User login
Firm, non-tender mass in right breast • worsening, nonproductive cough • pleuritic pain • Dx?
THE CASE
A 44-year-old woman with a 15-year history of type 2 diabetes sought care for a firm, non-tender mass in the medial lower quadrant of her right breast. She hadn’t experienced any skin changes or axillary lymphadenopathy. The patient had immigrated to California from Afghanistan 22 years earlier, at which time she was briefly married to an Afghan man suffering from a chronic cough.
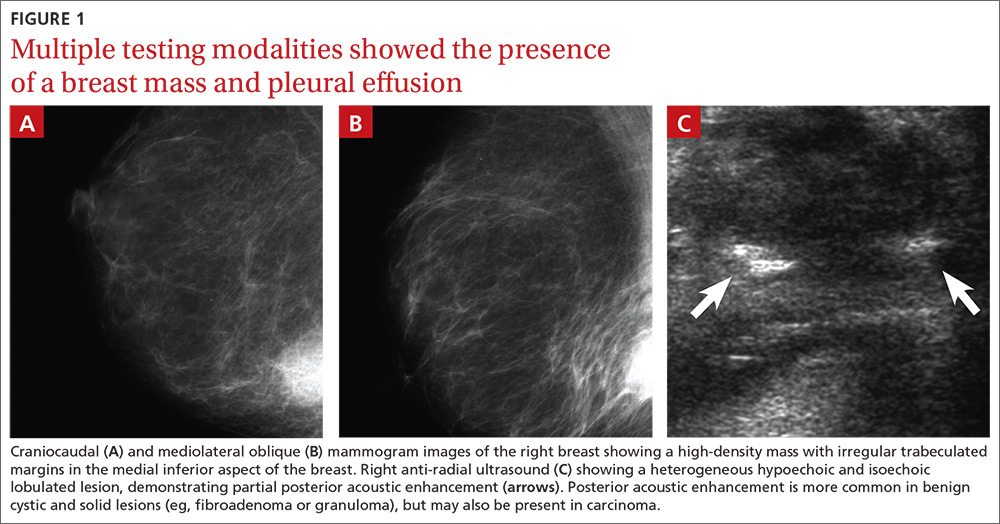
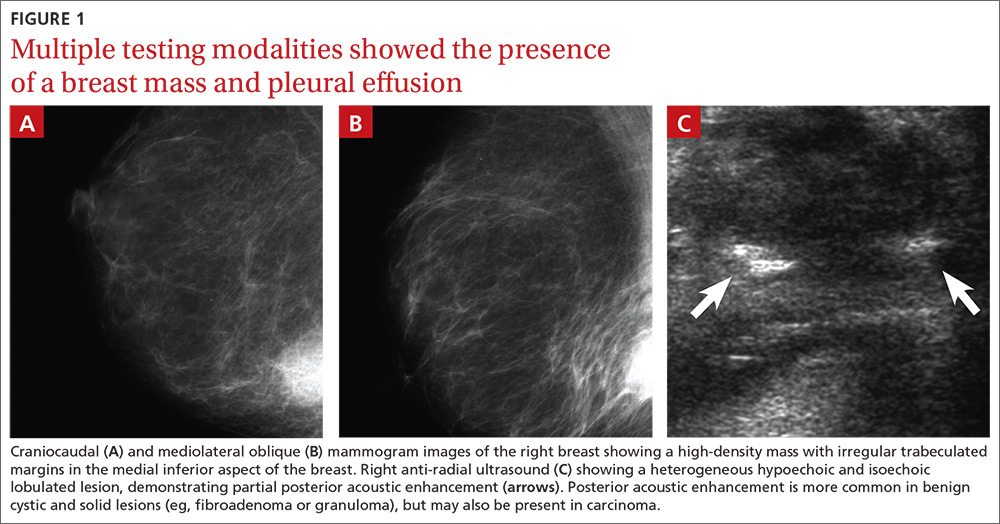
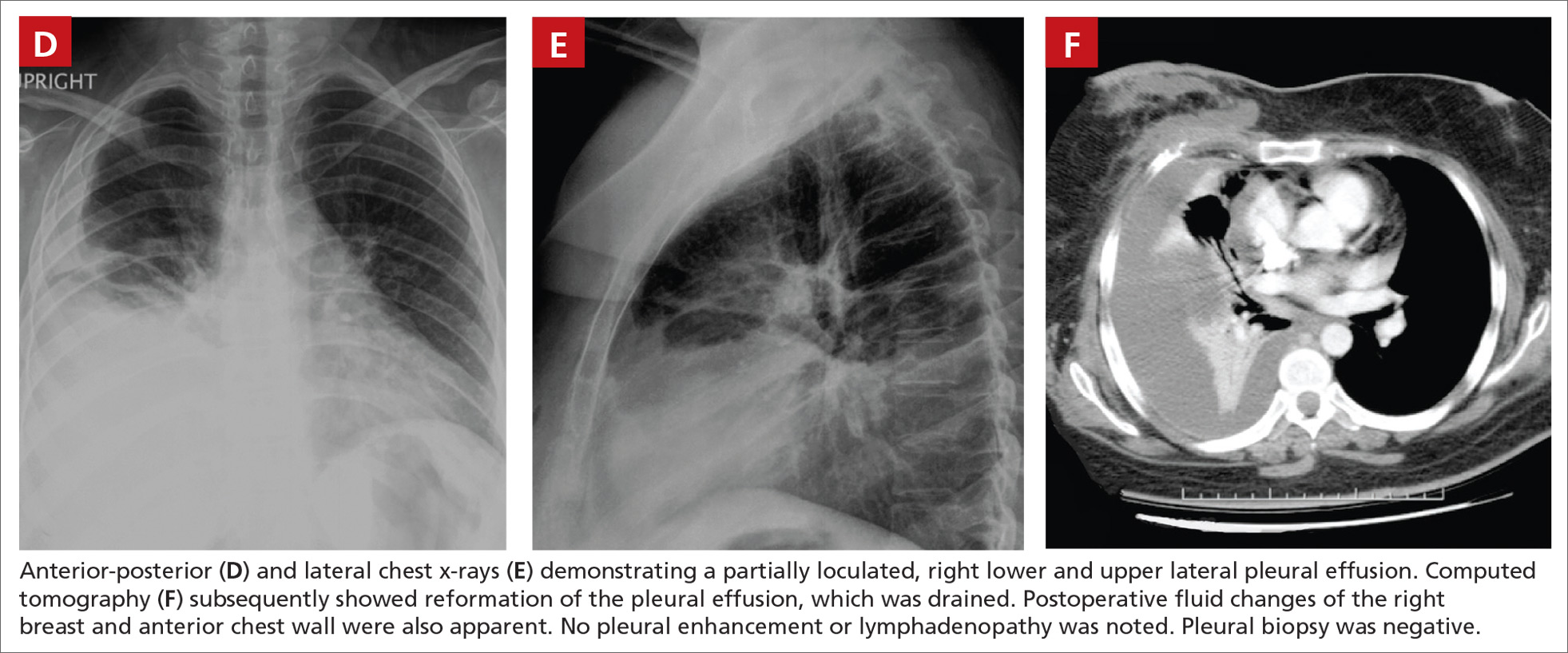
Mammography revealed a 3.5 x 4 x 4 cm lesion at the chest wall, which was highly suspicious for carcinoma (FIGURES 1A AND 1B). Sonography showed a heterogenous hypoechoic and isoechoic mass with posterior acoustic enhancement (FIGURE 1C). An excisional biopsy was performed.
One week postoperatively, the patient presented to the emergency department for a worsening nonproductive cough that intensified when supine, and was associated with subscapular pleuritic pain. She denied fever or weight loss. Biopsy results were pending.
THE DIAGNOSIS
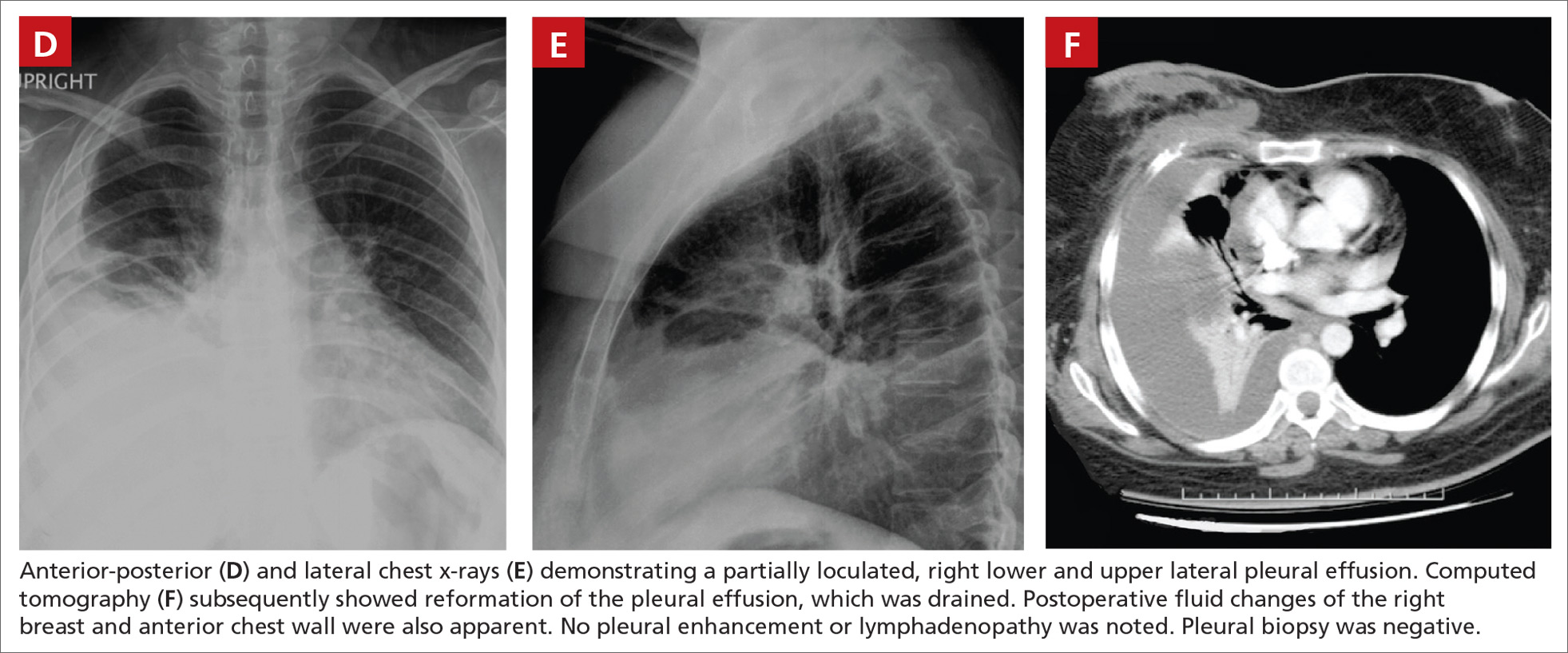
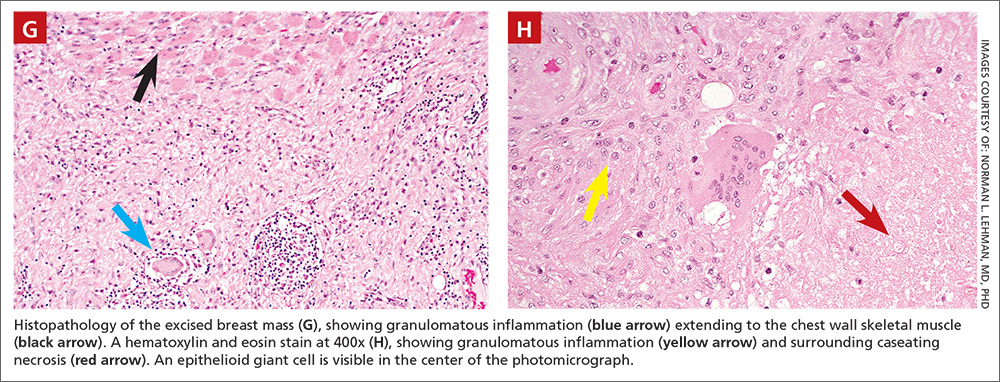
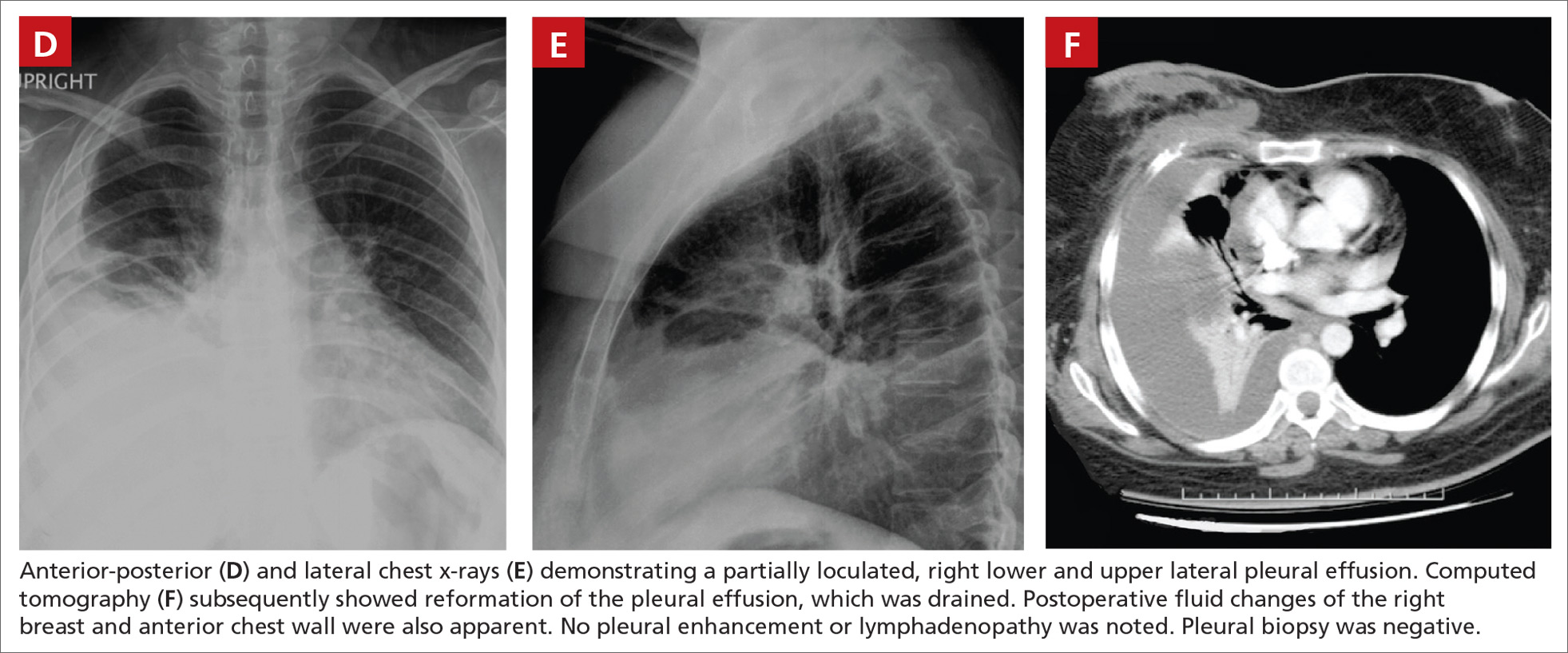
Chest x-rays revealed a large right pleural effusion that was presumed to be malignant (FIGURES 1D AND 1E). Thoracentesis yielded 1.5 liters of tea-colored exudate containing 2800 nucleated cells/mL—63% lymphocytes and 37% neutrophils—and a pleural fluid to serum protein ratio >0.5. Adenosine deaminase was <1 U/L. Fluid Gram stain, acid-fast bacillus (AFB) fluorescent antibody testing, AFB cultures, and cytology were negative. Computed tomography (CT) subsequently demonstrated recurrent effusion without hilar or mediastinal lymphadenopathy or pleural enhancement (FIGURE 1F).
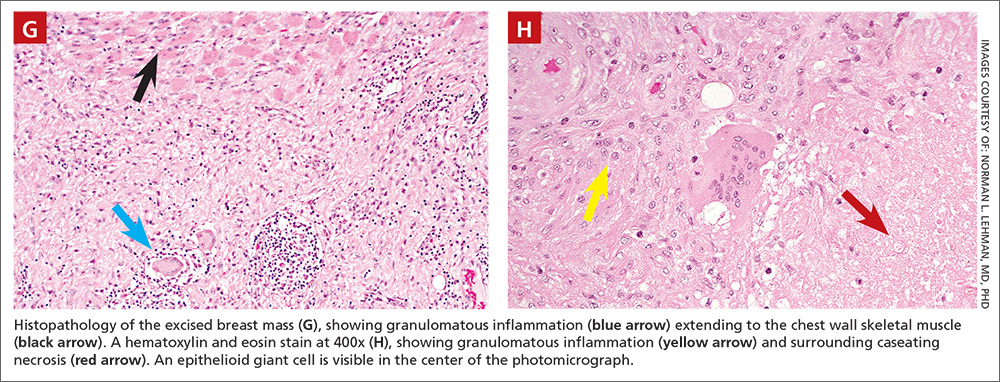
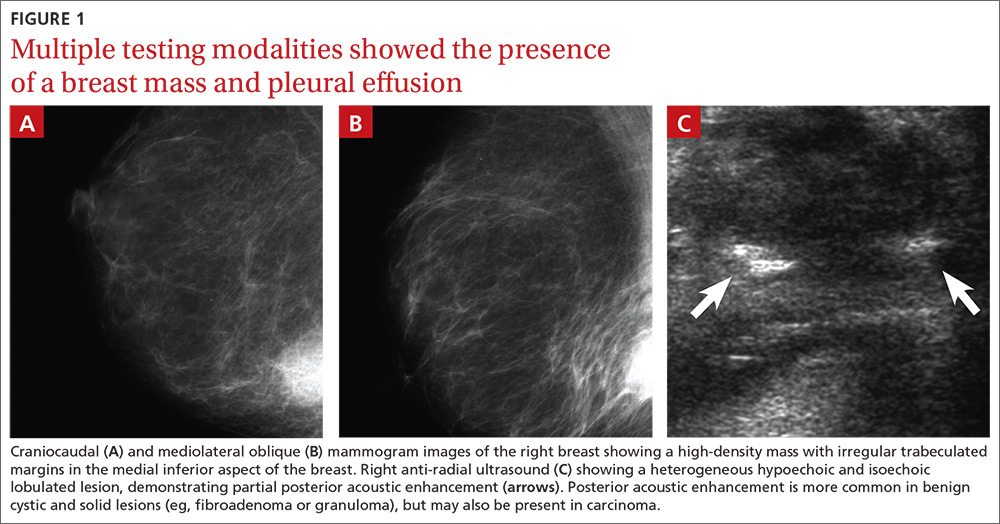
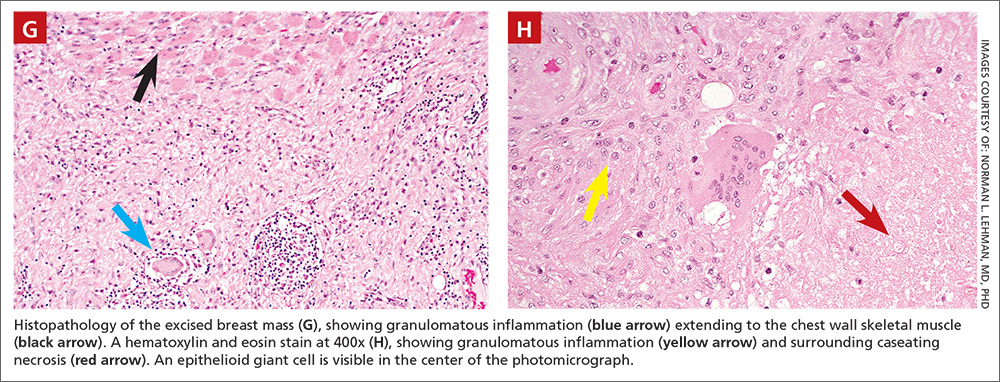
Histologically, the breast mass showed caseating granulomatous inflammation (FIGURES 1G AND 1H). An AFB stain was negative. Polymerase chain reaction (PCR) performed on DNA extracted from the formalin-fixed, paraffin-embedded biopsy material was positive for Mycobacterium tuberculosis.1 A CT-guided pleural biopsy showed only normal tissue. A follow-up tuberculin skin test (purified protein derivative [PPD]) yielded a 10-mm indurated reaction.
DISCUSSION
Granulomatous lesions, such as foreign body granuloma, idiopathic granulomatous mastitis (IGM), and sarcoidosis can mimic breast carcinoma.2,3 IGM is associated with elevated prolactin (eg, pregnancy or oral contraceptive use) and is usually subareolar.2 Infection, however, is also commonly subareolar. Sarcoidosis rarely exhibits unilateral pleural effusion and usually manifests with bilateral interstitial lung disease, hilar lymphadenopathy, and non-necrotizing granulomas.3,4
M tuberculosis and other granulomatous infections may also feign breast cancer.5-13 Breast TB, which is highly uncommon in the developed world, often demonstrates imaging similar to that which was seen in this case. Breast TB may appear nodular with ill-defined contours. Masses are sometimes attached to the chest wall and usually lack microcalcifications on mammography; they are also typically hypoechoic and heterogenous on ultrasound, often showing posterior enhancement.5,7,8 Like other breast infections, tuberculosis may show cutaneous sinus tract formation, which is seen in about one-third of patients.6,7 Alternatively, it may manifest as a diffuse mastitis with skin thickening and axillary lymphadenopathy.8
Primary breast TB without chest disease comprises up to 86% of mammary tuberculosis.6,7 Infection may occur via contamination of the skin or nipple.5-7 Lactation, pregnancy, and other causes of immunosuppression (especially human immunodeficiency virus) have been associated with an increased risk of breast infection.6-8 This patient was at risk for immunosuppression from longstanding diabetes.14
Many patients from TB-endemic areas have received the bacille Calmette-Guerin (BCG) vaccine and may exhibit equivocal or false-positive PPD results. Because interferon-gamma release assay TB blood tests (eg, QuantiFERON-TB Gold or T-SPOT.TB) are not affected by BCG, they are not associated with false-positive repeat testing results.15
Biopsy is necessary to rule out malignancy and diagnose breast TB
A pleural fluid to serum protein ratio >0.5 is consistent with infection, but also with sarcoidosis or malignancy.3,16 Elevated pleural fluid adenosine deaminase (>40 U/L) is sensitive, albeit nonspecific, for the presence of TB microorganisms. If a lymphocyte-dominant exudate is also present, however, its reliability greatly increases.16,17 Increased pleural fluid interferon-gamma is also sensitive and specific for TB pleurisy.18 Culture, along with drug sensitivity testing, should be performed on all unexplained pleural effusions.
A biopsy is often required to diagnose breast TB and should be performed on all suspicious lesions to exclude malignancy.5-7,9 AFB stains and cultures of aspirate fluids or tissue are often negative.7,9 PCR or other nucleic acid amplification tests of sputum, body fluids, or biopsy material may be positive in culture-negative cases and can rapidly confirm M tuberculosis infection.17,19 No testing modality offers 100% sensitivity or specificity; therefore, an additional confirmatory test is desirable.
Possible routes of transmission include activation of latent pulmonary tuberculosis and direct, lymphatic, or hematologic extension to the chest wall and breast.5-7 In this patient, we believe that activation of a latent breast granuloma may have resulted in a secondary or “sympathetic” pleural effusion, possibly triggered by surgical manipulation. This is compatible with her negative pleural adenosine deaminase result, negative culture, absence of pulmonary parenchymal disease, and negative pleural biopsy. Although we conducted a PubMed search, reviewing material as far back as 1966, we were unable to find a previous case of apparent sympathetic effusion associated with breast TB.
Our patient was treated with daily oral isoniazid, rifabutin, pyrazinamide, and ethambutol for 2 months, followed by isoniazid and rifabutin for 4 months. She has been disease-free for over 10 years.
THE TAKEAWAY
We describe a rare case of breast TB mimicking carcinoma that was associated with unilateral pleural effusion in a woman who had emigrated from Afghanistan. Patients at particular risk for breast TB include immigrants from endemic regions—especially parous females,6,7 those with a history of TB contacts, and those who are immunosuppressed.8 This case emphasizes the need for increased awareness of extrapulmonary TB by physicians in developed countries.
ACKNOWLEDGEMENTS
The authors thank Drs. Margie Scott, Harpreet Dhillon, Samir Vora, Todd Williams, Jeffrey Hawley, and Mr. Sergio Landeros. This report is dedicated to the memory of our friend and colleague in medicine, Dr. Jeanie Care Gillinta.
1. Bayer-Garner IB, Cox MD, Scott MA, et al. Mycobacteria other than Mycobacterium tuberculosis are not present in erythema induratum/nodular vasculitis: a case series and literature review of the clinical and histologic findings. J Cutan Pathol. 2005;32:220-226.
2. Verfaillie G, Breucq C, Sacre R, et al. Granulomatous lobular mastitis: a rare chronic inflammatory disease of the breast which can mimic breast carcinoma. Acta Chir Belg. 2006;106:222-224.
3. Fiorucci F, Conti V, Lucantoni G, et al. Sarcoidosis of the breast: a rare case report and a review. Eur Rev Med Pharmacol Sci. 2006;10:47-50.
4. Huggins JT, Doelken P, Sahn SA, et al. Pleural effusions in a series of 181 outpatients with sarcoidosis. Chest. 2006;129:1599-1604.
5. Zandrino F, Monetti F, Gandolfo N. Primary tuberculosis of the breast. A case report. Acta Radiol. 2000;41:61-63.
6. Khanna R, Prasanna GV, Gupta P, et al. Mammary tuberculosis: report on 52 cases. Postgrad Med J. 2002;78:422-424.
7. Harris SH, Khan MA, Khan R, et al. Mammary tuberculosis: analysis of thirty-eight patients. ANZ J Surg. 2006;76:234-237.
8. Meerkotter D, Spiegel K, Page-Shipp LS. Imaging of tuberculosis of the breast: 21 cases and a review of the literature. J Med Imaging Radiat Oncol. 2011;55:453-460.
9. Khodabakhshi B, Mehravar F. Breast tuberculosis in northeast Iran: review of 22 cases. BMC Womens Health. 2014;14:72.
10. Osborne BM. Granulomatous mastitis caused by histoplasma and mimicking inflammatory breast carcinoma. Hum Pathol. 1989;20:47-52.
11. Bocian JJ, Fahmy RN, Michas CA. A rare case of ‘coccidioidoma’ of the breast. Arch Pathol Lab Med. 1991;115:1064-1067.
12. Haddow LJ, Sahid F, Moosa MY. Cryptococcal breast abscess in an HIV-positive patient: arguments for reviewing the definition of immune reconstitution inflammatory syndrome. J Infect. 2008;57:82-84.
13. Lefkowitz M, Wear DJ. Cat-scratch disease masquerading as a solitary tumor of the breast. Arch Pathol Lab Med. 1989;113:473-475.
14. Ponce-De-Leon A, Garcia-Garcia Md Mde L, Garcia-Sancho MC, et al. Tuberculosis and diabetes in southern Mexico. Diabetes Care. 2004;27:1584-1590.
15. Mazurek GH, LoBue PA, Daley CL, et al. Comparison of a whole-blood interferon gamma assay with tuberculin skin testing for detecting latent Mycobacterium tuberculosis infection. JAMA. 2001;286:1740-1747.
16. Porcel JM, Light RW. Diagnostic approach to pleural effusion in adults. Am Fam Physician. 2006;73:1211-1220.
17. Burgess LJ, Maritz FJ, Le Roux I, et al. Combined use of pleural adenosine deaminase with lymphocyte/neutrophil ratio. Increased specificity for the diagnosis of tuberculous pleuritis. Chest. 1996;109:414-419.
18. Klimiuk J, Krenke R, Safianowska A, et al. Diagnostic performance of different pleural fluid biomarkers in tuberculous pleurisy. Adv Exp Med Biol. 2015;852:21-30.
19. Gopi A, Madhavan SM, Sharma SK, et al. Diagnosis and treatment of tuberculous pleural effusion in 2006. Chest. 2007;131:880-889.
THE CASE
A 44-year-old woman with a 15-year history of type 2 diabetes sought care for a firm, non-tender mass in the medial lower quadrant of her right breast. She hadn’t experienced any skin changes or axillary lymphadenopathy. The patient had immigrated to California from Afghanistan 22 years earlier, at which time she was briefly married to an Afghan man suffering from a chronic cough.
Mammography revealed a 3.5 x 4 x 4 cm lesion at the chest wall, which was highly suspicious for carcinoma (FIGURES 1A AND 1B). Sonography showed a heterogenous hypoechoic and isoechoic mass with posterior acoustic enhancement (FIGURE 1C). An excisional biopsy was performed.
One week postoperatively, the patient presented to the emergency department for a worsening nonproductive cough that intensified when supine, and was associated with subscapular pleuritic pain. She denied fever or weight loss. Biopsy results were pending.
THE DIAGNOSIS
Chest x-rays revealed a large right pleural effusion that was presumed to be malignant (FIGURES 1D AND 1E). Thoracentesis yielded 1.5 liters of tea-colored exudate containing 2800 nucleated cells/mL—63% lymphocytes and 37% neutrophils—and a pleural fluid to serum protein ratio >0.5. Adenosine deaminase was <1 U/L. Fluid Gram stain, acid-fast bacillus (AFB) fluorescent antibody testing, AFB cultures, and cytology were negative. Computed tomography (CT) subsequently demonstrated recurrent effusion without hilar or mediastinal lymphadenopathy or pleural enhancement (FIGURE 1F).
Histologically, the breast mass showed caseating granulomatous inflammation (FIGURES 1G AND 1H). An AFB stain was negative. Polymerase chain reaction (PCR) performed on DNA extracted from the formalin-fixed, paraffin-embedded biopsy material was positive for Mycobacterium tuberculosis.1 A CT-guided pleural biopsy showed only normal tissue. A follow-up tuberculin skin test (purified protein derivative [PPD]) yielded a 10-mm indurated reaction.
DISCUSSION
Granulomatous lesions, such as foreign body granuloma, idiopathic granulomatous mastitis (IGM), and sarcoidosis can mimic breast carcinoma.2,3 IGM is associated with elevated prolactin (eg, pregnancy or oral contraceptive use) and is usually subareolar.2 Infection, however, is also commonly subareolar. Sarcoidosis rarely exhibits unilateral pleural effusion and usually manifests with bilateral interstitial lung disease, hilar lymphadenopathy, and non-necrotizing granulomas.3,4
M tuberculosis and other granulomatous infections may also feign breast cancer.5-13 Breast TB, which is highly uncommon in the developed world, often demonstrates imaging similar to that which was seen in this case. Breast TB may appear nodular with ill-defined contours. Masses are sometimes attached to the chest wall and usually lack microcalcifications on mammography; they are also typically hypoechoic and heterogenous on ultrasound, often showing posterior enhancement.5,7,8 Like other breast infections, tuberculosis may show cutaneous sinus tract formation, which is seen in about one-third of patients.6,7 Alternatively, it may manifest as a diffuse mastitis with skin thickening and axillary lymphadenopathy.8
Primary breast TB without chest disease comprises up to 86% of mammary tuberculosis.6,7 Infection may occur via contamination of the skin or nipple.5-7 Lactation, pregnancy, and other causes of immunosuppression (especially human immunodeficiency virus) have been associated with an increased risk of breast infection.6-8 This patient was at risk for immunosuppression from longstanding diabetes.14
Many patients from TB-endemic areas have received the bacille Calmette-Guerin (BCG) vaccine and may exhibit equivocal or false-positive PPD results. Because interferon-gamma release assay TB blood tests (eg, QuantiFERON-TB Gold or T-SPOT.TB) are not affected by BCG, they are not associated with false-positive repeat testing results.15
Biopsy is necessary to rule out malignancy and diagnose breast TB
A pleural fluid to serum protein ratio >0.5 is consistent with infection, but also with sarcoidosis or malignancy.3,16 Elevated pleural fluid adenosine deaminase (>40 U/L) is sensitive, albeit nonspecific, for the presence of TB microorganisms. If a lymphocyte-dominant exudate is also present, however, its reliability greatly increases.16,17 Increased pleural fluid interferon-gamma is also sensitive and specific for TB pleurisy.18 Culture, along with drug sensitivity testing, should be performed on all unexplained pleural effusions.
A biopsy is often required to diagnose breast TB and should be performed on all suspicious lesions to exclude malignancy.5-7,9 AFB stains and cultures of aspirate fluids or tissue are often negative.7,9 PCR or other nucleic acid amplification tests of sputum, body fluids, or biopsy material may be positive in culture-negative cases and can rapidly confirm M tuberculosis infection.17,19 No testing modality offers 100% sensitivity or specificity; therefore, an additional confirmatory test is desirable.
Possible routes of transmission include activation of latent pulmonary tuberculosis and direct, lymphatic, or hematologic extension to the chest wall and breast.5-7 In this patient, we believe that activation of a latent breast granuloma may have resulted in a secondary or “sympathetic” pleural effusion, possibly triggered by surgical manipulation. This is compatible with her negative pleural adenosine deaminase result, negative culture, absence of pulmonary parenchymal disease, and negative pleural biopsy. Although we conducted a PubMed search, reviewing material as far back as 1966, we were unable to find a previous case of apparent sympathetic effusion associated with breast TB.
Our patient was treated with daily oral isoniazid, rifabutin, pyrazinamide, and ethambutol for 2 months, followed by isoniazid and rifabutin for 4 months. She has been disease-free for over 10 years.
THE TAKEAWAY
We describe a rare case of breast TB mimicking carcinoma that was associated with unilateral pleural effusion in a woman who had emigrated from Afghanistan. Patients at particular risk for breast TB include immigrants from endemic regions—especially parous females,6,7 those with a history of TB contacts, and those who are immunosuppressed.8 This case emphasizes the need for increased awareness of extrapulmonary TB by physicians in developed countries.
ACKNOWLEDGEMENTS
The authors thank Drs. Margie Scott, Harpreet Dhillon, Samir Vora, Todd Williams, Jeffrey Hawley, and Mr. Sergio Landeros. This report is dedicated to the memory of our friend and colleague in medicine, Dr. Jeanie Care Gillinta.
THE CASE
A 44-year-old woman with a 15-year history of type 2 diabetes sought care for a firm, non-tender mass in the medial lower quadrant of her right breast. She hadn’t experienced any skin changes or axillary lymphadenopathy. The patient had immigrated to California from Afghanistan 22 years earlier, at which time she was briefly married to an Afghan man suffering from a chronic cough.
Mammography revealed a 3.5 x 4 x 4 cm lesion at the chest wall, which was highly suspicious for carcinoma (FIGURES 1A AND 1B). Sonography showed a heterogenous hypoechoic and isoechoic mass with posterior acoustic enhancement (FIGURE 1C). An excisional biopsy was performed.
One week postoperatively, the patient presented to the emergency department for a worsening nonproductive cough that intensified when supine, and was associated with subscapular pleuritic pain. She denied fever or weight loss. Biopsy results were pending.
THE DIAGNOSIS
Chest x-rays revealed a large right pleural effusion that was presumed to be malignant (FIGURES 1D AND 1E). Thoracentesis yielded 1.5 liters of tea-colored exudate containing 2800 nucleated cells/mL—63% lymphocytes and 37% neutrophils—and a pleural fluid to serum protein ratio >0.5. Adenosine deaminase was <1 U/L. Fluid Gram stain, acid-fast bacillus (AFB) fluorescent antibody testing, AFB cultures, and cytology were negative. Computed tomography (CT) subsequently demonstrated recurrent effusion without hilar or mediastinal lymphadenopathy or pleural enhancement (FIGURE 1F).
Histologically, the breast mass showed caseating granulomatous inflammation (FIGURES 1G AND 1H). An AFB stain was negative. Polymerase chain reaction (PCR) performed on DNA extracted from the formalin-fixed, paraffin-embedded biopsy material was positive for Mycobacterium tuberculosis.1 A CT-guided pleural biopsy showed only normal tissue. A follow-up tuberculin skin test (purified protein derivative [PPD]) yielded a 10-mm indurated reaction.
DISCUSSION
Granulomatous lesions, such as foreign body granuloma, idiopathic granulomatous mastitis (IGM), and sarcoidosis can mimic breast carcinoma.2,3 IGM is associated with elevated prolactin (eg, pregnancy or oral contraceptive use) and is usually subareolar.2 Infection, however, is also commonly subareolar. Sarcoidosis rarely exhibits unilateral pleural effusion and usually manifests with bilateral interstitial lung disease, hilar lymphadenopathy, and non-necrotizing granulomas.3,4
M tuberculosis and other granulomatous infections may also feign breast cancer.5-13 Breast TB, which is highly uncommon in the developed world, often demonstrates imaging similar to that which was seen in this case. Breast TB may appear nodular with ill-defined contours. Masses are sometimes attached to the chest wall and usually lack microcalcifications on mammography; they are also typically hypoechoic and heterogenous on ultrasound, often showing posterior enhancement.5,7,8 Like other breast infections, tuberculosis may show cutaneous sinus tract formation, which is seen in about one-third of patients.6,7 Alternatively, it may manifest as a diffuse mastitis with skin thickening and axillary lymphadenopathy.8
Primary breast TB without chest disease comprises up to 86% of mammary tuberculosis.6,7 Infection may occur via contamination of the skin or nipple.5-7 Lactation, pregnancy, and other causes of immunosuppression (especially human immunodeficiency virus) have been associated with an increased risk of breast infection.6-8 This patient was at risk for immunosuppression from longstanding diabetes.14
Many patients from TB-endemic areas have received the bacille Calmette-Guerin (BCG) vaccine and may exhibit equivocal or false-positive PPD results. Because interferon-gamma release assay TB blood tests (eg, QuantiFERON-TB Gold or T-SPOT.TB) are not affected by BCG, they are not associated with false-positive repeat testing results.15
Biopsy is necessary to rule out malignancy and diagnose breast TB
A pleural fluid to serum protein ratio >0.5 is consistent with infection, but also with sarcoidosis or malignancy.3,16 Elevated pleural fluid adenosine deaminase (>40 U/L) is sensitive, albeit nonspecific, for the presence of TB microorganisms. If a lymphocyte-dominant exudate is also present, however, its reliability greatly increases.16,17 Increased pleural fluid interferon-gamma is also sensitive and specific for TB pleurisy.18 Culture, along with drug sensitivity testing, should be performed on all unexplained pleural effusions.
A biopsy is often required to diagnose breast TB and should be performed on all suspicious lesions to exclude malignancy.5-7,9 AFB stains and cultures of aspirate fluids or tissue are often negative.7,9 PCR or other nucleic acid amplification tests of sputum, body fluids, or biopsy material may be positive in culture-negative cases and can rapidly confirm M tuberculosis infection.17,19 No testing modality offers 100% sensitivity or specificity; therefore, an additional confirmatory test is desirable.
Possible routes of transmission include activation of latent pulmonary tuberculosis and direct, lymphatic, or hematologic extension to the chest wall and breast.5-7 In this patient, we believe that activation of a latent breast granuloma may have resulted in a secondary or “sympathetic” pleural effusion, possibly triggered by surgical manipulation. This is compatible with her negative pleural adenosine deaminase result, negative culture, absence of pulmonary parenchymal disease, and negative pleural biopsy. Although we conducted a PubMed search, reviewing material as far back as 1966, we were unable to find a previous case of apparent sympathetic effusion associated with breast TB.
Our patient was treated with daily oral isoniazid, rifabutin, pyrazinamide, and ethambutol for 2 months, followed by isoniazid and rifabutin for 4 months. She has been disease-free for over 10 years.
THE TAKEAWAY
We describe a rare case of breast TB mimicking carcinoma that was associated with unilateral pleural effusion in a woman who had emigrated from Afghanistan. Patients at particular risk for breast TB include immigrants from endemic regions—especially parous females,6,7 those with a history of TB contacts, and those who are immunosuppressed.8 This case emphasizes the need for increased awareness of extrapulmonary TB by physicians in developed countries.
ACKNOWLEDGEMENTS
The authors thank Drs. Margie Scott, Harpreet Dhillon, Samir Vora, Todd Williams, Jeffrey Hawley, and Mr. Sergio Landeros. This report is dedicated to the memory of our friend and colleague in medicine, Dr. Jeanie Care Gillinta.
1. Bayer-Garner IB, Cox MD, Scott MA, et al. Mycobacteria other than Mycobacterium tuberculosis are not present in erythema induratum/nodular vasculitis: a case series and literature review of the clinical and histologic findings. J Cutan Pathol. 2005;32:220-226.
2. Verfaillie G, Breucq C, Sacre R, et al. Granulomatous lobular mastitis: a rare chronic inflammatory disease of the breast which can mimic breast carcinoma. Acta Chir Belg. 2006;106:222-224.
3. Fiorucci F, Conti V, Lucantoni G, et al. Sarcoidosis of the breast: a rare case report and a review. Eur Rev Med Pharmacol Sci. 2006;10:47-50.
4. Huggins JT, Doelken P, Sahn SA, et al. Pleural effusions in a series of 181 outpatients with sarcoidosis. Chest. 2006;129:1599-1604.
5. Zandrino F, Monetti F, Gandolfo N. Primary tuberculosis of the breast. A case report. Acta Radiol. 2000;41:61-63.
6. Khanna R, Prasanna GV, Gupta P, et al. Mammary tuberculosis: report on 52 cases. Postgrad Med J. 2002;78:422-424.
7. Harris SH, Khan MA, Khan R, et al. Mammary tuberculosis: analysis of thirty-eight patients. ANZ J Surg. 2006;76:234-237.
8. Meerkotter D, Spiegel K, Page-Shipp LS. Imaging of tuberculosis of the breast: 21 cases and a review of the literature. J Med Imaging Radiat Oncol. 2011;55:453-460.
9. Khodabakhshi B, Mehravar F. Breast tuberculosis in northeast Iran: review of 22 cases. BMC Womens Health. 2014;14:72.
10. Osborne BM. Granulomatous mastitis caused by histoplasma and mimicking inflammatory breast carcinoma. Hum Pathol. 1989;20:47-52.
11. Bocian JJ, Fahmy RN, Michas CA. A rare case of ‘coccidioidoma’ of the breast. Arch Pathol Lab Med. 1991;115:1064-1067.
12. Haddow LJ, Sahid F, Moosa MY. Cryptococcal breast abscess in an HIV-positive patient: arguments for reviewing the definition of immune reconstitution inflammatory syndrome. J Infect. 2008;57:82-84.
13. Lefkowitz M, Wear DJ. Cat-scratch disease masquerading as a solitary tumor of the breast. Arch Pathol Lab Med. 1989;113:473-475.
14. Ponce-De-Leon A, Garcia-Garcia Md Mde L, Garcia-Sancho MC, et al. Tuberculosis and diabetes in southern Mexico. Diabetes Care. 2004;27:1584-1590.
15. Mazurek GH, LoBue PA, Daley CL, et al. Comparison of a whole-blood interferon gamma assay with tuberculin skin testing for detecting latent Mycobacterium tuberculosis infection. JAMA. 2001;286:1740-1747.
16. Porcel JM, Light RW. Diagnostic approach to pleural effusion in adults. Am Fam Physician. 2006;73:1211-1220.
17. Burgess LJ, Maritz FJ, Le Roux I, et al. Combined use of pleural adenosine deaminase with lymphocyte/neutrophil ratio. Increased specificity for the diagnosis of tuberculous pleuritis. Chest. 1996;109:414-419.
18. Klimiuk J, Krenke R, Safianowska A, et al. Diagnostic performance of different pleural fluid biomarkers in tuberculous pleurisy. Adv Exp Med Biol. 2015;852:21-30.
19. Gopi A, Madhavan SM, Sharma SK, et al. Diagnosis and treatment of tuberculous pleural effusion in 2006. Chest. 2007;131:880-889.
1. Bayer-Garner IB, Cox MD, Scott MA, et al. Mycobacteria other than Mycobacterium tuberculosis are not present in erythema induratum/nodular vasculitis: a case series and literature review of the clinical and histologic findings. J Cutan Pathol. 2005;32:220-226.
2. Verfaillie G, Breucq C, Sacre R, et al. Granulomatous lobular mastitis: a rare chronic inflammatory disease of the breast which can mimic breast carcinoma. Acta Chir Belg. 2006;106:222-224.
3. Fiorucci F, Conti V, Lucantoni G, et al. Sarcoidosis of the breast: a rare case report and a review. Eur Rev Med Pharmacol Sci. 2006;10:47-50.
4. Huggins JT, Doelken P, Sahn SA, et al. Pleural effusions in a series of 181 outpatients with sarcoidosis. Chest. 2006;129:1599-1604.
5. Zandrino F, Monetti F, Gandolfo N. Primary tuberculosis of the breast. A case report. Acta Radiol. 2000;41:61-63.
6. Khanna R, Prasanna GV, Gupta P, et al. Mammary tuberculosis: report on 52 cases. Postgrad Med J. 2002;78:422-424.
7. Harris SH, Khan MA, Khan R, et al. Mammary tuberculosis: analysis of thirty-eight patients. ANZ J Surg. 2006;76:234-237.
8. Meerkotter D, Spiegel K, Page-Shipp LS. Imaging of tuberculosis of the breast: 21 cases and a review of the literature. J Med Imaging Radiat Oncol. 2011;55:453-460.
9. Khodabakhshi B, Mehravar F. Breast tuberculosis in northeast Iran: review of 22 cases. BMC Womens Health. 2014;14:72.
10. Osborne BM. Granulomatous mastitis caused by histoplasma and mimicking inflammatory breast carcinoma. Hum Pathol. 1989;20:47-52.
11. Bocian JJ, Fahmy RN, Michas CA. A rare case of ‘coccidioidoma’ of the breast. Arch Pathol Lab Med. 1991;115:1064-1067.
12. Haddow LJ, Sahid F, Moosa MY. Cryptococcal breast abscess in an HIV-positive patient: arguments for reviewing the definition of immune reconstitution inflammatory syndrome. J Infect. 2008;57:82-84.
13. Lefkowitz M, Wear DJ. Cat-scratch disease masquerading as a solitary tumor of the breast. Arch Pathol Lab Med. 1989;113:473-475.
14. Ponce-De-Leon A, Garcia-Garcia Md Mde L, Garcia-Sancho MC, et al. Tuberculosis and diabetes in southern Mexico. Diabetes Care. 2004;27:1584-1590.
15. Mazurek GH, LoBue PA, Daley CL, et al. Comparison of a whole-blood interferon gamma assay with tuberculin skin testing for detecting latent Mycobacterium tuberculosis infection. JAMA. 2001;286:1740-1747.
16. Porcel JM, Light RW. Diagnostic approach to pleural effusion in adults. Am Fam Physician. 2006;73:1211-1220.
17. Burgess LJ, Maritz FJ, Le Roux I, et al. Combined use of pleural adenosine deaminase with lymphocyte/neutrophil ratio. Increased specificity for the diagnosis of tuberculous pleuritis. Chest. 1996;109:414-419.
18. Klimiuk J, Krenke R, Safianowska A, et al. Diagnostic performance of different pleural fluid biomarkers in tuberculous pleurisy. Adv Exp Med Biol. 2015;852:21-30.
19. Gopi A, Madhavan SM, Sharma SK, et al. Diagnosis and treatment of tuberculous pleural effusion in 2006. Chest. 2007;131:880-889.
