User login
Nuts and bolts of preoperative clinics: The view from three institutions
Weiner Center for Preoperative Evaluation at Brigham and Women’s Hospital
By Angela M. Bader, MD, MPH
When organizing our preoperative clinic at Brigham and Women’s Hospital, we had several goals. Overall, we wanted a standardized process to help us achieve a high level of excellence. We hoped that creating a new system would eliminate ambiguity about who was responsible for following up on a patient’s abnormal laboratory test result—the surgeon, anesthesiologist, or primary care physician. We also wanted to better coordinate the various care teams involved throughout the perioperative period.
STANDARDIZATION HELPS MEET MANY GOALS
Standardization can occur at many levels:
- Performance of assessments and testing
- Organization of the patient chart and medical records
- Systems checks throughout the process to ensure that nothing is missed
- Team-to-team communication.
Documentation requirements apply regardless of institutional structure
When considering any system of preoperative assessment, keep in mind that the hospital must meet and appropriately document compliance with all regulatory, accreditation, and payer requirements and guidelines, such as those of the Joint Commission, the Centers for Medicare and Medicaid Services (CMS), and the National Surgical Quality Improvement Program. For example, the Joint Commission requires that a surgical history and physical examination be done within 30 days of a procedure. An anesthesiology assessment and a nursing assessment are also required. All of these assessments have mandatory elements, including documenting “never events” and ordering appropriate laboratory tests, electrocardiograms (ECGs), and radiographs.
Sometimes administrators of other hospitals say to me, “We can’t afford a preoperative clinic, and we don’t need one.” My response is that regardless of whether a hospital has a preoperative clinic, the regulatory requirements and guidelines must be met: it is not an issue of avoiding certain steps. Having a dedicated preoperative clinic simply shifts the work to a standardized, centralized system and avoids delaying these required steps until the day of surgery, when taking care of a problem involves the most inefficient use of resources.
Tailor system to institutional needs and characteristics
Within the regulatory framework, the organizational scheme of every institution must address issues of volume and acuity, the types of surgery performed, and the time frames required. A system must be able to deal with the preoperative needs of patients undergoing operations that are booked weeks in advance (often the case for orthopedic surgery) as well as those that may not be booked until a day before the procedure (eg, cancer surgery).
Our plan was developed for our very high-volume, tertiary care institution. In 2008, 24,000 patients used our clinic (roughly 100 patients per day).
DESIGN OF THE PREOPERATIVE CLINIC
A nurse practitioner–based model for ‘one-stop shopping’
We decided that the clinic should offer all elements of the preoperative assessment and thereby give patients “one-stop shopping.” Each patient sees a nurse practitioner, who performs the surgical history and physical examination as well as the anesthesiology and nursing assessments. The result is a multidisciplinary approach with a single assessment output. We shifted employees who had been responsible for preoperative assessment in the offices of various surgeons to a central clinic so that all assessments could be standardized, and we provided additional training to enable them to perform various assessments. The nurse practitioners are supervised by an on-site attending physician, as detailed below.
This model offers a number of advantages:
- Patients see a single provider.
- Assessment is facilitated for our surgeons, who may not be completely up-to-date on perioperative risk assessment and management.
- We have a central location for standardized education programs for our physicians, nurses, and residents.
- The clinic’s standardized records and processes facilitate data generation for research and clinical practice improvement.
Independent budgetary and staffing structure
The preoperative clinic is a separate cost center under the leadership of the department of anesthesiology. Resources were shifted to a central location so that as volume increases, we can add resources to meet the additional volume. We contracted with the hospital administration to provide payment for two full-time-equivalent anesthesiologists per day, who serve as on-site attending physicians. The hospital is willing to do this because not only do these attending physicians supervise the anesthesiology assessment, they are the collaborating physicians for the entire perioperative assessment. They review every patient, order tests and write prescriptions as needed, and discuss issues with the primary care physicians and referring specialists.
The preoperative clinic has an anesthesiologist director (me) who reports directly to the hospital’s vice president for surgical services on budget and staffing issues. I also report to the chairman of the department of anesthesiology, though he is not involved in budgetary functions (the hospital contracts with him to provide the anesthesiology staffing). The clerical and nursing staff work directly for the clinic.
The clinic is run in a self-contained area with a central waiting room and space for doing all the assessments and laboratory work internally, including 16 examination rooms and a room for chart organization.
MORE BENEFITS OF STANDARDIZATION
Standardized scheduling ensures reliability
The secretaries in each surgeon’s office schedule appointments through a central computer system after registration and insurance precertification. Our computer system does not allow an operation to be scheduled without an evaluation also being scheduled. The evaluation can involve either a visit or a telephone screen; we provide algorithms so that the surgeons’ secretaries know which is required. This system has substantially reduced the number of walk-ins, allowing for a more even distribution of patients and ensuring that medical records will be available when a patient is seen.
We watch our schedule carefully. Our computer system monitors the time that each patient is in our clinic to determine his or her waiting time and assessment time. It takes about 75 minutes to go through the whole process, including the time for a nurse practitioner to do the surgical history and physical examination and the anesthesiology and nursing assessments, a laboratory technician to do an ECG and laboratory tests if indicated, and completion of all required documentation. Accordingly, patients are scheduled in 75-minute blocks between 7:00 am and 6:30 pm. We do not have evening or weekend hours because of the difficulty of contacting surgeons and primary care physicians when questions arise. It is simply not cost-effective to have to do that type of follow-up on a case after the patient leaves.
Only about 10% of our patients are screened by telephone, since most of our operations are complicated and require in-person assessment (most low-acuity procedures are done at other hospitals). Of the patients who visit the preoperative clinic, about 75% undergo the single assessment model for surgery, anesthesiology, and nursing as described above. The remaining 25% of patients have their history and physical exam completed outside Brigham and Women’s Hospital for insurance reasons; the remainder of their assessment is conducted in our preoperative clinic by a registered nurse and an anesthesiology resident.
Multiple systems checks
Our model also incorporates standardization in the form of multiple systems checks:
- Case presentation. Every case is presented to an attending anesthesiologist, who reviews the ECG (if ordered) before the patient leaves the clinic.
- Post-visit chart check. A registered nurse or nurse practitioner signs off on each chart after the visit, confirming test results and resolution of all paperwork issues.
- Surgical checklist. The end result is a checklist that serves as the front sheet of the operating room chart.
Our ability to use this system of checks to get the chart completed comprehensively and reliably and deliver it to the operating room when needed was key to securing institutional support and funding for the preoperative clinic.
ROLE OF THE ATTENDING ANESTHESIOLOGISTS
Two full-time attending anesthesiologists are present in the preoperative clinic each day. One is responsible largely for supervising the nurse practitioner assessments and reviewing case presentations, while the other also oversees the education and supervision of residents. Residents rotate through the clinic for 2 weeks (one or two at a time) and have a designated curriculum consisting of daily lectures and competencies in preoperative evaluation.
Because our anesthesiologists are expert in preoperative assessment, we require very few outside consults. We can communicate directly with the cardiologists and other physicians and order tests when indicated. We have a clerical assistant who obtains all necessary paperwork and prior testing from outside providers so that the clinicians need not waste time on this.
A GROWING CHALLENGE: ASSESSMENT FOR PROCEDURES IN AMBULATORY SETTINGS
Looking forward, a rapidly growing challenge facing our clinic stems from the tremendous growth in patients who require anesthesia for procedures performed outside the operating room. In these situations, the proceduralists need a system for deciding whether an anesthesiologist must be present for any given case.
We have started to develop appropriate screening processes to ensure that the proceduralists in multiple departments know which patients to refer for preprocedure assessment. We hope to soon develop protocols for high-risk patients and for various procedures such as implanting a pacemaker or defibrillator, catheter procedures, interventional radiology, and endoscopy.
Anesthesia Perioperative Medicine Clinic at University of Chicago
By BobbieJean Sweitzer, MD
Detsky and Naglie have argued that the costs and clinical outcomes associated with any intervention must be compared with those of alternate strategies for treating the same patients,1 and I believe their point applies well to preoperative clinics. Although certain requirements of the Joint Commission and CMS must be met, as noted by Dr. Bader, they can be met in various ways. I will preface my comments by emphasizing that one size does not fit all: every institution must decide the best approach to preoperative assessment based on its patient population, the types of procedures it performs, and the volume it handles.
TRIAGE STREAMLINES THE PROCESS
Our preoperative clinic at the University of Chicago emphasizes triage. Not every patient should have to go to the trouble of coming in to see a provider. In the future, we will likely see more “virtual” preoperative assessments using devices in development, such as handheld ultrasonography machines. Just as patients can have their pacemakers and implantable cardiac defibrillators remotely checked via phone contact, more tools will one day be available for remote assessment.
Although not every surgical patient needs to come in to the preoperative clinic, every patient must have a physical examination. All patients will be seen on the day of surgery, so in some cases the physical exam may be able to wait until then. For example, an airway assessment need not be done ahead of time. Most anesthesiologists are prepared to manage airways on very short notice, so extensive advance planning is not always necessary.
Obtain basic info by questionnaire to save staff time
Information about the patient is key to triage, and it may be either paper- or computer-based. An initial priority should be to develop some mechanism for getting information from patients before the day of their procedure without a visit to the hospital or ambulatory surgery center.
We use a two-page paper questionnaire to obtain basic information from patients, including (among other pertinent questions) age, planned operation, names of the surgeon and primary doctor, past operations and medical history, allergies, a list of medications, social history (drug, alcohol, tobacco use), whether they have ever taken steroids, whether they have high blood pressure, and whether they can comfortably walk up a flight of stairs. We provide the primary care physicians and surgeons with blank questionnaires, which their patients can fill out in their waiting rooms or take home and fax to us (or drop off) later. The questionnaire gives us a good deal of essential information without using staff time.
Various computer-based and Web-based systems are also available for collecting basic patient information. Smaller institutions need not purchase an entire electronic medical record system, which can be very expensive. Some Web-based tools operate on a pay-per-use basis and can be very helpful.
Review the information to guide triage
We then review the patient information to determine the extent of preoperative evaluation required. Some patients, especially those scheduled at an ambulatory surgery center, are healthy enough that they can just come in on the day of surgery for an examination and an update of their information. Others will need an appointment at the clinic before the day of surgery for more extensive preoperative evaluation. For other patients, review of their questionnaire responses may prompt a phone call or e-mail from the clinic for more information to determine whether a day-of-surgery exam will suffice or whether evaluation in advance is needed. When in doubt, concerns raised by the questionnaire should be explored before the day of surgery to avoid surprises and allow sufficient time for a consultation, if needed.
STANDARDIZED GUIDELINES KEEP CARE CONSISTENT
We encourage our staff to minimize preoperative testing and ECGs. A majority of diagnoses are made based on the history and physical exam.2 Generally, a test should confirm what is already suspected and merely provide objective evidence when needed. Testing in this setting should not be done to “find out what is wrong” with a patient.
It is helpful to develop standardized guidelines for preoperative assessment and make them available to everyone in the institution via the Web. The guidelines should address recommended preoperative tests and management practices according to specific patient conditions or surgical procedures. The clear objective is to avoid disagreement about what a patient needs between the provider who evaluated the patient in advance and the surgeon or anesthesiologist who evaluates the patient on the day of surgery.
Our guidelines at the University of Chicago include recommendations for patients on long-term anticoagulant therapy, for patients with coronary stents, for medications that should be discontinued (and those that may be continued) on the day of surgery, and for numerous other conditions and issues. Our testing guidelines list indicated tests for various medical problems, which in turn link to other guidelines. Other links are based on the medications a patient is using or the type of operation that is planned.
We collaborated with our electrophysiology department to create guidelines for managing patients with pacemakers and defibrillators. Almost every patient with one of these devices has a little card associated with the device, and we ask the surgeons to copy the card and send it to the clinic if we will not be directly seeing the patient. Using a national database, the electrophysiology department can determine from the card the type of pacemaker or defibrillator a patient has, and they fax or e-mail us back a page of instructions to let us know whether the device requires special consideration during surgery, whether it should be checked preoperatively, and whether its battery needs replacing. With this system, we have markedly reduced problems on the day of surgery.
CONSULTS HAVE AN IMPORTANT ROLE
Consults should never be requested in order to “clear a patient for surgery.” Consult requests should rather address specific issues, such as, “Is this patient medically optimized?” or “Please address this patient’s hypertension.” In turn, consult notes should provide meaningful information that can be used in a specific way. A clearance letter or simple risk assessment is not helpful.
If a patient has not seen a primary care doctor in a long time, a consult request should (in addition to requesting a global risk assessment) specify any particular concerns, such as, “The patient reports snoring; please address sleep apnea and cardiac risk.”
Case study: Beware consult notes with no specifics
Consider a case we encountered of a 54-year-old man who had a preoperative cardiac risk assessment. The cardiology consultant completed a short form consisting of a multiple-choice check-off list indicating low, moderate, or high cardiac risk. The consultant checked that the patient had low cardiac risk but provided no other instructions or information other than his own contact information.
When we reviewed the patient’s questionnaire, we saw that his medications included metoprolol, clopidogrel, and aspirin even though the patient did not mention that he had coronary artery disease. On this basis, we requested details about his cardiac evaluation from his cardiologist. It turned out that the patient had a history of four catheterizations with several cardiac stents placed. The most recent stent was implanted to overlap a previous stent that had been found “floating” in the blood vessel; this last stent was placed just 6 months before the cardiologist issued the consult note indicating “low cardiac risk.”
The moral is to approach consult notes with caution, especially if they offer no specifics. It actually makes me nervous when a note states “low risk” because if something unexpectedly goes wrong in surgery, it appears that the perioperative team took poor care of the patient even if the complication actually may have stemmed from higher-than-recognized underlying patient risk.
PROVIDE, AND REINFORCE, CLEAR INSTRUCTIONS
We give patients written preoperative instructions that become part of our computerized records. We first verbally give explicit instructions for each medication—ie, whether it can be taken as usual or when it needs to be stopped before surgery (and why). Then we provide the same information in writing, after which we try to have the patient repeat the instructions back to the clinician. We include a phone number that patients can call if they need help understanding their preoperative instructions.
Web-based programs also can provide patients online instructions about their medications. Some services even customize information by providing, for example, lists of local surgeons who are willing to allow a patient to continue on aspirin therapy until the day of surgery.
USE THE RIGHT RESOURCES
Staffing
Our model at the University of Chicago relies mainly on residents in training and physician assistants, but advanced nurse practitioners are well suited to a preoperative clinic as well. These types of providers have background training in history-taking, physical examination, diagnostic testing, and disease management. Registered nurses have more limited abilities, although they may be appropriate for a clinic that deals primarily with healthy patients for whom only history taking and a list of medications is needed. Additionally, our clinic is staffed by one attending anesthesiologist at all times (from among a group of rotating anesthesiologists) as well as medical assistants and clerical staff.
Some clinics perform the surgical history and physical exam at the same time as the anesthesia assessment. I would urge caution with this practice. Just as primary care doctors should not be conducting the anesthesia assessment, nonsurgeons should not be conducting the surgical assessment; doing so puts them out on a limb from a medicolegal standpoint. Advanced nurse practitioners and physician assistants may do surgical assessments under the supervision of a surgeon, but only surgeons should ultimately decide—and document—whether an operation is necessary and what degree of examination is required in advance.
Computer technology for records, messaging, billing
Using electronic medical records and corresponding with colleagues by e-mail make preoperative care much more efficient. We have standardized computer forms for ordering tests and documenting the physical exam. Patients usually understand that electronic medical records are safe and more efficient, and they are often more accepting of their use than practitioners are. Many patients want e-mail access to doctors, to schedule appointments online, and to receive appointment reminders by e-mail.3
Electronic medical records also avoid redundancy. If a patient has been seen in our preoperative clinic and is later scheduled for another surgery (even if a different surgeon is involved), a return visit to our clinic may not be necessary. In some cases, we can send the old work-up stamped “For information only,” which can then be updated by the anesthesiologist on the day of surgery.
A central, standardized process also makes billing more efficient and helps to ensure that payment is received for all services provided. Standardized documentation makes it easier for coders to enter the correct evaluation and management codes and ensures that all required criteria are met.
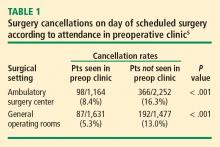
THE PAYOFF: LIVES AND DOLLARS SAVED
A thorough and efficient preoperative assessment system is cost-effective. Every minute of operating room time is worth $10 to $15,4,5 so delays should be avoided. Everything that is done ahead of time saves money for the whole enterprise by reducing unnecessary case setups and reducing “down time” due to lack of patient, equipment, or staff readiness. We routinely bill for preoperative evaluations when this service goes beyond a routine preoperative assessment based on CMS (and other insurance) requirements. However, a preoperative evaluation is required by CMS and most payers if one wants to be paid for any anesthesia-provided service. As a result, a cost is incurred without offsetting revenue if a case is cancelled on the day of surgery after one performs the anesthesia evaluation.
Yesterday I heard someone ask, “Do we really need all this preoperative evaluation? Does it really improve outcomes?” There is some evidence that it does. A study from 2000 based on data from the Australian Incident Monitoring Study found that 11% of the 6,271 critical incidents that occurred following operations were attributable to inadequate preoperative evaluation and that 3% were unequivocally related to problems with preoperative assessment or preparation. More than half of the incidents were deemed preventable.6
Preoperative clinics are good for patients and make good sense economically. We just need to demonstrate to our administrators and to payers that we are offering an excellent service.
Cleveland Clinic IMPACT Center
By Ajay Kumar, MD
Cleveland Clinic is structured differently from most other institutions in that its surgeons, anesthesiologists, and hospitalists are all direct employees of the institution. Despite this unique structure, many aspects of our preoperative clinic—known as the Internal Medicine Preoperative Assessment, Consultation and Treatment (IMPACT) Center—are applicable to other institutions.
Cleveland Clinic is a busy surgical hospital whose preoperative optimization system is designed to provide high-quality care. The IMPACT Center is consulted for most complicated noncardiac surgery patients, and its referral sources include most of the institution’s surgical specialties.
QUEST FOR A BETTER PATIENT EXPERIENCE
When the IMPACT Center was created in 1997, the aim was to focus on the same objectives highlighted by Drs. Bader and Sweitzer: safety, a positive patient experience, enhanced communication, better continuity of care, effective use of resources, and improving throughput by standardizing care.
A prime motivator was the desire to move away from the tendency for presurgical consults to simply “clear the patient for surgery,” and we have indeed evolved considerably from that point. The focus of our perioperative care program today is to comprehensively evaluate risk by taking into account patient-, procedure-, and anesthesia-related factors.
We offer “one-stop shopping,” and our priority is for efficient throughput. We are located in a 12-story building that includes outpatient, preoperative, and surgical clinics and offices. The IMPACT Center is on the first floor along with the preoperative anesthesia consultation and evaluation (PACE) clinic, the laboratory, and ECG and stress-test labs. Patients can undergo radiographic studies on the second floor.
The patient experience counts for a lot. Many of our patients are from another state or country, so efficiency and convenience are especially important. Patients can usually get all assessment and testing done in a single day.
A TIGHTLY MANAGED PROCESS
A ‘smart’ questionnaire starts the process
A computerized report based on the questionnaire guides the surgical office in scheduling the patient to specific areas according to algorithms. Based on case complexity and clinical needs, patients are scheduled for the IMPACT Center along with the PACE clinic; if needed (based on the algorithms), patients also are scheduled for laboratory tests or imaging. This standardized approach helps create a safe passage for patients through the preoperative process with less confusion.
Patient is given a personalized binder
Once all appointments and tests are scheduled, the patient is given a binder containing specific information about the procedure and preoperative instructions. The medical appointment at the IMPACT Center is usually scheduled before the PACE clinic appointment. Patients receive an itinerary for all preoperative appointments and surgical office appointments before the planned surgery. The itinerary is planned so that if additional testing is requested, it can be accommodated on the same day.
At the end of the preoperative assessment, the patient receives printed information with specific preoperative instructions, including which medications to continue or stop.
Standardized, computer-based medical records
Our systems and processes have undergone a good deal of evolution. We have integrated our medical records and use a standard outside medical record retrieval process. The template for the history and physical exam is standard for all Cleveland Clinic patients and is used for all presurgical assessments before all noncardiac surgeries. The template is comprehensive, including the history of the present illness, the review of systems, the physical exam, and anesthesia-related issues. All outside documents are scanned into our electronic medical record system and are available for viewing prior to surgery from any computer connected to the system.
Our preoperative assessment guidelines are also kept updated at a central online location so that all providers have access to them.
Staff keeps process running efficiently
The IMPACT Center is managed by the department of hospital medicine and supported by at least 5.5 full-time physicians every day. We also have two registered nurses, two assistants who help with scheduling and testing, and three secretaries who support the doctors, obtain records, and make arrangements with outside doctors for testing if a patient wants to return home before our testing can be completed.
A secretary also keeps a log for each patient seen in the clinic, tracking all pending issues. The day before surgery, the secretary contacts the appropriate office for anything that is still pending. If she gets no response, the matter is transferred to one of our doctors so that the problem can be resolved at once. This strategy allows us to achieve a nearly 0% rate of surgery delay or cancellation attributable to unavailable test results.
Our patient volumes have increased significantly since we started in 1997. Last year more than 15,000 patients visited the IMPACT Center and now we have expanded our services to regional hospitals within the Cleveland Clinic Health System.
INTERDEPARTMENTAL COMMUNICATION IS CRITICAL
Interdepartmental communication is a must for patient safety, so we encourage a culture of communication between the hospitalist and the surgical team. The location of most of our surgical clinics within the same building as the IMPACT Center further facilitates communication, as does the proximity of the PACE clinic. Additionally, one of our IMPACT Center physicians is accessible around the clock to answer to our surgeon or anesthesiologist colleagues as needed.
We regularly assess our process and seek feedback from surgeons and anesthesiologists. We also conduct yearly patient experience surveys to make sure we are providing patients with the highest quality of care.
Discussion
Question from the audience: Our anesthesia assessment department was approached by our surgeons to do both the anesthesia and surgical assessments, but we felt that would put us in a potential legal conflict if a patient who was assessed that way developed problems. Can you comment?
Dr. Bader: Although we do surgical assessments at our preoperative clinic, we don’t make any decisions about whether or not to proceed with an operation. We get an office note from the surgeon that is directed specifically toward the need for surgery, indications for surgery, and surgical consent. We perform the surgical history and physical examination. Our process is essentially the same as when surgeons have a physician assistant do the history and physical examination in their office. Our practitioners are employed by the hospital, so there is no conflict of interest there.
Comment from the audience: I’m a strong believer in hands-on patient contact. Over my 15 years of practice, we have encountered a lot of unexpected problems during the preoperative exam—aortic stenoses, infections, ventricular septal defects—all of which would never have been detected from a screening form.
Dr. Sweitzer: I agree that we pick up many things by seeing the patient in person. I’ve picked up more cases of aortic stenosis as an anesthesiologist in the preoperative clinic than I ever did as an internist, because the population is high-risk. But patients who have such problems tend to have risk factors and be in certain age groups. Studies indicate that the history is more important than the physical exam: the history suggests about 75% of conditions that are present. The physical exam adds only a little more—perhaps another 15%. Our recommendations are very much consistent with the American College of Cardiology and American Heart Association guidelines on preoperative cardiac evaluation.7 It is more important to identify whether a patient has risk factors for coronary artery disease than to find out whether a stress test or ECG is normal. One needs to do a really good history, but it can be done remotely. Based on certain risk factors identified, high-risk patients can be selected who need to come in and have a physical exam.
Question from the audience: Could you elaborate on the electronic medical record system used at the University of Chicago? I’ve heard there’s a steep learning curve when implementing these kinds of systems. They also are very expensive—I’ve heard that some cost $40 to $80 million. Has enhanced revenue flow offset the costs?
Dr. Sweitzer: We have a home-grown system developed with FileMaker Pro by a computer programmer at our institution. It was a lot easier to develop than people tend to think. There are many savvy computer programmers out there; I’ve had medical students assist me with updating it. We’re now considering developing it as a commercial system. Many systems are available for purchase, including Epic, Pyxis, one from General Electric, and many others. They are very expensive, so smaller institutions might want to use a pay-for-service system.
There definitely is a learning curve to switching to electronic medical records, but it is not nearly as steep as many believe. The extra time it takes a clinician to initially make a computer entry rather than write on paper is vastly recouped downstream: the electronic medical record is legible and organized, and it doesn’t get lost or need to be redone. You can bring up a patient record from 6 months before and reuse it as a template.
Dr. Bader: The discussion of cost savings from preoperative clinics usually focuses on savings from avoiding surgery cancellations and delays and from more efficient laboratory testing, but the biggest savings for an institution is better reimbursement through better diagnosis-related groups (DRG) coding. That’s an important reason our institution is funding our clinic. Electronic medical records allow standardization of information so that coders know exactly where to look for the comorbidities and other pertinent information. This increases payments for DRGs, which can be documented for the hospital. This literally runs into millions of dollars a year and more than offsets the costs of the system.
Question from the audience: Dr. Bader, I’m impressed with the number of patients going through your preoperative clinic. How many patients are seen per nurse practitioner in your clinic?
Dr. Bader: The nurse practitioners have 10-hour shifts and see one patient every 75 minutes. The process of seeing a patient takes a lot less time now than with the old system, in which patients saw an anesthesiologist plus a nurse. Our current system eliminates redundancy: questions need to be asked only once.
Question from the audience: My compliance office says that preoperative assessments for early-morning admission patients are good for only 7 days. Is that true?
Dr. Bader: There are sometimes differences between Joint Commission requirements and those of certain insurance companies. That kind of issue needs to be discussed with your hospital compliance office. We program rules into our scheduling system to accommodate different insurance policies and other requirements so that a patient is not scheduled beyond the allowable period.
- Detsky AS, Naglie IG. A clinician’s guide to cost-effectiveness analysis. Ann Intern Med 1990; 113:147–154.
- Sandler G. The importance of the history in the medical clinic and the cost of unnecessary tests. Am Heart J 1980; 100:928–931.
- Blumenthal D, Glaser JP. Information technology comes to medicine. N Engl J Med 2007; 356:2527–2534.
- Strum DP, Vargas LG, May JH. Surgical subspecialty block utilization and capacity planning: a minimal cost analysis model. Anesthesiology 1999; 90:1176–1185.
- Ferschl MB, Tung A, Sweitzer B, Huo D, Glick DB. Preoperative clinic visits reduce operating room cancellations and delays. Anesthesiology 2005; 103:855–859.
- Kluger MT, Tham EJ, Coleman NA, et al. Inadequate preoperative evaluation and preparation: a review of 197 reports from the Australian incident monitoring study. Anaesthesia 2000; 55:1173–1178.
- Fleisher LA, Beckman JA, Brown KA, et al. ACC/AHA 2007 guidelines on perioperative cardiovascular evaluation and care for noncardiac surgery: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. J Am Coll Cardiol 2007; 50:1707–1732.
Weiner Center for Preoperative Evaluation at Brigham and Women’s Hospital
By Angela M. Bader, MD, MPH
When organizing our preoperative clinic at Brigham and Women’s Hospital, we had several goals. Overall, we wanted a standardized process to help us achieve a high level of excellence. We hoped that creating a new system would eliminate ambiguity about who was responsible for following up on a patient’s abnormal laboratory test result—the surgeon, anesthesiologist, or primary care physician. We also wanted to better coordinate the various care teams involved throughout the perioperative period.
STANDARDIZATION HELPS MEET MANY GOALS
Standardization can occur at many levels:
- Performance of assessments and testing
- Organization of the patient chart and medical records
- Systems checks throughout the process to ensure that nothing is missed
- Team-to-team communication.
Documentation requirements apply regardless of institutional structure
When considering any system of preoperative assessment, keep in mind that the hospital must meet and appropriately document compliance with all regulatory, accreditation, and payer requirements and guidelines, such as those of the Joint Commission, the Centers for Medicare and Medicaid Services (CMS), and the National Surgical Quality Improvement Program. For example, the Joint Commission requires that a surgical history and physical examination be done within 30 days of a procedure. An anesthesiology assessment and a nursing assessment are also required. All of these assessments have mandatory elements, including documenting “never events” and ordering appropriate laboratory tests, electrocardiograms (ECGs), and radiographs.
Sometimes administrators of other hospitals say to me, “We can’t afford a preoperative clinic, and we don’t need one.” My response is that regardless of whether a hospital has a preoperative clinic, the regulatory requirements and guidelines must be met: it is not an issue of avoiding certain steps. Having a dedicated preoperative clinic simply shifts the work to a standardized, centralized system and avoids delaying these required steps until the day of surgery, when taking care of a problem involves the most inefficient use of resources.
Tailor system to institutional needs and characteristics
Within the regulatory framework, the organizational scheme of every institution must address issues of volume and acuity, the types of surgery performed, and the time frames required. A system must be able to deal with the preoperative needs of patients undergoing operations that are booked weeks in advance (often the case for orthopedic surgery) as well as those that may not be booked until a day before the procedure (eg, cancer surgery).
Our plan was developed for our very high-volume, tertiary care institution. In 2008, 24,000 patients used our clinic (roughly 100 patients per day).
DESIGN OF THE PREOPERATIVE CLINIC
A nurse practitioner–based model for ‘one-stop shopping’
We decided that the clinic should offer all elements of the preoperative assessment and thereby give patients “one-stop shopping.” Each patient sees a nurse practitioner, who performs the surgical history and physical examination as well as the anesthesiology and nursing assessments. The result is a multidisciplinary approach with a single assessment output. We shifted employees who had been responsible for preoperative assessment in the offices of various surgeons to a central clinic so that all assessments could be standardized, and we provided additional training to enable them to perform various assessments. The nurse practitioners are supervised by an on-site attending physician, as detailed below.
This model offers a number of advantages:
- Patients see a single provider.
- Assessment is facilitated for our surgeons, who may not be completely up-to-date on perioperative risk assessment and management.
- We have a central location for standardized education programs for our physicians, nurses, and residents.
- The clinic’s standardized records and processes facilitate data generation for research and clinical practice improvement.
Independent budgetary and staffing structure
The preoperative clinic is a separate cost center under the leadership of the department of anesthesiology. Resources were shifted to a central location so that as volume increases, we can add resources to meet the additional volume. We contracted with the hospital administration to provide payment for two full-time-equivalent anesthesiologists per day, who serve as on-site attending physicians. The hospital is willing to do this because not only do these attending physicians supervise the anesthesiology assessment, they are the collaborating physicians for the entire perioperative assessment. They review every patient, order tests and write prescriptions as needed, and discuss issues with the primary care physicians and referring specialists.
The preoperative clinic has an anesthesiologist director (me) who reports directly to the hospital’s vice president for surgical services on budget and staffing issues. I also report to the chairman of the department of anesthesiology, though he is not involved in budgetary functions (the hospital contracts with him to provide the anesthesiology staffing). The clerical and nursing staff work directly for the clinic.
The clinic is run in a self-contained area with a central waiting room and space for doing all the assessments and laboratory work internally, including 16 examination rooms and a room for chart organization.
MORE BENEFITS OF STANDARDIZATION
Standardized scheduling ensures reliability
The secretaries in each surgeon’s office schedule appointments through a central computer system after registration and insurance precertification. Our computer system does not allow an operation to be scheduled without an evaluation also being scheduled. The evaluation can involve either a visit or a telephone screen; we provide algorithms so that the surgeons’ secretaries know which is required. This system has substantially reduced the number of walk-ins, allowing for a more even distribution of patients and ensuring that medical records will be available when a patient is seen.
We watch our schedule carefully. Our computer system monitors the time that each patient is in our clinic to determine his or her waiting time and assessment time. It takes about 75 minutes to go through the whole process, including the time for a nurse practitioner to do the surgical history and physical examination and the anesthesiology and nursing assessments, a laboratory technician to do an ECG and laboratory tests if indicated, and completion of all required documentation. Accordingly, patients are scheduled in 75-minute blocks between 7:00 am and 6:30 pm. We do not have evening or weekend hours because of the difficulty of contacting surgeons and primary care physicians when questions arise. It is simply not cost-effective to have to do that type of follow-up on a case after the patient leaves.
Only about 10% of our patients are screened by telephone, since most of our operations are complicated and require in-person assessment (most low-acuity procedures are done at other hospitals). Of the patients who visit the preoperative clinic, about 75% undergo the single assessment model for surgery, anesthesiology, and nursing as described above. The remaining 25% of patients have their history and physical exam completed outside Brigham and Women’s Hospital for insurance reasons; the remainder of their assessment is conducted in our preoperative clinic by a registered nurse and an anesthesiology resident.
Multiple systems checks
Our model also incorporates standardization in the form of multiple systems checks:
- Case presentation. Every case is presented to an attending anesthesiologist, who reviews the ECG (if ordered) before the patient leaves the clinic.
- Post-visit chart check. A registered nurse or nurse practitioner signs off on each chart after the visit, confirming test results and resolution of all paperwork issues.
- Surgical checklist. The end result is a checklist that serves as the front sheet of the operating room chart.
Our ability to use this system of checks to get the chart completed comprehensively and reliably and deliver it to the operating room when needed was key to securing institutional support and funding for the preoperative clinic.
ROLE OF THE ATTENDING ANESTHESIOLOGISTS
Two full-time attending anesthesiologists are present in the preoperative clinic each day. One is responsible largely for supervising the nurse practitioner assessments and reviewing case presentations, while the other also oversees the education and supervision of residents. Residents rotate through the clinic for 2 weeks (one or two at a time) and have a designated curriculum consisting of daily lectures and competencies in preoperative evaluation.
Because our anesthesiologists are expert in preoperative assessment, we require very few outside consults. We can communicate directly with the cardiologists and other physicians and order tests when indicated. We have a clerical assistant who obtains all necessary paperwork and prior testing from outside providers so that the clinicians need not waste time on this.
A GROWING CHALLENGE: ASSESSMENT FOR PROCEDURES IN AMBULATORY SETTINGS
Looking forward, a rapidly growing challenge facing our clinic stems from the tremendous growth in patients who require anesthesia for procedures performed outside the operating room. In these situations, the proceduralists need a system for deciding whether an anesthesiologist must be present for any given case.
We have started to develop appropriate screening processes to ensure that the proceduralists in multiple departments know which patients to refer for preprocedure assessment. We hope to soon develop protocols for high-risk patients and for various procedures such as implanting a pacemaker or defibrillator, catheter procedures, interventional radiology, and endoscopy.
Anesthesia Perioperative Medicine Clinic at University of Chicago
By BobbieJean Sweitzer, MD
Detsky and Naglie have argued that the costs and clinical outcomes associated with any intervention must be compared with those of alternate strategies for treating the same patients,1 and I believe their point applies well to preoperative clinics. Although certain requirements of the Joint Commission and CMS must be met, as noted by Dr. Bader, they can be met in various ways. I will preface my comments by emphasizing that one size does not fit all: every institution must decide the best approach to preoperative assessment based on its patient population, the types of procedures it performs, and the volume it handles.
TRIAGE STREAMLINES THE PROCESS
Our preoperative clinic at the University of Chicago emphasizes triage. Not every patient should have to go to the trouble of coming in to see a provider. In the future, we will likely see more “virtual” preoperative assessments using devices in development, such as handheld ultrasonography machines. Just as patients can have their pacemakers and implantable cardiac defibrillators remotely checked via phone contact, more tools will one day be available for remote assessment.
Although not every surgical patient needs to come in to the preoperative clinic, every patient must have a physical examination. All patients will be seen on the day of surgery, so in some cases the physical exam may be able to wait until then. For example, an airway assessment need not be done ahead of time. Most anesthesiologists are prepared to manage airways on very short notice, so extensive advance planning is not always necessary.
Obtain basic info by questionnaire to save staff time
Information about the patient is key to triage, and it may be either paper- or computer-based. An initial priority should be to develop some mechanism for getting information from patients before the day of their procedure without a visit to the hospital or ambulatory surgery center.
We use a two-page paper questionnaire to obtain basic information from patients, including (among other pertinent questions) age, planned operation, names of the surgeon and primary doctor, past operations and medical history, allergies, a list of medications, social history (drug, alcohol, tobacco use), whether they have ever taken steroids, whether they have high blood pressure, and whether they can comfortably walk up a flight of stairs. We provide the primary care physicians and surgeons with blank questionnaires, which their patients can fill out in their waiting rooms or take home and fax to us (or drop off) later. The questionnaire gives us a good deal of essential information without using staff time.
Various computer-based and Web-based systems are also available for collecting basic patient information. Smaller institutions need not purchase an entire electronic medical record system, which can be very expensive. Some Web-based tools operate on a pay-per-use basis and can be very helpful.
Review the information to guide triage
We then review the patient information to determine the extent of preoperative evaluation required. Some patients, especially those scheduled at an ambulatory surgery center, are healthy enough that they can just come in on the day of surgery for an examination and an update of their information. Others will need an appointment at the clinic before the day of surgery for more extensive preoperative evaluation. For other patients, review of their questionnaire responses may prompt a phone call or e-mail from the clinic for more information to determine whether a day-of-surgery exam will suffice or whether evaluation in advance is needed. When in doubt, concerns raised by the questionnaire should be explored before the day of surgery to avoid surprises and allow sufficient time for a consultation, if needed.
STANDARDIZED GUIDELINES KEEP CARE CONSISTENT
We encourage our staff to minimize preoperative testing and ECGs. A majority of diagnoses are made based on the history and physical exam.2 Generally, a test should confirm what is already suspected and merely provide objective evidence when needed. Testing in this setting should not be done to “find out what is wrong” with a patient.
It is helpful to develop standardized guidelines for preoperative assessment and make them available to everyone in the institution via the Web. The guidelines should address recommended preoperative tests and management practices according to specific patient conditions or surgical procedures. The clear objective is to avoid disagreement about what a patient needs between the provider who evaluated the patient in advance and the surgeon or anesthesiologist who evaluates the patient on the day of surgery.
Our guidelines at the University of Chicago include recommendations for patients on long-term anticoagulant therapy, for patients with coronary stents, for medications that should be discontinued (and those that may be continued) on the day of surgery, and for numerous other conditions and issues. Our testing guidelines list indicated tests for various medical problems, which in turn link to other guidelines. Other links are based on the medications a patient is using or the type of operation that is planned.
We collaborated with our electrophysiology department to create guidelines for managing patients with pacemakers and defibrillators. Almost every patient with one of these devices has a little card associated with the device, and we ask the surgeons to copy the card and send it to the clinic if we will not be directly seeing the patient. Using a national database, the electrophysiology department can determine from the card the type of pacemaker or defibrillator a patient has, and they fax or e-mail us back a page of instructions to let us know whether the device requires special consideration during surgery, whether it should be checked preoperatively, and whether its battery needs replacing. With this system, we have markedly reduced problems on the day of surgery.
CONSULTS HAVE AN IMPORTANT ROLE
Consults should never be requested in order to “clear a patient for surgery.” Consult requests should rather address specific issues, such as, “Is this patient medically optimized?” or “Please address this patient’s hypertension.” In turn, consult notes should provide meaningful information that can be used in a specific way. A clearance letter or simple risk assessment is not helpful.
If a patient has not seen a primary care doctor in a long time, a consult request should (in addition to requesting a global risk assessment) specify any particular concerns, such as, “The patient reports snoring; please address sleep apnea and cardiac risk.”
Case study: Beware consult notes with no specifics
Consider a case we encountered of a 54-year-old man who had a preoperative cardiac risk assessment. The cardiology consultant completed a short form consisting of a multiple-choice check-off list indicating low, moderate, or high cardiac risk. The consultant checked that the patient had low cardiac risk but provided no other instructions or information other than his own contact information.
When we reviewed the patient’s questionnaire, we saw that his medications included metoprolol, clopidogrel, and aspirin even though the patient did not mention that he had coronary artery disease. On this basis, we requested details about his cardiac evaluation from his cardiologist. It turned out that the patient had a history of four catheterizations with several cardiac stents placed. The most recent stent was implanted to overlap a previous stent that had been found “floating” in the blood vessel; this last stent was placed just 6 months before the cardiologist issued the consult note indicating “low cardiac risk.”
The moral is to approach consult notes with caution, especially if they offer no specifics. It actually makes me nervous when a note states “low risk” because if something unexpectedly goes wrong in surgery, it appears that the perioperative team took poor care of the patient even if the complication actually may have stemmed from higher-than-recognized underlying patient risk.
PROVIDE, AND REINFORCE, CLEAR INSTRUCTIONS
We give patients written preoperative instructions that become part of our computerized records. We first verbally give explicit instructions for each medication—ie, whether it can be taken as usual or when it needs to be stopped before surgery (and why). Then we provide the same information in writing, after which we try to have the patient repeat the instructions back to the clinician. We include a phone number that patients can call if they need help understanding their preoperative instructions.
Web-based programs also can provide patients online instructions about their medications. Some services even customize information by providing, for example, lists of local surgeons who are willing to allow a patient to continue on aspirin therapy until the day of surgery.
USE THE RIGHT RESOURCES
Staffing
Our model at the University of Chicago relies mainly on residents in training and physician assistants, but advanced nurse practitioners are well suited to a preoperative clinic as well. These types of providers have background training in history-taking, physical examination, diagnostic testing, and disease management. Registered nurses have more limited abilities, although they may be appropriate for a clinic that deals primarily with healthy patients for whom only history taking and a list of medications is needed. Additionally, our clinic is staffed by one attending anesthesiologist at all times (from among a group of rotating anesthesiologists) as well as medical assistants and clerical staff.
Some clinics perform the surgical history and physical exam at the same time as the anesthesia assessment. I would urge caution with this practice. Just as primary care doctors should not be conducting the anesthesia assessment, nonsurgeons should not be conducting the surgical assessment; doing so puts them out on a limb from a medicolegal standpoint. Advanced nurse practitioners and physician assistants may do surgical assessments under the supervision of a surgeon, but only surgeons should ultimately decide—and document—whether an operation is necessary and what degree of examination is required in advance.
Computer technology for records, messaging, billing
Using electronic medical records and corresponding with colleagues by e-mail make preoperative care much more efficient. We have standardized computer forms for ordering tests and documenting the physical exam. Patients usually understand that electronic medical records are safe and more efficient, and they are often more accepting of their use than practitioners are. Many patients want e-mail access to doctors, to schedule appointments online, and to receive appointment reminders by e-mail.3
Electronic medical records also avoid redundancy. If a patient has been seen in our preoperative clinic and is later scheduled for another surgery (even if a different surgeon is involved), a return visit to our clinic may not be necessary. In some cases, we can send the old work-up stamped “For information only,” which can then be updated by the anesthesiologist on the day of surgery.
A central, standardized process also makes billing more efficient and helps to ensure that payment is received for all services provided. Standardized documentation makes it easier for coders to enter the correct evaluation and management codes and ensures that all required criteria are met.
THE PAYOFF: LIVES AND DOLLARS SAVED
A thorough and efficient preoperative assessment system is cost-effective. Every minute of operating room time is worth $10 to $15,4,5 so delays should be avoided. Everything that is done ahead of time saves money for the whole enterprise by reducing unnecessary case setups and reducing “down time” due to lack of patient, equipment, or staff readiness. We routinely bill for preoperative evaluations when this service goes beyond a routine preoperative assessment based on CMS (and other insurance) requirements. However, a preoperative evaluation is required by CMS and most payers if one wants to be paid for any anesthesia-provided service. As a result, a cost is incurred without offsetting revenue if a case is cancelled on the day of surgery after one performs the anesthesia evaluation.
Yesterday I heard someone ask, “Do we really need all this preoperative evaluation? Does it really improve outcomes?” There is some evidence that it does. A study from 2000 based on data from the Australian Incident Monitoring Study found that 11% of the 6,271 critical incidents that occurred following operations were attributable to inadequate preoperative evaluation and that 3% were unequivocally related to problems with preoperative assessment or preparation. More than half of the incidents were deemed preventable.6
Preoperative clinics are good for patients and make good sense economically. We just need to demonstrate to our administrators and to payers that we are offering an excellent service.
Cleveland Clinic IMPACT Center
By Ajay Kumar, MD
Cleveland Clinic is structured differently from most other institutions in that its surgeons, anesthesiologists, and hospitalists are all direct employees of the institution. Despite this unique structure, many aspects of our preoperative clinic—known as the Internal Medicine Preoperative Assessment, Consultation and Treatment (IMPACT) Center—are applicable to other institutions.
Cleveland Clinic is a busy surgical hospital whose preoperative optimization system is designed to provide high-quality care. The IMPACT Center is consulted for most complicated noncardiac surgery patients, and its referral sources include most of the institution’s surgical specialties.
QUEST FOR A BETTER PATIENT EXPERIENCE
When the IMPACT Center was created in 1997, the aim was to focus on the same objectives highlighted by Drs. Bader and Sweitzer: safety, a positive patient experience, enhanced communication, better continuity of care, effective use of resources, and improving throughput by standardizing care.
A prime motivator was the desire to move away from the tendency for presurgical consults to simply “clear the patient for surgery,” and we have indeed evolved considerably from that point. The focus of our perioperative care program today is to comprehensively evaluate risk by taking into account patient-, procedure-, and anesthesia-related factors.
We offer “one-stop shopping,” and our priority is for efficient throughput. We are located in a 12-story building that includes outpatient, preoperative, and surgical clinics and offices. The IMPACT Center is on the first floor along with the preoperative anesthesia consultation and evaluation (PACE) clinic, the laboratory, and ECG and stress-test labs. Patients can undergo radiographic studies on the second floor.
The patient experience counts for a lot. Many of our patients are from another state or country, so efficiency and convenience are especially important. Patients can usually get all assessment and testing done in a single day.
A TIGHTLY MANAGED PROCESS
A ‘smart’ questionnaire starts the process
A computerized report based on the questionnaire guides the surgical office in scheduling the patient to specific areas according to algorithms. Based on case complexity and clinical needs, patients are scheduled for the IMPACT Center along with the PACE clinic; if needed (based on the algorithms), patients also are scheduled for laboratory tests or imaging. This standardized approach helps create a safe passage for patients through the preoperative process with less confusion.
Patient is given a personalized binder
Once all appointments and tests are scheduled, the patient is given a binder containing specific information about the procedure and preoperative instructions. The medical appointment at the IMPACT Center is usually scheduled before the PACE clinic appointment. Patients receive an itinerary for all preoperative appointments and surgical office appointments before the planned surgery. The itinerary is planned so that if additional testing is requested, it can be accommodated on the same day.
At the end of the preoperative assessment, the patient receives printed information with specific preoperative instructions, including which medications to continue or stop.
Standardized, computer-based medical records
Our systems and processes have undergone a good deal of evolution. We have integrated our medical records and use a standard outside medical record retrieval process. The template for the history and physical exam is standard for all Cleveland Clinic patients and is used for all presurgical assessments before all noncardiac surgeries. The template is comprehensive, including the history of the present illness, the review of systems, the physical exam, and anesthesia-related issues. All outside documents are scanned into our electronic medical record system and are available for viewing prior to surgery from any computer connected to the system.
Our preoperative assessment guidelines are also kept updated at a central online location so that all providers have access to them.
Staff keeps process running efficiently
The IMPACT Center is managed by the department of hospital medicine and supported by at least 5.5 full-time physicians every day. We also have two registered nurses, two assistants who help with scheduling and testing, and three secretaries who support the doctors, obtain records, and make arrangements with outside doctors for testing if a patient wants to return home before our testing can be completed.
A secretary also keeps a log for each patient seen in the clinic, tracking all pending issues. The day before surgery, the secretary contacts the appropriate office for anything that is still pending. If she gets no response, the matter is transferred to one of our doctors so that the problem can be resolved at once. This strategy allows us to achieve a nearly 0% rate of surgery delay or cancellation attributable to unavailable test results.
Our patient volumes have increased significantly since we started in 1997. Last year more than 15,000 patients visited the IMPACT Center and now we have expanded our services to regional hospitals within the Cleveland Clinic Health System.
INTERDEPARTMENTAL COMMUNICATION IS CRITICAL
Interdepartmental communication is a must for patient safety, so we encourage a culture of communication between the hospitalist and the surgical team. The location of most of our surgical clinics within the same building as the IMPACT Center further facilitates communication, as does the proximity of the PACE clinic. Additionally, one of our IMPACT Center physicians is accessible around the clock to answer to our surgeon or anesthesiologist colleagues as needed.
We regularly assess our process and seek feedback from surgeons and anesthesiologists. We also conduct yearly patient experience surveys to make sure we are providing patients with the highest quality of care.
Discussion
Question from the audience: Our anesthesia assessment department was approached by our surgeons to do both the anesthesia and surgical assessments, but we felt that would put us in a potential legal conflict if a patient who was assessed that way developed problems. Can you comment?
Dr. Bader: Although we do surgical assessments at our preoperative clinic, we don’t make any decisions about whether or not to proceed with an operation. We get an office note from the surgeon that is directed specifically toward the need for surgery, indications for surgery, and surgical consent. We perform the surgical history and physical examination. Our process is essentially the same as when surgeons have a physician assistant do the history and physical examination in their office. Our practitioners are employed by the hospital, so there is no conflict of interest there.
Comment from the audience: I’m a strong believer in hands-on patient contact. Over my 15 years of practice, we have encountered a lot of unexpected problems during the preoperative exam—aortic stenoses, infections, ventricular septal defects—all of which would never have been detected from a screening form.
Dr. Sweitzer: I agree that we pick up many things by seeing the patient in person. I’ve picked up more cases of aortic stenosis as an anesthesiologist in the preoperative clinic than I ever did as an internist, because the population is high-risk. But patients who have such problems tend to have risk factors and be in certain age groups. Studies indicate that the history is more important than the physical exam: the history suggests about 75% of conditions that are present. The physical exam adds only a little more—perhaps another 15%. Our recommendations are very much consistent with the American College of Cardiology and American Heart Association guidelines on preoperative cardiac evaluation.7 It is more important to identify whether a patient has risk factors for coronary artery disease than to find out whether a stress test or ECG is normal. One needs to do a really good history, but it can be done remotely. Based on certain risk factors identified, high-risk patients can be selected who need to come in and have a physical exam.
Question from the audience: Could you elaborate on the electronic medical record system used at the University of Chicago? I’ve heard there’s a steep learning curve when implementing these kinds of systems. They also are very expensive—I’ve heard that some cost $40 to $80 million. Has enhanced revenue flow offset the costs?
Dr. Sweitzer: We have a home-grown system developed with FileMaker Pro by a computer programmer at our institution. It was a lot easier to develop than people tend to think. There are many savvy computer programmers out there; I’ve had medical students assist me with updating it. We’re now considering developing it as a commercial system. Many systems are available for purchase, including Epic, Pyxis, one from General Electric, and many others. They are very expensive, so smaller institutions might want to use a pay-for-service system.
There definitely is a learning curve to switching to electronic medical records, but it is not nearly as steep as many believe. The extra time it takes a clinician to initially make a computer entry rather than write on paper is vastly recouped downstream: the electronic medical record is legible and organized, and it doesn’t get lost or need to be redone. You can bring up a patient record from 6 months before and reuse it as a template.
Dr. Bader: The discussion of cost savings from preoperative clinics usually focuses on savings from avoiding surgery cancellations and delays and from more efficient laboratory testing, but the biggest savings for an institution is better reimbursement through better diagnosis-related groups (DRG) coding. That’s an important reason our institution is funding our clinic. Electronic medical records allow standardization of information so that coders know exactly where to look for the comorbidities and other pertinent information. This increases payments for DRGs, which can be documented for the hospital. This literally runs into millions of dollars a year and more than offsets the costs of the system.
Question from the audience: Dr. Bader, I’m impressed with the number of patients going through your preoperative clinic. How many patients are seen per nurse practitioner in your clinic?
Dr. Bader: The nurse practitioners have 10-hour shifts and see one patient every 75 minutes. The process of seeing a patient takes a lot less time now than with the old system, in which patients saw an anesthesiologist plus a nurse. Our current system eliminates redundancy: questions need to be asked only once.
Question from the audience: My compliance office says that preoperative assessments for early-morning admission patients are good for only 7 days. Is that true?
Dr. Bader: There are sometimes differences between Joint Commission requirements and those of certain insurance companies. That kind of issue needs to be discussed with your hospital compliance office. We program rules into our scheduling system to accommodate different insurance policies and other requirements so that a patient is not scheduled beyond the allowable period.
Weiner Center for Preoperative Evaluation at Brigham and Women’s Hospital
By Angela M. Bader, MD, MPH
When organizing our preoperative clinic at Brigham and Women’s Hospital, we had several goals. Overall, we wanted a standardized process to help us achieve a high level of excellence. We hoped that creating a new system would eliminate ambiguity about who was responsible for following up on a patient’s abnormal laboratory test result—the surgeon, anesthesiologist, or primary care physician. We also wanted to better coordinate the various care teams involved throughout the perioperative period.
STANDARDIZATION HELPS MEET MANY GOALS
Standardization can occur at many levels:
- Performance of assessments and testing
- Organization of the patient chart and medical records
- Systems checks throughout the process to ensure that nothing is missed
- Team-to-team communication.
Documentation requirements apply regardless of institutional structure
When considering any system of preoperative assessment, keep in mind that the hospital must meet and appropriately document compliance with all regulatory, accreditation, and payer requirements and guidelines, such as those of the Joint Commission, the Centers for Medicare and Medicaid Services (CMS), and the National Surgical Quality Improvement Program. For example, the Joint Commission requires that a surgical history and physical examination be done within 30 days of a procedure. An anesthesiology assessment and a nursing assessment are also required. All of these assessments have mandatory elements, including documenting “never events” and ordering appropriate laboratory tests, electrocardiograms (ECGs), and radiographs.
Sometimes administrators of other hospitals say to me, “We can’t afford a preoperative clinic, and we don’t need one.” My response is that regardless of whether a hospital has a preoperative clinic, the regulatory requirements and guidelines must be met: it is not an issue of avoiding certain steps. Having a dedicated preoperative clinic simply shifts the work to a standardized, centralized system and avoids delaying these required steps until the day of surgery, when taking care of a problem involves the most inefficient use of resources.
Tailor system to institutional needs and characteristics
Within the regulatory framework, the organizational scheme of every institution must address issues of volume and acuity, the types of surgery performed, and the time frames required. A system must be able to deal with the preoperative needs of patients undergoing operations that are booked weeks in advance (often the case for orthopedic surgery) as well as those that may not be booked until a day before the procedure (eg, cancer surgery).
Our plan was developed for our very high-volume, tertiary care institution. In 2008, 24,000 patients used our clinic (roughly 100 patients per day).
DESIGN OF THE PREOPERATIVE CLINIC
A nurse practitioner–based model for ‘one-stop shopping’
We decided that the clinic should offer all elements of the preoperative assessment and thereby give patients “one-stop shopping.” Each patient sees a nurse practitioner, who performs the surgical history and physical examination as well as the anesthesiology and nursing assessments. The result is a multidisciplinary approach with a single assessment output. We shifted employees who had been responsible for preoperative assessment in the offices of various surgeons to a central clinic so that all assessments could be standardized, and we provided additional training to enable them to perform various assessments. The nurse practitioners are supervised by an on-site attending physician, as detailed below.
This model offers a number of advantages:
- Patients see a single provider.
- Assessment is facilitated for our surgeons, who may not be completely up-to-date on perioperative risk assessment and management.
- We have a central location for standardized education programs for our physicians, nurses, and residents.
- The clinic’s standardized records and processes facilitate data generation for research and clinical practice improvement.
Independent budgetary and staffing structure
The preoperative clinic is a separate cost center under the leadership of the department of anesthesiology. Resources were shifted to a central location so that as volume increases, we can add resources to meet the additional volume. We contracted with the hospital administration to provide payment for two full-time-equivalent anesthesiologists per day, who serve as on-site attending physicians. The hospital is willing to do this because not only do these attending physicians supervise the anesthesiology assessment, they are the collaborating physicians for the entire perioperative assessment. They review every patient, order tests and write prescriptions as needed, and discuss issues with the primary care physicians and referring specialists.
The preoperative clinic has an anesthesiologist director (me) who reports directly to the hospital’s vice president for surgical services on budget and staffing issues. I also report to the chairman of the department of anesthesiology, though he is not involved in budgetary functions (the hospital contracts with him to provide the anesthesiology staffing). The clerical and nursing staff work directly for the clinic.
The clinic is run in a self-contained area with a central waiting room and space for doing all the assessments and laboratory work internally, including 16 examination rooms and a room for chart organization.
MORE BENEFITS OF STANDARDIZATION
Standardized scheduling ensures reliability
The secretaries in each surgeon’s office schedule appointments through a central computer system after registration and insurance precertification. Our computer system does not allow an operation to be scheduled without an evaluation also being scheduled. The evaluation can involve either a visit or a telephone screen; we provide algorithms so that the surgeons’ secretaries know which is required. This system has substantially reduced the number of walk-ins, allowing for a more even distribution of patients and ensuring that medical records will be available when a patient is seen.
We watch our schedule carefully. Our computer system monitors the time that each patient is in our clinic to determine his or her waiting time and assessment time. It takes about 75 minutes to go through the whole process, including the time for a nurse practitioner to do the surgical history and physical examination and the anesthesiology and nursing assessments, a laboratory technician to do an ECG and laboratory tests if indicated, and completion of all required documentation. Accordingly, patients are scheduled in 75-minute blocks between 7:00 am and 6:30 pm. We do not have evening or weekend hours because of the difficulty of contacting surgeons and primary care physicians when questions arise. It is simply not cost-effective to have to do that type of follow-up on a case after the patient leaves.
Only about 10% of our patients are screened by telephone, since most of our operations are complicated and require in-person assessment (most low-acuity procedures are done at other hospitals). Of the patients who visit the preoperative clinic, about 75% undergo the single assessment model for surgery, anesthesiology, and nursing as described above. The remaining 25% of patients have their history and physical exam completed outside Brigham and Women’s Hospital for insurance reasons; the remainder of their assessment is conducted in our preoperative clinic by a registered nurse and an anesthesiology resident.
Multiple systems checks
Our model also incorporates standardization in the form of multiple systems checks:
- Case presentation. Every case is presented to an attending anesthesiologist, who reviews the ECG (if ordered) before the patient leaves the clinic.
- Post-visit chart check. A registered nurse or nurse practitioner signs off on each chart after the visit, confirming test results and resolution of all paperwork issues.
- Surgical checklist. The end result is a checklist that serves as the front sheet of the operating room chart.
Our ability to use this system of checks to get the chart completed comprehensively and reliably and deliver it to the operating room when needed was key to securing institutional support and funding for the preoperative clinic.
ROLE OF THE ATTENDING ANESTHESIOLOGISTS
Two full-time attending anesthesiologists are present in the preoperative clinic each day. One is responsible largely for supervising the nurse practitioner assessments and reviewing case presentations, while the other also oversees the education and supervision of residents. Residents rotate through the clinic for 2 weeks (one or two at a time) and have a designated curriculum consisting of daily lectures and competencies in preoperative evaluation.
Because our anesthesiologists are expert in preoperative assessment, we require very few outside consults. We can communicate directly with the cardiologists and other physicians and order tests when indicated. We have a clerical assistant who obtains all necessary paperwork and prior testing from outside providers so that the clinicians need not waste time on this.
A GROWING CHALLENGE: ASSESSMENT FOR PROCEDURES IN AMBULATORY SETTINGS
Looking forward, a rapidly growing challenge facing our clinic stems from the tremendous growth in patients who require anesthesia for procedures performed outside the operating room. In these situations, the proceduralists need a system for deciding whether an anesthesiologist must be present for any given case.
We have started to develop appropriate screening processes to ensure that the proceduralists in multiple departments know which patients to refer for preprocedure assessment. We hope to soon develop protocols for high-risk patients and for various procedures such as implanting a pacemaker or defibrillator, catheter procedures, interventional radiology, and endoscopy.
Anesthesia Perioperative Medicine Clinic at University of Chicago
By BobbieJean Sweitzer, MD
Detsky and Naglie have argued that the costs and clinical outcomes associated with any intervention must be compared with those of alternate strategies for treating the same patients,1 and I believe their point applies well to preoperative clinics. Although certain requirements of the Joint Commission and CMS must be met, as noted by Dr. Bader, they can be met in various ways. I will preface my comments by emphasizing that one size does not fit all: every institution must decide the best approach to preoperative assessment based on its patient population, the types of procedures it performs, and the volume it handles.
TRIAGE STREAMLINES THE PROCESS
Our preoperative clinic at the University of Chicago emphasizes triage. Not every patient should have to go to the trouble of coming in to see a provider. In the future, we will likely see more “virtual” preoperative assessments using devices in development, such as handheld ultrasonography machines. Just as patients can have their pacemakers and implantable cardiac defibrillators remotely checked via phone contact, more tools will one day be available for remote assessment.
Although not every surgical patient needs to come in to the preoperative clinic, every patient must have a physical examination. All patients will be seen on the day of surgery, so in some cases the physical exam may be able to wait until then. For example, an airway assessment need not be done ahead of time. Most anesthesiologists are prepared to manage airways on very short notice, so extensive advance planning is not always necessary.
Obtain basic info by questionnaire to save staff time
Information about the patient is key to triage, and it may be either paper- or computer-based. An initial priority should be to develop some mechanism for getting information from patients before the day of their procedure without a visit to the hospital or ambulatory surgery center.
We use a two-page paper questionnaire to obtain basic information from patients, including (among other pertinent questions) age, planned operation, names of the surgeon and primary doctor, past operations and medical history, allergies, a list of medications, social history (drug, alcohol, tobacco use), whether they have ever taken steroids, whether they have high blood pressure, and whether they can comfortably walk up a flight of stairs. We provide the primary care physicians and surgeons with blank questionnaires, which their patients can fill out in their waiting rooms or take home and fax to us (or drop off) later. The questionnaire gives us a good deal of essential information without using staff time.
Various computer-based and Web-based systems are also available for collecting basic patient information. Smaller institutions need not purchase an entire electronic medical record system, which can be very expensive. Some Web-based tools operate on a pay-per-use basis and can be very helpful.
Review the information to guide triage
We then review the patient information to determine the extent of preoperative evaluation required. Some patients, especially those scheduled at an ambulatory surgery center, are healthy enough that they can just come in on the day of surgery for an examination and an update of their information. Others will need an appointment at the clinic before the day of surgery for more extensive preoperative evaluation. For other patients, review of their questionnaire responses may prompt a phone call or e-mail from the clinic for more information to determine whether a day-of-surgery exam will suffice or whether evaluation in advance is needed. When in doubt, concerns raised by the questionnaire should be explored before the day of surgery to avoid surprises and allow sufficient time for a consultation, if needed.
STANDARDIZED GUIDELINES KEEP CARE CONSISTENT
We encourage our staff to minimize preoperative testing and ECGs. A majority of diagnoses are made based on the history and physical exam.2 Generally, a test should confirm what is already suspected and merely provide objective evidence when needed. Testing in this setting should not be done to “find out what is wrong” with a patient.
It is helpful to develop standardized guidelines for preoperative assessment and make them available to everyone in the institution via the Web. The guidelines should address recommended preoperative tests and management practices according to specific patient conditions or surgical procedures. The clear objective is to avoid disagreement about what a patient needs between the provider who evaluated the patient in advance and the surgeon or anesthesiologist who evaluates the patient on the day of surgery.
Our guidelines at the University of Chicago include recommendations for patients on long-term anticoagulant therapy, for patients with coronary stents, for medications that should be discontinued (and those that may be continued) on the day of surgery, and for numerous other conditions and issues. Our testing guidelines list indicated tests for various medical problems, which in turn link to other guidelines. Other links are based on the medications a patient is using or the type of operation that is planned.
We collaborated with our electrophysiology department to create guidelines for managing patients with pacemakers and defibrillators. Almost every patient with one of these devices has a little card associated with the device, and we ask the surgeons to copy the card and send it to the clinic if we will not be directly seeing the patient. Using a national database, the electrophysiology department can determine from the card the type of pacemaker or defibrillator a patient has, and they fax or e-mail us back a page of instructions to let us know whether the device requires special consideration during surgery, whether it should be checked preoperatively, and whether its battery needs replacing. With this system, we have markedly reduced problems on the day of surgery.
CONSULTS HAVE AN IMPORTANT ROLE
Consults should never be requested in order to “clear a patient for surgery.” Consult requests should rather address specific issues, such as, “Is this patient medically optimized?” or “Please address this patient’s hypertension.” In turn, consult notes should provide meaningful information that can be used in a specific way. A clearance letter or simple risk assessment is not helpful.
If a patient has not seen a primary care doctor in a long time, a consult request should (in addition to requesting a global risk assessment) specify any particular concerns, such as, “The patient reports snoring; please address sleep apnea and cardiac risk.”
Case study: Beware consult notes with no specifics
Consider a case we encountered of a 54-year-old man who had a preoperative cardiac risk assessment. The cardiology consultant completed a short form consisting of a multiple-choice check-off list indicating low, moderate, or high cardiac risk. The consultant checked that the patient had low cardiac risk but provided no other instructions or information other than his own contact information.
When we reviewed the patient’s questionnaire, we saw that his medications included metoprolol, clopidogrel, and aspirin even though the patient did not mention that he had coronary artery disease. On this basis, we requested details about his cardiac evaluation from his cardiologist. It turned out that the patient had a history of four catheterizations with several cardiac stents placed. The most recent stent was implanted to overlap a previous stent that had been found “floating” in the blood vessel; this last stent was placed just 6 months before the cardiologist issued the consult note indicating “low cardiac risk.”
The moral is to approach consult notes with caution, especially if they offer no specifics. It actually makes me nervous when a note states “low risk” because if something unexpectedly goes wrong in surgery, it appears that the perioperative team took poor care of the patient even if the complication actually may have stemmed from higher-than-recognized underlying patient risk.
PROVIDE, AND REINFORCE, CLEAR INSTRUCTIONS
We give patients written preoperative instructions that become part of our computerized records. We first verbally give explicit instructions for each medication—ie, whether it can be taken as usual or when it needs to be stopped before surgery (and why). Then we provide the same information in writing, after which we try to have the patient repeat the instructions back to the clinician. We include a phone number that patients can call if they need help understanding their preoperative instructions.
Web-based programs also can provide patients online instructions about their medications. Some services even customize information by providing, for example, lists of local surgeons who are willing to allow a patient to continue on aspirin therapy until the day of surgery.
USE THE RIGHT RESOURCES
Staffing
Our model at the University of Chicago relies mainly on residents in training and physician assistants, but advanced nurse practitioners are well suited to a preoperative clinic as well. These types of providers have background training in history-taking, physical examination, diagnostic testing, and disease management. Registered nurses have more limited abilities, although they may be appropriate for a clinic that deals primarily with healthy patients for whom only history taking and a list of medications is needed. Additionally, our clinic is staffed by one attending anesthesiologist at all times (from among a group of rotating anesthesiologists) as well as medical assistants and clerical staff.
Some clinics perform the surgical history and physical exam at the same time as the anesthesia assessment. I would urge caution with this practice. Just as primary care doctors should not be conducting the anesthesia assessment, nonsurgeons should not be conducting the surgical assessment; doing so puts them out on a limb from a medicolegal standpoint. Advanced nurse practitioners and physician assistants may do surgical assessments under the supervision of a surgeon, but only surgeons should ultimately decide—and document—whether an operation is necessary and what degree of examination is required in advance.
Computer technology for records, messaging, billing
Using electronic medical records and corresponding with colleagues by e-mail make preoperative care much more efficient. We have standardized computer forms for ordering tests and documenting the physical exam. Patients usually understand that electronic medical records are safe and more efficient, and they are often more accepting of their use than practitioners are. Many patients want e-mail access to doctors, to schedule appointments online, and to receive appointment reminders by e-mail.3
Electronic medical records also avoid redundancy. If a patient has been seen in our preoperative clinic and is later scheduled for another surgery (even if a different surgeon is involved), a return visit to our clinic may not be necessary. In some cases, we can send the old work-up stamped “For information only,” which can then be updated by the anesthesiologist on the day of surgery.
A central, standardized process also makes billing more efficient and helps to ensure that payment is received for all services provided. Standardized documentation makes it easier for coders to enter the correct evaluation and management codes and ensures that all required criteria are met.
THE PAYOFF: LIVES AND DOLLARS SAVED
A thorough and efficient preoperative assessment system is cost-effective. Every minute of operating room time is worth $10 to $15,4,5 so delays should be avoided. Everything that is done ahead of time saves money for the whole enterprise by reducing unnecessary case setups and reducing “down time” due to lack of patient, equipment, or staff readiness. We routinely bill for preoperative evaluations when this service goes beyond a routine preoperative assessment based on CMS (and other insurance) requirements. However, a preoperative evaluation is required by CMS and most payers if one wants to be paid for any anesthesia-provided service. As a result, a cost is incurred without offsetting revenue if a case is cancelled on the day of surgery after one performs the anesthesia evaluation.
Yesterday I heard someone ask, “Do we really need all this preoperative evaluation? Does it really improve outcomes?” There is some evidence that it does. A study from 2000 based on data from the Australian Incident Monitoring Study found that 11% of the 6,271 critical incidents that occurred following operations were attributable to inadequate preoperative evaluation and that 3% were unequivocally related to problems with preoperative assessment or preparation. More than half of the incidents were deemed preventable.6
Preoperative clinics are good for patients and make good sense economically. We just need to demonstrate to our administrators and to payers that we are offering an excellent service.
Cleveland Clinic IMPACT Center
By Ajay Kumar, MD
Cleveland Clinic is structured differently from most other institutions in that its surgeons, anesthesiologists, and hospitalists are all direct employees of the institution. Despite this unique structure, many aspects of our preoperative clinic—known as the Internal Medicine Preoperative Assessment, Consultation and Treatment (IMPACT) Center—are applicable to other institutions.
Cleveland Clinic is a busy surgical hospital whose preoperative optimization system is designed to provide high-quality care. The IMPACT Center is consulted for most complicated noncardiac surgery patients, and its referral sources include most of the institution’s surgical specialties.
QUEST FOR A BETTER PATIENT EXPERIENCE
When the IMPACT Center was created in 1997, the aim was to focus on the same objectives highlighted by Drs. Bader and Sweitzer: safety, a positive patient experience, enhanced communication, better continuity of care, effective use of resources, and improving throughput by standardizing care.
A prime motivator was the desire to move away from the tendency for presurgical consults to simply “clear the patient for surgery,” and we have indeed evolved considerably from that point. The focus of our perioperative care program today is to comprehensively evaluate risk by taking into account patient-, procedure-, and anesthesia-related factors.
We offer “one-stop shopping,” and our priority is for efficient throughput. We are located in a 12-story building that includes outpatient, preoperative, and surgical clinics and offices. The IMPACT Center is on the first floor along with the preoperative anesthesia consultation and evaluation (PACE) clinic, the laboratory, and ECG and stress-test labs. Patients can undergo radiographic studies on the second floor.
The patient experience counts for a lot. Many of our patients are from another state or country, so efficiency and convenience are especially important. Patients can usually get all assessment and testing done in a single day.
A TIGHTLY MANAGED PROCESS
A ‘smart’ questionnaire starts the process
A computerized report based on the questionnaire guides the surgical office in scheduling the patient to specific areas according to algorithms. Based on case complexity and clinical needs, patients are scheduled for the IMPACT Center along with the PACE clinic; if needed (based on the algorithms), patients also are scheduled for laboratory tests or imaging. This standardized approach helps create a safe passage for patients through the preoperative process with less confusion.
Patient is given a personalized binder
Once all appointments and tests are scheduled, the patient is given a binder containing specific information about the procedure and preoperative instructions. The medical appointment at the IMPACT Center is usually scheduled before the PACE clinic appointment. Patients receive an itinerary for all preoperative appointments and surgical office appointments before the planned surgery. The itinerary is planned so that if additional testing is requested, it can be accommodated on the same day.
At the end of the preoperative assessment, the patient receives printed information with specific preoperative instructions, including which medications to continue or stop.
Standardized, computer-based medical records
Our systems and processes have undergone a good deal of evolution. We have integrated our medical records and use a standard outside medical record retrieval process. The template for the history and physical exam is standard for all Cleveland Clinic patients and is used for all presurgical assessments before all noncardiac surgeries. The template is comprehensive, including the history of the present illness, the review of systems, the physical exam, and anesthesia-related issues. All outside documents are scanned into our electronic medical record system and are available for viewing prior to surgery from any computer connected to the system.
Our preoperative assessment guidelines are also kept updated at a central online location so that all providers have access to them.
Staff keeps process running efficiently
The IMPACT Center is managed by the department of hospital medicine and supported by at least 5.5 full-time physicians every day. We also have two registered nurses, two assistants who help with scheduling and testing, and three secretaries who support the doctors, obtain records, and make arrangements with outside doctors for testing if a patient wants to return home before our testing can be completed.
A secretary also keeps a log for each patient seen in the clinic, tracking all pending issues. The day before surgery, the secretary contacts the appropriate office for anything that is still pending. If she gets no response, the matter is transferred to one of our doctors so that the problem can be resolved at once. This strategy allows us to achieve a nearly 0% rate of surgery delay or cancellation attributable to unavailable test results.
Our patient volumes have increased significantly since we started in 1997. Last year more than 15,000 patients visited the IMPACT Center and now we have expanded our services to regional hospitals within the Cleveland Clinic Health System.
INTERDEPARTMENTAL COMMUNICATION IS CRITICAL
Interdepartmental communication is a must for patient safety, so we encourage a culture of communication between the hospitalist and the surgical team. The location of most of our surgical clinics within the same building as the IMPACT Center further facilitates communication, as does the proximity of the PACE clinic. Additionally, one of our IMPACT Center physicians is accessible around the clock to answer to our surgeon or anesthesiologist colleagues as needed.
We regularly assess our process and seek feedback from surgeons and anesthesiologists. We also conduct yearly patient experience surveys to make sure we are providing patients with the highest quality of care.
Discussion
Question from the audience: Our anesthesia assessment department was approached by our surgeons to do both the anesthesia and surgical assessments, but we felt that would put us in a potential legal conflict if a patient who was assessed that way developed problems. Can you comment?
Dr. Bader: Although we do surgical assessments at our preoperative clinic, we don’t make any decisions about whether or not to proceed with an operation. We get an office note from the surgeon that is directed specifically toward the need for surgery, indications for surgery, and surgical consent. We perform the surgical history and physical examination. Our process is essentially the same as when surgeons have a physician assistant do the history and physical examination in their office. Our practitioners are employed by the hospital, so there is no conflict of interest there.
Comment from the audience: I’m a strong believer in hands-on patient contact. Over my 15 years of practice, we have encountered a lot of unexpected problems during the preoperative exam—aortic stenoses, infections, ventricular septal defects—all of which would never have been detected from a screening form.
Dr. Sweitzer: I agree that we pick up many things by seeing the patient in person. I’ve picked up more cases of aortic stenosis as an anesthesiologist in the preoperative clinic than I ever did as an internist, because the population is high-risk. But patients who have such problems tend to have risk factors and be in certain age groups. Studies indicate that the history is more important than the physical exam: the history suggests about 75% of conditions that are present. The physical exam adds only a little more—perhaps another 15%. Our recommendations are very much consistent with the American College of Cardiology and American Heart Association guidelines on preoperative cardiac evaluation.7 It is more important to identify whether a patient has risk factors for coronary artery disease than to find out whether a stress test or ECG is normal. One needs to do a really good history, but it can be done remotely. Based on certain risk factors identified, high-risk patients can be selected who need to come in and have a physical exam.
Question from the audience: Could you elaborate on the electronic medical record system used at the University of Chicago? I’ve heard there’s a steep learning curve when implementing these kinds of systems. They also are very expensive—I’ve heard that some cost $40 to $80 million. Has enhanced revenue flow offset the costs?
Dr. Sweitzer: We have a home-grown system developed with FileMaker Pro by a computer programmer at our institution. It was a lot easier to develop than people tend to think. There are many savvy computer programmers out there; I’ve had medical students assist me with updating it. We’re now considering developing it as a commercial system. Many systems are available for purchase, including Epic, Pyxis, one from General Electric, and many others. They are very expensive, so smaller institutions might want to use a pay-for-service system.
There definitely is a learning curve to switching to electronic medical records, but it is not nearly as steep as many believe. The extra time it takes a clinician to initially make a computer entry rather than write on paper is vastly recouped downstream: the electronic medical record is legible and organized, and it doesn’t get lost or need to be redone. You can bring up a patient record from 6 months before and reuse it as a template.
Dr. Bader: The discussion of cost savings from preoperative clinics usually focuses on savings from avoiding surgery cancellations and delays and from more efficient laboratory testing, but the biggest savings for an institution is better reimbursement through better diagnosis-related groups (DRG) coding. That’s an important reason our institution is funding our clinic. Electronic medical records allow standardization of information so that coders know exactly where to look for the comorbidities and other pertinent information. This increases payments for DRGs, which can be documented for the hospital. This literally runs into millions of dollars a year and more than offsets the costs of the system.
Question from the audience: Dr. Bader, I’m impressed with the number of patients going through your preoperative clinic. How many patients are seen per nurse practitioner in your clinic?
Dr. Bader: The nurse practitioners have 10-hour shifts and see one patient every 75 minutes. The process of seeing a patient takes a lot less time now than with the old system, in which patients saw an anesthesiologist plus a nurse. Our current system eliminates redundancy: questions need to be asked only once.
Question from the audience: My compliance office says that preoperative assessments for early-morning admission patients are good for only 7 days. Is that true?
Dr. Bader: There are sometimes differences between Joint Commission requirements and those of certain insurance companies. That kind of issue needs to be discussed with your hospital compliance office. We program rules into our scheduling system to accommodate different insurance policies and other requirements so that a patient is not scheduled beyond the allowable period.
- Detsky AS, Naglie IG. A clinician’s guide to cost-effectiveness analysis. Ann Intern Med 1990; 113:147–154.
- Sandler G. The importance of the history in the medical clinic and the cost of unnecessary tests. Am Heart J 1980; 100:928–931.
- Blumenthal D, Glaser JP. Information technology comes to medicine. N Engl J Med 2007; 356:2527–2534.
- Strum DP, Vargas LG, May JH. Surgical subspecialty block utilization and capacity planning: a minimal cost analysis model. Anesthesiology 1999; 90:1176–1185.
- Ferschl MB, Tung A, Sweitzer B, Huo D, Glick DB. Preoperative clinic visits reduce operating room cancellations and delays. Anesthesiology 2005; 103:855–859.
- Kluger MT, Tham EJ, Coleman NA, et al. Inadequate preoperative evaluation and preparation: a review of 197 reports from the Australian incident monitoring study. Anaesthesia 2000; 55:1173–1178.
- Fleisher LA, Beckman JA, Brown KA, et al. ACC/AHA 2007 guidelines on perioperative cardiovascular evaluation and care for noncardiac surgery: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. J Am Coll Cardiol 2007; 50:1707–1732.
- Detsky AS, Naglie IG. A clinician’s guide to cost-effectiveness analysis. Ann Intern Med 1990; 113:147–154.
- Sandler G. The importance of the history in the medical clinic and the cost of unnecessary tests. Am Heart J 1980; 100:928–931.
- Blumenthal D, Glaser JP. Information technology comes to medicine. N Engl J Med 2007; 356:2527–2534.
- Strum DP, Vargas LG, May JH. Surgical subspecialty block utilization and capacity planning: a minimal cost analysis model. Anesthesiology 1999; 90:1176–1185.
- Ferschl MB, Tung A, Sweitzer B, Huo D, Glick DB. Preoperative clinic visits reduce operating room cancellations and delays. Anesthesiology 2005; 103:855–859.
- Kluger MT, Tham EJ, Coleman NA, et al. Inadequate preoperative evaluation and preparation: a review of 197 reports from the Australian incident monitoring study. Anaesthesia 2000; 55:1173–1178.
- Fleisher LA, Beckman JA, Brown KA, et al. ACC/AHA 2007 guidelines on perioperative cardiovascular evaluation and care for noncardiac surgery: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. J Am Coll Cardiol 2007; 50:1707–1732.
KEY POINTS
- Standardizing the preoperative assessment process helps ensure that regulatory, accreditation, and payer requirements and guidelines are met.
- Careful triage based on a patient’s history can help avoid unnecessary assessment of low-risk patients and ensure that necessary assessments for higher-risk patients are completed before the day of surgery.
- Perioperative assessment and management guidelines for various types of surgery and patient risk factors should be developed, continuously updated, and made available online to all providers within the institution.
- Electronic medical records allow standardization of patient information, avoid redundancy, and provide a database for research.