User login
The American Board of Pediatrics Response to the Pediatric Hospital Medicine Petition
In August of 2014, the Pediatric Hospital Medicine (PHM) community petitioned the American Board of Pediatrics (ABP) for a subspecialty certificate in PHM. A lengthy vetting process ensued during which the ABP consulted with a wide array of stakeholders. The ABP Board of Directors approved the request from the PHM community for a subspecialty certificate in December 2015 and published the results of the vetting process.1
The ABP received a second petition posted on PHM listserv, which opened with the following statement:
“We submit this petition letter to register a formal complaint, demand immediate action, and request a formal response from the ABP regarding the practice pathway criteria and the application of these criteria for the Pediatric Hospital Medicine specialty exam. Recently there has been considerable discussion on the Pediatric Hospital Medicine ListServ suggesting that the ABP’s implementation of the career pathway criteria has failed to respect and fairly assess the diverse career paths of numerous experienced pediatric hospitalists, which may impede their opportunities for professional advancement. Anecdotal reports on the ListServ also suggest that the use of the current practice pathway criteria to evaluate exam applicants disadvantages women, though sufficient data is not available at this time to evaluate this assertion objectively.”
The ABP response to the PHM community’s concerns regarding the practice pathway for the first certifying exam in PHM is as follows.
THE ABP RESPONSE
ABP thanks the PHM community for the opportunity to respond to the attached petition. Our approach and response are grounded in our mission:
“Advancing child health by certifying pediatricians who meet standards of excellence and are committed to continuous learning and improvement.”
Transparency is one of the ABP’s core values, which underpins this response. The ABP acknowledges that the petitioners did not find the guidance on the ABP website sufficiently transparent. We regret the distress this may have caused, will do our best to answer the questions forthrightly, and have revised the website language for greater clarity.
ALLEGATION OF GENDER BIAS
Some posts on the PHM listserv alleged gender (sex) bias against women in the ABP application process and outcomes. This allegation is not supported by the facts. A peer group of pediatric hospitalists constitutes the ABP PHM subboard which determined the eligibility criteria. The subboard thoughtfully developed these criteria and the American Board of Medical Specialties (ABMS) approved the broad eligibility criteria. The PHM subboard is composed of practicing pediatric hospitalists with a diversity of practice location, age, gender, and race. The majority of ABP PHM subboard members and medical editors are women.
Making unbiased decisions is also a core value of the ABP. Among the 1,627 applicants for the exam, the ABP has approved 1,515 (93%) as of August 15, 2019. Seventy percent of applications were from women, which mirrors the demographics of the pediatric workforce. There was no significant difference between the percentage of women (4.0%) and men (3.7%) who were denied admission to the exam (Table 1). As of August 15, 2019, the credentials committee of the PHM subboard is still reviewing 48 applications, including 35 appeals, of which 60% (N = 21) were from women and 40% (N = 14) were from men. Thirteen (N = 13) remaining applications are under review but not in the appeals process.
PRACTICE PATHWAY CRITERIA USED IN THE APPLICATION PROCESS
PHM is the 15th pediatric subspecialty to begin the certification process with a practice pathway. In none of the prior cases was it possible to do a detailed implementation study to understand the myriad of ways in which individual pediatricians arrange their professional and personal time. This reality has led to the publication of only general, rather than specific practice pathway criteria at the start of the application process for PHM and every other pediatric subspecialty. Rather, in each case, a well-informed and diverse peer group of subspecialists (the subboard) has reviewed the applications to get a sense of the variations of practice and then decided on the criteria that a subspecialist must meet to be considered eligible to sit for the certifying exam. Clear-cut criteria were used consistently in adjudicating all applications. Although the ABP has not done this for other subspecialties, we agree that publishing the specific criteria once they had been decided upon would have improved the process. We commit to doing so in the future.
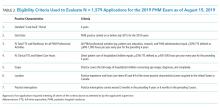
The eligibility criteria were designed to be true to the mission of the ABP and seek parity with the requirements used by other subspecialties and by the PHM training pathway. The assumption is that competent PHM practice of sufficient duration and breadth, attested to by a supervisor, would allow the ABP to represent to the public that the candidate is qualified to sit for the exam. The eligibility criteria focused on seven practice characteristics (Table 2):
(2) The July 2015 start date follows from the four-year look-back window for the November 2019 exam date.
(3) The minimum percentage full-time equivalent (%FTE) for all PHM professional activities (ie, clinical care, research, education, and PHM administration) was set at 50% FTE. Recognizing that an FTE may be defined differently at different institutions, the ABP defined the workweek as 40 hours and the 50% FTE as 900-1,000 hours per year.
(4) The minimum percentage FTE for PHM direct patient care (as described below) was set at 25% FTE and defined as 450-500 hours per year. Every candidate must satisfy both the minimum hours for all PHM professional activities and the minimum hours for the direct care of hospitalized children. Applicants must meet or exceed these minima if the ABP is to represent to the public that an applicant has the necessary experience to be called a subspecialist. Similarly, all other ABP subspecialties required at least 50% FTE commitment for the candidate to be considered a subspecialist.
(5) The scope of practice seeks to maintain parity with the training pathway by requiring care of the full spectrum of hospitalized children. This full spectrum is defined as children on general pediatric wards, ages birth to 21 years, and specifically includes children with complex chronic disease, surgical care and comanagement, sedation, palliative care, and common procedures. Care devoted exclusively to a narrow patient population (“niched care”), such as newborns in the nursery, does not meet the eligibility requirements.
(6) The location for patient care must have occurred in the United States or Canada.
(7) The possibility of practice interruption was included among the eligibility criteria. Attempting to strike a balance between an applicant demonstrating sufficient recent experience to be called a subspecialist versus the reality of some individuals needing to interrupt professional and clinical practice, the subboard stipulated that interruptions of PHM professional activities should not exceed three months during the preceding four years and six months during the preceding five years.
CLARIFICATION AND SIMPLIFICATION OF ELIGIBILITY CRITERIA
The ABP recognizes that the use of %FTE, work hours, and leave exceptions led to unintended confusion among applicants. The intent had been to acknowledge the many valid reasons for interruption of practice, including parental leave. This response to the petition clarifies that the critical question from the public’s perspective is whether the candidate has accumulated enough hours of sustained practice to be considered competent in the field of PHM and specifically caring for hospitalized children (as defined above). Upon review, the ABP believes the workhours criteria (items 3 and 4) accomplish this critical goal and make the %FTE and practice interruption criteria largely redundant. Table 3 reflects the clarified and streamlined requirements. Re-examination of all the denied applications showed that using the criteria in Table 3 did not have a significant impact on the outcomes. One additional applicant’s appeal was granted, and this applicant has been so notified.
APPEALS PROCESS
The right to appeal and the Appellate Review Procedure are included in a denial letter. The applicant is given a deadline of 14 days to notify the ABP of the intent to appeal. There is no appellate fee. Within one to three days, the ABP acknowledges receipt of the applicant’s intent to appeal and sends the applicant a date by which additional supporting information should be provided.
The appeal material is shared with the subboard credentials committee and each member individually reviews and votes on the appeal. The application is approved if a majority votes in favor of the applicant’s appeal. If there is no majority, the credentials committee discusses the case to reach a decision. The results of the appeal are final according to the ABP Appellate Review Procedure. We remain in the appeal process for several PHM applicants as of the date of this response.
Thank you for the opportunity to respond to the petition. The ABP is committed to dialogue, transparency, and continuously improving its processes.
Acknowledgment
The authors thank the ABP board of directors and the ABP PHM subboard for their review and thoughtful contributions.
Disclosures
Dr. Nichols reports other from The American Board of Pediatrics, during the conduct of the work. Dr. Woods has nothing to disclose.
1. Barrett DJ, McGuinness GA, Cunha CA, et al. Pediatric hospital medicine: A proposed new subspecialty. Pediatrics. 2017;139(3). https://doi.org/10.1542/peds.2016-1823.
In August of 2014, the Pediatric Hospital Medicine (PHM) community petitioned the American Board of Pediatrics (ABP) for a subspecialty certificate in PHM. A lengthy vetting process ensued during which the ABP consulted with a wide array of stakeholders. The ABP Board of Directors approved the request from the PHM community for a subspecialty certificate in December 2015 and published the results of the vetting process.1
The ABP received a second petition posted on PHM listserv, which opened with the following statement:
“We submit this petition letter to register a formal complaint, demand immediate action, and request a formal response from the ABP regarding the practice pathway criteria and the application of these criteria for the Pediatric Hospital Medicine specialty exam. Recently there has been considerable discussion on the Pediatric Hospital Medicine ListServ suggesting that the ABP’s implementation of the career pathway criteria has failed to respect and fairly assess the diverse career paths of numerous experienced pediatric hospitalists, which may impede their opportunities for professional advancement. Anecdotal reports on the ListServ also suggest that the use of the current practice pathway criteria to evaluate exam applicants disadvantages women, though sufficient data is not available at this time to evaluate this assertion objectively.”
The ABP response to the PHM community’s concerns regarding the practice pathway for the first certifying exam in PHM is as follows.
THE ABP RESPONSE
ABP thanks the PHM community for the opportunity to respond to the attached petition. Our approach and response are grounded in our mission:
“Advancing child health by certifying pediatricians who meet standards of excellence and are committed to continuous learning and improvement.”
Transparency is one of the ABP’s core values, which underpins this response. The ABP acknowledges that the petitioners did not find the guidance on the ABP website sufficiently transparent. We regret the distress this may have caused, will do our best to answer the questions forthrightly, and have revised the website language for greater clarity.
ALLEGATION OF GENDER BIAS
Some posts on the PHM listserv alleged gender (sex) bias against women in the ABP application process and outcomes. This allegation is not supported by the facts. A peer group of pediatric hospitalists constitutes the ABP PHM subboard which determined the eligibility criteria. The subboard thoughtfully developed these criteria and the American Board of Medical Specialties (ABMS) approved the broad eligibility criteria. The PHM subboard is composed of practicing pediatric hospitalists with a diversity of practice location, age, gender, and race. The majority of ABP PHM subboard members and medical editors are women.
Making unbiased decisions is also a core value of the ABP. Among the 1,627 applicants for the exam, the ABP has approved 1,515 (93%) as of August 15, 2019. Seventy percent of applications were from women, which mirrors the demographics of the pediatric workforce. There was no significant difference between the percentage of women (4.0%) and men (3.7%) who were denied admission to the exam (Table 1). As of August 15, 2019, the credentials committee of the PHM subboard is still reviewing 48 applications, including 35 appeals, of which 60% (N = 21) were from women and 40% (N = 14) were from men. Thirteen (N = 13) remaining applications are under review but not in the appeals process.
PRACTICE PATHWAY CRITERIA USED IN THE APPLICATION PROCESS
PHM is the 15th pediatric subspecialty to begin the certification process with a practice pathway. In none of the prior cases was it possible to do a detailed implementation study to understand the myriad of ways in which individual pediatricians arrange their professional and personal time. This reality has led to the publication of only general, rather than specific practice pathway criteria at the start of the application process for PHM and every other pediatric subspecialty. Rather, in each case, a well-informed and diverse peer group of subspecialists (the subboard) has reviewed the applications to get a sense of the variations of practice and then decided on the criteria that a subspecialist must meet to be considered eligible to sit for the certifying exam. Clear-cut criteria were used consistently in adjudicating all applications. Although the ABP has not done this for other subspecialties, we agree that publishing the specific criteria once they had been decided upon would have improved the process. We commit to doing so in the future.
The eligibility criteria were designed to be true to the mission of the ABP and seek parity with the requirements used by other subspecialties and by the PHM training pathway. The assumption is that competent PHM practice of sufficient duration and breadth, attested to by a supervisor, would allow the ABP to represent to the public that the candidate is qualified to sit for the exam. The eligibility criteria focused on seven practice characteristics (Table 2):
(2) The July 2015 start date follows from the four-year look-back window for the November 2019 exam date.
(3) The minimum percentage full-time equivalent (%FTE) for all PHM professional activities (ie, clinical care, research, education, and PHM administration) was set at 50% FTE. Recognizing that an FTE may be defined differently at different institutions, the ABP defined the workweek as 40 hours and the 50% FTE as 900-1,000 hours per year.
(4) The minimum percentage FTE for PHM direct patient care (as described below) was set at 25% FTE and defined as 450-500 hours per year. Every candidate must satisfy both the minimum hours for all PHM professional activities and the minimum hours for the direct care of hospitalized children. Applicants must meet or exceed these minima if the ABP is to represent to the public that an applicant has the necessary experience to be called a subspecialist. Similarly, all other ABP subspecialties required at least 50% FTE commitment for the candidate to be considered a subspecialist.
(5) The scope of practice seeks to maintain parity with the training pathway by requiring care of the full spectrum of hospitalized children. This full spectrum is defined as children on general pediatric wards, ages birth to 21 years, and specifically includes children with complex chronic disease, surgical care and comanagement, sedation, palliative care, and common procedures. Care devoted exclusively to a narrow patient population (“niched care”), such as newborns in the nursery, does not meet the eligibility requirements.
(6) The location for patient care must have occurred in the United States or Canada.
(7) The possibility of practice interruption was included among the eligibility criteria. Attempting to strike a balance between an applicant demonstrating sufficient recent experience to be called a subspecialist versus the reality of some individuals needing to interrupt professional and clinical practice, the subboard stipulated that interruptions of PHM professional activities should not exceed three months during the preceding four years and six months during the preceding five years.
CLARIFICATION AND SIMPLIFICATION OF ELIGIBILITY CRITERIA
The ABP recognizes that the use of %FTE, work hours, and leave exceptions led to unintended confusion among applicants. The intent had been to acknowledge the many valid reasons for interruption of practice, including parental leave. This response to the petition clarifies that the critical question from the public’s perspective is whether the candidate has accumulated enough hours of sustained practice to be considered competent in the field of PHM and specifically caring for hospitalized children (as defined above). Upon review, the ABP believes the workhours criteria (items 3 and 4) accomplish this critical goal and make the %FTE and practice interruption criteria largely redundant. Table 3 reflects the clarified and streamlined requirements. Re-examination of all the denied applications showed that using the criteria in Table 3 did not have a significant impact on the outcomes. One additional applicant’s appeal was granted, and this applicant has been so notified.
APPEALS PROCESS
The right to appeal and the Appellate Review Procedure are included in a denial letter. The applicant is given a deadline of 14 days to notify the ABP of the intent to appeal. There is no appellate fee. Within one to three days, the ABP acknowledges receipt of the applicant’s intent to appeal and sends the applicant a date by which additional supporting information should be provided.
The appeal material is shared with the subboard credentials committee and each member individually reviews and votes on the appeal. The application is approved if a majority votes in favor of the applicant’s appeal. If there is no majority, the credentials committee discusses the case to reach a decision. The results of the appeal are final according to the ABP Appellate Review Procedure. We remain in the appeal process for several PHM applicants as of the date of this response.
Thank you for the opportunity to respond to the petition. The ABP is committed to dialogue, transparency, and continuously improving its processes.
Acknowledgment
The authors thank the ABP board of directors and the ABP PHM subboard for their review and thoughtful contributions.
Disclosures
Dr. Nichols reports other from The American Board of Pediatrics, during the conduct of the work. Dr. Woods has nothing to disclose.
In August of 2014, the Pediatric Hospital Medicine (PHM) community petitioned the American Board of Pediatrics (ABP) for a subspecialty certificate in PHM. A lengthy vetting process ensued during which the ABP consulted with a wide array of stakeholders. The ABP Board of Directors approved the request from the PHM community for a subspecialty certificate in December 2015 and published the results of the vetting process.1
The ABP received a second petition posted on PHM listserv, which opened with the following statement:
“We submit this petition letter to register a formal complaint, demand immediate action, and request a formal response from the ABP regarding the practice pathway criteria and the application of these criteria for the Pediatric Hospital Medicine specialty exam. Recently there has been considerable discussion on the Pediatric Hospital Medicine ListServ suggesting that the ABP’s implementation of the career pathway criteria has failed to respect and fairly assess the diverse career paths of numerous experienced pediatric hospitalists, which may impede their opportunities for professional advancement. Anecdotal reports on the ListServ also suggest that the use of the current practice pathway criteria to evaluate exam applicants disadvantages women, though sufficient data is not available at this time to evaluate this assertion objectively.”
The ABP response to the PHM community’s concerns regarding the practice pathway for the first certifying exam in PHM is as follows.
THE ABP RESPONSE
ABP thanks the PHM community for the opportunity to respond to the attached petition. Our approach and response are grounded in our mission:
“Advancing child health by certifying pediatricians who meet standards of excellence and are committed to continuous learning and improvement.”
Transparency is one of the ABP’s core values, which underpins this response. The ABP acknowledges that the petitioners did not find the guidance on the ABP website sufficiently transparent. We regret the distress this may have caused, will do our best to answer the questions forthrightly, and have revised the website language for greater clarity.
ALLEGATION OF GENDER BIAS
Some posts on the PHM listserv alleged gender (sex) bias against women in the ABP application process and outcomes. This allegation is not supported by the facts. A peer group of pediatric hospitalists constitutes the ABP PHM subboard which determined the eligibility criteria. The subboard thoughtfully developed these criteria and the American Board of Medical Specialties (ABMS) approved the broad eligibility criteria. The PHM subboard is composed of practicing pediatric hospitalists with a diversity of practice location, age, gender, and race. The majority of ABP PHM subboard members and medical editors are women.
Making unbiased decisions is also a core value of the ABP. Among the 1,627 applicants for the exam, the ABP has approved 1,515 (93%) as of August 15, 2019. Seventy percent of applications were from women, which mirrors the demographics of the pediatric workforce. There was no significant difference between the percentage of women (4.0%) and men (3.7%) who were denied admission to the exam (Table 1). As of August 15, 2019, the credentials committee of the PHM subboard is still reviewing 48 applications, including 35 appeals, of which 60% (N = 21) were from women and 40% (N = 14) were from men. Thirteen (N = 13) remaining applications are under review but not in the appeals process.
PRACTICE PATHWAY CRITERIA USED IN THE APPLICATION PROCESS
PHM is the 15th pediatric subspecialty to begin the certification process with a practice pathway. In none of the prior cases was it possible to do a detailed implementation study to understand the myriad of ways in which individual pediatricians arrange their professional and personal time. This reality has led to the publication of only general, rather than specific practice pathway criteria at the start of the application process for PHM and every other pediatric subspecialty. Rather, in each case, a well-informed and diverse peer group of subspecialists (the subboard) has reviewed the applications to get a sense of the variations of practice and then decided on the criteria that a subspecialist must meet to be considered eligible to sit for the certifying exam. Clear-cut criteria were used consistently in adjudicating all applications. Although the ABP has not done this for other subspecialties, we agree that publishing the specific criteria once they had been decided upon would have improved the process. We commit to doing so in the future.
The eligibility criteria were designed to be true to the mission of the ABP and seek parity with the requirements used by other subspecialties and by the PHM training pathway. The assumption is that competent PHM practice of sufficient duration and breadth, attested to by a supervisor, would allow the ABP to represent to the public that the candidate is qualified to sit for the exam. The eligibility criteria focused on seven practice characteristics (Table 2):
(2) The July 2015 start date follows from the four-year look-back window for the November 2019 exam date.
(3) The minimum percentage full-time equivalent (%FTE) for all PHM professional activities (ie, clinical care, research, education, and PHM administration) was set at 50% FTE. Recognizing that an FTE may be defined differently at different institutions, the ABP defined the workweek as 40 hours and the 50% FTE as 900-1,000 hours per year.
(4) The minimum percentage FTE for PHM direct patient care (as described below) was set at 25% FTE and defined as 450-500 hours per year. Every candidate must satisfy both the minimum hours for all PHM professional activities and the minimum hours for the direct care of hospitalized children. Applicants must meet or exceed these minima if the ABP is to represent to the public that an applicant has the necessary experience to be called a subspecialist. Similarly, all other ABP subspecialties required at least 50% FTE commitment for the candidate to be considered a subspecialist.
(5) The scope of practice seeks to maintain parity with the training pathway by requiring care of the full spectrum of hospitalized children. This full spectrum is defined as children on general pediatric wards, ages birth to 21 years, and specifically includes children with complex chronic disease, surgical care and comanagement, sedation, palliative care, and common procedures. Care devoted exclusively to a narrow patient population (“niched care”), such as newborns in the nursery, does not meet the eligibility requirements.
(6) The location for patient care must have occurred in the United States or Canada.
(7) The possibility of practice interruption was included among the eligibility criteria. Attempting to strike a balance between an applicant demonstrating sufficient recent experience to be called a subspecialist versus the reality of some individuals needing to interrupt professional and clinical practice, the subboard stipulated that interruptions of PHM professional activities should not exceed three months during the preceding four years and six months during the preceding five years.
CLARIFICATION AND SIMPLIFICATION OF ELIGIBILITY CRITERIA
The ABP recognizes that the use of %FTE, work hours, and leave exceptions led to unintended confusion among applicants. The intent had been to acknowledge the many valid reasons for interruption of practice, including parental leave. This response to the petition clarifies that the critical question from the public’s perspective is whether the candidate has accumulated enough hours of sustained practice to be considered competent in the field of PHM and specifically caring for hospitalized children (as defined above). Upon review, the ABP believes the workhours criteria (items 3 and 4) accomplish this critical goal and make the %FTE and practice interruption criteria largely redundant. Table 3 reflects the clarified and streamlined requirements. Re-examination of all the denied applications showed that using the criteria in Table 3 did not have a significant impact on the outcomes. One additional applicant’s appeal was granted, and this applicant has been so notified.
APPEALS PROCESS
The right to appeal and the Appellate Review Procedure are included in a denial letter. The applicant is given a deadline of 14 days to notify the ABP of the intent to appeal. There is no appellate fee. Within one to three days, the ABP acknowledges receipt of the applicant’s intent to appeal and sends the applicant a date by which additional supporting information should be provided.
The appeal material is shared with the subboard credentials committee and each member individually reviews and votes on the appeal. The application is approved if a majority votes in favor of the applicant’s appeal. If there is no majority, the credentials committee discusses the case to reach a decision. The results of the appeal are final according to the ABP Appellate Review Procedure. We remain in the appeal process for several PHM applicants as of the date of this response.
Thank you for the opportunity to respond to the petition. The ABP is committed to dialogue, transparency, and continuously improving its processes.
Acknowledgment
The authors thank the ABP board of directors and the ABP PHM subboard for their review and thoughtful contributions.
Disclosures
Dr. Nichols reports other from The American Board of Pediatrics, during the conduct of the work. Dr. Woods has nothing to disclose.
1. Barrett DJ, McGuinness GA, Cunha CA, et al. Pediatric hospital medicine: A proposed new subspecialty. Pediatrics. 2017;139(3). https://doi.org/10.1542/peds.2016-1823.
1. Barrett DJ, McGuinness GA, Cunha CA, et al. Pediatric hospital medicine: A proposed new subspecialty. Pediatrics. 2017;139(3). https://doi.org/10.1542/peds.2016-1823.
© 2019 Society of Hospital Medicine