User login
CHMP recommends authorization of rituximab biosimilar

Photo by Linda Bartlett
The European Medicines Agency’s Committee for Medicinal Products for Human Use (CHMP) has recommended that the rituximab biosimilar Truxima receive marketing authorization for the treatment of several conditions.
The CHMP said studies have shown that Truxima is comparable to the reference product, Mabthera, which was authorized for use in the European Union in 1998.
The active substance in both products is the anti-CD20 monoclonal antibody rituximab.
Truxima is being developed by Celltrion Healthcare Hungary Kft.
The CHMP’s recommendation for Truxima will be reviewed by the European Commission, which normally issues its decision on a product within 67 days of the time the CHMP adopts its opinion.
If the European Commission grants marketing authorization for Truxima, it will be available as a 500 mg concentrate for solution for infusion.
The CHMP has recommended marketing authorization for Truxima in the treatment of non-Hodgkin lymphoma, chronic lymphocytic leukemia, rheumatoid arthritis, and granulomatosis with polyangiitis and microscopic polyangiitis.
The full indications are as follows.
Non-Hodgkin lymphoma
Truxima is indicated for use in combination with chemotherapy to treat previously untreated patients with stage III-IV follicular lymphoma.
Truxima maintenance therapy is indicated for the treatment of follicular lymphoma patients responding to induction therapy.
Truxima monotherapy is indicated for treatment of patients with stage III-IV follicular lymphoma who are chemo-resistant or are in their second or subsequent relapse after chemotherapy.
Truxima is indicated for use in combination with CHOP (cyclophosphamide, doxorubicin, vincristine, prednisolone) for the treatment of patients with CD20-positive diffuse large B-cell lymphoma.
Chronic lymphocytic leukemia
Truxima in combination with chemotherapy is indicated for the treatment of patients with previously untreated and relapsed/refractory chronic lymphocytic leukemia.
The CHMP noted that only limited data are available on efficacy and safety for patients previously treated with monoclonal antibodies, including Truxima, or patients refractory to previous Truxima plus chemotherapy.
Rheumatoid arthritis
Truxima in combination with methotrexate is indicated for the treatment of adults with severe active rheumatoid arthritis who have had an inadequate response or cannot tolerate other disease-modifying anti-rheumatic drugs, including one or more tumor necrosis factor inhibitor therapies.
The CHMP noted that Truxima has been shown to reduce the rate of progression of joint damage as measured by X-ray and to improve physical function, when given in combination with methotrexate.
Granulomatosis with polyangiitis and microscopic polyangiitis
Truxima in combination with glucocorticoids is indicated for the induction of remission in adults with severe, active granulomatosis with polyangiitis and microscopic polyangiitis.
The CHMP proposed that Truxima be administered under the close supervision of an experienced healthcare professional and in an environment where full resuscitation facilities are immediately available. ![]()

Photo by Linda Bartlett
The European Medicines Agency’s Committee for Medicinal Products for Human Use (CHMP) has recommended that the rituximab biosimilar Truxima receive marketing authorization for the treatment of several conditions.
The CHMP said studies have shown that Truxima is comparable to the reference product, Mabthera, which was authorized for use in the European Union in 1998.
The active substance in both products is the anti-CD20 monoclonal antibody rituximab.
Truxima is being developed by Celltrion Healthcare Hungary Kft.
The CHMP’s recommendation for Truxima will be reviewed by the European Commission, which normally issues its decision on a product within 67 days of the time the CHMP adopts its opinion.
If the European Commission grants marketing authorization for Truxima, it will be available as a 500 mg concentrate for solution for infusion.
The CHMP has recommended marketing authorization for Truxima in the treatment of non-Hodgkin lymphoma, chronic lymphocytic leukemia, rheumatoid arthritis, and granulomatosis with polyangiitis and microscopic polyangiitis.
The full indications are as follows.
Non-Hodgkin lymphoma
Truxima is indicated for use in combination with chemotherapy to treat previously untreated patients with stage III-IV follicular lymphoma.
Truxima maintenance therapy is indicated for the treatment of follicular lymphoma patients responding to induction therapy.
Truxima monotherapy is indicated for treatment of patients with stage III-IV follicular lymphoma who are chemo-resistant or are in their second or subsequent relapse after chemotherapy.
Truxima is indicated for use in combination with CHOP (cyclophosphamide, doxorubicin, vincristine, prednisolone) for the treatment of patients with CD20-positive diffuse large B-cell lymphoma.
Chronic lymphocytic leukemia
Truxima in combination with chemotherapy is indicated for the treatment of patients with previously untreated and relapsed/refractory chronic lymphocytic leukemia.
The CHMP noted that only limited data are available on efficacy and safety for patients previously treated with monoclonal antibodies, including Truxima, or patients refractory to previous Truxima plus chemotherapy.
Rheumatoid arthritis
Truxima in combination with methotrexate is indicated for the treatment of adults with severe active rheumatoid arthritis who have had an inadequate response or cannot tolerate other disease-modifying anti-rheumatic drugs, including one or more tumor necrosis factor inhibitor therapies.
The CHMP noted that Truxima has been shown to reduce the rate of progression of joint damage as measured by X-ray and to improve physical function, when given in combination with methotrexate.
Granulomatosis with polyangiitis and microscopic polyangiitis
Truxima in combination with glucocorticoids is indicated for the induction of remission in adults with severe, active granulomatosis with polyangiitis and microscopic polyangiitis.
The CHMP proposed that Truxima be administered under the close supervision of an experienced healthcare professional and in an environment where full resuscitation facilities are immediately available. ![]()

Photo by Linda Bartlett
The European Medicines Agency’s Committee for Medicinal Products for Human Use (CHMP) has recommended that the rituximab biosimilar Truxima receive marketing authorization for the treatment of several conditions.
The CHMP said studies have shown that Truxima is comparable to the reference product, Mabthera, which was authorized for use in the European Union in 1998.
The active substance in both products is the anti-CD20 monoclonal antibody rituximab.
Truxima is being developed by Celltrion Healthcare Hungary Kft.
The CHMP’s recommendation for Truxima will be reviewed by the European Commission, which normally issues its decision on a product within 67 days of the time the CHMP adopts its opinion.
If the European Commission grants marketing authorization for Truxima, it will be available as a 500 mg concentrate for solution for infusion.
The CHMP has recommended marketing authorization for Truxima in the treatment of non-Hodgkin lymphoma, chronic lymphocytic leukemia, rheumatoid arthritis, and granulomatosis with polyangiitis and microscopic polyangiitis.
The full indications are as follows.
Non-Hodgkin lymphoma
Truxima is indicated for use in combination with chemotherapy to treat previously untreated patients with stage III-IV follicular lymphoma.
Truxima maintenance therapy is indicated for the treatment of follicular lymphoma patients responding to induction therapy.
Truxima monotherapy is indicated for treatment of patients with stage III-IV follicular lymphoma who are chemo-resistant or are in their second or subsequent relapse after chemotherapy.
Truxima is indicated for use in combination with CHOP (cyclophosphamide, doxorubicin, vincristine, prednisolone) for the treatment of patients with CD20-positive diffuse large B-cell lymphoma.
Chronic lymphocytic leukemia
Truxima in combination with chemotherapy is indicated for the treatment of patients with previously untreated and relapsed/refractory chronic lymphocytic leukemia.
The CHMP noted that only limited data are available on efficacy and safety for patients previously treated with monoclonal antibodies, including Truxima, or patients refractory to previous Truxima plus chemotherapy.
Rheumatoid arthritis
Truxima in combination with methotrexate is indicated for the treatment of adults with severe active rheumatoid arthritis who have had an inadequate response or cannot tolerate other disease-modifying anti-rheumatic drugs, including one or more tumor necrosis factor inhibitor therapies.
The CHMP noted that Truxima has been shown to reduce the rate of progression of joint damage as measured by X-ray and to improve physical function, when given in combination with methotrexate.
Granulomatosis with polyangiitis and microscopic polyangiitis
Truxima in combination with glucocorticoids is indicated for the induction of remission in adults with severe, active granulomatosis with polyangiitis and microscopic polyangiitis.
The CHMP proposed that Truxima be administered under the close supervision of an experienced healthcare professional and in an environment where full resuscitation facilities are immediately available. ![]()
CHMP recommends approval of topical gel for MF

mycosis fungoides
The European Medicines Agency’s Committee for Medicinal Products for Human Use (CHMP) has recommended that chlormethine gel (Ledaga®) be approved for use in adults with mycosis fungoides (MF).
Ledaga is a hybrid medicine of Caryolysine, which has been approved for use in the European Union since 1946.
Ledaga contains the same active substance as Caryolysine but is a gel intended for cutaneous use.
The active substance of Ledaga is chlormethine, a bifunctional alkylating agent that inhibits rapidly proliferating cells.
Hybrid drug applications rely, in part, on the results of preclinical tests and clinical trials for a reference product and, in part, on new data.
The CHMP said studies have demonstrated the satisfactory quality of Ledaga. Since Ledaga is administered as a topical agent and results in no systemic exposure, a bioequivalence study versus the reference product, Caryolysine, was not required.
The CHMP’s recommendation for Ledaga will be reviewed by the European Commission, which is expected to issue a final decision by the end of February 2017.
If approved, Ledaga will be available as a 160 μg/g gel.
Actelion Pharmaceuticals Ltd, the company developing Ledaga, has agreed to a list of recommendations from the CHMP (post-authorization measures) with regard to the release of Ledaga in Europe.
Subject to the agreed recommendations and achieving market access in different countries, a potential first launch of Ledaga could occur at the end of 2017, at the earliest.
Phase 2 study
The CHMP’s positive opinion of Ledaga is based on results of a multicenter, randomized, observer-blinded, active-controlled study of patients with stage I and IIA MF. Results from this phase 2 study were published in JAMA Dermatology.
The study enrolled 260 patients who were randomized 1:1 to receive topical treatment with Ledaga or compounded control—chlormethine HCl 0.02% compounded in Aquaphor® ointment—once daily for up to 12 months.
A response was defined as at least a 50% improvement in the baseline Composite Assessment of Index Lesion Severity score.
In the intent-to-treat population, 59% (76/130) of patients who received Ledaga achieved a clinical response, compared to 48% (62/130) of patients treated with the compounded control. The rate of complete response was 14% (n=18) and 12% (n=15), respectively.
Patients who were treated for at least 6 months were included in the efficacy-evaluable population. In this population, 77% (69/90) of patients who received Ledaga achieved a clinical response, compared to 59% (56/95) of patients treated with the compounded control. The rate of complete response was 19% (n=17) and 15% (n=14), respectively.
Reductions in mean lesion severity were seen as early as 4 weeks into the study, with further reductions observed with continuing therapy. The time to first confirmed response favored Ledaga.
The most frequent adverse reactions reported with Ledaga were skin-related—dermatitis (55%; eg, skin irritation, erythema, rash, urticaria, skin-burning sensation, pain of the skin), pruritus (20%), skin infections (12%), skin ulceration and blistering (6%), and skin hyperpigmentation (6%).
No systemic absorption of chlormethine was detected with treatment. ![]()

mycosis fungoides
The European Medicines Agency’s Committee for Medicinal Products for Human Use (CHMP) has recommended that chlormethine gel (Ledaga®) be approved for use in adults with mycosis fungoides (MF).
Ledaga is a hybrid medicine of Caryolysine, which has been approved for use in the European Union since 1946.
Ledaga contains the same active substance as Caryolysine but is a gel intended for cutaneous use.
The active substance of Ledaga is chlormethine, a bifunctional alkylating agent that inhibits rapidly proliferating cells.
Hybrid drug applications rely, in part, on the results of preclinical tests and clinical trials for a reference product and, in part, on new data.
The CHMP said studies have demonstrated the satisfactory quality of Ledaga. Since Ledaga is administered as a topical agent and results in no systemic exposure, a bioequivalence study versus the reference product, Caryolysine, was not required.
The CHMP’s recommendation for Ledaga will be reviewed by the European Commission, which is expected to issue a final decision by the end of February 2017.
If approved, Ledaga will be available as a 160 μg/g gel.
Actelion Pharmaceuticals Ltd, the company developing Ledaga, has agreed to a list of recommendations from the CHMP (post-authorization measures) with regard to the release of Ledaga in Europe.
Subject to the agreed recommendations and achieving market access in different countries, a potential first launch of Ledaga could occur at the end of 2017, at the earliest.
Phase 2 study
The CHMP’s positive opinion of Ledaga is based on results of a multicenter, randomized, observer-blinded, active-controlled study of patients with stage I and IIA MF. Results from this phase 2 study were published in JAMA Dermatology.
The study enrolled 260 patients who were randomized 1:1 to receive topical treatment with Ledaga or compounded control—chlormethine HCl 0.02% compounded in Aquaphor® ointment—once daily for up to 12 months.
A response was defined as at least a 50% improvement in the baseline Composite Assessment of Index Lesion Severity score.
In the intent-to-treat population, 59% (76/130) of patients who received Ledaga achieved a clinical response, compared to 48% (62/130) of patients treated with the compounded control. The rate of complete response was 14% (n=18) and 12% (n=15), respectively.
Patients who were treated for at least 6 months were included in the efficacy-evaluable population. In this population, 77% (69/90) of patients who received Ledaga achieved a clinical response, compared to 59% (56/95) of patients treated with the compounded control. The rate of complete response was 19% (n=17) and 15% (n=14), respectively.
Reductions in mean lesion severity were seen as early as 4 weeks into the study, with further reductions observed with continuing therapy. The time to first confirmed response favored Ledaga.
The most frequent adverse reactions reported with Ledaga were skin-related—dermatitis (55%; eg, skin irritation, erythema, rash, urticaria, skin-burning sensation, pain of the skin), pruritus (20%), skin infections (12%), skin ulceration and blistering (6%), and skin hyperpigmentation (6%).
No systemic absorption of chlormethine was detected with treatment. ![]()

mycosis fungoides
The European Medicines Agency’s Committee for Medicinal Products for Human Use (CHMP) has recommended that chlormethine gel (Ledaga®) be approved for use in adults with mycosis fungoides (MF).
Ledaga is a hybrid medicine of Caryolysine, which has been approved for use in the European Union since 1946.
Ledaga contains the same active substance as Caryolysine but is a gel intended for cutaneous use.
The active substance of Ledaga is chlormethine, a bifunctional alkylating agent that inhibits rapidly proliferating cells.
Hybrid drug applications rely, in part, on the results of preclinical tests and clinical trials for a reference product and, in part, on new data.
The CHMP said studies have demonstrated the satisfactory quality of Ledaga. Since Ledaga is administered as a topical agent and results in no systemic exposure, a bioequivalence study versus the reference product, Caryolysine, was not required.
The CHMP’s recommendation for Ledaga will be reviewed by the European Commission, which is expected to issue a final decision by the end of February 2017.
If approved, Ledaga will be available as a 160 μg/g gel.
Actelion Pharmaceuticals Ltd, the company developing Ledaga, has agreed to a list of recommendations from the CHMP (post-authorization measures) with regard to the release of Ledaga in Europe.
Subject to the agreed recommendations and achieving market access in different countries, a potential first launch of Ledaga could occur at the end of 2017, at the earliest.
Phase 2 study
The CHMP’s positive opinion of Ledaga is based on results of a multicenter, randomized, observer-blinded, active-controlled study of patients with stage I and IIA MF. Results from this phase 2 study were published in JAMA Dermatology.
The study enrolled 260 patients who were randomized 1:1 to receive topical treatment with Ledaga or compounded control—chlormethine HCl 0.02% compounded in Aquaphor® ointment—once daily for up to 12 months.
A response was defined as at least a 50% improvement in the baseline Composite Assessment of Index Lesion Severity score.
In the intent-to-treat population, 59% (76/130) of patients who received Ledaga achieved a clinical response, compared to 48% (62/130) of patients treated with the compounded control. The rate of complete response was 14% (n=18) and 12% (n=15), respectively.
Patients who were treated for at least 6 months were included in the efficacy-evaluable population. In this population, 77% (69/90) of patients who received Ledaga achieved a clinical response, compared to 59% (56/95) of patients treated with the compounded control. The rate of complete response was 19% (n=17) and 15% (n=14), respectively.
Reductions in mean lesion severity were seen as early as 4 weeks into the study, with further reductions observed with continuing therapy. The time to first confirmed response favored Ledaga.
The most frequent adverse reactions reported with Ledaga were skin-related—dermatitis (55%; eg, skin irritation, erythema, rash, urticaria, skin-burning sensation, pain of the skin), pruritus (20%), skin infections (12%), skin ulceration and blistering (6%), and skin hyperpigmentation (6%).
No systemic absorption of chlormethine was detected with treatment. ![]()
CAR met primary endpoint at interim analysis in DLBCL
2016 ASH Annual Meeting
SAN DIEGO—The chimeric antigen receptor (CAR) T-cell therapy KTE-C19 has met its primary endpoint at the pre-specified interim analysis of the phase 2 ZUMA-1 trial in diffuse large B-cell lymphoma (DLBCL), according to data presented at the 2016 ASH Annual Meeting.
DLBCL patients had an overall response rate (ORR) of 76% and a complete response (CR) rate of 47% (P<0.0001) after 3 months or more of follow-up. And most responses were evident by day 30, the researchers report.
ZUMA-1 is the first multicenter trial of an anti-CD19 CAR T-cell therapy in refractory, aggressive non-Hodgkin lymphoma (NHL).
A second NHL cohort of primary mediastinal B-cell lymphoma or transformed follicular lymphoma (PMBCL/TFL) patients were also treated. Together, the cohorts achieved an ORR of 79% and a CR rate of 52%.
Sattva Neelapu, MD, of The University of Texas MD Anderson Cancer Center in Houston, Texas, presented the results as a late-breaking abstract (LBA-6*).
Detailed results of the PMBCL/TFL cohort were presented separately (abstract 998) at the meeting.
Earlier data from the phase 2 study have been reported in Hematology Times.
Phase 2 interim analysis
The study enrolled 111 patients, all of whom underwent leukapheresis. Seven of these patients were not treated, 5 due to serious adverse events (SAEs), 1 due to unavailable product, and 2 due to non-measurable disease.
“Importantly, there was no bridging therapy allowed on the study,” Dr Neelapu pointed out.
Patients then received a conditioning regimen of cyclophosphamide (500 mg/m2) and fludarabine (30 mg/m2) for 3 days. Two patients experienced SAEs after the conditioning regimen, making it a total of 10 patients who could not be treated.
Two days after the conditioning regimen was completed, investigators dosed 101 patients with KTE-C19 at a target dose of 2 × 106 anti-CD19 CAR T cells/kg.
“The majority of patients that were enrolled on the study were treated,” Dr Neelapu emphasized. “In fact, 91% of the 111 patients enrolled were treated and received the target dose of KTE-C19.”
Dr Neelapu noted that the success rate for manufacturing the CAR T cells was 99%, and the average turnaround time from apheresis to delivery to the clinical site was 17 days.
The study called for a pre-specified interim efficacy analysis when 50 patients in cohort 1—DLBCL patients—had at least 3 months of follow-up. This occurred on August 24, 2016, and the data was analyzed as of that date.
The primary endpoint was ORR of P<0.0001 using an exact binomial test comparing observed ORR to a historical control assumption of 20%. Key secondary endpoints included duration of response, overall survival, safety, and levels of CAR T cells and cytokines.
At the time of the pre-specified interim analysis, 93 patients had at least 1 month of follow-up. Fifty-one patients with DLBCL and 11 patients with PMBCL/TFL had at least 3 months of follow-up.
Patient characteristics
Dr Neelapu reported data on 73 DLBCL patients (cohort 1) and 20 PMBCL/TFL patients (cohort 2) evaluable with at least 1 month of follow-up at the time of the presentation.
The median age of all 93 patients was 59 (range, 25-76), and about half were 60 years or older.
Two-thirds of patients in cohort 1 and three-quarters in cohort 2 were male. Sixty-six percent of cohort 1 and 40% of cohort 2 had an ECOG performance status of 1.
Cohort 1 had a median of 3 prior therapies (range, 1-7), and 44% had an International Prognostic Index (IPI) risk score of 3-4. Cohort 2 had a median of 4 prior therapies (range, 2-12), and 45% had an IPI risk score of 3-4.
Fifty-six DLBCL patients (77%) were refractory to their second or later line of therapy, and 15 (21%) had relapsed after autologous stem cell transplant.
Sixteen PMBCL/TFL patients (80%) were refractory to their second or later line of therapy, and 4 (20%) relapsed after autologous stem cell transplant.
Results
Dr Neelapu indicated that patients responded rapidly to treatment, and most responses were evident at the first tumor assessment.
At 3 months’ follow-up or longer, the ORR was 76% and the CR rate 47% for the 51 DLBCL patients in cohort 1. This was a 6-fold higher CR rate compared with historical outcomes.
For the 11 PMBCL/TFL patients in cohort 2, the ORR was 91% and the CR rate was 73% at 3 months or longer.
Both cohorts combined yielded an ORR of 79% and a CR rate of 52%.
The treatment effect was consistent across key covariates—refractory patients, disease stage, IPI risk score, CD4/CD8 ratio, and steroid and tocilizumab use.
Dr Neelapu described the case of a 62-year-old male with refractory DLBCL who had 4 prior rituximab-based therapies. He had no response to his last 3 therapies combining rituximab with GDP (gemcitabine, cisplatin, and dexamethasone), ICE (ifosfamide, carboplatin, and etoposide), or lenalidomide.
After KTE-C19 therapy, the patient has an ongoing CR that has lasted more than 9 months.
Adverse events
Sixty-eight DLBCL patients (93%) experienced grade 3 or higher adverse events (AEs). These included 10 patients (14%) with cytokine release syndrome (CRS) and 18 (25%) with neurologic events.
Eighteen PMBCL/TFL patients (90%) experienced grade 3 or higher AEs, 2 (10%) with grade 3 or higher CRS and 9 (45%) with grade 3 or higher neurologic events.
CRS and neurological events were generally reversible, Dr Neelapu said. All CRS events resolved except 1 in the PMBCL/TFL cohort.
In both cohorts combined, 38% of patients received tocilizumab, 17% received corticosteroids, and 17% received both.
Three neurological events were ongoing at the data cut-off—grade 1 memory impairment, grade 1 tremor, and grade 2 tremor.
There were no cases of cerebral edema.
Three patients died from causes other than progressive disease—1 DLBCL patient and 2 in the PMBCL/TFL cohort.
Investigators considered the DLBCL patient death (due to hemophagocytic lymphohistiocytosis) and 1 death in the PMBCL/TFL arm (due to cardiac arrest) to be treatment-related.
Investigators did not consider the other death in the PMBCL/TFL arm (due to pulmonary embolism) to be treatment-related.
The most frequent grade 3 or higher treatment-emergent AEs in both arms combined included neutropenia (63%), anemia (42%), leukopenia (40%), febrile neutropenia (29%), thrombocytopenia (26%), encephalopathy (19%), hypophosphatemia (17%), and decreased lymphocyte count (17%).
Peak CAR T-cell expansion occurred between 7 and 14 days and was associated with ongoing CRs and grade 3 or greater neurological events, but not with CRS.
AEs were managed effectively across the 22 study sites, Dr Neelapu added, and most sites had no prior CAR T-cell therapy experience.
Dr Neelapu noted that the ZUMA-1 results are consistent with earlier KTE-C19 trials in aggressive NHL.
The primary analysis for this phase 2 study is expected to occur when all treated patients have 6 months of follow-up in the first quarter of 2017.
The study is sponsored by Kite Pharma but is also funded, in part, by the Leukemia and Lymphoma Society Therapy Acceleration Program. ![]()
*Information in the abstract differs from that presented at the meeting.
2016 ASH Annual Meeting
SAN DIEGO—The chimeric antigen receptor (CAR) T-cell therapy KTE-C19 has met its primary endpoint at the pre-specified interim analysis of the phase 2 ZUMA-1 trial in diffuse large B-cell lymphoma (DLBCL), according to data presented at the 2016 ASH Annual Meeting.
DLBCL patients had an overall response rate (ORR) of 76% and a complete response (CR) rate of 47% (P<0.0001) after 3 months or more of follow-up. And most responses were evident by day 30, the researchers report.
ZUMA-1 is the first multicenter trial of an anti-CD19 CAR T-cell therapy in refractory, aggressive non-Hodgkin lymphoma (NHL).
A second NHL cohort of primary mediastinal B-cell lymphoma or transformed follicular lymphoma (PMBCL/TFL) patients were also treated. Together, the cohorts achieved an ORR of 79% and a CR rate of 52%.
Sattva Neelapu, MD, of The University of Texas MD Anderson Cancer Center in Houston, Texas, presented the results as a late-breaking abstract (LBA-6*).
Detailed results of the PMBCL/TFL cohort were presented separately (abstract 998) at the meeting.
Earlier data from the phase 2 study have been reported in Hematology Times.
Phase 2 interim analysis
The study enrolled 111 patients, all of whom underwent leukapheresis. Seven of these patients were not treated, 5 due to serious adverse events (SAEs), 1 due to unavailable product, and 2 due to non-measurable disease.
“Importantly, there was no bridging therapy allowed on the study,” Dr Neelapu pointed out.
Patients then received a conditioning regimen of cyclophosphamide (500 mg/m2) and fludarabine (30 mg/m2) for 3 days. Two patients experienced SAEs after the conditioning regimen, making it a total of 10 patients who could not be treated.
Two days after the conditioning regimen was completed, investigators dosed 101 patients with KTE-C19 at a target dose of 2 × 106 anti-CD19 CAR T cells/kg.
“The majority of patients that were enrolled on the study were treated,” Dr Neelapu emphasized. “In fact, 91% of the 111 patients enrolled were treated and received the target dose of KTE-C19.”
Dr Neelapu noted that the success rate for manufacturing the CAR T cells was 99%, and the average turnaround time from apheresis to delivery to the clinical site was 17 days.
The study called for a pre-specified interim efficacy analysis when 50 patients in cohort 1—DLBCL patients—had at least 3 months of follow-up. This occurred on August 24, 2016, and the data was analyzed as of that date.
The primary endpoint was ORR of P<0.0001 using an exact binomial test comparing observed ORR to a historical control assumption of 20%. Key secondary endpoints included duration of response, overall survival, safety, and levels of CAR T cells and cytokines.
At the time of the pre-specified interim analysis, 93 patients had at least 1 month of follow-up. Fifty-one patients with DLBCL and 11 patients with PMBCL/TFL had at least 3 months of follow-up.
Patient characteristics
Dr Neelapu reported data on 73 DLBCL patients (cohort 1) and 20 PMBCL/TFL patients (cohort 2) evaluable with at least 1 month of follow-up at the time of the presentation.
The median age of all 93 patients was 59 (range, 25-76), and about half were 60 years or older.
Two-thirds of patients in cohort 1 and three-quarters in cohort 2 were male. Sixty-six percent of cohort 1 and 40% of cohort 2 had an ECOG performance status of 1.
Cohort 1 had a median of 3 prior therapies (range, 1-7), and 44% had an International Prognostic Index (IPI) risk score of 3-4. Cohort 2 had a median of 4 prior therapies (range, 2-12), and 45% had an IPI risk score of 3-4.
Fifty-six DLBCL patients (77%) were refractory to their second or later line of therapy, and 15 (21%) had relapsed after autologous stem cell transplant.
Sixteen PMBCL/TFL patients (80%) were refractory to their second or later line of therapy, and 4 (20%) relapsed after autologous stem cell transplant.
Results
Dr Neelapu indicated that patients responded rapidly to treatment, and most responses were evident at the first tumor assessment.
At 3 months’ follow-up or longer, the ORR was 76% and the CR rate 47% for the 51 DLBCL patients in cohort 1. This was a 6-fold higher CR rate compared with historical outcomes.
For the 11 PMBCL/TFL patients in cohort 2, the ORR was 91% and the CR rate was 73% at 3 months or longer.
Both cohorts combined yielded an ORR of 79% and a CR rate of 52%.
The treatment effect was consistent across key covariates—refractory patients, disease stage, IPI risk score, CD4/CD8 ratio, and steroid and tocilizumab use.
Dr Neelapu described the case of a 62-year-old male with refractory DLBCL who had 4 prior rituximab-based therapies. He had no response to his last 3 therapies combining rituximab with GDP (gemcitabine, cisplatin, and dexamethasone), ICE (ifosfamide, carboplatin, and etoposide), or lenalidomide.
After KTE-C19 therapy, the patient has an ongoing CR that has lasted more than 9 months.
Adverse events
Sixty-eight DLBCL patients (93%) experienced grade 3 or higher adverse events (AEs). These included 10 patients (14%) with cytokine release syndrome (CRS) and 18 (25%) with neurologic events.
Eighteen PMBCL/TFL patients (90%) experienced grade 3 or higher AEs, 2 (10%) with grade 3 or higher CRS and 9 (45%) with grade 3 or higher neurologic events.
CRS and neurological events were generally reversible, Dr Neelapu said. All CRS events resolved except 1 in the PMBCL/TFL cohort.
In both cohorts combined, 38% of patients received tocilizumab, 17% received corticosteroids, and 17% received both.
Three neurological events were ongoing at the data cut-off—grade 1 memory impairment, grade 1 tremor, and grade 2 tremor.
There were no cases of cerebral edema.
Three patients died from causes other than progressive disease—1 DLBCL patient and 2 in the PMBCL/TFL cohort.
Investigators considered the DLBCL patient death (due to hemophagocytic lymphohistiocytosis) and 1 death in the PMBCL/TFL arm (due to cardiac arrest) to be treatment-related.
Investigators did not consider the other death in the PMBCL/TFL arm (due to pulmonary embolism) to be treatment-related.
The most frequent grade 3 or higher treatment-emergent AEs in both arms combined included neutropenia (63%), anemia (42%), leukopenia (40%), febrile neutropenia (29%), thrombocytopenia (26%), encephalopathy (19%), hypophosphatemia (17%), and decreased lymphocyte count (17%).
Peak CAR T-cell expansion occurred between 7 and 14 days and was associated with ongoing CRs and grade 3 or greater neurological events, but not with CRS.
AEs were managed effectively across the 22 study sites, Dr Neelapu added, and most sites had no prior CAR T-cell therapy experience.
Dr Neelapu noted that the ZUMA-1 results are consistent with earlier KTE-C19 trials in aggressive NHL.
The primary analysis for this phase 2 study is expected to occur when all treated patients have 6 months of follow-up in the first quarter of 2017.
The study is sponsored by Kite Pharma but is also funded, in part, by the Leukemia and Lymphoma Society Therapy Acceleration Program. ![]()
*Information in the abstract differs from that presented at the meeting.
2016 ASH Annual Meeting
SAN DIEGO—The chimeric antigen receptor (CAR) T-cell therapy KTE-C19 has met its primary endpoint at the pre-specified interim analysis of the phase 2 ZUMA-1 trial in diffuse large B-cell lymphoma (DLBCL), according to data presented at the 2016 ASH Annual Meeting.
DLBCL patients had an overall response rate (ORR) of 76% and a complete response (CR) rate of 47% (P<0.0001) after 3 months or more of follow-up. And most responses were evident by day 30, the researchers report.
ZUMA-1 is the first multicenter trial of an anti-CD19 CAR T-cell therapy in refractory, aggressive non-Hodgkin lymphoma (NHL).
A second NHL cohort of primary mediastinal B-cell lymphoma or transformed follicular lymphoma (PMBCL/TFL) patients were also treated. Together, the cohorts achieved an ORR of 79% and a CR rate of 52%.
Sattva Neelapu, MD, of The University of Texas MD Anderson Cancer Center in Houston, Texas, presented the results as a late-breaking abstract (LBA-6*).
Detailed results of the PMBCL/TFL cohort were presented separately (abstract 998) at the meeting.
Earlier data from the phase 2 study have been reported in Hematology Times.
Phase 2 interim analysis
The study enrolled 111 patients, all of whom underwent leukapheresis. Seven of these patients were not treated, 5 due to serious adverse events (SAEs), 1 due to unavailable product, and 2 due to non-measurable disease.
“Importantly, there was no bridging therapy allowed on the study,” Dr Neelapu pointed out.
Patients then received a conditioning regimen of cyclophosphamide (500 mg/m2) and fludarabine (30 mg/m2) for 3 days. Two patients experienced SAEs after the conditioning regimen, making it a total of 10 patients who could not be treated.
Two days after the conditioning regimen was completed, investigators dosed 101 patients with KTE-C19 at a target dose of 2 × 106 anti-CD19 CAR T cells/kg.
“The majority of patients that were enrolled on the study were treated,” Dr Neelapu emphasized. “In fact, 91% of the 111 patients enrolled were treated and received the target dose of KTE-C19.”
Dr Neelapu noted that the success rate for manufacturing the CAR T cells was 99%, and the average turnaround time from apheresis to delivery to the clinical site was 17 days.
The study called for a pre-specified interim efficacy analysis when 50 patients in cohort 1—DLBCL patients—had at least 3 months of follow-up. This occurred on August 24, 2016, and the data was analyzed as of that date.
The primary endpoint was ORR of P<0.0001 using an exact binomial test comparing observed ORR to a historical control assumption of 20%. Key secondary endpoints included duration of response, overall survival, safety, and levels of CAR T cells and cytokines.
At the time of the pre-specified interim analysis, 93 patients had at least 1 month of follow-up. Fifty-one patients with DLBCL and 11 patients with PMBCL/TFL had at least 3 months of follow-up.
Patient characteristics
Dr Neelapu reported data on 73 DLBCL patients (cohort 1) and 20 PMBCL/TFL patients (cohort 2) evaluable with at least 1 month of follow-up at the time of the presentation.
The median age of all 93 patients was 59 (range, 25-76), and about half were 60 years or older.
Two-thirds of patients in cohort 1 and three-quarters in cohort 2 were male. Sixty-six percent of cohort 1 and 40% of cohort 2 had an ECOG performance status of 1.
Cohort 1 had a median of 3 prior therapies (range, 1-7), and 44% had an International Prognostic Index (IPI) risk score of 3-4. Cohort 2 had a median of 4 prior therapies (range, 2-12), and 45% had an IPI risk score of 3-4.
Fifty-six DLBCL patients (77%) were refractory to their second or later line of therapy, and 15 (21%) had relapsed after autologous stem cell transplant.
Sixteen PMBCL/TFL patients (80%) were refractory to their second or later line of therapy, and 4 (20%) relapsed after autologous stem cell transplant.
Results
Dr Neelapu indicated that patients responded rapidly to treatment, and most responses were evident at the first tumor assessment.
At 3 months’ follow-up or longer, the ORR was 76% and the CR rate 47% for the 51 DLBCL patients in cohort 1. This was a 6-fold higher CR rate compared with historical outcomes.
For the 11 PMBCL/TFL patients in cohort 2, the ORR was 91% and the CR rate was 73% at 3 months or longer.
Both cohorts combined yielded an ORR of 79% and a CR rate of 52%.
The treatment effect was consistent across key covariates—refractory patients, disease stage, IPI risk score, CD4/CD8 ratio, and steroid and tocilizumab use.
Dr Neelapu described the case of a 62-year-old male with refractory DLBCL who had 4 prior rituximab-based therapies. He had no response to his last 3 therapies combining rituximab with GDP (gemcitabine, cisplatin, and dexamethasone), ICE (ifosfamide, carboplatin, and etoposide), or lenalidomide.
After KTE-C19 therapy, the patient has an ongoing CR that has lasted more than 9 months.
Adverse events
Sixty-eight DLBCL patients (93%) experienced grade 3 or higher adverse events (AEs). These included 10 patients (14%) with cytokine release syndrome (CRS) and 18 (25%) with neurologic events.
Eighteen PMBCL/TFL patients (90%) experienced grade 3 or higher AEs, 2 (10%) with grade 3 or higher CRS and 9 (45%) with grade 3 or higher neurologic events.
CRS and neurological events were generally reversible, Dr Neelapu said. All CRS events resolved except 1 in the PMBCL/TFL cohort.
In both cohorts combined, 38% of patients received tocilizumab, 17% received corticosteroids, and 17% received both.
Three neurological events were ongoing at the data cut-off—grade 1 memory impairment, grade 1 tremor, and grade 2 tremor.
There were no cases of cerebral edema.
Three patients died from causes other than progressive disease—1 DLBCL patient and 2 in the PMBCL/TFL cohort.
Investigators considered the DLBCL patient death (due to hemophagocytic lymphohistiocytosis) and 1 death in the PMBCL/TFL arm (due to cardiac arrest) to be treatment-related.
Investigators did not consider the other death in the PMBCL/TFL arm (due to pulmonary embolism) to be treatment-related.
The most frequent grade 3 or higher treatment-emergent AEs in both arms combined included neutropenia (63%), anemia (42%), leukopenia (40%), febrile neutropenia (29%), thrombocytopenia (26%), encephalopathy (19%), hypophosphatemia (17%), and decreased lymphocyte count (17%).
Peak CAR T-cell expansion occurred between 7 and 14 days and was associated with ongoing CRs and grade 3 or greater neurological events, but not with CRS.
AEs were managed effectively across the 22 study sites, Dr Neelapu added, and most sites had no prior CAR T-cell therapy experience.
Dr Neelapu noted that the ZUMA-1 results are consistent with earlier KTE-C19 trials in aggressive NHL.
The primary analysis for this phase 2 study is expected to occur when all treated patients have 6 months of follow-up in the first quarter of 2017.
The study is sponsored by Kite Pharma but is also funded, in part, by the Leukemia and Lymphoma Society Therapy Acceleration Program. ![]()
*Information in the abstract differs from that presented at the meeting.
Characterizing FL transformation, progression

Patients with transformed follicular lymphoma (FL) and FL patients with early progression have “widely divergent patterns of clonal
dynamics,” according to researchers.
The team investigated the molecular events underlying transformation and early progression in FL and found that disparate evolutionary trajectories and mutational profiles drive these 2 distinct clinical endpoints.
Sohrab Shah, PhD, of the University of British Columbia in Vancouver, Canada, and his colleagues reported these findings in PLOS Medicine.
The researchers used whole-genome sequencing to analyze tumor specimens and matched normal specimens from 41 FL patients.
The team then classified the patients according to the following clinical endpoints:
- Patients who presented with transformation (n=15)
- Patients who experienced tumor progression within 2.5 years of starting treatment, without evidence of transformation (n=6)
- Patients who had neither transformation nor progression up to 5 years post-diagnosis (n=20).
The researchers also used targeted capture sequencing of known FL-associated genes in a larger cohort of 277 FL patients (395 samples) to investigate discrete genetic events that drive transformation and early progression.
Results showed that tumors that progress early evolve in different ways from those that transform.
The team found that, for tumors that transform, the cells or clones that constitute the majority of the aggressive tumor were extremely rare at diagnosis, if they were present at all.
In contrast, for early progressive FL, the clonal architecture remained similar from the time of diagnosis to relapse, indicating that the diagnostic tumor may already contain the properties that confer resistance to treatment.
Analysis of the larger cohort revealed genes and biological processes that were associated with transformation and progression.
The researchers identified 12 genes that were more commonly mutated at the time of transformation than the time of diagnosis—TP53, B2M, EZH2, MYC, CCND3, EBF1, PIM1, GNA13, ITPKB, CHD8, S1PR2, and P2RY8.
The team said their findings suggest that defective DNA damage response, increased proliferation, escape from immune surveillance, and loss of confinement within the germinal center are key features that drive histological transformation from indolent to aggressive lymphoma.
The researchers also identified 10 genes that were more commonly mutated in patients with early progression than in patients with late/no progression—B2M, BTG1, FAS, IKZF3, KMT2C, MKI67, MYD88, SOCS1, TP53, and XBP1.
The team noted that most patients with early progression (80%) had mutations in at least 1 of these 10 genes, but none of the genes were mutated at a frequency greater than 27%. This suggests that early progression is related to relatively infrequent genetic alterations.
The researchers said these findings provide a basis for future research on prognostic assay development and potential strategies for monitoring and treatment of patients with FL. ![]()

Patients with transformed follicular lymphoma (FL) and FL patients with early progression have “widely divergent patterns of clonal
dynamics,” according to researchers.
The team investigated the molecular events underlying transformation and early progression in FL and found that disparate evolutionary trajectories and mutational profiles drive these 2 distinct clinical endpoints.
Sohrab Shah, PhD, of the University of British Columbia in Vancouver, Canada, and his colleagues reported these findings in PLOS Medicine.
The researchers used whole-genome sequencing to analyze tumor specimens and matched normal specimens from 41 FL patients.
The team then classified the patients according to the following clinical endpoints:
- Patients who presented with transformation (n=15)
- Patients who experienced tumor progression within 2.5 years of starting treatment, without evidence of transformation (n=6)
- Patients who had neither transformation nor progression up to 5 years post-diagnosis (n=20).
The researchers also used targeted capture sequencing of known FL-associated genes in a larger cohort of 277 FL patients (395 samples) to investigate discrete genetic events that drive transformation and early progression.
Results showed that tumors that progress early evolve in different ways from those that transform.
The team found that, for tumors that transform, the cells or clones that constitute the majority of the aggressive tumor were extremely rare at diagnosis, if they were present at all.
In contrast, for early progressive FL, the clonal architecture remained similar from the time of diagnosis to relapse, indicating that the diagnostic tumor may already contain the properties that confer resistance to treatment.
Analysis of the larger cohort revealed genes and biological processes that were associated with transformation and progression.
The researchers identified 12 genes that were more commonly mutated at the time of transformation than the time of diagnosis—TP53, B2M, EZH2, MYC, CCND3, EBF1, PIM1, GNA13, ITPKB, CHD8, S1PR2, and P2RY8.
The team said their findings suggest that defective DNA damage response, increased proliferation, escape from immune surveillance, and loss of confinement within the germinal center are key features that drive histological transformation from indolent to aggressive lymphoma.
The researchers also identified 10 genes that were more commonly mutated in patients with early progression than in patients with late/no progression—B2M, BTG1, FAS, IKZF3, KMT2C, MKI67, MYD88, SOCS1, TP53, and XBP1.
The team noted that most patients with early progression (80%) had mutations in at least 1 of these 10 genes, but none of the genes were mutated at a frequency greater than 27%. This suggests that early progression is related to relatively infrequent genetic alterations.
The researchers said these findings provide a basis for future research on prognostic assay development and potential strategies for monitoring and treatment of patients with FL. ![]()

Patients with transformed follicular lymphoma (FL) and FL patients with early progression have “widely divergent patterns of clonal
dynamics,” according to researchers.
The team investigated the molecular events underlying transformation and early progression in FL and found that disparate evolutionary trajectories and mutational profiles drive these 2 distinct clinical endpoints.
Sohrab Shah, PhD, of the University of British Columbia in Vancouver, Canada, and his colleagues reported these findings in PLOS Medicine.
The researchers used whole-genome sequencing to analyze tumor specimens and matched normal specimens from 41 FL patients.
The team then classified the patients according to the following clinical endpoints:
- Patients who presented with transformation (n=15)
- Patients who experienced tumor progression within 2.5 years of starting treatment, without evidence of transformation (n=6)
- Patients who had neither transformation nor progression up to 5 years post-diagnosis (n=20).
The researchers also used targeted capture sequencing of known FL-associated genes in a larger cohort of 277 FL patients (395 samples) to investigate discrete genetic events that drive transformation and early progression.
Results showed that tumors that progress early evolve in different ways from those that transform.
The team found that, for tumors that transform, the cells or clones that constitute the majority of the aggressive tumor were extremely rare at diagnosis, if they were present at all.
In contrast, for early progressive FL, the clonal architecture remained similar from the time of diagnosis to relapse, indicating that the diagnostic tumor may already contain the properties that confer resistance to treatment.
Analysis of the larger cohort revealed genes and biological processes that were associated with transformation and progression.
The researchers identified 12 genes that were more commonly mutated at the time of transformation than the time of diagnosis—TP53, B2M, EZH2, MYC, CCND3, EBF1, PIM1, GNA13, ITPKB, CHD8, S1PR2, and P2RY8.
The team said their findings suggest that defective DNA damage response, increased proliferation, escape from immune surveillance, and loss of confinement within the germinal center are key features that drive histological transformation from indolent to aggressive lymphoma.
The researchers also identified 10 genes that were more commonly mutated in patients with early progression than in patients with late/no progression—B2M, BTG1, FAS, IKZF3, KMT2C, MKI67, MYD88, SOCS1, TP53, and XBP1.
The team noted that most patients with early progression (80%) had mutations in at least 1 of these 10 genes, but none of the genes were mutated at a frequency greater than 27%. This suggests that early progression is related to relatively infrequent genetic alterations.
The researchers said these findings provide a basis for future research on prognostic assay development and potential strategies for monitoring and treatment of patients with FL. ![]()
EC authorizes new use for ofatumumab in CLL

Photo courtesy of GSK
The European Commission (EC) has granted marketing authorization for ofatumumab (Arzerra®) to be used in combination with fludarabine and cyclophosphamide (FC) in the treatment of adults with relapsed chronic lymphocytic leukemia (CLL).
Ofatumumab is a monoclonal antibody designed to target CD20. The drug is marketed under a collaboration agreement between Genmab and Novartis.
The EC previously authorized the use of ofatumumab as a single agent to treat CLL patients who are refractory to fludarabine and alemtuzumab.
The agency also authorized the use of ofatumumab in combination with chlorambucil or bendamustine in CLL patients who have not received prior therapy and are not eligible for fludarabine-based therapy.
The EC’s decision to approve the use of ofatumumab in combination with FC was based on results from the phase 3 COMPLEMENT 2 study, which were published in Leukemia & Lymphoma in October.
The trial enrolled 365 patients with relapsed CLL. The patients were randomized 1:1 to receive up to 6 cycles of ofatumumab in combination with FC or up to 6 cycles of FC alone.
The primary endpoint was progression-free survival, as assessed by an independent review committee.
The median progression-free survival was 28.9 months for patients receiving ofatumumab plus FC, compared to 18.8 months for patients receiving FC only (hazard ratio=0.67, P=0.0032).
The incidence of grade 3 or higher adverse events was 74% in the ofatumumab-plus-FC arm and 69% in the FC-only arm. Neutropenia was the most common of these events, occurring in 49% and 36% of patients, respectively. ![]()

Photo courtesy of GSK
The European Commission (EC) has granted marketing authorization for ofatumumab (Arzerra®) to be used in combination with fludarabine and cyclophosphamide (FC) in the treatment of adults with relapsed chronic lymphocytic leukemia (CLL).
Ofatumumab is a monoclonal antibody designed to target CD20. The drug is marketed under a collaboration agreement between Genmab and Novartis.
The EC previously authorized the use of ofatumumab as a single agent to treat CLL patients who are refractory to fludarabine and alemtuzumab.
The agency also authorized the use of ofatumumab in combination with chlorambucil or bendamustine in CLL patients who have not received prior therapy and are not eligible for fludarabine-based therapy.
The EC’s decision to approve the use of ofatumumab in combination with FC was based on results from the phase 3 COMPLEMENT 2 study, which were published in Leukemia & Lymphoma in October.
The trial enrolled 365 patients with relapsed CLL. The patients were randomized 1:1 to receive up to 6 cycles of ofatumumab in combination with FC or up to 6 cycles of FC alone.
The primary endpoint was progression-free survival, as assessed by an independent review committee.
The median progression-free survival was 28.9 months for patients receiving ofatumumab plus FC, compared to 18.8 months for patients receiving FC only (hazard ratio=0.67, P=0.0032).
The incidence of grade 3 or higher adverse events was 74% in the ofatumumab-plus-FC arm and 69% in the FC-only arm. Neutropenia was the most common of these events, occurring in 49% and 36% of patients, respectively. ![]()

Photo courtesy of GSK
The European Commission (EC) has granted marketing authorization for ofatumumab (Arzerra®) to be used in combination with fludarabine and cyclophosphamide (FC) in the treatment of adults with relapsed chronic lymphocytic leukemia (CLL).
Ofatumumab is a monoclonal antibody designed to target CD20. The drug is marketed under a collaboration agreement between Genmab and Novartis.
The EC previously authorized the use of ofatumumab as a single agent to treat CLL patients who are refractory to fludarabine and alemtuzumab.
The agency also authorized the use of ofatumumab in combination with chlorambucil or bendamustine in CLL patients who have not received prior therapy and are not eligible for fludarabine-based therapy.
The EC’s decision to approve the use of ofatumumab in combination with FC was based on results from the phase 3 COMPLEMENT 2 study, which were published in Leukemia & Lymphoma in October.
The trial enrolled 365 patients with relapsed CLL. The patients were randomized 1:1 to receive up to 6 cycles of ofatumumab in combination with FC or up to 6 cycles of FC alone.
The primary endpoint was progression-free survival, as assessed by an independent review committee.
The median progression-free survival was 28.9 months for patients receiving ofatumumab plus FC, compared to 18.8 months for patients receiving FC only (hazard ratio=0.67, P=0.0032).
The incidence of grade 3 or higher adverse events was 74% in the ofatumumab-plus-FC arm and 69% in the FC-only arm. Neutropenia was the most common of these events, occurring in 49% and 36% of patients, respectively. ![]()
EC grants venetoclax conditional approval for CLL
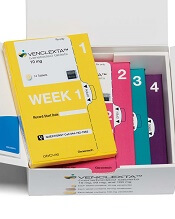
(US version, Venclexta)
Photo courtesy of Abbvie
The European Commission (EC) has granted conditional marketing authorization for the oral BCL-2 inhibitor venetoclax (Venclyxto™) to treat certain patients with chronic lymphocytic leukemia (CLL).
The drug is now approved as monotherapy to treat adults with CLL who have 17p deletion or TP53 mutation and are unsuitable for or have failed a B-cell receptor pathway inhibitor.
Venetoclax is also approved as monotherapy to treat CLL in the absence of 17p deletion or TP53 mutation in adults who have failed both chemoimmunotherapy and a B-cell receptor pathway inhibitor.
Venetoclax is the first BCL-2 inhibitor authorized for use in Europe.
Conditional marketing authorization represents an expedited path for approval. The EC grants conditional marketing authorization to products whose benefits are thought to outweigh their risks, products that address unmet needs, and products that are expected to provide a significant public health benefit.
Conditional marketing authorization is granted before pivotal registration studies of a product are completed, but the company developing the product is required to complete post-marketing studies showing that the product provides a clinical benefit.
Venetoclax is being developed by AbbVie and Genentech, a member of the Roche Group. The drug is jointly commercialized by the companies in the US and by AbbVie outside of the US.
Phase 2 trials
Venetoclax has produced high objective response rates (ORR) in two phase 2 trials of CLL patients.
In one of these trials, researchers tested venetoclax in 107 patients with previously treated CLL and 17p deletion. The results were published in The Lancet Oncology in June.
The ORR in this trial was 79%. At the time of analysis, the median duration of response had not been reached. The same was true for progression-free survival and overall survival.
The progression-free survival estimate for 12 months was 72%, and the overall survival estimate was 87%.
The incidence of treatment-emergent adverse events was 96%, and the incidence of serious adverse events was 55%.
Grade 3 laboratory tumor lysis syndrome (TLS) was reported in 5 patients. Three of these patients continued on venetoclax, but 2 patients required a dose interruption of 1 day each.
In the second trial, researchers tested venetoclax in 64 patients with CLL who had failed treatment with ibrutinib and/or idelalisib. Results from this trial were presented at the 2016 ASH Annual Meeting.
The ORR was 67%. At 11.8 months of follow-up, the median duration of response, progression-free survival, and overall survival had not been reached. The estimated 12-month progression-free survival was 80%.
The incidence of adverse events was 100%, and the incidence of serious adverse events was 53%. No clinical TLS was observed, but 1 patient met Howard criteria for laboratory TLS. ![]()
(US version, Venclexta)
Photo courtesy of Abbvie
The European Commission (EC) has granted conditional marketing authorization for the oral BCL-2 inhibitor venetoclax (Venclyxto™) to treat certain patients with chronic lymphocytic leukemia (CLL).
The drug is now approved as monotherapy to treat adults with CLL who have 17p deletion or TP53 mutation and are unsuitable for or have failed a B-cell receptor pathway inhibitor.
Venetoclax is also approved as monotherapy to treat CLL in the absence of 17p deletion or TP53 mutation in adults who have failed both chemoimmunotherapy and a B-cell receptor pathway inhibitor.
Venetoclax is the first BCL-2 inhibitor authorized for use in Europe.
Conditional marketing authorization represents an expedited path for approval. The EC grants conditional marketing authorization to products whose benefits are thought to outweigh their risks, products that address unmet needs, and products that are expected to provide a significant public health benefit.
Conditional marketing authorization is granted before pivotal registration studies of a product are completed, but the company developing the product is required to complete post-marketing studies showing that the product provides a clinical benefit.
Venetoclax is being developed by AbbVie and Genentech, a member of the Roche Group. The drug is jointly commercialized by the companies in the US and by AbbVie outside of the US.
Phase 2 trials
Venetoclax has produced high objective response rates (ORR) in two phase 2 trials of CLL patients.
In one of these trials, researchers tested venetoclax in 107 patients with previously treated CLL and 17p deletion. The results were published in The Lancet Oncology in June.
The ORR in this trial was 79%. At the time of analysis, the median duration of response had not been reached. The same was true for progression-free survival and overall survival.
The progression-free survival estimate for 12 months was 72%, and the overall survival estimate was 87%.
The incidence of treatment-emergent adverse events was 96%, and the incidence of serious adverse events was 55%.
Grade 3 laboratory tumor lysis syndrome (TLS) was reported in 5 patients. Three of these patients continued on venetoclax, but 2 patients required a dose interruption of 1 day each.
In the second trial, researchers tested venetoclax in 64 patients with CLL who had failed treatment with ibrutinib and/or idelalisib. Results from this trial were presented at the 2016 ASH Annual Meeting.
The ORR was 67%. At 11.8 months of follow-up, the median duration of response, progression-free survival, and overall survival had not been reached. The estimated 12-month progression-free survival was 80%.
The incidence of adverse events was 100%, and the incidence of serious adverse events was 53%. No clinical TLS was observed, but 1 patient met Howard criteria for laboratory TLS. ![]()
(US version, Venclexta)
Photo courtesy of Abbvie
The European Commission (EC) has granted conditional marketing authorization for the oral BCL-2 inhibitor venetoclax (Venclyxto™) to treat certain patients with chronic lymphocytic leukemia (CLL).
The drug is now approved as monotherapy to treat adults with CLL who have 17p deletion or TP53 mutation and are unsuitable for or have failed a B-cell receptor pathway inhibitor.
Venetoclax is also approved as monotherapy to treat CLL in the absence of 17p deletion or TP53 mutation in adults who have failed both chemoimmunotherapy and a B-cell receptor pathway inhibitor.
Venetoclax is the first BCL-2 inhibitor authorized for use in Europe.
Conditional marketing authorization represents an expedited path for approval. The EC grants conditional marketing authorization to products whose benefits are thought to outweigh their risks, products that address unmet needs, and products that are expected to provide a significant public health benefit.
Conditional marketing authorization is granted before pivotal registration studies of a product are completed, but the company developing the product is required to complete post-marketing studies showing that the product provides a clinical benefit.
Venetoclax is being developed by AbbVie and Genentech, a member of the Roche Group. The drug is jointly commercialized by the companies in the US and by AbbVie outside of the US.
Phase 2 trials
Venetoclax has produced high objective response rates (ORR) in two phase 2 trials of CLL patients.
In one of these trials, researchers tested venetoclax in 107 patients with previously treated CLL and 17p deletion. The results were published in The Lancet Oncology in June.
The ORR in this trial was 79%. At the time of analysis, the median duration of response had not been reached. The same was true for progression-free survival and overall survival.
The progression-free survival estimate for 12 months was 72%, and the overall survival estimate was 87%.
The incidence of treatment-emergent adverse events was 96%, and the incidence of serious adverse events was 55%.
Grade 3 laboratory tumor lysis syndrome (TLS) was reported in 5 patients. Three of these patients continued on venetoclax, but 2 patients required a dose interruption of 1 day each.
In the second trial, researchers tested venetoclax in 64 patients with CLL who had failed treatment with ibrutinib and/or idelalisib. Results from this trial were presented at the 2016 ASH Annual Meeting.
The ORR was 67%. At 11.8 months of follow-up, the median duration of response, progression-free survival, and overall survival had not been reached. The estimated 12-month progression-free survival was 80%.
The incidence of adverse events was 100%, and the incidence of serious adverse events was 53%. No clinical TLS was observed, but 1 patient met Howard criteria for laboratory TLS. ![]()
Drug produces responses in ‘challenging’ patients

© Todd Buchanan 2016
SAN DIEGO—The oral BCL-2 inhibitor venetoclax can produce high objective response rates (ORRs) in chronic lymphocytic leukemia (CLL) patients who have failed treatment with at least one B-cell receptor inhibitor, according to investigators.
In a phase 2 study, venetoclax produced an ORR of 67% among all patients enrolled.
The drug produced a 70% ORR among patients who had failed treatment with ibrutinib and a 62% ORR among patients who had failed idelalisib.
“This represents the first prospective study in this patient population and does demonstrate high rates of durable responses, certainly making [venetoclax] a very viable option for a challenging group of patients to treat,” said study investigator Jeffrey Jones, MD, of The Ohio State University in Columbus.
Dr Jones presented results from this trial at the 2016 ASH Annual Meeting (abstract 637*). This study is sponsored by AbbVie in collaboration with Genentech/Roche.
The trial enrolled patients with CLL who relapsed after or were refractory to ibrutinib (arm A) or idelalisib (arm B). At the time of the data cut-off, 64 patients had been enrolled and treated with venetoclax, including 43 patients in arm A and 21 in arm B.
Patients received venetoclax via a recommended dose-titration schedule—20 mg once daily in week 1, 50 mg daily in week 2, 100 mg daily in week 3, 200 mg daily in week 4, and 400 mg daily from week 5 onward. Patients continued to receive the drug until disease progression or unacceptable toxicity.
To mitigate the risk of tumor lysis syndrome (TLS), patients received prophylaxis with uric acid lowering agents and hydration starting at least 72 hours before the first dose of venetoclax.
Patients with a high tumor burden were hospitalized for the first 20 mg dose and the first 50 mg dose, and they received intravenous hydration and rasburicase. Laboratory values were monitored at the first dose and all dose increases.
Patient characteristics: Arm A
Among patients who had failed ibrutinib, the median age was 66 (range, 48-80). Forty-nine percent of the patients had del(17p), and 35% had bulky nodal disease (5 cm or greater).
The median number of prior treatments was 4 (range, 1-12). All patients had received ibrutinib, but 9% had also received idelalisib. Ninety-one percent of patients were refractory to ibrutinib, and 5% were refractory to idelalisib.
The median time on ibrutinib was 17 months (range, 1-56), and the median time on idelalisib was 10 months (range, 2-31).
Patient characteristics: Arm B
Among patients who had failed idelalisib, the median age was 68 (range, 56-85). Ten percent of patients had del(17p), and 52% had bulky nodal disease (5 cm or greater).
The median number of prior treatments was 3 (range, 1-11). All patients had received idelalisib, but 24% had also received ibrutinib. Sixty-seven percent of patients were refractory to idelalisib, and 10% were refractory to ibrutinib.
The median time on idelalisib was 8 months (range, 1-27), and the median time on ibrutinib was 6 months (range, 2-11).
Results: Arm A
The median time on study in arm A was 13 months (range, 0.1-18). Eighteen patients in this arm discontinued the study—12 due to disease progression, 3 due to adverse events (AEs), 2 due to stem cell transplant, and 1 patient withdrew consent.
The ORR was 70% according to an independent review committee (IRC) and 67% according to investigators.
The rate of complete response (CR) was 0%, and the rate of CR with incomplete bone marrow recovery (CRi) was 2% according to the IRC. According to investigators, the CR rate was 5%, and the CRi rate was 2%.
Sixty-seven percent of patients had a partial response (PR) according to the IRC, and 56% had a PR according to investigators.
Results: Arm B
The median time on study in arm B was 9 months (range, 1.3-16). Four patients in this arm discontinued the study—3 related to disease progression and 1 for an “other” reason.
The ORR was 62% according to the IRC and 57% according to investigators.
The rate of CR/CRi was 0% according to the IRC. According to investigators, the CR rate was 10%, and the CRi rate was 5%.
Sixty-two percent of patients had a PR according to the IRC, and 43% had a PR according to investigators.
Results: Overall
The ORR was 67% according to the IRC and 64% according to investigators.
Forty-five percent of patient samples analyzed (14/31) demonstrated minimal residual disease (MRD) negativity in the peripheral blood between weeks 24 and 48. Five patients with sustained MRD negativity had bone marrow evaluations, and 1 was MRD negative.
At 11.8 months of follow-up, the median duration of response, progression-free survival, and overall survival had not been reached. The estimated 12-month progression-free survival for all patients was 80%.
“Venetoclax has been well-tolerated,” Dr Jones noted. “The toxicity profile in this study is consistent with previous reports. Most of the toxicity has been cytopenias, which can be managed with dose adjustments or supportive care interventions, such as G-CSF.”
All 64 patients experienced an AE. Common AEs were neutropenia (58%), thrombocytopenia (44%), diarrhea (42%), nausea (41%), anemia (36%), fatigue (31%), decreased white blood cell count (22%), and hyperphosphatemia (22%).
Eighty-three percent of patients had grade 3/4 AEs, including neutropenia (45%), thrombocytopenia (28%), anemia (22%), decreased white blood cell count (13%), febrile neutropenia (11%), and pneumonia (11%).
Fifty-three percent of patients had serious AEs, including febrile neutropenia (9%), pneumonia (8%), multi-organ failure (3%), septic shock (3%), and increased potassium (3%).
There were no cases of clinical TLS. However, 1 patient with high tumor burden met Howard criteria for laboratory TLS. ![]()
*Information presented at the meeting differs from the abstract.

© Todd Buchanan 2016
SAN DIEGO—The oral BCL-2 inhibitor venetoclax can produce high objective response rates (ORRs) in chronic lymphocytic leukemia (CLL) patients who have failed treatment with at least one B-cell receptor inhibitor, according to investigators.
In a phase 2 study, venetoclax produced an ORR of 67% among all patients enrolled.
The drug produced a 70% ORR among patients who had failed treatment with ibrutinib and a 62% ORR among patients who had failed idelalisib.
“This represents the first prospective study in this patient population and does demonstrate high rates of durable responses, certainly making [venetoclax] a very viable option for a challenging group of patients to treat,” said study investigator Jeffrey Jones, MD, of The Ohio State University in Columbus.
Dr Jones presented results from this trial at the 2016 ASH Annual Meeting (abstract 637*). This study is sponsored by AbbVie in collaboration with Genentech/Roche.
The trial enrolled patients with CLL who relapsed after or were refractory to ibrutinib (arm A) or idelalisib (arm B). At the time of the data cut-off, 64 patients had been enrolled and treated with venetoclax, including 43 patients in arm A and 21 in arm B.
Patients received venetoclax via a recommended dose-titration schedule—20 mg once daily in week 1, 50 mg daily in week 2, 100 mg daily in week 3, 200 mg daily in week 4, and 400 mg daily from week 5 onward. Patients continued to receive the drug until disease progression or unacceptable toxicity.
To mitigate the risk of tumor lysis syndrome (TLS), patients received prophylaxis with uric acid lowering agents and hydration starting at least 72 hours before the first dose of venetoclax.
Patients with a high tumor burden were hospitalized for the first 20 mg dose and the first 50 mg dose, and they received intravenous hydration and rasburicase. Laboratory values were monitored at the first dose and all dose increases.
Patient characteristics: Arm A
Among patients who had failed ibrutinib, the median age was 66 (range, 48-80). Forty-nine percent of the patients had del(17p), and 35% had bulky nodal disease (5 cm or greater).
The median number of prior treatments was 4 (range, 1-12). All patients had received ibrutinib, but 9% had also received idelalisib. Ninety-one percent of patients were refractory to ibrutinib, and 5% were refractory to idelalisib.
The median time on ibrutinib was 17 months (range, 1-56), and the median time on idelalisib was 10 months (range, 2-31).
Patient characteristics: Arm B
Among patients who had failed idelalisib, the median age was 68 (range, 56-85). Ten percent of patients had del(17p), and 52% had bulky nodal disease (5 cm or greater).
The median number of prior treatments was 3 (range, 1-11). All patients had received idelalisib, but 24% had also received ibrutinib. Sixty-seven percent of patients were refractory to idelalisib, and 10% were refractory to ibrutinib.
The median time on idelalisib was 8 months (range, 1-27), and the median time on ibrutinib was 6 months (range, 2-11).
Results: Arm A
The median time on study in arm A was 13 months (range, 0.1-18). Eighteen patients in this arm discontinued the study—12 due to disease progression, 3 due to adverse events (AEs), 2 due to stem cell transplant, and 1 patient withdrew consent.
The ORR was 70% according to an independent review committee (IRC) and 67% according to investigators.
The rate of complete response (CR) was 0%, and the rate of CR with incomplete bone marrow recovery (CRi) was 2% according to the IRC. According to investigators, the CR rate was 5%, and the CRi rate was 2%.
Sixty-seven percent of patients had a partial response (PR) according to the IRC, and 56% had a PR according to investigators.
Results: Arm B
The median time on study in arm B was 9 months (range, 1.3-16). Four patients in this arm discontinued the study—3 related to disease progression and 1 for an “other” reason.
The ORR was 62% according to the IRC and 57% according to investigators.
The rate of CR/CRi was 0% according to the IRC. According to investigators, the CR rate was 10%, and the CRi rate was 5%.
Sixty-two percent of patients had a PR according to the IRC, and 43% had a PR according to investigators.
Results: Overall
The ORR was 67% according to the IRC and 64% according to investigators.
Forty-five percent of patient samples analyzed (14/31) demonstrated minimal residual disease (MRD) negativity in the peripheral blood between weeks 24 and 48. Five patients with sustained MRD negativity had bone marrow evaluations, and 1 was MRD negative.
At 11.8 months of follow-up, the median duration of response, progression-free survival, and overall survival had not been reached. The estimated 12-month progression-free survival for all patients was 80%.
“Venetoclax has been well-tolerated,” Dr Jones noted. “The toxicity profile in this study is consistent with previous reports. Most of the toxicity has been cytopenias, which can be managed with dose adjustments or supportive care interventions, such as G-CSF.”
All 64 patients experienced an AE. Common AEs were neutropenia (58%), thrombocytopenia (44%), diarrhea (42%), nausea (41%), anemia (36%), fatigue (31%), decreased white blood cell count (22%), and hyperphosphatemia (22%).
Eighty-three percent of patients had grade 3/4 AEs, including neutropenia (45%), thrombocytopenia (28%), anemia (22%), decreased white blood cell count (13%), febrile neutropenia (11%), and pneumonia (11%).
Fifty-three percent of patients had serious AEs, including febrile neutropenia (9%), pneumonia (8%), multi-organ failure (3%), septic shock (3%), and increased potassium (3%).
There were no cases of clinical TLS. However, 1 patient with high tumor burden met Howard criteria for laboratory TLS. ![]()
*Information presented at the meeting differs from the abstract.

© Todd Buchanan 2016
SAN DIEGO—The oral BCL-2 inhibitor venetoclax can produce high objective response rates (ORRs) in chronic lymphocytic leukemia (CLL) patients who have failed treatment with at least one B-cell receptor inhibitor, according to investigators.
In a phase 2 study, venetoclax produced an ORR of 67% among all patients enrolled.
The drug produced a 70% ORR among patients who had failed treatment with ibrutinib and a 62% ORR among patients who had failed idelalisib.
“This represents the first prospective study in this patient population and does demonstrate high rates of durable responses, certainly making [venetoclax] a very viable option for a challenging group of patients to treat,” said study investigator Jeffrey Jones, MD, of The Ohio State University in Columbus.
Dr Jones presented results from this trial at the 2016 ASH Annual Meeting (abstract 637*). This study is sponsored by AbbVie in collaboration with Genentech/Roche.
The trial enrolled patients with CLL who relapsed after or were refractory to ibrutinib (arm A) or idelalisib (arm B). At the time of the data cut-off, 64 patients had been enrolled and treated with venetoclax, including 43 patients in arm A and 21 in arm B.
Patients received venetoclax via a recommended dose-titration schedule—20 mg once daily in week 1, 50 mg daily in week 2, 100 mg daily in week 3, 200 mg daily in week 4, and 400 mg daily from week 5 onward. Patients continued to receive the drug until disease progression or unacceptable toxicity.
To mitigate the risk of tumor lysis syndrome (TLS), patients received prophylaxis with uric acid lowering agents and hydration starting at least 72 hours before the first dose of venetoclax.
Patients with a high tumor burden were hospitalized for the first 20 mg dose and the first 50 mg dose, and they received intravenous hydration and rasburicase. Laboratory values were monitored at the first dose and all dose increases.
Patient characteristics: Arm A
Among patients who had failed ibrutinib, the median age was 66 (range, 48-80). Forty-nine percent of the patients had del(17p), and 35% had bulky nodal disease (5 cm or greater).
The median number of prior treatments was 4 (range, 1-12). All patients had received ibrutinib, but 9% had also received idelalisib. Ninety-one percent of patients were refractory to ibrutinib, and 5% were refractory to idelalisib.
The median time on ibrutinib was 17 months (range, 1-56), and the median time on idelalisib was 10 months (range, 2-31).
Patient characteristics: Arm B
Among patients who had failed idelalisib, the median age was 68 (range, 56-85). Ten percent of patients had del(17p), and 52% had bulky nodal disease (5 cm or greater).
The median number of prior treatments was 3 (range, 1-11). All patients had received idelalisib, but 24% had also received ibrutinib. Sixty-seven percent of patients were refractory to idelalisib, and 10% were refractory to ibrutinib.
The median time on idelalisib was 8 months (range, 1-27), and the median time on ibrutinib was 6 months (range, 2-11).
Results: Arm A
The median time on study in arm A was 13 months (range, 0.1-18). Eighteen patients in this arm discontinued the study—12 due to disease progression, 3 due to adverse events (AEs), 2 due to stem cell transplant, and 1 patient withdrew consent.
The ORR was 70% according to an independent review committee (IRC) and 67% according to investigators.
The rate of complete response (CR) was 0%, and the rate of CR with incomplete bone marrow recovery (CRi) was 2% according to the IRC. According to investigators, the CR rate was 5%, and the CRi rate was 2%.
Sixty-seven percent of patients had a partial response (PR) according to the IRC, and 56% had a PR according to investigators.
Results: Arm B
The median time on study in arm B was 9 months (range, 1.3-16). Four patients in this arm discontinued the study—3 related to disease progression and 1 for an “other” reason.
The ORR was 62% according to the IRC and 57% according to investigators.
The rate of CR/CRi was 0% according to the IRC. According to investigators, the CR rate was 10%, and the CRi rate was 5%.
Sixty-two percent of patients had a PR according to the IRC, and 43% had a PR according to investigators.
Results: Overall
The ORR was 67% according to the IRC and 64% according to investigators.
Forty-five percent of patient samples analyzed (14/31) demonstrated minimal residual disease (MRD) negativity in the peripheral blood between weeks 24 and 48. Five patients with sustained MRD negativity had bone marrow evaluations, and 1 was MRD negative.
At 11.8 months of follow-up, the median duration of response, progression-free survival, and overall survival had not been reached. The estimated 12-month progression-free survival for all patients was 80%.
“Venetoclax has been well-tolerated,” Dr Jones noted. “The toxicity profile in this study is consistent with previous reports. Most of the toxicity has been cytopenias, which can be managed with dose adjustments or supportive care interventions, such as G-CSF.”
All 64 patients experienced an AE. Common AEs were neutropenia (58%), thrombocytopenia (44%), diarrhea (42%), nausea (41%), anemia (36%), fatigue (31%), decreased white blood cell count (22%), and hyperphosphatemia (22%).
Eighty-three percent of patients had grade 3/4 AEs, including neutropenia (45%), thrombocytopenia (28%), anemia (22%), decreased white blood cell count (13%), febrile neutropenia (11%), and pneumonia (11%).
Fifty-three percent of patients had serious AEs, including febrile neutropenia (9%), pneumonia (8%), multi-organ failure (3%), septic shock (3%), and increased potassium (3%).
There were no cases of clinical TLS. However, 1 patient with high tumor burden met Howard criteria for laboratory TLS.
*Information presented at the meeting differs from the abstract.
Group estimates global cancer cases, deaths in 2015

receiving chemotherapy
Photo by Rhoda Baer
Researchers have estimated the global incidence of 32 cancer types and deaths related to these malignancies in 2015.
The group’s data, published in JAMA Oncology, suggest there were 17.5 million cancer cases and 8.7 million cancer deaths last year.
There were 78,000 cases of Hodgkin lymphoma and 24,000 deaths from the disease, as well as 666,000 cases of non-Hodgkin lymphoma (NHL) and 231,000 NHL deaths.
There were 154,000 cases of multiple myeloma and 101,000 deaths from the disease.
And there were 606,000 cases of leukemia, with 353,000 leukemia deaths. This included 161,000 cases of acute lymphoid leukemia (110,000 deaths), 191,000 cases of chronic lymphoid leukemia (61,000 deaths), 190,000 cases of acute myeloid leukemia (147,000 deaths), and 64,000 cases of chronic myeloid leukemia (35,000 deaths).
The data also show that, between 2005 and 2015, cancer cases increased by 33%, mostly due to population aging and growth, plus changes in age-specific cancer rates.
Globally, the odds of developing cancer during a lifetime were 1 in 3 for men and 1 in 4 for women in 2015.
Prostate cancer was the most common cancer in men (1.6 million cases), although tracheal, bronchus, and lung cancer was the leading cause of cancer deaths for men.
Breast cancer was the most common cancer for women (2.4 million cases) and the leading cause of cancer deaths in women.
The most common childhood cancers were leukemia, “other neoplasms,” NHL, and brain and nervous system cancers.

receiving chemotherapy
Photo by Rhoda Baer
Researchers have estimated the global incidence of 32 cancer types and deaths related to these malignancies in 2015.
The group’s data, published in JAMA Oncology, suggest there were 17.5 million cancer cases and 8.7 million cancer deaths last year.
There were 78,000 cases of Hodgkin lymphoma and 24,000 deaths from the disease, as well as 666,000 cases of non-Hodgkin lymphoma (NHL) and 231,000 NHL deaths.
There were 154,000 cases of multiple myeloma and 101,000 deaths from the disease.
And there were 606,000 cases of leukemia, with 353,000 leukemia deaths. This included 161,000 cases of acute lymphoid leukemia (110,000 deaths), 191,000 cases of chronic lymphoid leukemia (61,000 deaths), 190,000 cases of acute myeloid leukemia (147,000 deaths), and 64,000 cases of chronic myeloid leukemia (35,000 deaths).
The data also show that, between 2005 and 2015, cancer cases increased by 33%, mostly due to population aging and growth, plus changes in age-specific cancer rates.
Globally, the odds of developing cancer during a lifetime were 1 in 3 for men and 1 in 4 for women in 2015.
Prostate cancer was the most common cancer in men (1.6 million cases), although tracheal, bronchus, and lung cancer was the leading cause of cancer deaths for men.
Breast cancer was the most common cancer for women (2.4 million cases) and the leading cause of cancer deaths in women.
The most common childhood cancers were leukemia, “other neoplasms,” NHL, and brain and nervous system cancers.

receiving chemotherapy
Photo by Rhoda Baer
Researchers have estimated the global incidence of 32 cancer types and deaths related to these malignancies in 2015.
The group’s data, published in JAMA Oncology, suggest there were 17.5 million cancer cases and 8.7 million cancer deaths last year.
There were 78,000 cases of Hodgkin lymphoma and 24,000 deaths from the disease, as well as 666,000 cases of non-Hodgkin lymphoma (NHL) and 231,000 NHL deaths.
There were 154,000 cases of multiple myeloma and 101,000 deaths from the disease.
And there were 606,000 cases of leukemia, with 353,000 leukemia deaths. This included 161,000 cases of acute lymphoid leukemia (110,000 deaths), 191,000 cases of chronic lymphoid leukemia (61,000 deaths), 190,000 cases of acute myeloid leukemia (147,000 deaths), and 64,000 cases of chronic myeloid leukemia (35,000 deaths).
The data also show that, between 2005 and 2015, cancer cases increased by 33%, mostly due to population aging and growth, plus changes in age-specific cancer rates.
Globally, the odds of developing cancer during a lifetime were 1 in 3 for men and 1 in 4 for women in 2015.
Prostate cancer was the most common cancer in men (1.6 million cases), although tracheal, bronchus, and lung cancer was the leading cause of cancer deaths for men.
Breast cancer was the most common cancer for women (2.4 million cases) and the leading cause of cancer deaths in women.
The most common childhood cancers were leukemia, “other neoplasms,” NHL, and brain and nervous system cancers.
Data suggest one BTK inhibitor could replace another
ASH Annual Meeting
SAN DIEGO—When patients with chronic lymphocytic leukemia (CLL) cannot tolerate one Bruton’s tyrosine kinase (BTK) inhibitor, they may do well on another, according to a presentation at the 2016 ASH Annual Meeting.
Researchers conducting a phase 1/2 study found that acalabrutinib was “well-tolerated” and demonstrated “promising activity” in patients intolerant to ibrutinib.
Seventy-nine percent of patients responded to acalabrutinib.
And although 36% of patients had a recurrence of an adverse event (AE) they experienced while on ibrutinib, none of the patients discontinued acalabrutinib due to AE recurrence.
Farrukh T. Awan, MD, of The Ohio State University in Columbus, Ohio, presented these results at the meeting as abstract 638.*
Dr Awan noted that integrating ibrutinib into standard CLL therapy has improved patient outcomes, but a lack of tolerability observed in some patients suggests that more selective BTK inhibition may be desirable.
“We know that around 10% to 20% of patients who are treated with ibrutinib would have to stop therapy because of an adverse event,” Dr Awan said. “Acalabrutinib is a highly selective, potent BTK inhibitor that has shown promising efficacy, and that [research] was published last year.”
In this ongoing, phase 1/2 study, Dr Awan and his colleagues are testing acalabrutinib in patients with CLL/small lymphocytic leukemia. The study has enrolled multiple cohorts of patients—relapsed/refractory, treatment-naïve, Richter’s transformation/prolymphocytic leukemia, and ibrutinib intolerant.
At this year’s ASH meeting, Dr Awan presented data on the 33 CLL patients who were ibrutinib intolerant. The patients’ median age was 64 (range, 50-82), 61% were male, 97% had an ECOG performance status of 0-1, 52% had Rai stage III-IV, and 31% had bulky disease.
The median number of prior therapies was 4 (range, 2-13), and 91% of patients had ibrutinib as their last therapy. The median duration of prior ibrutinib treatment was 11.5 months (range, 1-62), and the median time from ending ibrutinib to starting acalabrutinib was 47 days (range, 3-331 days).
Treatment and safety
Patients received acalabrutinib at 100 mg twice daily (n=30) or 200 mg daily (n=3) until disease progression or discontinuation for another reason. The patients’ median time on therapy was 12.2 months (range, 0.2-23.6 months).
Nine patients discontinued treatment—3 due to disease progression, 3 due to AEs, 2 due to an increase in BTK C481S mutation frequency in the peripheral blood and central nervous system involvement, and 1 due to physician decision (because the patient had concurrent hemophilia).
The 3 AEs that led to treatment discontinuation were fatal hemorrhagic stroke, fatal fungal infection, and metastatic endometrial cancer. All 3 events were considered unrelated to acalabrutinib.
Serious AEs occurred in 11 patients (33%). A serious AE that occurred in more than 1 patient was pneumonia (n=2).
The most common AEs were diarrhea (52%, grade 1-2), headache (39%, grade 1-2), cough (24%, grade 1-2), increased weight (24%, grade 1-2), nausea (21%, grade 1-2), contusion (18%, grade 1-2), ecchymosis (18%, grade 1-2), fatigue (18%, grade 1-2), hypertension (18% overall, 6% ≥ grade 3), pyrexia (18% overall, 3% ≥ grade 3), vomiting (18%, grade 1-2), myalgia (15% overall, 3% ≥ grade 3), rash (15%, grade 1-2), stomatitis (15%, grade 1-2), upper respiratory tract infection (15%, grade 1-2), and urinary tract infection (15%, grade 1-2).
AE recurrence
Twelve patients (36%) had a recurrence of ibrutinib-related AEs—a total of 16 events. Fourteen of these events either decreased in severity or were unchanged with acalabrutinib treatment.
The events without a change in severity were atrial fibrillation (n=1), fatigue (n=1), muscle spasms (n=1), myalgia (n=1), peripheral edema (n=1), panniculitis (n=1), and rash (n=1).
The events that decreased in severity were diarrhea (n=2), arthralgia (n=1), ecchymosis (n=1), fatigue (n=1), panniculitis (n=1), and rash (n=1).
The events that increased in severity were contusion (n=1, grade 1 to 2) and fatigue (n=1, grade 1 to 2).
None of the patients discontinued acalabrutinib due to AE recurrence.
Efficacy
Twenty-nine patients were evaluable for efficacy.
The overall response rate was 79% (n=23). One patient had a complete response (3%), 15 had a partial response (52%), and 7 had a partial response with lymphocytosis (24%). Six patients had stable disease (21%).
The median time to response was 1.9 months. Eighty-one percent of responding patients have a response duration of 12 months or longer.
The median progression-free survival has not been reached.
The research is sponsored by Acerta Pharma.
*Information presented at the meeting differs from the abstract.
ASH Annual Meeting
SAN DIEGO—When patients with chronic lymphocytic leukemia (CLL) cannot tolerate one Bruton’s tyrosine kinase (BTK) inhibitor, they may do well on another, according to a presentation at the 2016 ASH Annual Meeting.
Researchers conducting a phase 1/2 study found that acalabrutinib was “well-tolerated” and demonstrated “promising activity” in patients intolerant to ibrutinib.
Seventy-nine percent of patients responded to acalabrutinib.
And although 36% of patients had a recurrence of an adverse event (AE) they experienced while on ibrutinib, none of the patients discontinued acalabrutinib due to AE recurrence.
Farrukh T. Awan, MD, of The Ohio State University in Columbus, Ohio, presented these results at the meeting as abstract 638.*
Dr Awan noted that integrating ibrutinib into standard CLL therapy has improved patient outcomes, but a lack of tolerability observed in some patients suggests that more selective BTK inhibition may be desirable.
“We know that around 10% to 20% of patients who are treated with ibrutinib would have to stop therapy because of an adverse event,” Dr Awan said. “Acalabrutinib is a highly selective, potent BTK inhibitor that has shown promising efficacy, and that [research] was published last year.”
In this ongoing, phase 1/2 study, Dr Awan and his colleagues are testing acalabrutinib in patients with CLL/small lymphocytic leukemia. The study has enrolled multiple cohorts of patients—relapsed/refractory, treatment-naïve, Richter’s transformation/prolymphocytic leukemia, and ibrutinib intolerant.
At this year’s ASH meeting, Dr Awan presented data on the 33 CLL patients who were ibrutinib intolerant. The patients’ median age was 64 (range, 50-82), 61% were male, 97% had an ECOG performance status of 0-1, 52% had Rai stage III-IV, and 31% had bulky disease.
The median number of prior therapies was 4 (range, 2-13), and 91% of patients had ibrutinib as their last therapy. The median duration of prior ibrutinib treatment was 11.5 months (range, 1-62), and the median time from ending ibrutinib to starting acalabrutinib was 47 days (range, 3-331 days).
Treatment and safety
Patients received acalabrutinib at 100 mg twice daily (n=30) or 200 mg daily (n=3) until disease progression or discontinuation for another reason. The patients’ median time on therapy was 12.2 months (range, 0.2-23.6 months).
Nine patients discontinued treatment—3 due to disease progression, 3 due to AEs, 2 due to an increase in BTK C481S mutation frequency in the peripheral blood and central nervous system involvement, and 1 due to physician decision (because the patient had concurrent hemophilia).
The 3 AEs that led to treatment discontinuation were fatal hemorrhagic stroke, fatal fungal infection, and metastatic endometrial cancer. All 3 events were considered unrelated to acalabrutinib.
Serious AEs occurred in 11 patients (33%). A serious AE that occurred in more than 1 patient was pneumonia (n=2).
The most common AEs were diarrhea (52%, grade 1-2), headache (39%, grade 1-2), cough (24%, grade 1-2), increased weight (24%, grade 1-2), nausea (21%, grade 1-2), contusion (18%, grade 1-2), ecchymosis (18%, grade 1-2), fatigue (18%, grade 1-2), hypertension (18% overall, 6% ≥ grade 3), pyrexia (18% overall, 3% ≥ grade 3), vomiting (18%, grade 1-2), myalgia (15% overall, 3% ≥ grade 3), rash (15%, grade 1-2), stomatitis (15%, grade 1-2), upper respiratory tract infection (15%, grade 1-2), and urinary tract infection (15%, grade 1-2).
AE recurrence
Twelve patients (36%) had a recurrence of ibrutinib-related AEs—a total of 16 events. Fourteen of these events either decreased in severity or were unchanged with acalabrutinib treatment.
The events without a change in severity were atrial fibrillation (n=1), fatigue (n=1), muscle spasms (n=1), myalgia (n=1), peripheral edema (n=1), panniculitis (n=1), and rash (n=1).
The events that decreased in severity were diarrhea (n=2), arthralgia (n=1), ecchymosis (n=1), fatigue (n=1), panniculitis (n=1), and rash (n=1).
The events that increased in severity were contusion (n=1, grade 1 to 2) and fatigue (n=1, grade 1 to 2).
None of the patients discontinued acalabrutinib due to AE recurrence.
Efficacy
Twenty-nine patients were evaluable for efficacy.
The overall response rate was 79% (n=23). One patient had a complete response (3%), 15 had a partial response (52%), and 7 had a partial response with lymphocytosis (24%). Six patients had stable disease (21%).
The median time to response was 1.9 months. Eighty-one percent of responding patients have a response duration of 12 months or longer.
The median progression-free survival has not been reached.
The research is sponsored by Acerta Pharma.
*Information presented at the meeting differs from the abstract.
ASH Annual Meeting
SAN DIEGO—When patients with chronic lymphocytic leukemia (CLL) cannot tolerate one Bruton’s tyrosine kinase (BTK) inhibitor, they may do well on another, according to a presentation at the 2016 ASH Annual Meeting.
Researchers conducting a phase 1/2 study found that acalabrutinib was “well-tolerated” and demonstrated “promising activity” in patients intolerant to ibrutinib.
Seventy-nine percent of patients responded to acalabrutinib.
And although 36% of patients had a recurrence of an adverse event (AE) they experienced while on ibrutinib, none of the patients discontinued acalabrutinib due to AE recurrence.
Farrukh T. Awan, MD, of The Ohio State University in Columbus, Ohio, presented these results at the meeting as abstract 638.*
Dr Awan noted that integrating ibrutinib into standard CLL therapy has improved patient outcomes, but a lack of tolerability observed in some patients suggests that more selective BTK inhibition may be desirable.
“We know that around 10% to 20% of patients who are treated with ibrutinib would have to stop therapy because of an adverse event,” Dr Awan said. “Acalabrutinib is a highly selective, potent BTK inhibitor that has shown promising efficacy, and that [research] was published last year.”
In this ongoing, phase 1/2 study, Dr Awan and his colleagues are testing acalabrutinib in patients with CLL/small lymphocytic leukemia. The study has enrolled multiple cohorts of patients—relapsed/refractory, treatment-naïve, Richter’s transformation/prolymphocytic leukemia, and ibrutinib intolerant.
At this year’s ASH meeting, Dr Awan presented data on the 33 CLL patients who were ibrutinib intolerant. The patients’ median age was 64 (range, 50-82), 61% were male, 97% had an ECOG performance status of 0-1, 52% had Rai stage III-IV, and 31% had bulky disease.
The median number of prior therapies was 4 (range, 2-13), and 91% of patients had ibrutinib as their last therapy. The median duration of prior ibrutinib treatment was 11.5 months (range, 1-62), and the median time from ending ibrutinib to starting acalabrutinib was 47 days (range, 3-331 days).
Treatment and safety
Patients received acalabrutinib at 100 mg twice daily (n=30) or 200 mg daily (n=3) until disease progression or discontinuation for another reason. The patients’ median time on therapy was 12.2 months (range, 0.2-23.6 months).
Nine patients discontinued treatment—3 due to disease progression, 3 due to AEs, 2 due to an increase in BTK C481S mutation frequency in the peripheral blood and central nervous system involvement, and 1 due to physician decision (because the patient had concurrent hemophilia).
The 3 AEs that led to treatment discontinuation were fatal hemorrhagic stroke, fatal fungal infection, and metastatic endometrial cancer. All 3 events were considered unrelated to acalabrutinib.
Serious AEs occurred in 11 patients (33%). A serious AE that occurred in more than 1 patient was pneumonia (n=2).
The most common AEs were diarrhea (52%, grade 1-2), headache (39%, grade 1-2), cough (24%, grade 1-2), increased weight (24%, grade 1-2), nausea (21%, grade 1-2), contusion (18%, grade 1-2), ecchymosis (18%, grade 1-2), fatigue (18%, grade 1-2), hypertension (18% overall, 6% ≥ grade 3), pyrexia (18% overall, 3% ≥ grade 3), vomiting (18%, grade 1-2), myalgia (15% overall, 3% ≥ grade 3), rash (15%, grade 1-2), stomatitis (15%, grade 1-2), upper respiratory tract infection (15%, grade 1-2), and urinary tract infection (15%, grade 1-2).
AE recurrence
Twelve patients (36%) had a recurrence of ibrutinib-related AEs—a total of 16 events. Fourteen of these events either decreased in severity or were unchanged with acalabrutinib treatment.
The events without a change in severity were atrial fibrillation (n=1), fatigue (n=1), muscle spasms (n=1), myalgia (n=1), peripheral edema (n=1), panniculitis (n=1), and rash (n=1).
The events that decreased in severity were diarrhea (n=2), arthralgia (n=1), ecchymosis (n=1), fatigue (n=1), panniculitis (n=1), and rash (n=1).
The events that increased in severity were contusion (n=1, grade 1 to 2) and fatigue (n=1, grade 1 to 2).
None of the patients discontinued acalabrutinib due to AE recurrence.
Efficacy
Twenty-nine patients were evaluable for efficacy.
The overall response rate was 79% (n=23). One patient had a complete response (3%), 15 had a partial response (52%), and 7 had a partial response with lymphocytosis (24%). Six patients had stable disease (21%).
The median time to response was 1.9 months. Eighty-one percent of responding patients have a response duration of 12 months or longer.
The median progression-free survival has not been reached.
The research is sponsored by Acerta Pharma.
*Information presented at the meeting differs from the abstract.
Obinutuzumab bests rituximab in FL study
ASH Annual Meeting
SAN DIEGO—Interim results of the phase 3 GALLIUM trial suggest an obinutuzumab-based treatment regimen provides a progression-free survival (PFS) benefit over a rituximab-based regimen for patients with previously untreated follicular lymphoma (FL).
According to investigators, patients who received obinutuzumab plus chemotherapy followed by obinutuzumab maintenance had a “clinically meaningful” improvement in PFS, when compared to patients who received rituximab plus chemotherapy followed by rituximab maintenance.
However, there was no significant difference between the treatment arms with regard to overall survival. And the incidence of non-fatal adverse events (AEs) was higher among the patients who received obinutuzumab.
Nevertheless, the data suggest that obinutuzumab-based therapy significantly improves outcomes and should be considered as a first-line treatment for FL, according to Robert Marcus, MBBS, of King’s College Hospital in London, UK.
Dr Marcus presented data from GALLIUM during the plenary session at the 2016 ASH Annual Meeting (abstract 6). GALLIUM is sponsored by Hoffmann-La Roche.
Patients and treatment
The study has enrolled 1401 patients with previously untreated, indolent non-Hodgkin lymphoma, including 1202 with FL.
Half of the FL patients (n=601) were randomized to obinutuzumab plus chemotherapy followed by obinutuzumab alone for up to 2 years, and half were randomized to rituximab plus chemotherapy followed by rituximab alone for up to 2 years.
The different chemotherapies used were CHOP (cyclophosphamide, doxorubicin, vincristine, and prednisolone), CVP (cyclophosphamide, vincristine, and prednisolone), and bendamustine. The regimens were selected by each participating study site prior to beginning enrollment.
Baseline characteristics were similar between the treatment arms. The median age was about 60 (overall range, 23-88), roughly 40% of patients had high-risk disease, and the median time from diagnosis to randomization was about 1.5 months.
A total of 341 patients in the rituximab arm and 361 patients in the obinutuzumab arm completed maintenance therapy.
The median follow-up was 34.5 months. Maintenance is ongoing in 114 patients—54 on rituximab and 60 on obinutuzumab.
Efficacy
At the end of induction, the overall response rate was 86.9% in the rituximab arm and 88.5% in the obinutuzumab arm. The complete response rates were 23.8% and 19.5%, respectively. And the rates of stable disease were 1.3% and 0.5%, respectively.
The study’s primary endpoint is investigator-assessed PFS. The 3-year PFS rate is 73.3% in the rituximab arm and 80% in the obinutuzumab arm (hazard ratio [HR]=0.66, P=0.0012).
According to an independent review committee, the 3-year PFS is 77.9% in the rituximab arm and 81.9% in the obinutuzumab arm (HR=0.71, P=0.0138).
The 3-year overall survival is 92.1% in the rituximab arm and 94% in the obinutuzumab arm (HR=0.75, P=0.21).
Safety
The overall incidence of AEs was 98.3% in the rituximab arm and 99.5% in the obinutuzumab arm. The incidence of serious AEs was 39.9% and 46.1%, respectively.
The incidence of AEs leading to treatment discontinuation was 14.2% and 16.3%, respectively. And the incidence of second neoplasms was 2.7% and 4.7%, respectively.
Grade 5 AEs occurred in 3.4% of patients in the rituximab arm and 4.0% of patients in the obinutuzumab arm. The investigators found that fatal AEs were more common in patients taking bendamustine, regardless of the treatment arm.
Grade 3 or higher AEs occurring in at least 5% of patients in either arm (rituximab and obinutuzumab, respectively) included neutropenia (67.8% and 74.6%), leukopenia (37.9% and 43.9%), febrile neutropenia (4.9% and 6.9%), infections and infestations (3.7% and 6.7%), and thrombocytopenia (2.7% and 6.1%).
ASH Annual Meeting
SAN DIEGO—Interim results of the phase 3 GALLIUM trial suggest an obinutuzumab-based treatment regimen provides a progression-free survival (PFS) benefit over a rituximab-based regimen for patients with previously untreated follicular lymphoma (FL).
According to investigators, patients who received obinutuzumab plus chemotherapy followed by obinutuzumab maintenance had a “clinically meaningful” improvement in PFS, when compared to patients who received rituximab plus chemotherapy followed by rituximab maintenance.
However, there was no significant difference between the treatment arms with regard to overall survival. And the incidence of non-fatal adverse events (AEs) was higher among the patients who received obinutuzumab.
Nevertheless, the data suggest that obinutuzumab-based therapy significantly improves outcomes and should be considered as a first-line treatment for FL, according to Robert Marcus, MBBS, of King’s College Hospital in London, UK.
Dr Marcus presented data from GALLIUM during the plenary session at the 2016 ASH Annual Meeting (abstract 6). GALLIUM is sponsored by Hoffmann-La Roche.
Patients and treatment
The study has enrolled 1401 patients with previously untreated, indolent non-Hodgkin lymphoma, including 1202 with FL.
Half of the FL patients (n=601) were randomized to obinutuzumab plus chemotherapy followed by obinutuzumab alone for up to 2 years, and half were randomized to rituximab plus chemotherapy followed by rituximab alone for up to 2 years.
The different chemotherapies used were CHOP (cyclophosphamide, doxorubicin, vincristine, and prednisolone), CVP (cyclophosphamide, vincristine, and prednisolone), and bendamustine. The regimens were selected by each participating study site prior to beginning enrollment.
Baseline characteristics were similar between the treatment arms. The median age was about 60 (overall range, 23-88), roughly 40% of patients had high-risk disease, and the median time from diagnosis to randomization was about 1.5 months.
A total of 341 patients in the rituximab arm and 361 patients in the obinutuzumab arm completed maintenance therapy.
The median follow-up was 34.5 months. Maintenance is ongoing in 114 patients—54 on rituximab and 60 on obinutuzumab.
Efficacy
At the end of induction, the overall response rate was 86.9% in the rituximab arm and 88.5% in the obinutuzumab arm. The complete response rates were 23.8% and 19.5%, respectively. And the rates of stable disease were 1.3% and 0.5%, respectively.
The study’s primary endpoint is investigator-assessed PFS. The 3-year PFS rate is 73.3% in the rituximab arm and 80% in the obinutuzumab arm (hazard ratio [HR]=0.66, P=0.0012).
According to an independent review committee, the 3-year PFS is 77.9% in the rituximab arm and 81.9% in the obinutuzumab arm (HR=0.71, P=0.0138).
The 3-year overall survival is 92.1% in the rituximab arm and 94% in the obinutuzumab arm (HR=0.75, P=0.21).
Safety
The overall incidence of AEs was 98.3% in the rituximab arm and 99.5% in the obinutuzumab arm. The incidence of serious AEs was 39.9% and 46.1%, respectively.
The incidence of AEs leading to treatment discontinuation was 14.2% and 16.3%, respectively. And the incidence of second neoplasms was 2.7% and 4.7%, respectively.
Grade 5 AEs occurred in 3.4% of patients in the rituximab arm and 4.0% of patients in the obinutuzumab arm. The investigators found that fatal AEs were more common in patients taking bendamustine, regardless of the treatment arm.
Grade 3 or higher AEs occurring in at least 5% of patients in either arm (rituximab and obinutuzumab, respectively) included neutropenia (67.8% and 74.6%), leukopenia (37.9% and 43.9%), febrile neutropenia (4.9% and 6.9%), infections and infestations (3.7% and 6.7%), and thrombocytopenia (2.7% and 6.1%).
ASH Annual Meeting
SAN DIEGO—Interim results of the phase 3 GALLIUM trial suggest an obinutuzumab-based treatment regimen provides a progression-free survival (PFS) benefit over a rituximab-based regimen for patients with previously untreated follicular lymphoma (FL).
According to investigators, patients who received obinutuzumab plus chemotherapy followed by obinutuzumab maintenance had a “clinically meaningful” improvement in PFS, when compared to patients who received rituximab plus chemotherapy followed by rituximab maintenance.
However, there was no significant difference between the treatment arms with regard to overall survival. And the incidence of non-fatal adverse events (AEs) was higher among the patients who received obinutuzumab.
Nevertheless, the data suggest that obinutuzumab-based therapy significantly improves outcomes and should be considered as a first-line treatment for FL, according to Robert Marcus, MBBS, of King’s College Hospital in London, UK.
Dr Marcus presented data from GALLIUM during the plenary session at the 2016 ASH Annual Meeting (abstract 6). GALLIUM is sponsored by Hoffmann-La Roche.
Patients and treatment
The study has enrolled 1401 patients with previously untreated, indolent non-Hodgkin lymphoma, including 1202 with FL.
Half of the FL patients (n=601) were randomized to obinutuzumab plus chemotherapy followed by obinutuzumab alone for up to 2 years, and half were randomized to rituximab plus chemotherapy followed by rituximab alone for up to 2 years.
The different chemotherapies used were CHOP (cyclophosphamide, doxorubicin, vincristine, and prednisolone), CVP (cyclophosphamide, vincristine, and prednisolone), and bendamustine. The regimens were selected by each participating study site prior to beginning enrollment.
Baseline characteristics were similar between the treatment arms. The median age was about 60 (overall range, 23-88), roughly 40% of patients had high-risk disease, and the median time from diagnosis to randomization was about 1.5 months.
A total of 341 patients in the rituximab arm and 361 patients in the obinutuzumab arm completed maintenance therapy.
The median follow-up was 34.5 months. Maintenance is ongoing in 114 patients—54 on rituximab and 60 on obinutuzumab.
Efficacy
At the end of induction, the overall response rate was 86.9% in the rituximab arm and 88.5% in the obinutuzumab arm. The complete response rates were 23.8% and 19.5%, respectively. And the rates of stable disease were 1.3% and 0.5%, respectively.
The study’s primary endpoint is investigator-assessed PFS. The 3-year PFS rate is 73.3% in the rituximab arm and 80% in the obinutuzumab arm (hazard ratio [HR]=0.66, P=0.0012).
According to an independent review committee, the 3-year PFS is 77.9% in the rituximab arm and 81.9% in the obinutuzumab arm (HR=0.71, P=0.0138).
The 3-year overall survival is 92.1% in the rituximab arm and 94% in the obinutuzumab arm (HR=0.75, P=0.21).
Safety
The overall incidence of AEs was 98.3% in the rituximab arm and 99.5% in the obinutuzumab arm. The incidence of serious AEs was 39.9% and 46.1%, respectively.
The incidence of AEs leading to treatment discontinuation was 14.2% and 16.3%, respectively. And the incidence of second neoplasms was 2.7% and 4.7%, respectively.
Grade 5 AEs occurred in 3.4% of patients in the rituximab arm and 4.0% of patients in the obinutuzumab arm. The investigators found that fatal AEs were more common in patients taking bendamustine, regardless of the treatment arm.
Grade 3 or higher AEs occurring in at least 5% of patients in either arm (rituximab and obinutuzumab, respectively) included neutropenia (67.8% and 74.6%), leukopenia (37.9% and 43.9%), febrile neutropenia (4.9% and 6.9%), infections and infestations (3.7% and 6.7%), and thrombocytopenia (2.7% and 6.1%).