User login
Tension Pneumocephalus as Complication of Hematoma Evacuation
A 78‐year‐old man was transferred from an outside hospital where he presented with declining mental status and a history of falls. A computed tomography (CT) scan of the brain revealed a chronic subdural hematoma with superimposed acute hemorrhage. The subdural hematoma was attributed to a fall at home approximately 5 weeks prior to admission. He was taken to the operating room for urgent craniotomy and hemorrhage evacuation and postoperatively comanaged by neurosurgery, hospitalists, and medicine residents. He tolerated the procedure and was noted to have marked improvement in mental status after the procedure. He was monitored overnight in our intensive care unit without intracranial pressure monitoring.
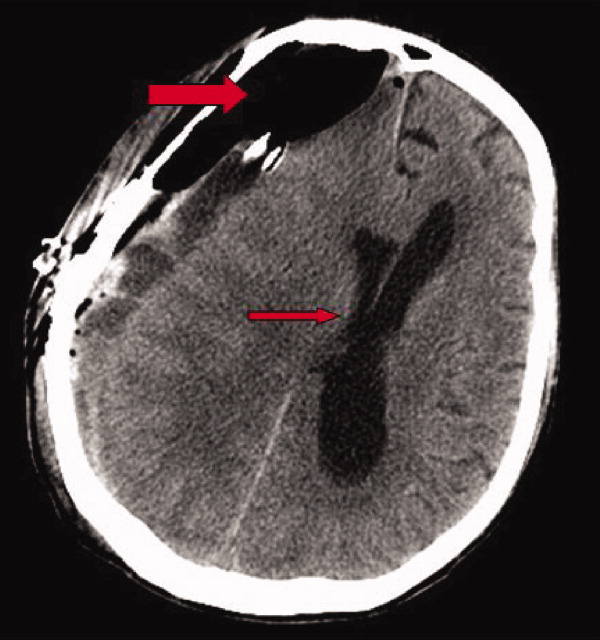
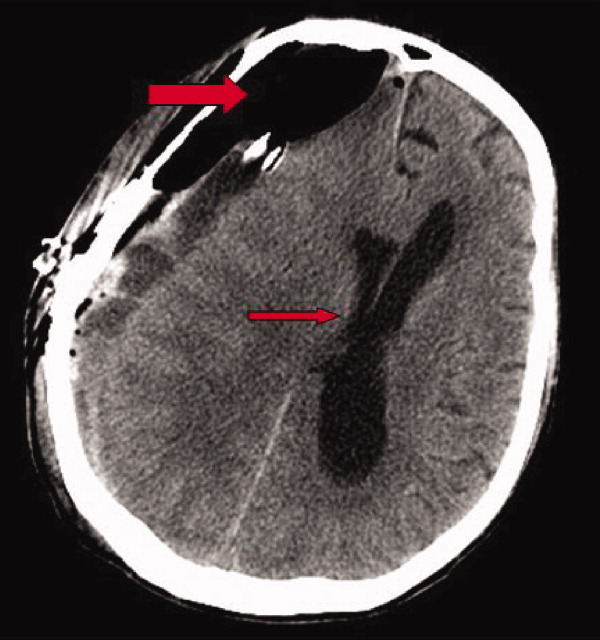
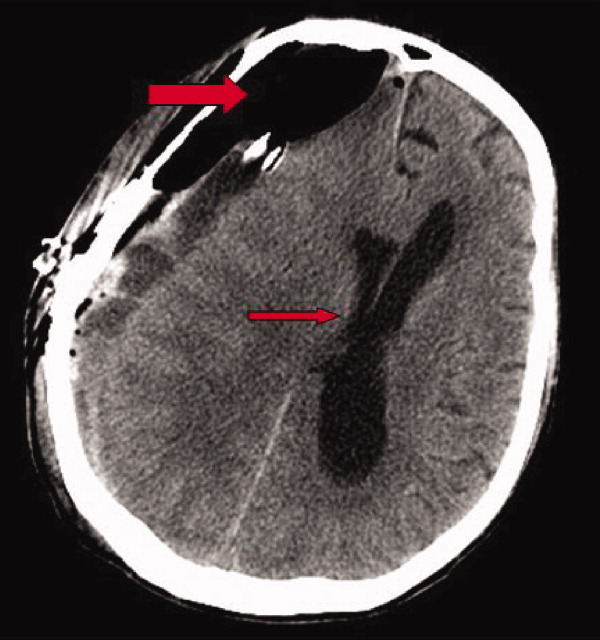
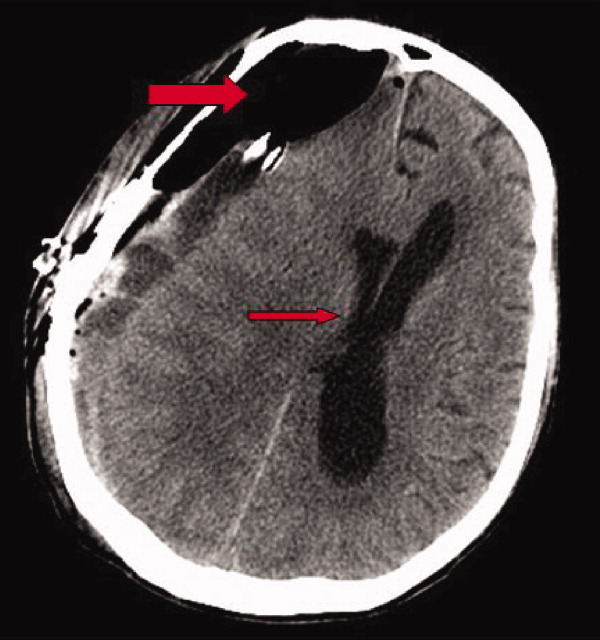
Early on postoperative day 1, he was awake, alert, following commands, and felt to be stable enough to be transferred to our transitional intensive care unit. However, later in the day he became progressively more confused. A follow‐up CT scan of the brain was ordered (Fig. 1) by the medicine team which revealed a large collection of air (wide arrow) and marked midline shift (thin arrow) consistent with tension pneumocephaly and subfalcine herniation (Fig. 2; arrow). Examination revealed that he was grossly obtunded with marked anisocoria, decerebrate posturing, and rigid tone. Neurosurgery was immediately contacted and recommended accessing 2 indwelling catheters left in the cerebrum as part of the normal postoperative course. Approximately 100 mL of serosanguinous fluid and air was aspirated with immediate improvement in his mental status and exam findings. Over the next few days, he remained clinically stable, and repeat CT scan showed slow resolution of the pneumocephalus and a decrease of his mass effect and midline shift. He was ultimately transferred to our skilled nursing facility for physical therapy and has done relatively well.

Pneumocephalus is a relatively common finding in many neurosurgical, intracranial procedures. However, tension pneumocephalus is a rare, life‐threatening form of pneumocephalus in which intracranial air causes mass effect and midline shift. In a review of 295 cases of pneumocephalus, 75% were caused by surgery, mostly intracranial and transsphenoidal, and head trauma. About 9% of cases resulted from infection with gas‐forming bacteria and rare causes include invasion of a nasopharyngeal carcinoma, frequent Valsalva maneuver, and air travel.1 Tension pneumocephalus occurs most commonly after the neurosurgical evacuation of a subdural hematoma. The prevalence of tension pneumocephalus following the evacuation of chronic subdural hematomas has been reported from 2.5% to 16%.2
There are 2 proposed mechanisms for the development of pneumocephalus; 1 proposes that air passes through a dural tear by a ball valve effect in which air can be forced into the intracranial cavity by a rapid increase in intrasinus pressure that occurs during sneezing, coughing, or straining. The air is then trapped intracranially. The second theory proposes that cerebrospinal fluid leakage permits air to enter the intracranial cavity because negative pressure is created as cerebrospinal fluid leaves the space.3 The conversion to tension physiology in either of these theories is less well understood.
- ,,,,.Pneumocephalus secondary to septic thrombosis of the superior sagittal sinus: report of a case.J Formos Med Assoc.2001;100(2):142‐144.
- ,,, et al.Subdural tension pneumocephalus following surgery for chronic subdural hematoma.J Neurosurg.1988;68:58‐61.
- ,,,.Nontraumatic tension pneumocephalus—a differential diagnosis of headache in the ED.Am J Emerg Med.2005, Vol.23, pp235‐236.
A 78‐year‐old man was transferred from an outside hospital where he presented with declining mental status and a history of falls. A computed tomography (CT) scan of the brain revealed a chronic subdural hematoma with superimposed acute hemorrhage. The subdural hematoma was attributed to a fall at home approximately 5 weeks prior to admission. He was taken to the operating room for urgent craniotomy and hemorrhage evacuation and postoperatively comanaged by neurosurgery, hospitalists, and medicine residents. He tolerated the procedure and was noted to have marked improvement in mental status after the procedure. He was monitored overnight in our intensive care unit without intracranial pressure monitoring.
Early on postoperative day 1, he was awake, alert, following commands, and felt to be stable enough to be transferred to our transitional intensive care unit. However, later in the day he became progressively more confused. A follow‐up CT scan of the brain was ordered (Fig. 1) by the medicine team which revealed a large collection of air (wide arrow) and marked midline shift (thin arrow) consistent with tension pneumocephaly and subfalcine herniation (Fig. 2; arrow). Examination revealed that he was grossly obtunded with marked anisocoria, decerebrate posturing, and rigid tone. Neurosurgery was immediately contacted and recommended accessing 2 indwelling catheters left in the cerebrum as part of the normal postoperative course. Approximately 100 mL of serosanguinous fluid and air was aspirated with immediate improvement in his mental status and exam findings. Over the next few days, he remained clinically stable, and repeat CT scan showed slow resolution of the pneumocephalus and a decrease of his mass effect and midline shift. He was ultimately transferred to our skilled nursing facility for physical therapy and has done relatively well.

Pneumocephalus is a relatively common finding in many neurosurgical, intracranial procedures. However, tension pneumocephalus is a rare, life‐threatening form of pneumocephalus in which intracranial air causes mass effect and midline shift. In a review of 295 cases of pneumocephalus, 75% were caused by surgery, mostly intracranial and transsphenoidal, and head trauma. About 9% of cases resulted from infection with gas‐forming bacteria and rare causes include invasion of a nasopharyngeal carcinoma, frequent Valsalva maneuver, and air travel.1 Tension pneumocephalus occurs most commonly after the neurosurgical evacuation of a subdural hematoma. The prevalence of tension pneumocephalus following the evacuation of chronic subdural hematomas has been reported from 2.5% to 16%.2
There are 2 proposed mechanisms for the development of pneumocephalus; 1 proposes that air passes through a dural tear by a ball valve effect in which air can be forced into the intracranial cavity by a rapid increase in intrasinus pressure that occurs during sneezing, coughing, or straining. The air is then trapped intracranially. The second theory proposes that cerebrospinal fluid leakage permits air to enter the intracranial cavity because negative pressure is created as cerebrospinal fluid leaves the space.3 The conversion to tension physiology in either of these theories is less well understood.
A 78‐year‐old man was transferred from an outside hospital where he presented with declining mental status and a history of falls. A computed tomography (CT) scan of the brain revealed a chronic subdural hematoma with superimposed acute hemorrhage. The subdural hematoma was attributed to a fall at home approximately 5 weeks prior to admission. He was taken to the operating room for urgent craniotomy and hemorrhage evacuation and postoperatively comanaged by neurosurgery, hospitalists, and medicine residents. He tolerated the procedure and was noted to have marked improvement in mental status after the procedure. He was monitored overnight in our intensive care unit without intracranial pressure monitoring.
Early on postoperative day 1, he was awake, alert, following commands, and felt to be stable enough to be transferred to our transitional intensive care unit. However, later in the day he became progressively more confused. A follow‐up CT scan of the brain was ordered (Fig. 1) by the medicine team which revealed a large collection of air (wide arrow) and marked midline shift (thin arrow) consistent with tension pneumocephaly and subfalcine herniation (Fig. 2; arrow). Examination revealed that he was grossly obtunded with marked anisocoria, decerebrate posturing, and rigid tone. Neurosurgery was immediately contacted and recommended accessing 2 indwelling catheters left in the cerebrum as part of the normal postoperative course. Approximately 100 mL of serosanguinous fluid and air was aspirated with immediate improvement in his mental status and exam findings. Over the next few days, he remained clinically stable, and repeat CT scan showed slow resolution of the pneumocephalus and a decrease of his mass effect and midline shift. He was ultimately transferred to our skilled nursing facility for physical therapy and has done relatively well.

Pneumocephalus is a relatively common finding in many neurosurgical, intracranial procedures. However, tension pneumocephalus is a rare, life‐threatening form of pneumocephalus in which intracranial air causes mass effect and midline shift. In a review of 295 cases of pneumocephalus, 75% were caused by surgery, mostly intracranial and transsphenoidal, and head trauma. About 9% of cases resulted from infection with gas‐forming bacteria and rare causes include invasion of a nasopharyngeal carcinoma, frequent Valsalva maneuver, and air travel.1 Tension pneumocephalus occurs most commonly after the neurosurgical evacuation of a subdural hematoma. The prevalence of tension pneumocephalus following the evacuation of chronic subdural hematomas has been reported from 2.5% to 16%.2
There are 2 proposed mechanisms for the development of pneumocephalus; 1 proposes that air passes through a dural tear by a ball valve effect in which air can be forced into the intracranial cavity by a rapid increase in intrasinus pressure that occurs during sneezing, coughing, or straining. The air is then trapped intracranially. The second theory proposes that cerebrospinal fluid leakage permits air to enter the intracranial cavity because negative pressure is created as cerebrospinal fluid leaves the space.3 The conversion to tension physiology in either of these theories is less well understood.
- ,,,,.Pneumocephalus secondary to septic thrombosis of the superior sagittal sinus: report of a case.J Formos Med Assoc.2001;100(2):142‐144.
- ,,, et al.Subdural tension pneumocephalus following surgery for chronic subdural hematoma.J Neurosurg.1988;68:58‐61.
- ,,,.Nontraumatic tension pneumocephalus—a differential diagnosis of headache in the ED.Am J Emerg Med.2005, Vol.23, pp235‐236.
- ,,,,.Pneumocephalus secondary to septic thrombosis of the superior sagittal sinus: report of a case.J Formos Med Assoc.2001;100(2):142‐144.
- ,,, et al.Subdural tension pneumocephalus following surgery for chronic subdural hematoma.J Neurosurg.1988;68:58‐61.
- ,,,.Nontraumatic tension pneumocephalus—a differential diagnosis of headache in the ED.Am J Emerg Med.2005, Vol.23, pp235‐236.