User login
Elevated Waist-to-Height Ratio Linked to Increased Migraine Incidence in Young Adults
Key clinical point: An increased waist-to-height ratio (WHtR), indicating central obesity, was associated with an increased incidence of migraine, particularly in individuals aged <60 years.
Major findings: Each unit increase in WHtR was associated with a 70% increase in the incidence of migraines (odds ratio [OR], 1.70; 95% CI, 1.04-2.78). Individuals in the highest WHtR quartile (WHtR values, 0.64-1.01) had a 13% greater incidence of migraines than those in the lowest quartile (WHtR values, 0.35-0.52; OR, 1.13; 95% CI, 0.99-1.28). For individuals aged <60 years, each unit increase in WHtR was associated with an 82% increased risk for migraine (P < .01); however, WHtR was negatively associated with migraine risk among those aged ≥60 years.
Study details: This cross-sectional study analyzed data from the National Health and Nutrition Examination Survey, including 13,344 participants, of whom 2764 had migraines. Disclosure: The study did not receive any funding. The authors declared no conflicts of interest.
Source: Jin J, Zheng Y, Gao T, Lin X, Li S, Huang C. Associations between the waist-to-height ratio index and migraine: A cross-section study of the NHANES 1999–2004. PLoS ONE. Published online October 23, 2024. Source
Key clinical point: An increased waist-to-height ratio (WHtR), indicating central obesity, was associated with an increased incidence of migraine, particularly in individuals aged <60 years.
Major findings: Each unit increase in WHtR was associated with a 70% increase in the incidence of migraines (odds ratio [OR], 1.70; 95% CI, 1.04-2.78). Individuals in the highest WHtR quartile (WHtR values, 0.64-1.01) had a 13% greater incidence of migraines than those in the lowest quartile (WHtR values, 0.35-0.52; OR, 1.13; 95% CI, 0.99-1.28). For individuals aged <60 years, each unit increase in WHtR was associated with an 82% increased risk for migraine (P < .01); however, WHtR was negatively associated with migraine risk among those aged ≥60 years.
Study details: This cross-sectional study analyzed data from the National Health and Nutrition Examination Survey, including 13,344 participants, of whom 2764 had migraines. Disclosure: The study did not receive any funding. The authors declared no conflicts of interest.
Source: Jin J, Zheng Y, Gao T, Lin X, Li S, Huang C. Associations between the waist-to-height ratio index and migraine: A cross-section study of the NHANES 1999–2004. PLoS ONE. Published online October 23, 2024. Source
Key clinical point: An increased waist-to-height ratio (WHtR), indicating central obesity, was associated with an increased incidence of migraine, particularly in individuals aged <60 years.
Major findings: Each unit increase in WHtR was associated with a 70% increase in the incidence of migraines (odds ratio [OR], 1.70; 95% CI, 1.04-2.78). Individuals in the highest WHtR quartile (WHtR values, 0.64-1.01) had a 13% greater incidence of migraines than those in the lowest quartile (WHtR values, 0.35-0.52; OR, 1.13; 95% CI, 0.99-1.28). For individuals aged <60 years, each unit increase in WHtR was associated with an 82% increased risk for migraine (P < .01); however, WHtR was negatively associated with migraine risk among those aged ≥60 years.
Study details: This cross-sectional study analyzed data from the National Health and Nutrition Examination Survey, including 13,344 participants, of whom 2764 had migraines. Disclosure: The study did not receive any funding. The authors declared no conflicts of interest.
Source: Jin J, Zheng Y, Gao T, Lin X, Li S, Huang C. Associations between the waist-to-height ratio index and migraine: A cross-section study of the NHANES 1999–2004. PLoS ONE. Published online October 23, 2024. Source
Weakness on one side of the body
FHM is a rare phenotype of migraine with aura with a characteristic presentation of motor aura. Motor aura presents as unilateral muscle weakness that tends to be felt first in the hands or arm and may spread to the face. To date, three distinct types have been identified by mutations in one of three genes. Type 1 is the most common and is associated with mutations in the gene CACNA1A. Mutations in ATP1A2 underlie type 2 FHM, and mutations in SCN1A underlie type 3 FHM.
FHM is distinguished from other hemiplegic migraine by family history of one or more affected first- or second-degree relatives. Genetic studies have shown FHM to have autosomal dominant inheritance. From half to three quarters of patients with FHM will have one of the more than 30 identified mutations on CACNA1A that diagnose type 1 FHM. These mutations affect transmission of glutamate in the neurons and neuronal reactions, increasing the susceptibility to cortical spreading depression associated with migraine. Mutations in ATP1A2 are found in about 20% of patients with FHM (type 2). More than 80 individual mutations have been identified, which alter sodium-potassium metabolism in neurons. About 5% of patients have type 3 FHM, associated with mutations in SCN1A that create gain of function or loss of function in neuronal voltage-gated sodium channels. Studies of other possible genes and mutations in relation to FHM, including PRRT2, are ongoing, but to date the associations are not clearly established.
Patients with FHM may also report sensory symptoms, visual disturbances, or aphasia. FHM generally affects people in their teens and twenties (women more than men) and has an estimated prevalence of 0.003% of the population. On average, patients report having two to three attacks per year, and some patients go for extended periods without a recurrent attack. Motor aura may occur on the same or opposite side of the body as headache and may alternate affected sides with each attack. Differential diagnoses that should be ruled out include transient ischemic attacks, infections (eg, meningitis, encephalitis), tumors, seizures, other inherited disorders, and metabolic issues.
Like other forms of migraine with aura, FHM is treated with abortive and/or preventive medications. Given the rarity of FHM, there are few studies specifically in families with this phenotype. Patients should be counseled on trigger avoidance to limit exposure. Acute treatment includes nonsteroidal anti-inflammatory drugs, acetaminophen, and other nonopioid pain relievers. The class of calcitonin gene-related peptide (CGRP) antagonists (rimegepant, ubrogepant, zavegepant) may be considered. However, with FHM, medications associated with ischemia must be avoided. As such, triptans and ergotamines are generally contraindicated, as are beta-blockers. Patients with FHM and more frequent or severe attacks may be considered for preventive treatment to improve function and quality of life and avoid reliance on acute therapies. Options include CGRP monoclonal antibodies (mAbs), administered subcutaneously or by intravenous infusion, and onabotulinumtoxinA injection. Current CGRP mAbs include eptinezumab, erenumab, fremanezumab, and galcanezumab. Combined CGRP mAb therapy with onabotulinumtoxinA may be an effective alternative for patients with resistant FHM.
Heidi Moawad, MD, Clinical Assistant Professor, Department of Medical Education, Case Western Reserve University School of Medicine, Cleveland, Ohio.
Heidi Moawad, MD, has disclosed no relevant financial relationships.
Image Quizzes are fictional or fictionalized clinical scenarios intended to provide evidence-based educational takeaways.
FHM is a rare phenotype of migraine with aura with a characteristic presentation of motor aura. Motor aura presents as unilateral muscle weakness that tends to be felt first in the hands or arm and may spread to the face. To date, three distinct types have been identified by mutations in one of three genes. Type 1 is the most common and is associated with mutations in the gene CACNA1A. Mutations in ATP1A2 underlie type 2 FHM, and mutations in SCN1A underlie type 3 FHM.
FHM is distinguished from other hemiplegic migraine by family history of one or more affected first- or second-degree relatives. Genetic studies have shown FHM to have autosomal dominant inheritance. From half to three quarters of patients with FHM will have one of the more than 30 identified mutations on CACNA1A that diagnose type 1 FHM. These mutations affect transmission of glutamate in the neurons and neuronal reactions, increasing the susceptibility to cortical spreading depression associated with migraine. Mutations in ATP1A2 are found in about 20% of patients with FHM (type 2). More than 80 individual mutations have been identified, which alter sodium-potassium metabolism in neurons. About 5% of patients have type 3 FHM, associated with mutations in SCN1A that create gain of function or loss of function in neuronal voltage-gated sodium channels. Studies of other possible genes and mutations in relation to FHM, including PRRT2, are ongoing, but to date the associations are not clearly established.
Patients with FHM may also report sensory symptoms, visual disturbances, or aphasia. FHM generally affects people in their teens and twenties (women more than men) and has an estimated prevalence of 0.003% of the population. On average, patients report having two to three attacks per year, and some patients go for extended periods without a recurrent attack. Motor aura may occur on the same or opposite side of the body as headache and may alternate affected sides with each attack. Differential diagnoses that should be ruled out include transient ischemic attacks, infections (eg, meningitis, encephalitis), tumors, seizures, other inherited disorders, and metabolic issues.
Like other forms of migraine with aura, FHM is treated with abortive and/or preventive medications. Given the rarity of FHM, there are few studies specifically in families with this phenotype. Patients should be counseled on trigger avoidance to limit exposure. Acute treatment includes nonsteroidal anti-inflammatory drugs, acetaminophen, and other nonopioid pain relievers. The class of calcitonin gene-related peptide (CGRP) antagonists (rimegepant, ubrogepant, zavegepant) may be considered. However, with FHM, medications associated with ischemia must be avoided. As such, triptans and ergotamines are generally contraindicated, as are beta-blockers. Patients with FHM and more frequent or severe attacks may be considered for preventive treatment to improve function and quality of life and avoid reliance on acute therapies. Options include CGRP monoclonal antibodies (mAbs), administered subcutaneously or by intravenous infusion, and onabotulinumtoxinA injection. Current CGRP mAbs include eptinezumab, erenumab, fremanezumab, and galcanezumab. Combined CGRP mAb therapy with onabotulinumtoxinA may be an effective alternative for patients with resistant FHM.
Heidi Moawad, MD, Clinical Assistant Professor, Department of Medical Education, Case Western Reserve University School of Medicine, Cleveland, Ohio.
Heidi Moawad, MD, has disclosed no relevant financial relationships.
Image Quizzes are fictional or fictionalized clinical scenarios intended to provide evidence-based educational takeaways.
FHM is a rare phenotype of migraine with aura with a characteristic presentation of motor aura. Motor aura presents as unilateral muscle weakness that tends to be felt first in the hands or arm and may spread to the face. To date, three distinct types have been identified by mutations in one of three genes. Type 1 is the most common and is associated with mutations in the gene CACNA1A. Mutations in ATP1A2 underlie type 2 FHM, and mutations in SCN1A underlie type 3 FHM.
FHM is distinguished from other hemiplegic migraine by family history of one or more affected first- or second-degree relatives. Genetic studies have shown FHM to have autosomal dominant inheritance. From half to three quarters of patients with FHM will have one of the more than 30 identified mutations on CACNA1A that diagnose type 1 FHM. These mutations affect transmission of glutamate in the neurons and neuronal reactions, increasing the susceptibility to cortical spreading depression associated with migraine. Mutations in ATP1A2 are found in about 20% of patients with FHM (type 2). More than 80 individual mutations have been identified, which alter sodium-potassium metabolism in neurons. About 5% of patients have type 3 FHM, associated with mutations in SCN1A that create gain of function or loss of function in neuronal voltage-gated sodium channels. Studies of other possible genes and mutations in relation to FHM, including PRRT2, are ongoing, but to date the associations are not clearly established.
Patients with FHM may also report sensory symptoms, visual disturbances, or aphasia. FHM generally affects people in their teens and twenties (women more than men) and has an estimated prevalence of 0.003% of the population. On average, patients report having two to three attacks per year, and some patients go for extended periods without a recurrent attack. Motor aura may occur on the same or opposite side of the body as headache and may alternate affected sides with each attack. Differential diagnoses that should be ruled out include transient ischemic attacks, infections (eg, meningitis, encephalitis), tumors, seizures, other inherited disorders, and metabolic issues.
Like other forms of migraine with aura, FHM is treated with abortive and/or preventive medications. Given the rarity of FHM, there are few studies specifically in families with this phenotype. Patients should be counseled on trigger avoidance to limit exposure. Acute treatment includes nonsteroidal anti-inflammatory drugs, acetaminophen, and other nonopioid pain relievers. The class of calcitonin gene-related peptide (CGRP) antagonists (rimegepant, ubrogepant, zavegepant) may be considered. However, with FHM, medications associated with ischemia must be avoided. As such, triptans and ergotamines are generally contraindicated, as are beta-blockers. Patients with FHM and more frequent or severe attacks may be considered for preventive treatment to improve function and quality of life and avoid reliance on acute therapies. Options include CGRP monoclonal antibodies (mAbs), administered subcutaneously or by intravenous infusion, and onabotulinumtoxinA injection. Current CGRP mAbs include eptinezumab, erenumab, fremanezumab, and galcanezumab. Combined CGRP mAb therapy with onabotulinumtoxinA may be an effective alternative for patients with resistant FHM.
Heidi Moawad, MD, Clinical Assistant Professor, Department of Medical Education, Case Western Reserve University School of Medicine, Cleveland, Ohio.
Heidi Moawad, MD, has disclosed no relevant financial relationships.
Image Quizzes are fictional or fictionalized clinical scenarios intended to provide evidence-based educational takeaways.
The patient is 35-year-old woman presenting for recurrent, unilateral headaches associated with weakness in the hand, arm, or face on one side of the body. The patient says this weakness sometimes occurs on the right side and other times on the left, often with a tingling sensation in the affected side, and is followed by an intense headache lasting for several hours.
She notes that the headaches started after recovery from a mild case of COVID. Over the past 2 years, five attacks have occurred, all following a similar pattern. With each attack, the motor weakness fully resolved with resolution of the headache. Two of the headaches were preceded by visual disturbances that resolved with headache onset.
Physical exam reveals an apparently healthy woman without fever or respiratory symptoms. Weight, blood pressure, and heart rate are within healthy ranges. All lab work is within normal ranges. Her facial appearance is normal at presentation, but she shows a photo taken during her last attack, in which she shows left side facial paralysis. Family history includes her mother with hemiplegic migraine and father with type 2 diabetes. You suspect familial hemiplegic migraine (FHM) and order genetic testing.
Migraine Differential Diagnosis
Throbbing headache and nausea
Migraine is a form of recurrent headache that can present as migraine with aura or migraine without aura, with the latter being the most common form. As in this patient, migraine without aura is a chronic form of headache of moderate to severe intensity that usually lasts for several hours but rarely may persist for up to 3 days. Headache pain is unilateral and often aggravated by triggers such as routine physical activity. The American Headache Society diagnostic criteria for migraine without aura include having symptoms of nausea and/or hypersensitivity to light or sound. This patient also described symptoms typical of the prodromal phase of migraine, which include yawning, temperature control, excessive thirst, and mood swings.
Patients who have migraine with aura also have unilateral headache pain of several hours' duration but experience visual (eg, dots or flashes) or sensory (prickly sensation on skin) symptoms, or may have brief difficulty with speech or motor function. These aura symptoms generally last 5 to 60 minutes before abating.
The worldwide impact of migraine potentially reaches a billion individuals. Its prevalence is second only to tension-type headaches. Migraine occurs in patients of all ages and affects women at a rate two to three times higher than in men. Prevalence appears to peak in the third and fourth decades of life and tends to be lower among older adults. Migraine also has a negative effect on patients' work, school, or social lives, and is associated with increased rates of depression and anxiety in adults. For patients who are prone to migraines, potential triggers include some foods and beverages (including those that contain caffeine and alcohol), menstrual cycles in women, exposure to strobing or bright lights or loud sounds, stressful situations, extra physical activity, and too much or too little sleep.
Migraine is a clinical diagnosis based on number of headaches (five or more episodes) plus two or more of the characteristic signs (unilateral, throbbing pain, pain intensity of ≥ 5 on a 10-point scale, and pain aggravated by routine physical motion, such as climbing stairs or bending over) plus nausea and/or photosensitivity or phonosensitivity. Prodrome symptoms are reported by about 70% of adult patients. Diagnosis rarely requires neuroimaging; however, before prescribing medication, a complete lab and metabolic workup should be done.
Management of migraine without aura includes acute and preventive interventions. Acute interventions cited by the American Headache Society include nonsteroidal anti-inflammatory drugs and acetaminophen for mild pain, and migraine-specific therapies such as the triptans, ergotamine derivatives, gepants (rimegepant, ubrogepant), and lasmiditan. Because response to any of these therapies will differ among patients with migraine, shared decision-making with patients about benefits and potential side effects is necessary and should include flexibility to change therapy if needed.
Preventive therapy should be offered to patients experiencing six or more migraines a month (regardless of impairment) and those, like this patient, with three or more migraines a month that significantly impair daily activities. Preventive therapy can be considered for those with fewer monthly episodes, depending on the degree of impairment. Oral preventive therapies with established efficacy include candesartan, certain beta-blockers, topiramate, and valproate. Parenteral monoclonal antibodies that inhibit calcitonin gene-related peptide activity (eptinezumab, erenumab, fremanezumab, and galcanezumab) and onabotulinumtoxinA may be considered if oral therapies provide inadequate prevention.
Tension-type headache is the most common form of primary headache. These headaches are bilateral and characterized by a pressing or dull sensation that is often mild in intensity. They are different from migraine in that they occur infrequently, lack sensory symptoms, and generally are of shorter duration (30 minutes to 24 hours). Fasting-related headache is characterized by diffuse, nonpulsating pain and is relieved with food.
Heidi Moawad, MD, Clinical Assistant Professor, Department of Medical Education, Case Western Reserve University School of Medicine, Cleveland, Ohio.
Heidi Moawad, MD, has disclosed no relevant financial relationships.
Image Quizzes are fictional or fictionalized clinical scenarios intended to provide evidence-based educational takeaways.
Migraine is a form of recurrent headache that can present as migraine with aura or migraine without aura, with the latter being the most common form. As in this patient, migraine without aura is a chronic form of headache of moderate to severe intensity that usually lasts for several hours but rarely may persist for up to 3 days. Headache pain is unilateral and often aggravated by triggers such as routine physical activity. The American Headache Society diagnostic criteria for migraine without aura include having symptoms of nausea and/or hypersensitivity to light or sound. This patient also described symptoms typical of the prodromal phase of migraine, which include yawning, temperature control, excessive thirst, and mood swings.
Patients who have migraine with aura also have unilateral headache pain of several hours' duration but experience visual (eg, dots or flashes) or sensory (prickly sensation on skin) symptoms, or may have brief difficulty with speech or motor function. These aura symptoms generally last 5 to 60 minutes before abating.
The worldwide impact of migraine potentially reaches a billion individuals. Its prevalence is second only to tension-type headaches. Migraine occurs in patients of all ages and affects women at a rate two to three times higher than in men. Prevalence appears to peak in the third and fourth decades of life and tends to be lower among older adults. Migraine also has a negative effect on patients' work, school, or social lives, and is associated with increased rates of depression and anxiety in adults. For patients who are prone to migraines, potential triggers include some foods and beverages (including those that contain caffeine and alcohol), menstrual cycles in women, exposure to strobing or bright lights or loud sounds, stressful situations, extra physical activity, and too much or too little sleep.
Migraine is a clinical diagnosis based on number of headaches (five or more episodes) plus two or more of the characteristic signs (unilateral, throbbing pain, pain intensity of ≥ 5 on a 10-point scale, and pain aggravated by routine physical motion, such as climbing stairs or bending over) plus nausea and/or photosensitivity or phonosensitivity. Prodrome symptoms are reported by about 70% of adult patients. Diagnosis rarely requires neuroimaging; however, before prescribing medication, a complete lab and metabolic workup should be done.
Management of migraine without aura includes acute and preventive interventions. Acute interventions cited by the American Headache Society include nonsteroidal anti-inflammatory drugs and acetaminophen for mild pain, and migraine-specific therapies such as the triptans, ergotamine derivatives, gepants (rimegepant, ubrogepant), and lasmiditan. Because response to any of these therapies will differ among patients with migraine, shared decision-making with patients about benefits and potential side effects is necessary and should include flexibility to change therapy if needed.
Preventive therapy should be offered to patients experiencing six or more migraines a month (regardless of impairment) and those, like this patient, with three or more migraines a month that significantly impair daily activities. Preventive therapy can be considered for those with fewer monthly episodes, depending on the degree of impairment. Oral preventive therapies with established efficacy include candesartan, certain beta-blockers, topiramate, and valproate. Parenteral monoclonal antibodies that inhibit calcitonin gene-related peptide activity (eptinezumab, erenumab, fremanezumab, and galcanezumab) and onabotulinumtoxinA may be considered if oral therapies provide inadequate prevention.
Tension-type headache is the most common form of primary headache. These headaches are bilateral and characterized by a pressing or dull sensation that is often mild in intensity. They are different from migraine in that they occur infrequently, lack sensory symptoms, and generally are of shorter duration (30 minutes to 24 hours). Fasting-related headache is characterized by diffuse, nonpulsating pain and is relieved with food.
Heidi Moawad, MD, Clinical Assistant Professor, Department of Medical Education, Case Western Reserve University School of Medicine, Cleveland, Ohio.
Heidi Moawad, MD, has disclosed no relevant financial relationships.
Image Quizzes are fictional or fictionalized clinical scenarios intended to provide evidence-based educational takeaways.
Migraine is a form of recurrent headache that can present as migraine with aura or migraine without aura, with the latter being the most common form. As in this patient, migraine without aura is a chronic form of headache of moderate to severe intensity that usually lasts for several hours but rarely may persist for up to 3 days. Headache pain is unilateral and often aggravated by triggers such as routine physical activity. The American Headache Society diagnostic criteria for migraine without aura include having symptoms of nausea and/or hypersensitivity to light or sound. This patient also described symptoms typical of the prodromal phase of migraine, which include yawning, temperature control, excessive thirst, and mood swings.
Patients who have migraine with aura also have unilateral headache pain of several hours' duration but experience visual (eg, dots or flashes) or sensory (prickly sensation on skin) symptoms, or may have brief difficulty with speech or motor function. These aura symptoms generally last 5 to 60 minutes before abating.
The worldwide impact of migraine potentially reaches a billion individuals. Its prevalence is second only to tension-type headaches. Migraine occurs in patients of all ages and affects women at a rate two to three times higher than in men. Prevalence appears to peak in the third and fourth decades of life and tends to be lower among older adults. Migraine also has a negative effect on patients' work, school, or social lives, and is associated with increased rates of depression and anxiety in adults. For patients who are prone to migraines, potential triggers include some foods and beverages (including those that contain caffeine and alcohol), menstrual cycles in women, exposure to strobing or bright lights or loud sounds, stressful situations, extra physical activity, and too much or too little sleep.
Migraine is a clinical diagnosis based on number of headaches (five or more episodes) plus two or more of the characteristic signs (unilateral, throbbing pain, pain intensity of ≥ 5 on a 10-point scale, and pain aggravated by routine physical motion, such as climbing stairs or bending over) plus nausea and/or photosensitivity or phonosensitivity. Prodrome symptoms are reported by about 70% of adult patients. Diagnosis rarely requires neuroimaging; however, before prescribing medication, a complete lab and metabolic workup should be done.
Management of migraine without aura includes acute and preventive interventions. Acute interventions cited by the American Headache Society include nonsteroidal anti-inflammatory drugs and acetaminophen for mild pain, and migraine-specific therapies such as the triptans, ergotamine derivatives, gepants (rimegepant, ubrogepant), and lasmiditan. Because response to any of these therapies will differ among patients with migraine, shared decision-making with patients about benefits and potential side effects is necessary and should include flexibility to change therapy if needed.
Preventive therapy should be offered to patients experiencing six or more migraines a month (regardless of impairment) and those, like this patient, with three or more migraines a month that significantly impair daily activities. Preventive therapy can be considered for those with fewer monthly episodes, depending on the degree of impairment. Oral preventive therapies with established efficacy include candesartan, certain beta-blockers, topiramate, and valproate. Parenteral monoclonal antibodies that inhibit calcitonin gene-related peptide activity (eptinezumab, erenumab, fremanezumab, and galcanezumab) and onabotulinumtoxinA may be considered if oral therapies provide inadequate prevention.
Tension-type headache is the most common form of primary headache. These headaches are bilateral and characterized by a pressing or dull sensation that is often mild in intensity. They are different from migraine in that they occur infrequently, lack sensory symptoms, and generally are of shorter duration (30 minutes to 24 hours). Fasting-related headache is characterized by diffuse, nonpulsating pain and is relieved with food.
Heidi Moawad, MD, Clinical Assistant Professor, Department of Medical Education, Case Western Reserve University School of Medicine, Cleveland, Ohio.
Heidi Moawad, MD, has disclosed no relevant financial relationships.
Image Quizzes are fictional or fictionalized clinical scenarios intended to provide evidence-based educational takeaways.
A 30-year-old female patient (140 lb and 5 ft 7 in; BMI 21.9) presents at the emergency department with a throbbing headache that began after dinner and was accompanied by queasy nausea. She reports immediately going to bed and sleeping through the night, but pain and other symptoms were still present in the morning. At this point, headache duration is approaching 15 hours. The patient describes the headache pain as throbbing and intense on the left side of her head.
The patient has a demanding job in advertising and often works very long hours on little sleep; this latest headache developed after working through the night before. When asked, she admits to feeling lethargic, yawning (to the point where coworkers commented), and experiencing intervals of excessive sweating earlier in the day before the headache emerged. The patient attributed these to being tired and hungry because of skipped meals since the previous night's dinner.
She has no history of cardiovascular or other chronic illness, and her blood pressure is within normal range. She describes having had about seven similar headaches of shorter duration, over the past 2 months; in each case, the headache led to a missed workday or having to leave work early and/or cancel social plans.
Comorbidities of Migraine
Sudden onset of symptoms
Migraines are episodic or chronic headaches, typically occurring on one side of the head, that have distinct characteristics and definitions from the International Classification of Headache Disorders, 3rd edition (ICHD 3). Migraine can occur at any age and is thought to affect about 5% of children before puberty, increases in prevalence after puberty, and reaches about 30% prevalence at age 25-30 years. Patients with migraine with aura have recurrent, fully reversible symptoms that can include diplopia, motor or sensory disturbances, and/or trouble with language that generally precede headache development. In some cases, aura may develop and resolve without headache. Migraine with aura can present at any age from early childhood onward and is present in about 30% of children and adolescents with migraine. In general, migraine with aura is more prevalent in female than in male individuals, especially adolescents.
Migraine with brainstem aura, as is the case here, is a specific subtype of migraine with aura, in which the aura specifically reflects an origin within the brainstem. Brainstem symptoms include diplopia, vertigo, difficulty controlling speech muscles, tinnitus, hearing loss, loss of coordination, and possibly impaired consciousness. For the diagnosis of migraine with brainstem aura, patients must not have motor or retinal symptoms. Aura development often is preceded by premonitory symptoms, such as fatigue, hunger or food cravings, and mood elevations.
Migraine without aura, in contrast, is characterized by recurrent moderate to severe pulsating headache lasting from a few hours to up to 3 days. Migraine without aura often causes nausea and sensitivity to light and/or sound.
Chronic migraine is defined as headache (with or without aura) occurring 15 or more days per month for at least the past 3 months. This patient's history does not fit the definition of chronic migraine.
Tension-type headaches generally are bilateral, with durations ranging from minutes to days. They tend to be mild to moderate in intensity and symptoms are not worsened by physical activity. In addition to their bilateral nature, these headaches differ from migraine in lacking associated visual, cortical, or other symptoms.
Any diagnosis of migraine requires assessment over time, using diagnostic criteria established by the International Headache Society in ICHD 3. It is not necessary to perform neuroimaging studies or CT in patients with migraine symptoms and an otherwise normal neurologic exam.
When a diagnosis of migraine with brainstem aura is established, pediatric or adolescent patients and their families should first be counseled on nonpharmacologic interventions. These interventions, which have demonstrated benefits in reducing headache frequency, include lifestyle modifications, regular sleep and meal schedules, adequate fluid intake, cognitive-behavioral therapy, stress management techniques, massage, and biofeedback techniques. Recommended for acute treatment of migraine are nonsteroidal anti-inflammatory drugs, acetaminophen, and triptans. There is limited evidence in pediatric or adolescent patients with use of preventive medications, such as topiramate, amitriptyline, or onabotulinumtoxinA. In clinical trials, patients receiving placebo saw improvements, and active treatments were only marginally, if at all, more effective. Current guidelines recommend a frank discussion with parents about the limitations of preventive therapies before making decisions to use them.
Heidi Moawad, MD, Clinical Assistant Professor, Department of Medical Education, Case Western Reserve University School of Medicine, Cleveland, Ohio.
Heidi Moawad, MD, has disclosed no relevant financial relationships.
Image Quizzes are fictional or fictionalized clinical scenarios intended to provide evidence-based educational takeaways.
Migraines are episodic or chronic headaches, typically occurring on one side of the head, that have distinct characteristics and definitions from the International Classification of Headache Disorders, 3rd edition (ICHD 3). Migraine can occur at any age and is thought to affect about 5% of children before puberty, increases in prevalence after puberty, and reaches about 30% prevalence at age 25-30 years. Patients with migraine with aura have recurrent, fully reversible symptoms that can include diplopia, motor or sensory disturbances, and/or trouble with language that generally precede headache development. In some cases, aura may develop and resolve without headache. Migraine with aura can present at any age from early childhood onward and is present in about 30% of children and adolescents with migraine. In general, migraine with aura is more prevalent in female than in male individuals, especially adolescents.
Migraine with brainstem aura, as is the case here, is a specific subtype of migraine with aura, in which the aura specifically reflects an origin within the brainstem. Brainstem symptoms include diplopia, vertigo, difficulty controlling speech muscles, tinnitus, hearing loss, loss of coordination, and possibly impaired consciousness. For the diagnosis of migraine with brainstem aura, patients must not have motor or retinal symptoms. Aura development often is preceded by premonitory symptoms, such as fatigue, hunger or food cravings, and mood elevations.
Migraine without aura, in contrast, is characterized by recurrent moderate to severe pulsating headache lasting from a few hours to up to 3 days. Migraine without aura often causes nausea and sensitivity to light and/or sound.
Chronic migraine is defined as headache (with or without aura) occurring 15 or more days per month for at least the past 3 months. This patient's history does not fit the definition of chronic migraine.
Tension-type headaches generally are bilateral, with durations ranging from minutes to days. They tend to be mild to moderate in intensity and symptoms are not worsened by physical activity. In addition to their bilateral nature, these headaches differ from migraine in lacking associated visual, cortical, or other symptoms.
Any diagnosis of migraine requires assessment over time, using diagnostic criteria established by the International Headache Society in ICHD 3. It is not necessary to perform neuroimaging studies or CT in patients with migraine symptoms and an otherwise normal neurologic exam.
When a diagnosis of migraine with brainstem aura is established, pediatric or adolescent patients and their families should first be counseled on nonpharmacologic interventions. These interventions, which have demonstrated benefits in reducing headache frequency, include lifestyle modifications, regular sleep and meal schedules, adequate fluid intake, cognitive-behavioral therapy, stress management techniques, massage, and biofeedback techniques. Recommended for acute treatment of migraine are nonsteroidal anti-inflammatory drugs, acetaminophen, and triptans. There is limited evidence in pediatric or adolescent patients with use of preventive medications, such as topiramate, amitriptyline, or onabotulinumtoxinA. In clinical trials, patients receiving placebo saw improvements, and active treatments were only marginally, if at all, more effective. Current guidelines recommend a frank discussion with parents about the limitations of preventive therapies before making decisions to use them.
Heidi Moawad, MD, Clinical Assistant Professor, Department of Medical Education, Case Western Reserve University School of Medicine, Cleveland, Ohio.
Heidi Moawad, MD, has disclosed no relevant financial relationships.
Image Quizzes are fictional or fictionalized clinical scenarios intended to provide evidence-based educational takeaways.
Migraines are episodic or chronic headaches, typically occurring on one side of the head, that have distinct characteristics and definitions from the International Classification of Headache Disorders, 3rd edition (ICHD 3). Migraine can occur at any age and is thought to affect about 5% of children before puberty, increases in prevalence after puberty, and reaches about 30% prevalence at age 25-30 years. Patients with migraine with aura have recurrent, fully reversible symptoms that can include diplopia, motor or sensory disturbances, and/or trouble with language that generally precede headache development. In some cases, aura may develop and resolve without headache. Migraine with aura can present at any age from early childhood onward and is present in about 30% of children and adolescents with migraine. In general, migraine with aura is more prevalent in female than in male individuals, especially adolescents.
Migraine with brainstem aura, as is the case here, is a specific subtype of migraine with aura, in which the aura specifically reflects an origin within the brainstem. Brainstem symptoms include diplopia, vertigo, difficulty controlling speech muscles, tinnitus, hearing loss, loss of coordination, and possibly impaired consciousness. For the diagnosis of migraine with brainstem aura, patients must not have motor or retinal symptoms. Aura development often is preceded by premonitory symptoms, such as fatigue, hunger or food cravings, and mood elevations.
Migraine without aura, in contrast, is characterized by recurrent moderate to severe pulsating headache lasting from a few hours to up to 3 days. Migraine without aura often causes nausea and sensitivity to light and/or sound.
Chronic migraine is defined as headache (with or without aura) occurring 15 or more days per month for at least the past 3 months. This patient's history does not fit the definition of chronic migraine.
Tension-type headaches generally are bilateral, with durations ranging from minutes to days. They tend to be mild to moderate in intensity and symptoms are not worsened by physical activity. In addition to their bilateral nature, these headaches differ from migraine in lacking associated visual, cortical, or other symptoms.
Any diagnosis of migraine requires assessment over time, using diagnostic criteria established by the International Headache Society in ICHD 3. It is not necessary to perform neuroimaging studies or CT in patients with migraine symptoms and an otherwise normal neurologic exam.
When a diagnosis of migraine with brainstem aura is established, pediatric or adolescent patients and their families should first be counseled on nonpharmacologic interventions. These interventions, which have demonstrated benefits in reducing headache frequency, include lifestyle modifications, regular sleep and meal schedules, adequate fluid intake, cognitive-behavioral therapy, stress management techniques, massage, and biofeedback techniques. Recommended for acute treatment of migraine are nonsteroidal anti-inflammatory drugs, acetaminophen, and triptans. There is limited evidence in pediatric or adolescent patients with use of preventive medications, such as topiramate, amitriptyline, or onabotulinumtoxinA. In clinical trials, patients receiving placebo saw improvements, and active treatments were only marginally, if at all, more effective. Current guidelines recommend a frank discussion with parents about the limitations of preventive therapies before making decisions to use them.
Heidi Moawad, MD, Clinical Assistant Professor, Department of Medical Education, Case Western Reserve University School of Medicine, Cleveland, Ohio.
Heidi Moawad, MD, has disclosed no relevant financial relationships.
Image Quizzes are fictional or fictionalized clinical scenarios intended to provide evidence-based educational takeaways.
A 13-year-old girl presents with symptoms of sudden onset of double vision, vertigo, and ataxia that have occurred six or seven times over the past 2 months and usually precede a headache. These symptoms generally last less than 10 minutes. The girl says she has noticed that she often feels a bit manic and has food cravings a few hours before the double vision and other symptoms occur. She is an athlete at school but says during these attacks she avoids even walking around the house because the movement makes her symptoms worse. She has no muscle weakness or changes on her ophthalmologic exam.
No obvious issues on physical exam nor evidence of visual or neurologic deficits are present at the time of the office visit; the patient has 20/20 vision. Relevant medical history includes menarche at age 12 years. The patient is on the track team at school and is physically fit, without previous evidence of balance or other neurologic issues.
Migraine Variants
Homonymous blurred vision
Migraine is one of the most common neurologic diseases, affecting about 14% of the population. Migraines may also be associated with auras or visual or sensory symptoms that precede the headache. However, approximately 4% of people with migraine experience their usual migraines and sometimes also experience episodes of an aura that is not followed by a headache. Silent migraines, also known as acephalgic migraines or "migraine auras without headache," typically cause symptoms that accompany the phases of a migraine, but without the classic headache pain. It is most common among young adults in their 20s and 30s and older adults between 40 and 60 years of age, especially in those who had auras accompanied by migraine headaches when younger.
According to the International Headache Society, a migraine aura develops gradually over 5 to 10 minutes and lasts for less than 1 hour. Although the symptoms of a silent migraine may vary from person to person, visual symptoms occur in more than 90% of migraine auras. Visual symptoms may also be accompanied by other neurologic symptoms such as dizziness, numbness or tingling, and aphasia. The most common visual symptoms are positive symptoms, such as flash scotoma, visual distortion, colored spots, and flash hallucinations. Visual symptoms may easily be confused with symptoms of a transient ischemic attack (TIA). However, migraine auras generally last 15 to 30 minutes. They are often described as dynamic, bright, multicolored forms in geometric patterns. In contrast, the visual symptoms of a TIA last on average 3 to 10 minutes and are described as a static, dark dimming of vision.
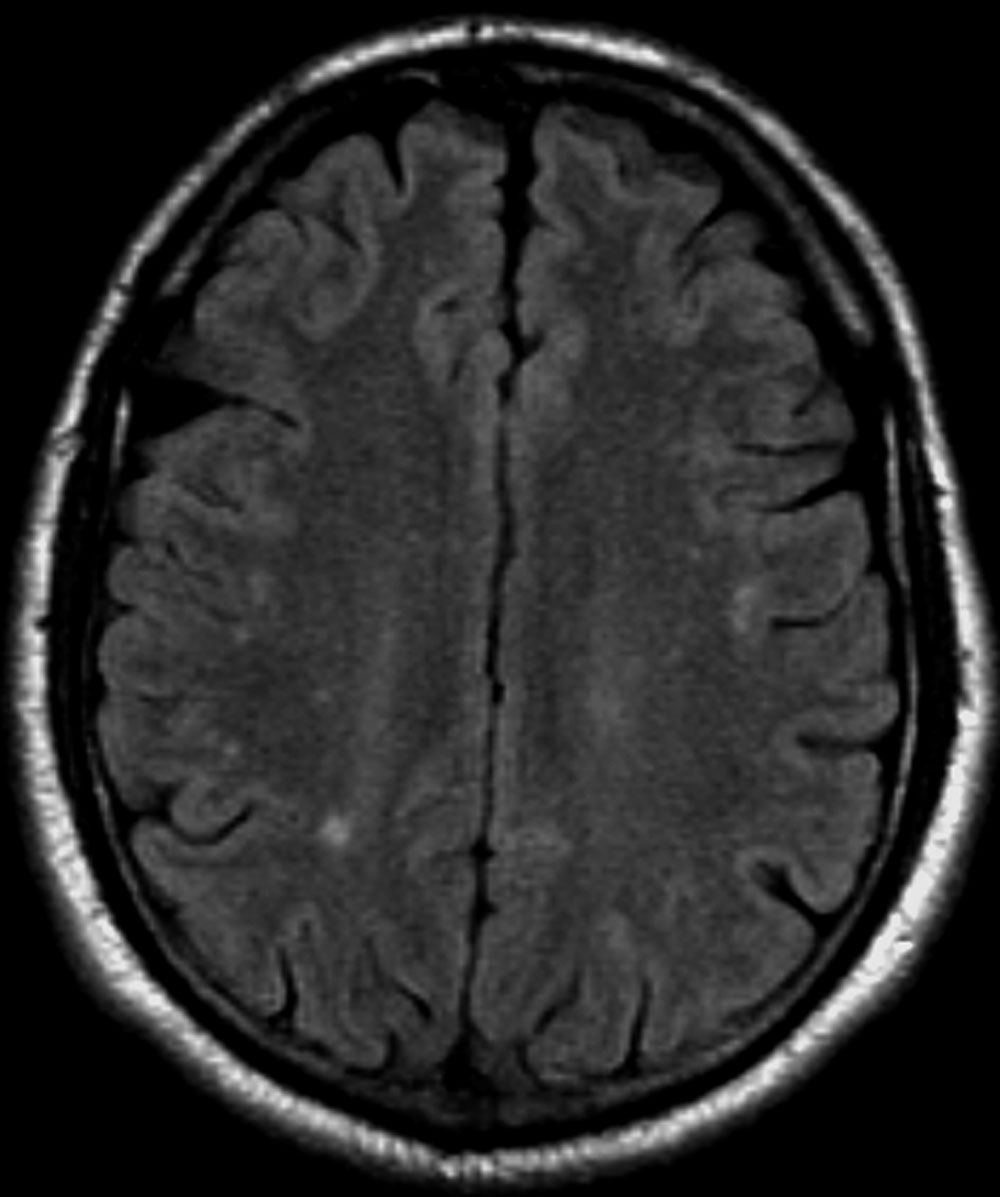
The diagnosis of migraine aura without headache should be made after all other possible causes have been excluded, particularly TIAs and focal seizures because of the diagnostic, therapeutic, and prognostic implications. Testing may include a neurologic and eye examination, MRI, CT angiography, and laboratory testing for clotting disorders.
Migraine aura without headache is a benign condition and generally does not require treatment. When symptoms of silent migraines are severe enough, low-dose aspirin and calcium-channel blockers may be considered as treatment options. However, triptans, which are often used in patients with migraine headaches, should not be used to treat silent migraines because they do not act fast enough to affect an aura. In addition, triptans should be used with caution in older patients, who may have vascular disease, hypertension, and other cardiovascular risk factors.
Jasmin Harpe, MD, MPH, Headache Fellow, Department of Neurology, Harvard University, John R. Graham Headache Center, Mass General Brigham, Boston, MA
Jasmin Harpe, MD, MPH, has disclosed no relevant financial relationships.
Image Quizzes are fictional or fictionalized clinical scenarios intended to provide evidence-based educational takeaways.
Migraine is one of the most common neurologic diseases, affecting about 14% of the population. Migraines may also be associated with auras or visual or sensory symptoms that precede the headache. However, approximately 4% of people with migraine experience their usual migraines and sometimes also experience episodes of an aura that is not followed by a headache. Silent migraines, also known as acephalgic migraines or "migraine auras without headache," typically cause symptoms that accompany the phases of a migraine, but without the classic headache pain. It is most common among young adults in their 20s and 30s and older adults between 40 and 60 years of age, especially in those who had auras accompanied by migraine headaches when younger.
According to the International Headache Society, a migraine aura develops gradually over 5 to 10 minutes and lasts for less than 1 hour. Although the symptoms of a silent migraine may vary from person to person, visual symptoms occur in more than 90% of migraine auras. Visual symptoms may also be accompanied by other neurologic symptoms such as dizziness, numbness or tingling, and aphasia. The most common visual symptoms are positive symptoms, such as flash scotoma, visual distortion, colored spots, and flash hallucinations. Visual symptoms may easily be confused with symptoms of a transient ischemic attack (TIA). However, migraine auras generally last 15 to 30 minutes. They are often described as dynamic, bright, multicolored forms in geometric patterns. In contrast, the visual symptoms of a TIA last on average 3 to 10 minutes and are described as a static, dark dimming of vision.
The diagnosis of migraine aura without headache should be made after all other possible causes have been excluded, particularly TIAs and focal seizures because of the diagnostic, therapeutic, and prognostic implications. Testing may include a neurologic and eye examination, MRI, CT angiography, and laboratory testing for clotting disorders.
Migraine aura without headache is a benign condition and generally does not require treatment. When symptoms of silent migraines are severe enough, low-dose aspirin and calcium-channel blockers may be considered as treatment options. However, triptans, which are often used in patients with migraine headaches, should not be used to treat silent migraines because they do not act fast enough to affect an aura. In addition, triptans should be used with caution in older patients, who may have vascular disease, hypertension, and other cardiovascular risk factors.
Jasmin Harpe, MD, MPH, Headache Fellow, Department of Neurology, Harvard University, John R. Graham Headache Center, Mass General Brigham, Boston, MA
Jasmin Harpe, MD, MPH, has disclosed no relevant financial relationships.
Image Quizzes are fictional or fictionalized clinical scenarios intended to provide evidence-based educational takeaways.
Migraine is one of the most common neurologic diseases, affecting about 14% of the population. Migraines may also be associated with auras or visual or sensory symptoms that precede the headache. However, approximately 4% of people with migraine experience their usual migraines and sometimes also experience episodes of an aura that is not followed by a headache. Silent migraines, also known as acephalgic migraines or "migraine auras without headache," typically cause symptoms that accompany the phases of a migraine, but without the classic headache pain. It is most common among young adults in their 20s and 30s and older adults between 40 and 60 years of age, especially in those who had auras accompanied by migraine headaches when younger.
According to the International Headache Society, a migraine aura develops gradually over 5 to 10 minutes and lasts for less than 1 hour. Although the symptoms of a silent migraine may vary from person to person, visual symptoms occur in more than 90% of migraine auras. Visual symptoms may also be accompanied by other neurologic symptoms such as dizziness, numbness or tingling, and aphasia. The most common visual symptoms are positive symptoms, such as flash scotoma, visual distortion, colored spots, and flash hallucinations. Visual symptoms may easily be confused with symptoms of a transient ischemic attack (TIA). However, migraine auras generally last 15 to 30 minutes. They are often described as dynamic, bright, multicolored forms in geometric patterns. In contrast, the visual symptoms of a TIA last on average 3 to 10 minutes and are described as a static, dark dimming of vision.
The diagnosis of migraine aura without headache should be made after all other possible causes have been excluded, particularly TIAs and focal seizures because of the diagnostic, therapeutic, and prognostic implications. Testing may include a neurologic and eye examination, MRI, CT angiography, and laboratory testing for clotting disorders.
Migraine aura without headache is a benign condition and generally does not require treatment. When symptoms of silent migraines are severe enough, low-dose aspirin and calcium-channel blockers may be considered as treatment options. However, triptans, which are often used in patients with migraine headaches, should not be used to treat silent migraines because they do not act fast enough to affect an aura. In addition, triptans should be used with caution in older patients, who may have vascular disease, hypertension, and other cardiovascular risk factors.
Jasmin Harpe, MD, MPH, Headache Fellow, Department of Neurology, Harvard University, John R. Graham Headache Center, Mass General Brigham, Boston, MA
Jasmin Harpe, MD, MPH, has disclosed no relevant financial relationships.
Image Quizzes are fictional or fictionalized clinical scenarios intended to provide evidence-based educational takeaways.
A 56-year-old woman with no significant past medical history presents for a neurologic evaluation owing to three episodes of homonymous blurred vision for the past year. She describes the episodes as presenting as irregular shapes in both eyes. The shapes are located at the top left and right side of the visual fields and have a purple, light blue and brown color. During the episodes, the symptoms develop gradually over 5 to 10 minutes and resolve within 45 minutes. She has not noticed any precipitating factors. Her symptoms are not associated with muscle weakness, dizziness, or changes in speech. The patient denies ever having headaches in the past, but her mother and sister both see a neurologist for migraines. She denies the use of alcohol or drugs but has smoked 10 cigarettes daily for the past 30 years.
Test results from neurologic and eye examinations are normal. Routine laboratory tests are within reference normal limits. A carotid Doppler ultrasound indicates no carotid plaques. Brain MRI and CT angiography display normal results.