurance-for-consumer-in-less-than-perfect-health-report.pdf. Accessed Nov. 17, 2016.
6. The Affordable Care Act and Medicare. The Commonwealth Fund website. Available at: http://www.commonwealthfund.org/publications/fund-reports/2015/jun/medicare-affordable-care-act Accessed Nov. 17, 2016.
Theranos Receives Biggest Blow as CMS Revokes Certificate for Government Payments
Theranos Inc founder and CEO Elizabeth Holmes, once touted as the Steve Jobs of biotech for her company's innovative blood-testing technology, has been barred by a U.S. regulator from owning or operating a lab for at least two years.
Dealing the biggest blow yet to the privately held company, the Centers for Medicare & Medicaid Services revoked a key certificate for its California lab and terminated the facility's approval to receive government payments.
Medicare is the government's medical insurance program for the elderly, while Medicaid is for the poor.
The sanctions, which also include an unspecified monetary penalty, come six months after the regulator sent a scathing letter to the company, saying its practices were jeopardizing patient health and safety.
Theranos said late on Thursday that it would continue to service its customers through its Arizona lab.
The company, once valued at $9 billion, was founded by Holmes in 2003 to develop an innovative blood testing device that would give quicker results using just one drop of blood.
However, its fortunes waned after the Wall Street Journal published a series of articles starting in October last year that suggested the devices were flawed and inaccurate.
Forbes magazine said last month that the company's value had fallen to about $800 million, while Holmes' own net worth had shrunk to zero from about $4.5 billion - a figure the magazine had said had made her the richest self-made woman in America.
"Everyone wanted her to succeed," Steve Brozak, president of WBB Securities, told Reuters, noting that the basic blood diagnostics sector has not had a significant advance in technology in 90 years.
Walgreens Boots Alliance terminated its relationship with the company last month and closed operations at all 40 Theranos Wellness Centers at its drug stores in Arizona.
Theranos is also facing a class action lawsuit filed in May accusing it of endangering customer health through "massive failures" that misrepresented test results.
The Palo Alto, California-based company is also being investigated by other federal and state agencies, including the U.S. Securities and Exchange Commission and the State Department of Health in Arizona.
Theranos Inc founder and CEO Elizabeth Holmes, once touted as the Steve Jobs of biotech for her company's innovative blood-testing technology, has been barred by a U.S. regulator from owning or operating a lab for at least two years.
Dealing the biggest blow yet to the privately held company, the Centers for Medicare & Medicaid Services revoked a key certificate for its California lab and terminated the facility's approval to receive government payments.
Medicare is the government's medical insurance program for the elderly, while Medicaid is for the poor.
The sanctions, which also include an unspecified monetary penalty, come six months after the regulator sent a scathing letter to the company, saying its practices were jeopardizing patient health and safety.
Theranos said late on Thursday that it would continue to service its customers through its Arizona lab.
The company, once valued at $9 billion, was founded by Holmes in 2003 to develop an innovative blood testing device that would give quicker results using just one drop of blood.
However, its fortunes waned after the Wall Street Journal published a series of articles starting in October last year that suggested the devices were flawed and inaccurate.
Forbes magazine said last month that the company's value had fallen to about $800 million, while Holmes' own net worth had shrunk to zero from about $4.5 billion - a figure the magazine had said had made her the richest self-made woman in America.
"Everyone wanted her to succeed," Steve Brozak, president of WBB Securities, told Reuters, noting that the basic blood diagnostics sector has not had a significant advance in technology in 90 years.
Walgreens Boots Alliance terminated its relationship with the company last month and closed operations at all 40 Theranos Wellness Centers at its drug stores in Arizona.
Theranos is also facing a class action lawsuit filed in May accusing it of endangering customer health through "massive failures" that misrepresented test results.
The Palo Alto, California-based company is also being investigated by other federal and state agencies, including the U.S. Securities and Exchange Commission and the State Department of Health in Arizona.
Theranos Inc founder and CEO Elizabeth Holmes, once touted as the Steve Jobs of biotech for her company's innovative blood-testing technology, has been barred by a U.S. regulator from owning or operating a lab for at least two years.
Dealing the biggest blow yet to the privately held company, the Centers for Medicare & Medicaid Services revoked a key certificate for its California lab and terminated the facility's approval to receive government payments.
Medicare is the government's medical insurance program for the elderly, while Medicaid is for the poor.
The sanctions, which also include an unspecified monetary penalty, come six months after the regulator sent a scathing letter to the company, saying its practices were jeopardizing patient health and safety.
Theranos said late on Thursday that it would continue to service its customers through its Arizona lab.
The company, once valued at $9 billion, was founded by Holmes in 2003 to develop an innovative blood testing device that would give quicker results using just one drop of blood.
However, its fortunes waned after the Wall Street Journal published a series of articles starting in October last year that suggested the devices were flawed and inaccurate.
Forbes magazine said last month that the company's value had fallen to about $800 million, while Holmes' own net worth had shrunk to zero from about $4.5 billion - a figure the magazine had said had made her the richest self-made woman in America.
"Everyone wanted her to succeed," Steve Brozak, president of WBB Securities, told Reuters, noting that the basic blood diagnostics sector has not had a significant advance in technology in 90 years.
Walgreens Boots Alliance terminated its relationship with the company last month and closed operations at all 40 Theranos Wellness Centers at its drug stores in Arizona.
Theranos is also facing a class action lawsuit filed in May accusing it of endangering customer health through "massive failures" that misrepresented test results.
The Palo Alto, California-based company is also being investigated by other federal and state agencies, including the U.S. Securities and Exchange Commission and the State Department of Health in Arizona.
When Introducing Innovations, Context Matters
“We are missing an important opportunity to learn from what is going on in health systems every day that could tell us how to make healthcare better and cheaper,” says Dr. Fisher, lead author of a January 2016 JAMA “Viewpoint” called “Implementation Science: A Potential Catalyst for Delivery System Reform.” “That’s the argument for the the field of implementation science.”
Implementation science studies ways to promote the integration of research findings and evidence into the healthcare system. Dr. Fisher says that integration is influenced by multiple factors: the characteristic of the innovation itself, the organizational setting, and the policy or community environment within which that organization is working. Context matters.
“We tend to think about adopting innovations like a new blood pressure medication or a new device,” Dr. Fisher says. “Those decisions rest almost entirely on the shoulders of physicians, so adoption requires thinking about the attributes of biomedical innovations and how physicians think.”
With care delivery innovations—for example, how to provide optimal care for people with heart failure across home, hospital, and nursing home—those are often developed with clinical input but by people who are fundamentally managers.
“It’s a more complex set of actors,” he says, “so you have to think about those decision makers if you’re going to get the best evidence-based practice into their setting.”
A third category of innovation focuses on individual behavior change, where the decision makers are the clinician and the patient and family. “You’ve got to persuade the patient the innovation is worth doing, so different factors may influence the successful adoptions of those interventions,” Dr. Fisher says.
Reference
1. Fisher ES, Shortell SM, Savitz LA. Implementation science: a potential catalyst for delivery system reform. JAMA. 2016;315(4):339-340. doi:10.1001/jama.2015.17949.
“We are missing an important opportunity to learn from what is going on in health systems every day that could tell us how to make healthcare better and cheaper,” says Dr. Fisher, lead author of a January 2016 JAMA “Viewpoint” called “Implementation Science: A Potential Catalyst for Delivery System Reform.” “That’s the argument for the the field of implementation science.”
Implementation science studies ways to promote the integration of research findings and evidence into the healthcare system. Dr. Fisher says that integration is influenced by multiple factors: the characteristic of the innovation itself, the organizational setting, and the policy or community environment within which that organization is working. Context matters.
“We tend to think about adopting innovations like a new blood pressure medication or a new device,” Dr. Fisher says. “Those decisions rest almost entirely on the shoulders of physicians, so adoption requires thinking about the attributes of biomedical innovations and how physicians think.”
With care delivery innovations—for example, how to provide optimal care for people with heart failure across home, hospital, and nursing home—those are often developed with clinical input but by people who are fundamentally managers.
“It’s a more complex set of actors,” he says, “so you have to think about those decision makers if you’re going to get the best evidence-based practice into their setting.”
A third category of innovation focuses on individual behavior change, where the decision makers are the clinician and the patient and family. “You’ve got to persuade the patient the innovation is worth doing, so different factors may influence the successful adoptions of those interventions,” Dr. Fisher says.
Reference
1. Fisher ES, Shortell SM, Savitz LA. Implementation science: a potential catalyst for delivery system reform. JAMA. 2016;315(4):339-340. doi:10.1001/jama.2015.17949.
“We are missing an important opportunity to learn from what is going on in health systems every day that could tell us how to make healthcare better and cheaper,” says Dr. Fisher, lead author of a January 2016 JAMA “Viewpoint” called “Implementation Science: A Potential Catalyst for Delivery System Reform.” “That’s the argument for the the field of implementation science.”
Implementation science studies ways to promote the integration of research findings and evidence into the healthcare system. Dr. Fisher says that integration is influenced by multiple factors: the characteristic of the innovation itself, the organizational setting, and the policy or community environment within which that organization is working. Context matters.
“We tend to think about adopting innovations like a new blood pressure medication or a new device,” Dr. Fisher says. “Those decisions rest almost entirely on the shoulders of physicians, so adoption requires thinking about the attributes of biomedical innovations and how physicians think.”
With care delivery innovations—for example, how to provide optimal care for people with heart failure across home, hospital, and nursing home—those are often developed with clinical input but by people who are fundamentally managers.
“It’s a more complex set of actors,” he says, “so you have to think about those decision makers if you’re going to get the best evidence-based practice into their setting.”
A third category of innovation focuses on individual behavior change, where the decision makers are the clinician and the patient and family. “You’ve got to persuade the patient the innovation is worth doing, so different factors may influence the successful adoptions of those interventions,” Dr. Fisher says.
Reference
1. Fisher ES, Shortell SM, Savitz LA. Implementation science: a potential catalyst for delivery system reform. JAMA. 2016;315(4):339-340. doi:10.1001/jama.2015.17949.
LISTEN NOW: UCSF's Christopher Moriates, MD, discusses waste-reduction efforts in hospitals
CHRISTOPHER MORIATES, MD, assistant clinical professor in the Division of Hospital Medicine at the University of California, San Francisco, talks about the change in focus and priorities needed for medicine to make progress in waste-reduction efforts.
CHRISTOPHER MORIATES, MD, assistant clinical professor in the Division of Hospital Medicine at the University of California, San Francisco, talks about the change in focus and priorities needed for medicine to make progress in waste-reduction efforts.
CHRISTOPHER MORIATES, MD, assistant clinical professor in the Division of Hospital Medicine at the University of California, San Francisco, talks about the change in focus and priorities needed for medicine to make progress in waste-reduction efforts.
Technology May Offer Solutions to Hospitalists' Readmissions Exposure
Almost weekly, a white paper, report, journal article, or press release touts a new program, software, or technology system offering to help hospitals improve their readmissions avoidance processes and penalty exposure. Does this new readmissions cottage industry offer value to hospitals?
Some technologies focus on interdisciplinary team communication, with electronic repositories or virtual rounding, automated communications to the PCP, personalized patient instructions booklets, or telecommunications or mobile applications. Others aim to help coordinate patients’ care transitions and providers’ post-discharge outreach, empower patients, increase compliance with discharge instructions, or schedule and coordinate follow-up activities.
An August 16, 2013, blog post at HISTalk identified other technologies and services being employed by advisory panelists’ hospitals to reduce their readmissions, including electronic health record (EHR) vendors, predictive modeling vendors, home-grown analytics reports, decision support, niche software vendors focused on supporting case management, telemonitoring programs, and use of the LACE (length of stay, acuity of admission, co-morbidities, and number of previous ED visits in the last six months) index to identify patients at risk.
“I view these as tools and, like any tool, they can be helpful if they are the right tool for the job, applied correctly,” says Gregory Maynard, MD, MSc, SFHM, clinical professor and chief quality officer at the University of California Davis Medical Center in Sacramento. “In many cases, these tech tools are trying to reproduce virtually what ideally would be done in person—interdisciplinary bedside rounds with the active engagement of the patient.”
Mark V. Williams, MD, FACP, MHM, director of the Center for Health Services Research and vice chair of the department of internal medicine at the University of Kentucky in Lexington, says he’s stunned by the sheer number of entrepreneurial readmissions management programs and systems on the market.
“Obviously, people see a need. But I’m not that sanguine about this new tech stuff,” says Dr. Williams, Project BOOST’s principal investigator.
There has to be some kind of integration with the hospital’s EHR, he says; otherwise, it just makes extra work.
“I wish our existing EHRs had the capacity to develop their own readmissions applications,” he says.
Larry Beresford is a freelance writer in Alameda, Calif.
Almost weekly, a white paper, report, journal article, or press release touts a new program, software, or technology system offering to help hospitals improve their readmissions avoidance processes and penalty exposure. Does this new readmissions cottage industry offer value to hospitals?
Some technologies focus on interdisciplinary team communication, with electronic repositories or virtual rounding, automated communications to the PCP, personalized patient instructions booklets, or telecommunications or mobile applications. Others aim to help coordinate patients’ care transitions and providers’ post-discharge outreach, empower patients, increase compliance with discharge instructions, or schedule and coordinate follow-up activities.
An August 16, 2013, blog post at HISTalk identified other technologies and services being employed by advisory panelists’ hospitals to reduce their readmissions, including electronic health record (EHR) vendors, predictive modeling vendors, home-grown analytics reports, decision support, niche software vendors focused on supporting case management, telemonitoring programs, and use of the LACE (length of stay, acuity of admission, co-morbidities, and number of previous ED visits in the last six months) index to identify patients at risk.
“I view these as tools and, like any tool, they can be helpful if they are the right tool for the job, applied correctly,” says Gregory Maynard, MD, MSc, SFHM, clinical professor and chief quality officer at the University of California Davis Medical Center in Sacramento. “In many cases, these tech tools are trying to reproduce virtually what ideally would be done in person—interdisciplinary bedside rounds with the active engagement of the patient.”
Mark V. Williams, MD, FACP, MHM, director of the Center for Health Services Research and vice chair of the department of internal medicine at the University of Kentucky in Lexington, says he’s stunned by the sheer number of entrepreneurial readmissions management programs and systems on the market.
“Obviously, people see a need. But I’m not that sanguine about this new tech stuff,” says Dr. Williams, Project BOOST’s principal investigator.
There has to be some kind of integration with the hospital’s EHR, he says; otherwise, it just makes extra work.
“I wish our existing EHRs had the capacity to develop their own readmissions applications,” he says.
Larry Beresford is a freelance writer in Alameda, Calif.
Almost weekly, a white paper, report, journal article, or press release touts a new program, software, or technology system offering to help hospitals improve their readmissions avoidance processes and penalty exposure. Does this new readmissions cottage industry offer value to hospitals?
Some technologies focus on interdisciplinary team communication, with electronic repositories or virtual rounding, automated communications to the PCP, personalized patient instructions booklets, or telecommunications or mobile applications. Others aim to help coordinate patients’ care transitions and providers’ post-discharge outreach, empower patients, increase compliance with discharge instructions, or schedule and coordinate follow-up activities.
An August 16, 2013, blog post at HISTalk identified other technologies and services being employed by advisory panelists’ hospitals to reduce their readmissions, including electronic health record (EHR) vendors, predictive modeling vendors, home-grown analytics reports, decision support, niche software vendors focused on supporting case management, telemonitoring programs, and use of the LACE (length of stay, acuity of admission, co-morbidities, and number of previous ED visits in the last six months) index to identify patients at risk.
“I view these as tools and, like any tool, they can be helpful if they are the right tool for the job, applied correctly,” says Gregory Maynard, MD, MSc, SFHM, clinical professor and chief quality officer at the University of California Davis Medical Center in Sacramento. “In many cases, these tech tools are trying to reproduce virtually what ideally would be done in person—interdisciplinary bedside rounds with the active engagement of the patient.”
Mark V. Williams, MD, FACP, MHM, director of the Center for Health Services Research and vice chair of the department of internal medicine at the University of Kentucky in Lexington, says he’s stunned by the sheer number of entrepreneurial readmissions management programs and systems on the market.
“Obviously, people see a need. But I’m not that sanguine about this new tech stuff,” says Dr. Williams, Project BOOST’s principal investigator.
There has to be some kind of integration with the hospital’s EHR, he says; otherwise, it just makes extra work.
“I wish our existing EHRs had the capacity to develop their own readmissions applications,” he says.
Larry Beresford is a freelance writer in Alameda, Calif.
Mobile Apps to Improve Quality, Value at Point-of-Care for Inpatients
Summary: The panel of high-tech doctors helped a standing-room-only crowd navigate numerous apps to be used at point-of-care [PDF, 458 kb]. Groups worked through case studies utilizing applicable mobile apps. Examples and most useful apps, including occasional user reviews, follow:
Provider-to-Provider Communication, HIPAA secure
- Doximity.
- HIPAA-chat.
- Pros: HIPAA-secure, real-time communication.
- Cons: Both parties must be on app to securely communicate.
Provider-to-Patient Communication, Language Translators
- Google Translate: multiple platforms, free, 90 languages.
- MediBabble: iOS only, free, seven languages, dedicated medical application.
Diagnostic Apps for Providers
- Calculate by QxM.
- PreOpEval14: iOS only.
- PreopRisk Assessment: Android only.
- ASCVD Risk Estimator.
- MDCalc.com in addition to usual formulas, great abg-analyzer (online version only).
- AnticoagEvaluator.
- epocrates: calculators.
Click here for a PDF of useful apps and resource links [PDF, 177 kb]
Resources for Evidence-Based Practice
- ACP Clinical Guidelines.
- ACP Smart Medicine.
- Read by QxMD.
- UpToDate.
- AHRQ ePPS: identifies clinical preventive services.
- epocrates.
Patient Engagement Apps
- Medication reminders: MediSafe, CareZone.
- Pharmaceutical costs: Walmart, Target Healthful, GoodRx.
- Proper inhaler usage: User Inhalers App.
- Smoking cessation: QuitSTART.
HM15 takeaways
- Apps are available to providers and patients to enhance quality, value, and compliance;
- Before “prescribing” any app to patients, vet the application yourself; and
- Use apps to supplement your clinical practice, but be wary of becoming over-reliant upon them, to the detriment of long-term memory. In order to utilize information in critical-thinking processes, it must be stored in long-term memory. TH
Summary: The panel of high-tech doctors helped a standing-room-only crowd navigate numerous apps to be used at point-of-care [PDF, 458 kb]. Groups worked through case studies utilizing applicable mobile apps. Examples and most useful apps, including occasional user reviews, follow:
Provider-to-Provider Communication, HIPAA secure
- Doximity.
- HIPAA-chat.
- Pros: HIPAA-secure, real-time communication.
- Cons: Both parties must be on app to securely communicate.
Provider-to-Patient Communication, Language Translators
- Google Translate: multiple platforms, free, 90 languages.
- MediBabble: iOS only, free, seven languages, dedicated medical application.
Diagnostic Apps for Providers
- Calculate by QxM.
- PreOpEval14: iOS only.
- PreopRisk Assessment: Android only.
- ASCVD Risk Estimator.
- MDCalc.com in addition to usual formulas, great abg-analyzer (online version only).
- AnticoagEvaluator.
- epocrates: calculators.
Click here for a PDF of useful apps and resource links [PDF, 177 kb]
Resources for Evidence-Based Practice
- ACP Clinical Guidelines.
- ACP Smart Medicine.
- Read by QxMD.
- UpToDate.
- AHRQ ePPS: identifies clinical preventive services.
- epocrates.
Patient Engagement Apps
- Medication reminders: MediSafe, CareZone.
- Pharmaceutical costs: Walmart, Target Healthful, GoodRx.
- Proper inhaler usage: User Inhalers App.
- Smoking cessation: QuitSTART.
HM15 takeaways
- Apps are available to providers and patients to enhance quality, value, and compliance;
- Before “prescribing” any app to patients, vet the application yourself; and
- Use apps to supplement your clinical practice, but be wary of becoming over-reliant upon them, to the detriment of long-term memory. In order to utilize information in critical-thinking processes, it must be stored in long-term memory. TH
Summary: The panel of high-tech doctors helped a standing-room-only crowd navigate numerous apps to be used at point-of-care [PDF, 458 kb]. Groups worked through case studies utilizing applicable mobile apps. Examples and most useful apps, including occasional user reviews, follow:
Provider-to-Provider Communication, HIPAA secure
- Doximity.
- HIPAA-chat.
- Pros: HIPAA-secure, real-time communication.
- Cons: Both parties must be on app to securely communicate.
Provider-to-Patient Communication, Language Translators
- Google Translate: multiple platforms, free, 90 languages.
- MediBabble: iOS only, free, seven languages, dedicated medical application.
Diagnostic Apps for Providers
- Calculate by QxM.
- PreOpEval14: iOS only.
- PreopRisk Assessment: Android only.
- ASCVD Risk Estimator.
- MDCalc.com in addition to usual formulas, great abg-analyzer (online version only).
- AnticoagEvaluator.
- epocrates: calculators.
Click here for a PDF of useful apps and resource links [PDF, 177 kb]
Resources for Evidence-Based Practice
- ACP Clinical Guidelines.
- ACP Smart Medicine.
- Read by QxMD.
- UpToDate.
- AHRQ ePPS: identifies clinical preventive services.
- epocrates.
Patient Engagement Apps
- Medication reminders: MediSafe, CareZone.
- Pharmaceutical costs: Walmart, Target Healthful, GoodRx.
- Proper inhaler usage: User Inhalers App.
- Smoking cessation: QuitSTART.
HM15 takeaways
- Apps are available to providers and patients to enhance quality, value, and compliance;
- Before “prescribing” any app to patients, vet the application yourself; and
- Use apps to supplement your clinical practice, but be wary of becoming over-reliant upon them, to the detriment of long-term memory. In order to utilize information in critical-thinking processes, it must be stored in long-term memory. TH
WATCH: Hospital Medicine 2015 Day Four Highlights
Day Four highlights from HM15, the Society of Hospital Medicine’s (SHM) annual meeting in National Harbor, Md., just outside Washington, D.C.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
Day Four highlights from HM15, the Society of Hospital Medicine’s (SHM) annual meeting in National Harbor, Md., just outside Washington, D.C.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
Day Four highlights from HM15, the Society of Hospital Medicine’s (SHM) annual meeting in National Harbor, Md., just outside Washington, D.C.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
Health Information Technology Could Improve Hospital Discharge Planning
An RIV poster presented at SHM’s annual meeting describes the application of health information technology to improve the quality of hospital discharge summaries.4 Lead author Kristen Lewis, MD, in the clinical division of hospital medicine at The Ohio State University (OSU) Wexner Medical Center in Columbus, described how SHM’s 2009 “Transitions of Care Consensus Policy Statement” was adopted as the medical center’s standard of care—although at baseline this standard was being fully met at the hospital only 4% of the time.5 Discharge summaries frequently lacked important information, including tests pending at discharge, and were not made available to those clinicians who needed them following discharge.
“We developed, piloted, and implemented an innovative electronic discharge summary template that incorporated prompts and automatically populated core components of a quality discharge summary,” Dr. Lewis says, adding that the process also offered opportunities for customization and free-text entries. Initial experience following a series of multidisciplinary educational initiatives to help physicians and case managers understand these mechanisms found full compliance rising to 75%.
Next steps for the project include improving the availability of discharge data for primary care providers, specialist physicians, and extended care facilities not affiliated with OSU; inclusion of the discharge summary in the “After Visit Summary” given to patients; and assessment of outpatient providers’ satisfaction with the process.
For more information about the electronic discharge template, contact Dr. Lewis at [email protected].
Larry Beresford is a freelance writer in Alameda, Calif.
References
- Bailey FA, Williams BR, Woodby LL, et al. Intervention to improve care at life's end in inpatient settings: The BEACON trial. J Gen Intern Med. 2014;29(6):836-843.
- Burling S. Yogurt a solution to hospital infection? Philadelphia Inquirer website. December 10, 2013. Available at: http://articles.philly.com/2013-12-10/news/44946926_1_holy-redeemer-probiotics-yogurt. Accessed June 5, 2014.
- Landelle C, Verachten M, Legrand P, Girou E, Barbut F, Buisson CB. Contamination of healthcare workers’ hands with Clostridium difficile spores after caring for patients with C. difficile infection. Infect Control Hosp Epidemiol. 2014;35(1):10-15.
- Lewis K, Walker C. Development and application of information technology solutions to improve the quality and availability of discharge summaries. Journal of Hospital Medicine RIV abstracts website. Available at: http://www.shmabstracts.com/abstract.asp?MeetingID=793&id=104276&meeting=JHM201305. Published May 2013. Accessed June 14, 2014.
- Snow V, Beck D, Budnitz T, et al. Transitions of Care Consensus Policy Statement. American College of Physicians; Society of General Internal Medicine; Society of Hospital Medicine; American Geriatrics Society; American College of Emergency Physicians; Society of Academic Emergency Medicine. J Gen Intern Med. 2009;24(8):971-976.
- American Hospital Association: Uncompensated hospital care cost fact sheet. January 2014. Available at: http://www.aha.org/content/14/14uncompensatedcare.pdf. Accessed June 5, 2014.
An RIV poster presented at SHM’s annual meeting describes the application of health information technology to improve the quality of hospital discharge summaries.4 Lead author Kristen Lewis, MD, in the clinical division of hospital medicine at The Ohio State University (OSU) Wexner Medical Center in Columbus, described how SHM’s 2009 “Transitions of Care Consensus Policy Statement” was adopted as the medical center’s standard of care—although at baseline this standard was being fully met at the hospital only 4% of the time.5 Discharge summaries frequently lacked important information, including tests pending at discharge, and were not made available to those clinicians who needed them following discharge.
“We developed, piloted, and implemented an innovative electronic discharge summary template that incorporated prompts and automatically populated core components of a quality discharge summary,” Dr. Lewis says, adding that the process also offered opportunities for customization and free-text entries. Initial experience following a series of multidisciplinary educational initiatives to help physicians and case managers understand these mechanisms found full compliance rising to 75%.
Next steps for the project include improving the availability of discharge data for primary care providers, specialist physicians, and extended care facilities not affiliated with OSU; inclusion of the discharge summary in the “After Visit Summary” given to patients; and assessment of outpatient providers’ satisfaction with the process.
For more information about the electronic discharge template, contact Dr. Lewis at [email protected].
Larry Beresford is a freelance writer in Alameda, Calif.
References
- Bailey FA, Williams BR, Woodby LL, et al. Intervention to improve care at life's end in inpatient settings: The BEACON trial. J Gen Intern Med. 2014;29(6):836-843.
- Burling S. Yogurt a solution to hospital infection? Philadelphia Inquirer website. December 10, 2013. Available at: http://articles.philly.com/2013-12-10/news/44946926_1_holy-redeemer-probiotics-yogurt. Accessed June 5, 2014.
- Landelle C, Verachten M, Legrand P, Girou E, Barbut F, Buisson CB. Contamination of healthcare workers’ hands with Clostridium difficile spores after caring for patients with C. difficile infection. Infect Control Hosp Epidemiol. 2014;35(1):10-15.
- Lewis K, Walker C. Development and application of information technology solutions to improve the quality and availability of discharge summaries. Journal of Hospital Medicine RIV abstracts website. Available at: http://www.shmabstracts.com/abstract.asp?MeetingID=793&id=104276&meeting=JHM201305. Published May 2013. Accessed June 14, 2014.
- Snow V, Beck D, Budnitz T, et al. Transitions of Care Consensus Policy Statement. American College of Physicians; Society of General Internal Medicine; Society of Hospital Medicine; American Geriatrics Society; American College of Emergency Physicians; Society of Academic Emergency Medicine. J Gen Intern Med. 2009;24(8):971-976.
- American Hospital Association: Uncompensated hospital care cost fact sheet. January 2014. Available at: http://www.aha.org/content/14/14uncompensatedcare.pdf. Accessed June 5, 2014.
An RIV poster presented at SHM’s annual meeting describes the application of health information technology to improve the quality of hospital discharge summaries.4 Lead author Kristen Lewis, MD, in the clinical division of hospital medicine at The Ohio State University (OSU) Wexner Medical Center in Columbus, described how SHM’s 2009 “Transitions of Care Consensus Policy Statement” was adopted as the medical center’s standard of care—although at baseline this standard was being fully met at the hospital only 4% of the time.5 Discharge summaries frequently lacked important information, including tests pending at discharge, and were not made available to those clinicians who needed them following discharge.
“We developed, piloted, and implemented an innovative electronic discharge summary template that incorporated prompts and automatically populated core components of a quality discharge summary,” Dr. Lewis says, adding that the process also offered opportunities for customization and free-text entries. Initial experience following a series of multidisciplinary educational initiatives to help physicians and case managers understand these mechanisms found full compliance rising to 75%.
Next steps for the project include improving the availability of discharge data for primary care providers, specialist physicians, and extended care facilities not affiliated with OSU; inclusion of the discharge summary in the “After Visit Summary” given to patients; and assessment of outpatient providers’ satisfaction with the process.
For more information about the electronic discharge template, contact Dr. Lewis at [email protected].
Larry Beresford is a freelance writer in Alameda, Calif.
References
- Bailey FA, Williams BR, Woodby LL, et al. Intervention to improve care at life's end in inpatient settings: The BEACON trial. J Gen Intern Med. 2014;29(6):836-843.
- Burling S. Yogurt a solution to hospital infection? Philadelphia Inquirer website. December 10, 2013. Available at: http://articles.philly.com/2013-12-10/news/44946926_1_holy-redeemer-probiotics-yogurt. Accessed June 5, 2014.
- Landelle C, Verachten M, Legrand P, Girou E, Barbut F, Buisson CB. Contamination of healthcare workers’ hands with Clostridium difficile spores after caring for patients with C. difficile infection. Infect Control Hosp Epidemiol. 2014;35(1):10-15.
- Lewis K, Walker C. Development and application of information technology solutions to improve the quality and availability of discharge summaries. Journal of Hospital Medicine RIV abstracts website. Available at: http://www.shmabstracts.com/abstract.asp?MeetingID=793&id=104276&meeting=JHM201305. Published May 2013. Accessed June 14, 2014.
- Snow V, Beck D, Budnitz T, et al. Transitions of Care Consensus Policy Statement. American College of Physicians; Society of General Internal Medicine; Society of Hospital Medicine; American Geriatrics Society; American College of Emergency Physicians; Society of Academic Emergency Medicine. J Gen Intern Med. 2009;24(8):971-976.
- American Hospital Association: Uncompensated hospital care cost fact sheet. January 2014. Available at: http://www.aha.org/content/14/14uncompensatedcare.pdf. Accessed June 5, 2014.
Registration for ASHP’s Medication Safety Collaborative Still Open
Maybe you just returned from HM14 in Las Vegas and are ready to head back. Or maybe you missed out on SHM’s annual meeting but would like to meet up with an important part of the hospitalist team: hospital and health system pharmacists.
Regardless of your motivation, the American Society of Health-System Pharmacist’s (ASHP’s) combination of three meetings in one brings a wealth of information to hospitalists—physicians and pharmacists alike—and now SHM members can register for the Medication Safety Collaborative at the applicable ASHP member rates.
SHM members receive the ASHP member rate at ASHP’s meeting within a meeting for hospital and health system pharmacists, to be held May 31-June 4 in Las Vegas.
Many hospitalists will be especially interested in the Medication Safety Collaborative, which brings the entire hospital team together to share best practices in medication and patient safety.
The Medication Safety Collaborative consists of three meetings:
- ASHP Informatics Institute: An event for informaticists to innovate, interact, and improve the use of information technology in healthcare;
- The Medication Safety Collaborative: For inter-professional teams of health system-based clinicians, coordinators, managers, and administrators who focus on patient safety and quality; and
- Pharmacy Practice Policy: The most relevant issues affecting health system pharmacy practice today at ASHP’s first Pharmacy Practice and Policy Meeting.
Maybe you just returned from HM14 in Las Vegas and are ready to head back. Or maybe you missed out on SHM’s annual meeting but would like to meet up with an important part of the hospitalist team: hospital and health system pharmacists.
Regardless of your motivation, the American Society of Health-System Pharmacist’s (ASHP’s) combination of three meetings in one brings a wealth of information to hospitalists—physicians and pharmacists alike—and now SHM members can register for the Medication Safety Collaborative at the applicable ASHP member rates.
SHM members receive the ASHP member rate at ASHP’s meeting within a meeting for hospital and health system pharmacists, to be held May 31-June 4 in Las Vegas.
Many hospitalists will be especially interested in the Medication Safety Collaborative, which brings the entire hospital team together to share best practices in medication and patient safety.
The Medication Safety Collaborative consists of three meetings:
- ASHP Informatics Institute: An event for informaticists to innovate, interact, and improve the use of information technology in healthcare;
- The Medication Safety Collaborative: For inter-professional teams of health system-based clinicians, coordinators, managers, and administrators who focus on patient safety and quality; and
- Pharmacy Practice Policy: The most relevant issues affecting health system pharmacy practice today at ASHP’s first Pharmacy Practice and Policy Meeting.
Maybe you just returned from HM14 in Las Vegas and are ready to head back. Or maybe you missed out on SHM’s annual meeting but would like to meet up with an important part of the hospitalist team: hospital and health system pharmacists.
Regardless of your motivation, the American Society of Health-System Pharmacist’s (ASHP’s) combination of three meetings in one brings a wealth of information to hospitalists—physicians and pharmacists alike—and now SHM members can register for the Medication Safety Collaborative at the applicable ASHP member rates.
SHM members receive the ASHP member rate at ASHP’s meeting within a meeting for hospital and health system pharmacists, to be held May 31-June 4 in Las Vegas.
Many hospitalists will be especially interested in the Medication Safety Collaborative, which brings the entire hospital team together to share best practices in medication and patient safety.
The Medication Safety Collaborative consists of three meetings:
- ASHP Informatics Institute: An event for informaticists to innovate, interact, and improve the use of information technology in healthcare;
- The Medication Safety Collaborative: For inter-professional teams of health system-based clinicians, coordinators, managers, and administrators who focus on patient safety and quality; and
- Pharmacy Practice Policy: The most relevant issues affecting health system pharmacy practice today at ASHP’s first Pharmacy Practice and Policy Meeting.