User login
A Year 3 Progress Report on Graduate Medical Education Expansion in the Veterans Choice Act
The VHA is the largest healthcare delivery system in the U.S. It includes 146 medical centers (VAMCs), 1,063 community-based outpatient centers (CBOCs) and various other sites of care. General Omar Bradley, the first VA Secretary, established education as one of VA’s 4 statutory missions in Policy Memorandum No.2.1 In addition to training physicians to care for active-duty service members and veterans, 38 USC §7302 directs the VA to assist in providing an adequate supply of health personnel. The 4 statutory missions of the VA are inclusive of not only developing, operating, and maintaining a health care system for veterans, but also including contingency support services as part of emergency preparedness, conducting research, and offering a program of education for health professions.
Background
Today, with few exceptions, the VHA does not act as a graduate medical education (GME) sponsoring institution. Through its Office of Academic Affiliations (OAA), the VHA develops partnerships with Liaison Committee for Medical Education (LCME)/American Osteopathic Association (AOA)-approved medical colleges/universities and with institutions that sponsor Accreditation Council for Graduate Medical Education (ACGME)/AOA-accredited residency program-sponsoring institutions. These collaborations include 144 out of 149 allopathic medical schools and all 34 osteopathic medical schools. The VHA provided training to 43,565 medical residents and 24,683 medical students through these partnerships in 2017.2 Since funding of the GME positions is not provided through the Centers for Medicare & Medicaid Services (CMS), program sponsors may use these partnerships to expand GME positions beyond their funding (but not ACGME) cap.
The gap between supply and demand of physicians continues to grow nationally.3,4 This gap is particularly significant in rural and other underserved areas. U.S. Census Bureau data show that about 5 million veterans (24%) live in rural areas.5 Compared with the urban veteran population, the rural veteran experiences higher disease prevalence and lower physical and mental quality-of-life scores.6 Addressing the problem of physician shortages is a mission-critical priority for the VHA.7
With an eye toward enhancing 2 of the 4 statutory missions of the VA and to mitigate the shortage of physicians and improve the access of veterans to VHA medical services, on August 7, 2014, the Veterans Access, Choice, and Accountability Act of 2014 (Public Law [PL] 113-146), known as the Choice Act was enacted.8 Title III, §301(b) of the Choice Act requires VHA to increase GME residency positions by:
Establishing new medical residency programs, or ensuring that already established medical residency programs have a sufficient number of residency positions, at any VHA medical facility that is: (a) experiencing a shortage of physicians and (b) located in a community that is designated as a health professional shortage area.
The legislation specifies that priority must be placed on medical occupations that experience the largest staffing shortages throughout the VHA and “programs in primary care, mental health, and any other specialty that the Secretary of the VA determines appropriate.” The Choice Act authorized the VHA to increase the number of GME residency positions by up to 1,500 over a 5-year period. In December 2016, as amended by PL 114–315, Title VI, §617(a), this authorization was extended by another 5 years for a total of 10 years and will run through 2024.9
GME Development/Distribution
To distribute these newly created GME positions as mandated by Congress, the OAA is using a system with 3 types of request for proposal (RFP) applications. These include planning, infrastructure, and position grants. This phased approach was taken with the understanding that the development of new training sites requires a properly staffed education office and dedicated faculty time. Planning and infrastructure grants provide start-up funds for smaller VAMCs, allowing them to keep facility resources focused on their clinical mission.
Planning grants (of up to $250,000 over 2 years) primarily were designed for VA facilities with no or low numbers of physician residents at the desired teaching location. Priority was given to facilities in rural and/or underserved areas as well as those developing new affiliations. Applications were reviewed by OAA staff along with peer-selected Designated Education Officers (DEOs) from VA facilities across the nation that were not applying for the grants. Awards were based on the priorities mentioned earlier, with additional credit for programs focused on 2 VHA fundamental services areas—primary care and/or mental health training. Facilities receiving planning grants were mentored by an OAA physician staff member, anticipating a 2- to 3-year time line to request positions and begin GME training.
Infrastructure grants (of up to $520,000 used over 2-3 years) were designed as bridge funds after approval of Veterans Access, Choice, and Accountability Act (VACAA) GME positions. Infrastructure grants are appropriate to sustain a local education office, develop VA faculty, purchase equipment, and make minor modifications to the clinical space in the VAMCs or CBOCs to enhance the learning environment during the period before VA supportive funds from the Veterans Equitable Resource Allocation (VERA) (similar to indirect GME funds from CMS) become available. Applications were managed the same as planning grant submissions.
Position RFPs, unlike planning and infrastructure RFPs, are available to all VAMCs. The primary purpose of the VACAA Position RFP is to fund new positions in primary care and psychiatry. Graduate medical education positions in subspecialty programs also are considered when there is documentation of critical need to improve access to these services. Applications were reviewed by OAA staff along with selected DEOs from VA facilities around the U.S. Award criteria prioritized primary care (family medicine, internal medicine, geriatrics), and mental health (psychiatry and psychiatry subspecialties). Priority also was given to positions in areas with a documented shortage of physicians and areas with high concentrations of veterans.
Current Progress
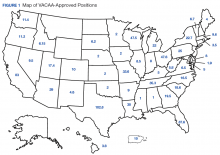
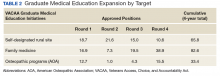
To date the OAA has offered 3 RFP cycles consisting of planning/infrastructure grants, and 4 RFP cycles for salary/benefit support for additional resident full-time equivalent (FTE) positions. Resident positions were defined as residency or fellowship FTEs that were part of an ACGME or AOA-accredited training program. Figure 1 illustrates the geographic distribution of awarded GME positions.
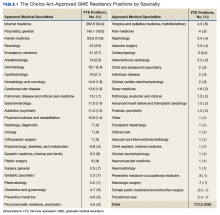
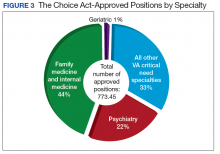
In primary care specialties (family medicine, internal medicine, and geriatrics, a total of 349.4 FTE positions have been approved (Table 1). Due to a low number of applications, only 6.3 of these positions were awarded in geriatrics. In mental health, 167.6 FTE positions have been approved, whereas in critical needs specialties (needed to support rural/underserved healthcare and improve specialty access) 256.5 FTE positions have been added.
Discussion
There are several important desired short-term outcomes from VACAA. The first is improved access to high-quality care for both rural and urban veterans. There is an emphasis on primary care and mental health because shortages in these areas across the U.S. are well established.3,4,10 Likewise, rural areas have been prioritized because often there is a disparity of care.
One area of concern is the small number of applicants in geriatrics. Even with VACAA specifically targeting geriatrics as a primary care specialty, we have only received enough applications to approve 6.3 positions over the first 3 years of the program. As the veteran and overall population in the U.S. ages, it is important to develop a medical workforce that is willing and able to address their needs.
The VACAA statute is not intended to alter medical students’ career choice but rather to provide funded positions for those choosing primary care, geriatrics, psychiatry (including psychiatric subspecialties), and experience in the VA clinical settings. The hope is that this experience will encourage practitioners to competently care for veterans after training in the VA and/or other civilian settings.
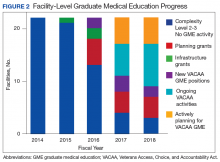
By enabling smaller VA facilities to become training sites through planning and infrastructure grants, residents have the opportunity to gain experience in more rural settings. Physicians who choose to train in rural areas are likely to spend time practicing in those areas after they complete training.15 The process of developing facilities with no GME into training sitestakes time and resources. Establishing an education office and choosing site directors and core faculty are all important steps that must be done before resident rotations begin. Resources provided through VACAA have enabled the VHA to reduce the number of VAMCs with no GME activity to just 3.
Another benefit of VACAA GME expansion is the opportunity to engage new LCME/AOA-accredited medical schools and ACGME/AOA-accredited residency-sponsoring institutions.16,17 Representatives of these institutions may have perceived a reluctance of their local VAs to develop GME affiliations in the past. This statute has enabled many VAMCs to use nontraditional training sites and modalities to overcome barriers and create new academic affiliations.
However, VACAA only provides funds for training that occurs in established VA sites of care. This can hinder the development of partnerships where other funding sources are required for non-VA rotations. Another VACAA limitation is that it does not fund undergraduate medical education as does the Armed Forces Health Professional Scholarship Program (HPSP). In addition, the primary financial relationship is between the VA and the sponsoring institution, thus VHA cannot send residents to underserved locations.
Conclusion
The VHA has a rich tradition of educating physician and other health care providers in the U.S. More than 60% of U.S. trained physicians received a portion of their training through VHA.2 Through VACAA GME expansion initiative, the 113th Congress has asked VHA to continue its important training mission “to bind up the Nations wounds” and “to care for him who shall have borne the battle.”18
Acknowledgments
In memoriam – Robert Louis Jesse MD, PhD. Dr. Jesse, the Chief of the Office of Academic Affiliations passed away on September 2, 2017, at age 64. He had an illustrious medical career as a cardiologist and served in many leadership roles including Principal Deputy Under Secretary for Health in the U.S. Department of Veterans Affairs. His expertise, visionary leadership, and friendship will be missed by all involved in the VA’s academic training mission but particularly by those of us who worked for and with him at OAA.
1. U.S. Department of Veteran Affairs. Policy Memorandum No. 2. Policy in association of veterans’ hospitals with medical schools. https://www.va.gov/oaa/Archive/PolicyMemo2.pdf. Published January 30, 1947. Accessed December 13, 2017.
2. U.S. Department of Veteran Affairs, Office of Academic Affiliations. 2017 statistics: health professions trainees. https://www .va.gov/OAA/docs/OAA_Statistics.pdf. Accessed January 8, 2018.
3. IHS, Inc. The complexities of physician supply and demand 2016 update: projections from 2014 to 2025, final report. https://www.aamc.org/download/458082/data/2016_complexities_of_supply_and_demand_projections.pdf. Published April 5, 2016. Accessed December 13, 2017.
4. Petterson SM, Liaw WR, Tran C, Bazemore AW. Estimating the residency expansion required to avoid projected primary care physician shortages by 2035. Ann Fam Med. 2015;13(2):107-114.
5. Holder KA. Veterans in rural America 2011-2015. https://www.census.gov/content/dam/Census/library/publica tions/2017/acs/acs-36.pdf. Published January 2017. Accessed January 18, 2018.
6. Weeks WB, Wallace AE, Wang S, Lee A, Kazis LE. Rural-urban disparities in health-related quality of life within disease categories of veterans. J Rural Health. 2006;22(3):204-211.
7. U.S. Government Accountability Office. GAO-18-124. VHA Physician Staffing and Recruitment. https://www.gao.gov/assets/690/687853.pdf. Published October 19, 2017. Accessed January 23, 2018.
8. Veterans Access, Choice, and Accountability Act, section 301 (b): Increase of graduate medical education residency positions, 38 USC § 74 (2014) .
9. Jeff Miller and Richard Blumenthal Veterans Health Care and Benefits Improvement Act of 2016, 38 USC §101 (2016).
10. Thomas KC, Ellis AR, Konrad TR, Holzer CE, Morrissey JP. County-level estimates of mental health professional shortage in the United States. Psychiatr Serv. 2009;60(10):1323-1328.
11. Garibaldi RA, Popkave C, Bylsma W. Career plans for trainees in internal medicine residency programs. Acad Med. 2005;80(5):507-512.
12. West CP, Dupras DM. General medicine vs subspecialty career plans among internal medicine residents. JAMA. 2012;308(21):2241-2247.
13. Stimmel B, Haddow S, Smith L. The practice of general internal medicine by subspecialists. J Urban Health. 1998;75(1):184-190.
14. Shea JA, Kleetke PR, Wozniak GD, Polsky D, Escarce JJ. Self-reported physician specialties and the primary care content of medical practice: a study of the AMA physician masterfile. American Medical Association. Med Care. 1999;37(4):333-338.
15. Rabinowitz HK, Diamond JJ, Markham FW, Paynter NP. Critical factors for designing
16. Accredited MD programs in the United States. http://lcme.org /directory/accredited-u-s-programs/. Updated December 12, 2017. Accessed January 8, 2018.
17. Osteopathic medical schools. http://www.osteopathic.org/in side-aoa/about/affiliates/Pages/osteopathic-medical-schools.aspx Published 2017. Accessed January 8, 2018.
18. Lincoln A. Second inaugural address. https://www.va.gov/opa/publications/celebrate/vamotto.pdf. Accessed January 8. 2018.
The VHA is the largest healthcare delivery system in the U.S. It includes 146 medical centers (VAMCs), 1,063 community-based outpatient centers (CBOCs) and various other sites of care. General Omar Bradley, the first VA Secretary, established education as one of VA’s 4 statutory missions in Policy Memorandum No.2.1 In addition to training physicians to care for active-duty service members and veterans, 38 USC §7302 directs the VA to assist in providing an adequate supply of health personnel. The 4 statutory missions of the VA are inclusive of not only developing, operating, and maintaining a health care system for veterans, but also including contingency support services as part of emergency preparedness, conducting research, and offering a program of education for health professions.
Background
Today, with few exceptions, the VHA does not act as a graduate medical education (GME) sponsoring institution. Through its Office of Academic Affiliations (OAA), the VHA develops partnerships with Liaison Committee for Medical Education (LCME)/American Osteopathic Association (AOA)-approved medical colleges/universities and with institutions that sponsor Accreditation Council for Graduate Medical Education (ACGME)/AOA-accredited residency program-sponsoring institutions. These collaborations include 144 out of 149 allopathic medical schools and all 34 osteopathic medical schools. The VHA provided training to 43,565 medical residents and 24,683 medical students through these partnerships in 2017.2 Since funding of the GME positions is not provided through the Centers for Medicare & Medicaid Services (CMS), program sponsors may use these partnerships to expand GME positions beyond their funding (but not ACGME) cap.
The gap between supply and demand of physicians continues to grow nationally.3,4 This gap is particularly significant in rural and other underserved areas. U.S. Census Bureau data show that about 5 million veterans (24%) live in rural areas.5 Compared with the urban veteran population, the rural veteran experiences higher disease prevalence and lower physical and mental quality-of-life scores.6 Addressing the problem of physician shortages is a mission-critical priority for the VHA.7
With an eye toward enhancing 2 of the 4 statutory missions of the VA and to mitigate the shortage of physicians and improve the access of veterans to VHA medical services, on August 7, 2014, the Veterans Access, Choice, and Accountability Act of 2014 (Public Law [PL] 113-146), known as the Choice Act was enacted.8 Title III, §301(b) of the Choice Act requires VHA to increase GME residency positions by:
Establishing new medical residency programs, or ensuring that already established medical residency programs have a sufficient number of residency positions, at any VHA medical facility that is: (a) experiencing a shortage of physicians and (b) located in a community that is designated as a health professional shortage area.
The legislation specifies that priority must be placed on medical occupations that experience the largest staffing shortages throughout the VHA and “programs in primary care, mental health, and any other specialty that the Secretary of the VA determines appropriate.” The Choice Act authorized the VHA to increase the number of GME residency positions by up to 1,500 over a 5-year period. In December 2016, as amended by PL 114–315, Title VI, §617(a), this authorization was extended by another 5 years for a total of 10 years and will run through 2024.9
GME Development/Distribution
To distribute these newly created GME positions as mandated by Congress, the OAA is using a system with 3 types of request for proposal (RFP) applications. These include planning, infrastructure, and position grants. This phased approach was taken with the understanding that the development of new training sites requires a properly staffed education office and dedicated faculty time. Planning and infrastructure grants provide start-up funds for smaller VAMCs, allowing them to keep facility resources focused on their clinical mission.
Planning grants (of up to $250,000 over 2 years) primarily were designed for VA facilities with no or low numbers of physician residents at the desired teaching location. Priority was given to facilities in rural and/or underserved areas as well as those developing new affiliations. Applications were reviewed by OAA staff along with peer-selected Designated Education Officers (DEOs) from VA facilities across the nation that were not applying for the grants. Awards were based on the priorities mentioned earlier, with additional credit for programs focused on 2 VHA fundamental services areas—primary care and/or mental health training. Facilities receiving planning grants were mentored by an OAA physician staff member, anticipating a 2- to 3-year time line to request positions and begin GME training.
Infrastructure grants (of up to $520,000 used over 2-3 years) were designed as bridge funds after approval of Veterans Access, Choice, and Accountability Act (VACAA) GME positions. Infrastructure grants are appropriate to sustain a local education office, develop VA faculty, purchase equipment, and make minor modifications to the clinical space in the VAMCs or CBOCs to enhance the learning environment during the period before VA supportive funds from the Veterans Equitable Resource Allocation (VERA) (similar to indirect GME funds from CMS) become available. Applications were managed the same as planning grant submissions.
Position RFPs, unlike planning and infrastructure RFPs, are available to all VAMCs. The primary purpose of the VACAA Position RFP is to fund new positions in primary care and psychiatry. Graduate medical education positions in subspecialty programs also are considered when there is documentation of critical need to improve access to these services. Applications were reviewed by OAA staff along with selected DEOs from VA facilities around the U.S. Award criteria prioritized primary care (family medicine, internal medicine, geriatrics), and mental health (psychiatry and psychiatry subspecialties). Priority also was given to positions in areas with a documented shortage of physicians and areas with high concentrations of veterans.
Current Progress
To date the OAA has offered 3 RFP cycles consisting of planning/infrastructure grants, and 4 RFP cycles for salary/benefit support for additional resident full-time equivalent (FTE) positions. Resident positions were defined as residency or fellowship FTEs that were part of an ACGME or AOA-accredited training program. Figure 1 illustrates the geographic distribution of awarded GME positions.
In primary care specialties (family medicine, internal medicine, and geriatrics, a total of 349.4 FTE positions have been approved (Table 1). Due to a low number of applications, only 6.3 of these positions were awarded in geriatrics. In mental health, 167.6 FTE positions have been approved, whereas in critical needs specialties (needed to support rural/underserved healthcare and improve specialty access) 256.5 FTE positions have been added.
Discussion
There are several important desired short-term outcomes from VACAA. The first is improved access to high-quality care for both rural and urban veterans. There is an emphasis on primary care and mental health because shortages in these areas across the U.S. are well established.3,4,10 Likewise, rural areas have been prioritized because often there is a disparity of care.
One area of concern is the small number of applicants in geriatrics. Even with VACAA specifically targeting geriatrics as a primary care specialty, we have only received enough applications to approve 6.3 positions over the first 3 years of the program. As the veteran and overall population in the U.S. ages, it is important to develop a medical workforce that is willing and able to address their needs.
The VACAA statute is not intended to alter medical students’ career choice but rather to provide funded positions for those choosing primary care, geriatrics, psychiatry (including psychiatric subspecialties), and experience in the VA clinical settings. The hope is that this experience will encourage practitioners to competently care for veterans after training in the VA and/or other civilian settings.
By enabling smaller VA facilities to become training sites through planning and infrastructure grants, residents have the opportunity to gain experience in more rural settings. Physicians who choose to train in rural areas are likely to spend time practicing in those areas after they complete training.15 The process of developing facilities with no GME into training sitestakes time and resources. Establishing an education office and choosing site directors and core faculty are all important steps that must be done before resident rotations begin. Resources provided through VACAA have enabled the VHA to reduce the number of VAMCs with no GME activity to just 3.
Another benefit of VACAA GME expansion is the opportunity to engage new LCME/AOA-accredited medical schools and ACGME/AOA-accredited residency-sponsoring institutions.16,17 Representatives of these institutions may have perceived a reluctance of their local VAs to develop GME affiliations in the past. This statute has enabled many VAMCs to use nontraditional training sites and modalities to overcome barriers and create new academic affiliations.
However, VACAA only provides funds for training that occurs in established VA sites of care. This can hinder the development of partnerships where other funding sources are required for non-VA rotations. Another VACAA limitation is that it does not fund undergraduate medical education as does the Armed Forces Health Professional Scholarship Program (HPSP). In addition, the primary financial relationship is between the VA and the sponsoring institution, thus VHA cannot send residents to underserved locations.
Conclusion
The VHA has a rich tradition of educating physician and other health care providers in the U.S. More than 60% of U.S. trained physicians received a portion of their training through VHA.2 Through VACAA GME expansion initiative, the 113th Congress has asked VHA to continue its important training mission “to bind up the Nations wounds” and “to care for him who shall have borne the battle.”18
Acknowledgments
In memoriam – Robert Louis Jesse MD, PhD. Dr. Jesse, the Chief of the Office of Academic Affiliations passed away on September 2, 2017, at age 64. He had an illustrious medical career as a cardiologist and served in many leadership roles including Principal Deputy Under Secretary for Health in the U.S. Department of Veterans Affairs. His expertise, visionary leadership, and friendship will be missed by all involved in the VA’s academic training mission but particularly by those of us who worked for and with him at OAA.
The VHA is the largest healthcare delivery system in the U.S. It includes 146 medical centers (VAMCs), 1,063 community-based outpatient centers (CBOCs) and various other sites of care. General Omar Bradley, the first VA Secretary, established education as one of VA’s 4 statutory missions in Policy Memorandum No.2.1 In addition to training physicians to care for active-duty service members and veterans, 38 USC §7302 directs the VA to assist in providing an adequate supply of health personnel. The 4 statutory missions of the VA are inclusive of not only developing, operating, and maintaining a health care system for veterans, but also including contingency support services as part of emergency preparedness, conducting research, and offering a program of education for health professions.
Background
Today, with few exceptions, the VHA does not act as a graduate medical education (GME) sponsoring institution. Through its Office of Academic Affiliations (OAA), the VHA develops partnerships with Liaison Committee for Medical Education (LCME)/American Osteopathic Association (AOA)-approved medical colleges/universities and with institutions that sponsor Accreditation Council for Graduate Medical Education (ACGME)/AOA-accredited residency program-sponsoring institutions. These collaborations include 144 out of 149 allopathic medical schools and all 34 osteopathic medical schools. The VHA provided training to 43,565 medical residents and 24,683 medical students through these partnerships in 2017.2 Since funding of the GME positions is not provided through the Centers for Medicare & Medicaid Services (CMS), program sponsors may use these partnerships to expand GME positions beyond their funding (but not ACGME) cap.
The gap between supply and demand of physicians continues to grow nationally.3,4 This gap is particularly significant in rural and other underserved areas. U.S. Census Bureau data show that about 5 million veterans (24%) live in rural areas.5 Compared with the urban veteran population, the rural veteran experiences higher disease prevalence and lower physical and mental quality-of-life scores.6 Addressing the problem of physician shortages is a mission-critical priority for the VHA.7
With an eye toward enhancing 2 of the 4 statutory missions of the VA and to mitigate the shortage of physicians and improve the access of veterans to VHA medical services, on August 7, 2014, the Veterans Access, Choice, and Accountability Act of 2014 (Public Law [PL] 113-146), known as the Choice Act was enacted.8 Title III, §301(b) of the Choice Act requires VHA to increase GME residency positions by:
Establishing new medical residency programs, or ensuring that already established medical residency programs have a sufficient number of residency positions, at any VHA medical facility that is: (a) experiencing a shortage of physicians and (b) located in a community that is designated as a health professional shortage area.
The legislation specifies that priority must be placed on medical occupations that experience the largest staffing shortages throughout the VHA and “programs in primary care, mental health, and any other specialty that the Secretary of the VA determines appropriate.” The Choice Act authorized the VHA to increase the number of GME residency positions by up to 1,500 over a 5-year period. In December 2016, as amended by PL 114–315, Title VI, §617(a), this authorization was extended by another 5 years for a total of 10 years and will run through 2024.9
GME Development/Distribution
To distribute these newly created GME positions as mandated by Congress, the OAA is using a system with 3 types of request for proposal (RFP) applications. These include planning, infrastructure, and position grants. This phased approach was taken with the understanding that the development of new training sites requires a properly staffed education office and dedicated faculty time. Planning and infrastructure grants provide start-up funds for smaller VAMCs, allowing them to keep facility resources focused on their clinical mission.
Planning grants (of up to $250,000 over 2 years) primarily were designed for VA facilities with no or low numbers of physician residents at the desired teaching location. Priority was given to facilities in rural and/or underserved areas as well as those developing new affiliations. Applications were reviewed by OAA staff along with peer-selected Designated Education Officers (DEOs) from VA facilities across the nation that were not applying for the grants. Awards were based on the priorities mentioned earlier, with additional credit for programs focused on 2 VHA fundamental services areas—primary care and/or mental health training. Facilities receiving planning grants were mentored by an OAA physician staff member, anticipating a 2- to 3-year time line to request positions and begin GME training.
Infrastructure grants (of up to $520,000 used over 2-3 years) were designed as bridge funds after approval of Veterans Access, Choice, and Accountability Act (VACAA) GME positions. Infrastructure grants are appropriate to sustain a local education office, develop VA faculty, purchase equipment, and make minor modifications to the clinical space in the VAMCs or CBOCs to enhance the learning environment during the period before VA supportive funds from the Veterans Equitable Resource Allocation (VERA) (similar to indirect GME funds from CMS) become available. Applications were managed the same as planning grant submissions.
Position RFPs, unlike planning and infrastructure RFPs, are available to all VAMCs. The primary purpose of the VACAA Position RFP is to fund new positions in primary care and psychiatry. Graduate medical education positions in subspecialty programs also are considered when there is documentation of critical need to improve access to these services. Applications were reviewed by OAA staff along with selected DEOs from VA facilities around the U.S. Award criteria prioritized primary care (family medicine, internal medicine, geriatrics), and mental health (psychiatry and psychiatry subspecialties). Priority also was given to positions in areas with a documented shortage of physicians and areas with high concentrations of veterans.
Current Progress
To date the OAA has offered 3 RFP cycles consisting of planning/infrastructure grants, and 4 RFP cycles for salary/benefit support for additional resident full-time equivalent (FTE) positions. Resident positions were defined as residency or fellowship FTEs that were part of an ACGME or AOA-accredited training program. Figure 1 illustrates the geographic distribution of awarded GME positions.
In primary care specialties (family medicine, internal medicine, and geriatrics, a total of 349.4 FTE positions have been approved (Table 1). Due to a low number of applications, only 6.3 of these positions were awarded in geriatrics. In mental health, 167.6 FTE positions have been approved, whereas in critical needs specialties (needed to support rural/underserved healthcare and improve specialty access) 256.5 FTE positions have been added.
Discussion
There are several important desired short-term outcomes from VACAA. The first is improved access to high-quality care for both rural and urban veterans. There is an emphasis on primary care and mental health because shortages in these areas across the U.S. are well established.3,4,10 Likewise, rural areas have been prioritized because often there is a disparity of care.
One area of concern is the small number of applicants in geriatrics. Even with VACAA specifically targeting geriatrics as a primary care specialty, we have only received enough applications to approve 6.3 positions over the first 3 years of the program. As the veteran and overall population in the U.S. ages, it is important to develop a medical workforce that is willing and able to address their needs.
The VACAA statute is not intended to alter medical students’ career choice but rather to provide funded positions for those choosing primary care, geriatrics, psychiatry (including psychiatric subspecialties), and experience in the VA clinical settings. The hope is that this experience will encourage practitioners to competently care for veterans after training in the VA and/or other civilian settings.
By enabling smaller VA facilities to become training sites through planning and infrastructure grants, residents have the opportunity to gain experience in more rural settings. Physicians who choose to train in rural areas are likely to spend time practicing in those areas after they complete training.15 The process of developing facilities with no GME into training sitestakes time and resources. Establishing an education office and choosing site directors and core faculty are all important steps that must be done before resident rotations begin. Resources provided through VACAA have enabled the VHA to reduce the number of VAMCs with no GME activity to just 3.
Another benefit of VACAA GME expansion is the opportunity to engage new LCME/AOA-accredited medical schools and ACGME/AOA-accredited residency-sponsoring institutions.16,17 Representatives of these institutions may have perceived a reluctance of their local VAs to develop GME affiliations in the past. This statute has enabled many VAMCs to use nontraditional training sites and modalities to overcome barriers and create new academic affiliations.
However, VACAA only provides funds for training that occurs in established VA sites of care. This can hinder the development of partnerships where other funding sources are required for non-VA rotations. Another VACAA limitation is that it does not fund undergraduate medical education as does the Armed Forces Health Professional Scholarship Program (HPSP). In addition, the primary financial relationship is between the VA and the sponsoring institution, thus VHA cannot send residents to underserved locations.
Conclusion
The VHA has a rich tradition of educating physician and other health care providers in the U.S. More than 60% of U.S. trained physicians received a portion of their training through VHA.2 Through VACAA GME expansion initiative, the 113th Congress has asked VHA to continue its important training mission “to bind up the Nations wounds” and “to care for him who shall have borne the battle.”18
Acknowledgments
In memoriam – Robert Louis Jesse MD, PhD. Dr. Jesse, the Chief of the Office of Academic Affiliations passed away on September 2, 2017, at age 64. He had an illustrious medical career as a cardiologist and served in many leadership roles including Principal Deputy Under Secretary for Health in the U.S. Department of Veterans Affairs. His expertise, visionary leadership, and friendship will be missed by all involved in the VA’s academic training mission but particularly by those of us who worked for and with him at OAA.
1. U.S. Department of Veteran Affairs. Policy Memorandum No. 2. Policy in association of veterans’ hospitals with medical schools. https://www.va.gov/oaa/Archive/PolicyMemo2.pdf. Published January 30, 1947. Accessed December 13, 2017.
2. U.S. Department of Veteran Affairs, Office of Academic Affiliations. 2017 statistics: health professions trainees. https://www .va.gov/OAA/docs/OAA_Statistics.pdf. Accessed January 8, 2018.
3. IHS, Inc. The complexities of physician supply and demand 2016 update: projections from 2014 to 2025, final report. https://www.aamc.org/download/458082/data/2016_complexities_of_supply_and_demand_projections.pdf. Published April 5, 2016. Accessed December 13, 2017.
4. Petterson SM, Liaw WR, Tran C, Bazemore AW. Estimating the residency expansion required to avoid projected primary care physician shortages by 2035. Ann Fam Med. 2015;13(2):107-114.
5. Holder KA. Veterans in rural America 2011-2015. https://www.census.gov/content/dam/Census/library/publica tions/2017/acs/acs-36.pdf. Published January 2017. Accessed January 18, 2018.
6. Weeks WB, Wallace AE, Wang S, Lee A, Kazis LE. Rural-urban disparities in health-related quality of life within disease categories of veterans. J Rural Health. 2006;22(3):204-211.
7. U.S. Government Accountability Office. GAO-18-124. VHA Physician Staffing and Recruitment. https://www.gao.gov/assets/690/687853.pdf. Published October 19, 2017. Accessed January 23, 2018.
8. Veterans Access, Choice, and Accountability Act, section 301 (b): Increase of graduate medical education residency positions, 38 USC § 74 (2014) .
9. Jeff Miller and Richard Blumenthal Veterans Health Care and Benefits Improvement Act of 2016, 38 USC §101 (2016).
10. Thomas KC, Ellis AR, Konrad TR, Holzer CE, Morrissey JP. County-level estimates of mental health professional shortage in the United States. Psychiatr Serv. 2009;60(10):1323-1328.
11. Garibaldi RA, Popkave C, Bylsma W. Career plans for trainees in internal medicine residency programs. Acad Med. 2005;80(5):507-512.
12. West CP, Dupras DM. General medicine vs subspecialty career plans among internal medicine residents. JAMA. 2012;308(21):2241-2247.
13. Stimmel B, Haddow S, Smith L. The practice of general internal medicine by subspecialists. J Urban Health. 1998;75(1):184-190.
14. Shea JA, Kleetke PR, Wozniak GD, Polsky D, Escarce JJ. Self-reported physician specialties and the primary care content of medical practice: a study of the AMA physician masterfile. American Medical Association. Med Care. 1999;37(4):333-338.
15. Rabinowitz HK, Diamond JJ, Markham FW, Paynter NP. Critical factors for designing
16. Accredited MD programs in the United States. http://lcme.org /directory/accredited-u-s-programs/. Updated December 12, 2017. Accessed January 8, 2018.
17. Osteopathic medical schools. http://www.osteopathic.org/in side-aoa/about/affiliates/Pages/osteopathic-medical-schools.aspx Published 2017. Accessed January 8, 2018.
18. Lincoln A. Second inaugural address. https://www.va.gov/opa/publications/celebrate/vamotto.pdf. Accessed January 8. 2018.
1. U.S. Department of Veteran Affairs. Policy Memorandum No. 2. Policy in association of veterans’ hospitals with medical schools. https://www.va.gov/oaa/Archive/PolicyMemo2.pdf. Published January 30, 1947. Accessed December 13, 2017.
2. U.S. Department of Veteran Affairs, Office of Academic Affiliations. 2017 statistics: health professions trainees. https://www .va.gov/OAA/docs/OAA_Statistics.pdf. Accessed January 8, 2018.
3. IHS, Inc. The complexities of physician supply and demand 2016 update: projections from 2014 to 2025, final report. https://www.aamc.org/download/458082/data/2016_complexities_of_supply_and_demand_projections.pdf. Published April 5, 2016. Accessed December 13, 2017.
4. Petterson SM, Liaw WR, Tran C, Bazemore AW. Estimating the residency expansion required to avoid projected primary care physician shortages by 2035. Ann Fam Med. 2015;13(2):107-114.
5. Holder KA. Veterans in rural America 2011-2015. https://www.census.gov/content/dam/Census/library/publica tions/2017/acs/acs-36.pdf. Published January 2017. Accessed January 18, 2018.
6. Weeks WB, Wallace AE, Wang S, Lee A, Kazis LE. Rural-urban disparities in health-related quality of life within disease categories of veterans. J Rural Health. 2006;22(3):204-211.
7. U.S. Government Accountability Office. GAO-18-124. VHA Physician Staffing and Recruitment. https://www.gao.gov/assets/690/687853.pdf. Published October 19, 2017. Accessed January 23, 2018.
8. Veterans Access, Choice, and Accountability Act, section 301 (b): Increase of graduate medical education residency positions, 38 USC § 74 (2014) .
9. Jeff Miller and Richard Blumenthal Veterans Health Care and Benefits Improvement Act of 2016, 38 USC §101 (2016).
10. Thomas KC, Ellis AR, Konrad TR, Holzer CE, Morrissey JP. County-level estimates of mental health professional shortage in the United States. Psychiatr Serv. 2009;60(10):1323-1328.
11. Garibaldi RA, Popkave C, Bylsma W. Career plans for trainees in internal medicine residency programs. Acad Med. 2005;80(5):507-512.
12. West CP, Dupras DM. General medicine vs subspecialty career plans among internal medicine residents. JAMA. 2012;308(21):2241-2247.
13. Stimmel B, Haddow S, Smith L. The practice of general internal medicine by subspecialists. J Urban Health. 1998;75(1):184-190.
14. Shea JA, Kleetke PR, Wozniak GD, Polsky D, Escarce JJ. Self-reported physician specialties and the primary care content of medical practice: a study of the AMA physician masterfile. American Medical Association. Med Care. 1999;37(4):333-338.
15. Rabinowitz HK, Diamond JJ, Markham FW, Paynter NP. Critical factors for designing
16. Accredited MD programs in the United States. http://lcme.org /directory/accredited-u-s-programs/. Updated December 12, 2017. Accessed January 8, 2018.
17. Osteopathic medical schools. http://www.osteopathic.org/in side-aoa/about/affiliates/Pages/osteopathic-medical-schools.aspx Published 2017. Accessed January 8, 2018.
18. Lincoln A. Second inaugural address. https://www.va.gov/opa/publications/celebrate/vamotto.pdf. Accessed January 8. 2018.
Who’s at greatest risk for delirium tremens
Ms. J, 42, was admitted to the OB-GYN service for a routine vaginal hysterectomy to treat dysfunctional uterine bleeding. In the presurgical history, she described having a few drinks daily. Shortly after a successful uncomplicated procedure, the patient became tremulous and was given several doses of lorazepam.
Two days after surgery, the patient became delirious. She complained of tactile and visual hallucinations, her level of consciousness waxed and waned, and she showed significant autonomic instability. A psychiatry consult was ordered. The consult team recommended IV fluids, IV diazepam, and haloperidol, supplemented with a multivitamin and 100 mg/d of thiamine. When the patient’s delirium resolved within 4 days, a more detailed discussion revealed a history of alcohol abuse and withdrawal seizures.
It is not uncommon for a patient to develop acute alcohol withdrawal and delirium tremens (DTs) while recovering from routine surgery. Delirium tremens remains a medical emergency, even though advances have reduced its associated mortality rates (Box).1-7
Psychiatrists who know the risk factors for DTs—also termed alcohol withdrawal delirium—can identify and protect patients who are susceptible to this life-threatening complication. We describe the clinical features of DTs, potential predisposing factors, theories behind its mechanisms, and strategies for preventing and managing DTs in patients experiencing alcohol withdrawal.
Clinical features
Disorientation and confusion are the hallmark features of DTs. Other clinical manifestations include vivid hallucinations, extreme tremulousness, autonomic hyperactivity, sweating, tachycardia, and agitation. Men experiencing DTs seem to demonstrate a greater degree of autonomic hyperactivity than women.8
Symptoms usually arise in the alcoholic patient between the third and fifth days of abstinence but have been known to occur several weeks after a patient’s last drink. Symptoms usually resolve within a few days9 but have been known to resolve within hours in some patients and to persist for several months in others.10
Differential diagnosis. Clinicians often fail to differentiate alcohol hallucinosis from DTs. Alcohol hallucinosis—which occurs in 3 to 10% of patients with severe alcohol withdrawal11 —manifests as auditory, visual, or tactile hallucinations with a clear sensorium. Patients experiencing DTs also may experience hallucinations but with confusion, disorientation, and severe autonomic hyperactivity. Unlike DTs, alcohol hallucinosis is not fatal.9
DTs also should be differentiated from:
- other causes of delirium, such as medication or infection. If the cause is identified and removed, the delirium should gradually resolve.
- Wernicke’s encephalopathy—caused by glucose exposure in the thiamine-deficient alcoholic—which is characterized by confusion, ophthalmoplegia, and ataxia.
Completing a thorough history and physical exam, talking to family members, and reviewing past medical charts are often the best ways to differentiate DTs from other conditions.
What causes DTs?
Vitamin deficiencies were initially thought to cause alcohol withdrawal.3 More recent evidence points toward multiple neuroadaptive changes in the brain associated with chronic alcohol exposure.12 Although numerous neurotransmitter systems may play a role in alcohol withdrawal, recent research has focused on glutamate13 and gamma-aminobutyric acid (GABA).14
Approximately 1.5 to 2 million Americans seek treatment for alcohol abuse or dependence each year.1 As many as 71% of these patients manifest symptoms of alcohol withdrawal.2 Of those individuals who experience alcohol withdrawal, delirium tremens (DTs) may occur in up to 5%.3-5 Utilizing these percentages, it can be estimated that as many as 50,000 to 70,000 individuals develop DTs each year in the United States alone.
Although the incidence of DTs can be assumed to be relatively low, the condition should be considered a medical emergency. Studies list mortality rates for DTs as high as 15% and as low as 2 to 3%.7,8
The brain seems to compensate for alcohol’s enhancement of GABA (inhibitory) neurons by up-regulating excitatory neurons (glutamate). Alcohol has been shown to have some effects on neurons.15 The implication is that withdrawing alcohol triggers an “excitatory state” until the brain can readjust the fine balance between excitation and inhibition, a process that takes weeks to months. Some changes may never reverse because of the neurotoxic effects of alcohol and alcohol withdrawal.
Repeated alcohol exposure and withdrawal may lead to neuroadaptive changes in the brain and to more severe withdrawal symptoms, such as DTs. Repeated alcohol withdrawal episodes can produce a kindling effect. As outlined by Becker, kindling occurs “when a weak electrical or chemical stimulus, which initially causes no overt behavioral responses, results in the appearance of behavioral effects, such as seizures, when it is administered repeatedly.”16 Thus, repeated alcohol withdrawal worsens future episodes and eventually leads to alcohol withdrawal seizures.
Whereas most of these theories apply to alcohol withdrawal, they are also compatible with the neuronal mechanisms that may underlie DTs. Alcohol withdrawal and DTs share the presence of a “hyperactive state.” Most likely, DTs is the progression to more severe or pronounced neuroadaptive changes seen in mild to moderate alcohol withdrawal. One could certainly imagine that the possible neurotoxic effects of alcohol, alcohol withdrawal, and repeated detoxifications could sensitize the CNS to the more severe symptoms seen in DTs. Infection and metabolic abnormalities may also enhance the progression. Unfortunately, why some but not all patients experiencing alcohol withdrawal progress to DTs is unknown.
Table 1
RISK FACTORS FOR DELIRIUM TREMENS
| Comorbid medical illness (with electrolyte, fluid abnormalities)* |
| History of delirium tremens* |
| Blood alcohol level >300 mg/dL on presentation* |
| Presentation after an alcohol withdrawal seizure* |
| Older age* |
| Longer history of alcohol dependence |
| Intense alcohol craving |
| Abnormal liver function |
| * Supported with studies and/or in the medical literature |
| Source: Saitz R. Introduction to alcohol withdrawal. Alcohol Health Res World 1998;22(1):5-12. |
Table 2
STRATEGIES TO PREVENT AND TREAT DELIRIUM TREMENS
| Assess risk for DTs with a thorough history, including collaborative family information and medical charts |
| Admit patients with a history of serious withdrawal symptoms or potential for inpatient detoxification (based on degree of tolerance) |
| Check complete lab values (chemistry panel, liver function tests including ALT and AST, complete blood count, blood alcohol level, GGT, and others if relevant), and correct any fluid, vitamin, or electrolyte abnormalities |
| Treat comorbid medical conditions |
| Differentiate DTs from alcohol hallucinosis, other causes of delirium, and Wernicke’s encephalopathy |
| Consider giving benzodiazepines along with low-dose neuroleptics, if appropriate, and monitor for disinhibition/ confusion and extrapyramidal symptoms, respectively |
| Place the patient in a low-stimulation environment with frequent monitoring |
Predisposing risk factors
Past withdrawal complicated by seizures or DTs is the single best predictor of future alcohol withdrawal symptoms.17 Also consider the following patients to be at elevated risk:
- any individual who presents with a blood alcohol level >300 mg/dl or after experiencing a withdrawal seizure9
- patients with comorbid medical conditions, such as electrolyte abnormalities, infection, or poorly treated cardiovascular or respiratory diseases
- older persons, who tend to be susceptible to delirium associated with hospitalization, medical illnesses such as urinary tract infections or pneumonia, or use of certain medications.18
Potential risk factors for developing DTs are summarized in Table 1.1 Although few studies have been done, clinicians can use these factors as a guide for aggressively preventing DTs in at-risk patients.
Managing and preventing DTs
Management. Drug therapy is considered crucial to quell withdrawal symptoms and reduce the risk of death.19 Patients usually are treated with one of several benzodiazepines (such as chlordiazepoxide, diazepam, oxazepam, or lorazepam) to decrease autonomic instability and reduce seizure risk during acute alcohol withdrawal. Although dosages of these medications are estimated based on drinking history, some general starting ranges are often used in clinical practice:
- chlordiazepoxide, 50 to 100 mg tid
- lorazepam, 1 to 2 mg every 4 hours
- oxazepam, 15 to 30 mg qid
- diazepam, 10 to 20 mg tid/qid.
Treating DTs often requires the use of IV benzodiazepines because of their quick onset of action and benefit for acutely agitated patients who have difficulty taking medications by mouth.
Prevention. Correcting fluid and electrolyte abnormalities may be critical in preventing DTs (Table 2). In one study of patients who died while experiencing DTs, only 25% received adequate fluid replacement, which can be as much as 6 liters per day.20 Ideally, comorbid conditions should be addressed early in presentation and before DTs develop.21
High-dose benzodiazepine therapy does not completely protect a patient from DTs or reduce its duration,22 but it may reduce mortality. A meta-analysis of prospective, placebocontrolled trials reported a risk reduction of 4.9 cases of DTs per 100 patients treated with benzodiazepines. Mortality also seems to have been reduced in patients with DTs who were treated with sedative hypnotics.9 Benzodiazepines may cause increased confusion and disinhibition, as is frequently seen when patients with dementia are treated with these agents.23
Neuroleptics such as haloperidol have been used to prevent and treat DTs, but studies of their ability to reduce mortality have produced inconsistent results. What’s more, neuroleptics can reduce the seizure threshold and produce extrapyramidal symptoms.23 Atypical antipsychotics may offer a safer alternative, although more studies are needed to evaluate whether they decrease the occurrence and severity of DTs.
In summary, a rational approach to preventing and treating DTs is to:
- manage comorbid medical illnesses, and correct fluid and electrolyte abnormalities
- place the patient in a safe, low-stimulation environment with frequent monitoring
- use benzodiazepines judiciously.
Related resources
- National Institute on Alcohol Abuse and Alcoholism.
- www.niaaa.nih.gov
- 1995;30(6):765-70 (a thorough review of benzodiazepine use in alcohol withdrawal).
Drug brand names
- Chlordiazepoxide • Librium
- Diazepam • Valium
- Haloperidol • Haldol
- Lorazepam • Ativan
- Oxazepam • Serax
Disclosure
The authors report no financial relationship with any company whose products are mentioned in this article, or with manufacturers of competing products.
1. Saitz R. Introduction to alcohol withdrawal. Alcohol Health Res World 1998;22(1):5-12.
2. Saitz R, Redmond MS, Mayo-Smith MF, et al. Individualized treatment for alcohol withdrawal. Randomized, double-blind, controlled trial. JAMA 1994;272:519-23.
3. Victor M, Adams RD. The effect of alcoholism on the nervous system. Research Publication of the Association for Research on Nervous and Mental Disorders 1953;32:526-73.
4. Victor M, Braush C. The role of abstinence in the genesis of alcoholic epilepsy. Epilepsia 1967;8:1-20.
5. Sellars EM, Kalant H. Alcohol intoxication and withdrawal. N Engl J Med 1976;294:757-62.
6. Victor M. Treatment of alcoholic intoxication and the withdrawal syndrome. Psychosomat Med 1966;28:636-50.
7. Guthrie S. The treatment of alcohol withdrawal. Pharmacotherapy 1989;9:131-43.
8. Trevisan LA, Boutrous N, Petrakis I, Krystal JH. Complications of alcohol withdrawal. Alcohol World 1998;22(1):61-66.
9. Mayo-Smith MF. Management of alcohol intoxication, overdose, and withdrawal. In: Graham AW, Schultz TK (eds). Principles of addiction medicine (2nd ed). Chevy Chase, MD: American Society of Addiction Medicine, 1998;434-41.
10. Wolf KM, Shaughnessy AF, Middleton DB. Prolonged delirium tremens requiring massive doses of medication. J Am Board Fam Pract 1993;6:502-4.
11. Platz WE, Oberlaender FA, Seidel ML. The phenomenology of perceptual hallucinations in alcohol-induced delirium tremens. Psychopathology 1995;28:247-55.
12. Littleton J. Neurochemical mechanisms underlying alcohol withdrawal. Alcohol Health Res World 1998;22(1):13-24.
13. Hoffman PL, Rabe CS, Grant KA, Valverius P, Hudspith M, Tabakoff B. Ethanol and the NMDA receptor. Alcohol 1990;7(3):229-31.
14. Morrow AL, Montpied P, Lingford-Hughes A, Paul SM. Chronic ethanol and pentobarbital administration in the rat: effects on GABAA receptor function and expression in brain. Alcohol 1990;7(3):237-44.
15. Begleiter H Kissin B (eds) The pharmacology of alcohol and alcohol dependence. New York: Oxford University Press, 1996.
16. Becker HC. Kindling in alcohol withdrawal. Alcohol World 1998;22(1):25-33.
17. Gold M, Miller N. Management of withdrawal syndromes and relapse prevention in drug and alcohol dependence. Am Fam Phys 1998;58:139-46.
18. Kraemer K, Mayo-Smith MF, Calkins R. Pharmacological management of alcohol withdrawal: a meta analysis of evidence-based practical guidelines. JAMA 1997;278:144-51.
19. Shaw GK. Detoxification: the use of benzodiazepines. Alcohol Alcohol 1995;30(6):765-70.
20. Victor M. Diagnosis and treatment of alcohol withdrawal states. Pract Gastroenteritis 1983;7(5):6-15.
21. Myrick H, Anton R. Treatment of alcohol withdrawal. Alcohol Health Res World 1998;22(1):38-43.
22. Hersh D, Kranzler HR, Meyer RE. Persistent delirium following cessation of heavy alcohol consumption: diagnostic and treatment implications. Am J Psychiatry 1997;154(6):846-51.
23. Myrick H, Anton R. Clinical management of alcohol withdrawal. CNS Spectrums 2000;5(2):22-32.
Ms. J, 42, was admitted to the OB-GYN service for a routine vaginal hysterectomy to treat dysfunctional uterine bleeding. In the presurgical history, she described having a few drinks daily. Shortly after a successful uncomplicated procedure, the patient became tremulous and was given several doses of lorazepam.
Two days after surgery, the patient became delirious. She complained of tactile and visual hallucinations, her level of consciousness waxed and waned, and she showed significant autonomic instability. A psychiatry consult was ordered. The consult team recommended IV fluids, IV diazepam, and haloperidol, supplemented with a multivitamin and 100 mg/d of thiamine. When the patient’s delirium resolved within 4 days, a more detailed discussion revealed a history of alcohol abuse and withdrawal seizures.
It is not uncommon for a patient to develop acute alcohol withdrawal and delirium tremens (DTs) while recovering from routine surgery. Delirium tremens remains a medical emergency, even though advances have reduced its associated mortality rates (Box).1-7
Psychiatrists who know the risk factors for DTs—also termed alcohol withdrawal delirium—can identify and protect patients who are susceptible to this life-threatening complication. We describe the clinical features of DTs, potential predisposing factors, theories behind its mechanisms, and strategies for preventing and managing DTs in patients experiencing alcohol withdrawal.
Clinical features
Disorientation and confusion are the hallmark features of DTs. Other clinical manifestations include vivid hallucinations, extreme tremulousness, autonomic hyperactivity, sweating, tachycardia, and agitation. Men experiencing DTs seem to demonstrate a greater degree of autonomic hyperactivity than women.8
Symptoms usually arise in the alcoholic patient between the third and fifth days of abstinence but have been known to occur several weeks after a patient’s last drink. Symptoms usually resolve within a few days9 but have been known to resolve within hours in some patients and to persist for several months in others.10
Differential diagnosis. Clinicians often fail to differentiate alcohol hallucinosis from DTs. Alcohol hallucinosis—which occurs in 3 to 10% of patients with severe alcohol withdrawal11 —manifests as auditory, visual, or tactile hallucinations with a clear sensorium. Patients experiencing DTs also may experience hallucinations but with confusion, disorientation, and severe autonomic hyperactivity. Unlike DTs, alcohol hallucinosis is not fatal.9
DTs also should be differentiated from:
- other causes of delirium, such as medication or infection. If the cause is identified and removed, the delirium should gradually resolve.
- Wernicke’s encephalopathy—caused by glucose exposure in the thiamine-deficient alcoholic—which is characterized by confusion, ophthalmoplegia, and ataxia.
Completing a thorough history and physical exam, talking to family members, and reviewing past medical charts are often the best ways to differentiate DTs from other conditions.
What causes DTs?
Vitamin deficiencies were initially thought to cause alcohol withdrawal.3 More recent evidence points toward multiple neuroadaptive changes in the brain associated with chronic alcohol exposure.12 Although numerous neurotransmitter systems may play a role in alcohol withdrawal, recent research has focused on glutamate13 and gamma-aminobutyric acid (GABA).14
Approximately 1.5 to 2 million Americans seek treatment for alcohol abuse or dependence each year.1 As many as 71% of these patients manifest symptoms of alcohol withdrawal.2 Of those individuals who experience alcohol withdrawal, delirium tremens (DTs) may occur in up to 5%.3-5 Utilizing these percentages, it can be estimated that as many as 50,000 to 70,000 individuals develop DTs each year in the United States alone.
Although the incidence of DTs can be assumed to be relatively low, the condition should be considered a medical emergency. Studies list mortality rates for DTs as high as 15% and as low as 2 to 3%.7,8
The brain seems to compensate for alcohol’s enhancement of GABA (inhibitory) neurons by up-regulating excitatory neurons (glutamate). Alcohol has been shown to have some effects on neurons.15 The implication is that withdrawing alcohol triggers an “excitatory state” until the brain can readjust the fine balance between excitation and inhibition, a process that takes weeks to months. Some changes may never reverse because of the neurotoxic effects of alcohol and alcohol withdrawal.
Repeated alcohol exposure and withdrawal may lead to neuroadaptive changes in the brain and to more severe withdrawal symptoms, such as DTs. Repeated alcohol withdrawal episodes can produce a kindling effect. As outlined by Becker, kindling occurs “when a weak electrical or chemical stimulus, which initially causes no overt behavioral responses, results in the appearance of behavioral effects, such as seizures, when it is administered repeatedly.”16 Thus, repeated alcohol withdrawal worsens future episodes and eventually leads to alcohol withdrawal seizures.
Whereas most of these theories apply to alcohol withdrawal, they are also compatible with the neuronal mechanisms that may underlie DTs. Alcohol withdrawal and DTs share the presence of a “hyperactive state.” Most likely, DTs is the progression to more severe or pronounced neuroadaptive changes seen in mild to moderate alcohol withdrawal. One could certainly imagine that the possible neurotoxic effects of alcohol, alcohol withdrawal, and repeated detoxifications could sensitize the CNS to the more severe symptoms seen in DTs. Infection and metabolic abnormalities may also enhance the progression. Unfortunately, why some but not all patients experiencing alcohol withdrawal progress to DTs is unknown.
Table 1
RISK FACTORS FOR DELIRIUM TREMENS
| Comorbid medical illness (with electrolyte, fluid abnormalities)* |
| History of delirium tremens* |
| Blood alcohol level >300 mg/dL on presentation* |
| Presentation after an alcohol withdrawal seizure* |
| Older age* |
| Longer history of alcohol dependence |
| Intense alcohol craving |
| Abnormal liver function |
| * Supported with studies and/or in the medical literature |
| Source: Saitz R. Introduction to alcohol withdrawal. Alcohol Health Res World 1998;22(1):5-12. |
Table 2
STRATEGIES TO PREVENT AND TREAT DELIRIUM TREMENS
| Assess risk for DTs with a thorough history, including collaborative family information and medical charts |
| Admit patients with a history of serious withdrawal symptoms or potential for inpatient detoxification (based on degree of tolerance) |
| Check complete lab values (chemistry panel, liver function tests including ALT and AST, complete blood count, blood alcohol level, GGT, and others if relevant), and correct any fluid, vitamin, or electrolyte abnormalities |
| Treat comorbid medical conditions |
| Differentiate DTs from alcohol hallucinosis, other causes of delirium, and Wernicke’s encephalopathy |
| Consider giving benzodiazepines along with low-dose neuroleptics, if appropriate, and monitor for disinhibition/ confusion and extrapyramidal symptoms, respectively |
| Place the patient in a low-stimulation environment with frequent monitoring |
Predisposing risk factors
Past withdrawal complicated by seizures or DTs is the single best predictor of future alcohol withdrawal symptoms.17 Also consider the following patients to be at elevated risk:
- any individual who presents with a blood alcohol level >300 mg/dl or after experiencing a withdrawal seizure9
- patients with comorbid medical conditions, such as electrolyte abnormalities, infection, or poorly treated cardiovascular or respiratory diseases
- older persons, who tend to be susceptible to delirium associated with hospitalization, medical illnesses such as urinary tract infections or pneumonia, or use of certain medications.18
Potential risk factors for developing DTs are summarized in Table 1.1 Although few studies have been done, clinicians can use these factors as a guide for aggressively preventing DTs in at-risk patients.
Managing and preventing DTs
Management. Drug therapy is considered crucial to quell withdrawal symptoms and reduce the risk of death.19 Patients usually are treated with one of several benzodiazepines (such as chlordiazepoxide, diazepam, oxazepam, or lorazepam) to decrease autonomic instability and reduce seizure risk during acute alcohol withdrawal. Although dosages of these medications are estimated based on drinking history, some general starting ranges are often used in clinical practice:
- chlordiazepoxide, 50 to 100 mg tid
- lorazepam, 1 to 2 mg every 4 hours
- oxazepam, 15 to 30 mg qid
- diazepam, 10 to 20 mg tid/qid.
Treating DTs often requires the use of IV benzodiazepines because of their quick onset of action and benefit for acutely agitated patients who have difficulty taking medications by mouth.
Prevention. Correcting fluid and electrolyte abnormalities may be critical in preventing DTs (Table 2). In one study of patients who died while experiencing DTs, only 25% received adequate fluid replacement, which can be as much as 6 liters per day.20 Ideally, comorbid conditions should be addressed early in presentation and before DTs develop.21
High-dose benzodiazepine therapy does not completely protect a patient from DTs or reduce its duration,22 but it may reduce mortality. A meta-analysis of prospective, placebocontrolled trials reported a risk reduction of 4.9 cases of DTs per 100 patients treated with benzodiazepines. Mortality also seems to have been reduced in patients with DTs who were treated with sedative hypnotics.9 Benzodiazepines may cause increased confusion and disinhibition, as is frequently seen when patients with dementia are treated with these agents.23
Neuroleptics such as haloperidol have been used to prevent and treat DTs, but studies of their ability to reduce mortality have produced inconsistent results. What’s more, neuroleptics can reduce the seizure threshold and produce extrapyramidal symptoms.23 Atypical antipsychotics may offer a safer alternative, although more studies are needed to evaluate whether they decrease the occurrence and severity of DTs.
In summary, a rational approach to preventing and treating DTs is to:
- manage comorbid medical illnesses, and correct fluid and electrolyte abnormalities
- place the patient in a safe, low-stimulation environment with frequent monitoring
- use benzodiazepines judiciously.
Related resources
- National Institute on Alcohol Abuse and Alcoholism.
- www.niaaa.nih.gov
- 1995;30(6):765-70 (a thorough review of benzodiazepine use in alcohol withdrawal).
Drug brand names
- Chlordiazepoxide • Librium
- Diazepam • Valium
- Haloperidol • Haldol
- Lorazepam • Ativan
- Oxazepam • Serax
Disclosure
The authors report no financial relationship with any company whose products are mentioned in this article, or with manufacturers of competing products.
Ms. J, 42, was admitted to the OB-GYN service for a routine vaginal hysterectomy to treat dysfunctional uterine bleeding. In the presurgical history, she described having a few drinks daily. Shortly after a successful uncomplicated procedure, the patient became tremulous and was given several doses of lorazepam.
Two days after surgery, the patient became delirious. She complained of tactile and visual hallucinations, her level of consciousness waxed and waned, and she showed significant autonomic instability. A psychiatry consult was ordered. The consult team recommended IV fluids, IV diazepam, and haloperidol, supplemented with a multivitamin and 100 mg/d of thiamine. When the patient’s delirium resolved within 4 days, a more detailed discussion revealed a history of alcohol abuse and withdrawal seizures.
It is not uncommon for a patient to develop acute alcohol withdrawal and delirium tremens (DTs) while recovering from routine surgery. Delirium tremens remains a medical emergency, even though advances have reduced its associated mortality rates (Box).1-7
Psychiatrists who know the risk factors for DTs—also termed alcohol withdrawal delirium—can identify and protect patients who are susceptible to this life-threatening complication. We describe the clinical features of DTs, potential predisposing factors, theories behind its mechanisms, and strategies for preventing and managing DTs in patients experiencing alcohol withdrawal.
Clinical features
Disorientation and confusion are the hallmark features of DTs. Other clinical manifestations include vivid hallucinations, extreme tremulousness, autonomic hyperactivity, sweating, tachycardia, and agitation. Men experiencing DTs seem to demonstrate a greater degree of autonomic hyperactivity than women.8
Symptoms usually arise in the alcoholic patient between the third and fifth days of abstinence but have been known to occur several weeks after a patient’s last drink. Symptoms usually resolve within a few days9 but have been known to resolve within hours in some patients and to persist for several months in others.10
Differential diagnosis. Clinicians often fail to differentiate alcohol hallucinosis from DTs. Alcohol hallucinosis—which occurs in 3 to 10% of patients with severe alcohol withdrawal11 —manifests as auditory, visual, or tactile hallucinations with a clear sensorium. Patients experiencing DTs also may experience hallucinations but with confusion, disorientation, and severe autonomic hyperactivity. Unlike DTs, alcohol hallucinosis is not fatal.9
DTs also should be differentiated from:
- other causes of delirium, such as medication or infection. If the cause is identified and removed, the delirium should gradually resolve.
- Wernicke’s encephalopathy—caused by glucose exposure in the thiamine-deficient alcoholic—which is characterized by confusion, ophthalmoplegia, and ataxia.
Completing a thorough history and physical exam, talking to family members, and reviewing past medical charts are often the best ways to differentiate DTs from other conditions.
What causes DTs?
Vitamin deficiencies were initially thought to cause alcohol withdrawal.3 More recent evidence points toward multiple neuroadaptive changes in the brain associated with chronic alcohol exposure.12 Although numerous neurotransmitter systems may play a role in alcohol withdrawal, recent research has focused on glutamate13 and gamma-aminobutyric acid (GABA).14
Approximately 1.5 to 2 million Americans seek treatment for alcohol abuse or dependence each year.1 As many as 71% of these patients manifest symptoms of alcohol withdrawal.2 Of those individuals who experience alcohol withdrawal, delirium tremens (DTs) may occur in up to 5%.3-5 Utilizing these percentages, it can be estimated that as many as 50,000 to 70,000 individuals develop DTs each year in the United States alone.
Although the incidence of DTs can be assumed to be relatively low, the condition should be considered a medical emergency. Studies list mortality rates for DTs as high as 15% and as low as 2 to 3%.7,8
The brain seems to compensate for alcohol’s enhancement of GABA (inhibitory) neurons by up-regulating excitatory neurons (glutamate). Alcohol has been shown to have some effects on neurons.15 The implication is that withdrawing alcohol triggers an “excitatory state” until the brain can readjust the fine balance between excitation and inhibition, a process that takes weeks to months. Some changes may never reverse because of the neurotoxic effects of alcohol and alcohol withdrawal.
Repeated alcohol exposure and withdrawal may lead to neuroadaptive changes in the brain and to more severe withdrawal symptoms, such as DTs. Repeated alcohol withdrawal episodes can produce a kindling effect. As outlined by Becker, kindling occurs “when a weak electrical or chemical stimulus, which initially causes no overt behavioral responses, results in the appearance of behavioral effects, such as seizures, when it is administered repeatedly.”16 Thus, repeated alcohol withdrawal worsens future episodes and eventually leads to alcohol withdrawal seizures.
Whereas most of these theories apply to alcohol withdrawal, they are also compatible with the neuronal mechanisms that may underlie DTs. Alcohol withdrawal and DTs share the presence of a “hyperactive state.” Most likely, DTs is the progression to more severe or pronounced neuroadaptive changes seen in mild to moderate alcohol withdrawal. One could certainly imagine that the possible neurotoxic effects of alcohol, alcohol withdrawal, and repeated detoxifications could sensitize the CNS to the more severe symptoms seen in DTs. Infection and metabolic abnormalities may also enhance the progression. Unfortunately, why some but not all patients experiencing alcohol withdrawal progress to DTs is unknown.
Table 1
RISK FACTORS FOR DELIRIUM TREMENS
| Comorbid medical illness (with electrolyte, fluid abnormalities)* |
| History of delirium tremens* |
| Blood alcohol level >300 mg/dL on presentation* |
| Presentation after an alcohol withdrawal seizure* |
| Older age* |
| Longer history of alcohol dependence |
| Intense alcohol craving |
| Abnormal liver function |
| * Supported with studies and/or in the medical literature |
| Source: Saitz R. Introduction to alcohol withdrawal. Alcohol Health Res World 1998;22(1):5-12. |
Table 2
STRATEGIES TO PREVENT AND TREAT DELIRIUM TREMENS
| Assess risk for DTs with a thorough history, including collaborative family information and medical charts |
| Admit patients with a history of serious withdrawal symptoms or potential for inpatient detoxification (based on degree of tolerance) |
| Check complete lab values (chemistry panel, liver function tests including ALT and AST, complete blood count, blood alcohol level, GGT, and others if relevant), and correct any fluid, vitamin, or electrolyte abnormalities |
| Treat comorbid medical conditions |
| Differentiate DTs from alcohol hallucinosis, other causes of delirium, and Wernicke’s encephalopathy |
| Consider giving benzodiazepines along with low-dose neuroleptics, if appropriate, and monitor for disinhibition/ confusion and extrapyramidal symptoms, respectively |
| Place the patient in a low-stimulation environment with frequent monitoring |
Predisposing risk factors
Past withdrawal complicated by seizures or DTs is the single best predictor of future alcohol withdrawal symptoms.17 Also consider the following patients to be at elevated risk:
- any individual who presents with a blood alcohol level >300 mg/dl or after experiencing a withdrawal seizure9
- patients with comorbid medical conditions, such as electrolyte abnormalities, infection, or poorly treated cardiovascular or respiratory diseases
- older persons, who tend to be susceptible to delirium associated with hospitalization, medical illnesses such as urinary tract infections or pneumonia, or use of certain medications.18
Potential risk factors for developing DTs are summarized in Table 1.1 Although few studies have been done, clinicians can use these factors as a guide for aggressively preventing DTs in at-risk patients.
Managing and preventing DTs
Management. Drug therapy is considered crucial to quell withdrawal symptoms and reduce the risk of death.19 Patients usually are treated with one of several benzodiazepines (such as chlordiazepoxide, diazepam, oxazepam, or lorazepam) to decrease autonomic instability and reduce seizure risk during acute alcohol withdrawal. Although dosages of these medications are estimated based on drinking history, some general starting ranges are often used in clinical practice:
- chlordiazepoxide, 50 to 100 mg tid
- lorazepam, 1 to 2 mg every 4 hours
- oxazepam, 15 to 30 mg qid
- diazepam, 10 to 20 mg tid/qid.
Treating DTs often requires the use of IV benzodiazepines because of their quick onset of action and benefit for acutely agitated patients who have difficulty taking medications by mouth.
Prevention. Correcting fluid and electrolyte abnormalities may be critical in preventing DTs (Table 2). In one study of patients who died while experiencing DTs, only 25% received adequate fluid replacement, which can be as much as 6 liters per day.20 Ideally, comorbid conditions should be addressed early in presentation and before DTs develop.21
High-dose benzodiazepine therapy does not completely protect a patient from DTs or reduce its duration,22 but it may reduce mortality. A meta-analysis of prospective, placebocontrolled trials reported a risk reduction of 4.9 cases of DTs per 100 patients treated with benzodiazepines. Mortality also seems to have been reduced in patients with DTs who were treated with sedative hypnotics.9 Benzodiazepines may cause increased confusion and disinhibition, as is frequently seen when patients with dementia are treated with these agents.23
Neuroleptics such as haloperidol have been used to prevent and treat DTs, but studies of their ability to reduce mortality have produced inconsistent results. What’s more, neuroleptics can reduce the seizure threshold and produce extrapyramidal symptoms.23 Atypical antipsychotics may offer a safer alternative, although more studies are needed to evaluate whether they decrease the occurrence and severity of DTs.
In summary, a rational approach to preventing and treating DTs is to:
- manage comorbid medical illnesses, and correct fluid and electrolyte abnormalities
- place the patient in a safe, low-stimulation environment with frequent monitoring
- use benzodiazepines judiciously.
Related resources
- National Institute on Alcohol Abuse and Alcoholism.
- www.niaaa.nih.gov
- 1995;30(6):765-70 (a thorough review of benzodiazepine use in alcohol withdrawal).
Drug brand names
- Chlordiazepoxide • Librium
- Diazepam • Valium
- Haloperidol • Haldol
- Lorazepam • Ativan
- Oxazepam • Serax
Disclosure
The authors report no financial relationship with any company whose products are mentioned in this article, or with manufacturers of competing products.
1. Saitz R. Introduction to alcohol withdrawal. Alcohol Health Res World 1998;22(1):5-12.
2. Saitz R, Redmond MS, Mayo-Smith MF, et al. Individualized treatment for alcohol withdrawal. Randomized, double-blind, controlled trial. JAMA 1994;272:519-23.
3. Victor M, Adams RD. The effect of alcoholism on the nervous system. Research Publication of the Association for Research on Nervous and Mental Disorders 1953;32:526-73.
4. Victor M, Braush C. The role of abstinence in the genesis of alcoholic epilepsy. Epilepsia 1967;8:1-20.
5. Sellars EM, Kalant H. Alcohol intoxication and withdrawal. N Engl J Med 1976;294:757-62.
6. Victor M. Treatment of alcoholic intoxication and the withdrawal syndrome. Psychosomat Med 1966;28:636-50.
7. Guthrie S. The treatment of alcohol withdrawal. Pharmacotherapy 1989;9:131-43.
8. Trevisan LA, Boutrous N, Petrakis I, Krystal JH. Complications of alcohol withdrawal. Alcohol World 1998;22(1):61-66.
9. Mayo-Smith MF. Management of alcohol intoxication, overdose, and withdrawal. In: Graham AW, Schultz TK (eds). Principles of addiction medicine (2nd ed). Chevy Chase, MD: American Society of Addiction Medicine, 1998;434-41.
10. Wolf KM, Shaughnessy AF, Middleton DB. Prolonged delirium tremens requiring massive doses of medication. J Am Board Fam Pract 1993;6:502-4.
11. Platz WE, Oberlaender FA, Seidel ML. The phenomenology of perceptual hallucinations in alcohol-induced delirium tremens. Psychopathology 1995;28:247-55.
12. Littleton J. Neurochemical mechanisms underlying alcohol withdrawal. Alcohol Health Res World 1998;22(1):13-24.
13. Hoffman PL, Rabe CS, Grant KA, Valverius P, Hudspith M, Tabakoff B. Ethanol and the NMDA receptor. Alcohol 1990;7(3):229-31.
14. Morrow AL, Montpied P, Lingford-Hughes A, Paul SM. Chronic ethanol and pentobarbital administration in the rat: effects on GABAA receptor function and expression in brain. Alcohol 1990;7(3):237-44.
15. Begleiter H Kissin B (eds) The pharmacology of alcohol and alcohol dependence. New York: Oxford University Press, 1996.
16. Becker HC. Kindling in alcohol withdrawal. Alcohol World 1998;22(1):25-33.
17. Gold M, Miller N. Management of withdrawal syndromes and relapse prevention in drug and alcohol dependence. Am Fam Phys 1998;58:139-46.
18. Kraemer K, Mayo-Smith MF, Calkins R. Pharmacological management of alcohol withdrawal: a meta analysis of evidence-based practical guidelines. JAMA 1997;278:144-51.
19. Shaw GK. Detoxification: the use of benzodiazepines. Alcohol Alcohol 1995;30(6):765-70.
20. Victor M. Diagnosis and treatment of alcohol withdrawal states. Pract Gastroenteritis 1983;7(5):6-15.
21. Myrick H, Anton R. Treatment of alcohol withdrawal. Alcohol Health Res World 1998;22(1):38-43.
22. Hersh D, Kranzler HR, Meyer RE. Persistent delirium following cessation of heavy alcohol consumption: diagnostic and treatment implications. Am J Psychiatry 1997;154(6):846-51.
23. Myrick H, Anton R. Clinical management of alcohol withdrawal. CNS Spectrums 2000;5(2):22-32.
1. Saitz R. Introduction to alcohol withdrawal. Alcohol Health Res World 1998;22(1):5-12.
2. Saitz R, Redmond MS, Mayo-Smith MF, et al. Individualized treatment for alcohol withdrawal. Randomized, double-blind, controlled trial. JAMA 1994;272:519-23.
3. Victor M, Adams RD. The effect of alcoholism on the nervous system. Research Publication of the Association for Research on Nervous and Mental Disorders 1953;32:526-73.
4. Victor M, Braush C. The role of abstinence in the genesis of alcoholic epilepsy. Epilepsia 1967;8:1-20.
5. Sellars EM, Kalant H. Alcohol intoxication and withdrawal. N Engl J Med 1976;294:757-62.
6. Victor M. Treatment of alcoholic intoxication and the withdrawal syndrome. Psychosomat Med 1966;28:636-50.
7. Guthrie S. The treatment of alcohol withdrawal. Pharmacotherapy 1989;9:131-43.
8. Trevisan LA, Boutrous N, Petrakis I, Krystal JH. Complications of alcohol withdrawal. Alcohol World 1998;22(1):61-66.
9. Mayo-Smith MF. Management of alcohol intoxication, overdose, and withdrawal. In: Graham AW, Schultz TK (eds). Principles of addiction medicine (2nd ed). Chevy Chase, MD: American Society of Addiction Medicine, 1998;434-41.
10. Wolf KM, Shaughnessy AF, Middleton DB. Prolonged delirium tremens requiring massive doses of medication. J Am Board Fam Pract 1993;6:502-4.
11. Platz WE, Oberlaender FA, Seidel ML. The phenomenology of perceptual hallucinations in alcohol-induced delirium tremens. Psychopathology 1995;28:247-55.
12. Littleton J. Neurochemical mechanisms underlying alcohol withdrawal. Alcohol Health Res World 1998;22(1):13-24.
13. Hoffman PL, Rabe CS, Grant KA, Valverius P, Hudspith M, Tabakoff B. Ethanol and the NMDA receptor. Alcohol 1990;7(3):229-31.
14. Morrow AL, Montpied P, Lingford-Hughes A, Paul SM. Chronic ethanol and pentobarbital administration in the rat: effects on GABAA receptor function and expression in brain. Alcohol 1990;7(3):237-44.
15. Begleiter H Kissin B (eds) The pharmacology of alcohol and alcohol dependence. New York: Oxford University Press, 1996.
16. Becker HC. Kindling in alcohol withdrawal. Alcohol World 1998;22(1):25-33.
17. Gold M, Miller N. Management of withdrawal syndromes and relapse prevention in drug and alcohol dependence. Am Fam Phys 1998;58:139-46.
18. Kraemer K, Mayo-Smith MF, Calkins R. Pharmacological management of alcohol withdrawal: a meta analysis of evidence-based practical guidelines. JAMA 1997;278:144-51.
19. Shaw GK. Detoxification: the use of benzodiazepines. Alcohol Alcohol 1995;30(6):765-70.
20. Victor M. Diagnosis and treatment of alcohol withdrawal states. Pract Gastroenteritis 1983;7(5):6-15.
21. Myrick H, Anton R. Treatment of alcohol withdrawal. Alcohol Health Res World 1998;22(1):38-43.
22. Hersh D, Kranzler HR, Meyer RE. Persistent delirium following cessation of heavy alcohol consumption: diagnostic and treatment implications. Am J Psychiatry 1997;154(6):846-51.
23. Myrick H, Anton R. Clinical management of alcohol withdrawal. CNS Spectrums 2000;5(2):22-32.