User login
Genetics of Asthma
Severe Asthma Combination Therapy
History of nonproductive cough
The history and findings in this case are suggestive of eosinophilic asthma.
Asthma is a common, chronic, and heterogeneous respiratory disease, most often characterized by chronic airway inflammation. Affected individuals experience respiratory symptoms (ie, wheezing, dyspnea, chest tightness, and cough) that may fluctuate over time and in intensity, as well as variable expiratory airflow limitation, which may become persistent. For many patients, asthma has a significant impact on quality of life. According to the World Health Organization, asthma affected an estimated 262 million people and caused 455,000 deaths. Currently, approximately 334 million people worldwide are believed to be affected by asthma.
Asthma frequently begins in childhood, but adult-onset asthma can occur and often presents as a nonatopic and eosinophilic condition. In fact, asthma is an umbrella diagnosis that encompasses several diseases with distinct mechanistic pathways (endotypes) and variable clinical presentations (phenotypes), all of which manifest with respiratory symptoms and are accompanied by variable airflow obstruction.
Broadly, asthma endotypes are categorized as type 2 (T2)-high or T2-low. Eosinophilic asthma falls under the T2-high endotype and comprises three phenotypes: atopic, late-onset, and aspirin-exacerbated respiratory disease. Late-onset T2-high asthma is characterized by prominent blood and sputum eosinophilia and is refractory to inhaled/oral corticosteroid treatment. Patients in this subgroup tend to be older and have more severe asthma with fixed airflow obstruction and more frequent exacerbations; patients may also have comorbid chronic rhinosinusitis with nasal polyps, which usually precedes asthma development. High FeNO levels and normal or elevated serum total IgE levels are also often seen in this subgroup.
The late-onset eosinophilic asthma phenotype accounts for 20%-40% of severe asthma cases and is associated with rapid decline of respiratory functions. Thus, earlier escalation of therapy may be indicated in patients with this phenotype.
According to a 2022 report from the Global Initiative for Asthma, the possibility of refractory T2 asthma should be considered when any of the following is found in patients taking high-dose ICS or daily oral corticosteroids:
• Blood eosinophils ≥ 150/μL, and/or
• FeNO ≥ 20 ppb, and/or
• Sputum eosinophils ≥ 2%, and/or
• Asthma is clinically allergen driven
Biologic T2-targeted therapies are available as add-on therapies for patients with T2 airway inflammation and severe asthma despite taking at least a high-dose ICS-LABA, and who have eosinophilic or allergic biomarkers or need maintenance oral corticosteroids. Available options for eosinophilic asthma include anti-interleukin (IL)-5/anti-IL-5R therapies (benralizumab, mepolizumab, reslizumab) and anti-IL-4R therapy (dupilumab).
Zab Mosenifar, MD, Medical Director, Women's Lung Institute; Executive Vice Chairman, Department of Medicine, Cedars Sinai Medical Center, Los Angeles, California.
Zab Mosenifar, MD, has disclosed no relevant financial relationships.
Image Quizzes are fictional or fictionalized clinical scenarios intended to provide evidence-based educational takeaways.
The history and findings in this case are suggestive of eosinophilic asthma.
Asthma is a common, chronic, and heterogeneous respiratory disease, most often characterized by chronic airway inflammation. Affected individuals experience respiratory symptoms (ie, wheezing, dyspnea, chest tightness, and cough) that may fluctuate over time and in intensity, as well as variable expiratory airflow limitation, which may become persistent. For many patients, asthma has a significant impact on quality of life. According to the World Health Organization, asthma affected an estimated 262 million people and caused 455,000 deaths. Currently, approximately 334 million people worldwide are believed to be affected by asthma.
Asthma frequently begins in childhood, but adult-onset asthma can occur and often presents as a nonatopic and eosinophilic condition. In fact, asthma is an umbrella diagnosis that encompasses several diseases with distinct mechanistic pathways (endotypes) and variable clinical presentations (phenotypes), all of which manifest with respiratory symptoms and are accompanied by variable airflow obstruction.
Broadly, asthma endotypes are categorized as type 2 (T2)-high or T2-low. Eosinophilic asthma falls under the T2-high endotype and comprises three phenotypes: atopic, late-onset, and aspirin-exacerbated respiratory disease. Late-onset T2-high asthma is characterized by prominent blood and sputum eosinophilia and is refractory to inhaled/oral corticosteroid treatment. Patients in this subgroup tend to be older and have more severe asthma with fixed airflow obstruction and more frequent exacerbations; patients may also have comorbid chronic rhinosinusitis with nasal polyps, which usually precedes asthma development. High FeNO levels and normal or elevated serum total IgE levels are also often seen in this subgroup.
The late-onset eosinophilic asthma phenotype accounts for 20%-40% of severe asthma cases and is associated with rapid decline of respiratory functions. Thus, earlier escalation of therapy may be indicated in patients with this phenotype.
According to a 2022 report from the Global Initiative for Asthma, the possibility of refractory T2 asthma should be considered when any of the following is found in patients taking high-dose ICS or daily oral corticosteroids:
• Blood eosinophils ≥ 150/μL, and/or
• FeNO ≥ 20 ppb, and/or
• Sputum eosinophils ≥ 2%, and/or
• Asthma is clinically allergen driven
Biologic T2-targeted therapies are available as add-on therapies for patients with T2 airway inflammation and severe asthma despite taking at least a high-dose ICS-LABA, and who have eosinophilic or allergic biomarkers or need maintenance oral corticosteroids. Available options for eosinophilic asthma include anti-interleukin (IL)-5/anti-IL-5R therapies (benralizumab, mepolizumab, reslizumab) and anti-IL-4R therapy (dupilumab).
Zab Mosenifar, MD, Medical Director, Women's Lung Institute; Executive Vice Chairman, Department of Medicine, Cedars Sinai Medical Center, Los Angeles, California.
Zab Mosenifar, MD, has disclosed no relevant financial relationships.
Image Quizzes are fictional or fictionalized clinical scenarios intended to provide evidence-based educational takeaways.
The history and findings in this case are suggestive of eosinophilic asthma.
Asthma is a common, chronic, and heterogeneous respiratory disease, most often characterized by chronic airway inflammation. Affected individuals experience respiratory symptoms (ie, wheezing, dyspnea, chest tightness, and cough) that may fluctuate over time and in intensity, as well as variable expiratory airflow limitation, which may become persistent. For many patients, asthma has a significant impact on quality of life. According to the World Health Organization, asthma affected an estimated 262 million people and caused 455,000 deaths. Currently, approximately 334 million people worldwide are believed to be affected by asthma.
Asthma frequently begins in childhood, but adult-onset asthma can occur and often presents as a nonatopic and eosinophilic condition. In fact, asthma is an umbrella diagnosis that encompasses several diseases with distinct mechanistic pathways (endotypes) and variable clinical presentations (phenotypes), all of which manifest with respiratory symptoms and are accompanied by variable airflow obstruction.
Broadly, asthma endotypes are categorized as type 2 (T2)-high or T2-low. Eosinophilic asthma falls under the T2-high endotype and comprises three phenotypes: atopic, late-onset, and aspirin-exacerbated respiratory disease. Late-onset T2-high asthma is characterized by prominent blood and sputum eosinophilia and is refractory to inhaled/oral corticosteroid treatment. Patients in this subgroup tend to be older and have more severe asthma with fixed airflow obstruction and more frequent exacerbations; patients may also have comorbid chronic rhinosinusitis with nasal polyps, which usually precedes asthma development. High FeNO levels and normal or elevated serum total IgE levels are also often seen in this subgroup.
The late-onset eosinophilic asthma phenotype accounts for 20%-40% of severe asthma cases and is associated with rapid decline of respiratory functions. Thus, earlier escalation of therapy may be indicated in patients with this phenotype.
According to a 2022 report from the Global Initiative for Asthma, the possibility of refractory T2 asthma should be considered when any of the following is found in patients taking high-dose ICS or daily oral corticosteroids:
• Blood eosinophils ≥ 150/μL, and/or
• FeNO ≥ 20 ppb, and/or
• Sputum eosinophils ≥ 2%, and/or
• Asthma is clinically allergen driven
Biologic T2-targeted therapies are available as add-on therapies for patients with T2 airway inflammation and severe asthma despite taking at least a high-dose ICS-LABA, and who have eosinophilic or allergic biomarkers or need maintenance oral corticosteroids. Available options for eosinophilic asthma include anti-interleukin (IL)-5/anti-IL-5R therapies (benralizumab, mepolizumab, reslizumab) and anti-IL-4R therapy (dupilumab).
Zab Mosenifar, MD, Medical Director, Women's Lung Institute; Executive Vice Chairman, Department of Medicine, Cedars Sinai Medical Center, Los Angeles, California.
Zab Mosenifar, MD, has disclosed no relevant financial relationships.
Image Quizzes are fictional or fictionalized clinical scenarios intended to provide evidence-based educational takeaways.
A 42-year-old nonsmoking man presents with complaints of a 9-month history of wheezing, nonproductive cough, and exertional dyspnea. The patient reports nighttime awakenings from his symptoms three to five times per month. He was diagnosed with asthma by his primary care provider about 3 months after his symptoms began. On diagnosis, he was prescribed a short-acting beta-2 adrenergic agonist rescue inhaler and an inhaled corticosteroid (ICS), twice daily. Because the patient remained symptomatic, his primary care provider stepped up his daily therapy to a combined ICS and long-acting beta2-adrenergic agonist (LABA). At today's visit, the patient reports continued symptoms and use of his rescue inhaler at least twice per week. He has no other significant medical history aside from a history of mild atopic dermatitis. He is 5 ft 11 in and currently weighs 172 lb (BMI 24). He demonstrates proper inhaler technique and states that he is compliant with his therapy.
Physical examination reveals loud wheezing during inspiration and throughout expiration. The patient's heart rate is 110 beats/min; blood pressure is 130/70 mm Hg. Pulse oximetry is 93%. Spirometry reveals a forced expiratory volume in the first second (FEV1) of 78% predicted. Fractional exhaled nitric oxide (FeNO) is 56 ppb. Chest radiography is normal. High-resolution CT shows air trapping, mosaic lung attenuations, and bronchial wall thickening. IgE level is normal; sputum culture reveals 6% eosinophils.
Severe Asthma Guidelines
Pediatric Asthma
Chest tightness and wheezing
This patient's physical examination and imaging findings are consistent with a diagnosis of acute severe asthma. Agitation, breathlessness during rest, and a respiratory rate > 30 breaths/min are some manifestations of an acute severe episode. During severe episodes, accessory muscles of respiration are usually used, and suprasternal retractions are often present. The heart rate is > 120 beats/min and the respiratory rate is > 30 breaths/min. Loud biphasic (expiratory and inspiratory) wheezing can be heard, and pulsus paradoxus is often present (20-40 mm Hg). Oxyhemoglobin saturation with room air is < 91%. As the severity increases, the patient increasingly assumes a hunched-over sitting position with the hands supporting the torso, termed the tripod position.
Asthma is a chronic, heterogenous inflammatory airway disorder characterized by variable expiratory flow; airway wall thickening; respiratory symptoms; and exacerbations, which sometimes require hospitalization. According to the World Health Organization, asthma affected an estimated 262 million people in 2019. The presence of airway hyperresponsiveness or bronchial hyperreactivity in asthma is an exaggerated response to various exogenous and endogenous stimuli. Mechanisms implicated in the development of asthma include direct stimulation of airway smooth muscle and indirect stimulation by pharmacologically active substances from mediator-secreting cells, such as mast cells or nonmyelinated sensory neurons. The degree of airway hyperresponsiveness is associated with the clinical severity of asthma.
Acute severe asthma is a life-threatening emergency characterized by severe airflow limitation that is unresponsive to the typical appropriate bronchodilator therapy. As a result of pathophysiologic changes, airflow is severely restricted in severe asthma, leading to premature closure of the airway on expiration; impaired gas exchange; and dynamic hyperinflation, or air-trapping. In such cases, urgent action is essential to thwart serious outcomes, including mechanical ventilation and death.
Asthma severity is defined by the level of treatment required to control a patient's symptoms and exacerbations. According to the 2022 Global Initiative for Asthma (GINA) guidelines, a severe asthma exacerbation describes a patient who talks in words (rather than sentences); leans forward; is agitated; uses accessory respiratory muscles; and has a respiratory rate > 30 breaths/min, heart rate > 120 beats/min, oxygen saturation on air < 90%, and peak expiratory flow ≤ 50% of their best or of predicted value. Given the heterogeneity of asthma, patients with acute severe asthma may present with a variety of signs and symptoms, including dyspnea, chest tightness, cough and wheezing, agitation, drowsiness or signs of confusion, and significant breathlessness at rest.
Exposure to external agents, such as indoor and outdoor allergens, air pollutants, and respiratory tract infections (primarily viral), are the most common causes of asthma exacerbations, which vary in severity. Numerous other factors can trigger an asthma exacerbation, including exercise, weather changes, certain foods, additives, drugs, extreme emotional expressions, rhinitis, sinusitis, polyposis, gastroesophageal reflux, menstruation, and pregnancy. Importantly, a patient with known asthma of any level of severity can experience an asthma exacerbation, including patients with mild or well-controlled asthma.
Patients with a history of poorly controlled asthma or a recent exacerbation are at risk for an acute asthma exacerbation. Other risk factors include poor perception of airflow limitation, regular or overuse of short-acting beta agonists, incorrect inhaler technique, and suboptimal adherence to therapy. Comorbidities associated with risk for an acute asthma exacerbation include obesity, chronic rhinosinusitis, inducible laryngeal obstruction (vocal cord dysfunction), gastroesophageal reflux disease, chronic obstructive pulmonary disease, obstructive sleep apnea, bronchiectasis, cardiac disease, and kyphosis due to osteoporosis (followed by corticosteroid overuse). The lack of a written asthma action plan and socioeconomic factors are also associated with increased risk for a severe exacerbation.
In the emergency department setting, pharmacologic therapy of acute severe asthma should consist of a short-acting beta agonist, ipratropium bromide, systemic corticosteroids (oral or intravenous), and controlled oxygen therapy. Clinicians may also consider intravenous magnesium sulfate and high-dose inhaled corticosteroids. Once stable, patients should be treated with optimal asthma-controlling therapy, as outlined in GINA guidelines. Optimizing patients' inhaler technique and adherence to therapy are imperative, and comorbidities should be appropriately managed. Nonpharmacologic interventions, such as smoking cessation, pulmonary rehabilitation, exercise, weight loss, and influenza/COVID-19 vaccination, are also recommended as indicated.
Zab Mosenifar, MD, Medical Director, Women's Lung Institute; Executive Vice Chairman, Department of Medicine, Cedars Sinai Medical Center, Los Angeles, California.
Zab Mosenifar, MD, has disclosed no relevant financial relationships.
Image Quizzes are fictional or fictionalized clinical scenarios intended to provide evidence-based educational takeaways.
This patient's physical examination and imaging findings are consistent with a diagnosis of acute severe asthma. Agitation, breathlessness during rest, and a respiratory rate > 30 breaths/min are some manifestations of an acute severe episode. During severe episodes, accessory muscles of respiration are usually used, and suprasternal retractions are often present. The heart rate is > 120 beats/min and the respiratory rate is > 30 breaths/min. Loud biphasic (expiratory and inspiratory) wheezing can be heard, and pulsus paradoxus is often present (20-40 mm Hg). Oxyhemoglobin saturation with room air is < 91%. As the severity increases, the patient increasingly assumes a hunched-over sitting position with the hands supporting the torso, termed the tripod position.
Asthma is a chronic, heterogenous inflammatory airway disorder characterized by variable expiratory flow; airway wall thickening; respiratory symptoms; and exacerbations, which sometimes require hospitalization. According to the World Health Organization, asthma affected an estimated 262 million people in 2019. The presence of airway hyperresponsiveness or bronchial hyperreactivity in asthma is an exaggerated response to various exogenous and endogenous stimuli. Mechanisms implicated in the development of asthma include direct stimulation of airway smooth muscle and indirect stimulation by pharmacologically active substances from mediator-secreting cells, such as mast cells or nonmyelinated sensory neurons. The degree of airway hyperresponsiveness is associated with the clinical severity of asthma.
Acute severe asthma is a life-threatening emergency characterized by severe airflow limitation that is unresponsive to the typical appropriate bronchodilator therapy. As a result of pathophysiologic changes, airflow is severely restricted in severe asthma, leading to premature closure of the airway on expiration; impaired gas exchange; and dynamic hyperinflation, or air-trapping. In such cases, urgent action is essential to thwart serious outcomes, including mechanical ventilation and death.
Asthma severity is defined by the level of treatment required to control a patient's symptoms and exacerbations. According to the 2022 Global Initiative for Asthma (GINA) guidelines, a severe asthma exacerbation describes a patient who talks in words (rather than sentences); leans forward; is agitated; uses accessory respiratory muscles; and has a respiratory rate > 30 breaths/min, heart rate > 120 beats/min, oxygen saturation on air < 90%, and peak expiratory flow ≤ 50% of their best or of predicted value. Given the heterogeneity of asthma, patients with acute severe asthma may present with a variety of signs and symptoms, including dyspnea, chest tightness, cough and wheezing, agitation, drowsiness or signs of confusion, and significant breathlessness at rest.
Exposure to external agents, such as indoor and outdoor allergens, air pollutants, and respiratory tract infections (primarily viral), are the most common causes of asthma exacerbations, which vary in severity. Numerous other factors can trigger an asthma exacerbation, including exercise, weather changes, certain foods, additives, drugs, extreme emotional expressions, rhinitis, sinusitis, polyposis, gastroesophageal reflux, menstruation, and pregnancy. Importantly, a patient with known asthma of any level of severity can experience an asthma exacerbation, including patients with mild or well-controlled asthma.
Patients with a history of poorly controlled asthma or a recent exacerbation are at risk for an acute asthma exacerbation. Other risk factors include poor perception of airflow limitation, regular or overuse of short-acting beta agonists, incorrect inhaler technique, and suboptimal adherence to therapy. Comorbidities associated with risk for an acute asthma exacerbation include obesity, chronic rhinosinusitis, inducible laryngeal obstruction (vocal cord dysfunction), gastroesophageal reflux disease, chronic obstructive pulmonary disease, obstructive sleep apnea, bronchiectasis, cardiac disease, and kyphosis due to osteoporosis (followed by corticosteroid overuse). The lack of a written asthma action plan and socioeconomic factors are also associated with increased risk for a severe exacerbation.
In the emergency department setting, pharmacologic therapy of acute severe asthma should consist of a short-acting beta agonist, ipratropium bromide, systemic corticosteroids (oral or intravenous), and controlled oxygen therapy. Clinicians may also consider intravenous magnesium sulfate and high-dose inhaled corticosteroids. Once stable, patients should be treated with optimal asthma-controlling therapy, as outlined in GINA guidelines. Optimizing patients' inhaler technique and adherence to therapy are imperative, and comorbidities should be appropriately managed. Nonpharmacologic interventions, such as smoking cessation, pulmonary rehabilitation, exercise, weight loss, and influenza/COVID-19 vaccination, are also recommended as indicated.
Zab Mosenifar, MD, Medical Director, Women's Lung Institute; Executive Vice Chairman, Department of Medicine, Cedars Sinai Medical Center, Los Angeles, California.
Zab Mosenifar, MD, has disclosed no relevant financial relationships.
Image Quizzes are fictional or fictionalized clinical scenarios intended to provide evidence-based educational takeaways.
This patient's physical examination and imaging findings are consistent with a diagnosis of acute severe asthma. Agitation, breathlessness during rest, and a respiratory rate > 30 breaths/min are some manifestations of an acute severe episode. During severe episodes, accessory muscles of respiration are usually used, and suprasternal retractions are often present. The heart rate is > 120 beats/min and the respiratory rate is > 30 breaths/min. Loud biphasic (expiratory and inspiratory) wheezing can be heard, and pulsus paradoxus is often present (20-40 mm Hg). Oxyhemoglobin saturation with room air is < 91%. As the severity increases, the patient increasingly assumes a hunched-over sitting position with the hands supporting the torso, termed the tripod position.
Asthma is a chronic, heterogenous inflammatory airway disorder characterized by variable expiratory flow; airway wall thickening; respiratory symptoms; and exacerbations, which sometimes require hospitalization. According to the World Health Organization, asthma affected an estimated 262 million people in 2019. The presence of airway hyperresponsiveness or bronchial hyperreactivity in asthma is an exaggerated response to various exogenous and endogenous stimuli. Mechanisms implicated in the development of asthma include direct stimulation of airway smooth muscle and indirect stimulation by pharmacologically active substances from mediator-secreting cells, such as mast cells or nonmyelinated sensory neurons. The degree of airway hyperresponsiveness is associated with the clinical severity of asthma.
Acute severe asthma is a life-threatening emergency characterized by severe airflow limitation that is unresponsive to the typical appropriate bronchodilator therapy. As a result of pathophysiologic changes, airflow is severely restricted in severe asthma, leading to premature closure of the airway on expiration; impaired gas exchange; and dynamic hyperinflation, or air-trapping. In such cases, urgent action is essential to thwart serious outcomes, including mechanical ventilation and death.
Asthma severity is defined by the level of treatment required to control a patient's symptoms and exacerbations. According to the 2022 Global Initiative for Asthma (GINA) guidelines, a severe asthma exacerbation describes a patient who talks in words (rather than sentences); leans forward; is agitated; uses accessory respiratory muscles; and has a respiratory rate > 30 breaths/min, heart rate > 120 beats/min, oxygen saturation on air < 90%, and peak expiratory flow ≤ 50% of their best or of predicted value. Given the heterogeneity of asthma, patients with acute severe asthma may present with a variety of signs and symptoms, including dyspnea, chest tightness, cough and wheezing, agitation, drowsiness or signs of confusion, and significant breathlessness at rest.
Exposure to external agents, such as indoor and outdoor allergens, air pollutants, and respiratory tract infections (primarily viral), are the most common causes of asthma exacerbations, which vary in severity. Numerous other factors can trigger an asthma exacerbation, including exercise, weather changes, certain foods, additives, drugs, extreme emotional expressions, rhinitis, sinusitis, polyposis, gastroesophageal reflux, menstruation, and pregnancy. Importantly, a patient with known asthma of any level of severity can experience an asthma exacerbation, including patients with mild or well-controlled asthma.
Patients with a history of poorly controlled asthma or a recent exacerbation are at risk for an acute asthma exacerbation. Other risk factors include poor perception of airflow limitation, regular or overuse of short-acting beta agonists, incorrect inhaler technique, and suboptimal adherence to therapy. Comorbidities associated with risk for an acute asthma exacerbation include obesity, chronic rhinosinusitis, inducible laryngeal obstruction (vocal cord dysfunction), gastroesophageal reflux disease, chronic obstructive pulmonary disease, obstructive sleep apnea, bronchiectasis, cardiac disease, and kyphosis due to osteoporosis (followed by corticosteroid overuse). The lack of a written asthma action plan and socioeconomic factors are also associated with increased risk for a severe exacerbation.
In the emergency department setting, pharmacologic therapy of acute severe asthma should consist of a short-acting beta agonist, ipratropium bromide, systemic corticosteroids (oral or intravenous), and controlled oxygen therapy. Clinicians may also consider intravenous magnesium sulfate and high-dose inhaled corticosteroids. Once stable, patients should be treated with optimal asthma-controlling therapy, as outlined in GINA guidelines. Optimizing patients' inhaler technique and adherence to therapy are imperative, and comorbidities should be appropriately managed. Nonpharmacologic interventions, such as smoking cessation, pulmonary rehabilitation, exercise, weight loss, and influenza/COVID-19 vaccination, are also recommended as indicated.
Zab Mosenifar, MD, Medical Director, Women's Lung Institute; Executive Vice Chairman, Department of Medicine, Cedars Sinai Medical Center, Los Angeles, California.
Zab Mosenifar, MD, has disclosed no relevant financial relationships.
Image Quizzes are fictional or fictionalized clinical scenarios intended to provide evidence-based educational takeaways.
A 32-year-old Black man presents to the emergency department with severe dyspnea, chest tightness, and wheezing. The patient is sitting forward in the tripod position and appears agitated and confused. Use of accessory respiratory muscles and suprasternal retractions are noted. He reports an approximate 2-week history of rhinorrhea, cough, and mild fever, for which he has been taking an over-the-counter nonsteroidal anti-inflammatory agent and cough suppressant. His prior medical history is notable for obesity, type 2 diabetes, allergic rhinitis, mild asthma, and hypercholesterolemia. The patient is a current smoker (17 pack-years). Pertinent physical examination reveals a respiratory rate of 48 breaths/min, heart rate of 135 beats/min, 87% oxygen saturation, and peak expiratory flow of 300 L/min. Low biphasic wheezing can be heard. Rapid antigen and PCR tests for SARS-CoV-2 detected by nasopharyngeal swabs both come back negative. Chest radiography is ordered and shows pulmonary hyperinflation with bronchial wall thickening.
Severe Asthma: Eosinophilic Asthma
Severe Asthma: Allergic Asthma
6-year-old with loud wheezing, difficulty breathing
The patient is probably presenting with a moderate asthma exacerbation. To confirm the diagnosis, spirometry assessments should be performed to establish the presence of baseline airway obstruction and determine its severity. Measurements should be obtained before and after inhalation of a short-acting bronchodilator. In addition, chest radiography can help to exclude other diagnoses, and pulse oximetry can exclude hypoxemia.
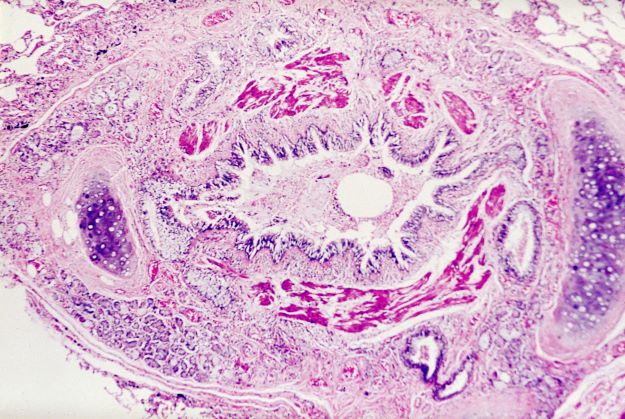
Asthma is a heterogeneous inflammatory disease and the most common chronic condition among children. Histologically, it is marked by vascular congestion, increased vascular permeability, increased tissue volume, and the presence of an exudate. Because the asthmatic lung undergoes a cycle of injury, repair, and regeneration, inflammation creates histologic changes and functional abnormalities in the airway mucosal epithelium. It is hypothesized that these changes play a major role in the pathophysiology of asthma.
Eosinophilic infiltration is a hallmark of this inflammatory activity. Histologic evaluations of the large airways may also reveal narrowing of lumina, bronchial and bronchiolar epithelial denudation, and mucus plugs. Other relevant findings can include epithelial desquamation and hyperplasia, goblet cell metaplasia, subbasement membrane thickening, smooth muscle hypertrophy or hyperplasia, and submucosal gland hypertrophy. In patients with severe asthma, the basement membrane may be significantly thickened. In terms of the small airways, pathologic study from the lungs of living patients is rarely undertaken, and therefore the histopathologic findings of asthma at the level of the distal airways and alveolated lung parenchyma remains largely unknown.
Asthma is treated using a stepwise approach. As directed for pediatric patients younger than 5 years, the patient in this case may be provided with an as-needed inhaled short-acting beta2-agonist (SABA) and should be followed up every 2-6 weeks while gaining control of her symptoms.
Nathan L. Boyer, MD, Assistant Professor, Department of Medicine, Uniformed Services University, Bethesda, Maryland; Chief of Critical Care, Landstuhl Regional Medical Center, Landstuhl, Germany.
Nathan L. Boyer, MD, has disclosed no relevant financial relationships.
Image Quizzes are fictional or fictionalized clinical scenarios intended to provide evidence-based educational takeaways.
The patient is probably presenting with a moderate asthma exacerbation. To confirm the diagnosis, spirometry assessments should be performed to establish the presence of baseline airway obstruction and determine its severity. Measurements should be obtained before and after inhalation of a short-acting bronchodilator. In addition, chest radiography can help to exclude other diagnoses, and pulse oximetry can exclude hypoxemia.
Asthma is a heterogeneous inflammatory disease and the most common chronic condition among children. Histologically, it is marked by vascular congestion, increased vascular permeability, increased tissue volume, and the presence of an exudate. Because the asthmatic lung undergoes a cycle of injury, repair, and regeneration, inflammation creates histologic changes and functional abnormalities in the airway mucosal epithelium. It is hypothesized that these changes play a major role in the pathophysiology of asthma.
Eosinophilic infiltration is a hallmark of this inflammatory activity. Histologic evaluations of the large airways may also reveal narrowing of lumina, bronchial and bronchiolar epithelial denudation, and mucus plugs. Other relevant findings can include epithelial desquamation and hyperplasia, goblet cell metaplasia, subbasement membrane thickening, smooth muscle hypertrophy or hyperplasia, and submucosal gland hypertrophy. In patients with severe asthma, the basement membrane may be significantly thickened. In terms of the small airways, pathologic study from the lungs of living patients is rarely undertaken, and therefore the histopathologic findings of asthma at the level of the distal airways and alveolated lung parenchyma remains largely unknown.
Asthma is treated using a stepwise approach. As directed for pediatric patients younger than 5 years, the patient in this case may be provided with an as-needed inhaled short-acting beta2-agonist (SABA) and should be followed up every 2-6 weeks while gaining control of her symptoms.
Nathan L. Boyer, MD, Assistant Professor, Department of Medicine, Uniformed Services University, Bethesda, Maryland; Chief of Critical Care, Landstuhl Regional Medical Center, Landstuhl, Germany.
Nathan L. Boyer, MD, has disclosed no relevant financial relationships.
Image Quizzes are fictional or fictionalized clinical scenarios intended to provide evidence-based educational takeaways.
The patient is probably presenting with a moderate asthma exacerbation. To confirm the diagnosis, spirometry assessments should be performed to establish the presence of baseline airway obstruction and determine its severity. Measurements should be obtained before and after inhalation of a short-acting bronchodilator. In addition, chest radiography can help to exclude other diagnoses, and pulse oximetry can exclude hypoxemia.
Asthma is a heterogeneous inflammatory disease and the most common chronic condition among children. Histologically, it is marked by vascular congestion, increased vascular permeability, increased tissue volume, and the presence of an exudate. Because the asthmatic lung undergoes a cycle of injury, repair, and regeneration, inflammation creates histologic changes and functional abnormalities in the airway mucosal epithelium. It is hypothesized that these changes play a major role in the pathophysiology of asthma.
Eosinophilic infiltration is a hallmark of this inflammatory activity. Histologic evaluations of the large airways may also reveal narrowing of lumina, bronchial and bronchiolar epithelial denudation, and mucus plugs. Other relevant findings can include epithelial desquamation and hyperplasia, goblet cell metaplasia, subbasement membrane thickening, smooth muscle hypertrophy or hyperplasia, and submucosal gland hypertrophy. In patients with severe asthma, the basement membrane may be significantly thickened. In terms of the small airways, pathologic study from the lungs of living patients is rarely undertaken, and therefore the histopathologic findings of asthma at the level of the distal airways and alveolated lung parenchyma remains largely unknown.
Asthma is treated using a stepwise approach. As directed for pediatric patients younger than 5 years, the patient in this case may be provided with an as-needed inhaled short-acting beta2-agonist (SABA) and should be followed up every 2-6 weeks while gaining control of her symptoms.
Nathan L. Boyer, MD, Assistant Professor, Department of Medicine, Uniformed Services University, Bethesda, Maryland; Chief of Critical Care, Landstuhl Regional Medical Center, Landstuhl, Germany.
Nathan L. Boyer, MD, has disclosed no relevant financial relationships.
Image Quizzes are fictional or fictionalized clinical scenarios intended to provide evidence-based educational takeaways.
A 6-year-old girl presents with loud wheezing, difficulty breathing, and nasal flaring. She becomes particularly breathless while talking. The only abnormalities on chest CT are reduced airway luminal area and mucus plugs. Heart rate is 110 beats/min. Oxyhemoglobin saturation with room air is 94%. Skin examination is nonrevealing. The patient's mother cannot identify any factors that may have precipitated the episode.