User login
Agios stops developing drug for PK deficiency

Agios Pharmaceuticals, Inc. is no longer developing one of its pyruvate kinase-R (PKR) activators, AG-519, for the treatment of pyruvate kinase (PK) deficiency.
The company withdrew its investigational new drug application for AG-519 following a verbal notification of a clinical hold from the US Food and Drug Administration (FDA).
The hold resulted from an adverse event—cholestatic hepatitis—observed in a phase 1 trial of healthy volunteers.
“[W]e received feedback from the FDA that AG-519 no longer has an appropriate risk-benefit ratio to move forward in clinical development and was placed on clinical hold due to that case of cholestatic hepatitis,” said David Schenkein, MD, chief executive officer at Agios.
“We made the decision to withdraw the IND [investigational new drug application] and discontinue development of AG-519 and advance AG-348, our first-in-class and lead pyruvate kinase activator into pivotal development. We share the FDA’s commitment to patient safety and believe this is the right decision to ultimately help people with PK deficiency.”
About AG-519
Agios has described AG-519 as a potent, highly selective, and orally bioavailable PKR activator devoid of the aromatase inhibitory effects that were observed with the company’s other PKR activator, AG-348.
AG-519 was evaluated in a phase 1 study of healthy volunteers in the UK. The goal of this study was to assess the drug’s safety, tolerability, pharmacokinetics, pharmacodynamics, and bioavailability.
A case of drug-induced cholestatic hepatitis occurred in the bioavailability portion of the study. This volunteer continues to be monitored and is showing improvement, according to Dr Schenkein.
Agios said other adverse events observed in this trial were largely mild or moderate (grade 1/2). The most common of these was headache.
The company did note a case of grade 2 thrombocytopenia that resolved spontaneously within 7 days after the last dose of AG-519.
Results from this trial were presented at the 2015 ASH Annual Meeting (abstract 1264).
AG-519 was also under investigation in a palatability study of volunteers in the US. The goal of this study was to develop a formulation of the drug for potential future development.
In total, 98 volunteers have received AG-519. No volunteers or patients are currently receiving the drug.
About AG-348
Agios’s decision to stop developing AG-519 does not affect the company’s ongoing phase 2 study (DRIVE PK) of AG-348, an activator of both wild-type and mutated PKR enzymes.
“AG-348 and AG-519 are different molecules with different structures,” Dr Schenkein noted.
Agios is advancing AG-348 into development as the first potential disease-modifying treatment for PK deficiency.
Results from a pair of phase 1 studies of AG-348 were presented at the 2014 ASH Annual Meeting (abstract 4007).
About PK deficiency
PK deficiency is a rare inherited disease that presents as hemolytic anemia. The inherited mutations in PKR enzymes cause a deficit in cellular energy within the red blood cell, as evidenced by lower PK enzyme activity, a decline in adenosine triphosphate levels, and a build-up of upstream metabolites, including 2,3-DPG.
The current standard of care for PK deficiency is supportive care, including blood transfusions, splenectomy, chelation therapy to address iron overload, and/or interventions for other treatment- and disease-related morbidities.
There is, at present, no approved therapy to treat the underlying cause of PK deficiency. ![]()

Agios Pharmaceuticals, Inc. is no longer developing one of its pyruvate kinase-R (PKR) activators, AG-519, for the treatment of pyruvate kinase (PK) deficiency.
The company withdrew its investigational new drug application for AG-519 following a verbal notification of a clinical hold from the US Food and Drug Administration (FDA).
The hold resulted from an adverse event—cholestatic hepatitis—observed in a phase 1 trial of healthy volunteers.
“[W]e received feedback from the FDA that AG-519 no longer has an appropriate risk-benefit ratio to move forward in clinical development and was placed on clinical hold due to that case of cholestatic hepatitis,” said David Schenkein, MD, chief executive officer at Agios.
“We made the decision to withdraw the IND [investigational new drug application] and discontinue development of AG-519 and advance AG-348, our first-in-class and lead pyruvate kinase activator into pivotal development. We share the FDA’s commitment to patient safety and believe this is the right decision to ultimately help people with PK deficiency.”
About AG-519
Agios has described AG-519 as a potent, highly selective, and orally bioavailable PKR activator devoid of the aromatase inhibitory effects that were observed with the company’s other PKR activator, AG-348.
AG-519 was evaluated in a phase 1 study of healthy volunteers in the UK. The goal of this study was to assess the drug’s safety, tolerability, pharmacokinetics, pharmacodynamics, and bioavailability.
A case of drug-induced cholestatic hepatitis occurred in the bioavailability portion of the study. This volunteer continues to be monitored and is showing improvement, according to Dr Schenkein.
Agios said other adverse events observed in this trial were largely mild or moderate (grade 1/2). The most common of these was headache.
The company did note a case of grade 2 thrombocytopenia that resolved spontaneously within 7 days after the last dose of AG-519.
Results from this trial were presented at the 2015 ASH Annual Meeting (abstract 1264).
AG-519 was also under investigation in a palatability study of volunteers in the US. The goal of this study was to develop a formulation of the drug for potential future development.
In total, 98 volunteers have received AG-519. No volunteers or patients are currently receiving the drug.
About AG-348
Agios’s decision to stop developing AG-519 does not affect the company’s ongoing phase 2 study (DRIVE PK) of AG-348, an activator of both wild-type and mutated PKR enzymes.
“AG-348 and AG-519 are different molecules with different structures,” Dr Schenkein noted.
Agios is advancing AG-348 into development as the first potential disease-modifying treatment for PK deficiency.
Results from a pair of phase 1 studies of AG-348 were presented at the 2014 ASH Annual Meeting (abstract 4007).
About PK deficiency
PK deficiency is a rare inherited disease that presents as hemolytic anemia. The inherited mutations in PKR enzymes cause a deficit in cellular energy within the red blood cell, as evidenced by lower PK enzyme activity, a decline in adenosine triphosphate levels, and a build-up of upstream metabolites, including 2,3-DPG.
The current standard of care for PK deficiency is supportive care, including blood transfusions, splenectomy, chelation therapy to address iron overload, and/or interventions for other treatment- and disease-related morbidities.
There is, at present, no approved therapy to treat the underlying cause of PK deficiency. ![]()

Agios Pharmaceuticals, Inc. is no longer developing one of its pyruvate kinase-R (PKR) activators, AG-519, for the treatment of pyruvate kinase (PK) deficiency.
The company withdrew its investigational new drug application for AG-519 following a verbal notification of a clinical hold from the US Food and Drug Administration (FDA).
The hold resulted from an adverse event—cholestatic hepatitis—observed in a phase 1 trial of healthy volunteers.
“[W]e received feedback from the FDA that AG-519 no longer has an appropriate risk-benefit ratio to move forward in clinical development and was placed on clinical hold due to that case of cholestatic hepatitis,” said David Schenkein, MD, chief executive officer at Agios.
“We made the decision to withdraw the IND [investigational new drug application] and discontinue development of AG-519 and advance AG-348, our first-in-class and lead pyruvate kinase activator into pivotal development. We share the FDA’s commitment to patient safety and believe this is the right decision to ultimately help people with PK deficiency.”
About AG-519
Agios has described AG-519 as a potent, highly selective, and orally bioavailable PKR activator devoid of the aromatase inhibitory effects that were observed with the company’s other PKR activator, AG-348.
AG-519 was evaluated in a phase 1 study of healthy volunteers in the UK. The goal of this study was to assess the drug’s safety, tolerability, pharmacokinetics, pharmacodynamics, and bioavailability.
A case of drug-induced cholestatic hepatitis occurred in the bioavailability portion of the study. This volunteer continues to be monitored and is showing improvement, according to Dr Schenkein.
Agios said other adverse events observed in this trial were largely mild or moderate (grade 1/2). The most common of these was headache.
The company did note a case of grade 2 thrombocytopenia that resolved spontaneously within 7 days after the last dose of AG-519.
Results from this trial were presented at the 2015 ASH Annual Meeting (abstract 1264).
AG-519 was also under investigation in a palatability study of volunteers in the US. The goal of this study was to develop a formulation of the drug for potential future development.
In total, 98 volunteers have received AG-519. No volunteers or patients are currently receiving the drug.
About AG-348
Agios’s decision to stop developing AG-519 does not affect the company’s ongoing phase 2 study (DRIVE PK) of AG-348, an activator of both wild-type and mutated PKR enzymes.
“AG-348 and AG-519 are different molecules with different structures,” Dr Schenkein noted.
Agios is advancing AG-348 into development as the first potential disease-modifying treatment for PK deficiency.
Results from a pair of phase 1 studies of AG-348 were presented at the 2014 ASH Annual Meeting (abstract 4007).
About PK deficiency
PK deficiency is a rare inherited disease that presents as hemolytic anemia. The inherited mutations in PKR enzymes cause a deficit in cellular energy within the red blood cell, as evidenced by lower PK enzyme activity, a decline in adenosine triphosphate levels, and a build-up of upstream metabolites, including 2,3-DPG.
The current standard of care for PK deficiency is supportive care, including blood transfusions, splenectomy, chelation therapy to address iron overload, and/or interventions for other treatment- and disease-related morbidities.
There is, at present, no approved therapy to treat the underlying cause of PK deficiency. ![]()
CHMP recommends authorization of rituximab biosimilar

Photo by Linda Bartlett
The European Medicines Agency’s Committee for Medicinal Products for Human Use (CHMP) has recommended that the rituximab biosimilar Truxima receive marketing authorization for the treatment of several conditions.
The CHMP said studies have shown that Truxima is comparable to the reference product, Mabthera, which was authorized for use in the European Union in 1998.
The active substance in both products is the anti-CD20 monoclonal antibody rituximab.
Truxima is being developed by Celltrion Healthcare Hungary Kft.
The CHMP’s recommendation for Truxima will be reviewed by the European Commission, which normally issues its decision on a product within 67 days of the time the CHMP adopts its opinion.
If the European Commission grants marketing authorization for Truxima, it will be available as a 500 mg concentrate for solution for infusion.
The CHMP has recommended marketing authorization for Truxima in the treatment of non-Hodgkin lymphoma, chronic lymphocytic leukemia, rheumatoid arthritis, and granulomatosis with polyangiitis and microscopic polyangiitis.
The full indications are as follows.
Non-Hodgkin lymphoma
Truxima is indicated for use in combination with chemotherapy to treat previously untreated patients with stage III-IV follicular lymphoma.
Truxima maintenance therapy is indicated for the treatment of follicular lymphoma patients responding to induction therapy.
Truxima monotherapy is indicated for treatment of patients with stage III-IV follicular lymphoma who are chemo-resistant or are in their second or subsequent relapse after chemotherapy.
Truxima is indicated for use in combination with CHOP (cyclophosphamide, doxorubicin, vincristine, prednisolone) for the treatment of patients with CD20-positive diffuse large B-cell lymphoma.
Chronic lymphocytic leukemia
Truxima in combination with chemotherapy is indicated for the treatment of patients with previously untreated and relapsed/refractory chronic lymphocytic leukemia.
The CHMP noted that only limited data are available on efficacy and safety for patients previously treated with monoclonal antibodies, including Truxima, or patients refractory to previous Truxima plus chemotherapy.
Rheumatoid arthritis
Truxima in combination with methotrexate is indicated for the treatment of adults with severe active rheumatoid arthritis who have had an inadequate response or cannot tolerate other disease-modifying anti-rheumatic drugs, including one or more tumor necrosis factor inhibitor therapies.
The CHMP noted that Truxima has been shown to reduce the rate of progression of joint damage as measured by X-ray and to improve physical function, when given in combination with methotrexate.
Granulomatosis with polyangiitis and microscopic polyangiitis
Truxima in combination with glucocorticoids is indicated for the induction of remission in adults with severe, active granulomatosis with polyangiitis and microscopic polyangiitis.
The CHMP proposed that Truxima be administered under the close supervision of an experienced healthcare professional and in an environment where full resuscitation facilities are immediately available. ![]()

Photo by Linda Bartlett
The European Medicines Agency’s Committee for Medicinal Products for Human Use (CHMP) has recommended that the rituximab biosimilar Truxima receive marketing authorization for the treatment of several conditions.
The CHMP said studies have shown that Truxima is comparable to the reference product, Mabthera, which was authorized for use in the European Union in 1998.
The active substance in both products is the anti-CD20 monoclonal antibody rituximab.
Truxima is being developed by Celltrion Healthcare Hungary Kft.
The CHMP’s recommendation for Truxima will be reviewed by the European Commission, which normally issues its decision on a product within 67 days of the time the CHMP adopts its opinion.
If the European Commission grants marketing authorization for Truxima, it will be available as a 500 mg concentrate for solution for infusion.
The CHMP has recommended marketing authorization for Truxima in the treatment of non-Hodgkin lymphoma, chronic lymphocytic leukemia, rheumatoid arthritis, and granulomatosis with polyangiitis and microscopic polyangiitis.
The full indications are as follows.
Non-Hodgkin lymphoma
Truxima is indicated for use in combination with chemotherapy to treat previously untreated patients with stage III-IV follicular lymphoma.
Truxima maintenance therapy is indicated for the treatment of follicular lymphoma patients responding to induction therapy.
Truxima monotherapy is indicated for treatment of patients with stage III-IV follicular lymphoma who are chemo-resistant or are in their second or subsequent relapse after chemotherapy.
Truxima is indicated for use in combination with CHOP (cyclophosphamide, doxorubicin, vincristine, prednisolone) for the treatment of patients with CD20-positive diffuse large B-cell lymphoma.
Chronic lymphocytic leukemia
Truxima in combination with chemotherapy is indicated for the treatment of patients with previously untreated and relapsed/refractory chronic lymphocytic leukemia.
The CHMP noted that only limited data are available on efficacy and safety for patients previously treated with monoclonal antibodies, including Truxima, or patients refractory to previous Truxima plus chemotherapy.
Rheumatoid arthritis
Truxima in combination with methotrexate is indicated for the treatment of adults with severe active rheumatoid arthritis who have had an inadequate response or cannot tolerate other disease-modifying anti-rheumatic drugs, including one or more tumor necrosis factor inhibitor therapies.
The CHMP noted that Truxima has been shown to reduce the rate of progression of joint damage as measured by X-ray and to improve physical function, when given in combination with methotrexate.
Granulomatosis with polyangiitis and microscopic polyangiitis
Truxima in combination with glucocorticoids is indicated for the induction of remission in adults with severe, active granulomatosis with polyangiitis and microscopic polyangiitis.
The CHMP proposed that Truxima be administered under the close supervision of an experienced healthcare professional and in an environment where full resuscitation facilities are immediately available. ![]()

Photo by Linda Bartlett
The European Medicines Agency’s Committee for Medicinal Products for Human Use (CHMP) has recommended that the rituximab biosimilar Truxima receive marketing authorization for the treatment of several conditions.
The CHMP said studies have shown that Truxima is comparable to the reference product, Mabthera, which was authorized for use in the European Union in 1998.
The active substance in both products is the anti-CD20 monoclonal antibody rituximab.
Truxima is being developed by Celltrion Healthcare Hungary Kft.
The CHMP’s recommendation for Truxima will be reviewed by the European Commission, which normally issues its decision on a product within 67 days of the time the CHMP adopts its opinion.
If the European Commission grants marketing authorization for Truxima, it will be available as a 500 mg concentrate for solution for infusion.
The CHMP has recommended marketing authorization for Truxima in the treatment of non-Hodgkin lymphoma, chronic lymphocytic leukemia, rheumatoid arthritis, and granulomatosis with polyangiitis and microscopic polyangiitis.
The full indications are as follows.
Non-Hodgkin lymphoma
Truxima is indicated for use in combination with chemotherapy to treat previously untreated patients with stage III-IV follicular lymphoma.
Truxima maintenance therapy is indicated for the treatment of follicular lymphoma patients responding to induction therapy.
Truxima monotherapy is indicated for treatment of patients with stage III-IV follicular lymphoma who are chemo-resistant or are in their second or subsequent relapse after chemotherapy.
Truxima is indicated for use in combination with CHOP (cyclophosphamide, doxorubicin, vincristine, prednisolone) for the treatment of patients with CD20-positive diffuse large B-cell lymphoma.
Chronic lymphocytic leukemia
Truxima in combination with chemotherapy is indicated for the treatment of patients with previously untreated and relapsed/refractory chronic lymphocytic leukemia.
The CHMP noted that only limited data are available on efficacy and safety for patients previously treated with monoclonal antibodies, including Truxima, or patients refractory to previous Truxima plus chemotherapy.
Rheumatoid arthritis
Truxima in combination with methotrexate is indicated for the treatment of adults with severe active rheumatoid arthritis who have had an inadequate response or cannot tolerate other disease-modifying anti-rheumatic drugs, including one or more tumor necrosis factor inhibitor therapies.
The CHMP noted that Truxima has been shown to reduce the rate of progression of joint damage as measured by X-ray and to improve physical function, when given in combination with methotrexate.
Granulomatosis with polyangiitis and microscopic polyangiitis
Truxima in combination with glucocorticoids is indicated for the induction of remission in adults with severe, active granulomatosis with polyangiitis and microscopic polyangiitis.
The CHMP proposed that Truxima be administered under the close supervision of an experienced healthcare professional and in an environment where full resuscitation facilities are immediately available. ![]()
Health Canada approves therapy for hemophilia A

Health Canada has approved the use of lonoctocog alfa (Afstyla), a recombinant factor VIII (FVIII) single-chain therapy, in hemophilia A patients of all ages.
Lonoctocog alfa is indicated for use as routine prophylaxis to prevent or reduce the frequency of bleeding episodes, for on-demand treatment to control bleeding episodes, and for perioperative management of bleeding (surgical prophylaxis).
Lonoctocog alfa is the first and only single-chain recombinant FVIII therapy for hemophilia A specifically designed to provide long-lasting protection from bleeds with 2- to 3-times weekly dosing, according to CSL Behring, the company developing the product.
The company says lonoctocog alfa uses a covalent bond that forms one structural entity—a single polypeptide chain—to improve the stability of FVIII and provide FVIII activity with the option of twice-weekly dosing.
Health Canada’s approval of lonoctocog alfa is based on results from the AFFINITY clinical development program, which includes a trial of children (n=84) and a trial of adolescents and adults (n=175).
Among patients who received lonoctocog alfa prophylactically, the median annualized bleeding rate was 1.14 in the adults/adolescents and 3.69 in children younger than 12.
In all, there were 1195 bleeding events—848 in the adults/adolescents and 347 in the children.
Ninety-four percent of bleeds in adults/adolescents and 96% of bleeds in pediatric patients were effectively controlled with no more than 2 infusions of lonoctocog alfa weekly.
Eighty-one percent of bleeds in adults/adolescents and 86% of bleeds in pediatric patients were controlled by a single infusion.
Researchers assessed safety in 258 patients from both studies. Adverse reactions occurred in 14 patients and included hypersensitivity (n=4), dizziness (n=2), paresthesia (n=1), rash (n=1), erythema (n=1), pruritus (n=1), pyrexia (n=1), injection-site pain (n=1), chills (n=1), and feeling hot (n=1).
One patient withdrew from treatment due to hypersensitivity.
None of the patients developed neutralizing antibodies to FVIII or antibodies to host cell proteins. There were no reports of anaphylaxis or thrombosis.
Results from the trial of adolescents/adults were published in Blood in August. Results from the trial of children were presented at the World Federation of Hemophilia 2016 World Congress in July.* ![]()

Health Canada has approved the use of lonoctocog alfa (Afstyla), a recombinant factor VIII (FVIII) single-chain therapy, in hemophilia A patients of all ages.
Lonoctocog alfa is indicated for use as routine prophylaxis to prevent or reduce the frequency of bleeding episodes, for on-demand treatment to control bleeding episodes, and for perioperative management of bleeding (surgical prophylaxis).
Lonoctocog alfa is the first and only single-chain recombinant FVIII therapy for hemophilia A specifically designed to provide long-lasting protection from bleeds with 2- to 3-times weekly dosing, according to CSL Behring, the company developing the product.
The company says lonoctocog alfa uses a covalent bond that forms one structural entity—a single polypeptide chain—to improve the stability of FVIII and provide FVIII activity with the option of twice-weekly dosing.
Health Canada’s approval of lonoctocog alfa is based on results from the AFFINITY clinical development program, which includes a trial of children (n=84) and a trial of adolescents and adults (n=175).
Among patients who received lonoctocog alfa prophylactically, the median annualized bleeding rate was 1.14 in the adults/adolescents and 3.69 in children younger than 12.
In all, there were 1195 bleeding events—848 in the adults/adolescents and 347 in the children.
Ninety-four percent of bleeds in adults/adolescents and 96% of bleeds in pediatric patients were effectively controlled with no more than 2 infusions of lonoctocog alfa weekly.
Eighty-one percent of bleeds in adults/adolescents and 86% of bleeds in pediatric patients were controlled by a single infusion.
Researchers assessed safety in 258 patients from both studies. Adverse reactions occurred in 14 patients and included hypersensitivity (n=4), dizziness (n=2), paresthesia (n=1), rash (n=1), erythema (n=1), pruritus (n=1), pyrexia (n=1), injection-site pain (n=1), chills (n=1), and feeling hot (n=1).
One patient withdrew from treatment due to hypersensitivity.
None of the patients developed neutralizing antibodies to FVIII or antibodies to host cell proteins. There were no reports of anaphylaxis or thrombosis.
Results from the trial of adolescents/adults were published in Blood in August. Results from the trial of children were presented at the World Federation of Hemophilia 2016 World Congress in July.* ![]()

Health Canada has approved the use of lonoctocog alfa (Afstyla), a recombinant factor VIII (FVIII) single-chain therapy, in hemophilia A patients of all ages.
Lonoctocog alfa is indicated for use as routine prophylaxis to prevent or reduce the frequency of bleeding episodes, for on-demand treatment to control bleeding episodes, and for perioperative management of bleeding (surgical prophylaxis).
Lonoctocog alfa is the first and only single-chain recombinant FVIII therapy for hemophilia A specifically designed to provide long-lasting protection from bleeds with 2- to 3-times weekly dosing, according to CSL Behring, the company developing the product.
The company says lonoctocog alfa uses a covalent bond that forms one structural entity—a single polypeptide chain—to improve the stability of FVIII and provide FVIII activity with the option of twice-weekly dosing.
Health Canada’s approval of lonoctocog alfa is based on results from the AFFINITY clinical development program, which includes a trial of children (n=84) and a trial of adolescents and adults (n=175).
Among patients who received lonoctocog alfa prophylactically, the median annualized bleeding rate was 1.14 in the adults/adolescents and 3.69 in children younger than 12.
In all, there were 1195 bleeding events—848 in the adults/adolescents and 347 in the children.
Ninety-four percent of bleeds in adults/adolescents and 96% of bleeds in pediatric patients were effectively controlled with no more than 2 infusions of lonoctocog alfa weekly.
Eighty-one percent of bleeds in adults/adolescents and 86% of bleeds in pediatric patients were controlled by a single infusion.
Researchers assessed safety in 258 patients from both studies. Adverse reactions occurred in 14 patients and included hypersensitivity (n=4), dizziness (n=2), paresthesia (n=1), rash (n=1), erythema (n=1), pruritus (n=1), pyrexia (n=1), injection-site pain (n=1), chills (n=1), and feeling hot (n=1).
One patient withdrew from treatment due to hypersensitivity.
None of the patients developed neutralizing antibodies to FVIII or antibodies to host cell proteins. There were no reports of anaphylaxis or thrombosis.
Results from the trial of adolescents/adults were published in Blood in August. Results from the trial of children were presented at the World Federation of Hemophilia 2016 World Congress in July.* ![]()
EC authorizes new use for ofatumumab in CLL

Photo courtesy of GSK
The European Commission (EC) has granted marketing authorization for ofatumumab (Arzerra®) to be used in combination with fludarabine and cyclophosphamide (FC) in the treatment of adults with relapsed chronic lymphocytic leukemia (CLL).
Ofatumumab is a monoclonal antibody designed to target CD20. The drug is marketed under a collaboration agreement between Genmab and Novartis.
The EC previously authorized the use of ofatumumab as a single agent to treat CLL patients who are refractory to fludarabine and alemtuzumab.
The agency also authorized the use of ofatumumab in combination with chlorambucil or bendamustine in CLL patients who have not received prior therapy and are not eligible for fludarabine-based therapy.
The EC’s decision to approve the use of ofatumumab in combination with FC was based on results from the phase 3 COMPLEMENT 2 study, which were published in Leukemia & Lymphoma in October.
The trial enrolled 365 patients with relapsed CLL. The patients were randomized 1:1 to receive up to 6 cycles of ofatumumab in combination with FC or up to 6 cycles of FC alone.
The primary endpoint was progression-free survival, as assessed by an independent review committee.
The median progression-free survival was 28.9 months for patients receiving ofatumumab plus FC, compared to 18.8 months for patients receiving FC only (hazard ratio=0.67, P=0.0032).
The incidence of grade 3 or higher adverse events was 74% in the ofatumumab-plus-FC arm and 69% in the FC-only arm. Neutropenia was the most common of these events, occurring in 49% and 36% of patients, respectively. ![]()

Photo courtesy of GSK
The European Commission (EC) has granted marketing authorization for ofatumumab (Arzerra®) to be used in combination with fludarabine and cyclophosphamide (FC) in the treatment of adults with relapsed chronic lymphocytic leukemia (CLL).
Ofatumumab is a monoclonal antibody designed to target CD20. The drug is marketed under a collaboration agreement between Genmab and Novartis.
The EC previously authorized the use of ofatumumab as a single agent to treat CLL patients who are refractory to fludarabine and alemtuzumab.
The agency also authorized the use of ofatumumab in combination with chlorambucil or bendamustine in CLL patients who have not received prior therapy and are not eligible for fludarabine-based therapy.
The EC’s decision to approve the use of ofatumumab in combination with FC was based on results from the phase 3 COMPLEMENT 2 study, which were published in Leukemia & Lymphoma in October.
The trial enrolled 365 patients with relapsed CLL. The patients were randomized 1:1 to receive up to 6 cycles of ofatumumab in combination with FC or up to 6 cycles of FC alone.
The primary endpoint was progression-free survival, as assessed by an independent review committee.
The median progression-free survival was 28.9 months for patients receiving ofatumumab plus FC, compared to 18.8 months for patients receiving FC only (hazard ratio=0.67, P=0.0032).
The incidence of grade 3 or higher adverse events was 74% in the ofatumumab-plus-FC arm and 69% in the FC-only arm. Neutropenia was the most common of these events, occurring in 49% and 36% of patients, respectively. ![]()

Photo courtesy of GSK
The European Commission (EC) has granted marketing authorization for ofatumumab (Arzerra®) to be used in combination with fludarabine and cyclophosphamide (FC) in the treatment of adults with relapsed chronic lymphocytic leukemia (CLL).
Ofatumumab is a monoclonal antibody designed to target CD20. The drug is marketed under a collaboration agreement between Genmab and Novartis.
The EC previously authorized the use of ofatumumab as a single agent to treat CLL patients who are refractory to fludarabine and alemtuzumab.
The agency also authorized the use of ofatumumab in combination with chlorambucil or bendamustine in CLL patients who have not received prior therapy and are not eligible for fludarabine-based therapy.
The EC’s decision to approve the use of ofatumumab in combination with FC was based on results from the phase 3 COMPLEMENT 2 study, which were published in Leukemia & Lymphoma in October.
The trial enrolled 365 patients with relapsed CLL. The patients were randomized 1:1 to receive up to 6 cycles of ofatumumab in combination with FC or up to 6 cycles of FC alone.
The primary endpoint was progression-free survival, as assessed by an independent review committee.
The median progression-free survival was 28.9 months for patients receiving ofatumumab plus FC, compared to 18.8 months for patients receiving FC only (hazard ratio=0.67, P=0.0032).
The incidence of grade 3 or higher adverse events was 74% in the ofatumumab-plus-FC arm and 69% in the FC-only arm. Neutropenia was the most common of these events, occurring in 49% and 36% of patients, respectively. ![]()
EC grants venetoclax conditional approval for CLL
(US version, Venclexta)
Photo courtesy of Abbvie
The European Commission (EC) has granted conditional marketing authorization for the oral BCL-2 inhibitor venetoclax (Venclyxto™) to treat certain patients with chronic lymphocytic leukemia (CLL).
The drug is now approved as monotherapy to treat adults with CLL who have 17p deletion or TP53 mutation and are unsuitable for or have failed a B-cell receptor pathway inhibitor.
Venetoclax is also approved as monotherapy to treat CLL in the absence of 17p deletion or TP53 mutation in adults who have failed both chemoimmunotherapy and a B-cell receptor pathway inhibitor.
Venetoclax is the first BCL-2 inhibitor authorized for use in Europe.
Conditional marketing authorization represents an expedited path for approval. The EC grants conditional marketing authorization to products whose benefits are thought to outweigh their risks, products that address unmet needs, and products that are expected to provide a significant public health benefit.
Conditional marketing authorization is granted before pivotal registration studies of a product are completed, but the company developing the product is required to complete post-marketing studies showing that the product provides a clinical benefit.
Venetoclax is being developed by AbbVie and Genentech, a member of the Roche Group. The drug is jointly commercialized by the companies in the US and by AbbVie outside of the US.
Phase 2 trials
Venetoclax has produced high objective response rates (ORR) in two phase 2 trials of CLL patients.
In one of these trials, researchers tested venetoclax in 107 patients with previously treated CLL and 17p deletion. The results were published in The Lancet Oncology in June.
The ORR in this trial was 79%. At the time of analysis, the median duration of response had not been reached. The same was true for progression-free survival and overall survival.
The progression-free survival estimate for 12 months was 72%, and the overall survival estimate was 87%.
The incidence of treatment-emergent adverse events was 96%, and the incidence of serious adverse events was 55%.
Grade 3 laboratory tumor lysis syndrome (TLS) was reported in 5 patients. Three of these patients continued on venetoclax, but 2 patients required a dose interruption of 1 day each.
In the second trial, researchers tested venetoclax in 64 patients with CLL who had failed treatment with ibrutinib and/or idelalisib. Results from this trial were presented at the 2016 ASH Annual Meeting.
The ORR was 67%. At 11.8 months of follow-up, the median duration of response, progression-free survival, and overall survival had not been reached. The estimated 12-month progression-free survival was 80%.
The incidence of adverse events was 100%, and the incidence of serious adverse events was 53%. No clinical TLS was observed, but 1 patient met Howard criteria for laboratory TLS. ![]()
(US version, Venclexta)
Photo courtesy of Abbvie
The European Commission (EC) has granted conditional marketing authorization for the oral BCL-2 inhibitor venetoclax (Venclyxto™) to treat certain patients with chronic lymphocytic leukemia (CLL).
The drug is now approved as monotherapy to treat adults with CLL who have 17p deletion or TP53 mutation and are unsuitable for or have failed a B-cell receptor pathway inhibitor.
Venetoclax is also approved as monotherapy to treat CLL in the absence of 17p deletion or TP53 mutation in adults who have failed both chemoimmunotherapy and a B-cell receptor pathway inhibitor.
Venetoclax is the first BCL-2 inhibitor authorized for use in Europe.
Conditional marketing authorization represents an expedited path for approval. The EC grants conditional marketing authorization to products whose benefits are thought to outweigh their risks, products that address unmet needs, and products that are expected to provide a significant public health benefit.
Conditional marketing authorization is granted before pivotal registration studies of a product are completed, but the company developing the product is required to complete post-marketing studies showing that the product provides a clinical benefit.
Venetoclax is being developed by AbbVie and Genentech, a member of the Roche Group. The drug is jointly commercialized by the companies in the US and by AbbVie outside of the US.
Phase 2 trials
Venetoclax has produced high objective response rates (ORR) in two phase 2 trials of CLL patients.
In one of these trials, researchers tested venetoclax in 107 patients with previously treated CLL and 17p deletion. The results were published in The Lancet Oncology in June.
The ORR in this trial was 79%. At the time of analysis, the median duration of response had not been reached. The same was true for progression-free survival and overall survival.
The progression-free survival estimate for 12 months was 72%, and the overall survival estimate was 87%.
The incidence of treatment-emergent adverse events was 96%, and the incidence of serious adverse events was 55%.
Grade 3 laboratory tumor lysis syndrome (TLS) was reported in 5 patients. Three of these patients continued on venetoclax, but 2 patients required a dose interruption of 1 day each.
In the second trial, researchers tested venetoclax in 64 patients with CLL who had failed treatment with ibrutinib and/or idelalisib. Results from this trial were presented at the 2016 ASH Annual Meeting.
The ORR was 67%. At 11.8 months of follow-up, the median duration of response, progression-free survival, and overall survival had not been reached. The estimated 12-month progression-free survival was 80%.
The incidence of adverse events was 100%, and the incidence of serious adverse events was 53%. No clinical TLS was observed, but 1 patient met Howard criteria for laboratory TLS. ![]()
(US version, Venclexta)
Photo courtesy of Abbvie
The European Commission (EC) has granted conditional marketing authorization for the oral BCL-2 inhibitor venetoclax (Venclyxto™) to treat certain patients with chronic lymphocytic leukemia (CLL).
The drug is now approved as monotherapy to treat adults with CLL who have 17p deletion or TP53 mutation and are unsuitable for or have failed a B-cell receptor pathway inhibitor.
Venetoclax is also approved as monotherapy to treat CLL in the absence of 17p deletion or TP53 mutation in adults who have failed both chemoimmunotherapy and a B-cell receptor pathway inhibitor.
Venetoclax is the first BCL-2 inhibitor authorized for use in Europe.
Conditional marketing authorization represents an expedited path for approval. The EC grants conditional marketing authorization to products whose benefits are thought to outweigh their risks, products that address unmet needs, and products that are expected to provide a significant public health benefit.
Conditional marketing authorization is granted before pivotal registration studies of a product are completed, but the company developing the product is required to complete post-marketing studies showing that the product provides a clinical benefit.
Venetoclax is being developed by AbbVie and Genentech, a member of the Roche Group. The drug is jointly commercialized by the companies in the US and by AbbVie outside of the US.
Phase 2 trials
Venetoclax has produced high objective response rates (ORR) in two phase 2 trials of CLL patients.
In one of these trials, researchers tested venetoclax in 107 patients with previously treated CLL and 17p deletion. The results were published in The Lancet Oncology in June.
The ORR in this trial was 79%. At the time of analysis, the median duration of response had not been reached. The same was true for progression-free survival and overall survival.
The progression-free survival estimate for 12 months was 72%, and the overall survival estimate was 87%.
The incidence of treatment-emergent adverse events was 96%, and the incidence of serious adverse events was 55%.
Grade 3 laboratory tumor lysis syndrome (TLS) was reported in 5 patients. Three of these patients continued on venetoclax, but 2 patients required a dose interruption of 1 day each.
In the second trial, researchers tested venetoclax in 64 patients with CLL who had failed treatment with ibrutinib and/or idelalisib. Results from this trial were presented at the 2016 ASH Annual Meeting.
The ORR was 67%. At 11.8 months of follow-up, the median duration of response, progression-free survival, and overall survival had not been reached. The estimated 12-month progression-free survival was 80%.
The incidence of adverse events was 100%, and the incidence of serious adverse events was 53%. No clinical TLS was observed, but 1 patient met Howard criteria for laboratory TLS. ![]()
FDA grants priority review to sBLA for pembrolizumab

Photo courtesy of Merck
The US Food and Drug Administration (FDA) has granted priority review to the supplemental biologics license application (sBLA) for pembrolizumab (Keytruda®) as a treatment for patients with refractory classical Hodgkin lymphoma (cHL) and for cHL patients who have relapsed after 3 or more prior lines of therapy.
The sBLA will be reviewed under the FDA’s accelerated approval program. The target action date is March 15, 2017.
Pembrolizumab is a monoclonal antibody that binds to the PD-1 receptor and blocks its interaction with PD-L1 and PD-L2, releasing PD-1 pathway-mediated inhibition of the immune response, including the antitumor immune response.
The drug, which is being developed by Merck, already has FDA approval as a treatment for melanoma, lung cancer, and head and neck cancer.
Pembrolizumab also has breakthrough therapy designation as a treatment for relapsed/refractory cHL.
The current sBLA for pembrolizumab is seeking approval for the drug at a fixed dose of 200 mg, administered intravenously every 3 weeks.
This is the first application for regulatory approval of pembrolizumab in a hematologic malignancy.
The sBLA is supported by data from the phase 1 KEYNOTE-013 trial and the phase 2 KEYNOTE-087 trial.
Results from KEYNOTE-013 (in cHL patients) were presented at the 2014 ASH Annual Meeting, and results from KEYNOTE-087 were presented at the 2016 ASCO Annual Meeting. ![]()

Photo courtesy of Merck
The US Food and Drug Administration (FDA) has granted priority review to the supplemental biologics license application (sBLA) for pembrolizumab (Keytruda®) as a treatment for patients with refractory classical Hodgkin lymphoma (cHL) and for cHL patients who have relapsed after 3 or more prior lines of therapy.
The sBLA will be reviewed under the FDA’s accelerated approval program. The target action date is March 15, 2017.
Pembrolizumab is a monoclonal antibody that binds to the PD-1 receptor and blocks its interaction with PD-L1 and PD-L2, releasing PD-1 pathway-mediated inhibition of the immune response, including the antitumor immune response.
The drug, which is being developed by Merck, already has FDA approval as a treatment for melanoma, lung cancer, and head and neck cancer.
Pembrolizumab also has breakthrough therapy designation as a treatment for relapsed/refractory cHL.
The current sBLA for pembrolizumab is seeking approval for the drug at a fixed dose of 200 mg, administered intravenously every 3 weeks.
This is the first application for regulatory approval of pembrolizumab in a hematologic malignancy.
The sBLA is supported by data from the phase 1 KEYNOTE-013 trial and the phase 2 KEYNOTE-087 trial.
Results from KEYNOTE-013 (in cHL patients) were presented at the 2014 ASH Annual Meeting, and results from KEYNOTE-087 were presented at the 2016 ASCO Annual Meeting. ![]()

Photo courtesy of Merck
The US Food and Drug Administration (FDA) has granted priority review to the supplemental biologics license application (sBLA) for pembrolizumab (Keytruda®) as a treatment for patients with refractory classical Hodgkin lymphoma (cHL) and for cHL patients who have relapsed after 3 or more prior lines of therapy.
The sBLA will be reviewed under the FDA’s accelerated approval program. The target action date is March 15, 2017.
Pembrolizumab is a monoclonal antibody that binds to the PD-1 receptor and blocks its interaction with PD-L1 and PD-L2, releasing PD-1 pathway-mediated inhibition of the immune response, including the antitumor immune response.
The drug, which is being developed by Merck, already has FDA approval as a treatment for melanoma, lung cancer, and head and neck cancer.
Pembrolizumab also has breakthrough therapy designation as a treatment for relapsed/refractory cHL.
The current sBLA for pembrolizumab is seeking approval for the drug at a fixed dose of 200 mg, administered intravenously every 3 weeks.
This is the first application for regulatory approval of pembrolizumab in a hematologic malignancy.
The sBLA is supported by data from the phase 1 KEYNOTE-013 trial and the phase 2 KEYNOTE-087 trial.
Results from KEYNOTE-013 (in cHL patients) were presented at the 2014 ASH Annual Meeting, and results from KEYNOTE-087 were presented at the 2016 ASCO Annual Meeting. ![]()
EC grants drug orphan designation for SCD

beside a normal one
Image by Betty Pace
The European Commission (EC) has designated GBT440 as an orphan medicinal product for the treatment of sickle cell disease (SCD).
GBT440 is being developed as a potentially disease-modifying therapy for SCD. The drug works by increasing hemoglobin’s affinity for oxygen.
Since oxygenated sickle hemoglobin does not polymerize, it is believed that GBT440 blocks polymerization and the resultant sickling of red blood cells.
If GBT440 can restore normal hemoglobin function and improve oxygen delivery, the drug may be capable of modifying the progression of SCD.
Preclinical research published in the British Journal of Haematology earlier this year suggests that GBT440 is disease-modifying.
Early results from an ongoing phase 1/2 study of GBT440, which were presented at the 2015 ASH Annual Meeting, appeared promising as well.
Results from that study suggest that GBT440 can increase hemoglobin levels while decreasing reticulocyte counts, erythropoietin levels, and sickle cell counts.
Researchers also found the drug to be well tolerated, with no serious adverse events attributed to GBT440.
“Receiving orphan designation from the EC marks a significant milestone both for the SCD community and for GBT [Global Blood Therapeutics Inc.],” said Ted W. Love, MD, president and chief executive officer of Global Blood Therapeutics Inc., the company developing GBT440.
“SCD is a devastatingly severe disease with limited treatment options, and this designation, together with our fast track and orphan drug designations by the United States Food and Drug Administration, reflect the recognition of the broader regulatory community of this urgent unmet medical need.”
The EC grants orphan designation to therapies intended to treat life-threatening or chronically debilitating conditions affecting no more than 5 in 10,000 people in the European Union, and where no satisfactory treatment is available.
Orphan designation provides the company developing a drug with regulatory and financial incentives, including protocol assistance, 10 years of market exclusivity once the drug is approved, and reductions in, or exemptions from, fees. ![]()

beside a normal one
Image by Betty Pace
The European Commission (EC) has designated GBT440 as an orphan medicinal product for the treatment of sickle cell disease (SCD).
GBT440 is being developed as a potentially disease-modifying therapy for SCD. The drug works by increasing hemoglobin’s affinity for oxygen.
Since oxygenated sickle hemoglobin does not polymerize, it is believed that GBT440 blocks polymerization and the resultant sickling of red blood cells.
If GBT440 can restore normal hemoglobin function and improve oxygen delivery, the drug may be capable of modifying the progression of SCD.
Preclinical research published in the British Journal of Haematology earlier this year suggests that GBT440 is disease-modifying.
Early results from an ongoing phase 1/2 study of GBT440, which were presented at the 2015 ASH Annual Meeting, appeared promising as well.
Results from that study suggest that GBT440 can increase hemoglobin levels while decreasing reticulocyte counts, erythropoietin levels, and sickle cell counts.
Researchers also found the drug to be well tolerated, with no serious adverse events attributed to GBT440.
“Receiving orphan designation from the EC marks a significant milestone both for the SCD community and for GBT [Global Blood Therapeutics Inc.],” said Ted W. Love, MD, president and chief executive officer of Global Blood Therapeutics Inc., the company developing GBT440.
“SCD is a devastatingly severe disease with limited treatment options, and this designation, together with our fast track and orphan drug designations by the United States Food and Drug Administration, reflect the recognition of the broader regulatory community of this urgent unmet medical need.”
The EC grants orphan designation to therapies intended to treat life-threatening or chronically debilitating conditions affecting no more than 5 in 10,000 people in the European Union, and where no satisfactory treatment is available.
Orphan designation provides the company developing a drug with regulatory and financial incentives, including protocol assistance, 10 years of market exclusivity once the drug is approved, and reductions in, or exemptions from, fees. ![]()

beside a normal one
Image by Betty Pace
The European Commission (EC) has designated GBT440 as an orphan medicinal product for the treatment of sickle cell disease (SCD).
GBT440 is being developed as a potentially disease-modifying therapy for SCD. The drug works by increasing hemoglobin’s affinity for oxygen.
Since oxygenated sickle hemoglobin does not polymerize, it is believed that GBT440 blocks polymerization and the resultant sickling of red blood cells.
If GBT440 can restore normal hemoglobin function and improve oxygen delivery, the drug may be capable of modifying the progression of SCD.
Preclinical research published in the British Journal of Haematology earlier this year suggests that GBT440 is disease-modifying.
Early results from an ongoing phase 1/2 study of GBT440, which were presented at the 2015 ASH Annual Meeting, appeared promising as well.
Results from that study suggest that GBT440 can increase hemoglobin levels while decreasing reticulocyte counts, erythropoietin levels, and sickle cell counts.
Researchers also found the drug to be well tolerated, with no serious adverse events attributed to GBT440.
“Receiving orphan designation from the EC marks a significant milestone both for the SCD community and for GBT [Global Blood Therapeutics Inc.],” said Ted W. Love, MD, president and chief executive officer of Global Blood Therapeutics Inc., the company developing GBT440.
“SCD is a devastatingly severe disease with limited treatment options, and this designation, together with our fast track and orphan drug designations by the United States Food and Drug Administration, reflect the recognition of the broader regulatory community of this urgent unmet medical need.”
The EC grants orphan designation to therapies intended to treat life-threatening or chronically debilitating conditions affecting no more than 5 in 10,000 people in the European Union, and where no satisfactory treatment is available.
Orphan designation provides the company developing a drug with regulatory and financial incentives, including protocol assistance, 10 years of market exclusivity once the drug is approved, and reductions in, or exemptions from, fees.
NICE recommends pomalidomide for routine use

Photo from Business Wire
The National Institute for Health and Care Excellence (NICE) has issued a final appraisal determination recommending that pomalidomide be made available through the National Health Service (NHS).
NICE is recommending pomalidomide be available for use in combination with low-dose dexamethasone to treat adults with multiple myeloma who have received at least 3 previous treatments, including lenalidomide and bortezomib.
NICE previously evaluated pomalidomide in 2015 and said it could not recommend the drug, as analyses suggested pomalidomide doesn’t provide enough benefit to justify its high price.
Since that time, a committee advising NICE has reviewed additional data on pomalidomide.
And Celgene, the company that makes pomalidomide, has agreed to provide the NHS with a discount.
The cost of pomalidomide is £8884 per 21-tablet pack (excluding tax). The average cost of a course of treatment is £44,420 (excluding tax).
The discount Celgene will provide to the NHS is confidential.
NICE’s final appraisal determination on pomalidomide is now with consultees who have the opportunity to appeal against it. If there is no appeal, or an appeal is not upheld, the final appraisal determination is issued by NICE as a guidance.
The final guidance is expected in January 2017. Once NICE issues a final guidance on pomalidomide, the NHS must make the drug available within 3 months.

Photo from Business Wire
The National Institute for Health and Care Excellence (NICE) has issued a final appraisal determination recommending that pomalidomide be made available through the National Health Service (NHS).
NICE is recommending pomalidomide be available for use in combination with low-dose dexamethasone to treat adults with multiple myeloma who have received at least 3 previous treatments, including lenalidomide and bortezomib.
NICE previously evaluated pomalidomide in 2015 and said it could not recommend the drug, as analyses suggested pomalidomide doesn’t provide enough benefit to justify its high price.
Since that time, a committee advising NICE has reviewed additional data on pomalidomide.
And Celgene, the company that makes pomalidomide, has agreed to provide the NHS with a discount.
The cost of pomalidomide is £8884 per 21-tablet pack (excluding tax). The average cost of a course of treatment is £44,420 (excluding tax).
The discount Celgene will provide to the NHS is confidential.
NICE’s final appraisal determination on pomalidomide is now with consultees who have the opportunity to appeal against it. If there is no appeal, or an appeal is not upheld, the final appraisal determination is issued by NICE as a guidance.
The final guidance is expected in January 2017. Once NICE issues a final guidance on pomalidomide, the NHS must make the drug available within 3 months.

Photo from Business Wire
The National Institute for Health and Care Excellence (NICE) has issued a final appraisal determination recommending that pomalidomide be made available through the National Health Service (NHS).
NICE is recommending pomalidomide be available for use in combination with low-dose dexamethasone to treat adults with multiple myeloma who have received at least 3 previous treatments, including lenalidomide and bortezomib.
NICE previously evaluated pomalidomide in 2015 and said it could not recommend the drug, as analyses suggested pomalidomide doesn’t provide enough benefit to justify its high price.
Since that time, a committee advising NICE has reviewed additional data on pomalidomide.
And Celgene, the company that makes pomalidomide, has agreed to provide the NHS with a discount.
The cost of pomalidomide is £8884 per 21-tablet pack (excluding tax). The average cost of a course of treatment is £44,420 (excluding tax).
The discount Celgene will provide to the NHS is confidential.
NICE’s final appraisal determination on pomalidomide is now with consultees who have the opportunity to appeal against it. If there is no appeal, or an appeal is not upheld, the final appraisal determination is issued by NICE as a guidance.
The final guidance is expected in January 2017. Once NICE issues a final guidance on pomalidomide, the NHS must make the drug available within 3 months.
NICE recommends taking ibrutinib off CDF

Photo courtesy of Janssen
The National Institute for Health and Care Excellence (NICE) has issued a final appraisal determination recommending that ibrutinib come off the Cancer Drugs Fund (CDF) and be made available through the National Health Service (NHS).
Ibrutinib is a Bruton’s tyrosine kinase inhibitor approved by the European Commission treat patients with chronic lymphocytic leukemia (CLL).
NICE is recommending that ibrutinib be made available through the NHS for previously treated CLL patients and untreated CLL patients who have 17p deletion or TP53 mutation.
This means patients will no longer have to apply to the CDF to obtain ibrutinib. The CDF is money the English government sets aside to pay for cancer drugs that haven’t been approved by NICE and aren’t available within the NHS.
Though certain NICE products and services are provided to Wales, Scotland, and Northern Ireland, the governments of these countries do not have a CDF
or similar program.
Following the decision to reform the CDF earlier this year, NICE began to reappraise all drugs in the CDF in April.
New recommendation
NICE previously said it could not recommend ibrutinib for routine NHS use. However, Janssen, the company that makes ibrutinib, agreed to reduce the
price of the drug for the NHS. Because of the discount, an independent appraisal committee was able to deem ibrutinib cost-effective.
The list price for a single tablet of ibrutinib (140 mg) is £51.10 (excluding tax). The cost of a year’s course of ibrutinib treatment is £55,954.50 (excluding tax).
The discount the NHS will receive is confidential. The Department of Health said the cost of ibrutinib will not constitute an excessive administrative burden on the NHS.
NICE’s final appraisal determination on ibrutinib is now with consultees who have the opportunity to appeal against it. If there is no appeal, or an appeal is not upheld, the final appraisal determination is issued by NICE as a guidance.
Once NICE issues a final guidance on ibrutinib, the NHS must make the drug available within 3 months.

Photo courtesy of Janssen
The National Institute for Health and Care Excellence (NICE) has issued a final appraisal determination recommending that ibrutinib come off the Cancer Drugs Fund (CDF) and be made available through the National Health Service (NHS).
Ibrutinib is a Bruton’s tyrosine kinase inhibitor approved by the European Commission treat patients with chronic lymphocytic leukemia (CLL).
NICE is recommending that ibrutinib be made available through the NHS for previously treated CLL patients and untreated CLL patients who have 17p deletion or TP53 mutation.
This means patients will no longer have to apply to the CDF to obtain ibrutinib. The CDF is money the English government sets aside to pay for cancer drugs that haven’t been approved by NICE and aren’t available within the NHS.
Though certain NICE products and services are provided to Wales, Scotland, and Northern Ireland, the governments of these countries do not have a CDF
or similar program.
Following the decision to reform the CDF earlier this year, NICE began to reappraise all drugs in the CDF in April.
New recommendation
NICE previously said it could not recommend ibrutinib for routine NHS use. However, Janssen, the company that makes ibrutinib, agreed to reduce the
price of the drug for the NHS. Because of the discount, an independent appraisal committee was able to deem ibrutinib cost-effective.
The list price for a single tablet of ibrutinib (140 mg) is £51.10 (excluding tax). The cost of a year’s course of ibrutinib treatment is £55,954.50 (excluding tax).
The discount the NHS will receive is confidential. The Department of Health said the cost of ibrutinib will not constitute an excessive administrative burden on the NHS.
NICE’s final appraisal determination on ibrutinib is now with consultees who have the opportunity to appeal against it. If there is no appeal, or an appeal is not upheld, the final appraisal determination is issued by NICE as a guidance.
Once NICE issues a final guidance on ibrutinib, the NHS must make the drug available within 3 months.

Photo courtesy of Janssen
The National Institute for Health and Care Excellence (NICE) has issued a final appraisal determination recommending that ibrutinib come off the Cancer Drugs Fund (CDF) and be made available through the National Health Service (NHS).
Ibrutinib is a Bruton’s tyrosine kinase inhibitor approved by the European Commission treat patients with chronic lymphocytic leukemia (CLL).
NICE is recommending that ibrutinib be made available through the NHS for previously treated CLL patients and untreated CLL patients who have 17p deletion or TP53 mutation.
This means patients will no longer have to apply to the CDF to obtain ibrutinib. The CDF is money the English government sets aside to pay for cancer drugs that haven’t been approved by NICE and aren’t available within the NHS.
Though certain NICE products and services are provided to Wales, Scotland, and Northern Ireland, the governments of these countries do not have a CDF
or similar program.
Following the decision to reform the CDF earlier this year, NICE began to reappraise all drugs in the CDF in April.
New recommendation
NICE previously said it could not recommend ibrutinib for routine NHS use. However, Janssen, the company that makes ibrutinib, agreed to reduce the
price of the drug for the NHS. Because of the discount, an independent appraisal committee was able to deem ibrutinib cost-effective.
The list price for a single tablet of ibrutinib (140 mg) is £51.10 (excluding tax). The cost of a year’s course of ibrutinib treatment is £55,954.50 (excluding tax).
The discount the NHS will receive is confidential. The Department of Health said the cost of ibrutinib will not constitute an excessive administrative burden on the NHS.
NICE’s final appraisal determination on ibrutinib is now with consultees who have the opportunity to appeal against it. If there is no appeal, or an appeal is not upheld, the final appraisal determination is issued by NICE as a guidance.
Once NICE issues a final guidance on ibrutinib, the NHS must make the drug available within 3 months.
FDA grants full approval for ponatinib
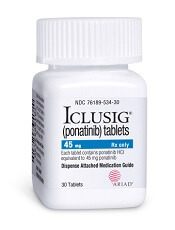
Photo from Business Wire
The US Food and Drug Administration (FDA) has granted full approval for the kinase inhibitor ponatinib (Iclusig®) and updated the drug’s label.
Ponatinib now has full approval as a treatment for adults with chronic myeloid leukemia (CML) or Philadelphia chromosome-positive acute lymphoblastic leukemia (Ph+ ALL) when no other tyrosine kinase inhibitor is indicated.
Ponatinib is also approved to treat adults with T315I-positive CML or T315I-positive Ph+ ALL.
Ponatinib was initially approved in December 2012 under the FDA’s accelerated approval program.
This program allows the FDA to approve a drug to treat a serious or life-threatening disease based on clinical data showing the drug has an effect on a surrogate endpoint reasonably likely to predict clinical benefit to patients.
The company developing the drug must conduct post-approval research to determine if the drug provides a clinical benefit. If so, the drug can be granted full approval.
The full approval and label update for ponatinib is based on 48-month follow-up data (as of August 2015) from the phase 2 PACE trial, which enrolled heavily pretreated patients with resistant or intolerant CML or Ph+ ALL. These data were presented at the 2016 ASCO Annual Meeting.
“The longer follow up of the PACE study confirms the clinical benefit of ponatinib in this setting,” said Jorge Cortes, MD, a professor at The University of Texas MD Anderson Cancer Center in Houston and a leading investigator in the PACE trial.
“We had learned from the initial report of the high response rate with ponatinib among CML patients with resistance or intolerance to prior therapies. The 4-year follow-up and updated safety profile demonstrate durability of responses in this heavily pretreated population. These results solidify ponatinib as an important and valuable treatment option for refractory patients with CML where no other TKI therapy is appropriate, including those who have the T315I mutation.”
Past problems with ponatinib
Previous follow-up data from the PACE trial, collected in 2013, suggested ponatinib can increase the risk of thrombotic events. When these data came to light, officials in the US and European Union, where ponatinib had already been approved, began to investigate the drug.
Ponatinib was pulled from the US market for a little over 2 months, and trials of the drug were placed on partial hold while the FDA evaluated the drug’s safety. Ponatinib went back on the market in January 2014, with new safety measures in place.
Ponatinib was not pulled from the market in the European Union, but the European Medicine’s Agency released recommendations for safer use of the drug. The Committee for Medicinal Products for Human Use reviewed data on ponatinib and decided its benefits outweigh its risks.
Photo from Business Wire
The US Food and Drug Administration (FDA) has granted full approval for the kinase inhibitor ponatinib (Iclusig®) and updated the drug’s label.
Ponatinib now has full approval as a treatment for adults with chronic myeloid leukemia (CML) or Philadelphia chromosome-positive acute lymphoblastic leukemia (Ph+ ALL) when no other tyrosine kinase inhibitor is indicated.
Ponatinib is also approved to treat adults with T315I-positive CML or T315I-positive Ph+ ALL.
Ponatinib was initially approved in December 2012 under the FDA’s accelerated approval program.
This program allows the FDA to approve a drug to treat a serious or life-threatening disease based on clinical data showing the drug has an effect on a surrogate endpoint reasonably likely to predict clinical benefit to patients.
The company developing the drug must conduct post-approval research to determine if the drug provides a clinical benefit. If so, the drug can be granted full approval.
The full approval and label update for ponatinib is based on 48-month follow-up data (as of August 2015) from the phase 2 PACE trial, which enrolled heavily pretreated patients with resistant or intolerant CML or Ph+ ALL. These data were presented at the 2016 ASCO Annual Meeting.
“The longer follow up of the PACE study confirms the clinical benefit of ponatinib in this setting,” said Jorge Cortes, MD, a professor at The University of Texas MD Anderson Cancer Center in Houston and a leading investigator in the PACE trial.
“We had learned from the initial report of the high response rate with ponatinib among CML patients with resistance or intolerance to prior therapies. The 4-year follow-up and updated safety profile demonstrate durability of responses in this heavily pretreated population. These results solidify ponatinib as an important and valuable treatment option for refractory patients with CML where no other TKI therapy is appropriate, including those who have the T315I mutation.”
Past problems with ponatinib
Previous follow-up data from the PACE trial, collected in 2013, suggested ponatinib can increase the risk of thrombotic events. When these data came to light, officials in the US and European Union, where ponatinib had already been approved, began to investigate the drug.
Ponatinib was pulled from the US market for a little over 2 months, and trials of the drug were placed on partial hold while the FDA evaluated the drug’s safety. Ponatinib went back on the market in January 2014, with new safety measures in place.
Ponatinib was not pulled from the market in the European Union, but the European Medicine’s Agency released recommendations for safer use of the drug. The Committee for Medicinal Products for Human Use reviewed data on ponatinib and decided its benefits outweigh its risks.
Photo from Business Wire
The US Food and Drug Administration (FDA) has granted full approval for the kinase inhibitor ponatinib (Iclusig®) and updated the drug’s label.
Ponatinib now has full approval as a treatment for adults with chronic myeloid leukemia (CML) or Philadelphia chromosome-positive acute lymphoblastic leukemia (Ph+ ALL) when no other tyrosine kinase inhibitor is indicated.
Ponatinib is also approved to treat adults with T315I-positive CML or T315I-positive Ph+ ALL.
Ponatinib was initially approved in December 2012 under the FDA’s accelerated approval program.
This program allows the FDA to approve a drug to treat a serious or life-threatening disease based on clinical data showing the drug has an effect on a surrogate endpoint reasonably likely to predict clinical benefit to patients.
The company developing the drug must conduct post-approval research to determine if the drug provides a clinical benefit. If so, the drug can be granted full approval.
The full approval and label update for ponatinib is based on 48-month follow-up data (as of August 2015) from the phase 2 PACE trial, which enrolled heavily pretreated patients with resistant or intolerant CML or Ph+ ALL. These data were presented at the 2016 ASCO Annual Meeting.
“The longer follow up of the PACE study confirms the clinical benefit of ponatinib in this setting,” said Jorge Cortes, MD, a professor at The University of Texas MD Anderson Cancer Center in Houston and a leading investigator in the PACE trial.
“We had learned from the initial report of the high response rate with ponatinib among CML patients with resistance or intolerance to prior therapies. The 4-year follow-up and updated safety profile demonstrate durability of responses in this heavily pretreated population. These results solidify ponatinib as an important and valuable treatment option for refractory patients with CML where no other TKI therapy is appropriate, including those who have the T315I mutation.”
Past problems with ponatinib
Previous follow-up data from the PACE trial, collected in 2013, suggested ponatinib can increase the risk of thrombotic events. When these data came to light, officials in the US and European Union, where ponatinib had already been approved, began to investigate the drug.
Ponatinib was pulled from the US market for a little over 2 months, and trials of the drug were placed on partial hold while the FDA evaluated the drug’s safety. Ponatinib went back on the market in January 2014, with new safety measures in place.
Ponatinib was not pulled from the market in the European Union, but the European Medicine’s Agency released recommendations for safer use of the drug. The Committee for Medicinal Products for Human Use reviewed data on ponatinib and decided its benefits outweigh its risks.