User login
What is your diagnosis? - January 2019
Primary intestinal lymphangiectasia
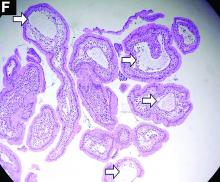
Histologic examination shows chronic inflammation of the ileum characterized by increased lymphoplasma cell infiltration of lamina propria without malignancy. Moreover, marked dilatation of lymphatic ducts that involved the mucosa was identified (Figure F, arrows; stain: hematoxylin and eosin; original magnification, ×100). On the basis of pathologic examinations, a diagnosis of primary intestinal lymphangiectasia (PIL) was made.
PIL is an extremely rare cause of protein-losing enteropathy characterized by the presence of dilated lymphatic channels in the mucosa, submucosa, or subserosa leading to protein-losing enteropathy.1 The true incidence and prevalence of this disease remains unclear. The disease affects males and females equally, and usually occurs in children and young adults. To date, less than 200 cases of PIL have been reported in the literature. The clinical manifestations of PIL may be asymptomatic or symptomatic such as abdominal pain, edema, diarrhea, and dyspnea. The diagnosis is based on the typical endoscopic findings of diffuse scattered mucosal white blebs with characteristic histologic findings of abnormal lymphatic dilatation. Double-balloon enteroscopy and capsule endoscopy are powerful modalities to evaluate the entire affected area of PIL.2 Although diet modification is a major treatment of PIL, several medicines have been reported to be useful such as corticosteroids, octreotide, and antiplasmin.3 Moreover, in patients with segmental lesions, surgery with local bowel resection is a useful treatment.3 In addition, PIL had a 5% risk of malignant transformation into lymphoma.3
References
1. Waldmann TA, Steinfeld JL, Dutcher TF, et al. The role of the gastrointestinal system in “idiopathic hypoproteinemia.” Gastroenterology. 1961;41:197-207.
2. Oh TG, Chung JW, Kim HM, et al. Primary intestinal lymphangiectasia diagnosed by capsule endoscopy and double balloon enteroscopy. World J Gastrointest Endosc. 2011;3:235-40.
3. Wen J, Tang Q, Wu, J. Primary intestinal lymphangiectasia: four case reports and a review of the literature. Dig Dis Sci. 2010;55:3466-72.
Primary intestinal lymphangiectasia
Histologic examination shows chronic inflammation of the ileum characterized by increased lymphoplasma cell infiltration of lamina propria without malignancy. Moreover, marked dilatation of lymphatic ducts that involved the mucosa was identified (Figure F, arrows; stain: hematoxylin and eosin; original magnification, ×100). On the basis of pathologic examinations, a diagnosis of primary intestinal lymphangiectasia (PIL) was made.
PIL is an extremely rare cause of protein-losing enteropathy characterized by the presence of dilated lymphatic channels in the mucosa, submucosa, or subserosa leading to protein-losing enteropathy.1 The true incidence and prevalence of this disease remains unclear. The disease affects males and females equally, and usually occurs in children and young adults. To date, less than 200 cases of PIL have been reported in the literature. The clinical manifestations of PIL may be asymptomatic or symptomatic such as abdominal pain, edema, diarrhea, and dyspnea. The diagnosis is based on the typical endoscopic findings of diffuse scattered mucosal white blebs with characteristic histologic findings of abnormal lymphatic dilatation. Double-balloon enteroscopy and capsule endoscopy are powerful modalities to evaluate the entire affected area of PIL.2 Although diet modification is a major treatment of PIL, several medicines have been reported to be useful such as corticosteroids, octreotide, and antiplasmin.3 Moreover, in patients with segmental lesions, surgery with local bowel resection is a useful treatment.3 In addition, PIL had a 5% risk of malignant transformation into lymphoma.3
References
1. Waldmann TA, Steinfeld JL, Dutcher TF, et al. The role of the gastrointestinal system in “idiopathic hypoproteinemia.” Gastroenterology. 1961;41:197-207.
2. Oh TG, Chung JW, Kim HM, et al. Primary intestinal lymphangiectasia diagnosed by capsule endoscopy and double balloon enteroscopy. World J Gastrointest Endosc. 2011;3:235-40.
3. Wen J, Tang Q, Wu, J. Primary intestinal lymphangiectasia: four case reports and a review of the literature. Dig Dis Sci. 2010;55:3466-72.
Primary intestinal lymphangiectasia
Histologic examination shows chronic inflammation of the ileum characterized by increased lymphoplasma cell infiltration of lamina propria without malignancy. Moreover, marked dilatation of lymphatic ducts that involved the mucosa was identified (Figure F, arrows; stain: hematoxylin and eosin; original magnification, ×100). On the basis of pathologic examinations, a diagnosis of primary intestinal lymphangiectasia (PIL) was made.
PIL is an extremely rare cause of protein-losing enteropathy characterized by the presence of dilated lymphatic channels in the mucosa, submucosa, or subserosa leading to protein-losing enteropathy.1 The true incidence and prevalence of this disease remains unclear. The disease affects males and females equally, and usually occurs in children and young adults. To date, less than 200 cases of PIL have been reported in the literature. The clinical manifestations of PIL may be asymptomatic or symptomatic such as abdominal pain, edema, diarrhea, and dyspnea. The diagnosis is based on the typical endoscopic findings of diffuse scattered mucosal white blebs with characteristic histologic findings of abnormal lymphatic dilatation. Double-balloon enteroscopy and capsule endoscopy are powerful modalities to evaluate the entire affected area of PIL.2 Although diet modification is a major treatment of PIL, several medicines have been reported to be useful such as corticosteroids, octreotide, and antiplasmin.3 Moreover, in patients with segmental lesions, surgery with local bowel resection is a useful treatment.3 In addition, PIL had a 5% risk of malignant transformation into lymphoma.3
References
1. Waldmann TA, Steinfeld JL, Dutcher TF, et al. The role of the gastrointestinal system in “idiopathic hypoproteinemia.” Gastroenterology. 1961;41:197-207.
2. Oh TG, Chung JW, Kim HM, et al. Primary intestinal lymphangiectasia diagnosed by capsule endoscopy and double balloon enteroscopy. World J Gastrointest Endosc. 2011;3:235-40.
3. Wen J, Tang Q, Wu, J. Primary intestinal lymphangiectasia: four case reports and a review of the literature. Dig Dis Sci. 2010;55:3466-72.
A 19-year-old boy presented to our hospital because of a 6-month history of progressive dyspnea and generalized edema. He developed cough, abdominal fullness, diarrhea, and leg edema 5 years ago.
Liver cirrhosis was suspected at that time. However, he seemed to have a poor response to medical treatment. Physical examination showed decreased breathing sounds and rales of the bilateral lower chest area, a distended abdomen with multiple purple striae, and edema of bilateral lower legs.
Laboratory tests showed a low serum total protein of 3.8 g/dL (normal range, 5.5–8), albumin of 2.0 g/dL (normal range, 3.8–5.4), total calcium of 7 mg/dL (normal range, 8.4–10.8), C-reactive protein of 11.02 mg/dL (normal, below 0.8). His hemogram showed a white blood cell count of 13,310 × 109/L (normal range, 3.5–11 × 109/L) with lymphocytopenia (9.8%).
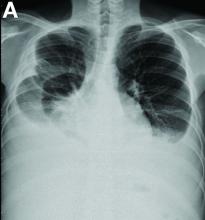
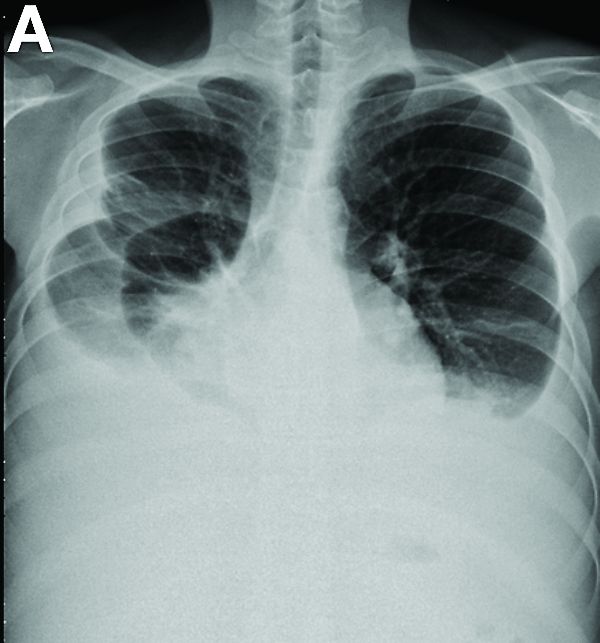
Other blood tests were within normal limits. The urinalysis and stool analysis were normal. Chest radiography showed bilateral pleural effusions (Figure A). Abdominal computed tomography demonstrated large ascites (Figure B). Paracentesis showed his serum ascites albumin gradient was 1.9 g/dL.
Subsequently, antegrade double-balloon enteroscopy (Fujinon EN-450T5; Fujinon, Saitama, Japan) demonstrated nodular mucosal lesions with a milk-like surface in the duodenum (Figure C).
Moreover, a snowflake appearance of mucosa was found in the jejunum and proximal ileum (Figure D). However, normal appearance of mucosa was identified in the middle ileum (Figure E). Biopsy specimens from these abnormal mucosal lesions were taken for pathology.