User login
Following the path of leadership
VA Hospitalist Dr. Matthew Tuck
For Matthew Tuck, MD, MEd, FACP, associate section chief for hospital medicine at the Veterans Affairs Medical Center (VAMC) in Washington, leadership is something that hospitalists can and should be learning at every opportunity.
Some of the best insights about effective leadership, teamwork, and process improvement come from the business world and have been slower to infiltrate into hospital settings and hospitalist groups, he says. But Dr. Tuck has tried to take advantage of numerous opportunities for leadership development in his own career.
He has been a hospitalist since 2010 and is part of a group of 13 physicians, all of whom carry clinical, teaching, and research responsibilities while pursuing a variety of education, quality improvement, and performance improvement topics.
“My chair has been generous about giving me time to do teaching and research and to pursue opportunities for career development,” he said. The Washington VAMC works with four affiliate medical schools in the area, and its six daily hospital medicine services are all 100% teaching services with assigned residents and interns.
Dr. Tuck divides his professional time roughly one-third each between clinical – seeing patients 5 months a year on a consultative or inpatient basis with resident teams; administrative in a variety of roles; and research. He has academic appointments at the George Washington University (GWU) School of Medicine and at the Uniformed Services University of Health Sciences in Bethesda, Md. He developed the coursework for teaching evidence-based medicine to first- and second-year medical students at GWU.
He is also part of a large research consortium with five sites and $7.5 million in funding over 5 years from NIH’s National Institute on Minority Health and Health Disparities to study how genetic information from African American patients can predict their response to cardiovascular medications. He serves as the study’s site Principal Investigator at the VAMC.
Opportunities to advance his leadership skills have included the VA’s Aspiring Leaders Program and Leadership Development Mentoring Program, which teach leadership skills on topical subjects such as teaching, communications skills, and finance. The Master Teacher Leadership Development Program for medical faculty at GWU, where he attended medical school and did his internship and residency, offers six intensive, classroom-based 8-week courses over a 1-year period. They cover various topical subjects with faculty from the business world teaching principles of leadership. The program includes a mentoring action plan for participants and leads to a graduate certificate in leadership development from GWU’s Graduate School of Education and Human Development at the end of the year’s studies.
Dr. Tuck credits completing this kind of coursework for his current position of leadership in the VA and he tries to share what he has learned with the medical students he teaches.
“When I was starting out as a physician, I never received training in how to lead a team. I found myself trying to get everything done for my patients while teaching my learners, and I really struggled for the first couple of years to manage these competing demands on my time,” he said.
Now, on the first day of a new clinical rotation, he meets one-on-one with his residents to set out goals and expectations. “I say: ‘This is how I want rounds to be run. What are your expectations?’ That way we make sure we’re collaborating as a team. I don’t know that medical school prepares you for this kind of teamwork. Unless you bring a background in business, you can really struggle.”
Interest in hospital medicine
“Throughout our medical training we do a variety of rotations and clerkships. I found myself falling in love with all of them – surgery, psychiatry, obstetrics, and gynecology,” Dr. Tuck explained, as he reflected on how he ended up in hospital medicine. “As someone who was interested in all of these different fields of medicine, I considered myself a true medical generalist. And in hospitalized patients, who struggle with all of the different issues that bring them to the hospital, I saw a compilation of all my experiences in residency training combined in one setting.”
Hospital medicine was a relatively young field at that time, with few academic hospitalists, he said. “But I had good mentors who encouraged me to pursue my educational, research, and administrative interests. My affinity for the VA was also largely due to my training. We worked in multiple settings – academic, community-based, National Institutes of Health, and at the VA.”
Dr. Tuck said that, of all the settings in which he practiced, he felt the VA truly trained him best to be a doctor. “The experience made me feel like a holistic practitioner,” he said. “The system allowed me to take the best care of my patients, since I didn’t have to worry about whether I could make needed referrals to specialists. Very early in my internship year we were seeing very sick patients with multiple comorbidities, but it was easy to get a social worker or case manager involved, compared to other settings, which can be more difficult to navigate.”
While the VA is a “great health system,” Dr. Tuck said, the challenge is learning how to work with its bureaucracy. “If you don’t know how the system works, it can seem to get in your way.” But overall, he said, the VA functions well and compares favorably with private sector hospitals and health systems. That was also the conclusion of a recent study in the Journal of General Internal Medicine, which compared the quality of outpatient and inpatient care in VA and non-VA settings using recent performance measure data.1 The authors concluded that the VA system performed similarly or better than non-VA health care on most nationally recognized measures of inpatient and outpatient care quality, although there is wide variation between VA facilities.
Working with the team
Another major interest for Dr. Tuck is team-based learning, which also grew out of his GWU leadership certificate course work on teaching teams and team development. He is working on a draft paper for publication with coauthor Patrick Rendon, MD, associate program director for the University of New Mexico’s internal medicine residency program, building on the group development stage theory – “Forming/Storming/Norming/Performing” – developed by Tuckman and Jenson.2
The theory offers 12 tips for optimizing inpatient ward team performance, such as getting the learners to buy in at an early stage of a project. “Everyone I talk to about our research is eager to learn how to apply these principles. I don’t think we’re unique at this center. We’re constantly rotating learners through the program. If you apply these principles, you can get learners to be more efficient starting from the first day,” he said.
The current inpatient team model at the Washington VAMC involves a broadly representative team from nursing, case management, social work, the business office, medical coding, utilization management, and administration that convenes every morning to discuss patient navigation and difficult discharges. “Everyone sits around a big table, and the six hospital medicine teams rotate through every fifteen minutes to review their patients’ admitting diagnoses, barriers to discharge and plans of care.”
At the patient’s bedside, a Focused Interdisciplinary Team (FIT) model, which Dr. Tuck helped to implement, incorporates a four-step process with clearly defined roles for the attending, nurse, pharmacist, and case manager or social worker. “Since implementation, our data show overall reductions in lengths of stay,” he said.
Dr. Tuck urges other hospitalists to pursue opportunities available to them to develop their leadership skills. “Look to your professional societies such as the Society of General Internal Medicine (SGIM) or SHM.” For example, SGIM’s Academic Hospitalist Commission, which he cochairs, provides a voice on the national stage for academic hospitalists and cosponsors with SHM an annual Academic Hospitalist Academy to support career development for junior academic hospitalists as educational leaders. Since 2016, its Distinguished Professor of Hospital Medicine recognizes a professor of hospital medicine to give a plenary address at the SGIM national meeting.
SGIM’s SCHOLAR Project, a subgroup of its Academic Hospitalist Commission, has worked to identify features of successful academic hospitalist programs, with the results published in the Journal of Hospital Medicine.3
“We learned that what sets successful programs apart is their leadership – as well as protected time for scholarly pursuits,” he said. “We’re all leaders in this field, whether we view ourselves that way or not.”
References
1. Price RA et al. Comparing quality of care in Veterans Affairs and Non–Veterans Affairs settings. J Gen Intern Med. 2018 Oct;33(10):1631-38.
2. Tuckman B, Jensen M. Stages of small group development revisited. Group and Organizational Studies. 1977;2:419-427.
3. Seymann GB et al. Features of successful academic hospitalist programs: Insights from the SCHOLAR (Successful hospitalists in academics and research) project. J Hosp Med. 2016 Oct;11(10):708-13.
VA Hospitalist Dr. Matthew Tuck
VA Hospitalist Dr. Matthew Tuck
For Matthew Tuck, MD, MEd, FACP, associate section chief for hospital medicine at the Veterans Affairs Medical Center (VAMC) in Washington, leadership is something that hospitalists can and should be learning at every opportunity.
Some of the best insights about effective leadership, teamwork, and process improvement come from the business world and have been slower to infiltrate into hospital settings and hospitalist groups, he says. But Dr. Tuck has tried to take advantage of numerous opportunities for leadership development in his own career.
He has been a hospitalist since 2010 and is part of a group of 13 physicians, all of whom carry clinical, teaching, and research responsibilities while pursuing a variety of education, quality improvement, and performance improvement topics.
“My chair has been generous about giving me time to do teaching and research and to pursue opportunities for career development,” he said. The Washington VAMC works with four affiliate medical schools in the area, and its six daily hospital medicine services are all 100% teaching services with assigned residents and interns.
Dr. Tuck divides his professional time roughly one-third each between clinical – seeing patients 5 months a year on a consultative or inpatient basis with resident teams; administrative in a variety of roles; and research. He has academic appointments at the George Washington University (GWU) School of Medicine and at the Uniformed Services University of Health Sciences in Bethesda, Md. He developed the coursework for teaching evidence-based medicine to first- and second-year medical students at GWU.
He is also part of a large research consortium with five sites and $7.5 million in funding over 5 years from NIH’s National Institute on Minority Health and Health Disparities to study how genetic information from African American patients can predict their response to cardiovascular medications. He serves as the study’s site Principal Investigator at the VAMC.
Opportunities to advance his leadership skills have included the VA’s Aspiring Leaders Program and Leadership Development Mentoring Program, which teach leadership skills on topical subjects such as teaching, communications skills, and finance. The Master Teacher Leadership Development Program for medical faculty at GWU, where he attended medical school and did his internship and residency, offers six intensive, classroom-based 8-week courses over a 1-year period. They cover various topical subjects with faculty from the business world teaching principles of leadership. The program includes a mentoring action plan for participants and leads to a graduate certificate in leadership development from GWU’s Graduate School of Education and Human Development at the end of the year’s studies.
Dr. Tuck credits completing this kind of coursework for his current position of leadership in the VA and he tries to share what he has learned with the medical students he teaches.
“When I was starting out as a physician, I never received training in how to lead a team. I found myself trying to get everything done for my patients while teaching my learners, and I really struggled for the first couple of years to manage these competing demands on my time,” he said.
Now, on the first day of a new clinical rotation, he meets one-on-one with his residents to set out goals and expectations. “I say: ‘This is how I want rounds to be run. What are your expectations?’ That way we make sure we’re collaborating as a team. I don’t know that medical school prepares you for this kind of teamwork. Unless you bring a background in business, you can really struggle.”
Interest in hospital medicine
“Throughout our medical training we do a variety of rotations and clerkships. I found myself falling in love with all of them – surgery, psychiatry, obstetrics, and gynecology,” Dr. Tuck explained, as he reflected on how he ended up in hospital medicine. “As someone who was interested in all of these different fields of medicine, I considered myself a true medical generalist. And in hospitalized patients, who struggle with all of the different issues that bring them to the hospital, I saw a compilation of all my experiences in residency training combined in one setting.”
Hospital medicine was a relatively young field at that time, with few academic hospitalists, he said. “But I had good mentors who encouraged me to pursue my educational, research, and administrative interests. My affinity for the VA was also largely due to my training. We worked in multiple settings – academic, community-based, National Institutes of Health, and at the VA.”
Dr. Tuck said that, of all the settings in which he practiced, he felt the VA truly trained him best to be a doctor. “The experience made me feel like a holistic practitioner,” he said. “The system allowed me to take the best care of my patients, since I didn’t have to worry about whether I could make needed referrals to specialists. Very early in my internship year we were seeing very sick patients with multiple comorbidities, but it was easy to get a social worker or case manager involved, compared to other settings, which can be more difficult to navigate.”
While the VA is a “great health system,” Dr. Tuck said, the challenge is learning how to work with its bureaucracy. “If you don’t know how the system works, it can seem to get in your way.” But overall, he said, the VA functions well and compares favorably with private sector hospitals and health systems. That was also the conclusion of a recent study in the Journal of General Internal Medicine, which compared the quality of outpatient and inpatient care in VA and non-VA settings using recent performance measure data.1 The authors concluded that the VA system performed similarly or better than non-VA health care on most nationally recognized measures of inpatient and outpatient care quality, although there is wide variation between VA facilities.
Working with the team
Another major interest for Dr. Tuck is team-based learning, which also grew out of his GWU leadership certificate course work on teaching teams and team development. He is working on a draft paper for publication with coauthor Patrick Rendon, MD, associate program director for the University of New Mexico’s internal medicine residency program, building on the group development stage theory – “Forming/Storming/Norming/Performing” – developed by Tuckman and Jenson.2
The theory offers 12 tips for optimizing inpatient ward team performance, such as getting the learners to buy in at an early stage of a project. “Everyone I talk to about our research is eager to learn how to apply these principles. I don’t think we’re unique at this center. We’re constantly rotating learners through the program. If you apply these principles, you can get learners to be more efficient starting from the first day,” he said.
The current inpatient team model at the Washington VAMC involves a broadly representative team from nursing, case management, social work, the business office, medical coding, utilization management, and administration that convenes every morning to discuss patient navigation and difficult discharges. “Everyone sits around a big table, and the six hospital medicine teams rotate through every fifteen minutes to review their patients’ admitting diagnoses, barriers to discharge and plans of care.”
At the patient’s bedside, a Focused Interdisciplinary Team (FIT) model, which Dr. Tuck helped to implement, incorporates a four-step process with clearly defined roles for the attending, nurse, pharmacist, and case manager or social worker. “Since implementation, our data show overall reductions in lengths of stay,” he said.
Dr. Tuck urges other hospitalists to pursue opportunities available to them to develop their leadership skills. “Look to your professional societies such as the Society of General Internal Medicine (SGIM) or SHM.” For example, SGIM’s Academic Hospitalist Commission, which he cochairs, provides a voice on the national stage for academic hospitalists and cosponsors with SHM an annual Academic Hospitalist Academy to support career development for junior academic hospitalists as educational leaders. Since 2016, its Distinguished Professor of Hospital Medicine recognizes a professor of hospital medicine to give a plenary address at the SGIM national meeting.
SGIM’s SCHOLAR Project, a subgroup of its Academic Hospitalist Commission, has worked to identify features of successful academic hospitalist programs, with the results published in the Journal of Hospital Medicine.3
“We learned that what sets successful programs apart is their leadership – as well as protected time for scholarly pursuits,” he said. “We’re all leaders in this field, whether we view ourselves that way or not.”
References
1. Price RA et al. Comparing quality of care in Veterans Affairs and Non–Veterans Affairs settings. J Gen Intern Med. 2018 Oct;33(10):1631-38.
2. Tuckman B, Jensen M. Stages of small group development revisited. Group and Organizational Studies. 1977;2:419-427.
3. Seymann GB et al. Features of successful academic hospitalist programs: Insights from the SCHOLAR (Successful hospitalists in academics and research) project. J Hosp Med. 2016 Oct;11(10):708-13.
For Matthew Tuck, MD, MEd, FACP, associate section chief for hospital medicine at the Veterans Affairs Medical Center (VAMC) in Washington, leadership is something that hospitalists can and should be learning at every opportunity.
Some of the best insights about effective leadership, teamwork, and process improvement come from the business world and have been slower to infiltrate into hospital settings and hospitalist groups, he says. But Dr. Tuck has tried to take advantage of numerous opportunities for leadership development in his own career.
He has been a hospitalist since 2010 and is part of a group of 13 physicians, all of whom carry clinical, teaching, and research responsibilities while pursuing a variety of education, quality improvement, and performance improvement topics.
“My chair has been generous about giving me time to do teaching and research and to pursue opportunities for career development,” he said. The Washington VAMC works with four affiliate medical schools in the area, and its six daily hospital medicine services are all 100% teaching services with assigned residents and interns.
Dr. Tuck divides his professional time roughly one-third each between clinical – seeing patients 5 months a year on a consultative or inpatient basis with resident teams; administrative in a variety of roles; and research. He has academic appointments at the George Washington University (GWU) School of Medicine and at the Uniformed Services University of Health Sciences in Bethesda, Md. He developed the coursework for teaching evidence-based medicine to first- and second-year medical students at GWU.
He is also part of a large research consortium with five sites and $7.5 million in funding over 5 years from NIH’s National Institute on Minority Health and Health Disparities to study how genetic information from African American patients can predict their response to cardiovascular medications. He serves as the study’s site Principal Investigator at the VAMC.
Opportunities to advance his leadership skills have included the VA’s Aspiring Leaders Program and Leadership Development Mentoring Program, which teach leadership skills on topical subjects such as teaching, communications skills, and finance. The Master Teacher Leadership Development Program for medical faculty at GWU, where he attended medical school and did his internship and residency, offers six intensive, classroom-based 8-week courses over a 1-year period. They cover various topical subjects with faculty from the business world teaching principles of leadership. The program includes a mentoring action plan for participants and leads to a graduate certificate in leadership development from GWU’s Graduate School of Education and Human Development at the end of the year’s studies.
Dr. Tuck credits completing this kind of coursework for his current position of leadership in the VA and he tries to share what he has learned with the medical students he teaches.
“When I was starting out as a physician, I never received training in how to lead a team. I found myself trying to get everything done for my patients while teaching my learners, and I really struggled for the first couple of years to manage these competing demands on my time,” he said.
Now, on the first day of a new clinical rotation, he meets one-on-one with his residents to set out goals and expectations. “I say: ‘This is how I want rounds to be run. What are your expectations?’ That way we make sure we’re collaborating as a team. I don’t know that medical school prepares you for this kind of teamwork. Unless you bring a background in business, you can really struggle.”
Interest in hospital medicine
“Throughout our medical training we do a variety of rotations and clerkships. I found myself falling in love with all of them – surgery, psychiatry, obstetrics, and gynecology,” Dr. Tuck explained, as he reflected on how he ended up in hospital medicine. “As someone who was interested in all of these different fields of medicine, I considered myself a true medical generalist. And in hospitalized patients, who struggle with all of the different issues that bring them to the hospital, I saw a compilation of all my experiences in residency training combined in one setting.”
Hospital medicine was a relatively young field at that time, with few academic hospitalists, he said. “But I had good mentors who encouraged me to pursue my educational, research, and administrative interests. My affinity for the VA was also largely due to my training. We worked in multiple settings – academic, community-based, National Institutes of Health, and at the VA.”
Dr. Tuck said that, of all the settings in which he practiced, he felt the VA truly trained him best to be a doctor. “The experience made me feel like a holistic practitioner,” he said. “The system allowed me to take the best care of my patients, since I didn’t have to worry about whether I could make needed referrals to specialists. Very early in my internship year we were seeing very sick patients with multiple comorbidities, but it was easy to get a social worker or case manager involved, compared to other settings, which can be more difficult to navigate.”
While the VA is a “great health system,” Dr. Tuck said, the challenge is learning how to work with its bureaucracy. “If you don’t know how the system works, it can seem to get in your way.” But overall, he said, the VA functions well and compares favorably with private sector hospitals and health systems. That was also the conclusion of a recent study in the Journal of General Internal Medicine, which compared the quality of outpatient and inpatient care in VA and non-VA settings using recent performance measure data.1 The authors concluded that the VA system performed similarly or better than non-VA health care on most nationally recognized measures of inpatient and outpatient care quality, although there is wide variation between VA facilities.
Working with the team
Another major interest for Dr. Tuck is team-based learning, which also grew out of his GWU leadership certificate course work on teaching teams and team development. He is working on a draft paper for publication with coauthor Patrick Rendon, MD, associate program director for the University of New Mexico’s internal medicine residency program, building on the group development stage theory – “Forming/Storming/Norming/Performing” – developed by Tuckman and Jenson.2
The theory offers 12 tips for optimizing inpatient ward team performance, such as getting the learners to buy in at an early stage of a project. “Everyone I talk to about our research is eager to learn how to apply these principles. I don’t think we’re unique at this center. We’re constantly rotating learners through the program. If you apply these principles, you can get learners to be more efficient starting from the first day,” he said.
The current inpatient team model at the Washington VAMC involves a broadly representative team from nursing, case management, social work, the business office, medical coding, utilization management, and administration that convenes every morning to discuss patient navigation and difficult discharges. “Everyone sits around a big table, and the six hospital medicine teams rotate through every fifteen minutes to review their patients’ admitting diagnoses, barriers to discharge and plans of care.”
At the patient’s bedside, a Focused Interdisciplinary Team (FIT) model, which Dr. Tuck helped to implement, incorporates a four-step process with clearly defined roles for the attending, nurse, pharmacist, and case manager or social worker. “Since implementation, our data show overall reductions in lengths of stay,” he said.
Dr. Tuck urges other hospitalists to pursue opportunities available to them to develop their leadership skills. “Look to your professional societies such as the Society of General Internal Medicine (SGIM) or SHM.” For example, SGIM’s Academic Hospitalist Commission, which he cochairs, provides a voice on the national stage for academic hospitalists and cosponsors with SHM an annual Academic Hospitalist Academy to support career development for junior academic hospitalists as educational leaders. Since 2016, its Distinguished Professor of Hospital Medicine recognizes a professor of hospital medicine to give a plenary address at the SGIM national meeting.
SGIM’s SCHOLAR Project, a subgroup of its Academic Hospitalist Commission, has worked to identify features of successful academic hospitalist programs, with the results published in the Journal of Hospital Medicine.3
“We learned that what sets successful programs apart is their leadership – as well as protected time for scholarly pursuits,” he said. “We’re all leaders in this field, whether we view ourselves that way or not.”
References
1. Price RA et al. Comparing quality of care in Veterans Affairs and Non–Veterans Affairs settings. J Gen Intern Med. 2018 Oct;33(10):1631-38.
2. Tuckman B, Jensen M. Stages of small group development revisited. Group and Organizational Studies. 1977;2:419-427.
3. Seymann GB et al. Features of successful academic hospitalist programs: Insights from the SCHOLAR (Successful hospitalists in academics and research) project. J Hosp Med. 2016 Oct;11(10):708-13.
Culture: An unseen force in the hospital workplace
Parallels from the airline industry
“Workplace culture” has a profound influence on the success or failure of a team in the modern-day work environment, where teamwork and interpersonal interactions have paramount importance. Crew resource management (CRM), a technique developed originally by the airline industry, has been used as a tool to improve safety and quality in ICUs, trauma rooms, and operating rooms.1,2 This article discusses the use of CRM in hospital medicine as a tool for training and maintaining a favorable workplace culture.
Origin and evolution of CRM
United Airlines instituted the airline industry’s first crew resource management for pilots in 1981, following the 1978 crash of United Flight 173 in Portland, Ore. CRM was created based on recommendations from the National Transportation Safety Board and from a NASA workshop held subsequently.3 CRM has since evolved through five generations, and is a required annual training for most major commercial airline companies around the world. It also has been adapted for personnel training by several modern international industries.4
From the airline industry to the hospital
The health care industry is similar to the airline industry in that there is absolutely no margin of error, and that workplace culture plays a very important role. The culture being referred to here is the sum total of values, beliefs, work ethics, work strategies, strengths, and weaknesses of a group of people, and how they interact as a group. In other words, it is the dynamics of a group.
According to Donelson R. Forsyth, a social and personality psychologist at the University of Richmond (Virginia), the two key determinants of successful teamwork are a “shared mental representation of the task,” which refers to an in-depth understanding of the team and the tasks they are attempting; and “group unity/cohesion,” which means that, generally, members of cohesive groups like each other and the group, and they also are united in their pursuit of collective, group-level goals.5
Understanding the culture of a hospitalist team
Analyzing group dynamics and actively managing them toward both the institutional and global goals of health care is critical for the success of an organization. This is the core of successfully managing any team in any industry.
Additionally, the rapidly changing health care climate and insurance payment systems requires hospital medicine groups to rapidly adapt to the constantly changing health care business environment. As a result, there are a couple of ways to evaluate the effectiveness of the team:
- Measure tangible outcomes. The outcomes have to be well defined, important and measurable. These could be cost of care, quality of care, engagement of the team etc. These tangible measures’ outcome over a period of time can be used as a measure of how effective the team is.
- Simply ask your team! It is very important to know what core values the team holds dear. The best way to get that information from the team is to find out the de facto leaders of the team. They should be involved in the decision-making process, thus making them valuable to the management as well as the team.
Culture shapes outcomes
We have used the analogy of a convex and concave lens to help understand this better. A well-developed and well-coordinated team is like convex lens. A lens’ ability to converge or diverge light rays depends on certain characteristics like the curvature of surfaces and refractory index. Likewise, the culture of a group determines its ability to transform all the demands of the collective workload toward a unified goal/outcome. If it is favorable, the group will work as one and success will happen automatically.
Unfortunately, the opposite of this, (the concave lens effect), is more commonplace, where the dynamics of a team prevent the goals being achieved, as there is discordance, poor coordination of ideas and values, and team members not liking each other.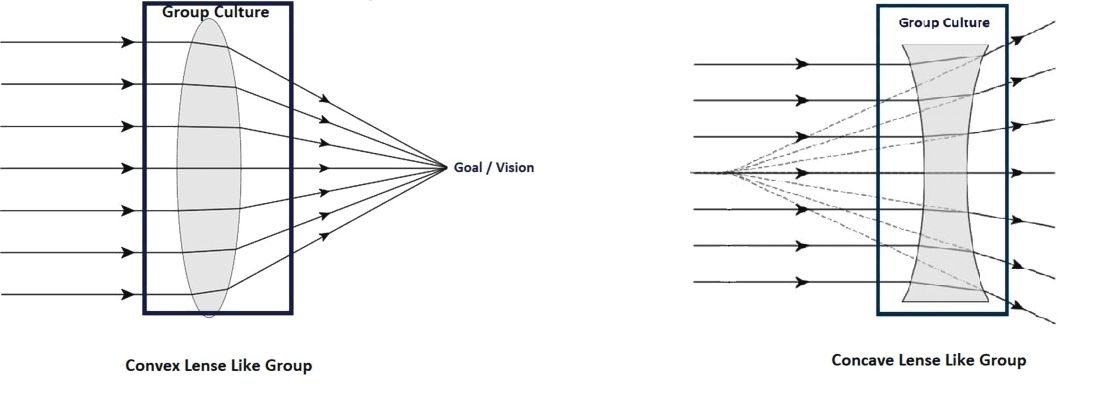
Most teams would fall somewhere within this spectrum, spanning the most favorable convex lens–like group to the least favorable concave lens–like group.
Change team dynamics using CRM principles
The concept of using CRM principles in health care is not entirely new. Such agencies as the Joint Commission and the Agency for Healthcare Research and Quality recommend using principles of CRM to improve communications, and as an error-prevention tool in health care.6
This approach can be broken down into four important steps:
1. Recruit right. It is important to make sure that the new recruit is the right fit for the team and that the de facto leaders and a few other team members are involved in interviewing the candidates. Their assessment should be given due consideration in making the decision to give the new recruit the job.
Every program looks for aspects like clinical competence, interpersonal communication, teamwork, etc., in a candidate, but it is even more important to make sure the candidate has the tenets that would make him/her a part of that particular team.
2. Train well. The newly recruited providers should be given focused training and the seasoned providers should be given refresher training at regular intervals. Care should be taken in designing the training programs in such a way that the providers are trained in skills that they don’t always think about, things that aren’t readily obvious, and in skills that they never get trained in during medical school and residency.
Specifically, they should be trained in:
- Values. These should include the values of both the organization and the team.
- Safety. This should include all the safety protocols that are in place in the organization - where to get help, how to report unsafe events etc.
- Communication.
Within the group: Have a mentor for the new provider, and also develop a culture where he/she feels comfortable to reach out to anyone in the team for help.
With patients and families: This training should ideally be done in a simulated environment if possible.
With other groups in the hospital: Consultants, nurses, other ancillary staff. Give them an idea about the prevailing culture in the organization with regard to these groups, so that they know what to expect when dealing with them.
- Managing perceptions. How the providers are viewed in the hospital, and how to improve it or maintain it.
- Nurturing the good. Use positive reinforcements to solidify the positive aspects of group dynamics these individuals might possess.
- Weeding out the bad. Use training and feedback to alter the negative group dynamic aspects.
3. Intervene. This is necessary either to maintain the positive aspects of a team that is already high-functioning, or to transform a poorly functioning team into a well-coordinated team. This is where the principles of CRM are going to be most useful.
There are five generations of CRM, each with a different focus.6 Only the aspects relevant to hospital medicine training are mentioned here.
- Communication. Address the gaps in communication. It is important to include people who are trusted by the team in designing and executing these sessions.
- Leadership. The goal should be to encourage the team to take ownership of the program. This will make a tremendous change in the ability of a team to deliver and rise up to challenges. The organizational leadership has to be willing to elevate the leaders of the group to positions where they can meaningfully take part in managing the team and making decisions that are critical to the team.
- Burnout management. Providers getting disillusioned: having no work-life balance; not getting enough respect from management, as well as other groups of doctors/nurses/etc. in the hospital; they are subject to bad scheduling and poor pay – all of which can all lead to career-ending burnout. It is important to recognize this and mitigate the factors that cause burnout.
- Organizational culture. If the team feels valued and supported, they will, in turn, work hard toward success. Creative leadership and a willingness to accommodate what matters the most to the team is essential for achieving this.
- Simulated training. These can be done in simulation labs, or in-group sessions with the team, re-creating difficult scenarios or problems in which the whole team can come together and solve them.
- Error containment and management. The team needs to identify possible sources of error and contain them before errors happen. The group should get together if a serious event happens and brainstorm why it happened and take measures to prevent it.
4. Reevaluate. Team dynamics tend to change over time. It is important to constantly re-evaluate the team and make sure that the team’s culture remains favorable. There should be recurrent cycles of retraining and interventions to maintain the positive growth that has been attained, as depicted in the schematic below:
Conclusion
CRM is widely accepted as an effective tool in training individuals in many high performing industries. This article describes a framework in which the principles of CRM can be applied to hospital medicine to maintain positive work culture.
Dr. Prabhakaran is director of hospital medicine transitions of care, Baystate Medical Center, Springfield, Mass., and assistant professor of medicine, University of Massachusetts, Worcester. Dr. Medarametla is medical director, hospital medicine, Baystate Medical Center, and assistant professor of medicine, University of Massachusetts.
References
1. Haerkens MH et al. Crew Resource Management in the ICU: The need for culture change. Ann Intensive Care. 2012 Aug 22;2:39.
2. Haerkens MH et al. Crew Resource Management in the trauma room: A prospective 3-year cohort study. Eur J Emerg Med. 2018 Aug;25(4):281-7.
3. Malcolm Gladwell. The ethnic theory of plane crashes. Outliers: The Story of Success. (Boston: Little, Brown and Company; 2008:177-223).
4. Helmreich RL et al. The evolution of Crew Resource Management training in commercial aviation. Int J Aviat Psychol. 1999;9(1):19-32.
5. Forsyth DR. The psychology of groups. In R. Biswas-Diener & E. Diener (eds), Noba textbook series: Psychology. Champaign, Ill: DEF publishers; 2017.
6. Crew Resource Management. Available at Aviation Knowledge. Accessed Dec. 20, 2017.
Parallels from the airline industry
Parallels from the airline industry
“Workplace culture” has a profound influence on the success or failure of a team in the modern-day work environment, where teamwork and interpersonal interactions have paramount importance. Crew resource management (CRM), a technique developed originally by the airline industry, has been used as a tool to improve safety and quality in ICUs, trauma rooms, and operating rooms.1,2 This article discusses the use of CRM in hospital medicine as a tool for training and maintaining a favorable workplace culture.
Origin and evolution of CRM
United Airlines instituted the airline industry’s first crew resource management for pilots in 1981, following the 1978 crash of United Flight 173 in Portland, Ore. CRM was created based on recommendations from the National Transportation Safety Board and from a NASA workshop held subsequently.3 CRM has since evolved through five generations, and is a required annual training for most major commercial airline companies around the world. It also has been adapted for personnel training by several modern international industries.4
From the airline industry to the hospital
The health care industry is similar to the airline industry in that there is absolutely no margin of error, and that workplace culture plays a very important role. The culture being referred to here is the sum total of values, beliefs, work ethics, work strategies, strengths, and weaknesses of a group of people, and how they interact as a group. In other words, it is the dynamics of a group.
According to Donelson R. Forsyth, a social and personality psychologist at the University of Richmond (Virginia), the two key determinants of successful teamwork are a “shared mental representation of the task,” which refers to an in-depth understanding of the team and the tasks they are attempting; and “group unity/cohesion,” which means that, generally, members of cohesive groups like each other and the group, and they also are united in their pursuit of collective, group-level goals.5
Understanding the culture of a hospitalist team
Analyzing group dynamics and actively managing them toward both the institutional and global goals of health care is critical for the success of an organization. This is the core of successfully managing any team in any industry.
Additionally, the rapidly changing health care climate and insurance payment systems requires hospital medicine groups to rapidly adapt to the constantly changing health care business environment. As a result, there are a couple of ways to evaluate the effectiveness of the team:
- Measure tangible outcomes. The outcomes have to be well defined, important and measurable. These could be cost of care, quality of care, engagement of the team etc. These tangible measures’ outcome over a period of time can be used as a measure of how effective the team is.
- Simply ask your team! It is very important to know what core values the team holds dear. The best way to get that information from the team is to find out the de facto leaders of the team. They should be involved in the decision-making process, thus making them valuable to the management as well as the team.
Culture shapes outcomes
We have used the analogy of a convex and concave lens to help understand this better. A well-developed and well-coordinated team is like convex lens. A lens’ ability to converge or diverge light rays depends on certain characteristics like the curvature of surfaces and refractory index. Likewise, the culture of a group determines its ability to transform all the demands of the collective workload toward a unified goal/outcome. If it is favorable, the group will work as one and success will happen automatically.
Unfortunately, the opposite of this, (the concave lens effect), is more commonplace, where the dynamics of a team prevent the goals being achieved, as there is discordance, poor coordination of ideas and values, and team members not liking each other.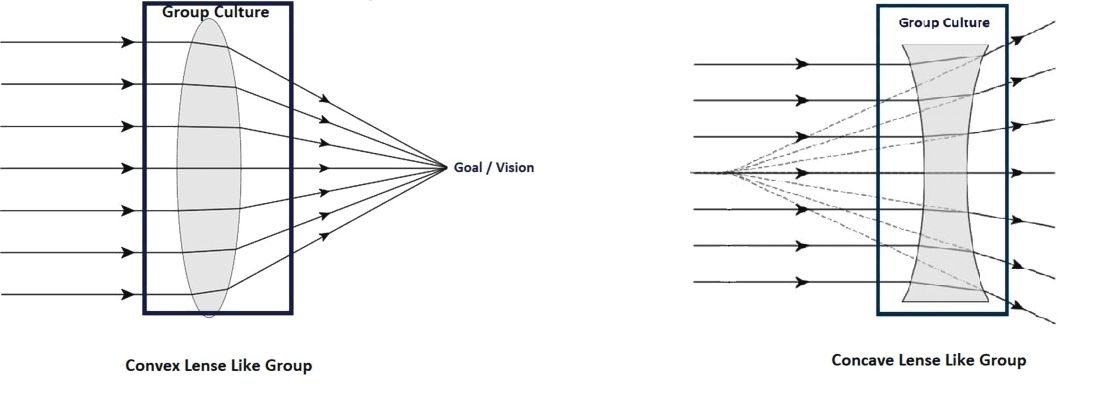
Most teams would fall somewhere within this spectrum, spanning the most favorable convex lens–like group to the least favorable concave lens–like group.
Change team dynamics using CRM principles
The concept of using CRM principles in health care is not entirely new. Such agencies as the Joint Commission and the Agency for Healthcare Research and Quality recommend using principles of CRM to improve communications, and as an error-prevention tool in health care.6
This approach can be broken down into four important steps:
1. Recruit right. It is important to make sure that the new recruit is the right fit for the team and that the de facto leaders and a few other team members are involved in interviewing the candidates. Their assessment should be given due consideration in making the decision to give the new recruit the job.
Every program looks for aspects like clinical competence, interpersonal communication, teamwork, etc., in a candidate, but it is even more important to make sure the candidate has the tenets that would make him/her a part of that particular team.
2. Train well. The newly recruited providers should be given focused training and the seasoned providers should be given refresher training at regular intervals. Care should be taken in designing the training programs in such a way that the providers are trained in skills that they don’t always think about, things that aren’t readily obvious, and in skills that they never get trained in during medical school and residency.
Specifically, they should be trained in:
- Values. These should include the values of both the organization and the team.
- Safety. This should include all the safety protocols that are in place in the organization - where to get help, how to report unsafe events etc.
- Communication.
Within the group: Have a mentor for the new provider, and also develop a culture where he/she feels comfortable to reach out to anyone in the team for help.
With patients and families: This training should ideally be done in a simulated environment if possible.
With other groups in the hospital: Consultants, nurses, other ancillary staff. Give them an idea about the prevailing culture in the organization with regard to these groups, so that they know what to expect when dealing with them.
- Managing perceptions. How the providers are viewed in the hospital, and how to improve it or maintain it.
- Nurturing the good. Use positive reinforcements to solidify the positive aspects of group dynamics these individuals might possess.
- Weeding out the bad. Use training and feedback to alter the negative group dynamic aspects.
3. Intervene. This is necessary either to maintain the positive aspects of a team that is already high-functioning, or to transform a poorly functioning team into a well-coordinated team. This is where the principles of CRM are going to be most useful.
There are five generations of CRM, each with a different focus.6 Only the aspects relevant to hospital medicine training are mentioned here.
- Communication. Address the gaps in communication. It is important to include people who are trusted by the team in designing and executing these sessions.
- Leadership. The goal should be to encourage the team to take ownership of the program. This will make a tremendous change in the ability of a team to deliver and rise up to challenges. The organizational leadership has to be willing to elevate the leaders of the group to positions where they can meaningfully take part in managing the team and making decisions that are critical to the team.
- Burnout management. Providers getting disillusioned: having no work-life balance; not getting enough respect from management, as well as other groups of doctors/nurses/etc. in the hospital; they are subject to bad scheduling and poor pay – all of which can all lead to career-ending burnout. It is important to recognize this and mitigate the factors that cause burnout.
- Organizational culture. If the team feels valued and supported, they will, in turn, work hard toward success. Creative leadership and a willingness to accommodate what matters the most to the team is essential for achieving this.
- Simulated training. These can be done in simulation labs, or in-group sessions with the team, re-creating difficult scenarios or problems in which the whole team can come together and solve them.
- Error containment and management. The team needs to identify possible sources of error and contain them before errors happen. The group should get together if a serious event happens and brainstorm why it happened and take measures to prevent it.
4. Reevaluate. Team dynamics tend to change over time. It is important to constantly re-evaluate the team and make sure that the team’s culture remains favorable. There should be recurrent cycles of retraining and interventions to maintain the positive growth that has been attained, as depicted in the schematic below:
Conclusion
CRM is widely accepted as an effective tool in training individuals in many high performing industries. This article describes a framework in which the principles of CRM can be applied to hospital medicine to maintain positive work culture.
Dr. Prabhakaran is director of hospital medicine transitions of care, Baystate Medical Center, Springfield, Mass., and assistant professor of medicine, University of Massachusetts, Worcester. Dr. Medarametla is medical director, hospital medicine, Baystate Medical Center, and assistant professor of medicine, University of Massachusetts.
References
1. Haerkens MH et al. Crew Resource Management in the ICU: The need for culture change. Ann Intensive Care. 2012 Aug 22;2:39.
2. Haerkens MH et al. Crew Resource Management in the trauma room: A prospective 3-year cohort study. Eur J Emerg Med. 2018 Aug;25(4):281-7.
3. Malcolm Gladwell. The ethnic theory of plane crashes. Outliers: The Story of Success. (Boston: Little, Brown and Company; 2008:177-223).
4. Helmreich RL et al. The evolution of Crew Resource Management training in commercial aviation. Int J Aviat Psychol. 1999;9(1):19-32.
5. Forsyth DR. The psychology of groups. In R. Biswas-Diener & E. Diener (eds), Noba textbook series: Psychology. Champaign, Ill: DEF publishers; 2017.
6. Crew Resource Management. Available at Aviation Knowledge. Accessed Dec. 20, 2017.
“Workplace culture” has a profound influence on the success or failure of a team in the modern-day work environment, where teamwork and interpersonal interactions have paramount importance. Crew resource management (CRM), a technique developed originally by the airline industry, has been used as a tool to improve safety and quality in ICUs, trauma rooms, and operating rooms.1,2 This article discusses the use of CRM in hospital medicine as a tool for training and maintaining a favorable workplace culture.
Origin and evolution of CRM
United Airlines instituted the airline industry’s first crew resource management for pilots in 1981, following the 1978 crash of United Flight 173 in Portland, Ore. CRM was created based on recommendations from the National Transportation Safety Board and from a NASA workshop held subsequently.3 CRM has since evolved through five generations, and is a required annual training for most major commercial airline companies around the world. It also has been adapted for personnel training by several modern international industries.4
From the airline industry to the hospital
The health care industry is similar to the airline industry in that there is absolutely no margin of error, and that workplace culture plays a very important role. The culture being referred to here is the sum total of values, beliefs, work ethics, work strategies, strengths, and weaknesses of a group of people, and how they interact as a group. In other words, it is the dynamics of a group.
According to Donelson R. Forsyth, a social and personality psychologist at the University of Richmond (Virginia), the two key determinants of successful teamwork are a “shared mental representation of the task,” which refers to an in-depth understanding of the team and the tasks they are attempting; and “group unity/cohesion,” which means that, generally, members of cohesive groups like each other and the group, and they also are united in their pursuit of collective, group-level goals.5
Understanding the culture of a hospitalist team
Analyzing group dynamics and actively managing them toward both the institutional and global goals of health care is critical for the success of an organization. This is the core of successfully managing any team in any industry.
Additionally, the rapidly changing health care climate and insurance payment systems requires hospital medicine groups to rapidly adapt to the constantly changing health care business environment. As a result, there are a couple of ways to evaluate the effectiveness of the team:
- Measure tangible outcomes. The outcomes have to be well defined, important and measurable. These could be cost of care, quality of care, engagement of the team etc. These tangible measures’ outcome over a period of time can be used as a measure of how effective the team is.
- Simply ask your team! It is very important to know what core values the team holds dear. The best way to get that information from the team is to find out the de facto leaders of the team. They should be involved in the decision-making process, thus making them valuable to the management as well as the team.
Culture shapes outcomes
We have used the analogy of a convex and concave lens to help understand this better. A well-developed and well-coordinated team is like convex lens. A lens’ ability to converge or diverge light rays depends on certain characteristics like the curvature of surfaces and refractory index. Likewise, the culture of a group determines its ability to transform all the demands of the collective workload toward a unified goal/outcome. If it is favorable, the group will work as one and success will happen automatically.
Unfortunately, the opposite of this, (the concave lens effect), is more commonplace, where the dynamics of a team prevent the goals being achieved, as there is discordance, poor coordination of ideas and values, and team members not liking each other.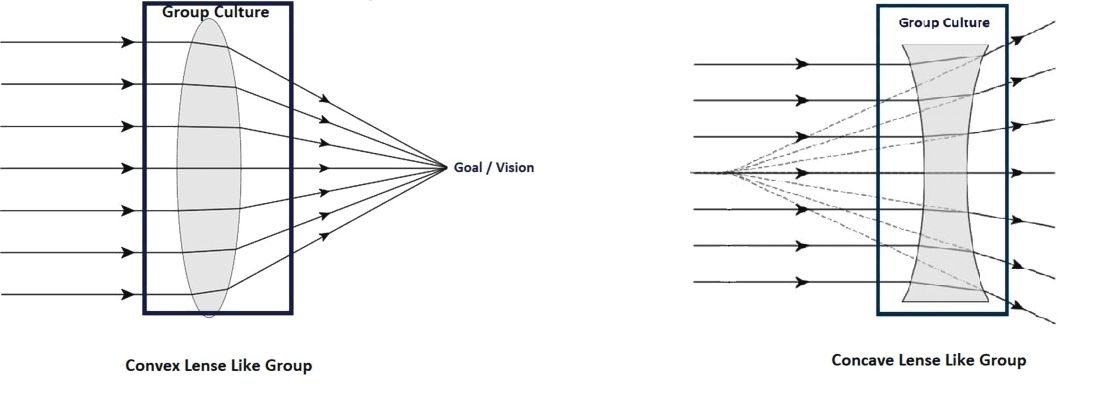
Most teams would fall somewhere within this spectrum, spanning the most favorable convex lens–like group to the least favorable concave lens–like group.
Change team dynamics using CRM principles
The concept of using CRM principles in health care is not entirely new. Such agencies as the Joint Commission and the Agency for Healthcare Research and Quality recommend using principles of CRM to improve communications, and as an error-prevention tool in health care.6
This approach can be broken down into four important steps:
1. Recruit right. It is important to make sure that the new recruit is the right fit for the team and that the de facto leaders and a few other team members are involved in interviewing the candidates. Their assessment should be given due consideration in making the decision to give the new recruit the job.
Every program looks for aspects like clinical competence, interpersonal communication, teamwork, etc., in a candidate, but it is even more important to make sure the candidate has the tenets that would make him/her a part of that particular team.
2. Train well. The newly recruited providers should be given focused training and the seasoned providers should be given refresher training at regular intervals. Care should be taken in designing the training programs in such a way that the providers are trained in skills that they don’t always think about, things that aren’t readily obvious, and in skills that they never get trained in during medical school and residency.
Specifically, they should be trained in:
- Values. These should include the values of both the organization and the team.
- Safety. This should include all the safety protocols that are in place in the organization - where to get help, how to report unsafe events etc.
- Communication.
Within the group: Have a mentor for the new provider, and also develop a culture where he/she feels comfortable to reach out to anyone in the team for help.
With patients and families: This training should ideally be done in a simulated environment if possible.
With other groups in the hospital: Consultants, nurses, other ancillary staff. Give them an idea about the prevailing culture in the organization with regard to these groups, so that they know what to expect when dealing with them.
- Managing perceptions. How the providers are viewed in the hospital, and how to improve it or maintain it.
- Nurturing the good. Use positive reinforcements to solidify the positive aspects of group dynamics these individuals might possess.
- Weeding out the bad. Use training and feedback to alter the negative group dynamic aspects.
3. Intervene. This is necessary either to maintain the positive aspects of a team that is already high-functioning, or to transform a poorly functioning team into a well-coordinated team. This is where the principles of CRM are going to be most useful.
There are five generations of CRM, each with a different focus.6 Only the aspects relevant to hospital medicine training are mentioned here.
- Communication. Address the gaps in communication. It is important to include people who are trusted by the team in designing and executing these sessions.
- Leadership. The goal should be to encourage the team to take ownership of the program. This will make a tremendous change in the ability of a team to deliver and rise up to challenges. The organizational leadership has to be willing to elevate the leaders of the group to positions where they can meaningfully take part in managing the team and making decisions that are critical to the team.
- Burnout management. Providers getting disillusioned: having no work-life balance; not getting enough respect from management, as well as other groups of doctors/nurses/etc. in the hospital; they are subject to bad scheduling and poor pay – all of which can all lead to career-ending burnout. It is important to recognize this and mitigate the factors that cause burnout.
- Organizational culture. If the team feels valued and supported, they will, in turn, work hard toward success. Creative leadership and a willingness to accommodate what matters the most to the team is essential for achieving this.
- Simulated training. These can be done in simulation labs, or in-group sessions with the team, re-creating difficult scenarios or problems in which the whole team can come together and solve them.
- Error containment and management. The team needs to identify possible sources of error and contain them before errors happen. The group should get together if a serious event happens and brainstorm why it happened and take measures to prevent it.
4. Reevaluate. Team dynamics tend to change over time. It is important to constantly re-evaluate the team and make sure that the team’s culture remains favorable. There should be recurrent cycles of retraining and interventions to maintain the positive growth that has been attained, as depicted in the schematic below:
Conclusion
CRM is widely accepted as an effective tool in training individuals in many high performing industries. This article describes a framework in which the principles of CRM can be applied to hospital medicine to maintain positive work culture.
Dr. Prabhakaran is director of hospital medicine transitions of care, Baystate Medical Center, Springfield, Mass., and assistant professor of medicine, University of Massachusetts, Worcester. Dr. Medarametla is medical director, hospital medicine, Baystate Medical Center, and assistant professor of medicine, University of Massachusetts.
References
1. Haerkens MH et al. Crew Resource Management in the ICU: The need for culture change. Ann Intensive Care. 2012 Aug 22;2:39.
2. Haerkens MH et al. Crew Resource Management in the trauma room: A prospective 3-year cohort study. Eur J Emerg Med. 2018 Aug;25(4):281-7.
3. Malcolm Gladwell. The ethnic theory of plane crashes. Outliers: The Story of Success. (Boston: Little, Brown and Company; 2008:177-223).
4. Helmreich RL et al. The evolution of Crew Resource Management training in commercial aviation. Int J Aviat Psychol. 1999;9(1):19-32.
5. Forsyth DR. The psychology of groups. In R. Biswas-Diener & E. Diener (eds), Noba textbook series: Psychology. Champaign, Ill: DEF publishers; 2017.
6. Crew Resource Management. Available at Aviation Knowledge. Accessed Dec. 20, 2017.
Living into your legacy
What I learned from women of impact
The word legacy has been synonymous with death to me. When so and so dies, we discuss their legacy. I had a powerful experience that changed my mind on this word that is befitting for this Legacies column.
Seven years ago, I was sitting in a room of powerful women and I was the youngest one there. I wasn’t sure how I got there, but I was glad I did because it changed my life. At the time, I was panicked. The exercise was called “Craft your legacy statement.”
But, this exercise was different. The ask was to “live into your legacy.” Craft a legacy statement in THREE minutes that summarizes what you want your legacy to be … and then decide the three things you need to do now to get there. So, here is my exact legacy 3-minute statement: I am an innovator pushing teaching hospitals to optimize training and patient care delivery through novel technologies and systems science. Clearly, I did not aim high enough. One of the other attendees stated her legacy simply as “Unleash the impossible!” So clearly, I was not able to think big at that moment, but I trudged on.
Next, I had to write the three things I was going to do to enact my legacy today. Things went from bad to worse quickly since I knew this was not going to be easy. The #1 thing had to be something I was going to stop doing because it did not fit with my legacy; #2 was what I was going to start doing to enact this legacy now; and, #3 was something I was going to do to get me closer to what I wanted to be doing. So, my #1, resign my current leadership role that I had had for 8 years; #2, start joining national committees that bridge education and quality; and #3, meet with senior leadership to pitch this new role as a bridging leader, aligning education and quality.
Like all conferences, I went home and forgot what I had done and learned. I settled back into my old life and routines. A few weeks later, a plain looking envelope with awful penmanship showed up at my doorstep addressed to me. It wasn’t until after I opened it and read what was inside that I realized I was the one with horrible penmanship! I completely forgot that I wrote this letter to myself even though they told me it would come and I would forget I wrote it! So, how did I do? Let’s just say if the letter did not arrive, I am not sure where I would be. Fortunately, it did come, and I followed my own orders. Fast forward to present day and I recently stepped into a new role – associate chief medical officer: clinical learning environment – a bridging leader who aligns education and clinical care missions for our health system. Let’s just say again, had that letter not arrived, I am not sure where I would be now.
I have been fortunate to do many things in hospital medicine – clinician, researcher, educator, and my latest role as a leader. Through it all, I would say that there are some lessons that I have picked up along the way that helped me advance, in ways I did not realize:
- Be bold. Years ago, when I was asked by my chair who they should pick to be chief resident, I thought “This must be a trick question – I should definitely tell him why I should be chosen – and then pick the next best person who I want to work with.” Apparently, I was the only person who did that, and that is why my chair chose me. Everyone else picked two other people. So the take-home point here is do not sell yourself short … ever.
- Look for the hidden gateways. A few years ago, I was asked if I wanted to be an institutional leader by the person who currently had that role. I was kind of thrown for a loop, since of course I would not want to appear like I wanted to take his job. I said everything was fine and I felt pretty good about my current positions. It was only a few weeks later that I realized that he was ascertaining my interest in his job since he was leaving. They gave the job to someone else and the word on the street was I was not interested. I totally missed the gate! While it wasn’t necessarily the job I missed out on, it was the opportunity to consider the job because I was afraid. So, don’t miss the gate. It’s the wormhole to a different life that may be the right one for you, but you need to “see it” to seize it.
- Work hard for the money and for the fun. There are many things Gwyneth Paltrow does that I do not agree with, but I will give her credit for one important lesson: she divides her movie roles into those she does for love (for example, The Royal Tenenbaums) and those she does for money (for example, Shallow Hal). It made me realize that even a Hollywood starlet has to do the stuff she may not want to do for the money. So, as a young person, you have to work hard for the money, but ideally it will help you take on a project you love, whatever it is. You’ve won the game when you’re mostly paid to work for the fun ... but that may take some time.
- Always optimize what is best for you personally AND professionally. While I was on maternity leave, the job of my dreams presented itself – or so I thought it did. It was at the intersection of policy, quality, and education, with a national stage, and I would not need to move. But, I knew I could not accept the travel commitment with a young child. While I wondered if I would have regrets, it turns out the right decision professionally also has to work personally. Likewise, there are professional obligations that I take on because it works personally.
- Figure out who your tea house pals are. A few years ago, I was in San Francisco with two close friends having an epic moment about what to do with our lives as adults. We were all on the cusp of changing our directions. Not surprisingly, we could see what the other needed to do, but we could not see it for ourselves. We still text each other sometimes about the need to go back to the Tea House. Sometimes your “tea house pals” are not necessarily those around you every day. They know you, but not everyone in your work place. This “arm’s length” or distance gives them the rational, unbiased perspective to advise you, that you or your colleagues will never have.
- Look for ways to enjoy the journey. Medicine is a very long road. I routinely think about this working with all the trainees and junior faculty I encounter. You can’t be in this solely for the end of the journey. The key is to find the joy in the journey. For me, that has always come from seeking out like-minded fellow travelers to share my highs and lows. While I tweet for many reasons, a big reason is that I take pleasure in watching others on the journey and also sharing my own journey.
Here’s to your journey and living your legacy!
Dr. Arora is associate chief medical officer, clinical learning environment, at University of Chicago Medicine, and assistant dean for scholarship and discovery at the University of Chicago Pritzker School of Medicine. You can follow her journey on Twitter.
What I learned from women of impact
What I learned from women of impact
The word legacy has been synonymous with death to me. When so and so dies, we discuss their legacy. I had a powerful experience that changed my mind on this word that is befitting for this Legacies column.
Seven years ago, I was sitting in a room of powerful women and I was the youngest one there. I wasn’t sure how I got there, but I was glad I did because it changed my life. At the time, I was panicked. The exercise was called “Craft your legacy statement.”
But, this exercise was different. The ask was to “live into your legacy.” Craft a legacy statement in THREE minutes that summarizes what you want your legacy to be … and then decide the three things you need to do now to get there. So, here is my exact legacy 3-minute statement: I am an innovator pushing teaching hospitals to optimize training and patient care delivery through novel technologies and systems science. Clearly, I did not aim high enough. One of the other attendees stated her legacy simply as “Unleash the impossible!” So clearly, I was not able to think big at that moment, but I trudged on.
Next, I had to write the three things I was going to do to enact my legacy today. Things went from bad to worse quickly since I knew this was not going to be easy. The #1 thing had to be something I was going to stop doing because it did not fit with my legacy; #2 was what I was going to start doing to enact this legacy now; and, #3 was something I was going to do to get me closer to what I wanted to be doing. So, my #1, resign my current leadership role that I had had for 8 years; #2, start joining national committees that bridge education and quality; and #3, meet with senior leadership to pitch this new role as a bridging leader, aligning education and quality.
Like all conferences, I went home and forgot what I had done and learned. I settled back into my old life and routines. A few weeks later, a plain looking envelope with awful penmanship showed up at my doorstep addressed to me. It wasn’t until after I opened it and read what was inside that I realized I was the one with horrible penmanship! I completely forgot that I wrote this letter to myself even though they told me it would come and I would forget I wrote it! So, how did I do? Let’s just say if the letter did not arrive, I am not sure where I would be. Fortunately, it did come, and I followed my own orders. Fast forward to present day and I recently stepped into a new role – associate chief medical officer: clinical learning environment – a bridging leader who aligns education and clinical care missions for our health system. Let’s just say again, had that letter not arrived, I am not sure where I would be now.
I have been fortunate to do many things in hospital medicine – clinician, researcher, educator, and my latest role as a leader. Through it all, I would say that there are some lessons that I have picked up along the way that helped me advance, in ways I did not realize:
- Be bold. Years ago, when I was asked by my chair who they should pick to be chief resident, I thought “This must be a trick question – I should definitely tell him why I should be chosen – and then pick the next best person who I want to work with.” Apparently, I was the only person who did that, and that is why my chair chose me. Everyone else picked two other people. So the take-home point here is do not sell yourself short … ever.
- Look for the hidden gateways. A few years ago, I was asked if I wanted to be an institutional leader by the person who currently had that role. I was kind of thrown for a loop, since of course I would not want to appear like I wanted to take his job. I said everything was fine and I felt pretty good about my current positions. It was only a few weeks later that I realized that he was ascertaining my interest in his job since he was leaving. They gave the job to someone else and the word on the street was I was not interested. I totally missed the gate! While it wasn’t necessarily the job I missed out on, it was the opportunity to consider the job because I was afraid. So, don’t miss the gate. It’s the wormhole to a different life that may be the right one for you, but you need to “see it” to seize it.
- Work hard for the money and for the fun. There are many things Gwyneth Paltrow does that I do not agree with, but I will give her credit for one important lesson: she divides her movie roles into those she does for love (for example, The Royal Tenenbaums) and those she does for money (for example, Shallow Hal). It made me realize that even a Hollywood starlet has to do the stuff she may not want to do for the money. So, as a young person, you have to work hard for the money, but ideally it will help you take on a project you love, whatever it is. You’ve won the game when you’re mostly paid to work for the fun ... but that may take some time.
- Always optimize what is best for you personally AND professionally. While I was on maternity leave, the job of my dreams presented itself – or so I thought it did. It was at the intersection of policy, quality, and education, with a national stage, and I would not need to move. But, I knew I could not accept the travel commitment with a young child. While I wondered if I would have regrets, it turns out the right decision professionally also has to work personally. Likewise, there are professional obligations that I take on because it works personally.
- Figure out who your tea house pals are. A few years ago, I was in San Francisco with two close friends having an epic moment about what to do with our lives as adults. We were all on the cusp of changing our directions. Not surprisingly, we could see what the other needed to do, but we could not see it for ourselves. We still text each other sometimes about the need to go back to the Tea House. Sometimes your “tea house pals” are not necessarily those around you every day. They know you, but not everyone in your work place. This “arm’s length” or distance gives them the rational, unbiased perspective to advise you, that you or your colleagues will never have.
- Look for ways to enjoy the journey. Medicine is a very long road. I routinely think about this working with all the trainees and junior faculty I encounter. You can’t be in this solely for the end of the journey. The key is to find the joy in the journey. For me, that has always come from seeking out like-minded fellow travelers to share my highs and lows. While I tweet for many reasons, a big reason is that I take pleasure in watching others on the journey and also sharing my own journey.
Here’s to your journey and living your legacy!
Dr. Arora is associate chief medical officer, clinical learning environment, at University of Chicago Medicine, and assistant dean for scholarship and discovery at the University of Chicago Pritzker School of Medicine. You can follow her journey on Twitter.
The word legacy has been synonymous with death to me. When so and so dies, we discuss their legacy. I had a powerful experience that changed my mind on this word that is befitting for this Legacies column.
Seven years ago, I was sitting in a room of powerful women and I was the youngest one there. I wasn’t sure how I got there, but I was glad I did because it changed my life. At the time, I was panicked. The exercise was called “Craft your legacy statement.”
But, this exercise was different. The ask was to “live into your legacy.” Craft a legacy statement in THREE minutes that summarizes what you want your legacy to be … and then decide the three things you need to do now to get there. So, here is my exact legacy 3-minute statement: I am an innovator pushing teaching hospitals to optimize training and patient care delivery through novel technologies and systems science. Clearly, I did not aim high enough. One of the other attendees stated her legacy simply as “Unleash the impossible!” So clearly, I was not able to think big at that moment, but I trudged on.
Next, I had to write the three things I was going to do to enact my legacy today. Things went from bad to worse quickly since I knew this was not going to be easy. The #1 thing had to be something I was going to stop doing because it did not fit with my legacy; #2 was what I was going to start doing to enact this legacy now; and, #3 was something I was going to do to get me closer to what I wanted to be doing. So, my #1, resign my current leadership role that I had had for 8 years; #2, start joining national committees that bridge education and quality; and #3, meet with senior leadership to pitch this new role as a bridging leader, aligning education and quality.
Like all conferences, I went home and forgot what I had done and learned. I settled back into my old life and routines. A few weeks later, a plain looking envelope with awful penmanship showed up at my doorstep addressed to me. It wasn’t until after I opened it and read what was inside that I realized I was the one with horrible penmanship! I completely forgot that I wrote this letter to myself even though they told me it would come and I would forget I wrote it! So, how did I do? Let’s just say if the letter did not arrive, I am not sure where I would be. Fortunately, it did come, and I followed my own orders. Fast forward to present day and I recently stepped into a new role – associate chief medical officer: clinical learning environment – a bridging leader who aligns education and clinical care missions for our health system. Let’s just say again, had that letter not arrived, I am not sure where I would be now.
I have been fortunate to do many things in hospital medicine – clinician, researcher, educator, and my latest role as a leader. Through it all, I would say that there are some lessons that I have picked up along the way that helped me advance, in ways I did not realize:
- Be bold. Years ago, when I was asked by my chair who they should pick to be chief resident, I thought “This must be a trick question – I should definitely tell him why I should be chosen – and then pick the next best person who I want to work with.” Apparently, I was the only person who did that, and that is why my chair chose me. Everyone else picked two other people. So the take-home point here is do not sell yourself short … ever.
- Look for the hidden gateways. A few years ago, I was asked if I wanted to be an institutional leader by the person who currently had that role. I was kind of thrown for a loop, since of course I would not want to appear like I wanted to take his job. I said everything was fine and I felt pretty good about my current positions. It was only a few weeks later that I realized that he was ascertaining my interest in his job since he was leaving. They gave the job to someone else and the word on the street was I was not interested. I totally missed the gate! While it wasn’t necessarily the job I missed out on, it was the opportunity to consider the job because I was afraid. So, don’t miss the gate. It’s the wormhole to a different life that may be the right one for you, but you need to “see it” to seize it.
- Work hard for the money and for the fun. There are many things Gwyneth Paltrow does that I do not agree with, but I will give her credit for one important lesson: she divides her movie roles into those she does for love (for example, The Royal Tenenbaums) and those she does for money (for example, Shallow Hal). It made me realize that even a Hollywood starlet has to do the stuff she may not want to do for the money. So, as a young person, you have to work hard for the money, but ideally it will help you take on a project you love, whatever it is. You’ve won the game when you’re mostly paid to work for the fun ... but that may take some time.
- Always optimize what is best for you personally AND professionally. While I was on maternity leave, the job of my dreams presented itself – or so I thought it did. It was at the intersection of policy, quality, and education, with a national stage, and I would not need to move. But, I knew I could not accept the travel commitment with a young child. While I wondered if I would have regrets, it turns out the right decision professionally also has to work personally. Likewise, there are professional obligations that I take on because it works personally.
- Figure out who your tea house pals are. A few years ago, I was in San Francisco with two close friends having an epic moment about what to do with our lives as adults. We were all on the cusp of changing our directions. Not surprisingly, we could see what the other needed to do, but we could not see it for ourselves. We still text each other sometimes about the need to go back to the Tea House. Sometimes your “tea house pals” are not necessarily those around you every day. They know you, but not everyone in your work place. This “arm’s length” or distance gives them the rational, unbiased perspective to advise you, that you or your colleagues will never have.
- Look for ways to enjoy the journey. Medicine is a very long road. I routinely think about this working with all the trainees and junior faculty I encounter. You can’t be in this solely for the end of the journey. The key is to find the joy in the journey. For me, that has always come from seeking out like-minded fellow travelers to share my highs and lows. While I tweet for many reasons, a big reason is that I take pleasure in watching others on the journey and also sharing my own journey.
Here’s to your journey and living your legacy!
Dr. Arora is associate chief medical officer, clinical learning environment, at University of Chicago Medicine, and assistant dean for scholarship and discovery at the University of Chicago Pritzker School of Medicine. You can follow her journey on Twitter.
Hospitalist movers and shakers – May 2019
Christina L. Andrew, DO, a medical director on the hospitalist team at McLeod Regional Medical Center in Florence, S.C., and Zeshan Anwar, MD, medical director of Evangelical Community Hospital’s hospitalist group in Lewisburg, Pa., recently were named Senior Fellows in Hospital Medicine (SFHM) by the Society of Hospital Medicine. SFHMs are dedicated to promoting excellence, innovation and improving the quality of patient care.
Dr. Andrew has been with McLeod since 2008. The board-certified internist received her medical degree from Des Moines (Iowa) University Osteopathic Medical Center and did her residency at the Cleveland Clinic. To earn SFHM status, physicians must have worked as a hospitalist for at least 5 years and be a member of SHM for 5 years, as well.
Dr. Anwar has been in his current position since 2015. He coordinates staff resources and inpatient care for the facility where he has worked since 2013. He has his medical degree from King Edward Medical University, Lahore, Pakistan, and did his residency at Bronx-Lebanon Hospital Center in New York.
Tiffany Egbe, MD, has been named to the board of directors of Refuge International, an organization that builds relationships in Guatemala that allow for medical services to be provided to an underserved population.
Dr. Egbe is a hospitalist in internal medicine at Christus Good Shepherd in Longview and Marshall, Tex. She also serves as program director of internal medicine residency for the University of Texas Health Science Center in Tyler, Tex.
Dr. Egbe earned her medical degree from the University of Alabama at Birmingham.
Il Jun Chon, MD, has been named vice president of medical affairs with WellSpan Ephrata (Pa.) Community Hospital. Dr. Chon, a hospitalist, had previously been the medical director of WellSpan Ephrata’s hospitalist services and president of the facility’s medical staff.
Dr. Chon earned his medical degree from the Medical College of Pennsylvania (now Drexel College of Medicine) and completed his residency at Thomas Jefferson University Hospital, both in Philadelphia.
Megan Hamreus, DO, recently was named chief of staff at Scripps Mercy Hospital in San Diego, Calif. Dr. Hamreus will oversee 1,000 doctors at two facilities.
Dr. Hamreus has been with Scripps Mercy for 10 years, serving as a hospitalist and a faculty member of the family medicine residence training program of Family Health Centers of San Diego.
Chief of staff is a 2-year, elected term. Among her duties, Dr. Hamreus will be Scripps Mercy’s liaison to the facilities’ administrative staff and Scripps Health’s board of trustees.
Jade Brice Roshell, MD, recently was named chief medical officer at Shelby Baptist Medical Center in Alabaster, Ala. Dr. Brice Roshell was promoted from director of the center’s hospitalist program.
In addition to her new position, Dr. Brice Roshell was named as one of 68 honorees on Becker’s 2019 list of African-American Leaders in Health.
Dr. Brice Roshell has been with Shelby Baptist since 2015. Previously, she was an internist at centers in Louisiana, Georgia, and Nebraska. Her medical degree is from Howard University in Washington, and she completed her residency at Tulane University in New Orleans.
Anju Manral, MD, recently was appointed as medical director for the University of New Mexico Student Health and Counseling Center in Albuquerque. The internist has experience as a hospitalist focused on palliative care and most recently has worked at UNM’s Family Health Clinic, providing care to patients of all ages and conditions.
Dr. Manral also serves as an assistant professor in the UNM General Internal Medicine Department and mentors UNM medical students in the health science learning community.
The Hiawatha (Kan.) Community Hospital unveiled its new hospitalist program on Feb. 12.
The program will be led by Dustin Williams, DNP. Dr. Williams will provide hospitalist and emergency medical services to patients every Tuesday through Friday, while an on-call specialist will serve as hospitalist on Saturday, Sunday, and Monday.
Christina L. Andrew, DO, a medical director on the hospitalist team at McLeod Regional Medical Center in Florence, S.C., and Zeshan Anwar, MD, medical director of Evangelical Community Hospital’s hospitalist group in Lewisburg, Pa., recently were named Senior Fellows in Hospital Medicine (SFHM) by the Society of Hospital Medicine. SFHMs are dedicated to promoting excellence, innovation and improving the quality of patient care.
Dr. Andrew has been with McLeod since 2008. The board-certified internist received her medical degree from Des Moines (Iowa) University Osteopathic Medical Center and did her residency at the Cleveland Clinic. To earn SFHM status, physicians must have worked as a hospitalist for at least 5 years and be a member of SHM for 5 years, as well.
Dr. Anwar has been in his current position since 2015. He coordinates staff resources and inpatient care for the facility where he has worked since 2013. He has his medical degree from King Edward Medical University, Lahore, Pakistan, and did his residency at Bronx-Lebanon Hospital Center in New York.
Tiffany Egbe, MD, has been named to the board of directors of Refuge International, an organization that builds relationships in Guatemala that allow for medical services to be provided to an underserved population.
Dr. Egbe is a hospitalist in internal medicine at Christus Good Shepherd in Longview and Marshall, Tex. She also serves as program director of internal medicine residency for the University of Texas Health Science Center in Tyler, Tex.
Dr. Egbe earned her medical degree from the University of Alabama at Birmingham.
Il Jun Chon, MD, has been named vice president of medical affairs with WellSpan Ephrata (Pa.) Community Hospital. Dr. Chon, a hospitalist, had previously been the medical director of WellSpan Ephrata’s hospitalist services and president of the facility’s medical staff.
Dr. Chon earned his medical degree from the Medical College of Pennsylvania (now Drexel College of Medicine) and completed his residency at Thomas Jefferson University Hospital, both in Philadelphia.
Megan Hamreus, DO, recently was named chief of staff at Scripps Mercy Hospital in San Diego, Calif. Dr. Hamreus will oversee 1,000 doctors at two facilities.
Dr. Hamreus has been with Scripps Mercy for 10 years, serving as a hospitalist and a faculty member of the family medicine residence training program of Family Health Centers of San Diego.
Chief of staff is a 2-year, elected term. Among her duties, Dr. Hamreus will be Scripps Mercy’s liaison to the facilities’ administrative staff and Scripps Health’s board of trustees.
Jade Brice Roshell, MD, recently was named chief medical officer at Shelby Baptist Medical Center in Alabaster, Ala. Dr. Brice Roshell was promoted from director of the center’s hospitalist program.
In addition to her new position, Dr. Brice Roshell was named as one of 68 honorees on Becker’s 2019 list of African-American Leaders in Health.
Dr. Brice Roshell has been with Shelby Baptist since 2015. Previously, she was an internist at centers in Louisiana, Georgia, and Nebraska. Her medical degree is from Howard University in Washington, and she completed her residency at Tulane University in New Orleans.
Anju Manral, MD, recently was appointed as medical director for the University of New Mexico Student Health and Counseling Center in Albuquerque. The internist has experience as a hospitalist focused on palliative care and most recently has worked at UNM’s Family Health Clinic, providing care to patients of all ages and conditions.
Dr. Manral also serves as an assistant professor in the UNM General Internal Medicine Department and mentors UNM medical students in the health science learning community.
The Hiawatha (Kan.) Community Hospital unveiled its new hospitalist program on Feb. 12.
The program will be led by Dustin Williams, DNP. Dr. Williams will provide hospitalist and emergency medical services to patients every Tuesday through Friday, while an on-call specialist will serve as hospitalist on Saturday, Sunday, and Monday.
Christina L. Andrew, DO, a medical director on the hospitalist team at McLeod Regional Medical Center in Florence, S.C., and Zeshan Anwar, MD, medical director of Evangelical Community Hospital’s hospitalist group in Lewisburg, Pa., recently were named Senior Fellows in Hospital Medicine (SFHM) by the Society of Hospital Medicine. SFHMs are dedicated to promoting excellence, innovation and improving the quality of patient care.
Dr. Andrew has been with McLeod since 2008. The board-certified internist received her medical degree from Des Moines (Iowa) University Osteopathic Medical Center and did her residency at the Cleveland Clinic. To earn SFHM status, physicians must have worked as a hospitalist for at least 5 years and be a member of SHM for 5 years, as well.
Dr. Anwar has been in his current position since 2015. He coordinates staff resources and inpatient care for the facility where he has worked since 2013. He has his medical degree from King Edward Medical University, Lahore, Pakistan, and did his residency at Bronx-Lebanon Hospital Center in New York.
Tiffany Egbe, MD, has been named to the board of directors of Refuge International, an organization that builds relationships in Guatemala that allow for medical services to be provided to an underserved population.
Dr. Egbe is a hospitalist in internal medicine at Christus Good Shepherd in Longview and Marshall, Tex. She also serves as program director of internal medicine residency for the University of Texas Health Science Center in Tyler, Tex.
Dr. Egbe earned her medical degree from the University of Alabama at Birmingham.
Il Jun Chon, MD, has been named vice president of medical affairs with WellSpan Ephrata (Pa.) Community Hospital. Dr. Chon, a hospitalist, had previously been the medical director of WellSpan Ephrata’s hospitalist services and president of the facility’s medical staff.
Dr. Chon earned his medical degree from the Medical College of Pennsylvania (now Drexel College of Medicine) and completed his residency at Thomas Jefferson University Hospital, both in Philadelphia.
Megan Hamreus, DO, recently was named chief of staff at Scripps Mercy Hospital in San Diego, Calif. Dr. Hamreus will oversee 1,000 doctors at two facilities.
Dr. Hamreus has been with Scripps Mercy for 10 years, serving as a hospitalist and a faculty member of the family medicine residence training program of Family Health Centers of San Diego.
Chief of staff is a 2-year, elected term. Among her duties, Dr. Hamreus will be Scripps Mercy’s liaison to the facilities’ administrative staff and Scripps Health’s board of trustees.
Jade Brice Roshell, MD, recently was named chief medical officer at Shelby Baptist Medical Center in Alabaster, Ala. Dr. Brice Roshell was promoted from director of the center’s hospitalist program.
In addition to her new position, Dr. Brice Roshell was named as one of 68 honorees on Becker’s 2019 list of African-American Leaders in Health.
Dr. Brice Roshell has been with Shelby Baptist since 2015. Previously, she was an internist at centers in Louisiana, Georgia, and Nebraska. Her medical degree is from Howard University in Washington, and she completed her residency at Tulane University in New Orleans.
Anju Manral, MD, recently was appointed as medical director for the University of New Mexico Student Health and Counseling Center in Albuquerque. The internist has experience as a hospitalist focused on palliative care and most recently has worked at UNM’s Family Health Clinic, providing care to patients of all ages and conditions.
Dr. Manral also serves as an assistant professor in the UNM General Internal Medicine Department and mentors UNM medical students in the health science learning community.
The Hiawatha (Kan.) Community Hospital unveiled its new hospitalist program on Feb. 12.
The program will be led by Dustin Williams, DNP. Dr. Williams will provide hospitalist and emergency medical services to patients every Tuesday through Friday, while an on-call specialist will serve as hospitalist on Saturday, Sunday, and Monday.
Just a series of fortunate events?
Building a career in hospital medicine
Residents and junior faculty have frequently asked me how they can attain a position similar to mine, focused on quality and leadership in a health care system. When I was first asked to offer advice on this topic, my response was generally something like, “Heck if I know! I just had a series of lucky accidents to get here!”
Back then, I would recount my career history. I established myself as a clinician educator and associate program director soon after Chief Residency. After that, I would explain, a series of fortunate events and health care trends shaped my career. Evidence-based medicine (EBM), the patient safety movement, a shift to incorporate value (as well as volume) into reimbursement models, and the hospital medicine movement all emerged in interesting and often synergistic ways.
A young SHM organization (then known as NAIP) grew rapidly even while the hospitalist programs I led in Phoenix, then at University of California, San Diego, grew in size and influence. Inevitably, it seemed, I was increasingly involved in quality improvement (QI) efforts, and began to publish and speak about them. Collaborative work with SHM and a number of hospital systems broadened my visibility regionally and nationally. Finally, in 2015, I was recruited away from UC San Diego into a new position, as chief quality officer at UC Davis.
On hearing this history, those seeking my sage advice would look a little confused, and then say something like, “So your advice is that I should get lucky??? Gee, thanks a lot! Really helpful!” (Insert sarcasm here).
The honor of being asked to contribute to the “Legacies” series in The Hospitalist gave me an opportunity to think about this a little differently. No one really wanted to know about how past changes in the health care environment led to my career success. They wanted advice on tools and strategies that will allow them to thrive in an environment of ongoing, disruptive change that is likely only going to accelerate. I now present my upgraded points of advice, intertwined with examples of how SHM positively influenced my career (and could assist yours):
Learn how your hospital works. Hospitalists obviously have an inside track on many aspects of hospital operations, but sometimes remain oblivious to the organizational and committee structure, priorities of hospital leadership, and the mechanism for implementing standardized care. Knowing where to go with new ideas, and the process of implementing protocols, will keep you from hitting political land mines and unintentionally encroaching on someone else’s turf, while aligning your efforts with institutional priorities improves the buy-in and resources available to do the work.
Start small, but think big. Don’t bite off more than you can chew, and make sure your ideas for change work on a small scale before trying to sell the world on them. On the other hand, think big! The care you and others provide is dependent on systems that go far beyond your immediate control. Policies, protocols, standardized order sets, checklists, and an array of other tools can be leveraged to influence care across an entire health system, and in the SHM Mentored Implementation programs, can impact hundreds of hospitals.
Broaden your skills. Commit to learning new skills that can increase your impact and career diversity. Procedural skills; information technology; and EMR, EBM, research, public health, QI, business, leadership, public speaking, advocacy, and telehealth, can all open up a whole world of possibilities when combined with a medical degree. These skills can move you into areas that keep you engaged and excited to go to work.
Engage in mentor/mentee relationships. As an associate program director and clinician-educator, I had a lot of opportunity to mentor residents and fellows. It is so rewarding to watch the mentee grow in experience and skills, and to eventually see many of them assume leadership and mentoring roles themselves. You don’t have to be in a teaching position to act as a mentor (my experience mentoring hospitalists and others in leadership and quality improvement now far surpasses my experience with house staff).
The mentor often benefits as much as the mentee from this relationship. I have been inspired by their passion and dedication, educated by their ideas and innovation, and frequently find I am learning more from them, than they are from me. I have had great experiences in the SHM Mentored Implementation program in the role of mentee and mentor.
Participate in a community. When I first joined NAIP, I was amazed that the giants (Wachter, Nelson, Whitcomb, Holman, Williams, Greeno, Howell, Huddleston, Wellikson, and on and on) were not only approachable, they were warm, friendly, interesting, and extraordinarily welcoming. The ever-expanding and evolving community at SHM continues that tradition and offers a forum to share innovative work, discuss common problems and solutions, contact world experts, or just find an empathetic ear. Working on toolkits and collaborative efforts with this community remains a real highlight of my career, and the source of several lasting friendships. So don’t be shy; step right up; and introduce yourself!
Avoid my past mistakes (this might be a long list). Random things you should try to avoid.
- Tribalism – It is natural to be protective of your hospitalist group, and to focus on the injustices heaped upon you from (insert favorite punching bag here, e.g., ED, orthopedists, cardiologists, nursing staff, evil administration penny pinchers, etc). While some of those injustices might be real, tribalism, defensiveness, and circling the wagons generally only makes things worse. Sit down face to face, learn a little bit about the opposing tribe (both about their work, and about them as people), and see how much more fun and productive work can be.
- Storming out of a meeting with the CMO and CEO, slamming the door, etc. – not productive. Administrative leaders are doing their own juggling act and are generally well intentioned and doing the best they can. Respect that, argue your case, but if things don’t pan out, shake their hand, and live to fight another day.
- Using e-mail (evil-mail) to resolve conflict – And if you’re a young whippersnapper, don’t use Twitter, Facebook, Snapchat, or other social media to address conflict either!
- Forgetting to put patients first – Frame decisions for your group around what best serves your patients, not your doctors. Long term, this gives your group credibility and will serve the hospitalists better as well. SHM does this on a large scale with their advocacy efforts, resulting in more credibility and influence on Capitol Hill.
Make time for friends, family, fitness, fun, and reflection. A sense of humor and an occasional laugh when dealing with ill patients, hospital medicine politics, and the EMR all day provides resilience, as does taking the time to foster self-awareness and insight into your own weaknesses, strengths, and how you react to different stressors. A little bit of exercise and time with family and friends can go a long way towards improving your outlook, work, and life in general, while reducing burnout. Oh yeah, it’s also a good idea to choose a great life partner as well. Thanks Michelle!
Dr. Maynard is chief quality officer, University of California Davis Medical Center, Sacramento, Calif.
Building a career in hospital medicine
Building a career in hospital medicine
Residents and junior faculty have frequently asked me how they can attain a position similar to mine, focused on quality and leadership in a health care system. When I was first asked to offer advice on this topic, my response was generally something like, “Heck if I know! I just had a series of lucky accidents to get here!”
Back then, I would recount my career history. I established myself as a clinician educator and associate program director soon after Chief Residency. After that, I would explain, a series of fortunate events and health care trends shaped my career. Evidence-based medicine (EBM), the patient safety movement, a shift to incorporate value (as well as volume) into reimbursement models, and the hospital medicine movement all emerged in interesting and often synergistic ways.
A young SHM organization (then known as NAIP) grew rapidly even while the hospitalist programs I led in Phoenix, then at University of California, San Diego, grew in size and influence. Inevitably, it seemed, I was increasingly involved in quality improvement (QI) efforts, and began to publish and speak about them. Collaborative work with SHM and a number of hospital systems broadened my visibility regionally and nationally. Finally, in 2015, I was recruited away from UC San Diego into a new position, as chief quality officer at UC Davis.
On hearing this history, those seeking my sage advice would look a little confused, and then say something like, “So your advice is that I should get lucky??? Gee, thanks a lot! Really helpful!” (Insert sarcasm here).
The honor of being asked to contribute to the “Legacies” series in The Hospitalist gave me an opportunity to think about this a little differently. No one really wanted to know about how past changes in the health care environment led to my career success. They wanted advice on tools and strategies that will allow them to thrive in an environment of ongoing, disruptive change that is likely only going to accelerate. I now present my upgraded points of advice, intertwined with examples of how SHM positively influenced my career (and could assist yours):
Learn how your hospital works. Hospitalists obviously have an inside track on many aspects of hospital operations, but sometimes remain oblivious to the organizational and committee structure, priorities of hospital leadership, and the mechanism for implementing standardized care. Knowing where to go with new ideas, and the process of implementing protocols, will keep you from hitting political land mines and unintentionally encroaching on someone else’s turf, while aligning your efforts with institutional priorities improves the buy-in and resources available to do the work.
Start small, but think big. Don’t bite off more than you can chew, and make sure your ideas for change work on a small scale before trying to sell the world on them. On the other hand, think big! The care you and others provide is dependent on systems that go far beyond your immediate control. Policies, protocols, standardized order sets, checklists, and an array of other tools can be leveraged to influence care across an entire health system, and in the SHM Mentored Implementation programs, can impact hundreds of hospitals.
Broaden your skills. Commit to learning new skills that can increase your impact and career diversity. Procedural skills; information technology; and EMR, EBM, research, public health, QI, business, leadership, public speaking, advocacy, and telehealth, can all open up a whole world of possibilities when combined with a medical degree. These skills can move you into areas that keep you engaged and excited to go to work.
Engage in mentor/mentee relationships. As an associate program director and clinician-educator, I had a lot of opportunity to mentor residents and fellows. It is so rewarding to watch the mentee grow in experience and skills, and to eventually see many of them assume leadership and mentoring roles themselves. You don’t have to be in a teaching position to act as a mentor (my experience mentoring hospitalists and others in leadership and quality improvement now far surpasses my experience with house staff).
The mentor often benefits as much as the mentee from this relationship. I have been inspired by their passion and dedication, educated by their ideas and innovation, and frequently find I am learning more from them, than they are from me. I have had great experiences in the SHM Mentored Implementation program in the role of mentee and mentor.
Participate in a community. When I first joined NAIP, I was amazed that the giants (Wachter, Nelson, Whitcomb, Holman, Williams, Greeno, Howell, Huddleston, Wellikson, and on and on) were not only approachable, they were warm, friendly, interesting, and extraordinarily welcoming. The ever-expanding and evolving community at SHM continues that tradition and offers a forum to share innovative work, discuss common problems and solutions, contact world experts, or just find an empathetic ear. Working on toolkits and collaborative efforts with this community remains a real highlight of my career, and the source of several lasting friendships. So don’t be shy; step right up; and introduce yourself!
Avoid my past mistakes (this might be a long list). Random things you should try to avoid.
- Tribalism – It is natural to be protective of your hospitalist group, and to focus on the injustices heaped upon you from (insert favorite punching bag here, e.g., ED, orthopedists, cardiologists, nursing staff, evil administration penny pinchers, etc). While some of those injustices might be real, tribalism, defensiveness, and circling the wagons generally only makes things worse. Sit down face to face, learn a little bit about the opposing tribe (both about their work, and about them as people), and see how much more fun and productive work can be.
- Storming out of a meeting with the CMO and CEO, slamming the door, etc. – not productive. Administrative leaders are doing their own juggling act and are generally well intentioned and doing the best they can. Respect that, argue your case, but if things don’t pan out, shake their hand, and live to fight another day.
- Using e-mail (evil-mail) to resolve conflict – And if you’re a young whippersnapper, don’t use Twitter, Facebook, Snapchat, or other social media to address conflict either!
- Forgetting to put patients first – Frame decisions for your group around what best serves your patients, not your doctors. Long term, this gives your group credibility and will serve the hospitalists better as well. SHM does this on a large scale with their advocacy efforts, resulting in more credibility and influence on Capitol Hill.
Make time for friends, family, fitness, fun, and reflection. A sense of humor and an occasional laugh when dealing with ill patients, hospital medicine politics, and the EMR all day provides resilience, as does taking the time to foster self-awareness and insight into your own weaknesses, strengths, and how you react to different stressors. A little bit of exercise and time with family and friends can go a long way towards improving your outlook, work, and life in general, while reducing burnout. Oh yeah, it’s also a good idea to choose a great life partner as well. Thanks Michelle!
Dr. Maynard is chief quality officer, University of California Davis Medical Center, Sacramento, Calif.
Residents and junior faculty have frequently asked me how they can attain a position similar to mine, focused on quality and leadership in a health care system. When I was first asked to offer advice on this topic, my response was generally something like, “Heck if I know! I just had a series of lucky accidents to get here!”
Back then, I would recount my career history. I established myself as a clinician educator and associate program director soon after Chief Residency. After that, I would explain, a series of fortunate events and health care trends shaped my career. Evidence-based medicine (EBM), the patient safety movement, a shift to incorporate value (as well as volume) into reimbursement models, and the hospital medicine movement all emerged in interesting and often synergistic ways.
A young SHM organization (then known as NAIP) grew rapidly even while the hospitalist programs I led in Phoenix, then at University of California, San Diego, grew in size and influence. Inevitably, it seemed, I was increasingly involved in quality improvement (QI) efforts, and began to publish and speak about them. Collaborative work with SHM and a number of hospital systems broadened my visibility regionally and nationally. Finally, in 2015, I was recruited away from UC San Diego into a new position, as chief quality officer at UC Davis.
On hearing this history, those seeking my sage advice would look a little confused, and then say something like, “So your advice is that I should get lucky??? Gee, thanks a lot! Really helpful!” (Insert sarcasm here).
The honor of being asked to contribute to the “Legacies” series in The Hospitalist gave me an opportunity to think about this a little differently. No one really wanted to know about how past changes in the health care environment led to my career success. They wanted advice on tools and strategies that will allow them to thrive in an environment of ongoing, disruptive change that is likely only going to accelerate. I now present my upgraded points of advice, intertwined with examples of how SHM positively influenced my career (and could assist yours):
Learn how your hospital works. Hospitalists obviously have an inside track on many aspects of hospital operations, but sometimes remain oblivious to the organizational and committee structure, priorities of hospital leadership, and the mechanism for implementing standardized care. Knowing where to go with new ideas, and the process of implementing protocols, will keep you from hitting political land mines and unintentionally encroaching on someone else’s turf, while aligning your efforts with institutional priorities improves the buy-in and resources available to do the work.
Start small, but think big. Don’t bite off more than you can chew, and make sure your ideas for change work on a small scale before trying to sell the world on them. On the other hand, think big! The care you and others provide is dependent on systems that go far beyond your immediate control. Policies, protocols, standardized order sets, checklists, and an array of other tools can be leveraged to influence care across an entire health system, and in the SHM Mentored Implementation programs, can impact hundreds of hospitals.
Broaden your skills. Commit to learning new skills that can increase your impact and career diversity. Procedural skills; information technology; and EMR, EBM, research, public health, QI, business, leadership, public speaking, advocacy, and telehealth, can all open up a whole world of possibilities when combined with a medical degree. These skills can move you into areas that keep you engaged and excited to go to work.
Engage in mentor/mentee relationships. As an associate program director and clinician-educator, I had a lot of opportunity to mentor residents and fellows. It is so rewarding to watch the mentee grow in experience and skills, and to eventually see many of them assume leadership and mentoring roles themselves. You don’t have to be in a teaching position to act as a mentor (my experience mentoring hospitalists and others in leadership and quality improvement now far surpasses my experience with house staff).
The mentor often benefits as much as the mentee from this relationship. I have been inspired by their passion and dedication, educated by their ideas and innovation, and frequently find I am learning more from them, than they are from me. I have had great experiences in the SHM Mentored Implementation program in the role of mentee and mentor.
Participate in a community. When I first joined NAIP, I was amazed that the giants (Wachter, Nelson, Whitcomb, Holman, Williams, Greeno, Howell, Huddleston, Wellikson, and on and on) were not only approachable, they were warm, friendly, interesting, and extraordinarily welcoming. The ever-expanding and evolving community at SHM continues that tradition and offers a forum to share innovative work, discuss common problems and solutions, contact world experts, or just find an empathetic ear. Working on toolkits and collaborative efforts with this community remains a real highlight of my career, and the source of several lasting friendships. So don’t be shy; step right up; and introduce yourself!
Avoid my past mistakes (this might be a long list). Random things you should try to avoid.
- Tribalism – It is natural to be protective of your hospitalist group, and to focus on the injustices heaped upon you from (insert favorite punching bag here, e.g., ED, orthopedists, cardiologists, nursing staff, evil administration penny pinchers, etc). While some of those injustices might be real, tribalism, defensiveness, and circling the wagons generally only makes things worse. Sit down face to face, learn a little bit about the opposing tribe (both about their work, and about them as people), and see how much more fun and productive work can be.
- Storming out of a meeting with the CMO and CEO, slamming the door, etc. – not productive. Administrative leaders are doing their own juggling act and are generally well intentioned and doing the best they can. Respect that, argue your case, but if things don’t pan out, shake their hand, and live to fight another day.
- Using e-mail (evil-mail) to resolve conflict – And if you’re a young whippersnapper, don’t use Twitter, Facebook, Snapchat, or other social media to address conflict either!
- Forgetting to put patients first – Frame decisions for your group around what best serves your patients, not your doctors. Long term, this gives your group credibility and will serve the hospitalists better as well. SHM does this on a large scale with their advocacy efforts, resulting in more credibility and influence on Capitol Hill.
Make time for friends, family, fitness, fun, and reflection. A sense of humor and an occasional laugh when dealing with ill patients, hospital medicine politics, and the EMR all day provides resilience, as does taking the time to foster self-awareness and insight into your own weaknesses, strengths, and how you react to different stressors. A little bit of exercise and time with family and friends can go a long way towards improving your outlook, work, and life in general, while reducing burnout. Oh yeah, it’s also a good idea to choose a great life partner as well. Thanks Michelle!
Dr. Maynard is chief quality officer, University of California Davis Medical Center, Sacramento, Calif.
Utilizing mentorship to achieve equity in leadership
Academic medicine and the health care industry
Achieving equity in leadership in academic medicine and the health care industry doesn’t have to be a pipe dream. There are clear, actionable steps that will lead us there.
The benefits of diversity are numerous and well documented. Diversity brings competitive advantage to organizations and strength to teams. With academic health centers (AHCs) facing continual stressors while at the same time being significant financial contributors to – and anchors in – their communities, ensuring their high performance is critical to society as a whole. To grow, thrive, and be ethical examples to their communities, health centers need the strongest and most innovative leaders who are reflective of the communities that they serve. This means more diversity in leadership positions.
When we look at the facts of the gender makeup of academic medicine and the health care industry, we can clearly see inequity – only 22% of medical school full professors, 18% of medical school department chairs, and 17% of medical school deans are women. Note that it has taken 50 years to get from 0 women deans to the 25 women deans who are now in this role. Only 28% of full and associate professors and 21% of department chairs are nonwhite. In the health care industry, only 13% of CEOs are women. The pace toward equity has been excruciatingly slow, and it’s not only women and underrepresented minorities who lose, but also the AHCs and their communities.
So how do we reach equity? Mentorship is a key pathway to this goal. In a session at Hospital Medicine 2019 (HM19), “What Mentorship Has Meant To Me (And What It Can Do For You): High Impact Stories from Leaders in Hospital Medicine,” fellow panelists and I outlined how mentorship can positively affect your career, define the qualities of effective mentors and mentees, describe the difference between mentorship and sponsorship, and explained how to navigate common pitfalls in mentor-mentee relationships.
We spoke about the responsibility the mentee has in the relationship and the need to “manage up,” a term borrowed from the corporate world, where the mentee takes responsibility for his or her part in the relationship and takes a leadership role in the relationship. The mentee must be an “active participant” in the relationship for the relationship to be successful. We hope that attendees at the session took some key points back to their institutions to open dialogue on strategies to achieve equity through building mentoring relationships.
When I look back on my time in residency and fellowship, I recognize that I was surrounded by people who offered guidance and advice. But once I became a faculty member, that guidance was less apparent, and I struggled in the first few years. It wasn’t until I attended a conference on peer mentoring that I recognized that I didn’t just need a didactic mentor, but that I needed a portfolio of mentors and that I had to take the initiative to actively engage mentorship. So I did, and its effects on my career have been powerful and numerous.
The evidence is there that mentorship can play a major role in advancing careers. Now it is up to the leadership of academic and nonacademic health centers to take the initiative and establish formalized programs in their institutions. We all benefit when we have diversity in leadership – so let’s get there together.
Dr. Spector is executive director, Executive Leadership in Academic Medicine, associate dean of faculty development, Drexel University, Philadelphia.
Academic medicine and the health care industry
Academic medicine and the health care industry
Achieving equity in leadership in academic medicine and the health care industry doesn’t have to be a pipe dream. There are clear, actionable steps that will lead us there.
The benefits of diversity are numerous and well documented. Diversity brings competitive advantage to organizations and strength to teams. With academic health centers (AHCs) facing continual stressors while at the same time being significant financial contributors to – and anchors in – their communities, ensuring their high performance is critical to society as a whole. To grow, thrive, and be ethical examples to their communities, health centers need the strongest and most innovative leaders who are reflective of the communities that they serve. This means more diversity in leadership positions.
When we look at the facts of the gender makeup of academic medicine and the health care industry, we can clearly see inequity – only 22% of medical school full professors, 18% of medical school department chairs, and 17% of medical school deans are women. Note that it has taken 50 years to get from 0 women deans to the 25 women deans who are now in this role. Only 28% of full and associate professors and 21% of department chairs are nonwhite. In the health care industry, only 13% of CEOs are women. The pace toward equity has been excruciatingly slow, and it’s not only women and underrepresented minorities who lose, but also the AHCs and their communities.
So how do we reach equity? Mentorship is a key pathway to this goal. In a session at Hospital Medicine 2019 (HM19), “What Mentorship Has Meant To Me (And What It Can Do For You): High Impact Stories from Leaders in Hospital Medicine,” fellow panelists and I outlined how mentorship can positively affect your career, define the qualities of effective mentors and mentees, describe the difference between mentorship and sponsorship, and explained how to navigate common pitfalls in mentor-mentee relationships.
We spoke about the responsibility the mentee has in the relationship and the need to “manage up,” a term borrowed from the corporate world, where the mentee takes responsibility for his or her part in the relationship and takes a leadership role in the relationship. The mentee must be an “active participant” in the relationship for the relationship to be successful. We hope that attendees at the session took some key points back to their institutions to open dialogue on strategies to achieve equity through building mentoring relationships.
When I look back on my time in residency and fellowship, I recognize that I was surrounded by people who offered guidance and advice. But once I became a faculty member, that guidance was less apparent, and I struggled in the first few years. It wasn’t until I attended a conference on peer mentoring that I recognized that I didn’t just need a didactic mentor, but that I needed a portfolio of mentors and that I had to take the initiative to actively engage mentorship. So I did, and its effects on my career have been powerful and numerous.
The evidence is there that mentorship can play a major role in advancing careers. Now it is up to the leadership of academic and nonacademic health centers to take the initiative and establish formalized programs in their institutions. We all benefit when we have diversity in leadership – so let’s get there together.
Dr. Spector is executive director, Executive Leadership in Academic Medicine, associate dean of faculty development, Drexel University, Philadelphia.
Achieving equity in leadership in academic medicine and the health care industry doesn’t have to be a pipe dream. There are clear, actionable steps that will lead us there.
The benefits of diversity are numerous and well documented. Diversity brings competitive advantage to organizations and strength to teams. With academic health centers (AHCs) facing continual stressors while at the same time being significant financial contributors to – and anchors in – their communities, ensuring their high performance is critical to society as a whole. To grow, thrive, and be ethical examples to their communities, health centers need the strongest and most innovative leaders who are reflective of the communities that they serve. This means more diversity in leadership positions.
When we look at the facts of the gender makeup of academic medicine and the health care industry, we can clearly see inequity – only 22% of medical school full professors, 18% of medical school department chairs, and 17% of medical school deans are women. Note that it has taken 50 years to get from 0 women deans to the 25 women deans who are now in this role. Only 28% of full and associate professors and 21% of department chairs are nonwhite. In the health care industry, only 13% of CEOs are women. The pace toward equity has been excruciatingly slow, and it’s not only women and underrepresented minorities who lose, but also the AHCs and their communities.
So how do we reach equity? Mentorship is a key pathway to this goal. In a session at Hospital Medicine 2019 (HM19), “What Mentorship Has Meant To Me (And What It Can Do For You): High Impact Stories from Leaders in Hospital Medicine,” fellow panelists and I outlined how mentorship can positively affect your career, define the qualities of effective mentors and mentees, describe the difference between mentorship and sponsorship, and explained how to navigate common pitfalls in mentor-mentee relationships.
We spoke about the responsibility the mentee has in the relationship and the need to “manage up,” a term borrowed from the corporate world, where the mentee takes responsibility for his or her part in the relationship and takes a leadership role in the relationship. The mentee must be an “active participant” in the relationship for the relationship to be successful. We hope that attendees at the session took some key points back to their institutions to open dialogue on strategies to achieve equity through building mentoring relationships.
When I look back on my time in residency and fellowship, I recognize that I was surrounded by people who offered guidance and advice. But once I became a faculty member, that guidance was less apparent, and I struggled in the first few years. It wasn’t until I attended a conference on peer mentoring that I recognized that I didn’t just need a didactic mentor, but that I needed a portfolio of mentors and that I had to take the initiative to actively engage mentorship. So I did, and its effects on my career have been powerful and numerous.
The evidence is there that mentorship can play a major role in advancing careers. Now it is up to the leadership of academic and nonacademic health centers to take the initiative and establish formalized programs in their institutions. We all benefit when we have diversity in leadership – so let’s get there together.
Dr. Spector is executive director, Executive Leadership in Academic Medicine, associate dean of faculty development, Drexel University, Philadelphia.
Speaking at a conference? Read these tips first
Recently, I was asked to present my top public speaking tips for a group of women leaders. This is a topic near and dear to my heart, and one that I teach a number of groups, from medical students to faculty.
I also benefited from just returning from the Harvard Macy Educators Course, where Victoria Brazil, MD, an experienced emergency medicine physician from Australia, provided her top tips. Here is a mash-up of the top tips to think about for any of the speakers out there among us – with a few shout-outs for the ladies out there. Please add your own!
The Dos
- Do project power: Stand tall with a relaxed stance and shoulders back – posture is everything. This is especially important for women, who may tend to shrink their bodies, or anyone who is short. A powerful messenger is just as important as the power of the message. The same also applies to sitting down, especially if you are on a panel. Do not look like you are falling into the table.
- Do look up: Think about addressing the people in the back, not in the front row. This looks better in photos as well since you are appealing to the large audience and not the front row. Dr. Brazil’s tip came from Cate Blanchett who said that before she gives talks, she literally and physically advises “picking up your crown and put it on your head.” Not only will you feel better, you will look it too.
- Do pause strategically: The human brain needs rest to process what you are about to say. You can ask people to “think of a time” and take a pause. Or “I want you to all think about what I just said for one moment.” And TAKE a moment. But think about Emma’s pause during the March For Your Lives. Pauses are powerful and serve as a way to cement what you are saying for even the most critical crowd. Think about when anyone on their phone pauses, even if you’re on a boring conference call others will wake up and wonder what is going on and are now engaged in the talk.
- Do strategically summarize: Before you end, or in between important sections, say the following: “There are three main things you can do.” Even if someone fell asleep, they will wake up to take note. It’s a way to get folks’ attention back. There is nothing like challenging others to do something.
The Don’ts
- Don’t start with an apology for “not being an expert”: Or whatever you are thinking about apologizing for. The voice in your head does not need to be broadcast to others. Just say thank you after you are introduced, and launch in. Someone has asked you to talk, so bring your own unique expertise and don’t start with undermining yourself!
- Don’t use your slides as a crutch: Make your audience look at you and not your slides. That means at times, you may be talking and your slides will not be moving. Other times, if you are starting with a story, maybe there is no slide behind you and the screen is blacked out. Some of the most powerful moments in a talk are when slides are not being used.
- Don’t stand behind the podium if you can help it. This means ask for a wireless microphone. Most podiums will overwhelm you. If you have to use a podium, go back to the posture in the “dos.” One year, I had a leg injury and definitely used the podium, so obviously there may be times you need to use a podium; even then, try as hard as possible to make sure you are seen.
- Don’t engage grandstanders during Q&A: Invariably, you will get someone who stands up and goes into a long comment that is not a question to hear themselves speak. Insert yourself, say “thank you” and take the next question. If there is not a next question, you can add, “Before I forget, I want to share another question I am often asked which may be of help to you.” Then, answer your own question. You get the final word this way!
Happy speaking! I look forward to seeing you in warmer weather during the spring conference season.
For more posts from the Hospital Leader blog, visit hospitalleader.org.
Recently, I was asked to present my top public speaking tips for a group of women leaders. This is a topic near and dear to my heart, and one that I teach a number of groups, from medical students to faculty.
I also benefited from just returning from the Harvard Macy Educators Course, where Victoria Brazil, MD, an experienced emergency medicine physician from Australia, provided her top tips. Here is a mash-up of the top tips to think about for any of the speakers out there among us – with a few shout-outs for the ladies out there. Please add your own!
The Dos
- Do project power: Stand tall with a relaxed stance and shoulders back – posture is everything. This is especially important for women, who may tend to shrink their bodies, or anyone who is short. A powerful messenger is just as important as the power of the message. The same also applies to sitting down, especially if you are on a panel. Do not look like you are falling into the table.
- Do look up: Think about addressing the people in the back, not in the front row. This looks better in photos as well since you are appealing to the large audience and not the front row. Dr. Brazil’s tip came from Cate Blanchett who said that before she gives talks, she literally and physically advises “picking up your crown and put it on your head.” Not only will you feel better, you will look it too.
- Do pause strategically: The human brain needs rest to process what you are about to say. You can ask people to “think of a time” and take a pause. Or “I want you to all think about what I just said for one moment.” And TAKE a moment. But think about Emma’s pause during the March For Your Lives. Pauses are powerful and serve as a way to cement what you are saying for even the most critical crowd. Think about when anyone on their phone pauses, even if you’re on a boring conference call others will wake up and wonder what is going on and are now engaged in the talk.
- Do strategically summarize: Before you end, or in between important sections, say the following: “There are three main things you can do.” Even if someone fell asleep, they will wake up to take note. It’s a way to get folks’ attention back. There is nothing like challenging others to do something.
The Don’ts
- Don’t start with an apology for “not being an expert”: Or whatever you are thinking about apologizing for. The voice in your head does not need to be broadcast to others. Just say thank you after you are introduced, and launch in. Someone has asked you to talk, so bring your own unique expertise and don’t start with undermining yourself!
- Don’t use your slides as a crutch: Make your audience look at you and not your slides. That means at times, you may be talking and your slides will not be moving. Other times, if you are starting with a story, maybe there is no slide behind you and the screen is blacked out. Some of the most powerful moments in a talk are when slides are not being used.
- Don’t stand behind the podium if you can help it. This means ask for a wireless microphone. Most podiums will overwhelm you. If you have to use a podium, go back to the posture in the “dos.” One year, I had a leg injury and definitely used the podium, so obviously there may be times you need to use a podium; even then, try as hard as possible to make sure you are seen.
- Don’t engage grandstanders during Q&A: Invariably, you will get someone who stands up and goes into a long comment that is not a question to hear themselves speak. Insert yourself, say “thank you” and take the next question. If there is not a next question, you can add, “Before I forget, I want to share another question I am often asked which may be of help to you.” Then, answer your own question. You get the final word this way!
Happy speaking! I look forward to seeing you in warmer weather during the spring conference season.
For more posts from the Hospital Leader blog, visit hospitalleader.org.
Recently, I was asked to present my top public speaking tips for a group of women leaders. This is a topic near and dear to my heart, and one that I teach a number of groups, from medical students to faculty.
I also benefited from just returning from the Harvard Macy Educators Course, where Victoria Brazil, MD, an experienced emergency medicine physician from Australia, provided her top tips. Here is a mash-up of the top tips to think about for any of the speakers out there among us – with a few shout-outs for the ladies out there. Please add your own!
The Dos
- Do project power: Stand tall with a relaxed stance and shoulders back – posture is everything. This is especially important for women, who may tend to shrink their bodies, or anyone who is short. A powerful messenger is just as important as the power of the message. The same also applies to sitting down, especially if you are on a panel. Do not look like you are falling into the table.
- Do look up: Think about addressing the people in the back, not in the front row. This looks better in photos as well since you are appealing to the large audience and not the front row. Dr. Brazil’s tip came from Cate Blanchett who said that before she gives talks, she literally and physically advises “picking up your crown and put it on your head.” Not only will you feel better, you will look it too.
- Do pause strategically: The human brain needs rest to process what you are about to say. You can ask people to “think of a time” and take a pause. Or “I want you to all think about what I just said for one moment.” And TAKE a moment. But think about Emma’s pause during the March For Your Lives. Pauses are powerful and serve as a way to cement what you are saying for even the most critical crowd. Think about when anyone on their phone pauses, even if you’re on a boring conference call others will wake up and wonder what is going on and are now engaged in the talk.
- Do strategically summarize: Before you end, or in between important sections, say the following: “There are three main things you can do.” Even if someone fell asleep, they will wake up to take note. It’s a way to get folks’ attention back. There is nothing like challenging others to do something.
The Don’ts
- Don’t start with an apology for “not being an expert”: Or whatever you are thinking about apologizing for. The voice in your head does not need to be broadcast to others. Just say thank you after you are introduced, and launch in. Someone has asked you to talk, so bring your own unique expertise and don’t start with undermining yourself!
- Don’t use your slides as a crutch: Make your audience look at you and not your slides. That means at times, you may be talking and your slides will not be moving. Other times, if you are starting with a story, maybe there is no slide behind you and the screen is blacked out. Some of the most powerful moments in a talk are when slides are not being used.
- Don’t stand behind the podium if you can help it. This means ask for a wireless microphone. Most podiums will overwhelm you. If you have to use a podium, go back to the posture in the “dos.” One year, I had a leg injury and definitely used the podium, so obviously there may be times you need to use a podium; even then, try as hard as possible to make sure you are seen.
- Don’t engage grandstanders during Q&A: Invariably, you will get someone who stands up and goes into a long comment that is not a question to hear themselves speak. Insert yourself, say “thank you” and take the next question. If there is not a next question, you can add, “Before I forget, I want to share another question I am often asked which may be of help to you.” Then, answer your own question. You get the final word this way!
Happy speaking! I look forward to seeing you in warmer weather during the spring conference season.
For more posts from the Hospital Leader blog, visit hospitalleader.org.
In defense of hospital administrators
Improving relationships between leaders and clinicians
In the March 2019 issue of The Hospitalist, I wrote about some key findings from a 2018 survey of U.S. physicians by The Physicians Foundation. It’s no surprise to anyone working in health care today that the survey found alarming levels of professional dissatisfaction, burnout, and pessimism about the future of medicine among respondent physicians. Sadly, it appears that much of that pessimism is directed toward hospitals and their leaders: 46% of survey respondents viewed the relationships between physicians and hospitals as somewhat or mostly negative and adversarial.
Several physicians posted comments online, and they deeply saddened me. My heart hurt for those doctors who wrote, “I loved medicine. It was good for my soul, but medicine left me. Doctors gave up most of their power and large corporations without an ethical foundation and no god, but money took over.” Or “They are waiting so all the senior physicians will retire. Nurses will become leaders who will follow administration’s lead and control physicians. Money and cost cutting is the major driver. Physicians are not valuable anymore because they have different opinions which cost a lot. There is a lot of window dressing, but they actually don’t care. They just want to run a business.” I also read “I was tossed out like dirty laundry water at age 59.” And “On a personal basis, I will try to reason with management exactly once before I bail.” Sigh.
These commenters are well-meaning physicians who had bad experiences with hospital leaders they saw as uncaring and unresponsive to their concerns as clinicians. Their experiences left them demoralized and embittered. I’m truly sorry for that.
I’m a recovering hospital administrator myself. My business partner John Nelson, MD, MHM, likes to tell people that he has successfully deprogrammed me from the way most administrators think about doctors, but he’s mostly joking (at least I think he is). I can tell you that most of the hospital leaders I have met – both when I was still an administrator and now in my consulting work – are well-intentioned people who care deeply about patients and their fellow health care professionals and are trying hard to do the right thing. Many of them could have earned more and had better career opportunities doing similar work in a field other than health care, but they chose health care out of a sincere desire to do good and help people.
A big part of the problem is that doctors and administrators come to health care from very different starting points, and so have very different perspectives. They generally function in separate silos, each paying attention to their own comfortable little part of that monster we call a health care delivery system. Often, neither administrators nor doctors have made enough effort to cross over and understand the issues and perspectives of people in other silos. As a result, it’s easy for assumptions and biases to creep in and poison our interactions.
When we interpret the behavior of others, we humans tend to overemphasize dispositional factors, such as personality or motives, and to discount situational factors, such as external stressors. Psychologists call this the fundamental attribution error or correspondence bias, and the result is usually heightened conflict as a result of presumed negative intentions on the part of others (“All she cares about is making a profit”) and discounting circumstantial factors that might be influencing others’ behavior (“She is facing reduced market share and a funding shortfall, and she’s fearful for the future of the institution”).
Add in another phenomenon known as the actor-observer bias, in which we tend to attribute others’ behavior to their dispositions but attribute our own behavior to the circumstances (“That administrator lost his temper because he’s a demanding jerk, but I only lost my temper because he pushed me over the edge”).
Is it possible that hospital leaders and doctors are reading each other inaccurately and that they’re making assumptions about each other’s intentions that get in the way of having constructive dialogue? How can we get to a place of greater trust? I don’t know the whole answer, of course, but I have a few ideas to offer.
Read the full post at hospitalleader.org.
Improving relationships between leaders and clinicians
Improving relationships between leaders and clinicians
In the March 2019 issue of The Hospitalist, I wrote about some key findings from a 2018 survey of U.S. physicians by The Physicians Foundation. It’s no surprise to anyone working in health care today that the survey found alarming levels of professional dissatisfaction, burnout, and pessimism about the future of medicine among respondent physicians. Sadly, it appears that much of that pessimism is directed toward hospitals and their leaders: 46% of survey respondents viewed the relationships between physicians and hospitals as somewhat or mostly negative and adversarial.
Several physicians posted comments online, and they deeply saddened me. My heart hurt for those doctors who wrote, “I loved medicine. It was good for my soul, but medicine left me. Doctors gave up most of their power and large corporations without an ethical foundation and no god, but money took over.” Or “They are waiting so all the senior physicians will retire. Nurses will become leaders who will follow administration’s lead and control physicians. Money and cost cutting is the major driver. Physicians are not valuable anymore because they have different opinions which cost a lot. There is a lot of window dressing, but they actually don’t care. They just want to run a business.” I also read “I was tossed out like dirty laundry water at age 59.” And “On a personal basis, I will try to reason with management exactly once before I bail.” Sigh.
These commenters are well-meaning physicians who had bad experiences with hospital leaders they saw as uncaring and unresponsive to their concerns as clinicians. Their experiences left them demoralized and embittered. I’m truly sorry for that.
I’m a recovering hospital administrator myself. My business partner John Nelson, MD, MHM, likes to tell people that he has successfully deprogrammed me from the way most administrators think about doctors, but he’s mostly joking (at least I think he is). I can tell you that most of the hospital leaders I have met – both when I was still an administrator and now in my consulting work – are well-intentioned people who care deeply about patients and their fellow health care professionals and are trying hard to do the right thing. Many of them could have earned more and had better career opportunities doing similar work in a field other than health care, but they chose health care out of a sincere desire to do good and help people.
A big part of the problem is that doctors and administrators come to health care from very different starting points, and so have very different perspectives. They generally function in separate silos, each paying attention to their own comfortable little part of that monster we call a health care delivery system. Often, neither administrators nor doctors have made enough effort to cross over and understand the issues and perspectives of people in other silos. As a result, it’s easy for assumptions and biases to creep in and poison our interactions.
When we interpret the behavior of others, we humans tend to overemphasize dispositional factors, such as personality or motives, and to discount situational factors, such as external stressors. Psychologists call this the fundamental attribution error or correspondence bias, and the result is usually heightened conflict as a result of presumed negative intentions on the part of others (“All she cares about is making a profit”) and discounting circumstantial factors that might be influencing others’ behavior (“She is facing reduced market share and a funding shortfall, and she’s fearful for the future of the institution”).
Add in another phenomenon known as the actor-observer bias, in which we tend to attribute others’ behavior to their dispositions but attribute our own behavior to the circumstances (“That administrator lost his temper because he’s a demanding jerk, but I only lost my temper because he pushed me over the edge”).
Is it possible that hospital leaders and doctors are reading each other inaccurately and that they’re making assumptions about each other’s intentions that get in the way of having constructive dialogue? How can we get to a place of greater trust? I don’t know the whole answer, of course, but I have a few ideas to offer.
Read the full post at hospitalleader.org.
In the March 2019 issue of The Hospitalist, I wrote about some key findings from a 2018 survey of U.S. physicians by The Physicians Foundation. It’s no surprise to anyone working in health care today that the survey found alarming levels of professional dissatisfaction, burnout, and pessimism about the future of medicine among respondent physicians. Sadly, it appears that much of that pessimism is directed toward hospitals and their leaders: 46% of survey respondents viewed the relationships between physicians and hospitals as somewhat or mostly negative and adversarial.
Several physicians posted comments online, and they deeply saddened me. My heart hurt for those doctors who wrote, “I loved medicine. It was good for my soul, but medicine left me. Doctors gave up most of their power and large corporations without an ethical foundation and no god, but money took over.” Or “They are waiting so all the senior physicians will retire. Nurses will become leaders who will follow administration’s lead and control physicians. Money and cost cutting is the major driver. Physicians are not valuable anymore because they have different opinions which cost a lot. There is a lot of window dressing, but they actually don’t care. They just want to run a business.” I also read “I was tossed out like dirty laundry water at age 59.” And “On a personal basis, I will try to reason with management exactly once before I bail.” Sigh.
These commenters are well-meaning physicians who had bad experiences with hospital leaders they saw as uncaring and unresponsive to their concerns as clinicians. Their experiences left them demoralized and embittered. I’m truly sorry for that.
I’m a recovering hospital administrator myself. My business partner John Nelson, MD, MHM, likes to tell people that he has successfully deprogrammed me from the way most administrators think about doctors, but he’s mostly joking (at least I think he is). I can tell you that most of the hospital leaders I have met – both when I was still an administrator and now in my consulting work – are well-intentioned people who care deeply about patients and their fellow health care professionals and are trying hard to do the right thing. Many of them could have earned more and had better career opportunities doing similar work in a field other than health care, but they chose health care out of a sincere desire to do good and help people.
A big part of the problem is that doctors and administrators come to health care from very different starting points, and so have very different perspectives. They generally function in separate silos, each paying attention to their own comfortable little part of that monster we call a health care delivery system. Often, neither administrators nor doctors have made enough effort to cross over and understand the issues and perspectives of people in other silos. As a result, it’s easy for assumptions and biases to creep in and poison our interactions.
When we interpret the behavior of others, we humans tend to overemphasize dispositional factors, such as personality or motives, and to discount situational factors, such as external stressors. Psychologists call this the fundamental attribution error or correspondence bias, and the result is usually heightened conflict as a result of presumed negative intentions on the part of others (“All she cares about is making a profit”) and discounting circumstantial factors that might be influencing others’ behavior (“She is facing reduced market share and a funding shortfall, and she’s fearful for the future of the institution”).
Add in another phenomenon known as the actor-observer bias, in which we tend to attribute others’ behavior to their dispositions but attribute our own behavior to the circumstances (“That administrator lost his temper because he’s a demanding jerk, but I only lost my temper because he pushed me over the edge”).
Is it possible that hospital leaders and doctors are reading each other inaccurately and that they’re making assumptions about each other’s intentions that get in the way of having constructive dialogue? How can we get to a place of greater trust? I don’t know the whole answer, of course, but I have a few ideas to offer.
Read the full post at hospitalleader.org.
Embracing an executive leadership role
Dr. Bryce Gartland says hospitalists thrive as leaders
Bryce Gartland, MD, was working as a full-time hospitalist at Emory University Hospital in Atlanta when hospital administrators first started asking him to take on administrative roles, such as clinical site director or medical director of care coordination.
Today, Dr. Gartland is hospital group president and cochief of clinical operations for Emory Healthcare, with responsibility for overall performance and achievement across all 11 Emory hospitals. In that role, he keeps his eyes open for similar talent and leadership potential in younger physicians.
Following internal medicine residency at Cedars-Sinai Medical Center in Los Angeles, Dr. Gartland moved into a traditional private practice setting in Beverly Hills. “Two years later, my wife and I decided to move back to my home town of Atlanta. This was 2005 and hospital medicine was a nascent movement in health care. I was intrigued, and Emory had a strong hospitalist program based in a major academic medical setting, which has since grown from approximately 20 physicians to over 120 across seven hospitals,” he said.
Senior leaders at Emory recognized something in Dr. Gartland and more administrative offers were forthcoming.
“After a year of practicing at Emory, the system’s chief financial officer knocked on my door to ask if I would be interested in becoming medical director for care coordination. This role afforded me tremendous opportunities to get involved in clinical/administrative activities at Emory – utilization review, hospice and palliative care, transitions of care, interface with managed care organizations. The role was very rewarding. In some ways, I became a kind of chief translator at the hospital for anything clinical that also had financial implications,” he recalled.
“Then we went through a reorganization and I was offered the opportunity to step into the chief operating officer position at Emory University Hospital. Shortly thereafter, there was leadership turnover within the division of hospital medicine and I was asked by the CEO of Emory Healthcare and chair of the department of medicine to serve as section head for hospital medicine.” Dr. Gartland wore both of those hats for about 2 years, later becoming the CEO of Emory University Hospital and two other facilities within the system. He was appointed to his current position as hospital group president and cochief of clinical operations for Emory Healthcare in 2018.
Consumed with administrative responsibilities, he largely had to step away from patient care, although with mixed emotions.
“Over the years, I worked hard to maintain a strong clinical role, but the reality is that if you are not delivering patient care routinely, it’s difficult to practice at the highest level of current medical practice,” he said. Nonetheless, Dr. Gartland tries to keep a hand in patient care by routinely rounding with hospitalist teams and attending care conferences.
Fixing the larger health care system
“I am a huge supporter of more physicians becoming actively engaged in administrative positions in health care. They are key to helping us best fix the larger health care system,” Dr. Gartland said. “However, we’ve all seen clinicians drafted into administrative positions who were not great administrators. One needs to be bilingual in both medicine and business. While some skills, such as strong communication, may cross over, it’s important to recognize that clinical strength and success do not necessarily equate to administrative achievement.”
Dr. Gartland also believes in the importance of mentorship in developing future leaders and in seeking and engaging mentors from other disciplines outside of one’s own specialty. “I’ve been fortunate to have a number of mentors who saw something in me and supported investment in my personal and professional development. I am now fortunate to be in the position to give back by mentoring a number of younger hospitalists who are interested in growing their nonclinical roles.”
“One bit of advice from a mentor that really resonated with me was: Don’t let the urgent get in the way of the important,” Dr. Gartland said. “Life is busy and full of urgent day-to-day fires. It’s important to take the time to pause and consider where you are going and what you are doing to enhance your career development. Are you getting the right kinds of feedback?” He explained that a coach or mentor who can provide constructive feedback is important and is something he has relied upon throughout his own professional development.
Different paths to learning business
Dr. Gartland did not pursue formal business training before the administrative opportunities started to multiply for him at Emory, although in college he had a strong interest in both business and medicine and at one time contemplated going into either.
“Over the years, my mentors have given me a lot of advice, one of which was that a medical degree can be a passport to a lot of different career paths, with real opportunities for merging business and medicine,” he said.
He has since intentionally pursued business training opportunities wherever they came up, such as courses offered by the American College of Physician Executives (now the American Association for Physician Leadership). “At one point, I considered going back to college in an MBA program, but that’s when John Fox – then Emory Healthcare’s CEO – called and said he wanted to send me to the Harvard Business School’s Managing Health Care Delivery executive education program, with an Emory team comprising the chief nurse executive, chief of human resources, and CEO for one of our hospitals.” Harvard’s roughly 9-month program involves 3 weeks on campus with assignments between the on-campus visits.
“In my current role as hospital group president, I have direct responsibility for our hospitals’ and system’s clinically essential services such as radiology, laboratory, pharmacy, and perioperative medicine. I also still serve as CEO for Emory University Hospital while we recruit my replacement,” Dr. Gartland said. “Overall, my work time breaks down roughly into thirds. One-third is spent on strategy and strategic initiatives – such as organizational and program design. Our system recently acquired a large community health system whose strategic and operational integration I am actively leading.”
Another third of his time is focused on operations, and the final third is focused on talent management and development. “People are truly the most valuable asset any organization has, particularly in health care,” he noted. “Being intentional about organizational design, coaching, and supporting the development and deployment of talent at all levels of the organization helps everyone achieve their full potential. It is one of the most important roles a leader can play.”
Dr. Gartland said that Emory is committed to Lean-based management systems, using both horizontal and vertical strategies for process improvement and waste reduction, with implementation beginning in urology, transplant, and heart and vascular services. Experts say Lean success starts at the very top, and Emory and Dr. Gartland are all in.
“These types of changes are measured in 5- to 7-year increments or more, not in months. We believe this is key to creating the best workplace to support the highest quality, experience, and value in health care delivery. It creates and supports the right culture within an organization, and we have made the commitment to following that path,” he said.
Recognizing leadership potential
What does Dr. Gartland look for in physicians with leadership potential?
“Are you someone who collaborates well?” he asked. “Someone who raises your hand at meetings or gets engaged with the issues? Do you volunteer to take on assignments? Are you someone with a balanced perspective, system minded in thinking and inquisitive, with a positive approach to problem solving?”
A lot of physicians might come to a meeting with the hospital or their boss and complain about all the things that aren’t working, he said, but “it’s rarer for them to come in and say: ‘I see these problems, and here’s where I think we can make improvements. How can I help?’ ” Dr. Gartland looks for evidence of emotional intelligence and the ability to effect change management across disciplines. Another skill with ever-greater importance is comfort with data and data-driven decision making.
“When our national health care system is experiencing so much change and upheaval, much of which is captured in newspaper headlines, it can sound scary,” he said. “I encourage people to see that complex, dynamic times like these, filled with so much change, are also a tremendous opportunity. Run towards and embrace the opportunity for change. Hospitalists, by nature, bring with them a tremendous background and experience set that is invaluable to help lead positive change in these dynamic times.”
The SHM has offerings for hospitalists wanting to advance in leadership positions, Dr. Gartland said, including its annual Leadership Academy. The next one is scheduled to be held in Nashville, Tenn., Nov. 4-7, 2019.
“The Leadership Academy is a great initial step for physicians, especially those early in their careers. Also, try to gain exposure to a variety of perspectives outside of hospital medicine,” he said. “I’d love to see further advances in leadership for our specialty – growing the number of hospitalists who serve as hospital CEOs or CMOs and in other leadership roles. We have more to learn collectively about leadership as a specialty, and I’d love to see us grow that capacity by offering further learning opportunities and bringing together hospitalists who have an interest in advancing leadership.”
Dr. Bryce Gartland says hospitalists thrive as leaders
Dr. Bryce Gartland says hospitalists thrive as leaders
Bryce Gartland, MD, was working as a full-time hospitalist at Emory University Hospital in Atlanta when hospital administrators first started asking him to take on administrative roles, such as clinical site director or medical director of care coordination.
Today, Dr. Gartland is hospital group president and cochief of clinical operations for Emory Healthcare, with responsibility for overall performance and achievement across all 11 Emory hospitals. In that role, he keeps his eyes open for similar talent and leadership potential in younger physicians.
Following internal medicine residency at Cedars-Sinai Medical Center in Los Angeles, Dr. Gartland moved into a traditional private practice setting in Beverly Hills. “Two years later, my wife and I decided to move back to my home town of Atlanta. This was 2005 and hospital medicine was a nascent movement in health care. I was intrigued, and Emory had a strong hospitalist program based in a major academic medical setting, which has since grown from approximately 20 physicians to over 120 across seven hospitals,” he said.
Senior leaders at Emory recognized something in Dr. Gartland and more administrative offers were forthcoming.
“After a year of practicing at Emory, the system’s chief financial officer knocked on my door to ask if I would be interested in becoming medical director for care coordination. This role afforded me tremendous opportunities to get involved in clinical/administrative activities at Emory – utilization review, hospice and palliative care, transitions of care, interface with managed care organizations. The role was very rewarding. In some ways, I became a kind of chief translator at the hospital for anything clinical that also had financial implications,” he recalled.
“Then we went through a reorganization and I was offered the opportunity to step into the chief operating officer position at Emory University Hospital. Shortly thereafter, there was leadership turnover within the division of hospital medicine and I was asked by the CEO of Emory Healthcare and chair of the department of medicine to serve as section head for hospital medicine.” Dr. Gartland wore both of those hats for about 2 years, later becoming the CEO of Emory University Hospital and two other facilities within the system. He was appointed to his current position as hospital group president and cochief of clinical operations for Emory Healthcare in 2018.
Consumed with administrative responsibilities, he largely had to step away from patient care, although with mixed emotions.
“Over the years, I worked hard to maintain a strong clinical role, but the reality is that if you are not delivering patient care routinely, it’s difficult to practice at the highest level of current medical practice,” he said. Nonetheless, Dr. Gartland tries to keep a hand in patient care by routinely rounding with hospitalist teams and attending care conferences.
Fixing the larger health care system
“I am a huge supporter of more physicians becoming actively engaged in administrative positions in health care. They are key to helping us best fix the larger health care system,” Dr. Gartland said. “However, we’ve all seen clinicians drafted into administrative positions who were not great administrators. One needs to be bilingual in both medicine and business. While some skills, such as strong communication, may cross over, it’s important to recognize that clinical strength and success do not necessarily equate to administrative achievement.”
Dr. Gartland also believes in the importance of mentorship in developing future leaders and in seeking and engaging mentors from other disciplines outside of one’s own specialty. “I’ve been fortunate to have a number of mentors who saw something in me and supported investment in my personal and professional development. I am now fortunate to be in the position to give back by mentoring a number of younger hospitalists who are interested in growing their nonclinical roles.”
“One bit of advice from a mentor that really resonated with me was: Don’t let the urgent get in the way of the important,” Dr. Gartland said. “Life is busy and full of urgent day-to-day fires. It’s important to take the time to pause and consider where you are going and what you are doing to enhance your career development. Are you getting the right kinds of feedback?” He explained that a coach or mentor who can provide constructive feedback is important and is something he has relied upon throughout his own professional development.
Different paths to learning business
Dr. Gartland did not pursue formal business training before the administrative opportunities started to multiply for him at Emory, although in college he had a strong interest in both business and medicine and at one time contemplated going into either.
“Over the years, my mentors have given me a lot of advice, one of which was that a medical degree can be a passport to a lot of different career paths, with real opportunities for merging business and medicine,” he said.
He has since intentionally pursued business training opportunities wherever they came up, such as courses offered by the American College of Physician Executives (now the American Association for Physician Leadership). “At one point, I considered going back to college in an MBA program, but that’s when John Fox – then Emory Healthcare’s CEO – called and said he wanted to send me to the Harvard Business School’s Managing Health Care Delivery executive education program, with an Emory team comprising the chief nurse executive, chief of human resources, and CEO for one of our hospitals.” Harvard’s roughly 9-month program involves 3 weeks on campus with assignments between the on-campus visits.
“In my current role as hospital group president, I have direct responsibility for our hospitals’ and system’s clinically essential services such as radiology, laboratory, pharmacy, and perioperative medicine. I also still serve as CEO for Emory University Hospital while we recruit my replacement,” Dr. Gartland said. “Overall, my work time breaks down roughly into thirds. One-third is spent on strategy and strategic initiatives – such as organizational and program design. Our system recently acquired a large community health system whose strategic and operational integration I am actively leading.”
Another third of his time is focused on operations, and the final third is focused on talent management and development. “People are truly the most valuable asset any organization has, particularly in health care,” he noted. “Being intentional about organizational design, coaching, and supporting the development and deployment of talent at all levels of the organization helps everyone achieve their full potential. It is one of the most important roles a leader can play.”
Dr. Gartland said that Emory is committed to Lean-based management systems, using both horizontal and vertical strategies for process improvement and waste reduction, with implementation beginning in urology, transplant, and heart and vascular services. Experts say Lean success starts at the very top, and Emory and Dr. Gartland are all in.
“These types of changes are measured in 5- to 7-year increments or more, not in months. We believe this is key to creating the best workplace to support the highest quality, experience, and value in health care delivery. It creates and supports the right culture within an organization, and we have made the commitment to following that path,” he said.
Recognizing leadership potential
What does Dr. Gartland look for in physicians with leadership potential?
“Are you someone who collaborates well?” he asked. “Someone who raises your hand at meetings or gets engaged with the issues? Do you volunteer to take on assignments? Are you someone with a balanced perspective, system minded in thinking and inquisitive, with a positive approach to problem solving?”
A lot of physicians might come to a meeting with the hospital or their boss and complain about all the things that aren’t working, he said, but “it’s rarer for them to come in and say: ‘I see these problems, and here’s where I think we can make improvements. How can I help?’ ” Dr. Gartland looks for evidence of emotional intelligence and the ability to effect change management across disciplines. Another skill with ever-greater importance is comfort with data and data-driven decision making.
“When our national health care system is experiencing so much change and upheaval, much of which is captured in newspaper headlines, it can sound scary,” he said. “I encourage people to see that complex, dynamic times like these, filled with so much change, are also a tremendous opportunity. Run towards and embrace the opportunity for change. Hospitalists, by nature, bring with them a tremendous background and experience set that is invaluable to help lead positive change in these dynamic times.”
The SHM has offerings for hospitalists wanting to advance in leadership positions, Dr. Gartland said, including its annual Leadership Academy. The next one is scheduled to be held in Nashville, Tenn., Nov. 4-7, 2019.
“The Leadership Academy is a great initial step for physicians, especially those early in their careers. Also, try to gain exposure to a variety of perspectives outside of hospital medicine,” he said. “I’d love to see further advances in leadership for our specialty – growing the number of hospitalists who serve as hospital CEOs or CMOs and in other leadership roles. We have more to learn collectively about leadership as a specialty, and I’d love to see us grow that capacity by offering further learning opportunities and bringing together hospitalists who have an interest in advancing leadership.”
Bryce Gartland, MD, was working as a full-time hospitalist at Emory University Hospital in Atlanta when hospital administrators first started asking him to take on administrative roles, such as clinical site director or medical director of care coordination.
Today, Dr. Gartland is hospital group president and cochief of clinical operations for Emory Healthcare, with responsibility for overall performance and achievement across all 11 Emory hospitals. In that role, he keeps his eyes open for similar talent and leadership potential in younger physicians.
Following internal medicine residency at Cedars-Sinai Medical Center in Los Angeles, Dr. Gartland moved into a traditional private practice setting in Beverly Hills. “Two years later, my wife and I decided to move back to my home town of Atlanta. This was 2005 and hospital medicine was a nascent movement in health care. I was intrigued, and Emory had a strong hospitalist program based in a major academic medical setting, which has since grown from approximately 20 physicians to over 120 across seven hospitals,” he said.
Senior leaders at Emory recognized something in Dr. Gartland and more administrative offers were forthcoming.
“After a year of practicing at Emory, the system’s chief financial officer knocked on my door to ask if I would be interested in becoming medical director for care coordination. This role afforded me tremendous opportunities to get involved in clinical/administrative activities at Emory – utilization review, hospice and palliative care, transitions of care, interface with managed care organizations. The role was very rewarding. In some ways, I became a kind of chief translator at the hospital for anything clinical that also had financial implications,” he recalled.
“Then we went through a reorganization and I was offered the opportunity to step into the chief operating officer position at Emory University Hospital. Shortly thereafter, there was leadership turnover within the division of hospital medicine and I was asked by the CEO of Emory Healthcare and chair of the department of medicine to serve as section head for hospital medicine.” Dr. Gartland wore both of those hats for about 2 years, later becoming the CEO of Emory University Hospital and two other facilities within the system. He was appointed to his current position as hospital group president and cochief of clinical operations for Emory Healthcare in 2018.
Consumed with administrative responsibilities, he largely had to step away from patient care, although with mixed emotions.
“Over the years, I worked hard to maintain a strong clinical role, but the reality is that if you are not delivering patient care routinely, it’s difficult to practice at the highest level of current medical practice,” he said. Nonetheless, Dr. Gartland tries to keep a hand in patient care by routinely rounding with hospitalist teams and attending care conferences.
Fixing the larger health care system
“I am a huge supporter of more physicians becoming actively engaged in administrative positions in health care. They are key to helping us best fix the larger health care system,” Dr. Gartland said. “However, we’ve all seen clinicians drafted into administrative positions who were not great administrators. One needs to be bilingual in both medicine and business. While some skills, such as strong communication, may cross over, it’s important to recognize that clinical strength and success do not necessarily equate to administrative achievement.”
Dr. Gartland also believes in the importance of mentorship in developing future leaders and in seeking and engaging mentors from other disciplines outside of one’s own specialty. “I’ve been fortunate to have a number of mentors who saw something in me and supported investment in my personal and professional development. I am now fortunate to be in the position to give back by mentoring a number of younger hospitalists who are interested in growing their nonclinical roles.”
“One bit of advice from a mentor that really resonated with me was: Don’t let the urgent get in the way of the important,” Dr. Gartland said. “Life is busy and full of urgent day-to-day fires. It’s important to take the time to pause and consider where you are going and what you are doing to enhance your career development. Are you getting the right kinds of feedback?” He explained that a coach or mentor who can provide constructive feedback is important and is something he has relied upon throughout his own professional development.
Different paths to learning business
Dr. Gartland did not pursue formal business training before the administrative opportunities started to multiply for him at Emory, although in college he had a strong interest in both business and medicine and at one time contemplated going into either.
“Over the years, my mentors have given me a lot of advice, one of which was that a medical degree can be a passport to a lot of different career paths, with real opportunities for merging business and medicine,” he said.
He has since intentionally pursued business training opportunities wherever they came up, such as courses offered by the American College of Physician Executives (now the American Association for Physician Leadership). “At one point, I considered going back to college in an MBA program, but that’s when John Fox – then Emory Healthcare’s CEO – called and said he wanted to send me to the Harvard Business School’s Managing Health Care Delivery executive education program, with an Emory team comprising the chief nurse executive, chief of human resources, and CEO for one of our hospitals.” Harvard’s roughly 9-month program involves 3 weeks on campus with assignments between the on-campus visits.
“In my current role as hospital group president, I have direct responsibility for our hospitals’ and system’s clinically essential services such as radiology, laboratory, pharmacy, and perioperative medicine. I also still serve as CEO for Emory University Hospital while we recruit my replacement,” Dr. Gartland said. “Overall, my work time breaks down roughly into thirds. One-third is spent on strategy and strategic initiatives – such as organizational and program design. Our system recently acquired a large community health system whose strategic and operational integration I am actively leading.”
Another third of his time is focused on operations, and the final third is focused on talent management and development. “People are truly the most valuable asset any organization has, particularly in health care,” he noted. “Being intentional about organizational design, coaching, and supporting the development and deployment of talent at all levels of the organization helps everyone achieve their full potential. It is one of the most important roles a leader can play.”
Dr. Gartland said that Emory is committed to Lean-based management systems, using both horizontal and vertical strategies for process improvement and waste reduction, with implementation beginning in urology, transplant, and heart and vascular services. Experts say Lean success starts at the very top, and Emory and Dr. Gartland are all in.
“These types of changes are measured in 5- to 7-year increments or more, not in months. We believe this is key to creating the best workplace to support the highest quality, experience, and value in health care delivery. It creates and supports the right culture within an organization, and we have made the commitment to following that path,” he said.
Recognizing leadership potential
What does Dr. Gartland look for in physicians with leadership potential?
“Are you someone who collaborates well?” he asked. “Someone who raises your hand at meetings or gets engaged with the issues? Do you volunteer to take on assignments? Are you someone with a balanced perspective, system minded in thinking and inquisitive, with a positive approach to problem solving?”
A lot of physicians might come to a meeting with the hospital or their boss and complain about all the things that aren’t working, he said, but “it’s rarer for them to come in and say: ‘I see these problems, and here’s where I think we can make improvements. How can I help?’ ” Dr. Gartland looks for evidence of emotional intelligence and the ability to effect change management across disciplines. Another skill with ever-greater importance is comfort with data and data-driven decision making.
“When our national health care system is experiencing so much change and upheaval, much of which is captured in newspaper headlines, it can sound scary,” he said. “I encourage people to see that complex, dynamic times like these, filled with so much change, are also a tremendous opportunity. Run towards and embrace the opportunity for change. Hospitalists, by nature, bring with them a tremendous background and experience set that is invaluable to help lead positive change in these dynamic times.”
The SHM has offerings for hospitalists wanting to advance in leadership positions, Dr. Gartland said, including its annual Leadership Academy. The next one is scheduled to be held in Nashville, Tenn., Nov. 4-7, 2019.
“The Leadership Academy is a great initial step for physicians, especially those early in their careers. Also, try to gain exposure to a variety of perspectives outside of hospital medicine,” he said. “I’d love to see further advances in leadership for our specialty – growing the number of hospitalists who serve as hospital CEOs or CMOs and in other leadership roles. We have more to learn collectively about leadership as a specialty, and I’d love to see us grow that capacity by offering further learning opportunities and bringing together hospitalists who have an interest in advancing leadership.”
In search of high-value care
Six steps that can help your team
U.S. spending on health care is growing rapidly and expected to reach 19.7% of gross domestic product by 2026.1 In response, the Centers for Medicare and Medicaid Services and national organizations such as the American Board of Internal Medicine (ABIM) and the American College of Physicians (ACP) have launched initiatives to ensure that the value being delivered to patients is on par with the escalating cost of care.
Over the past 10 years, I have led and advised hundreds of small- and large-scale projects that focused on improving patient care quality and cost. Below, I share what I, along with other leaders in high-value care, have observed that it takes to implement successful and lasting improvements – for the benefit of patients and hospitals.
A brief history of high-value care
When compared to other wealthy countries, the United States spends disproportionately more money on health care. In 2016, U.S. health care spending was $3.3 trillion1, or $10,348 per person.2 Hospital care alone was responsible for a third of health spending and amounted to $1.1 trillion in 20161. By 2026, national health spending is projected to reach $5.7 trillion1.
In response to escalating health care costs, CMS and other payers have shifted toward value-based reimbursements that tie payments to health care facilities and clinicians to their performance on selected quality, cost, and efficiency measures. For example, under the CMS Merit-based Incentive Payment System (MIPS), 5% of clinicians’ revenue in 2020 is tied to their 2018 performance in four categories: Quality, Cost, Improvement Activities, and Promoting Interoperability. The percentage of revenue at risk will increase to 9% in 2022, based on 2020 performance.
Rising health care costs put a burden not just on the federal and state budgets, but on individual and family budgets as well. Out-of-pocket spending grew 3.9% in 2016 to $352.5 billion1 and is expected to increase in the future. High health care costs rightfully bring into question the value individual consumers of health care services are getting in return. If value is defined as the level of benefit achieved for a given cost, what is high-value care? The 2013 Institute of Medicine report3 defined high-value care as “the best care for the patient, with the optimal result for the circumstances, delivered at the right price.” It goes beyond a set of quality and cost measures used by payers to affect provider reimbursement and is driven by day-to-day individual providers’ decisions that affect individual patients’ outcomes and their cost of care.
High-value care has been embraced by national organizations. In 2012, the ABIM Foundation launched the Choosing Wisely initiative to support and promote conversations between clinicians and patients in choosing care that is truly necessary, supported by evidence, and free from harm. The result was an evidence-based list of recommendations from 540 specialty societies, including the Society of Hospital Medicine. The SHM – Adult Hospital Medicine list4 features the following “Five things physicians and patients should question”:
- Don’t place, or leave in place, urinary catheters for incontinence or convenience or monitoring of output for non–critically ill patients.
- Don’t prescribe medications for stress ulcer prophylaxis to medical inpatients unless at high risk for GI complications.
- Avoid transfusions of red blood cells for arbitrary hemoglobin or hematocrit thresholds and in the absence of symptoms of active coronary disease, heart failure, or stroke.
- Don’t order continuous telemetry monitoring outside of the ICU without using a protocol that governs continuation.
- Don’t perform repetitive CBC and chemistry testing in the face of clinical and lab stability.
The ACP launched a high-value care initiative that offers learning resources for clinicians and medical educators, clinical guidelines, and best practice advice. In 2012, a workgroup of internists convened by ACP developed a list of 37 clinical situations in which medical tests are commonly used but do not provide high value.5 Seven of those situations are applicable to adult hospital medicine.
High-value care today: What the experts say
More than 5 years later, what progress have hospitalists made in adopting high-value care practices? To answer this and other questions, I reached out to three national experts in high-value care in hospital medicine: Amit Pahwa, MD, assistant professor of medicine and pediatrics at Johns Hopkins University, Baltimore, and a course director of “Topics in interdisciplinary medicine: High-value health care”; Christopher Petrilli, MD, clinical assistant professor in the department of medicine at New York University Langone Health and clinical lead, Manhattan campus, value-based management; and Charlie Wray, DO, MS, assistant professor of medicine at the University of California in San Francisco and a coauthor of an article on high-value care in hospital medicine published recently in the Journal of General Internal Medicine6.
The experts agree that awareness of high-value care among practicing physicians and medical trainees has increased in the last few years. Major professional publications have highlighted the topic, including The Journal of Hospital Medicine’s “Things We Do For No Reason” series, JAMA’s “Teachable Moments,” and the American Journal of Medicine’s recurring column dedicated to high-value care practice. Leading teaching institutions have built high-value care curricula as a part of their medical student and resident training. However, widespread adoption has been slow and sometimes difficult.
The barriers to adoption of high-value practices among hospitalists are numerous and deep rooted in historical practices and culture. As Dr. Petrilli said, the “culture of overordering [diagnostic tests] is hard to break.” Hospitalists may not have well-developed relationships with patients, or time to explain why some tests or treatments are unnecessary. There is a lack of cost transparency, including the cost of the tests themselves and the downstream costs of additional tests and follow-ups. The best intended interventions fail to produce durable change unless they are seamlessly integrated into a hospitalist’s daily workflow.
Six steps to implementing a successful high-value care initiative
What can hospitalists do to improve the value of care they provide to their patients and hospital partners?
1. Identify high-value care opportunities at your hospital.
Dr. Wray pointed out that “all high-value care is local.” Start by looking at the national guidelines and talking to your senior clinical leaders and colleagues. Review your hospital data to identify opportunities and understand the root causes, including variability among providers.
If you choose to analyze and present provider-specific data, first be transparent on why you are doing that. Your goal is not to tell physicians how to practice or to score them, but instead, to promote adoption of evidence-based high-value care by identifying and discussing provider practice variations, and to generate possible solutions. Second, make sure that the data you present is credible and trustworthy by clearly outlining the data source, time frame, sample size per provider, any inclusion and exclusion criteria, attribution logic, and severity adjustment methodology. Third, expect initial pushback as transparency and change can be scary. But most doctors are inherently competitive and will want to be the best at caring for their patients.
2. Assemble the team.
Identify an executive sponsor – a senior clinical executive (for example, the chief medical officer or vice president of medical affairs) whose role is to help engage stakeholders, secure resources, and remove barriers. When assembling the rest of the team, include a representative from each major stakeholder group, but keep the team small enough to be effective. For example, if your project focuses on improving telemetry utilization, seek representation from hospitalists, cardiologists, nurses, utilization managers, and possibly IT. Look for people with the relevant knowledge and experience who are respected by their peers and can influence opinion.
3. Design a sustainable solution.
To be sustainable, a solution must be evidence based, well integrated in provider workflow, and have acceptable impact on daily workload (e.g., additional time per patient). If an estimated impact is significant, you need to discuss adding resources or negotiating trade-offs.
A great example of a sustainable solution, aimed to control overutilization of telemetry and urinary catheters, is the one implemented by Dr. Wray and his team.7 They designed an EHR-based “silent” indicator that clearly signaled an active telemetry or urinary catheter order for each patient. Clicking on the indicator directed a provider to a “manage order” screen where she could cancel the order, if necessary.
4. Engage providers.
You may design the best solution, but it will not succeed unless it is embraced by others. To engage providers, you must clearly communicate why the change is urgently needed for the benefit of their patients, hospital, or community, and appeal to their minds, hearts, and competitive nature.
For example, if you are focusing on overutilization of urinary catheters, you may share your hospital’s urinary catheter device utilization ratio (# of indwelling catheter days/# patient days) against national benchmarks, or the impact on hospital catheter–associated urinary tract infections (CAUTI) rates to appeal to the physicians’ minds. Often, data alone are not enough to move people to action. You must appeal to their hearts by sharing stories of real patients whose lives were affected by preventable CAUTI. Leverage physicians’ competitive nature by using provider-specific data to compare against their peers to spark a discussion.
5. Evaluate impact.
Even before you implement a solution, select metrics to measure impact and set SMART (specific, measurable, achievable, relevant, and time-bound) goals. As your implementation moves forward, do not let up or give up – continue to evaluate impact, remove barriers, refine your solution to get back on track if needed, and constantly communicate to share ongoing project results and lessons learned.
6. Sustain improvements.
Sustainable improvements require well-designed solutions integrated into provider workflow, but that is just the first step. Once you demonstrate the impact, consider including the metric (e.g., telemetry or urinary catheter utilization) in your team and/or individual provider performance dashboard, regularly reviewing and discussing performance during your team meetings to maintain engagement, and if needed, making improvements to get back on track.
Successful adoption of high-value care practices requires a disciplined approach to design and implement solutions that are patient-centric, evidence-based, data-driven and integrated in provider workflow.
Dr. Farah is a hospitalist, Physician Advisor, and Lean Six Sigma Black Belt. She is a performance improvement consultant based in Corvallis, Ore., and a member of The Hospitalist’s editorial advisory board.
References
1. From the Centers for Medicare & Medicaid Services: National Health Expenditure Projections 2018-2027.
2. Peterson-Kaiser Health System Tracker: How does health spending in the U.S. compare to other countries?
3. Creating a new culture of care, in “Best care at lower cost: The path to continuously learning health care in America.” (Washington: National Academies Press, 2013, pp. 255-80).
4. Choosing Wisely: SHM – Adult Hospital Medicine; Five things physicians and patients should question.
5. Qaseem A et al. Appropriate use of screening and diagnostic tests to foster high-value, cost-conscious care. Ann Intern Med. 2012 Jan 17;156(2):147-9.
6. Cho HJ et al. Right care in hospital medicine: Co-creation of ten opportunities in overuse and underuse for improving value in hospital medicine. J Gen Intern Med. 2018 Jun;33(6):804-6.
7. Wray CM et al. Improving value by reducing unnecessary telemetry and urinary catheter utilization in hospitalized patients. Am J Med. 2017 Sep;130(9):1037-41.
Six steps that can help your team
Six steps that can help your team
U.S. spending on health care is growing rapidly and expected to reach 19.7% of gross domestic product by 2026.1 In response, the Centers for Medicare and Medicaid Services and national organizations such as the American Board of Internal Medicine (ABIM) and the American College of Physicians (ACP) have launched initiatives to ensure that the value being delivered to patients is on par with the escalating cost of care.
Over the past 10 years, I have led and advised hundreds of small- and large-scale projects that focused on improving patient care quality and cost. Below, I share what I, along with other leaders in high-value care, have observed that it takes to implement successful and lasting improvements – for the benefit of patients and hospitals.
A brief history of high-value care
When compared to other wealthy countries, the United States spends disproportionately more money on health care. In 2016, U.S. health care spending was $3.3 trillion1, or $10,348 per person.2 Hospital care alone was responsible for a third of health spending and amounted to $1.1 trillion in 20161. By 2026, national health spending is projected to reach $5.7 trillion1.
In response to escalating health care costs, CMS and other payers have shifted toward value-based reimbursements that tie payments to health care facilities and clinicians to their performance on selected quality, cost, and efficiency measures. For example, under the CMS Merit-based Incentive Payment System (MIPS), 5% of clinicians’ revenue in 2020 is tied to their 2018 performance in four categories: Quality, Cost, Improvement Activities, and Promoting Interoperability. The percentage of revenue at risk will increase to 9% in 2022, based on 2020 performance.
Rising health care costs put a burden not just on the federal and state budgets, but on individual and family budgets as well. Out-of-pocket spending grew 3.9% in 2016 to $352.5 billion1 and is expected to increase in the future. High health care costs rightfully bring into question the value individual consumers of health care services are getting in return. If value is defined as the level of benefit achieved for a given cost, what is high-value care? The 2013 Institute of Medicine report3 defined high-value care as “the best care for the patient, with the optimal result for the circumstances, delivered at the right price.” It goes beyond a set of quality and cost measures used by payers to affect provider reimbursement and is driven by day-to-day individual providers’ decisions that affect individual patients’ outcomes and their cost of care.
High-value care has been embraced by national organizations. In 2012, the ABIM Foundation launched the Choosing Wisely initiative to support and promote conversations between clinicians and patients in choosing care that is truly necessary, supported by evidence, and free from harm. The result was an evidence-based list of recommendations from 540 specialty societies, including the Society of Hospital Medicine. The SHM – Adult Hospital Medicine list4 features the following “Five things physicians and patients should question”:
- Don’t place, or leave in place, urinary catheters for incontinence or convenience or monitoring of output for non–critically ill patients.
- Don’t prescribe medications for stress ulcer prophylaxis to medical inpatients unless at high risk for GI complications.
- Avoid transfusions of red blood cells for arbitrary hemoglobin or hematocrit thresholds and in the absence of symptoms of active coronary disease, heart failure, or stroke.
- Don’t order continuous telemetry monitoring outside of the ICU without using a protocol that governs continuation.
- Don’t perform repetitive CBC and chemistry testing in the face of clinical and lab stability.
The ACP launched a high-value care initiative that offers learning resources for clinicians and medical educators, clinical guidelines, and best practice advice. In 2012, a workgroup of internists convened by ACP developed a list of 37 clinical situations in which medical tests are commonly used but do not provide high value.5 Seven of those situations are applicable to adult hospital medicine.
High-value care today: What the experts say
More than 5 years later, what progress have hospitalists made in adopting high-value care practices? To answer this and other questions, I reached out to three national experts in high-value care in hospital medicine: Amit Pahwa, MD, assistant professor of medicine and pediatrics at Johns Hopkins University, Baltimore, and a course director of “Topics in interdisciplinary medicine: High-value health care”; Christopher Petrilli, MD, clinical assistant professor in the department of medicine at New York University Langone Health and clinical lead, Manhattan campus, value-based management; and Charlie Wray, DO, MS, assistant professor of medicine at the University of California in San Francisco and a coauthor of an article on high-value care in hospital medicine published recently in the Journal of General Internal Medicine6.
The experts agree that awareness of high-value care among practicing physicians and medical trainees has increased in the last few years. Major professional publications have highlighted the topic, including The Journal of Hospital Medicine’s “Things We Do For No Reason” series, JAMA’s “Teachable Moments,” and the American Journal of Medicine’s recurring column dedicated to high-value care practice. Leading teaching institutions have built high-value care curricula as a part of their medical student and resident training. However, widespread adoption has been slow and sometimes difficult.
The barriers to adoption of high-value practices among hospitalists are numerous and deep rooted in historical practices and culture. As Dr. Petrilli said, the “culture of overordering [diagnostic tests] is hard to break.” Hospitalists may not have well-developed relationships with patients, or time to explain why some tests or treatments are unnecessary. There is a lack of cost transparency, including the cost of the tests themselves and the downstream costs of additional tests and follow-ups. The best intended interventions fail to produce durable change unless they are seamlessly integrated into a hospitalist’s daily workflow.
Six steps to implementing a successful high-value care initiative
What can hospitalists do to improve the value of care they provide to their patients and hospital partners?
1. Identify high-value care opportunities at your hospital.
Dr. Wray pointed out that “all high-value care is local.” Start by looking at the national guidelines and talking to your senior clinical leaders and colleagues. Review your hospital data to identify opportunities and understand the root causes, including variability among providers.
If you choose to analyze and present provider-specific data, first be transparent on why you are doing that. Your goal is not to tell physicians how to practice or to score them, but instead, to promote adoption of evidence-based high-value care by identifying and discussing provider practice variations, and to generate possible solutions. Second, make sure that the data you present is credible and trustworthy by clearly outlining the data source, time frame, sample size per provider, any inclusion and exclusion criteria, attribution logic, and severity adjustment methodology. Third, expect initial pushback as transparency and change can be scary. But most doctors are inherently competitive and will want to be the best at caring for their patients.
2. Assemble the team.
Identify an executive sponsor – a senior clinical executive (for example, the chief medical officer or vice president of medical affairs) whose role is to help engage stakeholders, secure resources, and remove barriers. When assembling the rest of the team, include a representative from each major stakeholder group, but keep the team small enough to be effective. For example, if your project focuses on improving telemetry utilization, seek representation from hospitalists, cardiologists, nurses, utilization managers, and possibly IT. Look for people with the relevant knowledge and experience who are respected by their peers and can influence opinion.
3. Design a sustainable solution.
To be sustainable, a solution must be evidence based, well integrated in provider workflow, and have acceptable impact on daily workload (e.g., additional time per patient). If an estimated impact is significant, you need to discuss adding resources or negotiating trade-offs.
A great example of a sustainable solution, aimed to control overutilization of telemetry and urinary catheters, is the one implemented by Dr. Wray and his team.7 They designed an EHR-based “silent” indicator that clearly signaled an active telemetry or urinary catheter order for each patient. Clicking on the indicator directed a provider to a “manage order” screen where she could cancel the order, if necessary.
4. Engage providers.
You may design the best solution, but it will not succeed unless it is embraced by others. To engage providers, you must clearly communicate why the change is urgently needed for the benefit of their patients, hospital, or community, and appeal to their minds, hearts, and competitive nature.
For example, if you are focusing on overutilization of urinary catheters, you may share your hospital’s urinary catheter device utilization ratio (# of indwelling catheter days/# patient days) against national benchmarks, or the impact on hospital catheter–associated urinary tract infections (CAUTI) rates to appeal to the physicians’ minds. Often, data alone are not enough to move people to action. You must appeal to their hearts by sharing stories of real patients whose lives were affected by preventable CAUTI. Leverage physicians’ competitive nature by using provider-specific data to compare against their peers to spark a discussion.
5. Evaluate impact.
Even before you implement a solution, select metrics to measure impact and set SMART (specific, measurable, achievable, relevant, and time-bound) goals. As your implementation moves forward, do not let up or give up – continue to evaluate impact, remove barriers, refine your solution to get back on track if needed, and constantly communicate to share ongoing project results and lessons learned.
6. Sustain improvements.
Sustainable improvements require well-designed solutions integrated into provider workflow, but that is just the first step. Once you demonstrate the impact, consider including the metric (e.g., telemetry or urinary catheter utilization) in your team and/or individual provider performance dashboard, regularly reviewing and discussing performance during your team meetings to maintain engagement, and if needed, making improvements to get back on track.
Successful adoption of high-value care practices requires a disciplined approach to design and implement solutions that are patient-centric, evidence-based, data-driven and integrated in provider workflow.
Dr. Farah is a hospitalist, Physician Advisor, and Lean Six Sigma Black Belt. She is a performance improvement consultant based in Corvallis, Ore., and a member of The Hospitalist’s editorial advisory board.
References
1. From the Centers for Medicare & Medicaid Services: National Health Expenditure Projections 2018-2027.
2. Peterson-Kaiser Health System Tracker: How does health spending in the U.S. compare to other countries?
3. Creating a new culture of care, in “Best care at lower cost: The path to continuously learning health care in America.” (Washington: National Academies Press, 2013, pp. 255-80).
4. Choosing Wisely: SHM – Adult Hospital Medicine; Five things physicians and patients should question.
5. Qaseem A et al. Appropriate use of screening and diagnostic tests to foster high-value, cost-conscious care. Ann Intern Med. 2012 Jan 17;156(2):147-9.
6. Cho HJ et al. Right care in hospital medicine: Co-creation of ten opportunities in overuse and underuse for improving value in hospital medicine. J Gen Intern Med. 2018 Jun;33(6):804-6.
7. Wray CM et al. Improving value by reducing unnecessary telemetry and urinary catheter utilization in hospitalized patients. Am J Med. 2017 Sep;130(9):1037-41.
U.S. spending on health care is growing rapidly and expected to reach 19.7% of gross domestic product by 2026.1 In response, the Centers for Medicare and Medicaid Services and national organizations such as the American Board of Internal Medicine (ABIM) and the American College of Physicians (ACP) have launched initiatives to ensure that the value being delivered to patients is on par with the escalating cost of care.
Over the past 10 years, I have led and advised hundreds of small- and large-scale projects that focused on improving patient care quality and cost. Below, I share what I, along with other leaders in high-value care, have observed that it takes to implement successful and lasting improvements – for the benefit of patients and hospitals.
A brief history of high-value care
When compared to other wealthy countries, the United States spends disproportionately more money on health care. In 2016, U.S. health care spending was $3.3 trillion1, or $10,348 per person.2 Hospital care alone was responsible for a third of health spending and amounted to $1.1 trillion in 20161. By 2026, national health spending is projected to reach $5.7 trillion1.
In response to escalating health care costs, CMS and other payers have shifted toward value-based reimbursements that tie payments to health care facilities and clinicians to their performance on selected quality, cost, and efficiency measures. For example, under the CMS Merit-based Incentive Payment System (MIPS), 5% of clinicians’ revenue in 2020 is tied to their 2018 performance in four categories: Quality, Cost, Improvement Activities, and Promoting Interoperability. The percentage of revenue at risk will increase to 9% in 2022, based on 2020 performance.
Rising health care costs put a burden not just on the federal and state budgets, but on individual and family budgets as well. Out-of-pocket spending grew 3.9% in 2016 to $352.5 billion1 and is expected to increase in the future. High health care costs rightfully bring into question the value individual consumers of health care services are getting in return. If value is defined as the level of benefit achieved for a given cost, what is high-value care? The 2013 Institute of Medicine report3 defined high-value care as “the best care for the patient, with the optimal result for the circumstances, delivered at the right price.” It goes beyond a set of quality and cost measures used by payers to affect provider reimbursement and is driven by day-to-day individual providers’ decisions that affect individual patients’ outcomes and their cost of care.
High-value care has been embraced by national organizations. In 2012, the ABIM Foundation launched the Choosing Wisely initiative to support and promote conversations between clinicians and patients in choosing care that is truly necessary, supported by evidence, and free from harm. The result was an evidence-based list of recommendations from 540 specialty societies, including the Society of Hospital Medicine. The SHM – Adult Hospital Medicine list4 features the following “Five things physicians and patients should question”:
- Don’t place, or leave in place, urinary catheters for incontinence or convenience or monitoring of output for non–critically ill patients.
- Don’t prescribe medications for stress ulcer prophylaxis to medical inpatients unless at high risk for GI complications.
- Avoid transfusions of red blood cells for arbitrary hemoglobin or hematocrit thresholds and in the absence of symptoms of active coronary disease, heart failure, or stroke.
- Don’t order continuous telemetry monitoring outside of the ICU without using a protocol that governs continuation.
- Don’t perform repetitive CBC and chemistry testing in the face of clinical and lab stability.
The ACP launched a high-value care initiative that offers learning resources for clinicians and medical educators, clinical guidelines, and best practice advice. In 2012, a workgroup of internists convened by ACP developed a list of 37 clinical situations in which medical tests are commonly used but do not provide high value.5 Seven of those situations are applicable to adult hospital medicine.
High-value care today: What the experts say
More than 5 years later, what progress have hospitalists made in adopting high-value care practices? To answer this and other questions, I reached out to three national experts in high-value care in hospital medicine: Amit Pahwa, MD, assistant professor of medicine and pediatrics at Johns Hopkins University, Baltimore, and a course director of “Topics in interdisciplinary medicine: High-value health care”; Christopher Petrilli, MD, clinical assistant professor in the department of medicine at New York University Langone Health and clinical lead, Manhattan campus, value-based management; and Charlie Wray, DO, MS, assistant professor of medicine at the University of California in San Francisco and a coauthor of an article on high-value care in hospital medicine published recently in the Journal of General Internal Medicine6.
The experts agree that awareness of high-value care among practicing physicians and medical trainees has increased in the last few years. Major professional publications have highlighted the topic, including The Journal of Hospital Medicine’s “Things We Do For No Reason” series, JAMA’s “Teachable Moments,” and the American Journal of Medicine’s recurring column dedicated to high-value care practice. Leading teaching institutions have built high-value care curricula as a part of their medical student and resident training. However, widespread adoption has been slow and sometimes difficult.
The barriers to adoption of high-value practices among hospitalists are numerous and deep rooted in historical practices and culture. As Dr. Petrilli said, the “culture of overordering [diagnostic tests] is hard to break.” Hospitalists may not have well-developed relationships with patients, or time to explain why some tests or treatments are unnecessary. There is a lack of cost transparency, including the cost of the tests themselves and the downstream costs of additional tests and follow-ups. The best intended interventions fail to produce durable change unless they are seamlessly integrated into a hospitalist’s daily workflow.
Six steps to implementing a successful high-value care initiative
What can hospitalists do to improve the value of care they provide to their patients and hospital partners?
1. Identify high-value care opportunities at your hospital.
Dr. Wray pointed out that “all high-value care is local.” Start by looking at the national guidelines and talking to your senior clinical leaders and colleagues. Review your hospital data to identify opportunities and understand the root causes, including variability among providers.
If you choose to analyze and present provider-specific data, first be transparent on why you are doing that. Your goal is not to tell physicians how to practice or to score them, but instead, to promote adoption of evidence-based high-value care by identifying and discussing provider practice variations, and to generate possible solutions. Second, make sure that the data you present is credible and trustworthy by clearly outlining the data source, time frame, sample size per provider, any inclusion and exclusion criteria, attribution logic, and severity adjustment methodology. Third, expect initial pushback as transparency and change can be scary. But most doctors are inherently competitive and will want to be the best at caring for their patients.
2. Assemble the team.
Identify an executive sponsor – a senior clinical executive (for example, the chief medical officer or vice president of medical affairs) whose role is to help engage stakeholders, secure resources, and remove barriers. When assembling the rest of the team, include a representative from each major stakeholder group, but keep the team small enough to be effective. For example, if your project focuses on improving telemetry utilization, seek representation from hospitalists, cardiologists, nurses, utilization managers, and possibly IT. Look for people with the relevant knowledge and experience who are respected by their peers and can influence opinion.
3. Design a sustainable solution.
To be sustainable, a solution must be evidence based, well integrated in provider workflow, and have acceptable impact on daily workload (e.g., additional time per patient). If an estimated impact is significant, you need to discuss adding resources or negotiating trade-offs.
A great example of a sustainable solution, aimed to control overutilization of telemetry and urinary catheters, is the one implemented by Dr. Wray and his team.7 They designed an EHR-based “silent” indicator that clearly signaled an active telemetry or urinary catheter order for each patient. Clicking on the indicator directed a provider to a “manage order” screen where she could cancel the order, if necessary.
4. Engage providers.
You may design the best solution, but it will not succeed unless it is embraced by others. To engage providers, you must clearly communicate why the change is urgently needed for the benefit of their patients, hospital, or community, and appeal to their minds, hearts, and competitive nature.
For example, if you are focusing on overutilization of urinary catheters, you may share your hospital’s urinary catheter device utilization ratio (# of indwelling catheter days/# patient days) against national benchmarks, or the impact on hospital catheter–associated urinary tract infections (CAUTI) rates to appeal to the physicians’ minds. Often, data alone are not enough to move people to action. You must appeal to their hearts by sharing stories of real patients whose lives were affected by preventable CAUTI. Leverage physicians’ competitive nature by using provider-specific data to compare against their peers to spark a discussion.
5. Evaluate impact.
Even before you implement a solution, select metrics to measure impact and set SMART (specific, measurable, achievable, relevant, and time-bound) goals. As your implementation moves forward, do not let up or give up – continue to evaluate impact, remove barriers, refine your solution to get back on track if needed, and constantly communicate to share ongoing project results and lessons learned.
6. Sustain improvements.
Sustainable improvements require well-designed solutions integrated into provider workflow, but that is just the first step. Once you demonstrate the impact, consider including the metric (e.g., telemetry or urinary catheter utilization) in your team and/or individual provider performance dashboard, regularly reviewing and discussing performance during your team meetings to maintain engagement, and if needed, making improvements to get back on track.
Successful adoption of high-value care practices requires a disciplined approach to design and implement solutions that are patient-centric, evidence-based, data-driven and integrated in provider workflow.
Dr. Farah is a hospitalist, Physician Advisor, and Lean Six Sigma Black Belt. She is a performance improvement consultant based in Corvallis, Ore., and a member of The Hospitalist’s editorial advisory board.
References
1. From the Centers for Medicare & Medicaid Services: National Health Expenditure Projections 2018-2027.
2. Peterson-Kaiser Health System Tracker: How does health spending in the U.S. compare to other countries?
3. Creating a new culture of care, in “Best care at lower cost: The path to continuously learning health care in America.” (Washington: National Academies Press, 2013, pp. 255-80).
4. Choosing Wisely: SHM – Adult Hospital Medicine; Five things physicians and patients should question.
5. Qaseem A et al. Appropriate use of screening and diagnostic tests to foster high-value, cost-conscious care. Ann Intern Med. 2012 Jan 17;156(2):147-9.
6. Cho HJ et al. Right care in hospital medicine: Co-creation of ten opportunities in overuse and underuse for improving value in hospital medicine. J Gen Intern Med. 2018 Jun;33(6):804-6.
7. Wray CM et al. Improving value by reducing unnecessary telemetry and urinary catheter utilization in hospitalized patients. Am J Med. 2017 Sep;130(9):1037-41.
























