User login
The ‘fun’ in leader-fun-ship
Add value to relationships, loyalty, commitment
Leadership and “fun” are not often linked in the same sentence, let alone in the same word. However, as a student, observer, and teacher of leadership, I find that leaders who are having fun in their practice deftly share the energy, engagement, appeal, dedication, exuberance, and pleasure with others.
Imagine going to work and meeting all those qualities at the front door. Leaders who are having fun impart that same joy to others. It’s a great source of motivation, problem solving capacity, and morale enhancement. And when the going gets tough, it helps you and others make it through.
What takes the fun out of leadership? There are difficult decisions, complicated personalities, messy histories, conflict, and, of course, the “buck stops here” responsibility. Leadership is a lot of work, going above and beyond your clinical duties. Many arrive at leadership positions without the requisite training and preparation, and success at leading can be elusive for reasons you can’t control. There are budget constraints, difficult personalities, laws, and rules. For some leaders, it is an oxymoron to place leadership and fun together. For them, leadership is not fun.
At the 2018 Society of Hospital Medicine Leadership Academy in Vancouver, this combination of fun and leadership arose in a number of my conversations. I asked people if they were having fun. I heard the enjoyment, excitement, amusement, and playfulness of leading. And I could see these leaders – who found fun in their work – were transmitting those very qualities to their followers. They talked about exceptional productivity, expanding programs, heightened commitment, and a knack for overcoming occasional setbacks. In many ways, “work” works better when people are having fun.
How might putting fun into your leadership style, practices, and assessment make you a more effective leader? Start with our definition of leadership: “People follow you.” Whether people follow you, in fact, has to do with a lot more than just fun. Your clinical expertise and skills, your management capabilities, and your devotion to the job all are ingredients in what makes you an effective leader. Add fun into the equation and relationships, loyalty, and commitment assume new value. That value translates into the joy, fulfillment, and pleasure of doing important work with people who matter to you.
I once asked a C-suite leader at Southwest Airlines about fun and leadership. He told me that fun was incorporated into the airline’s company culture. It was also included in his annual performance review: He is responsible for ensuring that his subordinates find working for him to be fun. That week he was hosting a barbecue and fun was on the menu. He explained that this attitude is baked into Southwest philosophy. It transmits out to frontline employees, flight attendants, and gate agents. Their job is making the passengers’ experience safe, comfortable, and, at the same time, fun. That combination has made the company consistently profitable and remarkably resilient. (My wife and her university friend – now both therapists – call this a “fun unit,” which made their grueling graduate school work far more tolerable.)
How do you translate this lesson into your leadership practices? First, don’t expect others to have fun working and following you if you aren’t having fun yourself, or if you are not fun to be with. Assess your own work experience. What is it that you truly enjoy? What tasks and responsibilities detract from that engagement and delight? What provides you that sense of fulfillment and value in what you are doing and the direction you are leading? Dissect your priorities and ask whether your allotment of time and attention track to what is really important. What changes could you make?
Second, ask those same questions of the group of people whom you lead. Assess their experiences, what supports their sense of accomplishment, their satisfaction with their job, and their engagement with the people with whom they work. Every one of your followers is different. However, on the whole, have you built, encouraged, and rewarded team spirit among people who value being together, who are committed to the shared mission, and who together take pride in their achievements?
Finally, ask yourself what would make your work experience and that of your followers more fun? Similarly, what would better engage the patients, family members, and colleagues you serve? Ask a leader you respect – a leader enthusiast – what they find fun in their leading. As you become more engaged, you likely will become a more effective leader, and those who follow you will be so too. What could you do to elevate the work experiences of others and thereby the value, success, and meaning of their work? Fun has many ways to express itself.
Bottom line, ask yourself: Are you someone who others want to work for? Do you care? Can you bring out the best in people because of who you are and what you do?
Your work is as serious as it gets. You are at the cusp of life and death, quality of life decisions, and medical care. The fun comes in putting your all into it and getting the satisfaction and interpersonal bonds that make that effort worthwhile. Often, you have the privilege of making people healthier and happier. What a gift! Excellence can be fun.
Keep an appropriate sense of humor in your pocket and an ample supply of personal and professional curiosity in your backpack. Relish the delight of something or someone new and pleasantly unexpected. The fun for others comes in your rewarding flash of a smile, your laugh, or your approval when it matters most.
Your job as leader is tough. Health care is hard work and the changes and shifts in the health care system are only making it more so. Imagine how a dash of humanity and relationships can make that all far more bearable.
And have fun finding out.
Dr. Marcus is coauthor of “Renegotiating Health Care: Resolving Conflict to Build Collaboration, Second Edition” (San Francisco: Jossey-Bass Publishers, 2011) and is director of the program for health care negotiation and conflict resolution at Harvard School of Public Health, Boston. Dr. Marcus teaches regularly in the SHM Leadership Academy. He can be reached at [email protected].
Add value to relationships, loyalty, commitment
Add value to relationships, loyalty, commitment
Leadership and “fun” are not often linked in the same sentence, let alone in the same word. However, as a student, observer, and teacher of leadership, I find that leaders who are having fun in their practice deftly share the energy, engagement, appeal, dedication, exuberance, and pleasure with others.
Imagine going to work and meeting all those qualities at the front door. Leaders who are having fun impart that same joy to others. It’s a great source of motivation, problem solving capacity, and morale enhancement. And when the going gets tough, it helps you and others make it through.
What takes the fun out of leadership? There are difficult decisions, complicated personalities, messy histories, conflict, and, of course, the “buck stops here” responsibility. Leadership is a lot of work, going above and beyond your clinical duties. Many arrive at leadership positions without the requisite training and preparation, and success at leading can be elusive for reasons you can’t control. There are budget constraints, difficult personalities, laws, and rules. For some leaders, it is an oxymoron to place leadership and fun together. For them, leadership is not fun.
At the 2018 Society of Hospital Medicine Leadership Academy in Vancouver, this combination of fun and leadership arose in a number of my conversations. I asked people if they were having fun. I heard the enjoyment, excitement, amusement, and playfulness of leading. And I could see these leaders – who found fun in their work – were transmitting those very qualities to their followers. They talked about exceptional productivity, expanding programs, heightened commitment, and a knack for overcoming occasional setbacks. In many ways, “work” works better when people are having fun.
How might putting fun into your leadership style, practices, and assessment make you a more effective leader? Start with our definition of leadership: “People follow you.” Whether people follow you, in fact, has to do with a lot more than just fun. Your clinical expertise and skills, your management capabilities, and your devotion to the job all are ingredients in what makes you an effective leader. Add fun into the equation and relationships, loyalty, and commitment assume new value. That value translates into the joy, fulfillment, and pleasure of doing important work with people who matter to you.
I once asked a C-suite leader at Southwest Airlines about fun and leadership. He told me that fun was incorporated into the airline’s company culture. It was also included in his annual performance review: He is responsible for ensuring that his subordinates find working for him to be fun. That week he was hosting a barbecue and fun was on the menu. He explained that this attitude is baked into Southwest philosophy. It transmits out to frontline employees, flight attendants, and gate agents. Their job is making the passengers’ experience safe, comfortable, and, at the same time, fun. That combination has made the company consistently profitable and remarkably resilient. (My wife and her university friend – now both therapists – call this a “fun unit,” which made their grueling graduate school work far more tolerable.)
How do you translate this lesson into your leadership practices? First, don’t expect others to have fun working and following you if you aren’t having fun yourself, or if you are not fun to be with. Assess your own work experience. What is it that you truly enjoy? What tasks and responsibilities detract from that engagement and delight? What provides you that sense of fulfillment and value in what you are doing and the direction you are leading? Dissect your priorities and ask whether your allotment of time and attention track to what is really important. What changes could you make?
Second, ask those same questions of the group of people whom you lead. Assess their experiences, what supports their sense of accomplishment, their satisfaction with their job, and their engagement with the people with whom they work. Every one of your followers is different. However, on the whole, have you built, encouraged, and rewarded team spirit among people who value being together, who are committed to the shared mission, and who together take pride in their achievements?
Finally, ask yourself what would make your work experience and that of your followers more fun? Similarly, what would better engage the patients, family members, and colleagues you serve? Ask a leader you respect – a leader enthusiast – what they find fun in their leading. As you become more engaged, you likely will become a more effective leader, and those who follow you will be so too. What could you do to elevate the work experiences of others and thereby the value, success, and meaning of their work? Fun has many ways to express itself.
Bottom line, ask yourself: Are you someone who others want to work for? Do you care? Can you bring out the best in people because of who you are and what you do?
Your work is as serious as it gets. You are at the cusp of life and death, quality of life decisions, and medical care. The fun comes in putting your all into it and getting the satisfaction and interpersonal bonds that make that effort worthwhile. Often, you have the privilege of making people healthier and happier. What a gift! Excellence can be fun.
Keep an appropriate sense of humor in your pocket and an ample supply of personal and professional curiosity in your backpack. Relish the delight of something or someone new and pleasantly unexpected. The fun for others comes in your rewarding flash of a smile, your laugh, or your approval when it matters most.
Your job as leader is tough. Health care is hard work and the changes and shifts in the health care system are only making it more so. Imagine how a dash of humanity and relationships can make that all far more bearable.
And have fun finding out.
Dr. Marcus is coauthor of “Renegotiating Health Care: Resolving Conflict to Build Collaboration, Second Edition” (San Francisco: Jossey-Bass Publishers, 2011) and is director of the program for health care negotiation and conflict resolution at Harvard School of Public Health, Boston. Dr. Marcus teaches regularly in the SHM Leadership Academy. He can be reached at [email protected].
Leadership and “fun” are not often linked in the same sentence, let alone in the same word. However, as a student, observer, and teacher of leadership, I find that leaders who are having fun in their practice deftly share the energy, engagement, appeal, dedication, exuberance, and pleasure with others.
Imagine going to work and meeting all those qualities at the front door. Leaders who are having fun impart that same joy to others. It’s a great source of motivation, problem solving capacity, and morale enhancement. And when the going gets tough, it helps you and others make it through.
What takes the fun out of leadership? There are difficult decisions, complicated personalities, messy histories, conflict, and, of course, the “buck stops here” responsibility. Leadership is a lot of work, going above and beyond your clinical duties. Many arrive at leadership positions without the requisite training and preparation, and success at leading can be elusive for reasons you can’t control. There are budget constraints, difficult personalities, laws, and rules. For some leaders, it is an oxymoron to place leadership and fun together. For them, leadership is not fun.
At the 2018 Society of Hospital Medicine Leadership Academy in Vancouver, this combination of fun and leadership arose in a number of my conversations. I asked people if they were having fun. I heard the enjoyment, excitement, amusement, and playfulness of leading. And I could see these leaders – who found fun in their work – were transmitting those very qualities to their followers. They talked about exceptional productivity, expanding programs, heightened commitment, and a knack for overcoming occasional setbacks. In many ways, “work” works better when people are having fun.
How might putting fun into your leadership style, practices, and assessment make you a more effective leader? Start with our definition of leadership: “People follow you.” Whether people follow you, in fact, has to do with a lot more than just fun. Your clinical expertise and skills, your management capabilities, and your devotion to the job all are ingredients in what makes you an effective leader. Add fun into the equation and relationships, loyalty, and commitment assume new value. That value translates into the joy, fulfillment, and pleasure of doing important work with people who matter to you.
I once asked a C-suite leader at Southwest Airlines about fun and leadership. He told me that fun was incorporated into the airline’s company culture. It was also included in his annual performance review: He is responsible for ensuring that his subordinates find working for him to be fun. That week he was hosting a barbecue and fun was on the menu. He explained that this attitude is baked into Southwest philosophy. It transmits out to frontline employees, flight attendants, and gate agents. Their job is making the passengers’ experience safe, comfortable, and, at the same time, fun. That combination has made the company consistently profitable and remarkably resilient. (My wife and her university friend – now both therapists – call this a “fun unit,” which made their grueling graduate school work far more tolerable.)
How do you translate this lesson into your leadership practices? First, don’t expect others to have fun working and following you if you aren’t having fun yourself, or if you are not fun to be with. Assess your own work experience. What is it that you truly enjoy? What tasks and responsibilities detract from that engagement and delight? What provides you that sense of fulfillment and value in what you are doing and the direction you are leading? Dissect your priorities and ask whether your allotment of time and attention track to what is really important. What changes could you make?
Second, ask those same questions of the group of people whom you lead. Assess their experiences, what supports their sense of accomplishment, their satisfaction with their job, and their engagement with the people with whom they work. Every one of your followers is different. However, on the whole, have you built, encouraged, and rewarded team spirit among people who value being together, who are committed to the shared mission, and who together take pride in their achievements?
Finally, ask yourself what would make your work experience and that of your followers more fun? Similarly, what would better engage the patients, family members, and colleagues you serve? Ask a leader you respect – a leader enthusiast – what they find fun in their leading. As you become more engaged, you likely will become a more effective leader, and those who follow you will be so too. What could you do to elevate the work experiences of others and thereby the value, success, and meaning of their work? Fun has many ways to express itself.
Bottom line, ask yourself: Are you someone who others want to work for? Do you care? Can you bring out the best in people because of who you are and what you do?
Your work is as serious as it gets. You are at the cusp of life and death, quality of life decisions, and medical care. The fun comes in putting your all into it and getting the satisfaction and interpersonal bonds that make that effort worthwhile. Often, you have the privilege of making people healthier and happier. What a gift! Excellence can be fun.
Keep an appropriate sense of humor in your pocket and an ample supply of personal and professional curiosity in your backpack. Relish the delight of something or someone new and pleasantly unexpected. The fun for others comes in your rewarding flash of a smile, your laugh, or your approval when it matters most.
Your job as leader is tough. Health care is hard work and the changes and shifts in the health care system are only making it more so. Imagine how a dash of humanity and relationships can make that all far more bearable.
And have fun finding out.
Dr. Marcus is coauthor of “Renegotiating Health Care: Resolving Conflict to Build Collaboration, Second Edition” (San Francisco: Jossey-Bass Publishers, 2011) and is director of the program for health care negotiation and conflict resolution at Harvard School of Public Health, Boston. Dr. Marcus teaches regularly in the SHM Leadership Academy. He can be reached at [email protected].
Obtain proper reimbursements with more effective documentation and coding
SHM webinar series provides hospitalists with best practices to improve accuracy and compliance
Hospitalists cannot bill for everything they do, but they can document and code to obtain appropriate reimbursements. It is important for hospitalists to know the factors that influence coding to ensure accuracy and compliance.
The Society of Hospital Medicine developed the Clinical Documentation & Coding for Hospitalists webinar series (formerly known as CODE-H) to provide hospitalists with the latest information on best practices in coding, documentation, and compliance from nationally recognized experts, along with the opportunity to claim CME.
The Hospitalist recently spoke with Carol Pohlig, BSN, RN, CPC, ACS, course director of the webinar series and a coding and documentation expert at the University of Pennsylvania Medical Center in Philadelphia. She was instrumental in developing the content in the series to ensure it was specifically designed to address challenges regularly faced by hospitalists.
What inspired the creation of Clinical Documentation & Coding for Hospitalists?
Providers are so busy trying to keep up with regulations for their institution, such as malpractice and quality issues, that the focus isn’t always on the documentation required for reimbursement. The creation of the series rose out of a need for providers to understand key issues related to documentation and billing and some of the hurdles that they need to overcome – or need to be aware of in the first place.
This series brings awareness and solutions to some of these problems. It is available on an ongoing basis, so viewers can move at their own pace. Given the wealth of information in the series, it made sense to create it in this format.
What are some common challenges that hospitalists encounter when coding, and how does this webinar series help to address these challenges?
Some common challenges relate to concurrent care or comanagement. Hospitalists are hired to be the gatekeepers – the ones overseeing patient care. When other consultants are on board, they wind up sharing responsibilities, which can muddy the waters at times, especially with billing and coding. It is important for hospitalists to understand their role in comanagement and, in turn, how the payers view their role.
We highlight everything – including requirements for history, exam, and medical decision making – and review each component in depth. We also discuss billing based on these key components or, when it is appropriate, billing based on time. However, when billing time-based services, you have to meet certain qualifications because it is different from the standard way of reporting, which is something we break down in the series.
Related to mitigating risk, EMRs and their copy and paste function is another topic we delve into. It’s easy to copy and paste and pull forward information from a previous note to help save time. However, it is important to understand what the ramifications are. Each of these copied and pasted encounters must be modified to make it applicable to the current day’s patient and ensure care is not being misrepresented.
Those are just a few of the items covered, but we believe that each of the eight modules in the series offers something unique that will help improve documentation and coding practices.
How can this webinar series go beyond the hospital medicine care team and more broadly affect the institution as a whole?
Hospitalists are often involved in a number of different categories of services, including observation and same-day admission/discharge. The series reviews rules and challenges specific to those sites of service, which on a broader scale, impact not only providers in other service lines but also those who work in the revenue cycle at the parent institution. How each of these parties understands the nuances explained in the series can directly affect the successful processing of the submitted claims.
In addition, interpretation of rules when it comes to coding and documentation can vary at a local level. We raise awareness of local interpretations to ensure everyone involved in the documentation and coding process knows things to look out for when reading rules. You might think it means one thing when, in reality, it could mean another. With this series, everyone involved with billing and coding can reflect on the implications that incorrect or inaccurate coding may have on their hospital.
Who would benefit from viewing this webinar series?
Although we primarily had hospitalists of all types – including physicians, nurse practitioners, and physician assistants – in mind during the development of course content, anyone who works as a practice manager, biller, coder, or internal auditor has the potential to benefit from the series. If they understand broader challenges in coding, it could help them proactively prevent issues throughout the process with more accurate documentation that could reduce claims denials.
Let SHM’s Clinical Documentation & Coding for Hospitalists webinar series bolster your and your team’s accuracy and compliance. Individual and group subscriptions are available. For more information, visit hospitalmedicine.org/coding.
SHM webinar series provides hospitalists with best practices to improve accuracy and compliance
SHM webinar series provides hospitalists with best practices to improve accuracy and compliance
Hospitalists cannot bill for everything they do, but they can document and code to obtain appropriate reimbursements. It is important for hospitalists to know the factors that influence coding to ensure accuracy and compliance.
The Society of Hospital Medicine developed the Clinical Documentation & Coding for Hospitalists webinar series (formerly known as CODE-H) to provide hospitalists with the latest information on best practices in coding, documentation, and compliance from nationally recognized experts, along with the opportunity to claim CME.
The Hospitalist recently spoke with Carol Pohlig, BSN, RN, CPC, ACS, course director of the webinar series and a coding and documentation expert at the University of Pennsylvania Medical Center in Philadelphia. She was instrumental in developing the content in the series to ensure it was specifically designed to address challenges regularly faced by hospitalists.
What inspired the creation of Clinical Documentation & Coding for Hospitalists?
Providers are so busy trying to keep up with regulations for their institution, such as malpractice and quality issues, that the focus isn’t always on the documentation required for reimbursement. The creation of the series rose out of a need for providers to understand key issues related to documentation and billing and some of the hurdles that they need to overcome – or need to be aware of in the first place.
This series brings awareness and solutions to some of these problems. It is available on an ongoing basis, so viewers can move at their own pace. Given the wealth of information in the series, it made sense to create it in this format.
What are some common challenges that hospitalists encounter when coding, and how does this webinar series help to address these challenges?
Some common challenges relate to concurrent care or comanagement. Hospitalists are hired to be the gatekeepers – the ones overseeing patient care. When other consultants are on board, they wind up sharing responsibilities, which can muddy the waters at times, especially with billing and coding. It is important for hospitalists to understand their role in comanagement and, in turn, how the payers view their role.
We highlight everything – including requirements for history, exam, and medical decision making – and review each component in depth. We also discuss billing based on these key components or, when it is appropriate, billing based on time. However, when billing time-based services, you have to meet certain qualifications because it is different from the standard way of reporting, which is something we break down in the series.
Related to mitigating risk, EMRs and their copy and paste function is another topic we delve into. It’s easy to copy and paste and pull forward information from a previous note to help save time. However, it is important to understand what the ramifications are. Each of these copied and pasted encounters must be modified to make it applicable to the current day’s patient and ensure care is not being misrepresented.
Those are just a few of the items covered, but we believe that each of the eight modules in the series offers something unique that will help improve documentation and coding practices.
How can this webinar series go beyond the hospital medicine care team and more broadly affect the institution as a whole?
Hospitalists are often involved in a number of different categories of services, including observation and same-day admission/discharge. The series reviews rules and challenges specific to those sites of service, which on a broader scale, impact not only providers in other service lines but also those who work in the revenue cycle at the parent institution. How each of these parties understands the nuances explained in the series can directly affect the successful processing of the submitted claims.
In addition, interpretation of rules when it comes to coding and documentation can vary at a local level. We raise awareness of local interpretations to ensure everyone involved in the documentation and coding process knows things to look out for when reading rules. You might think it means one thing when, in reality, it could mean another. With this series, everyone involved with billing and coding can reflect on the implications that incorrect or inaccurate coding may have on their hospital.
Who would benefit from viewing this webinar series?
Although we primarily had hospitalists of all types – including physicians, nurse practitioners, and physician assistants – in mind during the development of course content, anyone who works as a practice manager, biller, coder, or internal auditor has the potential to benefit from the series. If they understand broader challenges in coding, it could help them proactively prevent issues throughout the process with more accurate documentation that could reduce claims denials.
Let SHM’s Clinical Documentation & Coding for Hospitalists webinar series bolster your and your team’s accuracy and compliance. Individual and group subscriptions are available. For more information, visit hospitalmedicine.org/coding.
Hospitalists cannot bill for everything they do, but they can document and code to obtain appropriate reimbursements. It is important for hospitalists to know the factors that influence coding to ensure accuracy and compliance.
The Society of Hospital Medicine developed the Clinical Documentation & Coding for Hospitalists webinar series (formerly known as CODE-H) to provide hospitalists with the latest information on best practices in coding, documentation, and compliance from nationally recognized experts, along with the opportunity to claim CME.
The Hospitalist recently spoke with Carol Pohlig, BSN, RN, CPC, ACS, course director of the webinar series and a coding and documentation expert at the University of Pennsylvania Medical Center in Philadelphia. She was instrumental in developing the content in the series to ensure it was specifically designed to address challenges regularly faced by hospitalists.
What inspired the creation of Clinical Documentation & Coding for Hospitalists?
Providers are so busy trying to keep up with regulations for their institution, such as malpractice and quality issues, that the focus isn’t always on the documentation required for reimbursement. The creation of the series rose out of a need for providers to understand key issues related to documentation and billing and some of the hurdles that they need to overcome – or need to be aware of in the first place.
This series brings awareness and solutions to some of these problems. It is available on an ongoing basis, so viewers can move at their own pace. Given the wealth of information in the series, it made sense to create it in this format.
What are some common challenges that hospitalists encounter when coding, and how does this webinar series help to address these challenges?
Some common challenges relate to concurrent care or comanagement. Hospitalists are hired to be the gatekeepers – the ones overseeing patient care. When other consultants are on board, they wind up sharing responsibilities, which can muddy the waters at times, especially with billing and coding. It is important for hospitalists to understand their role in comanagement and, in turn, how the payers view their role.
We highlight everything – including requirements for history, exam, and medical decision making – and review each component in depth. We also discuss billing based on these key components or, when it is appropriate, billing based on time. However, when billing time-based services, you have to meet certain qualifications because it is different from the standard way of reporting, which is something we break down in the series.
Related to mitigating risk, EMRs and their copy and paste function is another topic we delve into. It’s easy to copy and paste and pull forward information from a previous note to help save time. However, it is important to understand what the ramifications are. Each of these copied and pasted encounters must be modified to make it applicable to the current day’s patient and ensure care is not being misrepresented.
Those are just a few of the items covered, but we believe that each of the eight modules in the series offers something unique that will help improve documentation and coding practices.
How can this webinar series go beyond the hospital medicine care team and more broadly affect the institution as a whole?
Hospitalists are often involved in a number of different categories of services, including observation and same-day admission/discharge. The series reviews rules and challenges specific to those sites of service, which on a broader scale, impact not only providers in other service lines but also those who work in the revenue cycle at the parent institution. How each of these parties understands the nuances explained in the series can directly affect the successful processing of the submitted claims.
In addition, interpretation of rules when it comes to coding and documentation can vary at a local level. We raise awareness of local interpretations to ensure everyone involved in the documentation and coding process knows things to look out for when reading rules. You might think it means one thing when, in reality, it could mean another. With this series, everyone involved with billing and coding can reflect on the implications that incorrect or inaccurate coding may have on their hospital.
Who would benefit from viewing this webinar series?
Although we primarily had hospitalists of all types – including physicians, nurse practitioners, and physician assistants – in mind during the development of course content, anyone who works as a practice manager, biller, coder, or internal auditor has the potential to benefit from the series. If they understand broader challenges in coding, it could help them proactively prevent issues throughout the process with more accurate documentation that could reduce claims denials.
Let SHM’s Clinical Documentation & Coding for Hospitalists webinar series bolster your and your team’s accuracy and compliance. Individual and group subscriptions are available. For more information, visit hospitalmedicine.org/coding.
Am I still a hospitalist?
HM as a force for change
I wear a suit every day to work. I count the time between shifts in months, not days. Rather than looking for subtle diagnostic clues hidden in clinical information, I find myself up to my elbows in performance and financial data. Instead of meetings complicated by challenging family dynamics, I spend my time calming the waters between clinical departments that each feel slighted.
And yet, when people ask me what I do, I do not say I am a health system CEO. Rather, I am a hospitalist. I say it, not out of habit, but with pride and clear intention. Almost 20 years ago, I had to explain to my parents what a hospitalist was as I made the transition from primary care doctor to hospitalist. I told them that hospitalists take care of sick people who are in the hospital, but also are charged with making the hospital a better place to take care of people. I hope that in some small way, in every role I have had over the past 20 years as a hospitalist, I have been able to do that.
While the small changes we can all make every day are important, massive changes to health care, hospitals, and providers are coming. The forces driving these changes are manifold, complex, and powerful. Individual hospitalists, hospital groups, and hospitals will be challenged to keep up with responding to these changes. I hope, though, that our field, hospital medicine, will not be sitting there, waiting for the changes to come, but will instead be one of the forces for change.
I also believe that hospital medicine and health care delivery systems should drive the change in a coordinated and collaborative partnership. A partnership not built on self-advocacy but one in which we remember why we exist – to take care of people. A force for change that preserves the essential, evolves what needs improvement, and revolutionizes the archaic.
Partnerships between hospitalist groups and health care administration will always face the day-to-day challenges of balancing the need for resources with the ability to provide them, agreeing on how to measure and assess quality, and aligning rewards with priorities. However, by working together in venues that allow us to think beyond the day-to-day issues, we in hospital medicine will be leaders in the change that is coming. I believe that today, the Society of Hospital Medicine must be one of those venues. Through its committees, meetings, advocacy, publications, and most importantly, members, SHM will continue to shape the future of care delivery in this country and beyond.
SHM has been my professional home for almost 20 years, helping me think about how to make the hospital a better place to take care of people. Recent examples of SHM and its members partnering in this area include advocacy work to improve alternative payment models, such as Medicare Access and CHIP Reauthorization Act of 2015 (MACRA), as well as educational efforts for its members on how to navigate the current rules around MACRA.
For many years, SHM has been the leader in professional organizations for leading the way on quality improvement. Through the Center for Quality Improvement, SHM not only offers robust educational tools to better enable members to lead efforts at their home institutions but also has led multi-institutional efforts to reduce harm that have been recognized nationally for their impact.
As we move further down the path from volume to value toward population health, the SHM Board will be sure that the society continues to be a leader for both its members and the health system at large as we face these changes. We have the opportunity in front of us to collectively embrace and create the changes coming toward us with that shared purpose of making wherever it is that we care for people better places to provide that care. How could one not be proud to say, with intent, “I am a hospitalist,” regardless of what it is that brings each of us to SHM.
Dr. Whelan is CEO of Banner–University Medical Center Tucson (Ariz.) and a member of the SHM Board of Directors.
HM as a force for change
HM as a force for change
I wear a suit every day to work. I count the time between shifts in months, not days. Rather than looking for subtle diagnostic clues hidden in clinical information, I find myself up to my elbows in performance and financial data. Instead of meetings complicated by challenging family dynamics, I spend my time calming the waters between clinical departments that each feel slighted.
And yet, when people ask me what I do, I do not say I am a health system CEO. Rather, I am a hospitalist. I say it, not out of habit, but with pride and clear intention. Almost 20 years ago, I had to explain to my parents what a hospitalist was as I made the transition from primary care doctor to hospitalist. I told them that hospitalists take care of sick people who are in the hospital, but also are charged with making the hospital a better place to take care of people. I hope that in some small way, in every role I have had over the past 20 years as a hospitalist, I have been able to do that.
While the small changes we can all make every day are important, massive changes to health care, hospitals, and providers are coming. The forces driving these changes are manifold, complex, and powerful. Individual hospitalists, hospital groups, and hospitals will be challenged to keep up with responding to these changes. I hope, though, that our field, hospital medicine, will not be sitting there, waiting for the changes to come, but will instead be one of the forces for change.
I also believe that hospital medicine and health care delivery systems should drive the change in a coordinated and collaborative partnership. A partnership not built on self-advocacy but one in which we remember why we exist – to take care of people. A force for change that preserves the essential, evolves what needs improvement, and revolutionizes the archaic.
Partnerships between hospitalist groups and health care administration will always face the day-to-day challenges of balancing the need for resources with the ability to provide them, agreeing on how to measure and assess quality, and aligning rewards with priorities. However, by working together in venues that allow us to think beyond the day-to-day issues, we in hospital medicine will be leaders in the change that is coming. I believe that today, the Society of Hospital Medicine must be one of those venues. Through its committees, meetings, advocacy, publications, and most importantly, members, SHM will continue to shape the future of care delivery in this country and beyond.
SHM has been my professional home for almost 20 years, helping me think about how to make the hospital a better place to take care of people. Recent examples of SHM and its members partnering in this area include advocacy work to improve alternative payment models, such as Medicare Access and CHIP Reauthorization Act of 2015 (MACRA), as well as educational efforts for its members on how to navigate the current rules around MACRA.
For many years, SHM has been the leader in professional organizations for leading the way on quality improvement. Through the Center for Quality Improvement, SHM not only offers robust educational tools to better enable members to lead efforts at their home institutions but also has led multi-institutional efforts to reduce harm that have been recognized nationally for their impact.
As we move further down the path from volume to value toward population health, the SHM Board will be sure that the society continues to be a leader for both its members and the health system at large as we face these changes. We have the opportunity in front of us to collectively embrace and create the changes coming toward us with that shared purpose of making wherever it is that we care for people better places to provide that care. How could one not be proud to say, with intent, “I am a hospitalist,” regardless of what it is that brings each of us to SHM.
Dr. Whelan is CEO of Banner–University Medical Center Tucson (Ariz.) and a member of the SHM Board of Directors.
I wear a suit every day to work. I count the time between shifts in months, not days. Rather than looking for subtle diagnostic clues hidden in clinical information, I find myself up to my elbows in performance and financial data. Instead of meetings complicated by challenging family dynamics, I spend my time calming the waters between clinical departments that each feel slighted.
And yet, when people ask me what I do, I do not say I am a health system CEO. Rather, I am a hospitalist. I say it, not out of habit, but with pride and clear intention. Almost 20 years ago, I had to explain to my parents what a hospitalist was as I made the transition from primary care doctor to hospitalist. I told them that hospitalists take care of sick people who are in the hospital, but also are charged with making the hospital a better place to take care of people. I hope that in some small way, in every role I have had over the past 20 years as a hospitalist, I have been able to do that.
While the small changes we can all make every day are important, massive changes to health care, hospitals, and providers are coming. The forces driving these changes are manifold, complex, and powerful. Individual hospitalists, hospital groups, and hospitals will be challenged to keep up with responding to these changes. I hope, though, that our field, hospital medicine, will not be sitting there, waiting for the changes to come, but will instead be one of the forces for change.
I also believe that hospital medicine and health care delivery systems should drive the change in a coordinated and collaborative partnership. A partnership not built on self-advocacy but one in which we remember why we exist – to take care of people. A force for change that preserves the essential, evolves what needs improvement, and revolutionizes the archaic.
Partnerships between hospitalist groups and health care administration will always face the day-to-day challenges of balancing the need for resources with the ability to provide them, agreeing on how to measure and assess quality, and aligning rewards with priorities. However, by working together in venues that allow us to think beyond the day-to-day issues, we in hospital medicine will be leaders in the change that is coming. I believe that today, the Society of Hospital Medicine must be one of those venues. Through its committees, meetings, advocacy, publications, and most importantly, members, SHM will continue to shape the future of care delivery in this country and beyond.
SHM has been my professional home for almost 20 years, helping me think about how to make the hospital a better place to take care of people. Recent examples of SHM and its members partnering in this area include advocacy work to improve alternative payment models, such as Medicare Access and CHIP Reauthorization Act of 2015 (MACRA), as well as educational efforts for its members on how to navigate the current rules around MACRA.
For many years, SHM has been the leader in professional organizations for leading the way on quality improvement. Through the Center for Quality Improvement, SHM not only offers robust educational tools to better enable members to lead efforts at their home institutions but also has led multi-institutional efforts to reduce harm that have been recognized nationally for their impact.
As we move further down the path from volume to value toward population health, the SHM Board will be sure that the society continues to be a leader for both its members and the health system at large as we face these changes. We have the opportunity in front of us to collectively embrace and create the changes coming toward us with that shared purpose of making wherever it is that we care for people better places to provide that care. How could one not be proud to say, with intent, “I am a hospitalist,” regardless of what it is that brings each of us to SHM.
Dr. Whelan is CEO of Banner–University Medical Center Tucson (Ariz.) and a member of the SHM Board of Directors.
The changing landscape of medical education
A brave new world
It’s Monday morning, and your intern is presenting an overnight admission. Lost in the details of his disorganized introduction, your mind wanders. “Why doesn’t this intern know how to present? When I trained, all those admissions during long sleepless nights really taught me to do this right.” But can we equate hours worked with competency achieved? And if not, what is the alternative? This article introduces some major changes in medical education and their implications for hospitalists.
Most hospitalists trained in an educational system influenced by Sir William Osler. In the early 1900s, he introduced the natural method of teaching, positing that student exposure to patients and experience over time ensured that physicians in training would become competent doctors.1 His influence led to the current structure of medical education, which includes conventional third-year clerkships and time-limited rotations (such as a 2-week nephrology block).
While familiarity may be comforting, there are signs our current model of medical education is inefficient, inadequate, and obsolete.
For one, the traditional system is failing to adequately prepare physicians to provide safe and complex care. Reports, such as the Institute of Medicine’s (IOM) “To Err is Human,”2 describe a high rate of preventable errors, highlighting considerable room for improvement in training the next generation of physicians.3,4
Meanwhile, trainees are still largely being deemed ready for the workforce by length of training completed (for example, completion of four-year medical school) rather than a skill set distinctly achieved. Our system leaves little flexibility to individualize learner goals, which is significant given some students and residents take shorter or longer periods of time to achieve proficiency. In addition, learner outcomes can be quite variable, as we have all experienced.
Even our methods of assessment may not adequately evaluate trainees’ skill sets. For example, most clerkships still rely heavily on the shelf exam5 as a surrogate for medical knowledge. As such, learners may conclude that testing performance trumps development of other professional skills.6 Efforts are being made to revamp evaluation systems to reflect mastery (such as Entrustable Professional Activities, or EPAs) toward competencies.7 Still, many institutions continue to rely on faculty evaluations that often reflect interpersonal dynamics rather than true critical thinking skills.6
Recognizing the above limitations, many educators have called for changing to outcome-based, or competency-based, training (CBME). CBME targets attainment of skills in performing concrete critical clinical activities,8 such as identifying unstable patients, providing initial management, and obtaining help. To be successful, supervisors must directly observe trainees, assess demonstrated skills, and provide feedback about progress.
Unfortunately, this considerable investment of time and effort is often poorly compensated. Additionally, unanswered questions remain. For example, how will residency programs continue to challenge physicians deemed “competent” in a required skill? What happens when a trainee is deficient and not appropriately progressing in a required skill? Is flexible training time part of the future of medical education? While CBME appears to be a more effective method of education, questions like these must be addressed during implementation.
Beyond the fact that hours worked cannot be used as a surrogate for competency, excessive unregulated work hours can be detrimental to learners, their supervisors, and patients. In 2003, the Accreditation Council for Graduate Medical Education (ACGME) implemented a major change in medical education: duty hour limitations. The premise that sleep-deprived providers are more prone to error is well established. However, controversy remains as to whether these regulations translate into improved patient care and provider well-being. Studies published following the ACGME change demonstrate increasing burnout among physicians,9-11 which has led some educators to explore the potential relationship between burnout and duty hour restrictions.
The recent “iCOMPARE” trial, which compared internal medicine (IM) residencies with “standard duty-hour” policies to those with “flexible” policies (that is, they did not specify limits on shift length or mandatory time off between shifts), supported a lack of correlation between hours worked and burnout.12 Researchers administered the Maslach Burnout Inventory to all participants.13 While those in the “flexible hours” arm reported greater dissatisfaction with the effect of the program on their personal lives, both groups reported significant burnout, with interns recording high scores in emotional exhaustion (79% in flexible programs vs. 72% in standard), depersonalization (75% vs. 72%), and lack of personal accomplishment (71% vs. 69%).
Disturbingly, these scores were not restricted to interns but were present in all residents. The good news? Limiting duty hours does not cause burnout. On the other hand, it does not protect from burnout. Trainee burnout appears to transcend the issue of hours worked. Clearly, we need to address the systemic flaws in our work environments that contribute to this epidemic. Nationwide, educators and organizations are continuing to define causes of burnout and test interventions to improve wellness.
A final front of change in medical education worth mentioning is the use of the electronic medical record (EMR). While the EMR has improved many aspects of patient care, its implementation is associated with decreased time spent with patients and parallels the rise in burnout. Another unforeseen consequence has been its disruptive impact on medical student documentation. A national survey of clerkship directors found that, while 64% of programs allowed students to use the EMR, only two-thirds of those programs permitted students to document electronically.14
Many institutions limit student access because of either liability concerns or the fact that student notes cannot be used to support medical billing. Concerning workarounds among preceptors, such as logging in students under their own credentials to write notes, have been identified.15 Yet medical students need to learn how to document a clinical encounter and maintain medical records.7,16 Authoring notes engages students, promotes a sense of patient ownership, and empowers them to feel like essential team members. Participating in the EMR also allows for critical feedback and skill development.
In 2016, the Society of Hospital Medicine joined several major internal medicine organizations in asking the federal government to reconsider guidelines prohibiting attendings from referring to medical student notes. In February 2018, the Centers for Medicare & Medicaid Services (CMS) revised its student documentation guidelines (see Box A), allowing teaching physicians to use all student documentation (not just Review of Systems, Family History, and Social History) for billable services.
While the guidelines officially went into effect in March 2018, many institutions are still fine-tuning their implementation, in part because of nonspecific policy language. For instance, if a student composes a note and a resident edits and signs it, can the attending physician simply cosign the resident note? Also, once a student has presented a case, can the attending see the patient and verify findings without the student present?
Despite the above challenges, the revision to CMS guidelines is a significant “win” and can potentially reduce the documentation burden on teaching physicians. With more oversight of their notes, the next generation of students will be encouraged to produce accurate, high-quality documentation.
In summary, these changes in the way we define competency, in duty hours, and in the use of the EMR demonstrate that medical education is continuously improving via robust critique and educator engagement in outcomes. We are fortunate to train in a system that respects the scientific method and utilizes data and critical events to drive important changes in practice. Understanding these changes might help hospitalists relate to the backgrounds and needs of learners. And who knows – maybe next time that intern will do a better job presenting!
Dr. Kwan is a hospitalist at the Veterans Affairs San Diego Healthcare System (VASDHS) and an associate professor at the University of California, San Diego, in the division of hospital medicine. He is the chair of the SHM Physicians in Training committee. Dr. Sebasky is an associate clinical professor at UCSD in the division of hospital medicine. Dr. Muchmore is a hematologist/oncologist and professor of clinical medicine in the department of medicine at UCSD and associate chief of staff for education at VASDHS.
References
1. Osler W. “The Hospital as a College.” In Aequanimitas. Osler W, Ed. (Philadelphia: P. Blakiston’s Son & Co., 1932).
2. Kohn LT, Corrigan JM, Donaldson MS, eds. To Err Is Human: Building a Safer Health Care System. (Washington: National Academies Press, 1999).
3. Ten Cate O. Competency-based postgraduate medical education: Past, present and future. GMS J Med Educ. 2017 Nov 15. doi: 10.3205/zma001146.
4. Carraccio C, Englander R, Van Melle E, et al. Advancing competency-based medical education: A charter for clinician–educators. Acad Med. 2016;91(5):645-9.
5. 2016 NBME Clinical Clerkship Subject Examination Survey.
6. Mehta NB, Hull AL, Young JB, et al. Just imagine: New paradigms for medical education. Acad Med. 2013;88(10):1418-23.
7. Fazio SB, Ledford CH, Aronowitz PB, et al. Competency-based medical education in the internal medicine clerkship: A report from the Alliance for Academic Internal Medicine Undergraduate Medical Education Task Force. Acad Med. 2018;93(3):421-7.
8. Ten Cate O, Scheele F. Competency-based postgraduate training: Can we bridge the gap between theory and clinical practice? Acad Med. 2007 Jun;82(6):542-7.
9. Dewa CS, Loong D, Bonato S, et al. The relationship between physician burnout and quality of healthcare in terms of safety and acceptability: A systematic review. BMJ Open. 2017. doi: 10.1136/bmjopen-2016-015141.
10. Hall LH, Johnson J, Watt I, et al. Healthcare Staff wellbeing, burnout, and patient safety: A systematic review. PLoS ONE. 2016. doi: 10.1371/journal.pone.0159015.
11. Salyers MP, Bonfils KA, Luther L, et al. The relationship between professional burnout and quality and safety in healthcare: A meta-analysis. Gen Intern Med. 2017 Apr; 32(4):475-82.
12. Desai SV, Asch DA, Bellini LM, et al. Education outcomes in a duty hour flexibility trial in internal medicine. N Engl J Med. 2018 378:1494-508.
13. Maslach C, Jackson SE, Leiter MP. Maslach burnout inventory manual. 3rd ed. (Palo Alto, CA: Consulting Psychologists Press, 1996).
14. Hammoud MM, Margo K, Christner JG, et al. Opportunities and challenges in integrating electronic health records into undergraduate medical education: A national survey of clerkship directors. Teach Learn Med. 2012;24(3):219-24.
15. White J, Anthony D, WinklerPrins V, et al. Electronic medical records, medical students, and ambulatory family physicians: A multi-institution study. Acad Med. 2017;92(10):1485-90.
16. Pageler NM, Friedman CP, Longhurst CA. Refocusing medical education in the EMR era. JAMA 2013;310(21):2249-50.
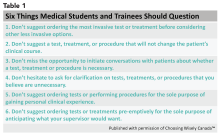
Box A
“Students may document services in the medical record. However, the teaching physician must verify in the medical record all student documentation or findings, including history, physical exam, and/or medical decision making. The teaching physician must personally perform (or re-perform) the physical exam and medical decision making activities of the E/M service being billed, but may verify any student documentation of them in the medical record, rather than re-documenting this work.”
A brave new world
A brave new world
It’s Monday morning, and your intern is presenting an overnight admission. Lost in the details of his disorganized introduction, your mind wanders. “Why doesn’t this intern know how to present? When I trained, all those admissions during long sleepless nights really taught me to do this right.” But can we equate hours worked with competency achieved? And if not, what is the alternative? This article introduces some major changes in medical education and their implications for hospitalists.
Most hospitalists trained in an educational system influenced by Sir William Osler. In the early 1900s, he introduced the natural method of teaching, positing that student exposure to patients and experience over time ensured that physicians in training would become competent doctors.1 His influence led to the current structure of medical education, which includes conventional third-year clerkships and time-limited rotations (such as a 2-week nephrology block).
While familiarity may be comforting, there are signs our current model of medical education is inefficient, inadequate, and obsolete.
For one, the traditional system is failing to adequately prepare physicians to provide safe and complex care. Reports, such as the Institute of Medicine’s (IOM) “To Err is Human,”2 describe a high rate of preventable errors, highlighting considerable room for improvement in training the next generation of physicians.3,4
Meanwhile, trainees are still largely being deemed ready for the workforce by length of training completed (for example, completion of four-year medical school) rather than a skill set distinctly achieved. Our system leaves little flexibility to individualize learner goals, which is significant given some students and residents take shorter or longer periods of time to achieve proficiency. In addition, learner outcomes can be quite variable, as we have all experienced.
Even our methods of assessment may not adequately evaluate trainees’ skill sets. For example, most clerkships still rely heavily on the shelf exam5 as a surrogate for medical knowledge. As such, learners may conclude that testing performance trumps development of other professional skills.6 Efforts are being made to revamp evaluation systems to reflect mastery (such as Entrustable Professional Activities, or EPAs) toward competencies.7 Still, many institutions continue to rely on faculty evaluations that often reflect interpersonal dynamics rather than true critical thinking skills.6
Recognizing the above limitations, many educators have called for changing to outcome-based, or competency-based, training (CBME). CBME targets attainment of skills in performing concrete critical clinical activities,8 such as identifying unstable patients, providing initial management, and obtaining help. To be successful, supervisors must directly observe trainees, assess demonstrated skills, and provide feedback about progress.
Unfortunately, this considerable investment of time and effort is often poorly compensated. Additionally, unanswered questions remain. For example, how will residency programs continue to challenge physicians deemed “competent” in a required skill? What happens when a trainee is deficient and not appropriately progressing in a required skill? Is flexible training time part of the future of medical education? While CBME appears to be a more effective method of education, questions like these must be addressed during implementation.
Beyond the fact that hours worked cannot be used as a surrogate for competency, excessive unregulated work hours can be detrimental to learners, their supervisors, and patients. In 2003, the Accreditation Council for Graduate Medical Education (ACGME) implemented a major change in medical education: duty hour limitations. The premise that sleep-deprived providers are more prone to error is well established. However, controversy remains as to whether these regulations translate into improved patient care and provider well-being. Studies published following the ACGME change demonstrate increasing burnout among physicians,9-11 which has led some educators to explore the potential relationship between burnout and duty hour restrictions.
The recent “iCOMPARE” trial, which compared internal medicine (IM) residencies with “standard duty-hour” policies to those with “flexible” policies (that is, they did not specify limits on shift length or mandatory time off between shifts), supported a lack of correlation between hours worked and burnout.12 Researchers administered the Maslach Burnout Inventory to all participants.13 While those in the “flexible hours” arm reported greater dissatisfaction with the effect of the program on their personal lives, both groups reported significant burnout, with interns recording high scores in emotional exhaustion (79% in flexible programs vs. 72% in standard), depersonalization (75% vs. 72%), and lack of personal accomplishment (71% vs. 69%).
Disturbingly, these scores were not restricted to interns but were present in all residents. The good news? Limiting duty hours does not cause burnout. On the other hand, it does not protect from burnout. Trainee burnout appears to transcend the issue of hours worked. Clearly, we need to address the systemic flaws in our work environments that contribute to this epidemic. Nationwide, educators and organizations are continuing to define causes of burnout and test interventions to improve wellness.
A final front of change in medical education worth mentioning is the use of the electronic medical record (EMR). While the EMR has improved many aspects of patient care, its implementation is associated with decreased time spent with patients and parallels the rise in burnout. Another unforeseen consequence has been its disruptive impact on medical student documentation. A national survey of clerkship directors found that, while 64% of programs allowed students to use the EMR, only two-thirds of those programs permitted students to document electronically.14
Many institutions limit student access because of either liability concerns or the fact that student notes cannot be used to support medical billing. Concerning workarounds among preceptors, such as logging in students under their own credentials to write notes, have been identified.15 Yet medical students need to learn how to document a clinical encounter and maintain medical records.7,16 Authoring notes engages students, promotes a sense of patient ownership, and empowers them to feel like essential team members. Participating in the EMR also allows for critical feedback and skill development.
In 2016, the Society of Hospital Medicine joined several major internal medicine organizations in asking the federal government to reconsider guidelines prohibiting attendings from referring to medical student notes. In February 2018, the Centers for Medicare & Medicaid Services (CMS) revised its student documentation guidelines (see Box A), allowing teaching physicians to use all student documentation (not just Review of Systems, Family History, and Social History) for billable services.
While the guidelines officially went into effect in March 2018, many institutions are still fine-tuning their implementation, in part because of nonspecific policy language. For instance, if a student composes a note and a resident edits and signs it, can the attending physician simply cosign the resident note? Also, once a student has presented a case, can the attending see the patient and verify findings without the student present?
Despite the above challenges, the revision to CMS guidelines is a significant “win” and can potentially reduce the documentation burden on teaching physicians. With more oversight of their notes, the next generation of students will be encouraged to produce accurate, high-quality documentation.
In summary, these changes in the way we define competency, in duty hours, and in the use of the EMR demonstrate that medical education is continuously improving via robust critique and educator engagement in outcomes. We are fortunate to train in a system that respects the scientific method and utilizes data and critical events to drive important changes in practice. Understanding these changes might help hospitalists relate to the backgrounds and needs of learners. And who knows – maybe next time that intern will do a better job presenting!
Dr. Kwan is a hospitalist at the Veterans Affairs San Diego Healthcare System (VASDHS) and an associate professor at the University of California, San Diego, in the division of hospital medicine. He is the chair of the SHM Physicians in Training committee. Dr. Sebasky is an associate clinical professor at UCSD in the division of hospital medicine. Dr. Muchmore is a hematologist/oncologist and professor of clinical medicine in the department of medicine at UCSD and associate chief of staff for education at VASDHS.
References
1. Osler W. “The Hospital as a College.” In Aequanimitas. Osler W, Ed. (Philadelphia: P. Blakiston’s Son & Co., 1932).
2. Kohn LT, Corrigan JM, Donaldson MS, eds. To Err Is Human: Building a Safer Health Care System. (Washington: National Academies Press, 1999).
3. Ten Cate O. Competency-based postgraduate medical education: Past, present and future. GMS J Med Educ. 2017 Nov 15. doi: 10.3205/zma001146.
4. Carraccio C, Englander R, Van Melle E, et al. Advancing competency-based medical education: A charter for clinician–educators. Acad Med. 2016;91(5):645-9.
5. 2016 NBME Clinical Clerkship Subject Examination Survey.
6. Mehta NB, Hull AL, Young JB, et al. Just imagine: New paradigms for medical education. Acad Med. 2013;88(10):1418-23.
7. Fazio SB, Ledford CH, Aronowitz PB, et al. Competency-based medical education in the internal medicine clerkship: A report from the Alliance for Academic Internal Medicine Undergraduate Medical Education Task Force. Acad Med. 2018;93(3):421-7.
8. Ten Cate O, Scheele F. Competency-based postgraduate training: Can we bridge the gap between theory and clinical practice? Acad Med. 2007 Jun;82(6):542-7.
9. Dewa CS, Loong D, Bonato S, et al. The relationship between physician burnout and quality of healthcare in terms of safety and acceptability: A systematic review. BMJ Open. 2017. doi: 10.1136/bmjopen-2016-015141.
10. Hall LH, Johnson J, Watt I, et al. Healthcare Staff wellbeing, burnout, and patient safety: A systematic review. PLoS ONE. 2016. doi: 10.1371/journal.pone.0159015.
11. Salyers MP, Bonfils KA, Luther L, et al. The relationship between professional burnout and quality and safety in healthcare: A meta-analysis. Gen Intern Med. 2017 Apr; 32(4):475-82.
12. Desai SV, Asch DA, Bellini LM, et al. Education outcomes in a duty hour flexibility trial in internal medicine. N Engl J Med. 2018 378:1494-508.
13. Maslach C, Jackson SE, Leiter MP. Maslach burnout inventory manual. 3rd ed. (Palo Alto, CA: Consulting Psychologists Press, 1996).
14. Hammoud MM, Margo K, Christner JG, et al. Opportunities and challenges in integrating electronic health records into undergraduate medical education: A national survey of clerkship directors. Teach Learn Med. 2012;24(3):219-24.
15. White J, Anthony D, WinklerPrins V, et al. Electronic medical records, medical students, and ambulatory family physicians: A multi-institution study. Acad Med. 2017;92(10):1485-90.
16. Pageler NM, Friedman CP, Longhurst CA. Refocusing medical education in the EMR era. JAMA 2013;310(21):2249-50.
Box A
“Students may document services in the medical record. However, the teaching physician must verify in the medical record all student documentation or findings, including history, physical exam, and/or medical decision making. The teaching physician must personally perform (or re-perform) the physical exam and medical decision making activities of the E/M service being billed, but may verify any student documentation of them in the medical record, rather than re-documenting this work.”
It’s Monday morning, and your intern is presenting an overnight admission. Lost in the details of his disorganized introduction, your mind wanders. “Why doesn’t this intern know how to present? When I trained, all those admissions during long sleepless nights really taught me to do this right.” But can we equate hours worked with competency achieved? And if not, what is the alternative? This article introduces some major changes in medical education and their implications for hospitalists.
Most hospitalists trained in an educational system influenced by Sir William Osler. In the early 1900s, he introduced the natural method of teaching, positing that student exposure to patients and experience over time ensured that physicians in training would become competent doctors.1 His influence led to the current structure of medical education, which includes conventional third-year clerkships and time-limited rotations (such as a 2-week nephrology block).
While familiarity may be comforting, there are signs our current model of medical education is inefficient, inadequate, and obsolete.
For one, the traditional system is failing to adequately prepare physicians to provide safe and complex care. Reports, such as the Institute of Medicine’s (IOM) “To Err is Human,”2 describe a high rate of preventable errors, highlighting considerable room for improvement in training the next generation of physicians.3,4
Meanwhile, trainees are still largely being deemed ready for the workforce by length of training completed (for example, completion of four-year medical school) rather than a skill set distinctly achieved. Our system leaves little flexibility to individualize learner goals, which is significant given some students and residents take shorter or longer periods of time to achieve proficiency. In addition, learner outcomes can be quite variable, as we have all experienced.
Even our methods of assessment may not adequately evaluate trainees’ skill sets. For example, most clerkships still rely heavily on the shelf exam5 as a surrogate for medical knowledge. As such, learners may conclude that testing performance trumps development of other professional skills.6 Efforts are being made to revamp evaluation systems to reflect mastery (such as Entrustable Professional Activities, or EPAs) toward competencies.7 Still, many institutions continue to rely on faculty evaluations that often reflect interpersonal dynamics rather than true critical thinking skills.6
Recognizing the above limitations, many educators have called for changing to outcome-based, or competency-based, training (CBME). CBME targets attainment of skills in performing concrete critical clinical activities,8 such as identifying unstable patients, providing initial management, and obtaining help. To be successful, supervisors must directly observe trainees, assess demonstrated skills, and provide feedback about progress.
Unfortunately, this considerable investment of time and effort is often poorly compensated. Additionally, unanswered questions remain. For example, how will residency programs continue to challenge physicians deemed “competent” in a required skill? What happens when a trainee is deficient and not appropriately progressing in a required skill? Is flexible training time part of the future of medical education? While CBME appears to be a more effective method of education, questions like these must be addressed during implementation.
Beyond the fact that hours worked cannot be used as a surrogate for competency, excessive unregulated work hours can be detrimental to learners, their supervisors, and patients. In 2003, the Accreditation Council for Graduate Medical Education (ACGME) implemented a major change in medical education: duty hour limitations. The premise that sleep-deprived providers are more prone to error is well established. However, controversy remains as to whether these regulations translate into improved patient care and provider well-being. Studies published following the ACGME change demonstrate increasing burnout among physicians,9-11 which has led some educators to explore the potential relationship between burnout and duty hour restrictions.
The recent “iCOMPARE” trial, which compared internal medicine (IM) residencies with “standard duty-hour” policies to those with “flexible” policies (that is, they did not specify limits on shift length or mandatory time off between shifts), supported a lack of correlation between hours worked and burnout.12 Researchers administered the Maslach Burnout Inventory to all participants.13 While those in the “flexible hours” arm reported greater dissatisfaction with the effect of the program on their personal lives, both groups reported significant burnout, with interns recording high scores in emotional exhaustion (79% in flexible programs vs. 72% in standard), depersonalization (75% vs. 72%), and lack of personal accomplishment (71% vs. 69%).
Disturbingly, these scores were not restricted to interns but were present in all residents. The good news? Limiting duty hours does not cause burnout. On the other hand, it does not protect from burnout. Trainee burnout appears to transcend the issue of hours worked. Clearly, we need to address the systemic flaws in our work environments that contribute to this epidemic. Nationwide, educators and organizations are continuing to define causes of burnout and test interventions to improve wellness.
A final front of change in medical education worth mentioning is the use of the electronic medical record (EMR). While the EMR has improved many aspects of patient care, its implementation is associated with decreased time spent with patients and parallels the rise in burnout. Another unforeseen consequence has been its disruptive impact on medical student documentation. A national survey of clerkship directors found that, while 64% of programs allowed students to use the EMR, only two-thirds of those programs permitted students to document electronically.14
Many institutions limit student access because of either liability concerns or the fact that student notes cannot be used to support medical billing. Concerning workarounds among preceptors, such as logging in students under their own credentials to write notes, have been identified.15 Yet medical students need to learn how to document a clinical encounter and maintain medical records.7,16 Authoring notes engages students, promotes a sense of patient ownership, and empowers them to feel like essential team members. Participating in the EMR also allows for critical feedback and skill development.
In 2016, the Society of Hospital Medicine joined several major internal medicine organizations in asking the federal government to reconsider guidelines prohibiting attendings from referring to medical student notes. In February 2018, the Centers for Medicare & Medicaid Services (CMS) revised its student documentation guidelines (see Box A), allowing teaching physicians to use all student documentation (not just Review of Systems, Family History, and Social History) for billable services.
While the guidelines officially went into effect in March 2018, many institutions are still fine-tuning their implementation, in part because of nonspecific policy language. For instance, if a student composes a note and a resident edits and signs it, can the attending physician simply cosign the resident note? Also, once a student has presented a case, can the attending see the patient and verify findings without the student present?
Despite the above challenges, the revision to CMS guidelines is a significant “win” and can potentially reduce the documentation burden on teaching physicians. With more oversight of their notes, the next generation of students will be encouraged to produce accurate, high-quality documentation.
In summary, these changes in the way we define competency, in duty hours, and in the use of the EMR demonstrate that medical education is continuously improving via robust critique and educator engagement in outcomes. We are fortunate to train in a system that respects the scientific method and utilizes data and critical events to drive important changes in practice. Understanding these changes might help hospitalists relate to the backgrounds and needs of learners. And who knows – maybe next time that intern will do a better job presenting!
Dr. Kwan is a hospitalist at the Veterans Affairs San Diego Healthcare System (VASDHS) and an associate professor at the University of California, San Diego, in the division of hospital medicine. He is the chair of the SHM Physicians in Training committee. Dr. Sebasky is an associate clinical professor at UCSD in the division of hospital medicine. Dr. Muchmore is a hematologist/oncologist and professor of clinical medicine in the department of medicine at UCSD and associate chief of staff for education at VASDHS.
References
1. Osler W. “The Hospital as a College.” In Aequanimitas. Osler W, Ed. (Philadelphia: P. Blakiston’s Son & Co., 1932).
2. Kohn LT, Corrigan JM, Donaldson MS, eds. To Err Is Human: Building a Safer Health Care System. (Washington: National Academies Press, 1999).
3. Ten Cate O. Competency-based postgraduate medical education: Past, present and future. GMS J Med Educ. 2017 Nov 15. doi: 10.3205/zma001146.
4. Carraccio C, Englander R, Van Melle E, et al. Advancing competency-based medical education: A charter for clinician–educators. Acad Med. 2016;91(5):645-9.
5. 2016 NBME Clinical Clerkship Subject Examination Survey.
6. Mehta NB, Hull AL, Young JB, et al. Just imagine: New paradigms for medical education. Acad Med. 2013;88(10):1418-23.
7. Fazio SB, Ledford CH, Aronowitz PB, et al. Competency-based medical education in the internal medicine clerkship: A report from the Alliance for Academic Internal Medicine Undergraduate Medical Education Task Force. Acad Med. 2018;93(3):421-7.
8. Ten Cate O, Scheele F. Competency-based postgraduate training: Can we bridge the gap between theory and clinical practice? Acad Med. 2007 Jun;82(6):542-7.
9. Dewa CS, Loong D, Bonato S, et al. The relationship between physician burnout and quality of healthcare in terms of safety and acceptability: A systematic review. BMJ Open. 2017. doi: 10.1136/bmjopen-2016-015141.
10. Hall LH, Johnson J, Watt I, et al. Healthcare Staff wellbeing, burnout, and patient safety: A systematic review. PLoS ONE. 2016. doi: 10.1371/journal.pone.0159015.
11. Salyers MP, Bonfils KA, Luther L, et al. The relationship between professional burnout and quality and safety in healthcare: A meta-analysis. Gen Intern Med. 2017 Apr; 32(4):475-82.
12. Desai SV, Asch DA, Bellini LM, et al. Education outcomes in a duty hour flexibility trial in internal medicine. N Engl J Med. 2018 378:1494-508.
13. Maslach C, Jackson SE, Leiter MP. Maslach burnout inventory manual. 3rd ed. (Palo Alto, CA: Consulting Psychologists Press, 1996).
14. Hammoud MM, Margo K, Christner JG, et al. Opportunities and challenges in integrating electronic health records into undergraduate medical education: A national survey of clerkship directors. Teach Learn Med. 2012;24(3):219-24.
15. White J, Anthony D, WinklerPrins V, et al. Electronic medical records, medical students, and ambulatory family physicians: A multi-institution study. Acad Med. 2017;92(10):1485-90.
16. Pageler NM, Friedman CP, Longhurst CA. Refocusing medical education in the EMR era. JAMA 2013;310(21):2249-50.
Box A
“Students may document services in the medical record. However, the teaching physician must verify in the medical record all student documentation or findings, including history, physical exam, and/or medical decision making. The teaching physician must personally perform (or re-perform) the physical exam and medical decision making activities of the E/M service being billed, but may verify any student documentation of them in the medical record, rather than re-documenting this work.”
Laurence Wellikson, MD, MHM, announces retirement as CEO of Society of Hospital Medicine
Society recognizes Dr. Wellikson’s leadership, retains Spencer Stuart for successor search
Philadelphia – After serving as the first and only chief executive officer of the Society of Hospital Medicine since January of 2000, Laurence Wellikson, MD, MHM, has announced his retirement effective on Dec. 31, 2020. In parallel, the SHM Board of Directors have commenced a search for his successor.
“When I began as CEO 20 years ago, SHM – then known as the National Association of Inpatient Physicians – was a young national organization with approximately 500 members, and there was minimal understanding as to the value that hospitalists could add to their health communities,” Dr. Wellikson said. “I am proud to say that, nearly 20 years later, SHM boasts a growing membership of more than 17,000, and hospitalists are on the front line of innovation as a driving force in improving patient care.”
SHM has not only grown its membership but also its diverse portfolio of offerings for hospital medicine professionals under Dr. Wellikson’s leadership. Its first annual conference welcomed approximately 300 attendees; the most recent conference, Hospital Medicine 2019, saw that number increase more than tenfold to nearly 4,000. Its conferences, publications, online education, chapter program, advocacy efforts, quality improvement programs, and more have evolved significantly to ensure hospitalists at all stages of their careers – and those who support them – have access to resources to keep them up to date and demonstrate their value in America’s health care system.
During Dr. Wellikson’s tenure, SHM launched its peer-reviewed Journal of Hospital Medicine, the premier, ISI-indexed publication for the specialty, successfully advocated for a Focused Practice in Hospital Medicine certification option and C6 hospitalist specialty code, and earned the John M. Eisenberg Patient Safety and Quality Award for its quality improvement programs. These are just a few of the noteworthy accomplishments that have elevated SHM as a key partner for hospitalists and their institutions.
To assist with the search for SHM’s next CEO, the society has retained Spencer Stuart, a leading global executive and leadership advisory firm. The search process is being overseen by a diverse search committee led by the president-elect of SHM’s Board of Directors, Danielle Scheurer, MD, MSCR, SFHM.
“On behalf of the society and its members, I want to extend a sincere thank you to Larry for his years of dedication and service to SHM, its staff, and the hospital medicine professionals we serve,” said Christopher Frost, MD, SFHM, president of SHM’s Board of Directors. “His legacy will allow SHM to continue its growth trajectory through key programs and services supporting members’ needs for years to come. Larry has taken the specialty of hospital medicine and created a movement in SHM, where the entire hospital medicine team can come for education, community, and betterment of the care we provide to our patients. We are indebted to him beyond words.”
Those who are interested in leading SHM into the future as its next CEO are encouraged to contact either Jennifer P. Heenan ([email protected]) or Mark Furman, MD ([email protected]).
Society recognizes Dr. Wellikson’s leadership, retains Spencer Stuart for successor search
Society recognizes Dr. Wellikson’s leadership, retains Spencer Stuart for successor search
Philadelphia – After serving as the first and only chief executive officer of the Society of Hospital Medicine since January of 2000, Laurence Wellikson, MD, MHM, has announced his retirement effective on Dec. 31, 2020. In parallel, the SHM Board of Directors have commenced a search for his successor.
“When I began as CEO 20 years ago, SHM – then known as the National Association of Inpatient Physicians – was a young national organization with approximately 500 members, and there was minimal understanding as to the value that hospitalists could add to their health communities,” Dr. Wellikson said. “I am proud to say that, nearly 20 years later, SHM boasts a growing membership of more than 17,000, and hospitalists are on the front line of innovation as a driving force in improving patient care.”
SHM has not only grown its membership but also its diverse portfolio of offerings for hospital medicine professionals under Dr. Wellikson’s leadership. Its first annual conference welcomed approximately 300 attendees; the most recent conference, Hospital Medicine 2019, saw that number increase more than tenfold to nearly 4,000. Its conferences, publications, online education, chapter program, advocacy efforts, quality improvement programs, and more have evolved significantly to ensure hospitalists at all stages of their careers – and those who support them – have access to resources to keep them up to date and demonstrate their value in America’s health care system.
During Dr. Wellikson’s tenure, SHM launched its peer-reviewed Journal of Hospital Medicine, the premier, ISI-indexed publication for the specialty, successfully advocated for a Focused Practice in Hospital Medicine certification option and C6 hospitalist specialty code, and earned the John M. Eisenberg Patient Safety and Quality Award for its quality improvement programs. These are just a few of the noteworthy accomplishments that have elevated SHM as a key partner for hospitalists and their institutions.
To assist with the search for SHM’s next CEO, the society has retained Spencer Stuart, a leading global executive and leadership advisory firm. The search process is being overseen by a diverse search committee led by the president-elect of SHM’s Board of Directors, Danielle Scheurer, MD, MSCR, SFHM.
“On behalf of the society and its members, I want to extend a sincere thank you to Larry for his years of dedication and service to SHM, its staff, and the hospital medicine professionals we serve,” said Christopher Frost, MD, SFHM, president of SHM’s Board of Directors. “His legacy will allow SHM to continue its growth trajectory through key programs and services supporting members’ needs for years to come. Larry has taken the specialty of hospital medicine and created a movement in SHM, where the entire hospital medicine team can come for education, community, and betterment of the care we provide to our patients. We are indebted to him beyond words.”
Those who are interested in leading SHM into the future as its next CEO are encouraged to contact either Jennifer P. Heenan ([email protected]) or Mark Furman, MD ([email protected]).
Philadelphia – After serving as the first and only chief executive officer of the Society of Hospital Medicine since January of 2000, Laurence Wellikson, MD, MHM, has announced his retirement effective on Dec. 31, 2020. In parallel, the SHM Board of Directors have commenced a search for his successor.
“When I began as CEO 20 years ago, SHM – then known as the National Association of Inpatient Physicians – was a young national organization with approximately 500 members, and there was minimal understanding as to the value that hospitalists could add to their health communities,” Dr. Wellikson said. “I am proud to say that, nearly 20 years later, SHM boasts a growing membership of more than 17,000, and hospitalists are on the front line of innovation as a driving force in improving patient care.”
SHM has not only grown its membership but also its diverse portfolio of offerings for hospital medicine professionals under Dr. Wellikson’s leadership. Its first annual conference welcomed approximately 300 attendees; the most recent conference, Hospital Medicine 2019, saw that number increase more than tenfold to nearly 4,000. Its conferences, publications, online education, chapter program, advocacy efforts, quality improvement programs, and more have evolved significantly to ensure hospitalists at all stages of their careers – and those who support them – have access to resources to keep them up to date and demonstrate their value in America’s health care system.
During Dr. Wellikson’s tenure, SHM launched its peer-reviewed Journal of Hospital Medicine, the premier, ISI-indexed publication for the specialty, successfully advocated for a Focused Practice in Hospital Medicine certification option and C6 hospitalist specialty code, and earned the John M. Eisenberg Patient Safety and Quality Award for its quality improvement programs. These are just a few of the noteworthy accomplishments that have elevated SHM as a key partner for hospitalists and their institutions.
To assist with the search for SHM’s next CEO, the society has retained Spencer Stuart, a leading global executive and leadership advisory firm. The search process is being overseen by a diverse search committee led by the president-elect of SHM’s Board of Directors, Danielle Scheurer, MD, MSCR, SFHM.
“On behalf of the society and its members, I want to extend a sincere thank you to Larry for his years of dedication and service to SHM, its staff, and the hospital medicine professionals we serve,” said Christopher Frost, MD, SFHM, president of SHM’s Board of Directors. “His legacy will allow SHM to continue its growth trajectory through key programs and services supporting members’ needs for years to come. Larry has taken the specialty of hospital medicine and created a movement in SHM, where the entire hospital medicine team can come for education, community, and betterment of the care we provide to our patients. We are indebted to him beyond words.”
Those who are interested in leading SHM into the future as its next CEO are encouraged to contact either Jennifer P. Heenan ([email protected]) or Mark Furman, MD ([email protected]).
Maximize your leadership in academic hospital medicine
AHA Level 2 course now available
Over the past 2 decades, hospital medicine has grown from a nascent collection of hospitalists to one of the fastest growing specialties, with more than 60,000 active practitioners today.
Ten years ago, the need for mentoring and growth of a new generation of young academic faculty led to the development of the first Academic Hospitalist Academy (AHA) through the coordinated efforts of the Society of Hospital Medicine, the Society of General Internal Medicine, and the Association of Clinical Leaders of General Internal Medicine.
As modern medicine moves at an increasing pace, the intersection of patient care, research, and education has opened further opportunities for fostering the expertise of hospital medicine practitioners. The next level of training is now available with the advent of AHA’s Level 2 course.
Ever wonder why the new clinical service you’ve designed to improve physician and patient efficiency isn’t functioning like it did in the beginning? Patients are staying longer in the hospital, and physicians are working harder. The principles of change management, personal leadership styles, and adult learning will be covered in the AHA Level 2 course. How do I get my project funded and then what do I do with the results? Keys to negotiating for time and resources as well as the skills to write and disseminate your work are integrated into the curriculum.
Participants will be engaged in an interactive course designed around the challenges of practicing and leading in an academic environment. AHA Level 2 aims to help attendees – regardless of their areas of interest – identify and acquire the skills necessary to advance their career, describe the business and cultural landscape of academic health systems, and learn how to leverage that knowledge; to list resources and techniques to continue to further build their skills, and identify and pursue their unique scholarly niche.
Based on the success of AHA’s Level 1 course and the feedback from the almost 1,000 participants who have attended, AHA Level 2 is a 2.5-day course that will allow for the exchange of ideas and skills from nationally regarded faculty and fellow attendees. Through plenary sessions, workshops, small groups, and networking opportunities, attendees will be immersed in the realm of modern academic hospital medicine. The new course is offered in parallel with AHA Level 1 at the Inverness Resort, outside of Denver, on Sept. 10-12, 2019.
The course will leave attendees with an individualized career plan and enhance their area of expertise. The lessons learned and shared will allow participants to return to their institutions and continue to lead in the areas of patient care, financial resourcefulness, and the education of current and future generations of hospital medicine specialists.
Dr. O’Dorisio is a Med-Peds hospitalist at the Ohio State University, Columbus.
AHA Level 2 course now available
AHA Level 2 course now available
Over the past 2 decades, hospital medicine has grown from a nascent collection of hospitalists to one of the fastest growing specialties, with more than 60,000 active practitioners today.
Ten years ago, the need for mentoring and growth of a new generation of young academic faculty led to the development of the first Academic Hospitalist Academy (AHA) through the coordinated efforts of the Society of Hospital Medicine, the Society of General Internal Medicine, and the Association of Clinical Leaders of General Internal Medicine.
As modern medicine moves at an increasing pace, the intersection of patient care, research, and education has opened further opportunities for fostering the expertise of hospital medicine practitioners. The next level of training is now available with the advent of AHA’s Level 2 course.
Ever wonder why the new clinical service you’ve designed to improve physician and patient efficiency isn’t functioning like it did in the beginning? Patients are staying longer in the hospital, and physicians are working harder. The principles of change management, personal leadership styles, and adult learning will be covered in the AHA Level 2 course. How do I get my project funded and then what do I do with the results? Keys to negotiating for time and resources as well as the skills to write and disseminate your work are integrated into the curriculum.
Participants will be engaged in an interactive course designed around the challenges of practicing and leading in an academic environment. AHA Level 2 aims to help attendees – regardless of their areas of interest – identify and acquire the skills necessary to advance their career, describe the business and cultural landscape of academic health systems, and learn how to leverage that knowledge; to list resources and techniques to continue to further build their skills, and identify and pursue their unique scholarly niche.
Based on the success of AHA’s Level 1 course and the feedback from the almost 1,000 participants who have attended, AHA Level 2 is a 2.5-day course that will allow for the exchange of ideas and skills from nationally regarded faculty and fellow attendees. Through plenary sessions, workshops, small groups, and networking opportunities, attendees will be immersed in the realm of modern academic hospital medicine. The new course is offered in parallel with AHA Level 1 at the Inverness Resort, outside of Denver, on Sept. 10-12, 2019.
The course will leave attendees with an individualized career plan and enhance their area of expertise. The lessons learned and shared will allow participants to return to their institutions and continue to lead in the areas of patient care, financial resourcefulness, and the education of current and future generations of hospital medicine specialists.
Dr. O’Dorisio is a Med-Peds hospitalist at the Ohio State University, Columbus.
Over the past 2 decades, hospital medicine has grown from a nascent collection of hospitalists to one of the fastest growing specialties, with more than 60,000 active practitioners today.
Ten years ago, the need for mentoring and growth of a new generation of young academic faculty led to the development of the first Academic Hospitalist Academy (AHA) through the coordinated efforts of the Society of Hospital Medicine, the Society of General Internal Medicine, and the Association of Clinical Leaders of General Internal Medicine.
As modern medicine moves at an increasing pace, the intersection of patient care, research, and education has opened further opportunities for fostering the expertise of hospital medicine practitioners. The next level of training is now available with the advent of AHA’s Level 2 course.
Ever wonder why the new clinical service you’ve designed to improve physician and patient efficiency isn’t functioning like it did in the beginning? Patients are staying longer in the hospital, and physicians are working harder. The principles of change management, personal leadership styles, and adult learning will be covered in the AHA Level 2 course. How do I get my project funded and then what do I do with the results? Keys to negotiating for time and resources as well as the skills to write and disseminate your work are integrated into the curriculum.
Participants will be engaged in an interactive course designed around the challenges of practicing and leading in an academic environment. AHA Level 2 aims to help attendees – regardless of their areas of interest – identify and acquire the skills necessary to advance their career, describe the business and cultural landscape of academic health systems, and learn how to leverage that knowledge; to list resources and techniques to continue to further build their skills, and identify and pursue their unique scholarly niche.
Based on the success of AHA’s Level 1 course and the feedback from the almost 1,000 participants who have attended, AHA Level 2 is a 2.5-day course that will allow for the exchange of ideas and skills from nationally regarded faculty and fellow attendees. Through plenary sessions, workshops, small groups, and networking opportunities, attendees will be immersed in the realm of modern academic hospital medicine. The new course is offered in parallel with AHA Level 1 at the Inverness Resort, outside of Denver, on Sept. 10-12, 2019.
The course will leave attendees with an individualized career plan and enhance their area of expertise. The lessons learned and shared will allow participants to return to their institutions and continue to lead in the areas of patient care, financial resourcefulness, and the education of current and future generations of hospital medicine specialists.
Dr. O’Dorisio is a Med-Peds hospitalist at the Ohio State University, Columbus.
Hospitalist movers and shakers – July 2019
Christopher Moriates, MD, has been named executive director of the nonprofit health care organization Costs of Care (Boston). He replaces Neel Shah, MD, who was tabbed chairperson of the board.
Dr. Moriates serves a number of roles at the University of Texas at Austin. He is the assistant dean for health care value; associate chair for quality, safety and value; and associate professor of internal medicine.
In his role at Costs of Care, Dr. Moriates will direct an organization that uses feedback and stories from frontline physicians to help health systems provide high-quality care at lower costs.
Kai Mebust, MD, was recently named the new associate chief of medicine at Bassett Hospital (Cooperstown, N.Y.), where he has worked the past 15 years as a hospitalist and internist, serving as chief of hospitalists for the last decade. Dr. Mebust also completed his internship and residency at Bassett, and he is a fellow with the Society of Hospital Medicine.
Dr. Mebust will work closely with Dr. Charles Hyman, the center’s physician in chief, who is leaving the role at the end of the calendar year. Dr. Mebust will oversee inpatient services and be part of the transition process when Dr. Hyman departs.
Ronak Bhimani, MD, has been appointed chief medical officer at Lower Bucks Hospital (Bristol, Pa.). Dr. Bhimani moves over from Suburban Community Hospital (Norristown, Pa.), where he served as an academic hospitalist the past 2 years.
Previously, Dr. Bhimani was medical director of Kindred/Avalon Hospice and a core faculty member in the internal medicine program for residents at Suburban Community.
Danielle Prince, MD, was recently named associate medical director at St. Luke’s Siouxland PACE (Sioux City, Iowa), an affiliate of UnityPoint Health. Dr. Prince is a practicing hospitalist at UnityPoint Health St. Luke’s and served previously in as a family physician while working as chief medical informatics officer at Mercy Medical Center (Sioux City).
At Siouxland PACE, Dr. Prince will assist in managing the full-service care of elderly patients, including home health, specialty care, medications, transportation, and other therapies.
Alex Rankin, MD, has been named the new associate chief medical officer for the University of New Mexico Health Transfer Center and Patient Throughput in Albuquerque. A hospitalist with UNMH’s Family and Community Medicine department, Dr. Rankin was previously the medical director at the system’s 3 North facility since 2014.
Dr. Rankin came to UNMH after working for hospitals in Colorado and Nebraska and is a founding member of the UNMH patient flow committee, striving to improve patient care processes throughout the institution.
Tom Guirkin, MD, has been appointed vice president of medical affairs for Virginia Commonwealth University Community Memorial Hospital (South Hill, Va.). Dr. Guirkin, a Virginia native, returns to his home state after most recently overseeing the hospitalist group at Saint Francis Health System (Tulsa, Okla.).
Dr. Guirkin will have the opportunity to continue practicing medicine at CMH while helping to manage the quality management side of the business. He received his MBA from Virginia Commonwealth, working for James River Hospitalist Group in Richmond at the same time.
Alteon Health (Germantown, Md.) has become the manager of hospitalist services for three facilities in Maryland and Ohio, including Carroll Hospital (Westminster, Md.), Washington Adventist Hospital (Takoma Park, Md.), and University Hospitals Cleveland Medical Center.
At Carroll, Alteon physicians will provide critical care services in addition to hospitalist duties. Alteon has been Carroll’s emergency medicine provider for more than two decades.
At Washington Adventist, Alteon will take over the hospitalist program, adding to the emergency medicine services it has provided since 1991 and critical care services it has managed since 1996.
At UH Cleveland, Alteon will assume hospitalist management at its third University Hospitals facility. Alteon controls emergency medicine at 14 UH locations as well. UH Cleveland is an affiliate of Case Western Reserve University.
Christopher Moriates, MD, has been named executive director of the nonprofit health care organization Costs of Care (Boston). He replaces Neel Shah, MD, who was tabbed chairperson of the board.
Dr. Moriates serves a number of roles at the University of Texas at Austin. He is the assistant dean for health care value; associate chair for quality, safety and value; and associate professor of internal medicine.
In his role at Costs of Care, Dr. Moriates will direct an organization that uses feedback and stories from frontline physicians to help health systems provide high-quality care at lower costs.
Kai Mebust, MD, was recently named the new associate chief of medicine at Bassett Hospital (Cooperstown, N.Y.), where he has worked the past 15 years as a hospitalist and internist, serving as chief of hospitalists for the last decade. Dr. Mebust also completed his internship and residency at Bassett, and he is a fellow with the Society of Hospital Medicine.
Dr. Mebust will work closely with Dr. Charles Hyman, the center’s physician in chief, who is leaving the role at the end of the calendar year. Dr. Mebust will oversee inpatient services and be part of the transition process when Dr. Hyman departs.
Ronak Bhimani, MD, has been appointed chief medical officer at Lower Bucks Hospital (Bristol, Pa.). Dr. Bhimani moves over from Suburban Community Hospital (Norristown, Pa.), where he served as an academic hospitalist the past 2 years.
Previously, Dr. Bhimani was medical director of Kindred/Avalon Hospice and a core faculty member in the internal medicine program for residents at Suburban Community.
Danielle Prince, MD, was recently named associate medical director at St. Luke’s Siouxland PACE (Sioux City, Iowa), an affiliate of UnityPoint Health. Dr. Prince is a practicing hospitalist at UnityPoint Health St. Luke’s and served previously in as a family physician while working as chief medical informatics officer at Mercy Medical Center (Sioux City).
At Siouxland PACE, Dr. Prince will assist in managing the full-service care of elderly patients, including home health, specialty care, medications, transportation, and other therapies.
Alex Rankin, MD, has been named the new associate chief medical officer for the University of New Mexico Health Transfer Center and Patient Throughput in Albuquerque. A hospitalist with UNMH’s Family and Community Medicine department, Dr. Rankin was previously the medical director at the system’s 3 North facility since 2014.
Dr. Rankin came to UNMH after working for hospitals in Colorado and Nebraska and is a founding member of the UNMH patient flow committee, striving to improve patient care processes throughout the institution.
Tom Guirkin, MD, has been appointed vice president of medical affairs for Virginia Commonwealth University Community Memorial Hospital (South Hill, Va.). Dr. Guirkin, a Virginia native, returns to his home state after most recently overseeing the hospitalist group at Saint Francis Health System (Tulsa, Okla.).
Dr. Guirkin will have the opportunity to continue practicing medicine at CMH while helping to manage the quality management side of the business. He received his MBA from Virginia Commonwealth, working for James River Hospitalist Group in Richmond at the same time.
Alteon Health (Germantown, Md.) has become the manager of hospitalist services for three facilities in Maryland and Ohio, including Carroll Hospital (Westminster, Md.), Washington Adventist Hospital (Takoma Park, Md.), and University Hospitals Cleveland Medical Center.
At Carroll, Alteon physicians will provide critical care services in addition to hospitalist duties. Alteon has been Carroll’s emergency medicine provider for more than two decades.
At Washington Adventist, Alteon will take over the hospitalist program, adding to the emergency medicine services it has provided since 1991 and critical care services it has managed since 1996.
At UH Cleveland, Alteon will assume hospitalist management at its third University Hospitals facility. Alteon controls emergency medicine at 14 UH locations as well. UH Cleveland is an affiliate of Case Western Reserve University.
Christopher Moriates, MD, has been named executive director of the nonprofit health care organization Costs of Care (Boston). He replaces Neel Shah, MD, who was tabbed chairperson of the board.
Dr. Moriates serves a number of roles at the University of Texas at Austin. He is the assistant dean for health care value; associate chair for quality, safety and value; and associate professor of internal medicine.
In his role at Costs of Care, Dr. Moriates will direct an organization that uses feedback and stories from frontline physicians to help health systems provide high-quality care at lower costs.
Kai Mebust, MD, was recently named the new associate chief of medicine at Bassett Hospital (Cooperstown, N.Y.), where he has worked the past 15 years as a hospitalist and internist, serving as chief of hospitalists for the last decade. Dr. Mebust also completed his internship and residency at Bassett, and he is a fellow with the Society of Hospital Medicine.
Dr. Mebust will work closely with Dr. Charles Hyman, the center’s physician in chief, who is leaving the role at the end of the calendar year. Dr. Mebust will oversee inpatient services and be part of the transition process when Dr. Hyman departs.
Ronak Bhimani, MD, has been appointed chief medical officer at Lower Bucks Hospital (Bristol, Pa.). Dr. Bhimani moves over from Suburban Community Hospital (Norristown, Pa.), where he served as an academic hospitalist the past 2 years.
Previously, Dr. Bhimani was medical director of Kindred/Avalon Hospice and a core faculty member in the internal medicine program for residents at Suburban Community.
Danielle Prince, MD, was recently named associate medical director at St. Luke’s Siouxland PACE (Sioux City, Iowa), an affiliate of UnityPoint Health. Dr. Prince is a practicing hospitalist at UnityPoint Health St. Luke’s and served previously in as a family physician while working as chief medical informatics officer at Mercy Medical Center (Sioux City).
At Siouxland PACE, Dr. Prince will assist in managing the full-service care of elderly patients, including home health, specialty care, medications, transportation, and other therapies.
Alex Rankin, MD, has been named the new associate chief medical officer for the University of New Mexico Health Transfer Center and Patient Throughput in Albuquerque. A hospitalist with UNMH’s Family and Community Medicine department, Dr. Rankin was previously the medical director at the system’s 3 North facility since 2014.
Dr. Rankin came to UNMH after working for hospitals in Colorado and Nebraska and is a founding member of the UNMH patient flow committee, striving to improve patient care processes throughout the institution.
Tom Guirkin, MD, has been appointed vice president of medical affairs for Virginia Commonwealth University Community Memorial Hospital (South Hill, Va.). Dr. Guirkin, a Virginia native, returns to his home state after most recently overseeing the hospitalist group at Saint Francis Health System (Tulsa, Okla.).
Dr. Guirkin will have the opportunity to continue practicing medicine at CMH while helping to manage the quality management side of the business. He received his MBA from Virginia Commonwealth, working for James River Hospitalist Group in Richmond at the same time.
Alteon Health (Germantown, Md.) has become the manager of hospitalist services for three facilities in Maryland and Ohio, including Carroll Hospital (Westminster, Md.), Washington Adventist Hospital (Takoma Park, Md.), and University Hospitals Cleveland Medical Center.
At Carroll, Alteon physicians will provide critical care services in addition to hospitalist duties. Alteon has been Carroll’s emergency medicine provider for more than two decades.
At Washington Adventist, Alteon will take over the hospitalist program, adding to the emergency medicine services it has provided since 1991 and critical care services it has managed since 1996.
At UH Cleveland, Alteon will assume hospitalist management at its third University Hospitals facility. Alteon controls emergency medicine at 14 UH locations as well. UH Cleveland is an affiliate of Case Western Reserve University.
Becoming a high-value care physician
‘Culture shift’ comes from collective efforts
It’s Monday morning, and Mrs. Jones still has abdominal pain. Your ward team decides to order a CT. On chart review you notice she’s had three other abdominal CTs for the same indication this year. How did this happen? What should you do?
High-value care has been defined by the Institute of Medicine as “the best care for the patient, with the optimal result for the circumstances, delivered at the right price.”1 With an estimated $700 billion dollars – 30% of medical expenditures – spent on wasted care, there are rising calls for a transformational shift.2
You are now asked to consider not just everything you can do for a patient, but also the benefits, harms, and costs associated with those choices. But where to start? We recommend that trainees integrate these tips for high-value care into their routine practice.
1. Use evidence-based resources that highlight value
A great place to begin is the “Six Things Medical Students and Trainees Should Question,” originally published in Academic Medicine and created by Choosing Wisely Canada™. Recommendations range from avoiding tests or treatments that will not change a patient’s clinical course to holding off on ordering tests solely based on what you assume your preceptor will want (see the full list in Table 1).3
Other ways to avoid low-value care include following the United States Choosing Wisely™ campaign, which has collected more than 500 specialty society recommendations. Likewise, the American College of Radiology Appropriateness Criteria are designed to assist providers with ordering the appropriate imaging tests (for a more extensive list see Table 2).
2. Express your clinical reasoning
One driver of health care expenditures that is especially prevalent in academia is the pressure to demonstrate knowledge by recommending extensive testing. While these tests may rule out obscure diagnoses, they often do not change management.
You can still demonstrate a mastery of your patients’ care by expressing your thought process overtly. For instance, “I considered secondary causes of the patient’s severe hypertension but felt it was most reasonable to first treat her pain and restart her home medications before pursuing a larger work-up. If the patient’s blood pressure remains elevated and she is hypokalemic, we could consider testing for hyperaldosteronism.” If you explain why you think a diagnosis is less likely and order tests accordingly, others will be encouraged to consider value in their own medical decision making.
3. Hone your communication skills
One of the most cited reasons for providing unnecessary care is the time required to discuss treatment plans with patients – it’s much faster to just order the test than to explain why it isn’t needed. Research, however, shows that these cost conversations take 68 seconds on average.4 Costs of Care (see Table 2) has an excellent video series that highlights how effective communication allows for shared decision making, which promotes both patient engagement and helps avoid wasteful care.
Physicians’ first instincts are often defensive when a patient asks for care we perceive as unnecessary. However, exploring what the patient hopes to gain from said test or treatment frequently reveals concern for a specific, missed diagnosis or complication. Addressing this underlying fear, rather than defending your ordering patterns, can create improved rapport and may serve to provide more reassurance than a test ever could.5
As a physician-in-training, try to observe others having these conversations and take every opportunity to practice. By focusing on this key skill set, you will increase your comfort with in-depth discussions on the value of care.
4. Get involved in a project related to high-value care
While you are developing your own practice patterns, you may be inspired to tackle areas of overuse and underuse at a more systemwide level. If your hospital does not have a committee for high-value care, perhaps a quality improvement leader can support your ideas to launch a project or participate in an ongoing initiative. Physicians-in-training have been identified as crucial to these projects’ success – your frontline insight can highlight potential problems and the nuances of workflow that are key to effective solutions.6
5. Embrace lifelong learning and reflection
The process of becoming a physician and of practicing high-value care is not a sprint but a marathon. Multiple barriers to high-value care exist, and you may feel these pressures differently at various points in your career. These include malpractice concerns, addressing patient expectations, and the desire to take action “just to be safe.”6
Interestingly, fear of malpractice does not seem to dissipate in areas where tort reform has provided stronger provider protections.7 Practitioners may also inaccurately assume a patient’s desire for additional work-up or treatment.8 Furthermore, be aware of the role of “commission bias” by which a provider regrets not doing something that could have helped a previous patient. This regret can prove to be a stronger motivator than the potential harm related to unnecessary diagnostic tests or treatments.9
While these barriers cannot be removed easily, learners and providers can practice active reflection by examining their own fears, biases, and motivations before and after they order additional testing or treatment.
As a physician-in-training, you may feel that your decisions do not have a major impact on the health care system as a whole. However, the culture shift needed to “bend the cost curve” will come from the collective efforts of individuals like you. Practicing high-value care is not just a matter of ordering fewer tests – appropriate ordering of an expensive test that expedites a diagnosis may be more cost-effective and enhance the quality of care provided. Increasing your own awareness of both necessary and unnecessary practices is a major step toward realizing system change. Your efforts to resist and reform the medical culture that propagates low value care will encourage your colleagues to follow suit.
Dr. Lacy is assistant professor and associate clerkship director at the University of New Mexico, Albuquerque, as well as division director of high-value care for the division of hospital medicine. Dr. Goetz is assistant professor at Rush University Medical Center, Chicago. They met as 2015 Copello Fellows at the National Physician Alliance. Both have been involved in numerous high-value care initiatives, curricular development, and medical education at their respective institutions.
References
1. Committee on the Learning Health Care System in America, Institute of Medicine. “Best Care at Lower Cost: The Path to Continuously Learning Health Care in America.” Edited by Smith M, Saunders R, Stuckhardt L, and McGinnis JM. (Washington: National Academies Press, 2013). http://www.ncbi.nlm.nih.gov/books/NBK207225/.
2. Berwick DM, Hackbarth AD. Eliminating waste in US health care. JAMA. 2012;307(14):1513-6.
3. Lakhani A et al. Choosing Wisely for Medical Education: Six things medical students and trainees should question. Acad Med. 2016 Oct;91(10):1374-8.
4. Hunter WG et al. Patient-physician discussions about costs: Definitions and impact on cost conversation incidence estimates. BMC Health Serv Res. 2016;16:108.
5. van Ravesteijn H et al. The reassuring value of diagnostic tests: a systematic review. Patient Educ Couns. 2012;86(1):3-8.
6. Moriates C, Wong BM. High-value care programmes from the bottom-up… and the top-down. BMJ Qual Saf. 2016;25(11):821-3.
7. Snyder Sulmasy L, Weinberger SE. Better care is the best defense: High-value clinical practice vs. defensive medicine. Cleve Clin J Med. 2014;81(8):464-7.
8. Mulley AG, Trimble C, Elwyn G. Stop the silent misdiagnosis: Patients’ preferences matter. BMJ. 2012;345:e6572.
9. Scott IA. Cognitive challenges to minimising low value care. Intern Med J. 2017;47(9):1079-1083.
‘Culture shift’ comes from collective efforts
‘Culture shift’ comes from collective efforts
It’s Monday morning, and Mrs. Jones still has abdominal pain. Your ward team decides to order a CT. On chart review you notice she’s had three other abdominal CTs for the same indication this year. How did this happen? What should you do?
High-value care has been defined by the Institute of Medicine as “the best care for the patient, with the optimal result for the circumstances, delivered at the right price.”1 With an estimated $700 billion dollars – 30% of medical expenditures – spent on wasted care, there are rising calls for a transformational shift.2
You are now asked to consider not just everything you can do for a patient, but also the benefits, harms, and costs associated with those choices. But where to start? We recommend that trainees integrate these tips for high-value care into their routine practice.
1. Use evidence-based resources that highlight value
A great place to begin is the “Six Things Medical Students and Trainees Should Question,” originally published in Academic Medicine and created by Choosing Wisely Canada™. Recommendations range from avoiding tests or treatments that will not change a patient’s clinical course to holding off on ordering tests solely based on what you assume your preceptor will want (see the full list in Table 1).3
Other ways to avoid low-value care include following the United States Choosing Wisely™ campaign, which has collected more than 500 specialty society recommendations. Likewise, the American College of Radiology Appropriateness Criteria are designed to assist providers with ordering the appropriate imaging tests (for a more extensive list see Table 2).
2. Express your clinical reasoning
One driver of health care expenditures that is especially prevalent in academia is the pressure to demonstrate knowledge by recommending extensive testing. While these tests may rule out obscure diagnoses, they often do not change management.
You can still demonstrate a mastery of your patients’ care by expressing your thought process overtly. For instance, “I considered secondary causes of the patient’s severe hypertension but felt it was most reasonable to first treat her pain and restart her home medications before pursuing a larger work-up. If the patient’s blood pressure remains elevated and she is hypokalemic, we could consider testing for hyperaldosteronism.” If you explain why you think a diagnosis is less likely and order tests accordingly, others will be encouraged to consider value in their own medical decision making.
3. Hone your communication skills
One of the most cited reasons for providing unnecessary care is the time required to discuss treatment plans with patients – it’s much faster to just order the test than to explain why it isn’t needed. Research, however, shows that these cost conversations take 68 seconds on average.4 Costs of Care (see Table 2) has an excellent video series that highlights how effective communication allows for shared decision making, which promotes both patient engagement and helps avoid wasteful care.
Physicians’ first instincts are often defensive when a patient asks for care we perceive as unnecessary. However, exploring what the patient hopes to gain from said test or treatment frequently reveals concern for a specific, missed diagnosis or complication. Addressing this underlying fear, rather than defending your ordering patterns, can create improved rapport and may serve to provide more reassurance than a test ever could.5
As a physician-in-training, try to observe others having these conversations and take every opportunity to practice. By focusing on this key skill set, you will increase your comfort with in-depth discussions on the value of care.
4. Get involved in a project related to high-value care
While you are developing your own practice patterns, you may be inspired to tackle areas of overuse and underuse at a more systemwide level. If your hospital does not have a committee for high-value care, perhaps a quality improvement leader can support your ideas to launch a project or participate in an ongoing initiative. Physicians-in-training have been identified as crucial to these projects’ success – your frontline insight can highlight potential problems and the nuances of workflow that are key to effective solutions.6
5. Embrace lifelong learning and reflection
The process of becoming a physician and of practicing high-value care is not a sprint but a marathon. Multiple barriers to high-value care exist, and you may feel these pressures differently at various points in your career. These include malpractice concerns, addressing patient expectations, and the desire to take action “just to be safe.”6
Interestingly, fear of malpractice does not seem to dissipate in areas where tort reform has provided stronger provider protections.7 Practitioners may also inaccurately assume a patient’s desire for additional work-up or treatment.8 Furthermore, be aware of the role of “commission bias” by which a provider regrets not doing something that could have helped a previous patient. This regret can prove to be a stronger motivator than the potential harm related to unnecessary diagnostic tests or treatments.9
While these barriers cannot be removed easily, learners and providers can practice active reflection by examining their own fears, biases, and motivations before and after they order additional testing or treatment.
As a physician-in-training, you may feel that your decisions do not have a major impact on the health care system as a whole. However, the culture shift needed to “bend the cost curve” will come from the collective efforts of individuals like you. Practicing high-value care is not just a matter of ordering fewer tests – appropriate ordering of an expensive test that expedites a diagnosis may be more cost-effective and enhance the quality of care provided. Increasing your own awareness of both necessary and unnecessary practices is a major step toward realizing system change. Your efforts to resist and reform the medical culture that propagates low value care will encourage your colleagues to follow suit.
Dr. Lacy is assistant professor and associate clerkship director at the University of New Mexico, Albuquerque, as well as division director of high-value care for the division of hospital medicine. Dr. Goetz is assistant professor at Rush University Medical Center, Chicago. They met as 2015 Copello Fellows at the National Physician Alliance. Both have been involved in numerous high-value care initiatives, curricular development, and medical education at their respective institutions.
References
1. Committee on the Learning Health Care System in America, Institute of Medicine. “Best Care at Lower Cost: The Path to Continuously Learning Health Care in America.” Edited by Smith M, Saunders R, Stuckhardt L, and McGinnis JM. (Washington: National Academies Press, 2013). http://www.ncbi.nlm.nih.gov/books/NBK207225/.
2. Berwick DM, Hackbarth AD. Eliminating waste in US health care. JAMA. 2012;307(14):1513-6.
3. Lakhani A et al. Choosing Wisely for Medical Education: Six things medical students and trainees should question. Acad Med. 2016 Oct;91(10):1374-8.
4. Hunter WG et al. Patient-physician discussions about costs: Definitions and impact on cost conversation incidence estimates. BMC Health Serv Res. 2016;16:108.
5. van Ravesteijn H et al. The reassuring value of diagnostic tests: a systematic review. Patient Educ Couns. 2012;86(1):3-8.
6. Moriates C, Wong BM. High-value care programmes from the bottom-up… and the top-down. BMJ Qual Saf. 2016;25(11):821-3.
7. Snyder Sulmasy L, Weinberger SE. Better care is the best defense: High-value clinical practice vs. defensive medicine. Cleve Clin J Med. 2014;81(8):464-7.
8. Mulley AG, Trimble C, Elwyn G. Stop the silent misdiagnosis: Patients’ preferences matter. BMJ. 2012;345:e6572.
9. Scott IA. Cognitive challenges to minimising low value care. Intern Med J. 2017;47(9):1079-1083.
It’s Monday morning, and Mrs. Jones still has abdominal pain. Your ward team decides to order a CT. On chart review you notice she’s had three other abdominal CTs for the same indication this year. How did this happen? What should you do?
High-value care has been defined by the Institute of Medicine as “the best care for the patient, with the optimal result for the circumstances, delivered at the right price.”1 With an estimated $700 billion dollars – 30% of medical expenditures – spent on wasted care, there are rising calls for a transformational shift.2
You are now asked to consider not just everything you can do for a patient, but also the benefits, harms, and costs associated with those choices. But where to start? We recommend that trainees integrate these tips for high-value care into their routine practice.
1. Use evidence-based resources that highlight value
A great place to begin is the “Six Things Medical Students and Trainees Should Question,” originally published in Academic Medicine and created by Choosing Wisely Canada™. Recommendations range from avoiding tests or treatments that will not change a patient’s clinical course to holding off on ordering tests solely based on what you assume your preceptor will want (see the full list in Table 1).3
Other ways to avoid low-value care include following the United States Choosing Wisely™ campaign, which has collected more than 500 specialty society recommendations. Likewise, the American College of Radiology Appropriateness Criteria are designed to assist providers with ordering the appropriate imaging tests (for a more extensive list see Table 2).
2. Express your clinical reasoning
One driver of health care expenditures that is especially prevalent in academia is the pressure to demonstrate knowledge by recommending extensive testing. While these tests may rule out obscure diagnoses, they often do not change management.
You can still demonstrate a mastery of your patients’ care by expressing your thought process overtly. For instance, “I considered secondary causes of the patient’s severe hypertension but felt it was most reasonable to first treat her pain and restart her home medications before pursuing a larger work-up. If the patient’s blood pressure remains elevated and she is hypokalemic, we could consider testing for hyperaldosteronism.” If you explain why you think a diagnosis is less likely and order tests accordingly, others will be encouraged to consider value in their own medical decision making.
3. Hone your communication skills
One of the most cited reasons for providing unnecessary care is the time required to discuss treatment plans with patients – it’s much faster to just order the test than to explain why it isn’t needed. Research, however, shows that these cost conversations take 68 seconds on average.4 Costs of Care (see Table 2) has an excellent video series that highlights how effective communication allows for shared decision making, which promotes both patient engagement and helps avoid wasteful care.
Physicians’ first instincts are often defensive when a patient asks for care we perceive as unnecessary. However, exploring what the patient hopes to gain from said test or treatment frequently reveals concern for a specific, missed diagnosis or complication. Addressing this underlying fear, rather than defending your ordering patterns, can create improved rapport and may serve to provide more reassurance than a test ever could.5
As a physician-in-training, try to observe others having these conversations and take every opportunity to practice. By focusing on this key skill set, you will increase your comfort with in-depth discussions on the value of care.
4. Get involved in a project related to high-value care
While you are developing your own practice patterns, you may be inspired to tackle areas of overuse and underuse at a more systemwide level. If your hospital does not have a committee for high-value care, perhaps a quality improvement leader can support your ideas to launch a project or participate in an ongoing initiative. Physicians-in-training have been identified as crucial to these projects’ success – your frontline insight can highlight potential problems and the nuances of workflow that are key to effective solutions.6
5. Embrace lifelong learning and reflection
The process of becoming a physician and of practicing high-value care is not a sprint but a marathon. Multiple barriers to high-value care exist, and you may feel these pressures differently at various points in your career. These include malpractice concerns, addressing patient expectations, and the desire to take action “just to be safe.”6
Interestingly, fear of malpractice does not seem to dissipate in areas where tort reform has provided stronger provider protections.7 Practitioners may also inaccurately assume a patient’s desire for additional work-up or treatment.8 Furthermore, be aware of the role of “commission bias” by which a provider regrets not doing something that could have helped a previous patient. This regret can prove to be a stronger motivator than the potential harm related to unnecessary diagnostic tests or treatments.9
While these barriers cannot be removed easily, learners and providers can practice active reflection by examining their own fears, biases, and motivations before and after they order additional testing or treatment.
As a physician-in-training, you may feel that your decisions do not have a major impact on the health care system as a whole. However, the culture shift needed to “bend the cost curve” will come from the collective efforts of individuals like you. Practicing high-value care is not just a matter of ordering fewer tests – appropriate ordering of an expensive test that expedites a diagnosis may be more cost-effective and enhance the quality of care provided. Increasing your own awareness of both necessary and unnecessary practices is a major step toward realizing system change. Your efforts to resist and reform the medical culture that propagates low value care will encourage your colleagues to follow suit.
Dr. Lacy is assistant professor and associate clerkship director at the University of New Mexico, Albuquerque, as well as division director of high-value care for the division of hospital medicine. Dr. Goetz is assistant professor at Rush University Medical Center, Chicago. They met as 2015 Copello Fellows at the National Physician Alliance. Both have been involved in numerous high-value care initiatives, curricular development, and medical education at their respective institutions.
References
1. Committee on the Learning Health Care System in America, Institute of Medicine. “Best Care at Lower Cost: The Path to Continuously Learning Health Care in America.” Edited by Smith M, Saunders R, Stuckhardt L, and McGinnis JM. (Washington: National Academies Press, 2013). http://www.ncbi.nlm.nih.gov/books/NBK207225/.
2. Berwick DM, Hackbarth AD. Eliminating waste in US health care. JAMA. 2012;307(14):1513-6.
3. Lakhani A et al. Choosing Wisely for Medical Education: Six things medical students and trainees should question. Acad Med. 2016 Oct;91(10):1374-8.
4. Hunter WG et al. Patient-physician discussions about costs: Definitions and impact on cost conversation incidence estimates. BMC Health Serv Res. 2016;16:108.
5. van Ravesteijn H et al. The reassuring value of diagnostic tests: a systematic review. Patient Educ Couns. 2012;86(1):3-8.
6. Moriates C, Wong BM. High-value care programmes from the bottom-up… and the top-down. BMJ Qual Saf. 2016;25(11):821-3.
7. Snyder Sulmasy L, Weinberger SE. Better care is the best defense: High-value clinical practice vs. defensive medicine. Cleve Clin J Med. 2014;81(8):464-7.
8. Mulley AG, Trimble C, Elwyn G. Stop the silent misdiagnosis: Patients’ preferences matter. BMJ. 2012;345:e6572.
9. Scott IA. Cognitive challenges to minimising low value care. Intern Med J. 2017;47(9):1079-1083.
HM19: One chapter’s experience
The Society of Hospital Medicine is an organization vested in improving the quality of inpatient medicine by empowering its members with education and providing venues for professional development including networking, advocacy, and leadership advancement. Every year, SHM holds a national conference which is a focused meeting point for over 5,000 hospitalists.
SHM hosts more than 50 local chapters nationwide to increase networking, education, and collaboration within the hospital medicine community. The Wiregrass chapter of SHM is based in the southeast corner of Alabama, covering the counties of lower Alabama and the panhandle of Florida. This year we were recognized as a platinum status chapter, which is the highest status, based on our work and participation to improve the quality of inpatient medicine.
As part of winning the platinum ribbon, we were awarded three complimentary registration scholarships to the SHM Annual Conference in 2019. The chapter leadership met and selected three individuals who have been involved with the chapter actively but have never had an opportunity to experience SHM’s Annual Conference. We selected a first-year resident, Dr. Avani Parrekh; a hospital medicine nurse practitioner, Madison Rivenbark; and a fourth-year medical student who is about to start his internal medicine residency, William Bancroft.
After the meeting we interviewed them to better understand their experience. Below are their thoughts.
Avani Parekh, MD
First year, Internal Medicine Residency
Southeast Health Medical Center
Dothan, Ala.
I am so thankful for the opportunity that was given to me by the Wiregrass chapter by sponsoring my attendance at the 2019 SHM Annual Conference in Washington. This was my first SHM conference, and it was truly a rewarding experience.
I thoroughly enjoyed attending the lectures. They were very informative and engaging. Every presenter was so passionate and inspiring. Coming from an “all-female class” of PGY-1 at my program, I especially enjoyed the “Fe(male) in medicine” talk, as well as Quick Talks on women in medicine. The “Updates in Hospital Medicine” session on various topics such as heart failure, pneumonia, and sepsis was outstanding. I was excited to apply the knowledge I gained from this event into my patient care.
Overall, it was a well-organized and up-to-date event. I am looking forward to attending more SHM conferences in the future.
Madison Rivenbark, NP
Department of Hospital Medicine
Southeast Health Medical Center
Dothan, Ala.
I was extremely fortunate to be selected to receive a scholarship that covered the conference fee for the 2019 SHM Annual Conference. This was my first SHM conference, and it was quite the learning experience. I enjoyed each educational session that I attended. I felt like I was able to bring something home with me that I can incorporate into my practice to better care for the patients that I see each day.
As mentioned above, I learned from each session, but my personal favorite was the “Updates in Hospital Medicine” session. I was very impressed by the enthusiasm of the two speakers. The information provided was presented so that it engaged each attendee.
Not only did I learn a wealth of valuable information that will help me in my career, I gained affirmation concerning my future educational endeavors. I was inspired to pursue a higher level of learning regarding my career. I witnessed this awesome organization that is filled with encouraging and motivating people, and I realized I wanted to be more involved on a local level, and maybe one day, on a larger level. In addition, this conference inspired me to continue to be a lifetime learner and to always crave more knowledge. I am blessed to be a part of hospital medicine. I look forward to the future of this specialty.
William Bancroft, MS IV
Alabama College of Osteopathic Medicine
Dothan, Ala.
I was honored to have been chosen by the Wiregrass chapter as the medical student representative for the SHM Annual Conference. I have been serving in the local chapter during both my 3rd and 4th years in different roles, from helping as a student liaison for our medical students to executive planning coordinator for events. It was a surprise when I got asked by the chapter to be their student representative, but one that I was very excited to accept.
This was my first medical conference. I had heard about what different conferences were like from many of my attendings, so I had some expectations, but this experience was so much better. I enjoyed meeting and networking with people. I also found myself eagerly waiting to get to the next lecture because I was getting an opportunity to hear about different case studies, new research outcomes, and new standards of care.
It was a real treat to learn about all the new changes to treatment, but even more encouraging to know that most of it was just reinforcing everything my attendings have been teaching us as medical students. I enjoyed my time at the SHM Annual Conference so much that I emailed all my new coresidents and encouraged them to join the Society.
Dr. Skandhan is a hospitalist at Southeast Health Medical Center in Dothan, Ala., as well as president and founder of the Wiregrass chapter of SHM.
The Society of Hospital Medicine is an organization vested in improving the quality of inpatient medicine by empowering its members with education and providing venues for professional development including networking, advocacy, and leadership advancement. Every year, SHM holds a national conference which is a focused meeting point for over 5,000 hospitalists.
SHM hosts more than 50 local chapters nationwide to increase networking, education, and collaboration within the hospital medicine community. The Wiregrass chapter of SHM is based in the southeast corner of Alabama, covering the counties of lower Alabama and the panhandle of Florida. This year we were recognized as a platinum status chapter, which is the highest status, based on our work and participation to improve the quality of inpatient medicine.
As part of winning the platinum ribbon, we were awarded three complimentary registration scholarships to the SHM Annual Conference in 2019. The chapter leadership met and selected three individuals who have been involved with the chapter actively but have never had an opportunity to experience SHM’s Annual Conference. We selected a first-year resident, Dr. Avani Parrekh; a hospital medicine nurse practitioner, Madison Rivenbark; and a fourth-year medical student who is about to start his internal medicine residency, William Bancroft.
After the meeting we interviewed them to better understand their experience. Below are their thoughts.
Avani Parekh, MD
First year, Internal Medicine Residency
Southeast Health Medical Center
Dothan, Ala.
I am so thankful for the opportunity that was given to me by the Wiregrass chapter by sponsoring my attendance at the 2019 SHM Annual Conference in Washington. This was my first SHM conference, and it was truly a rewarding experience.
I thoroughly enjoyed attending the lectures. They were very informative and engaging. Every presenter was so passionate and inspiring. Coming from an “all-female class” of PGY-1 at my program, I especially enjoyed the “Fe(male) in medicine” talk, as well as Quick Talks on women in medicine. The “Updates in Hospital Medicine” session on various topics such as heart failure, pneumonia, and sepsis was outstanding. I was excited to apply the knowledge I gained from this event into my patient care.
Overall, it was a well-organized and up-to-date event. I am looking forward to attending more SHM conferences in the future.
Madison Rivenbark, NP
Department of Hospital Medicine
Southeast Health Medical Center
Dothan, Ala.
I was extremely fortunate to be selected to receive a scholarship that covered the conference fee for the 2019 SHM Annual Conference. This was my first SHM conference, and it was quite the learning experience. I enjoyed each educational session that I attended. I felt like I was able to bring something home with me that I can incorporate into my practice to better care for the patients that I see each day.
As mentioned above, I learned from each session, but my personal favorite was the “Updates in Hospital Medicine” session. I was very impressed by the enthusiasm of the two speakers. The information provided was presented so that it engaged each attendee.
Not only did I learn a wealth of valuable information that will help me in my career, I gained affirmation concerning my future educational endeavors. I was inspired to pursue a higher level of learning regarding my career. I witnessed this awesome organization that is filled with encouraging and motivating people, and I realized I wanted to be more involved on a local level, and maybe one day, on a larger level. In addition, this conference inspired me to continue to be a lifetime learner and to always crave more knowledge. I am blessed to be a part of hospital medicine. I look forward to the future of this specialty.
William Bancroft, MS IV
Alabama College of Osteopathic Medicine
Dothan, Ala.
I was honored to have been chosen by the Wiregrass chapter as the medical student representative for the SHM Annual Conference. I have been serving in the local chapter during both my 3rd and 4th years in different roles, from helping as a student liaison for our medical students to executive planning coordinator for events. It was a surprise when I got asked by the chapter to be their student representative, but one that I was very excited to accept.
This was my first medical conference. I had heard about what different conferences were like from many of my attendings, so I had some expectations, but this experience was so much better. I enjoyed meeting and networking with people. I also found myself eagerly waiting to get to the next lecture because I was getting an opportunity to hear about different case studies, new research outcomes, and new standards of care.
It was a real treat to learn about all the new changes to treatment, but even more encouraging to know that most of it was just reinforcing everything my attendings have been teaching us as medical students. I enjoyed my time at the SHM Annual Conference so much that I emailed all my new coresidents and encouraged them to join the Society.
Dr. Skandhan is a hospitalist at Southeast Health Medical Center in Dothan, Ala., as well as president and founder of the Wiregrass chapter of SHM.
The Society of Hospital Medicine is an organization vested in improving the quality of inpatient medicine by empowering its members with education and providing venues for professional development including networking, advocacy, and leadership advancement. Every year, SHM holds a national conference which is a focused meeting point for over 5,000 hospitalists.
SHM hosts more than 50 local chapters nationwide to increase networking, education, and collaboration within the hospital medicine community. The Wiregrass chapter of SHM is based in the southeast corner of Alabama, covering the counties of lower Alabama and the panhandle of Florida. This year we were recognized as a platinum status chapter, which is the highest status, based on our work and participation to improve the quality of inpatient medicine.
As part of winning the platinum ribbon, we were awarded three complimentary registration scholarships to the SHM Annual Conference in 2019. The chapter leadership met and selected three individuals who have been involved with the chapter actively but have never had an opportunity to experience SHM’s Annual Conference. We selected a first-year resident, Dr. Avani Parrekh; a hospital medicine nurse practitioner, Madison Rivenbark; and a fourth-year medical student who is about to start his internal medicine residency, William Bancroft.
After the meeting we interviewed them to better understand their experience. Below are their thoughts.
Avani Parekh, MD
First year, Internal Medicine Residency
Southeast Health Medical Center
Dothan, Ala.
I am so thankful for the opportunity that was given to me by the Wiregrass chapter by sponsoring my attendance at the 2019 SHM Annual Conference in Washington. This was my first SHM conference, and it was truly a rewarding experience.
I thoroughly enjoyed attending the lectures. They were very informative and engaging. Every presenter was so passionate and inspiring. Coming from an “all-female class” of PGY-1 at my program, I especially enjoyed the “Fe(male) in medicine” talk, as well as Quick Talks on women in medicine. The “Updates in Hospital Medicine” session on various topics such as heart failure, pneumonia, and sepsis was outstanding. I was excited to apply the knowledge I gained from this event into my patient care.
Overall, it was a well-organized and up-to-date event. I am looking forward to attending more SHM conferences in the future.
Madison Rivenbark, NP
Department of Hospital Medicine
Southeast Health Medical Center
Dothan, Ala.
I was extremely fortunate to be selected to receive a scholarship that covered the conference fee for the 2019 SHM Annual Conference. This was my first SHM conference, and it was quite the learning experience. I enjoyed each educational session that I attended. I felt like I was able to bring something home with me that I can incorporate into my practice to better care for the patients that I see each day.
As mentioned above, I learned from each session, but my personal favorite was the “Updates in Hospital Medicine” session. I was very impressed by the enthusiasm of the two speakers. The information provided was presented so that it engaged each attendee.
Not only did I learn a wealth of valuable information that will help me in my career, I gained affirmation concerning my future educational endeavors. I was inspired to pursue a higher level of learning regarding my career. I witnessed this awesome organization that is filled with encouraging and motivating people, and I realized I wanted to be more involved on a local level, and maybe one day, on a larger level. In addition, this conference inspired me to continue to be a lifetime learner and to always crave more knowledge. I am blessed to be a part of hospital medicine. I look forward to the future of this specialty.
William Bancroft, MS IV
Alabama College of Osteopathic Medicine
Dothan, Ala.
I was honored to have been chosen by the Wiregrass chapter as the medical student representative for the SHM Annual Conference. I have been serving in the local chapter during both my 3rd and 4th years in different roles, from helping as a student liaison for our medical students to executive planning coordinator for events. It was a surprise when I got asked by the chapter to be their student representative, but one that I was very excited to accept.
This was my first medical conference. I had heard about what different conferences were like from many of my attendings, so I had some expectations, but this experience was so much better. I enjoyed meeting and networking with people. I also found myself eagerly waiting to get to the next lecture because I was getting an opportunity to hear about different case studies, new research outcomes, and new standards of care.
It was a real treat to learn about all the new changes to treatment, but even more encouraging to know that most of it was just reinforcing everything my attendings have been teaching us as medical students. I enjoyed my time at the SHM Annual Conference so much that I emailed all my new coresidents and encouraged them to join the Society.
Dr. Skandhan is a hospitalist at Southeast Health Medical Center in Dothan, Ala., as well as president and founder of the Wiregrass chapter of SHM.
The impact of HM19 on my practice
As an academic nurse practitioner hospitalist with faculty and leadership roles, I found that HM19 had many important and helpful topics that apply directly to my practice.
The “Onboarding Best Practices” session provided specific examples and tips for clinical ramp up, enculturation, and orienting staff to an academic career. As a result of this talk, I began the process of establishing a formal enculturation activity for new hires that includes a panel of senior advanced practice provider (APP) hospitalists to give career path advice.
The “Adaptive Leadership for Hospitalists” workshop provided the opportunity to practice emotional intelligence and effective communication in managing routine and difficult leadership interactions. The “Practice Models/Models of Care for Optimal Integration of NPs and PAs” presentation provided insight into variable team structures at other institutions that could be considered for improved efficiency in my group. The “Academic NP/PA” session provided ideas for how to apply for faculty positions in academic institutions. It also gave APPs who have faculty appointment specific illustrations of using current educational, quality improvement, and research projects to promote. I particularly found the “What Mentorship Has Meant to Me” talk significant. It gave practical essential advice on making sure there is chemistry and trust when seeking a mentor and staying engaged to be a successful mentee.
APPs, whether practicing in academic, private, or community settings, should attend the SHM Annual Conference. SHM is very inclusive and proud of APPs as colleagues and leaders. There are topics that directly apply to the needs of APP hospitalists – including career advancement – and that create excitement for APP practice in hospital medicine.
The Annual Conference also provides the very unique opportunity to meet and establish relationships with APP and physician colleagues and leaders nationwide. These relationships lend to career advancing opportunities for collaboration in clinical excellence, education, quality improvement, research, and leadership.
Dr. Apodaca is assistant professor and nurse practitioner hospitalist at the University of New Mexico. She is one of the first APPNP/PAs to receive faculty appointment at UNM. She serves as codirector of the UNM APP Hospital Medicine Fellowship and director of the APP Hospital Medicine Team. She is also the president of the New Mexico Chapter of SHM and is the first APP at her institution to achieve designation as a Fellow in Hospital Medicine.
As an academic nurse practitioner hospitalist with faculty and leadership roles, I found that HM19 had many important and helpful topics that apply directly to my practice.
The “Onboarding Best Practices” session provided specific examples and tips for clinical ramp up, enculturation, and orienting staff to an academic career. As a result of this talk, I began the process of establishing a formal enculturation activity for new hires that includes a panel of senior advanced practice provider (APP) hospitalists to give career path advice.
The “Adaptive Leadership for Hospitalists” workshop provided the opportunity to practice emotional intelligence and effective communication in managing routine and difficult leadership interactions. The “Practice Models/Models of Care for Optimal Integration of NPs and PAs” presentation provided insight into variable team structures at other institutions that could be considered for improved efficiency in my group. The “Academic NP/PA” session provided ideas for how to apply for faculty positions in academic institutions. It also gave APPs who have faculty appointment specific illustrations of using current educational, quality improvement, and research projects to promote. I particularly found the “What Mentorship Has Meant to Me” talk significant. It gave practical essential advice on making sure there is chemistry and trust when seeking a mentor and staying engaged to be a successful mentee.
APPs, whether practicing in academic, private, or community settings, should attend the SHM Annual Conference. SHM is very inclusive and proud of APPs as colleagues and leaders. There are topics that directly apply to the needs of APP hospitalists – including career advancement – and that create excitement for APP practice in hospital medicine.
The Annual Conference also provides the very unique opportunity to meet and establish relationships with APP and physician colleagues and leaders nationwide. These relationships lend to career advancing opportunities for collaboration in clinical excellence, education, quality improvement, research, and leadership.
Dr. Apodaca is assistant professor and nurse practitioner hospitalist at the University of New Mexico. She is one of the first APPNP/PAs to receive faculty appointment at UNM. She serves as codirector of the UNM APP Hospital Medicine Fellowship and director of the APP Hospital Medicine Team. She is also the president of the New Mexico Chapter of SHM and is the first APP at her institution to achieve designation as a Fellow in Hospital Medicine.
As an academic nurse practitioner hospitalist with faculty and leadership roles, I found that HM19 had many important and helpful topics that apply directly to my practice.
The “Onboarding Best Practices” session provided specific examples and tips for clinical ramp up, enculturation, and orienting staff to an academic career. As a result of this talk, I began the process of establishing a formal enculturation activity for new hires that includes a panel of senior advanced practice provider (APP) hospitalists to give career path advice.
The “Adaptive Leadership for Hospitalists” workshop provided the opportunity to practice emotional intelligence and effective communication in managing routine and difficult leadership interactions. The “Practice Models/Models of Care for Optimal Integration of NPs and PAs” presentation provided insight into variable team structures at other institutions that could be considered for improved efficiency in my group. The “Academic NP/PA” session provided ideas for how to apply for faculty positions in academic institutions. It also gave APPs who have faculty appointment specific illustrations of using current educational, quality improvement, and research projects to promote. I particularly found the “What Mentorship Has Meant to Me” talk significant. It gave practical essential advice on making sure there is chemistry and trust when seeking a mentor and staying engaged to be a successful mentee.
APPs, whether practicing in academic, private, or community settings, should attend the SHM Annual Conference. SHM is very inclusive and proud of APPs as colleagues and leaders. There are topics that directly apply to the needs of APP hospitalists – including career advancement – and that create excitement for APP practice in hospital medicine.
The Annual Conference also provides the very unique opportunity to meet and establish relationships with APP and physician colleagues and leaders nationwide. These relationships lend to career advancing opportunities for collaboration in clinical excellence, education, quality improvement, research, and leadership.
Dr. Apodaca is assistant professor and nurse practitioner hospitalist at the University of New Mexico. She is one of the first APPNP/PAs to receive faculty appointment at UNM. She serves as codirector of the UNM APP Hospital Medicine Fellowship and director of the APP Hospital Medicine Team. She is also the president of the New Mexico Chapter of SHM and is the first APP at her institution to achieve designation as a Fellow in Hospital Medicine.