User login
A mediastinal mass
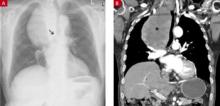
A 79-YEAR-OLD MAN came to our emergency department and asked that we check on a mediastinal mass that was first detected on a routine chest film 3 years earlier. The patient was asymptomatic; his medical history was unremarkable except for vitamin B12 deficiency. Physical examination revealed no abnormalities except for minor ataxia that was attributed to the lack of sufficient vitamin B12. A chest radiograph (FIGURE 1A) revealed a mass located in the upper right thorax with a slight deviation of the trachea to the left, consistent with previous x-ray findings. A computed tomography (CT) scan of the thorax (FIGURE 1B) showed a heterogeneous, multinodular mass in the anterior mediastinum with a maximal longitudinal diameter of 13.5 cm and a diagonal diameter of 9 cm. There was no obstruction or invasion of the trachea, esophagus, or mediastinal vessels.
FIGURE 1
X-ray and CT point to a diagnosis
The patient’s x-ray (A) revealed a mass in the upper right thorax with slight deviation of the trachea to the left (arrow). A CT scan of the thorax (B) revealed a heterogeneous, multinodular mass in the anterior mediastinum (asterisk). The mass did not obstruct or invade the trachea, esophagus, or mediastinal vessels.
WHAT IS YOUR DIAGNOSIS?
HOW WOULD YOU MANAGE THIS CONDITION?
Diagnosis: Retrosternal goiter
A retrosternal goiter was the most plausible diagnosis because of the patient’s advanced age, the asymptomatic behavior of the tumor, and its development over several years. The multilobular heterogenous appearance in the CT scan supported this diagnosis and made other disorders, such as thymoma and non-Hodgkin’s disease (to be discussed in a bit) very unlikely. In addition, the noninfiltrative behavior of the tumor suggested a benign mass, and CT images obtained from the neck (not shown) demonstrated that the mass originated from the right thyroid lobe without infiltrative or obstructive growth.
Benign mediastinal goiters are relatively common in adults, and the incidence increases with age.1,2 When a goiter affects adjacent structures or obstructs the trachea, common symptoms include dyspnea, wheezing, coughing, jugular vein compression, dysphagia, vocal cord palsy, phrenic nerve palsy, and Horner’s syndrome.
Differential diagnosis includes thymomas and thymic carcinomas
Masses in the anterior mediastinum comprise a variety of pathologic entities and are more likely to be malignant than masses in other mediastinal compartments.3 The most common lesions are thymomas and thymic carcinomas, lymphomas, germ cell tumors, intrathoracic thyroid or parathyroid lesions, and metastases. Up to 50% of mediastinal tumors are detected incidentally, and cause few—if any—symptoms.4,5
Thymoma and thymic carcinomas represent approximately 20% of the cases of primary anterior mediastinal masses, and can be invasive. In addition, myasthenia gravis or tumor-related syndromes are very suggestive of thymoma.6 CT or magnetic resonance imaging (MRI) studies may help to differentiate the mass in the anterior mediastinum, but histopathological analysis is required to establish a definitive diagnosis.
Lymphomas account for 10% to 20% of primary anterior mediastinal masses. While Hodgkin’s lymphoma predominantly occurs in the third and fourth decade, non-Hodgkin’s disease may affect people at any age.7,8 Most patients are symptomatic at the time of diagnosis, complaining of fever, weight loss, and night sweats. Diagnosis is suggested by a CT scan showing a lobulated mass, but confirmatory histology is necessary to guide treatment and may be accomplished by needle biopsy or lymph node excision on a different body site.
Germ cell tumors represent 15% of anterior mediastinal masses, with an even higher share in children, and include benign teratoma, seminomas, and nonseminomatous germ cell tumors.9 CT and MRI studies may help to clarify the relationship of the tumor tissue to surrounding structures. While teratomas are most likely to occur in children and young adults (and contain various amounts of tissue derived from the ectoderm, endoderm, and mesoderm), seminomas occur predominantly in young men between 20 and 40 years of age (and often have cellular heterogeneity and contain elements of embryonal malignancy).10,11 Seminomas are the most common malignant germ cell tumors, but need to be distinguished from nonseminomatous germ cell tumors; serum levels for alpha-fetoprotein and beta-human chorionic gonadotropin may help, but fine needle aspiration cytology is definitely needed.
Mediastinal cysts are common benign lesions of the mediastinum of pericardial, enteric, bronchogenic, or thymic origin, and are easily detected by CT or MRI studies. In addition, growth of parathyroid tissue can result in a retrosternal tumor, but such tumors are rarely of significant size.
Diagnosis hinges primarily on the CT scan
CT imaging is the method of choice to determine whether a mediastinal mass is thyroidal in origin and to define the extent of substernal goiter and the potential impingement on adjacent structures.12 These scans drive the need for and choice of therapy.13 An MRI of the thyroid gland may be helpful in distinguishing the thyroid from other tissue; ultrasonography is more accurate for defining thyroid anatomy in the anterior neck.
In the case of our patient, we used thyroid ultrasonography to confirm the CT findings. Further diagnostic tests included measurements of serum thyroid-stimulating hormone, triiodothyronine, and thyroxine, showing euthyroidism. Thyroid radionuclide imaging with 123-iodine was not performed in this case. While it can identify a substernal tumor as being thyroid tissue, the method can also be misleading because of impaired radioiodine uptake in some substernal goiters.14
Given our patient’s lack of pain, tenderness, or firmness in the cervical goiter and the results of his imaging studies, a fine-needle aspiration biopsy was not performed to rule out a malignant disorder like thyroid cancer.
Treatment ranges from watch and wait to surgery
Treatment of asymptomatic retrosternal goiter remains controversial. Levothyroxine suppression has a limited role in reducing the size or stopping the growth of the thyroid. Surgery is the method of choice in patients with obstructive symptoms, given the risk of progressive tracheal compression.
In the present case, we decided to watch and wait because of the patient’s age, history, and lack of any signs of obstruction of the trachea, esophagus, or mediastinal vessels. We recommended that the patient come back for a follow-up visit in 6 to 12 months.
CORRESPONDENCE: Christian S. Haas, MD, University Hospital Schleswig-Holstein–Campus Luebeck, Department of Medicine I, Ratzeburger Allee 160, 23538 Luebeck, Germany; [email protected]
1. Singh B, Lucente FE, Shaha AR. Substernal goiter: a clinical review. Am J Otolaryngol. 1994;15:409-416.
2. Strollo DC, Rosado de Christenson ML, Jett JR. Primary mediastinal tumors. Part 1: tumors of the anterior mediastinum. Chest. 1997;112:511-522.
3. Hoffman OA, Gillespie DJ, Aughenbaugh GL, et al. Primary mediastinal neoplasms (other than thymoma). Mayo Clin Proc. 1993;68:880-891.
4. Davis RD, Jr, Oldham HN, Jr, Sabiston DC, Jr. Primary cysts and neoplasms of the mediastinum: recent changes in clinical presentation, methods of diagnosis, management, and results. Ann Thorac Surg. 1987;44:229-237.
5. den Bakker MA, Oosterhuis JW. Tumours and tumour-like conditions of the thymus other than thymoma; a practical approach. Histopathology. 2009;54:69-89.
6. Gerein AN, Srivastava SP, Burgess J. Thymoma: a ten year review. Am J Surg. 1978;136:49-53.
7. van Heerden JA, Harison EG, Jr, Bernatz PE, et al. Mediastinal malignant lymphoma. Chest. 1970;57:518-529.
8. Hoppe RT. The non-Hodgkin’s lymphomas: pathology, staging, treatment. Curr Probl Cancer. 1987;11:363-447.
9. Luna MA, Valenquela-Tamariz J. Germ cell tumors of the mediastinum: postmortem findings. Am J Clin Pathol. 1976;65:450-454.
10. Moran CA, Suster S, Koss MN. Primary germ cell tumors of the mediastinum: III. Yolk sac tumor, embryonal carcinoma, choriocarcinoma, and combined nonteratomatous germ cell tumors of the mediastinum—a clinicopathologic and immunohistochemical study of 64 cases. Cancer. 1997;80:699-707.
11. Polansky SM, Barwick KW, Ravin CE. Primary mediastinal seminoma. AJR Am J Roentgenol. 1979;132:17-21.
12. Jennings A. Evaluation of substernal goiters using computed tomography and MR imaging. Endocrinol Metab Clin North Am. 2001;30:401-414, ix.
13. Wright CD, Mathisen DJ. Mediastinal tumors: diagnosis and treatment. World J Surg. 2001;25:204-209.
14. Park HM, Tarver RD, Siddiqui AR, et al. Efficacy of thyroid scintigraphy in the diagnosis of intrathoracic goiter. AJR Am J Roentgenol. 1987;148:527-529.
A 79-YEAR-OLD MAN came to our emergency department and asked that we check on a mediastinal mass that was first detected on a routine chest film 3 years earlier. The patient was asymptomatic; his medical history was unremarkable except for vitamin B12 deficiency. Physical examination revealed no abnormalities except for minor ataxia that was attributed to the lack of sufficient vitamin B12. A chest radiograph (FIGURE 1A) revealed a mass located in the upper right thorax with a slight deviation of the trachea to the left, consistent with previous x-ray findings. A computed tomography (CT) scan of the thorax (FIGURE 1B) showed a heterogeneous, multinodular mass in the anterior mediastinum with a maximal longitudinal diameter of 13.5 cm and a diagonal diameter of 9 cm. There was no obstruction or invasion of the trachea, esophagus, or mediastinal vessels.
FIGURE 1
X-ray and CT point to a diagnosis
The patient’s x-ray (A) revealed a mass in the upper right thorax with slight deviation of the trachea to the left (arrow). A CT scan of the thorax (B) revealed a heterogeneous, multinodular mass in the anterior mediastinum (asterisk). The mass did not obstruct or invade the trachea, esophagus, or mediastinal vessels.
WHAT IS YOUR DIAGNOSIS?
HOW WOULD YOU MANAGE THIS CONDITION?
Diagnosis: Retrosternal goiter
A retrosternal goiter was the most plausible diagnosis because of the patient’s advanced age, the asymptomatic behavior of the tumor, and its development over several years. The multilobular heterogenous appearance in the CT scan supported this diagnosis and made other disorders, such as thymoma and non-Hodgkin’s disease (to be discussed in a bit) very unlikely. In addition, the noninfiltrative behavior of the tumor suggested a benign mass, and CT images obtained from the neck (not shown) demonstrated that the mass originated from the right thyroid lobe without infiltrative or obstructive growth.
Benign mediastinal goiters are relatively common in adults, and the incidence increases with age.1,2 When a goiter affects adjacent structures or obstructs the trachea, common symptoms include dyspnea, wheezing, coughing, jugular vein compression, dysphagia, vocal cord palsy, phrenic nerve palsy, and Horner’s syndrome.
Differential diagnosis includes thymomas and thymic carcinomas
Masses in the anterior mediastinum comprise a variety of pathologic entities and are more likely to be malignant than masses in other mediastinal compartments.3 The most common lesions are thymomas and thymic carcinomas, lymphomas, germ cell tumors, intrathoracic thyroid or parathyroid lesions, and metastases. Up to 50% of mediastinal tumors are detected incidentally, and cause few—if any—symptoms.4,5
Thymoma and thymic carcinomas represent approximately 20% of the cases of primary anterior mediastinal masses, and can be invasive. In addition, myasthenia gravis or tumor-related syndromes are very suggestive of thymoma.6 CT or magnetic resonance imaging (MRI) studies may help to differentiate the mass in the anterior mediastinum, but histopathological analysis is required to establish a definitive diagnosis.
Lymphomas account for 10% to 20% of primary anterior mediastinal masses. While Hodgkin’s lymphoma predominantly occurs in the third and fourth decade, non-Hodgkin’s disease may affect people at any age.7,8 Most patients are symptomatic at the time of diagnosis, complaining of fever, weight loss, and night sweats. Diagnosis is suggested by a CT scan showing a lobulated mass, but confirmatory histology is necessary to guide treatment and may be accomplished by needle biopsy or lymph node excision on a different body site.
Germ cell tumors represent 15% of anterior mediastinal masses, with an even higher share in children, and include benign teratoma, seminomas, and nonseminomatous germ cell tumors.9 CT and MRI studies may help to clarify the relationship of the tumor tissue to surrounding structures. While teratomas are most likely to occur in children and young adults (and contain various amounts of tissue derived from the ectoderm, endoderm, and mesoderm), seminomas occur predominantly in young men between 20 and 40 years of age (and often have cellular heterogeneity and contain elements of embryonal malignancy).10,11 Seminomas are the most common malignant germ cell tumors, but need to be distinguished from nonseminomatous germ cell tumors; serum levels for alpha-fetoprotein and beta-human chorionic gonadotropin may help, but fine needle aspiration cytology is definitely needed.
Mediastinal cysts are common benign lesions of the mediastinum of pericardial, enteric, bronchogenic, or thymic origin, and are easily detected by CT or MRI studies. In addition, growth of parathyroid tissue can result in a retrosternal tumor, but such tumors are rarely of significant size.
Diagnosis hinges primarily on the CT scan
CT imaging is the method of choice to determine whether a mediastinal mass is thyroidal in origin and to define the extent of substernal goiter and the potential impingement on adjacent structures.12 These scans drive the need for and choice of therapy.13 An MRI of the thyroid gland may be helpful in distinguishing the thyroid from other tissue; ultrasonography is more accurate for defining thyroid anatomy in the anterior neck.
In the case of our patient, we used thyroid ultrasonography to confirm the CT findings. Further diagnostic tests included measurements of serum thyroid-stimulating hormone, triiodothyronine, and thyroxine, showing euthyroidism. Thyroid radionuclide imaging with 123-iodine was not performed in this case. While it can identify a substernal tumor as being thyroid tissue, the method can also be misleading because of impaired radioiodine uptake in some substernal goiters.14
Given our patient’s lack of pain, tenderness, or firmness in the cervical goiter and the results of his imaging studies, a fine-needle aspiration biopsy was not performed to rule out a malignant disorder like thyroid cancer.
Treatment ranges from watch and wait to surgery
Treatment of asymptomatic retrosternal goiter remains controversial. Levothyroxine suppression has a limited role in reducing the size or stopping the growth of the thyroid. Surgery is the method of choice in patients with obstructive symptoms, given the risk of progressive tracheal compression.
In the present case, we decided to watch and wait because of the patient’s age, history, and lack of any signs of obstruction of the trachea, esophagus, or mediastinal vessels. We recommended that the patient come back for a follow-up visit in 6 to 12 months.
CORRESPONDENCE: Christian S. Haas, MD, University Hospital Schleswig-Holstein–Campus Luebeck, Department of Medicine I, Ratzeburger Allee 160, 23538 Luebeck, Germany; [email protected]
A 79-YEAR-OLD MAN came to our emergency department and asked that we check on a mediastinal mass that was first detected on a routine chest film 3 years earlier. The patient was asymptomatic; his medical history was unremarkable except for vitamin B12 deficiency. Physical examination revealed no abnormalities except for minor ataxia that was attributed to the lack of sufficient vitamin B12. A chest radiograph (FIGURE 1A) revealed a mass located in the upper right thorax with a slight deviation of the trachea to the left, consistent with previous x-ray findings. A computed tomography (CT) scan of the thorax (FIGURE 1B) showed a heterogeneous, multinodular mass in the anterior mediastinum with a maximal longitudinal diameter of 13.5 cm and a diagonal diameter of 9 cm. There was no obstruction or invasion of the trachea, esophagus, or mediastinal vessels.
FIGURE 1
X-ray and CT point to a diagnosis
The patient’s x-ray (A) revealed a mass in the upper right thorax with slight deviation of the trachea to the left (arrow). A CT scan of the thorax (B) revealed a heterogeneous, multinodular mass in the anterior mediastinum (asterisk). The mass did not obstruct or invade the trachea, esophagus, or mediastinal vessels.
WHAT IS YOUR DIAGNOSIS?
HOW WOULD YOU MANAGE THIS CONDITION?
Diagnosis: Retrosternal goiter
A retrosternal goiter was the most plausible diagnosis because of the patient’s advanced age, the asymptomatic behavior of the tumor, and its development over several years. The multilobular heterogenous appearance in the CT scan supported this diagnosis and made other disorders, such as thymoma and non-Hodgkin’s disease (to be discussed in a bit) very unlikely. In addition, the noninfiltrative behavior of the tumor suggested a benign mass, and CT images obtained from the neck (not shown) demonstrated that the mass originated from the right thyroid lobe without infiltrative or obstructive growth.
Benign mediastinal goiters are relatively common in adults, and the incidence increases with age.1,2 When a goiter affects adjacent structures or obstructs the trachea, common symptoms include dyspnea, wheezing, coughing, jugular vein compression, dysphagia, vocal cord palsy, phrenic nerve palsy, and Horner’s syndrome.
Differential diagnosis includes thymomas and thymic carcinomas
Masses in the anterior mediastinum comprise a variety of pathologic entities and are more likely to be malignant than masses in other mediastinal compartments.3 The most common lesions are thymomas and thymic carcinomas, lymphomas, germ cell tumors, intrathoracic thyroid or parathyroid lesions, and metastases. Up to 50% of mediastinal tumors are detected incidentally, and cause few—if any—symptoms.4,5
Thymoma and thymic carcinomas represent approximately 20% of the cases of primary anterior mediastinal masses, and can be invasive. In addition, myasthenia gravis or tumor-related syndromes are very suggestive of thymoma.6 CT or magnetic resonance imaging (MRI) studies may help to differentiate the mass in the anterior mediastinum, but histopathological analysis is required to establish a definitive diagnosis.
Lymphomas account for 10% to 20% of primary anterior mediastinal masses. While Hodgkin’s lymphoma predominantly occurs in the third and fourth decade, non-Hodgkin’s disease may affect people at any age.7,8 Most patients are symptomatic at the time of diagnosis, complaining of fever, weight loss, and night sweats. Diagnosis is suggested by a CT scan showing a lobulated mass, but confirmatory histology is necessary to guide treatment and may be accomplished by needle biopsy or lymph node excision on a different body site.
Germ cell tumors represent 15% of anterior mediastinal masses, with an even higher share in children, and include benign teratoma, seminomas, and nonseminomatous germ cell tumors.9 CT and MRI studies may help to clarify the relationship of the tumor tissue to surrounding structures. While teratomas are most likely to occur in children and young adults (and contain various amounts of tissue derived from the ectoderm, endoderm, and mesoderm), seminomas occur predominantly in young men between 20 and 40 years of age (and often have cellular heterogeneity and contain elements of embryonal malignancy).10,11 Seminomas are the most common malignant germ cell tumors, but need to be distinguished from nonseminomatous germ cell tumors; serum levels for alpha-fetoprotein and beta-human chorionic gonadotropin may help, but fine needle aspiration cytology is definitely needed.
Mediastinal cysts are common benign lesions of the mediastinum of pericardial, enteric, bronchogenic, or thymic origin, and are easily detected by CT or MRI studies. In addition, growth of parathyroid tissue can result in a retrosternal tumor, but such tumors are rarely of significant size.
Diagnosis hinges primarily on the CT scan
CT imaging is the method of choice to determine whether a mediastinal mass is thyroidal in origin and to define the extent of substernal goiter and the potential impingement on adjacent structures.12 These scans drive the need for and choice of therapy.13 An MRI of the thyroid gland may be helpful in distinguishing the thyroid from other tissue; ultrasonography is more accurate for defining thyroid anatomy in the anterior neck.
In the case of our patient, we used thyroid ultrasonography to confirm the CT findings. Further diagnostic tests included measurements of serum thyroid-stimulating hormone, triiodothyronine, and thyroxine, showing euthyroidism. Thyroid radionuclide imaging with 123-iodine was not performed in this case. While it can identify a substernal tumor as being thyroid tissue, the method can also be misleading because of impaired radioiodine uptake in some substernal goiters.14
Given our patient’s lack of pain, tenderness, or firmness in the cervical goiter and the results of his imaging studies, a fine-needle aspiration biopsy was not performed to rule out a malignant disorder like thyroid cancer.
Treatment ranges from watch and wait to surgery
Treatment of asymptomatic retrosternal goiter remains controversial. Levothyroxine suppression has a limited role in reducing the size or stopping the growth of the thyroid. Surgery is the method of choice in patients with obstructive symptoms, given the risk of progressive tracheal compression.
In the present case, we decided to watch and wait because of the patient’s age, history, and lack of any signs of obstruction of the trachea, esophagus, or mediastinal vessels. We recommended that the patient come back for a follow-up visit in 6 to 12 months.
CORRESPONDENCE: Christian S. Haas, MD, University Hospital Schleswig-Holstein–Campus Luebeck, Department of Medicine I, Ratzeburger Allee 160, 23538 Luebeck, Germany; [email protected]
1. Singh B, Lucente FE, Shaha AR. Substernal goiter: a clinical review. Am J Otolaryngol. 1994;15:409-416.
2. Strollo DC, Rosado de Christenson ML, Jett JR. Primary mediastinal tumors. Part 1: tumors of the anterior mediastinum. Chest. 1997;112:511-522.
3. Hoffman OA, Gillespie DJ, Aughenbaugh GL, et al. Primary mediastinal neoplasms (other than thymoma). Mayo Clin Proc. 1993;68:880-891.
4. Davis RD, Jr, Oldham HN, Jr, Sabiston DC, Jr. Primary cysts and neoplasms of the mediastinum: recent changes in clinical presentation, methods of diagnosis, management, and results. Ann Thorac Surg. 1987;44:229-237.
5. den Bakker MA, Oosterhuis JW. Tumours and tumour-like conditions of the thymus other than thymoma; a practical approach. Histopathology. 2009;54:69-89.
6. Gerein AN, Srivastava SP, Burgess J. Thymoma: a ten year review. Am J Surg. 1978;136:49-53.
7. van Heerden JA, Harison EG, Jr, Bernatz PE, et al. Mediastinal malignant lymphoma. Chest. 1970;57:518-529.
8. Hoppe RT. The non-Hodgkin’s lymphomas: pathology, staging, treatment. Curr Probl Cancer. 1987;11:363-447.
9. Luna MA, Valenquela-Tamariz J. Germ cell tumors of the mediastinum: postmortem findings. Am J Clin Pathol. 1976;65:450-454.
10. Moran CA, Suster S, Koss MN. Primary germ cell tumors of the mediastinum: III. Yolk sac tumor, embryonal carcinoma, choriocarcinoma, and combined nonteratomatous germ cell tumors of the mediastinum—a clinicopathologic and immunohistochemical study of 64 cases. Cancer. 1997;80:699-707.
11. Polansky SM, Barwick KW, Ravin CE. Primary mediastinal seminoma. AJR Am J Roentgenol. 1979;132:17-21.
12. Jennings A. Evaluation of substernal goiters using computed tomography and MR imaging. Endocrinol Metab Clin North Am. 2001;30:401-414, ix.
13. Wright CD, Mathisen DJ. Mediastinal tumors: diagnosis and treatment. World J Surg. 2001;25:204-209.
14. Park HM, Tarver RD, Siddiqui AR, et al. Efficacy of thyroid scintigraphy in the diagnosis of intrathoracic goiter. AJR Am J Roentgenol. 1987;148:527-529.
1. Singh B, Lucente FE, Shaha AR. Substernal goiter: a clinical review. Am J Otolaryngol. 1994;15:409-416.
2. Strollo DC, Rosado de Christenson ML, Jett JR. Primary mediastinal tumors. Part 1: tumors of the anterior mediastinum. Chest. 1997;112:511-522.
3. Hoffman OA, Gillespie DJ, Aughenbaugh GL, et al. Primary mediastinal neoplasms (other than thymoma). Mayo Clin Proc. 1993;68:880-891.
4. Davis RD, Jr, Oldham HN, Jr, Sabiston DC, Jr. Primary cysts and neoplasms of the mediastinum: recent changes in clinical presentation, methods of diagnosis, management, and results. Ann Thorac Surg. 1987;44:229-237.
5. den Bakker MA, Oosterhuis JW. Tumours and tumour-like conditions of the thymus other than thymoma; a practical approach. Histopathology. 2009;54:69-89.
6. Gerein AN, Srivastava SP, Burgess J. Thymoma: a ten year review. Am J Surg. 1978;136:49-53.
7. van Heerden JA, Harison EG, Jr, Bernatz PE, et al. Mediastinal malignant lymphoma. Chest. 1970;57:518-529.
8. Hoppe RT. The non-Hodgkin’s lymphomas: pathology, staging, treatment. Curr Probl Cancer. 1987;11:363-447.
9. Luna MA, Valenquela-Tamariz J. Germ cell tumors of the mediastinum: postmortem findings. Am J Clin Pathol. 1976;65:450-454.
10. Moran CA, Suster S, Koss MN. Primary germ cell tumors of the mediastinum: III. Yolk sac tumor, embryonal carcinoma, choriocarcinoma, and combined nonteratomatous germ cell tumors of the mediastinum—a clinicopathologic and immunohistochemical study of 64 cases. Cancer. 1997;80:699-707.
11. Polansky SM, Barwick KW, Ravin CE. Primary mediastinal seminoma. AJR Am J Roentgenol. 1979;132:17-21.
12. Jennings A. Evaluation of substernal goiters using computed tomography and MR imaging. Endocrinol Metab Clin North Am. 2001;30:401-414, ix.
13. Wright CD, Mathisen DJ. Mediastinal tumors: diagnosis and treatment. World J Surg. 2001;25:204-209.
14. Park HM, Tarver RD, Siddiqui AR, et al. Efficacy of thyroid scintigraphy in the diagnosis of intrathoracic goiter. AJR Am J Roentgenol. 1987;148:527-529.