User login
What's your diagnosis?
Answer: Blue rubber bleb nevus syndrome.
According to an American College of Gastroenterology Clinical Guideline,1 for patients with recurrence of small bowel bleeding, endoscopic management could be considered depending on the patient’s clinical course and response to prior therapy. Consequently, injections of lauromacrogol with SBE (single-balloon enteroscopy) were given (Figure D). Lesions that ranged from 1 to 2 cm were injected with 1-2 mL lauromacrogol until the mucosa turned white. Three SBEs had been performed in a 5-month period. A total of 20 lesions were successfully treated with lauromacrogol. The treated hemangiomas became small, and the site healed 5 months after treatment (Figures E and F). The patient has been followed for 1 year, and he remains in good clinical condition with his latest hemoglobin level at 110 g/L. No further blood transfusion is needed.
BRBNS is a rare disorder characterized by discrete venous malformations of varying size and appearance that are present on the skin and within the gastrointestinal tract.2With wider application of video capsule endoscopy (VCE) and the increase of image resolution, the detection rate and diagnostic accuracy of BRBNS are significantly improved. Treatment of BRBNS varies depending on the site, size, and number of lesions. Medication, surgery, and endoscopic therapy are currently clinically applied. The successful use of sirolimus was recently reported in the treatment of vascular lesions.3Sirolimus has potential adverse effects on renal function, bone marrow, and cholesterol metabolism, however. In consideration of the patient’s young age, we did not adopt this method. Surgical resection is more suitable for limited or life-threatening lesions. The lesions in this patient were mild and sporadic. Consequently, in this case, endoscopic injection of lauromacrogol was performed. This was the most complicated case of endoscopic treatment of BRBNS in our center and proved lauromacrogol injection was a feasible approach. According to a literature review, lauromacrogol has been used to treat vascular lesions for decades, but there is still no standard instruction for the dosage of lauromacrogol. We hope that our experience can be a reference for the endoscopic treatment of BRBNS.
References (add links)
1. Gerson LB et al. ACG clinical guideline: Diagnosis and management of small bowel bleeding. Am J Gastroenterol.
2. Felton SJ and Ferguson JE. Multiple cutaneous swellings associated with sudden collapse. JAMA.
3. Yuksekkaya H et al. Blue rubber bleb nevus syndrome: Successful treatment with sirolimus. Pediatrics.
Answer: Blue rubber bleb nevus syndrome.
According to an American College of Gastroenterology Clinical Guideline,1 for patients with recurrence of small bowel bleeding, endoscopic management could be considered depending on the patient’s clinical course and response to prior therapy. Consequently, injections of lauromacrogol with SBE (single-balloon enteroscopy) were given (Figure D). Lesions that ranged from 1 to 2 cm were injected with 1-2 mL lauromacrogol until the mucosa turned white. Three SBEs had been performed in a 5-month period. A total of 20 lesions were successfully treated with lauromacrogol. The treated hemangiomas became small, and the site healed 5 months after treatment (Figures E and F). The patient has been followed for 1 year, and he remains in good clinical condition with his latest hemoglobin level at 110 g/L. No further blood transfusion is needed.
BRBNS is a rare disorder characterized by discrete venous malformations of varying size and appearance that are present on the skin and within the gastrointestinal tract.2With wider application of video capsule endoscopy (VCE) and the increase of image resolution, the detection rate and diagnostic accuracy of BRBNS are significantly improved. Treatment of BRBNS varies depending on the site, size, and number of lesions. Medication, surgery, and endoscopic therapy are currently clinically applied. The successful use of sirolimus was recently reported in the treatment of vascular lesions.3Sirolimus has potential adverse effects on renal function, bone marrow, and cholesterol metabolism, however. In consideration of the patient’s young age, we did not adopt this method. Surgical resection is more suitable for limited or life-threatening lesions. The lesions in this patient were mild and sporadic. Consequently, in this case, endoscopic injection of lauromacrogol was performed. This was the most complicated case of endoscopic treatment of BRBNS in our center and proved lauromacrogol injection was a feasible approach. According to a literature review, lauromacrogol has been used to treat vascular lesions for decades, but there is still no standard instruction for the dosage of lauromacrogol. We hope that our experience can be a reference for the endoscopic treatment of BRBNS.
References (add links)
1. Gerson LB et al. ACG clinical guideline: Diagnosis and management of small bowel bleeding. Am J Gastroenterol.
2. Felton SJ and Ferguson JE. Multiple cutaneous swellings associated with sudden collapse. JAMA.
3. Yuksekkaya H et al. Blue rubber bleb nevus syndrome: Successful treatment with sirolimus. Pediatrics.
Answer: Blue rubber bleb nevus syndrome.
According to an American College of Gastroenterology Clinical Guideline,1 for patients with recurrence of small bowel bleeding, endoscopic management could be considered depending on the patient’s clinical course and response to prior therapy. Consequently, injections of lauromacrogol with SBE (single-balloon enteroscopy) were given (Figure D). Lesions that ranged from 1 to 2 cm were injected with 1-2 mL lauromacrogol until the mucosa turned white. Three SBEs had been performed in a 5-month period. A total of 20 lesions were successfully treated with lauromacrogol. The treated hemangiomas became small, and the site healed 5 months after treatment (Figures E and F). The patient has been followed for 1 year, and he remains in good clinical condition with his latest hemoglobin level at 110 g/L. No further blood transfusion is needed.
BRBNS is a rare disorder characterized by discrete venous malformations of varying size and appearance that are present on the skin and within the gastrointestinal tract.2With wider application of video capsule endoscopy (VCE) and the increase of image resolution, the detection rate and diagnostic accuracy of BRBNS are significantly improved. Treatment of BRBNS varies depending on the site, size, and number of lesions. Medication, surgery, and endoscopic therapy are currently clinically applied. The successful use of sirolimus was recently reported in the treatment of vascular lesions.3Sirolimus has potential adverse effects on renal function, bone marrow, and cholesterol metabolism, however. In consideration of the patient’s young age, we did not adopt this method. Surgical resection is more suitable for limited or life-threatening lesions. The lesions in this patient were mild and sporadic. Consequently, in this case, endoscopic injection of lauromacrogol was performed. This was the most complicated case of endoscopic treatment of BRBNS in our center and proved lauromacrogol injection was a feasible approach. According to a literature review, lauromacrogol has been used to treat vascular lesions for decades, but there is still no standard instruction for the dosage of lauromacrogol. We hope that our experience can be a reference for the endoscopic treatment of BRBNS.
References (add links)
1. Gerson LB et al. ACG clinical guideline: Diagnosis and management of small bowel bleeding. Am J Gastroenterol.
2. Felton SJ and Ferguson JE. Multiple cutaneous swellings associated with sudden collapse. JAMA.
3. Yuksekkaya H et al. Blue rubber bleb nevus syndrome: Successful treatment with sirolimus. Pediatrics.
A 13-year-old boy presented with recurrent melena for 10 years accompanied with dizziness and fatigue. This patient had no history of nonsteroidal anti-inflammatory drug use, peptic ulcer, or chronic liver disease, and no family history of gastrointestinal bleeding. He was born with a right foot hemangioma that was resected when he was 2 years old. Additionally, he had received multiple blood transfusions for iron deficiency anemia since childhood. The body mass index was 16.5 kg/m2 and physical examination revealed active bowel sounds.
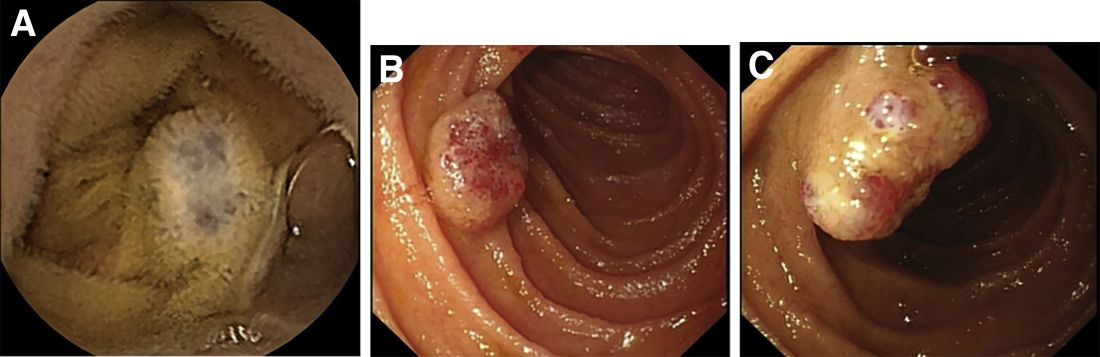
Laboratory examinations showed severe iron deficiency anemia (the lowest hemoglobin available was 36 g/L) and positive stool occult blood. Gastroscopy unveiled superficial gastritis and colonoscopy was normal. Second-look examinations showed the same results. No clinically important signs were observed on computed tomography scan. Given these results, small intestinal bleeding was considered. Therefore, a video capsule endoscopy (VCE) was carried out and revealed multifocal hemangioma-like purplish blue lesions in jejunum and ileum (Figure A). Then a single-balloon enteroscopy (SBE) was performed, which showed multifocal vascular lesions ranging between 1.0 and 2.0 cm in the jejunum and ileum (Figure B, C).
Based on these findings, what is your diagnosis? What is the next step in management for this patient?