User login
Bacterium may increase risk of DLBCL, FL
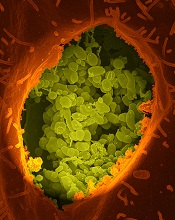
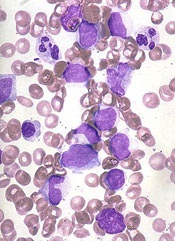
Coxiella burnetii
Image courtesy of NIAID
The bacterium that causes Q fever may confer an increased risk of diffuse large B-cell lymphoma (DLBCL) and follicular lymphoma (FL), according to a study published in Blood.
Q fever is an infectious disease caused by Coxiella burnetii, a bacterium primarily transmitted through the excrements of cattle, sheep, and goats.
Because some patients with Q fever develop lymphoma, researchers believed the malignancy could be a risk factor for Q fever.
However, the experience of 1 patient prompted a group of researchers in France to consider the opposite—that the infection might cause the lymphoma.
“During a follow-up scan in a patient we had successfully treated for Q fever, we observed a tumor close to the location of the previous infection,” said study author Didier Raoult, MD, PhD, of Aix-Marseille University in Marseille, France.
“The discovery that it was a lymphoma tumor containing C burnetii encouraged us to consider that the infection might have contributed to the development of the cancer.”
To better understand the association between C burnetii and lymphoma, Dr Raoult and his colleagues screened 1468 patients treated at the French National Referral Center for Q Fever from 2004 to 2014.
The researchers imaged patient tissue samples and identified 7 people, including the initial patient, who developed lymphoma after C burnetii infection. Six patients were diagnosed with DLBCL and 1 with FL.
To determine if patients with Q fever have a higher risk of lymphoma than the general population, the researchers compared the incidence of lymphoma in the Q fever registry to the incidence reported in France’s general population.
This revealed an excess risk of DLBCL and FL in the Q fever population, with standardized incidence ratios of 25.4 for DLBCL and 6.7 for FL.
In addition, the odds of developing lymphoma were higher in patients with persistent, concentrated infections than in those with other forms of Q fever. The hazard ratio for patients with persistent, concentrated infection was 9.35.
Finally, the researchers observed interleukin-10 overproduction in Q fever patients with lymphoma. The team said this suggests that suppression of the immune system may have allowed the lymphoma cells to evade immune detection and multiply.
“As we continue to learn more about the association between C burnetii and lymphoma, these results should encourage clinicians to survey high-risk patients as early as possible for potential cancer,” Dr Raoult said.
“Ultimately, this early diagnosis and treatment would improve outcomes for Q fever patients who subsequently develop lymphoma, particularly those with B-cell non-Hodgkin lymphoma.” ![]()
Coxiella burnetii
Image courtesy of NIAID
The bacterium that causes Q fever may confer an increased risk of diffuse large B-cell lymphoma (DLBCL) and follicular lymphoma (FL), according to a study published in Blood.
Q fever is an infectious disease caused by Coxiella burnetii, a bacterium primarily transmitted through the excrements of cattle, sheep, and goats.
Because some patients with Q fever develop lymphoma, researchers believed the malignancy could be a risk factor for Q fever.
However, the experience of 1 patient prompted a group of researchers in France to consider the opposite—that the infection might cause the lymphoma.
“During a follow-up scan in a patient we had successfully treated for Q fever, we observed a tumor close to the location of the previous infection,” said study author Didier Raoult, MD, PhD, of Aix-Marseille University in Marseille, France.
“The discovery that it was a lymphoma tumor containing C burnetii encouraged us to consider that the infection might have contributed to the development of the cancer.”
To better understand the association between C burnetii and lymphoma, Dr Raoult and his colleagues screened 1468 patients treated at the French National Referral Center for Q Fever from 2004 to 2014.
The researchers imaged patient tissue samples and identified 7 people, including the initial patient, who developed lymphoma after C burnetii infection. Six patients were diagnosed with DLBCL and 1 with FL.
To determine if patients with Q fever have a higher risk of lymphoma than the general population, the researchers compared the incidence of lymphoma in the Q fever registry to the incidence reported in France’s general population.
This revealed an excess risk of DLBCL and FL in the Q fever population, with standardized incidence ratios of 25.4 for DLBCL and 6.7 for FL.
In addition, the odds of developing lymphoma were higher in patients with persistent, concentrated infections than in those with other forms of Q fever. The hazard ratio for patients with persistent, concentrated infection was 9.35.
Finally, the researchers observed interleukin-10 overproduction in Q fever patients with lymphoma. The team said this suggests that suppression of the immune system may have allowed the lymphoma cells to evade immune detection and multiply.
“As we continue to learn more about the association between C burnetii and lymphoma, these results should encourage clinicians to survey high-risk patients as early as possible for potential cancer,” Dr Raoult said.
“Ultimately, this early diagnosis and treatment would improve outcomes for Q fever patients who subsequently develop lymphoma, particularly those with B-cell non-Hodgkin lymphoma.” ![]()
Coxiella burnetii
Image courtesy of NIAID
The bacterium that causes Q fever may confer an increased risk of diffuse large B-cell lymphoma (DLBCL) and follicular lymphoma (FL), according to a study published in Blood.
Q fever is an infectious disease caused by Coxiella burnetii, a bacterium primarily transmitted through the excrements of cattle, sheep, and goats.
Because some patients with Q fever develop lymphoma, researchers believed the malignancy could be a risk factor for Q fever.
However, the experience of 1 patient prompted a group of researchers in France to consider the opposite—that the infection might cause the lymphoma.
“During a follow-up scan in a patient we had successfully treated for Q fever, we observed a tumor close to the location of the previous infection,” said study author Didier Raoult, MD, PhD, of Aix-Marseille University in Marseille, France.
“The discovery that it was a lymphoma tumor containing C burnetii encouraged us to consider that the infection might have contributed to the development of the cancer.”
To better understand the association between C burnetii and lymphoma, Dr Raoult and his colleagues screened 1468 patients treated at the French National Referral Center for Q Fever from 2004 to 2014.
The researchers imaged patient tissue samples and identified 7 people, including the initial patient, who developed lymphoma after C burnetii infection. Six patients were diagnosed with DLBCL and 1 with FL.
To determine if patients with Q fever have a higher risk of lymphoma than the general population, the researchers compared the incidence of lymphoma in the Q fever registry to the incidence reported in France’s general population.
This revealed an excess risk of DLBCL and FL in the Q fever population, with standardized incidence ratios of 25.4 for DLBCL and 6.7 for FL.
In addition, the odds of developing lymphoma were higher in patients with persistent, concentrated infections than in those with other forms of Q fever. The hazard ratio for patients with persistent, concentrated infection was 9.35.
Finally, the researchers observed interleukin-10 overproduction in Q fever patients with lymphoma. The team said this suggests that suppression of the immune system may have allowed the lymphoma cells to evade immune detection and multiply.
“As we continue to learn more about the association between C burnetii and lymphoma, these results should encourage clinicians to survey high-risk patients as early as possible for potential cancer,” Dr Raoult said.
“Ultimately, this early diagnosis and treatment would improve outcomes for Q fever patients who subsequently develop lymphoma, particularly those with B-cell non-Hodgkin lymphoma.” ![]()
Method can identify CTCL quickly, study suggests
High-throughput sequencing (HTS) may enable earlier diagnosis of cutaneous T-cell lymphoma (CTCL), according to a study published in Science Translational Medicine.
Researchers said HTS, which provided new insights into the biology of CTCL, accurately diagnosed 100% of patients with the disease, including those with early stage and recurrent CTCL.
HTS exhibited greater sensitivity and specificity than polymerase chain reaction.
The researchers noted that, in CTCL, cancerous T cells accumulate in the skin, causing skin tumors but also rashes that are often mistaken for benign inflammatory skin conditions. And this delays diagnosis.
“Using current methods, it takes, on average, 6 years for patients to receive a definitive CTCL diagnosis,” said Rachael Clark, MD, PhD, of Brigham and Women’s Hospital in Boston, Massachusetts.
“As a result, appropriate therapy is delayed, often until the disease worsens to the point where diagnosis is clear, but effective treatment is more difficult.”
In search of a new diagnostic approach, Dr Clark and her colleagues used HTS to analyze T-cell receptor genes from blood and skin tissue samples. The team compared samples from 46 CTCL patients to samples from healthy individuals and patients with psoriasis, eczema, and other non-cancerous, inflammatory skin diseases.
By identifying and quantifying malignant T cells, HTS accurately distinguished CTCL from other skin diseases in all 46 patients. In contrast, polymerase chain reaction correctly identified 70% of the CTCL samples, often missing earlier-stage tumors.
For a subset of patients, the researchers used HTS to track malignant T cells over time, allowing them to detect early recurrence and monitor patient response to treatment.
HTS also revealed new insights into the cell of origin for CTCL, which has remained unresolved. The researchers found that CTCL arises from mature T cells, a discovery that may aid the development of more effective therapy.
The team said that, altogether, their findings suggest HTS is a promising tool for guiding earlier diagnosis and, thus, treatment of CTCL patients.
HTS was performed using ImmunoSEQ, an assay developed by Adaptive Biotechnologies. The company did not sponsor the study, but company employees were involved in the research. ![]()
High-throughput sequencing (HTS) may enable earlier diagnosis of cutaneous T-cell lymphoma (CTCL), according to a study published in Science Translational Medicine.
Researchers said HTS, which provided new insights into the biology of CTCL, accurately diagnosed 100% of patients with the disease, including those with early stage and recurrent CTCL.
HTS exhibited greater sensitivity and specificity than polymerase chain reaction.
The researchers noted that, in CTCL, cancerous T cells accumulate in the skin, causing skin tumors but also rashes that are often mistaken for benign inflammatory skin conditions. And this delays diagnosis.
“Using current methods, it takes, on average, 6 years for patients to receive a definitive CTCL diagnosis,” said Rachael Clark, MD, PhD, of Brigham and Women’s Hospital in Boston, Massachusetts.
“As a result, appropriate therapy is delayed, often until the disease worsens to the point where diagnosis is clear, but effective treatment is more difficult.”
In search of a new diagnostic approach, Dr Clark and her colleagues used HTS to analyze T-cell receptor genes from blood and skin tissue samples. The team compared samples from 46 CTCL patients to samples from healthy individuals and patients with psoriasis, eczema, and other non-cancerous, inflammatory skin diseases.
By identifying and quantifying malignant T cells, HTS accurately distinguished CTCL from other skin diseases in all 46 patients. In contrast, polymerase chain reaction correctly identified 70% of the CTCL samples, often missing earlier-stage tumors.
For a subset of patients, the researchers used HTS to track malignant T cells over time, allowing them to detect early recurrence and monitor patient response to treatment.
HTS also revealed new insights into the cell of origin for CTCL, which has remained unresolved. The researchers found that CTCL arises from mature T cells, a discovery that may aid the development of more effective therapy.
The team said that, altogether, their findings suggest HTS is a promising tool for guiding earlier diagnosis and, thus, treatment of CTCL patients.
HTS was performed using ImmunoSEQ, an assay developed by Adaptive Biotechnologies. The company did not sponsor the study, but company employees were involved in the research. ![]()
High-throughput sequencing (HTS) may enable earlier diagnosis of cutaneous T-cell lymphoma (CTCL), according to a study published in Science Translational Medicine.
Researchers said HTS, which provided new insights into the biology of CTCL, accurately diagnosed 100% of patients with the disease, including those with early stage and recurrent CTCL.
HTS exhibited greater sensitivity and specificity than polymerase chain reaction.
The researchers noted that, in CTCL, cancerous T cells accumulate in the skin, causing skin tumors but also rashes that are often mistaken for benign inflammatory skin conditions. And this delays diagnosis.
“Using current methods, it takes, on average, 6 years for patients to receive a definitive CTCL diagnosis,” said Rachael Clark, MD, PhD, of Brigham and Women’s Hospital in Boston, Massachusetts.
“As a result, appropriate therapy is delayed, often until the disease worsens to the point where diagnosis is clear, but effective treatment is more difficult.”
In search of a new diagnostic approach, Dr Clark and her colleagues used HTS to analyze T-cell receptor genes from blood and skin tissue samples. The team compared samples from 46 CTCL patients to samples from healthy individuals and patients with psoriasis, eczema, and other non-cancerous, inflammatory skin diseases.
By identifying and quantifying malignant T cells, HTS accurately distinguished CTCL from other skin diseases in all 46 patients. In contrast, polymerase chain reaction correctly identified 70% of the CTCL samples, often missing earlier-stage tumors.
For a subset of patients, the researchers used HTS to track malignant T cells over time, allowing them to detect early recurrence and monitor patient response to treatment.
HTS also revealed new insights into the cell of origin for CTCL, which has remained unresolved. The researchers found that CTCL arises from mature T cells, a discovery that may aid the development of more effective therapy.
The team said that, altogether, their findings suggest HTS is a promising tool for guiding earlier diagnosis and, thus, treatment of CTCL patients.
HTS was performed using ImmunoSEQ, an assay developed by Adaptive Biotechnologies. The company did not sponsor the study, but company employees were involved in the research. ![]()
JAK inhibitors could treat Sézary syndrome, team says

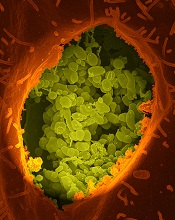
Photo courtesy of NIGMS
Patients with Sézary syndrome (SS) may have a more complex array of genetic mutations than we thought, according to a paper published in Nature Communications.
Investigators uncovered a genomic landscape that, they believe, can be used to design personalized treatment regimens for SS patients.
In particular, the team found mutations in the JAK/STAT pathway and discovered that JAK-mutated SS cells are sensitive to JAK inhibitors.
To conduct this research, the investigators sequenced SS patient samples using 3 different approaches. They performed whole-genome sequencing (n=6), whole-exome sequencing (n=66), and array comparative genomic hybridization-based copy-number analysis (n=80).
“We basically found chromosomal chaos in all of our samples,” said study author Kojo Elenitoba-Johnson, MD, of the University of Pennsylvania in Philadelphia.
“We did not expect the degree of genetic complexity that we found in our study.”
The investigators identified previously unknown, recurrent, loss-of-function mutations that target genes regulating epigenetic pathways.
One of these targets is ARID1A, and the team found that loss-of-function mutations and/or deletions in ARID1A occurred in more than 40% of the SS genome studied.
The investigators also identified gain-of-function mutations in PLCG1, JAK1, JAK3, STAT3, and STAT5B.
And in preliminary drug-mutation matching studies, JAK1-mutated SS cells were sensitive to JAK inhibitors.
“With knowledge like this, we can design clinical trials using JAK inhibitors for SS patients based on their JAK mutations,” Dr Elenitoba-Johnson said. “But this is just the start. These results highlight the genetic vulnerabilities that we can use in designing precision medicine therapies.”
Now, the investigators want to develop a molecular taxonomy for mutations in SS patients. Using the sequencing technology they used in this study, the team hopes to pinpoint the exact mistakes in each patient’s SS-related genes.
From this, the investigators hope to identify distinct subsets of the disease and stratify patients for precision therapy based on their mutations and the inhibitors available for those mutations. ![]()

Photo courtesy of NIGMS
Patients with Sézary syndrome (SS) may have a more complex array of genetic mutations than we thought, according to a paper published in Nature Communications.
Investigators uncovered a genomic landscape that, they believe, can be used to design personalized treatment regimens for SS patients.
In particular, the team found mutations in the JAK/STAT pathway and discovered that JAK-mutated SS cells are sensitive to JAK inhibitors.
To conduct this research, the investigators sequenced SS patient samples using 3 different approaches. They performed whole-genome sequencing (n=6), whole-exome sequencing (n=66), and array comparative genomic hybridization-based copy-number analysis (n=80).
“We basically found chromosomal chaos in all of our samples,” said study author Kojo Elenitoba-Johnson, MD, of the University of Pennsylvania in Philadelphia.
“We did not expect the degree of genetic complexity that we found in our study.”
The investigators identified previously unknown, recurrent, loss-of-function mutations that target genes regulating epigenetic pathways.
One of these targets is ARID1A, and the team found that loss-of-function mutations and/or deletions in ARID1A occurred in more than 40% of the SS genome studied.
The investigators also identified gain-of-function mutations in PLCG1, JAK1, JAK3, STAT3, and STAT5B.
And in preliminary drug-mutation matching studies, JAK1-mutated SS cells were sensitive to JAK inhibitors.
“With knowledge like this, we can design clinical trials using JAK inhibitors for SS patients based on their JAK mutations,” Dr Elenitoba-Johnson said. “But this is just the start. These results highlight the genetic vulnerabilities that we can use in designing precision medicine therapies.”
Now, the investigators want to develop a molecular taxonomy for mutations in SS patients. Using the sequencing technology they used in this study, the team hopes to pinpoint the exact mistakes in each patient’s SS-related genes.
From this, the investigators hope to identify distinct subsets of the disease and stratify patients for precision therapy based on their mutations and the inhibitors available for those mutations. ![]()

Photo courtesy of NIGMS
Patients with Sézary syndrome (SS) may have a more complex array of genetic mutations than we thought, according to a paper published in Nature Communications.
Investigators uncovered a genomic landscape that, they believe, can be used to design personalized treatment regimens for SS patients.
In particular, the team found mutations in the JAK/STAT pathway and discovered that JAK-mutated SS cells are sensitive to JAK inhibitors.
To conduct this research, the investigators sequenced SS patient samples using 3 different approaches. They performed whole-genome sequencing (n=6), whole-exome sequencing (n=66), and array comparative genomic hybridization-based copy-number analysis (n=80).
“We basically found chromosomal chaos in all of our samples,” said study author Kojo Elenitoba-Johnson, MD, of the University of Pennsylvania in Philadelphia.
“We did not expect the degree of genetic complexity that we found in our study.”
The investigators identified previously unknown, recurrent, loss-of-function mutations that target genes regulating epigenetic pathways.
One of these targets is ARID1A, and the team found that loss-of-function mutations and/or deletions in ARID1A occurred in more than 40% of the SS genome studied.
The investigators also identified gain-of-function mutations in PLCG1, JAK1, JAK3, STAT3, and STAT5B.
And in preliminary drug-mutation matching studies, JAK1-mutated SS cells were sensitive to JAK inhibitors.
“With knowledge like this, we can design clinical trials using JAK inhibitors for SS patients based on their JAK mutations,” Dr Elenitoba-Johnson said. “But this is just the start. These results highlight the genetic vulnerabilities that we can use in designing precision medicine therapies.”
Now, the investigators want to develop a molecular taxonomy for mutations in SS patients. Using the sequencing technology they used in this study, the team hopes to pinpoint the exact mistakes in each patient’s SS-related genes.
From this, the investigators hope to identify distinct subsets of the disease and stratify patients for precision therapy based on their mutations and the inhibitors available for those mutations. ![]()
Treating EBV-associated lymphomas with VSTs

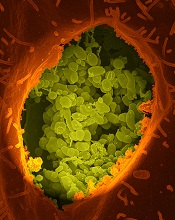
among uninfected cells (blue)
Image by Benjamin
Chaigne-Delalande
NEW YORK—Type 2 Epstein-Barr virus (EBV) tumors, such as Hodgkin and non-Hodgkin lymphomas, are challenging to treat with virus-specific T (VST) cells, according to researchers.
These lymphomas express a more restricted array of EBV antigens that are not particularly immunogenic.
Nevertheless, researchers are devising an approach using peptide mixtures to activate EBV VSTs for use in these patients.
Helen Heslop, MD, of Baylor College of Medicine in Houston, Texas, described this work at the inaugural CRI-CIMT-EATI-AACR International Immunotherapy of Cancer Conference. She also described the researchers’ efforts to create off-the-shelf VSTs.
Dr Heslop explained that, in addition to the more restricted array of EBV antigens, EBV-associated tumors often produce inhibitory cytokines that can impede the activity of T cells.
So the researchers devised a strategy to expand these low-frequency clones by stimulating responding T cells with dendritic cells genetically modified with an ADV viral vector to overexpress LMP1 and LMP2. After multiple stimulations, they obtained an autologous product from the patient.
The team then tested the cytotoxic T cells in 21 patients with relapsed disease and in 29 patients as adjuvant therapy after stem cell transplant (n=14) or chemotherapy (n=15).
In the adjuvant arm, all patients but 1 remain in remission up to 5 years later.
In the relapsed arm, 11 had a complete response (CR), 2 had a partial response (PR), and 8 had progressive disease within 2 to 8 weeks.
“Importantly, there was no toxicity,” Dr Heslop said. “[A]ll were heavily pretreated with multiple lines of therapy for lymphoma, so I think the response rate is encouraging.”
An alternative approach: Pepmix-activated EBV VSTs
Although the antitumor effects of the above approach were encouraging, “we had a very complex manufacturing methodology that we didn’t think was sufficiently scaleable and robust for clinical studies,” Dr Heslop said.
“We also thought there would be potential regulatory issues with live EBV virus and the adenoviral vector,” she added.
And the researchers were concerned about the competition from the EBV/Ad-LMP dominant antigens.
So they devised an alternative approach using peptide mixture (pepmix)-activated EBVSTs.
This approach used autologous monocyte-derived dendritic cells as the antigen-presenting cells for the first stimulation.
The researchers pulsed them with overlapping peptides derived from 4 EBV antigens expressed in the tumors (EBV-LMP1, LMP2, EBNA1, and BARF1). They then expanded and opsonized the cells with IL-7 and IL-15.
For the second stimulation, the team used the T cells pulsed with the peptides and a K562 line pulsed with co-stimulatory molecules. And this process took 23 days, as opposed to the 2-3 months with the previous product.
The researchers have treated 9 patients with these EBVSTs as adjuvant therapy after autologous stem cell transplant. All patients remain in remission.
They also treated 6 patients with active disease. Two are in CR, 2 are in PR, and 2 have progressed.
This trial is ongoing, but the researchers believe that targeting the more challenging type 2 latency tumors with autologous cells can overcome T-cell anergy by using IL-7 and IL-15.
“Obviously, we need more numbers to know what the range of response is,” Dr Heslop said, although, at this early stage, it appears pepmix-activated T cells can produce antitumor responses. ![]()

among uninfected cells (blue)
Image by Benjamin
Chaigne-Delalande
NEW YORK—Type 2 Epstein-Barr virus (EBV) tumors, such as Hodgkin and non-Hodgkin lymphomas, are challenging to treat with virus-specific T (VST) cells, according to researchers.
These lymphomas express a more restricted array of EBV antigens that are not particularly immunogenic.
Nevertheless, researchers are devising an approach using peptide mixtures to activate EBV VSTs for use in these patients.
Helen Heslop, MD, of Baylor College of Medicine in Houston, Texas, described this work at the inaugural CRI-CIMT-EATI-AACR International Immunotherapy of Cancer Conference. She also described the researchers’ efforts to create off-the-shelf VSTs.
Dr Heslop explained that, in addition to the more restricted array of EBV antigens, EBV-associated tumors often produce inhibitory cytokines that can impede the activity of T cells.
So the researchers devised a strategy to expand these low-frequency clones by stimulating responding T cells with dendritic cells genetically modified with an ADV viral vector to overexpress LMP1 and LMP2. After multiple stimulations, they obtained an autologous product from the patient.
The team then tested the cytotoxic T cells in 21 patients with relapsed disease and in 29 patients as adjuvant therapy after stem cell transplant (n=14) or chemotherapy (n=15).
In the adjuvant arm, all patients but 1 remain in remission up to 5 years later.
In the relapsed arm, 11 had a complete response (CR), 2 had a partial response (PR), and 8 had progressive disease within 2 to 8 weeks.
“Importantly, there was no toxicity,” Dr Heslop said. “[A]ll were heavily pretreated with multiple lines of therapy for lymphoma, so I think the response rate is encouraging.”
An alternative approach: Pepmix-activated EBV VSTs
Although the antitumor effects of the above approach were encouraging, “we had a very complex manufacturing methodology that we didn’t think was sufficiently scaleable and robust for clinical studies,” Dr Heslop said.
“We also thought there would be potential regulatory issues with live EBV virus and the adenoviral vector,” she added.
And the researchers were concerned about the competition from the EBV/Ad-LMP dominant antigens.
So they devised an alternative approach using peptide mixture (pepmix)-activated EBVSTs.
This approach used autologous monocyte-derived dendritic cells as the antigen-presenting cells for the first stimulation.
The researchers pulsed them with overlapping peptides derived from 4 EBV antigens expressed in the tumors (EBV-LMP1, LMP2, EBNA1, and BARF1). They then expanded and opsonized the cells with IL-7 and IL-15.
For the second stimulation, the team used the T cells pulsed with the peptides and a K562 line pulsed with co-stimulatory molecules. And this process took 23 days, as opposed to the 2-3 months with the previous product.
The researchers have treated 9 patients with these EBVSTs as adjuvant therapy after autologous stem cell transplant. All patients remain in remission.
They also treated 6 patients with active disease. Two are in CR, 2 are in PR, and 2 have progressed.
This trial is ongoing, but the researchers believe that targeting the more challenging type 2 latency tumors with autologous cells can overcome T-cell anergy by using IL-7 and IL-15.
“Obviously, we need more numbers to know what the range of response is,” Dr Heslop said, although, at this early stage, it appears pepmix-activated T cells can produce antitumor responses. ![]()

among uninfected cells (blue)
Image by Benjamin
Chaigne-Delalande
NEW YORK—Type 2 Epstein-Barr virus (EBV) tumors, such as Hodgkin and non-Hodgkin lymphomas, are challenging to treat with virus-specific T (VST) cells, according to researchers.
These lymphomas express a more restricted array of EBV antigens that are not particularly immunogenic.
Nevertheless, researchers are devising an approach using peptide mixtures to activate EBV VSTs for use in these patients.
Helen Heslop, MD, of Baylor College of Medicine in Houston, Texas, described this work at the inaugural CRI-CIMT-EATI-AACR International Immunotherapy of Cancer Conference. She also described the researchers’ efforts to create off-the-shelf VSTs.
Dr Heslop explained that, in addition to the more restricted array of EBV antigens, EBV-associated tumors often produce inhibitory cytokines that can impede the activity of T cells.
So the researchers devised a strategy to expand these low-frequency clones by stimulating responding T cells with dendritic cells genetically modified with an ADV viral vector to overexpress LMP1 and LMP2. After multiple stimulations, they obtained an autologous product from the patient.
The team then tested the cytotoxic T cells in 21 patients with relapsed disease and in 29 patients as adjuvant therapy after stem cell transplant (n=14) or chemotherapy (n=15).
In the adjuvant arm, all patients but 1 remain in remission up to 5 years later.
In the relapsed arm, 11 had a complete response (CR), 2 had a partial response (PR), and 8 had progressive disease within 2 to 8 weeks.
“Importantly, there was no toxicity,” Dr Heslop said. “[A]ll were heavily pretreated with multiple lines of therapy for lymphoma, so I think the response rate is encouraging.”
An alternative approach: Pepmix-activated EBV VSTs
Although the antitumor effects of the above approach were encouraging, “we had a very complex manufacturing methodology that we didn’t think was sufficiently scaleable and robust for clinical studies,” Dr Heslop said.
“We also thought there would be potential regulatory issues with live EBV virus and the adenoviral vector,” she added.
And the researchers were concerned about the competition from the EBV/Ad-LMP dominant antigens.
So they devised an alternative approach using peptide mixture (pepmix)-activated EBVSTs.
This approach used autologous monocyte-derived dendritic cells as the antigen-presenting cells for the first stimulation.
The researchers pulsed them with overlapping peptides derived from 4 EBV antigens expressed in the tumors (EBV-LMP1, LMP2, EBNA1, and BARF1). They then expanded and opsonized the cells with IL-7 and IL-15.
For the second stimulation, the team used the T cells pulsed with the peptides and a K562 line pulsed with co-stimulatory molecules. And this process took 23 days, as opposed to the 2-3 months with the previous product.
The researchers have treated 9 patients with these EBVSTs as adjuvant therapy after autologous stem cell transplant. All patients remain in remission.
They also treated 6 patients with active disease. Two are in CR, 2 are in PR, and 2 have progressed.
This trial is ongoing, but the researchers believe that targeting the more challenging type 2 latency tumors with autologous cells can overcome T-cell anergy by using IL-7 and IL-15.
“Obviously, we need more numbers to know what the range of response is,” Dr Heslop said, although, at this early stage, it appears pepmix-activated T cells can produce antitumor responses. ![]()
Variations in blood cancer survival across Europe

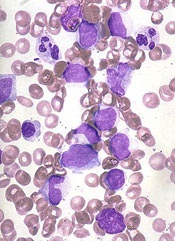
chemotherapy
Photo by Rhoda Baer
VIENNA—Results of the EUROCARE-5 study have revealed regional differences in survival for European patients with hematologic malignancies.
The data showed regional variations in 5-year relative survival rates for a number of cancers.
But the differences were particularly pronounced for leukemias, non-Hodgkin lymphomas (NHLs), and plasma cell neoplasms (PCNs).
Milena Sant, MD, of the Fondazione IRCCS Istituto Nazionale dei Tumori in Milan, Italy, presented these results at the 2015 European Cancer Congress (LBA 1).
Data from this study have also been published in several articles in the October 2015 issue of the European Journal of Cancer.
EUROCARE-5 includes records from 22 million cancer patients diagnosed between 1978 and 2007. The latest data encompass more than 10 million patients (ages 15 and older) diagnosed from 1995 to 2007 and followed up to 2008.
The data came from 107 cancer registries in 29 countries. The researchers estimated 5-year relative survival and trends from 1999 to 2007 according to region—Ireland/UK, Northern Europe, Central Europe, Southern Europe, and Eastern Europe.
“In general, 5-year relative survival—survival that is adjusted for causes of death other than cancer—increased steadily over time in Europe, particularly in Eastern Europe, for most cancers,” Dr Sant said.
“However, the most dramatic geographical variations were observed for cancers of the blood where there have been recent advances in treatment, such as chronic myeloid and lymphocytic leukemias, non-Hodgkin lymphoma and 2 of its subtypes (follicular and diffuse large B-cell lymphoma), and multiple myeloma. Hodgkin lymphoma was the exception, with smaller regional variations and a fairly good prognosis in most countries.”
Hodgkin lymphoma and NHL
Of all the hematologic malignancies, 5-year relative survival was highest for Hodgkin lymphoma, at 80.8% (40,625 cases). Five-year survival was 79.4% in Ireland and the UK, 85% in Northern countries, and 74.3% in Eastern Europe, which was significantly below the European average (P<0.0001).
For NHL, the 5-year relative survival was 59.4% (329,204 cases). Survival rates for NHL patients ranged from 49.7% in Eastern Europe to 63.3% in Northern Europe.
CLL/SLL
For chronic lymphocytic leukemia/small lymphocytic lymphoma (CLL/SLL), the 5-year relative survival was 70.4% (81,914 cases). CLL/SLL survival ranged from 58% in Eastern Europe to about 74% in Central and Northern Europe.
The researchers noted that between-country variations in CLL/SLL survival were high in all regions. Outliers that were significantly below the regional average were Austria (67%), Croatia (52%), and Bulgaria (45.5%).
PCNs
PCNs included multiple myeloma, plasmacytoma, and plasma cell leukemias. The 5-year relative survival for all PCNs was 39.2% (94,024 cases).
PCN survival rates were lowest in Eastern Europe (31.7%), slightly higher in the UK/Ireland (35.9%), and between 39.1% and 42% in the rest of Europe.
Myeloid leukemias
Of all the hematologic malignancies, 5-year relative survival was poorest for patients with acute myeloid leukemia (AML), at 17.1% (57,026 cases).
AML survival rates in Ireland/UK (15.0%) and Eastern Europe (13.0%) were significantly below the European average. But AML survival in Sweden, Belgium, France, and Germany was significantly higher than the average (P<0.005).
Five-year relative survival for chronic myeloid leukemia (CML) was 52.9% (17,713 cases).
Of all the hematologic malignancies, the survival gap between Eastern Europe and the rest of Europe was highest for CML. Five-year survival for CML patients was 33% in Eastern Europe and ranged from 51% to 58% in the rest of Europe.
The researchers also said there were striking survival variations by country in all areas. They found significant deviations from the regional average in Sweden (69.7%), Scotland (64.6%), France (71.7%), Austria (48.2%), Croatia (37.8%), Estonia (48.9%), Czech Republic (45.2%), and Latvia (22.1%).
“Results from EUROCARE can help to identify regions of low survival where action is needed to improve patients’ outcomes,” Dr Sant noted.
“Population-based survival information is essential for physicians, policy-makers, administrators, researchers, and patient organizations who deal with the needs of cancer patients, as well as with the issue of the growing expenditure on healthcare.” ![]()

chemotherapy
Photo by Rhoda Baer
VIENNA—Results of the EUROCARE-5 study have revealed regional differences in survival for European patients with hematologic malignancies.
The data showed regional variations in 5-year relative survival rates for a number of cancers.
But the differences were particularly pronounced for leukemias, non-Hodgkin lymphomas (NHLs), and plasma cell neoplasms (PCNs).
Milena Sant, MD, of the Fondazione IRCCS Istituto Nazionale dei Tumori in Milan, Italy, presented these results at the 2015 European Cancer Congress (LBA 1).
Data from this study have also been published in several articles in the October 2015 issue of the European Journal of Cancer.
EUROCARE-5 includes records from 22 million cancer patients diagnosed between 1978 and 2007. The latest data encompass more than 10 million patients (ages 15 and older) diagnosed from 1995 to 2007 and followed up to 2008.
The data came from 107 cancer registries in 29 countries. The researchers estimated 5-year relative survival and trends from 1999 to 2007 according to region—Ireland/UK, Northern Europe, Central Europe, Southern Europe, and Eastern Europe.
“In general, 5-year relative survival—survival that is adjusted for causes of death other than cancer—increased steadily over time in Europe, particularly in Eastern Europe, for most cancers,” Dr Sant said.
“However, the most dramatic geographical variations were observed for cancers of the blood where there have been recent advances in treatment, such as chronic myeloid and lymphocytic leukemias, non-Hodgkin lymphoma and 2 of its subtypes (follicular and diffuse large B-cell lymphoma), and multiple myeloma. Hodgkin lymphoma was the exception, with smaller regional variations and a fairly good prognosis in most countries.”
Hodgkin lymphoma and NHL
Of all the hematologic malignancies, 5-year relative survival was highest for Hodgkin lymphoma, at 80.8% (40,625 cases). Five-year survival was 79.4% in Ireland and the UK, 85% in Northern countries, and 74.3% in Eastern Europe, which was significantly below the European average (P<0.0001).
For NHL, the 5-year relative survival was 59.4% (329,204 cases). Survival rates for NHL patients ranged from 49.7% in Eastern Europe to 63.3% in Northern Europe.
CLL/SLL
For chronic lymphocytic leukemia/small lymphocytic lymphoma (CLL/SLL), the 5-year relative survival was 70.4% (81,914 cases). CLL/SLL survival ranged from 58% in Eastern Europe to about 74% in Central and Northern Europe.
The researchers noted that between-country variations in CLL/SLL survival were high in all regions. Outliers that were significantly below the regional average were Austria (67%), Croatia (52%), and Bulgaria (45.5%).
PCNs
PCNs included multiple myeloma, plasmacytoma, and plasma cell leukemias. The 5-year relative survival for all PCNs was 39.2% (94,024 cases).
PCN survival rates were lowest in Eastern Europe (31.7%), slightly higher in the UK/Ireland (35.9%), and between 39.1% and 42% in the rest of Europe.
Myeloid leukemias
Of all the hematologic malignancies, 5-year relative survival was poorest for patients with acute myeloid leukemia (AML), at 17.1% (57,026 cases).
AML survival rates in Ireland/UK (15.0%) and Eastern Europe (13.0%) were significantly below the European average. But AML survival in Sweden, Belgium, France, and Germany was significantly higher than the average (P<0.005).
Five-year relative survival for chronic myeloid leukemia (CML) was 52.9% (17,713 cases).
Of all the hematologic malignancies, the survival gap between Eastern Europe and the rest of Europe was highest for CML. Five-year survival for CML patients was 33% in Eastern Europe and ranged from 51% to 58% in the rest of Europe.
The researchers also said there were striking survival variations by country in all areas. They found significant deviations from the regional average in Sweden (69.7%), Scotland (64.6%), France (71.7%), Austria (48.2%), Croatia (37.8%), Estonia (48.9%), Czech Republic (45.2%), and Latvia (22.1%).
“Results from EUROCARE can help to identify regions of low survival where action is needed to improve patients’ outcomes,” Dr Sant noted.
“Population-based survival information is essential for physicians, policy-makers, administrators, researchers, and patient organizations who deal with the needs of cancer patients, as well as with the issue of the growing expenditure on healthcare.” ![]()

chemotherapy
Photo by Rhoda Baer
VIENNA—Results of the EUROCARE-5 study have revealed regional differences in survival for European patients with hematologic malignancies.
The data showed regional variations in 5-year relative survival rates for a number of cancers.
But the differences were particularly pronounced for leukemias, non-Hodgkin lymphomas (NHLs), and plasma cell neoplasms (PCNs).
Milena Sant, MD, of the Fondazione IRCCS Istituto Nazionale dei Tumori in Milan, Italy, presented these results at the 2015 European Cancer Congress (LBA 1).
Data from this study have also been published in several articles in the October 2015 issue of the European Journal of Cancer.
EUROCARE-5 includes records from 22 million cancer patients diagnosed between 1978 and 2007. The latest data encompass more than 10 million patients (ages 15 and older) diagnosed from 1995 to 2007 and followed up to 2008.
The data came from 107 cancer registries in 29 countries. The researchers estimated 5-year relative survival and trends from 1999 to 2007 according to region—Ireland/UK, Northern Europe, Central Europe, Southern Europe, and Eastern Europe.
“In general, 5-year relative survival—survival that is adjusted for causes of death other than cancer—increased steadily over time in Europe, particularly in Eastern Europe, for most cancers,” Dr Sant said.
“However, the most dramatic geographical variations were observed for cancers of the blood where there have been recent advances in treatment, such as chronic myeloid and lymphocytic leukemias, non-Hodgkin lymphoma and 2 of its subtypes (follicular and diffuse large B-cell lymphoma), and multiple myeloma. Hodgkin lymphoma was the exception, with smaller regional variations and a fairly good prognosis in most countries.”
Hodgkin lymphoma and NHL
Of all the hematologic malignancies, 5-year relative survival was highest for Hodgkin lymphoma, at 80.8% (40,625 cases). Five-year survival was 79.4% in Ireland and the UK, 85% in Northern countries, and 74.3% in Eastern Europe, which was significantly below the European average (P<0.0001).
For NHL, the 5-year relative survival was 59.4% (329,204 cases). Survival rates for NHL patients ranged from 49.7% in Eastern Europe to 63.3% in Northern Europe.
CLL/SLL
For chronic lymphocytic leukemia/small lymphocytic lymphoma (CLL/SLL), the 5-year relative survival was 70.4% (81,914 cases). CLL/SLL survival ranged from 58% in Eastern Europe to about 74% in Central and Northern Europe.
The researchers noted that between-country variations in CLL/SLL survival were high in all regions. Outliers that were significantly below the regional average were Austria (67%), Croatia (52%), and Bulgaria (45.5%).
PCNs
PCNs included multiple myeloma, plasmacytoma, and plasma cell leukemias. The 5-year relative survival for all PCNs was 39.2% (94,024 cases).
PCN survival rates were lowest in Eastern Europe (31.7%), slightly higher in the UK/Ireland (35.9%), and between 39.1% and 42% in the rest of Europe.
Myeloid leukemias
Of all the hematologic malignancies, 5-year relative survival was poorest for patients with acute myeloid leukemia (AML), at 17.1% (57,026 cases).
AML survival rates in Ireland/UK (15.0%) and Eastern Europe (13.0%) were significantly below the European average. But AML survival in Sweden, Belgium, France, and Germany was significantly higher than the average (P<0.005).
Five-year relative survival for chronic myeloid leukemia (CML) was 52.9% (17,713 cases).
Of all the hematologic malignancies, the survival gap between Eastern Europe and the rest of Europe was highest for CML. Five-year survival for CML patients was 33% in Eastern Europe and ranged from 51% to 58% in the rest of Europe.
The researchers also said there were striking survival variations by country in all areas. They found significant deviations from the regional average in Sweden (69.7%), Scotland (64.6%), France (71.7%), Austria (48.2%), Croatia (37.8%), Estonia (48.9%), Czech Republic (45.2%), and Latvia (22.1%).
“Results from EUROCARE can help to identify regions of low survival where action is needed to improve patients’ outcomes,” Dr Sant noted.
“Population-based survival information is essential for physicians, policy-makers, administrators, researchers, and patient organizations who deal with the needs of cancer patients, as well as with the issue of the growing expenditure on healthcare.” ![]()
NICE backs discounted idelalisib for CLL

The UK’s National Institute for Health and Care Excellence (NICE) has issued a final draft guidance recommending that the PI3Kδ inhibitor idelalisib (Zydelig) be made available on the National Health Service (NHS) for some adults with chronic lymphocytic leukemia (CLL).
NICE is recommending idelalisib in combination with rituximab for adults with previously untreated CLL who have a 17p deletion or TP53 mutation and for adults with CLL who have relapsed within 24 months of their previous treatment.
This decision follows a preliminary decision earlier this year, when NICE asked Gilead Sciences, the company developing idelalisib, to provide further information on the cost-effectiveness of the drug.
Gilead responded by submitting new economic analyses and a simple discount agreement to the list price of idelalisib.
NICE’s recommendation for idelalisib is contingent upon the company providing the agreed upon discount.
NICE’s draft guidance is now with consultees, who have the opportunity to appeal against it. Until NICE issues a final guidance, NHS bodies should make decisions locally on the funding of specific treatments.
Patients whose treatment with idelalisib is not recommended in this NICE guidance but was started within the NHS before this guidance was published should be able to continue treatment until they and their NHS clinician consider it appropriate to stop.
Clinical effectiveness
The committee advising NICE concluded that idelalisib could not be recommended for patients whose disease had relapsed more than 24 months after previous treatment, as no evidence was submitted for this patient group.
For the other populations, the clinical effectiveness data from Study 116 showed that idelalisib plus rituximab produced a significant improvement in progression-free survival and overall survival, compared with rituximab alone, for patients with high-risk, relapsed or refractory CLL.
Cost-effectiveness
Idelalisib is priced at £3114.75 for sixty 150-mg tablets (British national formulary 2015). The mean cost of a 1-year treatment course is £37,922.
Gilead’s agreement provides a discount to the list price of idelalisib, but the level of the discount is currently confidential.
Analyses suggested that, at the discount agreement price, idelalisib plus rituximab was associated with higher costs and greater quality-adjusted life-year (QALY) gains when compared with rituximab alone.
The deterministic incremental cost-effectiveness ratio (ICER) for idelalisib plus rituximab compared with rituximab alone was £13,634 per QALY gained (incremental costs £26,128; incremental QALYs 1.92).
Compared with best supportive care, the ICER for idelalisib plus rituximab was £20,461 per QALY gained (incremental costs £39,211; incremental QALYs 1.92). And compared with ofatumumab, the ICER was £1527 per QALY gained (incremental costs £2926; incremental QALYs 1.92). ![]()

The UK’s National Institute for Health and Care Excellence (NICE) has issued a final draft guidance recommending that the PI3Kδ inhibitor idelalisib (Zydelig) be made available on the National Health Service (NHS) for some adults with chronic lymphocytic leukemia (CLL).
NICE is recommending idelalisib in combination with rituximab for adults with previously untreated CLL who have a 17p deletion or TP53 mutation and for adults with CLL who have relapsed within 24 months of their previous treatment.
This decision follows a preliminary decision earlier this year, when NICE asked Gilead Sciences, the company developing idelalisib, to provide further information on the cost-effectiveness of the drug.
Gilead responded by submitting new economic analyses and a simple discount agreement to the list price of idelalisib.
NICE’s recommendation for idelalisib is contingent upon the company providing the agreed upon discount.
NICE’s draft guidance is now with consultees, who have the opportunity to appeal against it. Until NICE issues a final guidance, NHS bodies should make decisions locally on the funding of specific treatments.
Patients whose treatment with idelalisib is not recommended in this NICE guidance but was started within the NHS before this guidance was published should be able to continue treatment until they and their NHS clinician consider it appropriate to stop.
Clinical effectiveness
The committee advising NICE concluded that idelalisib could not be recommended for patients whose disease had relapsed more than 24 months after previous treatment, as no evidence was submitted for this patient group.
For the other populations, the clinical effectiveness data from Study 116 showed that idelalisib plus rituximab produced a significant improvement in progression-free survival and overall survival, compared with rituximab alone, for patients with high-risk, relapsed or refractory CLL.
Cost-effectiveness
Idelalisib is priced at £3114.75 for sixty 150-mg tablets (British national formulary 2015). The mean cost of a 1-year treatment course is £37,922.
Gilead’s agreement provides a discount to the list price of idelalisib, but the level of the discount is currently confidential.
Analyses suggested that, at the discount agreement price, idelalisib plus rituximab was associated with higher costs and greater quality-adjusted life-year (QALY) gains when compared with rituximab alone.
The deterministic incremental cost-effectiveness ratio (ICER) for idelalisib plus rituximab compared with rituximab alone was £13,634 per QALY gained (incremental costs £26,128; incremental QALYs 1.92).
Compared with best supportive care, the ICER for idelalisib plus rituximab was £20,461 per QALY gained (incremental costs £39,211; incremental QALYs 1.92). And compared with ofatumumab, the ICER was £1527 per QALY gained (incremental costs £2926; incremental QALYs 1.92). ![]()

The UK’s National Institute for Health and Care Excellence (NICE) has issued a final draft guidance recommending that the PI3Kδ inhibitor idelalisib (Zydelig) be made available on the National Health Service (NHS) for some adults with chronic lymphocytic leukemia (CLL).
NICE is recommending idelalisib in combination with rituximab for adults with previously untreated CLL who have a 17p deletion or TP53 mutation and for adults with CLL who have relapsed within 24 months of their previous treatment.
This decision follows a preliminary decision earlier this year, when NICE asked Gilead Sciences, the company developing idelalisib, to provide further information on the cost-effectiveness of the drug.
Gilead responded by submitting new economic analyses and a simple discount agreement to the list price of idelalisib.
NICE’s recommendation for idelalisib is contingent upon the company providing the agreed upon discount.
NICE’s draft guidance is now with consultees, who have the opportunity to appeal against it. Until NICE issues a final guidance, NHS bodies should make decisions locally on the funding of specific treatments.
Patients whose treatment with idelalisib is not recommended in this NICE guidance but was started within the NHS before this guidance was published should be able to continue treatment until they and their NHS clinician consider it appropriate to stop.
Clinical effectiveness
The committee advising NICE concluded that idelalisib could not be recommended for patients whose disease had relapsed more than 24 months after previous treatment, as no evidence was submitted for this patient group.
For the other populations, the clinical effectiveness data from Study 116 showed that idelalisib plus rituximab produced a significant improvement in progression-free survival and overall survival, compared with rituximab alone, for patients with high-risk, relapsed or refractory CLL.
Cost-effectiveness
Idelalisib is priced at £3114.75 for sixty 150-mg tablets (British national formulary 2015). The mean cost of a 1-year treatment course is £37,922.
Gilead’s agreement provides a discount to the list price of idelalisib, but the level of the discount is currently confidential.
Analyses suggested that, at the discount agreement price, idelalisib plus rituximab was associated with higher costs and greater quality-adjusted life-year (QALY) gains when compared with rituximab alone.
The deterministic incremental cost-effectiveness ratio (ICER) for idelalisib plus rituximab compared with rituximab alone was £13,634 per QALY gained (incremental costs £26,128; incremental QALYs 1.92).
Compared with best supportive care, the ICER for idelalisib plus rituximab was £20,461 per QALY gained (incremental costs £39,211; incremental QALYs 1.92). And compared with ofatumumab, the ICER was £1527 per QALY gained (incremental costs £2926; incremental QALYs 1.92). ![]()
Insights from the 5-year follow-up of CTL019 in CLL

Photo courtesy of the
University of Pennsylvania
NEW YORK—The 5-year follow-up of the phase 1 trial of CTL019 in relapsed or refractory chronic lymphoblastic leukemia (CLL) is allowing investigators to define more clearly who will respond to chimeric antigen receptor (CAR) T cells directed against CD19.
One thing investigators have determined is that persistence of the CARs is essential for long-term responses.
In the first 2 patients who achieved a complete remission (CR), CAR T cells persisted for more than 4 years. In addition, no patient in CR has relapsed to date.
Of the 14 patients enrolled in the trial, 4 (28%) achieved a CR, 4 (28%) achieved a partial response, and 6 (43%) had no response, for an overall response rate of 57%.
These results were recently published in Science Translational Medicine.
Carl June, MD, of the University of Pennsylvania in Philadelphia, shared some insights into the research with attendees at the inaugural CRI-CIMT-EATI-AACR International Cancer Immunotherapy Conference.
Dr June explained that CTL019 is a CD19-directed single chain variable fragment with a 4-1BB signaling module that transduces T cells with a lentiviral vector. The technology was developed at the University of Pennsylvania and subsequently licensed to Novartis.
In the phase 1 trial of CTL019 in CLL, patients who achieved complete remission have very high levels of CARs—100% of the circulating T cells—but the non-responders don’t. The CARs engrafted in non-responders but did not proliferate.
“So the biomarker correlate of success is persistence and proliferation, in CLL at least,” Dr June said.
The investigators performed IGH next-generation sequencing and found no detectable CLL clones in the complete responders, including 1 patient at 3.5 years and another at 4 years post-infusion.
“There was no clinically evident disease in these patients,” Dr June said, “and so the responses are durable.”
The team also believes that at least a subset of the cells remains functional because the patients still had B-cell aplasia.
The investigators have not observed a CD19 loss in any CLL patient who responded.
“Patients who have gone into remission stay in remission,” Dr June added.
Kinetics of delayed CR
Dr June discussed in detail Patient 10, whose response was somewhat different from the other complete responders. Patient 10 achieved a CR, but the response was delayed. It took 51 days after infusion, compared to about 10 days in the other complete responders.
Patient 10 was initially scored as a failure at the 28-day evaluation. Eventually, he had marked improvement, and, by a year, he was in CR.
He required hospitalization for tumor lysis syndrome and treatment with tocilizumab for cytokine release syndrome.
Patient 10 had a single cell that investigators surmise could have been responsible for the tumor elimination.
“In fact, on day 28, when he still had tumor, his CARs were polyclonal,” Dr June said. “So we stained and isolated his CARs by sorting, and, at time of tumor elimination, he had descendants of 1 CAR.”
Nevertheless, Patient 10’s response is durable. He is now 81 years old and remains engrafted with CAR19 cells.
Investigators hypothesize that the kinetics and CAR proliferation were so different in Patient 10 because Tet2 was disrupted by the integration of the CAR into the intronic region.
“What we don’t know is whether Tet2 was a passenger or a driver here,” Dr June observed. “Did it actually aid the function of the CAR cells or was it just a marker?”
He noted that Tet2 has been shown in acute myeloid leukemia to increase stem cell renewal, “and it may well have done that in this patient.” ![]()

Photo courtesy of the
University of Pennsylvania
NEW YORK—The 5-year follow-up of the phase 1 trial of CTL019 in relapsed or refractory chronic lymphoblastic leukemia (CLL) is allowing investigators to define more clearly who will respond to chimeric antigen receptor (CAR) T cells directed against CD19.
One thing investigators have determined is that persistence of the CARs is essential for long-term responses.
In the first 2 patients who achieved a complete remission (CR), CAR T cells persisted for more than 4 years. In addition, no patient in CR has relapsed to date.
Of the 14 patients enrolled in the trial, 4 (28%) achieved a CR, 4 (28%) achieved a partial response, and 6 (43%) had no response, for an overall response rate of 57%.
These results were recently published in Science Translational Medicine.
Carl June, MD, of the University of Pennsylvania in Philadelphia, shared some insights into the research with attendees at the inaugural CRI-CIMT-EATI-AACR International Cancer Immunotherapy Conference.
Dr June explained that CTL019 is a CD19-directed single chain variable fragment with a 4-1BB signaling module that transduces T cells with a lentiviral vector. The technology was developed at the University of Pennsylvania and subsequently licensed to Novartis.
In the phase 1 trial of CTL019 in CLL, patients who achieved complete remission have very high levels of CARs—100% of the circulating T cells—but the non-responders don’t. The CARs engrafted in non-responders but did not proliferate.
“So the biomarker correlate of success is persistence and proliferation, in CLL at least,” Dr June said.
The investigators performed IGH next-generation sequencing and found no detectable CLL clones in the complete responders, including 1 patient at 3.5 years and another at 4 years post-infusion.
“There was no clinically evident disease in these patients,” Dr June said, “and so the responses are durable.”
The team also believes that at least a subset of the cells remains functional because the patients still had B-cell aplasia.
The investigators have not observed a CD19 loss in any CLL patient who responded.
“Patients who have gone into remission stay in remission,” Dr June added.
Kinetics of delayed CR
Dr June discussed in detail Patient 10, whose response was somewhat different from the other complete responders. Patient 10 achieved a CR, but the response was delayed. It took 51 days after infusion, compared to about 10 days in the other complete responders.
Patient 10 was initially scored as a failure at the 28-day evaluation. Eventually, he had marked improvement, and, by a year, he was in CR.
He required hospitalization for tumor lysis syndrome and treatment with tocilizumab for cytokine release syndrome.
Patient 10 had a single cell that investigators surmise could have been responsible for the tumor elimination.
“In fact, on day 28, when he still had tumor, his CARs were polyclonal,” Dr June said. “So we stained and isolated his CARs by sorting, and, at time of tumor elimination, he had descendants of 1 CAR.”
Nevertheless, Patient 10’s response is durable. He is now 81 years old and remains engrafted with CAR19 cells.
Investigators hypothesize that the kinetics and CAR proliferation were so different in Patient 10 because Tet2 was disrupted by the integration of the CAR into the intronic region.
“What we don’t know is whether Tet2 was a passenger or a driver here,” Dr June observed. “Did it actually aid the function of the CAR cells or was it just a marker?”
He noted that Tet2 has been shown in acute myeloid leukemia to increase stem cell renewal, “and it may well have done that in this patient.” ![]()

Photo courtesy of the
University of Pennsylvania
NEW YORK—The 5-year follow-up of the phase 1 trial of CTL019 in relapsed or refractory chronic lymphoblastic leukemia (CLL) is allowing investigators to define more clearly who will respond to chimeric antigen receptor (CAR) T cells directed against CD19.
One thing investigators have determined is that persistence of the CARs is essential for long-term responses.
In the first 2 patients who achieved a complete remission (CR), CAR T cells persisted for more than 4 years. In addition, no patient in CR has relapsed to date.
Of the 14 patients enrolled in the trial, 4 (28%) achieved a CR, 4 (28%) achieved a partial response, and 6 (43%) had no response, for an overall response rate of 57%.
These results were recently published in Science Translational Medicine.
Carl June, MD, of the University of Pennsylvania in Philadelphia, shared some insights into the research with attendees at the inaugural CRI-CIMT-EATI-AACR International Cancer Immunotherapy Conference.
Dr June explained that CTL019 is a CD19-directed single chain variable fragment with a 4-1BB signaling module that transduces T cells with a lentiviral vector. The technology was developed at the University of Pennsylvania and subsequently licensed to Novartis.
In the phase 1 trial of CTL019 in CLL, patients who achieved complete remission have very high levels of CARs—100% of the circulating T cells—but the non-responders don’t. The CARs engrafted in non-responders but did not proliferate.
“So the biomarker correlate of success is persistence and proliferation, in CLL at least,” Dr June said.
The investigators performed IGH next-generation sequencing and found no detectable CLL clones in the complete responders, including 1 patient at 3.5 years and another at 4 years post-infusion.
“There was no clinically evident disease in these patients,” Dr June said, “and so the responses are durable.”
The team also believes that at least a subset of the cells remains functional because the patients still had B-cell aplasia.
The investigators have not observed a CD19 loss in any CLL patient who responded.
“Patients who have gone into remission stay in remission,” Dr June added.
Kinetics of delayed CR
Dr June discussed in detail Patient 10, whose response was somewhat different from the other complete responders. Patient 10 achieved a CR, but the response was delayed. It took 51 days after infusion, compared to about 10 days in the other complete responders.
Patient 10 was initially scored as a failure at the 28-day evaluation. Eventually, he had marked improvement, and, by a year, he was in CR.
He required hospitalization for tumor lysis syndrome and treatment with tocilizumab for cytokine release syndrome.
Patient 10 had a single cell that investigators surmise could have been responsible for the tumor elimination.
“In fact, on day 28, when he still had tumor, his CARs were polyclonal,” Dr June said. “So we stained and isolated his CARs by sorting, and, at time of tumor elimination, he had descendants of 1 CAR.”
Nevertheless, Patient 10’s response is durable. He is now 81 years old and remains engrafted with CAR19 cells.
Investigators hypothesize that the kinetics and CAR proliferation were so different in Patient 10 because Tet2 was disrupted by the integration of the CAR into the intronic region.
“What we don’t know is whether Tet2 was a passenger or a driver here,” Dr June observed. “Did it actually aid the function of the CAR cells or was it just a marker?”
He noted that Tet2 has been shown in acute myeloid leukemia to increase stem cell renewal, “and it may well have done that in this patient.”
mAb gets priority review as maintenance in CLL

Photo by Linda Bartlett
The US Food and Drug Administration (FDA) has granted priority review for an application for ofatumumab (Arzerra) as maintenance therapy in
patients with relapsed chronic lymphocytic leukemia (CLL).
The FDA grants priority review to investigational therapies that, if approved, may offer significant improvements in the treatment, prevention, or diagnosis of a serious condition.
The designation shortens the review period from 10 months to 6 months.
Ofatumumab is a human monoclonal antibody (mAb) designed to target CD20 on the surface of CLL cells and normal B lymphocytes.
The mAb is already FDA-approved to treat patients with CLL that is refractory to fludarabine and alemtuzumab. Ofatumumab is also approved for use in combination with chlorambucil to treat previously untreated patients with CLL for whom fludarabine-based therapy is considered inappropriate.
The FDA said it aims to complete its review of the application for ofatumumab as maintenance therapy in relapsed CLL by January 21, 2016.
PROLONG trial
The application for ofatumumab as maintenance is based on interim results from the phase 3 PROLONG (OMB112517) trial, which were presented at ASH 2014.
In this trial, researchers compared ofatumumab maintenance to no further treatment in patients with a complete or partial response after second-
or third-line treatment for CLL.
Interim results suggested that ofatumumab significantly improves progression-free survival but not overall survival.
The median progression-free survival was about 29 months in patients who received ofatumumab and about 15 months for patients who did not receive
maintenance (P<0.0001).
There was no significant difference in the median overall survival, which was not reached in either treatment arm.
Ofatumumab development
Ofatumumab is approved in more than 50 countries worldwide as monotherapy for CLL patients who are refractory to fludarabine and alemtuzumab.
In the European Union, ofatumumab is approved for use in combination with chlorambucil or bendamustine to treat CLL patients who have not received prior therapy and who are not eligible for fludarabine-based therapy.
Ofatumumab is not approved anywhere in the world as maintenance therapy for relapsed CLL. The drug is being developed by Genmab and Novartis.

Photo by Linda Bartlett
The US Food and Drug Administration (FDA) has granted priority review for an application for ofatumumab (Arzerra) as maintenance therapy in
patients with relapsed chronic lymphocytic leukemia (CLL).
The FDA grants priority review to investigational therapies that, if approved, may offer significant improvements in the treatment, prevention, or diagnosis of a serious condition.
The designation shortens the review period from 10 months to 6 months.
Ofatumumab is a human monoclonal antibody (mAb) designed to target CD20 on the surface of CLL cells and normal B lymphocytes.
The mAb is already FDA-approved to treat patients with CLL that is refractory to fludarabine and alemtuzumab. Ofatumumab is also approved for use in combination with chlorambucil to treat previously untreated patients with CLL for whom fludarabine-based therapy is considered inappropriate.
The FDA said it aims to complete its review of the application for ofatumumab as maintenance therapy in relapsed CLL by January 21, 2016.
PROLONG trial
The application for ofatumumab as maintenance is based on interim results from the phase 3 PROLONG (OMB112517) trial, which were presented at ASH 2014.
In this trial, researchers compared ofatumumab maintenance to no further treatment in patients with a complete or partial response after second-
or third-line treatment for CLL.
Interim results suggested that ofatumumab significantly improves progression-free survival but not overall survival.
The median progression-free survival was about 29 months in patients who received ofatumumab and about 15 months for patients who did not receive
maintenance (P<0.0001).
There was no significant difference in the median overall survival, which was not reached in either treatment arm.
Ofatumumab development
Ofatumumab is approved in more than 50 countries worldwide as monotherapy for CLL patients who are refractory to fludarabine and alemtuzumab.
In the European Union, ofatumumab is approved for use in combination with chlorambucil or bendamustine to treat CLL patients who have not received prior therapy and who are not eligible for fludarabine-based therapy.
Ofatumumab is not approved anywhere in the world as maintenance therapy for relapsed CLL. The drug is being developed by Genmab and Novartis.

Photo by Linda Bartlett
The US Food and Drug Administration (FDA) has granted priority review for an application for ofatumumab (Arzerra) as maintenance therapy in
patients with relapsed chronic lymphocytic leukemia (CLL).
The FDA grants priority review to investigational therapies that, if approved, may offer significant improvements in the treatment, prevention, or diagnosis of a serious condition.
The designation shortens the review period from 10 months to 6 months.
Ofatumumab is a human monoclonal antibody (mAb) designed to target CD20 on the surface of CLL cells and normal B lymphocytes.
The mAb is already FDA-approved to treat patients with CLL that is refractory to fludarabine and alemtuzumab. Ofatumumab is also approved for use in combination with chlorambucil to treat previously untreated patients with CLL for whom fludarabine-based therapy is considered inappropriate.
The FDA said it aims to complete its review of the application for ofatumumab as maintenance therapy in relapsed CLL by January 21, 2016.
PROLONG trial
The application for ofatumumab as maintenance is based on interim results from the phase 3 PROLONG (OMB112517) trial, which were presented at ASH 2014.
In this trial, researchers compared ofatumumab maintenance to no further treatment in patients with a complete or partial response after second-
or third-line treatment for CLL.
Interim results suggested that ofatumumab significantly improves progression-free survival but not overall survival.
The median progression-free survival was about 29 months in patients who received ofatumumab and about 15 months for patients who did not receive
maintenance (P<0.0001).
There was no significant difference in the median overall survival, which was not reached in either treatment arm.
Ofatumumab development
Ofatumumab is approved in more than 50 countries worldwide as monotherapy for CLL patients who are refractory to fludarabine and alemtuzumab.
In the European Union, ofatumumab is approved for use in combination with chlorambucil or bendamustine to treat CLL patients who have not received prior therapy and who are not eligible for fludarabine-based therapy.
Ofatumumab is not approved anywhere in the world as maintenance therapy for relapsed CLL. The drug is being developed by Genmab and Novartis.
CDK inhibitor active against lymphoma too

HOUSTON—Preclinical data suggest the second-generation cyclin-dependent kinase (CDK) inhibitor CYC065 is active against lymphomas as well as leukemias.
Previous research showed that CYC065 can fight acute myeloid leukemia (AML) in vitro and in vivo.
New research shows that CYC065 can decrease cell viability in a range of B-cell lymphoma cell lines, and the drug synergizes with both venetoclax and cytarabine.
Sheelagh Frame, PhD, and her colleagues presented these results at the SOHO 2015 Annual Meeting (poster 213). All of the investigators involved in the research are employees of Cyclacel Ltd., the company developing CYC065.
The investigators analyzed the anticancer activity of CYC065 in a range of cell lines and found that CYC065 induced apoptosis by inhibiting the expression of CDK9-dependent oncogenic transcripts, including Mcl-1, c-Myc, Hoxa9, and Meis1.
Results in AML
Experiments in the AML-MLL cell line MOLM-13 showed that short pulses of CYC065 (6 hours), rather than continuous treatment, were sufficient to achieve maximal cytotoxicity.
CYC065 induced apoptosis, in a dose-dependent manner, in other AML cell lines as well, including EOL-1 (MLL-PTD), MV4-11 (MLL-AF4, FLT3-ITD, and trisomy chr 8), HL60 (Myc amplified), and Kasumi-1.
The investigators noted that AML cell lines with MLL rearrangements were especially sensitive to CYC065, and the reliance of AML on Mcl-1 confers sensitivity to CYC065.
They also found evidence to suggest that Bak and Bcl-xL levels may be predictive of CYC065 response in AML. Cell lines that were less sensitive to treatment had high levels of Bcl-xL and negligible levels of Bak.
B-cell lymphomas
In B-cell lymphoma cell lines, the investigators observed a dose-dependent reduction in cell viability after CYC065 treatment (8-hour pulses).
CYC065 proved most effective in cell lines without genomic alterations associated with poor prognosis (HT and U-698-M) and in cell lines with Myc rearrangements (SU-DHL-8 and WILL-1).
The drug also decreased cell viability—but to a lesser degree—in cell lines with Bcl-2 rearrangements (SU-DHL-4 and U2932) and in double-hit lymphoma cell lines (MAVER-1, RI-1, SC-1, and SU-DHL-10).
The investigators therefore theorized that combining CYC065 with a Bcl-2 inhibitor might prove more effective in these cell lines.
CYC065 in combination
CYC065 synergized with the Bcl-2 inhibitor venetoclax in all B-cell lymphoma cell lines tested. The drugs were “strongly synergistic” in U2932 and RI-1 cell lines but simply “synergistic” in SU-CHL-4 and MAVER-1 cell lines.
CYC065 also synergized with cytarabine to fight AML. The combination proved synergistic at a range of doses in the HL60 and MV4-11 cell lines.
Considering these results together, the investigators concluded that CYC065 has shown potential for treating a range of leukemias and lymphomas with unmet clinical need, including MLL-rearranged leukemia and Myc-driven lymphoma.
And the drug might prove effective in combination with standard cytotoxic agents or agents targeting apoptotic regulators.

HOUSTON—Preclinical data suggest the second-generation cyclin-dependent kinase (CDK) inhibitor CYC065 is active against lymphomas as well as leukemias.
Previous research showed that CYC065 can fight acute myeloid leukemia (AML) in vitro and in vivo.
New research shows that CYC065 can decrease cell viability in a range of B-cell lymphoma cell lines, and the drug synergizes with both venetoclax and cytarabine.
Sheelagh Frame, PhD, and her colleagues presented these results at the SOHO 2015 Annual Meeting (poster 213). All of the investigators involved in the research are employees of Cyclacel Ltd., the company developing CYC065.
The investigators analyzed the anticancer activity of CYC065 in a range of cell lines and found that CYC065 induced apoptosis by inhibiting the expression of CDK9-dependent oncogenic transcripts, including Mcl-1, c-Myc, Hoxa9, and Meis1.
Results in AML
Experiments in the AML-MLL cell line MOLM-13 showed that short pulses of CYC065 (6 hours), rather than continuous treatment, were sufficient to achieve maximal cytotoxicity.
CYC065 induced apoptosis, in a dose-dependent manner, in other AML cell lines as well, including EOL-1 (MLL-PTD), MV4-11 (MLL-AF4, FLT3-ITD, and trisomy chr 8), HL60 (Myc amplified), and Kasumi-1.
The investigators noted that AML cell lines with MLL rearrangements were especially sensitive to CYC065, and the reliance of AML on Mcl-1 confers sensitivity to CYC065.
They also found evidence to suggest that Bak and Bcl-xL levels may be predictive of CYC065 response in AML. Cell lines that were less sensitive to treatment had high levels of Bcl-xL and negligible levels of Bak.
B-cell lymphomas
In B-cell lymphoma cell lines, the investigators observed a dose-dependent reduction in cell viability after CYC065 treatment (8-hour pulses).
CYC065 proved most effective in cell lines without genomic alterations associated with poor prognosis (HT and U-698-M) and in cell lines with Myc rearrangements (SU-DHL-8 and WILL-1).
The drug also decreased cell viability—but to a lesser degree—in cell lines with Bcl-2 rearrangements (SU-DHL-4 and U2932) and in double-hit lymphoma cell lines (MAVER-1, RI-1, SC-1, and SU-DHL-10).
The investigators therefore theorized that combining CYC065 with a Bcl-2 inhibitor might prove more effective in these cell lines.
CYC065 in combination
CYC065 synergized with the Bcl-2 inhibitor venetoclax in all B-cell lymphoma cell lines tested. The drugs were “strongly synergistic” in U2932 and RI-1 cell lines but simply “synergistic” in SU-CHL-4 and MAVER-1 cell lines.
CYC065 also synergized with cytarabine to fight AML. The combination proved synergistic at a range of doses in the HL60 and MV4-11 cell lines.
Considering these results together, the investigators concluded that CYC065 has shown potential for treating a range of leukemias and lymphomas with unmet clinical need, including MLL-rearranged leukemia and Myc-driven lymphoma.
And the drug might prove effective in combination with standard cytotoxic agents or agents targeting apoptotic regulators.

HOUSTON—Preclinical data suggest the second-generation cyclin-dependent kinase (CDK) inhibitor CYC065 is active against lymphomas as well as leukemias.
Previous research showed that CYC065 can fight acute myeloid leukemia (AML) in vitro and in vivo.
New research shows that CYC065 can decrease cell viability in a range of B-cell lymphoma cell lines, and the drug synergizes with both venetoclax and cytarabine.
Sheelagh Frame, PhD, and her colleagues presented these results at the SOHO 2015 Annual Meeting (poster 213). All of the investigators involved in the research are employees of Cyclacel Ltd., the company developing CYC065.
The investigators analyzed the anticancer activity of CYC065 in a range of cell lines and found that CYC065 induced apoptosis by inhibiting the expression of CDK9-dependent oncogenic transcripts, including Mcl-1, c-Myc, Hoxa9, and Meis1.
Results in AML
Experiments in the AML-MLL cell line MOLM-13 showed that short pulses of CYC065 (6 hours), rather than continuous treatment, were sufficient to achieve maximal cytotoxicity.
CYC065 induced apoptosis, in a dose-dependent manner, in other AML cell lines as well, including EOL-1 (MLL-PTD), MV4-11 (MLL-AF4, FLT3-ITD, and trisomy chr 8), HL60 (Myc amplified), and Kasumi-1.
The investigators noted that AML cell lines with MLL rearrangements were especially sensitive to CYC065, and the reliance of AML on Mcl-1 confers sensitivity to CYC065.
They also found evidence to suggest that Bak and Bcl-xL levels may be predictive of CYC065 response in AML. Cell lines that were less sensitive to treatment had high levels of Bcl-xL and negligible levels of Bak.
B-cell lymphomas
In B-cell lymphoma cell lines, the investigators observed a dose-dependent reduction in cell viability after CYC065 treatment (8-hour pulses).
CYC065 proved most effective in cell lines without genomic alterations associated with poor prognosis (HT and U-698-M) and in cell lines with Myc rearrangements (SU-DHL-8 and WILL-1).
The drug also decreased cell viability—but to a lesser degree—in cell lines with Bcl-2 rearrangements (SU-DHL-4 and U2932) and in double-hit lymphoma cell lines (MAVER-1, RI-1, SC-1, and SU-DHL-10).
The investigators therefore theorized that combining CYC065 with a Bcl-2 inhibitor might prove more effective in these cell lines.
CYC065 in combination
CYC065 synergized with the Bcl-2 inhibitor venetoclax in all B-cell lymphoma cell lines tested. The drugs were “strongly synergistic” in U2932 and RI-1 cell lines but simply “synergistic” in SU-CHL-4 and MAVER-1 cell lines.
CYC065 also synergized with cytarabine to fight AML. The combination proved synergistic at a range of doses in the HL60 and MV4-11 cell lines.
Considering these results together, the investigators concluded that CYC065 has shown potential for treating a range of leukemias and lymphomas with unmet clinical need, including MLL-rearranged leukemia and Myc-driven lymphoma.
And the drug might prove effective in combination with standard cytotoxic agents or agents targeting apoptotic regulators.
CAR T-cell therapy tested in Sweden
NEW YORK—For the first time, according to researchers, chimeric antigen receptor (CAR) T-cell therapy has been tested in a clinical trial in Sweden.
Early results have shown the treatment can produce complete responses (CRs) in leukemia and lymphoma, although most patients ultimately progressed.
Hannah Karlsson, PhD, of Uppsala University in Sweden, presented data from the phase 1/2a trial of the third-generation CD19 CAR T-cell therapy (abstract A041*) at the inaugural CRI-CIMT-EATI-AACR International Cancer Immunotherapy Conference.
The trial is a collaboration between Uppsala University and Baylor College of Medicine and was funded by AFA Insurances AB and the Swedish Cancer Society.
“Third-generation CAR T cells are being tested in clinical trials for leukemia patients in the United States with success,” said senior study author Angelica Loskog, PhD, also of Uppsala University.
“[T]he main purpose of our clinical trial was to evaluate whether we could reproduce the successful results in leukemia patients in Sweden and to also test if patients with lymphoma will also respond to this treatment.”
So the investigators enrolled 13 patients, 11 of whom were evaluable for efficacy at 3 months after CAR T-cell infusion. All patients had relapsed or refractory, CD19-positive, B-cell disease.
Two patients had acute lymphoblastic leukemia (ALL), 2 had chronic lymphocytic leukemia (CLL), and 7 had lymphoma—3 with diffuse large B-cell lymphoma (DLBCL), 2 with mantle cell lymphoma (MCL), 1 with follicular lymphoma (FL)/DLBCL, and 1 with Burkitt lymphoma.
All of the lymphoma patients received chemotherapy before CAR T-cell infusion to shrink their tumors. Seven patients—3 with leukemia and 4 with lymphoma—received pre-conditioning with cyclophosphamide plus fludarabine to reduce their immunosuppressive cell counts.
The investigators used CAR T cells containing signaling domains from both CD28 and 4-1BB and manufactured using a gamma retrovirus.
Patients received a single infusion of the CAR T cells, 2 patients at a dose of 2 x 107 cells/m2, 4 at a dose of 1 x 108 cells/m2, and 5 at 2 x 108 cells/m2.
Response and toxicity
Six patients had achieved a CR at the time of evaluation.
One patient with DLBCL experienced mild cytokine release syndrome (CRS) before achieving CR. However, the patient relapsed after a second CRS occurred (after 3 months).
Another DLBCL patient achieved a CR prior to T-cell infusion and remained in CR for 6 months before progressing.
One CLL patient and another DLBCL patient responded prior to T-cell infusion and remained in CR for more than 3 months. The CLL patient was still in CR at the time of the meeting.
One of the ALL patients achieved a CR after transient central nervous system toxicity but relapsed at 3 months with CD19-negative ALL. The other ALL patient was in CR for more than a month after experiencing CRS but ultimately progressed.
One CLL patient and 2 MCL patients had all progressed by 3 months.
The FL/DLBCL patient progressed after 1 month, with mild CRS. And the patient with Burkitt lymphoma had major CRS and progressive disease.
The investigators noted that 5 of the 6 patients who received pre-conditioning treatment had initial CRs.
The team is now analyzing whether there is any correlation between the level of immunosuppressive cells and patient response.
*Information presented at the meeting differs from the abstract.
NEW YORK—For the first time, according to researchers, chimeric antigen receptor (CAR) T-cell therapy has been tested in a clinical trial in Sweden.
Early results have shown the treatment can produce complete responses (CRs) in leukemia and lymphoma, although most patients ultimately progressed.
Hannah Karlsson, PhD, of Uppsala University in Sweden, presented data from the phase 1/2a trial of the third-generation CD19 CAR T-cell therapy (abstract A041*) at the inaugural CRI-CIMT-EATI-AACR International Cancer Immunotherapy Conference.
The trial is a collaboration between Uppsala University and Baylor College of Medicine and was funded by AFA Insurances AB and the Swedish Cancer Society.
“Third-generation CAR T cells are being tested in clinical trials for leukemia patients in the United States with success,” said senior study author Angelica Loskog, PhD, also of Uppsala University.
“[T]he main purpose of our clinical trial was to evaluate whether we could reproduce the successful results in leukemia patients in Sweden and to also test if patients with lymphoma will also respond to this treatment.”
So the investigators enrolled 13 patients, 11 of whom were evaluable for efficacy at 3 months after CAR T-cell infusion. All patients had relapsed or refractory, CD19-positive, B-cell disease.
Two patients had acute lymphoblastic leukemia (ALL), 2 had chronic lymphocytic leukemia (CLL), and 7 had lymphoma—3 with diffuse large B-cell lymphoma (DLBCL), 2 with mantle cell lymphoma (MCL), 1 with follicular lymphoma (FL)/DLBCL, and 1 with Burkitt lymphoma.
All of the lymphoma patients received chemotherapy before CAR T-cell infusion to shrink their tumors. Seven patients—3 with leukemia and 4 with lymphoma—received pre-conditioning with cyclophosphamide plus fludarabine to reduce their immunosuppressive cell counts.
The investigators used CAR T cells containing signaling domains from both CD28 and 4-1BB and manufactured using a gamma retrovirus.
Patients received a single infusion of the CAR T cells, 2 patients at a dose of 2 x 107 cells/m2, 4 at a dose of 1 x 108 cells/m2, and 5 at 2 x 108 cells/m2.
Response and toxicity
Six patients had achieved a CR at the time of evaluation.
One patient with DLBCL experienced mild cytokine release syndrome (CRS) before achieving CR. However, the patient relapsed after a second CRS occurred (after 3 months).
Another DLBCL patient achieved a CR prior to T-cell infusion and remained in CR for 6 months before progressing.
One CLL patient and another DLBCL patient responded prior to T-cell infusion and remained in CR for more than 3 months. The CLL patient was still in CR at the time of the meeting.
One of the ALL patients achieved a CR after transient central nervous system toxicity but relapsed at 3 months with CD19-negative ALL. The other ALL patient was in CR for more than a month after experiencing CRS but ultimately progressed.
One CLL patient and 2 MCL patients had all progressed by 3 months.
The FL/DLBCL patient progressed after 1 month, with mild CRS. And the patient with Burkitt lymphoma had major CRS and progressive disease.
The investigators noted that 5 of the 6 patients who received pre-conditioning treatment had initial CRs.
The team is now analyzing whether there is any correlation between the level of immunosuppressive cells and patient response.
*Information presented at the meeting differs from the abstract.
NEW YORK—For the first time, according to researchers, chimeric antigen receptor (CAR) T-cell therapy has been tested in a clinical trial in Sweden.
Early results have shown the treatment can produce complete responses (CRs) in leukemia and lymphoma, although most patients ultimately progressed.
Hannah Karlsson, PhD, of Uppsala University in Sweden, presented data from the phase 1/2a trial of the third-generation CD19 CAR T-cell therapy (abstract A041*) at the inaugural CRI-CIMT-EATI-AACR International Cancer Immunotherapy Conference.
The trial is a collaboration between Uppsala University and Baylor College of Medicine and was funded by AFA Insurances AB and the Swedish Cancer Society.
“Third-generation CAR T cells are being tested in clinical trials for leukemia patients in the United States with success,” said senior study author Angelica Loskog, PhD, also of Uppsala University.
“[T]he main purpose of our clinical trial was to evaluate whether we could reproduce the successful results in leukemia patients in Sweden and to also test if patients with lymphoma will also respond to this treatment.”
So the investigators enrolled 13 patients, 11 of whom were evaluable for efficacy at 3 months after CAR T-cell infusion. All patients had relapsed or refractory, CD19-positive, B-cell disease.
Two patients had acute lymphoblastic leukemia (ALL), 2 had chronic lymphocytic leukemia (CLL), and 7 had lymphoma—3 with diffuse large B-cell lymphoma (DLBCL), 2 with mantle cell lymphoma (MCL), 1 with follicular lymphoma (FL)/DLBCL, and 1 with Burkitt lymphoma.
All of the lymphoma patients received chemotherapy before CAR T-cell infusion to shrink their tumors. Seven patients—3 with leukemia and 4 with lymphoma—received pre-conditioning with cyclophosphamide plus fludarabine to reduce their immunosuppressive cell counts.
The investigators used CAR T cells containing signaling domains from both CD28 and 4-1BB and manufactured using a gamma retrovirus.
Patients received a single infusion of the CAR T cells, 2 patients at a dose of 2 x 107 cells/m2, 4 at a dose of 1 x 108 cells/m2, and 5 at 2 x 108 cells/m2.
Response and toxicity
Six patients had achieved a CR at the time of evaluation.
One patient with DLBCL experienced mild cytokine release syndrome (CRS) before achieving CR. However, the patient relapsed after a second CRS occurred (after 3 months).
Another DLBCL patient achieved a CR prior to T-cell infusion and remained in CR for 6 months before progressing.
One CLL patient and another DLBCL patient responded prior to T-cell infusion and remained in CR for more than 3 months. The CLL patient was still in CR at the time of the meeting.
One of the ALL patients achieved a CR after transient central nervous system toxicity but relapsed at 3 months with CD19-negative ALL. The other ALL patient was in CR for more than a month after experiencing CRS but ultimately progressed.
One CLL patient and 2 MCL patients had all progressed by 3 months.
The FL/DLBCL patient progressed after 1 month, with mild CRS. And the patient with Burkitt lymphoma had major CRS and progressive disease.
The investigators noted that 5 of the 6 patients who received pre-conditioning treatment had initial CRs.
The team is now analyzing whether there is any correlation between the level of immunosuppressive cells and patient response.
*Information presented at the meeting differs from the abstract.