User login
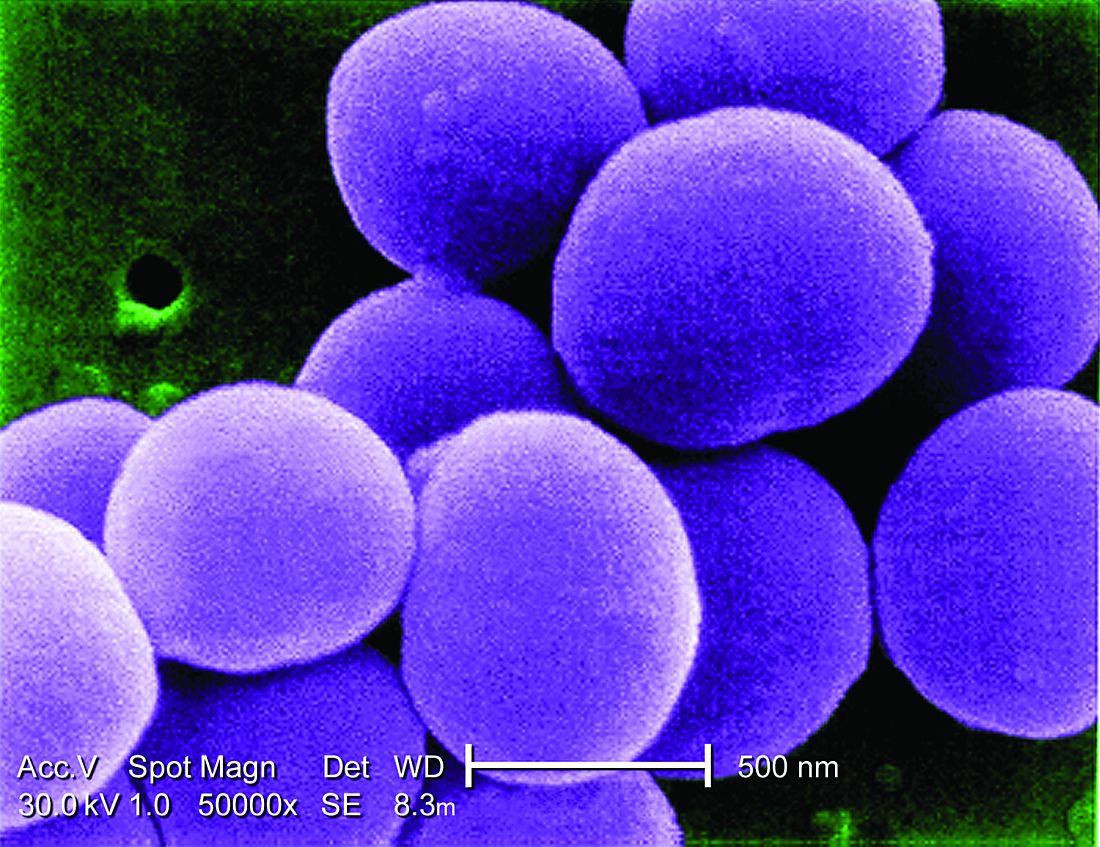
Early transition to oral beta-lactams for low-risk S. aureus bacteremia may be acceptable
Background: There is consensus that LR-SAB can be safely treated with 14 days of antibiotic therapy, but the use of and/or proportion of duration of oral antibiotics is not clear. There is evidence that oral therapy has fewer treatment complications, compared with IV treatments. Objective of this study was to assess the safety of early oral switch (EOS) prior to 14 days for LR-SAB.
Study design: Retrospective cohort study.
Setting: Single institution tertiary care hospital in Wellington, New Zealand.
Synopsis: Study population included adults with health care–associated SAB deemed low risk (no positive blood cultures >72 hours after initial positive culture, no evidence of deep infection as determined by an infectious disease consultant, no nonremovable prosthetics). The primary outcome was occurrence of SAB-related complication (recurrence of SAB, deep-seated infection, readmission, attributable mortality) within 90 days.
Of the initial 469 episodes of SAB, 100 met inclusion, and 84 of those patients had EOS. Line infection was the source in a majority of patients (79% and 88% in EOS and IV, respectively). Only 5% of patients had MRSA. Overall, 86% of EOS patients were treated with an oral beta-lactam, within the EOS group, median duration of IV and oral antibiotics was 5 and 10 days, respectively. SAB recurrence within 90 days occurred in three (4%) and one (6%) patients in EOS vs. IV groups, respectively (P = .64). No deaths within 90 days were deemed attributable to SAB. Limitations include small size, single center, and observational, retrospective framework.
Bottom line: The study suggests that EOS with oral beta-lactams in selected patients with LR-SAB may be adequate; however, the study is too small to provide robust high-level evidence. Instead, the authors hope the data will lead to larger, more powerful prospective studies to examine if a simpler, cheaper, and in some ways safer treatment course is possible.
Citation: Bupha-Intr O et al. Efficacy of early oral switch with beta-lactams for low-risk Staphylococcus aureus bacteremia. Antimicrob Agents Chemother. 2020 Feb 3;AAC.02345-19. doi: 10.1128/AAC.02345-19.
Dr. Sneed is assistant professor of medicine, section of hospital medicine, at the University of Virginia School of Medicine, Charlottesville.
Background: There is consensus that LR-SAB can be safely treated with 14 days of antibiotic therapy, but the use of and/or proportion of duration of oral antibiotics is not clear. There is evidence that oral therapy has fewer treatment complications, compared with IV treatments. Objective of this study was to assess the safety of early oral switch (EOS) prior to 14 days for LR-SAB.
Study design: Retrospective cohort study.
Setting: Single institution tertiary care hospital in Wellington, New Zealand.
Synopsis: Study population included adults with health care–associated SAB deemed low risk (no positive blood cultures >72 hours after initial positive culture, no evidence of deep infection as determined by an infectious disease consultant, no nonremovable prosthetics). The primary outcome was occurrence of SAB-related complication (recurrence of SAB, deep-seated infection, readmission, attributable mortality) within 90 days.
Of the initial 469 episodes of SAB, 100 met inclusion, and 84 of those patients had EOS. Line infection was the source in a majority of patients (79% and 88% in EOS and IV, respectively). Only 5% of patients had MRSA. Overall, 86% of EOS patients were treated with an oral beta-lactam, within the EOS group, median duration of IV and oral antibiotics was 5 and 10 days, respectively. SAB recurrence within 90 days occurred in three (4%) and one (6%) patients in EOS vs. IV groups, respectively (P = .64). No deaths within 90 days were deemed attributable to SAB. Limitations include small size, single center, and observational, retrospective framework.
Bottom line: The study suggests that EOS with oral beta-lactams in selected patients with LR-SAB may be adequate; however, the study is too small to provide robust high-level evidence. Instead, the authors hope the data will lead to larger, more powerful prospective studies to examine if a simpler, cheaper, and in some ways safer treatment course is possible.
Citation: Bupha-Intr O et al. Efficacy of early oral switch with beta-lactams for low-risk Staphylococcus aureus bacteremia. Antimicrob Agents Chemother. 2020 Feb 3;AAC.02345-19. doi: 10.1128/AAC.02345-19.
Dr. Sneed is assistant professor of medicine, section of hospital medicine, at the University of Virginia School of Medicine, Charlottesville.
Background: There is consensus that LR-SAB can be safely treated with 14 days of antibiotic therapy, but the use of and/or proportion of duration of oral antibiotics is not clear. There is evidence that oral therapy has fewer treatment complications, compared with IV treatments. Objective of this study was to assess the safety of early oral switch (EOS) prior to 14 days for LR-SAB.
Study design: Retrospective cohort study.
Setting: Single institution tertiary care hospital in Wellington, New Zealand.
Synopsis: Study population included adults with health care–associated SAB deemed low risk (no positive blood cultures >72 hours after initial positive culture, no evidence of deep infection as determined by an infectious disease consultant, no nonremovable prosthetics). The primary outcome was occurrence of SAB-related complication (recurrence of SAB, deep-seated infection, readmission, attributable mortality) within 90 days.
Of the initial 469 episodes of SAB, 100 met inclusion, and 84 of those patients had EOS. Line infection was the source in a majority of patients (79% and 88% in EOS and IV, respectively). Only 5% of patients had MRSA. Overall, 86% of EOS patients were treated with an oral beta-lactam, within the EOS group, median duration of IV and oral antibiotics was 5 and 10 days, respectively. SAB recurrence within 90 days occurred in three (4%) and one (6%) patients in EOS vs. IV groups, respectively (P = .64). No deaths within 90 days were deemed attributable to SAB. Limitations include small size, single center, and observational, retrospective framework.
Bottom line: The study suggests that EOS with oral beta-lactams in selected patients with LR-SAB may be adequate; however, the study is too small to provide robust high-level evidence. Instead, the authors hope the data will lead to larger, more powerful prospective studies to examine if a simpler, cheaper, and in some ways safer treatment course is possible.
Citation: Bupha-Intr O et al. Efficacy of early oral switch with beta-lactams for low-risk Staphylococcus aureus bacteremia. Antimicrob Agents Chemother. 2020 Feb 3;AAC.02345-19. doi: 10.1128/AAC.02345-19.
Dr. Sneed is assistant professor of medicine, section of hospital medicine, at the University of Virginia School of Medicine, Charlottesville.
Unclear benefit to home NIPPV in COPD
Background: Chronic obstructive pulmonary disease (COPD) is a prevalent condition that is associated with significant mortality, morbidity, and health care utilization. Use of noninvasive positive-pressure ventilation (NIPPV) in acute hypercapnic respiratory failure caused by COPD exacerbations is well established. However, the benefits of in-home NIPPV for COPD with chronic hypercapnia is unclear.
Study design: Systematic review and meta-analysis.
Setting: Multicenter catchment of 21 randomized control trials (RCTs) and 12 observational studies involving more than 51,000 patients during 1995-2019.
Synopsis: Patients included were those with COPD and hypercapnia who used NIPPV for more than 1 month. Home bilevel positive airway pressure (BiPAP), compared to no device use was associated with lower risk of mortality, all-cause hospital admission, and intubation, but no significant difference in quality of life. Noninvasive home mechanical ventilation, compared with no device was significantly associated with lower risk of hospital admission, but not a significant difference in mortality. Of note, there was no statistically significant difference in any outcome for either BiPAP or home mechanical ventilation if evidence was limited to RCTs. Importantly, on rigorous measure, the evidence was low to moderate quality or insufficient, and some outcomes analysis was based on small numbers of studies.
Bottom line: While there is suggestion of benefit on some measures with the use of home NIPPV, the evidence is not robust enough to clearly guide use.
Citation: Wilson et al. Association of home noninvasive positive pressure ventilation with clinical outcomes in chronic obstructive pulmonary disease. JAMA. 2020 Feb 4;323(5):455-65.
Dr. Sneed is assistant professor of medicine, section of hospital medicine, at the University of Virginia School of Medicine, Charlottesville.
Background: Chronic obstructive pulmonary disease (COPD) is a prevalent condition that is associated with significant mortality, morbidity, and health care utilization. Use of noninvasive positive-pressure ventilation (NIPPV) in acute hypercapnic respiratory failure caused by COPD exacerbations is well established. However, the benefits of in-home NIPPV for COPD with chronic hypercapnia is unclear.
Study design: Systematic review and meta-analysis.
Setting: Multicenter catchment of 21 randomized control trials (RCTs) and 12 observational studies involving more than 51,000 patients during 1995-2019.
Synopsis: Patients included were those with COPD and hypercapnia who used NIPPV for more than 1 month. Home bilevel positive airway pressure (BiPAP), compared to no device use was associated with lower risk of mortality, all-cause hospital admission, and intubation, but no significant difference in quality of life. Noninvasive home mechanical ventilation, compared with no device was significantly associated with lower risk of hospital admission, but not a significant difference in mortality. Of note, there was no statistically significant difference in any outcome for either BiPAP or home mechanical ventilation if evidence was limited to RCTs. Importantly, on rigorous measure, the evidence was low to moderate quality or insufficient, and some outcomes analysis was based on small numbers of studies.
Bottom line: While there is suggestion of benefit on some measures with the use of home NIPPV, the evidence is not robust enough to clearly guide use.
Citation: Wilson et al. Association of home noninvasive positive pressure ventilation with clinical outcomes in chronic obstructive pulmonary disease. JAMA. 2020 Feb 4;323(5):455-65.
Dr. Sneed is assistant professor of medicine, section of hospital medicine, at the University of Virginia School of Medicine, Charlottesville.
Background: Chronic obstructive pulmonary disease (COPD) is a prevalent condition that is associated with significant mortality, morbidity, and health care utilization. Use of noninvasive positive-pressure ventilation (NIPPV) in acute hypercapnic respiratory failure caused by COPD exacerbations is well established. However, the benefits of in-home NIPPV for COPD with chronic hypercapnia is unclear.
Study design: Systematic review and meta-analysis.
Setting: Multicenter catchment of 21 randomized control trials (RCTs) and 12 observational studies involving more than 51,000 patients during 1995-2019.
Synopsis: Patients included were those with COPD and hypercapnia who used NIPPV for more than 1 month. Home bilevel positive airway pressure (BiPAP), compared to no device use was associated with lower risk of mortality, all-cause hospital admission, and intubation, but no significant difference in quality of life. Noninvasive home mechanical ventilation, compared with no device was significantly associated with lower risk of hospital admission, but not a significant difference in mortality. Of note, there was no statistically significant difference in any outcome for either BiPAP or home mechanical ventilation if evidence was limited to RCTs. Importantly, on rigorous measure, the evidence was low to moderate quality or insufficient, and some outcomes analysis was based on small numbers of studies.
Bottom line: While there is suggestion of benefit on some measures with the use of home NIPPV, the evidence is not robust enough to clearly guide use.
Citation: Wilson et al. Association of home noninvasive positive pressure ventilation with clinical outcomes in chronic obstructive pulmonary disease. JAMA. 2020 Feb 4;323(5):455-65.
Dr. Sneed is assistant professor of medicine, section of hospital medicine, at the University of Virginia School of Medicine, Charlottesville.