User login
Fall Prevention Strategies
Inpatient falls are the most common type of inpatient adverse event,1 persist as a significant problem nationally, and result in patient injury, increased length of stay, healthcare costs, and litigation.27 Inpatient falls remain a main focus of patient safety and a measure of quality in this era of healthcare reform and quality improvement.8 Inpatient fall rates per 1000 patient‐days range from 1.4 to 18.2.4, 9 The absolute percentage of inpatients that fall ranges from 1.3% to 7%.4, 5, 9, 10 Of inpatient falls, almost all data suggest that roughly one‐third result in some type of injury while 3%‐8% result in serious injury or death.9, 1113
Fall prevention interventions have largely been aimed at modifiable risk factors such as getting out of bed with bed alarms, toileting needs with bedside commodes, and reducing delirium through reorientation techniques. There have been several attempts at decreasing fall rates in hospitals surrounding a multidisciplinary, team‐based approach. Two Cochrane reviews and 2 meta‐analyses have partially examined this issue with mixed results.1417 However, none of these reviews focused on the acute care inpatient population. In fact, the majority of the data analyzed for inpatients was from rehabilitation wards and long‐term care wards. Additionally, there exists almost no data examining fall prevention with single interventions in the acute inpatient population, likely due to the belief that falls are multifactorial in etiology and require more comprehensive interventions.
The aim of this article is to determine the impact of team‐based, multidisciplinary quality improvement efforts to reduce inpatient falls in acute care inpatient hospitals and identify key features that determine their effectiveness.
METHODS
Data Sources and Searches
A search of MEDLINE, CINAHL, EMBASE, and the Cochrane Library was done using the medical subject heading (MeSH) terms accidental falls, accident prevention, inpatients, and prevention and control. Non‐English language publications were included in the search. The search encompassed all published literature through December 1, 2011. In addition, reference lists of all systematic reviews and meta‐analyses were searched to identify all possible studies available.1416
Study Selection
Only primary research studies relating to acute care inpatient hospital fall prevention were included. Data generated exclusively or partially from psychiatric wards, rehabilitation units, subacute facilities, and long‐term facilities were excluded from the review.
Data Extraction and Quality Assessment
Each selected study was carefully hand searched by 2 authors for the purposes of data extraction. Data were collected for the following study characteristics and outcome measures: details of the fall prevention intervention used (allowing for all interventions used to be recorded in Table 3), markers of study quality, study period, study population, mean age of participants, sample size (in 1000 patient‐days), and fall rates (in 1000 patient‐days). In certain cases, sample size was converted to patient‐days using reported data points of total number of patients and average length of stay.
Two authors with experience in fall literature discussed methodological quality and reached a consensus regarding scores using a 20‐point scale previously described in fall literature for all studies included.14, 15 Ten individual criteria were scored on a 0‐2 point scale. No points were awarded when the criteria were not met, not clearly mentioned, or not mentioned at all. One point was awarded when the criterion was partially met, and both points awarded when it was fully met.
Data Synthesis and Analysis
Fall rate per 1000‐patient days was derived from reported data in both intervention and non‐intervention groups within each study. Effect sizes (odds ratios [OR]) and 95% confidence intervals (CI) were derived for individual studies and then combined across research reports using an inverse weighted random‐effects meta‐analysis.18 Random effects methodology was chosen to account for within‐study and between‐study variation. Statistical heterogeneity between trials was assessed using the Cochrane Q statistic and reported as I2, which estimates the percentage of variability across studies that is not due to chance.19 Due to the low number of included studies in our analysis, a formal statistical test on publication bias was not meaningful.20 Statistical significance was defined as P 0.05. Data analyses were done using Comprehensive Meta‐Analysis, Version 2 (Biostat, Englewood, NJ).
RESULTS
Selected Studies
Electronic search produced 259 results on MEDLINE, 2 results from the Cochrane Library, 94 from CINAHL, and 4 from EMBASE. Each result was hand searched to exclude duplicates, and irrelevant studies. Once such data were excluded, the above inclusion and exclusion criteria identified 6 primary articles for review.9, 2125 Additionally, a cluster randomized fall prevention trial in a mixed inpatient population was published by Cumming et al26 in 2008. The study was excluded, as the participants were pooled between rehabilitation wards and acute inpatient wards, and only incomplete data were reported separately for the acute inpatient wards. We were unsuccessful at obtaining necessary data to analyze the acute inpatient wards.
Study Quality
The quality assessment results scores ranged from 11 to 14 out of a possible 20 (Table 1). None of the studies explicitly used an intention‐to‐treat statistical model, as the nature of inpatient care largely prevents drop‐out or crossover, and all patients were included in individual study results.
| Included Study | Clearly Defined Inclusion and Exclusion Criteria | Randomization | Comparable Treatment Groups at Entry | Identical Standard Program for Both Groups | Fall Incident Clearly Defined and Staff Trained in Definition | Blinded Treatment Providers | Blinded Outcome Assessors | Blinded Patients | Identical Appraisal of Outcomes* | Intention‐to‐ Treat Analysis | Total Score (0‐20) |
|---|---|---|---|---|---|---|---|---|---|---|---|
| |||||||||||
| Dykes et al22 | 2 | 2 | 2 | 2 | 2 | 0 | 0 | 0 | 2 | 2 | 14 |
| Krauss et al23 | 2 | 0 | 2 | 2 | 2 | 0 | 0 | 0 | 2 | 2 | 12 |
| Brandis21 | 1 | 0 | 1 | 2 | 2 | 0 | 0 | 0 | 2 | 2 | 10 |
| Mitchell and Jones25 | 2 | 0 | 1 | 2 | 2 | 0 | 0 | 0 | 2 | 2 | 11 |
| Schwendimann et al9 | 2 | 0 | 1 | 2 | 2 | 0 | 0 | 0 | 2 | 2 | 11 |
| Williams et al24 | 2 | 0 | 1 | 2 | 2 | 0 | 0 | 0 | 2 | 2 | 11 |
Study Characteristics
The available data are skewed towards elderly patients being hospitalized in general medicine or geriatric units (Table 2). All but 1 study had a large sample size, with 1000‐patient days ranging from 11.1 to 160.3.9, 2124
| Included Study | Study Design | Study Period | Study Wards | Mean Age | Sample Size With Intervention (1000 Patient‐Days) | Sample Size in Control (1000 Patient‐Days) | Fall Rate With Intervention (Falls per 1000 Patient‐Days) | Fall Rate in Control (Falls per 1000 Patient‐Days) |
|---|---|---|---|---|---|---|---|---|
| ||||||||
| Dykes et al22 | RCT | 6 mo | 2 Medical units | 50% 65‐17% 65‐74 33% 75 | 24.1 | 24.1 | 4.18 | 4.64 |
| Krauss et al23 | Quasi‐experimental | 9 mo | General Medicine wards | 65.5 | 11.2 | 11.39 | 5.09 | 6.85 |
| Brandis21 | Pre/post | 12 mo | 500‐Bed acute care hospital | Not reported | 160.3 | 155.2 | 1.61 | 1.74 |
| Mitchell and Jones25 | Pre/post | 6 mo | Acute care hospital | 76.23 (Pre) 72.1 (Post) | 4.3 | 5 | 4.42 | 7.77 |
| Schwendimann et al9 | Pre/post | 4 yr | Internal Med, Surgery, and Geriatrics | 67.3 | 46.8 | 41.9 | 8.6 | 9.1 |
| Williams et al24 | Pre/post | 6 mo | 3 Medical wards and a Geriatrics ward | 79 | 15.88 | 12.53 | 8 | 9.5 |
Components of the Intervention
Multidisciplinary interventions were complex, and formulated based on available evidence for individual interventions and modifiable fall risk factors (Table 3). Each study reviewed included a fall risk assessment to risk‐stratify participants and modulate intervention according to risk.9, 2125
| Included Study | Fall Risk Assessment Used | Mobility Assessment and Assistance if Necessary | Mobility Aid Provided if Necessary | Medication Modification | Education About Risk Factors | Fall Risk Sign/Warning in Chart | Bedside Interventions (eg, Bed Alarm, Rail Adjustment, Bed Location/ Position, etc) | Toileting Schedule | Exercise Program | Other(s) |
|---|---|---|---|---|---|---|---|---|---|---|
| ||||||||||
| Dykes et al22* | + | + | + | + | + | + | + | + | Frequent bed checks, documented fall prevention plan | |
| Krauss et al23 | + | + | + | + | + | + | + | + | Use of bedside interventions was done based on discretion on a case‐by‐case basis | |
| Brandis21 | + | + | + | Ward modifications after OT assessment of patient rooms and bathrooms; hip protectors | ||||||
| Mitchell and Jones25 | + | + | + | + | Introduced detailed system to track fall details; used other preventive actions not specified | |||||
| Schwendimann et al9 | + | + | + | + | + | + | + | + | + | Reassessment of patients who did fall; hip protectors |
| Williams et al24 | + | + | + | + | + | + | Possible sitter | |||
Each study implemented fall prevention programs in a slightly different way. Krauss et al23 used nurses to complete a Morse Fall Scale and subsequently implement several standard interventions based on risk. Staff was then authorized to employ bedside interventions as necessary without systematic data collection. Schwendimann et al9 had nurses complete a simple fall risk assessment (based on history of falls, impaired mobility, and impaired cognition) that prompted the examination by a physician if risk was determined to be high. A subsequent team‐based intervention was employed with nursing, physiotherapy, and the physician. Brandis21 employed a team of nurses and the aid of the Director of Occupational Therapy to assess risk (using an undisclosed system) and carry out an intervention. Dykes et al22 examined an electronic fall prevention tool kit (FPTK) using the electronic medical record (EMR). This intervention began with the Morse Fall Score, which triggered automatically ordered interventions that did not require personal oversight. In fact, the multidisciplinary interventions in the intervention group were also used in the control arm. The difference was the automatic nature in which the interventions were ordered in the interventions arm. Williams et al24 used nurses and physiotherapists, who were specifically trained for the study, to carry out study interventions. The Mitchell and Jones25 study focused on nursing care alone to carry out intervention and used a novel risk assessment tool.
Fall Rates
Dykes et al22 and Williams et al24 found a statistically significant reduction in fall rate with falls reduced by 1.16 per 1000‐patient days and 1.5 per 1000‐patient days, respectively. Mitchell and Jones25 demonstrated a large fall reduction but had an extremely small sample size. Brandis21 found an extremely small reduction in fall rates and failed to report a P‐value. Krauss et al23 showed a trend towards reducing falls, and even showed a statistically significant reduction over the first 5 months of the study, but lost significance in the final 4 months. Similarly, Schwendimann et al9 saw more impressive fall reductions in the first year of the study that dissipated in the final 3 years of data collection.
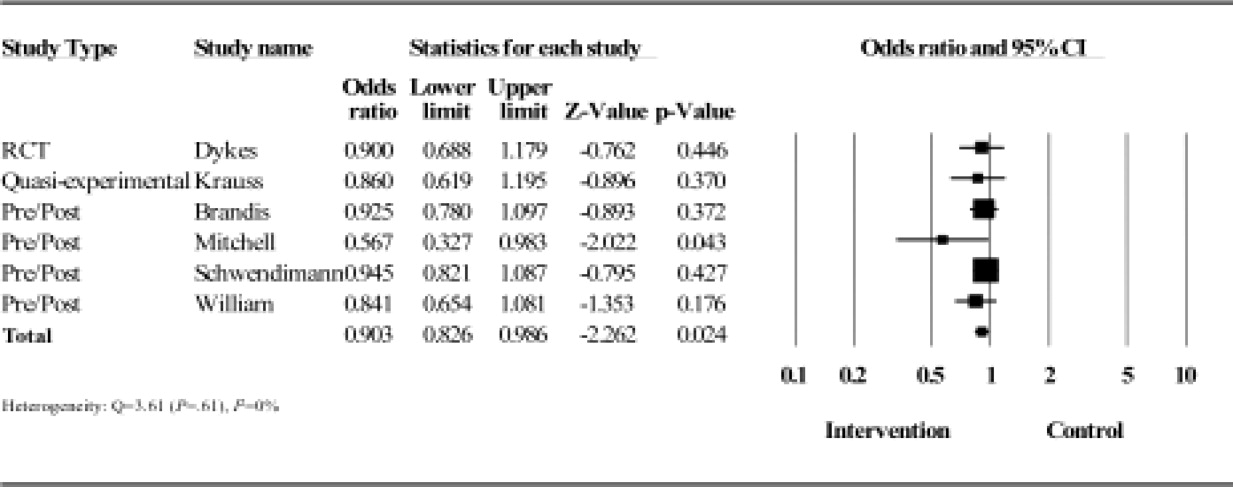
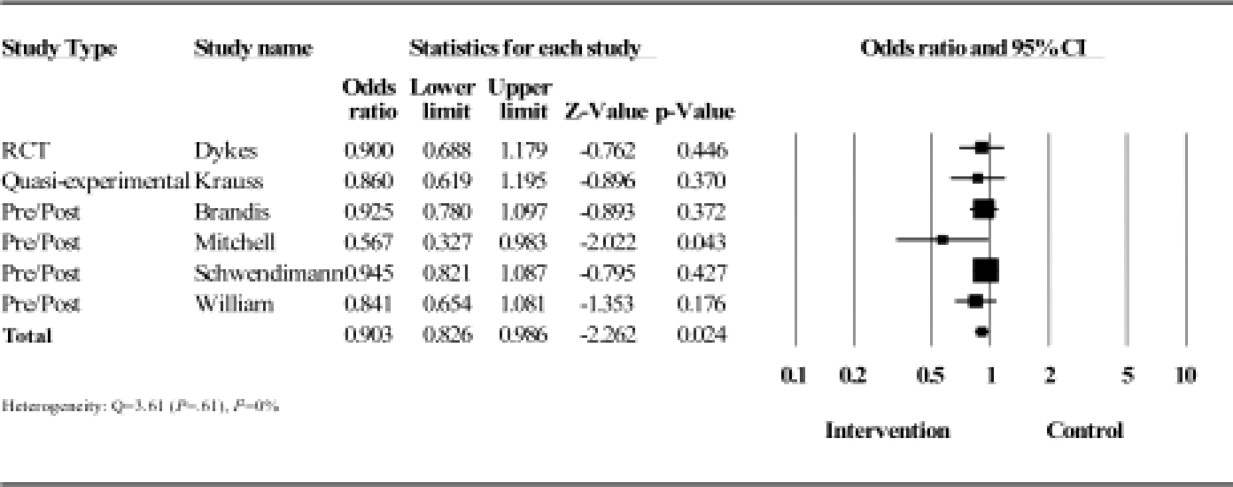
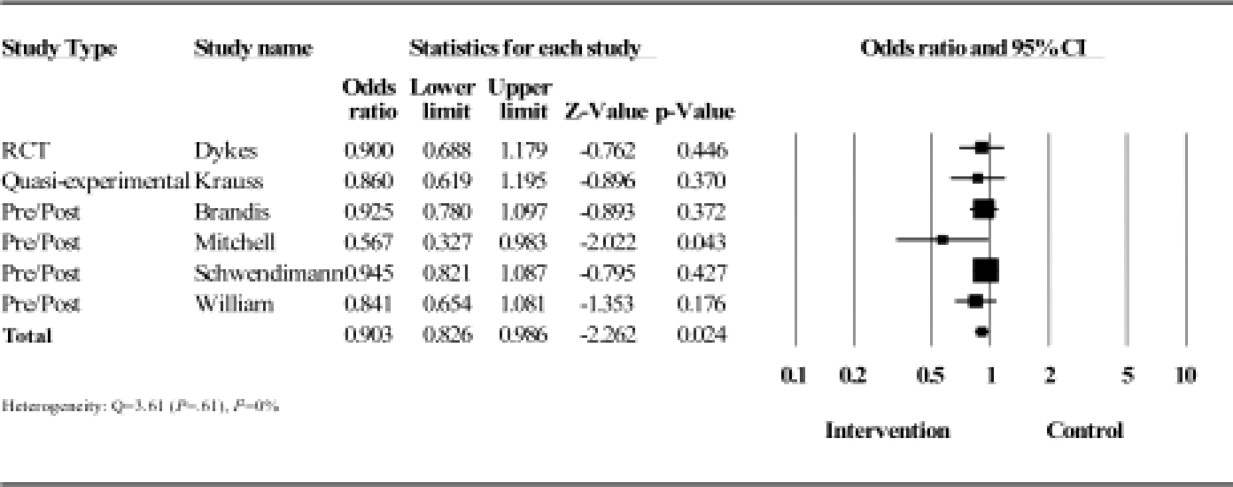
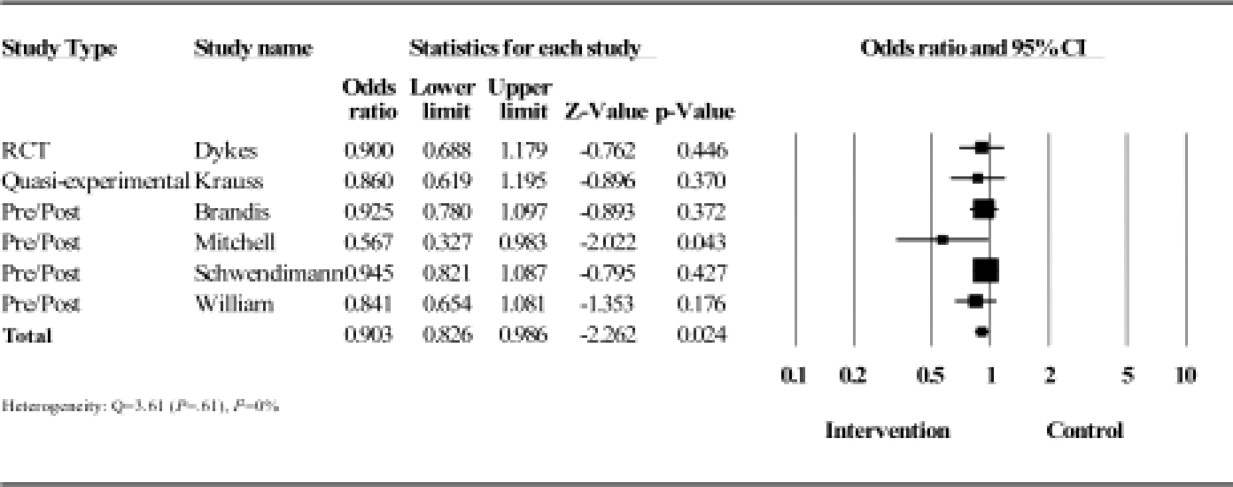
Results from the meta‐analysis of the 6 studies comparing odds ratios are displayed quantitatively and as a forest plot in Figure 1. The figure shows results with 95% CI for each individual study and overall. There was no statistical evidence of heterogeneity between the studies or study designs. Although, due to the small number of studies included, there is poor power to detect true heterogeneity among studies. The magnitude of boxes shown is a relative sample size indicator. Using the random‐effects model, the summary odds ratio is 0.90 (95% CI, 0.83 to 0.99) (P = 0.02) (I2 = 0%).27
DISCUSSION
The frequency and morbidity associated with inpatient falls is well established, based on reproduced epidemiologic data. Reducing these adverse events could reduce morbidity, mortality, and healthcare costs, and has become the focus of most hospitals quality and patient safety initiatives. The focus of this review was to examine multidisciplinary efforts to reduce falls in acute care inpatient hospitals. Despite the importance and scope of the problem, there is a paucity of research available on this topic, with a wide literature search yielding only 6 primary research studies.
Our major finding is that multidisciplinary fall prevention strategies have a statistically significant impact on fall rates with a combined OR of 0.90. While this review demonstrates a significant benefit to multidisciplinary fall prevention strategies in the acute inpatient population, the clinical impact of these efforts may be limited. Based on rates ranging from 1.7 to 9.5 falls per 1000‐patient days, multidisciplinary interventions would reduce falls by 1 to 10 falls per 10,000‐patient days using the combined OR calculated of 0.9. Using other available incidence data regarding inpatient falls,4, 9 a reasonable baseline frequency to consider would be 8 falls per 1000 patient‐days. Assuming that prevalence, the number needed to treat (NNT) to prevent a single inpatient fall is 1250 patient days. Furthermore, based on available data, only approximately one‐third of these falls result in injury and only a minor fraction of these results in serious injury.9, 1113 The magnitude of this apparent benefit in the context of fall incidence rates raises some concerns about cost‐effectiveness given the high staffing and systems needs that multidisciplinary prevention programs require. This also suggests that there are limitations when using inpatient falls as a measure of healthcare quality given the absence of high‐quality evidence demonstrating a viable solution to the problem. At present, the Center for Medicare and Medicaid services limit reimbursement for fall‐related injuries if they occur during an acute inpatient hospitalization.28
The complexity of the interventions used may help explain the limited impact. Krauss et al23 examined compliance to their interventions and found less than ideal results. They found only 36.4% of intervention floor patients had maintained a toileting schedule compared to 24.6% on control floors. Additionally, a greater proportion of patients on control floors had a physical or occupational therapy consult, and only 1.8% more patients on intervention floors had walking aids provided. These were all strategies emphasized on the intervention floors. Similarly, Schwendimann et al9 questioned their staff's adherence to protocol after fall prevention committee audits. This may help explain why a potential benefit lost statistical significance with time, based on a natural tendency towards more participation at the beginning of a new policy. Williams et al24 reported only a 64% compliance rate with fall care plan forms and 77% rate of missing information on fall care plans. A multidisciplinary fall prevention study that did not meet inclusion criteria (based on study population) yielded strongly positive results for which the authors commented mostly on changing of the hospital culture surrounding fall prevention as a key to their success.29 Adoptability of a multidisciplinary intervention will clearly impact adherence and the intervention's ultimate effectiveness.
Single intervention strategies, not analyzed in this review, are simpler to execute and adhere to. While these types of interventions may be superior, there is extremely limited data supporting or refuting patient fall benefits in the acute care inpatient population when using simple single interventions. However, some data generated partially on acute care geriatrics wards targeting patient education only showed benefit.30
Dykes et al22 was able to improve compliance rates by removing steps in the process of executing interventions with the FPTK built into the EMR. Importantly, the FPTK was compared against very similar fall prevention strategies, the difference being that patients randomized to the FPTK arm had the assessment and interventions automatically prompted on admission in the EMR. Adherence was measured through Morse Fall Scale completion rates (81% in control units versus 94% in intervention units).22 In many ways, the utility of this study was displaying a fall risk reduction by simply enhancing compliance using health information technology with automated alerts. Additionally, both arms of the study reported low fall rates compared to previously reported data, and there may have been larger benefit seen if the FPTK was compared against no fall prevention strategy. This diminishing of effect size may have been present in all studies reviewed, as usual hospital care commonly includes basic patient safety measures.
Another potential problem with the multidisciplinary fall prevention programs included in the meta‐analysis is the inability to target interventions. Each study employed a fall risk score in an attempt to focus resources on a select group of high‐risk patients. This method is problematic given that countless risk factors for inpatient falls have been identified in the literature. Factors that have been described range from clinical characteristics to laboratory tests.31 The most consistently reproducible patient‐related risks are altered mental status (including cognitive impairment and depression), altered mobility (particularly lower limb weakness), a history of falls, and toileting needs.13, 3236 Less consistency is seen with other traditional risk factors such as age, sedating medication, and length of stay.5, 13, 32, 3638 Attempting to risk‐stratify patients using simple and accurate assessment tools developed from these risk factors has proven to be very difficult. Many tools have been developed based on identified risk factors, but perform very poorly when trying to identify patients who will fall with reasonable specificity and positive predictive value.34, 3944 In fact, it has been demonstrated that using a nurse's judgment, a physician's opinion based on a patient's likelihood to wander or a simple 2‐question tool have all performed better than sophisticated risk calculators.33, 45, 46 Therefore, it is possible that interventions could benefit from including all patients, with de‐emphasis on unproven risk stratification tools.
In contrast to our findings, a modest risk reduction has been demonstrated in several primary articles and meta‐analyses in the subacute, rehabilitation, and long‐term care populations.15, 16, 4750 Additionally, a recent study has described a 63.9% risk reduction in a population that included medical, surgical, psychiatric, and rehabilitation wards.29 One important difference between these settings and the acute inpatient populations may be the amount of time and energy that can be dedicated to fall prevention and overall care planning. Another likely factor is the added challenge of preventing falls in patients with more active medical illnesses. In the acute care setting, a patient's chief complaint may not be completely addressed at the time of first mobilization and ambulation. This may be most relevant in patients who are admitted with syncope, seizure, vertigo, and dehydration.
Our study has several limitations; most notably, the available evidence is limited in quality and quantity. Furthermore, omission of unpublished data may also lead to effect bias, though this would likely be in the direction of ineffective interventions supporting a conclusion that multidisciplinary efforts have had only a small impact on fall rates. Ideally, future studies can limit confounding variables through randomization. However, it is difficult to adequately blind when studying a multidisciplinary fall intervention that depends on patient and provider participation. As a result, none of the papers reviewed met criteria for high quality. However, almost all available data examined in this review came from large sample sizes in which thoughtful interventions were used. Since an inpatient fall will not affect the majority of patients, it was crucial for these studies to recruit a large sample size to have adequate power to detect a difference in fall rates. However, each study used risk assessment tools, which are poor indicators of who will and will not fall in the hospital.34, 39, 42 This may suggest a need for improved risk assessment tools, or be further evidence to include all patients in fall prevention regardless of risk. Quantitative synthesis of multidisciplinary fall interventions has the added limitation of comparing complex, multifaceted treatments that are not perfectly uniform. It is our opinion that interventions are semi‐standardized using the grouping methods employed in Table 3.
Preventing inpatient falls remains a difficult issue to address while convincing data is lacking. Based on current evidence, multidisciplinary fall prevention efforts on acutely ill inpatients show a possible small benefit and should be explored from a cost‐effectiveness standpoint to ensure they garner appropriate investment. Many resources are required to run such teams including nursing staff, equipment, physical and occupational therapy staff, pharmacists, and specialized staff training. We are unaware of any such cost‐effectiveness data available. Effective interventions may be those that maximize compliance through health information technology, maintain staff dedication, increase staff availability, improve risk assessment, or include all patients regardless of calculated fall risk, and take the patient's chief complaint into account in the fall prevention strategy. Where resources are limited, it appears most reasonable to focus on major risk factors for inpatient falls that have independently been shown to be detrimental to outcomes, such as delirium.51 Additionally, using inpatient fall rates as a hospital quality measure may be premature, given the lack of proven efforts to lower fall rates. Multidisciplinary fall prevention efforts on acutely ill inpatients should be further studied using high‐quality, randomized trials. It remains to be seen whether these large programs are cost‐effective, or on balance clinically effective.
- ,,.Patient accidents in hospital: incidence, documentation and significance.Br J Clin Pract.1994;48(2):63–66.
- ,,,.Serious falls in hospitalized patients: correlates and resource utilization.Am J Med.1995;99(2):137–143.
- ,,,.Hospital falls: a persistent problem.Am J Public Health.1985;75(7):775–777.
- ,,.Falls in the acute hospital setting—impact on resource utilisation.Aust Health Rev.2007;31(3):471–477.
- ,,.Incidence and risk factors for inpatient falls in an academic acute‐care hospital.J Nippon Med Sch.2006;73(5):265–270.
- ,,,.Do falls and falls‐injuries in hospital indicate negligent care—and how big is the risk? A retrospective analysis of the NHS Litigation Authority Database of clinical negligence claims, resulting from falls in hospitals in England 1995 to 2006.Qual Saf Health Care.2008;17(6):431–436.
- ,,,.Hospital falls: development of a predictive model for clinical practice.Appl Nurs Res.1995;8(3):129–139.
- ,.Centers for Medicare and Medicaid Services' “never events”: an analysis and recommendations to hospitals.Health Care Manag (Frederick).2008;27(4):338–349.
- ,,,.Falls and consequent injuries in hospitalized patients: effects of an interdisciplinary falls prevention program.BMC Health Serv Res.2006;6:69.
- .Immobility and falls.Clin Geriatr Med.1998;14(4):699–726.
- ,,.A case control study of falls in the hospital setting.J Gerontol Nurs.1998;24(12):7–15.
- ,,,.A retrospective analysis of patient falls.Can J Public Health.1985;76(2):116–118.
- ,,, et al.Characteristics and circumstances of falls in a hospital setting: a prospective analysis.J Gen Intern Med.2004;19(7):732–739.
- ,,, et al.Interventions for preventing falls in older people in nursing care facilities and hospitals.Cochrane Database Syst Rev.2010(1):CD005465.
- , L,,,,.Interventions for preventing falls in acute‐ and chronic‐care hospitals: a systematic review and meta‐analysis.J Am Geriatr Soc.2008;56(1):29–36.
- ,,, et al.Strategies to prevent falls and fractures in hospitals and care homes and effect of cognitive impairment: systematic review and meta‐analyses.BMJ.2007;334(7584):82.
- ,,,,,.Interventions for preventing falls in elderly people.Cochrane Database Syst Rev.2003(4):CD000340.
- ,,,.Introduction to Meta‐Analysis.Chichester, UK:John Wiley 2009.
- ,.Quantifying heterogeneity in a meta‐analysis.Stat Med.2002;21(11):1539–1558.
- .The power of the standard test for the presence of heterogeneity in meta‐analysis.Stat Med.2006;25(15):2688–2699.
- .A collaborative occupational therapy and nursing approach to falls prevention in hospital inpatients.J Qual Clin Pract.1999;19(4):215–220.
- ,,, et al.Fall prevention in acute care hospitals: a randomized trial.JAMA.2010;304(17):1912–1918.
- ,,,,,.Intervention to prevent falls on the medical service in a teaching hospital.Infect Control Hosp Epidemiol.2008;29(6):539–545.
- ,,, et al.Evaluation of a falls prevention programme in an acute tertiary care hospital.J Clin Nurs.2007;16(2):316–324.
- ,.Striving to prevent falls in an acute care setting—action to enhance quality.J Clin Nurs.1996;5(4):213–220.
- ,,, et al.Cluster randomised trial of a targeted multifactorial intervention to prevent falls among older people in hospital.BMJ.2008;336(7647):758–760.
- ,.Graphical displays for meta‐analysis: an overview with suggestions for practice.Res Syn Meth.2010(1):66–80.
- Centers for Medicare 37(7):317–325.
- ,‐M,, et al.Patient education to prevent falls among older hospital inpatients: a randomized controlled trial.Arch Intern Med.2011;117:516–524.
- ,.The relationship between patient blood pathology values and patient falls in an acute‐care setting: a retrospective analysis.Int J Nurs Pract.2005;11(4):161–168.
- ,,,.Falls risk factors in the hospital setting: a systematic review.Int J Nurs Pract.2001;7(1):38–45.
- ,,.A simplified fall‐risk assessment tool for patients hospitalized in medical wards.Isr Med Assoc J.2008;10(2):125–129.
- ,,,.Risk factors and risk assessment tools for falls in hospital in‐patients: a systematic review.Age Ageing.2004;33(2):122–130.
- ,,, et al.Circumstances of patient falls and injuries in 9 hospitals in a midwestern healthcare system.Infect Control Hosp Epidemiol.2007;28(5):544–550.
- ,,, et al.A case‐control study of patient, medication, and care‐related risk factors for inpatient falls.J Gen Intern Med.2005;20(2):116–122.
- .The experience of a community hospital in quantifying and reducing patient falls.J Nurs Care Qual.2000;14(3):43–53.
- ,,,.Characteristics of hospital inpatient falls across clinical departments.Gerontology.2008;54(6):342–348.
- ,.Falls risk prediction tools for hospital inpatients: do they work?Nurs Times.2009;105(7):18–21.
- ,,,.Accidental falls in hospital inpatients: evaluation of sensitivity and specificity of two risk assessment tools.J Adv Nurs.2010;66(3):690–696.
- ,,,,,.A systematic review and meta‐analysis of studies using the STRATIFY tool for prediction of falls in hospital patients: how well does it work?Age Ageing.2008;37(6):621–627.
- .Falls risk‐prediction tools for hospital inpatients. Time to put them to bed?Age Ageing.2008;37(3):248–250.
- ,,,,.Evaluation of three fall‐risk assessment tools in an acute care setting.J Adv Nurs.2007;60(4):427–435.
- ,,, et al.Fall prediction in inpatients by bedside nurses using the St. Thomas's Risk Assessment Tool in Falling Elderly Inpatients (STRATIFY) instrument: a multicenter study.J Am Geriatr Soc.2007;55(5):725–733.
- ,,,.Comparison of a fall risk assessment tool with nurses' judgement alone: a cluster‐randomised controlled trial.Age Ageing.2009;38(4):417–423.
- ,,,,.Fall risk‐assessment tools compared with clinical judgment: an evaluation in a rehabilitation ward.Age Ageing.2008;37(3):277–281.
- ,.Incidence of in‐hospital falls in geriatric patients before and after the introduction of an interdisciplinary team‐based fall‐prevention intervention.J Am Geriatr Soc.2007;55(12):2068–2074.
- ,,,.Sustained reduction in serious fall‐related injuries in older people in hospital.Med J Aust.2006;184(8):379–382.
- ,,, et al.The effect of changing practice on fall prevention in a rehabilitative hospital: the Hospital Injury Prevention Study.J Am Geriatr Soc.2004;52(3):335–339.
- ,,,.Effectiveness of targeted falls prevention programme in subacute hospital setting: randomised controlled trial.BMJ.2004;328(7441):676.
- ,,,,.Does delirium contribute to poor hospital outcomes? A three‐site epidemiologic study.J Gen Intern Med.1998;13(4):234–242.
Inpatient falls are the most common type of inpatient adverse event,1 persist as a significant problem nationally, and result in patient injury, increased length of stay, healthcare costs, and litigation.27 Inpatient falls remain a main focus of patient safety and a measure of quality in this era of healthcare reform and quality improvement.8 Inpatient fall rates per 1000 patient‐days range from 1.4 to 18.2.4, 9 The absolute percentage of inpatients that fall ranges from 1.3% to 7%.4, 5, 9, 10 Of inpatient falls, almost all data suggest that roughly one‐third result in some type of injury while 3%‐8% result in serious injury or death.9, 1113
Fall prevention interventions have largely been aimed at modifiable risk factors such as getting out of bed with bed alarms, toileting needs with bedside commodes, and reducing delirium through reorientation techniques. There have been several attempts at decreasing fall rates in hospitals surrounding a multidisciplinary, team‐based approach. Two Cochrane reviews and 2 meta‐analyses have partially examined this issue with mixed results.1417 However, none of these reviews focused on the acute care inpatient population. In fact, the majority of the data analyzed for inpatients was from rehabilitation wards and long‐term care wards. Additionally, there exists almost no data examining fall prevention with single interventions in the acute inpatient population, likely due to the belief that falls are multifactorial in etiology and require more comprehensive interventions.
The aim of this article is to determine the impact of team‐based, multidisciplinary quality improvement efforts to reduce inpatient falls in acute care inpatient hospitals and identify key features that determine their effectiveness.
METHODS
Data Sources and Searches
A search of MEDLINE, CINAHL, EMBASE, and the Cochrane Library was done using the medical subject heading (MeSH) terms accidental falls, accident prevention, inpatients, and prevention and control. Non‐English language publications were included in the search. The search encompassed all published literature through December 1, 2011. In addition, reference lists of all systematic reviews and meta‐analyses were searched to identify all possible studies available.1416
Study Selection
Only primary research studies relating to acute care inpatient hospital fall prevention were included. Data generated exclusively or partially from psychiatric wards, rehabilitation units, subacute facilities, and long‐term facilities were excluded from the review.
Data Extraction and Quality Assessment
Each selected study was carefully hand searched by 2 authors for the purposes of data extraction. Data were collected for the following study characteristics and outcome measures: details of the fall prevention intervention used (allowing for all interventions used to be recorded in Table 3), markers of study quality, study period, study population, mean age of participants, sample size (in 1000 patient‐days), and fall rates (in 1000 patient‐days). In certain cases, sample size was converted to patient‐days using reported data points of total number of patients and average length of stay.
Two authors with experience in fall literature discussed methodological quality and reached a consensus regarding scores using a 20‐point scale previously described in fall literature for all studies included.14, 15 Ten individual criteria were scored on a 0‐2 point scale. No points were awarded when the criteria were not met, not clearly mentioned, or not mentioned at all. One point was awarded when the criterion was partially met, and both points awarded when it was fully met.
Data Synthesis and Analysis
Fall rate per 1000‐patient days was derived from reported data in both intervention and non‐intervention groups within each study. Effect sizes (odds ratios [OR]) and 95% confidence intervals (CI) were derived for individual studies and then combined across research reports using an inverse weighted random‐effects meta‐analysis.18 Random effects methodology was chosen to account for within‐study and between‐study variation. Statistical heterogeneity between trials was assessed using the Cochrane Q statistic and reported as I2, which estimates the percentage of variability across studies that is not due to chance.19 Due to the low number of included studies in our analysis, a formal statistical test on publication bias was not meaningful.20 Statistical significance was defined as P 0.05. Data analyses were done using Comprehensive Meta‐Analysis, Version 2 (Biostat, Englewood, NJ).
RESULTS
Selected Studies
Electronic search produced 259 results on MEDLINE, 2 results from the Cochrane Library, 94 from CINAHL, and 4 from EMBASE. Each result was hand searched to exclude duplicates, and irrelevant studies. Once such data were excluded, the above inclusion and exclusion criteria identified 6 primary articles for review.9, 2125 Additionally, a cluster randomized fall prevention trial in a mixed inpatient population was published by Cumming et al26 in 2008. The study was excluded, as the participants were pooled between rehabilitation wards and acute inpatient wards, and only incomplete data were reported separately for the acute inpatient wards. We were unsuccessful at obtaining necessary data to analyze the acute inpatient wards.
Study Quality
The quality assessment results scores ranged from 11 to 14 out of a possible 20 (Table 1). None of the studies explicitly used an intention‐to‐treat statistical model, as the nature of inpatient care largely prevents drop‐out or crossover, and all patients were included in individual study results.
| Included Study | Clearly Defined Inclusion and Exclusion Criteria | Randomization | Comparable Treatment Groups at Entry | Identical Standard Program for Both Groups | Fall Incident Clearly Defined and Staff Trained in Definition | Blinded Treatment Providers | Blinded Outcome Assessors | Blinded Patients | Identical Appraisal of Outcomes* | Intention‐to‐ Treat Analysis | Total Score (0‐20) |
|---|---|---|---|---|---|---|---|---|---|---|---|
| |||||||||||
| Dykes et al22 | 2 | 2 | 2 | 2 | 2 | 0 | 0 | 0 | 2 | 2 | 14 |
| Krauss et al23 | 2 | 0 | 2 | 2 | 2 | 0 | 0 | 0 | 2 | 2 | 12 |
| Brandis21 | 1 | 0 | 1 | 2 | 2 | 0 | 0 | 0 | 2 | 2 | 10 |
| Mitchell and Jones25 | 2 | 0 | 1 | 2 | 2 | 0 | 0 | 0 | 2 | 2 | 11 |
| Schwendimann et al9 | 2 | 0 | 1 | 2 | 2 | 0 | 0 | 0 | 2 | 2 | 11 |
| Williams et al24 | 2 | 0 | 1 | 2 | 2 | 0 | 0 | 0 | 2 | 2 | 11 |
Study Characteristics
The available data are skewed towards elderly patients being hospitalized in general medicine or geriatric units (Table 2). All but 1 study had a large sample size, with 1000‐patient days ranging from 11.1 to 160.3.9, 2124
| Included Study | Study Design | Study Period | Study Wards | Mean Age | Sample Size With Intervention (1000 Patient‐Days) | Sample Size in Control (1000 Patient‐Days) | Fall Rate With Intervention (Falls per 1000 Patient‐Days) | Fall Rate in Control (Falls per 1000 Patient‐Days) |
|---|---|---|---|---|---|---|---|---|
| ||||||||
| Dykes et al22 | RCT | 6 mo | 2 Medical units | 50% 65‐17% 65‐74 33% 75 | 24.1 | 24.1 | 4.18 | 4.64 |
| Krauss et al23 | Quasi‐experimental | 9 mo | General Medicine wards | 65.5 | 11.2 | 11.39 | 5.09 | 6.85 |
| Brandis21 | Pre/post | 12 mo | 500‐Bed acute care hospital | Not reported | 160.3 | 155.2 | 1.61 | 1.74 |
| Mitchell and Jones25 | Pre/post | 6 mo | Acute care hospital | 76.23 (Pre) 72.1 (Post) | 4.3 | 5 | 4.42 | 7.77 |
| Schwendimann et al9 | Pre/post | 4 yr | Internal Med, Surgery, and Geriatrics | 67.3 | 46.8 | 41.9 | 8.6 | 9.1 |
| Williams et al24 | Pre/post | 6 mo | 3 Medical wards and a Geriatrics ward | 79 | 15.88 | 12.53 | 8 | 9.5 |
Components of the Intervention
Multidisciplinary interventions were complex, and formulated based on available evidence for individual interventions and modifiable fall risk factors (Table 3). Each study reviewed included a fall risk assessment to risk‐stratify participants and modulate intervention according to risk.9, 2125
| Included Study | Fall Risk Assessment Used | Mobility Assessment and Assistance if Necessary | Mobility Aid Provided if Necessary | Medication Modification | Education About Risk Factors | Fall Risk Sign/Warning in Chart | Bedside Interventions (eg, Bed Alarm, Rail Adjustment, Bed Location/ Position, etc) | Toileting Schedule | Exercise Program | Other(s) |
|---|---|---|---|---|---|---|---|---|---|---|
| ||||||||||
| Dykes et al22* | + | + | + | + | + | + | + | + | Frequent bed checks, documented fall prevention plan | |
| Krauss et al23 | + | + | + | + | + | + | + | + | Use of bedside interventions was done based on discretion on a case‐by‐case basis | |
| Brandis21 | + | + | + | Ward modifications after OT assessment of patient rooms and bathrooms; hip protectors | ||||||
| Mitchell and Jones25 | + | + | + | + | Introduced detailed system to track fall details; used other preventive actions not specified | |||||
| Schwendimann et al9 | + | + | + | + | + | + | + | + | + | Reassessment of patients who did fall; hip protectors |
| Williams et al24 | + | + | + | + | + | + | Possible sitter | |||
Each study implemented fall prevention programs in a slightly different way. Krauss et al23 used nurses to complete a Morse Fall Scale and subsequently implement several standard interventions based on risk. Staff was then authorized to employ bedside interventions as necessary without systematic data collection. Schwendimann et al9 had nurses complete a simple fall risk assessment (based on history of falls, impaired mobility, and impaired cognition) that prompted the examination by a physician if risk was determined to be high. A subsequent team‐based intervention was employed with nursing, physiotherapy, and the physician. Brandis21 employed a team of nurses and the aid of the Director of Occupational Therapy to assess risk (using an undisclosed system) and carry out an intervention. Dykes et al22 examined an electronic fall prevention tool kit (FPTK) using the electronic medical record (EMR). This intervention began with the Morse Fall Score, which triggered automatically ordered interventions that did not require personal oversight. In fact, the multidisciplinary interventions in the intervention group were also used in the control arm. The difference was the automatic nature in which the interventions were ordered in the interventions arm. Williams et al24 used nurses and physiotherapists, who were specifically trained for the study, to carry out study interventions. The Mitchell and Jones25 study focused on nursing care alone to carry out intervention and used a novel risk assessment tool.
Fall Rates
Dykes et al22 and Williams et al24 found a statistically significant reduction in fall rate with falls reduced by 1.16 per 1000‐patient days and 1.5 per 1000‐patient days, respectively. Mitchell and Jones25 demonstrated a large fall reduction but had an extremely small sample size. Brandis21 found an extremely small reduction in fall rates and failed to report a P‐value. Krauss et al23 showed a trend towards reducing falls, and even showed a statistically significant reduction over the first 5 months of the study, but lost significance in the final 4 months. Similarly, Schwendimann et al9 saw more impressive fall reductions in the first year of the study that dissipated in the final 3 years of data collection.
Results from the meta‐analysis of the 6 studies comparing odds ratios are displayed quantitatively and as a forest plot in Figure 1. The figure shows results with 95% CI for each individual study and overall. There was no statistical evidence of heterogeneity between the studies or study designs. Although, due to the small number of studies included, there is poor power to detect true heterogeneity among studies. The magnitude of boxes shown is a relative sample size indicator. Using the random‐effects model, the summary odds ratio is 0.90 (95% CI, 0.83 to 0.99) (P = 0.02) (I2 = 0%).27
DISCUSSION
The frequency and morbidity associated with inpatient falls is well established, based on reproduced epidemiologic data. Reducing these adverse events could reduce morbidity, mortality, and healthcare costs, and has become the focus of most hospitals quality and patient safety initiatives. The focus of this review was to examine multidisciplinary efforts to reduce falls in acute care inpatient hospitals. Despite the importance and scope of the problem, there is a paucity of research available on this topic, with a wide literature search yielding only 6 primary research studies.
Our major finding is that multidisciplinary fall prevention strategies have a statistically significant impact on fall rates with a combined OR of 0.90. While this review demonstrates a significant benefit to multidisciplinary fall prevention strategies in the acute inpatient population, the clinical impact of these efforts may be limited. Based on rates ranging from 1.7 to 9.5 falls per 1000‐patient days, multidisciplinary interventions would reduce falls by 1 to 10 falls per 10,000‐patient days using the combined OR calculated of 0.9. Using other available incidence data regarding inpatient falls,4, 9 a reasonable baseline frequency to consider would be 8 falls per 1000 patient‐days. Assuming that prevalence, the number needed to treat (NNT) to prevent a single inpatient fall is 1250 patient days. Furthermore, based on available data, only approximately one‐third of these falls result in injury and only a minor fraction of these results in serious injury.9, 1113 The magnitude of this apparent benefit in the context of fall incidence rates raises some concerns about cost‐effectiveness given the high staffing and systems needs that multidisciplinary prevention programs require. This also suggests that there are limitations when using inpatient falls as a measure of healthcare quality given the absence of high‐quality evidence demonstrating a viable solution to the problem. At present, the Center for Medicare and Medicaid services limit reimbursement for fall‐related injuries if they occur during an acute inpatient hospitalization.28
The complexity of the interventions used may help explain the limited impact. Krauss et al23 examined compliance to their interventions and found less than ideal results. They found only 36.4% of intervention floor patients had maintained a toileting schedule compared to 24.6% on control floors. Additionally, a greater proportion of patients on control floors had a physical or occupational therapy consult, and only 1.8% more patients on intervention floors had walking aids provided. These were all strategies emphasized on the intervention floors. Similarly, Schwendimann et al9 questioned their staff's adherence to protocol after fall prevention committee audits. This may help explain why a potential benefit lost statistical significance with time, based on a natural tendency towards more participation at the beginning of a new policy. Williams et al24 reported only a 64% compliance rate with fall care plan forms and 77% rate of missing information on fall care plans. A multidisciplinary fall prevention study that did not meet inclusion criteria (based on study population) yielded strongly positive results for which the authors commented mostly on changing of the hospital culture surrounding fall prevention as a key to their success.29 Adoptability of a multidisciplinary intervention will clearly impact adherence and the intervention's ultimate effectiveness.
Single intervention strategies, not analyzed in this review, are simpler to execute and adhere to. While these types of interventions may be superior, there is extremely limited data supporting or refuting patient fall benefits in the acute care inpatient population when using simple single interventions. However, some data generated partially on acute care geriatrics wards targeting patient education only showed benefit.30
Dykes et al22 was able to improve compliance rates by removing steps in the process of executing interventions with the FPTK built into the EMR. Importantly, the FPTK was compared against very similar fall prevention strategies, the difference being that patients randomized to the FPTK arm had the assessment and interventions automatically prompted on admission in the EMR. Adherence was measured through Morse Fall Scale completion rates (81% in control units versus 94% in intervention units).22 In many ways, the utility of this study was displaying a fall risk reduction by simply enhancing compliance using health information technology with automated alerts. Additionally, both arms of the study reported low fall rates compared to previously reported data, and there may have been larger benefit seen if the FPTK was compared against no fall prevention strategy. This diminishing of effect size may have been present in all studies reviewed, as usual hospital care commonly includes basic patient safety measures.
Another potential problem with the multidisciplinary fall prevention programs included in the meta‐analysis is the inability to target interventions. Each study employed a fall risk score in an attempt to focus resources on a select group of high‐risk patients. This method is problematic given that countless risk factors for inpatient falls have been identified in the literature. Factors that have been described range from clinical characteristics to laboratory tests.31 The most consistently reproducible patient‐related risks are altered mental status (including cognitive impairment and depression), altered mobility (particularly lower limb weakness), a history of falls, and toileting needs.13, 3236 Less consistency is seen with other traditional risk factors such as age, sedating medication, and length of stay.5, 13, 32, 3638 Attempting to risk‐stratify patients using simple and accurate assessment tools developed from these risk factors has proven to be very difficult. Many tools have been developed based on identified risk factors, but perform very poorly when trying to identify patients who will fall with reasonable specificity and positive predictive value.34, 3944 In fact, it has been demonstrated that using a nurse's judgment, a physician's opinion based on a patient's likelihood to wander or a simple 2‐question tool have all performed better than sophisticated risk calculators.33, 45, 46 Therefore, it is possible that interventions could benefit from including all patients, with de‐emphasis on unproven risk stratification tools.
In contrast to our findings, a modest risk reduction has been demonstrated in several primary articles and meta‐analyses in the subacute, rehabilitation, and long‐term care populations.15, 16, 4750 Additionally, a recent study has described a 63.9% risk reduction in a population that included medical, surgical, psychiatric, and rehabilitation wards.29 One important difference between these settings and the acute inpatient populations may be the amount of time and energy that can be dedicated to fall prevention and overall care planning. Another likely factor is the added challenge of preventing falls in patients with more active medical illnesses. In the acute care setting, a patient's chief complaint may not be completely addressed at the time of first mobilization and ambulation. This may be most relevant in patients who are admitted with syncope, seizure, vertigo, and dehydration.
Our study has several limitations; most notably, the available evidence is limited in quality and quantity. Furthermore, omission of unpublished data may also lead to effect bias, though this would likely be in the direction of ineffective interventions supporting a conclusion that multidisciplinary efforts have had only a small impact on fall rates. Ideally, future studies can limit confounding variables through randomization. However, it is difficult to adequately blind when studying a multidisciplinary fall intervention that depends on patient and provider participation. As a result, none of the papers reviewed met criteria for high quality. However, almost all available data examined in this review came from large sample sizes in which thoughtful interventions were used. Since an inpatient fall will not affect the majority of patients, it was crucial for these studies to recruit a large sample size to have adequate power to detect a difference in fall rates. However, each study used risk assessment tools, which are poor indicators of who will and will not fall in the hospital.34, 39, 42 This may suggest a need for improved risk assessment tools, or be further evidence to include all patients in fall prevention regardless of risk. Quantitative synthesis of multidisciplinary fall interventions has the added limitation of comparing complex, multifaceted treatments that are not perfectly uniform. It is our opinion that interventions are semi‐standardized using the grouping methods employed in Table 3.
Preventing inpatient falls remains a difficult issue to address while convincing data is lacking. Based on current evidence, multidisciplinary fall prevention efforts on acutely ill inpatients show a possible small benefit and should be explored from a cost‐effectiveness standpoint to ensure they garner appropriate investment. Many resources are required to run such teams including nursing staff, equipment, physical and occupational therapy staff, pharmacists, and specialized staff training. We are unaware of any such cost‐effectiveness data available. Effective interventions may be those that maximize compliance through health information technology, maintain staff dedication, increase staff availability, improve risk assessment, or include all patients regardless of calculated fall risk, and take the patient's chief complaint into account in the fall prevention strategy. Where resources are limited, it appears most reasonable to focus on major risk factors for inpatient falls that have independently been shown to be detrimental to outcomes, such as delirium.51 Additionally, using inpatient fall rates as a hospital quality measure may be premature, given the lack of proven efforts to lower fall rates. Multidisciplinary fall prevention efforts on acutely ill inpatients should be further studied using high‐quality, randomized trials. It remains to be seen whether these large programs are cost‐effective, or on balance clinically effective.
Inpatient falls are the most common type of inpatient adverse event,1 persist as a significant problem nationally, and result in patient injury, increased length of stay, healthcare costs, and litigation.27 Inpatient falls remain a main focus of patient safety and a measure of quality in this era of healthcare reform and quality improvement.8 Inpatient fall rates per 1000 patient‐days range from 1.4 to 18.2.4, 9 The absolute percentage of inpatients that fall ranges from 1.3% to 7%.4, 5, 9, 10 Of inpatient falls, almost all data suggest that roughly one‐third result in some type of injury while 3%‐8% result in serious injury or death.9, 1113
Fall prevention interventions have largely been aimed at modifiable risk factors such as getting out of bed with bed alarms, toileting needs with bedside commodes, and reducing delirium through reorientation techniques. There have been several attempts at decreasing fall rates in hospitals surrounding a multidisciplinary, team‐based approach. Two Cochrane reviews and 2 meta‐analyses have partially examined this issue with mixed results.1417 However, none of these reviews focused on the acute care inpatient population. In fact, the majority of the data analyzed for inpatients was from rehabilitation wards and long‐term care wards. Additionally, there exists almost no data examining fall prevention with single interventions in the acute inpatient population, likely due to the belief that falls are multifactorial in etiology and require more comprehensive interventions.
The aim of this article is to determine the impact of team‐based, multidisciplinary quality improvement efforts to reduce inpatient falls in acute care inpatient hospitals and identify key features that determine their effectiveness.
METHODS
Data Sources and Searches
A search of MEDLINE, CINAHL, EMBASE, and the Cochrane Library was done using the medical subject heading (MeSH) terms accidental falls, accident prevention, inpatients, and prevention and control. Non‐English language publications were included in the search. The search encompassed all published literature through December 1, 2011. In addition, reference lists of all systematic reviews and meta‐analyses were searched to identify all possible studies available.1416
Study Selection
Only primary research studies relating to acute care inpatient hospital fall prevention were included. Data generated exclusively or partially from psychiatric wards, rehabilitation units, subacute facilities, and long‐term facilities were excluded from the review.
Data Extraction and Quality Assessment
Each selected study was carefully hand searched by 2 authors for the purposes of data extraction. Data were collected for the following study characteristics and outcome measures: details of the fall prevention intervention used (allowing for all interventions used to be recorded in Table 3), markers of study quality, study period, study population, mean age of participants, sample size (in 1000 patient‐days), and fall rates (in 1000 patient‐days). In certain cases, sample size was converted to patient‐days using reported data points of total number of patients and average length of stay.
Two authors with experience in fall literature discussed methodological quality and reached a consensus regarding scores using a 20‐point scale previously described in fall literature for all studies included.14, 15 Ten individual criteria were scored on a 0‐2 point scale. No points were awarded when the criteria were not met, not clearly mentioned, or not mentioned at all. One point was awarded when the criterion was partially met, and both points awarded when it was fully met.
Data Synthesis and Analysis
Fall rate per 1000‐patient days was derived from reported data in both intervention and non‐intervention groups within each study. Effect sizes (odds ratios [OR]) and 95% confidence intervals (CI) were derived for individual studies and then combined across research reports using an inverse weighted random‐effects meta‐analysis.18 Random effects methodology was chosen to account for within‐study and between‐study variation. Statistical heterogeneity between trials was assessed using the Cochrane Q statistic and reported as I2, which estimates the percentage of variability across studies that is not due to chance.19 Due to the low number of included studies in our analysis, a formal statistical test on publication bias was not meaningful.20 Statistical significance was defined as P 0.05. Data analyses were done using Comprehensive Meta‐Analysis, Version 2 (Biostat, Englewood, NJ).
RESULTS
Selected Studies
Electronic search produced 259 results on MEDLINE, 2 results from the Cochrane Library, 94 from CINAHL, and 4 from EMBASE. Each result was hand searched to exclude duplicates, and irrelevant studies. Once such data were excluded, the above inclusion and exclusion criteria identified 6 primary articles for review.9, 2125 Additionally, a cluster randomized fall prevention trial in a mixed inpatient population was published by Cumming et al26 in 2008. The study was excluded, as the participants were pooled between rehabilitation wards and acute inpatient wards, and only incomplete data were reported separately for the acute inpatient wards. We were unsuccessful at obtaining necessary data to analyze the acute inpatient wards.
Study Quality
The quality assessment results scores ranged from 11 to 14 out of a possible 20 (Table 1). None of the studies explicitly used an intention‐to‐treat statistical model, as the nature of inpatient care largely prevents drop‐out or crossover, and all patients were included in individual study results.
| Included Study | Clearly Defined Inclusion and Exclusion Criteria | Randomization | Comparable Treatment Groups at Entry | Identical Standard Program for Both Groups | Fall Incident Clearly Defined and Staff Trained in Definition | Blinded Treatment Providers | Blinded Outcome Assessors | Blinded Patients | Identical Appraisal of Outcomes* | Intention‐to‐ Treat Analysis | Total Score (0‐20) |
|---|---|---|---|---|---|---|---|---|---|---|---|
| |||||||||||
| Dykes et al22 | 2 | 2 | 2 | 2 | 2 | 0 | 0 | 0 | 2 | 2 | 14 |
| Krauss et al23 | 2 | 0 | 2 | 2 | 2 | 0 | 0 | 0 | 2 | 2 | 12 |
| Brandis21 | 1 | 0 | 1 | 2 | 2 | 0 | 0 | 0 | 2 | 2 | 10 |
| Mitchell and Jones25 | 2 | 0 | 1 | 2 | 2 | 0 | 0 | 0 | 2 | 2 | 11 |
| Schwendimann et al9 | 2 | 0 | 1 | 2 | 2 | 0 | 0 | 0 | 2 | 2 | 11 |
| Williams et al24 | 2 | 0 | 1 | 2 | 2 | 0 | 0 | 0 | 2 | 2 | 11 |
Study Characteristics
The available data are skewed towards elderly patients being hospitalized in general medicine or geriatric units (Table 2). All but 1 study had a large sample size, with 1000‐patient days ranging from 11.1 to 160.3.9, 2124
| Included Study | Study Design | Study Period | Study Wards | Mean Age | Sample Size With Intervention (1000 Patient‐Days) | Sample Size in Control (1000 Patient‐Days) | Fall Rate With Intervention (Falls per 1000 Patient‐Days) | Fall Rate in Control (Falls per 1000 Patient‐Days) |
|---|---|---|---|---|---|---|---|---|
| ||||||||
| Dykes et al22 | RCT | 6 mo | 2 Medical units | 50% 65‐17% 65‐74 33% 75 | 24.1 | 24.1 | 4.18 | 4.64 |
| Krauss et al23 | Quasi‐experimental | 9 mo | General Medicine wards | 65.5 | 11.2 | 11.39 | 5.09 | 6.85 |
| Brandis21 | Pre/post | 12 mo | 500‐Bed acute care hospital | Not reported | 160.3 | 155.2 | 1.61 | 1.74 |
| Mitchell and Jones25 | Pre/post | 6 mo | Acute care hospital | 76.23 (Pre) 72.1 (Post) | 4.3 | 5 | 4.42 | 7.77 |
| Schwendimann et al9 | Pre/post | 4 yr | Internal Med, Surgery, and Geriatrics | 67.3 | 46.8 | 41.9 | 8.6 | 9.1 |
| Williams et al24 | Pre/post | 6 mo | 3 Medical wards and a Geriatrics ward | 79 | 15.88 | 12.53 | 8 | 9.5 |
Components of the Intervention
Multidisciplinary interventions were complex, and formulated based on available evidence for individual interventions and modifiable fall risk factors (Table 3). Each study reviewed included a fall risk assessment to risk‐stratify participants and modulate intervention according to risk.9, 2125
| Included Study | Fall Risk Assessment Used | Mobility Assessment and Assistance if Necessary | Mobility Aid Provided if Necessary | Medication Modification | Education About Risk Factors | Fall Risk Sign/Warning in Chart | Bedside Interventions (eg, Bed Alarm, Rail Adjustment, Bed Location/ Position, etc) | Toileting Schedule | Exercise Program | Other(s) |
|---|---|---|---|---|---|---|---|---|---|---|
| ||||||||||
| Dykes et al22* | + | + | + | + | + | + | + | + | Frequent bed checks, documented fall prevention plan | |
| Krauss et al23 | + | + | + | + | + | + | + | + | Use of bedside interventions was done based on discretion on a case‐by‐case basis | |
| Brandis21 | + | + | + | Ward modifications after OT assessment of patient rooms and bathrooms; hip protectors | ||||||
| Mitchell and Jones25 | + | + | + | + | Introduced detailed system to track fall details; used other preventive actions not specified | |||||
| Schwendimann et al9 | + | + | + | + | + | + | + | + | + | Reassessment of patients who did fall; hip protectors |
| Williams et al24 | + | + | + | + | + | + | Possible sitter | |||
Each study implemented fall prevention programs in a slightly different way. Krauss et al23 used nurses to complete a Morse Fall Scale and subsequently implement several standard interventions based on risk. Staff was then authorized to employ bedside interventions as necessary without systematic data collection. Schwendimann et al9 had nurses complete a simple fall risk assessment (based on history of falls, impaired mobility, and impaired cognition) that prompted the examination by a physician if risk was determined to be high. A subsequent team‐based intervention was employed with nursing, physiotherapy, and the physician. Brandis21 employed a team of nurses and the aid of the Director of Occupational Therapy to assess risk (using an undisclosed system) and carry out an intervention. Dykes et al22 examined an electronic fall prevention tool kit (FPTK) using the electronic medical record (EMR). This intervention began with the Morse Fall Score, which triggered automatically ordered interventions that did not require personal oversight. In fact, the multidisciplinary interventions in the intervention group were also used in the control arm. The difference was the automatic nature in which the interventions were ordered in the interventions arm. Williams et al24 used nurses and physiotherapists, who were specifically trained for the study, to carry out study interventions. The Mitchell and Jones25 study focused on nursing care alone to carry out intervention and used a novel risk assessment tool.
Fall Rates
Dykes et al22 and Williams et al24 found a statistically significant reduction in fall rate with falls reduced by 1.16 per 1000‐patient days and 1.5 per 1000‐patient days, respectively. Mitchell and Jones25 demonstrated a large fall reduction but had an extremely small sample size. Brandis21 found an extremely small reduction in fall rates and failed to report a P‐value. Krauss et al23 showed a trend towards reducing falls, and even showed a statistically significant reduction over the first 5 months of the study, but lost significance in the final 4 months. Similarly, Schwendimann et al9 saw more impressive fall reductions in the first year of the study that dissipated in the final 3 years of data collection.
Results from the meta‐analysis of the 6 studies comparing odds ratios are displayed quantitatively and as a forest plot in Figure 1. The figure shows results with 95% CI for each individual study and overall. There was no statistical evidence of heterogeneity between the studies or study designs. Although, due to the small number of studies included, there is poor power to detect true heterogeneity among studies. The magnitude of boxes shown is a relative sample size indicator. Using the random‐effects model, the summary odds ratio is 0.90 (95% CI, 0.83 to 0.99) (P = 0.02) (I2 = 0%).27
DISCUSSION
The frequency and morbidity associated with inpatient falls is well established, based on reproduced epidemiologic data. Reducing these adverse events could reduce morbidity, mortality, and healthcare costs, and has become the focus of most hospitals quality and patient safety initiatives. The focus of this review was to examine multidisciplinary efforts to reduce falls in acute care inpatient hospitals. Despite the importance and scope of the problem, there is a paucity of research available on this topic, with a wide literature search yielding only 6 primary research studies.
Our major finding is that multidisciplinary fall prevention strategies have a statistically significant impact on fall rates with a combined OR of 0.90. While this review demonstrates a significant benefit to multidisciplinary fall prevention strategies in the acute inpatient population, the clinical impact of these efforts may be limited. Based on rates ranging from 1.7 to 9.5 falls per 1000‐patient days, multidisciplinary interventions would reduce falls by 1 to 10 falls per 10,000‐patient days using the combined OR calculated of 0.9. Using other available incidence data regarding inpatient falls,4, 9 a reasonable baseline frequency to consider would be 8 falls per 1000 patient‐days. Assuming that prevalence, the number needed to treat (NNT) to prevent a single inpatient fall is 1250 patient days. Furthermore, based on available data, only approximately one‐third of these falls result in injury and only a minor fraction of these results in serious injury.9, 1113 The magnitude of this apparent benefit in the context of fall incidence rates raises some concerns about cost‐effectiveness given the high staffing and systems needs that multidisciplinary prevention programs require. This also suggests that there are limitations when using inpatient falls as a measure of healthcare quality given the absence of high‐quality evidence demonstrating a viable solution to the problem. At present, the Center for Medicare and Medicaid services limit reimbursement for fall‐related injuries if they occur during an acute inpatient hospitalization.28
The complexity of the interventions used may help explain the limited impact. Krauss et al23 examined compliance to their interventions and found less than ideal results. They found only 36.4% of intervention floor patients had maintained a toileting schedule compared to 24.6% on control floors. Additionally, a greater proportion of patients on control floors had a physical or occupational therapy consult, and only 1.8% more patients on intervention floors had walking aids provided. These were all strategies emphasized on the intervention floors. Similarly, Schwendimann et al9 questioned their staff's adherence to protocol after fall prevention committee audits. This may help explain why a potential benefit lost statistical significance with time, based on a natural tendency towards more participation at the beginning of a new policy. Williams et al24 reported only a 64% compliance rate with fall care plan forms and 77% rate of missing information on fall care plans. A multidisciplinary fall prevention study that did not meet inclusion criteria (based on study population) yielded strongly positive results for which the authors commented mostly on changing of the hospital culture surrounding fall prevention as a key to their success.29 Adoptability of a multidisciplinary intervention will clearly impact adherence and the intervention's ultimate effectiveness.
Single intervention strategies, not analyzed in this review, are simpler to execute and adhere to. While these types of interventions may be superior, there is extremely limited data supporting or refuting patient fall benefits in the acute care inpatient population when using simple single interventions. However, some data generated partially on acute care geriatrics wards targeting patient education only showed benefit.30
Dykes et al22 was able to improve compliance rates by removing steps in the process of executing interventions with the FPTK built into the EMR. Importantly, the FPTK was compared against very similar fall prevention strategies, the difference being that patients randomized to the FPTK arm had the assessment and interventions automatically prompted on admission in the EMR. Adherence was measured through Morse Fall Scale completion rates (81% in control units versus 94% in intervention units).22 In many ways, the utility of this study was displaying a fall risk reduction by simply enhancing compliance using health information technology with automated alerts. Additionally, both arms of the study reported low fall rates compared to previously reported data, and there may have been larger benefit seen if the FPTK was compared against no fall prevention strategy. This diminishing of effect size may have been present in all studies reviewed, as usual hospital care commonly includes basic patient safety measures.
Another potential problem with the multidisciplinary fall prevention programs included in the meta‐analysis is the inability to target interventions. Each study employed a fall risk score in an attempt to focus resources on a select group of high‐risk patients. This method is problematic given that countless risk factors for inpatient falls have been identified in the literature. Factors that have been described range from clinical characteristics to laboratory tests.31 The most consistently reproducible patient‐related risks are altered mental status (including cognitive impairment and depression), altered mobility (particularly lower limb weakness), a history of falls, and toileting needs.13, 3236 Less consistency is seen with other traditional risk factors such as age, sedating medication, and length of stay.5, 13, 32, 3638 Attempting to risk‐stratify patients using simple and accurate assessment tools developed from these risk factors has proven to be very difficult. Many tools have been developed based on identified risk factors, but perform very poorly when trying to identify patients who will fall with reasonable specificity and positive predictive value.34, 3944 In fact, it has been demonstrated that using a nurse's judgment, a physician's opinion based on a patient's likelihood to wander or a simple 2‐question tool have all performed better than sophisticated risk calculators.33, 45, 46 Therefore, it is possible that interventions could benefit from including all patients, with de‐emphasis on unproven risk stratification tools.
In contrast to our findings, a modest risk reduction has been demonstrated in several primary articles and meta‐analyses in the subacute, rehabilitation, and long‐term care populations.15, 16, 4750 Additionally, a recent study has described a 63.9% risk reduction in a population that included medical, surgical, psychiatric, and rehabilitation wards.29 One important difference between these settings and the acute inpatient populations may be the amount of time and energy that can be dedicated to fall prevention and overall care planning. Another likely factor is the added challenge of preventing falls in patients with more active medical illnesses. In the acute care setting, a patient's chief complaint may not be completely addressed at the time of first mobilization and ambulation. This may be most relevant in patients who are admitted with syncope, seizure, vertigo, and dehydration.
Our study has several limitations; most notably, the available evidence is limited in quality and quantity. Furthermore, omission of unpublished data may also lead to effect bias, though this would likely be in the direction of ineffective interventions supporting a conclusion that multidisciplinary efforts have had only a small impact on fall rates. Ideally, future studies can limit confounding variables through randomization. However, it is difficult to adequately blind when studying a multidisciplinary fall intervention that depends on patient and provider participation. As a result, none of the papers reviewed met criteria for high quality. However, almost all available data examined in this review came from large sample sizes in which thoughtful interventions were used. Since an inpatient fall will not affect the majority of patients, it was crucial for these studies to recruit a large sample size to have adequate power to detect a difference in fall rates. However, each study used risk assessment tools, which are poor indicators of who will and will not fall in the hospital.34, 39, 42 This may suggest a need for improved risk assessment tools, or be further evidence to include all patients in fall prevention regardless of risk. Quantitative synthesis of multidisciplinary fall interventions has the added limitation of comparing complex, multifaceted treatments that are not perfectly uniform. It is our opinion that interventions are semi‐standardized using the grouping methods employed in Table 3.
Preventing inpatient falls remains a difficult issue to address while convincing data is lacking. Based on current evidence, multidisciplinary fall prevention efforts on acutely ill inpatients show a possible small benefit and should be explored from a cost‐effectiveness standpoint to ensure they garner appropriate investment. Many resources are required to run such teams including nursing staff, equipment, physical and occupational therapy staff, pharmacists, and specialized staff training. We are unaware of any such cost‐effectiveness data available. Effective interventions may be those that maximize compliance through health information technology, maintain staff dedication, increase staff availability, improve risk assessment, or include all patients regardless of calculated fall risk, and take the patient's chief complaint into account in the fall prevention strategy. Where resources are limited, it appears most reasonable to focus on major risk factors for inpatient falls that have independently been shown to be detrimental to outcomes, such as delirium.51 Additionally, using inpatient fall rates as a hospital quality measure may be premature, given the lack of proven efforts to lower fall rates. Multidisciplinary fall prevention efforts on acutely ill inpatients should be further studied using high‐quality, randomized trials. It remains to be seen whether these large programs are cost‐effective, or on balance clinically effective.
- ,,.Patient accidents in hospital: incidence, documentation and significance.Br J Clin Pract.1994;48(2):63–66.
- ,,,.Serious falls in hospitalized patients: correlates and resource utilization.Am J Med.1995;99(2):137–143.
- ,,,.Hospital falls: a persistent problem.Am J Public Health.1985;75(7):775–777.
- ,,.Falls in the acute hospital setting—impact on resource utilisation.Aust Health Rev.2007;31(3):471–477.
- ,,.Incidence and risk factors for inpatient falls in an academic acute‐care hospital.J Nippon Med Sch.2006;73(5):265–270.
- ,,,.Do falls and falls‐injuries in hospital indicate negligent care—and how big is the risk? A retrospective analysis of the NHS Litigation Authority Database of clinical negligence claims, resulting from falls in hospitals in England 1995 to 2006.Qual Saf Health Care.2008;17(6):431–436.
- ,,,.Hospital falls: development of a predictive model for clinical practice.Appl Nurs Res.1995;8(3):129–139.
- ,.Centers for Medicare and Medicaid Services' “never events”: an analysis and recommendations to hospitals.Health Care Manag (Frederick).2008;27(4):338–349.
- ,,,.Falls and consequent injuries in hospitalized patients: effects of an interdisciplinary falls prevention program.BMC Health Serv Res.2006;6:69.
- .Immobility and falls.Clin Geriatr Med.1998;14(4):699–726.
- ,,.A case control study of falls in the hospital setting.J Gerontol Nurs.1998;24(12):7–15.
- ,,,.A retrospective analysis of patient falls.Can J Public Health.1985;76(2):116–118.
- ,,, et al.Characteristics and circumstances of falls in a hospital setting: a prospective analysis.J Gen Intern Med.2004;19(7):732–739.
- ,,, et al.Interventions for preventing falls in older people in nursing care facilities and hospitals.Cochrane Database Syst Rev.2010(1):CD005465.
- , L,,,,.Interventions for preventing falls in acute‐ and chronic‐care hospitals: a systematic review and meta‐analysis.J Am Geriatr Soc.2008;56(1):29–36.
- ,,, et al.Strategies to prevent falls and fractures in hospitals and care homes and effect of cognitive impairment: systematic review and meta‐analyses.BMJ.2007;334(7584):82.
- ,,,,,.Interventions for preventing falls in elderly people.Cochrane Database Syst Rev.2003(4):CD000340.
- ,,,.Introduction to Meta‐Analysis.Chichester, UK:John Wiley 2009.
- ,.Quantifying heterogeneity in a meta‐analysis.Stat Med.2002;21(11):1539–1558.
- .The power of the standard test for the presence of heterogeneity in meta‐analysis.Stat Med.2006;25(15):2688–2699.
- .A collaborative occupational therapy and nursing approach to falls prevention in hospital inpatients.J Qual Clin Pract.1999;19(4):215–220.
- ,,, et al.Fall prevention in acute care hospitals: a randomized trial.JAMA.2010;304(17):1912–1918.
- ,,,,,.Intervention to prevent falls on the medical service in a teaching hospital.Infect Control Hosp Epidemiol.2008;29(6):539–545.
- ,,, et al.Evaluation of a falls prevention programme in an acute tertiary care hospital.J Clin Nurs.2007;16(2):316–324.
- ,.Striving to prevent falls in an acute care setting—action to enhance quality.J Clin Nurs.1996;5(4):213–220.
- ,,, et al.Cluster randomised trial of a targeted multifactorial intervention to prevent falls among older people in hospital.BMJ.2008;336(7647):758–760.
- ,.Graphical displays for meta‐analysis: an overview with suggestions for practice.Res Syn Meth.2010(1):66–80.
- Centers for Medicare 37(7):317–325.
- ,‐M,, et al.Patient education to prevent falls among older hospital inpatients: a randomized controlled trial.Arch Intern Med.2011;117:516–524.
- ,.The relationship between patient blood pathology values and patient falls in an acute‐care setting: a retrospective analysis.Int J Nurs Pract.2005;11(4):161–168.
- ,,,.Falls risk factors in the hospital setting: a systematic review.Int J Nurs Pract.2001;7(1):38–45.
- ,,.A simplified fall‐risk assessment tool for patients hospitalized in medical wards.Isr Med Assoc J.2008;10(2):125–129.
- ,,,.Risk factors and risk assessment tools for falls in hospital in‐patients: a systematic review.Age Ageing.2004;33(2):122–130.
- ,,, et al.Circumstances of patient falls and injuries in 9 hospitals in a midwestern healthcare system.Infect Control Hosp Epidemiol.2007;28(5):544–550.
- ,,, et al.A case‐control study of patient, medication, and care‐related risk factors for inpatient falls.J Gen Intern Med.2005;20(2):116–122.
- .The experience of a community hospital in quantifying and reducing patient falls.J Nurs Care Qual.2000;14(3):43–53.
- ,,,.Characteristics of hospital inpatient falls across clinical departments.Gerontology.2008;54(6):342–348.
- ,.Falls risk prediction tools for hospital inpatients: do they work?Nurs Times.2009;105(7):18–21.
- ,,,.Accidental falls in hospital inpatients: evaluation of sensitivity and specificity of two risk assessment tools.J Adv Nurs.2010;66(3):690–696.
- ,,,,,.A systematic review and meta‐analysis of studies using the STRATIFY tool for prediction of falls in hospital patients: how well does it work?Age Ageing.2008;37(6):621–627.
- .Falls risk‐prediction tools for hospital inpatients. Time to put them to bed?Age Ageing.2008;37(3):248–250.
- ,,,,.Evaluation of three fall‐risk assessment tools in an acute care setting.J Adv Nurs.2007;60(4):427–435.
- ,,, et al.Fall prediction in inpatients by bedside nurses using the St. Thomas's Risk Assessment Tool in Falling Elderly Inpatients (STRATIFY) instrument: a multicenter study.J Am Geriatr Soc.2007;55(5):725–733.
- ,,,.Comparison of a fall risk assessment tool with nurses' judgement alone: a cluster‐randomised controlled trial.Age Ageing.2009;38(4):417–423.
- ,,,,.Fall risk‐assessment tools compared with clinical judgment: an evaluation in a rehabilitation ward.Age Ageing.2008;37(3):277–281.
- ,.Incidence of in‐hospital falls in geriatric patients before and after the introduction of an interdisciplinary team‐based fall‐prevention intervention.J Am Geriatr Soc.2007;55(12):2068–2074.
- ,,,.Sustained reduction in serious fall‐related injuries in older people in hospital.Med J Aust.2006;184(8):379–382.
- ,,, et al.The effect of changing practice on fall prevention in a rehabilitative hospital: the Hospital Injury Prevention Study.J Am Geriatr Soc.2004;52(3):335–339.
- ,,,.Effectiveness of targeted falls prevention programme in subacute hospital setting: randomised controlled trial.BMJ.2004;328(7441):676.
- ,,,,.Does delirium contribute to poor hospital outcomes? A three‐site epidemiologic study.J Gen Intern Med.1998;13(4):234–242.
- ,,.Patient accidents in hospital: incidence, documentation and significance.Br J Clin Pract.1994;48(2):63–66.
- ,,,.Serious falls in hospitalized patients: correlates and resource utilization.Am J Med.1995;99(2):137–143.
- ,,,.Hospital falls: a persistent problem.Am J Public Health.1985;75(7):775–777.
- ,,.Falls in the acute hospital setting—impact on resource utilisation.Aust Health Rev.2007;31(3):471–477.
- ,,.Incidence and risk factors for inpatient falls in an academic acute‐care hospital.J Nippon Med Sch.2006;73(5):265–270.
- ,,,.Do falls and falls‐injuries in hospital indicate negligent care—and how big is the risk? A retrospective analysis of the NHS Litigation Authority Database of clinical negligence claims, resulting from falls in hospitals in England 1995 to 2006.Qual Saf Health Care.2008;17(6):431–436.
- ,,,.Hospital falls: development of a predictive model for clinical practice.Appl Nurs Res.1995;8(3):129–139.
- ,.Centers for Medicare and Medicaid Services' “never events”: an analysis and recommendations to hospitals.Health Care Manag (Frederick).2008;27(4):338–349.
- ,,,.Falls and consequent injuries in hospitalized patients: effects of an interdisciplinary falls prevention program.BMC Health Serv Res.2006;6:69.
- .Immobility and falls.Clin Geriatr Med.1998;14(4):699–726.
- ,,.A case control study of falls in the hospital setting.J Gerontol Nurs.1998;24(12):7–15.
- ,,,.A retrospective analysis of patient falls.Can J Public Health.1985;76(2):116–118.
- ,,, et al.Characteristics and circumstances of falls in a hospital setting: a prospective analysis.J Gen Intern Med.2004;19(7):732–739.
- ,,, et al.Interventions for preventing falls in older people in nursing care facilities and hospitals.Cochrane Database Syst Rev.2010(1):CD005465.
- , L,,,,.Interventions for preventing falls in acute‐ and chronic‐care hospitals: a systematic review and meta‐analysis.J Am Geriatr Soc.2008;56(1):29–36.
- ,,, et al.Strategies to prevent falls and fractures in hospitals and care homes and effect of cognitive impairment: systematic review and meta‐analyses.BMJ.2007;334(7584):82.
- ,,,,,.Interventions for preventing falls in elderly people.Cochrane Database Syst Rev.2003(4):CD000340.
- ,,,.Introduction to Meta‐Analysis.Chichester, UK:John Wiley 2009.
- ,.Quantifying heterogeneity in a meta‐analysis.Stat Med.2002;21(11):1539–1558.
- .The power of the standard test for the presence of heterogeneity in meta‐analysis.Stat Med.2006;25(15):2688–2699.
- .A collaborative occupational therapy and nursing approach to falls prevention in hospital inpatients.J Qual Clin Pract.1999;19(4):215–220.
- ,,, et al.Fall prevention in acute care hospitals: a randomized trial.JAMA.2010;304(17):1912–1918.
- ,,,,,.Intervention to prevent falls on the medical service in a teaching hospital.Infect Control Hosp Epidemiol.2008;29(6):539–545.
- ,,, et al.Evaluation of a falls prevention programme in an acute tertiary care hospital.J Clin Nurs.2007;16(2):316–324.
- ,.Striving to prevent falls in an acute care setting—action to enhance quality.J Clin Nurs.1996;5(4):213–220.
- ,,, et al.Cluster randomised trial of a targeted multifactorial intervention to prevent falls among older people in hospital.BMJ.2008;336(7647):758–760.
- ,.Graphical displays for meta‐analysis: an overview with suggestions for practice.Res Syn Meth.2010(1):66–80.
- Centers for Medicare 37(7):317–325.
- ,‐M,, et al.Patient education to prevent falls among older hospital inpatients: a randomized controlled trial.Arch Intern Med.2011;117:516–524.
- ,.The relationship between patient blood pathology values and patient falls in an acute‐care setting: a retrospective analysis.Int J Nurs Pract.2005;11(4):161–168.
- ,,,.Falls risk factors in the hospital setting: a systematic review.Int J Nurs Pract.2001;7(1):38–45.
- ,,.A simplified fall‐risk assessment tool for patients hospitalized in medical wards.Isr Med Assoc J.2008;10(2):125–129.
- ,,,.Risk factors and risk assessment tools for falls in hospital in‐patients: a systematic review.Age Ageing.2004;33(2):122–130.
- ,,, et al.Circumstances of patient falls and injuries in 9 hospitals in a midwestern healthcare system.Infect Control Hosp Epidemiol.2007;28(5):544–550.
- ,,, et al.A case‐control study of patient, medication, and care‐related risk factors for inpatient falls.J Gen Intern Med.2005;20(2):116–122.
- .The experience of a community hospital in quantifying and reducing patient falls.J Nurs Care Qual.2000;14(3):43–53.
- ,,,.Characteristics of hospital inpatient falls across clinical departments.Gerontology.2008;54(6):342–348.
- ,.Falls risk prediction tools for hospital inpatients: do they work?Nurs Times.2009;105(7):18–21.
- ,,,.Accidental falls in hospital inpatients: evaluation of sensitivity and specificity of two risk assessment tools.J Adv Nurs.2010;66(3):690–696.
- ,,,,,.A systematic review and meta‐analysis of studies using the STRATIFY tool for prediction of falls in hospital patients: how well does it work?Age Ageing.2008;37(6):621–627.
- .Falls risk‐prediction tools for hospital inpatients. Time to put them to bed?Age Ageing.2008;37(3):248–250.
- ,,,,.Evaluation of three fall‐risk assessment tools in an acute care setting.J Adv Nurs.2007;60(4):427–435.
- ,,, et al.Fall prediction in inpatients by bedside nurses using the St. Thomas's Risk Assessment Tool in Falling Elderly Inpatients (STRATIFY) instrument: a multicenter study.J Am Geriatr Soc.2007;55(5):725–733.
- ,,,.Comparison of a fall risk assessment tool with nurses' judgement alone: a cluster‐randomised controlled trial.Age Ageing.2009;38(4):417–423.
- ,,,,.Fall risk‐assessment tools compared with clinical judgment: an evaluation in a rehabilitation ward.Age Ageing.2008;37(3):277–281.
- ,.Incidence of in‐hospital falls in geriatric patients before and after the introduction of an interdisciplinary team‐based fall‐prevention intervention.J Am Geriatr Soc.2007;55(12):2068–2074.
- ,,,.Sustained reduction in serious fall‐related injuries in older people in hospital.Med J Aust.2006;184(8):379–382.
- ,,, et al.The effect of changing practice on fall prevention in a rehabilitative hospital: the Hospital Injury Prevention Study.J Am Geriatr Soc.2004;52(3):335–339.
- ,,,.Effectiveness of targeted falls prevention programme in subacute hospital setting: randomised controlled trial.BMJ.2004;328(7441):676.
- ,,,,.Does delirium contribute to poor hospital outcomes? A three‐site epidemiologic study.J Gen Intern Med.1998;13(4):234–242.