User login
COVID-19 and surge capacity in U.S. hospitals
Background
As of April 2020, the United States is faced with the early stages of the coronavirus disease 2019 (COVID-19) pandemic. Experts predict up to 60% of the population will become infected with a fatality rate of 1% and a hospitalization rate of approximately 20%. Efforts to suppress viral spread have been unsuccessful as cases are reported in all 50 states, and fatalities are rising. Currently many American hospitals are ill-prepared for a significant increase in their census of critically ill and contagious patients, i.e., hospitals lack adequate surge capacity to safely handle a nationwide outbreak of COVID-19. As seen in other nations such as Italy, China, and Iran, this leads to rationing of life-saving health care and potentially preventable morbidity and mortality.
Introduction
Hospitals will be unable to provide the current standard of care to patients as the rate of infection with coronavirus disease 2019 (COVID-19) escalates. As of April 9, the World Health Organization has confirmed 1,539,118 cases and 89,998 deaths globally; and the Centers for Disease Control and Prevention has confirmed 435,941 cases and 14,865 deaths in the United States.1,2 Experts predict up to 60% of the population will eventually become infected with a fatality rate of about 1% and a hospitalization rate of approximately 20%.3,4
In the United States, with a population of 300 million people, this represents up to 180 million infected, 36 million requiring hospitalization, 11 million requiring intensive care, and 2 million fatalities over the duration of the pandemic. On March 13, President Donald Trump declared a state of national emergency, authorizing $50 billion dollars in emergency health care spending as well as asking every hospital in the country to immediately activate its emergency response plan. The use of isolation and quarantine may space out casualties over time, however high rates and volumes of hospitalizations are still expected.4,5
As the influx of patients afflicted with COVID-19 grows, needs will outstrip hospital resources forcing clinicians to ration beds and supplies. In Italy, China, and Iran, physicians are already faced with these difficult decisions. Antonio Pesenti, head of the Italian Lombardy regional crisis response unit, characterized the change in health care delivery: “We’re now being forced to set up intensive care treatment in corridors, in operating theaters, in recovery rooms. We’ve emptied entire hospital sections to make space for seriously sick people.”6
Surge capacity
Surge capacity is a hospital’s ability to adequately care for a significant influx of patients.7 Since 2011, the American College of Emergency Physicians has published guidelines calling for hospitals to have a surge capacity accounting for infectious disease outbreaks, and demands on supplies, personnel, and physical space.7 Even prior to the development of COVID-19, many hospitals faced emergency department crowding and strains on hospital capacity.8 The Organization for Economic Co-operation and Development (OECD) estimates hospital beds per 1,000 inhabitants at 2.77 for the USA, 3.18 for Italy, 4.34 for China, and 13.05 for Japan.9 Before COVID-19 many American hospitals had an insufficient number of beds. Now, in the initial phase of the pandemic, it is even more important to optimize surge capacity across the American health care system.
Requirements for COVID-19 preparation
To prepare for the increased number of seriously and critically ill patients, individual hospitals and regions must perform a needs assessment. The fundamental disease process of COVID-19 is a contagious viral pneumonia; treatment hinges on four major categories of intervention: spatial isolation (including physical space, beds, partitions, droplet precautions, food, water, and sanitation), oxygenation (including wall and portable oxygen, nasal canulae, and masks), mechanical ventilation (including ventilator machines, tubing, anesthetics, and reliable electrical power) and personnel (including physicians, nurses, technicians, and adequate personal protective equipment).10 In special circumstances and where available, extra corporeal membrane oxygenation may be considered.10 The necessary interventions are summarized in Table 1. 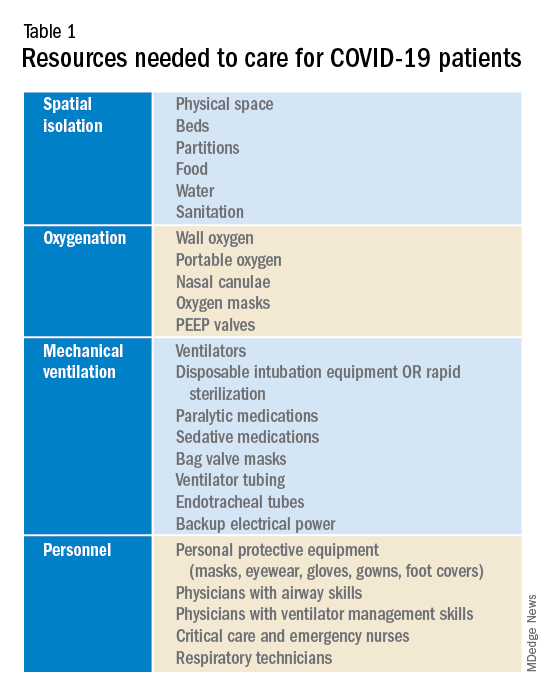
Emergency, critical care, nursing, and medical leadership should consider what sort of space, personnel, and supplies will be needed to care for a large volume of patients with contagious viral pneumonia at the same time as other hospital patients. Attention should also be given to potential need for morgue expansion. Hospitals must be proactive in procuring supplies and preparing for demands on beds and physical space. Specifically, logistics coordinators should start stockpiling ventilators, oxygen, respiratory equipment, and personal protective equipment. Reallocating supplies from other regions of the hospital such as operating rooms and ambulatory surgery centers may be considered. These resources, particularly ventilators and ventilator supplies, are already in disturbingly limited supply, and they are likely to be single most important limiting factor for survival rates. To prevent regional shortages, stockpiling efforts should ideally be aided by state and federal governments. The production and acquisition of ventilators should be immediately and significantly increased.
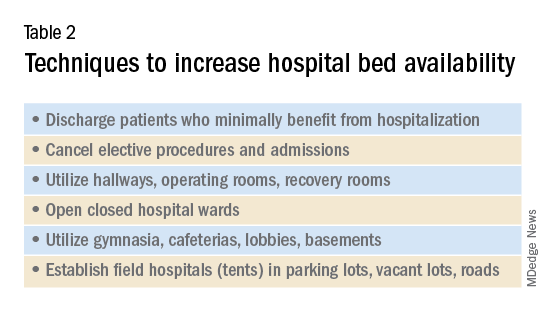
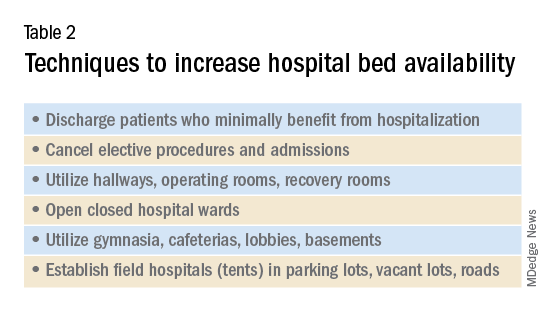
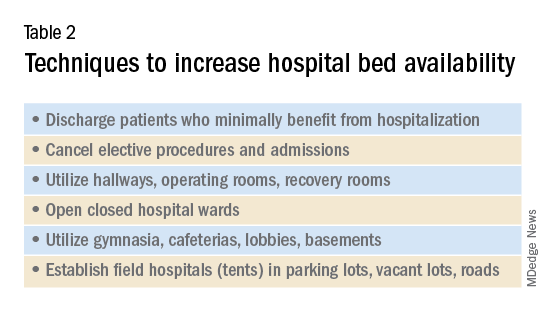
Hospitals must additionally prepare for demands for physical space and beds. Techniques to maximize space and bed availability (see Table 2) include discharging patients who do not require hospitalization, and canceling elective procedures and admissions. Additional methods would be to utilize unconventional preexisting spaces such as hallways, operating rooms, recovery rooms, hallways, closed hospital wards, basements, lobbies, cafeterias, and parking lots. Administrators should also consider establishing field hospitals or field wards, such as tents in open spaces and nearby roads. Medical care performed in unconventional environments will need to account for electricity, temperature control, oxygen delivery, and sanitation.
Conclusion
To minimize unnecessary loss of life and suffering, hospitals must expand their surge capacities in preparation for the predictable rise in demand for health care resources related to COVID-19. Numerous hospitals, particularly those that serve low-income and underserved communities, operate with a narrow financial margin.11 Independently preparing for the surge capacity needed to face COVID-19 may be infeasible for several hospitals. As a result, many health care systems will rely on government aid during this period for financial and material support. To maximize preparedness and response, hospitals should ask for and receive aid from the Federal Emergency Management Agency (FEMA), American Red Cross, state governments, and the military; these resources should be mobilized now.
Dr. Blumenberg, Dr. Noble, and Dr. Hendrickson are based in the department of emergency medicine & toxicology, Oregon Health and Science University, Portland.
References
1. Coronavirus disease 2019 (COVID-19) situation report – 60. 2020 Mar 19.
2. Coronavirus disease 2019 (COVID-19) Cases in the U.S. CDC. 2020 Apr 8.
3. Li Q et al. Early transmission dynamics in Wuhan, China, of novel coronavirus–infected pneumonia. N Engl J Med. 2020 Jan. doi: 10.1056/NEJMoa2001316.
4. Anderson RM et al. How will country-based mitigation measures influence the course of the COVID-19 epidemic? Lancet. 2020 Mar. doi: 10.1016/S0140-6736(20)30567-5.
5. Fraser C et al. Factors that make an infectious disease outbreak controllable. Proc Natl Acad Sci U S A. 2004;101(16):6146-51. doi: 10.1073/pnas.0307506101.
6. Mackenzie J and Balmer C. Italy locks down millions as its coronavirus deaths jump. Reuters. 2020 Mar 9.
7. Health care system surge capacity recognition, preparedness, and response. Ann Emerg Med. 2012;59(3):240-1. doi: 10.1016/j.annemergmed.2011.11.030.
8. Pitts SR et al. A cross-sectional study of emergency department boarding practices in the United States. Acad Emerg Med. 2014;21(5):497-503. doi: 10.1111/acem.12375.
9. Health at a Glance 2019. OECD; 2019. doi: 10.1787/4dd50c09-en.
10. Murthy S et al. Care for critically ill patients with COVID-19. JAMA. 2020 Mar. doi: 10.1001/jama.2020.3633.
11. Ly DP et al. The association between hospital margins, quality of care, and closure or other change in operating status. J Gen Intern Med. 2011;26(11):1291-6. doi: 10.1007/s11606-011-1815-5.
Background
As of April 2020, the United States is faced with the early stages of the coronavirus disease 2019 (COVID-19) pandemic. Experts predict up to 60% of the population will become infected with a fatality rate of 1% and a hospitalization rate of approximately 20%. Efforts to suppress viral spread have been unsuccessful as cases are reported in all 50 states, and fatalities are rising. Currently many American hospitals are ill-prepared for a significant increase in their census of critically ill and contagious patients, i.e., hospitals lack adequate surge capacity to safely handle a nationwide outbreak of COVID-19. As seen in other nations such as Italy, China, and Iran, this leads to rationing of life-saving health care and potentially preventable morbidity and mortality.
Introduction
Hospitals will be unable to provide the current standard of care to patients as the rate of infection with coronavirus disease 2019 (COVID-19) escalates. As of April 9, the World Health Organization has confirmed 1,539,118 cases and 89,998 deaths globally; and the Centers for Disease Control and Prevention has confirmed 435,941 cases and 14,865 deaths in the United States.1,2 Experts predict up to 60% of the population will eventually become infected with a fatality rate of about 1% and a hospitalization rate of approximately 20%.3,4
In the United States, with a population of 300 million people, this represents up to 180 million infected, 36 million requiring hospitalization, 11 million requiring intensive care, and 2 million fatalities over the duration of the pandemic. On March 13, President Donald Trump declared a state of national emergency, authorizing $50 billion dollars in emergency health care spending as well as asking every hospital in the country to immediately activate its emergency response plan. The use of isolation and quarantine may space out casualties over time, however high rates and volumes of hospitalizations are still expected.4,5
As the influx of patients afflicted with COVID-19 grows, needs will outstrip hospital resources forcing clinicians to ration beds and supplies. In Italy, China, and Iran, physicians are already faced with these difficult decisions. Antonio Pesenti, head of the Italian Lombardy regional crisis response unit, characterized the change in health care delivery: “We’re now being forced to set up intensive care treatment in corridors, in operating theaters, in recovery rooms. We’ve emptied entire hospital sections to make space for seriously sick people.”6
Surge capacity
Surge capacity is a hospital’s ability to adequately care for a significant influx of patients.7 Since 2011, the American College of Emergency Physicians has published guidelines calling for hospitals to have a surge capacity accounting for infectious disease outbreaks, and demands on supplies, personnel, and physical space.7 Even prior to the development of COVID-19, many hospitals faced emergency department crowding and strains on hospital capacity.8 The Organization for Economic Co-operation and Development (OECD) estimates hospital beds per 1,000 inhabitants at 2.77 for the USA, 3.18 for Italy, 4.34 for China, and 13.05 for Japan.9 Before COVID-19 many American hospitals had an insufficient number of beds. Now, in the initial phase of the pandemic, it is even more important to optimize surge capacity across the American health care system.
Requirements for COVID-19 preparation
To prepare for the increased number of seriously and critically ill patients, individual hospitals and regions must perform a needs assessment. The fundamental disease process of COVID-19 is a contagious viral pneumonia; treatment hinges on four major categories of intervention: spatial isolation (including physical space, beds, partitions, droplet precautions, food, water, and sanitation), oxygenation (including wall and portable oxygen, nasal canulae, and masks), mechanical ventilation (including ventilator machines, tubing, anesthetics, and reliable electrical power) and personnel (including physicians, nurses, technicians, and adequate personal protective equipment).10 In special circumstances and where available, extra corporeal membrane oxygenation may be considered.10 The necessary interventions are summarized in Table 1. 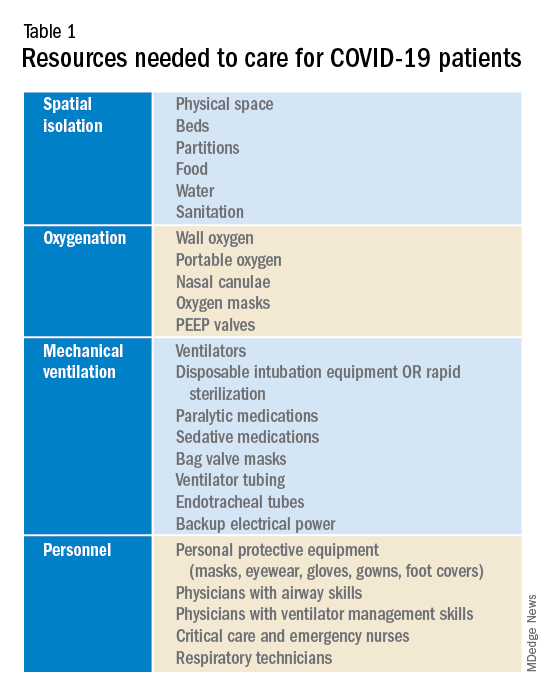
Emergency, critical care, nursing, and medical leadership should consider what sort of space, personnel, and supplies will be needed to care for a large volume of patients with contagious viral pneumonia at the same time as other hospital patients. Attention should also be given to potential need for morgue expansion. Hospitals must be proactive in procuring supplies and preparing for demands on beds and physical space. Specifically, logistics coordinators should start stockpiling ventilators, oxygen, respiratory equipment, and personal protective equipment. Reallocating supplies from other regions of the hospital such as operating rooms and ambulatory surgery centers may be considered. These resources, particularly ventilators and ventilator supplies, are already in disturbingly limited supply, and they are likely to be single most important limiting factor for survival rates. To prevent regional shortages, stockpiling efforts should ideally be aided by state and federal governments. The production and acquisition of ventilators should be immediately and significantly increased.
Hospitals must additionally prepare for demands for physical space and beds. Techniques to maximize space and bed availability (see Table 2) include discharging patients who do not require hospitalization, and canceling elective procedures and admissions. Additional methods would be to utilize unconventional preexisting spaces such as hallways, operating rooms, recovery rooms, hallways, closed hospital wards, basements, lobbies, cafeterias, and parking lots. Administrators should also consider establishing field hospitals or field wards, such as tents in open spaces and nearby roads. Medical care performed in unconventional environments will need to account for electricity, temperature control, oxygen delivery, and sanitation.
Conclusion
To minimize unnecessary loss of life and suffering, hospitals must expand their surge capacities in preparation for the predictable rise in demand for health care resources related to COVID-19. Numerous hospitals, particularly those that serve low-income and underserved communities, operate with a narrow financial margin.11 Independently preparing for the surge capacity needed to face COVID-19 may be infeasible for several hospitals. As a result, many health care systems will rely on government aid during this period for financial and material support. To maximize preparedness and response, hospitals should ask for and receive aid from the Federal Emergency Management Agency (FEMA), American Red Cross, state governments, and the military; these resources should be mobilized now.
Dr. Blumenberg, Dr. Noble, and Dr. Hendrickson are based in the department of emergency medicine & toxicology, Oregon Health and Science University, Portland.
References
1. Coronavirus disease 2019 (COVID-19) situation report – 60. 2020 Mar 19.
2. Coronavirus disease 2019 (COVID-19) Cases in the U.S. CDC. 2020 Apr 8.
3. Li Q et al. Early transmission dynamics in Wuhan, China, of novel coronavirus–infected pneumonia. N Engl J Med. 2020 Jan. doi: 10.1056/NEJMoa2001316.
4. Anderson RM et al. How will country-based mitigation measures influence the course of the COVID-19 epidemic? Lancet. 2020 Mar. doi: 10.1016/S0140-6736(20)30567-5.
5. Fraser C et al. Factors that make an infectious disease outbreak controllable. Proc Natl Acad Sci U S A. 2004;101(16):6146-51. doi: 10.1073/pnas.0307506101.
6. Mackenzie J and Balmer C. Italy locks down millions as its coronavirus deaths jump. Reuters. 2020 Mar 9.
7. Health care system surge capacity recognition, preparedness, and response. Ann Emerg Med. 2012;59(3):240-1. doi: 10.1016/j.annemergmed.2011.11.030.
8. Pitts SR et al. A cross-sectional study of emergency department boarding practices in the United States. Acad Emerg Med. 2014;21(5):497-503. doi: 10.1111/acem.12375.
9. Health at a Glance 2019. OECD; 2019. doi: 10.1787/4dd50c09-en.
10. Murthy S et al. Care for critically ill patients with COVID-19. JAMA. 2020 Mar. doi: 10.1001/jama.2020.3633.
11. Ly DP et al. The association between hospital margins, quality of care, and closure or other change in operating status. J Gen Intern Med. 2011;26(11):1291-6. doi: 10.1007/s11606-011-1815-5.
Background
As of April 2020, the United States is faced with the early stages of the coronavirus disease 2019 (COVID-19) pandemic. Experts predict up to 60% of the population will become infected with a fatality rate of 1% and a hospitalization rate of approximately 20%. Efforts to suppress viral spread have been unsuccessful as cases are reported in all 50 states, and fatalities are rising. Currently many American hospitals are ill-prepared for a significant increase in their census of critically ill and contagious patients, i.e., hospitals lack adequate surge capacity to safely handle a nationwide outbreak of COVID-19. As seen in other nations such as Italy, China, and Iran, this leads to rationing of life-saving health care and potentially preventable morbidity and mortality.
Introduction
Hospitals will be unable to provide the current standard of care to patients as the rate of infection with coronavirus disease 2019 (COVID-19) escalates. As of April 9, the World Health Organization has confirmed 1,539,118 cases and 89,998 deaths globally; and the Centers for Disease Control and Prevention has confirmed 435,941 cases and 14,865 deaths in the United States.1,2 Experts predict up to 60% of the population will eventually become infected with a fatality rate of about 1% and a hospitalization rate of approximately 20%.3,4
In the United States, with a population of 300 million people, this represents up to 180 million infected, 36 million requiring hospitalization, 11 million requiring intensive care, and 2 million fatalities over the duration of the pandemic. On March 13, President Donald Trump declared a state of national emergency, authorizing $50 billion dollars in emergency health care spending as well as asking every hospital in the country to immediately activate its emergency response plan. The use of isolation and quarantine may space out casualties over time, however high rates and volumes of hospitalizations are still expected.4,5
As the influx of patients afflicted with COVID-19 grows, needs will outstrip hospital resources forcing clinicians to ration beds and supplies. In Italy, China, and Iran, physicians are already faced with these difficult decisions. Antonio Pesenti, head of the Italian Lombardy regional crisis response unit, characterized the change in health care delivery: “We’re now being forced to set up intensive care treatment in corridors, in operating theaters, in recovery rooms. We’ve emptied entire hospital sections to make space for seriously sick people.”6
Surge capacity
Surge capacity is a hospital’s ability to adequately care for a significant influx of patients.7 Since 2011, the American College of Emergency Physicians has published guidelines calling for hospitals to have a surge capacity accounting for infectious disease outbreaks, and demands on supplies, personnel, and physical space.7 Even prior to the development of COVID-19, many hospitals faced emergency department crowding and strains on hospital capacity.8 The Organization for Economic Co-operation and Development (OECD) estimates hospital beds per 1,000 inhabitants at 2.77 for the USA, 3.18 for Italy, 4.34 for China, and 13.05 for Japan.9 Before COVID-19 many American hospitals had an insufficient number of beds. Now, in the initial phase of the pandemic, it is even more important to optimize surge capacity across the American health care system.
Requirements for COVID-19 preparation
To prepare for the increased number of seriously and critically ill patients, individual hospitals and regions must perform a needs assessment. The fundamental disease process of COVID-19 is a contagious viral pneumonia; treatment hinges on four major categories of intervention: spatial isolation (including physical space, beds, partitions, droplet precautions, food, water, and sanitation), oxygenation (including wall and portable oxygen, nasal canulae, and masks), mechanical ventilation (including ventilator machines, tubing, anesthetics, and reliable electrical power) and personnel (including physicians, nurses, technicians, and adequate personal protective equipment).10 In special circumstances and where available, extra corporeal membrane oxygenation may be considered.10 The necessary interventions are summarized in Table 1. 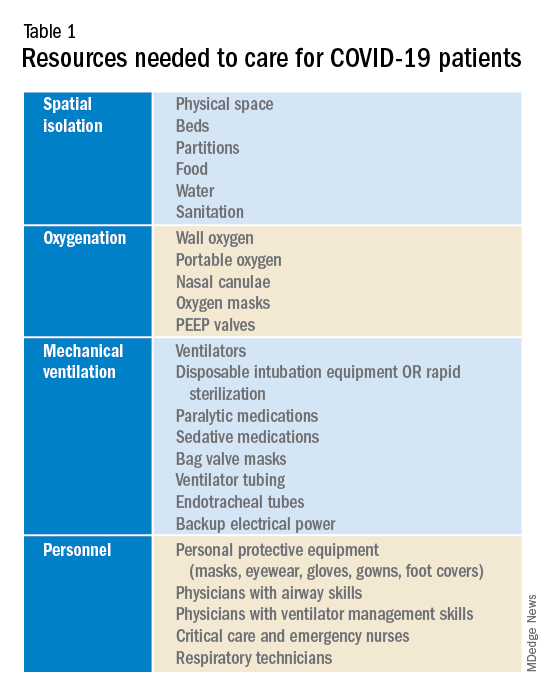
Emergency, critical care, nursing, and medical leadership should consider what sort of space, personnel, and supplies will be needed to care for a large volume of patients with contagious viral pneumonia at the same time as other hospital patients. Attention should also be given to potential need for morgue expansion. Hospitals must be proactive in procuring supplies and preparing for demands on beds and physical space. Specifically, logistics coordinators should start stockpiling ventilators, oxygen, respiratory equipment, and personal protective equipment. Reallocating supplies from other regions of the hospital such as operating rooms and ambulatory surgery centers may be considered. These resources, particularly ventilators and ventilator supplies, are already in disturbingly limited supply, and they are likely to be single most important limiting factor for survival rates. To prevent regional shortages, stockpiling efforts should ideally be aided by state and federal governments. The production and acquisition of ventilators should be immediately and significantly increased.
Hospitals must additionally prepare for demands for physical space and beds. Techniques to maximize space and bed availability (see Table 2) include discharging patients who do not require hospitalization, and canceling elective procedures and admissions. Additional methods would be to utilize unconventional preexisting spaces such as hallways, operating rooms, recovery rooms, hallways, closed hospital wards, basements, lobbies, cafeterias, and parking lots. Administrators should also consider establishing field hospitals or field wards, such as tents in open spaces and nearby roads. Medical care performed in unconventional environments will need to account for electricity, temperature control, oxygen delivery, and sanitation.
Conclusion
To minimize unnecessary loss of life and suffering, hospitals must expand their surge capacities in preparation for the predictable rise in demand for health care resources related to COVID-19. Numerous hospitals, particularly those that serve low-income and underserved communities, operate with a narrow financial margin.11 Independently preparing for the surge capacity needed to face COVID-19 may be infeasible for several hospitals. As a result, many health care systems will rely on government aid during this period for financial and material support. To maximize preparedness and response, hospitals should ask for and receive aid from the Federal Emergency Management Agency (FEMA), American Red Cross, state governments, and the military; these resources should be mobilized now.
Dr. Blumenberg, Dr. Noble, and Dr. Hendrickson are based in the department of emergency medicine & toxicology, Oregon Health and Science University, Portland.
References
1. Coronavirus disease 2019 (COVID-19) situation report – 60. 2020 Mar 19.
2. Coronavirus disease 2019 (COVID-19) Cases in the U.S. CDC. 2020 Apr 8.
3. Li Q et al. Early transmission dynamics in Wuhan, China, of novel coronavirus–infected pneumonia. N Engl J Med. 2020 Jan. doi: 10.1056/NEJMoa2001316.
4. Anderson RM et al. How will country-based mitigation measures influence the course of the COVID-19 epidemic? Lancet. 2020 Mar. doi: 10.1016/S0140-6736(20)30567-5.
5. Fraser C et al. Factors that make an infectious disease outbreak controllable. Proc Natl Acad Sci U S A. 2004;101(16):6146-51. doi: 10.1073/pnas.0307506101.
6. Mackenzie J and Balmer C. Italy locks down millions as its coronavirus deaths jump. Reuters. 2020 Mar 9.
7. Health care system surge capacity recognition, preparedness, and response. Ann Emerg Med. 2012;59(3):240-1. doi: 10.1016/j.annemergmed.2011.11.030.
8. Pitts SR et al. A cross-sectional study of emergency department boarding practices in the United States. Acad Emerg Med. 2014;21(5):497-503. doi: 10.1111/acem.12375.
9. Health at a Glance 2019. OECD; 2019. doi: 10.1787/4dd50c09-en.
10. Murthy S et al. Care for critically ill patients with COVID-19. JAMA. 2020 Mar. doi: 10.1001/jama.2020.3633.
11. Ly DP et al. The association between hospital margins, quality of care, and closure or other change in operating status. J Gen Intern Med. 2011;26(11):1291-6. doi: 10.1007/s11606-011-1815-5.



