User login
Resting injured limbs delays recovery: A systematic review
- Injured limbs are traditionally rested by splint or cast. This is undertaken both for palliation and also in the belief that resting improves recovery time, and reduces complications such as deformity, functional problems and long-term pain.
- Early mobilization decreases pain, swelling and stiffness, particularly in the short term, without longer-term cosmetic or radiologic deformity. (SOR: A)
- Patients usually (but not always) prefer early mobilization, and return to work earlier. (SOR: C)
- Rest may be overused for limbs injury, although the extent to which early mobilization should be adopted needs more research. (SOR: C)
- The scope of limb injuries explored with trials of mobilization also needs further research.
Objectives: Rest is commonly used as primary treatment, rather than just palliation, for injured limbs. We searched the literature for evidence of benefit or harm from immobilization or mobilization of acute limb injury in adults.
Data Sources: We systematically searched for and retrieved randomized controlled trials (RCTs) of mobilization or rest for treatment of acute limb injuries, in Medline (1966–2002), EMBASE, Web of Science, and the Cochrane library, in all languages.
Review Methods: We examined patient-centered outcomes (pain, swelling, and cost), functional outcomes (range of motion, days lost from work) and complications of treatment.
Results: Forty-nine trials of immobilization for soft tissue injuries and fractures of both upper and lower limbs were identified (3366 patients). All studies reported either no difference between rest and early mobilization protocols, or found in favor of early mobilization. Reported benefits of mobilization included earlier return to work; decreased pain, swelling, and stiffness; and a greater preserved range of joint motion. Early mobilization caused no increased complications, deformity or residual symptoms.
Conclusions: We should not assume any benefit for immobilization after acute upper or lower limb injuries in adults. Rest appears to be overused as a treatment. More trials are needed to identify optimal programs for early mobilization.
We know that bed rest generally is over-prescribed.1 But what about resting or immobilizing acutely injured limbs—from simple sprains to gunshot wounds? This specific application of rest is controversial.2-6
Theoretically, rest should reduce further tissue damage by limiting movement, decreasing pain and swelling, and lessening loss of fracture reduction.7-15 However, mobilization increases blood flow and so reduces muscle atrophy, disuse osteoporosis, adhesions, and joint stiffness.7-15
The first empirical trials to determine whether rest or mobilization would offer greater benefit were undertaken in the 1980s, using both human and animal models. Systematic reviews have looked at specific injuries: acute ankle sprains16; ankle ligament rupture17; isolated ulnar fracture18; metacarpal fractures19; collateral ankle ligament sprains20; and soft-tissue ankle injury.21 Each review independently suggests benefits for early mobilization.
However, most clinicians employ some period of enforced rest of injured limbs. For example, a survey of orthopedic surgeons in Denmark found early mobilization for ankle fractures is prescribed for only 6% of patients.22
We systematically reviewed the literature to find trials that compared rest with early mobilization in acute limb injuries.
Methods
Protocol and search strategy
We searched the literature to identify prospective randomized controlled trials (RCTs) comparing rest with mobilization for acute limb injuries, searching the Cochrane Controlled Trials Register and Systematic Reviews, Medline (1966–2002), EMBASE (Rehabilitation and Physical Therapy), and Web of Science, combined with the following terms:
- immobilis*, immobiliz*, mobilis*, mobiliz*,
injur*, fracture*, limb*, cast*, brace*, splint*,
leg*, arm*, wrist*, elbow*, joint*, *carpal*,
*tarsal*, knee*, ankle*, femur*, tibia*, fibula*,
colles*, ulna*, radi*, humer*, sprain*, soft tissue,
plaster slab, dislocat*
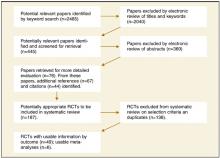
We accepted all publication languages and translated several papers. We found 445 potentially relevant papers by examining their titles or abstracts (Figure). Studies that did not fulfill our inclusion criteria were discarded.
We obtained full texts for 76 studies and undertook a prospective cited reference search in Web of Science for each study to identify more recent articles. A total of 187 papers were then evaluated further for duplicate data and inclusion criteria.
Trials that met our inclusion criteria:
- Were randomized and controlled
- Studied acute limb injuries
- Compared groups whose only treatment difference was mobilization (studies that compared surgery and immobilization against nonsurgical early mobilization were not included; studies with internal fixation were included only if internal fixation was applied to both groups)
- Had loss to follow-up of 20%, except where analysis was clearly intention to treat
- Studied populations not focussed solely on young children, (studies in which the given age range included a small number of patients as young as 11 or 12 years were accepted—in these studies the median age was much higher)
- adequately reported data collection and statistical analysis.
By these criteria, we excluded 138 studies (a list of which is available from the authors). Finally, 49 studies were included.
FIGURE
Literature search process, and methods by which randomized controlled trials (RCTs) were selected
Study methods quality and validity
Two authors independently scored the validity of each of the included 49 studies, meeting to discuss and resolve any disagreements. We relied on published data, without writing to authors to clarify or obtain information. Included studies were evaluated against 11 standard criteria.23 Each criterion was scored 0–2. However, the practical maximum possible score was 18 because it was impossible to blind patients or their caregivers to mobilization. We considered the quality of 16 studies scoring 11 to be high.
Results
Across the 49 eligible studies, the different interventions were well described and differentiated, and data collection methods were clearly explained. Duration of immobilization in a cast was described (if at all) from 10 days to 8 weeks. Mobilization strategies varied and included active exercise, orthoses, crutches, or bandages.
Study quality was poor in many respects: several did not include important demographic data (including age, sex, or the numbers randomized to control and experimental group). Most did not report data about the methods of randomization. Many studies used inadequate randomization methods, with only 5 reporting optimal methods. Loss to follow-up was addressed poorly (not described or intention-to-treat analysis was not used). Outcome assessment was not blinded (a serious shortcoming in view of the subjective assessment of some patient outcomes). Reporting of inclusion criteria was inadequate in a few studies.
Given these deficiencies, our discussion emphasizes conclusions supported by studies of high quality.
Reporting of the studies
We divided the 49 studies into 4 groups: lower-limb fractures, other lower-limb injuries, upper-limb fractures, and other upper-limb injuries (Table W, at www.jfponline.com). Each group was further divided into trials using some form of limb support (such as a brace, splint, or a short period of immobilization) or minimal or no support (bandage, crutches, or tape) in the early mobilization group.
Most studies used some form of dynamic treatment for the injured limb, with highest use in lowerlimb injuries (74%); 2 studies included both supported and unsupported mobilization.24-26 In studies of upper-limb fractures, support was used in 50%. In high-quality studies, 12 out of 16 studies used some support, but results were consistent with studies that did not. The smaller number of studies using minimal support makes comparison with supported mobilization difficult, but results suggest that supported mobilization may result in an earlier return to work or sport, whereas minimally supported patients achieved better composite scores and muscle strength. There was too much clinical heterogeneity to sensibly combine the results; however, we were interested to see whether mobilization was useful across a heterogeneous group of conditions.
Patient-centered outcomes
No study reported any significant improvement with rest on swelling and pain. To the contrary, 13 studies reported significant improvement with early mobilization compared with rest,16,17,27-37 and 9 studies reported enhanced patient satisfaction.16,30,36,38-43 High-quality studies that reported pain levels found no difference or favored early mobilization.25,26,30,31,39,44-51 This was significant in only 2 studies of lower-limb nonfractures.25,26,30 No study reported adverse patient opinion in an early mobilization regime,28,31,38,40,44-46,48,51-56 and patients appreciated their ability to use the affected limb.34,43,49
Functional outcomes
Ten studies measured global function, using composite scores including subjective and objective criteria—pain, stiffness, swelling, use of supports, and ability to climb stairs, play sport, work, and undertake activities of daily life (Table W). Seven studies reported significant improvements with early mobilization—after 6 months (6 studies),28,35,42,46,52,57 or 12 months (1 study).32 Four studies of high quality found significant benefit for early mobilization in composite scores, most of these for lower-limb fractures.46,47,52,54 Significantly more patients with acute ankle sprain, who were immobilized in a cast, sought medical and physiotherapy advice in the initial 3 weeks, compared with those mobilized early with a functional brace.50
Return to work and sport
Thirteen studies reported that early mobilization resulted in a significantly earlier return to work (about 30%–60% earlier),16,17,30,33,35,36,38-40,52,57-59 especially in lower-limb nonfracture injuries. In 1 study of ankle fractures, patients randomized to wear a cast reported better performance of daily activities at 6 weeks than those mobilized with crutches.28 Perhaps, this reflects practical difficulties associated with using crutches. Five studies of lower-limb injury reported an earlier return to sport,16,30,39,57,60 as did 3 studies of postoperative Achilles tendon repair30,39,60 and 2 of ankle ligament injury or sprains.16,57 Five studies reporting a significantly earlier return to work or sport were of high quality, as were all studies of lower limb injuries.25,26,30,39,46,52
Range of movement
Fourteen studies of upper- and lower-limb fractures reported significant improvements in range of movement. Significant differences in range of movement were typically observed within 13 weeks of the injury,12,27,29,34,38,42,45,46,49,52,61-64 although a few studies reported differences for longer periods. Similarly for lower-limb nonfractures, significantly better ranges of motion were found within short periods,25,33,37,39,43 and also after 12 months.30,39-41 Eleven studies reporting this outcome were of high quality,25,26,30,31,39,45,46,48-51,54 and 4 studies found significant benefit for early mobilization.25,26,30,46,49 The other 7 high-quality studies favored early mobilization, and 1 found no difference.45
Deformity and other complications
Four studies found early mobilization reduced deformity: for angular displacement61 and radial shortening32 in Colles’ fractures; displacement of metacarpal fractures58 and cosmetic deformity in radial fractures.42 Two studies were of high quality.30,65 Ten trials reported no changes in deformity, no loss of fracture reduction, or any other complications with early mobilization of fractures.28,31,45,48,50,59,62-64,66 In contrast, for Colles’ fractures, significantly greater dorsal angulation61 and significant increases in radial tilt and decreased radioulnar joint space49 were reported for mobilized wrists.
Patient preferences
Patients expressed preference for a brace following anterior cruciate ligament surgery because it helped reduce pain and swelling67; they expressed preference for a cast following surgery for ankle fracture because it improved ability to perform everyday activities.28
Patients with distal radius fractures preferred early treatment with a Tubigrip bandage and a back-slab instead of removable splints, which increased pain and decreased mobilization.53 Generally, patients with fractures preferred rigid support immediately after the injury. Some also expected to have a traditional cast applied after learning their injured wrist was fractured.53
Cost of treatment
Full economic evaluations were not usually satisfactorily undertaken in these clinical studies. The cost of early mobilization was more expensive than immobilization in some studies8,23 but cheaper in others.2,9,10,24,68 It is estimated that direct costs to the patient were lower for early mobilization because of the decreased loss of working time.10,44,68,69
Adherence and supervision
Ten studies excluded patients who were unable to understand the nature of the treatment; had dementia; existing joint disease; drug abuse; alcohol problems; or difficulty with walking aids.28,31,38-41,45,46,49,69 Thus, many researchers have assumed that early mobilization requires greater patient responsibility. Some researchers have recommended applying casts for patients deemed “uncooperative” or “unlikely to be compliant,” despite their positive findings for early mobilization.3,16
Although 10 trials employed physiotherapy or supervised mobilization sessions,25,26,28,29,40,41,46,65,70 11 studies relied on self-controlled mobilization.27,30,31,38,39,42,44,45,48,49,52 In addition, some interventions (eg, braces) intrinsically required more supervision with their removal and reapplication than others (eg, functional casts or semirigid bandages).
Discussion
Early mobilization seems to decrease pain, swelling, and stiffness—at least in the short-term—and patients generally prefer it to immobilization. It results in earlier return—to work and to a greater range of motion, which is most significant within the first 2 months of the injury and can be maintained for up to 12 months for nonfracture injuries. Early mobilization does not increase cosmetic or radiological deformity for stable fractures, and patients experience fewer complications and residual symptoms. However, early mobilization may place greater demands on patients and require higher levels of understanding and responsibility, therefore making it unsuitable for some patients.
This systematic review of all upper- and lower-limb injuries, including fractures, consistently found in favor of early mobilization over rest. We acknowledge that the range of injuries reviewed is very limited. However, the clear benefits of mobilization indicated by this review suggest we need research in a wider range of injuries.
Similarly, it would be naïve to assume mobilization is better than immobilization in all circumstances. Harm must occur at some level of increased activity. In addition we know that pain and discomfort are often experienced by patients who demand immobilization (a “palliative” form of management). Finding the ideal level and type of activity must be undertaken empirically. Therefore more quality clinical trials are required to determine and evaluate the best regimens for early mobilization.
Newer studies will probably find that mobilization can be employed more often (and perhaps more vigorously) than we now advise. The best evidence at hand suggests the medical profession generally errs too conservatively on the side of immobilization.
Acknowledgments
Charlotte Nash did the searches, assembled and analysed the tables and wrote the first draft. Charlotte Nash and Sharon Mickan assessed the quality of all included studies and edited drafts. Paul Glasziou and Chris Del Mar initiated the question and edited drafts. This work was supported in part by a scholarship awarded by the Centre for General Practice, The University of Queensland, and funded by the Australian Commonwealth Department of Health and Ageing through the Primary Health Care Research, Evaluation and Development Strategy.
Corresponding author
Professor Chris B. Del Mar, Centre for General Practice, Faculty Heath Science and Medicine, Bond University, Gold Coast, Queensland 4229, Australia. E-mail: [email protected].
1. Allen C, Glasziou P, Del Mar C. Bed rest: a potentially harmful treatment needing more careful evaluation. Lancet. 1999;354:1229-1233.
2. Madhok R, Bhopal RS. Coping with an upper limb fracture? A study of the elderly. Public Health. 1992;106:19-28.
3. Salter RB. Motion versus rest: Why immobilize joints? J Bone Joint Surg Br. 1982;64B:251-254.
4. Safran MR, Zachazewski JE, Benedetti RS, Bartolozzi AR, Mandelbaum R. Lateral ankle sprains: a comprehensive review. Part 2: treatment and rehabilitation with an emphasis on the athlete. Med Sci Sports Exerc. 1999;31:S438-S447.
5. Willems C. Immediate active mobilization in the treatment of gunshot wounds of joints. Medical Record. 1919;95:953-962.
6. Dent JA. Continuous passive motion in hand rehabilitation. Prosthet Orthot Int 1993;17:130-135.
7. Pneumaticos SG, Noble PC, McGarvey WC, Mody DR, Trevino SG. The effects of early mobilization in the healing of Achilles tendon repair. Foot Ankle Int. 2000;21:551-557.
8. Gelberman RH, Menon J, Gonsalves M, Akeson WH. The effects of mobilisation on the vascularisation of healing flexor tendons in dogs. Clin Orthop. 1980;153:283-289.
9. Kannus P. Immobilisation or early mobilisation after an acute soft tissue injury. The Physician and Sportsmedicine. 2000;28:55-63.
10. Halikis MN, Manske PR, Kubota H, Aoki M. Effect of immobilization, immediate mobilization and delayed mobilization of the resistance to digital flexion using a tendon injury model. J Hand Surg [Am]. 1997;22A:464-472.
11. Romanelli DA, Almekinders LC, Mandelbaum BR. Achilles rupture in the athlete: Current science and treatment. Sports Medicine and Arthroscopy Review. 2000;8:377-386.
12. Stockle U, Konig B, Tempka A, Sudkamp NP. Cast immobilisation or vacuum stabilizing system? Unfallchirurg. 2000;103:215-219.
13. Viidik A. The effect of training on the tensile strength of isolated rabbit tendons. Scandinavian Journal of Plastic and Reconstructive Surgery. 1967;1:141-147.
14. Woo SL, Gelberman RH, Cobb NG, Amiel D, Lothringer K, Akeson WH. The importance of controlled passive mobilization on flexor tendon healing. A biomechanical study. Acta Orthop Scand. 1981;52:615-622.
15. Peacock E. Biological principles in the healing of long tendons. Surg Clin North Am. 1965;45:461-476.
16. Kerkhoffs GMMJ, Rowe BH, Assendelft WJJ, Kelly KD, Struijs PAA, Niek van Dijk C. Immobilisation for acute ankle sprain: a systematic review. Arch Orthop Trauma Surg. 2001;121:462-471.
17. Pijnenburg ACM, van Dijk CN, Bossuyt PMM, Marti RK. Treatment of ruptures of the lateral ankle ligaments: A meta-analysis. J Bone Joint Surg Am. 2000;82A:761-773.
18. Mackay D, Wood L, Rangan A. The treatment of isolated ulnar fractures in adults: a systematic review. Injury. 2000;31:565-570.
19. Prokop A, Kulus S, Helling HJ, Burger C, Rehm KE. Are there concepts in treatment of metacarpal fractures? Own results and a review of the literature of the last 12 years. Unfallchirurg. 1999;102:50-58.
20. Shrier I. Treatment of lateral collateral ligament sprains of the ankle: a critical appraisal of the literature. Clin J Sport Med. 1995;5:187-195.
21. Ogilvie-Harris DJ, Gilbart M. Treatment modalities for soft tissue injuries of the ankle: a critical review. Clin J Sport Med. 1995;5:175-186.
22. Hviid K, Harager K, Schantz K. Aftercare of malleolar fractures in Denmark. A questionnaire study. Ugeskr Læger. 2000;62:2747-2750.
23. Gillespie W, Gillespie L, Morton L. Cochrane Musculoskeletal Injuries Group. Cochrane Database 2002.
24. Sommer HM, Schreiber H. Early functional conservative therapy of fresh fibular capsular ligament rupture from the socioeconomic viewpoint. Sportverletzung Sportschaden. 1993;7:40-46.
25. Dettori JR. Early ankle mobilization, part I: The immediate effect on acute, lateral ankle sprains. A randomised clinical trial. Mil Med. 1994;159:15-20.
26. Dettori JR, Basmania CJ. Early ankle mobilization, part II: A one-year follow-up of acute, lateral ankle sprains. A randomized clinical trial. Mil Med. 1994;159:20-24.
27. Stuart PR, Brumby C, Smith SR. Comparative study of functional bracing and plaster cast treatment of stable lateral malleolar fractures. Injury. 1989;20:323-326.
28. van Laarhoven CJHM, Meeuwis JD, van der Werken C. Postoperative treatment of internally fixed ankle fractures. J Bone Joint Surg Br. 1996;78B:395-399.
29. Søndenaa K, Høigaard U, Smith D, Alho A. Immobilisation of operated ankle fractures. Acta Orthop Scand. 1986;57:59-61.
30. Cetti R, Henriksen LO, Jacobsen KS. A new treatment of ruptured Achilles tendons. Clin Orthop. 1994;308:155-165.
31. Dias JJ, Wray CC, Jones JM, Gregg PJ. The value of early mobilisation in the treatment of Colles’ fractures. J Bone Joint Surg Br. 1987;69B:463-467.
32. Abbaszadegan H, Conradi P, Jonsson U. Fixation not needed for undisplaced Colles’ fracture. Acta Orthop Scand. 1989;60:60-62.
33. Nyska M, Weisel Y, Halperin N, Mann G, Segal D. Controlled mobilization after acute ankle inversion injury. Journal of Sports Traumatology and Related Research. 1999;21:114-120.
34. McMahon PJ, Woods DA, Burge PD. Initial treatment of closed metacarpal fractures. J Hand Surg [Br]. 1994;19B:597-600.
35. Konradsen L, Hølmer P, Søndergaard L. Early mobilizing treatment for grade III ankle ligament injuries. Foot and Ankle. 1991;12:69-73.
36. Cetti R, Christensen SE, Corfitzen MT. Ruptured fibular ankle ligament: Plaster or Pliton brace? Br J Sports Med. 1984;18:104-109.
37. Eiff MP, Smith AT, Smith GE. Early mobilisation versus immobilisation in the treatment of lateral ankle sprains. Am J Sports Med. 1994;22:83-86.
38. Gebuhr P, Hölmich P, Ørsnes T, Soelberg M, Krasheninnikoff M, Kjersgaard AG. Isolated ulnar shaft fractures. J Bone Joint Surg Br. 1992;74B:757-759.
39. Mortensen NHM, Skov O, Jensen PE. Early motion of the ankle after operative treatment of a rupture of the Achilles tendon. J Bone Joint Surg Am. 1999;81A:983-990.
40. Buchgraber A, Pässler HH. Percutaneous repair of Achilles tendon rupture. Clin Orthop. 1997;341:113-122.
41. Saleh M, Marshall PD, Senior R, MacFarlane A. The Sheffield Splint for controlled early mobilisation after rupture of the calcaneal tendon. J Bone Joint Surg Br. 1992;74B:206-209.
42. Davis TRC, Buchanan JM. A controlled prospective study of early mobilization of minimally displaced fractures of the distal radial metaphysis. Injury. 1987;18:283-285.
43. Avci S, Sayli U. Comparison of the results of short-term rigid and semi-rigid cast immobilization for the treatment of grade 3 inversion injuries of the ankle. Injury. 1998;29:581-584.
44. Dogra AS, Rangan A. Early mobilisation versus immobilisation of surgically treated ankle fracture. Prospective randomised control trial. Injury. 1999;30:417-419.
45. Hedström M, Ahl T, Dalén N. Early postoperative ankle exercises: a study of postoperative lateral malleolar fractures. Clin Orthop. 1994;300:193-196.
46. Port AM, McVie JL, Naylor G, Kreibich DN. Comparison of two conservative methods of treating an isolated fracture of the lateral malleous. J Bone Joint Surg Br. 1996;78B:568-572.
47. Klein J, Rixen D, Albring T, Tiling T. Functional treatment with a pneumatic ankle brace versus cast immobilisation for recent rupture of the fibular ligament in the ankle. A randomised clinical trial. Unfallchirurg. 1991;94:99-104.
48. Allain J, le Guilloux P, Mouël SL, Goutallier D. Trans-styloid fixation of fractures of the distal radius: A prospective randomized comparison between 6- and 1-week postoperative immobilization in 60 fractures. Acta Orthop Scand. 1999;70:119-123.
49. Millett PJ, Rushton N. Early mobilization in the treatment of Colles’ fracture: a 3 year prospective study. Injury. 1995;26:671-675.
50. Stewart HD, Innes AR, Burke FD. Functional cast-bracing for Colles’ fractures. A comparison between cast-bracing and conventional plaster casts. J Bone Joint Surg Br. 1984;66B:749-753.
51. Unsworth-White J, Koka R, Churchill M, D’Arcy JC, James SE. The non-operative management of radial head fractures: a randomized trial of three treatments. Injury. 1994;25:165-167.
52. Egol KA, Dolan R, Koval KJ. Functional outcome of surgery for fractures of the ankle. J Bone Joint Surg Br. 2000;82:246-249.
53. Stoffelen D, Broos P. Minimally displaced distal radius fractures: do they need plaster treatment? J Trauma. 1998;44:503-505.
54. DiStasio AJ, Jaggears FR, DePasquale LV, Frassica FJ, Turen CH. Protected early motion versus cast immobilization in postoperative management of ankle fractures. Contemporary Orthopaedics. 1994;29:273-277.
55. Regis D, Montanari M, Magnan B, Spagnol S, Bragantini A. Dynamic orthopaedic brace in the treatment of ankle sprains. Foot Ankle Int. 1995;16:422-426.
56. Grønmark T, Johnsen O, Kogstad O. Rupture of the lateral ligaments of the ankle: a controlled clinical trial. Injury. 1980;11:215-218.
57. Eggert A, Gruber J, Darda L. Treatment of ankle joint injuries. Randomized study of postoperative therapy and early functional treatment. Unfallchirurg. 1986;89:316-320.
58. Konradsen L, Nielsen PT, Albrecht-Beste E. Functional treatment of metacarpal fractures. Acta Orthop Scand. 1990;61:531-534.
59. Broström L. Sprained ankles. V. Treatment and prognosis in recent ligament ruptures. Acta Chir Scand. 1966;132:537-550.
60. Kerkhoffs GMMJ, Struijs PAA, Raaymakers ELFB, Marti RK. Functional treatment after surgical repair of acute Achilles tendon rupture: wrap vs walking cast. Arch Orthop Trauma Surg. 2002;122:102-105.
61. Ferris BD, Thomas NP, Dewar ME, Simpson DA. Brace treatment of Colles’ fracture. Acta Orthop Scand. 1989;60:63-65.
62. Braakman M, Oderwald EE, Haentjens MHHJ. Functional taping of fractures of the 5th metacarpal results in a quicker recovery. Injury. 1998;29:5-9.
63. Tropp H, Norlin R. Ankle performance after ankle fracture: randomised study of early mobilization. Foot Ankle Int. 1995;16:79-83.
64. Kuokkanen HOM, Mulari-Karanen SK, Niskanen RO, Haapala JK, Korkala OL. Treatment of subcapital fractures of the fifth metacarpal bone: a prospective randomised comparison between functional treatment and reposition and splinting. Scand J Plast Recontr Surg Hand Surg. 1999;33:315-317.
65. Murty AN, El Zebdeh MY, Ireland J. Tibial tunnel enlargement following anterior cruciate reconstruction: does post-operative immobilisation make a difference? Knee. 2001;8:39-43.
66. McAuliffe TB, Hilliar KM, Coates CJ, Grange WJ. Early mobilisation of Colles’ fractures: a prospective trial. J Bone Joint Surg Br. 1987;69B:727-729.
67. Brandsson S, Faxén E, Kartus J, Eriksson BI, Karlsson J. Is a knee brace advantageous after anterior cruciate ligament surgery? Scand J Med Sci Sports. 2001;11:110-114.
68. Lind K. Konservativ behandling af laterale ligamentrupturer i fodleddet. Ugeskr Lger. 1984;146:4017-4019.
69. Rafai M, Largab A, Cohen D, Trafeh M. Pure posterior luxation of the elbow in adults: immobilization or early mobilization. A randomized prospective study of 50 cases. Chir Main. 1999;18:272-278.
70. Strickland JW, Glogovac SV. Digital function following flexor tendon repair in Zone II: A comparison of immobilization and controlled passive motion techniques. Journal of Hand Surgery. 1980;5:537-543.
71. Møller-Larsen F, Wethelund JO, Jurik AG, de Carvalho A, Lucht U. Comparison of three different treatments for ruptured lateral ankle ligaments. Acta Orthop Scand. 1988;59:564-566.
72. Caro D, Craft IL, Howells JB, Shaw PC. Diagnosis and treatment of injury of lateral ligament of the ankle joint. Lancet. 1964;2:720-723.
- Injured limbs are traditionally rested by splint or cast. This is undertaken both for palliation and also in the belief that resting improves recovery time, and reduces complications such as deformity, functional problems and long-term pain.
- Early mobilization decreases pain, swelling and stiffness, particularly in the short term, without longer-term cosmetic or radiologic deformity. (SOR: A)
- Patients usually (but not always) prefer early mobilization, and return to work earlier. (SOR: C)
- Rest may be overused for limbs injury, although the extent to which early mobilization should be adopted needs more research. (SOR: C)
- The scope of limb injuries explored with trials of mobilization also needs further research.
Objectives: Rest is commonly used as primary treatment, rather than just palliation, for injured limbs. We searched the literature for evidence of benefit or harm from immobilization or mobilization of acute limb injury in adults.
Data Sources: We systematically searched for and retrieved randomized controlled trials (RCTs) of mobilization or rest for treatment of acute limb injuries, in Medline (1966–2002), EMBASE, Web of Science, and the Cochrane library, in all languages.
Review Methods: We examined patient-centered outcomes (pain, swelling, and cost), functional outcomes (range of motion, days lost from work) and complications of treatment.
Results: Forty-nine trials of immobilization for soft tissue injuries and fractures of both upper and lower limbs were identified (3366 patients). All studies reported either no difference between rest and early mobilization protocols, or found in favor of early mobilization. Reported benefits of mobilization included earlier return to work; decreased pain, swelling, and stiffness; and a greater preserved range of joint motion. Early mobilization caused no increased complications, deformity or residual symptoms.
Conclusions: We should not assume any benefit for immobilization after acute upper or lower limb injuries in adults. Rest appears to be overused as a treatment. More trials are needed to identify optimal programs for early mobilization.
We know that bed rest generally is over-prescribed.1 But what about resting or immobilizing acutely injured limbs—from simple sprains to gunshot wounds? This specific application of rest is controversial.2-6
Theoretically, rest should reduce further tissue damage by limiting movement, decreasing pain and swelling, and lessening loss of fracture reduction.7-15 However, mobilization increases blood flow and so reduces muscle atrophy, disuse osteoporosis, adhesions, and joint stiffness.7-15
The first empirical trials to determine whether rest or mobilization would offer greater benefit were undertaken in the 1980s, using both human and animal models. Systematic reviews have looked at specific injuries: acute ankle sprains16; ankle ligament rupture17; isolated ulnar fracture18; metacarpal fractures19; collateral ankle ligament sprains20; and soft-tissue ankle injury.21 Each review independently suggests benefits for early mobilization.
However, most clinicians employ some period of enforced rest of injured limbs. For example, a survey of orthopedic surgeons in Denmark found early mobilization for ankle fractures is prescribed for only 6% of patients.22
We systematically reviewed the literature to find trials that compared rest with early mobilization in acute limb injuries.
Methods
Protocol and search strategy
We searched the literature to identify prospective randomized controlled trials (RCTs) comparing rest with mobilization for acute limb injuries, searching the Cochrane Controlled Trials Register and Systematic Reviews, Medline (1966–2002), EMBASE (Rehabilitation and Physical Therapy), and Web of Science, combined with the following terms:
- immobilis*, immobiliz*, mobilis*, mobiliz*,
injur*, fracture*, limb*, cast*, brace*, splint*,
leg*, arm*, wrist*, elbow*, joint*, *carpal*,
*tarsal*, knee*, ankle*, femur*, tibia*, fibula*,
colles*, ulna*, radi*, humer*, sprain*, soft tissue,
plaster slab, dislocat*
We accepted all publication languages and translated several papers. We found 445 potentially relevant papers by examining their titles or abstracts (Figure). Studies that did not fulfill our inclusion criteria were discarded.
We obtained full texts for 76 studies and undertook a prospective cited reference search in Web of Science for each study to identify more recent articles. A total of 187 papers were then evaluated further for duplicate data and inclusion criteria.
Trials that met our inclusion criteria:
- Were randomized and controlled
- Studied acute limb injuries
- Compared groups whose only treatment difference was mobilization (studies that compared surgery and immobilization against nonsurgical early mobilization were not included; studies with internal fixation were included only if internal fixation was applied to both groups)
- Had loss to follow-up of 20%, except where analysis was clearly intention to treat
- Studied populations not focussed solely on young children, (studies in which the given age range included a small number of patients as young as 11 or 12 years were accepted—in these studies the median age was much higher)
- adequately reported data collection and statistical analysis.
By these criteria, we excluded 138 studies (a list of which is available from the authors). Finally, 49 studies were included.
FIGURE
Literature search process, and methods by which randomized controlled trials (RCTs) were selected
Study methods quality and validity
Two authors independently scored the validity of each of the included 49 studies, meeting to discuss and resolve any disagreements. We relied on published data, without writing to authors to clarify or obtain information. Included studies were evaluated against 11 standard criteria.23 Each criterion was scored 0–2. However, the practical maximum possible score was 18 because it was impossible to blind patients or their caregivers to mobilization. We considered the quality of 16 studies scoring 11 to be high.
Results
Across the 49 eligible studies, the different interventions were well described and differentiated, and data collection methods were clearly explained. Duration of immobilization in a cast was described (if at all) from 10 days to 8 weeks. Mobilization strategies varied and included active exercise, orthoses, crutches, or bandages.
Study quality was poor in many respects: several did not include important demographic data (including age, sex, or the numbers randomized to control and experimental group). Most did not report data about the methods of randomization. Many studies used inadequate randomization methods, with only 5 reporting optimal methods. Loss to follow-up was addressed poorly (not described or intention-to-treat analysis was not used). Outcome assessment was not blinded (a serious shortcoming in view of the subjective assessment of some patient outcomes). Reporting of inclusion criteria was inadequate in a few studies.
Given these deficiencies, our discussion emphasizes conclusions supported by studies of high quality.
Reporting of the studies
We divided the 49 studies into 4 groups: lower-limb fractures, other lower-limb injuries, upper-limb fractures, and other upper-limb injuries (Table W, at www.jfponline.com). Each group was further divided into trials using some form of limb support (such as a brace, splint, or a short period of immobilization) or minimal or no support (bandage, crutches, or tape) in the early mobilization group.
Most studies used some form of dynamic treatment for the injured limb, with highest use in lowerlimb injuries (74%); 2 studies included both supported and unsupported mobilization.24-26 In studies of upper-limb fractures, support was used in 50%. In high-quality studies, 12 out of 16 studies used some support, but results were consistent with studies that did not. The smaller number of studies using minimal support makes comparison with supported mobilization difficult, but results suggest that supported mobilization may result in an earlier return to work or sport, whereas minimally supported patients achieved better composite scores and muscle strength. There was too much clinical heterogeneity to sensibly combine the results; however, we were interested to see whether mobilization was useful across a heterogeneous group of conditions.
Patient-centered outcomes
No study reported any significant improvement with rest on swelling and pain. To the contrary, 13 studies reported significant improvement with early mobilization compared with rest,16,17,27-37 and 9 studies reported enhanced patient satisfaction.16,30,36,38-43 High-quality studies that reported pain levels found no difference or favored early mobilization.25,26,30,31,39,44-51 This was significant in only 2 studies of lower-limb nonfractures.25,26,30 No study reported adverse patient opinion in an early mobilization regime,28,31,38,40,44-46,48,51-56 and patients appreciated their ability to use the affected limb.34,43,49
Functional outcomes
Ten studies measured global function, using composite scores including subjective and objective criteria—pain, stiffness, swelling, use of supports, and ability to climb stairs, play sport, work, and undertake activities of daily life (Table W). Seven studies reported significant improvements with early mobilization—after 6 months (6 studies),28,35,42,46,52,57 or 12 months (1 study).32 Four studies of high quality found significant benefit for early mobilization in composite scores, most of these for lower-limb fractures.46,47,52,54 Significantly more patients with acute ankle sprain, who were immobilized in a cast, sought medical and physiotherapy advice in the initial 3 weeks, compared with those mobilized early with a functional brace.50
Return to work and sport
Thirteen studies reported that early mobilization resulted in a significantly earlier return to work (about 30%–60% earlier),16,17,30,33,35,36,38-40,52,57-59 especially in lower-limb nonfracture injuries. In 1 study of ankle fractures, patients randomized to wear a cast reported better performance of daily activities at 6 weeks than those mobilized with crutches.28 Perhaps, this reflects practical difficulties associated with using crutches. Five studies of lower-limb injury reported an earlier return to sport,16,30,39,57,60 as did 3 studies of postoperative Achilles tendon repair30,39,60 and 2 of ankle ligament injury or sprains.16,57 Five studies reporting a significantly earlier return to work or sport were of high quality, as were all studies of lower limb injuries.25,26,30,39,46,52
Range of movement
Fourteen studies of upper- and lower-limb fractures reported significant improvements in range of movement. Significant differences in range of movement were typically observed within 13 weeks of the injury,12,27,29,34,38,42,45,46,49,52,61-64 although a few studies reported differences for longer periods. Similarly for lower-limb nonfractures, significantly better ranges of motion were found within short periods,25,33,37,39,43 and also after 12 months.30,39-41 Eleven studies reporting this outcome were of high quality,25,26,30,31,39,45,46,48-51,54 and 4 studies found significant benefit for early mobilization.25,26,30,46,49 The other 7 high-quality studies favored early mobilization, and 1 found no difference.45
Deformity and other complications
Four studies found early mobilization reduced deformity: for angular displacement61 and radial shortening32 in Colles’ fractures; displacement of metacarpal fractures58 and cosmetic deformity in radial fractures.42 Two studies were of high quality.30,65 Ten trials reported no changes in deformity, no loss of fracture reduction, or any other complications with early mobilization of fractures.28,31,45,48,50,59,62-64,66 In contrast, for Colles’ fractures, significantly greater dorsal angulation61 and significant increases in radial tilt and decreased radioulnar joint space49 were reported for mobilized wrists.
Patient preferences
Patients expressed preference for a brace following anterior cruciate ligament surgery because it helped reduce pain and swelling67; they expressed preference for a cast following surgery for ankle fracture because it improved ability to perform everyday activities.28
Patients with distal radius fractures preferred early treatment with a Tubigrip bandage and a back-slab instead of removable splints, which increased pain and decreased mobilization.53 Generally, patients with fractures preferred rigid support immediately after the injury. Some also expected to have a traditional cast applied after learning their injured wrist was fractured.53
Cost of treatment
Full economic evaluations were not usually satisfactorily undertaken in these clinical studies. The cost of early mobilization was more expensive than immobilization in some studies8,23 but cheaper in others.2,9,10,24,68 It is estimated that direct costs to the patient were lower for early mobilization because of the decreased loss of working time.10,44,68,69
Adherence and supervision
Ten studies excluded patients who were unable to understand the nature of the treatment; had dementia; existing joint disease; drug abuse; alcohol problems; or difficulty with walking aids.28,31,38-41,45,46,49,69 Thus, many researchers have assumed that early mobilization requires greater patient responsibility. Some researchers have recommended applying casts for patients deemed “uncooperative” or “unlikely to be compliant,” despite their positive findings for early mobilization.3,16
Although 10 trials employed physiotherapy or supervised mobilization sessions,25,26,28,29,40,41,46,65,70 11 studies relied on self-controlled mobilization.27,30,31,38,39,42,44,45,48,49,52 In addition, some interventions (eg, braces) intrinsically required more supervision with their removal and reapplication than others (eg, functional casts or semirigid bandages).
Discussion
Early mobilization seems to decrease pain, swelling, and stiffness—at least in the short-term—and patients generally prefer it to immobilization. It results in earlier return—to work and to a greater range of motion, which is most significant within the first 2 months of the injury and can be maintained for up to 12 months for nonfracture injuries. Early mobilization does not increase cosmetic or radiological deformity for stable fractures, and patients experience fewer complications and residual symptoms. However, early mobilization may place greater demands on patients and require higher levels of understanding and responsibility, therefore making it unsuitable for some patients.
This systematic review of all upper- and lower-limb injuries, including fractures, consistently found in favor of early mobilization over rest. We acknowledge that the range of injuries reviewed is very limited. However, the clear benefits of mobilization indicated by this review suggest we need research in a wider range of injuries.
Similarly, it would be naïve to assume mobilization is better than immobilization in all circumstances. Harm must occur at some level of increased activity. In addition we know that pain and discomfort are often experienced by patients who demand immobilization (a “palliative” form of management). Finding the ideal level and type of activity must be undertaken empirically. Therefore more quality clinical trials are required to determine and evaluate the best regimens for early mobilization.
Newer studies will probably find that mobilization can be employed more often (and perhaps more vigorously) than we now advise. The best evidence at hand suggests the medical profession generally errs too conservatively on the side of immobilization.
Acknowledgments
Charlotte Nash did the searches, assembled and analysed the tables and wrote the first draft. Charlotte Nash and Sharon Mickan assessed the quality of all included studies and edited drafts. Paul Glasziou and Chris Del Mar initiated the question and edited drafts. This work was supported in part by a scholarship awarded by the Centre for General Practice, The University of Queensland, and funded by the Australian Commonwealth Department of Health and Ageing through the Primary Health Care Research, Evaluation and Development Strategy.
Corresponding author
Professor Chris B. Del Mar, Centre for General Practice, Faculty Heath Science and Medicine, Bond University, Gold Coast, Queensland 4229, Australia. E-mail: [email protected].
- Injured limbs are traditionally rested by splint or cast. This is undertaken both for palliation and also in the belief that resting improves recovery time, and reduces complications such as deformity, functional problems and long-term pain.
- Early mobilization decreases pain, swelling and stiffness, particularly in the short term, without longer-term cosmetic or radiologic deformity. (SOR: A)
- Patients usually (but not always) prefer early mobilization, and return to work earlier. (SOR: C)
- Rest may be overused for limbs injury, although the extent to which early mobilization should be adopted needs more research. (SOR: C)
- The scope of limb injuries explored with trials of mobilization also needs further research.
Objectives: Rest is commonly used as primary treatment, rather than just palliation, for injured limbs. We searched the literature for evidence of benefit or harm from immobilization or mobilization of acute limb injury in adults.
Data Sources: We systematically searched for and retrieved randomized controlled trials (RCTs) of mobilization or rest for treatment of acute limb injuries, in Medline (1966–2002), EMBASE, Web of Science, and the Cochrane library, in all languages.
Review Methods: We examined patient-centered outcomes (pain, swelling, and cost), functional outcomes (range of motion, days lost from work) and complications of treatment.
Results: Forty-nine trials of immobilization for soft tissue injuries and fractures of both upper and lower limbs were identified (3366 patients). All studies reported either no difference between rest and early mobilization protocols, or found in favor of early mobilization. Reported benefits of mobilization included earlier return to work; decreased pain, swelling, and stiffness; and a greater preserved range of joint motion. Early mobilization caused no increased complications, deformity or residual symptoms.
Conclusions: We should not assume any benefit for immobilization after acute upper or lower limb injuries in adults. Rest appears to be overused as a treatment. More trials are needed to identify optimal programs for early mobilization.
We know that bed rest generally is over-prescribed.1 But what about resting or immobilizing acutely injured limbs—from simple sprains to gunshot wounds? This specific application of rest is controversial.2-6
Theoretically, rest should reduce further tissue damage by limiting movement, decreasing pain and swelling, and lessening loss of fracture reduction.7-15 However, mobilization increases blood flow and so reduces muscle atrophy, disuse osteoporosis, adhesions, and joint stiffness.7-15
The first empirical trials to determine whether rest or mobilization would offer greater benefit were undertaken in the 1980s, using both human and animal models. Systematic reviews have looked at specific injuries: acute ankle sprains16; ankle ligament rupture17; isolated ulnar fracture18; metacarpal fractures19; collateral ankle ligament sprains20; and soft-tissue ankle injury.21 Each review independently suggests benefits for early mobilization.
However, most clinicians employ some period of enforced rest of injured limbs. For example, a survey of orthopedic surgeons in Denmark found early mobilization for ankle fractures is prescribed for only 6% of patients.22
We systematically reviewed the literature to find trials that compared rest with early mobilization in acute limb injuries.
Methods
Protocol and search strategy
We searched the literature to identify prospective randomized controlled trials (RCTs) comparing rest with mobilization for acute limb injuries, searching the Cochrane Controlled Trials Register and Systematic Reviews, Medline (1966–2002), EMBASE (Rehabilitation and Physical Therapy), and Web of Science, combined with the following terms:
- immobilis*, immobiliz*, mobilis*, mobiliz*,
injur*, fracture*, limb*, cast*, brace*, splint*,
leg*, arm*, wrist*, elbow*, joint*, *carpal*,
*tarsal*, knee*, ankle*, femur*, tibia*, fibula*,
colles*, ulna*, radi*, humer*, sprain*, soft tissue,
plaster slab, dislocat*
We accepted all publication languages and translated several papers. We found 445 potentially relevant papers by examining their titles or abstracts (Figure). Studies that did not fulfill our inclusion criteria were discarded.
We obtained full texts for 76 studies and undertook a prospective cited reference search in Web of Science for each study to identify more recent articles. A total of 187 papers were then evaluated further for duplicate data and inclusion criteria.
Trials that met our inclusion criteria:
- Were randomized and controlled
- Studied acute limb injuries
- Compared groups whose only treatment difference was mobilization (studies that compared surgery and immobilization against nonsurgical early mobilization were not included; studies with internal fixation were included only if internal fixation was applied to both groups)
- Had loss to follow-up of 20%, except where analysis was clearly intention to treat
- Studied populations not focussed solely on young children, (studies in which the given age range included a small number of patients as young as 11 or 12 years were accepted—in these studies the median age was much higher)
- adequately reported data collection and statistical analysis.
By these criteria, we excluded 138 studies (a list of which is available from the authors). Finally, 49 studies were included.
FIGURE
Literature search process, and methods by which randomized controlled trials (RCTs) were selected
Study methods quality and validity
Two authors independently scored the validity of each of the included 49 studies, meeting to discuss and resolve any disagreements. We relied on published data, without writing to authors to clarify or obtain information. Included studies were evaluated against 11 standard criteria.23 Each criterion was scored 0–2. However, the practical maximum possible score was 18 because it was impossible to blind patients or their caregivers to mobilization. We considered the quality of 16 studies scoring 11 to be high.
Results
Across the 49 eligible studies, the different interventions were well described and differentiated, and data collection methods were clearly explained. Duration of immobilization in a cast was described (if at all) from 10 days to 8 weeks. Mobilization strategies varied and included active exercise, orthoses, crutches, or bandages.
Study quality was poor in many respects: several did not include important demographic data (including age, sex, or the numbers randomized to control and experimental group). Most did not report data about the methods of randomization. Many studies used inadequate randomization methods, with only 5 reporting optimal methods. Loss to follow-up was addressed poorly (not described or intention-to-treat analysis was not used). Outcome assessment was not blinded (a serious shortcoming in view of the subjective assessment of some patient outcomes). Reporting of inclusion criteria was inadequate in a few studies.
Given these deficiencies, our discussion emphasizes conclusions supported by studies of high quality.
Reporting of the studies
We divided the 49 studies into 4 groups: lower-limb fractures, other lower-limb injuries, upper-limb fractures, and other upper-limb injuries (Table W, at www.jfponline.com). Each group was further divided into trials using some form of limb support (such as a brace, splint, or a short period of immobilization) or minimal or no support (bandage, crutches, or tape) in the early mobilization group.
Most studies used some form of dynamic treatment for the injured limb, with highest use in lowerlimb injuries (74%); 2 studies included both supported and unsupported mobilization.24-26 In studies of upper-limb fractures, support was used in 50%. In high-quality studies, 12 out of 16 studies used some support, but results were consistent with studies that did not. The smaller number of studies using minimal support makes comparison with supported mobilization difficult, but results suggest that supported mobilization may result in an earlier return to work or sport, whereas minimally supported patients achieved better composite scores and muscle strength. There was too much clinical heterogeneity to sensibly combine the results; however, we were interested to see whether mobilization was useful across a heterogeneous group of conditions.
Patient-centered outcomes
No study reported any significant improvement with rest on swelling and pain. To the contrary, 13 studies reported significant improvement with early mobilization compared with rest,16,17,27-37 and 9 studies reported enhanced patient satisfaction.16,30,36,38-43 High-quality studies that reported pain levels found no difference or favored early mobilization.25,26,30,31,39,44-51 This was significant in only 2 studies of lower-limb nonfractures.25,26,30 No study reported adverse patient opinion in an early mobilization regime,28,31,38,40,44-46,48,51-56 and patients appreciated their ability to use the affected limb.34,43,49
Functional outcomes
Ten studies measured global function, using composite scores including subjective and objective criteria—pain, stiffness, swelling, use of supports, and ability to climb stairs, play sport, work, and undertake activities of daily life (Table W). Seven studies reported significant improvements with early mobilization—after 6 months (6 studies),28,35,42,46,52,57 or 12 months (1 study).32 Four studies of high quality found significant benefit for early mobilization in composite scores, most of these for lower-limb fractures.46,47,52,54 Significantly more patients with acute ankle sprain, who were immobilized in a cast, sought medical and physiotherapy advice in the initial 3 weeks, compared with those mobilized early with a functional brace.50
Return to work and sport
Thirteen studies reported that early mobilization resulted in a significantly earlier return to work (about 30%–60% earlier),16,17,30,33,35,36,38-40,52,57-59 especially in lower-limb nonfracture injuries. In 1 study of ankle fractures, patients randomized to wear a cast reported better performance of daily activities at 6 weeks than those mobilized with crutches.28 Perhaps, this reflects practical difficulties associated with using crutches. Five studies of lower-limb injury reported an earlier return to sport,16,30,39,57,60 as did 3 studies of postoperative Achilles tendon repair30,39,60 and 2 of ankle ligament injury or sprains.16,57 Five studies reporting a significantly earlier return to work or sport were of high quality, as were all studies of lower limb injuries.25,26,30,39,46,52
Range of movement
Fourteen studies of upper- and lower-limb fractures reported significant improvements in range of movement. Significant differences in range of movement were typically observed within 13 weeks of the injury,12,27,29,34,38,42,45,46,49,52,61-64 although a few studies reported differences for longer periods. Similarly for lower-limb nonfractures, significantly better ranges of motion were found within short periods,25,33,37,39,43 and also after 12 months.30,39-41 Eleven studies reporting this outcome were of high quality,25,26,30,31,39,45,46,48-51,54 and 4 studies found significant benefit for early mobilization.25,26,30,46,49 The other 7 high-quality studies favored early mobilization, and 1 found no difference.45
Deformity and other complications
Four studies found early mobilization reduced deformity: for angular displacement61 and radial shortening32 in Colles’ fractures; displacement of metacarpal fractures58 and cosmetic deformity in radial fractures.42 Two studies were of high quality.30,65 Ten trials reported no changes in deformity, no loss of fracture reduction, or any other complications with early mobilization of fractures.28,31,45,48,50,59,62-64,66 In contrast, for Colles’ fractures, significantly greater dorsal angulation61 and significant increases in radial tilt and decreased radioulnar joint space49 were reported for mobilized wrists.
Patient preferences
Patients expressed preference for a brace following anterior cruciate ligament surgery because it helped reduce pain and swelling67; they expressed preference for a cast following surgery for ankle fracture because it improved ability to perform everyday activities.28
Patients with distal radius fractures preferred early treatment with a Tubigrip bandage and a back-slab instead of removable splints, which increased pain and decreased mobilization.53 Generally, patients with fractures preferred rigid support immediately after the injury. Some also expected to have a traditional cast applied after learning their injured wrist was fractured.53
Cost of treatment
Full economic evaluations were not usually satisfactorily undertaken in these clinical studies. The cost of early mobilization was more expensive than immobilization in some studies8,23 but cheaper in others.2,9,10,24,68 It is estimated that direct costs to the patient were lower for early mobilization because of the decreased loss of working time.10,44,68,69
Adherence and supervision
Ten studies excluded patients who were unable to understand the nature of the treatment; had dementia; existing joint disease; drug abuse; alcohol problems; or difficulty with walking aids.28,31,38-41,45,46,49,69 Thus, many researchers have assumed that early mobilization requires greater patient responsibility. Some researchers have recommended applying casts for patients deemed “uncooperative” or “unlikely to be compliant,” despite their positive findings for early mobilization.3,16
Although 10 trials employed physiotherapy or supervised mobilization sessions,25,26,28,29,40,41,46,65,70 11 studies relied on self-controlled mobilization.27,30,31,38,39,42,44,45,48,49,52 In addition, some interventions (eg, braces) intrinsically required more supervision with their removal and reapplication than others (eg, functional casts or semirigid bandages).
Discussion
Early mobilization seems to decrease pain, swelling, and stiffness—at least in the short-term—and patients generally prefer it to immobilization. It results in earlier return—to work and to a greater range of motion, which is most significant within the first 2 months of the injury and can be maintained for up to 12 months for nonfracture injuries. Early mobilization does not increase cosmetic or radiological deformity for stable fractures, and patients experience fewer complications and residual symptoms. However, early mobilization may place greater demands on patients and require higher levels of understanding and responsibility, therefore making it unsuitable for some patients.
This systematic review of all upper- and lower-limb injuries, including fractures, consistently found in favor of early mobilization over rest. We acknowledge that the range of injuries reviewed is very limited. However, the clear benefits of mobilization indicated by this review suggest we need research in a wider range of injuries.
Similarly, it would be naïve to assume mobilization is better than immobilization in all circumstances. Harm must occur at some level of increased activity. In addition we know that pain and discomfort are often experienced by patients who demand immobilization (a “palliative” form of management). Finding the ideal level and type of activity must be undertaken empirically. Therefore more quality clinical trials are required to determine and evaluate the best regimens for early mobilization.
Newer studies will probably find that mobilization can be employed more often (and perhaps more vigorously) than we now advise. The best evidence at hand suggests the medical profession generally errs too conservatively on the side of immobilization.
Acknowledgments
Charlotte Nash did the searches, assembled and analysed the tables and wrote the first draft. Charlotte Nash and Sharon Mickan assessed the quality of all included studies and edited drafts. Paul Glasziou and Chris Del Mar initiated the question and edited drafts. This work was supported in part by a scholarship awarded by the Centre for General Practice, The University of Queensland, and funded by the Australian Commonwealth Department of Health and Ageing through the Primary Health Care Research, Evaluation and Development Strategy.
Corresponding author
Professor Chris B. Del Mar, Centre for General Practice, Faculty Heath Science and Medicine, Bond University, Gold Coast, Queensland 4229, Australia. E-mail: [email protected].
1. Allen C, Glasziou P, Del Mar C. Bed rest: a potentially harmful treatment needing more careful evaluation. Lancet. 1999;354:1229-1233.
2. Madhok R, Bhopal RS. Coping with an upper limb fracture? A study of the elderly. Public Health. 1992;106:19-28.
3. Salter RB. Motion versus rest: Why immobilize joints? J Bone Joint Surg Br. 1982;64B:251-254.
4. Safran MR, Zachazewski JE, Benedetti RS, Bartolozzi AR, Mandelbaum R. Lateral ankle sprains: a comprehensive review. Part 2: treatment and rehabilitation with an emphasis on the athlete. Med Sci Sports Exerc. 1999;31:S438-S447.
5. Willems C. Immediate active mobilization in the treatment of gunshot wounds of joints. Medical Record. 1919;95:953-962.
6. Dent JA. Continuous passive motion in hand rehabilitation. Prosthet Orthot Int 1993;17:130-135.
7. Pneumaticos SG, Noble PC, McGarvey WC, Mody DR, Trevino SG. The effects of early mobilization in the healing of Achilles tendon repair. Foot Ankle Int. 2000;21:551-557.
8. Gelberman RH, Menon J, Gonsalves M, Akeson WH. The effects of mobilisation on the vascularisation of healing flexor tendons in dogs. Clin Orthop. 1980;153:283-289.
9. Kannus P. Immobilisation or early mobilisation after an acute soft tissue injury. The Physician and Sportsmedicine. 2000;28:55-63.
10. Halikis MN, Manske PR, Kubota H, Aoki M. Effect of immobilization, immediate mobilization and delayed mobilization of the resistance to digital flexion using a tendon injury model. J Hand Surg [Am]. 1997;22A:464-472.
11. Romanelli DA, Almekinders LC, Mandelbaum BR. Achilles rupture in the athlete: Current science and treatment. Sports Medicine and Arthroscopy Review. 2000;8:377-386.
12. Stockle U, Konig B, Tempka A, Sudkamp NP. Cast immobilisation or vacuum stabilizing system? Unfallchirurg. 2000;103:215-219.
13. Viidik A. The effect of training on the tensile strength of isolated rabbit tendons. Scandinavian Journal of Plastic and Reconstructive Surgery. 1967;1:141-147.
14. Woo SL, Gelberman RH, Cobb NG, Amiel D, Lothringer K, Akeson WH. The importance of controlled passive mobilization on flexor tendon healing. A biomechanical study. Acta Orthop Scand. 1981;52:615-622.
15. Peacock E. Biological principles in the healing of long tendons. Surg Clin North Am. 1965;45:461-476.
16. Kerkhoffs GMMJ, Rowe BH, Assendelft WJJ, Kelly KD, Struijs PAA, Niek van Dijk C. Immobilisation for acute ankle sprain: a systematic review. Arch Orthop Trauma Surg. 2001;121:462-471.
17. Pijnenburg ACM, van Dijk CN, Bossuyt PMM, Marti RK. Treatment of ruptures of the lateral ankle ligaments: A meta-analysis. J Bone Joint Surg Am. 2000;82A:761-773.
18. Mackay D, Wood L, Rangan A. The treatment of isolated ulnar fractures in adults: a systematic review. Injury. 2000;31:565-570.
19. Prokop A, Kulus S, Helling HJ, Burger C, Rehm KE. Are there concepts in treatment of metacarpal fractures? Own results and a review of the literature of the last 12 years. Unfallchirurg. 1999;102:50-58.
20. Shrier I. Treatment of lateral collateral ligament sprains of the ankle: a critical appraisal of the literature. Clin J Sport Med. 1995;5:187-195.
21. Ogilvie-Harris DJ, Gilbart M. Treatment modalities for soft tissue injuries of the ankle: a critical review. Clin J Sport Med. 1995;5:175-186.
22. Hviid K, Harager K, Schantz K. Aftercare of malleolar fractures in Denmark. A questionnaire study. Ugeskr Læger. 2000;62:2747-2750.
23. Gillespie W, Gillespie L, Morton L. Cochrane Musculoskeletal Injuries Group. Cochrane Database 2002.
24. Sommer HM, Schreiber H. Early functional conservative therapy of fresh fibular capsular ligament rupture from the socioeconomic viewpoint. Sportverletzung Sportschaden. 1993;7:40-46.
25. Dettori JR. Early ankle mobilization, part I: The immediate effect on acute, lateral ankle sprains. A randomised clinical trial. Mil Med. 1994;159:15-20.
26. Dettori JR, Basmania CJ. Early ankle mobilization, part II: A one-year follow-up of acute, lateral ankle sprains. A randomized clinical trial. Mil Med. 1994;159:20-24.
27. Stuart PR, Brumby C, Smith SR. Comparative study of functional bracing and plaster cast treatment of stable lateral malleolar fractures. Injury. 1989;20:323-326.
28. van Laarhoven CJHM, Meeuwis JD, van der Werken C. Postoperative treatment of internally fixed ankle fractures. J Bone Joint Surg Br. 1996;78B:395-399.
29. Søndenaa K, Høigaard U, Smith D, Alho A. Immobilisation of operated ankle fractures. Acta Orthop Scand. 1986;57:59-61.
30. Cetti R, Henriksen LO, Jacobsen KS. A new treatment of ruptured Achilles tendons. Clin Orthop. 1994;308:155-165.
31. Dias JJ, Wray CC, Jones JM, Gregg PJ. The value of early mobilisation in the treatment of Colles’ fractures. J Bone Joint Surg Br. 1987;69B:463-467.
32. Abbaszadegan H, Conradi P, Jonsson U. Fixation not needed for undisplaced Colles’ fracture. Acta Orthop Scand. 1989;60:60-62.
33. Nyska M, Weisel Y, Halperin N, Mann G, Segal D. Controlled mobilization after acute ankle inversion injury. Journal of Sports Traumatology and Related Research. 1999;21:114-120.
34. McMahon PJ, Woods DA, Burge PD. Initial treatment of closed metacarpal fractures. J Hand Surg [Br]. 1994;19B:597-600.
35. Konradsen L, Hølmer P, Søndergaard L. Early mobilizing treatment for grade III ankle ligament injuries. Foot and Ankle. 1991;12:69-73.
36. Cetti R, Christensen SE, Corfitzen MT. Ruptured fibular ankle ligament: Plaster or Pliton brace? Br J Sports Med. 1984;18:104-109.
37. Eiff MP, Smith AT, Smith GE. Early mobilisation versus immobilisation in the treatment of lateral ankle sprains. Am J Sports Med. 1994;22:83-86.
38. Gebuhr P, Hölmich P, Ørsnes T, Soelberg M, Krasheninnikoff M, Kjersgaard AG. Isolated ulnar shaft fractures. J Bone Joint Surg Br. 1992;74B:757-759.
39. Mortensen NHM, Skov O, Jensen PE. Early motion of the ankle after operative treatment of a rupture of the Achilles tendon. J Bone Joint Surg Am. 1999;81A:983-990.
40. Buchgraber A, Pässler HH. Percutaneous repair of Achilles tendon rupture. Clin Orthop. 1997;341:113-122.
41. Saleh M, Marshall PD, Senior R, MacFarlane A. The Sheffield Splint for controlled early mobilisation after rupture of the calcaneal tendon. J Bone Joint Surg Br. 1992;74B:206-209.
42. Davis TRC, Buchanan JM. A controlled prospective study of early mobilization of minimally displaced fractures of the distal radial metaphysis. Injury. 1987;18:283-285.
43. Avci S, Sayli U. Comparison of the results of short-term rigid and semi-rigid cast immobilization for the treatment of grade 3 inversion injuries of the ankle. Injury. 1998;29:581-584.
44. Dogra AS, Rangan A. Early mobilisation versus immobilisation of surgically treated ankle fracture. Prospective randomised control trial. Injury. 1999;30:417-419.
45. Hedström M, Ahl T, Dalén N. Early postoperative ankle exercises: a study of postoperative lateral malleolar fractures. Clin Orthop. 1994;300:193-196.
46. Port AM, McVie JL, Naylor G, Kreibich DN. Comparison of two conservative methods of treating an isolated fracture of the lateral malleous. J Bone Joint Surg Br. 1996;78B:568-572.
47. Klein J, Rixen D, Albring T, Tiling T. Functional treatment with a pneumatic ankle brace versus cast immobilisation for recent rupture of the fibular ligament in the ankle. A randomised clinical trial. Unfallchirurg. 1991;94:99-104.
48. Allain J, le Guilloux P, Mouël SL, Goutallier D. Trans-styloid fixation of fractures of the distal radius: A prospective randomized comparison between 6- and 1-week postoperative immobilization in 60 fractures. Acta Orthop Scand. 1999;70:119-123.
49. Millett PJ, Rushton N. Early mobilization in the treatment of Colles’ fracture: a 3 year prospective study. Injury. 1995;26:671-675.
50. Stewart HD, Innes AR, Burke FD. Functional cast-bracing for Colles’ fractures. A comparison between cast-bracing and conventional plaster casts. J Bone Joint Surg Br. 1984;66B:749-753.
51. Unsworth-White J, Koka R, Churchill M, D’Arcy JC, James SE. The non-operative management of radial head fractures: a randomized trial of three treatments. Injury. 1994;25:165-167.
52. Egol KA, Dolan R, Koval KJ. Functional outcome of surgery for fractures of the ankle. J Bone Joint Surg Br. 2000;82:246-249.
53. Stoffelen D, Broos P. Minimally displaced distal radius fractures: do they need plaster treatment? J Trauma. 1998;44:503-505.
54. DiStasio AJ, Jaggears FR, DePasquale LV, Frassica FJ, Turen CH. Protected early motion versus cast immobilization in postoperative management of ankle fractures. Contemporary Orthopaedics. 1994;29:273-277.
55. Regis D, Montanari M, Magnan B, Spagnol S, Bragantini A. Dynamic orthopaedic brace in the treatment of ankle sprains. Foot Ankle Int. 1995;16:422-426.
56. Grønmark T, Johnsen O, Kogstad O. Rupture of the lateral ligaments of the ankle: a controlled clinical trial. Injury. 1980;11:215-218.
57. Eggert A, Gruber J, Darda L. Treatment of ankle joint injuries. Randomized study of postoperative therapy and early functional treatment. Unfallchirurg. 1986;89:316-320.
58. Konradsen L, Nielsen PT, Albrecht-Beste E. Functional treatment of metacarpal fractures. Acta Orthop Scand. 1990;61:531-534.
59. Broström L. Sprained ankles. V. Treatment and prognosis in recent ligament ruptures. Acta Chir Scand. 1966;132:537-550.
60. Kerkhoffs GMMJ, Struijs PAA, Raaymakers ELFB, Marti RK. Functional treatment after surgical repair of acute Achilles tendon rupture: wrap vs walking cast. Arch Orthop Trauma Surg. 2002;122:102-105.
61. Ferris BD, Thomas NP, Dewar ME, Simpson DA. Brace treatment of Colles’ fracture. Acta Orthop Scand. 1989;60:63-65.
62. Braakman M, Oderwald EE, Haentjens MHHJ. Functional taping of fractures of the 5th metacarpal results in a quicker recovery. Injury. 1998;29:5-9.
63. Tropp H, Norlin R. Ankle performance after ankle fracture: randomised study of early mobilization. Foot Ankle Int. 1995;16:79-83.
64. Kuokkanen HOM, Mulari-Karanen SK, Niskanen RO, Haapala JK, Korkala OL. Treatment of subcapital fractures of the fifth metacarpal bone: a prospective randomised comparison between functional treatment and reposition and splinting. Scand J Plast Recontr Surg Hand Surg. 1999;33:315-317.
65. Murty AN, El Zebdeh MY, Ireland J. Tibial tunnel enlargement following anterior cruciate reconstruction: does post-operative immobilisation make a difference? Knee. 2001;8:39-43.
66. McAuliffe TB, Hilliar KM, Coates CJ, Grange WJ. Early mobilisation of Colles’ fractures: a prospective trial. J Bone Joint Surg Br. 1987;69B:727-729.
67. Brandsson S, Faxén E, Kartus J, Eriksson BI, Karlsson J. Is a knee brace advantageous after anterior cruciate ligament surgery? Scand J Med Sci Sports. 2001;11:110-114.
68. Lind K. Konservativ behandling af laterale ligamentrupturer i fodleddet. Ugeskr Lger. 1984;146:4017-4019.
69. Rafai M, Largab A, Cohen D, Trafeh M. Pure posterior luxation of the elbow in adults: immobilization or early mobilization. A randomized prospective study of 50 cases. Chir Main. 1999;18:272-278.
70. Strickland JW, Glogovac SV. Digital function following flexor tendon repair in Zone II: A comparison of immobilization and controlled passive motion techniques. Journal of Hand Surgery. 1980;5:537-543.
71. Møller-Larsen F, Wethelund JO, Jurik AG, de Carvalho A, Lucht U. Comparison of three different treatments for ruptured lateral ankle ligaments. Acta Orthop Scand. 1988;59:564-566.
72. Caro D, Craft IL, Howells JB, Shaw PC. Diagnosis and treatment of injury of lateral ligament of the ankle joint. Lancet. 1964;2:720-723.
1. Allen C, Glasziou P, Del Mar C. Bed rest: a potentially harmful treatment needing more careful evaluation. Lancet. 1999;354:1229-1233.
2. Madhok R, Bhopal RS. Coping with an upper limb fracture? A study of the elderly. Public Health. 1992;106:19-28.
3. Salter RB. Motion versus rest: Why immobilize joints? J Bone Joint Surg Br. 1982;64B:251-254.
4. Safran MR, Zachazewski JE, Benedetti RS, Bartolozzi AR, Mandelbaum R. Lateral ankle sprains: a comprehensive review. Part 2: treatment and rehabilitation with an emphasis on the athlete. Med Sci Sports Exerc. 1999;31:S438-S447.
5. Willems C. Immediate active mobilization in the treatment of gunshot wounds of joints. Medical Record. 1919;95:953-962.
6. Dent JA. Continuous passive motion in hand rehabilitation. Prosthet Orthot Int 1993;17:130-135.
7. Pneumaticos SG, Noble PC, McGarvey WC, Mody DR, Trevino SG. The effects of early mobilization in the healing of Achilles tendon repair. Foot Ankle Int. 2000;21:551-557.
8. Gelberman RH, Menon J, Gonsalves M, Akeson WH. The effects of mobilisation on the vascularisation of healing flexor tendons in dogs. Clin Orthop. 1980;153:283-289.
9. Kannus P. Immobilisation or early mobilisation after an acute soft tissue injury. The Physician and Sportsmedicine. 2000;28:55-63.
10. Halikis MN, Manske PR, Kubota H, Aoki M. Effect of immobilization, immediate mobilization and delayed mobilization of the resistance to digital flexion using a tendon injury model. J Hand Surg [Am]. 1997;22A:464-472.
11. Romanelli DA, Almekinders LC, Mandelbaum BR. Achilles rupture in the athlete: Current science and treatment. Sports Medicine and Arthroscopy Review. 2000;8:377-386.
12. Stockle U, Konig B, Tempka A, Sudkamp NP. Cast immobilisation or vacuum stabilizing system? Unfallchirurg. 2000;103:215-219.
13. Viidik A. The effect of training on the tensile strength of isolated rabbit tendons. Scandinavian Journal of Plastic and Reconstructive Surgery. 1967;1:141-147.
14. Woo SL, Gelberman RH, Cobb NG, Amiel D, Lothringer K, Akeson WH. The importance of controlled passive mobilization on flexor tendon healing. A biomechanical study. Acta Orthop Scand. 1981;52:615-622.
15. Peacock E. Biological principles in the healing of long tendons. Surg Clin North Am. 1965;45:461-476.
16. Kerkhoffs GMMJ, Rowe BH, Assendelft WJJ, Kelly KD, Struijs PAA, Niek van Dijk C. Immobilisation for acute ankle sprain: a systematic review. Arch Orthop Trauma Surg. 2001;121:462-471.
17. Pijnenburg ACM, van Dijk CN, Bossuyt PMM, Marti RK. Treatment of ruptures of the lateral ankle ligaments: A meta-analysis. J Bone Joint Surg Am. 2000;82A:761-773.
18. Mackay D, Wood L, Rangan A. The treatment of isolated ulnar fractures in adults: a systematic review. Injury. 2000;31:565-570.
19. Prokop A, Kulus S, Helling HJ, Burger C, Rehm KE. Are there concepts in treatment of metacarpal fractures? Own results and a review of the literature of the last 12 years. Unfallchirurg. 1999;102:50-58.
20. Shrier I. Treatment of lateral collateral ligament sprains of the ankle: a critical appraisal of the literature. Clin J Sport Med. 1995;5:187-195.
21. Ogilvie-Harris DJ, Gilbart M. Treatment modalities for soft tissue injuries of the ankle: a critical review. Clin J Sport Med. 1995;5:175-186.
22. Hviid K, Harager K, Schantz K. Aftercare of malleolar fractures in Denmark. A questionnaire study. Ugeskr Læger. 2000;62:2747-2750.
23. Gillespie W, Gillespie L, Morton L. Cochrane Musculoskeletal Injuries Group. Cochrane Database 2002.
24. Sommer HM, Schreiber H. Early functional conservative therapy of fresh fibular capsular ligament rupture from the socioeconomic viewpoint. Sportverletzung Sportschaden. 1993;7:40-46.
25. Dettori JR. Early ankle mobilization, part I: The immediate effect on acute, lateral ankle sprains. A randomised clinical trial. Mil Med. 1994;159:15-20.
26. Dettori JR, Basmania CJ. Early ankle mobilization, part II: A one-year follow-up of acute, lateral ankle sprains. A randomized clinical trial. Mil Med. 1994;159:20-24.
27. Stuart PR, Brumby C, Smith SR. Comparative study of functional bracing and plaster cast treatment of stable lateral malleolar fractures. Injury. 1989;20:323-326.
28. van Laarhoven CJHM, Meeuwis JD, van der Werken C. Postoperative treatment of internally fixed ankle fractures. J Bone Joint Surg Br. 1996;78B:395-399.
29. Søndenaa K, Høigaard U, Smith D, Alho A. Immobilisation of operated ankle fractures. Acta Orthop Scand. 1986;57:59-61.
30. Cetti R, Henriksen LO, Jacobsen KS. A new treatment of ruptured Achilles tendons. Clin Orthop. 1994;308:155-165.
31. Dias JJ, Wray CC, Jones JM, Gregg PJ. The value of early mobilisation in the treatment of Colles’ fractures. J Bone Joint Surg Br. 1987;69B:463-467.
32. Abbaszadegan H, Conradi P, Jonsson U. Fixation not needed for undisplaced Colles’ fracture. Acta Orthop Scand. 1989;60:60-62.
33. Nyska M, Weisel Y, Halperin N, Mann G, Segal D. Controlled mobilization after acute ankle inversion injury. Journal of Sports Traumatology and Related Research. 1999;21:114-120.
34. McMahon PJ, Woods DA, Burge PD. Initial treatment of closed metacarpal fractures. J Hand Surg [Br]. 1994;19B:597-600.
35. Konradsen L, Hølmer P, Søndergaard L. Early mobilizing treatment for grade III ankle ligament injuries. Foot and Ankle. 1991;12:69-73.
36. Cetti R, Christensen SE, Corfitzen MT. Ruptured fibular ankle ligament: Plaster or Pliton brace? Br J Sports Med. 1984;18:104-109.
37. Eiff MP, Smith AT, Smith GE. Early mobilisation versus immobilisation in the treatment of lateral ankle sprains. Am J Sports Med. 1994;22:83-86.
38. Gebuhr P, Hölmich P, Ørsnes T, Soelberg M, Krasheninnikoff M, Kjersgaard AG. Isolated ulnar shaft fractures. J Bone Joint Surg Br. 1992;74B:757-759.
39. Mortensen NHM, Skov O, Jensen PE. Early motion of the ankle after operative treatment of a rupture of the Achilles tendon. J Bone Joint Surg Am. 1999;81A:983-990.
40. Buchgraber A, Pässler HH. Percutaneous repair of Achilles tendon rupture. Clin Orthop. 1997;341:113-122.
41. Saleh M, Marshall PD, Senior R, MacFarlane A. The Sheffield Splint for controlled early mobilisation after rupture of the calcaneal tendon. J Bone Joint Surg Br. 1992;74B:206-209.
42. Davis TRC, Buchanan JM. A controlled prospective study of early mobilization of minimally displaced fractures of the distal radial metaphysis. Injury. 1987;18:283-285.
43. Avci S, Sayli U. Comparison of the results of short-term rigid and semi-rigid cast immobilization for the treatment of grade 3 inversion injuries of the ankle. Injury. 1998;29:581-584.
44. Dogra AS, Rangan A. Early mobilisation versus immobilisation of surgically treated ankle fracture. Prospective randomised control trial. Injury. 1999;30:417-419.
45. Hedström M, Ahl T, Dalén N. Early postoperative ankle exercises: a study of postoperative lateral malleolar fractures. Clin Orthop. 1994;300:193-196.
46. Port AM, McVie JL, Naylor G, Kreibich DN. Comparison of two conservative methods of treating an isolated fracture of the lateral malleous. J Bone Joint Surg Br. 1996;78B:568-572.
47. Klein J, Rixen D, Albring T, Tiling T. Functional treatment with a pneumatic ankle brace versus cast immobilisation for recent rupture of the fibular ligament in the ankle. A randomised clinical trial. Unfallchirurg. 1991;94:99-104.
48. Allain J, le Guilloux P, Mouël SL, Goutallier D. Trans-styloid fixation of fractures of the distal radius: A prospective randomized comparison between 6- and 1-week postoperative immobilization in 60 fractures. Acta Orthop Scand. 1999;70:119-123.
49. Millett PJ, Rushton N. Early mobilization in the treatment of Colles’ fracture: a 3 year prospective study. Injury. 1995;26:671-675.
50. Stewart HD, Innes AR, Burke FD. Functional cast-bracing for Colles’ fractures. A comparison between cast-bracing and conventional plaster casts. J Bone Joint Surg Br. 1984;66B:749-753.
51. Unsworth-White J, Koka R, Churchill M, D’Arcy JC, James SE. The non-operative management of radial head fractures: a randomized trial of three treatments. Injury. 1994;25:165-167.
52. Egol KA, Dolan R, Koval KJ. Functional outcome of surgery for fractures of the ankle. J Bone Joint Surg Br. 2000;82:246-249.
53. Stoffelen D, Broos P. Minimally displaced distal radius fractures: do they need plaster treatment? J Trauma. 1998;44:503-505.
54. DiStasio AJ, Jaggears FR, DePasquale LV, Frassica FJ, Turen CH. Protected early motion versus cast immobilization in postoperative management of ankle fractures. Contemporary Orthopaedics. 1994;29:273-277.
55. Regis D, Montanari M, Magnan B, Spagnol S, Bragantini A. Dynamic orthopaedic brace in the treatment of ankle sprains. Foot Ankle Int. 1995;16:422-426.
56. Grønmark T, Johnsen O, Kogstad O. Rupture of the lateral ligaments of the ankle: a controlled clinical trial. Injury. 1980;11:215-218.
57. Eggert A, Gruber J, Darda L. Treatment of ankle joint injuries. Randomized study of postoperative therapy and early functional treatment. Unfallchirurg. 1986;89:316-320.
58. Konradsen L, Nielsen PT, Albrecht-Beste E. Functional treatment of metacarpal fractures. Acta Orthop Scand. 1990;61:531-534.
59. Broström L. Sprained ankles. V. Treatment and prognosis in recent ligament ruptures. Acta Chir Scand. 1966;132:537-550.
60. Kerkhoffs GMMJ, Struijs PAA, Raaymakers ELFB, Marti RK. Functional treatment after surgical repair of acute Achilles tendon rupture: wrap vs walking cast. Arch Orthop Trauma Surg. 2002;122:102-105.
61. Ferris BD, Thomas NP, Dewar ME, Simpson DA. Brace treatment of Colles’ fracture. Acta Orthop Scand. 1989;60:63-65.
62. Braakman M, Oderwald EE, Haentjens MHHJ. Functional taping of fractures of the 5th metacarpal results in a quicker recovery. Injury. 1998;29:5-9.
63. Tropp H, Norlin R. Ankle performance after ankle fracture: randomised study of early mobilization. Foot Ankle Int. 1995;16:79-83.
64. Kuokkanen HOM, Mulari-Karanen SK, Niskanen RO, Haapala JK, Korkala OL. Treatment of subcapital fractures of the fifth metacarpal bone: a prospective randomised comparison between functional treatment and reposition and splinting. Scand J Plast Recontr Surg Hand Surg. 1999;33:315-317.
65. Murty AN, El Zebdeh MY, Ireland J. Tibial tunnel enlargement following anterior cruciate reconstruction: does post-operative immobilisation make a difference? Knee. 2001;8:39-43.
66. McAuliffe TB, Hilliar KM, Coates CJ, Grange WJ. Early mobilisation of Colles’ fractures: a prospective trial. J Bone Joint Surg Br. 1987;69B:727-729.
67. Brandsson S, Faxén E, Kartus J, Eriksson BI, Karlsson J. Is a knee brace advantageous after anterior cruciate ligament surgery? Scand J Med Sci Sports. 2001;11:110-114.
68. Lind K. Konservativ behandling af laterale ligamentrupturer i fodleddet. Ugeskr Lger. 1984;146:4017-4019.
69. Rafai M, Largab A, Cohen D, Trafeh M. Pure posterior luxation of the elbow in adults: immobilization or early mobilization. A randomized prospective study of 50 cases. Chir Main. 1999;18:272-278.
70. Strickland JW, Glogovac SV. Digital function following flexor tendon repair in Zone II: A comparison of immobilization and controlled passive motion techniques. Journal of Hand Surgery. 1980;5:537-543.
71. Møller-Larsen F, Wethelund JO, Jurik AG, de Carvalho A, Lucht U. Comparison of three different treatments for ruptured lateral ankle ligaments. Acta Orthop Scand. 1988;59:564-566.
72. Caro D, Craft IL, Howells JB, Shaw PC. Diagnosis and treatment of injury of lateral ligament of the ankle joint. Lancet. 1964;2:720-723.