User login
Potential therapeutic strategy for BL, DLBCL
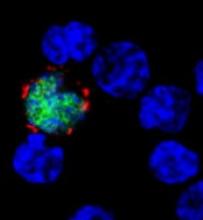
Preclinical research has revealed a potential strategy for treating Burkitt lymphoma (BL) and diffuse large B-cell lymphoma (DLBCL).
Investigators discovered that miR-28 inhibits the growth of B-cell lymphomas, but this microRNA is often lost in these lymphomas.
Re-expressing miR-28 in mouse models of BL and DLBCL inhibited tumor growth, which supports the potential of synthetic miR-28 analogs for the treatment of these lymphomas.
In fact, the investigators believe their work could lead to the development of the first miRNA analog therapy for the treatment of B-cell lymphoma and provide the basis for clinical trials.
Almudena Ramiro, PhD, of Centro Nacional de Investigaciones Cardiovasculares in Madrid, Spain, and her colleagues described the work in Blood.
The team characterized the function of miR-28 in the biology of mature B lymphocytes and in the development of lymphomas associated with this cell type.
The investigators found that miR-28 regulates the terminal differentiation of B lymphocytes, a fundamental process in the biology of these cells that generates memory B lymphocytes and highly specific plasma cells.
But the team found that miR-28 expression is lost in several germinal center-derived lymphoma subtypes, including BL, DLBCL, follicular lymphoma, and chronic lymphocytic leukemia.
In vitro experiments showed that miR-28 expression dampens B-cell receptor signaling and diminishes the proliferation and survival of primary B cells and lymphoma cells.
And in vivo experiments showed that re-establishing miR-28 expression slows tumor growth in DLBCL and BL.
The investigators re-expressed miR-28 in xenograft models of BL and DLBCL via the use of viral vectors or synthetic molecules and found that both methods blocked tumor growth. The same effect was observed in mice with established BL tumors.
Dr Ramiro and her colleagues said these results reveal the therapeutic potential of miR-28 and provide ample justification for the initiation of clinical trials of miR-28-based therapies to treat B-cell lymphomas. ![]()
Preclinical research has revealed a potential strategy for treating Burkitt lymphoma (BL) and diffuse large B-cell lymphoma (DLBCL).
Investigators discovered that miR-28 inhibits the growth of B-cell lymphomas, but this microRNA is often lost in these lymphomas.
Re-expressing miR-28 in mouse models of BL and DLBCL inhibited tumor growth, which supports the potential of synthetic miR-28 analogs for the treatment of these lymphomas.
In fact, the investigators believe their work could lead to the development of the first miRNA analog therapy for the treatment of B-cell lymphoma and provide the basis for clinical trials.
Almudena Ramiro, PhD, of Centro Nacional de Investigaciones Cardiovasculares in Madrid, Spain, and her colleagues described the work in Blood.
The team characterized the function of miR-28 in the biology of mature B lymphocytes and in the development of lymphomas associated with this cell type.
The investigators found that miR-28 regulates the terminal differentiation of B lymphocytes, a fundamental process in the biology of these cells that generates memory B lymphocytes and highly specific plasma cells.
But the team found that miR-28 expression is lost in several germinal center-derived lymphoma subtypes, including BL, DLBCL, follicular lymphoma, and chronic lymphocytic leukemia.
In vitro experiments showed that miR-28 expression dampens B-cell receptor signaling and diminishes the proliferation and survival of primary B cells and lymphoma cells.
And in vivo experiments showed that re-establishing miR-28 expression slows tumor growth in DLBCL and BL.
The investigators re-expressed miR-28 in xenograft models of BL and DLBCL via the use of viral vectors or synthetic molecules and found that both methods blocked tumor growth. The same effect was observed in mice with established BL tumors.
Dr Ramiro and her colleagues said these results reveal the therapeutic potential of miR-28 and provide ample justification for the initiation of clinical trials of miR-28-based therapies to treat B-cell lymphomas. ![]()
Preclinical research has revealed a potential strategy for treating Burkitt lymphoma (BL) and diffuse large B-cell lymphoma (DLBCL).
Investigators discovered that miR-28 inhibits the growth of B-cell lymphomas, but this microRNA is often lost in these lymphomas.
Re-expressing miR-28 in mouse models of BL and DLBCL inhibited tumor growth, which supports the potential of synthetic miR-28 analogs for the treatment of these lymphomas.
In fact, the investigators believe their work could lead to the development of the first miRNA analog therapy for the treatment of B-cell lymphoma and provide the basis for clinical trials.
Almudena Ramiro, PhD, of Centro Nacional de Investigaciones Cardiovasculares in Madrid, Spain, and her colleagues described the work in Blood.
The team characterized the function of miR-28 in the biology of mature B lymphocytes and in the development of lymphomas associated with this cell type.
The investigators found that miR-28 regulates the terminal differentiation of B lymphocytes, a fundamental process in the biology of these cells that generates memory B lymphocytes and highly specific plasma cells.
But the team found that miR-28 expression is lost in several germinal center-derived lymphoma subtypes, including BL, DLBCL, follicular lymphoma, and chronic lymphocytic leukemia.
In vitro experiments showed that miR-28 expression dampens B-cell receptor signaling and diminishes the proliferation and survival of primary B cells and lymphoma cells.
And in vivo experiments showed that re-establishing miR-28 expression slows tumor growth in DLBCL and BL.
The investigators re-expressed miR-28 in xenograft models of BL and DLBCL via the use of viral vectors or synthetic molecules and found that both methods blocked tumor growth. The same effect was observed in mice with established BL tumors.
Dr Ramiro and her colleagues said these results reveal the therapeutic potential of miR-28 and provide ample justification for the initiation of clinical trials of miR-28-based therapies to treat B-cell lymphomas. ![]()
Drug granted orphan status for follicular lymphoma
The US Food and Drug Administration (FDA) has granted orphan designation to G100 for the treatment of follicular lymphoma.
G100 is a synthetic small-molecule toll-like receptor-4 agonist, glucopyranosyl lipid A, formulated in a stable emulsion.
The FDA grants orphan designation to drugs and biologics intended to treat, diagnose, or prevent rare diseases/disorders affecting fewer than 200,000 people in the US.
Orphan designation provides companies with certain incentives to develop products for rare diseases. This includes a 50% tax break on research and development, a fee waiver, access to federal grants, and 7 years of market exclusivity if the product is approved.
G100 is being developed by Immune Design. The company says G100 works by leveraging the activation of innate and adaptive immunity in the tumor microenvironment to create an immune response against the tumor’s pre-existing antigens.
According to Immune Design, clinical and preclinical data have demonstrated G100’s ability to activate tumor-infiltrating lymphocytes, macrophages, and dendritic cells, and promote antigen-presentation and the recruitment of T cells to the tumor.
The ensuing induction of local and systemic immune responses has been shown to result in local and abscopal tumor control in preclinical studies.
In fact, G100, when combined with local radiation, demonstrated efficacy against A20 lymphoma in mice. This research was presented in a poster at the 2016 ASH Annual Meeting (abstract 4166).
In this study, investigators evaluated the immune response and therapeutic effects of intratumoral G100 alone, local radiation alone, and concomitant G100 and local radiation in mice with A20 lymphoma.
The investigators said the combination therapy demonstrated:
- Synergistic antitumor effects in both injected as well as uninjected tumors (abscopal effects)
- Synergistic induction of pro-inflammatory cytokine and chemokine environment, as well as induction of genes governing antigen processing and presentation
- Increased infiltration of T cells, including CD4 and CD8 T cells, in treated tumors.
In contrast, tumors that received only radiation had significantly lower T-cell levels than untreated tumors.
“These findings highlight the potential beneficial effect that immunotherapy with G100 could provide when given with radiation by modulating the tumor microenvironment to generate a systemic, durable, T-cell anti-tumor response,” said study investigator Ramesh Rengan, MD, of the University of Washington in Seattle.
“As shown in this model, G100 may hold potential as a treatment for lymphoma patients.”
To test that theory, Immune Design is conducting a phase 1/2 trial of G100 given with local radiation or the anti-PD-1 agent pembrolizumab to patients with follicular lymphoma. ![]()
The US Food and Drug Administration (FDA) has granted orphan designation to G100 for the treatment of follicular lymphoma.
G100 is a synthetic small-molecule toll-like receptor-4 agonist, glucopyranosyl lipid A, formulated in a stable emulsion.
The FDA grants orphan designation to drugs and biologics intended to treat, diagnose, or prevent rare diseases/disorders affecting fewer than 200,000 people in the US.
Orphan designation provides companies with certain incentives to develop products for rare diseases. This includes a 50% tax break on research and development, a fee waiver, access to federal grants, and 7 years of market exclusivity if the product is approved.
G100 is being developed by Immune Design. The company says G100 works by leveraging the activation of innate and adaptive immunity in the tumor microenvironment to create an immune response against the tumor’s pre-existing antigens.
According to Immune Design, clinical and preclinical data have demonstrated G100’s ability to activate tumor-infiltrating lymphocytes, macrophages, and dendritic cells, and promote antigen-presentation and the recruitment of T cells to the tumor.
The ensuing induction of local and systemic immune responses has been shown to result in local and abscopal tumor control in preclinical studies.
In fact, G100, when combined with local radiation, demonstrated efficacy against A20 lymphoma in mice. This research was presented in a poster at the 2016 ASH Annual Meeting (abstract 4166).
In this study, investigators evaluated the immune response and therapeutic effects of intratumoral G100 alone, local radiation alone, and concomitant G100 and local radiation in mice with A20 lymphoma.
The investigators said the combination therapy demonstrated:
- Synergistic antitumor effects in both injected as well as uninjected tumors (abscopal effects)
- Synergistic induction of pro-inflammatory cytokine and chemokine environment, as well as induction of genes governing antigen processing and presentation
- Increased infiltration of T cells, including CD4 and CD8 T cells, in treated tumors.
In contrast, tumors that received only radiation had significantly lower T-cell levels than untreated tumors.
“These findings highlight the potential beneficial effect that immunotherapy with G100 could provide when given with radiation by modulating the tumor microenvironment to generate a systemic, durable, T-cell anti-tumor response,” said study investigator Ramesh Rengan, MD, of the University of Washington in Seattle.
“As shown in this model, G100 may hold potential as a treatment for lymphoma patients.”
To test that theory, Immune Design is conducting a phase 1/2 trial of G100 given with local radiation or the anti-PD-1 agent pembrolizumab to patients with follicular lymphoma. ![]()
The US Food and Drug Administration (FDA) has granted orphan designation to G100 for the treatment of follicular lymphoma.
G100 is a synthetic small-molecule toll-like receptor-4 agonist, glucopyranosyl lipid A, formulated in a stable emulsion.
The FDA grants orphan designation to drugs and biologics intended to treat, diagnose, or prevent rare diseases/disorders affecting fewer than 200,000 people in the US.
Orphan designation provides companies with certain incentives to develop products for rare diseases. This includes a 50% tax break on research and development, a fee waiver, access to federal grants, and 7 years of market exclusivity if the product is approved.
G100 is being developed by Immune Design. The company says G100 works by leveraging the activation of innate and adaptive immunity in the tumor microenvironment to create an immune response against the tumor’s pre-existing antigens.
According to Immune Design, clinical and preclinical data have demonstrated G100’s ability to activate tumor-infiltrating lymphocytes, macrophages, and dendritic cells, and promote antigen-presentation and the recruitment of T cells to the tumor.
The ensuing induction of local and systemic immune responses has been shown to result in local and abscopal tumor control in preclinical studies.
In fact, G100, when combined with local radiation, demonstrated efficacy against A20 lymphoma in mice. This research was presented in a poster at the 2016 ASH Annual Meeting (abstract 4166).
In this study, investigators evaluated the immune response and therapeutic effects of intratumoral G100 alone, local radiation alone, and concomitant G100 and local radiation in mice with A20 lymphoma.
The investigators said the combination therapy demonstrated:
- Synergistic antitumor effects in both injected as well as uninjected tumors (abscopal effects)
- Synergistic induction of pro-inflammatory cytokine and chemokine environment, as well as induction of genes governing antigen processing and presentation
- Increased infiltration of T cells, including CD4 and CD8 T cells, in treated tumors.
In contrast, tumors that received only radiation had significantly lower T-cell levels than untreated tumors.
“These findings highlight the potential beneficial effect that immunotherapy with G100 could provide when given with radiation by modulating the tumor microenvironment to generate a systemic, durable, T-cell anti-tumor response,” said study investigator Ramesh Rengan, MD, of the University of Washington in Seattle.
“As shown in this model, G100 may hold potential as a treatment for lymphoma patients.”
To test that theory, Immune Design is conducting a phase 1/2 trial of G100 given with local radiation or the anti-PD-1 agent pembrolizumab to patients with follicular lymphoma. ![]()
Factors linked to B-NHL in Palestinians, Israelis
New research has revealed factors that may increase the risk of B-cell non-Hodgkin lymphoma (B-NHL) in Israelis and Palestinians.
This large-scale, epidemiological study indicated that each group had its own unique risk factors.
However, in both groups, recreational sun exposure, black hair-dye use, a history of hospitalization for infection, and having a first-degree relative with a hematopoietic malignancy were all associated with B-NHL.
A team of Palestinian and Israeli researchers reported these findings in PLOS ONE.
The researchers noted that Israelis and Palestinians share the same ecosystem but differ in terms of lifestyle, health behaviors, and medical systems. Yet both populations report high incidences of NHL.
To gain some insight into this phenomenon, the team conducted a study examining risk factors for B-NHL and its subtypes in these two populations.
The researchers looked at medical history, environmental factors, and lifestyle factors in 823 B-NHL patients and 808 healthy controls.
There were 516 Israeli Jews with B-NHL and 307 Palestinian Arabs with B-NHL. The mean age at diagnosis was 60 and 51, respectively.
The proportion of patients with diffuse large B-cell lymphoma was 71% of Palestinian Arabs and 41% of Israeli Jews. The proportion of patients with follicular lymphoma was 14% and 28%, respectively. And the proportion of patients with marginal zone lymphoma was 2% and 14%, respectively.
Using data from questionnaires, pathology review, serology, and genotyping, the researchers uncovered potential risk factors for B-NHL common to both populations and other factors unique to each population.
Results
The data showed that, in both Palestinian Arabs and Israeli Jews, B-NHL was associated with:
- Recreational sun exposure (odds ratio [OR]=1.4)
- Black hair-dye use (OR=1.70)
- A history of hospitalization for infection (OR=1.68)
- Having a first-degree relative with a hematopoietic malignancy (OR=1.69).
Smoking was associated with follicular lymphoma in both populations (OR=1.46). And greater-than-monthly indoor pesticide use was associated with diffuse large B-cell lymphoma in both populations (OR=2.01).
There was an inverse association between alcohol use and B-NHL for both populations (OR=0.46).
Among Palestinian Arabs only, risk factors for B-NHL included gardening (OR=1.93) and a history of herpes (OR=3.73), mononucleosis (OR=6.34), rubella (OR=2.86), and blood transfusion (OR=2.53).
Risk factors that applied to Israeli Jews only included growing fruits and vegetables (OR=1.87) and self-reported autoimmune diseases (OR=1.99).
The researchers said differences in risk factors by ethnicity could reflect differences in lifestyle, medical systems, and reporting patterns, while variations by B-NHL subtypes suggest specific causal factors for different types of disease. However, these findings require further investigation to reveal their mechanisms.
“Apart from the scientific contribution that this research provides in terms of understanding risk factors for NHL, the study entails an important research cooperation among many institutions,” said study author Ora Paltiel, of Hadassah-Hebrew University Medical Organization in Jerusalem, Israel.
“The study provided opportunities for training Palestinian and Israeli researchers and will provide for intellectual interaction for years to come. The data collected will also provide a research platform for the future study of lymphoma. Epidemiologic research has the potential to improve and preserve human health, and it can also serve as a bridge to dialogue among nations.” ![]()
New research has revealed factors that may increase the risk of B-cell non-Hodgkin lymphoma (B-NHL) in Israelis and Palestinians.
This large-scale, epidemiological study indicated that each group had its own unique risk factors.
However, in both groups, recreational sun exposure, black hair-dye use, a history of hospitalization for infection, and having a first-degree relative with a hematopoietic malignancy were all associated with B-NHL.
A team of Palestinian and Israeli researchers reported these findings in PLOS ONE.
The researchers noted that Israelis and Palestinians share the same ecosystem but differ in terms of lifestyle, health behaviors, and medical systems. Yet both populations report high incidences of NHL.
To gain some insight into this phenomenon, the team conducted a study examining risk factors for B-NHL and its subtypes in these two populations.
The researchers looked at medical history, environmental factors, and lifestyle factors in 823 B-NHL patients and 808 healthy controls.
There were 516 Israeli Jews with B-NHL and 307 Palestinian Arabs with B-NHL. The mean age at diagnosis was 60 and 51, respectively.
The proportion of patients with diffuse large B-cell lymphoma was 71% of Palestinian Arabs and 41% of Israeli Jews. The proportion of patients with follicular lymphoma was 14% and 28%, respectively. And the proportion of patients with marginal zone lymphoma was 2% and 14%, respectively.
Using data from questionnaires, pathology review, serology, and genotyping, the researchers uncovered potential risk factors for B-NHL common to both populations and other factors unique to each population.
Results
The data showed that, in both Palestinian Arabs and Israeli Jews, B-NHL was associated with:
- Recreational sun exposure (odds ratio [OR]=1.4)
- Black hair-dye use (OR=1.70)
- A history of hospitalization for infection (OR=1.68)
- Having a first-degree relative with a hematopoietic malignancy (OR=1.69).
Smoking was associated with follicular lymphoma in both populations (OR=1.46). And greater-than-monthly indoor pesticide use was associated with diffuse large B-cell lymphoma in both populations (OR=2.01).
There was an inverse association between alcohol use and B-NHL for both populations (OR=0.46).
Among Palestinian Arabs only, risk factors for B-NHL included gardening (OR=1.93) and a history of herpes (OR=3.73), mononucleosis (OR=6.34), rubella (OR=2.86), and blood transfusion (OR=2.53).
Risk factors that applied to Israeli Jews only included growing fruits and vegetables (OR=1.87) and self-reported autoimmune diseases (OR=1.99).
The researchers said differences in risk factors by ethnicity could reflect differences in lifestyle, medical systems, and reporting patterns, while variations by B-NHL subtypes suggest specific causal factors for different types of disease. However, these findings require further investigation to reveal their mechanisms.
“Apart from the scientific contribution that this research provides in terms of understanding risk factors for NHL, the study entails an important research cooperation among many institutions,” said study author Ora Paltiel, of Hadassah-Hebrew University Medical Organization in Jerusalem, Israel.
“The study provided opportunities for training Palestinian and Israeli researchers and will provide for intellectual interaction for years to come. The data collected will also provide a research platform for the future study of lymphoma. Epidemiologic research has the potential to improve and preserve human health, and it can also serve as a bridge to dialogue among nations.” ![]()
New research has revealed factors that may increase the risk of B-cell non-Hodgkin lymphoma (B-NHL) in Israelis and Palestinians.
This large-scale, epidemiological study indicated that each group had its own unique risk factors.
However, in both groups, recreational sun exposure, black hair-dye use, a history of hospitalization for infection, and having a first-degree relative with a hematopoietic malignancy were all associated with B-NHL.
A team of Palestinian and Israeli researchers reported these findings in PLOS ONE.
The researchers noted that Israelis and Palestinians share the same ecosystem but differ in terms of lifestyle, health behaviors, and medical systems. Yet both populations report high incidences of NHL.
To gain some insight into this phenomenon, the team conducted a study examining risk factors for B-NHL and its subtypes in these two populations.
The researchers looked at medical history, environmental factors, and lifestyle factors in 823 B-NHL patients and 808 healthy controls.
There were 516 Israeli Jews with B-NHL and 307 Palestinian Arabs with B-NHL. The mean age at diagnosis was 60 and 51, respectively.
The proportion of patients with diffuse large B-cell lymphoma was 71% of Palestinian Arabs and 41% of Israeli Jews. The proportion of patients with follicular lymphoma was 14% and 28%, respectively. And the proportion of patients with marginal zone lymphoma was 2% and 14%, respectively.
Using data from questionnaires, pathology review, serology, and genotyping, the researchers uncovered potential risk factors for B-NHL common to both populations and other factors unique to each population.
Results
The data showed that, in both Palestinian Arabs and Israeli Jews, B-NHL was associated with:
- Recreational sun exposure (odds ratio [OR]=1.4)
- Black hair-dye use (OR=1.70)
- A history of hospitalization for infection (OR=1.68)
- Having a first-degree relative with a hematopoietic malignancy (OR=1.69).
Smoking was associated with follicular lymphoma in both populations (OR=1.46). And greater-than-monthly indoor pesticide use was associated with diffuse large B-cell lymphoma in both populations (OR=2.01).
There was an inverse association between alcohol use and B-NHL for both populations (OR=0.46).
Among Palestinian Arabs only, risk factors for B-NHL included gardening (OR=1.93) and a history of herpes (OR=3.73), mononucleosis (OR=6.34), rubella (OR=2.86), and blood transfusion (OR=2.53).
Risk factors that applied to Israeli Jews only included growing fruits and vegetables (OR=1.87) and self-reported autoimmune diseases (OR=1.99).
The researchers said differences in risk factors by ethnicity could reflect differences in lifestyle, medical systems, and reporting patterns, while variations by B-NHL subtypes suggest specific causal factors for different types of disease. However, these findings require further investigation to reveal their mechanisms.
“Apart from the scientific contribution that this research provides in terms of understanding risk factors for NHL, the study entails an important research cooperation among many institutions,” said study author Ora Paltiel, of Hadassah-Hebrew University Medical Organization in Jerusalem, Israel.
“The study provided opportunities for training Palestinian and Israeli researchers and will provide for intellectual interaction for years to come. The data collected will also provide a research platform for the future study of lymphoma. Epidemiologic research has the potential to improve and preserve human health, and it can also serve as a bridge to dialogue among nations.” ![]()
European Commission approves rituximab biosimilar
The European Commission has approved a biosimilar rituximab product, Truxima™, for all the same indications as the reference product, MabThera.
This means Truxima (formerly called CT-P10) is approved for use in the European Union to treat patients with non-Hodgkin lymphoma, chronic lymphocytic leukemia, rheumatoid arthritis (RA), granulomatosis with polyangiitis (GPA), and microscopic polyangiitis (MPA).
Truxima, a product of Celltrion Healthcare Hungary Kft, is the first biosimilar monoclonal antibody approved in an oncology indication worldwide.
The approval is based on data submitted to the European Medicines Agency.
The agency’s Committee for Medicinal Products for Human Use (CHMP) said the evidence suggests Truxima and MabThera are similar in terms of efficacy, safety, immunogenicity, pharmacodynamics, and pharmacokinetics in patients with RA and advanced follicular lymphoma (FL).
Therefore, the European Commission approved Truxima for the following indications.
Non-Hodgkin lymphoma
Truxima is indicated for use in combination with chemotherapy to treat previously untreated patients with stage III-IV FL.
Truxima maintenance therapy is indicated for the treatment of FL patients responding to induction therapy.
Truxima monotherapy is indicated for the treatment of patients with stage III-IV FL who are chemo-resistant or are in their second or subsequent relapse after chemotherapy.
Truxima is indicated for use in combination with CHOP (cyclophosphamide, doxorubicin, vincristine, and prednisolone) for the treatment of patients with CD20-positive diffuse large B-cell lymphoma.
Chronic lymphocytic leukemia
Truxima in combination with chemotherapy is indicated for the treatment of patients with previously untreated and relapsed/refractory chronic lymphocytic leukemia.
The CHMP noted that limited efficacy and safety data are available for patients previously treated with monoclonal antibodies, including rituximab, or patients who are refractory to previous rituximab plus chemotherapy.
RA, GPA, and MPA
Truxima in combination with methotrexate is indicated for the treatment of adults with severe, active RA who have had an inadequate response to or cannot tolerate other disease-modifying anti-rheumatic drugs, including one or more tumor necrosis factor inhibitor therapies.
Truxima in combination with glucocorticoids is indicated for the induction of remission in adults with severe, active GPA or MPA.
Truxima studies
There are 3 ongoing, phase 3 trials of Truxima in patients with RA (NCT02149121), advanced FL (NCT02162771), and low-tumor-burden FL (NCT02260804).
Results from the phase 1/3 trial in patients with newly diagnosed, advanced FL suggest that Truxima and the reference rituximab are similar with regard to pharmacokinetics, immunogenicity, and safety (B Coiffier et al. ASH 2016, abstract 1807).
Results from the phase 3 study of RA patients indicate that Truxima is similar to reference products (EU and US-sourced rituximab) with regard to pharmacodynamics, safety, and efficacy for up to 24 weeks (DH Yoo et al. 2016 ACR/ARHP Annual Meeting, abstract 1635). ![]()
The European Commission has approved a biosimilar rituximab product, Truxima™, for all the same indications as the reference product, MabThera.
This means Truxima (formerly called CT-P10) is approved for use in the European Union to treat patients with non-Hodgkin lymphoma, chronic lymphocytic leukemia, rheumatoid arthritis (RA), granulomatosis with polyangiitis (GPA), and microscopic polyangiitis (MPA).
Truxima, a product of Celltrion Healthcare Hungary Kft, is the first biosimilar monoclonal antibody approved in an oncology indication worldwide.
The approval is based on data submitted to the European Medicines Agency.
The agency’s Committee for Medicinal Products for Human Use (CHMP) said the evidence suggests Truxima and MabThera are similar in terms of efficacy, safety, immunogenicity, pharmacodynamics, and pharmacokinetics in patients with RA and advanced follicular lymphoma (FL).
Therefore, the European Commission approved Truxima for the following indications.
Non-Hodgkin lymphoma
Truxima is indicated for use in combination with chemotherapy to treat previously untreated patients with stage III-IV FL.
Truxima maintenance therapy is indicated for the treatment of FL patients responding to induction therapy.
Truxima monotherapy is indicated for the treatment of patients with stage III-IV FL who are chemo-resistant or are in their second or subsequent relapse after chemotherapy.
Truxima is indicated for use in combination with CHOP (cyclophosphamide, doxorubicin, vincristine, and prednisolone) for the treatment of patients with CD20-positive diffuse large B-cell lymphoma.
Chronic lymphocytic leukemia
Truxima in combination with chemotherapy is indicated for the treatment of patients with previously untreated and relapsed/refractory chronic lymphocytic leukemia.
The CHMP noted that limited efficacy and safety data are available for patients previously treated with monoclonal antibodies, including rituximab, or patients who are refractory to previous rituximab plus chemotherapy.
RA, GPA, and MPA
Truxima in combination with methotrexate is indicated for the treatment of adults with severe, active RA who have had an inadequate response to or cannot tolerate other disease-modifying anti-rheumatic drugs, including one or more tumor necrosis factor inhibitor therapies.
Truxima in combination with glucocorticoids is indicated for the induction of remission in adults with severe, active GPA or MPA.
Truxima studies
There are 3 ongoing, phase 3 trials of Truxima in patients with RA (NCT02149121), advanced FL (NCT02162771), and low-tumor-burden FL (NCT02260804).
Results from the phase 1/3 trial in patients with newly diagnosed, advanced FL suggest that Truxima and the reference rituximab are similar with regard to pharmacokinetics, immunogenicity, and safety (B Coiffier et al. ASH 2016, abstract 1807).
Results from the phase 3 study of RA patients indicate that Truxima is similar to reference products (EU and US-sourced rituximab) with regard to pharmacodynamics, safety, and efficacy for up to 24 weeks (DH Yoo et al. 2016 ACR/ARHP Annual Meeting, abstract 1635). ![]()
The European Commission has approved a biosimilar rituximab product, Truxima™, for all the same indications as the reference product, MabThera.
This means Truxima (formerly called CT-P10) is approved for use in the European Union to treat patients with non-Hodgkin lymphoma, chronic lymphocytic leukemia, rheumatoid arthritis (RA), granulomatosis with polyangiitis (GPA), and microscopic polyangiitis (MPA).
Truxima, a product of Celltrion Healthcare Hungary Kft, is the first biosimilar monoclonal antibody approved in an oncology indication worldwide.
The approval is based on data submitted to the European Medicines Agency.
The agency’s Committee for Medicinal Products for Human Use (CHMP) said the evidence suggests Truxima and MabThera are similar in terms of efficacy, safety, immunogenicity, pharmacodynamics, and pharmacokinetics in patients with RA and advanced follicular lymphoma (FL).
Therefore, the European Commission approved Truxima for the following indications.
Non-Hodgkin lymphoma
Truxima is indicated for use in combination with chemotherapy to treat previously untreated patients with stage III-IV FL.
Truxima maintenance therapy is indicated for the treatment of FL patients responding to induction therapy.
Truxima monotherapy is indicated for the treatment of patients with stage III-IV FL who are chemo-resistant or are in their second or subsequent relapse after chemotherapy.
Truxima is indicated for use in combination with CHOP (cyclophosphamide, doxorubicin, vincristine, and prednisolone) for the treatment of patients with CD20-positive diffuse large B-cell lymphoma.
Chronic lymphocytic leukemia
Truxima in combination with chemotherapy is indicated for the treatment of patients with previously untreated and relapsed/refractory chronic lymphocytic leukemia.
The CHMP noted that limited efficacy and safety data are available for patients previously treated with monoclonal antibodies, including rituximab, or patients who are refractory to previous rituximab plus chemotherapy.
RA, GPA, and MPA
Truxima in combination with methotrexate is indicated for the treatment of adults with severe, active RA who have had an inadequate response to or cannot tolerate other disease-modifying anti-rheumatic drugs, including one or more tumor necrosis factor inhibitor therapies.
Truxima in combination with glucocorticoids is indicated for the induction of remission in adults with severe, active GPA or MPA.
Truxima studies
There are 3 ongoing, phase 3 trials of Truxima in patients with RA (NCT02149121), advanced FL (NCT02162771), and low-tumor-burden FL (NCT02260804).
Results from the phase 1/3 trial in patients with newly diagnosed, advanced FL suggest that Truxima and the reference rituximab are similar with regard to pharmacokinetics, immunogenicity, and safety (B Coiffier et al. ASH 2016, abstract 1807).
Results from the phase 3 study of RA patients indicate that Truxima is similar to reference products (EU and US-sourced rituximab) with regard to pharmacodynamics, safety, and efficacy for up to 24 weeks (DH Yoo et al. 2016 ACR/ARHP Annual Meeting, abstract 1635). ![]()
Immunotherapy receives fast track designation
The US Food and Drug Administration (FDA) has granted fast track designation to CMD-003 (baltaleucel-T) for patients with relapsed/refractory lymphoma and post-transplant lymphoproliferative disease associated with Epstein-Barr virus (EBV).
CMD-003 consists of patient-derived T cells that have been activated to kill malignant cells expressing antigens associated with EBV.
The T cells specifically target 4 EBV epitopes—LMP1, LMP2, EBNA, and BARF1.
CMD-003 is being developed by Cell Medica and the Baylor College of Medicine with funding provided, in part, by the Cancer Prevention and Research Institute of Texas.
About fast track designation
The FDA’s fast track program is designed to facilitate the development and expedite the review of products intended to treat or prevent serious or life-threatening conditions and address unmet medical need.
Through the FDA’s fast track program, a product may be eligible for priority review. In addition, the company developing the product may be allowed to submit sections of the biologic license application or new drug application on a rolling basis as data become available.
Fast track designation also provides the company with opportunities for more frequent meetings and written communications with the FDA.
CMD-003-related research
CMD-003 is currently under investigation in the phase 2 CITADEL trial for patients with extranodal natural killer T-cell lymphoma and the phase 2 CIVIC trial for patients with EBV-associated diffuse large B-cell lymphoma, Hodgkin lymphoma, and post-transplant lymphoproliferative disease.
Researchers have not published results from any trials of CMD-003, but they have published results with EBV-specific T-cell products related to CMD-003.
In one study, published in the Journal of Clinical Oncology in 2014, researchers administered cytotoxic T lymphocytes (CTLs) in 50 patients with EBV-associated Hodgkin or non-Hodgkin lymphoma.
Twenty-nine of the patients were in remission when they received CTL infusions, but they were at a high risk of relapse. The remaining 21 patients had relapsed or refractory disease at the time of CTL infusion.
Twenty-seven of the patients who received CTLs as an adjuvant treatment remained in remission at 3.1 years after treatment.
Their 2-year event-free survival rate was 82%. None of the patients died of lymphoma, but 9 died from complications associated with the chemotherapy and radiation they had received.
Of the 21 patients with relapsed or refractory disease, 13 responded to CTL infusions, and 11 patients achieved a complete response. In this group, the 2-year event-free survival rate was about 50%.
The researchers said there were no toxicities that were definitively related to CTL infusion.
One patient had central nervous system deterioration 2 weeks after infusion. This was attributed to disease progression but could possibly have been treatment-related.
Another patient developed respiratory complications about 4 weeks after a second CTL infusion that may have been treatment-related. However, the researchers attributed it to an intercurrent infection, and the patient made a complete recovery.
The US Food and Drug Administration (FDA) has granted fast track designation to CMD-003 (baltaleucel-T) for patients with relapsed/refractory lymphoma and post-transplant lymphoproliferative disease associated with Epstein-Barr virus (EBV).
CMD-003 consists of patient-derived T cells that have been activated to kill malignant cells expressing antigens associated with EBV.
The T cells specifically target 4 EBV epitopes—LMP1, LMP2, EBNA, and BARF1.
CMD-003 is being developed by Cell Medica and the Baylor College of Medicine with funding provided, in part, by the Cancer Prevention and Research Institute of Texas.
About fast track designation
The FDA’s fast track program is designed to facilitate the development and expedite the review of products intended to treat or prevent serious or life-threatening conditions and address unmet medical need.
Through the FDA’s fast track program, a product may be eligible for priority review. In addition, the company developing the product may be allowed to submit sections of the biologic license application or new drug application on a rolling basis as data become available.
Fast track designation also provides the company with opportunities for more frequent meetings and written communications with the FDA.
CMD-003-related research
CMD-003 is currently under investigation in the phase 2 CITADEL trial for patients with extranodal natural killer T-cell lymphoma and the phase 2 CIVIC trial for patients with EBV-associated diffuse large B-cell lymphoma, Hodgkin lymphoma, and post-transplant lymphoproliferative disease.
Researchers have not published results from any trials of CMD-003, but they have published results with EBV-specific T-cell products related to CMD-003.
In one study, published in the Journal of Clinical Oncology in 2014, researchers administered cytotoxic T lymphocytes (CTLs) in 50 patients with EBV-associated Hodgkin or non-Hodgkin lymphoma.
Twenty-nine of the patients were in remission when they received CTL infusions, but they were at a high risk of relapse. The remaining 21 patients had relapsed or refractory disease at the time of CTL infusion.
Twenty-seven of the patients who received CTLs as an adjuvant treatment remained in remission at 3.1 years after treatment.
Their 2-year event-free survival rate was 82%. None of the patients died of lymphoma, but 9 died from complications associated with the chemotherapy and radiation they had received.
Of the 21 patients with relapsed or refractory disease, 13 responded to CTL infusions, and 11 patients achieved a complete response. In this group, the 2-year event-free survival rate was about 50%.
The researchers said there were no toxicities that were definitively related to CTL infusion.
One patient had central nervous system deterioration 2 weeks after infusion. This was attributed to disease progression but could possibly have been treatment-related.
Another patient developed respiratory complications about 4 weeks after a second CTL infusion that may have been treatment-related. However, the researchers attributed it to an intercurrent infection, and the patient made a complete recovery.
The US Food and Drug Administration (FDA) has granted fast track designation to CMD-003 (baltaleucel-T) for patients with relapsed/refractory lymphoma and post-transplant lymphoproliferative disease associated with Epstein-Barr virus (EBV).
CMD-003 consists of patient-derived T cells that have been activated to kill malignant cells expressing antigens associated with EBV.
The T cells specifically target 4 EBV epitopes—LMP1, LMP2, EBNA, and BARF1.
CMD-003 is being developed by Cell Medica and the Baylor College of Medicine with funding provided, in part, by the Cancer Prevention and Research Institute of Texas.
About fast track designation
The FDA’s fast track program is designed to facilitate the development and expedite the review of products intended to treat or prevent serious or life-threatening conditions and address unmet medical need.
Through the FDA’s fast track program, a product may be eligible for priority review. In addition, the company developing the product may be allowed to submit sections of the biologic license application or new drug application on a rolling basis as data become available.
Fast track designation also provides the company with opportunities for more frequent meetings and written communications with the FDA.
CMD-003-related research
CMD-003 is currently under investigation in the phase 2 CITADEL trial for patients with extranodal natural killer T-cell lymphoma and the phase 2 CIVIC trial for patients with EBV-associated diffuse large B-cell lymphoma, Hodgkin lymphoma, and post-transplant lymphoproliferative disease.
Researchers have not published results from any trials of CMD-003, but they have published results with EBV-specific T-cell products related to CMD-003.
In one study, published in the Journal of Clinical Oncology in 2014, researchers administered cytotoxic T lymphocytes (CTLs) in 50 patients with EBV-associated Hodgkin or non-Hodgkin lymphoma.
Twenty-nine of the patients were in remission when they received CTL infusions, but they were at a high risk of relapse. The remaining 21 patients had relapsed or refractory disease at the time of CTL infusion.
Twenty-seven of the patients who received CTLs as an adjuvant treatment remained in remission at 3.1 years after treatment.
Their 2-year event-free survival rate was 82%. None of the patients died of lymphoma, but 9 died from complications associated with the chemotherapy and radiation they had received.
Of the 21 patients with relapsed or refractory disease, 13 responded to CTL infusions, and 11 patients achieved a complete response. In this group, the 2-year event-free survival rate was about 50%.
The researchers said there were no toxicities that were definitively related to CTL infusion.
One patient had central nervous system deterioration 2 weeks after infusion. This was attributed to disease progression but could possibly have been treatment-related.
Another patient developed respiratory complications about 4 weeks after a second CTL infusion that may have been treatment-related. However, the researchers attributed it to an intercurrent infection, and the patient made a complete recovery.
Proximity to oil, gas wells linked to ALL

A pumpjack is used to lift
liquid from an oil well.
Photo by Eric Kounce
Living in an area of high-density oil and gas development may increase a young person’s risk of developing acute lymphoblastic leukemia (ALL), according to research published in PLOS ONE.
The study showed that children and young adults in Colorado who had been diagnosed with ALL were more likely than young people with non-hematologic cancers to live in areas of high-density oil and gas development.
However, there was no such association for young people with non-Hodgkin lymphoma (NHL).
“Over 378,000 Coloradans and millions of Americans currently live within a mile of at least one oil and gas well, and petroleum development continues to expand into residential areas,” said study author Lisa McKenzie, PhD, of the University of Colorado Anschutz Campus in Aurora.
“The findings from our registry-based, case-control study indicate that young Coloradans diagnosed with one type of childhood leukemia are more likely to live in the densest areas of oil and gas sites. More comprehensive research that can address our study’s limitations is needed to understand and explain these results.”
Dr McKenzie and her colleagues said they conducted this study because oil and gas development emits known hematological carcinogens, such as benzene, and increasingly occurs in residential areas.
The team wanted to determine whether living near areas of oil and gas development was associated with risk for hematologic cancers. So they analyzed data from the Colorado Central Cancer Registry and the Colorado Oil and Gas Information System.
The study included 743 subjects, ages 0 to 24, living in rural Colorado and diagnosed with cancer between 2001 and 2013. This included 87 ALL cases, 50 NHL cases, and 528 controls with non-hematologic cancers. (Other hematologic malignancies were not included in the analysis due to small numbers.)
Data analysis
The researchers used information from the Colorado Oil and Gas Information System to build a geocoded dataset with coordinates of all oil and gas wells in rural Colorado and determined dates for when each well was active.
Geocoded residential addresses of cancer patients at the time of diagnosis were linked to active well locations in the year of diagnosis and active well locations in each of the 10 years preceding the cancer diagnosis.
The researchers then took the inverse of each distance and summed the inverse distances to calculate inverse distance weighted (IDW) oil and gas well counts within a 16.1 km radius of each participant’s residence at cancer diagnosis for each of the 10 years prior to the date of diagnosis. (The IDW well count method gives greater weight to the wells nearer the home.)
The team used logistic regression to estimate associations for cancers across IDW well count tertiles. The first tertile had less than 4.9 wells per 1.6 km, the second had 4.9 to 33.6 wells per 1.6 km, and the third had more than 33.6 wells per 1.6 km.
Results
The researchers found an increase in the odds of living near oil and gas development at the time of ALL diagnosis, even after adjusting for age, race, gender, income, elevation, and year of cancer diagnosis.
ALL patients ages 0 to 24 were twice as likely as controls to live in the densest area of active oil and gas wells (highest IDW well count tertile).
ALL patients ages 5 to 24 were 4.6 times more likely than controls to live in areas included in the highest IDW well count tertile.
However, there was no significant association between ALL and proximity to oil and gas development in ALL patients ages 0 to 4. The adjusted odds ratio was 0.51 for the highest IDW well count tertile.
Likewise, there were no significant associations between density of oil and gas development and NHL. The adjusted odds ratio was 0.99 for the highest IDW well count tertile.
Limitations and next steps
The researchers said this study was limited by the low occurrence of ALL and NHL in rural Colorado, lack of specific age at cancer diagnosis, and the fact that all study participants had been diagnosed with cancer.
In addition, the study was limited by the lack of information on specific activities at the well sites, place of residence before cancer diagnosis, other sources of pollution around the residence, and individual characteristics such as common infections and family history of cancer.
The team said future research should incorporate information on oil and gas development activities and production levels, as well as levels of specific pollutants of interest such as benzene, near homes, schools, and day care centers.
They recommended that such research consider specific ages and residential histories, compare cases to controls without cancer, and address other potential confounders and and environmental stressors. ![]()

A pumpjack is used to lift
liquid from an oil well.
Photo by Eric Kounce
Living in an area of high-density oil and gas development may increase a young person’s risk of developing acute lymphoblastic leukemia (ALL), according to research published in PLOS ONE.
The study showed that children and young adults in Colorado who had been diagnosed with ALL were more likely than young people with non-hematologic cancers to live in areas of high-density oil and gas development.
However, there was no such association for young people with non-Hodgkin lymphoma (NHL).
“Over 378,000 Coloradans and millions of Americans currently live within a mile of at least one oil and gas well, and petroleum development continues to expand into residential areas,” said study author Lisa McKenzie, PhD, of the University of Colorado Anschutz Campus in Aurora.
“The findings from our registry-based, case-control study indicate that young Coloradans diagnosed with one type of childhood leukemia are more likely to live in the densest areas of oil and gas sites. More comprehensive research that can address our study’s limitations is needed to understand and explain these results.”
Dr McKenzie and her colleagues said they conducted this study because oil and gas development emits known hematological carcinogens, such as benzene, and increasingly occurs in residential areas.
The team wanted to determine whether living near areas of oil and gas development was associated with risk for hematologic cancers. So they analyzed data from the Colorado Central Cancer Registry and the Colorado Oil and Gas Information System.
The study included 743 subjects, ages 0 to 24, living in rural Colorado and diagnosed with cancer between 2001 and 2013. This included 87 ALL cases, 50 NHL cases, and 528 controls with non-hematologic cancers. (Other hematologic malignancies were not included in the analysis due to small numbers.)
Data analysis
The researchers used information from the Colorado Oil and Gas Information System to build a geocoded dataset with coordinates of all oil and gas wells in rural Colorado and determined dates for when each well was active.
Geocoded residential addresses of cancer patients at the time of diagnosis were linked to active well locations in the year of diagnosis and active well locations in each of the 10 years preceding the cancer diagnosis.
The researchers then took the inverse of each distance and summed the inverse distances to calculate inverse distance weighted (IDW) oil and gas well counts within a 16.1 km radius of each participant’s residence at cancer diagnosis for each of the 10 years prior to the date of diagnosis. (The IDW well count method gives greater weight to the wells nearer the home.)
The team used logistic regression to estimate associations for cancers across IDW well count tertiles. The first tertile had less than 4.9 wells per 1.6 km, the second had 4.9 to 33.6 wells per 1.6 km, and the third had more than 33.6 wells per 1.6 km.
Results
The researchers found an increase in the odds of living near oil and gas development at the time of ALL diagnosis, even after adjusting for age, race, gender, income, elevation, and year of cancer diagnosis.
ALL patients ages 0 to 24 were twice as likely as controls to live in the densest area of active oil and gas wells (highest IDW well count tertile).
ALL patients ages 5 to 24 were 4.6 times more likely than controls to live in areas included in the highest IDW well count tertile.
However, there was no significant association between ALL and proximity to oil and gas development in ALL patients ages 0 to 4. The adjusted odds ratio was 0.51 for the highest IDW well count tertile.
Likewise, there were no significant associations between density of oil and gas development and NHL. The adjusted odds ratio was 0.99 for the highest IDW well count tertile.
Limitations and next steps
The researchers said this study was limited by the low occurrence of ALL and NHL in rural Colorado, lack of specific age at cancer diagnosis, and the fact that all study participants had been diagnosed with cancer.
In addition, the study was limited by the lack of information on specific activities at the well sites, place of residence before cancer diagnosis, other sources of pollution around the residence, and individual characteristics such as common infections and family history of cancer.
The team said future research should incorporate information on oil and gas development activities and production levels, as well as levels of specific pollutants of interest such as benzene, near homes, schools, and day care centers.
They recommended that such research consider specific ages and residential histories, compare cases to controls without cancer, and address other potential confounders and and environmental stressors. ![]()

A pumpjack is used to lift
liquid from an oil well.
Photo by Eric Kounce
Living in an area of high-density oil and gas development may increase a young person’s risk of developing acute lymphoblastic leukemia (ALL), according to research published in PLOS ONE.
The study showed that children and young adults in Colorado who had been diagnosed with ALL were more likely than young people with non-hematologic cancers to live in areas of high-density oil and gas development.
However, there was no such association for young people with non-Hodgkin lymphoma (NHL).
“Over 378,000 Coloradans and millions of Americans currently live within a mile of at least one oil and gas well, and petroleum development continues to expand into residential areas,” said study author Lisa McKenzie, PhD, of the University of Colorado Anschutz Campus in Aurora.
“The findings from our registry-based, case-control study indicate that young Coloradans diagnosed with one type of childhood leukemia are more likely to live in the densest areas of oil and gas sites. More comprehensive research that can address our study’s limitations is needed to understand and explain these results.”
Dr McKenzie and her colleagues said they conducted this study because oil and gas development emits known hematological carcinogens, such as benzene, and increasingly occurs in residential areas.
The team wanted to determine whether living near areas of oil and gas development was associated with risk for hematologic cancers. So they analyzed data from the Colorado Central Cancer Registry and the Colorado Oil and Gas Information System.
The study included 743 subjects, ages 0 to 24, living in rural Colorado and diagnosed with cancer between 2001 and 2013. This included 87 ALL cases, 50 NHL cases, and 528 controls with non-hematologic cancers. (Other hematologic malignancies were not included in the analysis due to small numbers.)
Data analysis
The researchers used information from the Colorado Oil and Gas Information System to build a geocoded dataset with coordinates of all oil and gas wells in rural Colorado and determined dates for when each well was active.
Geocoded residential addresses of cancer patients at the time of diagnosis were linked to active well locations in the year of diagnosis and active well locations in each of the 10 years preceding the cancer diagnosis.
The researchers then took the inverse of each distance and summed the inverse distances to calculate inverse distance weighted (IDW) oil and gas well counts within a 16.1 km radius of each participant’s residence at cancer diagnosis for each of the 10 years prior to the date of diagnosis. (The IDW well count method gives greater weight to the wells nearer the home.)
The team used logistic regression to estimate associations for cancers across IDW well count tertiles. The first tertile had less than 4.9 wells per 1.6 km, the second had 4.9 to 33.6 wells per 1.6 km, and the third had more than 33.6 wells per 1.6 km.
Results
The researchers found an increase in the odds of living near oil and gas development at the time of ALL diagnosis, even after adjusting for age, race, gender, income, elevation, and year of cancer diagnosis.
ALL patients ages 0 to 24 were twice as likely as controls to live in the densest area of active oil and gas wells (highest IDW well count tertile).
ALL patients ages 5 to 24 were 4.6 times more likely than controls to live in areas included in the highest IDW well count tertile.
However, there was no significant association between ALL and proximity to oil and gas development in ALL patients ages 0 to 4. The adjusted odds ratio was 0.51 for the highest IDW well count tertile.
Likewise, there were no significant associations between density of oil and gas development and NHL. The adjusted odds ratio was 0.99 for the highest IDW well count tertile.
Limitations and next steps
The researchers said this study was limited by the low occurrence of ALL and NHL in rural Colorado, lack of specific age at cancer diagnosis, and the fact that all study participants had been diagnosed with cancer.
In addition, the study was limited by the lack of information on specific activities at the well sites, place of residence before cancer diagnosis, other sources of pollution around the residence, and individual characteristics such as common infections and family history of cancer.
The team said future research should incorporate information on oil and gas development activities and production levels, as well as levels of specific pollutants of interest such as benzene, near homes, schools, and day care centers.
They recommended that such research consider specific ages and residential histories, compare cases to controls without cancer, and address other potential confounders and and environmental stressors. ![]()
Drug produces high response rates in AITL

Photo by Larry Young
SAN FRANCISCO—Treatment with 5-azacitidine (5-AZA) can produce a high response rate in patients with relapsed/refractory angioimmunoblastic T-cell lymphoma (AITL), according to a small study.
The overall response rate (ORR) among AITL patients was 75%, and the complete response (CR) rate was 42%.
However, this study also included patients with other types of peripheral T-cell lymphoma (PTCL), and most of these patients did not respond to 5-AZA.
Richard Delarue, MD, of Necker University Hospital in Paris, France, presented these results at the 9th Annual T-cell Lymphoma Forum.
Results were also presented at the 2016 ASH Annual Meeting (abstract 4164). Dr Delarue reported receiving honoraria from Celgene.
Patients
The study included 19 patients with relapsed/refractory PTCL. Twelve patients had AITL, 3 had adult T-cell leukemia/lymphoma (ATLL), 2 had PTCL not otherwise specified, 1 had enteropathy-associated T-cell lymphoma, and 1 had transformed mycosis fungoides.
At diagnosis, the median age was 71 (range, 39-85) for AITL patients and 59 (range, 32-83) for the other PTCL patients. Seventy-five percent of AITL patients had an IPI score of 3 to 5 and a PIT score of 3 to 4. Eighty-six percent of the other PTCL patients had an IPI score of 3 to 5, and 57% had a PIT score of 3 to 4.
At the time of 5-AZA treatment, all patients had stage III/IV disease. The AITL patients had received a median of 2 (range, 0-6) prior lines of therapy, and the other PTCL patients had received a median of 3 (range, 0-7).
Two patients did not receive chemotherapy before 5-AZA because of the presence of associated chronic myelomonocytic leukemia (CMML) that required treatment first.
Ninety-two percent of AITL patients had TET2 mutations (n=11), 33% had DNMT3A mutations (n=4), and 0% had IDH2 mutations. One of the non-AITL patients had a TET2 mutation.
Treatment
Patients received a subcutaneous injection of 5-AZA at 75 mg/m² for 7 consecutive days every 28 days until progression or unacceptable toxicity. Six patients also received 4 to 8 infusions of rituximab because of EBV-DNA positivity.
The patients received a median of 3 cycles of 5-AZA. At the time of analysis, 4 patients were still receiving therapy.
The median follow-up was 84 days (range, 19 to 1236).
Toxicity
“Hematological toxicity was as expected with 5-azacitidine,” Dr Delarue said.
However, 2 patients had “unusual” adverse reactions. One patient had grade 2 polyneuropathy, which was considered related to a paraneoplastic syndrome.
The other patient had grade 3 diarrhea related to colitis of unknown origin, and this led to treatment interruption.
There were no treatment-related deaths.
Efficacy
Dr Delarue noted that the ORR was significantly higher in AITL patients than in patients with the other PTCL subtypes (P=0.0198).
The ORR was 53% in the entire cohort (10/19), 75% (9/12) among AITL patients, and 14% among patients with other PTCLs (1/7).
“The only patient with a response in the ‘other PTCL’ group was a patient with HTLV1-associated ATLL . . . , but he relapsed a couple of weeks after the second cycle,” Dr Delarue explained.
Among the AITL patients, the CR rate was 42% (5/12), the partial response rate was 33% (4/12), and the rate of stable disease was 25% (3/12).
Six AITL patients eventually progressed—after 2, 2, 3, 4, 4, and 20 cycles of therapy, respectively.
Two AITL patients are off therapy but remain in CR after 9 and 10 months (5 and 6 cycles of treatment), respectively.
The median progression-free survival for AITL patients was 16 months, and the median overall survival was 17 months.
Dr DeLarue noted that 4 of the AITL patients had CMML, 1 had non-CMML myelodysplastic syndrome, 3 had monocytosis without CMML, and 4 had normal monocyte counts.
He also said that, at present, it’s not possible to correlate the results observed in the AITL patients with their mutational status.
However, he and his colleagues are planning a prospective study of 5-AZA in patients with relapsed/refractory AITL and T follicular helper cell PTCL not otherwise specified. 5-AZA will be compared to investigator’s choice in this study.
Dr DeLarue said this trial will provide an opportunity to use the new oral formulation of 5-AZA (CC-486). And he and his colleagues welcome collaborators. ![]()

Photo by Larry Young
SAN FRANCISCO—Treatment with 5-azacitidine (5-AZA) can produce a high response rate in patients with relapsed/refractory angioimmunoblastic T-cell lymphoma (AITL), according to a small study.
The overall response rate (ORR) among AITL patients was 75%, and the complete response (CR) rate was 42%.
However, this study also included patients with other types of peripheral T-cell lymphoma (PTCL), and most of these patients did not respond to 5-AZA.
Richard Delarue, MD, of Necker University Hospital in Paris, France, presented these results at the 9th Annual T-cell Lymphoma Forum.
Results were also presented at the 2016 ASH Annual Meeting (abstract 4164). Dr Delarue reported receiving honoraria from Celgene.
Patients
The study included 19 patients with relapsed/refractory PTCL. Twelve patients had AITL, 3 had adult T-cell leukemia/lymphoma (ATLL), 2 had PTCL not otherwise specified, 1 had enteropathy-associated T-cell lymphoma, and 1 had transformed mycosis fungoides.
At diagnosis, the median age was 71 (range, 39-85) for AITL patients and 59 (range, 32-83) for the other PTCL patients. Seventy-five percent of AITL patients had an IPI score of 3 to 5 and a PIT score of 3 to 4. Eighty-six percent of the other PTCL patients had an IPI score of 3 to 5, and 57% had a PIT score of 3 to 4.
At the time of 5-AZA treatment, all patients had stage III/IV disease. The AITL patients had received a median of 2 (range, 0-6) prior lines of therapy, and the other PTCL patients had received a median of 3 (range, 0-7).
Two patients did not receive chemotherapy before 5-AZA because of the presence of associated chronic myelomonocytic leukemia (CMML) that required treatment first.
Ninety-two percent of AITL patients had TET2 mutations (n=11), 33% had DNMT3A mutations (n=4), and 0% had IDH2 mutations. One of the non-AITL patients had a TET2 mutation.
Treatment
Patients received a subcutaneous injection of 5-AZA at 75 mg/m² for 7 consecutive days every 28 days until progression or unacceptable toxicity. Six patients also received 4 to 8 infusions of rituximab because of EBV-DNA positivity.
The patients received a median of 3 cycles of 5-AZA. At the time of analysis, 4 patients were still receiving therapy.
The median follow-up was 84 days (range, 19 to 1236).
Toxicity
“Hematological toxicity was as expected with 5-azacitidine,” Dr Delarue said.
However, 2 patients had “unusual” adverse reactions. One patient had grade 2 polyneuropathy, which was considered related to a paraneoplastic syndrome.
The other patient had grade 3 diarrhea related to colitis of unknown origin, and this led to treatment interruption.
There were no treatment-related deaths.
Efficacy
Dr Delarue noted that the ORR was significantly higher in AITL patients than in patients with the other PTCL subtypes (P=0.0198).
The ORR was 53% in the entire cohort (10/19), 75% (9/12) among AITL patients, and 14% among patients with other PTCLs (1/7).
“The only patient with a response in the ‘other PTCL’ group was a patient with HTLV1-associated ATLL . . . , but he relapsed a couple of weeks after the second cycle,” Dr Delarue explained.
Among the AITL patients, the CR rate was 42% (5/12), the partial response rate was 33% (4/12), and the rate of stable disease was 25% (3/12).
Six AITL patients eventually progressed—after 2, 2, 3, 4, 4, and 20 cycles of therapy, respectively.
Two AITL patients are off therapy but remain in CR after 9 and 10 months (5 and 6 cycles of treatment), respectively.
The median progression-free survival for AITL patients was 16 months, and the median overall survival was 17 months.
Dr DeLarue noted that 4 of the AITL patients had CMML, 1 had non-CMML myelodysplastic syndrome, 3 had monocytosis without CMML, and 4 had normal monocyte counts.
He also said that, at present, it’s not possible to correlate the results observed in the AITL patients with their mutational status.
However, he and his colleagues are planning a prospective study of 5-AZA in patients with relapsed/refractory AITL and T follicular helper cell PTCL not otherwise specified. 5-AZA will be compared to investigator’s choice in this study.
Dr DeLarue said this trial will provide an opportunity to use the new oral formulation of 5-AZA (CC-486). And he and his colleagues welcome collaborators. ![]()

Photo by Larry Young
SAN FRANCISCO—Treatment with 5-azacitidine (5-AZA) can produce a high response rate in patients with relapsed/refractory angioimmunoblastic T-cell lymphoma (AITL), according to a small study.
The overall response rate (ORR) among AITL patients was 75%, and the complete response (CR) rate was 42%.
However, this study also included patients with other types of peripheral T-cell lymphoma (PTCL), and most of these patients did not respond to 5-AZA.
Richard Delarue, MD, of Necker University Hospital in Paris, France, presented these results at the 9th Annual T-cell Lymphoma Forum.
Results were also presented at the 2016 ASH Annual Meeting (abstract 4164). Dr Delarue reported receiving honoraria from Celgene.
Patients
The study included 19 patients with relapsed/refractory PTCL. Twelve patients had AITL, 3 had adult T-cell leukemia/lymphoma (ATLL), 2 had PTCL not otherwise specified, 1 had enteropathy-associated T-cell lymphoma, and 1 had transformed mycosis fungoides.
At diagnosis, the median age was 71 (range, 39-85) for AITL patients and 59 (range, 32-83) for the other PTCL patients. Seventy-five percent of AITL patients had an IPI score of 3 to 5 and a PIT score of 3 to 4. Eighty-six percent of the other PTCL patients had an IPI score of 3 to 5, and 57% had a PIT score of 3 to 4.
At the time of 5-AZA treatment, all patients had stage III/IV disease. The AITL patients had received a median of 2 (range, 0-6) prior lines of therapy, and the other PTCL patients had received a median of 3 (range, 0-7).
Two patients did not receive chemotherapy before 5-AZA because of the presence of associated chronic myelomonocytic leukemia (CMML) that required treatment first.
Ninety-two percent of AITL patients had TET2 mutations (n=11), 33% had DNMT3A mutations (n=4), and 0% had IDH2 mutations. One of the non-AITL patients had a TET2 mutation.
Treatment
Patients received a subcutaneous injection of 5-AZA at 75 mg/m² for 7 consecutive days every 28 days until progression or unacceptable toxicity. Six patients also received 4 to 8 infusions of rituximab because of EBV-DNA positivity.
The patients received a median of 3 cycles of 5-AZA. At the time of analysis, 4 patients were still receiving therapy.
The median follow-up was 84 days (range, 19 to 1236).
Toxicity
“Hematological toxicity was as expected with 5-azacitidine,” Dr Delarue said.
However, 2 patients had “unusual” adverse reactions. One patient had grade 2 polyneuropathy, which was considered related to a paraneoplastic syndrome.
The other patient had grade 3 diarrhea related to colitis of unknown origin, and this led to treatment interruption.
There were no treatment-related deaths.
Efficacy
Dr Delarue noted that the ORR was significantly higher in AITL patients than in patients with the other PTCL subtypes (P=0.0198).
The ORR was 53% in the entire cohort (10/19), 75% (9/12) among AITL patients, and 14% among patients with other PTCLs (1/7).
“The only patient with a response in the ‘other PTCL’ group was a patient with HTLV1-associated ATLL . . . , but he relapsed a couple of weeks after the second cycle,” Dr Delarue explained.
Among the AITL patients, the CR rate was 42% (5/12), the partial response rate was 33% (4/12), and the rate of stable disease was 25% (3/12).
Six AITL patients eventually progressed—after 2, 2, 3, 4, 4, and 20 cycles of therapy, respectively.
Two AITL patients are off therapy but remain in CR after 9 and 10 months (5 and 6 cycles of treatment), respectively.
The median progression-free survival for AITL patients was 16 months, and the median overall survival was 17 months.
Dr DeLarue noted that 4 of the AITL patients had CMML, 1 had non-CMML myelodysplastic syndrome, 3 had monocytosis without CMML, and 4 had normal monocyte counts.
He also said that, at present, it’s not possible to correlate the results observed in the AITL patients with their mutational status.
However, he and his colleagues are planning a prospective study of 5-AZA in patients with relapsed/refractory AITL and T follicular helper cell PTCL not otherwise specified. 5-AZA will be compared to investigator’s choice in this study.
Dr DeLarue said this trial will provide an opportunity to use the new oral formulation of 5-AZA (CC-486). And he and his colleagues welcome collaborators. ![]()
Investigators report new risk loci for CLL

Investigators say they have identified 9 new risk loci for chronic lymphocytic leukemia (CLL).
The team says the research, published in Nature Communications, provides additional evidence for genetic susceptibility to CLL and sheds new light on the biological basis of CLL development.
They also believe their findings could aid the development of new drugs for CLL or help in selecting existing therapies for CLL
patients.
“We knew people were more likely to develop chronic lymphocytic leukemia if someone in their family had suffered from the disease, but our new research takes a big step towards explaining the underlying genetics,” said study author Richard Houlston, MD, PhD, of The Institute of Cancer Research in London, UK.
“CLL is essentially a disease of the immune system, and it’s fascinating that so many of the new genetic variants we have uncovered seem to directly affect the behavior of white blood cells and their ability to fight disease. Understanding the genetics of CLL can point us towards new treatments for the disease and help us to use existing targeted drugs more effectively.”
For this study, Dr Houlston and his colleagues analyzed data from 8 studies involving a total of 6200 CLL patients and 17,598 controls.
From this, the team identified 9 CLL risk loci:
- 1p36.11 (rs34676223, P=5.04 × 10−13)
- 1q42.13 (rs41271473, P=1.06 × 10−10)
- 4q24 (rs71597109, P=1.37 × 10−10)
- 4q35.1 (rs57214277, P=3.69 × 10−8)
- 6p21.31 (rs3800461, P=1.97 × 10−8)
- 11q23.2 (rs61904987, P=2.64 × 10−11)
- 18q21.1 (rs1036935, P=3.27 × 10−8)
- 19p13.3 (rs7254272, P=4.67 × 10−8)
- 22q13.33 (rs140522, P=2.70 × 10−9).
The investigators noted that the 4q24 association marked by rs71597109 maps to intron 1 of the gene encoding BANK1 (B-cell scaffold protein with ankyrin repeats 1). BANK1 is only ever activated in B cells and is linked to the autoimmune disease lupus.
The team also pointed out that the 19p13.3 association marked by rs7254272 maps 2.5 kb 5′ to ZBTB7A (zinc finger and BTB domain-containing protein 7a), which is a master regulator of B versus T lymphoid fate. So errors in ZBTB7A could lead to too many B cells in the bloodstream and bone marrow.
And rs140522 maps to 22q13.33, which has been linked to the development of multiple sclerosis. The investigators noted that this region of linkage disequilibrium contains 4 genes. One of them, NCAPH2 (non-SMC condensin II complex subunit H2), is differentially expressed in CLL and normal B cells.
“This fascinating study makes a link between genetic variants in the immune system and the development of leukemia and implicates regions of DNA which are also involved in autoimmune diseases,” said Paul Workman, PhD, chief executive and president of The Institute of Cancer Research, who was not involved in this research.
“The findings could point us towards new ways of treating leukemia or better ways of using existing treatments—potentially including immunotherapies.” ![]()

Investigators say they have identified 9 new risk loci for chronic lymphocytic leukemia (CLL).
The team says the research, published in Nature Communications, provides additional evidence for genetic susceptibility to CLL and sheds new light on the biological basis of CLL development.
They also believe their findings could aid the development of new drugs for CLL or help in selecting existing therapies for CLL
patients.
“We knew people were more likely to develop chronic lymphocytic leukemia if someone in their family had suffered from the disease, but our new research takes a big step towards explaining the underlying genetics,” said study author Richard Houlston, MD, PhD, of The Institute of Cancer Research in London, UK.
“CLL is essentially a disease of the immune system, and it’s fascinating that so many of the new genetic variants we have uncovered seem to directly affect the behavior of white blood cells and their ability to fight disease. Understanding the genetics of CLL can point us towards new treatments for the disease and help us to use existing targeted drugs more effectively.”
For this study, Dr Houlston and his colleagues analyzed data from 8 studies involving a total of 6200 CLL patients and 17,598 controls.
From this, the team identified 9 CLL risk loci:
- 1p36.11 (rs34676223, P=5.04 × 10−13)
- 1q42.13 (rs41271473, P=1.06 × 10−10)
- 4q24 (rs71597109, P=1.37 × 10−10)
- 4q35.1 (rs57214277, P=3.69 × 10−8)
- 6p21.31 (rs3800461, P=1.97 × 10−8)
- 11q23.2 (rs61904987, P=2.64 × 10−11)
- 18q21.1 (rs1036935, P=3.27 × 10−8)
- 19p13.3 (rs7254272, P=4.67 × 10−8)
- 22q13.33 (rs140522, P=2.70 × 10−9).
The investigators noted that the 4q24 association marked by rs71597109 maps to intron 1 of the gene encoding BANK1 (B-cell scaffold protein with ankyrin repeats 1). BANK1 is only ever activated in B cells and is linked to the autoimmune disease lupus.
The team also pointed out that the 19p13.3 association marked by rs7254272 maps 2.5 kb 5′ to ZBTB7A (zinc finger and BTB domain-containing protein 7a), which is a master regulator of B versus T lymphoid fate. So errors in ZBTB7A could lead to too many B cells in the bloodstream and bone marrow.
And rs140522 maps to 22q13.33, which has been linked to the development of multiple sclerosis. The investigators noted that this region of linkage disequilibrium contains 4 genes. One of them, NCAPH2 (non-SMC condensin II complex subunit H2), is differentially expressed in CLL and normal B cells.
“This fascinating study makes a link between genetic variants in the immune system and the development of leukemia and implicates regions of DNA which are also involved in autoimmune diseases,” said Paul Workman, PhD, chief executive and president of The Institute of Cancer Research, who was not involved in this research.
“The findings could point us towards new ways of treating leukemia or better ways of using existing treatments—potentially including immunotherapies.” ![]()

Investigators say they have identified 9 new risk loci for chronic lymphocytic leukemia (CLL).
The team says the research, published in Nature Communications, provides additional evidence for genetic susceptibility to CLL and sheds new light on the biological basis of CLL development.
They also believe their findings could aid the development of new drugs for CLL or help in selecting existing therapies for CLL
patients.
“We knew people were more likely to develop chronic lymphocytic leukemia if someone in their family had suffered from the disease, but our new research takes a big step towards explaining the underlying genetics,” said study author Richard Houlston, MD, PhD, of The Institute of Cancer Research in London, UK.
“CLL is essentially a disease of the immune system, and it’s fascinating that so many of the new genetic variants we have uncovered seem to directly affect the behavior of white blood cells and their ability to fight disease. Understanding the genetics of CLL can point us towards new treatments for the disease and help us to use existing targeted drugs more effectively.”
For this study, Dr Houlston and his colleagues analyzed data from 8 studies involving a total of 6200 CLL patients and 17,598 controls.
From this, the team identified 9 CLL risk loci:
- 1p36.11 (rs34676223, P=5.04 × 10−13)
- 1q42.13 (rs41271473, P=1.06 × 10−10)
- 4q24 (rs71597109, P=1.37 × 10−10)
- 4q35.1 (rs57214277, P=3.69 × 10−8)
- 6p21.31 (rs3800461, P=1.97 × 10−8)
- 11q23.2 (rs61904987, P=2.64 × 10−11)
- 18q21.1 (rs1036935, P=3.27 × 10−8)
- 19p13.3 (rs7254272, P=4.67 × 10−8)
- 22q13.33 (rs140522, P=2.70 × 10−9).
The investigators noted that the 4q24 association marked by rs71597109 maps to intron 1 of the gene encoding BANK1 (B-cell scaffold protein with ankyrin repeats 1). BANK1 is only ever activated in B cells and is linked to the autoimmune disease lupus.
The team also pointed out that the 19p13.3 association marked by rs7254272 maps 2.5 kb 5′ to ZBTB7A (zinc finger and BTB domain-containing protein 7a), which is a master regulator of B versus T lymphoid fate. So errors in ZBTB7A could lead to too many B cells in the bloodstream and bone marrow.
And rs140522 maps to 22q13.33, which has been linked to the development of multiple sclerosis. The investigators noted that this region of linkage disequilibrium contains 4 genes. One of them, NCAPH2 (non-SMC condensin II complex subunit H2), is differentially expressed in CLL and normal B cells.
“This fascinating study makes a link between genetic variants in the immune system and the development of leukemia and implicates regions of DNA which are also involved in autoimmune diseases,” said Paul Workman, PhD, chief executive and president of The Institute of Cancer Research, who was not involved in this research.
“The findings could point us towards new ways of treating leukemia or better ways of using existing treatments—potentially including immunotherapies.” ![]()
Obinutuzumab approved to treat FL in Canada

Health Canada has approved the use of obinutuzumab (Gazyva®), an anti-CD20 monoclonal antibody, in patients with follicular lymphoma (FL).
The approval means obinutuzumab can be given, first in combination with bendamustine and then alone as maintenance therapy, to FL patients who relapsed after, or are refractory to, a rituximab-containing regimen.
Obinutuzumab is also approved in Canada for use in combination with chlorambucil to treat patients with previously untreated chronic lymphocytic leukemia.
Obinutuzumab is a product of Roche.
Health Canada’s approval of obinutuzumab in FL is based on results from the phase 3 GADOLIN trial.
The study included 413 patients with rituximab-refractory non-Hodgkin lymphoma, including 321 patients with FL, 46 with marginal zone lymphoma, and 28 with small lymphocytic lymphoma.
The patients were randomized to receive bendamustine alone (control arm) or a combination of bendamustine and obinutuzumab followed by obinutuzumab maintenance (every 2 months for 2 years or until progression).
The primary endpoint of the study was progression-free survival (PFS), as assessed by an independent review committee (IRC). The secondary endpoints were PFS assessed by investigator review, best overall response, complete response (CR), partial response (PR), duration of response, overall survival, and safety profile.
Among patients with FL, the obinutuzumab regimen improved PFS compared to bendamustine alone, as assessed by the IRC (hazard ratio [HR]=0.48, P<0.0001). The median PFS was not reached in patients receiving the obinutuzumab regimen but was 13.8 months in those receiving bendamustine alone.
Investigator-assessed PFS was consistent with IRC-assessed PFS. Investigators said the median PFS with the obinutuzumab regimen was more than double that with bendamustine alone—29.2 months vs 13.7 months (HR=0.48, P<0.0001).
The best overall response for patients receiving the obinutuzumab regimen was 78.7% (15.5% CR, 63.2% PR), compared to 74.7% (18.7% CR, 56% PR) for those receiving bendamustine alone, as assessed by the IRC.
The median duration of response was not reached for patients receiving the obinutuzumab regimen and was 11.6 months for those receiving bendamustine alone.
At last follow-up, the median overall survival had not been reached in either study arm.
The most common grade 3/4 adverse events observed in patients receiving the obinutuzumab regimen were neutropenia (33%), infusion reactions (11%), and thrombocytopenia (10%).
The most common adverse events of any grade were infusion reactions (69%), neutropenia (35%), nausea (54%), fatigue (39%), cough (26%), diarrhea (27%), constipation (19%), fever (18%), thrombocytopenia (15%), vomiting (22%), upper respiratory tract infection (13%), decreased appetite (18%), joint or muscle pain (12%), sinusitis (12%), anemia (12%), general weakness (11%), and urinary tract infection (10%). ![]()

Health Canada has approved the use of obinutuzumab (Gazyva®), an anti-CD20 monoclonal antibody, in patients with follicular lymphoma (FL).
The approval means obinutuzumab can be given, first in combination with bendamustine and then alone as maintenance therapy, to FL patients who relapsed after, or are refractory to, a rituximab-containing regimen.
Obinutuzumab is also approved in Canada for use in combination with chlorambucil to treat patients with previously untreated chronic lymphocytic leukemia.
Obinutuzumab is a product of Roche.
Health Canada’s approval of obinutuzumab in FL is based on results from the phase 3 GADOLIN trial.
The study included 413 patients with rituximab-refractory non-Hodgkin lymphoma, including 321 patients with FL, 46 with marginal zone lymphoma, and 28 with small lymphocytic lymphoma.
The patients were randomized to receive bendamustine alone (control arm) or a combination of bendamustine and obinutuzumab followed by obinutuzumab maintenance (every 2 months for 2 years or until progression).
The primary endpoint of the study was progression-free survival (PFS), as assessed by an independent review committee (IRC). The secondary endpoints were PFS assessed by investigator review, best overall response, complete response (CR), partial response (PR), duration of response, overall survival, and safety profile.
Among patients with FL, the obinutuzumab regimen improved PFS compared to bendamustine alone, as assessed by the IRC (hazard ratio [HR]=0.48, P<0.0001). The median PFS was not reached in patients receiving the obinutuzumab regimen but was 13.8 months in those receiving bendamustine alone.
Investigator-assessed PFS was consistent with IRC-assessed PFS. Investigators said the median PFS with the obinutuzumab regimen was more than double that with bendamustine alone—29.2 months vs 13.7 months (HR=0.48, P<0.0001).
The best overall response for patients receiving the obinutuzumab regimen was 78.7% (15.5% CR, 63.2% PR), compared to 74.7% (18.7% CR, 56% PR) for those receiving bendamustine alone, as assessed by the IRC.
The median duration of response was not reached for patients receiving the obinutuzumab regimen and was 11.6 months for those receiving bendamustine alone.
At last follow-up, the median overall survival had not been reached in either study arm.
The most common grade 3/4 adverse events observed in patients receiving the obinutuzumab regimen were neutropenia (33%), infusion reactions (11%), and thrombocytopenia (10%).
The most common adverse events of any grade were infusion reactions (69%), neutropenia (35%), nausea (54%), fatigue (39%), cough (26%), diarrhea (27%), constipation (19%), fever (18%), thrombocytopenia (15%), vomiting (22%), upper respiratory tract infection (13%), decreased appetite (18%), joint or muscle pain (12%), sinusitis (12%), anemia (12%), general weakness (11%), and urinary tract infection (10%). ![]()

Health Canada has approved the use of obinutuzumab (Gazyva®), an anti-CD20 monoclonal antibody, in patients with follicular lymphoma (FL).
The approval means obinutuzumab can be given, first in combination with bendamustine and then alone as maintenance therapy, to FL patients who relapsed after, or are refractory to, a rituximab-containing regimen.
Obinutuzumab is also approved in Canada for use in combination with chlorambucil to treat patients with previously untreated chronic lymphocytic leukemia.
Obinutuzumab is a product of Roche.
Health Canada’s approval of obinutuzumab in FL is based on results from the phase 3 GADOLIN trial.
The study included 413 patients with rituximab-refractory non-Hodgkin lymphoma, including 321 patients with FL, 46 with marginal zone lymphoma, and 28 with small lymphocytic lymphoma.
The patients were randomized to receive bendamustine alone (control arm) or a combination of bendamustine and obinutuzumab followed by obinutuzumab maintenance (every 2 months for 2 years or until progression).
The primary endpoint of the study was progression-free survival (PFS), as assessed by an independent review committee (IRC). The secondary endpoints were PFS assessed by investigator review, best overall response, complete response (CR), partial response (PR), duration of response, overall survival, and safety profile.
Among patients with FL, the obinutuzumab regimen improved PFS compared to bendamustine alone, as assessed by the IRC (hazard ratio [HR]=0.48, P<0.0001). The median PFS was not reached in patients receiving the obinutuzumab regimen but was 13.8 months in those receiving bendamustine alone.
Investigator-assessed PFS was consistent with IRC-assessed PFS. Investigators said the median PFS with the obinutuzumab regimen was more than double that with bendamustine alone—29.2 months vs 13.7 months (HR=0.48, P<0.0001).
The best overall response for patients receiving the obinutuzumab regimen was 78.7% (15.5% CR, 63.2% PR), compared to 74.7% (18.7% CR, 56% PR) for those receiving bendamustine alone, as assessed by the IRC.
The median duration of response was not reached for patients receiving the obinutuzumab regimen and was 11.6 months for those receiving bendamustine alone.
At last follow-up, the median overall survival had not been reached in either study arm.
The most common grade 3/4 adverse events observed in patients receiving the obinutuzumab regimen were neutropenia (33%), infusion reactions (11%), and thrombocytopenia (10%).
The most common adverse events of any grade were infusion reactions (69%), neutropenia (35%), nausea (54%), fatigue (39%), cough (26%), diarrhea (27%), constipation (19%), fever (18%), thrombocytopenia (15%), vomiting (22%), upper respiratory tract infection (13%), decreased appetite (18%), joint or muscle pain (12%), sinusitis (12%), anemia (12%), general weakness (11%), and urinary tract infection (10%).
NCCN releases patient guidelines for WM/LPL

The National Comprehensive Cancer Network® (NCCN) has published a set of
guidelines for patients with
Waldenström’s macroglobulinemia/ lymphoplasmacytic lymphoma (WM/LPL).
This resource describes what WM is and how it develops,
explains testing for WM, and provides information on the treatment of
primary, relapsed, and refractory WM.
NCCN Guidelines for Patients are adaptations of the
NCCN Clinical Practice Guidelines in Oncology.
The NCCN also publishes Quick Guide™ sheets, which are 1-page summaries of key points in the patient guidelines.
Both patient resources are available free of charge at NCCN.org/patients as well as on the NCCN Patient Guides for Cancer mobile app.
“The treatment approach to patients with Waldenström’s macroglobulinemia has significantly changed in the recent years with better understanding of the disease biology and its natural history and availability of new drugs, allowing for a more individualized approach,” said Shaji Kumar, MD, of the Mayo Clinic in Rochester, Minnesota.
“The revised guidelines reflect these changes and will be a valuable guide for patients in shared decision-making with their oncologists.”
NCCN Guidelines for Patients are based on the same clinical practice guidelines used by healthcare professionals to determine the best way to treat a patient with cancer.
Each resource features expert guidance from US cancer centers designed to help people living with cancer talk to their physicians about the best treatment options for their disease.
The Guidelines for Patients and Quick Guide sheets are written in plain language and include patient-friendly elements, such as “questions to ask your doctor,” a glossary of terms, and medical illustrations of anatomy, tests, and treatment.
NCCN currently offers NCCN Guidelines for Patients covering the following topics: brain, breast, colon esophageal, kidney, non-small cell lung, ovarian, pancreatic, prostate, and stomach cancers; acute lymphoblastic leukemia; adolescents and young adults with cancer; chronic lymphocytic leukemia; chronic myelogenous leukemia; Hodgkin lymphoma; lung cancer screening; malignant pleural mesothelioma; melanoma; multiple myeloma; nausea and vomiting; non-Hodgkin lymphomas; soft tissue sarcoma; and WM/LPL.

The National Comprehensive Cancer Network® (NCCN) has published a set of
guidelines for patients with
Waldenström’s macroglobulinemia/ lymphoplasmacytic lymphoma (WM/LPL).
This resource describes what WM is and how it develops,
explains testing for WM, and provides information on the treatment of
primary, relapsed, and refractory WM.
NCCN Guidelines for Patients are adaptations of the
NCCN Clinical Practice Guidelines in Oncology.
The NCCN also publishes Quick Guide™ sheets, which are 1-page summaries of key points in the patient guidelines.
Both patient resources are available free of charge at NCCN.org/patients as well as on the NCCN Patient Guides for Cancer mobile app.
“The treatment approach to patients with Waldenström’s macroglobulinemia has significantly changed in the recent years with better understanding of the disease biology and its natural history and availability of new drugs, allowing for a more individualized approach,” said Shaji Kumar, MD, of the Mayo Clinic in Rochester, Minnesota.
“The revised guidelines reflect these changes and will be a valuable guide for patients in shared decision-making with their oncologists.”
NCCN Guidelines for Patients are based on the same clinical practice guidelines used by healthcare professionals to determine the best way to treat a patient with cancer.
Each resource features expert guidance from US cancer centers designed to help people living with cancer talk to their physicians about the best treatment options for their disease.
The Guidelines for Patients and Quick Guide sheets are written in plain language and include patient-friendly elements, such as “questions to ask your doctor,” a glossary of terms, and medical illustrations of anatomy, tests, and treatment.
NCCN currently offers NCCN Guidelines for Patients covering the following topics: brain, breast, colon esophageal, kidney, non-small cell lung, ovarian, pancreatic, prostate, and stomach cancers; acute lymphoblastic leukemia; adolescents and young adults with cancer; chronic lymphocytic leukemia; chronic myelogenous leukemia; Hodgkin lymphoma; lung cancer screening; malignant pleural mesothelioma; melanoma; multiple myeloma; nausea and vomiting; non-Hodgkin lymphomas; soft tissue sarcoma; and WM/LPL.

The National Comprehensive Cancer Network® (NCCN) has published a set of
guidelines for patients with
Waldenström’s macroglobulinemia/ lymphoplasmacytic lymphoma (WM/LPL).
This resource describes what WM is and how it develops,
explains testing for WM, and provides information on the treatment of
primary, relapsed, and refractory WM.
NCCN Guidelines for Patients are adaptations of the
NCCN Clinical Practice Guidelines in Oncology.
The NCCN also publishes Quick Guide™ sheets, which are 1-page summaries of key points in the patient guidelines.
Both patient resources are available free of charge at NCCN.org/patients as well as on the NCCN Patient Guides for Cancer mobile app.
“The treatment approach to patients with Waldenström’s macroglobulinemia has significantly changed in the recent years with better understanding of the disease biology and its natural history and availability of new drugs, allowing for a more individualized approach,” said Shaji Kumar, MD, of the Mayo Clinic in Rochester, Minnesota.
“The revised guidelines reflect these changes and will be a valuable guide for patients in shared decision-making with their oncologists.”
NCCN Guidelines for Patients are based on the same clinical practice guidelines used by healthcare professionals to determine the best way to treat a patient with cancer.
Each resource features expert guidance from US cancer centers designed to help people living with cancer talk to their physicians about the best treatment options for their disease.
The Guidelines for Patients and Quick Guide sheets are written in plain language and include patient-friendly elements, such as “questions to ask your doctor,” a glossary of terms, and medical illustrations of anatomy, tests, and treatment.
NCCN currently offers NCCN Guidelines for Patients covering the following topics: brain, breast, colon esophageal, kidney, non-small cell lung, ovarian, pancreatic, prostate, and stomach cancers; acute lymphoblastic leukemia; adolescents and young adults with cancer; chronic lymphocytic leukemia; chronic myelogenous leukemia; Hodgkin lymphoma; lung cancer screening; malignant pleural mesothelioma; melanoma; multiple myeloma; nausea and vomiting; non-Hodgkin lymphomas; soft tissue sarcoma; and WM/LPL.