User login
HM@15 - Is Hospital Medicine a Good Bet for Improving Patient Satisfaction?
At first glance, the deck might seem hopelessly stacked against hospitalists with regard to patient satisfaction. HM practitioners lack the long-term relationship with patients that many primary-care physicians (PCPs) have established. Unlike surgeons and other specialists, they tend to care for those patients—more complicated, lacking a regular doctor, or admitted through the ED, for example—who are more inclined to rate their hospital stay unfavorably.1 They may not even be accurately remembered by patients who encounter multiple doctors during the course of their hospitalization.2 And hospital information systems can misidentify the treating physician, while the actual surveys used to gauge hospitalists have been imperfect at best.3
And yet, the hospitalist model has evolved substantially on the question of how it can impact patient perceptions of care.
Initially, hospitalist champions adopted a largely defensive posture: The model would not negatively impact patient satisfaction as it delivered on efficiency—and later on quality. The healthcare system, however, is beginning to recognize the hospitalist as part of a care “team” whose patient-centered approach might pay big dividends in the inpatient experience and, eventually, on satisfaction scores.
“I think the next phase, which is a focus on the hospitalist as a team member and team builder, is going to be key,” says William Southern, MD, MPH, SFHM, chief of the division of hospital medicine at Montefiore Medical Center in Bronx, N.Y.
Recent studies suggest that hospitalists are helping to design and test new tools that will not only improve satisfaction, but also more fairly assess the impact of individual doctors. As the maturation process continues, experts say, hospitalists have an opportunity to influence both provider-based interventions and more programmatic decision-making that can have far-reaching effects. Certainly, the hand dealt to hospitalists is looking more favorable even as the ante has been raised with Medicare programs like value-based purchasing, and its pot of money tied to patient perceptions of care.
So how have hospitalists played their cards so far?
A Look at the Evidence
In its early years, the HM model faced a persistent criticism: Replacing traditional caregivers with these new inpatient providers in the name of efficiency would increase handoffs and, therefore, discontinuities of care delivered by a succession of unfamiliar faces. If patients didn’t see their PCP in the hospital, the thinking went, they might be more disgruntled at being tended to by hospitalists, leading to lower satisfaction scores.4
A particularly heated exchange played out in 1999 in the New England Journal of Medicine. Farris A. Manian, MD, MPH, of Infectious Disease Consultants in St. Louis wrote in one letter, “I am particularly concerned about what impressionable house-staff members will learn from hospitalists who place an inordinate emphasis on cost rather than the quality of patient care or teaching.”5
A few subsequent studies, however, hinted that such concerns might be overstated. A 2000 analysis in the American Journal of Medicine that examined North Mississippi Health Services in Tupelo, for instance, found that care administered by hospitalists led to a shorter length of stay and lower costs than care delivered by internists. Importantly, the study found that patient satisfaction was similar for both models, while quality metrics were likewise equal or even tilted slightly toward hospitalists.6
In their influential 2002 review of a profession that was only a half-decade old, Robert Wachter, MD, MHM, and Lee Goldman, MD, MPH, FACP from the University of California at San Francisco reinforced the message that HM wouldn’t lead to unhappy patients. “Empirical research supports the premise that hospitalists improve inpatient efficiency without harmful effects on quality or patient satisfaction,” they asserted.7
Among pediatric patients, a 2005 review found that “none of the four studies that evaluated patient satisfaction found statistically significant differences in satisfaction with inpatient care. However, two of the three evaluations that did assess parents’ satisfaction with care provided to their children found that parents were more satisfied with some aspects of care provided by hospitalists.”8

—William Southern, MD, chief, division of hospital medicine, Montefiore Medical Center, Bronx, N.Y.
Similar findings were popping up around the country: Replacing an internal medicine residency program with a physician assistant/hospitalist model at Brooklyn, N.Y.’s Coney Island Hospital did not adversely impact patient satisfaction, while it significantly improved mortality.9 Brigham & Women’s Hospital in Boston likewise reported no change in patient satisfaction in a study comparing a physician assistant/hospitalist service with traditional house staff services.10
The shift toward a more proactive position on patient satisfaction is exemplified within a 2008 white paper, “Hospitalists Meeting the Challenge of Patient Satisfaction,” written by a group of 19 private-practice HM experts known as The Phoenix Group.3 The paper acknowledged the flaws and limitations of existing survey methodologies, including Medicare’s Hospital Consumer Assessment of Healthcare Providers and Systems (HCAHPS) scores. Even so, the authors urged practice groups to adopt a team-oriented approach to communicate to hospital administrations “the belief that hospitalists are in the best position to improve survey scores overall for the facility.”
Carle Foundation Hospital in Urbana, Ill., is now publicly advertising its HM service’s contribution to high patient satisfaction scores on its website, and underscoring the hospitalists’ consistency, accessibility, and communication skills. “The hospital is never without a hospitalist, and our nurses know that they can rely on them,” says Lynn Barnes, vice president of hospital operations. “They’re available, they’re within a few minutes away, and patients’ needs get met very efficiently and rapidly.”
As a result, she says, their presence can lead to higher scores in patients’ perceptions of communication.
Hospitalists also have been central to several safety initiatives at Carle. Napoleon Knight, MD, medical director of hospital medicine and associate vice president for quality, says the HM team has helped address undiagnosed sleep apnea and implement rapid responses, such as “Code Speed.” Caregivers or family members can use the code to immediately call for help if they detect a downturn in a patient’s condition.
The ongoing initiatives, Dr. Knight and Barnes say, are helping the hospital improve how patients and their loved ones perceive care as Carle adapts to a rapidly shifting healthcare landscape. “With all of the changes that seem to be coming from the external environment weekly, we want to work collaboratively to make sure we’re connected and aligned and communicating in an ongoing fashion so we can react to all of these changes,” Dr. Knight says.
Continued below...
A Hopeful Trend
So far, evidence that the HM model is more broadly raising patient satisfaction scores is largely anecdotal. But a few analyses suggest the trend is moving in the right direction. A recent study in the American Journal of Medical Quality, for instance, concludes that facilities with hospitalists might have an advantage in patient satisfaction with nursing and such personal issues as privacy, emotional needs, and response to complaints.11 The study also posits that teaching facilities employing hospitalists could see benefits in overall satisfaction, while large facilities with hospitalists might see gains in satisfaction with admissions, nursing, and tests and treatments.
Brad Fulton, PhD, a researcher at South Bend, Ind.-based healthcare consulting firm Press Ganey and the study’s lead author, says the 30,000-foot view of patient satisfaction at the facility level can get foggy in a hurry due to differences in the kind and size of hospitalist programs. “And despite all of that fog, we’re still able to see through that and find something,” he says.
One limitation is that the study findings could also reflect differences in the culture of facilities that choose to add hospitalists. That caveat means it might not be possible to completely untangle the effect of an HM group on inpatient care from the larger, hospitalwide values that have allowed the group to set up shop. The wrinkle brings its own fascinating questions, according to Fulton. For example, is that kind of culture necessary for hospitalists to function as well as they do?

—Lynn Barnes, vice president of hospital operations, Carle Foundation Hospital, Urbana, Ill.
Such considerations will become more important as the healthcare system places additional emphasis on patient satisfaction, as Medicare’s value-based purchasing program is doing through its HCAHPS scores. With all the changes, success or failure on the patient experience front is going to carry “not just a reputational import, but also a financial impact,” says Ethan Cumbler, MD, FACP, director of Acute Care for the Elderly (ACE) Service at the University of Colorado Denver.
So how can HM fairly and accurately assess its own practitioners? “I think one starts by trying to apply some of the rigor that we have learned from our experience as hospitalists in quality improvement to the more warm and fuzzy field of patient experience,” Dr. Cumbler says. Many hospitals employ surveys supplied by consultants like Press Ganey to track the global patient satisfaction for their institution, he says.
“But for an individual hospitalist or hospitalist group, that kind of tool often lacks both the specificity and the timeliness necessary to make good decisions about impact of interventions on patient satisfaction,” he says.
Mark Williams, MD, FACP, FHM, professor and chief of the division of hospital medicine at Northwestern University’s Feinberg School of Medicine in Chicago, agrees that such imprecision could lead to unfair assessments. “You can imagine a scenario where a patient actually liked their hospitalist very much,” he says, “but when they got the survey, they said [their stay] was terrible and the reasons being because maybe the nurse call button was not answered and the food was terrible and medications were given to them incorrectly, or it was noisy at night so they couldn’t sleep.”
A recent study by Dr. Williams and his colleagues, in which they employed a new assessment method called the Communication Assessment Tool (CAT), confirmed the group’s suspicions: “that the results from the Press Ganey didn’t match up with the CAT, which was a direct assessment of the patient’s perception of the hospitalist’s communication skills,” he says.12
The validated tool, he adds, provides directed feedback to the physician based on the percentage of patients rating that provider as excellent, instead of on the average total score. Hospitalists have felt vindicated by the results. “They were very nervous because the hospital talked about basing an incentive off of the Press Ganey scores, and we said, ‘You can’t do that,’ because we didn’t feel they were accurate, and this study proved that,” Dr. Williams explains.
Fortunately, the message has reached researchers and consultants alike, and better tools are starting to reach hospitals around the country. At HM11 in May, Press Ganey unveiled a new survey designed to help patients assess the care delivered by two hospitalists, the average for inpatient stays. The item set is specific to HM functions, and includes the photo and name of each hospitalist, which Fulton says should improve the validity and accuracy of the data.
“The early response looks really good,” Fulton says, though it’s too early to say whether the tool, called Hospitalist Insight, will live up to its billing. If it proves its mettle, Fulton says, the survey could be used to reward top-performing hospitalists, and the growing dataset could allow hospitals to compare themselves with appropriate peer groups for fairer comparisons.
Meanwhile, researchers are testing out checklists to score hospitalist etiquette, and tracking and paging systems to help ensure continuity of care. They have found increased patient satisfaction when doctors engage in verbal communication during a discharge, in interdisciplinary team rounding, and in efforts to address religious and spiritual concerns.
Since 2000, when Montefiore’s hospitalist program began, Dr. Southern says the hospital has explained to patients the tradeoff accompanying the HM model. “I say something like this to every patient: ‘I know I’m not the doctor that you know, and you’re just meeting me. The downside is that you haven’t met me before and I’m a new face, but the upside is that if you need me during the day, I’m here all the time, I’m not someplace else. And so if you need something, I can be here quickly.’ ”
Being very explicit about that tradeoff, he says, has made patients very comfortable with the model of care, especially during a crisis moment in their lives. “I think it’s really important to say, ‘I know you don’t know me, but here’s the upside.’ And my experience is that patients easily understand that tradeoff and are very positive,” Dr. Southern says.
The Verdict
Available evidence suggests that practitioners of the HM model have pivoted from defending against early criticism that they may harm patient satisfaction to pitching themselves as team leaders who can boost facilitywide perceptions of care. So far, too little research has been conducted to suggest whether that optimism is fully warranted, but early signs look promising.
At facilities like Chicago’s Northwestern Memorial Hospital, medical floors staffed by hospitalists are beginning to beat out surgical floors for the traveling patient satisfaction award. And experts like Dr. Cumbler are pondering how ongoing initiatives to boost scores can follow in the footsteps of efficiency and quality-raising efforts by making the transition from focusing on individual doctors to adopting a more programmatic approach. “What’s happening to that patient during the 23 hours and 45 minutes of their hospital day that you are not sitting by the bedside? And what influence should a hospitalist have in affecting that other 23 hours and 45 minutes?” he says.
Handoffs, discharges, communication with PCPs, and other potential weak points in maintaining high levels of patient satisfaction, Dr. Cumbler says, all are amenable to systems-based improvement. “As hospitalists, we are in a unique position to influence not only our one-one-one interaction with the patient, but also to influence that system of care in a way that patients will notice in a real and tangible way,” he says. “I think we’ve recognized for some time that a healthy heart but a miserable patient is not a healthy person.”
Bryn Nelson is a freelance medical journalist based in Seattle.
References
- Williams M, Flanders SA, Whitcomb WF. Comprehensive hospital medicine: an evidence based approach. Elsevier;2007:971-976.
- Arora V, Gangireddy S, Mehrotra A, Ginde R, Tormey M, Meltzer D. Ability of hospitalized patients to identify their in-hospital physicians. Arch Intern Med. 2009;169(2):199-201.
- Singer AS, et al. Hospitalists meeting the challenge of patient satisfaction. The Phoenix Group. 2008;1-5.
- Manian FA. Whither continuity of care? N Engl J Med. 1999;340:1362-1363.
- Correspondence. Whither continuity of care? N Engl J Med. 1999;341:850-852.
- Davis KM, Koch KE, Harvey JK, et al. Effects of hospitalists on cost, outcomes, and patient satisfaction in a rural health system. Amer J Med. 2000;108(8):621-626.
- Wachter RM, Goldman L. The hospitalist movement 5 years later. JAMA. 2002;287(4):487-494.
- Coffman J, Rundall TG. The impact of hospitalists on the cost and quality of inpatient care in the United States (a research synthesis). Med Care Res Rev. 2005;62:379–406.
- Dhuper S, Choksi S. Replacing an academic internal medicine residency program with a physician assistant-hospitalist model: a comparative analysis study. Am J Med Qual. 2009;24(2):132-139.
- Roy CL, Liang CL, Lund M, et al. Implementation of a physician assistant/hospitalist service in an academic medical center: impact on efficiency and patient outcomes. J Hosp Med. 2008;3(5):361-368.
- Fulton BR, Drevs KE, Ayala LJ, Malott DL Jr. Patient satisfaction with hospitalists: facility-level analyses. Am J Med Qual. 2011;26(2):95-102.
- Ferranti DE, Makoul G, Forth VE, Rauworth J, Lee J, Williams MV. Assessing patient perceptions of hospitalist communication skills using the Communication Assessment Tool (CAT). J Hosp Med. 2010;5(9):522-527.
At first glance, the deck might seem hopelessly stacked against hospitalists with regard to patient satisfaction. HM practitioners lack the long-term relationship with patients that many primary-care physicians (PCPs) have established. Unlike surgeons and other specialists, they tend to care for those patients—more complicated, lacking a regular doctor, or admitted through the ED, for example—who are more inclined to rate their hospital stay unfavorably.1 They may not even be accurately remembered by patients who encounter multiple doctors during the course of their hospitalization.2 And hospital information systems can misidentify the treating physician, while the actual surveys used to gauge hospitalists have been imperfect at best.3
And yet, the hospitalist model has evolved substantially on the question of how it can impact patient perceptions of care.
Initially, hospitalist champions adopted a largely defensive posture: The model would not negatively impact patient satisfaction as it delivered on efficiency—and later on quality. The healthcare system, however, is beginning to recognize the hospitalist as part of a care “team” whose patient-centered approach might pay big dividends in the inpatient experience and, eventually, on satisfaction scores.
“I think the next phase, which is a focus on the hospitalist as a team member and team builder, is going to be key,” says William Southern, MD, MPH, SFHM, chief of the division of hospital medicine at Montefiore Medical Center in Bronx, N.Y.
Recent studies suggest that hospitalists are helping to design and test new tools that will not only improve satisfaction, but also more fairly assess the impact of individual doctors. As the maturation process continues, experts say, hospitalists have an opportunity to influence both provider-based interventions and more programmatic decision-making that can have far-reaching effects. Certainly, the hand dealt to hospitalists is looking more favorable even as the ante has been raised with Medicare programs like value-based purchasing, and its pot of money tied to patient perceptions of care.
So how have hospitalists played their cards so far?
A Look at the Evidence
In its early years, the HM model faced a persistent criticism: Replacing traditional caregivers with these new inpatient providers in the name of efficiency would increase handoffs and, therefore, discontinuities of care delivered by a succession of unfamiliar faces. If patients didn’t see their PCP in the hospital, the thinking went, they might be more disgruntled at being tended to by hospitalists, leading to lower satisfaction scores.4
A particularly heated exchange played out in 1999 in the New England Journal of Medicine. Farris A. Manian, MD, MPH, of Infectious Disease Consultants in St. Louis wrote in one letter, “I am particularly concerned about what impressionable house-staff members will learn from hospitalists who place an inordinate emphasis on cost rather than the quality of patient care or teaching.”5
A few subsequent studies, however, hinted that such concerns might be overstated. A 2000 analysis in the American Journal of Medicine that examined North Mississippi Health Services in Tupelo, for instance, found that care administered by hospitalists led to a shorter length of stay and lower costs than care delivered by internists. Importantly, the study found that patient satisfaction was similar for both models, while quality metrics were likewise equal or even tilted slightly toward hospitalists.6
In their influential 2002 review of a profession that was only a half-decade old, Robert Wachter, MD, MHM, and Lee Goldman, MD, MPH, FACP from the University of California at San Francisco reinforced the message that HM wouldn’t lead to unhappy patients. “Empirical research supports the premise that hospitalists improve inpatient efficiency without harmful effects on quality or patient satisfaction,” they asserted.7
Among pediatric patients, a 2005 review found that “none of the four studies that evaluated patient satisfaction found statistically significant differences in satisfaction with inpatient care. However, two of the three evaluations that did assess parents’ satisfaction with care provided to their children found that parents were more satisfied with some aspects of care provided by hospitalists.”8

—William Southern, MD, chief, division of hospital medicine, Montefiore Medical Center, Bronx, N.Y.
Similar findings were popping up around the country: Replacing an internal medicine residency program with a physician assistant/hospitalist model at Brooklyn, N.Y.’s Coney Island Hospital did not adversely impact patient satisfaction, while it significantly improved mortality.9 Brigham & Women’s Hospital in Boston likewise reported no change in patient satisfaction in a study comparing a physician assistant/hospitalist service with traditional house staff services.10
The shift toward a more proactive position on patient satisfaction is exemplified within a 2008 white paper, “Hospitalists Meeting the Challenge of Patient Satisfaction,” written by a group of 19 private-practice HM experts known as The Phoenix Group.3 The paper acknowledged the flaws and limitations of existing survey methodologies, including Medicare’s Hospital Consumer Assessment of Healthcare Providers and Systems (HCAHPS) scores. Even so, the authors urged practice groups to adopt a team-oriented approach to communicate to hospital administrations “the belief that hospitalists are in the best position to improve survey scores overall for the facility.”
Carle Foundation Hospital in Urbana, Ill., is now publicly advertising its HM service’s contribution to high patient satisfaction scores on its website, and underscoring the hospitalists’ consistency, accessibility, and communication skills. “The hospital is never without a hospitalist, and our nurses know that they can rely on them,” says Lynn Barnes, vice president of hospital operations. “They’re available, they’re within a few minutes away, and patients’ needs get met very efficiently and rapidly.”
As a result, she says, their presence can lead to higher scores in patients’ perceptions of communication.
Hospitalists also have been central to several safety initiatives at Carle. Napoleon Knight, MD, medical director of hospital medicine and associate vice president for quality, says the HM team has helped address undiagnosed sleep apnea and implement rapid responses, such as “Code Speed.” Caregivers or family members can use the code to immediately call for help if they detect a downturn in a patient’s condition.
The ongoing initiatives, Dr. Knight and Barnes say, are helping the hospital improve how patients and their loved ones perceive care as Carle adapts to a rapidly shifting healthcare landscape. “With all of the changes that seem to be coming from the external environment weekly, we want to work collaboratively to make sure we’re connected and aligned and communicating in an ongoing fashion so we can react to all of these changes,” Dr. Knight says.
Continued below...
A Hopeful Trend
So far, evidence that the HM model is more broadly raising patient satisfaction scores is largely anecdotal. But a few analyses suggest the trend is moving in the right direction. A recent study in the American Journal of Medical Quality, for instance, concludes that facilities with hospitalists might have an advantage in patient satisfaction with nursing and such personal issues as privacy, emotional needs, and response to complaints.11 The study also posits that teaching facilities employing hospitalists could see benefits in overall satisfaction, while large facilities with hospitalists might see gains in satisfaction with admissions, nursing, and tests and treatments.
Brad Fulton, PhD, a researcher at South Bend, Ind.-based healthcare consulting firm Press Ganey and the study’s lead author, says the 30,000-foot view of patient satisfaction at the facility level can get foggy in a hurry due to differences in the kind and size of hospitalist programs. “And despite all of that fog, we’re still able to see through that and find something,” he says.
One limitation is that the study findings could also reflect differences in the culture of facilities that choose to add hospitalists. That caveat means it might not be possible to completely untangle the effect of an HM group on inpatient care from the larger, hospitalwide values that have allowed the group to set up shop. The wrinkle brings its own fascinating questions, according to Fulton. For example, is that kind of culture necessary for hospitalists to function as well as they do?

—Lynn Barnes, vice president of hospital operations, Carle Foundation Hospital, Urbana, Ill.
Such considerations will become more important as the healthcare system places additional emphasis on patient satisfaction, as Medicare’s value-based purchasing program is doing through its HCAHPS scores. With all the changes, success or failure on the patient experience front is going to carry “not just a reputational import, but also a financial impact,” says Ethan Cumbler, MD, FACP, director of Acute Care for the Elderly (ACE) Service at the University of Colorado Denver.
So how can HM fairly and accurately assess its own practitioners? “I think one starts by trying to apply some of the rigor that we have learned from our experience as hospitalists in quality improvement to the more warm and fuzzy field of patient experience,” Dr. Cumbler says. Many hospitals employ surveys supplied by consultants like Press Ganey to track the global patient satisfaction for their institution, he says.
“But for an individual hospitalist or hospitalist group, that kind of tool often lacks both the specificity and the timeliness necessary to make good decisions about impact of interventions on patient satisfaction,” he says.
Mark Williams, MD, FACP, FHM, professor and chief of the division of hospital medicine at Northwestern University’s Feinberg School of Medicine in Chicago, agrees that such imprecision could lead to unfair assessments. “You can imagine a scenario where a patient actually liked their hospitalist very much,” he says, “but when they got the survey, they said [their stay] was terrible and the reasons being because maybe the nurse call button was not answered and the food was terrible and medications were given to them incorrectly, or it was noisy at night so they couldn’t sleep.”
A recent study by Dr. Williams and his colleagues, in which they employed a new assessment method called the Communication Assessment Tool (CAT), confirmed the group’s suspicions: “that the results from the Press Ganey didn’t match up with the CAT, which was a direct assessment of the patient’s perception of the hospitalist’s communication skills,” he says.12
The validated tool, he adds, provides directed feedback to the physician based on the percentage of patients rating that provider as excellent, instead of on the average total score. Hospitalists have felt vindicated by the results. “They were very nervous because the hospital talked about basing an incentive off of the Press Ganey scores, and we said, ‘You can’t do that,’ because we didn’t feel they were accurate, and this study proved that,” Dr. Williams explains.
Fortunately, the message has reached researchers and consultants alike, and better tools are starting to reach hospitals around the country. At HM11 in May, Press Ganey unveiled a new survey designed to help patients assess the care delivered by two hospitalists, the average for inpatient stays. The item set is specific to HM functions, and includes the photo and name of each hospitalist, which Fulton says should improve the validity and accuracy of the data.
“The early response looks really good,” Fulton says, though it’s too early to say whether the tool, called Hospitalist Insight, will live up to its billing. If it proves its mettle, Fulton says, the survey could be used to reward top-performing hospitalists, and the growing dataset could allow hospitals to compare themselves with appropriate peer groups for fairer comparisons.
Meanwhile, researchers are testing out checklists to score hospitalist etiquette, and tracking and paging systems to help ensure continuity of care. They have found increased patient satisfaction when doctors engage in verbal communication during a discharge, in interdisciplinary team rounding, and in efforts to address religious and spiritual concerns.
Since 2000, when Montefiore’s hospitalist program began, Dr. Southern says the hospital has explained to patients the tradeoff accompanying the HM model. “I say something like this to every patient: ‘I know I’m not the doctor that you know, and you’re just meeting me. The downside is that you haven’t met me before and I’m a new face, but the upside is that if you need me during the day, I’m here all the time, I’m not someplace else. And so if you need something, I can be here quickly.’ ”
Being very explicit about that tradeoff, he says, has made patients very comfortable with the model of care, especially during a crisis moment in their lives. “I think it’s really important to say, ‘I know you don’t know me, but here’s the upside.’ And my experience is that patients easily understand that tradeoff and are very positive,” Dr. Southern says.
The Verdict
Available evidence suggests that practitioners of the HM model have pivoted from defending against early criticism that they may harm patient satisfaction to pitching themselves as team leaders who can boost facilitywide perceptions of care. So far, too little research has been conducted to suggest whether that optimism is fully warranted, but early signs look promising.
At facilities like Chicago’s Northwestern Memorial Hospital, medical floors staffed by hospitalists are beginning to beat out surgical floors for the traveling patient satisfaction award. And experts like Dr. Cumbler are pondering how ongoing initiatives to boost scores can follow in the footsteps of efficiency and quality-raising efforts by making the transition from focusing on individual doctors to adopting a more programmatic approach. “What’s happening to that patient during the 23 hours and 45 minutes of their hospital day that you are not sitting by the bedside? And what influence should a hospitalist have in affecting that other 23 hours and 45 minutes?” he says.
Handoffs, discharges, communication with PCPs, and other potential weak points in maintaining high levels of patient satisfaction, Dr. Cumbler says, all are amenable to systems-based improvement. “As hospitalists, we are in a unique position to influence not only our one-one-one interaction with the patient, but also to influence that system of care in a way that patients will notice in a real and tangible way,” he says. “I think we’ve recognized for some time that a healthy heart but a miserable patient is not a healthy person.”
Bryn Nelson is a freelance medical journalist based in Seattle.
References
- Williams M, Flanders SA, Whitcomb WF. Comprehensive hospital medicine: an evidence based approach. Elsevier;2007:971-976.
- Arora V, Gangireddy S, Mehrotra A, Ginde R, Tormey M, Meltzer D. Ability of hospitalized patients to identify their in-hospital physicians. Arch Intern Med. 2009;169(2):199-201.
- Singer AS, et al. Hospitalists meeting the challenge of patient satisfaction. The Phoenix Group. 2008;1-5.
- Manian FA. Whither continuity of care? N Engl J Med. 1999;340:1362-1363.
- Correspondence. Whither continuity of care? N Engl J Med. 1999;341:850-852.
- Davis KM, Koch KE, Harvey JK, et al. Effects of hospitalists on cost, outcomes, and patient satisfaction in a rural health system. Amer J Med. 2000;108(8):621-626.
- Wachter RM, Goldman L. The hospitalist movement 5 years later. JAMA. 2002;287(4):487-494.
- Coffman J, Rundall TG. The impact of hospitalists on the cost and quality of inpatient care in the United States (a research synthesis). Med Care Res Rev. 2005;62:379–406.
- Dhuper S, Choksi S. Replacing an academic internal medicine residency program with a physician assistant-hospitalist model: a comparative analysis study. Am J Med Qual. 2009;24(2):132-139.
- Roy CL, Liang CL, Lund M, et al. Implementation of a physician assistant/hospitalist service in an academic medical center: impact on efficiency and patient outcomes. J Hosp Med. 2008;3(5):361-368.
- Fulton BR, Drevs KE, Ayala LJ, Malott DL Jr. Patient satisfaction with hospitalists: facility-level analyses. Am J Med Qual. 2011;26(2):95-102.
- Ferranti DE, Makoul G, Forth VE, Rauworth J, Lee J, Williams MV. Assessing patient perceptions of hospitalist communication skills using the Communication Assessment Tool (CAT). J Hosp Med. 2010;5(9):522-527.
At first glance, the deck might seem hopelessly stacked against hospitalists with regard to patient satisfaction. HM practitioners lack the long-term relationship with patients that many primary-care physicians (PCPs) have established. Unlike surgeons and other specialists, they tend to care for those patients—more complicated, lacking a regular doctor, or admitted through the ED, for example—who are more inclined to rate their hospital stay unfavorably.1 They may not even be accurately remembered by patients who encounter multiple doctors during the course of their hospitalization.2 And hospital information systems can misidentify the treating physician, while the actual surveys used to gauge hospitalists have been imperfect at best.3
And yet, the hospitalist model has evolved substantially on the question of how it can impact patient perceptions of care.
Initially, hospitalist champions adopted a largely defensive posture: The model would not negatively impact patient satisfaction as it delivered on efficiency—and later on quality. The healthcare system, however, is beginning to recognize the hospitalist as part of a care “team” whose patient-centered approach might pay big dividends in the inpatient experience and, eventually, on satisfaction scores.
“I think the next phase, which is a focus on the hospitalist as a team member and team builder, is going to be key,” says William Southern, MD, MPH, SFHM, chief of the division of hospital medicine at Montefiore Medical Center in Bronx, N.Y.
Recent studies suggest that hospitalists are helping to design and test new tools that will not only improve satisfaction, but also more fairly assess the impact of individual doctors. As the maturation process continues, experts say, hospitalists have an opportunity to influence both provider-based interventions and more programmatic decision-making that can have far-reaching effects. Certainly, the hand dealt to hospitalists is looking more favorable even as the ante has been raised with Medicare programs like value-based purchasing, and its pot of money tied to patient perceptions of care.
So how have hospitalists played their cards so far?
A Look at the Evidence
In its early years, the HM model faced a persistent criticism: Replacing traditional caregivers with these new inpatient providers in the name of efficiency would increase handoffs and, therefore, discontinuities of care delivered by a succession of unfamiliar faces. If patients didn’t see their PCP in the hospital, the thinking went, they might be more disgruntled at being tended to by hospitalists, leading to lower satisfaction scores.4
A particularly heated exchange played out in 1999 in the New England Journal of Medicine. Farris A. Manian, MD, MPH, of Infectious Disease Consultants in St. Louis wrote in one letter, “I am particularly concerned about what impressionable house-staff members will learn from hospitalists who place an inordinate emphasis on cost rather than the quality of patient care or teaching.”5
A few subsequent studies, however, hinted that such concerns might be overstated. A 2000 analysis in the American Journal of Medicine that examined North Mississippi Health Services in Tupelo, for instance, found that care administered by hospitalists led to a shorter length of stay and lower costs than care delivered by internists. Importantly, the study found that patient satisfaction was similar for both models, while quality metrics were likewise equal or even tilted slightly toward hospitalists.6
In their influential 2002 review of a profession that was only a half-decade old, Robert Wachter, MD, MHM, and Lee Goldman, MD, MPH, FACP from the University of California at San Francisco reinforced the message that HM wouldn’t lead to unhappy patients. “Empirical research supports the premise that hospitalists improve inpatient efficiency without harmful effects on quality or patient satisfaction,” they asserted.7
Among pediatric patients, a 2005 review found that “none of the four studies that evaluated patient satisfaction found statistically significant differences in satisfaction with inpatient care. However, two of the three evaluations that did assess parents’ satisfaction with care provided to their children found that parents were more satisfied with some aspects of care provided by hospitalists.”8

—William Southern, MD, chief, division of hospital medicine, Montefiore Medical Center, Bronx, N.Y.
Similar findings were popping up around the country: Replacing an internal medicine residency program with a physician assistant/hospitalist model at Brooklyn, N.Y.’s Coney Island Hospital did not adversely impact patient satisfaction, while it significantly improved mortality.9 Brigham & Women’s Hospital in Boston likewise reported no change in patient satisfaction in a study comparing a physician assistant/hospitalist service with traditional house staff services.10
The shift toward a more proactive position on patient satisfaction is exemplified within a 2008 white paper, “Hospitalists Meeting the Challenge of Patient Satisfaction,” written by a group of 19 private-practice HM experts known as The Phoenix Group.3 The paper acknowledged the flaws and limitations of existing survey methodologies, including Medicare’s Hospital Consumer Assessment of Healthcare Providers and Systems (HCAHPS) scores. Even so, the authors urged practice groups to adopt a team-oriented approach to communicate to hospital administrations “the belief that hospitalists are in the best position to improve survey scores overall for the facility.”
Carle Foundation Hospital in Urbana, Ill., is now publicly advertising its HM service’s contribution to high patient satisfaction scores on its website, and underscoring the hospitalists’ consistency, accessibility, and communication skills. “The hospital is never without a hospitalist, and our nurses know that they can rely on them,” says Lynn Barnes, vice president of hospital operations. “They’re available, they’re within a few minutes away, and patients’ needs get met very efficiently and rapidly.”
As a result, she says, their presence can lead to higher scores in patients’ perceptions of communication.
Hospitalists also have been central to several safety initiatives at Carle. Napoleon Knight, MD, medical director of hospital medicine and associate vice president for quality, says the HM team has helped address undiagnosed sleep apnea and implement rapid responses, such as “Code Speed.” Caregivers or family members can use the code to immediately call for help if they detect a downturn in a patient’s condition.
The ongoing initiatives, Dr. Knight and Barnes say, are helping the hospital improve how patients and their loved ones perceive care as Carle adapts to a rapidly shifting healthcare landscape. “With all of the changes that seem to be coming from the external environment weekly, we want to work collaboratively to make sure we’re connected and aligned and communicating in an ongoing fashion so we can react to all of these changes,” Dr. Knight says.
Continued below...
A Hopeful Trend
So far, evidence that the HM model is more broadly raising patient satisfaction scores is largely anecdotal. But a few analyses suggest the trend is moving in the right direction. A recent study in the American Journal of Medical Quality, for instance, concludes that facilities with hospitalists might have an advantage in patient satisfaction with nursing and such personal issues as privacy, emotional needs, and response to complaints.11 The study also posits that teaching facilities employing hospitalists could see benefits in overall satisfaction, while large facilities with hospitalists might see gains in satisfaction with admissions, nursing, and tests and treatments.
Brad Fulton, PhD, a researcher at South Bend, Ind.-based healthcare consulting firm Press Ganey and the study’s lead author, says the 30,000-foot view of patient satisfaction at the facility level can get foggy in a hurry due to differences in the kind and size of hospitalist programs. “And despite all of that fog, we’re still able to see through that and find something,” he says.
One limitation is that the study findings could also reflect differences in the culture of facilities that choose to add hospitalists. That caveat means it might not be possible to completely untangle the effect of an HM group on inpatient care from the larger, hospitalwide values that have allowed the group to set up shop. The wrinkle brings its own fascinating questions, according to Fulton. For example, is that kind of culture necessary for hospitalists to function as well as they do?

—Lynn Barnes, vice president of hospital operations, Carle Foundation Hospital, Urbana, Ill.
Such considerations will become more important as the healthcare system places additional emphasis on patient satisfaction, as Medicare’s value-based purchasing program is doing through its HCAHPS scores. With all the changes, success or failure on the patient experience front is going to carry “not just a reputational import, but also a financial impact,” says Ethan Cumbler, MD, FACP, director of Acute Care for the Elderly (ACE) Service at the University of Colorado Denver.
So how can HM fairly and accurately assess its own practitioners? “I think one starts by trying to apply some of the rigor that we have learned from our experience as hospitalists in quality improvement to the more warm and fuzzy field of patient experience,” Dr. Cumbler says. Many hospitals employ surveys supplied by consultants like Press Ganey to track the global patient satisfaction for their institution, he says.
“But for an individual hospitalist or hospitalist group, that kind of tool often lacks both the specificity and the timeliness necessary to make good decisions about impact of interventions on patient satisfaction,” he says.
Mark Williams, MD, FACP, FHM, professor and chief of the division of hospital medicine at Northwestern University’s Feinberg School of Medicine in Chicago, agrees that such imprecision could lead to unfair assessments. “You can imagine a scenario where a patient actually liked their hospitalist very much,” he says, “but when they got the survey, they said [their stay] was terrible and the reasons being because maybe the nurse call button was not answered and the food was terrible and medications were given to them incorrectly, or it was noisy at night so they couldn’t sleep.”
A recent study by Dr. Williams and his colleagues, in which they employed a new assessment method called the Communication Assessment Tool (CAT), confirmed the group’s suspicions: “that the results from the Press Ganey didn’t match up with the CAT, which was a direct assessment of the patient’s perception of the hospitalist’s communication skills,” he says.12
The validated tool, he adds, provides directed feedback to the physician based on the percentage of patients rating that provider as excellent, instead of on the average total score. Hospitalists have felt vindicated by the results. “They were very nervous because the hospital talked about basing an incentive off of the Press Ganey scores, and we said, ‘You can’t do that,’ because we didn’t feel they were accurate, and this study proved that,” Dr. Williams explains.
Fortunately, the message has reached researchers and consultants alike, and better tools are starting to reach hospitals around the country. At HM11 in May, Press Ganey unveiled a new survey designed to help patients assess the care delivered by two hospitalists, the average for inpatient stays. The item set is specific to HM functions, and includes the photo and name of each hospitalist, which Fulton says should improve the validity and accuracy of the data.
“The early response looks really good,” Fulton says, though it’s too early to say whether the tool, called Hospitalist Insight, will live up to its billing. If it proves its mettle, Fulton says, the survey could be used to reward top-performing hospitalists, and the growing dataset could allow hospitals to compare themselves with appropriate peer groups for fairer comparisons.
Meanwhile, researchers are testing out checklists to score hospitalist etiquette, and tracking and paging systems to help ensure continuity of care. They have found increased patient satisfaction when doctors engage in verbal communication during a discharge, in interdisciplinary team rounding, and in efforts to address religious and spiritual concerns.
Since 2000, when Montefiore’s hospitalist program began, Dr. Southern says the hospital has explained to patients the tradeoff accompanying the HM model. “I say something like this to every patient: ‘I know I’m not the doctor that you know, and you’re just meeting me. The downside is that you haven’t met me before and I’m a new face, but the upside is that if you need me during the day, I’m here all the time, I’m not someplace else. And so if you need something, I can be here quickly.’ ”
Being very explicit about that tradeoff, he says, has made patients very comfortable with the model of care, especially during a crisis moment in their lives. “I think it’s really important to say, ‘I know you don’t know me, but here’s the upside.’ And my experience is that patients easily understand that tradeoff and are very positive,” Dr. Southern says.
The Verdict
Available evidence suggests that practitioners of the HM model have pivoted from defending against early criticism that they may harm patient satisfaction to pitching themselves as team leaders who can boost facilitywide perceptions of care. So far, too little research has been conducted to suggest whether that optimism is fully warranted, but early signs look promising.
At facilities like Chicago’s Northwestern Memorial Hospital, medical floors staffed by hospitalists are beginning to beat out surgical floors for the traveling patient satisfaction award. And experts like Dr. Cumbler are pondering how ongoing initiatives to boost scores can follow in the footsteps of efficiency and quality-raising efforts by making the transition from focusing on individual doctors to adopting a more programmatic approach. “What’s happening to that patient during the 23 hours and 45 minutes of their hospital day that you are not sitting by the bedside? And what influence should a hospitalist have in affecting that other 23 hours and 45 minutes?” he says.
Handoffs, discharges, communication with PCPs, and other potential weak points in maintaining high levels of patient satisfaction, Dr. Cumbler says, all are amenable to systems-based improvement. “As hospitalists, we are in a unique position to influence not only our one-one-one interaction with the patient, but also to influence that system of care in a way that patients will notice in a real and tangible way,” he says. “I think we’ve recognized for some time that a healthy heart but a miserable patient is not a healthy person.”
Bryn Nelson is a freelance medical journalist based in Seattle.
References
- Williams M, Flanders SA, Whitcomb WF. Comprehensive hospital medicine: an evidence based approach. Elsevier;2007:971-976.
- Arora V, Gangireddy S, Mehrotra A, Ginde R, Tormey M, Meltzer D. Ability of hospitalized patients to identify their in-hospital physicians. Arch Intern Med. 2009;169(2):199-201.
- Singer AS, et al. Hospitalists meeting the challenge of patient satisfaction. The Phoenix Group. 2008;1-5.
- Manian FA. Whither continuity of care? N Engl J Med. 1999;340:1362-1363.
- Correspondence. Whither continuity of care? N Engl J Med. 1999;341:850-852.
- Davis KM, Koch KE, Harvey JK, et al. Effects of hospitalists on cost, outcomes, and patient satisfaction in a rural health system. Amer J Med. 2000;108(8):621-626.
- Wachter RM, Goldman L. The hospitalist movement 5 years later. JAMA. 2002;287(4):487-494.
- Coffman J, Rundall TG. The impact of hospitalists on the cost and quality of inpatient care in the United States (a research synthesis). Med Care Res Rev. 2005;62:379–406.
- Dhuper S, Choksi S. Replacing an academic internal medicine residency program with a physician assistant-hospitalist model: a comparative analysis study. Am J Med Qual. 2009;24(2):132-139.
- Roy CL, Liang CL, Lund M, et al. Implementation of a physician assistant/hospitalist service in an academic medical center: impact on efficiency and patient outcomes. J Hosp Med. 2008;3(5):361-368.
- Fulton BR, Drevs KE, Ayala LJ, Malott DL Jr. Patient satisfaction with hospitalists: facility-level analyses. Am J Med Qual. 2011;26(2):95-102.
- Ferranti DE, Makoul G, Forth VE, Rauworth J, Lee J, Williams MV. Assessing patient perceptions of hospitalist communication skills using the Communication Assessment Tool (CAT). J Hosp Med. 2010;5(9):522-527.
Our Wake-Up Call
For those who say they would pay $50 more per patient if the quality is better, here’s the problem: Show me the data that say hospitalist care is higher-quality.
I suspect most of you have reviewed the study or at least heard about it. Bob Wachter, MD, MHM, blogged about the study. An article about the study appeared in American Medical Association News. Even National Public Radio ran a piece about the study on their show “Morning Edition.”
I am, of course, referring to the study by Kuo and Goodwin, which was published in the Annals of Internal Medicine in early August.1
In this study, the authors looked at a sample of patients (5%) with primary-care physicians (PCPs) enrolled in Medicare who were cared for by their PCP or a hospitalist during a period from 2001 to 2006. The authors stated their underlying hypotheses as:
- Hospitalist care would be associated with costs shifting from the hospital to the post-hospital setting;
- Hospitalist care would be associated with a decrease in discharges directly to home; and
- Discontinuities of care associated with hospitalist care would lead to a greater rate of visits to the emergency room and readmissions to the hospital, resulting in increased Medicare costs.
Did the authors say hospitalist care cost more? They can’t possibly be correct, can they? Don’t all the hospitalist studies show that hospitalists provide the same quality of care as primary-care doctors, except the costs are lower and the hospital length of stay (LOS) is shorter when hospitalists care for patients?
The point here is that these investigators look at the care not only during a patient’s hospital stay, but also for 30 days after discharge. This is something that had not been done previously—at least not on this scale.
Focus on Facts
And what did the authors find? Patients cared for by hospitalists, as compared to their PCPs, had a shorter LOS and lower in-hospital costs, but these patients also were less likely to be discharged directly to home, less likely to see their PCPs post-discharge, and had more hospital readmissions, ED visits, and nursing home visits after discharge.
Since its release two months ago, I have heard a lot of discussion about the study. Here are a few of the comments I’ve heard:
- “This was an observational study. You can’t possibly remove all confounders in an observational study.”
- “The authors looked at a time period early in the hospitalist movement. If they did the study today, the results would be different.”
- “The additional costs hospitalists incurred were only $50 per patient. Wouldn’t you pay $50 more if the care was better?”
- “This is why hospitals hired hospitalists. They save money for the hospitals. What did they expect to find?”
I agree that observational studies have limitations (even the authors acknowledged this), but this doesn’t mean results from observational studies are invalid. Some of us don’t want to hear this, but this actually was a pretty well-done study with a robust statistical analysis. We should recognize the study has limitations and think about the results.
Kuo and Goodwin looked at data during a period of time early in the hospitalist movement; the results could be different if the study were to be repeated today. But we don’t know what the data would be today. I suppose the data could be better, worse, or about the same. The fact of the matter is that HM leaders—and most of the rest of us—knew that transitions of care, under the hospitalist model, were a potential weakness. How many times have you heard Win Whitcomb, MD, MHM, and John Nelson, MD, MHM, talk about the potential “voltage drop” with handoffs?
The good news is that leaders in our field have done something about this. Project BOOST (Better Outcomes for Older Adults through Safer Transitions) is a program SHM has helped implement at dozens of hospitals across the country to address the issue of unnecessary hospital readmissions (www.hospitalmedicine. org/boost). Improving transitions of care and preventing unnecessary readmissions should be on the minds of all hospitalists. If your program and your hospital have not yet taken steps to address this issue, please let this be your wake-up call.
Show Me the Money
For those who say they would pay $50 more per patient if the quality is better, here’s the problem: Show me the data that say hospitalist care is higher-quality. I agree with you that it is hard to look at costs without looking at quality. Therein lies the basis for our nation’s move toward value-based purchasing of healthcare (see “Value-Based Purchasing Raises the Stakes,” May 2011).
When I hear hospitalists explain why the role of hospitalists was developed, the explanation often involves some discussion of cost and LOS reduction. Don’t get me wrong; it’s not that I believe HM has focused too much attention on cost reduction. I believe we have not focused enough on improving quality. This should not be surprising. Moving the bar on cost reduction is a lot easier than moving the bar on quality and patient safety. The first step toward improvement is an understanding of what you are doing currently. If your hospitalist group has not implemented a program to help its hospitalists measure the quality of care being provided, again, this is your wake-up call.
Last, but not least, for those of you who are not “surprised” by the results because of the belief that hospitalists were created to help the hospital save money and nothing more, I could not disagree with you more. I look at the roles that hospitalists have taken on in our nation’s hospitals, and I am incredibly proud to call myself a hospitalist.
Hospitalists are providing timely care when patients need it. Hospitalists are caring for patients without PCPs. Not only do hospitalists allow PCPs to provide more care in their outpatient clinics, but hospitalists also are caring for patients in ICUs in many places where there are not enough doctors sufficiently trained in critical care.
Rather than acting as an indictment on HM, I believe the Annals article makes a comment on the misalignment of incentives in our healthcare system.
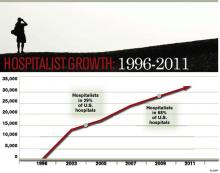
It is 2011, not 1996; HM is here to stay. Most acute-care hospitals in America could not function without hospitalists. I applaud Kuo and Goodwin for doing the research and publishing their results. Let this be an opportunity for hospitalists around the country to think about how to implement systems to improve transitions of care and the quality of care we provide.
Dr. Li is president of SHM.
Reference
For those who say they would pay $50 more per patient if the quality is better, here’s the problem: Show me the data that say hospitalist care is higher-quality.
I suspect most of you have reviewed the study or at least heard about it. Bob Wachter, MD, MHM, blogged about the study. An article about the study appeared in American Medical Association News. Even National Public Radio ran a piece about the study on their show “Morning Edition.”
I am, of course, referring to the study by Kuo and Goodwin, which was published in the Annals of Internal Medicine in early August.1
In this study, the authors looked at a sample of patients (5%) with primary-care physicians (PCPs) enrolled in Medicare who were cared for by their PCP or a hospitalist during a period from 2001 to 2006. The authors stated their underlying hypotheses as:
- Hospitalist care would be associated with costs shifting from the hospital to the post-hospital setting;
- Hospitalist care would be associated with a decrease in discharges directly to home; and
- Discontinuities of care associated with hospitalist care would lead to a greater rate of visits to the emergency room and readmissions to the hospital, resulting in increased Medicare costs.
Did the authors say hospitalist care cost more? They can’t possibly be correct, can they? Don’t all the hospitalist studies show that hospitalists provide the same quality of care as primary-care doctors, except the costs are lower and the hospital length of stay (LOS) is shorter when hospitalists care for patients?
The point here is that these investigators look at the care not only during a patient’s hospital stay, but also for 30 days after discharge. This is something that had not been done previously—at least not on this scale.
Focus on Facts
And what did the authors find? Patients cared for by hospitalists, as compared to their PCPs, had a shorter LOS and lower in-hospital costs, but these patients also were less likely to be discharged directly to home, less likely to see their PCPs post-discharge, and had more hospital readmissions, ED visits, and nursing home visits after discharge.
Since its release two months ago, I have heard a lot of discussion about the study. Here are a few of the comments I’ve heard:
- “This was an observational study. You can’t possibly remove all confounders in an observational study.”
- “The authors looked at a time period early in the hospitalist movement. If they did the study today, the results would be different.”
- “The additional costs hospitalists incurred were only $50 per patient. Wouldn’t you pay $50 more if the care was better?”
- “This is why hospitals hired hospitalists. They save money for the hospitals. What did they expect to find?”
I agree that observational studies have limitations (even the authors acknowledged this), but this doesn’t mean results from observational studies are invalid. Some of us don’t want to hear this, but this actually was a pretty well-done study with a robust statistical analysis. We should recognize the study has limitations and think about the results.
Kuo and Goodwin looked at data during a period of time early in the hospitalist movement; the results could be different if the study were to be repeated today. But we don’t know what the data would be today. I suppose the data could be better, worse, or about the same. The fact of the matter is that HM leaders—and most of the rest of us—knew that transitions of care, under the hospitalist model, were a potential weakness. How many times have you heard Win Whitcomb, MD, MHM, and John Nelson, MD, MHM, talk about the potential “voltage drop” with handoffs?
The good news is that leaders in our field have done something about this. Project BOOST (Better Outcomes for Older Adults through Safer Transitions) is a program SHM has helped implement at dozens of hospitals across the country to address the issue of unnecessary hospital readmissions (www.hospitalmedicine. org/boost). Improving transitions of care and preventing unnecessary readmissions should be on the minds of all hospitalists. If your program and your hospital have not yet taken steps to address this issue, please let this be your wake-up call.
Show Me the Money
For those who say they would pay $50 more per patient if the quality is better, here’s the problem: Show me the data that say hospitalist care is higher-quality. I agree with you that it is hard to look at costs without looking at quality. Therein lies the basis for our nation’s move toward value-based purchasing of healthcare (see “Value-Based Purchasing Raises the Stakes,” May 2011).
When I hear hospitalists explain why the role of hospitalists was developed, the explanation often involves some discussion of cost and LOS reduction. Don’t get me wrong; it’s not that I believe HM has focused too much attention on cost reduction. I believe we have not focused enough on improving quality. This should not be surprising. Moving the bar on cost reduction is a lot easier than moving the bar on quality and patient safety. The first step toward improvement is an understanding of what you are doing currently. If your hospitalist group has not implemented a program to help its hospitalists measure the quality of care being provided, again, this is your wake-up call.
Last, but not least, for those of you who are not “surprised” by the results because of the belief that hospitalists were created to help the hospital save money and nothing more, I could not disagree with you more. I look at the roles that hospitalists have taken on in our nation’s hospitals, and I am incredibly proud to call myself a hospitalist.
Hospitalists are providing timely care when patients need it. Hospitalists are caring for patients without PCPs. Not only do hospitalists allow PCPs to provide more care in their outpatient clinics, but hospitalists also are caring for patients in ICUs in many places where there are not enough doctors sufficiently trained in critical care.
Rather than acting as an indictment on HM, I believe the Annals article makes a comment on the misalignment of incentives in our healthcare system.
It is 2011, not 1996; HM is here to stay. Most acute-care hospitals in America could not function without hospitalists. I applaud Kuo and Goodwin for doing the research and publishing their results. Let this be an opportunity for hospitalists around the country to think about how to implement systems to improve transitions of care and the quality of care we provide.
Dr. Li is president of SHM.
Reference
For those who say they would pay $50 more per patient if the quality is better, here’s the problem: Show me the data that say hospitalist care is higher-quality.
I suspect most of you have reviewed the study or at least heard about it. Bob Wachter, MD, MHM, blogged about the study. An article about the study appeared in American Medical Association News. Even National Public Radio ran a piece about the study on their show “Morning Edition.”
I am, of course, referring to the study by Kuo and Goodwin, which was published in the Annals of Internal Medicine in early August.1
In this study, the authors looked at a sample of patients (5%) with primary-care physicians (PCPs) enrolled in Medicare who were cared for by their PCP or a hospitalist during a period from 2001 to 2006. The authors stated their underlying hypotheses as:
- Hospitalist care would be associated with costs shifting from the hospital to the post-hospital setting;
- Hospitalist care would be associated with a decrease in discharges directly to home; and
- Discontinuities of care associated with hospitalist care would lead to a greater rate of visits to the emergency room and readmissions to the hospital, resulting in increased Medicare costs.
Did the authors say hospitalist care cost more? They can’t possibly be correct, can they? Don’t all the hospitalist studies show that hospitalists provide the same quality of care as primary-care doctors, except the costs are lower and the hospital length of stay (LOS) is shorter when hospitalists care for patients?
The point here is that these investigators look at the care not only during a patient’s hospital stay, but also for 30 days after discharge. This is something that had not been done previously—at least not on this scale.
Focus on Facts
And what did the authors find? Patients cared for by hospitalists, as compared to their PCPs, had a shorter LOS and lower in-hospital costs, but these patients also were less likely to be discharged directly to home, less likely to see their PCPs post-discharge, and had more hospital readmissions, ED visits, and nursing home visits after discharge.
Since its release two months ago, I have heard a lot of discussion about the study. Here are a few of the comments I’ve heard:
- “This was an observational study. You can’t possibly remove all confounders in an observational study.”
- “The authors looked at a time period early in the hospitalist movement. If they did the study today, the results would be different.”
- “The additional costs hospitalists incurred were only $50 per patient. Wouldn’t you pay $50 more if the care was better?”
- “This is why hospitals hired hospitalists. They save money for the hospitals. What did they expect to find?”
I agree that observational studies have limitations (even the authors acknowledged this), but this doesn’t mean results from observational studies are invalid. Some of us don’t want to hear this, but this actually was a pretty well-done study with a robust statistical analysis. We should recognize the study has limitations and think about the results.
Kuo and Goodwin looked at data during a period of time early in the hospitalist movement; the results could be different if the study were to be repeated today. But we don’t know what the data would be today. I suppose the data could be better, worse, or about the same. The fact of the matter is that HM leaders—and most of the rest of us—knew that transitions of care, under the hospitalist model, were a potential weakness. How many times have you heard Win Whitcomb, MD, MHM, and John Nelson, MD, MHM, talk about the potential “voltage drop” with handoffs?
The good news is that leaders in our field have done something about this. Project BOOST (Better Outcomes for Older Adults through Safer Transitions) is a program SHM has helped implement at dozens of hospitals across the country to address the issue of unnecessary hospital readmissions (www.hospitalmedicine. org/boost). Improving transitions of care and preventing unnecessary readmissions should be on the minds of all hospitalists. If your program and your hospital have not yet taken steps to address this issue, please let this be your wake-up call.
Show Me the Money
For those who say they would pay $50 more per patient if the quality is better, here’s the problem: Show me the data that say hospitalist care is higher-quality. I agree with you that it is hard to look at costs without looking at quality. Therein lies the basis for our nation’s move toward value-based purchasing of healthcare (see “Value-Based Purchasing Raises the Stakes,” May 2011).
When I hear hospitalists explain why the role of hospitalists was developed, the explanation often involves some discussion of cost and LOS reduction. Don’t get me wrong; it’s not that I believe HM has focused too much attention on cost reduction. I believe we have not focused enough on improving quality. This should not be surprising. Moving the bar on cost reduction is a lot easier than moving the bar on quality and patient safety. The first step toward improvement is an understanding of what you are doing currently. If your hospitalist group has not implemented a program to help its hospitalists measure the quality of care being provided, again, this is your wake-up call.
Last, but not least, for those of you who are not “surprised” by the results because of the belief that hospitalists were created to help the hospital save money and nothing more, I could not disagree with you more. I look at the roles that hospitalists have taken on in our nation’s hospitals, and I am incredibly proud to call myself a hospitalist.
Hospitalists are providing timely care when patients need it. Hospitalists are caring for patients without PCPs. Not only do hospitalists allow PCPs to provide more care in their outpatient clinics, but hospitalists also are caring for patients in ICUs in many places where there are not enough doctors sufficiently trained in critical care.
Rather than acting as an indictment on HM, I believe the Annals article makes a comment on the misalignment of incentives in our healthcare system.
It is 2011, not 1996; HM is here to stay. Most acute-care hospitals in America could not function without hospitalists. I applaud Kuo and Goodwin for doing the research and publishing their results. Let this be an opportunity for hospitalists around the country to think about how to implement systems to improve transitions of care and the quality of care we provide.
Dr. Li is president of SHM.
Reference
ONLINE EXCLUSIVE: A Discharge Solution—or Problem?
In a bit of counterintuition, an empty discharge lounge might be the most successful kind.
Christine Collins, executive director of patient access services at Brigham and Women’s Hospital in Boston, says that the lounge should be a service for discharged patients who have completed medical treatment, but who for some reason remain unable to leave the institution. Such cases can include waiting on a prescription from the pharmacy, or simply waiting on a relative or friend to arrive with transportation.
—Christine Collins, executive director, patient access services, Brigham and Women’s Hospital, Boston
She does not view Brigham’s discharge lounge, a room with lounge chairs and light meals that is staffed by a registered nurse, as the answer to the throughput conundrum hospitals across the country face each and every day. So when the lounge is empty, it means patients have been discharged without any hang-ups.
“It’s not a patient-care area,” Collins says. “They’re people that should be home.”
Some view discharge lounges as a potential aid in smoothing out the discharge process. In theory, patients ready to be medically discharged but unable to leave the hospital have a place to go. But keeping the patients in the building, and under the eye of a nurse, could create liability issues, says Ken Simone, DO, SFHM, president of Hospitalist and Practice Solutions in Veazie, Maine, and a member of Team Hospitalist. Dr. Simone also wonders how the lounge concept impacts patient satisfaction, as some could view it negatively if they’re told they have to sit in what could be construed as a back-end waiting room.
“People need to assess what they’re doing it for and is it really accomplishing what they want it to accomplish,” Collins says.
Discharge lounges “can’t be another nursing unit because a patient is supposed to be discharged. ... Whether you have a discharge lounge or not, you need to improve your systems so that the patients leave when they leave.”
Richard Quinn is a freelance writer based in New Jersey.
In a bit of counterintuition, an empty discharge lounge might be the most successful kind.
Christine Collins, executive director of patient access services at Brigham and Women’s Hospital in Boston, says that the lounge should be a service for discharged patients who have completed medical treatment, but who for some reason remain unable to leave the institution. Such cases can include waiting on a prescription from the pharmacy, or simply waiting on a relative or friend to arrive with transportation.
—Christine Collins, executive director, patient access services, Brigham and Women’s Hospital, Boston
She does not view Brigham’s discharge lounge, a room with lounge chairs and light meals that is staffed by a registered nurse, as the answer to the throughput conundrum hospitals across the country face each and every day. So when the lounge is empty, it means patients have been discharged without any hang-ups.
“It’s not a patient-care area,” Collins says. “They’re people that should be home.”
Some view discharge lounges as a potential aid in smoothing out the discharge process. In theory, patients ready to be medically discharged but unable to leave the hospital have a place to go. But keeping the patients in the building, and under the eye of a nurse, could create liability issues, says Ken Simone, DO, SFHM, president of Hospitalist and Practice Solutions in Veazie, Maine, and a member of Team Hospitalist. Dr. Simone also wonders how the lounge concept impacts patient satisfaction, as some could view it negatively if they’re told they have to sit in what could be construed as a back-end waiting room.
“People need to assess what they’re doing it for and is it really accomplishing what they want it to accomplish,” Collins says.
Discharge lounges “can’t be another nursing unit because a patient is supposed to be discharged. ... Whether you have a discharge lounge or not, you need to improve your systems so that the patients leave when they leave.”
Richard Quinn is a freelance writer based in New Jersey.
In a bit of counterintuition, an empty discharge lounge might be the most successful kind.
Christine Collins, executive director of patient access services at Brigham and Women’s Hospital in Boston, says that the lounge should be a service for discharged patients who have completed medical treatment, but who for some reason remain unable to leave the institution. Such cases can include waiting on a prescription from the pharmacy, or simply waiting on a relative or friend to arrive with transportation.
—Christine Collins, executive director, patient access services, Brigham and Women’s Hospital, Boston
She does not view Brigham’s discharge lounge, a room with lounge chairs and light meals that is staffed by a registered nurse, as the answer to the throughput conundrum hospitals across the country face each and every day. So when the lounge is empty, it means patients have been discharged without any hang-ups.
“It’s not a patient-care area,” Collins says. “They’re people that should be home.”
Some view discharge lounges as a potential aid in smoothing out the discharge process. In theory, patients ready to be medically discharged but unable to leave the hospital have a place to go. But keeping the patients in the building, and under the eye of a nurse, could create liability issues, says Ken Simone, DO, SFHM, president of Hospitalist and Practice Solutions in Veazie, Maine, and a member of Team Hospitalist. Dr. Simone also wonders how the lounge concept impacts patient satisfaction, as some could view it negatively if they’re told they have to sit in what could be construed as a back-end waiting room.
“People need to assess what they’re doing it for and is it really accomplishing what they want it to accomplish,” Collins says.
Discharge lounges “can’t be another nursing unit because a patient is supposed to be discharged. ... Whether you have a discharge lounge or not, you need to improve your systems so that the patients leave when they leave.”
Richard Quinn is a freelance writer based in New Jersey.
ONLINE EXCLUSIVE: Experts discuss strategies to improve early discharges
HM@15 - Are You Living Up to High Expectations of Efficiency?
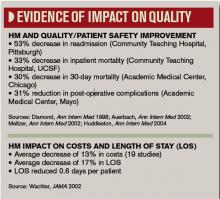
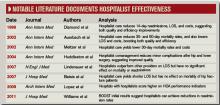
In 2002, a summary article in the Journal of the American Medical Association helped put the relatively small but rapidly growing HM profession on the map. Reviewing the available data, Robert Wachter, MD, MHM, and Lee Goldman, MD, MPH, of the University of California at San Francisco (UCSF) concluded that implementing a hospitalist program yielded an average savings of 13.4% in hospital costs and a 16.6% reduction in the length of stay (LOS).1
A decade later, the idea of efficiency has become so intertwined with hospitalists that SHM has included the concept in its definition of a profession that now comprises more than 30,000 doctors, nurses, and other care providers. HM practitioners work to enhance hospital and healthcare performance, in part, through “efficient use of hospital and healthcare resources,” according to SHM.
The growth of any profession can create exceptions and outliers, and observers point out that HM programs have become as varied as the hospitals in which they reside, complicating any attempt at broad generalizations. As a core part of the job description, though, efficiency and its implied benefit on costs have been widely promoted as arguments for expanding HM’s reach.
So are hospitalists meeting the lofty expectations?
A Look at the Evidence
A large retrospective study that examined outcomes of care for nearly 77,000 patients in 45 hospitals found that those cared for by hospitalists had a “modestly shorter” stay (by 0.4 days) in the hospital than those cared for by either general internists or family physicians.2 Hospitalists saved about $270 per hospitalization compared with general internists but only about $125 per stay compared with family physicians, the latter of which was not deemed statistically significant.
A more recent review of 33 studies found general agreement that hospitalist care led to reduced costs and length of stay but revealed less uniformity in the impacts on quality and patient outcomes.3
A more dramatic—albeit smaller—affirmation of HM as an efficient force has come from a study of patients admitted to 200-bed Olive View-UCLA Medical Center in Sylmar, Calif. The study, led by assistant medical director Scott Lundberg, MD, concluded that the arrival of an academic hospitalist program led to a one-year increase of $2.3 million in reimbursements from Medi-Cal, California’s Medicaid program.4
“Most other places that have demonstrated the cost-effectiveness of hospitalists generally point to reducing length of stay, which therefore reduces the costs,” Dr. Lundberg says. Under Medicare’s diagnosis-based reimbursement (DRG) system, hospitals could get paid the same amount whether the patient stays one day or five.
Medi-Cal, however, uses a straight-up per diem reimbursement system. “So reducing someone’s length of stay is not necessarily desirable if Medi-Cal would have paid you for all of those days,” Dr. Lundberg says. The state’s Medicare program also can deny coverage for days deemed medically unnecessary after a review of patient charts.
Hospitalists, he says, helped boost revenue in two ways. First, the program helped the hospital avoid denied coverage days by ensuring that patients stayed only as long as necessary. Average LOS, in fact, dropped to 1.92 days from 2.48 days, decreasing the Medi-Cal denial rate to 31.8% (from 43.8%) and bumping up the average reimbursement per inpatient day to $955 from $787.
Hospitalists also helped alleviate the work-hour limits for residents imposed by the Accreditation Council for Graduate Medical Education (ACGME), which had effectively capped the number of inpatients the center could admit. Because Olive View-UCLA receives per diem payments from Medi-Cal, making room to accept more patients into the hospital has meant increased revenues. Among the other benefits, the program has improved patient satisfaction and relieved some of the pressure on teaching teams.
With $310,000 for salary outlay in the hospitalist program’s first year, the study found a net cost benefit of $2 million. “One of the real challenges in getting this hospitalist thing going was getting our administrators to shell out the money for the salaries,” Dr. Lundberg says. The study demonstrated that a hospitalist program not only pays for itself, but also can substantially ramp up revenue. “I’m guessing that others, especially at public hospitals, face the same challenges,” he says. “I’m hoping they can point to this analysis and say, ‘Look, here’s what L.A. County did. They were able to show a net increase in revenue from this hospitalist service.’ ”
On the opposite side of the country, hospitalists are pointing to a success story in pediatric care. At the 120-bed Children’s Hospital at Montefiore at Albert Einstein College of Medicine in the Bronx, N.Y., a recent study concluded that establishing a pediatric HM program led to a significant reduction in LOS for patients with asthma or bronchiolitis.5 Nora Esteban-Cruciani, MD, MS, assistant director of pediatric hospital medicine and lead author of the report, which was presented at HM11, says it’s the first study to demonstrate such an effect for asthma in an inner-city academic setting.
Compared to a traditional resident-attending team, care administered by a resident-physician’s assistant-hospitalist team reduced LOS for bronchiolitis by 15.5% and asthma by 11.8%. With the 378 hospital-bed days saved annually, Children’s Hospital at Montefiore achieved an estimated savings of about $944,000 before taking salaries into account. “We anticipate seeing similar benefits in other groups of patients, and the total savings will far exceed the hospitalist salaries,” Dr. Esteban-Cruciani says.
After the pediatric HM program launched, her study also documented a 17% to 25% decrease in rehospitalizations among asthmatic children at four, six, and 12 months after their initial hospital discharge. As a result of the demonstrated value, Dr. Esteban-Cruciani says, the children’s hospital is expanding its HM program and hiring another 4.5 full-time equivalents.
So how did hospitalists achieve the positive results?
“Knowing the most up-to-date and evidence-based treatment plans, understanding how to use the hospital systems in the most efficient manner, being on the ward for eight to 12 hours per day to respond to issues that arise, as well as 24-hour availability by phone for the residents,” she says. “The day-to-day continuity, as well as the ability to consistently improve systems of care, are distinctive advantages to hospital medicine.”
The case for HM as a model of efficiency comes with a major caveat, however. David Meltzer, MD, PhD, FHM, chief of the section of hospital medicine and an economist and public-policy expert at the University of Chicago, points out that healthcare costs don’t end with a patient’s hospital discharge. Could savings achieved during inpatient care be offset by greater costs afterward?
A new study in the Annals of Internal Medicine by researchers at the University of Texas Medical Branch in Galveston has sharpened that question with the suggestion that, at least in some cases, hospitalist-procured savings might not last.6 When compared to care delivered by primary-care physicians (PCPs), the researchers found that hospitalist care yielded an average inpatient savings of $282 per Medicare beneficiary. But that reduction was wiped out by an extra $332 average cost in the month after discharge, due to higher readmissions, more emergency department visits, and more patients sent to nursing facilities instead of to their own homes. An accompanying editorial raises the uncomfortable question: “Are hospitalists discharging their patients more quickly but less appropriately, such that some of their patients bounce back?”7

—David Meltzer, MD, PhD, FHM, chief, section of hospital medicine, economist, University of Chicago
The study itself has its own share of caveats: Data were collected only until 2006, before reducing 30-day readmissions became a widespread focal point. The editorial also highlights the possibility that hospitalists might care for patients whose weaker relationships with outpatient providers could be the true driver of increased readmissions. In a statement, SHM President Joe Li, MD, SFHM, adds that constructive talks about healthcare costs must include the notion of quality, something the organization has worked to improve with interventions like Project BOOST.
At the very least, the new research highlights the importance of context when considering HM impacts on cost and quality. Separate studies, meanwhile, suggest that the jury is still out on whether other hospitalist-led models can consistently improve outcomes and costs. At academic centers, for instance, work-hour limits for medical residents have provided a strong impetus for joint-care arrangements, such as comanagement systems. A 2004 study found that an orthopedics-hospitalist comanagement structure led to a modest reduction in complications after elective hip and knee surgery. But the report documented no difference in costs or actual length of stay.8
More recently, a study of nearly 7,600 patients at UCSF Medical Center found that an HM-neurosurgery comanagement model had no significant impact on the center’s patient mortality, readmissions, LOS, or patient satisfaction. The comanagement system, however, yielded an average savings of $1,439 per hospitalization and boosted physicians’ perceptions of quality and safety.9
Andrew Auerbach, MD, MPH, SFHM, associate professor of medicine at UCSF Medical Center, says the savings, while not dramatic, nevertheless can add up when applied to the thousands of patients seen by the service every year. “That’s compelling because I think one of the things that you’re arguing when you’re doing these services is what the return on investment is going to be,” he says. “Traditionally, these have been implemented without any specific financial return on investment being applied, but the large expectation that clinical improvement is going to happen.”
His study at UCSF found just the opposite: no clinical improvement but a net cost benefit. “We were a little disappointed in some ways, but in other ways not surprised because there are very few data out in the community that suggest comanagement improves any outcomes,” Dr. Auerbach says. Among complicated neurosurgery patients, the strongest determinants of outcome might be beyond the scope of hospitalist-aided medical care.
With hospitals nervously eyeing their bottom lines, however, any financial improvement that does not adversely affect quality can still be seen as a positive development, and Dr. Auerbach says his study was the first to demonstrate that benefit. At UCSF Medical Center, at least, comanagement has proven compelling enough to spur plans for extending the service to orthopedic surgery patients.
Regardless of the care model, other studies suggest that specific interventions at key moments can yield substantial savings. A small, randomized controlled study led by hospitalists at Johns Hopkins University in Baltimore, for example, supports the idea that “simply showing providers the cost of some diagnostic tests at the time of order entry can affect behavior.”10 Although the study didn’t focus exclusively on hospitalists, experts say they’re in the best position to take the lead in curbing unnecessary costs.
“Hospitalists, I think, have a better understanding of the impact of resource utilization on the total cost of care and can be more prudent in the use of technologies,” says Kenneth Epstein, MD, MBA, FHM, FACP, chief medical officer for Traverse City, Mich.-based Hospitalist Consultants Inc. One reason is that hospitalists aren’t beholden to any specific technology, whether endoscopies or cardiac catheterization.

—Scott Lundberg, MD, assistant medical director, Olive View-UCLA Medical Center, Sylmar, Calif.
Mark Graban, author of the book “Lean Hospitals: Improving Quality, Patient Safety, and Employee Satisfaction,” says hospitalists can play another critical role in controlling costs by mapping out and simplifying the discharge processes. He recalls how hospitalists helped coordinate the effort by one of his hospital clients to prevent discharge delays that would have unnecessarily kept patients in the hospital for an additional night or two.
“That length-of-stay reduction, especially in a fixed-reimbursement setting, can have a huge financial impact,” Graban says. “And, inarguably, it’s the right thing to do for the patient, because it’s patients that are medically ready to be discharged. It gets them home and it reduces their increased risk of picking up infections or being involved in hospital errors.”
Focusing on patient safety could translate into big cost savings under the new Medicare system that penalizes providers for certain hospital-acquired conditions, such as skin ulcers and urinary tract infections, Dr. Epstein says. “There’s an emphasis by hospitalists in understanding the system and being willing to put energy into things like documenting ‘present on admission,’ which then has a huge impact on the hospital,” he says. Close monitoring of patients and developing standardization of care can likewise minimize the risk of conditions, such as catheter-associated infections, from cropping up in the hospital.
Dr. Meltzer says his own research suggests that experienced hospitalists are most effective at controlling costs. “So a program that is structured in such a way as to hire or retain experienced hospitalists is likely to have a higher cost savings than one that doesn’t,” he says.
In a broader sense, the maturation of the HM model and more widespread adoption of effective methods by practitioners might be boosting the overall impact of hospitalist care. A study that examined nearly 2 million Medicare admissions over six years found that the effects of the hospitalist care model on LOS became progressively more pronounced over time, from an average reduction of only 0.02 inpatient days in 2001-2002 to a decrease of 0.35 days by 2005-2006.11
Interestingly, the study’s authors suggest that effects attributable to hospitalists were most pronounced among older, complicated, nonsurgical patients cared for at nonprofit community hospitals.
The Verdict
Despite the variable design and scope of individual programs, experts say, HM’s overall net positive on the efficiency of inpatient care is fairly well documented. Future considerations of hospitalists’ true effects on costs, however, will demand an accounting of healthcare across an entire system, where the HM impact is decidedly less certain. “The right comparison in some sense is, What are the total costs of care for a patient cared for in a system that uses hospitalists versus the totals costs of similar patients cared for in a system that doesn’t use hospitalists?” Dr. Meltzer says.
David Mitchell, MD, PhD, a hospitalist at Sibley Memorial Hospital in Washington, D.C., and a member of SHM’s Performance Standards Committee, is among those with an additional concern: Providers may not be taking full advantage of their position to control costs.
“The reason is primarily that the reimbursement structure is not set up to incentivize us to cut costs,” he says. Dr. Mitchell, who has worked in 12 hospitals in six states, argues that hospitalists still are too detached from the true price of ordered tests. “That’s what I fear in hospital medicine, that we just become robots: chest pain means CT scan without thinking,” he says. “This just doesn’t make sense.” Dr. Mitchell also contends that the focus of some HM programs on seeing as many patients as possible to maximize reimbursements is leading to less efficiency. At HM11 in May, he met another hospitalist who said he regularly saw 40 to 45 patients every day. “I know there’s absolutely no way you can see that many patients and do an efficient job,” Dr. Mitchell says.
If one of the clearest areas of success for hospitalists has been in reducing length of stay within a hospital, experts acknowledge that it may no longer be enough. “In the new payment model, success is going to be defined differently, and it will be in terms of reducing the total cost of care,” Dr. Meltzer says.
Over the next decade, hospitalists will need to respond to new set of incentives. “And I think one of the really interesting questions will be how hospitalists can best do that, and the extent to which it causes them to rethink the ways in which they organize their practice,” he says.
Bryn Nelson is a freelance medical writer based in Seattle.
References
- Wachter RM, Goldman L. The hospitalist movement 5 years later. JAMA. 2002;287(4):487-494.
- Lindenauer PK, Rothberg MB, Pekow PS, Kenwood C, Benjamin EM, Auerbach AD. Outcomes of care by hospitalists, general internists, and family physicians. N Engl J Med. 2007;357:2589-2600.
- Peterson MC. A systematic review of outcomes and quality measures in adult patients cared for by hospitalists vs nonhospitalists. Mayo Clin Proc. 2009;84(3): 248-254.
- Lundberg S, Balingit P, Wali S, Cope D. Cost-effectiveness of a hospitalist service in a public teaching hospital. Acad Med. 2010;85(8):1312-1315.
- Esteban-Cruciani N, Montejo J, Azzarone G, Douglas L, et al. Impact of a pediatric hospital medicine program on resource utilization for children with respiratory disorders. J Hosp Med. 2011;6(4)Supp 2:S27.
- Kuo Y-F, Goodwin JS. Association of hospitalist care with medical utilization after discharge: evidence of cost shift from a cohort study. Ann Intern Med. 2011;155(3): 152-159.
- Chen LM, Saint S. Moments in time. Ann Intern Med. 2011;155(3):194-195.
- Huddleston JM, Long KH, Naessens JM, et al. Medical and surgical comanagement after elective hip and knee arthroplasty: a randomized, controlled trial. Ann Intern Med. 2004;141(1):28-38.
- Auerbach AD, Wachter RM, Cheng HQ, et al. Comanagement of surgical patients between neurosurgeons and hospitalists. Arch Intern Med. 2010;170(22): 2004-2010.
- Feldman L, Thiemann D, Brotman D. Financial impact of presenting lab cost data to providers at the time of order entry: a randomized controlled clinical trial. J Hosp Med. 2011;6(4)Supp 2:S93.
- Kuo Y-F, Goodwin JS. Effect of hospitalists on length of stay in the Medicare population: variation according to hospital and patient characteristics. J Am Geriatr Soc. 2010;58:1649-1657.
- Epstein K, Juarez E, Epstein A, Loya K, Singer A. The impact of fragmentation of hospitalist care on length of stay. J Hosp Med. 2010;5(6):335-8.
- Chandra S, Howell E, Wright S. CICLE: Creating incentives and continuity leading to efficiency. J Hosp Med. 2011;6(4)Supp 2:S17
In 2002, a summary article in the Journal of the American Medical Association helped put the relatively small but rapidly growing HM profession on the map. Reviewing the available data, Robert Wachter, MD, MHM, and Lee Goldman, MD, MPH, of the University of California at San Francisco (UCSF) concluded that implementing a hospitalist program yielded an average savings of 13.4% in hospital costs and a 16.6% reduction in the length of stay (LOS).1
A decade later, the idea of efficiency has become so intertwined with hospitalists that SHM has included the concept in its definition of a profession that now comprises more than 30,000 doctors, nurses, and other care providers. HM practitioners work to enhance hospital and healthcare performance, in part, through “efficient use of hospital and healthcare resources,” according to SHM.
The growth of any profession can create exceptions and outliers, and observers point out that HM programs have become as varied as the hospitals in which they reside, complicating any attempt at broad generalizations. As a core part of the job description, though, efficiency and its implied benefit on costs have been widely promoted as arguments for expanding HM’s reach.
So are hospitalists meeting the lofty expectations?
A Look at the Evidence
A large retrospective study that examined outcomes of care for nearly 77,000 patients in 45 hospitals found that those cared for by hospitalists had a “modestly shorter” stay (by 0.4 days) in the hospital than those cared for by either general internists or family physicians.2 Hospitalists saved about $270 per hospitalization compared with general internists but only about $125 per stay compared with family physicians, the latter of which was not deemed statistically significant.
A more recent review of 33 studies found general agreement that hospitalist care led to reduced costs and length of stay but revealed less uniformity in the impacts on quality and patient outcomes.3
A more dramatic—albeit smaller—affirmation of HM as an efficient force has come from a study of patients admitted to 200-bed Olive View-UCLA Medical Center in Sylmar, Calif. The study, led by assistant medical director Scott Lundberg, MD, concluded that the arrival of an academic hospitalist program led to a one-year increase of $2.3 million in reimbursements from Medi-Cal, California’s Medicaid program.4
“Most other places that have demonstrated the cost-effectiveness of hospitalists generally point to reducing length of stay, which therefore reduces the costs,” Dr. Lundberg says. Under Medicare’s diagnosis-based reimbursement (DRG) system, hospitals could get paid the same amount whether the patient stays one day or five.
Medi-Cal, however, uses a straight-up per diem reimbursement system. “So reducing someone’s length of stay is not necessarily desirable if Medi-Cal would have paid you for all of those days,” Dr. Lundberg says. The state’s Medicare program also can deny coverage for days deemed medically unnecessary after a review of patient charts.
Hospitalists, he says, helped boost revenue in two ways. First, the program helped the hospital avoid denied coverage days by ensuring that patients stayed only as long as necessary. Average LOS, in fact, dropped to 1.92 days from 2.48 days, decreasing the Medi-Cal denial rate to 31.8% (from 43.8%) and bumping up the average reimbursement per inpatient day to $955 from $787.
Hospitalists also helped alleviate the work-hour limits for residents imposed by the Accreditation Council for Graduate Medical Education (ACGME), which had effectively capped the number of inpatients the center could admit. Because Olive View-UCLA receives per diem payments from Medi-Cal, making room to accept more patients into the hospital has meant increased revenues. Among the other benefits, the program has improved patient satisfaction and relieved some of the pressure on teaching teams.
With $310,000 for salary outlay in the hospitalist program’s first year, the study found a net cost benefit of $2 million. “One of the real challenges in getting this hospitalist thing going was getting our administrators to shell out the money for the salaries,” Dr. Lundberg says. The study demonstrated that a hospitalist program not only pays for itself, but also can substantially ramp up revenue. “I’m guessing that others, especially at public hospitals, face the same challenges,” he says. “I’m hoping they can point to this analysis and say, ‘Look, here’s what L.A. County did. They were able to show a net increase in revenue from this hospitalist service.’ ”
On the opposite side of the country, hospitalists are pointing to a success story in pediatric care. At the 120-bed Children’s Hospital at Montefiore at Albert Einstein College of Medicine in the Bronx, N.Y., a recent study concluded that establishing a pediatric HM program led to a significant reduction in LOS for patients with asthma or bronchiolitis.5 Nora Esteban-Cruciani, MD, MS, assistant director of pediatric hospital medicine and lead author of the report, which was presented at HM11, says it’s the first study to demonstrate such an effect for asthma in an inner-city academic setting.
Compared to a traditional resident-attending team, care administered by a resident-physician’s assistant-hospitalist team reduced LOS for bronchiolitis by 15.5% and asthma by 11.8%. With the 378 hospital-bed days saved annually, Children’s Hospital at Montefiore achieved an estimated savings of about $944,000 before taking salaries into account. “We anticipate seeing similar benefits in other groups of patients, and the total savings will far exceed the hospitalist salaries,” Dr. Esteban-Cruciani says.
After the pediatric HM program launched, her study also documented a 17% to 25% decrease in rehospitalizations among asthmatic children at four, six, and 12 months after their initial hospital discharge. As a result of the demonstrated value, Dr. Esteban-Cruciani says, the children’s hospital is expanding its HM program and hiring another 4.5 full-time equivalents.
So how did hospitalists achieve the positive results?
“Knowing the most up-to-date and evidence-based treatment plans, understanding how to use the hospital systems in the most efficient manner, being on the ward for eight to 12 hours per day to respond to issues that arise, as well as 24-hour availability by phone for the residents,” she says. “The day-to-day continuity, as well as the ability to consistently improve systems of care, are distinctive advantages to hospital medicine.”
The case for HM as a model of efficiency comes with a major caveat, however. David Meltzer, MD, PhD, FHM, chief of the section of hospital medicine and an economist and public-policy expert at the University of Chicago, points out that healthcare costs don’t end with a patient’s hospital discharge. Could savings achieved during inpatient care be offset by greater costs afterward?
A new study in the Annals of Internal Medicine by researchers at the University of Texas Medical Branch in Galveston has sharpened that question with the suggestion that, at least in some cases, hospitalist-procured savings might not last.6 When compared to care delivered by primary-care physicians (PCPs), the researchers found that hospitalist care yielded an average inpatient savings of $282 per Medicare beneficiary. But that reduction was wiped out by an extra $332 average cost in the month after discharge, due to higher readmissions, more emergency department visits, and more patients sent to nursing facilities instead of to their own homes. An accompanying editorial raises the uncomfortable question: “Are hospitalists discharging their patients more quickly but less appropriately, such that some of their patients bounce back?”7

—David Meltzer, MD, PhD, FHM, chief, section of hospital medicine, economist, University of Chicago
The study itself has its own share of caveats: Data were collected only until 2006, before reducing 30-day readmissions became a widespread focal point. The editorial also highlights the possibility that hospitalists might care for patients whose weaker relationships with outpatient providers could be the true driver of increased readmissions. In a statement, SHM President Joe Li, MD, SFHM, adds that constructive talks about healthcare costs must include the notion of quality, something the organization has worked to improve with interventions like Project BOOST.
At the very least, the new research highlights the importance of context when considering HM impacts on cost and quality. Separate studies, meanwhile, suggest that the jury is still out on whether other hospitalist-led models can consistently improve outcomes and costs. At academic centers, for instance, work-hour limits for medical residents have provided a strong impetus for joint-care arrangements, such as comanagement systems. A 2004 study found that an orthopedics-hospitalist comanagement structure led to a modest reduction in complications after elective hip and knee surgery. But the report documented no difference in costs or actual length of stay.8
More recently, a study of nearly 7,600 patients at UCSF Medical Center found that an HM-neurosurgery comanagement model had no significant impact on the center’s patient mortality, readmissions, LOS, or patient satisfaction. The comanagement system, however, yielded an average savings of $1,439 per hospitalization and boosted physicians’ perceptions of quality and safety.9
Andrew Auerbach, MD, MPH, SFHM, associate professor of medicine at UCSF Medical Center, says the savings, while not dramatic, nevertheless can add up when applied to the thousands of patients seen by the service every year. “That’s compelling because I think one of the things that you’re arguing when you’re doing these services is what the return on investment is going to be,” he says. “Traditionally, these have been implemented without any specific financial return on investment being applied, but the large expectation that clinical improvement is going to happen.”
His study at UCSF found just the opposite: no clinical improvement but a net cost benefit. “We were a little disappointed in some ways, but in other ways not surprised because there are very few data out in the community that suggest comanagement improves any outcomes,” Dr. Auerbach says. Among complicated neurosurgery patients, the strongest determinants of outcome might be beyond the scope of hospitalist-aided medical care.
With hospitals nervously eyeing their bottom lines, however, any financial improvement that does not adversely affect quality can still be seen as a positive development, and Dr. Auerbach says his study was the first to demonstrate that benefit. At UCSF Medical Center, at least, comanagement has proven compelling enough to spur plans for extending the service to orthopedic surgery patients.
Regardless of the care model, other studies suggest that specific interventions at key moments can yield substantial savings. A small, randomized controlled study led by hospitalists at Johns Hopkins University in Baltimore, for example, supports the idea that “simply showing providers the cost of some diagnostic tests at the time of order entry can affect behavior.”10 Although the study didn’t focus exclusively on hospitalists, experts say they’re in the best position to take the lead in curbing unnecessary costs.
“Hospitalists, I think, have a better understanding of the impact of resource utilization on the total cost of care and can be more prudent in the use of technologies,” says Kenneth Epstein, MD, MBA, FHM, FACP, chief medical officer for Traverse City, Mich.-based Hospitalist Consultants Inc. One reason is that hospitalists aren’t beholden to any specific technology, whether endoscopies or cardiac catheterization.

—Scott Lundberg, MD, assistant medical director, Olive View-UCLA Medical Center, Sylmar, Calif.
Mark Graban, author of the book “Lean Hospitals: Improving Quality, Patient Safety, and Employee Satisfaction,” says hospitalists can play another critical role in controlling costs by mapping out and simplifying the discharge processes. He recalls how hospitalists helped coordinate the effort by one of his hospital clients to prevent discharge delays that would have unnecessarily kept patients in the hospital for an additional night or two.
“That length-of-stay reduction, especially in a fixed-reimbursement setting, can have a huge financial impact,” Graban says. “And, inarguably, it’s the right thing to do for the patient, because it’s patients that are medically ready to be discharged. It gets them home and it reduces their increased risk of picking up infections or being involved in hospital errors.”
Focusing on patient safety could translate into big cost savings under the new Medicare system that penalizes providers for certain hospital-acquired conditions, such as skin ulcers and urinary tract infections, Dr. Epstein says. “There’s an emphasis by hospitalists in understanding the system and being willing to put energy into things like documenting ‘present on admission,’ which then has a huge impact on the hospital,” he says. Close monitoring of patients and developing standardization of care can likewise minimize the risk of conditions, such as catheter-associated infections, from cropping up in the hospital.
Dr. Meltzer says his own research suggests that experienced hospitalists are most effective at controlling costs. “So a program that is structured in such a way as to hire or retain experienced hospitalists is likely to have a higher cost savings than one that doesn’t,” he says.
In a broader sense, the maturation of the HM model and more widespread adoption of effective methods by practitioners might be boosting the overall impact of hospitalist care. A study that examined nearly 2 million Medicare admissions over six years found that the effects of the hospitalist care model on LOS became progressively more pronounced over time, from an average reduction of only 0.02 inpatient days in 2001-2002 to a decrease of 0.35 days by 2005-2006.11
Interestingly, the study’s authors suggest that effects attributable to hospitalists were most pronounced among older, complicated, nonsurgical patients cared for at nonprofit community hospitals.
The Verdict
Despite the variable design and scope of individual programs, experts say, HM’s overall net positive on the efficiency of inpatient care is fairly well documented. Future considerations of hospitalists’ true effects on costs, however, will demand an accounting of healthcare across an entire system, where the HM impact is decidedly less certain. “The right comparison in some sense is, What are the total costs of care for a patient cared for in a system that uses hospitalists versus the totals costs of similar patients cared for in a system that doesn’t use hospitalists?” Dr. Meltzer says.
David Mitchell, MD, PhD, a hospitalist at Sibley Memorial Hospital in Washington, D.C., and a member of SHM’s Performance Standards Committee, is among those with an additional concern: Providers may not be taking full advantage of their position to control costs.
“The reason is primarily that the reimbursement structure is not set up to incentivize us to cut costs,” he says. Dr. Mitchell, who has worked in 12 hospitals in six states, argues that hospitalists still are too detached from the true price of ordered tests. “That’s what I fear in hospital medicine, that we just become robots: chest pain means CT scan without thinking,” he says. “This just doesn’t make sense.” Dr. Mitchell also contends that the focus of some HM programs on seeing as many patients as possible to maximize reimbursements is leading to less efficiency. At HM11 in May, he met another hospitalist who said he regularly saw 40 to 45 patients every day. “I know there’s absolutely no way you can see that many patients and do an efficient job,” Dr. Mitchell says.
If one of the clearest areas of success for hospitalists has been in reducing length of stay within a hospital, experts acknowledge that it may no longer be enough. “In the new payment model, success is going to be defined differently, and it will be in terms of reducing the total cost of care,” Dr. Meltzer says.
Over the next decade, hospitalists will need to respond to new set of incentives. “And I think one of the really interesting questions will be how hospitalists can best do that, and the extent to which it causes them to rethink the ways in which they organize their practice,” he says.
Bryn Nelson is a freelance medical writer based in Seattle.
References
- Wachter RM, Goldman L. The hospitalist movement 5 years later. JAMA. 2002;287(4):487-494.
- Lindenauer PK, Rothberg MB, Pekow PS, Kenwood C, Benjamin EM, Auerbach AD. Outcomes of care by hospitalists, general internists, and family physicians. N Engl J Med. 2007;357:2589-2600.
- Peterson MC. A systematic review of outcomes and quality measures in adult patients cared for by hospitalists vs nonhospitalists. Mayo Clin Proc. 2009;84(3): 248-254.
- Lundberg S, Balingit P, Wali S, Cope D. Cost-effectiveness of a hospitalist service in a public teaching hospital. Acad Med. 2010;85(8):1312-1315.
- Esteban-Cruciani N, Montejo J, Azzarone G, Douglas L, et al. Impact of a pediatric hospital medicine program on resource utilization for children with respiratory disorders. J Hosp Med. 2011;6(4)Supp 2:S27.
- Kuo Y-F, Goodwin JS. Association of hospitalist care with medical utilization after discharge: evidence of cost shift from a cohort study. Ann Intern Med. 2011;155(3): 152-159.
- Chen LM, Saint S. Moments in time. Ann Intern Med. 2011;155(3):194-195.
- Huddleston JM, Long KH, Naessens JM, et al. Medical and surgical comanagement after elective hip and knee arthroplasty: a randomized, controlled trial. Ann Intern Med. 2004;141(1):28-38.
- Auerbach AD, Wachter RM, Cheng HQ, et al. Comanagement of surgical patients between neurosurgeons and hospitalists. Arch Intern Med. 2010;170(22): 2004-2010.
- Feldman L, Thiemann D, Brotman D. Financial impact of presenting lab cost data to providers at the time of order entry: a randomized controlled clinical trial. J Hosp Med. 2011;6(4)Supp 2:S93.
- Kuo Y-F, Goodwin JS. Effect of hospitalists on length of stay in the Medicare population: variation according to hospital and patient characteristics. J Am Geriatr Soc. 2010;58:1649-1657.
- Epstein K, Juarez E, Epstein A, Loya K, Singer A. The impact of fragmentation of hospitalist care on length of stay. J Hosp Med. 2010;5(6):335-8.
- Chandra S, Howell E, Wright S. CICLE: Creating incentives and continuity leading to efficiency. J Hosp Med. 2011;6(4)Supp 2:S17
In 2002, a summary article in the Journal of the American Medical Association helped put the relatively small but rapidly growing HM profession on the map. Reviewing the available data, Robert Wachter, MD, MHM, and Lee Goldman, MD, MPH, of the University of California at San Francisco (UCSF) concluded that implementing a hospitalist program yielded an average savings of 13.4% in hospital costs and a 16.6% reduction in the length of stay (LOS).1
A decade later, the idea of efficiency has become so intertwined with hospitalists that SHM has included the concept in its definition of a profession that now comprises more than 30,000 doctors, nurses, and other care providers. HM practitioners work to enhance hospital and healthcare performance, in part, through “efficient use of hospital and healthcare resources,” according to SHM.
The growth of any profession can create exceptions and outliers, and observers point out that HM programs have become as varied as the hospitals in which they reside, complicating any attempt at broad generalizations. As a core part of the job description, though, efficiency and its implied benefit on costs have been widely promoted as arguments for expanding HM’s reach.
So are hospitalists meeting the lofty expectations?
A Look at the Evidence
A large retrospective study that examined outcomes of care for nearly 77,000 patients in 45 hospitals found that those cared for by hospitalists had a “modestly shorter” stay (by 0.4 days) in the hospital than those cared for by either general internists or family physicians.2 Hospitalists saved about $270 per hospitalization compared with general internists but only about $125 per stay compared with family physicians, the latter of which was not deemed statistically significant.
A more recent review of 33 studies found general agreement that hospitalist care led to reduced costs and length of stay but revealed less uniformity in the impacts on quality and patient outcomes.3
A more dramatic—albeit smaller—affirmation of HM as an efficient force has come from a study of patients admitted to 200-bed Olive View-UCLA Medical Center in Sylmar, Calif. The study, led by assistant medical director Scott Lundberg, MD, concluded that the arrival of an academic hospitalist program led to a one-year increase of $2.3 million in reimbursements from Medi-Cal, California’s Medicaid program.4
“Most other places that have demonstrated the cost-effectiveness of hospitalists generally point to reducing length of stay, which therefore reduces the costs,” Dr. Lundberg says. Under Medicare’s diagnosis-based reimbursement (DRG) system, hospitals could get paid the same amount whether the patient stays one day or five.
Medi-Cal, however, uses a straight-up per diem reimbursement system. “So reducing someone’s length of stay is not necessarily desirable if Medi-Cal would have paid you for all of those days,” Dr. Lundberg says. The state’s Medicare program also can deny coverage for days deemed medically unnecessary after a review of patient charts.
Hospitalists, he says, helped boost revenue in two ways. First, the program helped the hospital avoid denied coverage days by ensuring that patients stayed only as long as necessary. Average LOS, in fact, dropped to 1.92 days from 2.48 days, decreasing the Medi-Cal denial rate to 31.8% (from 43.8%) and bumping up the average reimbursement per inpatient day to $955 from $787.
Hospitalists also helped alleviate the work-hour limits for residents imposed by the Accreditation Council for Graduate Medical Education (ACGME), which had effectively capped the number of inpatients the center could admit. Because Olive View-UCLA receives per diem payments from Medi-Cal, making room to accept more patients into the hospital has meant increased revenues. Among the other benefits, the program has improved patient satisfaction and relieved some of the pressure on teaching teams.
With $310,000 for salary outlay in the hospitalist program’s first year, the study found a net cost benefit of $2 million. “One of the real challenges in getting this hospitalist thing going was getting our administrators to shell out the money for the salaries,” Dr. Lundberg says. The study demonstrated that a hospitalist program not only pays for itself, but also can substantially ramp up revenue. “I’m guessing that others, especially at public hospitals, face the same challenges,” he says. “I’m hoping they can point to this analysis and say, ‘Look, here’s what L.A. County did. They were able to show a net increase in revenue from this hospitalist service.’ ”
On the opposite side of the country, hospitalists are pointing to a success story in pediatric care. At the 120-bed Children’s Hospital at Montefiore at Albert Einstein College of Medicine in the Bronx, N.Y., a recent study concluded that establishing a pediatric HM program led to a significant reduction in LOS for patients with asthma or bronchiolitis.5 Nora Esteban-Cruciani, MD, MS, assistant director of pediatric hospital medicine and lead author of the report, which was presented at HM11, says it’s the first study to demonstrate such an effect for asthma in an inner-city academic setting.
Compared to a traditional resident-attending team, care administered by a resident-physician’s assistant-hospitalist team reduced LOS for bronchiolitis by 15.5% and asthma by 11.8%. With the 378 hospital-bed days saved annually, Children’s Hospital at Montefiore achieved an estimated savings of about $944,000 before taking salaries into account. “We anticipate seeing similar benefits in other groups of patients, and the total savings will far exceed the hospitalist salaries,” Dr. Esteban-Cruciani says.
After the pediatric HM program launched, her study also documented a 17% to 25% decrease in rehospitalizations among asthmatic children at four, six, and 12 months after their initial hospital discharge. As a result of the demonstrated value, Dr. Esteban-Cruciani says, the children’s hospital is expanding its HM program and hiring another 4.5 full-time equivalents.
So how did hospitalists achieve the positive results?
“Knowing the most up-to-date and evidence-based treatment plans, understanding how to use the hospital systems in the most efficient manner, being on the ward for eight to 12 hours per day to respond to issues that arise, as well as 24-hour availability by phone for the residents,” she says. “The day-to-day continuity, as well as the ability to consistently improve systems of care, are distinctive advantages to hospital medicine.”
The case for HM as a model of efficiency comes with a major caveat, however. David Meltzer, MD, PhD, FHM, chief of the section of hospital medicine and an economist and public-policy expert at the University of Chicago, points out that healthcare costs don’t end with a patient’s hospital discharge. Could savings achieved during inpatient care be offset by greater costs afterward?
A new study in the Annals of Internal Medicine by researchers at the University of Texas Medical Branch in Galveston has sharpened that question with the suggestion that, at least in some cases, hospitalist-procured savings might not last.6 When compared to care delivered by primary-care physicians (PCPs), the researchers found that hospitalist care yielded an average inpatient savings of $282 per Medicare beneficiary. But that reduction was wiped out by an extra $332 average cost in the month after discharge, due to higher readmissions, more emergency department visits, and more patients sent to nursing facilities instead of to their own homes. An accompanying editorial raises the uncomfortable question: “Are hospitalists discharging their patients more quickly but less appropriately, such that some of their patients bounce back?”7

—David Meltzer, MD, PhD, FHM, chief, section of hospital medicine, economist, University of Chicago
The study itself has its own share of caveats: Data were collected only until 2006, before reducing 30-day readmissions became a widespread focal point. The editorial also highlights the possibility that hospitalists might care for patients whose weaker relationships with outpatient providers could be the true driver of increased readmissions. In a statement, SHM President Joe Li, MD, SFHM, adds that constructive talks about healthcare costs must include the notion of quality, something the organization has worked to improve with interventions like Project BOOST.
At the very least, the new research highlights the importance of context when considering HM impacts on cost and quality. Separate studies, meanwhile, suggest that the jury is still out on whether other hospitalist-led models can consistently improve outcomes and costs. At academic centers, for instance, work-hour limits for medical residents have provided a strong impetus for joint-care arrangements, such as comanagement systems. A 2004 study found that an orthopedics-hospitalist comanagement structure led to a modest reduction in complications after elective hip and knee surgery. But the report documented no difference in costs or actual length of stay.8
More recently, a study of nearly 7,600 patients at UCSF Medical Center found that an HM-neurosurgery comanagement model had no significant impact on the center’s patient mortality, readmissions, LOS, or patient satisfaction. The comanagement system, however, yielded an average savings of $1,439 per hospitalization and boosted physicians’ perceptions of quality and safety.9
Andrew Auerbach, MD, MPH, SFHM, associate professor of medicine at UCSF Medical Center, says the savings, while not dramatic, nevertheless can add up when applied to the thousands of patients seen by the service every year. “That’s compelling because I think one of the things that you’re arguing when you’re doing these services is what the return on investment is going to be,” he says. “Traditionally, these have been implemented without any specific financial return on investment being applied, but the large expectation that clinical improvement is going to happen.”
His study at UCSF found just the opposite: no clinical improvement but a net cost benefit. “We were a little disappointed in some ways, but in other ways not surprised because there are very few data out in the community that suggest comanagement improves any outcomes,” Dr. Auerbach says. Among complicated neurosurgery patients, the strongest determinants of outcome might be beyond the scope of hospitalist-aided medical care.
With hospitals nervously eyeing their bottom lines, however, any financial improvement that does not adversely affect quality can still be seen as a positive development, and Dr. Auerbach says his study was the first to demonstrate that benefit. At UCSF Medical Center, at least, comanagement has proven compelling enough to spur plans for extending the service to orthopedic surgery patients.
Regardless of the care model, other studies suggest that specific interventions at key moments can yield substantial savings. A small, randomized controlled study led by hospitalists at Johns Hopkins University in Baltimore, for example, supports the idea that “simply showing providers the cost of some diagnostic tests at the time of order entry can affect behavior.”10 Although the study didn’t focus exclusively on hospitalists, experts say they’re in the best position to take the lead in curbing unnecessary costs.
“Hospitalists, I think, have a better understanding of the impact of resource utilization on the total cost of care and can be more prudent in the use of technologies,” says Kenneth Epstein, MD, MBA, FHM, FACP, chief medical officer for Traverse City, Mich.-based Hospitalist Consultants Inc. One reason is that hospitalists aren’t beholden to any specific technology, whether endoscopies or cardiac catheterization.

—Scott Lundberg, MD, assistant medical director, Olive View-UCLA Medical Center, Sylmar, Calif.
Mark Graban, author of the book “Lean Hospitals: Improving Quality, Patient Safety, and Employee Satisfaction,” says hospitalists can play another critical role in controlling costs by mapping out and simplifying the discharge processes. He recalls how hospitalists helped coordinate the effort by one of his hospital clients to prevent discharge delays that would have unnecessarily kept patients in the hospital for an additional night or two.
“That length-of-stay reduction, especially in a fixed-reimbursement setting, can have a huge financial impact,” Graban says. “And, inarguably, it’s the right thing to do for the patient, because it’s patients that are medically ready to be discharged. It gets them home and it reduces their increased risk of picking up infections or being involved in hospital errors.”
Focusing on patient safety could translate into big cost savings under the new Medicare system that penalizes providers for certain hospital-acquired conditions, such as skin ulcers and urinary tract infections, Dr. Epstein says. “There’s an emphasis by hospitalists in understanding the system and being willing to put energy into things like documenting ‘present on admission,’ which then has a huge impact on the hospital,” he says. Close monitoring of patients and developing standardization of care can likewise minimize the risk of conditions, such as catheter-associated infections, from cropping up in the hospital.
Dr. Meltzer says his own research suggests that experienced hospitalists are most effective at controlling costs. “So a program that is structured in such a way as to hire or retain experienced hospitalists is likely to have a higher cost savings than one that doesn’t,” he says.
In a broader sense, the maturation of the HM model and more widespread adoption of effective methods by practitioners might be boosting the overall impact of hospitalist care. A study that examined nearly 2 million Medicare admissions over six years found that the effects of the hospitalist care model on LOS became progressively more pronounced over time, from an average reduction of only 0.02 inpatient days in 2001-2002 to a decrease of 0.35 days by 2005-2006.11
Interestingly, the study’s authors suggest that effects attributable to hospitalists were most pronounced among older, complicated, nonsurgical patients cared for at nonprofit community hospitals.
The Verdict
Despite the variable design and scope of individual programs, experts say, HM’s overall net positive on the efficiency of inpatient care is fairly well documented. Future considerations of hospitalists’ true effects on costs, however, will demand an accounting of healthcare across an entire system, where the HM impact is decidedly less certain. “The right comparison in some sense is, What are the total costs of care for a patient cared for in a system that uses hospitalists versus the totals costs of similar patients cared for in a system that doesn’t use hospitalists?” Dr. Meltzer says.
David Mitchell, MD, PhD, a hospitalist at Sibley Memorial Hospital in Washington, D.C., and a member of SHM’s Performance Standards Committee, is among those with an additional concern: Providers may not be taking full advantage of their position to control costs.
“The reason is primarily that the reimbursement structure is not set up to incentivize us to cut costs,” he says. Dr. Mitchell, who has worked in 12 hospitals in six states, argues that hospitalists still are too detached from the true price of ordered tests. “That’s what I fear in hospital medicine, that we just become robots: chest pain means CT scan without thinking,” he says. “This just doesn’t make sense.” Dr. Mitchell also contends that the focus of some HM programs on seeing as many patients as possible to maximize reimbursements is leading to less efficiency. At HM11 in May, he met another hospitalist who said he regularly saw 40 to 45 patients every day. “I know there’s absolutely no way you can see that many patients and do an efficient job,” Dr. Mitchell says.
If one of the clearest areas of success for hospitalists has been in reducing length of stay within a hospital, experts acknowledge that it may no longer be enough. “In the new payment model, success is going to be defined differently, and it will be in terms of reducing the total cost of care,” Dr. Meltzer says.
Over the next decade, hospitalists will need to respond to new set of incentives. “And I think one of the really interesting questions will be how hospitalists can best do that, and the extent to which it causes them to rethink the ways in which they organize their practice,” he says.
Bryn Nelson is a freelance medical writer based in Seattle.
References
- Wachter RM, Goldman L. The hospitalist movement 5 years later. JAMA. 2002;287(4):487-494.
- Lindenauer PK, Rothberg MB, Pekow PS, Kenwood C, Benjamin EM, Auerbach AD. Outcomes of care by hospitalists, general internists, and family physicians. N Engl J Med. 2007;357:2589-2600.
- Peterson MC. A systematic review of outcomes and quality measures in adult patients cared for by hospitalists vs nonhospitalists. Mayo Clin Proc. 2009;84(3): 248-254.
- Lundberg S, Balingit P, Wali S, Cope D. Cost-effectiveness of a hospitalist service in a public teaching hospital. Acad Med. 2010;85(8):1312-1315.
- Esteban-Cruciani N, Montejo J, Azzarone G, Douglas L, et al. Impact of a pediatric hospital medicine program on resource utilization for children with respiratory disorders. J Hosp Med. 2011;6(4)Supp 2:S27.
- Kuo Y-F, Goodwin JS. Association of hospitalist care with medical utilization after discharge: evidence of cost shift from a cohort study. Ann Intern Med. 2011;155(3): 152-159.
- Chen LM, Saint S. Moments in time. Ann Intern Med. 2011;155(3):194-195.
- Huddleston JM, Long KH, Naessens JM, et al. Medical and surgical comanagement after elective hip and knee arthroplasty: a randomized, controlled trial. Ann Intern Med. 2004;141(1):28-38.
- Auerbach AD, Wachter RM, Cheng HQ, et al. Comanagement of surgical patients between neurosurgeons and hospitalists. Arch Intern Med. 2010;170(22): 2004-2010.
- Feldman L, Thiemann D, Brotman D. Financial impact of presenting lab cost data to providers at the time of order entry: a randomized controlled clinical trial. J Hosp Med. 2011;6(4)Supp 2:S93.
- Kuo Y-F, Goodwin JS. Effect of hospitalists on length of stay in the Medicare population: variation according to hospital and patient characteristics. J Am Geriatr Soc. 2010;58:1649-1657.
- Epstein K, Juarez E, Epstein A, Loya K, Singer A. The impact of fragmentation of hospitalist care on length of stay. J Hosp Med. 2010;5(6):335-8.
- Chandra S, Howell E, Wright S. CICLE: Creating incentives and continuity leading to efficiency. J Hosp Med. 2011;6(4)Supp 2:S17
ONLINE EXCLUSIVE: The “Weak Link” in Patient Handoffs
Increased handoffs are often viewed as a byproduct of the growth in hospital medicine, with heightened scrutiny on the quality of communication that accompanies these transfers of care. As research suggests, though, finding and fixing the weak links can require persistence.
A study led by Siddhartha Singh, MD, MS, associate chief medical officer of Medical College Physicians, the adult practice for Medical College of Wisconsin in Milwaukee, compared a traditional, resident-based model of care to one involving a hospitalist-physician assistant team. Initially, his study found a 6% higher length of stay (LOS) for the hospitalist-physician assistant teams, with no differences in costs or readmission rates.1
But when the researchers pored over their results, they discovered that the increased LOS was limited to patients admitted overnight. Those patients, Dr. Singh says, were admitted by other providers—a night-float resident or faculty hospitalist—and then transferred to the hospitalist-physician assistant teams when they arrived in the morning. These “overflow patients” also were admitted only during busy periods, when limits on the number of admissions by house staff required other arrangements.
To make a direct comparison, Dr. Singh focused on a window from 11 a.m. to 4 p.m., when patients would have an equal probability of being admitted by a resident team or a hospitalist-physician assistant team. From a pool of about 3,000 admitted patients, the study found no significant difference in LOS, cost, readmission rates, or mortality. Instead of highlighting significant differences in models of care, then, Dr. Singh says, his study highlighted a potential weak link in the “treacherous” overnight-to-morning handoffs during busy periods that should be addressed.
“There have been a lot of studies implicating poor communication as a cause of patient-safety issues,” notes Sunil Kripalani, MD, MSc, FHM, chief of the section of hospital medicine and an associate professor of medicine at Vanderbilt University Medical Center in Nashville, Tenn. But fewer studies, he says, have shown how to effectively improve communication in a way that improves patient safety.
One focal point is the often incomplete and inadequate nature of discharge summaries. Several models are emerging on how to build a better discharge summary, Dr. Kripalani says, with researchers offering solid recommendations (as multiple presentations at SHM’s annual meeting suggest). The trick is ensuring that those plans can be implemented into practice on a consistent and timely basis.
Dr. Kripalani says at least one straightforward strategy might help improve handoffs, however: building time into the schedule for them, such as 15-minute overlaps between shifts.—BN
Increased handoffs are often viewed as a byproduct of the growth in hospital medicine, with heightened scrutiny on the quality of communication that accompanies these transfers of care. As research suggests, though, finding and fixing the weak links can require persistence.
A study led by Siddhartha Singh, MD, MS, associate chief medical officer of Medical College Physicians, the adult practice for Medical College of Wisconsin in Milwaukee, compared a traditional, resident-based model of care to one involving a hospitalist-physician assistant team. Initially, his study found a 6% higher length of stay (LOS) for the hospitalist-physician assistant teams, with no differences in costs or readmission rates.1
But when the researchers pored over their results, they discovered that the increased LOS was limited to patients admitted overnight. Those patients, Dr. Singh says, were admitted by other providers—a night-float resident or faculty hospitalist—and then transferred to the hospitalist-physician assistant teams when they arrived in the morning. These “overflow patients” also were admitted only during busy periods, when limits on the number of admissions by house staff required other arrangements.
To make a direct comparison, Dr. Singh focused on a window from 11 a.m. to 4 p.m., when patients would have an equal probability of being admitted by a resident team or a hospitalist-physician assistant team. From a pool of about 3,000 admitted patients, the study found no significant difference in LOS, cost, readmission rates, or mortality. Instead of highlighting significant differences in models of care, then, Dr. Singh says, his study highlighted a potential weak link in the “treacherous” overnight-to-morning handoffs during busy periods that should be addressed.
“There have been a lot of studies implicating poor communication as a cause of patient-safety issues,” notes Sunil Kripalani, MD, MSc, FHM, chief of the section of hospital medicine and an associate professor of medicine at Vanderbilt University Medical Center in Nashville, Tenn. But fewer studies, he says, have shown how to effectively improve communication in a way that improves patient safety.
One focal point is the often incomplete and inadequate nature of discharge summaries. Several models are emerging on how to build a better discharge summary, Dr. Kripalani says, with researchers offering solid recommendations (as multiple presentations at SHM’s annual meeting suggest). The trick is ensuring that those plans can be implemented into practice on a consistent and timely basis.
Dr. Kripalani says at least one straightforward strategy might help improve handoffs, however: building time into the schedule for them, such as 15-minute overlaps between shifts.—BN
Increased handoffs are often viewed as a byproduct of the growth in hospital medicine, with heightened scrutiny on the quality of communication that accompanies these transfers of care. As research suggests, though, finding and fixing the weak links can require persistence.
A study led by Siddhartha Singh, MD, MS, associate chief medical officer of Medical College Physicians, the adult practice for Medical College of Wisconsin in Milwaukee, compared a traditional, resident-based model of care to one involving a hospitalist-physician assistant team. Initially, his study found a 6% higher length of stay (LOS) for the hospitalist-physician assistant teams, with no differences in costs or readmission rates.1
But when the researchers pored over their results, they discovered that the increased LOS was limited to patients admitted overnight. Those patients, Dr. Singh says, were admitted by other providers—a night-float resident or faculty hospitalist—and then transferred to the hospitalist-physician assistant teams when they arrived in the morning. These “overflow patients” also were admitted only during busy periods, when limits on the number of admissions by house staff required other arrangements.
To make a direct comparison, Dr. Singh focused on a window from 11 a.m. to 4 p.m., when patients would have an equal probability of being admitted by a resident team or a hospitalist-physician assistant team. From a pool of about 3,000 admitted patients, the study found no significant difference in LOS, cost, readmission rates, or mortality. Instead of highlighting significant differences in models of care, then, Dr. Singh says, his study highlighted a potential weak link in the “treacherous” overnight-to-morning handoffs during busy periods that should be addressed.
“There have been a lot of studies implicating poor communication as a cause of patient-safety issues,” notes Sunil Kripalani, MD, MSc, FHM, chief of the section of hospital medicine and an associate professor of medicine at Vanderbilt University Medical Center in Nashville, Tenn. But fewer studies, he says, have shown how to effectively improve communication in a way that improves patient safety.
One focal point is the often incomplete and inadequate nature of discharge summaries. Several models are emerging on how to build a better discharge summary, Dr. Kripalani says, with researchers offering solid recommendations (as multiple presentations at SHM’s annual meeting suggest). The trick is ensuring that those plans can be implemented into practice on a consistent and timely basis.
Dr. Kripalani says at least one straightforward strategy might help improve handoffs, however: building time into the schedule for them, such as 15-minute overlaps between shifts.—BN
A Critical First Step
For those of you who were kind enough to catch my column in last month’s issue of The Hospitalist (see “What Is Your Value,” p. 56), you spent a few minutes reading my thoughts on the value of hospitalists. I mentioned the fact that the U.S. is moving rapidly toward a value-based system of purchasing healthcare, and that all healthcare providers, including hospitalists, increasingly will be judged on the value of care they deliver to their patients and the healthcare system. (Remember, value=quality/cost.)
Hospitalists, like all other healthcare providers, can increase their “value” by improving the quality of care they provide and decreasing the cost of healthcare delivery. Seems simple enough, right? Take better care of patients and do so while minimizing unnecessary costs. (If you have figured out how to do this, I want to learn from you!)
As a doctor and as the leader of the hospitalist group at Beth Israel Deaconess Medical Center in Boston, I have given this topic considerable thought. How do I become a “high value” provider? How do I help my hospitalist colleagues become “high value” hospitalists? Another persistent thought that has crossed my mind is: “How do I know that I am not already a high-value hospitalist?”
Maybe all of my hospitalist colleagues at Beth Israel Deaconess Medical Center are high-value providers. Seems fair enough, right? Maybe each of us is providing “high quality” care and doing so while minimizing unnecessary costs.
I mean, who really wants to think of themselves as low-quality doctors spending a considerable amount of unnecessary resources?
Like many of you, it became evident to me that the first step to improving quality and/or decreasing cost is to define “quality” and “cost.”
The First Step
Although it might seem difficult for the individual hospitalist to know the cost of a patient’s hospitalization, such information is available, and your hospital administrator might be willing to share such information with you and your group. But when it comes to quality of care, I think most patients would expect that doctors should understand the definition of “high-quality care.”
So, what is the definition of “high-quality care?” Try asking this question of patients and doctors, and you are likely to get very different answers. Not surprised? Try asking this question just to doctors, and you are likely to get some different answers. (For fun, you could try this exercise with your hospitalist colleagues; I have.)
Honestly, none of us should be alarmed if a group of doctors cannot easily define “high-quality care.” Not being able to do so does not mean these are “bad” doctors. While it may not be easy to define high-quality care, I suspect most of us recognize it when we see it.
The process of defining the quality of care involves capturing the essence of what we see. For example, can we agree that prescribing aspirin for patients with acute coronary syndrome is optimal care? If so, it stands to reason that a patient with acute coronary syndrome who did not receive aspirin received suboptimal care.
This is how a group of hospitalists can go about creating a quality standard. If you are a hospitalist or HM group leader who is interested in improving the quality of care you and your colleagues are providing to your patients, defining a quality standard is the critical first step to process improvement. Do not limit yourself to clinical processes. Although clinical processes are important, so are communication and documentation processes.
For example, most of us, as hospitalists, believe that communication with outpatient providers is important to the provision of high-quality inpatient care. How often do your hospitalists communicate with patients’ primary-care providers? Is this a quality standard for your hospitalist group? What about the documentation of a patient’s code status at the time of admission or documentation of a patient’s functional status in the discharge summary?
If you believe these are important, your group should include these as quality standards. You should be measuring them and reporting the results to individual providers.
Start with Definition
At this point, some of us might be tempted to get ahead of ourselves and worry about what standards we can or cannot measure, but I urge you to complete this first step of defining “high-quality care” before worrying about anything else. (In other words, don’t start running before you can walk.)
Another suggestion: Please don’t try to do too much all at once. Nobody is going to argue that patients with acute coronary syndrome should not receive aspirin. Reaching consensus on other quality standards might not be as easy. But do not get bogged down trying to create too many quality standards all at once. Start with a few and get yourself and your colleagues accustomed to the process.
Remember, when it comes to doctors, we have centuries of history of not knowing exactly what we are doing. I hope it won’t take centuries to fix this problem, but I also know we are not going to fix this in a few days or weeks. Small victories along the way are important if we hope to succeed.
Once you and your hospitalist colleagues arrive at a mutually agreed upon quality standard, the next step is performance measurement. I honestly believe performance measurement is easy when we spend the time understanding and agreeing to the most appropriate quality standards for our hospitalist groups.
I am interested in learning about your efforts to define the quality standards for your hospitalist group. Feel free to email me at [email protected].
Dr. Li is president of SHM.
For those of you who were kind enough to catch my column in last month’s issue of The Hospitalist (see “What Is Your Value,” p. 56), you spent a few minutes reading my thoughts on the value of hospitalists. I mentioned the fact that the U.S. is moving rapidly toward a value-based system of purchasing healthcare, and that all healthcare providers, including hospitalists, increasingly will be judged on the value of care they deliver to their patients and the healthcare system. (Remember, value=quality/cost.)
Hospitalists, like all other healthcare providers, can increase their “value” by improving the quality of care they provide and decreasing the cost of healthcare delivery. Seems simple enough, right? Take better care of patients and do so while minimizing unnecessary costs. (If you have figured out how to do this, I want to learn from you!)
As a doctor and as the leader of the hospitalist group at Beth Israel Deaconess Medical Center in Boston, I have given this topic considerable thought. How do I become a “high value” provider? How do I help my hospitalist colleagues become “high value” hospitalists? Another persistent thought that has crossed my mind is: “How do I know that I am not already a high-value hospitalist?”
Maybe all of my hospitalist colleagues at Beth Israel Deaconess Medical Center are high-value providers. Seems fair enough, right? Maybe each of us is providing “high quality” care and doing so while minimizing unnecessary costs.
I mean, who really wants to think of themselves as low-quality doctors spending a considerable amount of unnecessary resources?
Like many of you, it became evident to me that the first step to improving quality and/or decreasing cost is to define “quality” and “cost.”
The First Step
Although it might seem difficult for the individual hospitalist to know the cost of a patient’s hospitalization, such information is available, and your hospital administrator might be willing to share such information with you and your group. But when it comes to quality of care, I think most patients would expect that doctors should understand the definition of “high-quality care.”
So, what is the definition of “high-quality care?” Try asking this question of patients and doctors, and you are likely to get very different answers. Not surprised? Try asking this question just to doctors, and you are likely to get some different answers. (For fun, you could try this exercise with your hospitalist colleagues; I have.)
Honestly, none of us should be alarmed if a group of doctors cannot easily define “high-quality care.” Not being able to do so does not mean these are “bad” doctors. While it may not be easy to define high-quality care, I suspect most of us recognize it when we see it.
The process of defining the quality of care involves capturing the essence of what we see. For example, can we agree that prescribing aspirin for patients with acute coronary syndrome is optimal care? If so, it stands to reason that a patient with acute coronary syndrome who did not receive aspirin received suboptimal care.
This is how a group of hospitalists can go about creating a quality standard. If you are a hospitalist or HM group leader who is interested in improving the quality of care you and your colleagues are providing to your patients, defining a quality standard is the critical first step to process improvement. Do not limit yourself to clinical processes. Although clinical processes are important, so are communication and documentation processes.
For example, most of us, as hospitalists, believe that communication with outpatient providers is important to the provision of high-quality inpatient care. How often do your hospitalists communicate with patients’ primary-care providers? Is this a quality standard for your hospitalist group? What about the documentation of a patient’s code status at the time of admission or documentation of a patient’s functional status in the discharge summary?
If you believe these are important, your group should include these as quality standards. You should be measuring them and reporting the results to individual providers.
Start with Definition
At this point, some of us might be tempted to get ahead of ourselves and worry about what standards we can or cannot measure, but I urge you to complete this first step of defining “high-quality care” before worrying about anything else. (In other words, don’t start running before you can walk.)
Another suggestion: Please don’t try to do too much all at once. Nobody is going to argue that patients with acute coronary syndrome should not receive aspirin. Reaching consensus on other quality standards might not be as easy. But do not get bogged down trying to create too many quality standards all at once. Start with a few and get yourself and your colleagues accustomed to the process.
Remember, when it comes to doctors, we have centuries of history of not knowing exactly what we are doing. I hope it won’t take centuries to fix this problem, but I also know we are not going to fix this in a few days or weeks. Small victories along the way are important if we hope to succeed.
Once you and your hospitalist colleagues arrive at a mutually agreed upon quality standard, the next step is performance measurement. I honestly believe performance measurement is easy when we spend the time understanding and agreeing to the most appropriate quality standards for our hospitalist groups.
I am interested in learning about your efforts to define the quality standards for your hospitalist group. Feel free to email me at [email protected].
Dr. Li is president of SHM.
For those of you who were kind enough to catch my column in last month’s issue of The Hospitalist (see “What Is Your Value,” p. 56), you spent a few minutes reading my thoughts on the value of hospitalists. I mentioned the fact that the U.S. is moving rapidly toward a value-based system of purchasing healthcare, and that all healthcare providers, including hospitalists, increasingly will be judged on the value of care they deliver to their patients and the healthcare system. (Remember, value=quality/cost.)
Hospitalists, like all other healthcare providers, can increase their “value” by improving the quality of care they provide and decreasing the cost of healthcare delivery. Seems simple enough, right? Take better care of patients and do so while minimizing unnecessary costs. (If you have figured out how to do this, I want to learn from you!)
As a doctor and as the leader of the hospitalist group at Beth Israel Deaconess Medical Center in Boston, I have given this topic considerable thought. How do I become a “high value” provider? How do I help my hospitalist colleagues become “high value” hospitalists? Another persistent thought that has crossed my mind is: “How do I know that I am not already a high-value hospitalist?”
Maybe all of my hospitalist colleagues at Beth Israel Deaconess Medical Center are high-value providers. Seems fair enough, right? Maybe each of us is providing “high quality” care and doing so while minimizing unnecessary costs.
I mean, who really wants to think of themselves as low-quality doctors spending a considerable amount of unnecessary resources?
Like many of you, it became evident to me that the first step to improving quality and/or decreasing cost is to define “quality” and “cost.”
The First Step
Although it might seem difficult for the individual hospitalist to know the cost of a patient’s hospitalization, such information is available, and your hospital administrator might be willing to share such information with you and your group. But when it comes to quality of care, I think most patients would expect that doctors should understand the definition of “high-quality care.”
So, what is the definition of “high-quality care?” Try asking this question of patients and doctors, and you are likely to get very different answers. Not surprised? Try asking this question just to doctors, and you are likely to get some different answers. (For fun, you could try this exercise with your hospitalist colleagues; I have.)
Honestly, none of us should be alarmed if a group of doctors cannot easily define “high-quality care.” Not being able to do so does not mean these are “bad” doctors. While it may not be easy to define high-quality care, I suspect most of us recognize it when we see it.
The process of defining the quality of care involves capturing the essence of what we see. For example, can we agree that prescribing aspirin for patients with acute coronary syndrome is optimal care? If so, it stands to reason that a patient with acute coronary syndrome who did not receive aspirin received suboptimal care.
This is how a group of hospitalists can go about creating a quality standard. If you are a hospitalist or HM group leader who is interested in improving the quality of care you and your colleagues are providing to your patients, defining a quality standard is the critical first step to process improvement. Do not limit yourself to clinical processes. Although clinical processes are important, so are communication and documentation processes.
For example, most of us, as hospitalists, believe that communication with outpatient providers is important to the provision of high-quality inpatient care. How often do your hospitalists communicate with patients’ primary-care providers? Is this a quality standard for your hospitalist group? What about the documentation of a patient’s code status at the time of admission or documentation of a patient’s functional status in the discharge summary?
If you believe these are important, your group should include these as quality standards. You should be measuring them and reporting the results to individual providers.
Start with Definition
At this point, some of us might be tempted to get ahead of ourselves and worry about what standards we can or cannot measure, but I urge you to complete this first step of defining “high-quality care” before worrying about anything else. (In other words, don’t start running before you can walk.)
Another suggestion: Please don’t try to do too much all at once. Nobody is going to argue that patients with acute coronary syndrome should not receive aspirin. Reaching consensus on other quality standards might not be as easy. But do not get bogged down trying to create too many quality standards all at once. Start with a few and get yourself and your colleagues accustomed to the process.
Remember, when it comes to doctors, we have centuries of history of not knowing exactly what we are doing. I hope it won’t take centuries to fix this problem, but I also know we are not going to fix this in a few days or weeks. Small victories along the way are important if we hope to succeed.
Once you and your hospitalist colleagues arrive at a mutually agreed upon quality standard, the next step is performance measurement. I honestly believe performance measurement is easy when we spend the time understanding and agreeing to the most appropriate quality standards for our hospitalist groups.
I am interested in learning about your efforts to define the quality standards for your hospitalist group. Feel free to email me at [email protected].
Dr. Li is president of SHM.
SQUINT Is Looking Out For You
Starting a new, hospital-based quality-improvement (QI) program can be a lonely task for hospitalists. What can begin with a rush of enthusiasm to solve a critical problem on your hospital floor quickly can lead to a single hospitalist in front of a computer screen wondering, "Has anyone else ever done this before?"
Unlike clinical knowledge, most of which comes from years of specialized formal training and volumes of peer-reviewed evidence on procedures, starting QI programs often presents a special challenge: a blank page and limited access to those who’ve taken on similar projects.
Those challenges, and the need to better understand what other hospitalists have already tried, motivated SHM’s Center for Hospital Innovation & Improvement, also known as The Center, to develop SQUINT, a new user-generated online repository of hospital-based QI programs.
"Being asked to lead a quality-improvement project is a daunting and difficult task," says Andrew Dunn, MD, FACP, professor of medicine and acting chief for Mount Sinai School of Medicine’s hospital medicine division in New York City. "Getting ideas on methods that have worked elsewhere is a great way to start. SQUINT is an easy way for hospitalists to get a head start on a project rather than start from scratch."
Access to SQUINT (SHM’s QUality Improve-ment NeTwork) is free to SHM members. Log in and gain access to summaries of QI programs from around the country. Because the summaries are searchable based on type, size, location, and specific kinds of topics, hospitalists can quickly find out whether projects similar to theirs are available through SQUINT.
For instance, a user could search for projects specifically related to transitions of care during discharge at community hospitals with 200-299 beds; a user in Oklahoma could search for all QI projects that have been uploaded from hospitals in the Sooner State. SQUINT also affords users keyword searches and browsing options.
For Hasan F. Shabbir, MD, SFHM, chief quality officer at Emory Johns Creek Hospital and assistant professor of medicine for Emory University School of Medicine’s division of hospital medicine in Atlanta, the ability to search user-generated, user-posted project files is especially important. Dr. Shabbir is no stranger to starting a QI project cold, or poring through literature and searching the Internet, worried that the materials don’t always explain the outcomes of a QI project that can be found through Google.
"You may just find a PDF on the Web and not know if it was a success," he says. "What’s unique about SQUINT is that it gives you a product, describes how it was utilized, and describes how it was—or wasn’t—effective. A lot of the work that needs to be done doesn’t always achieve the intended result."
Understanding the pitfalls and challenges of QI programs can save time and effort, he explains. "It’s equally important," he says. "Typically, only the successful stuff gets published in journals."
One of the first projects shared via SQUINT is a case study in using local resources to improve transitions of care for diabetic patients, submitted by medical director Jordan Messler, MD, SFHM, and his colleagues at Morton Plant Hospital in Clearwater, Fla.
"This was a project that we have done that we were probably not going to publish, but came up with some neat process things that we can share," says Dr. Messler, who hopes his team’s progress could help others get started. "If just one other program finds it and it saves them some time, that would be great."
Uploading descriptions of the QI programs can take as little as 15 minutes. Once project details and supporting documents are loaded into SQUINT, submissions are reviewed by members of SHM’s Health Quality and Patient Safety committee for clarity, the involvement of multidisciplinary team members, presentation of details, and the description of impacts and barriers to success.
Dr. Messler found the process of uploading simple and easy to use. He plans to add more.
"We have a variety of programs that we’ll probably upload," he says, including other recent QI programs addressing diabetes and DVT. "There’s no harm in putting them up there."
—Andrew Dunn, MD, FACP, professor, acting chief, hospital medicine division, Mount Sinai School of Medicine, New York City
Like other online user-submitted forums, submitting accepted content has added benefits: increased visibility among a community dedicated to improving the care of hospitalized patients and career advancement.
"This is a portal for you to spread what you’ve learned," Dr. Messler says. "Then, over time, this could be something that could be added to a resume or get to the point that folks will be proud of having a list of submissions to SQUINT."
For Dr. Shabbir, the utility of SQUINT extends beyond his own use.
"I have a junior colleague who is working on a new quality-improvement program. I’m going to tell her to look into SQUINT to see if others have worked on similar programs," he says. "If they have, that will put you two or three steps forward. For the novice, it also teaches the language and structure of how quality improvement happens."
Teaching and changing patient safety is a big part of SQUINT’s goal, according to Dr. Dunn.
"Hospitals should not need to start at ground zero, take months to get started and re-create every mistake made at other institutions," he says. "By sharing successful projects and learning from our errors, we can move patient safety initiatives along faster and better. … And that will, hopefully, improve outcomes across the country."
Brendon Shank is associate vice president of communications at SHM.
Starting a new, hospital-based quality-improvement (QI) program can be a lonely task for hospitalists. What can begin with a rush of enthusiasm to solve a critical problem on your hospital floor quickly can lead to a single hospitalist in front of a computer screen wondering, "Has anyone else ever done this before?"
Unlike clinical knowledge, most of which comes from years of specialized formal training and volumes of peer-reviewed evidence on procedures, starting QI programs often presents a special challenge: a blank page and limited access to those who’ve taken on similar projects.
Those challenges, and the need to better understand what other hospitalists have already tried, motivated SHM’s Center for Hospital Innovation & Improvement, also known as The Center, to develop SQUINT, a new user-generated online repository of hospital-based QI programs.
"Being asked to lead a quality-improvement project is a daunting and difficult task," says Andrew Dunn, MD, FACP, professor of medicine and acting chief for Mount Sinai School of Medicine’s hospital medicine division in New York City. "Getting ideas on methods that have worked elsewhere is a great way to start. SQUINT is an easy way for hospitalists to get a head start on a project rather than start from scratch."
Access to SQUINT (SHM’s QUality Improve-ment NeTwork) is free to SHM members. Log in and gain access to summaries of QI programs from around the country. Because the summaries are searchable based on type, size, location, and specific kinds of topics, hospitalists can quickly find out whether projects similar to theirs are available through SQUINT.
For instance, a user could search for projects specifically related to transitions of care during discharge at community hospitals with 200-299 beds; a user in Oklahoma could search for all QI projects that have been uploaded from hospitals in the Sooner State. SQUINT also affords users keyword searches and browsing options.
For Hasan F. Shabbir, MD, SFHM, chief quality officer at Emory Johns Creek Hospital and assistant professor of medicine for Emory University School of Medicine’s division of hospital medicine in Atlanta, the ability to search user-generated, user-posted project files is especially important. Dr. Shabbir is no stranger to starting a QI project cold, or poring through literature and searching the Internet, worried that the materials don’t always explain the outcomes of a QI project that can be found through Google.
"You may just find a PDF on the Web and not know if it was a success," he says. "What’s unique about SQUINT is that it gives you a product, describes how it was utilized, and describes how it was—or wasn’t—effective. A lot of the work that needs to be done doesn’t always achieve the intended result."
Understanding the pitfalls and challenges of QI programs can save time and effort, he explains. "It’s equally important," he says. "Typically, only the successful stuff gets published in journals."
One of the first projects shared via SQUINT is a case study in using local resources to improve transitions of care for diabetic patients, submitted by medical director Jordan Messler, MD, SFHM, and his colleagues at Morton Plant Hospital in Clearwater, Fla.
"This was a project that we have done that we were probably not going to publish, but came up with some neat process things that we can share," says Dr. Messler, who hopes his team’s progress could help others get started. "If just one other program finds it and it saves them some time, that would be great."
Uploading descriptions of the QI programs can take as little as 15 minutes. Once project details and supporting documents are loaded into SQUINT, submissions are reviewed by members of SHM’s Health Quality and Patient Safety committee for clarity, the involvement of multidisciplinary team members, presentation of details, and the description of impacts and barriers to success.
Dr. Messler found the process of uploading simple and easy to use. He plans to add more.
"We have a variety of programs that we’ll probably upload," he says, including other recent QI programs addressing diabetes and DVT. "There’s no harm in putting them up there."
—Andrew Dunn, MD, FACP, professor, acting chief, hospital medicine division, Mount Sinai School of Medicine, New York City
Like other online user-submitted forums, submitting accepted content has added benefits: increased visibility among a community dedicated to improving the care of hospitalized patients and career advancement.
"This is a portal for you to spread what you’ve learned," Dr. Messler says. "Then, over time, this could be something that could be added to a resume or get to the point that folks will be proud of having a list of submissions to SQUINT."
For Dr. Shabbir, the utility of SQUINT extends beyond his own use.
"I have a junior colleague who is working on a new quality-improvement program. I’m going to tell her to look into SQUINT to see if others have worked on similar programs," he says. "If they have, that will put you two or three steps forward. For the novice, it also teaches the language and structure of how quality improvement happens."
Teaching and changing patient safety is a big part of SQUINT’s goal, according to Dr. Dunn.
"Hospitals should not need to start at ground zero, take months to get started and re-create every mistake made at other institutions," he says. "By sharing successful projects and learning from our errors, we can move patient safety initiatives along faster and better. … And that will, hopefully, improve outcomes across the country."
Brendon Shank is associate vice president of communications at SHM.
Starting a new, hospital-based quality-improvement (QI) program can be a lonely task for hospitalists. What can begin with a rush of enthusiasm to solve a critical problem on your hospital floor quickly can lead to a single hospitalist in front of a computer screen wondering, "Has anyone else ever done this before?"
Unlike clinical knowledge, most of which comes from years of specialized formal training and volumes of peer-reviewed evidence on procedures, starting QI programs often presents a special challenge: a blank page and limited access to those who’ve taken on similar projects.
Those challenges, and the need to better understand what other hospitalists have already tried, motivated SHM’s Center for Hospital Innovation & Improvement, also known as The Center, to develop SQUINT, a new user-generated online repository of hospital-based QI programs.
"Being asked to lead a quality-improvement project is a daunting and difficult task," says Andrew Dunn, MD, FACP, professor of medicine and acting chief for Mount Sinai School of Medicine’s hospital medicine division in New York City. "Getting ideas on methods that have worked elsewhere is a great way to start. SQUINT is an easy way for hospitalists to get a head start on a project rather than start from scratch."
Access to SQUINT (SHM’s QUality Improve-ment NeTwork) is free to SHM members. Log in and gain access to summaries of QI programs from around the country. Because the summaries are searchable based on type, size, location, and specific kinds of topics, hospitalists can quickly find out whether projects similar to theirs are available through SQUINT.
For instance, a user could search for projects specifically related to transitions of care during discharge at community hospitals with 200-299 beds; a user in Oklahoma could search for all QI projects that have been uploaded from hospitals in the Sooner State. SQUINT also affords users keyword searches and browsing options.
For Hasan F. Shabbir, MD, SFHM, chief quality officer at Emory Johns Creek Hospital and assistant professor of medicine for Emory University School of Medicine’s division of hospital medicine in Atlanta, the ability to search user-generated, user-posted project files is especially important. Dr. Shabbir is no stranger to starting a QI project cold, or poring through literature and searching the Internet, worried that the materials don’t always explain the outcomes of a QI project that can be found through Google.
"You may just find a PDF on the Web and not know if it was a success," he says. "What’s unique about SQUINT is that it gives you a product, describes how it was utilized, and describes how it was—or wasn’t—effective. A lot of the work that needs to be done doesn’t always achieve the intended result."
Understanding the pitfalls and challenges of QI programs can save time and effort, he explains. "It’s equally important," he says. "Typically, only the successful stuff gets published in journals."
One of the first projects shared via SQUINT is a case study in using local resources to improve transitions of care for diabetic patients, submitted by medical director Jordan Messler, MD, SFHM, and his colleagues at Morton Plant Hospital in Clearwater, Fla.
"This was a project that we have done that we were probably not going to publish, but came up with some neat process things that we can share," says Dr. Messler, who hopes his team’s progress could help others get started. "If just one other program finds it and it saves them some time, that would be great."
Uploading descriptions of the QI programs can take as little as 15 minutes. Once project details and supporting documents are loaded into SQUINT, submissions are reviewed by members of SHM’s Health Quality and Patient Safety committee for clarity, the involvement of multidisciplinary team members, presentation of details, and the description of impacts and barriers to success.
Dr. Messler found the process of uploading simple and easy to use. He plans to add more.
"We have a variety of programs that we’ll probably upload," he says, including other recent QI programs addressing diabetes and DVT. "There’s no harm in putting them up there."
—Andrew Dunn, MD, FACP, professor, acting chief, hospital medicine division, Mount Sinai School of Medicine, New York City
Like other online user-submitted forums, submitting accepted content has added benefits: increased visibility among a community dedicated to improving the care of hospitalized patients and career advancement.
"This is a portal for you to spread what you’ve learned," Dr. Messler says. "Then, over time, this could be something that could be added to a resume or get to the point that folks will be proud of having a list of submissions to SQUINT."
For Dr. Shabbir, the utility of SQUINT extends beyond his own use.
"I have a junior colleague who is working on a new quality-improvement program. I’m going to tell her to look into SQUINT to see if others have worked on similar programs," he says. "If they have, that will put you two or three steps forward. For the novice, it also teaches the language and structure of how quality improvement happens."
Teaching and changing patient safety is a big part of SQUINT’s goal, according to Dr. Dunn.
"Hospitals should not need to start at ground zero, take months to get started and re-create every mistake made at other institutions," he says. "By sharing successful projects and learning from our errors, we can move patient safety initiatives along faster and better. … And that will, hopefully, improve outcomes across the country."
Brendon Shank is associate vice president of communications at SHM.
Are You Delivering on the Promise of Higher Quality?
One hospitalist-led pilot project produced a 61% decrease in heart failure readmission rates. Another resulted in a 33% drop in all-cause readmissions. The numbers might be impressive, but what do they really say about how hospitalists have influenced healthcare quality?
When HM emerged 15 years ago, advocates pitched the fledgling physician specialty as a model of efficient inpatient care, and subsequent findings that the concept led to reductions in length of stay encouraged more hospitals to bolster their staff with the newcomers. With a rising emphasis on quality and patient safety over the past decade, and the new era of pay-for-performance, the hospitalist model of care has expanded to embrace improved quality of care as a chief selling point.
Measuring quality is no easy task, however, and researchers still debate the relative merits of metrics like 30-day readmission rates and inpatient mortality. "Without question, quality measurement is an imperfect science, and all measures will contain some level of imprecision and bias," concluded a recent commentary in Health Affairs.1
Against that backdrop, relatively few studies have looked broadly at the contributions of hospital medicine. Most interventions have been individually tailored to a hospital or instituted at only a few sites, precluding large-scale, head-to-head comparisons.
And so the question remains: Has hospital medicine lived up to its promise on quality?
The Evidence
In one of the few national surveys of HM’s impact on patient care, a yearlong comparison of more than 3,600 hospitals found that the roughly 40% that employed hospitalists scored better on multiple Hospital Quality Alliance indicators. The 2009 Archives of Internal Medicine study suggested that hospitals with hospitalists outperformed their counterparts in quality metrics for acute myocardial infarction, pneumonia, overall disease treatment and diagnosis, and counseling and prevention. Congestive heart failure was the only category of the five reviewed that lacked a statistically significant difference.2
A separate editorial, however, argued that the study’s data were not persuasive enough to support the conclusion that hospitalists bring a higher quality of care to the table.3 And even less can be said about the national impact of HM on newly elevated metrics, such as readmission rates. The obligation to gather evidence, in fact, is largely falling upon hospitalists themselves, and the multitude of research abstracts from SHM’s annual meeting in May suggests that plenty of physician scientists are taking the responsibility seriously. Among the presentations, a study led by David Boyte, MD, assistant professor of medicine at Duke University and a hospitalist at Durham Regional Hospital, found that a multidisciplinary approach greatly improved one hospital unit’s 30-day readmission rates for heart failure patients. After a three-month pilot in the cardiac nursing unit, readmission rates fell to 10.7% from 27.6%.4
Although the multidisciplinary effort has included doctors, nurses, nutritionists, pharmacists, unit managers, and other personnel, Dr. Boyte says the involvement of hospitalists has been key to the project’s success. "We feel like we were the main participants who could see the whole picture from a patient-centered perspective," he says. "We were the glue; we were the center node of all the healthcare providers." Based on that dramatic improvement, Dr. Boyte says, the same interventional protocol has been rolled out in three other medical surgical units, and the hospital is using a similar approach to address AMI readmission rates.
SHM’s Project BOOST (Better Outcomes for Older Adults through Safe Transitions; www.hospitalmedicine.org/boost )—by far the largest study of how HM is impacting readmission rates—has amassed data from more than 20 hospitals, with more expected from a growing roster of participants. So far, however, the project has only released data from six pilot sites describing the six-month periods before and after the project’s start. Among those sites, initial results suggest that readmission rates fell by an average of more than 20%, to 11.2% from 14.2%.5
Though the early numbers are encouraging, experts say rates from a larger group of participants at the one-year mark will be more telling, as will direct comparisons between BOOST units and nonparticipating counterparts at the same hospitals. Principal investigator Mark Williams, MD, FHM, professor and chief of the division of hospital medicine at the Northwestern University Feinberg School of Medicine in Chicago, says researchers still need to clean up that data before they’re ready to share it publicly.
In the meantime, some individual BOOST case studies are suggesting that hospitalist-led changes could pay big dividends. To help create cohesiveness and a sense of ownership within its HM program, St. Mary’s Health Center in St. Louis started a 20-bed hospitalist unit in 2008. Philip Vaidyan, MD, FACP, head of the hospitalist program and practice group leader for IPC: The Hospitalist Company at St. Mary’s, says one unit, 3 West, has since functioned as a lab for testing new ideas that are then introduced hospitalwide.
One early change was to bring all of the unit’s care providers together, from doctors and nurses to the unit-based case manager and social worker, for 9 a.m. handoff meetings. "We have this collective brain to find unique solutions," Dr. Vaidyan says. After seeing positive trends on length of stay, 30-day readmission rates, and patient satisfaction scores, St. Mary’s upgraded to a 32-bed hospitalist unit in early 2009. That same year, the 525-bed community teaching hospital was accepted into the BOOST program.
The hospitalist unit’s improved quality scores continued under BOOST, leading to a 33% reduction in readmission rates from 2008 to 2010 (to 10.5% from 15.7%). Rates for a nonhospitalist unit, by contrast, hovered around 17%. "For reducing readmissions, people may think that you have to have a higher length of stay," Dr. Vaidyan says. But the unit trended toward a lower length of stay, in addition to its reduced 30-day readmissions and improved patient satisfaction scores.
Flush with success, the 10 physicians and four nurse practitioners in the hospitalist program have since begun spreading their best practices to the rest of the hospital units. "Hospitalists are in the best ‘sweet spot,’ " Dr. Vaidyan says, "partnering with all of the disciplines, bringing them together, and keeping everybody on the same page."
Ironically, pinpointing the contribution of hospitalists is harder when their changes produce an ecological effect throughout an entire institution, says Siddhartha Singh, MD, MS, associate chief medical officer of Medical College Physicians, the adult practice for Medical College of Wisconsin in Milwaukee. Even so, he stresses that the impact of the two dozen hospitalists at Medical College Physicians has been felt.
"Coinciding with and following the introduction of our hospitalist program in 2004, we have noticed dramatic decreases in our length of stay throughout medicine services," he says. The same has held true for inpatient mortality. "And that, we feel, is attributable to the standardization of processes introduced by the hospitalist group." Multidisciplinary rounds; whiteboards in patient rooms; and standardized admission orders, prophylactic treatments, and discharge processes—"all of this would’ve been impossible, absolutely impossible, without the hospitalist," he says.
Over the past decade, Dr. Singh’s assessment has been echoed by several studies suggesting that individual hospitalist programs have brought significant improvements in quality measures, such as complication rates and inpatient mortality. In 2002, for example, Andrew Auerbach, MD, MPH, at the University of California San Francisco Medical Center, led a study that compared HM care with that of community physicians in a community-based teaching hospital. Patients cared for by hospitalists, the study found, had a lower risk of death during the hospitalization, as well as at 30 days and 60 days after discharge.6
A separate report by David Meltzer, MD, PhD, and colleagues at the University of Chicago found that an HM program in an academic general medicine service led to a 30% reduction in 30-day mortality rates during its second year of operation.7 And a 2004 study led by Jeanne Huddleston, MD, at the Mayo Clinic College of Medicine in Rochester, Minn., found that a hospitalist-orthopedic co-management model (versus care by orthopedic surgeons with medical consultation) led to more patients being discharged with no complications after elective hip or knee surgery.8 Hospitalist co-management also reduced the rate of minor complications, but had no effect on actual length of stay or cost.
A subsequent study by the same group, however, documented improved efficiency of care through the HM model, but no effect on the mortality of hip fracture patients up to one year after discharge.9 Multiple studies of hospitalist programs, in fact, have seen increased efficiency but little or no impact on inpatient mortality, leading researchers to broadly conclude that such programs can decrease resource use without compromising quality.
In 2007, a retrospective study of nearly 77,000 patients admitted to 45 hospitals with one of seven common diagnoses compared the care delivered by hospitalists, general internists, and family physicians.10 Although the study authors found that hospitalist care yielded a small drop in length of stay, they saw no difference in the inpatient mortality rates or 14-day readmission rates. More recently, mortality has become ensnared in controversy over its reliability as an accurate indicator of quality.

-Shai Gavi, DO, MPH, chief, section of hospital medicine, assistant professor, Stony Brook University School of Medicine, Brookhaven, N.Y.
Half of the Equation
Despite a lack of ideal metrics, another promising sign for HM might be the model’s exportability. Lee Kheng Hock, MMed, senior consultant and head of the Department of Family Medicine and Continuing Care at Singapore General Hospital, says the 1,600-bed hospital began experimenting with the hospitalist model when officials realized the existing care system wasn’t sustainable. Amid an aging population and increasingly complex and fragmented care, Hock views the hospitalist movement as a natural evolution of the healthcare system to meet the needs of a changing environment.
In a recent study, Hock and his colleagues used the hospital’s administrative database to examine the resource use and outcomes of patients cared for in 2008 by family medicine hospitalists or by specialists.11 The comparison, based on several standard metrics, found no significant improvements in quality, with similar inpatient mortality rates and 30-day, all-cause, unscheduled readmission rates regardless of the care delivery method. The study, though, revealed a significantly shorter hospital stay (4.4 days vs. 5.3 days) and lower costs per patient for those cared for by hospitalists ($2,250 vs. $2,500).11
Hock points out that, like his study, most analyses of hospitalist programs have shown an improvement in length of stay and cost of care without any increase in mortality and morbidity. If value equals quality divided by cost, he says, it stands to reason that quality must increase as overall value remains the same but costs decrease.
"The main difference is that the patients received undivided attention from a well-rounded generalist physician who is focused on providing holistic general medical care," Hock says, adding that "it is really a no-brainer that the outcome would be different."
Patients Rule
Other measures like the effectiveness of communication and seamlessness of handoffs often are assessed through their impacts on patient outcomes. But Sunil Kripalani, MD, MSc, SFHM, chief of the section of hospital medicine and an associate professor of medicine at Vanderbilt University Medical Center in Nashville, Tenn., says communication is now a primary focal point in Medicare’s new hospital value-based purchasing program (VBP). Within VBP’s Hospital Consumer Assessment of Healthcare Providers and Systems (HCAHPS) component, worth 30% of a hospital’s sum score, four of the 10 survey-based measures deal directly with communication. Patients’ overall rating and recommendation of hospitals likely will reflect their satisfaction with communication as well. Dr. Kripalani says it’s inevitable that hospitals—and hospitalists—will pay more attention to communication ratings as patients become judges of quality.
The expertise of hospitalists in handling challenging patients also leads to improved quality over time, says Shai Gavi, DO, MPH, chief of the section of hospital medicine and assistant professor of clinical medicine at Stony Brook University School of Medicine in Brookhaven, N.Y. Hospitalists, he says, excel in handling such high-stakes medical issues as gastrointestinal bleeding, pancreatitis, sepsis, and pain management that can quickly impact patient outcomes if not addressed properly and proficiently. "I think there’s significant value to having people who do this on a pretty frequent basis," he says.
And because of their broad day-to-day interactions, Dr. Gavi says, hospitalists are natural choices for committees focused on improving quality. "When we sit on committees, people often look to us for answers and directions because they know we’re on the front lines and we’ve interfaced with all of the services in the hospital," he says. "You have a good view of the whole hospital operation from A to Z, and I think that’s pretty unique to hospitalists."
The Verdict
In a recent issue brief by Lisa Sprague, principal policy analyst at the National Health Policy Forum, she asserts, "Hospitalists have the undeniable advantage of being there when a crisis occurs, when a patient is ready for discharge, and so on."12
So is "being there" the defining concept of hospital medicine, as she subsequently suggests?
Based on both scientific and anecdotal evidence, the contribution of hospitalists to healthcare quality might be better summarized as "being involved." Whether as innovators, navigators, physician champions, the "sweet spot" of interdepartmental partnerships, the "glue" of multidisciplinary teams, or the nuclei of performance committees, hospitalists are increasingly described as being in the middle of efforts to improve quality. On this basis, the discipline appears to be living up to expectations, though experts say more research is needed to better assess the impacts of HM on quality.
Dr. Vaidyan says hospitalists are particularly well positioned to understand what constitutes ideal care from the perspective of patients. "They want to be treated well: That’s patient satisfaction," he says. "They want to have their chief complaint—why they came to the hospital—properly addressed, so you need a coordinated care team. They want to go home early and don’t want come back: That’s low length of stay and a reduction in 30-day readmissions. And they don’t want any hospital-acquired complications."
Treating patients better, then, should be reflected by improved quality, even if the participation of hospitalists cannot be precisely quantified. "Being involved is something that may be difficult to measure," Dr. Gavi says, "but nonetheless, it has an important impact." TH
Bryn Nelson is a medical writer based in Seattle.
References
- Pronovost PJ, Lilford R. Analysis & commentary: A roadmap for improving the performance of performance measures. Health Aff (Millwood). 2011;30(4):569-73.
- López L, Hicks LS, Cohen AP, McKean S, Weissman JS. Hospitalists and the quality of care in hospitals. Arch Intern Med. 2009;169(15):1389-1394.
- Centor RM, Taylor BB. Do hospitalists improve quality? Arch Intern Med. 2009;169(15):1351-1352.
- Boyte D, Verma L, Wightman M. A multidisciplinary approach to reducing heart failure readmissions. J Hosp Med. 2011;6(4)Supp 2:S14.
- Williams MV, Hansen L, Greenwald J, Howell E, et al. BOOST: impact of a quality improvement project to reduce rehospitalizations. J Hosp Med. 2011;6(4) Supp 2:S88. BOOST: impact of a quality improvement project to reduce rehospitalizations.
- Auerbach AD, Wachter RM, Katz P, Showstack J, Baron RB, Goldman L. Implementation of a voluntary hospitalist service at a community teaching hospital: improved clinical efficiency and patient outcomes. Ann Intern Med. 2002;137(11):859-865.
- Meltzer D, Manning WG, Morrison J, et al. Effects of physician experience on costs and outcomes on an academic general medicine service: results of a trial of hospitalists. Ann Intern Med. 2002;137(1):866-874.
- Huddleston JM, Hall K, Naessens JM, et al. Medical and surgical comanagement after elective hip and knee arthroplasty. Ann Intern Med. 2004;141(1):28-38.
- Batsis JA, Phy MP, Melton LJ, et al. Effects of a hospitalist care model on mortality of elderly patients with hip fractures. J Hosp Med. 2007;2(4): 219–225.
- Lindenauer PK, Rothberg MB, Pekow PS, et al. Outcomes of care by hospitalists, general internists, and family physicians. N Eng J Med. 2007;357:2589-2600.
- Hock Lee K, Yang Y, Soong Yang K, Chi Ong B, Seong Ng H. Bringing generalists into the hospital: outcomes of a family medicine hospitalist model in Singapore. J Hosp Med. 2011;6(3):115-121.
- Sprague L. The hospitalist: better value in inpatient care? National Health Policy Forum website. Available at: www.nhpf.org/library/issue-briefs/IB842_Hospitalist_03-30-11.pdf. Accessed June 28, 2011.
One hospitalist-led pilot project produced a 61% decrease in heart failure readmission rates. Another resulted in a 33% drop in all-cause readmissions. The numbers might be impressive, but what do they really say about how hospitalists have influenced healthcare quality?
When HM emerged 15 years ago, advocates pitched the fledgling physician specialty as a model of efficient inpatient care, and subsequent findings that the concept led to reductions in length of stay encouraged more hospitals to bolster their staff with the newcomers. With a rising emphasis on quality and patient safety over the past decade, and the new era of pay-for-performance, the hospitalist model of care has expanded to embrace improved quality of care as a chief selling point.
Measuring quality is no easy task, however, and researchers still debate the relative merits of metrics like 30-day readmission rates and inpatient mortality. "Without question, quality measurement is an imperfect science, and all measures will contain some level of imprecision and bias," concluded a recent commentary in Health Affairs.1
Against that backdrop, relatively few studies have looked broadly at the contributions of hospital medicine. Most interventions have been individually tailored to a hospital or instituted at only a few sites, precluding large-scale, head-to-head comparisons.
And so the question remains: Has hospital medicine lived up to its promise on quality?
The Evidence
In one of the few national surveys of HM’s impact on patient care, a yearlong comparison of more than 3,600 hospitals found that the roughly 40% that employed hospitalists scored better on multiple Hospital Quality Alliance indicators. The 2009 Archives of Internal Medicine study suggested that hospitals with hospitalists outperformed their counterparts in quality metrics for acute myocardial infarction, pneumonia, overall disease treatment and diagnosis, and counseling and prevention. Congestive heart failure was the only category of the five reviewed that lacked a statistically significant difference.2
A separate editorial, however, argued that the study’s data were not persuasive enough to support the conclusion that hospitalists bring a higher quality of care to the table.3 And even less can be said about the national impact of HM on newly elevated metrics, such as readmission rates. The obligation to gather evidence, in fact, is largely falling upon hospitalists themselves, and the multitude of research abstracts from SHM’s annual meeting in May suggests that plenty of physician scientists are taking the responsibility seriously. Among the presentations, a study led by David Boyte, MD, assistant professor of medicine at Duke University and a hospitalist at Durham Regional Hospital, found that a multidisciplinary approach greatly improved one hospital unit’s 30-day readmission rates for heart failure patients. After a three-month pilot in the cardiac nursing unit, readmission rates fell to 10.7% from 27.6%.4
Although the multidisciplinary effort has included doctors, nurses, nutritionists, pharmacists, unit managers, and other personnel, Dr. Boyte says the involvement of hospitalists has been key to the project’s success. "We feel like we were the main participants who could see the whole picture from a patient-centered perspective," he says. "We were the glue; we were the center node of all the healthcare providers." Based on that dramatic improvement, Dr. Boyte says, the same interventional protocol has been rolled out in three other medical surgical units, and the hospital is using a similar approach to address AMI readmission rates.
SHM’s Project BOOST (Better Outcomes for Older Adults through Safe Transitions; www.hospitalmedicine.org/boost )—by far the largest study of how HM is impacting readmission rates—has amassed data from more than 20 hospitals, with more expected from a growing roster of participants. So far, however, the project has only released data from six pilot sites describing the six-month periods before and after the project’s start. Among those sites, initial results suggest that readmission rates fell by an average of more than 20%, to 11.2% from 14.2%.5
Though the early numbers are encouraging, experts say rates from a larger group of participants at the one-year mark will be more telling, as will direct comparisons between BOOST units and nonparticipating counterparts at the same hospitals. Principal investigator Mark Williams, MD, FHM, professor and chief of the division of hospital medicine at the Northwestern University Feinberg School of Medicine in Chicago, says researchers still need to clean up that data before they’re ready to share it publicly.
In the meantime, some individual BOOST case studies are suggesting that hospitalist-led changes could pay big dividends. To help create cohesiveness and a sense of ownership within its HM program, St. Mary’s Health Center in St. Louis started a 20-bed hospitalist unit in 2008. Philip Vaidyan, MD, FACP, head of the hospitalist program and practice group leader for IPC: The Hospitalist Company at St. Mary’s, says one unit, 3 West, has since functioned as a lab for testing new ideas that are then introduced hospitalwide.
One early change was to bring all of the unit’s care providers together, from doctors and nurses to the unit-based case manager and social worker, for 9 a.m. handoff meetings. "We have this collective brain to find unique solutions," Dr. Vaidyan says. After seeing positive trends on length of stay, 30-day readmission rates, and patient satisfaction scores, St. Mary’s upgraded to a 32-bed hospitalist unit in early 2009. That same year, the 525-bed community teaching hospital was accepted into the BOOST program.
The hospitalist unit’s improved quality scores continued under BOOST, leading to a 33% reduction in readmission rates from 2008 to 2010 (to 10.5% from 15.7%). Rates for a nonhospitalist unit, by contrast, hovered around 17%. "For reducing readmissions, people may think that you have to have a higher length of stay," Dr. Vaidyan says. But the unit trended toward a lower length of stay, in addition to its reduced 30-day readmissions and improved patient satisfaction scores.
Flush with success, the 10 physicians and four nurse practitioners in the hospitalist program have since begun spreading their best practices to the rest of the hospital units. "Hospitalists are in the best ‘sweet spot,’ " Dr. Vaidyan says, "partnering with all of the disciplines, bringing them together, and keeping everybody on the same page."
Ironically, pinpointing the contribution of hospitalists is harder when their changes produce an ecological effect throughout an entire institution, says Siddhartha Singh, MD, MS, associate chief medical officer of Medical College Physicians, the adult practice for Medical College of Wisconsin in Milwaukee. Even so, he stresses that the impact of the two dozen hospitalists at Medical College Physicians has been felt.
"Coinciding with and following the introduction of our hospitalist program in 2004, we have noticed dramatic decreases in our length of stay throughout medicine services," he says. The same has held true for inpatient mortality. "And that, we feel, is attributable to the standardization of processes introduced by the hospitalist group." Multidisciplinary rounds; whiteboards in patient rooms; and standardized admission orders, prophylactic treatments, and discharge processes—"all of this would’ve been impossible, absolutely impossible, without the hospitalist," he says.
Over the past decade, Dr. Singh’s assessment has been echoed by several studies suggesting that individual hospitalist programs have brought significant improvements in quality measures, such as complication rates and inpatient mortality. In 2002, for example, Andrew Auerbach, MD, MPH, at the University of California San Francisco Medical Center, led a study that compared HM care with that of community physicians in a community-based teaching hospital. Patients cared for by hospitalists, the study found, had a lower risk of death during the hospitalization, as well as at 30 days and 60 days after discharge.6
A separate report by David Meltzer, MD, PhD, and colleagues at the University of Chicago found that an HM program in an academic general medicine service led to a 30% reduction in 30-day mortality rates during its second year of operation.7 And a 2004 study led by Jeanne Huddleston, MD, at the Mayo Clinic College of Medicine in Rochester, Minn., found that a hospitalist-orthopedic co-management model (versus care by orthopedic surgeons with medical consultation) led to more patients being discharged with no complications after elective hip or knee surgery.8 Hospitalist co-management also reduced the rate of minor complications, but had no effect on actual length of stay or cost.
A subsequent study by the same group, however, documented improved efficiency of care through the HM model, but no effect on the mortality of hip fracture patients up to one year after discharge.9 Multiple studies of hospitalist programs, in fact, have seen increased efficiency but little or no impact on inpatient mortality, leading researchers to broadly conclude that such programs can decrease resource use without compromising quality.
In 2007, a retrospective study of nearly 77,000 patients admitted to 45 hospitals with one of seven common diagnoses compared the care delivered by hospitalists, general internists, and family physicians.10 Although the study authors found that hospitalist care yielded a small drop in length of stay, they saw no difference in the inpatient mortality rates or 14-day readmission rates. More recently, mortality has become ensnared in controversy over its reliability as an accurate indicator of quality.

-Shai Gavi, DO, MPH, chief, section of hospital medicine, assistant professor, Stony Brook University School of Medicine, Brookhaven, N.Y.
Half of the Equation
Despite a lack of ideal metrics, another promising sign for HM might be the model’s exportability. Lee Kheng Hock, MMed, senior consultant and head of the Department of Family Medicine and Continuing Care at Singapore General Hospital, says the 1,600-bed hospital began experimenting with the hospitalist model when officials realized the existing care system wasn’t sustainable. Amid an aging population and increasingly complex and fragmented care, Hock views the hospitalist movement as a natural evolution of the healthcare system to meet the needs of a changing environment.
In a recent study, Hock and his colleagues used the hospital’s administrative database to examine the resource use and outcomes of patients cared for in 2008 by family medicine hospitalists or by specialists.11 The comparison, based on several standard metrics, found no significant improvements in quality, with similar inpatient mortality rates and 30-day, all-cause, unscheduled readmission rates regardless of the care delivery method. The study, though, revealed a significantly shorter hospital stay (4.4 days vs. 5.3 days) and lower costs per patient for those cared for by hospitalists ($2,250 vs. $2,500).11
Hock points out that, like his study, most analyses of hospitalist programs have shown an improvement in length of stay and cost of care without any increase in mortality and morbidity. If value equals quality divided by cost, he says, it stands to reason that quality must increase as overall value remains the same but costs decrease.
"The main difference is that the patients received undivided attention from a well-rounded generalist physician who is focused on providing holistic general medical care," Hock says, adding that "it is really a no-brainer that the outcome would be different."
Patients Rule
Other measures like the effectiveness of communication and seamlessness of handoffs often are assessed through their impacts on patient outcomes. But Sunil Kripalani, MD, MSc, SFHM, chief of the section of hospital medicine and an associate professor of medicine at Vanderbilt University Medical Center in Nashville, Tenn., says communication is now a primary focal point in Medicare’s new hospital value-based purchasing program (VBP). Within VBP’s Hospital Consumer Assessment of Healthcare Providers and Systems (HCAHPS) component, worth 30% of a hospital’s sum score, four of the 10 survey-based measures deal directly with communication. Patients’ overall rating and recommendation of hospitals likely will reflect their satisfaction with communication as well. Dr. Kripalani says it’s inevitable that hospitals—and hospitalists—will pay more attention to communication ratings as patients become judges of quality.
The expertise of hospitalists in handling challenging patients also leads to improved quality over time, says Shai Gavi, DO, MPH, chief of the section of hospital medicine and assistant professor of clinical medicine at Stony Brook University School of Medicine in Brookhaven, N.Y. Hospitalists, he says, excel in handling such high-stakes medical issues as gastrointestinal bleeding, pancreatitis, sepsis, and pain management that can quickly impact patient outcomes if not addressed properly and proficiently. "I think there’s significant value to having people who do this on a pretty frequent basis," he says.
And because of their broad day-to-day interactions, Dr. Gavi says, hospitalists are natural choices for committees focused on improving quality. "When we sit on committees, people often look to us for answers and directions because they know we’re on the front lines and we’ve interfaced with all of the services in the hospital," he says. "You have a good view of the whole hospital operation from A to Z, and I think that’s pretty unique to hospitalists."
The Verdict
In a recent issue brief by Lisa Sprague, principal policy analyst at the National Health Policy Forum, she asserts, "Hospitalists have the undeniable advantage of being there when a crisis occurs, when a patient is ready for discharge, and so on."12
So is "being there" the defining concept of hospital medicine, as she subsequently suggests?
Based on both scientific and anecdotal evidence, the contribution of hospitalists to healthcare quality might be better summarized as "being involved." Whether as innovators, navigators, physician champions, the "sweet spot" of interdepartmental partnerships, the "glue" of multidisciplinary teams, or the nuclei of performance committees, hospitalists are increasingly described as being in the middle of efforts to improve quality. On this basis, the discipline appears to be living up to expectations, though experts say more research is needed to better assess the impacts of HM on quality.
Dr. Vaidyan says hospitalists are particularly well positioned to understand what constitutes ideal care from the perspective of patients. "They want to be treated well: That’s patient satisfaction," he says. "They want to have their chief complaint—why they came to the hospital—properly addressed, so you need a coordinated care team. They want to go home early and don’t want come back: That’s low length of stay and a reduction in 30-day readmissions. And they don’t want any hospital-acquired complications."
Treating patients better, then, should be reflected by improved quality, even if the participation of hospitalists cannot be precisely quantified. "Being involved is something that may be difficult to measure," Dr. Gavi says, "but nonetheless, it has an important impact." TH
Bryn Nelson is a medical writer based in Seattle.
References
- Pronovost PJ, Lilford R. Analysis & commentary: A roadmap for improving the performance of performance measures. Health Aff (Millwood). 2011;30(4):569-73.
- López L, Hicks LS, Cohen AP, McKean S, Weissman JS. Hospitalists and the quality of care in hospitals. Arch Intern Med. 2009;169(15):1389-1394.
- Centor RM, Taylor BB. Do hospitalists improve quality? Arch Intern Med. 2009;169(15):1351-1352.
- Boyte D, Verma L, Wightman M. A multidisciplinary approach to reducing heart failure readmissions. J Hosp Med. 2011;6(4)Supp 2:S14.
- Williams MV, Hansen L, Greenwald J, Howell E, et al. BOOST: impact of a quality improvement project to reduce rehospitalizations. J Hosp Med. 2011;6(4) Supp 2:S88. BOOST: impact of a quality improvement project to reduce rehospitalizations.
- Auerbach AD, Wachter RM, Katz P, Showstack J, Baron RB, Goldman L. Implementation of a voluntary hospitalist service at a community teaching hospital: improved clinical efficiency and patient outcomes. Ann Intern Med. 2002;137(11):859-865.
- Meltzer D, Manning WG, Morrison J, et al. Effects of physician experience on costs and outcomes on an academic general medicine service: results of a trial of hospitalists. Ann Intern Med. 2002;137(1):866-874.
- Huddleston JM, Hall K, Naessens JM, et al. Medical and surgical comanagement after elective hip and knee arthroplasty. Ann Intern Med. 2004;141(1):28-38.
- Batsis JA, Phy MP, Melton LJ, et al. Effects of a hospitalist care model on mortality of elderly patients with hip fractures. J Hosp Med. 2007;2(4): 219–225.
- Lindenauer PK, Rothberg MB, Pekow PS, et al. Outcomes of care by hospitalists, general internists, and family physicians. N Eng J Med. 2007;357:2589-2600.
- Hock Lee K, Yang Y, Soong Yang K, Chi Ong B, Seong Ng H. Bringing generalists into the hospital: outcomes of a family medicine hospitalist model in Singapore. J Hosp Med. 2011;6(3):115-121.
- Sprague L. The hospitalist: better value in inpatient care? National Health Policy Forum website. Available at: www.nhpf.org/library/issue-briefs/IB842_Hospitalist_03-30-11.pdf. Accessed June 28, 2011.
One hospitalist-led pilot project produced a 61% decrease in heart failure readmission rates. Another resulted in a 33% drop in all-cause readmissions. The numbers might be impressive, but what do they really say about how hospitalists have influenced healthcare quality?
When HM emerged 15 years ago, advocates pitched the fledgling physician specialty as a model of efficient inpatient care, and subsequent findings that the concept led to reductions in length of stay encouraged more hospitals to bolster their staff with the newcomers. With a rising emphasis on quality and patient safety over the past decade, and the new era of pay-for-performance, the hospitalist model of care has expanded to embrace improved quality of care as a chief selling point.
Measuring quality is no easy task, however, and researchers still debate the relative merits of metrics like 30-day readmission rates and inpatient mortality. "Without question, quality measurement is an imperfect science, and all measures will contain some level of imprecision and bias," concluded a recent commentary in Health Affairs.1
Against that backdrop, relatively few studies have looked broadly at the contributions of hospital medicine. Most interventions have been individually tailored to a hospital or instituted at only a few sites, precluding large-scale, head-to-head comparisons.
And so the question remains: Has hospital medicine lived up to its promise on quality?
The Evidence
In one of the few national surveys of HM’s impact on patient care, a yearlong comparison of more than 3,600 hospitals found that the roughly 40% that employed hospitalists scored better on multiple Hospital Quality Alliance indicators. The 2009 Archives of Internal Medicine study suggested that hospitals with hospitalists outperformed their counterparts in quality metrics for acute myocardial infarction, pneumonia, overall disease treatment and diagnosis, and counseling and prevention. Congestive heart failure was the only category of the five reviewed that lacked a statistically significant difference.2
A separate editorial, however, argued that the study’s data were not persuasive enough to support the conclusion that hospitalists bring a higher quality of care to the table.3 And even less can be said about the national impact of HM on newly elevated metrics, such as readmission rates. The obligation to gather evidence, in fact, is largely falling upon hospitalists themselves, and the multitude of research abstracts from SHM’s annual meeting in May suggests that plenty of physician scientists are taking the responsibility seriously. Among the presentations, a study led by David Boyte, MD, assistant professor of medicine at Duke University and a hospitalist at Durham Regional Hospital, found that a multidisciplinary approach greatly improved one hospital unit’s 30-day readmission rates for heart failure patients. After a three-month pilot in the cardiac nursing unit, readmission rates fell to 10.7% from 27.6%.4
Although the multidisciplinary effort has included doctors, nurses, nutritionists, pharmacists, unit managers, and other personnel, Dr. Boyte says the involvement of hospitalists has been key to the project’s success. "We feel like we were the main participants who could see the whole picture from a patient-centered perspective," he says. "We were the glue; we were the center node of all the healthcare providers." Based on that dramatic improvement, Dr. Boyte says, the same interventional protocol has been rolled out in three other medical surgical units, and the hospital is using a similar approach to address AMI readmission rates.
SHM’s Project BOOST (Better Outcomes for Older Adults through Safe Transitions; www.hospitalmedicine.org/boost )—by far the largest study of how HM is impacting readmission rates—has amassed data from more than 20 hospitals, with more expected from a growing roster of participants. So far, however, the project has only released data from six pilot sites describing the six-month periods before and after the project’s start. Among those sites, initial results suggest that readmission rates fell by an average of more than 20%, to 11.2% from 14.2%.5
Though the early numbers are encouraging, experts say rates from a larger group of participants at the one-year mark will be more telling, as will direct comparisons between BOOST units and nonparticipating counterparts at the same hospitals. Principal investigator Mark Williams, MD, FHM, professor and chief of the division of hospital medicine at the Northwestern University Feinberg School of Medicine in Chicago, says researchers still need to clean up that data before they’re ready to share it publicly.
In the meantime, some individual BOOST case studies are suggesting that hospitalist-led changes could pay big dividends. To help create cohesiveness and a sense of ownership within its HM program, St. Mary’s Health Center in St. Louis started a 20-bed hospitalist unit in 2008. Philip Vaidyan, MD, FACP, head of the hospitalist program and practice group leader for IPC: The Hospitalist Company at St. Mary’s, says one unit, 3 West, has since functioned as a lab for testing new ideas that are then introduced hospitalwide.
One early change was to bring all of the unit’s care providers together, from doctors and nurses to the unit-based case manager and social worker, for 9 a.m. handoff meetings. "We have this collective brain to find unique solutions," Dr. Vaidyan says. After seeing positive trends on length of stay, 30-day readmission rates, and patient satisfaction scores, St. Mary’s upgraded to a 32-bed hospitalist unit in early 2009. That same year, the 525-bed community teaching hospital was accepted into the BOOST program.
The hospitalist unit’s improved quality scores continued under BOOST, leading to a 33% reduction in readmission rates from 2008 to 2010 (to 10.5% from 15.7%). Rates for a nonhospitalist unit, by contrast, hovered around 17%. "For reducing readmissions, people may think that you have to have a higher length of stay," Dr. Vaidyan says. But the unit trended toward a lower length of stay, in addition to its reduced 30-day readmissions and improved patient satisfaction scores.
Flush with success, the 10 physicians and four nurse practitioners in the hospitalist program have since begun spreading their best practices to the rest of the hospital units. "Hospitalists are in the best ‘sweet spot,’ " Dr. Vaidyan says, "partnering with all of the disciplines, bringing them together, and keeping everybody on the same page."
Ironically, pinpointing the contribution of hospitalists is harder when their changes produce an ecological effect throughout an entire institution, says Siddhartha Singh, MD, MS, associate chief medical officer of Medical College Physicians, the adult practice for Medical College of Wisconsin in Milwaukee. Even so, he stresses that the impact of the two dozen hospitalists at Medical College Physicians has been felt.
"Coinciding with and following the introduction of our hospitalist program in 2004, we have noticed dramatic decreases in our length of stay throughout medicine services," he says. The same has held true for inpatient mortality. "And that, we feel, is attributable to the standardization of processes introduced by the hospitalist group." Multidisciplinary rounds; whiteboards in patient rooms; and standardized admission orders, prophylactic treatments, and discharge processes—"all of this would’ve been impossible, absolutely impossible, without the hospitalist," he says.
Over the past decade, Dr. Singh’s assessment has been echoed by several studies suggesting that individual hospitalist programs have brought significant improvements in quality measures, such as complication rates and inpatient mortality. In 2002, for example, Andrew Auerbach, MD, MPH, at the University of California San Francisco Medical Center, led a study that compared HM care with that of community physicians in a community-based teaching hospital. Patients cared for by hospitalists, the study found, had a lower risk of death during the hospitalization, as well as at 30 days and 60 days after discharge.6
A separate report by David Meltzer, MD, PhD, and colleagues at the University of Chicago found that an HM program in an academic general medicine service led to a 30% reduction in 30-day mortality rates during its second year of operation.7 And a 2004 study led by Jeanne Huddleston, MD, at the Mayo Clinic College of Medicine in Rochester, Minn., found that a hospitalist-orthopedic co-management model (versus care by orthopedic surgeons with medical consultation) led to more patients being discharged with no complications after elective hip or knee surgery.8 Hospitalist co-management also reduced the rate of minor complications, but had no effect on actual length of stay or cost.
A subsequent study by the same group, however, documented improved efficiency of care through the HM model, but no effect on the mortality of hip fracture patients up to one year after discharge.9 Multiple studies of hospitalist programs, in fact, have seen increased efficiency but little or no impact on inpatient mortality, leading researchers to broadly conclude that such programs can decrease resource use without compromising quality.
In 2007, a retrospective study of nearly 77,000 patients admitted to 45 hospitals with one of seven common diagnoses compared the care delivered by hospitalists, general internists, and family physicians.10 Although the study authors found that hospitalist care yielded a small drop in length of stay, they saw no difference in the inpatient mortality rates or 14-day readmission rates. More recently, mortality has become ensnared in controversy over its reliability as an accurate indicator of quality.

-Shai Gavi, DO, MPH, chief, section of hospital medicine, assistant professor, Stony Brook University School of Medicine, Brookhaven, N.Y.
Half of the Equation
Despite a lack of ideal metrics, another promising sign for HM might be the model’s exportability. Lee Kheng Hock, MMed, senior consultant and head of the Department of Family Medicine and Continuing Care at Singapore General Hospital, says the 1,600-bed hospital began experimenting with the hospitalist model when officials realized the existing care system wasn’t sustainable. Amid an aging population and increasingly complex and fragmented care, Hock views the hospitalist movement as a natural evolution of the healthcare system to meet the needs of a changing environment.
In a recent study, Hock and his colleagues used the hospital’s administrative database to examine the resource use and outcomes of patients cared for in 2008 by family medicine hospitalists or by specialists.11 The comparison, based on several standard metrics, found no significant improvements in quality, with similar inpatient mortality rates and 30-day, all-cause, unscheduled readmission rates regardless of the care delivery method. The study, though, revealed a significantly shorter hospital stay (4.4 days vs. 5.3 days) and lower costs per patient for those cared for by hospitalists ($2,250 vs. $2,500).11
Hock points out that, like his study, most analyses of hospitalist programs have shown an improvement in length of stay and cost of care without any increase in mortality and morbidity. If value equals quality divided by cost, he says, it stands to reason that quality must increase as overall value remains the same but costs decrease.
"The main difference is that the patients received undivided attention from a well-rounded generalist physician who is focused on providing holistic general medical care," Hock says, adding that "it is really a no-brainer that the outcome would be different."
Patients Rule
Other measures like the effectiveness of communication and seamlessness of handoffs often are assessed through their impacts on patient outcomes. But Sunil Kripalani, MD, MSc, SFHM, chief of the section of hospital medicine and an associate professor of medicine at Vanderbilt University Medical Center in Nashville, Tenn., says communication is now a primary focal point in Medicare’s new hospital value-based purchasing program (VBP). Within VBP’s Hospital Consumer Assessment of Healthcare Providers and Systems (HCAHPS) component, worth 30% of a hospital’s sum score, four of the 10 survey-based measures deal directly with communication. Patients’ overall rating and recommendation of hospitals likely will reflect their satisfaction with communication as well. Dr. Kripalani says it’s inevitable that hospitals—and hospitalists—will pay more attention to communication ratings as patients become judges of quality.
The expertise of hospitalists in handling challenging patients also leads to improved quality over time, says Shai Gavi, DO, MPH, chief of the section of hospital medicine and assistant professor of clinical medicine at Stony Brook University School of Medicine in Brookhaven, N.Y. Hospitalists, he says, excel in handling such high-stakes medical issues as gastrointestinal bleeding, pancreatitis, sepsis, and pain management that can quickly impact patient outcomes if not addressed properly and proficiently. "I think there’s significant value to having people who do this on a pretty frequent basis," he says.
And because of their broad day-to-day interactions, Dr. Gavi says, hospitalists are natural choices for committees focused on improving quality. "When we sit on committees, people often look to us for answers and directions because they know we’re on the front lines and we’ve interfaced with all of the services in the hospital," he says. "You have a good view of the whole hospital operation from A to Z, and I think that’s pretty unique to hospitalists."
The Verdict
In a recent issue brief by Lisa Sprague, principal policy analyst at the National Health Policy Forum, she asserts, "Hospitalists have the undeniable advantage of being there when a crisis occurs, when a patient is ready for discharge, and so on."12
So is "being there" the defining concept of hospital medicine, as she subsequently suggests?
Based on both scientific and anecdotal evidence, the contribution of hospitalists to healthcare quality might be better summarized as "being involved." Whether as innovators, navigators, physician champions, the "sweet spot" of interdepartmental partnerships, the "glue" of multidisciplinary teams, or the nuclei of performance committees, hospitalists are increasingly described as being in the middle of efforts to improve quality. On this basis, the discipline appears to be living up to expectations, though experts say more research is needed to better assess the impacts of HM on quality.
Dr. Vaidyan says hospitalists are particularly well positioned to understand what constitutes ideal care from the perspective of patients. "They want to be treated well: That’s patient satisfaction," he says. "They want to have their chief complaint—why they came to the hospital—properly addressed, so you need a coordinated care team. They want to go home early and don’t want come back: That’s low length of stay and a reduction in 30-day readmissions. And they don’t want any hospital-acquired complications."
Treating patients better, then, should be reflected by improved quality, even if the participation of hospitalists cannot be precisely quantified. "Being involved is something that may be difficult to measure," Dr. Gavi says, "but nonetheless, it has an important impact." TH
Bryn Nelson is a medical writer based in Seattle.
References
- Pronovost PJ, Lilford R. Analysis & commentary: A roadmap for improving the performance of performance measures. Health Aff (Millwood). 2011;30(4):569-73.
- López L, Hicks LS, Cohen AP, McKean S, Weissman JS. Hospitalists and the quality of care in hospitals. Arch Intern Med. 2009;169(15):1389-1394.
- Centor RM, Taylor BB. Do hospitalists improve quality? Arch Intern Med. 2009;169(15):1351-1352.
- Boyte D, Verma L, Wightman M. A multidisciplinary approach to reducing heart failure readmissions. J Hosp Med. 2011;6(4)Supp 2:S14.
- Williams MV, Hansen L, Greenwald J, Howell E, et al. BOOST: impact of a quality improvement project to reduce rehospitalizations. J Hosp Med. 2011;6(4) Supp 2:S88. BOOST: impact of a quality improvement project to reduce rehospitalizations.
- Auerbach AD, Wachter RM, Katz P, Showstack J, Baron RB, Goldman L. Implementation of a voluntary hospitalist service at a community teaching hospital: improved clinical efficiency and patient outcomes. Ann Intern Med. 2002;137(11):859-865.
- Meltzer D, Manning WG, Morrison J, et al. Effects of physician experience on costs and outcomes on an academic general medicine service: results of a trial of hospitalists. Ann Intern Med. 2002;137(1):866-874.
- Huddleston JM, Hall K, Naessens JM, et al. Medical and surgical comanagement after elective hip and knee arthroplasty. Ann Intern Med. 2004;141(1):28-38.
- Batsis JA, Phy MP, Melton LJ, et al. Effects of a hospitalist care model on mortality of elderly patients with hip fractures. J Hosp Med. 2007;2(4): 219–225.
- Lindenauer PK, Rothberg MB, Pekow PS, et al. Outcomes of care by hospitalists, general internists, and family physicians. N Eng J Med. 2007;357:2589-2600.
- Hock Lee K, Yang Y, Soong Yang K, Chi Ong B, Seong Ng H. Bringing generalists into the hospital: outcomes of a family medicine hospitalist model in Singapore. J Hosp Med. 2011;6(3):115-121.
- Sprague L. The hospitalist: better value in inpatient care? National Health Policy Forum website. Available at: www.nhpf.org/library/issue-briefs/IB842_Hospitalist_03-30-11.pdf. Accessed June 28, 2011.
It Takes a Village
Gregory Misky, MD, has been a hospitalist for 12 years, first at a community hospital and for the past seven years at the University of Colorado Denver. In recent years, his frustration has grown over the challenges of discharge planning, care transitions, and preventing readmissions for vulnerable, disadvantaged patients, including the uninsured, underinsured, and medically indigent.
“There’s a big elephant in the room that we’re not talking about, and that elephant is having babies,” he says. “Access is such a big problem for these patients and, as a hospitalist, it’s just not OK to me anymore. I need to be proactive about finding solutions.”
Dr. Misky’s concerns led him to do research with mentor Eric Coleman, MD, the university’s creator of the Care Transitions Program (www.caretransitions.org), studying patients who lacked primary-care physicians (PCPs) or timely PCP follow-up, and their resulting higher rates of readmissions.1 Dr. Misky also helped develop care pathways, including post-discharge care, for VTE patients, a “common, costly, and dangerous” condition. He is working with a hospitalist colleague to explore how electronic health records (EHR) might be used to help trigger post-discharge follow-up for at-risk patients.
University of Colorado Hospital (UCH), a 425-bed urban academic tertiary-care center, is not the designated safety net hospital for metro Denver, yet 28% to 32% of patients discharged from its medical services are uninsured, Dr. Misky says. He finds that academic physicians at UCH are not always able to take on large numbers of uninsured patients in their clinics, given the productivity demands they face, while the hospital has not been able to participate in systemwide, comprehensive national models for improving care transitions, such as SHM’s Project BOOST (www.hospitalmedicine.org/boost) or Boston Medical Center’s Project RED (www.bu.edu/fammed/projectred/).
Dr. Misky is in discussions with local community services, such as the Metro Community Provider Network (MCPN) of clinics for underserved patients, and exploring the development of a collaborative model for integrating post-hospital care between UCH and MCPN. “A lot of our ideas are still very exploratory—trying to get the key providers to the table to talk about what these approaches might look like,” Dr. Misky explains. “I’ve been part of ongoing meetings, and I think similar kinds of conversations are happening at many levels at UCH, but there’s not a unified, consensus approach to care transitions—and that’s a problem. But I’m in the midst of it all, trying to highlight the issues and explore solutions.”
—Patricia Rutherford, RN, MS, vice president, Institute for Healthcare Improvement
Dr. Misky says every hospital-based provider—hospitalist, nurses, social workers—feels the same frustration and worry about the level of care when indigent patients are discharged to the community. Uninsured patients can run into problems post-hospitalization and return to the ED for their primary care because they lack other options, he says. “Without established liaisons to the community clinics,” he notes, “it can take three or four months for a new indigent patient to get seen at one.”
Disproportional Issues of the Uninsured
Hospitalists at San Francisco General Hospital, which is the safety-net provider for the Bay Area, are looking at similar issues, says Jeff Critchfield, MD, division chief of hospital medicine. “What we know about the uninsured is that they have a wealth of other challenges and barriers that they bring to the table,” he says. “First of all, un- and underinsured patients are more likely to have chronic illnesses, to be hospitalized for those illnesses, and then to be rehospitalized after discharge.”
Other issues disproportionally impacting uninsured or indigent patients include low literacy, low healthcare literacy, language barriers, cross-cultural barriers, substance abuse and mental health issues, homelessness or marginal housing, transportation barriers, and “social isolation, which also plagues our population and, I believe, places patients at risk, as does depression,” says Dr. Critchfield’s colleague Michelle Schneidermann, MD.
One-third of San Francisco General’s patients are uninsured and 40% have Medi-Cal (California’s version of Medicaid), which basically means they are underinsured.
“California has 19 safety-net hospitals, with 6% of the state’s inpatient beds but 50% of its uninsured population. So that’s what we do,” Dr. Critchfield says. But almost any hospital or hospitalist will see many of the same issues and problems, just not in the same proportions. “These are patients who can be most frustrating to hospitalists, requiring a disproportionate amount of our time,” he says, adding the greatest difficulty is helping these patients understand and follow post-discharge care plans. But if someone is ill enough to need acute hospitalization and is later discharged back to the street, readmission should not be a surprise. “We’ve done that experiment for many years, and we know how it turns out,” he says.
Dr. Schneidermann serves as medical director of San Francisco General’s medical respite program, a 45-bed emergency shelter that accepts homeless or marginally housed patients in need of follow-up care following discharge from any of the city’s acute-care hospitals. Research has shown that the programs can have a major effect on keeping discharged patients off the street, reducing their rates of rehospitalization by as much as 50%.2,3
“We know that homeless patients have longer lengths of hospital stay because their discharges are fraught with problems,” she says. A homeless patient hospitalized with a blood clot potentially could be kept in the hospital for a week while transitioning from heparin to Coumadin, while similar patients with community support might get discharged in a day.
“We are also fortunate to have a program called Healthy San Francisco,” which isn’t a health insurance program per se but since 2007 has provided access to outpatient, inpatient, and preventive care and medications for indigent patients, Dr. Schneidermann says. Sponsored by the city’s Department of Public Health, it is accessed through 32 medical homes located in both public and private clinics. The hospitalists’ goal is to have a follow-up appointment set with a receiving provider at the time of discharge. “It doesn’t always happen, but that’s the goal,” she explains. “Someone, by name, who has accepted the referral.”
Dr. Critchfield is running a randomized controlled trial of the hospital’s interventions to stem the tide of readmissions in patients 60 and older; many of these patients share the same indigent demographics of the rest of San Francisco General’s caseload, although most patients 65 and older qualify for Medicare. He describes the program as a hybrid of Project RED and Dr. Coleman’s Care Transitions Program, although it targets patients who speak English, Spanish, Cantonese, and Mandarin.
How many Americans are uninsured today is a moving target in the context of healthcare reform and its uncertain future, but the number increased to 53 million in 2007 from 42 million in 1998.4 The number of hospitalizations of uninsured patients also grew to 2.3 million from 1.8 million in the same time period, an increase of 31%, while total hospitalizations were increasing by 13%. A May 2011 research brief from the U.S. Department of Health and Human Services estimates that uncompensated costs of hospital care incurred for uninsured patients total $73 billion per year.5
The homeless in shelters or on the street number about 630,000 on any given evening, and 1.5 million Americans experienced homelessness last year, says Sabrina Edgington, MSSW, program and policy specialist at the National Health Care for the Homeless Council in Nashville, Tenn. That said, 30% of the U.S. homeless have health insurance. Uninsured patients are less likely to receive necessary diagnostic tests and labs while in the hospital, and they face limited access and longer wait times—even in the facilities that are willing to take them.7 Research published in the Journal of Hospital Medicine finds that uninsured or Medicaid patients with three common conditions are more likely to die in the hospital than insured patients.8 A 2008 national sample survey of physicians found that “most U.S. physicians limit their care of medically indigent patients.”9 Other recent research suggests that readmission rates are affected by race and by site of care—with hospitals serving a higher proportion of black patients also having higher readmission rates.10
“This is not a hospital problem—it’s a communitywide problem. So there’s not just a hospital solution; it will take the whole village,” says Patricia Rutherford, RN, MS, vice president of the Institute for Healthcare Improvement (IHI), which sponsors initiatives targeting care transitions.
The major national care-transitions programs that assist hospitals with addressing rehospitalizations all share similar objectives, Rutherford says, and all could be helpful in improving hospitals’ responses to indigent patients. The recognized programs include IHI’s STAAR (State Action on Avoidable Rehospitalizations: www.ihi.org/IHI/Programs), a multistate, multistakeholder quality improvement (QI) program; Project BOOST; Project RED; Dr. Coleman’s Care Transitions Project; the nursing-based Transitional Care Model (www.transitionalcare.info); and the American College of Cardiology’s Hospital to Home (www.cardiosource.org).

—Amy Boutwell, MD, MPP, hospitalist, Newton (Mass.) Wellesley Hospital, president, Collaborative Healthcare Strategies
Most of these “well-established, evidence-based interventions,” including BOOST, will be given preference in applications for grants from the federal Community-Based Care Transitions Program (CCTP). The program recently committed $500 million to support community-based coalitions that include hospitals that are working with community partners to create seamless care transitions. “It’s most important that hospitalists are integrally involved with these care-transition teams—if not leading them,” Rutherford says.
BOOST’s approach is built on a major change-management strategy to reconstruct hospitals’ care transitions and discharge processes from the ground up, says Tina Budnitz, MPH, the project’s director at SHM (see “Discharge Improvement,” p. 7.) “The first thing we do, we literally get out pens and paper and chart what happens before patients get into the hospital and what happens after they are discharged, all of the services that touch them—or should,” she says. “The planning process occurs on many levels, with all of the stakeholders in the community looking at the process map and seeing where people fall off and end up readmitted.”
—Jeff Critchfield, MD, division chief of hospital medicine, San Francisco General Hospital
SHM is planning to launch several new BOOST cohorts for participating hospitals this fall, along with a wider range of technical support, Budnitz says.
The Cross-Setting Team
Research on care transitions for uninsured or indigent patients “is not very robust,” observes Amy Boutwell, MD, MPP, a hospitalist at Newton Wellesley Hospital in Newton, Mass., former director of health policy at IHI and president of Collaborative Healthcare Strategies. “We don’t have the information we need, but there are great opportunities to improve our research base,” she explains.
Dr. Boutwell is a big fan of the “cross-setting team,” which brings together around a conference table professionals who work in different care settings, including the hospital, long-term care, and home-based care. She says it’s her job “to make sure patients are safe upon discharge, but if the community is under-resourced for primary-care physicians, if the patient is uninsured and we can’t find a PCP, the hospitalist and cross-setting team need to say, ‘We just can’t accept that.’ ”
A proper handoff should be done in a way that helps the patient and the physician providing the follow-up care. “But you won’t know what that is unless you ask the people you’re sending patients to how you’re doing,” she explains. “When we routinely review readmitted patients in cross-setting groups, it quickly breaks down the mindset that we in the hospital did everything we could have done to make the discharge successful.”
Dr. Boutwell recommends that hospitalists avoid thinking of these issues in a vacuum, as medical-clinical issues that only doctors can fix. “Because you can’t,” she says. “I would never ask an individual hospitalist to reduce readmissions. It requires a multidisciplinary, all-hands-on-deck approach by the hospital. This is different and more exciting than other quality-improvement efforts.” What’s more, she says, the day is coming—and soon—when failing to manage these readmissions will be a bad business proposition for the hospital (see “Value-Based Purchasing Raises the Stakes,” May 2011, p. 1).
IHI’s STAAR Initiative is working with coalitions of providers in Massachusetts, Michigan, Ohio, and Washington. One of those coalitions, Detroit CARR (Community Action to Reduce Rehospitalizations), convened by MPRO, a Michigan-based quality-improvement organization, is a great example of a cross-continuum team involving five inner-city hospitals, Dr. Boutwell says.
“CARR has really dug deeply into the needs of vulnerable patients in one of America’s most economically challenged communities, with a high proportion of Medicaid, uninsured, and disabled patients” and a shrinking population, she says. Many rehospitalizations are related to socio-economics. “The CARR coalition is meeting with the homeless shelters, the food pantries, and the faith-based agencies,” she says. “They’re really getting at the root of significant issues in their community.”
Nancy Vecchioni, RN, MSN, CPHQ, vice present of Medicare operations at MPRO, says CARR involves more than just healthcare providers; it also brings community agencies together with them to take ownership of the patient. Organizations that a year ago weren’t talking to each other are now meeting regularly to focus on the most vulnerable patients, reviewing cases of rehospitalized homeless patients, and sharing their experiences. Rehospitalized patients are being interviewed, using a prepared script (see Figure 1, p. 34), which allows the patient to tell their story. The information is shared within the coalition.
Each hospital has its own transition team, with post-acute providers, physicians, home health agencies, and community service providers, Vecchioni says. For patients who can’t get in to see a PCP within five days of discharge, some hospitals are opening continuity clinics. Others give patients three- to 30-day supplies of needed medications. “There’s no magic bullet—it’s just a different way of looking at how we do this work,” she adds. “Every day we see new barriers. But we’ve already seen a 5% overall reduction in readmissions. And I think hospitalists can be the champions and leaders of these efforts.”
Hospitalists have to raise the bar for themselves, Dr. Schneidermann says, “doing our best while recognizing we can only do so much. There is a lot we can learn from geriatrics, starting with truly embracing the multidisciplinary team.” If hospitalists feel like they are functioning in isolation, she says, they need to look around. “Are these kinds of interdisciplinary meetings happening? If so, join them. If not, light a fire. Convert your frustrating experiences with patients into action.” TH
Larry Beresford is a freelance medical writer based in California.
References
- Misky GJ, Wald HL, Coleman EA. Post-hospitalization transitions: Examining the effects of timing of primary care provider follow-up. J Hosp Med. 2010;5:392-397.
- Buchanan D, Doblin B, Sai T, Garcia P. The effects of respite care for homeless patients: a cohort study. Am J Public Health. 2006;96:1278-1281.
- Kertesz SG, Posner MA, O’Connell JJ, et al. Post-hospital medical respite care and hospital readmission of homeless persons. J Prev Inter Community. 2009;37:129-142.
- Nagamine M, Stocks C, Merrill C. Trends in uninsured hospital stays, 1998-2007. Health Care Cost & Utilization Project (HCUP) Statistical Brief #88. May 2010.
- U.S. Department of Health and Human Services. ASPE Research Brief. The value of health insurance: few of the uninsured have adequate resources to pay potential hospital bills. May 2011.
- U.S. Department of Housing and Urban Development. The Annual Housing Assessment Report to Congress, 2009.
- Kellerman A, Coleman M. Care without Coverage: Too Little, Too Late. Report by Institute of Medicine, May 2002.
- Hasan O, Orav EJ, Hicks LS. Insurance status and hospital care for myocardial infarction, stroke, and pneumonia. J Hosp Med. 2010;5(8):452-459.
- Chirayath HT, Wentworth AL. Constraints to caring: Service to medically indigent patients by allopathic and osteopathic physicians. J Health Care Poor Underserved. 2008;19:500-511.
- Joynt KE, Orav EJ, Jha AK. Thirty-day readmission rates for Medicare beneficiaries by race and site of care. JAMA. 2011;305:675-681.
- Buchanan D, Rohr L, Kehoe L, Glick SB, Jain S. Changing attitudes toward homeless people. J Gen Intern Med. 2004;19(5 Pt 2):566-568.
Gregory Misky, MD, has been a hospitalist for 12 years, first at a community hospital and for the past seven years at the University of Colorado Denver. In recent years, his frustration has grown over the challenges of discharge planning, care transitions, and preventing readmissions for vulnerable, disadvantaged patients, including the uninsured, underinsured, and medically indigent.
“There’s a big elephant in the room that we’re not talking about, and that elephant is having babies,” he says. “Access is such a big problem for these patients and, as a hospitalist, it’s just not OK to me anymore. I need to be proactive about finding solutions.”
Dr. Misky’s concerns led him to do research with mentor Eric Coleman, MD, the university’s creator of the Care Transitions Program (www.caretransitions.org), studying patients who lacked primary-care physicians (PCPs) or timely PCP follow-up, and their resulting higher rates of readmissions.1 Dr. Misky also helped develop care pathways, including post-discharge care, for VTE patients, a “common, costly, and dangerous” condition. He is working with a hospitalist colleague to explore how electronic health records (EHR) might be used to help trigger post-discharge follow-up for at-risk patients.
University of Colorado Hospital (UCH), a 425-bed urban academic tertiary-care center, is not the designated safety net hospital for metro Denver, yet 28% to 32% of patients discharged from its medical services are uninsured, Dr. Misky says. He finds that academic physicians at UCH are not always able to take on large numbers of uninsured patients in their clinics, given the productivity demands they face, while the hospital has not been able to participate in systemwide, comprehensive national models for improving care transitions, such as SHM’s Project BOOST (www.hospitalmedicine.org/boost) or Boston Medical Center’s Project RED (www.bu.edu/fammed/projectred/).
Dr. Misky is in discussions with local community services, such as the Metro Community Provider Network (MCPN) of clinics for underserved patients, and exploring the development of a collaborative model for integrating post-hospital care between UCH and MCPN. “A lot of our ideas are still very exploratory—trying to get the key providers to the table to talk about what these approaches might look like,” Dr. Misky explains. “I’ve been part of ongoing meetings, and I think similar kinds of conversations are happening at many levels at UCH, but there’s not a unified, consensus approach to care transitions—and that’s a problem. But I’m in the midst of it all, trying to highlight the issues and explore solutions.”
—Patricia Rutherford, RN, MS, vice president, Institute for Healthcare Improvement
Dr. Misky says every hospital-based provider—hospitalist, nurses, social workers—feels the same frustration and worry about the level of care when indigent patients are discharged to the community. Uninsured patients can run into problems post-hospitalization and return to the ED for their primary care because they lack other options, he says. “Without established liaisons to the community clinics,” he notes, “it can take three or four months for a new indigent patient to get seen at one.”
Disproportional Issues of the Uninsured
Hospitalists at San Francisco General Hospital, which is the safety-net provider for the Bay Area, are looking at similar issues, says Jeff Critchfield, MD, division chief of hospital medicine. “What we know about the uninsured is that they have a wealth of other challenges and barriers that they bring to the table,” he says. “First of all, un- and underinsured patients are more likely to have chronic illnesses, to be hospitalized for those illnesses, and then to be rehospitalized after discharge.”
Other issues disproportionally impacting uninsured or indigent patients include low literacy, low healthcare literacy, language barriers, cross-cultural barriers, substance abuse and mental health issues, homelessness or marginal housing, transportation barriers, and “social isolation, which also plagues our population and, I believe, places patients at risk, as does depression,” says Dr. Critchfield’s colleague Michelle Schneidermann, MD.
One-third of San Francisco General’s patients are uninsured and 40% have Medi-Cal (California’s version of Medicaid), which basically means they are underinsured.
“California has 19 safety-net hospitals, with 6% of the state’s inpatient beds but 50% of its uninsured population. So that’s what we do,” Dr. Critchfield says. But almost any hospital or hospitalist will see many of the same issues and problems, just not in the same proportions. “These are patients who can be most frustrating to hospitalists, requiring a disproportionate amount of our time,” he says, adding the greatest difficulty is helping these patients understand and follow post-discharge care plans. But if someone is ill enough to need acute hospitalization and is later discharged back to the street, readmission should not be a surprise. “We’ve done that experiment for many years, and we know how it turns out,” he says.
Dr. Schneidermann serves as medical director of San Francisco General’s medical respite program, a 45-bed emergency shelter that accepts homeless or marginally housed patients in need of follow-up care following discharge from any of the city’s acute-care hospitals. Research has shown that the programs can have a major effect on keeping discharged patients off the street, reducing their rates of rehospitalization by as much as 50%.2,3
“We know that homeless patients have longer lengths of hospital stay because their discharges are fraught with problems,” she says. A homeless patient hospitalized with a blood clot potentially could be kept in the hospital for a week while transitioning from heparin to Coumadin, while similar patients with community support might get discharged in a day.
“We are also fortunate to have a program called Healthy San Francisco,” which isn’t a health insurance program per se but since 2007 has provided access to outpatient, inpatient, and preventive care and medications for indigent patients, Dr. Schneidermann says. Sponsored by the city’s Department of Public Health, it is accessed through 32 medical homes located in both public and private clinics. The hospitalists’ goal is to have a follow-up appointment set with a receiving provider at the time of discharge. “It doesn’t always happen, but that’s the goal,” she explains. “Someone, by name, who has accepted the referral.”
Dr. Critchfield is running a randomized controlled trial of the hospital’s interventions to stem the tide of readmissions in patients 60 and older; many of these patients share the same indigent demographics of the rest of San Francisco General’s caseload, although most patients 65 and older qualify for Medicare. He describes the program as a hybrid of Project RED and Dr. Coleman’s Care Transitions Program, although it targets patients who speak English, Spanish, Cantonese, and Mandarin.
How many Americans are uninsured today is a moving target in the context of healthcare reform and its uncertain future, but the number increased to 53 million in 2007 from 42 million in 1998.4 The number of hospitalizations of uninsured patients also grew to 2.3 million from 1.8 million in the same time period, an increase of 31%, while total hospitalizations were increasing by 13%. A May 2011 research brief from the U.S. Department of Health and Human Services estimates that uncompensated costs of hospital care incurred for uninsured patients total $73 billion per year.5
The homeless in shelters or on the street number about 630,000 on any given evening, and 1.5 million Americans experienced homelessness last year, says Sabrina Edgington, MSSW, program and policy specialist at the National Health Care for the Homeless Council in Nashville, Tenn. That said, 30% of the U.S. homeless have health insurance. Uninsured patients are less likely to receive necessary diagnostic tests and labs while in the hospital, and they face limited access and longer wait times—even in the facilities that are willing to take them.7 Research published in the Journal of Hospital Medicine finds that uninsured or Medicaid patients with three common conditions are more likely to die in the hospital than insured patients.8 A 2008 national sample survey of physicians found that “most U.S. physicians limit their care of medically indigent patients.”9 Other recent research suggests that readmission rates are affected by race and by site of care—with hospitals serving a higher proportion of black patients also having higher readmission rates.10
“This is not a hospital problem—it’s a communitywide problem. So there’s not just a hospital solution; it will take the whole village,” says Patricia Rutherford, RN, MS, vice president of the Institute for Healthcare Improvement (IHI), which sponsors initiatives targeting care transitions.
The major national care-transitions programs that assist hospitals with addressing rehospitalizations all share similar objectives, Rutherford says, and all could be helpful in improving hospitals’ responses to indigent patients. The recognized programs include IHI’s STAAR (State Action on Avoidable Rehospitalizations: www.ihi.org/IHI/Programs), a multistate, multistakeholder quality improvement (QI) program; Project BOOST; Project RED; Dr. Coleman’s Care Transitions Project; the nursing-based Transitional Care Model (www.transitionalcare.info); and the American College of Cardiology’s Hospital to Home (www.cardiosource.org).

—Amy Boutwell, MD, MPP, hospitalist, Newton (Mass.) Wellesley Hospital, president, Collaborative Healthcare Strategies
Most of these “well-established, evidence-based interventions,” including BOOST, will be given preference in applications for grants from the federal Community-Based Care Transitions Program (CCTP). The program recently committed $500 million to support community-based coalitions that include hospitals that are working with community partners to create seamless care transitions. “It’s most important that hospitalists are integrally involved with these care-transition teams—if not leading them,” Rutherford says.
BOOST’s approach is built on a major change-management strategy to reconstruct hospitals’ care transitions and discharge processes from the ground up, says Tina Budnitz, MPH, the project’s director at SHM (see “Discharge Improvement,” p. 7.) “The first thing we do, we literally get out pens and paper and chart what happens before patients get into the hospital and what happens after they are discharged, all of the services that touch them—or should,” she says. “The planning process occurs on many levels, with all of the stakeholders in the community looking at the process map and seeing where people fall off and end up readmitted.”
—Jeff Critchfield, MD, division chief of hospital medicine, San Francisco General Hospital
SHM is planning to launch several new BOOST cohorts for participating hospitals this fall, along with a wider range of technical support, Budnitz says.
The Cross-Setting Team
Research on care transitions for uninsured or indigent patients “is not very robust,” observes Amy Boutwell, MD, MPP, a hospitalist at Newton Wellesley Hospital in Newton, Mass., former director of health policy at IHI and president of Collaborative Healthcare Strategies. “We don’t have the information we need, but there are great opportunities to improve our research base,” she explains.
Dr. Boutwell is a big fan of the “cross-setting team,” which brings together around a conference table professionals who work in different care settings, including the hospital, long-term care, and home-based care. She says it’s her job “to make sure patients are safe upon discharge, but if the community is under-resourced for primary-care physicians, if the patient is uninsured and we can’t find a PCP, the hospitalist and cross-setting team need to say, ‘We just can’t accept that.’ ”
A proper handoff should be done in a way that helps the patient and the physician providing the follow-up care. “But you won’t know what that is unless you ask the people you’re sending patients to how you’re doing,” she explains. “When we routinely review readmitted patients in cross-setting groups, it quickly breaks down the mindset that we in the hospital did everything we could have done to make the discharge successful.”
Dr. Boutwell recommends that hospitalists avoid thinking of these issues in a vacuum, as medical-clinical issues that only doctors can fix. “Because you can’t,” she says. “I would never ask an individual hospitalist to reduce readmissions. It requires a multidisciplinary, all-hands-on-deck approach by the hospital. This is different and more exciting than other quality-improvement efforts.” What’s more, she says, the day is coming—and soon—when failing to manage these readmissions will be a bad business proposition for the hospital (see “Value-Based Purchasing Raises the Stakes,” May 2011, p. 1).
IHI’s STAAR Initiative is working with coalitions of providers in Massachusetts, Michigan, Ohio, and Washington. One of those coalitions, Detroit CARR (Community Action to Reduce Rehospitalizations), convened by MPRO, a Michigan-based quality-improvement organization, is a great example of a cross-continuum team involving five inner-city hospitals, Dr. Boutwell says.
“CARR has really dug deeply into the needs of vulnerable patients in one of America’s most economically challenged communities, with a high proportion of Medicaid, uninsured, and disabled patients” and a shrinking population, she says. Many rehospitalizations are related to socio-economics. “The CARR coalition is meeting with the homeless shelters, the food pantries, and the faith-based agencies,” she says. “They’re really getting at the root of significant issues in their community.”
Nancy Vecchioni, RN, MSN, CPHQ, vice present of Medicare operations at MPRO, says CARR involves more than just healthcare providers; it also brings community agencies together with them to take ownership of the patient. Organizations that a year ago weren’t talking to each other are now meeting regularly to focus on the most vulnerable patients, reviewing cases of rehospitalized homeless patients, and sharing their experiences. Rehospitalized patients are being interviewed, using a prepared script (see Figure 1, p. 34), which allows the patient to tell their story. The information is shared within the coalition.
Each hospital has its own transition team, with post-acute providers, physicians, home health agencies, and community service providers, Vecchioni says. For patients who can’t get in to see a PCP within five days of discharge, some hospitals are opening continuity clinics. Others give patients three- to 30-day supplies of needed medications. “There’s no magic bullet—it’s just a different way of looking at how we do this work,” she adds. “Every day we see new barriers. But we’ve already seen a 5% overall reduction in readmissions. And I think hospitalists can be the champions and leaders of these efforts.”
Hospitalists have to raise the bar for themselves, Dr. Schneidermann says, “doing our best while recognizing we can only do so much. There is a lot we can learn from geriatrics, starting with truly embracing the multidisciplinary team.” If hospitalists feel like they are functioning in isolation, she says, they need to look around. “Are these kinds of interdisciplinary meetings happening? If so, join them. If not, light a fire. Convert your frustrating experiences with patients into action.” TH
Larry Beresford is a freelance medical writer based in California.
References
- Misky GJ, Wald HL, Coleman EA. Post-hospitalization transitions: Examining the effects of timing of primary care provider follow-up. J Hosp Med. 2010;5:392-397.
- Buchanan D, Doblin B, Sai T, Garcia P. The effects of respite care for homeless patients: a cohort study. Am J Public Health. 2006;96:1278-1281.
- Kertesz SG, Posner MA, O’Connell JJ, et al. Post-hospital medical respite care and hospital readmission of homeless persons. J Prev Inter Community. 2009;37:129-142.
- Nagamine M, Stocks C, Merrill C. Trends in uninsured hospital stays, 1998-2007. Health Care Cost & Utilization Project (HCUP) Statistical Brief #88. May 2010.
- U.S. Department of Health and Human Services. ASPE Research Brief. The value of health insurance: few of the uninsured have adequate resources to pay potential hospital bills. May 2011.
- U.S. Department of Housing and Urban Development. The Annual Housing Assessment Report to Congress, 2009.
- Kellerman A, Coleman M. Care without Coverage: Too Little, Too Late. Report by Institute of Medicine, May 2002.
- Hasan O, Orav EJ, Hicks LS. Insurance status and hospital care for myocardial infarction, stroke, and pneumonia. J Hosp Med. 2010;5(8):452-459.
- Chirayath HT, Wentworth AL. Constraints to caring: Service to medically indigent patients by allopathic and osteopathic physicians. J Health Care Poor Underserved. 2008;19:500-511.
- Joynt KE, Orav EJ, Jha AK. Thirty-day readmission rates for Medicare beneficiaries by race and site of care. JAMA. 2011;305:675-681.
- Buchanan D, Rohr L, Kehoe L, Glick SB, Jain S. Changing attitudes toward homeless people. J Gen Intern Med. 2004;19(5 Pt 2):566-568.
Gregory Misky, MD, has been a hospitalist for 12 years, first at a community hospital and for the past seven years at the University of Colorado Denver. In recent years, his frustration has grown over the challenges of discharge planning, care transitions, and preventing readmissions for vulnerable, disadvantaged patients, including the uninsured, underinsured, and medically indigent.
“There’s a big elephant in the room that we’re not talking about, and that elephant is having babies,” he says. “Access is such a big problem for these patients and, as a hospitalist, it’s just not OK to me anymore. I need to be proactive about finding solutions.”
Dr. Misky’s concerns led him to do research with mentor Eric Coleman, MD, the university’s creator of the Care Transitions Program (www.caretransitions.org), studying patients who lacked primary-care physicians (PCPs) or timely PCP follow-up, and their resulting higher rates of readmissions.1 Dr. Misky also helped develop care pathways, including post-discharge care, for VTE patients, a “common, costly, and dangerous” condition. He is working with a hospitalist colleague to explore how electronic health records (EHR) might be used to help trigger post-discharge follow-up for at-risk patients.
University of Colorado Hospital (UCH), a 425-bed urban academic tertiary-care center, is not the designated safety net hospital for metro Denver, yet 28% to 32% of patients discharged from its medical services are uninsured, Dr. Misky says. He finds that academic physicians at UCH are not always able to take on large numbers of uninsured patients in their clinics, given the productivity demands they face, while the hospital has not been able to participate in systemwide, comprehensive national models for improving care transitions, such as SHM’s Project BOOST (www.hospitalmedicine.org/boost) or Boston Medical Center’s Project RED (www.bu.edu/fammed/projectred/).
Dr. Misky is in discussions with local community services, such as the Metro Community Provider Network (MCPN) of clinics for underserved patients, and exploring the development of a collaborative model for integrating post-hospital care between UCH and MCPN. “A lot of our ideas are still very exploratory—trying to get the key providers to the table to talk about what these approaches might look like,” Dr. Misky explains. “I’ve been part of ongoing meetings, and I think similar kinds of conversations are happening at many levels at UCH, but there’s not a unified, consensus approach to care transitions—and that’s a problem. But I’m in the midst of it all, trying to highlight the issues and explore solutions.”
—Patricia Rutherford, RN, MS, vice president, Institute for Healthcare Improvement
Dr. Misky says every hospital-based provider—hospitalist, nurses, social workers—feels the same frustration and worry about the level of care when indigent patients are discharged to the community. Uninsured patients can run into problems post-hospitalization and return to the ED for their primary care because they lack other options, he says. “Without established liaisons to the community clinics,” he notes, “it can take three or four months for a new indigent patient to get seen at one.”
Disproportional Issues of the Uninsured
Hospitalists at San Francisco General Hospital, which is the safety-net provider for the Bay Area, are looking at similar issues, says Jeff Critchfield, MD, division chief of hospital medicine. “What we know about the uninsured is that they have a wealth of other challenges and barriers that they bring to the table,” he says. “First of all, un- and underinsured patients are more likely to have chronic illnesses, to be hospitalized for those illnesses, and then to be rehospitalized after discharge.”
Other issues disproportionally impacting uninsured or indigent patients include low literacy, low healthcare literacy, language barriers, cross-cultural barriers, substance abuse and mental health issues, homelessness or marginal housing, transportation barriers, and “social isolation, which also plagues our population and, I believe, places patients at risk, as does depression,” says Dr. Critchfield’s colleague Michelle Schneidermann, MD.
One-third of San Francisco General’s patients are uninsured and 40% have Medi-Cal (California’s version of Medicaid), which basically means they are underinsured.
“California has 19 safety-net hospitals, with 6% of the state’s inpatient beds but 50% of its uninsured population. So that’s what we do,” Dr. Critchfield says. But almost any hospital or hospitalist will see many of the same issues and problems, just not in the same proportions. “These are patients who can be most frustrating to hospitalists, requiring a disproportionate amount of our time,” he says, adding the greatest difficulty is helping these patients understand and follow post-discharge care plans. But if someone is ill enough to need acute hospitalization and is later discharged back to the street, readmission should not be a surprise. “We’ve done that experiment for many years, and we know how it turns out,” he says.
Dr. Schneidermann serves as medical director of San Francisco General’s medical respite program, a 45-bed emergency shelter that accepts homeless or marginally housed patients in need of follow-up care following discharge from any of the city’s acute-care hospitals. Research has shown that the programs can have a major effect on keeping discharged patients off the street, reducing their rates of rehospitalization by as much as 50%.2,3
“We know that homeless patients have longer lengths of hospital stay because their discharges are fraught with problems,” she says. A homeless patient hospitalized with a blood clot potentially could be kept in the hospital for a week while transitioning from heparin to Coumadin, while similar patients with community support might get discharged in a day.
“We are also fortunate to have a program called Healthy San Francisco,” which isn’t a health insurance program per se but since 2007 has provided access to outpatient, inpatient, and preventive care and medications for indigent patients, Dr. Schneidermann says. Sponsored by the city’s Department of Public Health, it is accessed through 32 medical homes located in both public and private clinics. The hospitalists’ goal is to have a follow-up appointment set with a receiving provider at the time of discharge. “It doesn’t always happen, but that’s the goal,” she explains. “Someone, by name, who has accepted the referral.”
Dr. Critchfield is running a randomized controlled trial of the hospital’s interventions to stem the tide of readmissions in patients 60 and older; many of these patients share the same indigent demographics of the rest of San Francisco General’s caseload, although most patients 65 and older qualify for Medicare. He describes the program as a hybrid of Project RED and Dr. Coleman’s Care Transitions Program, although it targets patients who speak English, Spanish, Cantonese, and Mandarin.
How many Americans are uninsured today is a moving target in the context of healthcare reform and its uncertain future, but the number increased to 53 million in 2007 from 42 million in 1998.4 The number of hospitalizations of uninsured patients also grew to 2.3 million from 1.8 million in the same time period, an increase of 31%, while total hospitalizations were increasing by 13%. A May 2011 research brief from the U.S. Department of Health and Human Services estimates that uncompensated costs of hospital care incurred for uninsured patients total $73 billion per year.5
The homeless in shelters or on the street number about 630,000 on any given evening, and 1.5 million Americans experienced homelessness last year, says Sabrina Edgington, MSSW, program and policy specialist at the National Health Care for the Homeless Council in Nashville, Tenn. That said, 30% of the U.S. homeless have health insurance. Uninsured patients are less likely to receive necessary diagnostic tests and labs while in the hospital, and they face limited access and longer wait times—even in the facilities that are willing to take them.7 Research published in the Journal of Hospital Medicine finds that uninsured or Medicaid patients with three common conditions are more likely to die in the hospital than insured patients.8 A 2008 national sample survey of physicians found that “most U.S. physicians limit their care of medically indigent patients.”9 Other recent research suggests that readmission rates are affected by race and by site of care—with hospitals serving a higher proportion of black patients also having higher readmission rates.10
“This is not a hospital problem—it’s a communitywide problem. So there’s not just a hospital solution; it will take the whole village,” says Patricia Rutherford, RN, MS, vice president of the Institute for Healthcare Improvement (IHI), which sponsors initiatives targeting care transitions.
The major national care-transitions programs that assist hospitals with addressing rehospitalizations all share similar objectives, Rutherford says, and all could be helpful in improving hospitals’ responses to indigent patients. The recognized programs include IHI’s STAAR (State Action on Avoidable Rehospitalizations: www.ihi.org/IHI/Programs), a multistate, multistakeholder quality improvement (QI) program; Project BOOST; Project RED; Dr. Coleman’s Care Transitions Project; the nursing-based Transitional Care Model (www.transitionalcare.info); and the American College of Cardiology’s Hospital to Home (www.cardiosource.org).

—Amy Boutwell, MD, MPP, hospitalist, Newton (Mass.) Wellesley Hospital, president, Collaborative Healthcare Strategies
Most of these “well-established, evidence-based interventions,” including BOOST, will be given preference in applications for grants from the federal Community-Based Care Transitions Program (CCTP). The program recently committed $500 million to support community-based coalitions that include hospitals that are working with community partners to create seamless care transitions. “It’s most important that hospitalists are integrally involved with these care-transition teams—if not leading them,” Rutherford says.
BOOST’s approach is built on a major change-management strategy to reconstruct hospitals’ care transitions and discharge processes from the ground up, says Tina Budnitz, MPH, the project’s director at SHM (see “Discharge Improvement,” p. 7.) “The first thing we do, we literally get out pens and paper and chart what happens before patients get into the hospital and what happens after they are discharged, all of the services that touch them—or should,” she says. “The planning process occurs on many levels, with all of the stakeholders in the community looking at the process map and seeing where people fall off and end up readmitted.”
—Jeff Critchfield, MD, division chief of hospital medicine, San Francisco General Hospital
SHM is planning to launch several new BOOST cohorts for participating hospitals this fall, along with a wider range of technical support, Budnitz says.
The Cross-Setting Team
Research on care transitions for uninsured or indigent patients “is not very robust,” observes Amy Boutwell, MD, MPP, a hospitalist at Newton Wellesley Hospital in Newton, Mass., former director of health policy at IHI and president of Collaborative Healthcare Strategies. “We don’t have the information we need, but there are great opportunities to improve our research base,” she explains.
Dr. Boutwell is a big fan of the “cross-setting team,” which brings together around a conference table professionals who work in different care settings, including the hospital, long-term care, and home-based care. She says it’s her job “to make sure patients are safe upon discharge, but if the community is under-resourced for primary-care physicians, if the patient is uninsured and we can’t find a PCP, the hospitalist and cross-setting team need to say, ‘We just can’t accept that.’ ”
A proper handoff should be done in a way that helps the patient and the physician providing the follow-up care. “But you won’t know what that is unless you ask the people you’re sending patients to how you’re doing,” she explains. “When we routinely review readmitted patients in cross-setting groups, it quickly breaks down the mindset that we in the hospital did everything we could have done to make the discharge successful.”
Dr. Boutwell recommends that hospitalists avoid thinking of these issues in a vacuum, as medical-clinical issues that only doctors can fix. “Because you can’t,” she says. “I would never ask an individual hospitalist to reduce readmissions. It requires a multidisciplinary, all-hands-on-deck approach by the hospital. This is different and more exciting than other quality-improvement efforts.” What’s more, she says, the day is coming—and soon—when failing to manage these readmissions will be a bad business proposition for the hospital (see “Value-Based Purchasing Raises the Stakes,” May 2011, p. 1).
IHI’s STAAR Initiative is working with coalitions of providers in Massachusetts, Michigan, Ohio, and Washington. One of those coalitions, Detroit CARR (Community Action to Reduce Rehospitalizations), convened by MPRO, a Michigan-based quality-improvement organization, is a great example of a cross-continuum team involving five inner-city hospitals, Dr. Boutwell says.
“CARR has really dug deeply into the needs of vulnerable patients in one of America’s most economically challenged communities, with a high proportion of Medicaid, uninsured, and disabled patients” and a shrinking population, she says. Many rehospitalizations are related to socio-economics. “The CARR coalition is meeting with the homeless shelters, the food pantries, and the faith-based agencies,” she says. “They’re really getting at the root of significant issues in their community.”
Nancy Vecchioni, RN, MSN, CPHQ, vice present of Medicare operations at MPRO, says CARR involves more than just healthcare providers; it also brings community agencies together with them to take ownership of the patient. Organizations that a year ago weren’t talking to each other are now meeting regularly to focus on the most vulnerable patients, reviewing cases of rehospitalized homeless patients, and sharing their experiences. Rehospitalized patients are being interviewed, using a prepared script (see Figure 1, p. 34), which allows the patient to tell their story. The information is shared within the coalition.
Each hospital has its own transition team, with post-acute providers, physicians, home health agencies, and community service providers, Vecchioni says. For patients who can’t get in to see a PCP within five days of discharge, some hospitals are opening continuity clinics. Others give patients three- to 30-day supplies of needed medications. “There’s no magic bullet—it’s just a different way of looking at how we do this work,” she adds. “Every day we see new barriers. But we’ve already seen a 5% overall reduction in readmissions. And I think hospitalists can be the champions and leaders of these efforts.”
Hospitalists have to raise the bar for themselves, Dr. Schneidermann says, “doing our best while recognizing we can only do so much. There is a lot we can learn from geriatrics, starting with truly embracing the multidisciplinary team.” If hospitalists feel like they are functioning in isolation, she says, they need to look around. “Are these kinds of interdisciplinary meetings happening? If so, join them. If not, light a fire. Convert your frustrating experiences with patients into action.” TH
Larry Beresford is a freelance medical writer based in California.
References
- Misky GJ, Wald HL, Coleman EA. Post-hospitalization transitions: Examining the effects of timing of primary care provider follow-up. J Hosp Med. 2010;5:392-397.
- Buchanan D, Doblin B, Sai T, Garcia P. The effects of respite care for homeless patients: a cohort study. Am J Public Health. 2006;96:1278-1281.
- Kertesz SG, Posner MA, O’Connell JJ, et al. Post-hospital medical respite care and hospital readmission of homeless persons. J Prev Inter Community. 2009;37:129-142.
- Nagamine M, Stocks C, Merrill C. Trends in uninsured hospital stays, 1998-2007. Health Care Cost & Utilization Project (HCUP) Statistical Brief #88. May 2010.
- U.S. Department of Health and Human Services. ASPE Research Brief. The value of health insurance: few of the uninsured have adequate resources to pay potential hospital bills. May 2011.
- U.S. Department of Housing and Urban Development. The Annual Housing Assessment Report to Congress, 2009.
- Kellerman A, Coleman M. Care without Coverage: Too Little, Too Late. Report by Institute of Medicine, May 2002.
- Hasan O, Orav EJ, Hicks LS. Insurance status and hospital care for myocardial infarction, stroke, and pneumonia. J Hosp Med. 2010;5(8):452-459.
- Chirayath HT, Wentworth AL. Constraints to caring: Service to medically indigent patients by allopathic and osteopathic physicians. J Health Care Poor Underserved. 2008;19:500-511.
- Joynt KE, Orav EJ, Jha AK. Thirty-day readmission rates for Medicare beneficiaries by race and site of care. JAMA. 2011;305:675-681.
- Buchanan D, Rohr L, Kehoe L, Glick SB, Jain S. Changing attitudes toward homeless people. J Gen Intern Med. 2004;19(5 Pt 2):566-568.