User login
Continuing Medical Education Program in
If you wish to receive credit for this activity, which beginson the next page, please refer to the website:
Accreditation and Designation Statement
Blackwell Futura Media Services designates this educational activity for a 1 AMA PRA Category 1 Credit. Physicians should only claim credit commensurate with the extent of their participation in the activity.
Blackwell Futura Media Services is accredited by the Accreditation Council for Continuing Medical Education to provide continuing medical education for physicians.
Educational Objectives
Continuous participation in the Journal of Hospital Medicine CME program will enable learners to be better able to:
-
Interpret clinical guidelines and their applications for higher quality and more efficient care for all hospitalized patients.
-
Describe the standard of care for common illnesses and conditions treated in the hospital; such as pneumonia, COPD exacerbation, acute coronary syndrome, HF exacerbation, glycemic control, venous thromboembolic disease, stroke, etc.
-
Discuss evidence‐based recommendations involving transitions of care, including the hospital discharge process.
-
Gain insights into the roles of hospitalists as medical educators, researchers, medical ethicists, palliative care providers, and hospital‐based geriatricians.
-
Incorporate best practices for hospitalist administration, including quality improvement, patient safety, practice management, leadership, and demonstrating hospitalist value.
-
Identify evidence‐based best practices and trends for both adult and pediatric hospital medicine.
Instructions on Receiving Credit
For information on applicability and acceptance of continuing medical education credit for this activity, please consult your professional licensing board.
This activity is designed to be completed within the time designated on the title page; physicians should claim only those credits that reflect the time actually spent in the activity. To successfully earn credit, participants must complete the activity during the valid credit period that is noted on the title page.
Follow these steps to earn credit:
-
Log on to www.blackwellpublishing.com/cme.
-
Read the target audience, learning objectives, and author disclosures.
-
Read the article in print or online format.
-
Reflect on the article.
-
Access the CME Exam, and choose the best answer to each question.
-
Complete the required evaluation component of the activity.
If you wish to receive credit for this activity, which beginson the next page, please refer to the website:
Accreditation and Designation Statement
Blackwell Futura Media Services designates this educational activity for a 1 AMA PRA Category 1 Credit. Physicians should only claim credit commensurate with the extent of their participation in the activity.
Blackwell Futura Media Services is accredited by the Accreditation Council for Continuing Medical Education to provide continuing medical education for physicians.
Educational Objectives
Continuous participation in the Journal of Hospital Medicine CME program will enable learners to be better able to:
-
Interpret clinical guidelines and their applications for higher quality and more efficient care for all hospitalized patients.
-
Describe the standard of care for common illnesses and conditions treated in the hospital; such as pneumonia, COPD exacerbation, acute coronary syndrome, HF exacerbation, glycemic control, venous thromboembolic disease, stroke, etc.
-
Discuss evidence‐based recommendations involving transitions of care, including the hospital discharge process.
-
Gain insights into the roles of hospitalists as medical educators, researchers, medical ethicists, palliative care providers, and hospital‐based geriatricians.
-
Incorporate best practices for hospitalist administration, including quality improvement, patient safety, practice management, leadership, and demonstrating hospitalist value.
-
Identify evidence‐based best practices and trends for both adult and pediatric hospital medicine.
Instructions on Receiving Credit
For information on applicability and acceptance of continuing medical education credit for this activity, please consult your professional licensing board.
This activity is designed to be completed within the time designated on the title page; physicians should claim only those credits that reflect the time actually spent in the activity. To successfully earn credit, participants must complete the activity during the valid credit period that is noted on the title page.
Follow these steps to earn credit:
-
Log on to www.blackwellpublishing.com/cme.
-
Read the target audience, learning objectives, and author disclosures.
-
Read the article in print or online format.
-
Reflect on the article.
-
Access the CME Exam, and choose the best answer to each question.
-
Complete the required evaluation component of the activity.
If you wish to receive credit for this activity, which beginson the next page, please refer to the website:
Accreditation and Designation Statement
Blackwell Futura Media Services designates this educational activity for a 1 AMA PRA Category 1 Credit. Physicians should only claim credit commensurate with the extent of their participation in the activity.
Blackwell Futura Media Services is accredited by the Accreditation Council for Continuing Medical Education to provide continuing medical education for physicians.
Educational Objectives
Continuous participation in the Journal of Hospital Medicine CME program will enable learners to be better able to:
-
Interpret clinical guidelines and their applications for higher quality and more efficient care for all hospitalized patients.
-
Describe the standard of care for common illnesses and conditions treated in the hospital; such as pneumonia, COPD exacerbation, acute coronary syndrome, HF exacerbation, glycemic control, venous thromboembolic disease, stroke, etc.
-
Discuss evidence‐based recommendations involving transitions of care, including the hospital discharge process.
-
Gain insights into the roles of hospitalists as medical educators, researchers, medical ethicists, palliative care providers, and hospital‐based geriatricians.
-
Incorporate best practices for hospitalist administration, including quality improvement, patient safety, practice management, leadership, and demonstrating hospitalist value.
-
Identify evidence‐based best practices and trends for both adult and pediatric hospital medicine.
Instructions on Receiving Credit
For information on applicability and acceptance of continuing medical education credit for this activity, please consult your professional licensing board.
This activity is designed to be completed within the time designated on the title page; physicians should claim only those credits that reflect the time actually spent in the activity. To successfully earn credit, participants must complete the activity during the valid credit period that is noted on the title page.
Follow these steps to earn credit:
-
Log on to www.blackwellpublishing.com/cme.
-
Read the target audience, learning objectives, and author disclosures.
-
Read the article in print or online format.
-
Reflect on the article.
-
Access the CME Exam, and choose the best answer to each question.
-
Complete the required evaluation component of the activity.
Management of Ischemic Stroke: Part 2
Inpatient stroke management includes many elements of care, at least as important as the initial portion of the patient's stay, as reviewed in part 1 of this article. The extent of further diagnostic evaluation varies widely depending on apparent risk factors on presentation. Likewise, further therapy, both inpatient and secondary prevention is based on identification of stroke mechanism. Hospitalists are uniquely positioned to have a tremendous impact on both stroke care and the prevention of recurrent disease.
Case Presentation
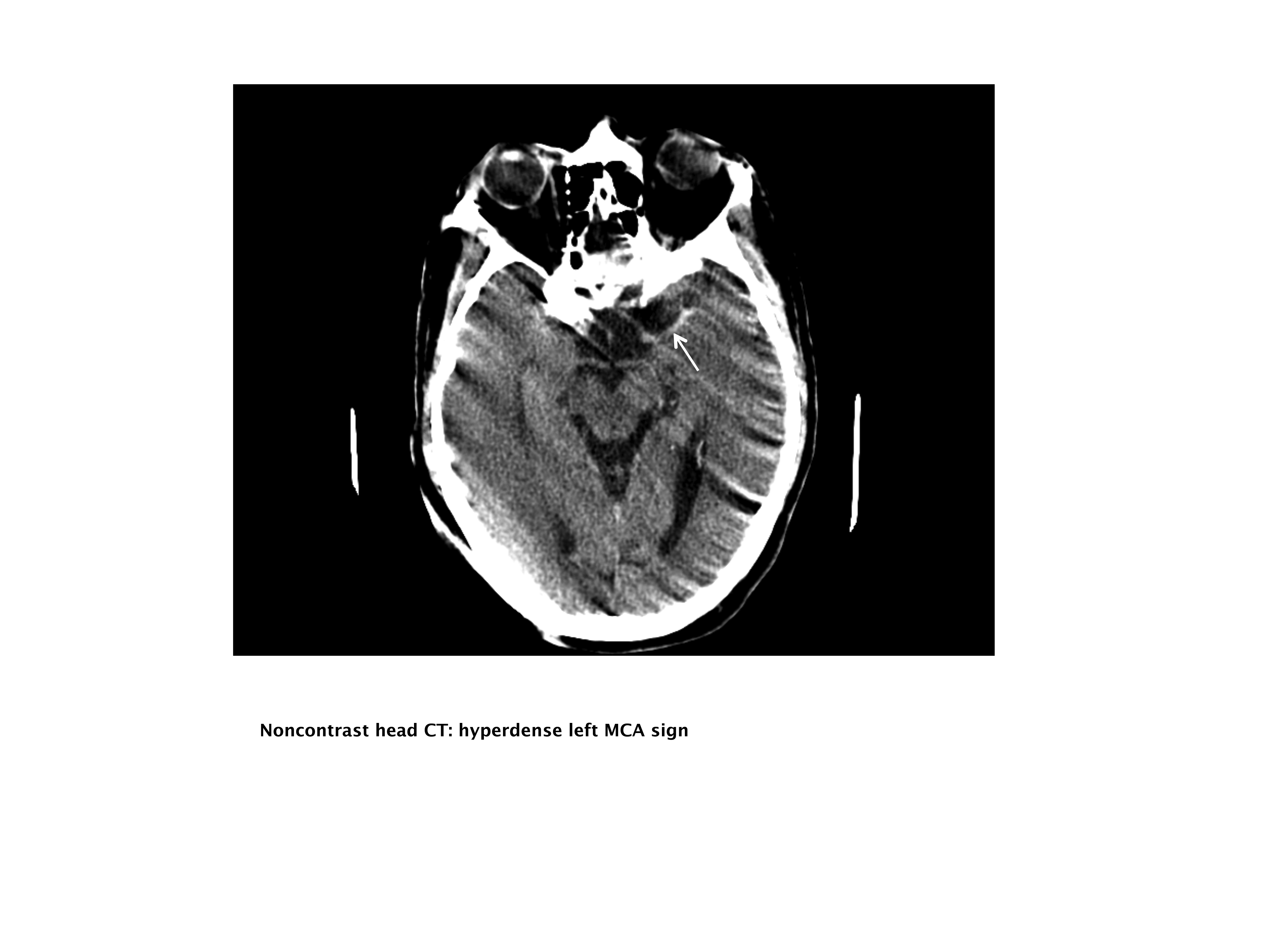
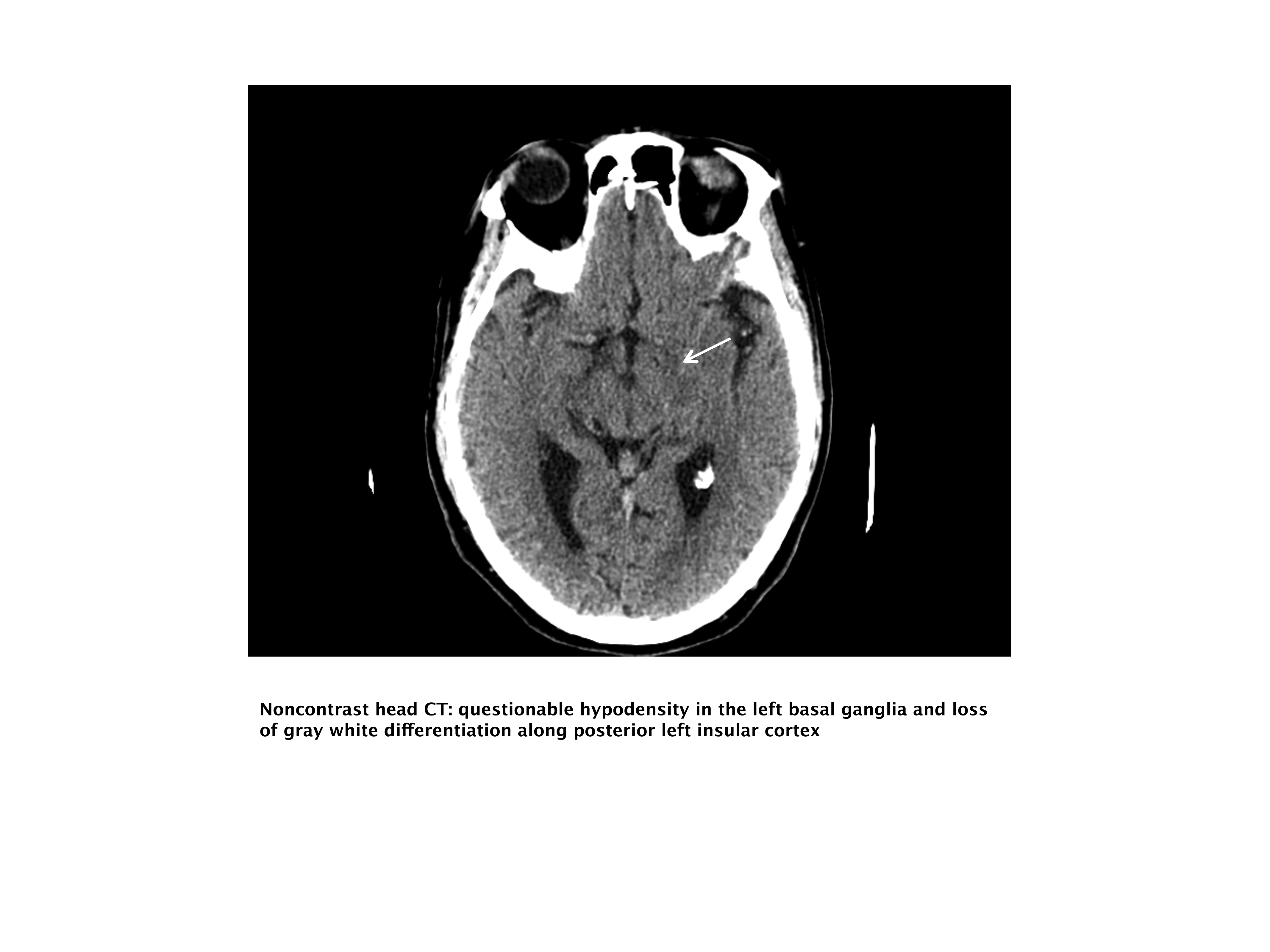
A 76‐year‐old right‐handed male with a history of hyperlipidemia and myocardial infarction was found at 7 AM with right‐sided paralysis and poor responsiveness on the morning of admission. Upon arrival to the emergency department (ED), with symptoms of partial aphasia, right hemiplegia, and left gaze preference, there was a high suspicion for a left middle cerebral artery (MCA) stroke. Unfortunately, he was excluded from receiving intravenous (IV) tissue plasminogen activator (tPA) or any other acute interventions as the last time he was known to be neurologically intact was the prior evening, which is taken to be the time of onset. Antiplatelet therapy was continued, and the patient admitted for further workup.
Inpatient Care
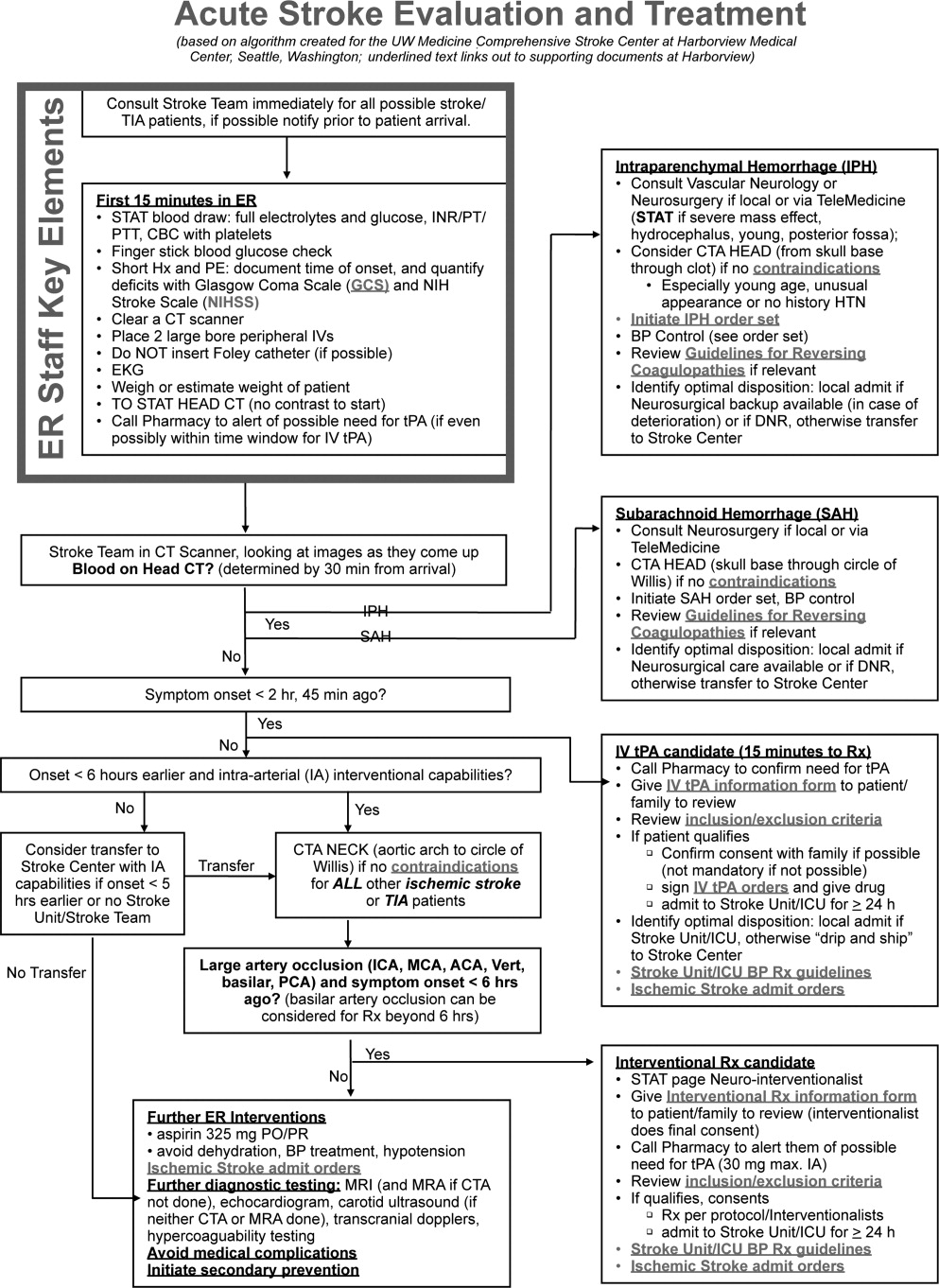
When an acute ischemic stroke patient is admitted to the hospital, he or she should be placed on a standardized acute stroke protocol (also known as (a.k.a.) a care map, order set, clinical pathway)commonly created by a hospitalist/neurologist and a multidisciplinary team and admitted to a stroke unit. A stroke unit can take many forms, either as a physically separate unit in hospitals with sufficient volume or a floor where a lower volume of stroke patients are always admitted. Multidisciplinary care providers in the stroke unit have special training in stroke, and strong evidence from randomized trials shows that patients cared for in these units have significantly decreased mortality with improved functional outcomes.1 Essentials of the stroke protocol or order set include cardiac telemetry, maintaining euthermia and euglycemia, closely following blood pressure and neurologic status, actively avoiding complications, initiation of secondary prevention treatment, early involvement of rehabilitation services, and patient education.
Euthermia may be assisted by administering scheduled Tylenol to the patient for the first 48 hours, but is not strictly evidence‐based.2 Though euthermia and euglycemia have not been shown to improve outcomes in acute stroke, studies have shown that hyperthermia and hyperglycemia are associated with worsened outcomes for patients with acute strokes.35
Blood Pressure Management
Normally, cerebral vascular autoregulation leads to stable cerebral blood flow over a range of systemic blood pressures. In the setting of an acute stroke, the ability to autoregulate is diminished or absent in regions of and surrounding an acute ischemic stroke; as the area becomes ischemic, autoregulation opens the local vasculature maximally in an effort to drawn in as much blood as possible. Maximally dilated arterioles are perfused in direct correlation with systemic blood pressure, thus any drop in the systemic blood pressure leads to direct decreases in blood flow specifically in the area of ischemia; if there is a penumbra of marginally perfused tissue, such systemic blood pressure drops risk extending the area of fatal ischemia (increasing the size of the ischemic stroke).68 Thus in the acute period of an ischemic stroke, the American Heart Association (AHA)/American Stroke Association (ASA) Guidelines for the Early Management of Adults With Ischemic Stroke (referred to herein as the Guidelines)10 suggest avoid treatment unless systolic blood pressures are >220 or diastolic pressures >105, and review the evidence to support this recommendation (p. 16711672). Those patients who receive tPA have a more stringent blood pressure threshold given their risk of intracranial hemorrhage; systolic blood pressures are accepted up to 180 prior to recommending treatment.
Higher‐quality Inpatient Stroke Care and Harmonized Performance Measures
Beginning in January 2008, a set of 10 performance measures (Table 1) for inpatient acute stroke care have been agreed upon (harmonized) by 3 major stakeholders including the Joint Commission, the ASA's Get with the GuidelinesStroke quality improvement program, and the Center for Disease Control and Prevention's (CDC's) Paul Coverdell Acute stroke registries. These performance measures were selected to help avoid complications (deep vein thrombosis [DVT], aspiration pneumonia), encourage appropriately aggressive care (tPA administration), optimize secondary prevention (antithrombotics, cholesterol lowering, smoking cessation, education), and facilitate functional recovery (early rehabilitation). All 10 measures are appropriate for consideration in every ischemic stroke patient, and 5 are appropriate for the hemorrhagic stroke types.
| Performance measure* | Definition* |
|---|---|
| |
| 1. DVT prophylaxis | Patients who are nonambulatory should start receiving DVT prophylaxis by end of hospital day 2 (can be either compression devices or any low‐dose heparin) |
| 2. Discharged on antithrombotic therapy | Antiplatelet agent(s) or warfarin anticoagulation |
| 3. Patients with atrial fibrillation receiving anticoagulation therapy | A proven approach to secondary prevention in such patients; practice at Harborview varies time of warfarin initiation based on infarct size with larger infarcts waiting up to 2 weeks before initiating warfarin (the best randomized trial showed no benefit for full‐dose low‐molecular‐weight heparin over aspirin in the first 2 weeks)50 |
| 4. Thrombolytic therapy administered | In ischemic stroke patients who arrive at the hospital within 120 minutes (2 hours) of time last known well, for whom IV tPA was initiated at this hospital within 180 minutes (3 hours) of time last known well, and who qualify under strict criteria |
| 5. Antithrombotic therapy by end of hospital day 2 | Usually just antiplatelet agents, a minimal standard of care for ischemic stroke patients; should be started as early as possible, usually in ER |
| 6. Discharged on statin medication | If LDL >100, or not measured or if on a statin drug prior to admission; to reduce risk of subsequent ischemic stroke |
| 7. Dysphagia screening | Prior to any PO food, fluids or medications; to reduce the chances of aspiration pneumonia |
| 8. Stroke education | Including for families if patient unable to participate, must include personal risk factors for stroke, warning signs for stroke, activation of emergency medical system, need for follow‐up after discharge, and medications prescribed |
| 9. Smoking cessation/advice/counseling | For any patient who has smoked in the last year |
| 10. Assessed for rehabilitation | Or received therapy services; to facilitate progress to an optimal function outcome |
Further Workup
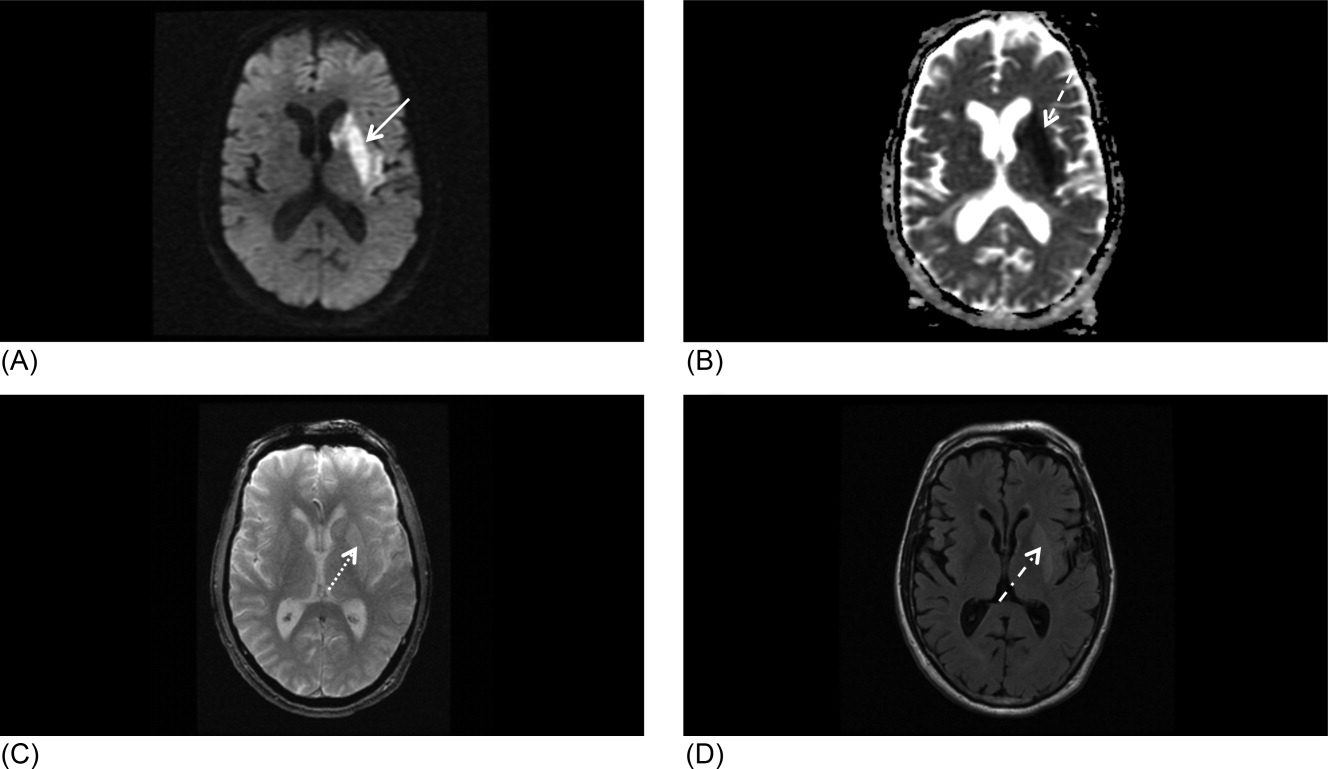
After the ischemic stroke patient has had their computed tomography (CT) scan, possibly a computed tomography angiography (CTA), been admitted to the stroke unit, started on an antithrombotic medication, and had their blood pressure appropriately treated, attention then turns to defining the pathophysiology related to the stroke and starting an optimal regimen for secondary prevention. Imaging of the cerebral vasculature including both extracranial and intracranial large vessels is a vital first step in understanding the cause of ischemic stroke. There are multiple potential modalities (magnetic resonance angiography [MRA], CTA, and duplex/transcranial Doppler), the choice of which depends on local availability and expertise as well as the specific clinical situation. Magnetic resonance imaging (MRI) of the brain for all ischemic stroke patients is standard of care at most stroke centers; per the Guidelines, MRI is better at distinguishing acute, small cortical, small deep, and posterior fossa infarcts; at distinguishing acute from chronic ischemia; and at identifying subclinical satellite ischemic lesions that provide information on stroke mechanism (p. 1668). New techniques including magnetic resonance (MR) and CT perfusion scanning can show the ischemic region in the acute setting and may one day help select patients for specific therapies, but are not yet widely available nor have they been shown to alter outcomes.
An electrocardiogram is indicated for all stroke patients, as is admission to a cardiac telemetry bed for at least 24 hours to document any arrhythmias, the most common being atrial fibrillation (Guidelines, p. 1666, 1673). An echocardiographic study (ECHO) of the heart with bubble study should be performed in most cases (although which cases may specifically benefit is unclear) to identify a cardioembolic source for the stroke, such as low cardiac ejection fraction, atrial septal aneurysm, patent foramen ovale (PFO), or a cardiac thrombus. The bubble study increases the sensitivity of detecting a PFO, which could serve as a gateway for venous embolization to the cerebral arteries. Assuming a large PFO is discovered, other studies such as lower extremity Doppler may be warranted to investigate other potential sources of thrombi (ie, DVT).
Regarding laboratory testing, fasting lipids should be checked as hyperlipidemia is a common modifiable risk factor for ischemic stroke. The Stroke Prevention by Aggressive Reduction in Cholesterol Levels (SPARCL) trial included ischemic stroke patients that had low‐density lipoprotein (LDL) cholesterol between 100 mg/dL and 190 mg/dL and randomized them to receive atorvastatin 80 mg/day vs. placebo. Results showed a 16% relative risk reduction in recurrent stroke; however, there was a small increased risk of intracranial hemorrhage.9 As shown in Table 1, use of a statin on discharge is now a national performance measure for ischemic stroke.
Dissection is a common cause of stroke in young patients without traditional risk factors. Other serologies, such as hypercoagulable studies, may be warranted in patients with no other risk factors for strokes, paradoxical embolus, or of young age (eg, 45 years and under). The arterial hypercoagulable panel consists of antiphospholipid antibody panel, homocysteine levels, lupus anticoagulant levels, and prothrombin time/partial thromboplastin time (PT/PTT). The venous hypercoagulable panel consists of the laboratory values checked, with the arterial hypercoagulable and activated protein C (APC) resistance, Factor VIII activity, Factor II DNA, Factor V DNA if the APC resistance is positive, antithrombin III activity, and activity of proteins C and S. If a patient is found to have a hypercoagulable state, long‐term therapy often involves careful consideration of the choice of antiplatelet therapy vs. anticoagulation with warfarin.10
Initiating Secondary Prevention
Upon admission, the clinician faces a variety of treatment choices for secondary stroke prevention. The proper choice depends on the results of the workup and the presumptive pathophysiology.
Noncardioembolic/Atherothrombotic/Lacunar
The Antithrombotic Trialists' Collaboration meta‐analysis found that patients with a prior stroke or transient ischemic attack (TIA) had a highly significant decrease in the rate of subsequent vascular events (over about 3 years) on antiplatelet therapy (17.8% vs. 21.4%, P 0.0001) and were unable to find a significant difference between low‐dose and high‐dose aspirin for secondary prevention.11 Thus, it is reasonable to place an acute stroke patient naive to antithrombotic therapy on 81 mg of aspirin or 325 mg for long‐term prevention (325 mg is specifically recommended in the acute setting). Several studies such as the WARSS and ESPRIT trials have shown antiplatelet agents to be at least as effective as anticoagulation in noncardioembolic ischemic strokes.12, 13 Guidelines from Europe, the American College of Chest Physicians, and the AHA/ASA all state it is acceptable to choose either aspirin monotherapy, aspirin/extended release dipyridamole combination therapy, or clopidogrel monotherapy as first‐line agents for long‐term secondary prevention in noncardioembolic ischemic stroke.1416 There is no clear evidence that patients who suffer an ischemic stroke while on aspirin will derive additional benefit from increasing the aspirin dose. The newer guidelines go on to recommend aspirin/extended release dipyridamole (ER‐DP) combination therapy or clopidogrel monotherapy over aspirin monotherapy, the former with a stronger level of recommendation based on the results of 2 randomized trials. These recommendations were all published without knowledge of the results of the Prevention Regimen For Effectively Avoiding Second Strokes (PRoFESS) study, which directly compared aspirin/extended release dipyridamole combination therapy to clopidogrel monotherapy for long‐term secondary prevention. The rate of first recurrent stroke was not significantly different between the 2 therapies (9.0% ER‐DP plus aspirin, 8.8% clopidogrel; hazard ratio [HR], 1.01; 95% confidence interval [CI], 0.921.11). Other outcomes also showed few differences, although there were more major hemorrhagic events in the ER‐DP plus aspirin group (4.1% vs. 3.6%; HR, 1.15; 95% CI, 1.001.32; P = 0.06).17
The ASA Stroke Prevention Guideline from 2006 states, with continued relevance, The selection of an antiplatelet agent should be individualized on the basis of patient risk factor profiles, tolerance, and other clinical characteristics.10 Of note, both the Clopidogrel for High Atherothrombotic Risk and Ischemic Stabilization, Management and Avoidance (CHARISMA) and Management of ATherothrombosis with Clopidogrel in High‐risk patients with recent TIA or ischemic stroke (MATCH) trials found a significant increased risk for hemorrhage complications with long‐term use of the aspirin and clopidogrel combination,18, 19 and the 2008 update to the ASA Stroke prevention guidelines state that the addition of aspirin to clopidogrel increases the risk of hemorrhage. Combination therapy of aspirin and clopidogrel is not routinely recommended for ischemic stroke or TIA patients unless they have a specific indication for this therapy (i.e., coronary stent or acute coronary syndrome).15
Atrial Fibrillation
Though our case patient did not have atrial fibrillation, this condition does deserve mention. About 15% to 20% of ischemic stroke patients have atrial fibrillation. The overall risk for stroke in patients with atrial fibrillation is about 5% per year; however, patients who have a history of stroke increase their risk factors for subsequent strokes to about 12% per year. In most cases, anticoagulation has proven to be the superior agent for primary and secondary stroke prevention with warfarin reducing the risk by 67% compared to aspirin, which only reduces the risk of stroke by 20%. A meta‐analysis from 2002 showed that patients who had a prior stroke or TIA decrease their risk of subsequent strokes to 4%/year on oral anticoagulation therapy, resulting in an 8% absolute risk reduction. Patients on aspirin therapy only decrease their risk to 10%/year, or a 2% reduction in stroke events.20 Unless there is a strong contraindication (eg, bleeding diathesis, history of life threatening gastrointestinal [GI] bleeding, history of fall with subdural hematoma, etc.), virtually all ischemic stroke patients with atrial fibrillation should be anticoagulated for life. Anticoagulation in the setting of atrial fibrillation is seriously underutilized.21 The highest quality study on early anticoagulation for ischemic stroke associated with atrial fibrillation suggested that there was no benefit to starting anticoagulation earlier than 2 weeks after a stroke, and there may actually be a higher complication rate (compared to aspirin).22 Other cardiac indications for anticoagulation include left ventricular thrombus and mechanical valves.
Carotid Stenosis
Significant ipsilateral stenosis of the internal carotid artery in a patient with ischemic stroke is a strong indication for intervention, usually a standard carotid endarterectomy (CEA). Stenosis of 70% to 99% is the strongest indication for CEA, and may be of greatest benefit in men, those 75+ years of age, and if surgery is done 2 weeks after the most recent symptoms.23 In patients with minor stroke or TIA, recent recommendations and our practice is to admit to the hospital and perform endarterectomy as soon as possible (those with major stroke may have a greater risk of complications with early CEA).24 Stenting should only be considered instead of CEA if high risk (for surgical complications) criteria are present. These high risk criteria include patients having significant comorbidities and/or anatomic risk factors (ie, recurrent stenosis and/or previous radical neck dissection), and [who] would be poor candidates for CEA in the opinion of a surgeon.25 For stenoses of 50% to 69%, intervention is not as compelling, and decisions should be individualized based on patient characteristics; in this group, stenting should only be considered in the setting of a clinical trial or if an investigational device exemption (IDE) exists at your institution.26
Dissection of the Carotid or Vertebral Arteries
This is a common cause of stroke in younger adults. It should be suspected in patients without other clear causes of stroke and significant disease of the extracranial arteries. Diagnosis can usually be made with CTA or MRA, though it is suggested that the best modality may be T1‐fat‐saturated MRI images of the neck. Debate exists as to the best approach to treatment of dissections due to the absence of randomized trials. A recent comprehensive review suggested anticoagulation for 3 to 6 months followed by indefinite antiplatelet therapy for symptomatic dissections and antiplatelet therapy alone for asymptomatic dissections.27
PFO‐related Stroke
If the patient is found to have a PFO, its role in comparison to traditional risk factors must be weighed carefully. Epidemiological studies suggest that PFO may be most relevant in younger patients, those with cryptogenic stroke (no obvious cause and lack of traditional risk factors), those with higher risk associations including interatrial septal aneurysm, larger PFOs or history of previous cryptogenic stroke.28, 29 The best medical therapy for seemingly PFO‐related ischemic stroke is also unclear; a reasonable approach might be aspirin if neither high‐risk associations nor a hypercoagulable state is present, and warfarin if either are present. Transcatheter closure of PFO is approved by the U.S. Food and Drug Administration (FDA) only under an IDE for patients who have had a recurrent event on maximally tolerated medical treatment, and requires approval from the human research committee (internal review board [IRB]) at your hospital. It is not known if closure is superior or inferior to best medical therapy, and a practice parameter from the American Academy of Neurology strongly encourages appropriate patients to consider participation in ongoing randomized trials.28 Further information on these trials is available at:
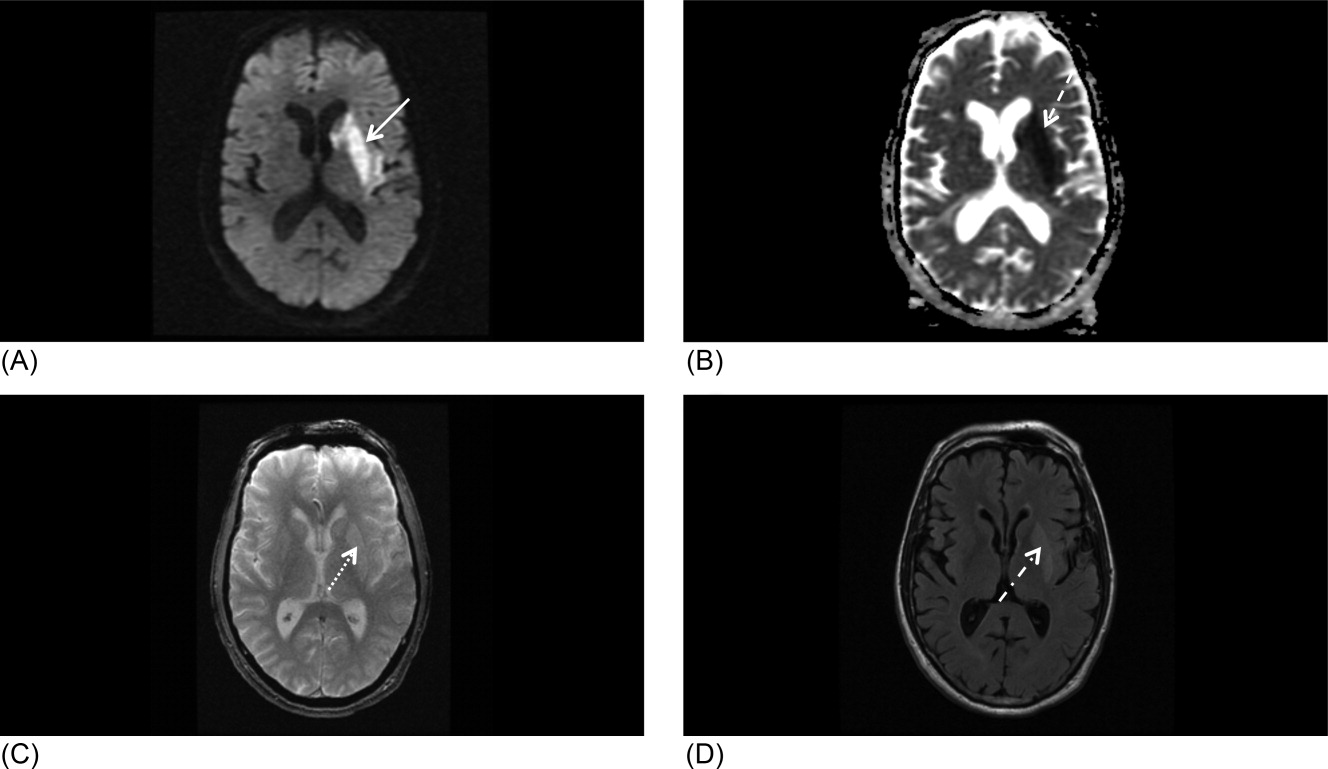
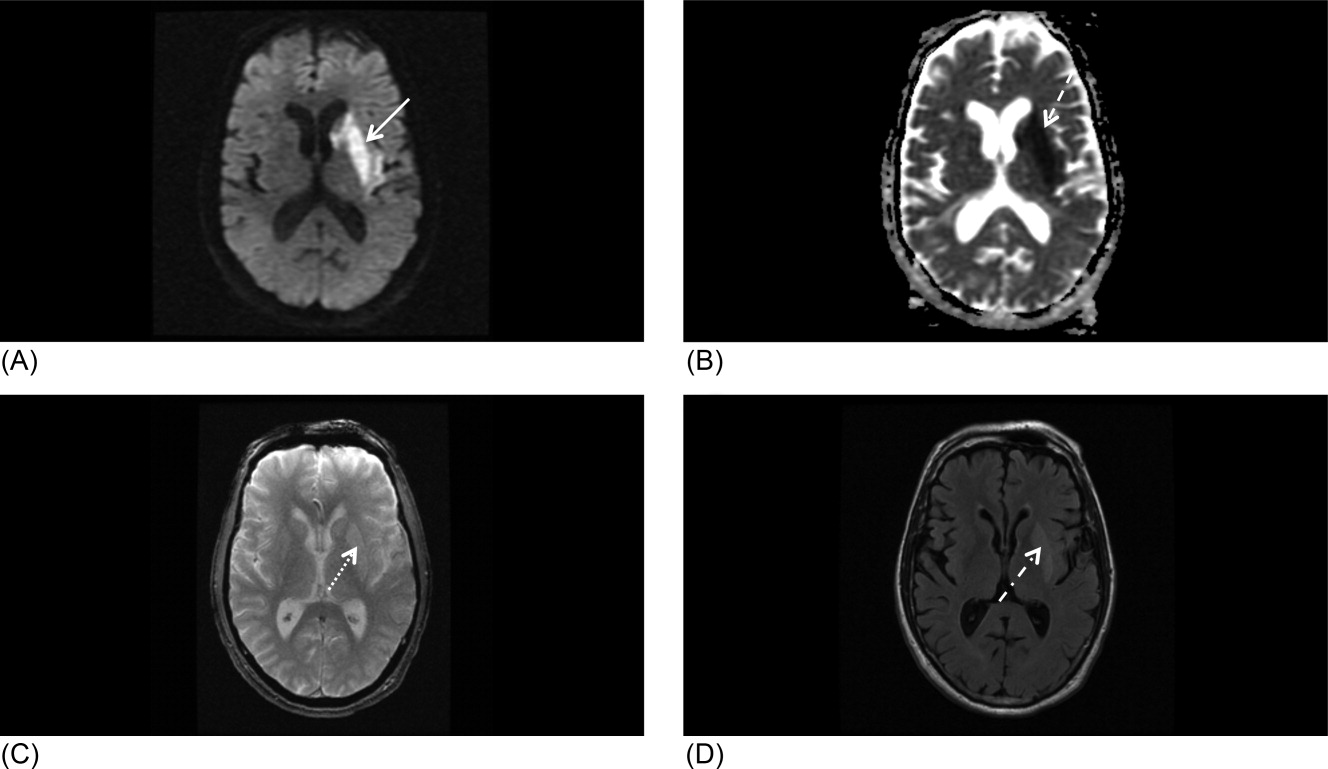
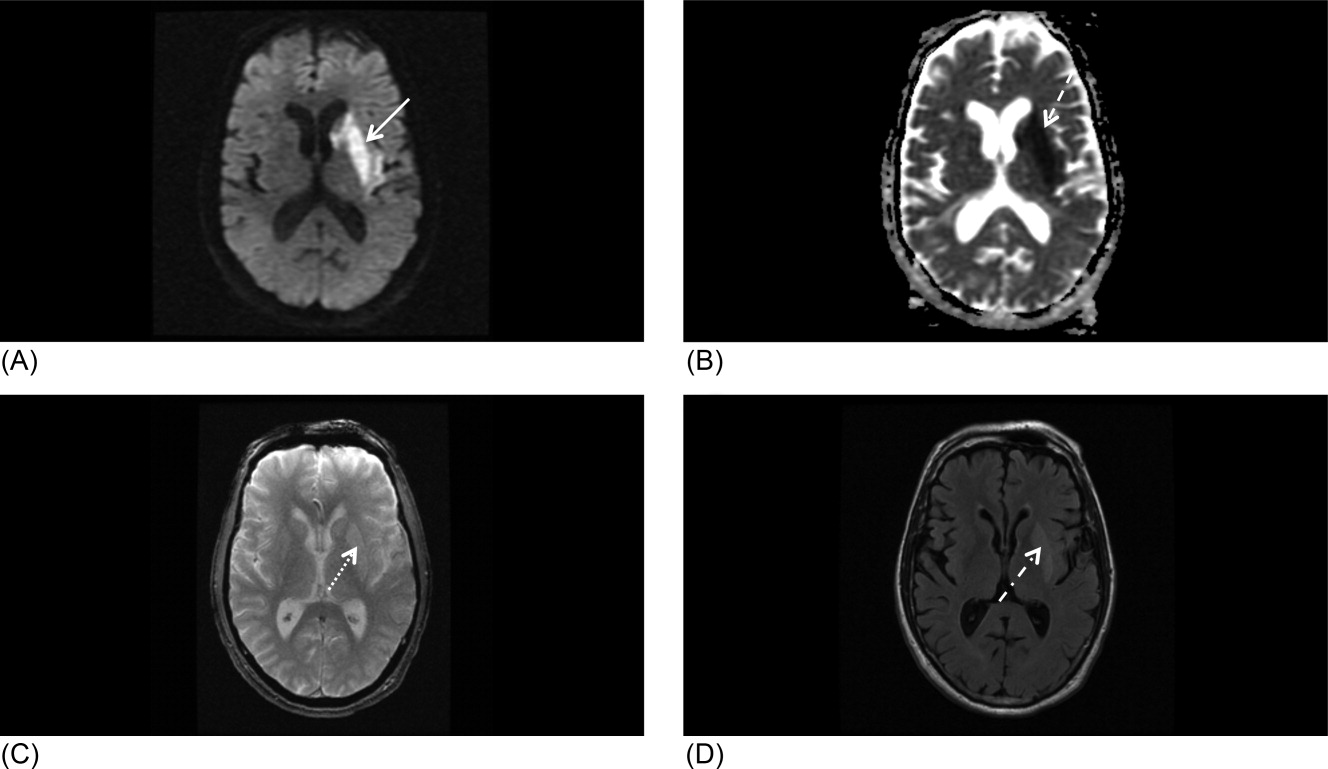
Our patient underwent a CTA of the head and neck in the emergency room to see if he would be a candidate for other interventions; unfortunately, he did not meet the time criteria. CTA showed complete occlusion of the left internal carotid artery at the bifurcation with heterogeneous retrograde filling (Supporting Figure 1). Complete occlusion of the proximal third of the left M1 segment was also seen with relative oligemia in the left MCA distribution, though several small peripheral M3/M4 vessels were opacified in the territory indicating collateralization (Supporting Figure 2). A MRI showed a large area of diffusion‐weighted abnormality (Figure 1). Interestingly, the patient's transthoracic echocardiography (TTE), which did not show evidence of a PFO, did reveal a calcified thrombus in the left ventricle. Though no arrhythmias were captured on telemetry, this thrombus does serve as a potential source of cardioembolic emboli to the cerebral vasculature. It was felt that the most likely source of the patient's acute infarct was from artery‐to‐artery emboli from his internal carotid occlusion given the infarct location and the lack of infarction in other vascular distributions (as one might see from a cardiac embolic source). Therefore, his medical management consisted of an antiplatelet regimen for 2 weeks followed by a transition to warfarin alone 2 weeks after his acute infarct as secondary stroke prevention due to the cardiac thrombus. Given the complete occlusion of the internal carotid artery and M1 segment, there was concern that the penumbra might be at risk of infarction (supporting standard guidelines of permissive hypertension). By the end of his hospitalization, the patient had improved and was transferred to inpatient rehabilitation.
The guidelines for acute stroke management continue to rapidly evolve. Certainly, there are effective treatments for acute ischemic stroke, with variation based on the timing of patient arrival at the hospital, the underlying pathophysiology, and the treatment capabilities of the individual hospital. Secondary stroke prevention is extremely important and has been emphasized during inpatient admissions with the establishment of an appropriate medication regime, given that patients are more likely to stay on treatment that is initiated around the time of a diagnosis.29 Evidence strongly suggests that management of acute stroke is improved by an organized approach to care, including the expertise of a multidisciplinary team in a specialized stroke unit. Hospitals committed to high quality of care for acute stroke patients should strongly consider the Joint Commission certification process or an analogous local certification. Such certification demonstrates a hospital's commitment to providing high‐quality care, what every stroke patient wants and deserves.
- Organised inpatient (stroke unit) care for stroke.Stroke Unit Trialists' Collaboration.Cochrane Database Syst Rev.2000(2):CD000197.
- ,,, et al.Acetaminophen for altering body temperature in acute stroke: a randomized clinical trial.Stroke.2002;33(1):130–134.
- ,,, et al.Fever in acute stroke worsens prognosis. A prospective study.Stroke.1995;26(11):2040–2043.
- ,.Combating hyperthermia in acute stroke: a significant clinical concern.Stroke.1998;29(2):529–534.
- ,,, et al.Body temperature in acute stroke: relation to stroke severity, infarct size, mortality, and outcome.Lancet. 171996;347(8999):422–425.
- ,,.Thresholds in cerebral ischemia—the ischemic penumbra.Stroke.1981;12(6):723–725.
- .Ischaemic brain damage of cerebral perfusion failure type after treatment of severe hypertension.Br Med J. 271975;4(5999):739.
- ,,,,.Imaging of acute stroke.Lancet Neurol.2006;5(9):755–768.
- ,,, et al.High‐dose atorvastatin after stroke or transient ischemic attack.N Engl J Med.2006;355(6):549–559.
- ,,, et al.Guidelines for prevention of stroke in patients with ischemic stroke or transient ischemic attack: a statement for healthcare professionals from the American Heart Association/American Stroke Association Council on Stroke: co‐sponsored by the Council on Cardiovascular Radiology and Intervention: the American Academy of Neurology affirms the value of this guideline.Stroke.2006;37(2):577–617.
- Antithrombotic Trialists' Collaboration.Collaborative meta‐analysis of randomised trials of antiplatelet therapy for prevention of death, myocardial infarction, and stroke in high risk patients.BMJ.2002;324(7329):71–86.
- ,,, et al.A comparison of warfarin and aspirin for the prevention of recurrent ischemic stroke.N Engl J Med.2001;345(20):1444–1451.
- .Warfarin or aspirin for recurrent ischemic stroke.N Engl J Med.2002;346(15):1169–1171.
- ,,, et al.Prevention. European Stroke Initiative.Cerebrovasc Dis.2004;17(suppl 2):15–29.
- ,,, et al.Update to the AHA/ASA recommendations for the prevention of stroke in patients with stroke and transient ischemic attack.Stroke.2008;39(5):1647–1652.
- ,,,,.Antithrombotic and thrombolytic therapy for ischemic stroke: American College of Chest Physicians Evidence‐Based Clinical Practice Guidelines (8th edition).Chest.2008;133(suppl):630S–669S.
- ,,, et al.Aspirin and extended‐release dipyridamole versus clopidogrel for recurrent stroke.N Engl J Med.2008;359(12):1238–1251.
- ,,, et al.Clopidogrel and aspirin versus aspirin alone for the prevention of atherothrombotic events.N Engl J Med.2006;354(16):1706–1717.
- ,,, et al.Aspirin and clopidogrel compared with clopidogrel alone after recent ischaemic stroke or transient ischaemic attack in high‐risk patients (MATCH): randomised, double‐blind, placebo‐controlled trial.Lancet.2004;364(9431):331–337.
- ,,, et al.Oral anticoagulants vs aspirin in nonvalvular atrial fibrillation: an individual patient meta‐analysis.JAMA.2002;288(19):2441–2448.
- .Effective anticoagulation therapy: defining the gap between clinical studies and clinical practice.Am J Manag Care.2004;10(suppl):S297–S306; discussionS312–S297.
- ,,,.Low molecular‐weight heparin versus aspirin in patients with acute ischaemic stroke and atrial fibrillation: a double‐blind randomised study. HAEST Study Group. Heparin in Acute Embolic Stroke Trial.Lancet.2000;355(9211):1205–1210.
- ,,,,.Endarterectomy for symptomatic carotid stenosis in relation to clinical subgroups and timing of surgery.Lancet.2004;363(9413):915–924.
- ,,.The timing of carotid endarterectomy post stroke.Neurol Clin.2006;24(4):669–680.
- Centers for Medicare and Medicaid Services (CMS). Department of Health and Human Services (DHHS). CMS Manual System. Pub 100–03 Medicare National Coverage Determinations. Available at: http://www.cms.hhs.gov/Transmittals/Downloads/R64NCD.pdf. Accessed May2009.
- .Current status of carotid endarterectomy and stenting for symptomatic carotid stenosis.Cerebrovasc Dis.2007;24(suppl 1):116–125.
- ,,, et al.Antiplatelets versus anticoagulation in cervical artery dissection.Stroke.2007;38(9):2605–2611.
- ,,, et al.A comparison of warfarin and aspirin for the prevention of recurrent ischemic stroke.N Engl J Med2001;345(20):1444–1451.
- .Warfarin or aspirin for recurrent ischemic stroke.N Engl J Med2002;346(15):1169–1171.
- ,,, et al.Practice parameter: recurrent stroke with patent foramen ovale and atrial septal aneurysm: report of the Quality Standards Subcommittee of the American Academy of Neurology.Neurology.2004;62(7):1042–1050.
- ,,, et al.In‐hospital initiation of secondary stroke prevention therapies yields high rates of adherence at follow‐up.Stroke.2004;35(12):2879–2883.
Inpatient stroke management includes many elements of care, at least as important as the initial portion of the patient's stay, as reviewed in part 1 of this article. The extent of further diagnostic evaluation varies widely depending on apparent risk factors on presentation. Likewise, further therapy, both inpatient and secondary prevention is based on identification of stroke mechanism. Hospitalists are uniquely positioned to have a tremendous impact on both stroke care and the prevention of recurrent disease.
Case Presentation
A 76‐year‐old right‐handed male with a history of hyperlipidemia and myocardial infarction was found at 7 AM with right‐sided paralysis and poor responsiveness on the morning of admission. Upon arrival to the emergency department (ED), with symptoms of partial aphasia, right hemiplegia, and left gaze preference, there was a high suspicion for a left middle cerebral artery (MCA) stroke. Unfortunately, he was excluded from receiving intravenous (IV) tissue plasminogen activator (tPA) or any other acute interventions as the last time he was known to be neurologically intact was the prior evening, which is taken to be the time of onset. Antiplatelet therapy was continued, and the patient admitted for further workup.
Inpatient Care
When an acute ischemic stroke patient is admitted to the hospital, he or she should be placed on a standardized acute stroke protocol (also known as (a.k.a.) a care map, order set, clinical pathway)commonly created by a hospitalist/neurologist and a multidisciplinary team and admitted to a stroke unit. A stroke unit can take many forms, either as a physically separate unit in hospitals with sufficient volume or a floor where a lower volume of stroke patients are always admitted. Multidisciplinary care providers in the stroke unit have special training in stroke, and strong evidence from randomized trials shows that patients cared for in these units have significantly decreased mortality with improved functional outcomes.1 Essentials of the stroke protocol or order set include cardiac telemetry, maintaining euthermia and euglycemia, closely following blood pressure and neurologic status, actively avoiding complications, initiation of secondary prevention treatment, early involvement of rehabilitation services, and patient education.
Euthermia may be assisted by administering scheduled Tylenol to the patient for the first 48 hours, but is not strictly evidence‐based.2 Though euthermia and euglycemia have not been shown to improve outcomes in acute stroke, studies have shown that hyperthermia and hyperglycemia are associated with worsened outcomes for patients with acute strokes.35
Blood Pressure Management
Normally, cerebral vascular autoregulation leads to stable cerebral blood flow over a range of systemic blood pressures. In the setting of an acute stroke, the ability to autoregulate is diminished or absent in regions of and surrounding an acute ischemic stroke; as the area becomes ischemic, autoregulation opens the local vasculature maximally in an effort to drawn in as much blood as possible. Maximally dilated arterioles are perfused in direct correlation with systemic blood pressure, thus any drop in the systemic blood pressure leads to direct decreases in blood flow specifically in the area of ischemia; if there is a penumbra of marginally perfused tissue, such systemic blood pressure drops risk extending the area of fatal ischemia (increasing the size of the ischemic stroke).68 Thus in the acute period of an ischemic stroke, the American Heart Association (AHA)/American Stroke Association (ASA) Guidelines for the Early Management of Adults With Ischemic Stroke (referred to herein as the Guidelines)10 suggest avoid treatment unless systolic blood pressures are >220 or diastolic pressures >105, and review the evidence to support this recommendation (p. 16711672). Those patients who receive tPA have a more stringent blood pressure threshold given their risk of intracranial hemorrhage; systolic blood pressures are accepted up to 180 prior to recommending treatment.
Higher‐quality Inpatient Stroke Care and Harmonized Performance Measures
Beginning in January 2008, a set of 10 performance measures (Table 1) for inpatient acute stroke care have been agreed upon (harmonized) by 3 major stakeholders including the Joint Commission, the ASA's Get with the GuidelinesStroke quality improvement program, and the Center for Disease Control and Prevention's (CDC's) Paul Coverdell Acute stroke registries. These performance measures were selected to help avoid complications (deep vein thrombosis [DVT], aspiration pneumonia), encourage appropriately aggressive care (tPA administration), optimize secondary prevention (antithrombotics, cholesterol lowering, smoking cessation, education), and facilitate functional recovery (early rehabilitation). All 10 measures are appropriate for consideration in every ischemic stroke patient, and 5 are appropriate for the hemorrhagic stroke types.
| Performance measure* | Definition* |
|---|---|
| |
| 1. DVT prophylaxis | Patients who are nonambulatory should start receiving DVT prophylaxis by end of hospital day 2 (can be either compression devices or any low‐dose heparin) |
| 2. Discharged on antithrombotic therapy | Antiplatelet agent(s) or warfarin anticoagulation |
| 3. Patients with atrial fibrillation receiving anticoagulation therapy | A proven approach to secondary prevention in such patients; practice at Harborview varies time of warfarin initiation based on infarct size with larger infarcts waiting up to 2 weeks before initiating warfarin (the best randomized trial showed no benefit for full‐dose low‐molecular‐weight heparin over aspirin in the first 2 weeks)50 |
| 4. Thrombolytic therapy administered | In ischemic stroke patients who arrive at the hospital within 120 minutes (2 hours) of time last known well, for whom IV tPA was initiated at this hospital within 180 minutes (3 hours) of time last known well, and who qualify under strict criteria |
| 5. Antithrombotic therapy by end of hospital day 2 | Usually just antiplatelet agents, a minimal standard of care for ischemic stroke patients; should be started as early as possible, usually in ER |
| 6. Discharged on statin medication | If LDL >100, or not measured or if on a statin drug prior to admission; to reduce risk of subsequent ischemic stroke |
| 7. Dysphagia screening | Prior to any PO food, fluids or medications; to reduce the chances of aspiration pneumonia |
| 8. Stroke education | Including for families if patient unable to participate, must include personal risk factors for stroke, warning signs for stroke, activation of emergency medical system, need for follow‐up after discharge, and medications prescribed |
| 9. Smoking cessation/advice/counseling | For any patient who has smoked in the last year |
| 10. Assessed for rehabilitation | Or received therapy services; to facilitate progress to an optimal function outcome |
Further Workup
After the ischemic stroke patient has had their computed tomography (CT) scan, possibly a computed tomography angiography (CTA), been admitted to the stroke unit, started on an antithrombotic medication, and had their blood pressure appropriately treated, attention then turns to defining the pathophysiology related to the stroke and starting an optimal regimen for secondary prevention. Imaging of the cerebral vasculature including both extracranial and intracranial large vessels is a vital first step in understanding the cause of ischemic stroke. There are multiple potential modalities (magnetic resonance angiography [MRA], CTA, and duplex/transcranial Doppler), the choice of which depends on local availability and expertise as well as the specific clinical situation. Magnetic resonance imaging (MRI) of the brain for all ischemic stroke patients is standard of care at most stroke centers; per the Guidelines, MRI is better at distinguishing acute, small cortical, small deep, and posterior fossa infarcts; at distinguishing acute from chronic ischemia; and at identifying subclinical satellite ischemic lesions that provide information on stroke mechanism (p. 1668). New techniques including magnetic resonance (MR) and CT perfusion scanning can show the ischemic region in the acute setting and may one day help select patients for specific therapies, but are not yet widely available nor have they been shown to alter outcomes.
An electrocardiogram is indicated for all stroke patients, as is admission to a cardiac telemetry bed for at least 24 hours to document any arrhythmias, the most common being atrial fibrillation (Guidelines, p. 1666, 1673). An echocardiographic study (ECHO) of the heart with bubble study should be performed in most cases (although which cases may specifically benefit is unclear) to identify a cardioembolic source for the stroke, such as low cardiac ejection fraction, atrial septal aneurysm, patent foramen ovale (PFO), or a cardiac thrombus. The bubble study increases the sensitivity of detecting a PFO, which could serve as a gateway for venous embolization to the cerebral arteries. Assuming a large PFO is discovered, other studies such as lower extremity Doppler may be warranted to investigate other potential sources of thrombi (ie, DVT).
Regarding laboratory testing, fasting lipids should be checked as hyperlipidemia is a common modifiable risk factor for ischemic stroke. The Stroke Prevention by Aggressive Reduction in Cholesterol Levels (SPARCL) trial included ischemic stroke patients that had low‐density lipoprotein (LDL) cholesterol between 100 mg/dL and 190 mg/dL and randomized them to receive atorvastatin 80 mg/day vs. placebo. Results showed a 16% relative risk reduction in recurrent stroke; however, there was a small increased risk of intracranial hemorrhage.9 As shown in Table 1, use of a statin on discharge is now a national performance measure for ischemic stroke.
Dissection is a common cause of stroke in young patients without traditional risk factors. Other serologies, such as hypercoagulable studies, may be warranted in patients with no other risk factors for strokes, paradoxical embolus, or of young age (eg, 45 years and under). The arterial hypercoagulable panel consists of antiphospholipid antibody panel, homocysteine levels, lupus anticoagulant levels, and prothrombin time/partial thromboplastin time (PT/PTT). The venous hypercoagulable panel consists of the laboratory values checked, with the arterial hypercoagulable and activated protein C (APC) resistance, Factor VIII activity, Factor II DNA, Factor V DNA if the APC resistance is positive, antithrombin III activity, and activity of proteins C and S. If a patient is found to have a hypercoagulable state, long‐term therapy often involves careful consideration of the choice of antiplatelet therapy vs. anticoagulation with warfarin.10
Initiating Secondary Prevention
Upon admission, the clinician faces a variety of treatment choices for secondary stroke prevention. The proper choice depends on the results of the workup and the presumptive pathophysiology.
Noncardioembolic/Atherothrombotic/Lacunar
The Antithrombotic Trialists' Collaboration meta‐analysis found that patients with a prior stroke or transient ischemic attack (TIA) had a highly significant decrease in the rate of subsequent vascular events (over about 3 years) on antiplatelet therapy (17.8% vs. 21.4%, P 0.0001) and were unable to find a significant difference between low‐dose and high‐dose aspirin for secondary prevention.11 Thus, it is reasonable to place an acute stroke patient naive to antithrombotic therapy on 81 mg of aspirin or 325 mg for long‐term prevention (325 mg is specifically recommended in the acute setting). Several studies such as the WARSS and ESPRIT trials have shown antiplatelet agents to be at least as effective as anticoagulation in noncardioembolic ischemic strokes.12, 13 Guidelines from Europe, the American College of Chest Physicians, and the AHA/ASA all state it is acceptable to choose either aspirin monotherapy, aspirin/extended release dipyridamole combination therapy, or clopidogrel monotherapy as first‐line agents for long‐term secondary prevention in noncardioembolic ischemic stroke.1416 There is no clear evidence that patients who suffer an ischemic stroke while on aspirin will derive additional benefit from increasing the aspirin dose. The newer guidelines go on to recommend aspirin/extended release dipyridamole (ER‐DP) combination therapy or clopidogrel monotherapy over aspirin monotherapy, the former with a stronger level of recommendation based on the results of 2 randomized trials. These recommendations were all published without knowledge of the results of the Prevention Regimen For Effectively Avoiding Second Strokes (PRoFESS) study, which directly compared aspirin/extended release dipyridamole combination therapy to clopidogrel monotherapy for long‐term secondary prevention. The rate of first recurrent stroke was not significantly different between the 2 therapies (9.0% ER‐DP plus aspirin, 8.8% clopidogrel; hazard ratio [HR], 1.01; 95% confidence interval [CI], 0.921.11). Other outcomes also showed few differences, although there were more major hemorrhagic events in the ER‐DP plus aspirin group (4.1% vs. 3.6%; HR, 1.15; 95% CI, 1.001.32; P = 0.06).17
The ASA Stroke Prevention Guideline from 2006 states, with continued relevance, The selection of an antiplatelet agent should be individualized on the basis of patient risk factor profiles, tolerance, and other clinical characteristics.10 Of note, both the Clopidogrel for High Atherothrombotic Risk and Ischemic Stabilization, Management and Avoidance (CHARISMA) and Management of ATherothrombosis with Clopidogrel in High‐risk patients with recent TIA or ischemic stroke (MATCH) trials found a significant increased risk for hemorrhage complications with long‐term use of the aspirin and clopidogrel combination,18, 19 and the 2008 update to the ASA Stroke prevention guidelines state that the addition of aspirin to clopidogrel increases the risk of hemorrhage. Combination therapy of aspirin and clopidogrel is not routinely recommended for ischemic stroke or TIA patients unless they have a specific indication for this therapy (i.e., coronary stent or acute coronary syndrome).15
Atrial Fibrillation
Though our case patient did not have atrial fibrillation, this condition does deserve mention. About 15% to 20% of ischemic stroke patients have atrial fibrillation. The overall risk for stroke in patients with atrial fibrillation is about 5% per year; however, patients who have a history of stroke increase their risk factors for subsequent strokes to about 12% per year. In most cases, anticoagulation has proven to be the superior agent for primary and secondary stroke prevention with warfarin reducing the risk by 67% compared to aspirin, which only reduces the risk of stroke by 20%. A meta‐analysis from 2002 showed that patients who had a prior stroke or TIA decrease their risk of subsequent strokes to 4%/year on oral anticoagulation therapy, resulting in an 8% absolute risk reduction. Patients on aspirin therapy only decrease their risk to 10%/year, or a 2% reduction in stroke events.20 Unless there is a strong contraindication (eg, bleeding diathesis, history of life threatening gastrointestinal [GI] bleeding, history of fall with subdural hematoma, etc.), virtually all ischemic stroke patients with atrial fibrillation should be anticoagulated for life. Anticoagulation in the setting of atrial fibrillation is seriously underutilized.21 The highest quality study on early anticoagulation for ischemic stroke associated with atrial fibrillation suggested that there was no benefit to starting anticoagulation earlier than 2 weeks after a stroke, and there may actually be a higher complication rate (compared to aspirin).22 Other cardiac indications for anticoagulation include left ventricular thrombus and mechanical valves.
Carotid Stenosis
Significant ipsilateral stenosis of the internal carotid artery in a patient with ischemic stroke is a strong indication for intervention, usually a standard carotid endarterectomy (CEA). Stenosis of 70% to 99% is the strongest indication for CEA, and may be of greatest benefit in men, those 75+ years of age, and if surgery is done 2 weeks after the most recent symptoms.23 In patients with minor stroke or TIA, recent recommendations and our practice is to admit to the hospital and perform endarterectomy as soon as possible (those with major stroke may have a greater risk of complications with early CEA).24 Stenting should only be considered instead of CEA if high risk (for surgical complications) criteria are present. These high risk criteria include patients having significant comorbidities and/or anatomic risk factors (ie, recurrent stenosis and/or previous radical neck dissection), and [who] would be poor candidates for CEA in the opinion of a surgeon.25 For stenoses of 50% to 69%, intervention is not as compelling, and decisions should be individualized based on patient characteristics; in this group, stenting should only be considered in the setting of a clinical trial or if an investigational device exemption (IDE) exists at your institution.26
Dissection of the Carotid or Vertebral Arteries
This is a common cause of stroke in younger adults. It should be suspected in patients without other clear causes of stroke and significant disease of the extracranial arteries. Diagnosis can usually be made with CTA or MRA, though it is suggested that the best modality may be T1‐fat‐saturated MRI images of the neck. Debate exists as to the best approach to treatment of dissections due to the absence of randomized trials. A recent comprehensive review suggested anticoagulation for 3 to 6 months followed by indefinite antiplatelet therapy for symptomatic dissections and antiplatelet therapy alone for asymptomatic dissections.27
PFO‐related Stroke
If the patient is found to have a PFO, its role in comparison to traditional risk factors must be weighed carefully. Epidemiological studies suggest that PFO may be most relevant in younger patients, those with cryptogenic stroke (no obvious cause and lack of traditional risk factors), those with higher risk associations including interatrial septal aneurysm, larger PFOs or history of previous cryptogenic stroke.28, 29 The best medical therapy for seemingly PFO‐related ischemic stroke is also unclear; a reasonable approach might be aspirin if neither high‐risk associations nor a hypercoagulable state is present, and warfarin if either are present. Transcatheter closure of PFO is approved by the U.S. Food and Drug Administration (FDA) only under an IDE for patients who have had a recurrent event on maximally tolerated medical treatment, and requires approval from the human research committee (internal review board [IRB]) at your hospital. It is not known if closure is superior or inferior to best medical therapy, and a practice parameter from the American Academy of Neurology strongly encourages appropriate patients to consider participation in ongoing randomized trials.28 Further information on these trials is available at:
Our patient underwent a CTA of the head and neck in the emergency room to see if he would be a candidate for other interventions; unfortunately, he did not meet the time criteria. CTA showed complete occlusion of the left internal carotid artery at the bifurcation with heterogeneous retrograde filling (Supporting Figure 1). Complete occlusion of the proximal third of the left M1 segment was also seen with relative oligemia in the left MCA distribution, though several small peripheral M3/M4 vessels were opacified in the territory indicating collateralization (Supporting Figure 2). A MRI showed a large area of diffusion‐weighted abnormality (Figure 1). Interestingly, the patient's transthoracic echocardiography (TTE), which did not show evidence of a PFO, did reveal a calcified thrombus in the left ventricle. Though no arrhythmias were captured on telemetry, this thrombus does serve as a potential source of cardioembolic emboli to the cerebral vasculature. It was felt that the most likely source of the patient's acute infarct was from artery‐to‐artery emboli from his internal carotid occlusion given the infarct location and the lack of infarction in other vascular distributions (as one might see from a cardiac embolic source). Therefore, his medical management consisted of an antiplatelet regimen for 2 weeks followed by a transition to warfarin alone 2 weeks after his acute infarct as secondary stroke prevention due to the cardiac thrombus. Given the complete occlusion of the internal carotid artery and M1 segment, there was concern that the penumbra might be at risk of infarction (supporting standard guidelines of permissive hypertension). By the end of his hospitalization, the patient had improved and was transferred to inpatient rehabilitation.
The guidelines for acute stroke management continue to rapidly evolve. Certainly, there are effective treatments for acute ischemic stroke, with variation based on the timing of patient arrival at the hospital, the underlying pathophysiology, and the treatment capabilities of the individual hospital. Secondary stroke prevention is extremely important and has been emphasized during inpatient admissions with the establishment of an appropriate medication regime, given that patients are more likely to stay on treatment that is initiated around the time of a diagnosis.29 Evidence strongly suggests that management of acute stroke is improved by an organized approach to care, including the expertise of a multidisciplinary team in a specialized stroke unit. Hospitals committed to high quality of care for acute stroke patients should strongly consider the Joint Commission certification process or an analogous local certification. Such certification demonstrates a hospital's commitment to providing high‐quality care, what every stroke patient wants and deserves.
Inpatient stroke management includes many elements of care, at least as important as the initial portion of the patient's stay, as reviewed in part 1 of this article. The extent of further diagnostic evaluation varies widely depending on apparent risk factors on presentation. Likewise, further therapy, both inpatient and secondary prevention is based on identification of stroke mechanism. Hospitalists are uniquely positioned to have a tremendous impact on both stroke care and the prevention of recurrent disease.
Case Presentation
A 76‐year‐old right‐handed male with a history of hyperlipidemia and myocardial infarction was found at 7 AM with right‐sided paralysis and poor responsiveness on the morning of admission. Upon arrival to the emergency department (ED), with symptoms of partial aphasia, right hemiplegia, and left gaze preference, there was a high suspicion for a left middle cerebral artery (MCA) stroke. Unfortunately, he was excluded from receiving intravenous (IV) tissue plasminogen activator (tPA) or any other acute interventions as the last time he was known to be neurologically intact was the prior evening, which is taken to be the time of onset. Antiplatelet therapy was continued, and the patient admitted for further workup.
Inpatient Care
When an acute ischemic stroke patient is admitted to the hospital, he or she should be placed on a standardized acute stroke protocol (also known as (a.k.a.) a care map, order set, clinical pathway)commonly created by a hospitalist/neurologist and a multidisciplinary team and admitted to a stroke unit. A stroke unit can take many forms, either as a physically separate unit in hospitals with sufficient volume or a floor where a lower volume of stroke patients are always admitted. Multidisciplinary care providers in the stroke unit have special training in stroke, and strong evidence from randomized trials shows that patients cared for in these units have significantly decreased mortality with improved functional outcomes.1 Essentials of the stroke protocol or order set include cardiac telemetry, maintaining euthermia and euglycemia, closely following blood pressure and neurologic status, actively avoiding complications, initiation of secondary prevention treatment, early involvement of rehabilitation services, and patient education.
Euthermia may be assisted by administering scheduled Tylenol to the patient for the first 48 hours, but is not strictly evidence‐based.2 Though euthermia and euglycemia have not been shown to improve outcomes in acute stroke, studies have shown that hyperthermia and hyperglycemia are associated with worsened outcomes for patients with acute strokes.35
Blood Pressure Management
Normally, cerebral vascular autoregulation leads to stable cerebral blood flow over a range of systemic blood pressures. In the setting of an acute stroke, the ability to autoregulate is diminished or absent in regions of and surrounding an acute ischemic stroke; as the area becomes ischemic, autoregulation opens the local vasculature maximally in an effort to drawn in as much blood as possible. Maximally dilated arterioles are perfused in direct correlation with systemic blood pressure, thus any drop in the systemic blood pressure leads to direct decreases in blood flow specifically in the area of ischemia; if there is a penumbra of marginally perfused tissue, such systemic blood pressure drops risk extending the area of fatal ischemia (increasing the size of the ischemic stroke).68 Thus in the acute period of an ischemic stroke, the American Heart Association (AHA)/American Stroke Association (ASA) Guidelines for the Early Management of Adults With Ischemic Stroke (referred to herein as the Guidelines)10 suggest avoid treatment unless systolic blood pressures are >220 or diastolic pressures >105, and review the evidence to support this recommendation (p. 16711672). Those patients who receive tPA have a more stringent blood pressure threshold given their risk of intracranial hemorrhage; systolic blood pressures are accepted up to 180 prior to recommending treatment.
Higher‐quality Inpatient Stroke Care and Harmonized Performance Measures
Beginning in January 2008, a set of 10 performance measures (Table 1) for inpatient acute stroke care have been agreed upon (harmonized) by 3 major stakeholders including the Joint Commission, the ASA's Get with the GuidelinesStroke quality improvement program, and the Center for Disease Control and Prevention's (CDC's) Paul Coverdell Acute stroke registries. These performance measures were selected to help avoid complications (deep vein thrombosis [DVT], aspiration pneumonia), encourage appropriately aggressive care (tPA administration), optimize secondary prevention (antithrombotics, cholesterol lowering, smoking cessation, education), and facilitate functional recovery (early rehabilitation). All 10 measures are appropriate for consideration in every ischemic stroke patient, and 5 are appropriate for the hemorrhagic stroke types.
| Performance measure* | Definition* |
|---|---|
| |
| 1. DVT prophylaxis | Patients who are nonambulatory should start receiving DVT prophylaxis by end of hospital day 2 (can be either compression devices or any low‐dose heparin) |
| 2. Discharged on antithrombotic therapy | Antiplatelet agent(s) or warfarin anticoagulation |
| 3. Patients with atrial fibrillation receiving anticoagulation therapy | A proven approach to secondary prevention in such patients; practice at Harborview varies time of warfarin initiation based on infarct size with larger infarcts waiting up to 2 weeks before initiating warfarin (the best randomized trial showed no benefit for full‐dose low‐molecular‐weight heparin over aspirin in the first 2 weeks)50 |
| 4. Thrombolytic therapy administered | In ischemic stroke patients who arrive at the hospital within 120 minutes (2 hours) of time last known well, for whom IV tPA was initiated at this hospital within 180 minutes (3 hours) of time last known well, and who qualify under strict criteria |
| 5. Antithrombotic therapy by end of hospital day 2 | Usually just antiplatelet agents, a minimal standard of care for ischemic stroke patients; should be started as early as possible, usually in ER |
| 6. Discharged on statin medication | If LDL >100, or not measured or if on a statin drug prior to admission; to reduce risk of subsequent ischemic stroke |
| 7. Dysphagia screening | Prior to any PO food, fluids or medications; to reduce the chances of aspiration pneumonia |
| 8. Stroke education | Including for families if patient unable to participate, must include personal risk factors for stroke, warning signs for stroke, activation of emergency medical system, need for follow‐up after discharge, and medications prescribed |
| 9. Smoking cessation/advice/counseling | For any patient who has smoked in the last year |
| 10. Assessed for rehabilitation | Or received therapy services; to facilitate progress to an optimal function outcome |
Further Workup
After the ischemic stroke patient has had their computed tomography (CT) scan, possibly a computed tomography angiography (CTA), been admitted to the stroke unit, started on an antithrombotic medication, and had their blood pressure appropriately treated, attention then turns to defining the pathophysiology related to the stroke and starting an optimal regimen for secondary prevention. Imaging of the cerebral vasculature including both extracranial and intracranial large vessels is a vital first step in understanding the cause of ischemic stroke. There are multiple potential modalities (magnetic resonance angiography [MRA], CTA, and duplex/transcranial Doppler), the choice of which depends on local availability and expertise as well as the specific clinical situation. Magnetic resonance imaging (MRI) of the brain for all ischemic stroke patients is standard of care at most stroke centers; per the Guidelines, MRI is better at distinguishing acute, small cortical, small deep, and posterior fossa infarcts; at distinguishing acute from chronic ischemia; and at identifying subclinical satellite ischemic lesions that provide information on stroke mechanism (p. 1668). New techniques including magnetic resonance (MR) and CT perfusion scanning can show the ischemic region in the acute setting and may one day help select patients for specific therapies, but are not yet widely available nor have they been shown to alter outcomes.
An electrocardiogram is indicated for all stroke patients, as is admission to a cardiac telemetry bed for at least 24 hours to document any arrhythmias, the most common being atrial fibrillation (Guidelines, p. 1666, 1673). An echocardiographic study (ECHO) of the heart with bubble study should be performed in most cases (although which cases may specifically benefit is unclear) to identify a cardioembolic source for the stroke, such as low cardiac ejection fraction, atrial septal aneurysm, patent foramen ovale (PFO), or a cardiac thrombus. The bubble study increases the sensitivity of detecting a PFO, which could serve as a gateway for venous embolization to the cerebral arteries. Assuming a large PFO is discovered, other studies such as lower extremity Doppler may be warranted to investigate other potential sources of thrombi (ie, DVT).
Regarding laboratory testing, fasting lipids should be checked as hyperlipidemia is a common modifiable risk factor for ischemic stroke. The Stroke Prevention by Aggressive Reduction in Cholesterol Levels (SPARCL) trial included ischemic stroke patients that had low‐density lipoprotein (LDL) cholesterol between 100 mg/dL and 190 mg/dL and randomized them to receive atorvastatin 80 mg/day vs. placebo. Results showed a 16% relative risk reduction in recurrent stroke; however, there was a small increased risk of intracranial hemorrhage.9 As shown in Table 1, use of a statin on discharge is now a national performance measure for ischemic stroke.
Dissection is a common cause of stroke in young patients without traditional risk factors. Other serologies, such as hypercoagulable studies, may be warranted in patients with no other risk factors for strokes, paradoxical embolus, or of young age (eg, 45 years and under). The arterial hypercoagulable panel consists of antiphospholipid antibody panel, homocysteine levels, lupus anticoagulant levels, and prothrombin time/partial thromboplastin time (PT/PTT). The venous hypercoagulable panel consists of the laboratory values checked, with the arterial hypercoagulable and activated protein C (APC) resistance, Factor VIII activity, Factor II DNA, Factor V DNA if the APC resistance is positive, antithrombin III activity, and activity of proteins C and S. If a patient is found to have a hypercoagulable state, long‐term therapy often involves careful consideration of the choice of antiplatelet therapy vs. anticoagulation with warfarin.10
Initiating Secondary Prevention
Upon admission, the clinician faces a variety of treatment choices for secondary stroke prevention. The proper choice depends on the results of the workup and the presumptive pathophysiology.
Noncardioembolic/Atherothrombotic/Lacunar
The Antithrombotic Trialists' Collaboration meta‐analysis found that patients with a prior stroke or transient ischemic attack (TIA) had a highly significant decrease in the rate of subsequent vascular events (over about 3 years) on antiplatelet therapy (17.8% vs. 21.4%, P 0.0001) and were unable to find a significant difference between low‐dose and high‐dose aspirin for secondary prevention.11 Thus, it is reasonable to place an acute stroke patient naive to antithrombotic therapy on 81 mg of aspirin or 325 mg for long‐term prevention (325 mg is specifically recommended in the acute setting). Several studies such as the WARSS and ESPRIT trials have shown antiplatelet agents to be at least as effective as anticoagulation in noncardioembolic ischemic strokes.12, 13 Guidelines from Europe, the American College of Chest Physicians, and the AHA/ASA all state it is acceptable to choose either aspirin monotherapy, aspirin/extended release dipyridamole combination therapy, or clopidogrel monotherapy as first‐line agents for long‐term secondary prevention in noncardioembolic ischemic stroke.1416 There is no clear evidence that patients who suffer an ischemic stroke while on aspirin will derive additional benefit from increasing the aspirin dose. The newer guidelines go on to recommend aspirin/extended release dipyridamole (ER‐DP) combination therapy or clopidogrel monotherapy over aspirin monotherapy, the former with a stronger level of recommendation based on the results of 2 randomized trials. These recommendations were all published without knowledge of the results of the Prevention Regimen For Effectively Avoiding Second Strokes (PRoFESS) study, which directly compared aspirin/extended release dipyridamole combination therapy to clopidogrel monotherapy for long‐term secondary prevention. The rate of first recurrent stroke was not significantly different between the 2 therapies (9.0% ER‐DP plus aspirin, 8.8% clopidogrel; hazard ratio [HR], 1.01; 95% confidence interval [CI], 0.921.11). Other outcomes also showed few differences, although there were more major hemorrhagic events in the ER‐DP plus aspirin group (4.1% vs. 3.6%; HR, 1.15; 95% CI, 1.001.32; P = 0.06).17
The ASA Stroke Prevention Guideline from 2006 states, with continued relevance, The selection of an antiplatelet agent should be individualized on the basis of patient risk factor profiles, tolerance, and other clinical characteristics.10 Of note, both the Clopidogrel for High Atherothrombotic Risk and Ischemic Stabilization, Management and Avoidance (CHARISMA) and Management of ATherothrombosis with Clopidogrel in High‐risk patients with recent TIA or ischemic stroke (MATCH) trials found a significant increased risk for hemorrhage complications with long‐term use of the aspirin and clopidogrel combination,18, 19 and the 2008 update to the ASA Stroke prevention guidelines state that the addition of aspirin to clopidogrel increases the risk of hemorrhage. Combination therapy of aspirin and clopidogrel is not routinely recommended for ischemic stroke or TIA patients unless they have a specific indication for this therapy (i.e., coronary stent or acute coronary syndrome).15
Atrial Fibrillation
Though our case patient did not have atrial fibrillation, this condition does deserve mention. About 15% to 20% of ischemic stroke patients have atrial fibrillation. The overall risk for stroke in patients with atrial fibrillation is about 5% per year; however, patients who have a history of stroke increase their risk factors for subsequent strokes to about 12% per year. In most cases, anticoagulation has proven to be the superior agent for primary and secondary stroke prevention with warfarin reducing the risk by 67% compared to aspirin, which only reduces the risk of stroke by 20%. A meta‐analysis from 2002 showed that patients who had a prior stroke or TIA decrease their risk of subsequent strokes to 4%/year on oral anticoagulation therapy, resulting in an 8% absolute risk reduction. Patients on aspirin therapy only decrease their risk to 10%/year, or a 2% reduction in stroke events.20 Unless there is a strong contraindication (eg, bleeding diathesis, history of life threatening gastrointestinal [GI] bleeding, history of fall with subdural hematoma, etc.), virtually all ischemic stroke patients with atrial fibrillation should be anticoagulated for life. Anticoagulation in the setting of atrial fibrillation is seriously underutilized.21 The highest quality study on early anticoagulation for ischemic stroke associated with atrial fibrillation suggested that there was no benefit to starting anticoagulation earlier than 2 weeks after a stroke, and there may actually be a higher complication rate (compared to aspirin).22 Other cardiac indications for anticoagulation include left ventricular thrombus and mechanical valves.
Carotid Stenosis
Significant ipsilateral stenosis of the internal carotid artery in a patient with ischemic stroke is a strong indication for intervention, usually a standard carotid endarterectomy (CEA). Stenosis of 70% to 99% is the strongest indication for CEA, and may be of greatest benefit in men, those 75+ years of age, and if surgery is done 2 weeks after the most recent symptoms.23 In patients with minor stroke or TIA, recent recommendations and our practice is to admit to the hospital and perform endarterectomy as soon as possible (those with major stroke may have a greater risk of complications with early CEA).24 Stenting should only be considered instead of CEA if high risk (for surgical complications) criteria are present. These high risk criteria include patients having significant comorbidities and/or anatomic risk factors (ie, recurrent stenosis and/or previous radical neck dissection), and [who] would be poor candidates for CEA in the opinion of a surgeon.25 For stenoses of 50% to 69%, intervention is not as compelling, and decisions should be individualized based on patient characteristics; in this group, stenting should only be considered in the setting of a clinical trial or if an investigational device exemption (IDE) exists at your institution.26
Dissection of the Carotid or Vertebral Arteries
This is a common cause of stroke in younger adults. It should be suspected in patients without other clear causes of stroke and significant disease of the extracranial arteries. Diagnosis can usually be made with CTA or MRA, though it is suggested that the best modality may be T1‐fat‐saturated MRI images of the neck. Debate exists as to the best approach to treatment of dissections due to the absence of randomized trials. A recent comprehensive review suggested anticoagulation for 3 to 6 months followed by indefinite antiplatelet therapy for symptomatic dissections and antiplatelet therapy alone for asymptomatic dissections.27
PFO‐related Stroke
If the patient is found to have a PFO, its role in comparison to traditional risk factors must be weighed carefully. Epidemiological studies suggest that PFO may be most relevant in younger patients, those with cryptogenic stroke (no obvious cause and lack of traditional risk factors), those with higher risk associations including interatrial septal aneurysm, larger PFOs or history of previous cryptogenic stroke.28, 29 The best medical therapy for seemingly PFO‐related ischemic stroke is also unclear; a reasonable approach might be aspirin if neither high‐risk associations nor a hypercoagulable state is present, and warfarin if either are present. Transcatheter closure of PFO is approved by the U.S. Food and Drug Administration (FDA) only under an IDE for patients who have had a recurrent event on maximally tolerated medical treatment, and requires approval from the human research committee (internal review board [IRB]) at your hospital. It is not known if closure is superior or inferior to best medical therapy, and a practice parameter from the American Academy of Neurology strongly encourages appropriate patients to consider participation in ongoing randomized trials.28 Further information on these trials is available at:
Our patient underwent a CTA of the head and neck in the emergency room to see if he would be a candidate for other interventions; unfortunately, he did not meet the time criteria. CTA showed complete occlusion of the left internal carotid artery at the bifurcation with heterogeneous retrograde filling (Supporting Figure 1). Complete occlusion of the proximal third of the left M1 segment was also seen with relative oligemia in the left MCA distribution, though several small peripheral M3/M4 vessels were opacified in the territory indicating collateralization (Supporting Figure 2). A MRI showed a large area of diffusion‐weighted abnormality (Figure 1). Interestingly, the patient's transthoracic echocardiography (TTE), which did not show evidence of a PFO, did reveal a calcified thrombus in the left ventricle. Though no arrhythmias were captured on telemetry, this thrombus does serve as a potential source of cardioembolic emboli to the cerebral vasculature. It was felt that the most likely source of the patient's acute infarct was from artery‐to‐artery emboli from his internal carotid occlusion given the infarct location and the lack of infarction in other vascular distributions (as one might see from a cardiac embolic source). Therefore, his medical management consisted of an antiplatelet regimen for 2 weeks followed by a transition to warfarin alone 2 weeks after his acute infarct as secondary stroke prevention due to the cardiac thrombus. Given the complete occlusion of the internal carotid artery and M1 segment, there was concern that the penumbra might be at risk of infarction (supporting standard guidelines of permissive hypertension). By the end of his hospitalization, the patient had improved and was transferred to inpatient rehabilitation.
The guidelines for acute stroke management continue to rapidly evolve. Certainly, there are effective treatments for acute ischemic stroke, with variation based on the timing of patient arrival at the hospital, the underlying pathophysiology, and the treatment capabilities of the individual hospital. Secondary stroke prevention is extremely important and has been emphasized during inpatient admissions with the establishment of an appropriate medication regime, given that patients are more likely to stay on treatment that is initiated around the time of a diagnosis.29 Evidence strongly suggests that management of acute stroke is improved by an organized approach to care, including the expertise of a multidisciplinary team in a specialized stroke unit. Hospitals committed to high quality of care for acute stroke patients should strongly consider the Joint Commission certification process or an analogous local certification. Such certification demonstrates a hospital's commitment to providing high‐quality care, what every stroke patient wants and deserves.
- Organised inpatient (stroke unit) care for stroke.Stroke Unit Trialists' Collaboration.Cochrane Database Syst Rev.2000(2):CD000197.
- ,,, et al.Acetaminophen for altering body temperature in acute stroke: a randomized clinical trial.Stroke.2002;33(1):130–134.
- ,,, et al.Fever in acute stroke worsens prognosis. A prospective study.Stroke.1995;26(11):2040–2043.
- ,.Combating hyperthermia in acute stroke: a significant clinical concern.Stroke.1998;29(2):529–534.
- ,,, et al.Body temperature in acute stroke: relation to stroke severity, infarct size, mortality, and outcome.Lancet. 171996;347(8999):422–425.
- ,,.Thresholds in cerebral ischemia—the ischemic penumbra.Stroke.1981;12(6):723–725.
- .Ischaemic brain damage of cerebral perfusion failure type after treatment of severe hypertension.Br Med J. 271975;4(5999):739.
- ,,,,.Imaging of acute stroke.Lancet Neurol.2006;5(9):755–768.
- ,,, et al.High‐dose atorvastatin after stroke or transient ischemic attack.N Engl J Med.2006;355(6):549–559.
- ,,, et al.Guidelines for prevention of stroke in patients with ischemic stroke or transient ischemic attack: a statement for healthcare professionals from the American Heart Association/American Stroke Association Council on Stroke: co‐sponsored by the Council on Cardiovascular Radiology and Intervention: the American Academy of Neurology affirms the value of this guideline.Stroke.2006;37(2):577–617.
- Antithrombotic Trialists' Collaboration.Collaborative meta‐analysis of randomised trials of antiplatelet therapy for prevention of death, myocardial infarction, and stroke in high risk patients.BMJ.2002;324(7329):71–86.
- ,,, et al.A comparison of warfarin and aspirin for the prevention of recurrent ischemic stroke.N Engl J Med.2001;345(20):1444–1451.
- .Warfarin or aspirin for recurrent ischemic stroke.N Engl J Med.2002;346(15):1169–1171.
- ,,, et al.Prevention. European Stroke Initiative.Cerebrovasc Dis.2004;17(suppl 2):15–29.
- ,,, et al.Update to the AHA/ASA recommendations for the prevention of stroke in patients with stroke and transient ischemic attack.Stroke.2008;39(5):1647–1652.
- ,,,,.Antithrombotic and thrombolytic therapy for ischemic stroke: American College of Chest Physicians Evidence‐Based Clinical Practice Guidelines (8th edition).Chest.2008;133(suppl):630S–669S.
- ,,, et al.Aspirin and extended‐release dipyridamole versus clopidogrel for recurrent stroke.N Engl J Med.2008;359(12):1238–1251.
- ,,, et al.Clopidogrel and aspirin versus aspirin alone for the prevention of atherothrombotic events.N Engl J Med.2006;354(16):1706–1717.
- ,,, et al.Aspirin and clopidogrel compared with clopidogrel alone after recent ischaemic stroke or transient ischaemic attack in high‐risk patients (MATCH): randomised, double‐blind, placebo‐controlled trial.Lancet.2004;364(9431):331–337.
- ,,, et al.Oral anticoagulants vs aspirin in nonvalvular atrial fibrillation: an individual patient meta‐analysis.JAMA.2002;288(19):2441–2448.
- .Effective anticoagulation therapy: defining the gap between clinical studies and clinical practice.Am J Manag Care.2004;10(suppl):S297–S306; discussionS312–S297.
- ,,,.Low molecular‐weight heparin versus aspirin in patients with acute ischaemic stroke and atrial fibrillation: a double‐blind randomised study. HAEST Study Group. Heparin in Acute Embolic Stroke Trial.Lancet.2000;355(9211):1205–1210.
- ,,,,.Endarterectomy for symptomatic carotid stenosis in relation to clinical subgroups and timing of surgery.Lancet.2004;363(9413):915–924.
- ,,.The timing of carotid endarterectomy post stroke.Neurol Clin.2006;24(4):669–680.
- Centers for Medicare and Medicaid Services (CMS). Department of Health and Human Services (DHHS). CMS Manual System. Pub 100–03 Medicare National Coverage Determinations. Available at: http://www.cms.hhs.gov/Transmittals/Downloads/R64NCD.pdf. Accessed May2009.
- .Current status of carotid endarterectomy and stenting for symptomatic carotid stenosis.Cerebrovasc Dis.2007;24(suppl 1):116–125.
- ,,, et al.Antiplatelets versus anticoagulation in cervical artery dissection.Stroke.2007;38(9):2605–2611.
- ,,, et al.A comparison of warfarin and aspirin for the prevention of recurrent ischemic stroke.N Engl J Med2001;345(20):1444–1451.
- .Warfarin or aspirin for recurrent ischemic stroke.N Engl J Med2002;346(15):1169–1171.
- ,,, et al.Practice parameter: recurrent stroke with patent foramen ovale and atrial septal aneurysm: report of the Quality Standards Subcommittee of the American Academy of Neurology.Neurology.2004;62(7):1042–1050.
- ,,, et al.In‐hospital initiation of secondary stroke prevention therapies yields high rates of adherence at follow‐up.Stroke.2004;35(12):2879–2883.
- Organised inpatient (stroke unit) care for stroke.Stroke Unit Trialists' Collaboration.Cochrane Database Syst Rev.2000(2):CD000197.
- ,,, et al.Acetaminophen for altering body temperature in acute stroke: a randomized clinical trial.Stroke.2002;33(1):130–134.
- ,,, et al.Fever in acute stroke worsens prognosis. A prospective study.Stroke.1995;26(11):2040–2043.
- ,.Combating hyperthermia in acute stroke: a significant clinical concern.Stroke.1998;29(2):529–534.
- ,,, et al.Body temperature in acute stroke: relation to stroke severity, infarct size, mortality, and outcome.Lancet. 171996;347(8999):422–425.
- ,,.Thresholds in cerebral ischemia—the ischemic penumbra.Stroke.1981;12(6):723–725.
- .Ischaemic brain damage of cerebral perfusion failure type after treatment of severe hypertension.Br Med J. 271975;4(5999):739.
- ,,,,.Imaging of acute stroke.Lancet Neurol.2006;5(9):755–768.
- ,,, et al.High‐dose atorvastatin after stroke or transient ischemic attack.N Engl J Med.2006;355(6):549–559.
- ,,, et al.Guidelines for prevention of stroke in patients with ischemic stroke or transient ischemic attack: a statement for healthcare professionals from the American Heart Association/American Stroke Association Council on Stroke: co‐sponsored by the Council on Cardiovascular Radiology and Intervention: the American Academy of Neurology affirms the value of this guideline.Stroke.2006;37(2):577–617.
- Antithrombotic Trialists' Collaboration.Collaborative meta‐analysis of randomised trials of antiplatelet therapy for prevention of death, myocardial infarction, and stroke in high risk patients.BMJ.2002;324(7329):71–86.
- ,,, et al.A comparison of warfarin and aspirin for the prevention of recurrent ischemic stroke.N Engl J Med.2001;345(20):1444–1451.
- .Warfarin or aspirin for recurrent ischemic stroke.N Engl J Med.2002;346(15):1169–1171.
- ,,, et al.Prevention. European Stroke Initiative.Cerebrovasc Dis.2004;17(suppl 2):15–29.
- ,,, et al.Update to the AHA/ASA recommendations for the prevention of stroke in patients with stroke and transient ischemic attack.Stroke.2008;39(5):1647–1652.
- ,,,,.Antithrombotic and thrombolytic therapy for ischemic stroke: American College of Chest Physicians Evidence‐Based Clinical Practice Guidelines (8th edition).Chest.2008;133(suppl):630S–669S.
- ,,, et al.Aspirin and extended‐release dipyridamole versus clopidogrel for recurrent stroke.N Engl J Med.2008;359(12):1238–1251.
- ,,, et al.Clopidogrel and aspirin versus aspirin alone for the prevention of atherothrombotic events.N Engl J Med.2006;354(16):1706–1717.
- ,,, et al.Aspirin and clopidogrel compared with clopidogrel alone after recent ischaemic stroke or transient ischaemic attack in high‐risk patients (MATCH): randomised, double‐blind, placebo‐controlled trial.Lancet.2004;364(9431):331–337.
- ,,, et al.Oral anticoagulants vs aspirin in nonvalvular atrial fibrillation: an individual patient meta‐analysis.JAMA.2002;288(19):2441–2448.
- .Effective anticoagulation therapy: defining the gap between clinical studies and clinical practice.Am J Manag Care.2004;10(suppl):S297–S306; discussionS312–S297.
- ,,,.Low molecular‐weight heparin versus aspirin in patients with acute ischaemic stroke and atrial fibrillation: a double‐blind randomised study. HAEST Study Group. Heparin in Acute Embolic Stroke Trial.Lancet.2000;355(9211):1205–1210.
- ,,,,.Endarterectomy for symptomatic carotid stenosis in relation to clinical subgroups and timing of surgery.Lancet.2004;363(9413):915–924.
- ,,.The timing of carotid endarterectomy post stroke.Neurol Clin.2006;24(4):669–680.
- Centers for Medicare and Medicaid Services (CMS). Department of Health and Human Services (DHHS). CMS Manual System. Pub 100–03 Medicare National Coverage Determinations. Available at: http://www.cms.hhs.gov/Transmittals/Downloads/R64NCD.pdf. Accessed May2009.
- .Current status of carotid endarterectomy and stenting for symptomatic carotid stenosis.Cerebrovasc Dis.2007;24(suppl 1):116–125.
- ,,, et al.Antiplatelets versus anticoagulation in cervical artery dissection.Stroke.2007;38(9):2605–2611.
- ,,, et al.A comparison of warfarin and aspirin for the prevention of recurrent ischemic stroke.N Engl J Med2001;345(20):1444–1451.
- .Warfarin or aspirin for recurrent ischemic stroke.N Engl J Med2002;346(15):1169–1171.
- ,,, et al.Practice parameter: recurrent stroke with patent foramen ovale and atrial septal aneurysm: report of the Quality Standards Subcommittee of the American Academy of Neurology.Neurology.2004;62(7):1042–1050.
- ,,, et al.In‐hospital initiation of secondary stroke prevention therapies yields high rates of adherence at follow‐up.Stroke.2004;35(12):2879–2883.
Management of Ischemic Stroke: Part 1
The term stroke is defined by the World Health Organization as rapidly developed clinical signs of focal (or global) disturbance of cerebral function lasting more than 24 hours (unless interrupted by surgery or death), with no apparent cause other than a vascular origin; it includes patients presenting clinical signs and symptoms suggestive of subarachnoid hemorrhage (SAH), intracerebral hemorrhage, or cerebral ischemic necrosis.1 Stroke is 1 of the leading causes of death and the number 1 cause of long‐term disability in the United States, with over 700,000 strokes and over 150,000 stroke deaths each year.2
Given the projections of 30,000 hospitalists nationally by 2010 (
Case Presentation
A 76‐year‐old right‐handed male with a history of hyperlipidemia and myocardial infarction was found at 7 AM with right‐sided paralysis and poor responsiveness on the morning of admission. He seemed to prefer looking to the left and to understand what was being said to him, but had great difficulty speaking. When he went to bed at 9 PM, he was at his neurological baseline. Upon finding him that morning, his wife called 911.
With increased knowledge regarding the pathophysiology of stroke, it has become clear that timeliness is of utmost importance (time is brain) and that acute stroke should be regarded as an acute medical/neurological emergency.
This article reviews the approach in evaluating an acute stroke patient, management strategies, and treatment options. Where not otherwise referenced, data to support our comments come from the recently updated and exhaustive American Heart Association (AHA)/American Stroke Association (ASA) Guidelines for the Early Management of Adults With Ischemic Stroke and will be referred to herein as the Guidelines.4 Harborview Medical Center in Seattle is a Joint Commissioncertified Primary Stroke Center and the home hospital of 2 of the authors (C.L.E., D.L.T.); it is referred to herein as Harborview.
Emergency Room Care (see Acute Stroke Algorithm, Figure 1)
The First 15 Minutes
After assuring stable airway, breathing, and circulation, immediate (STAT) blood draws should be performed, including full complete blood count (CBC) with platelets, international normalized ratio/prothrombin time/partial thromboplastin time (INR/PT/PTT), full electrolytes, and glucose (finger‐stick blood glucose also recommended). Glasgow Coma Scale (GCS) score and NIH Stroke Scale (NIHSS) score should be established via a focused history and physical exam. The GCS is most appropriate for patients with a significantly depressed level of consciousness, while the NIHSS can be scored for any stroke patient (1‐page version of NIHSS used at Harborview is shown in Figure 2). By quantifying stroke severity, the NIHSS score helps both to facilitate communication about neurologic deficit as well as serve as a documented baseline in case of subsequent clinical change. Emergency department (ED) physicians, hospitalists, neurologists, and nursing staff regularly caring for acute stroke patients would be well‐served by obtaining certification in the NIHSS (available free online at
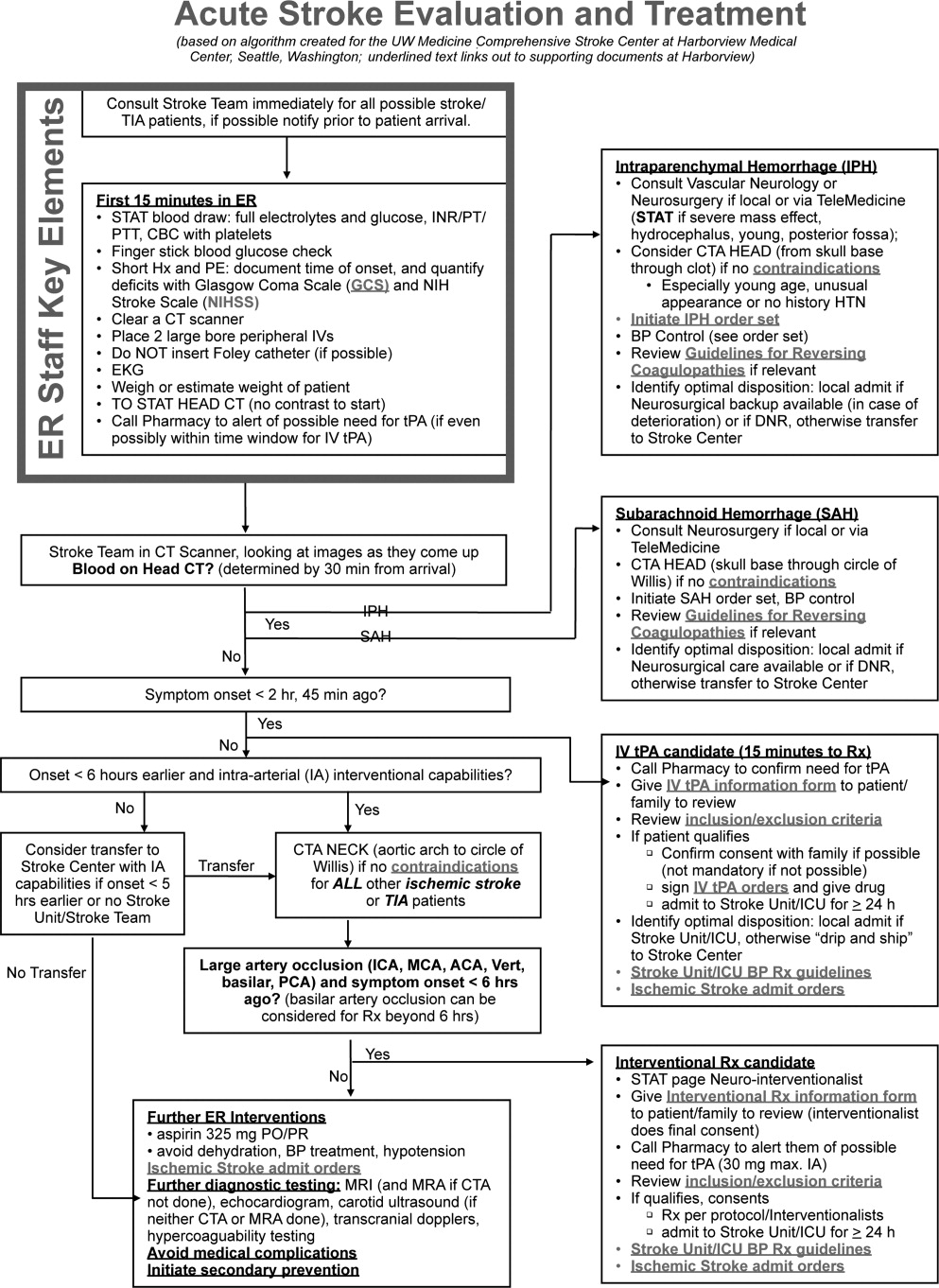
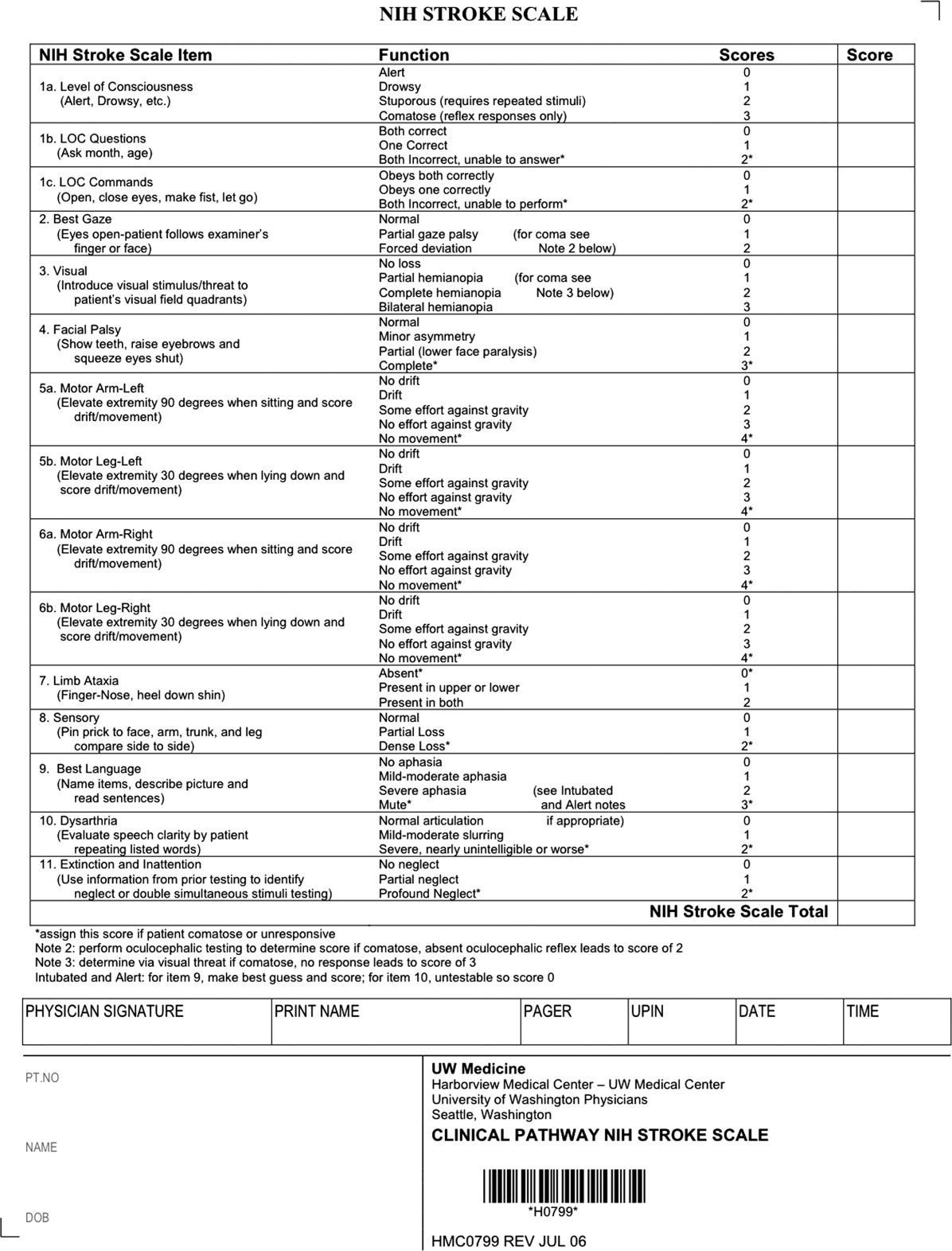
Our case patient's initial NIHSS score was 15, with points given for drowsiness, inability to answer questions, partial facial palsy, no movement in right arm or leg, mild‐moderate aphasia, and mild‐moderate dysarthria (Figure 2).
Differential Diagnosis
Many acute conditions can mimic stroke, and 1 of the goals of the initial emergency room (ER) evaluation is to rule out such stroke mimics. A report of 411 initial ER stroke diagnoses identified 19% as stroke mimics; the most common mimic diagnoses were seizure, systemic infection, brain tumor, and toxic‐metabolic.5 The same study identified decreased level of alertness as associated with a final mimic diagnosis and history of angina as associated with a final diagnosis of stroke. Another study looked at 350 presentations with an initial stroke diagnosis and found 31% stroke mimics; similarly, the main alternative diagnoses were seizure, sepsis, toxic‐metabolic, space‐occupying lesion, and syncope/presyncope.6 Findings associated with a mimic diagnosis included no cognitive impairment and abnormal findings in any other system, while findings associated with a stroke diagnosis were a definite history of focal neurological symptoms, NIHSS score, stroke type classification possible, an exact onset that could be determined, and abnormal vascular findings on imaging.6
Initial Imaging
The patient should receive a STAT noncontrast head CT to evaluate for the presence or absence of blood. At this time, magnetic resonance imaging (MRI) is not essential to confirm the diagnosis of ischemic stroke, as diagnosis is based on clinical suspicion. MRI is more sensitive at imaging acute ischemia (on diffusion‐weighted sequences) and recently has been shown to be equally sensitive in identifying acute blood (previously thought to be a relative advantage of CT).7, 8 Practical and pervasive barriers to emergent MRI include study duration, significant patient cooperation, and that few hospitals are currently set up to perform such rapid MRIS. The Guidelines specifically state that In most instances, CT will provide the information to make decisions about emergency management (p. 1668),4 that vascular imaging should not delay treatment of patients whose symptoms started 3 hours ago and who have acute ischemic stroke, and that emergency treatment of stroke should not be delayed in order to obtain multimodal imaging studies (p. 1669).4
Our case patient's initial imaging, a noncontrast head CT (Supporting Figures 1 and 2), showed subtle clues consistent with the diagnosis of acute ischemic stroke. These include a hyperdense middle cerebral artery (MCA) sign (presumably representing thrombus), possible obscuration of the basal ganglia, and, importantly, no acute intraparenchymal (IPH), SAH, or subdural hemorrhage.
Acute Treatments
After the patient's head CT is completed, the next steps are dependent upon what was seen on the scan and the time from symptom onset.
Blood on the CT Scan
If the initial brain imaging reveals IPH or SAH, further diagnostic testing and early treatments are quite different than for ischemic stroke. New guidelines are available for IPH management,9 and there have been recent review articles of care for SAH.1012 At the authors' institutions, early care of such patients always involves aggressive reversal of any antithrombotic medications the patient was taking prior to presentation. Our approach to warfarin reversal includes vitamin K and fresh frozen plasma (FFP) to achieve an INR 1.4; others have used prothrombin complex concentrate (PCC).13 Blood pressure (BP) treatment goals are generally more aggressive than for ischemic stroke, while supportive care to avoid aspiration, hyperglycemia, fever, and venous thrombosis (here initially with sequential compression devices alone) are similar. Early estimation of prognosis for these patients with IPH and SAH and discussions with families about continued aggressive care are of utmost importance, and should involve providers with sufficient expertise. Care should be taken to avoid overly pessimistic early prognostication, as early do not resuscitate (DNR) decisions in intercranial hemorrhage (ICH) can become a self‐fulfilling prophecy.1416 If the decision is to continue aggressive and supportive care, or if an appropriately expert consultation is not available at the presentation hospital, IPH and SAH patients should be considered for transfer to a hospital with the appropriate resources (including emergency access to neurosurgeons) or be evaluated by such an expert by telemedicine if available.
No Blood on the CT Scan, Results Back in 3 Hours From Symptom Onset
If such a patient is not rapidly resolving their symptoms, and the diagnosis continues to remain clear, inclusion/exclusion criteria for IV tPA should be reviewed (Table 1). Consent should be obtained much like any other procedure with significant risk. As many consider tPA to be standard of care, it is reasonable to proceed in cases of unobtainable consent as one would with any other emergent therapy. This situation is a topic of ongoing debate.17, 18 The Guidelines state that although written consent is not necessary before administration of recombinant tPA (rtPA) for treatment of stroke, a full discussion of the potential risks and benefits of treatment with rtPA with the family and the patient if possible is recommended (p. 1676).4 After tPA is given in the ER, the patient should be admitted to an intensive care unit (ICU) setting for 24 hours for careful monitoring of BP, avoidance of invasive procedures, and no use of antithrombotic medications during that period of time.
| Comments (from the authors) | |
|---|---|
| |
| Inclusion criteria | |
| Diagnosis of ischemic stroke causing measurable neurological deficit | Usually NIHSS > 4 |
| Neurological signs should not be clearing spontaneously | Such a patient may do well without tPA, but there is debate82 |
| Neurological signs should not be minor and isolated. | |
| Onset of symptoms >3 hours before beginning treatment | |
| Patient or family members understand the potential risks and benefits from treatment | Debated, as tPA considered standard of care by many |
| Cautionary criteria | |
| Caution should be exercised in treating a patient with major deficits | Higher risk of hemorrhage, but still may benefit from treatment |
| Exclusion criteria | |
| Symptoms of stroke should not be suggestive of subarachnoid hemorrhage | |
| No head trauma or prior stroke in previous 3 months | |
| No myocardial infarction in the previous 3 months | |
| No gastrointestinal or urinary tract hemorrhage in previous 21 days | |
| No major surgery in the previous 14 days | |
| No arterial puncture at a noncompressible site in the previous 7 days | |
| No history of previous intracranial hemorrhage | |
| Blood pressure not elevated (systolic >185 mm Hg or diastolic 110 mm Hg) | Okay to bring down with labetolol, nitropaste, or nicardipine* |
| No evidence of active bleeding or acute trauma (fracture) on examination | |
| Not taking an oral anticoagulant or, if anticoagulant being taken, INR 1.7 | |
| If receiving heparin in previous 48 hours, aPTT must be in normal range | |
| Platelet count 100,000 mm3 | |
| Blood glucose concentration 50 mg/dL (2.7 mmol/L) | |
| Seizure with postictal residual neurological impairments | Not absolute if treating physician feels stroke also present, or if confirmed by imaging |
| CT does not show a multilobar infarction (hypodensity >1/3 cerebral hemisphere) | Not strictly evidence based, in NINDS trial this finding did not preclude benefit of tPA |
Based mainly on the results of the National Institute of Neurological Disorders and Stroke (NINDS) tPA trial,19 and recently supported by a large Phase IV observational study from the European Union,20 IV tPA for acute ischemic stroke is approved for use in many countries and is endorsed for the treatment of carefully selected ischemic stroke patients in a number of practice guidelines.4 Despite this, the emergency medicine community has been less enthusiastic about the use of IV tPA.21, 22 Although the risk of hemorrhagic complications is greater in certain subgroups of patients (ie, the most severe strokes, significant early CT changes, older age), there is no definitive evidence to suggest that these groups do not still benefit from the treatment.23 It is also clear that if patients are not carefully selected, meeting strict inclusion and exclusion criteria, the rate of complications is increased.24 Thus, as summarized in a practice statement of the American College of Emergency Physicians, There is insufficient evidence at this time to endorse the use of intravenous tPA in clinical practice when systems are not in place to ensure that the inclusion/exclusion criteria established by the NINDS guidelines for tPA use in acute stroke are followed.21 When counseling patients and their families about the benefits and risks of IV tPA, one should keep in mind that the NINDS trial demonstrated increased odds of excellent outcomes despite a significant 10‐fold increase in the risk of symptomatic intracranial hemorrhage (6.4% vs. 0.6%), and did not alter 30‐day mortality. The largest Phase IV cohort study of IV tPA treatment, Safe Implementation of Thrombolysis in Stroke Monitoring Study (SITS‐MOST) was mandated by the European Union upon approval of the medication for use in acute ischemic stroke.20 The results in 6483 patients showed that tPA, when used in strict accordance with published inclusion and exclusion criteria, could perform as well as it did in randomized trials.
The recently published European Cooperative Acute Stroke Study3 (ECASS‐3) trial demonstrated that IV tPA has efficacy with adequate safety up to 4.5 hours after the onset of symptoms. A total of 821 patients were enrolled and 375 received tPA. Exclusion criteria included diabetes being treated with medication with a history of prior stroke, an NIHSS score >25, or treatment with warfarin. The rates of hemorrhage (27.0% vs. 17.6%, P = 0.001) were in line with those of the SITS‐MOST study patients who were treated within the 3‐hour time window. There was no significant difference in mortality (7.7% tPA vs. 8.4% placebo). This study is relatively new; therefore, the data have not been reviewed by guideline committees.25
No Blood on the CT Scan, Results Back in >3 Hours, but 8 Hours, From Symptom Onset
Unfortunately as with our patient, most people do not present to an ER in a timely fashion. Nonetheless, there may be other treatments and interventions possible. If the patient arrives 8 hours from onset of symptoms, intraarterial (IA) interventions are a possibility. In such a case, a CT angiogram (CTA) of the neck from the arch of the aorta to the circle of Willis is recommended (barring any contraindications such as renal failure or iodine allergy). The rationale behind this study is that other treatment options, such as IA tPA or mechanical thrombectomy may be considered if a large arterial occlusion is identified. CTA is preferred over magnetic resonance angiography (MRA) due to the same time and patient cooperation issues mentioned above, though some expert centers may be set up to perform MRI and MRA rapidly in the acute setting. CTA or MRA is of great value early on in the emergent assessment of ischemic stroke patients, as it allows detailed evaluation of the cerebral vasculature; this knowledge helps define the pathophysiology of the ongoing stroke (eg, is there a larger artery occlusion?) and can help inform the approach to subsequent therapies.
The Guidelines (p. 1678)4 recommend IA thrombolysis as a treatment option if it can be started within 6 hours, based on results from the Prolyse in Acute Cerebral Thromboembolism (PROACT) II trial. This study involved angiography with identification of the occluded vessel (the proximal MCA‐M1 in this study) and administration of recombinant pro‐urokinase to the clot with functional outcome as the primary endpoint.26 At 3 months, patients who received the IA thrombolytic had a 40% chance of slight disability; unable to carry out all previous activities, but able to look after own affairs without assistance or better (ie, a modified Rankin Scale score of 2) vs. 25% of those not receiving the IA thrombolytic. Pro‐urokinase is not available in the United States; therefore, many institutions substitute IA tPA. The Guidelines further state that IA thrombolysis can be considered for use in some patients with contraindications to IV tPA (eg, recent surgery), but should not be used instead of IV tPA in patients otherwise eligible (p. 1678).4
There are now two U.S. Food and Drug Administration (FDA)‐approved devices for mechanical cerebral vasculature thrombectomy for use up to 8 hours from symptom onset. The mechanical embolus removal in cerebral ischemia (MERCI) clot retrieval device was originally approved by the FDA in August 2004 for restoring blood flow in the neurovasculature by removing thrombus in patients experiencing ischemic stroke. Modified devices have been approved as recently as January 2007.27 The Penumbra System was FDA‐approved in December 2007 for revascularization of patients with acute ischemic stroke secondary to intracranial large vessel occlusive disease.28 In both cases, the FDA approval was based on demonstration of safety in case series of patients treated with the devices.2931 No randomized trials have shown the use of these devices improves outcomes for stroke patients. The Guidelines state that Although the MERCI device is a reasonable intervention for extraction of IA thrombi in carefully selected patients, the panel also recognizes that the utility of the device in improving outcomes after stroke is unclear (p. 1684);4 this statement applies similarly to the Penumbra device.
More complex imaging techniques, including multimodal CT (CT, CTA, and CT perfusion) and MR (MRI with diffusion, MRA, and MR perfusion) are being used in some stroke centers to make decisions about acute ischemic stroke treatments.32, 33 The theory is that by using these techniques, one can determine the presence or absence of a mismatch, whereby the perfusion imaging suggests more tissue at risk of infarction than is seen as already abnormal on MR diffusion‐weighted images or compared to a clinical assessment. These mismatch patients are then seen as appropriate candidates for the more aggressive interventions (ie, late IV tPA or IA interventions).34 Unfortunately, the 2 largest randomized trials to look at this issue with respect to >3‐hour IV tPA both failed to show a benefit for patients selected in this manner.35, 36 Standardized definitions of mismatch are still needed, and larger randomized trials are needed before this approach can be suggested for routine care.3739
More complex interventions, available only at tertiary or comprehensive stroke centers, include a bridging approach in which IV tPA (at 2/3 standard dose) is followed by IA tPA, IV tPA with transcranial Doppler (TCD)‐enhanced thrombolysis or IA rescue thrombectomy when vascular imaging after IV tPA shows a persistent large artery occlusion. The Guidelines suggests that these more complex combinations of interventions to restore perfusion cannot be recommended outside the setting of clinical trials (p. 1685).4
No Blood on the CT Scan, Results Back in >8 Hours From Symptom Onset (or if Contraindications to Above Interventions)
This time frame takes the more aggressive interventions off the table. Per the Guidelines, 325 mg of aspirin is the default antiplatelet agent for use, and has been shown in 2 very large randomized trials to reduce early death and longer‐term disability vs. placebo after acute ischemic stroke.40, 41 Importantly, all patients who do not qualify for thrombolysis in the 0‐hour to 8‐hour time window should receive aspirin.
Although a number of small or pilot studies suggest a benefit of the addition of clopidogrel to aspirin for a period (13 months) immediately after ischemic stroke,4244 this more aggressive antiplatelet intervention is not an endorsed standard of care. As described below, the long‐term use of this antiplatelet combination has been consistently associated with a higher risk of hemorrhagic complications. There are no published data regarding the use of aspirin plus dipyridamole in the acute stroke setting. A number of randomized trials have now been performed that have consistently failed to show a benefit of heparin, or heparin‐like medications, for the routine treatment of acute ischemic stroke. Despite this, a number of exceptions exist, based more on tradition and theory than on evidence. These exceptions, for which an IV heparin drip will at times still be considered, include acute ischemic stroke due to dissection of the carotid or vertebral arteries, cardioembolic stroke with fresh clot seen on echocardiogram (ECHO), and a clinically progressive syndrome suggestive of basilar artery occlusion (see below).45, 46 Good evidence exists to specifically recommend the use of full‐dose heparin in the setting of cerebral venous sinus thrombosis.47
Basilar Artery Occlusion Syndromes
Basilar artery occlusion syndromes warrant special mention. These may involve patients who present with quadriparesis, altered mental status, vertigo, diplopia, and other brainstem signs. Conventional treatment of basilar artery occlusion has been associated with 40% mortality with 65% of survivors having severe disability.48 If suspected, an urgent CTA can usually confirm the diagnosis, and urge the clinician to expeditiously consider aggressive intervention. Only case series have been reported regarding basilar artery thrombosis and acute treatments. Based on these studies, it is generally agreed upon that patients who appear comatose or quadriplegic for more than 3 hours will likely have a very poor functional outcome regardless of treatment, and interventional treatment is withheld. If a basilar occlusion patient presents within the 3‐hour time window for IV tPA, they are thus treated, with follow‐up vascular imaging, and possible rescue IA mechanical thrombectomy if recanalization from the IV tPA does not occur. However, if the patient still has preserved neurologic function, or is waxing and waning, there is no clear time limit for IA interventions and they may be useful a day or more after presentation. For basilar occlusion patients with severe stenoses not responsive to lysis, or continuing to be symptomatic, angioplasty and stenting has also been used.46 Despite a lack of evidence, many stroke clinicians will use an IV heparin drip for treatment of acute basilar occlusive disease.
Malignant Middle Cerebral Artery (MCA) Infarction
Malignant MCA infarction is another specific clinical syndrome worthy of special consideration. It is most generally defined as a large infarction (1/2 or 2/3) of the MCA territory, somewhat depressed level of consciousness, and high stroke scale scores (ie, severe deficits) that goes on to severe cerebral edema, mass effect, and often herniation with death.49, 50 Associated patient characteristics include younger age, abnormal (incomplete) ipsilateral collateral circulation, and internal carotid artery occlusion.51 Maximal edema occurs 2 to 5 days from stroke onset and, despite best intensive therapy, has been associated with mortality rates of 70% to 80%.49, 50 A recent pooling of 3 small randomized trials of early decompressive hemicraniectomy and durotomy showed a 50% absolute risk reduction for mortality and a 23% absolute benefit in long‐term independence (modified Rankin scale 3).49 This treatment option should be strongly considered in carefully selected patients., Transfer to an appropriately equipped facility should be offered if not available at your hospital.
Returning to our case patient, upon arrival to the ED with symptoms of partial aphasia, right hemiplegia, and left gaze preference, there was a high suspicion for a left MCA stroke. Unfortunately, he was excluded from receiving IV tPA or any other interventions, as the last time he was known to be neurologically intact was the prior evening, which is taken to be the time of onset. Antiplatelet therapy was continued, and the patient was admitted for further workup.
The initial care of the patient with a cerebrovascular event is often quite complicated. Assimilation of a great deal of data must occur and decisions around therapy must be made in a timely fashion. In prior years there was little to offer in the way of therapy, which also meant there was little initial potential for iatrogenic complication. Both diagnostic and therapeutic options are evolving rapidly. We now have much to offer these patients both emergently and in areas of secondary prevention. In part 2 of this article, the patient's inpatient course and therapy will be reviewed.
- Organization WH. MONICA Manual, Part IV: Event Registration. Available at: http://www.ktl.fi/publications/monica/manual/part4/iv‐2.htm#s2. Accessed May2009.
- ,,, et al.Heart disease and stroke statistics 2008 update. A report from the American Heart Association Statistics Committee and Stroke Statistics Subcommittee.Circulation.200829;117(4):e25–e146.
- .Neurology in the next two decades: report of the Workforce Task Force of the American Academy of Neurology.Neurology.2000;54(4):787–789.
- ,,, et al.Guidelines for the early management of adults with ischemic stroke: a guideline from the American Heart Association/American Stroke Association Stroke Council, Clinical Cardiology Council, Cardiovascular Radiology and Intervention Council, and the Atherosclerotic Peripheral Vascular Disease and Quality of Care Outcomes in Research Interdisciplinary Working Groups: the American Academy of Neurology affirms the value of this guideline as an educational tool for neurologists.Stroke.2007;38(5):1655–1711.
- ,,,.Conditions that mimic stroke in the emergency department. Implications for acute stroke trials.Arch Neurol.1995;52(11):1119–1122.
- ,,,,.Distinguishing between stroke and mimic at the bedside: the brain attack study.Stroke.2006;37(3):769–775.
- ,,, et al.Stroke magnetic resonance imaging is accurate in hyperacute intracerebral hemorrhage: a multicenter study on the validity of stroke imaging.Stroke.2004;35(2):502–506.
- ,,, et al.Comparison of MRI and CT for detection of acute intracerebral hemorrhage.JAMA.2004;292(15):1823–1830.
- ,,, et al.Guidelines for the management of spontaneous intracerebral hemorrhage in adults: 2007 update: a guideline from the American Heart Association/American Stroke Association Stroke Council, High Blood Pressure Research Council, and the Quality of Care and Outcomes in Research Interdisciplinary Working Group.Stroke.2007;38(6):2001–2023.
- ,,.Aneurysmal subarachnoid hemorrhage.N Engl J Med.2006;354(4):387–396.
- ,,,.Subarachnoid haemorrhage.BMJ.2006;333(7561):235–240.
- ,,.Subarachnoid haemorrhage.Lancet.2007;369(9558):306–318.
- ,,.Intracerebral hemorrhage associated with oral anticoagulant therapy: current practices and unresolved questions.Stroke.2006;37(1):256–262.
- ,,, et al.Withdrawal of support in intracerebral hemorrhage may lead to self‐fulfilling prophecies.Neurology.2001;56(6):766–772.
- ,,,.Hospital usage of early do‐not‐resuscitate orders and outcome after intracerebral hemorrhage.Stroke.2004;35(5):1130–1134.
- ,,, et al.Early care limitations independently predict mortality after intracerebral hemorrhage.Neurology.2007;68(20):1651–1657.
- ,,,.Consent for intravenous thrombolysis in acute stroke: review and future directions.Arch Neurol.2007;64(6):785–792.
- .Thrombolysis (tissue plasminogen activator) in stroke: a medicolegal quagmire.Stroke.2006;37(7):1917–1922.
- Tissue plasminogen activator for acute ischemic stroke.The National Institute of Neurological Disorders and Stroke rt‐PA Stroke Study Group.N Engl J Med.1995;333(24):1581–1587.
- ,,, et al.Thrombolysis with alteplase for acute ischaemic stroke in the Safe Implementation of Thrombolysis in Stroke‐Monitoring Study (SITS‐MOST): an observational study.Lancet.2007;369(9558):275–282.
- American College of Emergency Physicians (ACEP). Use of Intravenous tPA for the Management of Acute Stroke in the Emergency Department. ACEP Policy Statement. February 2002. Available at: http://www.acep.org/practres.aspx?id=29834. Accessed May2009.
- American Academy of Emergency Medicine (AAEM). Position statement on the use of intravenous thrombolytic therapy in the treatment of stroke. January 2002. Available at: http://aaem.org/positionstatements/thrombolytictherapy.php. Accessed May2009.
- ,,, et al.Lack of clinical significance of early ischemic changes on computed tomography in acute stroke.JAMA.2001;286(22):2830–2838.
- ,,,,.Thrombolysis for acute stroke in routine clinical practice.Arch Intern Med.2002;162(17):1994–2001.
- ,,, et al.Thrombolysis with alteplase 3 to 4.5 hours after acute ischemic stroke.N Engl J Med.2008;359:1317–1329,1393–1395.
- ,,, et al.Intra‐arterial prourokinase for acute ischemic stroke. The PROACT II study: a randomized controlled trial. Prolyse in Acute Cerebral Thromboembolism.JAMA.1999;282(21):2003–2011.
- Modified MERCI Retriever FDA marketing approval letter. Available at: www.fda.gov/cdrh/pdf6/K062046.pdf. Accessed May2009.
- Penumbra System FDA marketing approval letter. Available at: www.fda.gov/cdrh/pdf7/K072718.pdf. Accessed May2009.
- .Safety of mechanical thrombectomy and intravenous tissue plasminogen activator in acute ischemic stroke. Results of the multi mechanical embolus removal in cerebral ischemia (MERCI) trial, part I.AJNR Am J Neuroradiol.2006;27(6):1177–1182.
- ,,, et al.Safety and efficacy of mechanical embolectomy in acute ischemic stroke: results of the MERCI trial.Stroke.2005;36(7):1432–1438.
- ,,, et al.The Penumbra System: a mechanical device for the treatment of acute stroke due to thromboembolism.AJNR Am J Neuroradiol.2008;29(7):1409–1413.
- ,,, et al.Comparison of CT perfusion and angiography and MRI in selecting stroke patients for acute treatment.Neurology.2007;68(9):694–697.
- ,,, et al.Combined intravenous and intraarterial revascularization therapy using MRI perfusion/diffusion mismatch selection for acute ischemic stroke at 3–6 h after symptom onset.Neurocrit Care.2008;8(3):353–359.
- ,,, et al.Refining the perfusion‐diffusion mismatch hypothesis.Stroke.2005;36(6):1153–1159.
- . DIAS‐2: no benefit of desmoteplase in acute ischemic stroke. Available at: www.medscape.com/viewarticle/557663. Accessed May2009.
- ,,, et al.Effects of alteplase beyond 3 h after stroke in the Echoplanar Imaging Thrombolytic Evaluation Trial (EPITHET): a placebo‐controlled randomised trial.Lancet Neurol.2008;7(4):299–309.
- ,,.Magnetic resonance perfusion diffusion mismatch and thrombolysis in acute ischaemic stroke: a systematic review of the evidence to date.J Neurol Neurosurg Psychiatry.2007;78(5):485–491.
- ,,, et al.Optimal definition for PWI/DWI mismatch in acute ischemic stroke patients.J Cereb Blood Flow Metab.2008;28(5):887–891.
- ,,, et al.Rapid assessment of perfusion‐diffusion mismatch.Stroke.2008;39(1):75–81.
- CAST: randomised placebo‐controlled trial of early aspirin use in 20,000 patients with acute ischaemic stroke.CAST (Chinese Acute Stroke Trial) Collaborative Group.Lancet.1997;349(9066):1641–1649.
- The International Stroke Trial (IST): a randomised trial of aspirin, subcutaneous heparin, both, or neither among 19435 patients with acute ischaemic stroke.International Stroke Trial Collaborative Group.Lancet.1997;349(9065):1569–1581.
- ,,, et al.Dual antiplatelet therapy with clopidogrel and aspirin in symptomatic carotid stenosis evaluated using doppler embolic signal detection: the clopidogrel and aspirin for reduction of emboli in symptomatic carotid stenosis (CARESS) trial.Circulation.2005;111(17):2233–2240.
- ,,, et al.Effect of urgent treatment of transient ischaemic attack and minor stroke on early recurrent stroke (EXPRESS study): a prospective population‐based sequential comparison.Lancet.2007;370(9596):1432–1442.
- ,,,,,.Fast assessment of stroke and transient ischaemic attack to prevent early recurrence (FASTER): a randomised controlled pilot trial.Lancet Neurol.2007;6(11):961–969.
- ,,, et al.Antiplatelets versus anticoagulation in cervical artery dissection.Stroke.2007;38(9):2605–2611.
- ,,.Basilar artery occlusion.Neurocrit Care.2004;1(3):319–329.
- ,.Cerebral venous thrombosis: an update.Lancet Neurol.2007;6(2):162–170.
- ,,,,.Outcome in patients with basilar artery occlusion treated conventionally.J Neurol Neurosurg Psychiatry.2005;76(9):1238–1241.
- ,,, et al.Early decompressive surgery in malignant infarction of the middle cerebral artery: a pooled analysis of three randomised controlled trials.Lancet Neurol.2007;6(3):215–222.
- ,,,,,.‘Malignant’ middle cerebral artery territory infarction: clinical course and prognostic signs.Arch Neurol.1996;53(4):309–315.
- ,,,,.Predictors for malignant middle cerebral artery infarctions: a postmortem analysis.Neurology. 282006;66(6):815–820.
- ,,,,,.Poor outcomes in patients who do not receive intravenous tissue plasminogen activator because of mild or improving ischemic stroke.Stroke.2005;36(11):2497–2499.
The term stroke is defined by the World Health Organization as rapidly developed clinical signs of focal (or global) disturbance of cerebral function lasting more than 24 hours (unless interrupted by surgery or death), with no apparent cause other than a vascular origin; it includes patients presenting clinical signs and symptoms suggestive of subarachnoid hemorrhage (SAH), intracerebral hemorrhage, or cerebral ischemic necrosis.1 Stroke is 1 of the leading causes of death and the number 1 cause of long‐term disability in the United States, with over 700,000 strokes and over 150,000 stroke deaths each year.2
Given the projections of 30,000 hospitalists nationally by 2010 (
Case Presentation
A 76‐year‐old right‐handed male with a history of hyperlipidemia and myocardial infarction was found at 7 AM with right‐sided paralysis and poor responsiveness on the morning of admission. He seemed to prefer looking to the left and to understand what was being said to him, but had great difficulty speaking. When he went to bed at 9 PM, he was at his neurological baseline. Upon finding him that morning, his wife called 911.
With increased knowledge regarding the pathophysiology of stroke, it has become clear that timeliness is of utmost importance (time is brain) and that acute stroke should be regarded as an acute medical/neurological emergency.
This article reviews the approach in evaluating an acute stroke patient, management strategies, and treatment options. Where not otherwise referenced, data to support our comments come from the recently updated and exhaustive American Heart Association (AHA)/American Stroke Association (ASA) Guidelines for the Early Management of Adults With Ischemic Stroke and will be referred to herein as the Guidelines.4 Harborview Medical Center in Seattle is a Joint Commissioncertified Primary Stroke Center and the home hospital of 2 of the authors (C.L.E., D.L.T.); it is referred to herein as Harborview.
Emergency Room Care (see Acute Stroke Algorithm, Figure 1)
The First 15 Minutes
After assuring stable airway, breathing, and circulation, immediate (STAT) blood draws should be performed, including full complete blood count (CBC) with platelets, international normalized ratio/prothrombin time/partial thromboplastin time (INR/PT/PTT), full electrolytes, and glucose (finger‐stick blood glucose also recommended). Glasgow Coma Scale (GCS) score and NIH Stroke Scale (NIHSS) score should be established via a focused history and physical exam. The GCS is most appropriate for patients with a significantly depressed level of consciousness, while the NIHSS can be scored for any stroke patient (1‐page version of NIHSS used at Harborview is shown in Figure 2). By quantifying stroke severity, the NIHSS score helps both to facilitate communication about neurologic deficit as well as serve as a documented baseline in case of subsequent clinical change. Emergency department (ED) physicians, hospitalists, neurologists, and nursing staff regularly caring for acute stroke patients would be well‐served by obtaining certification in the NIHSS (available free online at
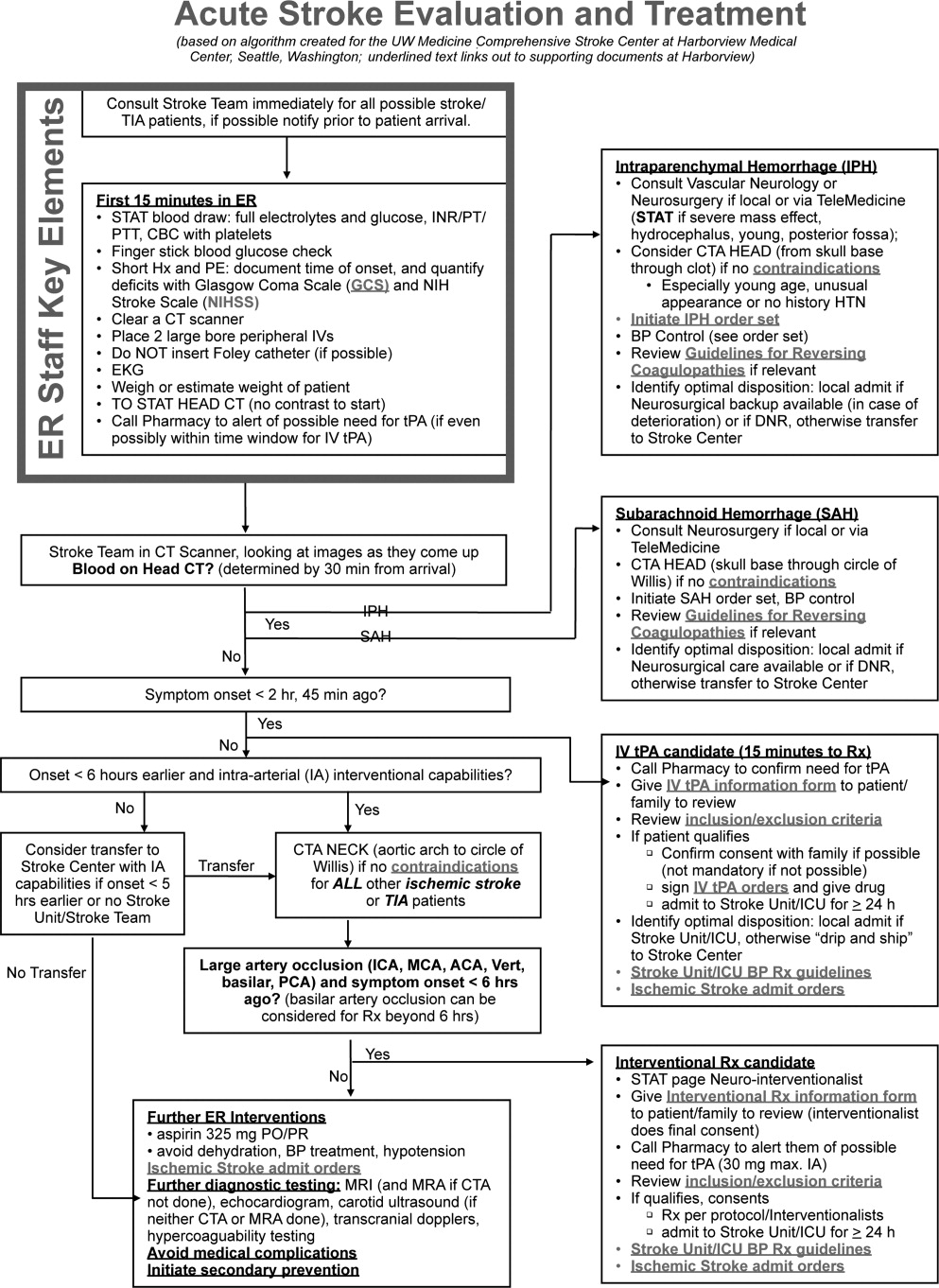
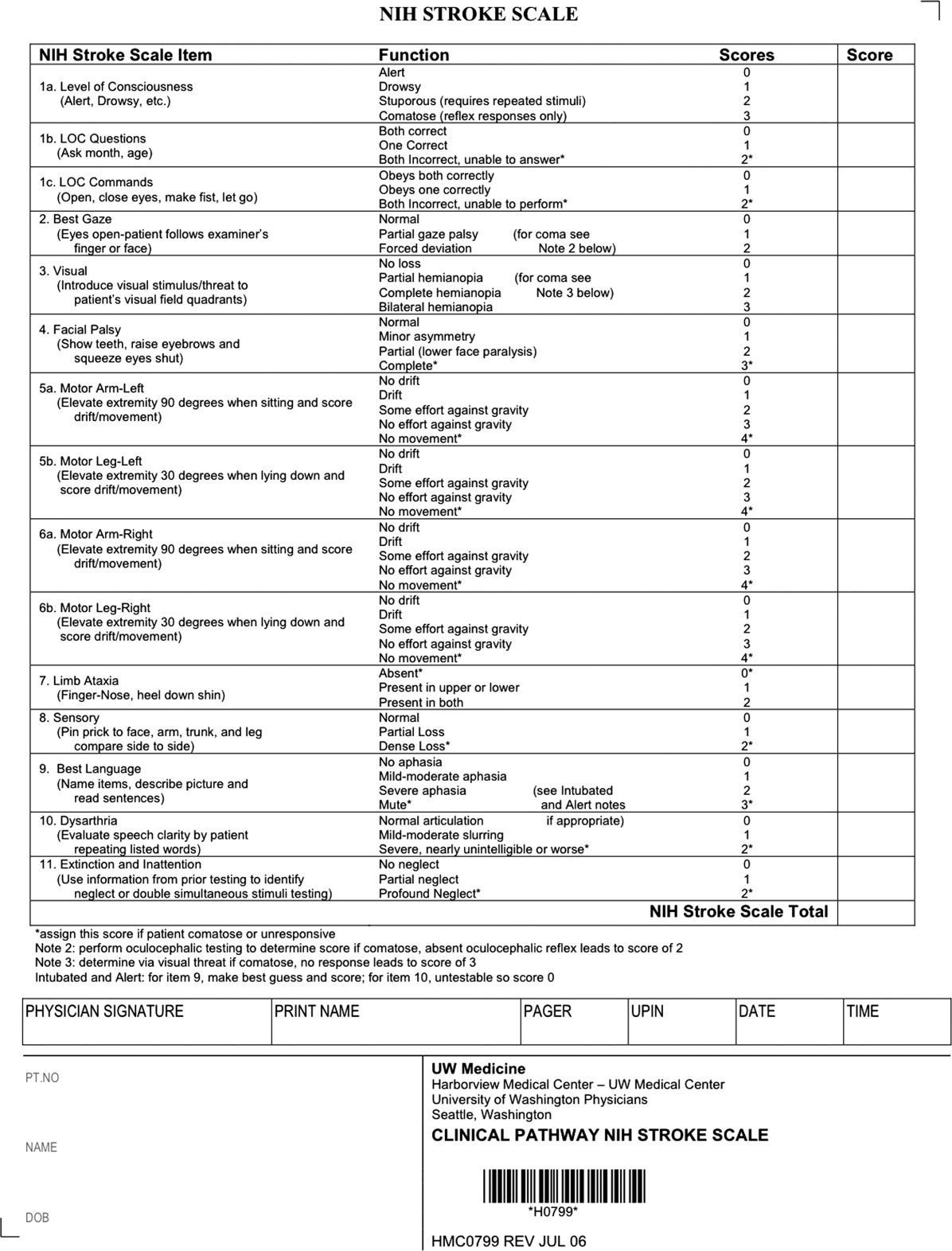
Our case patient's initial NIHSS score was 15, with points given for drowsiness, inability to answer questions, partial facial palsy, no movement in right arm or leg, mild‐moderate aphasia, and mild‐moderate dysarthria (Figure 2).
Differential Diagnosis
Many acute conditions can mimic stroke, and 1 of the goals of the initial emergency room (ER) evaluation is to rule out such stroke mimics. A report of 411 initial ER stroke diagnoses identified 19% as stroke mimics; the most common mimic diagnoses were seizure, systemic infection, brain tumor, and toxic‐metabolic.5 The same study identified decreased level of alertness as associated with a final mimic diagnosis and history of angina as associated with a final diagnosis of stroke. Another study looked at 350 presentations with an initial stroke diagnosis and found 31% stroke mimics; similarly, the main alternative diagnoses were seizure, sepsis, toxic‐metabolic, space‐occupying lesion, and syncope/presyncope.6 Findings associated with a mimic diagnosis included no cognitive impairment and abnormal findings in any other system, while findings associated with a stroke diagnosis were a definite history of focal neurological symptoms, NIHSS score, stroke type classification possible, an exact onset that could be determined, and abnormal vascular findings on imaging.6
Initial Imaging
The patient should receive a STAT noncontrast head CT to evaluate for the presence or absence of blood. At this time, magnetic resonance imaging (MRI) is not essential to confirm the diagnosis of ischemic stroke, as diagnosis is based on clinical suspicion. MRI is more sensitive at imaging acute ischemia (on diffusion‐weighted sequences) and recently has been shown to be equally sensitive in identifying acute blood (previously thought to be a relative advantage of CT).7, 8 Practical and pervasive barriers to emergent MRI include study duration, significant patient cooperation, and that few hospitals are currently set up to perform such rapid MRIS. The Guidelines specifically state that In most instances, CT will provide the information to make decisions about emergency management (p. 1668),4 that vascular imaging should not delay treatment of patients whose symptoms started 3 hours ago and who have acute ischemic stroke, and that emergency treatment of stroke should not be delayed in order to obtain multimodal imaging studies (p. 1669).4
Our case patient's initial imaging, a noncontrast head CT (Supporting Figures 1 and 2), showed subtle clues consistent with the diagnosis of acute ischemic stroke. These include a hyperdense middle cerebral artery (MCA) sign (presumably representing thrombus), possible obscuration of the basal ganglia, and, importantly, no acute intraparenchymal (IPH), SAH, or subdural hemorrhage.
Acute Treatments
After the patient's head CT is completed, the next steps are dependent upon what was seen on the scan and the time from symptom onset.
Blood on the CT Scan
If the initial brain imaging reveals IPH or SAH, further diagnostic testing and early treatments are quite different than for ischemic stroke. New guidelines are available for IPH management,9 and there have been recent review articles of care for SAH.1012 At the authors' institutions, early care of such patients always involves aggressive reversal of any antithrombotic medications the patient was taking prior to presentation. Our approach to warfarin reversal includes vitamin K and fresh frozen plasma (FFP) to achieve an INR 1.4; others have used prothrombin complex concentrate (PCC).13 Blood pressure (BP) treatment goals are generally more aggressive than for ischemic stroke, while supportive care to avoid aspiration, hyperglycemia, fever, and venous thrombosis (here initially with sequential compression devices alone) are similar. Early estimation of prognosis for these patients with IPH and SAH and discussions with families about continued aggressive care are of utmost importance, and should involve providers with sufficient expertise. Care should be taken to avoid overly pessimistic early prognostication, as early do not resuscitate (DNR) decisions in intercranial hemorrhage (ICH) can become a self‐fulfilling prophecy.1416 If the decision is to continue aggressive and supportive care, or if an appropriately expert consultation is not available at the presentation hospital, IPH and SAH patients should be considered for transfer to a hospital with the appropriate resources (including emergency access to neurosurgeons) or be evaluated by such an expert by telemedicine if available.
No Blood on the CT Scan, Results Back in 3 Hours From Symptom Onset
If such a patient is not rapidly resolving their symptoms, and the diagnosis continues to remain clear, inclusion/exclusion criteria for IV tPA should be reviewed (Table 1). Consent should be obtained much like any other procedure with significant risk. As many consider tPA to be standard of care, it is reasonable to proceed in cases of unobtainable consent as one would with any other emergent therapy. This situation is a topic of ongoing debate.17, 18 The Guidelines state that although written consent is not necessary before administration of recombinant tPA (rtPA) for treatment of stroke, a full discussion of the potential risks and benefits of treatment with rtPA with the family and the patient if possible is recommended (p. 1676).4 After tPA is given in the ER, the patient should be admitted to an intensive care unit (ICU) setting for 24 hours for careful monitoring of BP, avoidance of invasive procedures, and no use of antithrombotic medications during that period of time.
| Comments (from the authors) | |
|---|---|
| |
| Inclusion criteria | |
| Diagnosis of ischemic stroke causing measurable neurological deficit | Usually NIHSS > 4 |
| Neurological signs should not be clearing spontaneously | Such a patient may do well without tPA, but there is debate82 |
| Neurological signs should not be minor and isolated. | |
| Onset of symptoms >3 hours before beginning treatment | |
| Patient or family members understand the potential risks and benefits from treatment | Debated, as tPA considered standard of care by many |
| Cautionary criteria | |
| Caution should be exercised in treating a patient with major deficits | Higher risk of hemorrhage, but still may benefit from treatment |
| Exclusion criteria | |
| Symptoms of stroke should not be suggestive of subarachnoid hemorrhage | |
| No head trauma or prior stroke in previous 3 months | |
| No myocardial infarction in the previous 3 months | |
| No gastrointestinal or urinary tract hemorrhage in previous 21 days | |
| No major surgery in the previous 14 days | |
| No arterial puncture at a noncompressible site in the previous 7 days | |
| No history of previous intracranial hemorrhage | |
| Blood pressure not elevated (systolic >185 mm Hg or diastolic 110 mm Hg) | Okay to bring down with labetolol, nitropaste, or nicardipine* |
| No evidence of active bleeding or acute trauma (fracture) on examination | |
| Not taking an oral anticoagulant or, if anticoagulant being taken, INR 1.7 | |
| If receiving heparin in previous 48 hours, aPTT must be in normal range | |
| Platelet count 100,000 mm3 | |
| Blood glucose concentration 50 mg/dL (2.7 mmol/L) | |
| Seizure with postictal residual neurological impairments | Not absolute if treating physician feels stroke also present, or if confirmed by imaging |
| CT does not show a multilobar infarction (hypodensity >1/3 cerebral hemisphere) | Not strictly evidence based, in NINDS trial this finding did not preclude benefit of tPA |
Based mainly on the results of the National Institute of Neurological Disorders and Stroke (NINDS) tPA trial,19 and recently supported by a large Phase IV observational study from the European Union,20 IV tPA for acute ischemic stroke is approved for use in many countries and is endorsed for the treatment of carefully selected ischemic stroke patients in a number of practice guidelines.4 Despite this, the emergency medicine community has been less enthusiastic about the use of IV tPA.21, 22 Although the risk of hemorrhagic complications is greater in certain subgroups of patients (ie, the most severe strokes, significant early CT changes, older age), there is no definitive evidence to suggest that these groups do not still benefit from the treatment.23 It is also clear that if patients are not carefully selected, meeting strict inclusion and exclusion criteria, the rate of complications is increased.24 Thus, as summarized in a practice statement of the American College of Emergency Physicians, There is insufficient evidence at this time to endorse the use of intravenous tPA in clinical practice when systems are not in place to ensure that the inclusion/exclusion criteria established by the NINDS guidelines for tPA use in acute stroke are followed.21 When counseling patients and their families about the benefits and risks of IV tPA, one should keep in mind that the NINDS trial demonstrated increased odds of excellent outcomes despite a significant 10‐fold increase in the risk of symptomatic intracranial hemorrhage (6.4% vs. 0.6%), and did not alter 30‐day mortality. The largest Phase IV cohort study of IV tPA treatment, Safe Implementation of Thrombolysis in Stroke Monitoring Study (SITS‐MOST) was mandated by the European Union upon approval of the medication for use in acute ischemic stroke.20 The results in 6483 patients showed that tPA, when used in strict accordance with published inclusion and exclusion criteria, could perform as well as it did in randomized trials.
The recently published European Cooperative Acute Stroke Study3 (ECASS‐3) trial demonstrated that IV tPA has efficacy with adequate safety up to 4.5 hours after the onset of symptoms. A total of 821 patients were enrolled and 375 received tPA. Exclusion criteria included diabetes being treated with medication with a history of prior stroke, an NIHSS score >25, or treatment with warfarin. The rates of hemorrhage (27.0% vs. 17.6%, P = 0.001) were in line with those of the SITS‐MOST study patients who were treated within the 3‐hour time window. There was no significant difference in mortality (7.7% tPA vs. 8.4% placebo). This study is relatively new; therefore, the data have not been reviewed by guideline committees.25
No Blood on the CT Scan, Results Back in >3 Hours, but 8 Hours, From Symptom Onset
Unfortunately as with our patient, most people do not present to an ER in a timely fashion. Nonetheless, there may be other treatments and interventions possible. If the patient arrives 8 hours from onset of symptoms, intraarterial (IA) interventions are a possibility. In such a case, a CT angiogram (CTA) of the neck from the arch of the aorta to the circle of Willis is recommended (barring any contraindications such as renal failure or iodine allergy). The rationale behind this study is that other treatment options, such as IA tPA or mechanical thrombectomy may be considered if a large arterial occlusion is identified. CTA is preferred over magnetic resonance angiography (MRA) due to the same time and patient cooperation issues mentioned above, though some expert centers may be set up to perform MRI and MRA rapidly in the acute setting. CTA or MRA is of great value early on in the emergent assessment of ischemic stroke patients, as it allows detailed evaluation of the cerebral vasculature; this knowledge helps define the pathophysiology of the ongoing stroke (eg, is there a larger artery occlusion?) and can help inform the approach to subsequent therapies.
The Guidelines (p. 1678)4 recommend IA thrombolysis as a treatment option if it can be started within 6 hours, based on results from the Prolyse in Acute Cerebral Thromboembolism (PROACT) II trial. This study involved angiography with identification of the occluded vessel (the proximal MCA‐M1 in this study) and administration of recombinant pro‐urokinase to the clot with functional outcome as the primary endpoint.26 At 3 months, patients who received the IA thrombolytic had a 40% chance of slight disability; unable to carry out all previous activities, but able to look after own affairs without assistance or better (ie, a modified Rankin Scale score of 2) vs. 25% of those not receiving the IA thrombolytic. Pro‐urokinase is not available in the United States; therefore, many institutions substitute IA tPA. The Guidelines further state that IA thrombolysis can be considered for use in some patients with contraindications to IV tPA (eg, recent surgery), but should not be used instead of IV tPA in patients otherwise eligible (p. 1678).4
There are now two U.S. Food and Drug Administration (FDA)‐approved devices for mechanical cerebral vasculature thrombectomy for use up to 8 hours from symptom onset. The mechanical embolus removal in cerebral ischemia (MERCI) clot retrieval device was originally approved by the FDA in August 2004 for restoring blood flow in the neurovasculature by removing thrombus in patients experiencing ischemic stroke. Modified devices have been approved as recently as January 2007.27 The Penumbra System was FDA‐approved in December 2007 for revascularization of patients with acute ischemic stroke secondary to intracranial large vessel occlusive disease.28 In both cases, the FDA approval was based on demonstration of safety in case series of patients treated with the devices.2931 No randomized trials have shown the use of these devices improves outcomes for stroke patients. The Guidelines state that Although the MERCI device is a reasonable intervention for extraction of IA thrombi in carefully selected patients, the panel also recognizes that the utility of the device in improving outcomes after stroke is unclear (p. 1684);4 this statement applies similarly to the Penumbra device.
More complex imaging techniques, including multimodal CT (CT, CTA, and CT perfusion) and MR (MRI with diffusion, MRA, and MR perfusion) are being used in some stroke centers to make decisions about acute ischemic stroke treatments.32, 33 The theory is that by using these techniques, one can determine the presence or absence of a mismatch, whereby the perfusion imaging suggests more tissue at risk of infarction than is seen as already abnormal on MR diffusion‐weighted images or compared to a clinical assessment. These mismatch patients are then seen as appropriate candidates for the more aggressive interventions (ie, late IV tPA or IA interventions).34 Unfortunately, the 2 largest randomized trials to look at this issue with respect to >3‐hour IV tPA both failed to show a benefit for patients selected in this manner.35, 36 Standardized definitions of mismatch are still needed, and larger randomized trials are needed before this approach can be suggested for routine care.3739
More complex interventions, available only at tertiary or comprehensive stroke centers, include a bridging approach in which IV tPA (at 2/3 standard dose) is followed by IA tPA, IV tPA with transcranial Doppler (TCD)‐enhanced thrombolysis or IA rescue thrombectomy when vascular imaging after IV tPA shows a persistent large artery occlusion. The Guidelines suggests that these more complex combinations of interventions to restore perfusion cannot be recommended outside the setting of clinical trials (p. 1685).4
No Blood on the CT Scan, Results Back in >8 Hours From Symptom Onset (or if Contraindications to Above Interventions)
This time frame takes the more aggressive interventions off the table. Per the Guidelines, 325 mg of aspirin is the default antiplatelet agent for use, and has been shown in 2 very large randomized trials to reduce early death and longer‐term disability vs. placebo after acute ischemic stroke.40, 41 Importantly, all patients who do not qualify for thrombolysis in the 0‐hour to 8‐hour time window should receive aspirin.
Although a number of small or pilot studies suggest a benefit of the addition of clopidogrel to aspirin for a period (13 months) immediately after ischemic stroke,4244 this more aggressive antiplatelet intervention is not an endorsed standard of care. As described below, the long‐term use of this antiplatelet combination has been consistently associated with a higher risk of hemorrhagic complications. There are no published data regarding the use of aspirin plus dipyridamole in the acute stroke setting. A number of randomized trials have now been performed that have consistently failed to show a benefit of heparin, or heparin‐like medications, for the routine treatment of acute ischemic stroke. Despite this, a number of exceptions exist, based more on tradition and theory than on evidence. These exceptions, for which an IV heparin drip will at times still be considered, include acute ischemic stroke due to dissection of the carotid or vertebral arteries, cardioembolic stroke with fresh clot seen on echocardiogram (ECHO), and a clinically progressive syndrome suggestive of basilar artery occlusion (see below).45, 46 Good evidence exists to specifically recommend the use of full‐dose heparin in the setting of cerebral venous sinus thrombosis.47
Basilar Artery Occlusion Syndromes
Basilar artery occlusion syndromes warrant special mention. These may involve patients who present with quadriparesis, altered mental status, vertigo, diplopia, and other brainstem signs. Conventional treatment of basilar artery occlusion has been associated with 40% mortality with 65% of survivors having severe disability.48 If suspected, an urgent CTA can usually confirm the diagnosis, and urge the clinician to expeditiously consider aggressive intervention. Only case series have been reported regarding basilar artery thrombosis and acute treatments. Based on these studies, it is generally agreed upon that patients who appear comatose or quadriplegic for more than 3 hours will likely have a very poor functional outcome regardless of treatment, and interventional treatment is withheld. If a basilar occlusion patient presents within the 3‐hour time window for IV tPA, they are thus treated, with follow‐up vascular imaging, and possible rescue IA mechanical thrombectomy if recanalization from the IV tPA does not occur. However, if the patient still has preserved neurologic function, or is waxing and waning, there is no clear time limit for IA interventions and they may be useful a day or more after presentation. For basilar occlusion patients with severe stenoses not responsive to lysis, or continuing to be symptomatic, angioplasty and stenting has also been used.46 Despite a lack of evidence, many stroke clinicians will use an IV heparin drip for treatment of acute basilar occlusive disease.
Malignant Middle Cerebral Artery (MCA) Infarction
Malignant MCA infarction is another specific clinical syndrome worthy of special consideration. It is most generally defined as a large infarction (1/2 or 2/3) of the MCA territory, somewhat depressed level of consciousness, and high stroke scale scores (ie, severe deficits) that goes on to severe cerebral edema, mass effect, and often herniation with death.49, 50 Associated patient characteristics include younger age, abnormal (incomplete) ipsilateral collateral circulation, and internal carotid artery occlusion.51 Maximal edema occurs 2 to 5 days from stroke onset and, despite best intensive therapy, has been associated with mortality rates of 70% to 80%.49, 50 A recent pooling of 3 small randomized trials of early decompressive hemicraniectomy and durotomy showed a 50% absolute risk reduction for mortality and a 23% absolute benefit in long‐term independence (modified Rankin scale 3).49 This treatment option should be strongly considered in carefully selected patients., Transfer to an appropriately equipped facility should be offered if not available at your hospital.
Returning to our case patient, upon arrival to the ED with symptoms of partial aphasia, right hemiplegia, and left gaze preference, there was a high suspicion for a left MCA stroke. Unfortunately, he was excluded from receiving IV tPA or any other interventions, as the last time he was known to be neurologically intact was the prior evening, which is taken to be the time of onset. Antiplatelet therapy was continued, and the patient was admitted for further workup.
The initial care of the patient with a cerebrovascular event is often quite complicated. Assimilation of a great deal of data must occur and decisions around therapy must be made in a timely fashion. In prior years there was little to offer in the way of therapy, which also meant there was little initial potential for iatrogenic complication. Both diagnostic and therapeutic options are evolving rapidly. We now have much to offer these patients both emergently and in areas of secondary prevention. In part 2 of this article, the patient's inpatient course and therapy will be reviewed.
The term stroke is defined by the World Health Organization as rapidly developed clinical signs of focal (or global) disturbance of cerebral function lasting more than 24 hours (unless interrupted by surgery or death), with no apparent cause other than a vascular origin; it includes patients presenting clinical signs and symptoms suggestive of subarachnoid hemorrhage (SAH), intracerebral hemorrhage, or cerebral ischemic necrosis.1 Stroke is 1 of the leading causes of death and the number 1 cause of long‐term disability in the United States, with over 700,000 strokes and over 150,000 stroke deaths each year.2
Given the projections of 30,000 hospitalists nationally by 2010 (
Case Presentation
A 76‐year‐old right‐handed male with a history of hyperlipidemia and myocardial infarction was found at 7 AM with right‐sided paralysis and poor responsiveness on the morning of admission. He seemed to prefer looking to the left and to understand what was being said to him, but had great difficulty speaking. When he went to bed at 9 PM, he was at his neurological baseline. Upon finding him that morning, his wife called 911.
With increased knowledge regarding the pathophysiology of stroke, it has become clear that timeliness is of utmost importance (time is brain) and that acute stroke should be regarded as an acute medical/neurological emergency.
This article reviews the approach in evaluating an acute stroke patient, management strategies, and treatment options. Where not otherwise referenced, data to support our comments come from the recently updated and exhaustive American Heart Association (AHA)/American Stroke Association (ASA) Guidelines for the Early Management of Adults With Ischemic Stroke and will be referred to herein as the Guidelines.4 Harborview Medical Center in Seattle is a Joint Commissioncertified Primary Stroke Center and the home hospital of 2 of the authors (C.L.E., D.L.T.); it is referred to herein as Harborview.
Emergency Room Care (see Acute Stroke Algorithm, Figure 1)
The First 15 Minutes
After assuring stable airway, breathing, and circulation, immediate (STAT) blood draws should be performed, including full complete blood count (CBC) with platelets, international normalized ratio/prothrombin time/partial thromboplastin time (INR/PT/PTT), full electrolytes, and glucose (finger‐stick blood glucose also recommended). Glasgow Coma Scale (GCS) score and NIH Stroke Scale (NIHSS) score should be established via a focused history and physical exam. The GCS is most appropriate for patients with a significantly depressed level of consciousness, while the NIHSS can be scored for any stroke patient (1‐page version of NIHSS used at Harborview is shown in Figure 2). By quantifying stroke severity, the NIHSS score helps both to facilitate communication about neurologic deficit as well as serve as a documented baseline in case of subsequent clinical change. Emergency department (ED) physicians, hospitalists, neurologists, and nursing staff regularly caring for acute stroke patients would be well‐served by obtaining certification in the NIHSS (available free online at
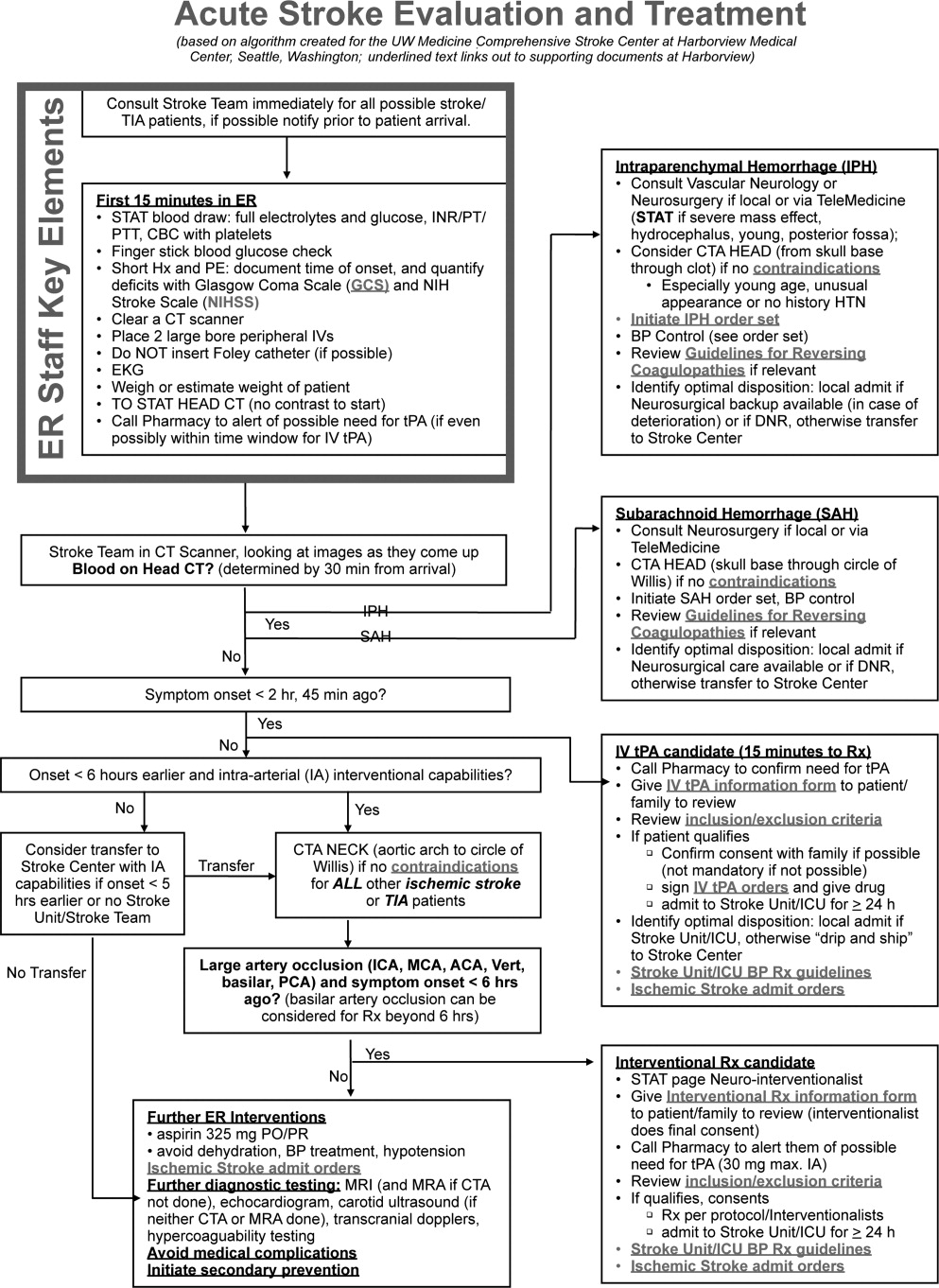
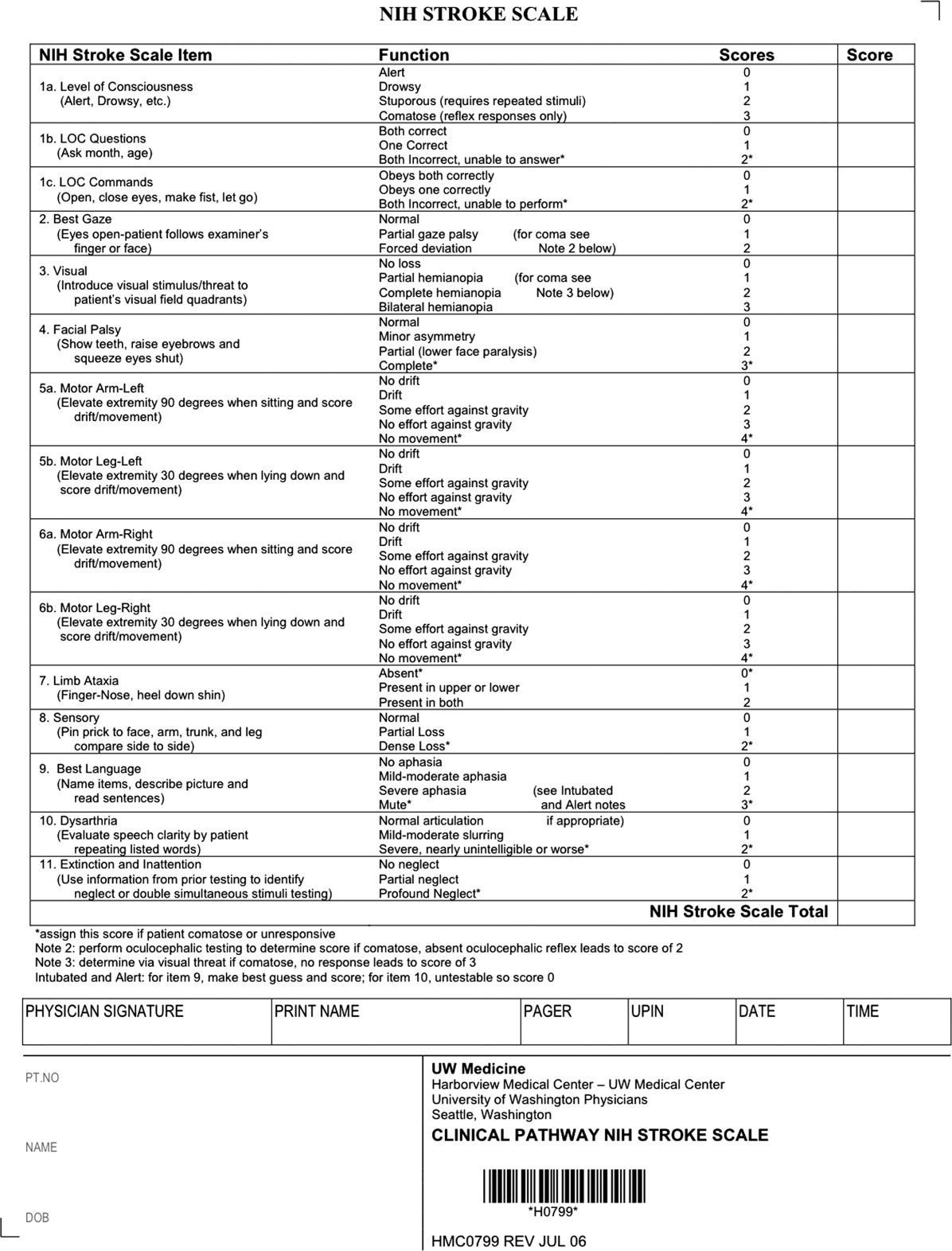
Our case patient's initial NIHSS score was 15, with points given for drowsiness, inability to answer questions, partial facial palsy, no movement in right arm or leg, mild‐moderate aphasia, and mild‐moderate dysarthria (Figure 2).
Differential Diagnosis
Many acute conditions can mimic stroke, and 1 of the goals of the initial emergency room (ER) evaluation is to rule out such stroke mimics. A report of 411 initial ER stroke diagnoses identified 19% as stroke mimics; the most common mimic diagnoses were seizure, systemic infection, brain tumor, and toxic‐metabolic.5 The same study identified decreased level of alertness as associated with a final mimic diagnosis and history of angina as associated with a final diagnosis of stroke. Another study looked at 350 presentations with an initial stroke diagnosis and found 31% stroke mimics; similarly, the main alternative diagnoses were seizure, sepsis, toxic‐metabolic, space‐occupying lesion, and syncope/presyncope.6 Findings associated with a mimic diagnosis included no cognitive impairment and abnormal findings in any other system, while findings associated with a stroke diagnosis were a definite history of focal neurological symptoms, NIHSS score, stroke type classification possible, an exact onset that could be determined, and abnormal vascular findings on imaging.6
Initial Imaging
The patient should receive a STAT noncontrast head CT to evaluate for the presence or absence of blood. At this time, magnetic resonance imaging (MRI) is not essential to confirm the diagnosis of ischemic stroke, as diagnosis is based on clinical suspicion. MRI is more sensitive at imaging acute ischemia (on diffusion‐weighted sequences) and recently has been shown to be equally sensitive in identifying acute blood (previously thought to be a relative advantage of CT).7, 8 Practical and pervasive barriers to emergent MRI include study duration, significant patient cooperation, and that few hospitals are currently set up to perform such rapid MRIS. The Guidelines specifically state that In most instances, CT will provide the information to make decisions about emergency management (p. 1668),4 that vascular imaging should not delay treatment of patients whose symptoms started 3 hours ago and who have acute ischemic stroke, and that emergency treatment of stroke should not be delayed in order to obtain multimodal imaging studies (p. 1669).4
Our case patient's initial imaging, a noncontrast head CT (Supporting Figures 1 and 2), showed subtle clues consistent with the diagnosis of acute ischemic stroke. These include a hyperdense middle cerebral artery (MCA) sign (presumably representing thrombus), possible obscuration of the basal ganglia, and, importantly, no acute intraparenchymal (IPH), SAH, or subdural hemorrhage.
Acute Treatments
After the patient's head CT is completed, the next steps are dependent upon what was seen on the scan and the time from symptom onset.
Blood on the CT Scan
If the initial brain imaging reveals IPH or SAH, further diagnostic testing and early treatments are quite different than for ischemic stroke. New guidelines are available for IPH management,9 and there have been recent review articles of care for SAH.1012 At the authors' institutions, early care of such patients always involves aggressive reversal of any antithrombotic medications the patient was taking prior to presentation. Our approach to warfarin reversal includes vitamin K and fresh frozen plasma (FFP) to achieve an INR 1.4; others have used prothrombin complex concentrate (PCC).13 Blood pressure (BP) treatment goals are generally more aggressive than for ischemic stroke, while supportive care to avoid aspiration, hyperglycemia, fever, and venous thrombosis (here initially with sequential compression devices alone) are similar. Early estimation of prognosis for these patients with IPH and SAH and discussions with families about continued aggressive care are of utmost importance, and should involve providers with sufficient expertise. Care should be taken to avoid overly pessimistic early prognostication, as early do not resuscitate (DNR) decisions in intercranial hemorrhage (ICH) can become a self‐fulfilling prophecy.1416 If the decision is to continue aggressive and supportive care, or if an appropriately expert consultation is not available at the presentation hospital, IPH and SAH patients should be considered for transfer to a hospital with the appropriate resources (including emergency access to neurosurgeons) or be evaluated by such an expert by telemedicine if available.
No Blood on the CT Scan, Results Back in 3 Hours From Symptom Onset
If such a patient is not rapidly resolving their symptoms, and the diagnosis continues to remain clear, inclusion/exclusion criteria for IV tPA should be reviewed (Table 1). Consent should be obtained much like any other procedure with significant risk. As many consider tPA to be standard of care, it is reasonable to proceed in cases of unobtainable consent as one would with any other emergent therapy. This situation is a topic of ongoing debate.17, 18 The Guidelines state that although written consent is not necessary before administration of recombinant tPA (rtPA) for treatment of stroke, a full discussion of the potential risks and benefits of treatment with rtPA with the family and the patient if possible is recommended (p. 1676).4 After tPA is given in the ER, the patient should be admitted to an intensive care unit (ICU) setting for 24 hours for careful monitoring of BP, avoidance of invasive procedures, and no use of antithrombotic medications during that period of time.
| Comments (from the authors) | |
|---|---|
| |
| Inclusion criteria | |
| Diagnosis of ischemic stroke causing measurable neurological deficit | Usually NIHSS > 4 |
| Neurological signs should not be clearing spontaneously | Such a patient may do well without tPA, but there is debate82 |
| Neurological signs should not be minor and isolated. | |
| Onset of symptoms >3 hours before beginning treatment | |
| Patient or family members understand the potential risks and benefits from treatment | Debated, as tPA considered standard of care by many |
| Cautionary criteria | |
| Caution should be exercised in treating a patient with major deficits | Higher risk of hemorrhage, but still may benefit from treatment |
| Exclusion criteria | |
| Symptoms of stroke should not be suggestive of subarachnoid hemorrhage | |
| No head trauma or prior stroke in previous 3 months | |
| No myocardial infarction in the previous 3 months | |
| No gastrointestinal or urinary tract hemorrhage in previous 21 days | |
| No major surgery in the previous 14 days | |
| No arterial puncture at a noncompressible site in the previous 7 days | |
| No history of previous intracranial hemorrhage | |
| Blood pressure not elevated (systolic >185 mm Hg or diastolic 110 mm Hg) | Okay to bring down with labetolol, nitropaste, or nicardipine* |
| No evidence of active bleeding or acute trauma (fracture) on examination | |
| Not taking an oral anticoagulant or, if anticoagulant being taken, INR 1.7 | |
| If receiving heparin in previous 48 hours, aPTT must be in normal range | |
| Platelet count 100,000 mm3 | |
| Blood glucose concentration 50 mg/dL (2.7 mmol/L) | |
| Seizure with postictal residual neurological impairments | Not absolute if treating physician feels stroke also present, or if confirmed by imaging |
| CT does not show a multilobar infarction (hypodensity >1/3 cerebral hemisphere) | Not strictly evidence based, in NINDS trial this finding did not preclude benefit of tPA |
Based mainly on the results of the National Institute of Neurological Disorders and Stroke (NINDS) tPA trial,19 and recently supported by a large Phase IV observational study from the European Union,20 IV tPA for acute ischemic stroke is approved for use in many countries and is endorsed for the treatment of carefully selected ischemic stroke patients in a number of practice guidelines.4 Despite this, the emergency medicine community has been less enthusiastic about the use of IV tPA.21, 22 Although the risk of hemorrhagic complications is greater in certain subgroups of patients (ie, the most severe strokes, significant early CT changes, older age), there is no definitive evidence to suggest that these groups do not still benefit from the treatment.23 It is also clear that if patients are not carefully selected, meeting strict inclusion and exclusion criteria, the rate of complications is increased.24 Thus, as summarized in a practice statement of the American College of Emergency Physicians, There is insufficient evidence at this time to endorse the use of intravenous tPA in clinical practice when systems are not in place to ensure that the inclusion/exclusion criteria established by the NINDS guidelines for tPA use in acute stroke are followed.21 When counseling patients and their families about the benefits and risks of IV tPA, one should keep in mind that the NINDS trial demonstrated increased odds of excellent outcomes despite a significant 10‐fold increase in the risk of symptomatic intracranial hemorrhage (6.4% vs. 0.6%), and did not alter 30‐day mortality. The largest Phase IV cohort study of IV tPA treatment, Safe Implementation of Thrombolysis in Stroke Monitoring Study (SITS‐MOST) was mandated by the European Union upon approval of the medication for use in acute ischemic stroke.20 The results in 6483 patients showed that tPA, when used in strict accordance with published inclusion and exclusion criteria, could perform as well as it did in randomized trials.
The recently published European Cooperative Acute Stroke Study3 (ECASS‐3) trial demonstrated that IV tPA has efficacy with adequate safety up to 4.5 hours after the onset of symptoms. A total of 821 patients were enrolled and 375 received tPA. Exclusion criteria included diabetes being treated with medication with a history of prior stroke, an NIHSS score >25, or treatment with warfarin. The rates of hemorrhage (27.0% vs. 17.6%, P = 0.001) were in line with those of the SITS‐MOST study patients who were treated within the 3‐hour time window. There was no significant difference in mortality (7.7% tPA vs. 8.4% placebo). This study is relatively new; therefore, the data have not been reviewed by guideline committees.25
No Blood on the CT Scan, Results Back in >3 Hours, but 8 Hours, From Symptom Onset
Unfortunately as with our patient, most people do not present to an ER in a timely fashion. Nonetheless, there may be other treatments and interventions possible. If the patient arrives 8 hours from onset of symptoms, intraarterial (IA) interventions are a possibility. In such a case, a CT angiogram (CTA) of the neck from the arch of the aorta to the circle of Willis is recommended (barring any contraindications such as renal failure or iodine allergy). The rationale behind this study is that other treatment options, such as IA tPA or mechanical thrombectomy may be considered if a large arterial occlusion is identified. CTA is preferred over magnetic resonance angiography (MRA) due to the same time and patient cooperation issues mentioned above, though some expert centers may be set up to perform MRI and MRA rapidly in the acute setting. CTA or MRA is of great value early on in the emergent assessment of ischemic stroke patients, as it allows detailed evaluation of the cerebral vasculature; this knowledge helps define the pathophysiology of the ongoing stroke (eg, is there a larger artery occlusion?) and can help inform the approach to subsequent therapies.
The Guidelines (p. 1678)4 recommend IA thrombolysis as a treatment option if it can be started within 6 hours, based on results from the Prolyse in Acute Cerebral Thromboembolism (PROACT) II trial. This study involved angiography with identification of the occluded vessel (the proximal MCA‐M1 in this study) and administration of recombinant pro‐urokinase to the clot with functional outcome as the primary endpoint.26 At 3 months, patients who received the IA thrombolytic had a 40% chance of slight disability; unable to carry out all previous activities, but able to look after own affairs without assistance or better (ie, a modified Rankin Scale score of 2) vs. 25% of those not receiving the IA thrombolytic. Pro‐urokinase is not available in the United States; therefore, many institutions substitute IA tPA. The Guidelines further state that IA thrombolysis can be considered for use in some patients with contraindications to IV tPA (eg, recent surgery), but should not be used instead of IV tPA in patients otherwise eligible (p. 1678).4
There are now two U.S. Food and Drug Administration (FDA)‐approved devices for mechanical cerebral vasculature thrombectomy for use up to 8 hours from symptom onset. The mechanical embolus removal in cerebral ischemia (MERCI) clot retrieval device was originally approved by the FDA in August 2004 for restoring blood flow in the neurovasculature by removing thrombus in patients experiencing ischemic stroke. Modified devices have been approved as recently as January 2007.27 The Penumbra System was FDA‐approved in December 2007 for revascularization of patients with acute ischemic stroke secondary to intracranial large vessel occlusive disease.28 In both cases, the FDA approval was based on demonstration of safety in case series of patients treated with the devices.2931 No randomized trials have shown the use of these devices improves outcomes for stroke patients. The Guidelines state that Although the MERCI device is a reasonable intervention for extraction of IA thrombi in carefully selected patients, the panel also recognizes that the utility of the device in improving outcomes after stroke is unclear (p. 1684);4 this statement applies similarly to the Penumbra device.
More complex imaging techniques, including multimodal CT (CT, CTA, and CT perfusion) and MR (MRI with diffusion, MRA, and MR perfusion) are being used in some stroke centers to make decisions about acute ischemic stroke treatments.32, 33 The theory is that by using these techniques, one can determine the presence or absence of a mismatch, whereby the perfusion imaging suggests more tissue at risk of infarction than is seen as already abnormal on MR diffusion‐weighted images or compared to a clinical assessment. These mismatch patients are then seen as appropriate candidates for the more aggressive interventions (ie, late IV tPA or IA interventions).34 Unfortunately, the 2 largest randomized trials to look at this issue with respect to >3‐hour IV tPA both failed to show a benefit for patients selected in this manner.35, 36 Standardized definitions of mismatch are still needed, and larger randomized trials are needed before this approach can be suggested for routine care.3739
More complex interventions, available only at tertiary or comprehensive stroke centers, include a bridging approach in which IV tPA (at 2/3 standard dose) is followed by IA tPA, IV tPA with transcranial Doppler (TCD)‐enhanced thrombolysis or IA rescue thrombectomy when vascular imaging after IV tPA shows a persistent large artery occlusion. The Guidelines suggests that these more complex combinations of interventions to restore perfusion cannot be recommended outside the setting of clinical trials (p. 1685).4
No Blood on the CT Scan, Results Back in >8 Hours From Symptom Onset (or if Contraindications to Above Interventions)
This time frame takes the more aggressive interventions off the table. Per the Guidelines, 325 mg of aspirin is the default antiplatelet agent for use, and has been shown in 2 very large randomized trials to reduce early death and longer‐term disability vs. placebo after acute ischemic stroke.40, 41 Importantly, all patients who do not qualify for thrombolysis in the 0‐hour to 8‐hour time window should receive aspirin.
Although a number of small or pilot studies suggest a benefit of the addition of clopidogrel to aspirin for a period (13 months) immediately after ischemic stroke,4244 this more aggressive antiplatelet intervention is not an endorsed standard of care. As described below, the long‐term use of this antiplatelet combination has been consistently associated with a higher risk of hemorrhagic complications. There are no published data regarding the use of aspirin plus dipyridamole in the acute stroke setting. A number of randomized trials have now been performed that have consistently failed to show a benefit of heparin, or heparin‐like medications, for the routine treatment of acute ischemic stroke. Despite this, a number of exceptions exist, based more on tradition and theory than on evidence. These exceptions, for which an IV heparin drip will at times still be considered, include acute ischemic stroke due to dissection of the carotid or vertebral arteries, cardioembolic stroke with fresh clot seen on echocardiogram (ECHO), and a clinically progressive syndrome suggestive of basilar artery occlusion (see below).45, 46 Good evidence exists to specifically recommend the use of full‐dose heparin in the setting of cerebral venous sinus thrombosis.47
Basilar Artery Occlusion Syndromes
Basilar artery occlusion syndromes warrant special mention. These may involve patients who present with quadriparesis, altered mental status, vertigo, diplopia, and other brainstem signs. Conventional treatment of basilar artery occlusion has been associated with 40% mortality with 65% of survivors having severe disability.48 If suspected, an urgent CTA can usually confirm the diagnosis, and urge the clinician to expeditiously consider aggressive intervention. Only case series have been reported regarding basilar artery thrombosis and acute treatments. Based on these studies, it is generally agreed upon that patients who appear comatose or quadriplegic for more than 3 hours will likely have a very poor functional outcome regardless of treatment, and interventional treatment is withheld. If a basilar occlusion patient presents within the 3‐hour time window for IV tPA, they are thus treated, with follow‐up vascular imaging, and possible rescue IA mechanical thrombectomy if recanalization from the IV tPA does not occur. However, if the patient still has preserved neurologic function, or is waxing and waning, there is no clear time limit for IA interventions and they may be useful a day or more after presentation. For basilar occlusion patients with severe stenoses not responsive to lysis, or continuing to be symptomatic, angioplasty and stenting has also been used.46 Despite a lack of evidence, many stroke clinicians will use an IV heparin drip for treatment of acute basilar occlusive disease.
Malignant Middle Cerebral Artery (MCA) Infarction
Malignant MCA infarction is another specific clinical syndrome worthy of special consideration. It is most generally defined as a large infarction (1/2 or 2/3) of the MCA territory, somewhat depressed level of consciousness, and high stroke scale scores (ie, severe deficits) that goes on to severe cerebral edema, mass effect, and often herniation with death.49, 50 Associated patient characteristics include younger age, abnormal (incomplete) ipsilateral collateral circulation, and internal carotid artery occlusion.51 Maximal edema occurs 2 to 5 days from stroke onset and, despite best intensive therapy, has been associated with mortality rates of 70% to 80%.49, 50 A recent pooling of 3 small randomized trials of early decompressive hemicraniectomy and durotomy showed a 50% absolute risk reduction for mortality and a 23% absolute benefit in long‐term independence (modified Rankin scale 3).49 This treatment option should be strongly considered in carefully selected patients., Transfer to an appropriately equipped facility should be offered if not available at your hospital.
Returning to our case patient, upon arrival to the ED with symptoms of partial aphasia, right hemiplegia, and left gaze preference, there was a high suspicion for a left MCA stroke. Unfortunately, he was excluded from receiving IV tPA or any other interventions, as the last time he was known to be neurologically intact was the prior evening, which is taken to be the time of onset. Antiplatelet therapy was continued, and the patient was admitted for further workup.
The initial care of the patient with a cerebrovascular event is often quite complicated. Assimilation of a great deal of data must occur and decisions around therapy must be made in a timely fashion. In prior years there was little to offer in the way of therapy, which also meant there was little initial potential for iatrogenic complication. Both diagnostic and therapeutic options are evolving rapidly. We now have much to offer these patients both emergently and in areas of secondary prevention. In part 2 of this article, the patient's inpatient course and therapy will be reviewed.
- Organization WH. MONICA Manual, Part IV: Event Registration. Available at: http://www.ktl.fi/publications/monica/manual/part4/iv‐2.htm#s2. Accessed May2009.
- ,,, et al.Heart disease and stroke statistics 2008 update. A report from the American Heart Association Statistics Committee and Stroke Statistics Subcommittee.Circulation.200829;117(4):e25–e146.
- .Neurology in the next two decades: report of the Workforce Task Force of the American Academy of Neurology.Neurology.2000;54(4):787–789.
- ,,, et al.Guidelines for the early management of adults with ischemic stroke: a guideline from the American Heart Association/American Stroke Association Stroke Council, Clinical Cardiology Council, Cardiovascular Radiology and Intervention Council, and the Atherosclerotic Peripheral Vascular Disease and Quality of Care Outcomes in Research Interdisciplinary Working Groups: the American Academy of Neurology affirms the value of this guideline as an educational tool for neurologists.Stroke.2007;38(5):1655–1711.
- ,,,.Conditions that mimic stroke in the emergency department. Implications for acute stroke trials.Arch Neurol.1995;52(11):1119–1122.
- ,,,,.Distinguishing between stroke and mimic at the bedside: the brain attack study.Stroke.2006;37(3):769–775.
- ,,, et al.Stroke magnetic resonance imaging is accurate in hyperacute intracerebral hemorrhage: a multicenter study on the validity of stroke imaging.Stroke.2004;35(2):502–506.
- ,,, et al.Comparison of MRI and CT for detection of acute intracerebral hemorrhage.JAMA.2004;292(15):1823–1830.
- ,,, et al.Guidelines for the management of spontaneous intracerebral hemorrhage in adults: 2007 update: a guideline from the American Heart Association/American Stroke Association Stroke Council, High Blood Pressure Research Council, and the Quality of Care and Outcomes in Research Interdisciplinary Working Group.Stroke.2007;38(6):2001–2023.
- ,,.Aneurysmal subarachnoid hemorrhage.N Engl J Med.2006;354(4):387–396.
- ,,,.Subarachnoid haemorrhage.BMJ.2006;333(7561):235–240.
- ,,.Subarachnoid haemorrhage.Lancet.2007;369(9558):306–318.
- ,,.Intracerebral hemorrhage associated with oral anticoagulant therapy: current practices and unresolved questions.Stroke.2006;37(1):256–262.
- ,,, et al.Withdrawal of support in intracerebral hemorrhage may lead to self‐fulfilling prophecies.Neurology.2001;56(6):766–772.
- ,,,.Hospital usage of early do‐not‐resuscitate orders and outcome after intracerebral hemorrhage.Stroke.2004;35(5):1130–1134.
- ,,, et al.Early care limitations independently predict mortality after intracerebral hemorrhage.Neurology.2007;68(20):1651–1657.
- ,,,.Consent for intravenous thrombolysis in acute stroke: review and future directions.Arch Neurol.2007;64(6):785–792.
- .Thrombolysis (tissue plasminogen activator) in stroke: a medicolegal quagmire.Stroke.2006;37(7):1917–1922.
- Tissue plasminogen activator for acute ischemic stroke.The National Institute of Neurological Disorders and Stroke rt‐PA Stroke Study Group.N Engl J Med.1995;333(24):1581–1587.
- ,,, et al.Thrombolysis with alteplase for acute ischaemic stroke in the Safe Implementation of Thrombolysis in Stroke‐Monitoring Study (SITS‐MOST): an observational study.Lancet.2007;369(9558):275–282.
- American College of Emergency Physicians (ACEP). Use of Intravenous tPA for the Management of Acute Stroke in the Emergency Department. ACEP Policy Statement. February 2002. Available at: http://www.acep.org/practres.aspx?id=29834. Accessed May2009.
- American Academy of Emergency Medicine (AAEM). Position statement on the use of intravenous thrombolytic therapy in the treatment of stroke. January 2002. Available at: http://aaem.org/positionstatements/thrombolytictherapy.php. Accessed May2009.
- ,,, et al.Lack of clinical significance of early ischemic changes on computed tomography in acute stroke.JAMA.2001;286(22):2830–2838.
- ,,,,.Thrombolysis for acute stroke in routine clinical practice.Arch Intern Med.2002;162(17):1994–2001.
- ,,, et al.Thrombolysis with alteplase 3 to 4.5 hours after acute ischemic stroke.N Engl J Med.2008;359:1317–1329,1393–1395.
- ,,, et al.Intra‐arterial prourokinase for acute ischemic stroke. The PROACT II study: a randomized controlled trial. Prolyse in Acute Cerebral Thromboembolism.JAMA.1999;282(21):2003–2011.
- Modified MERCI Retriever FDA marketing approval letter. Available at: www.fda.gov/cdrh/pdf6/K062046.pdf. Accessed May2009.
- Penumbra System FDA marketing approval letter. Available at: www.fda.gov/cdrh/pdf7/K072718.pdf. Accessed May2009.
- .Safety of mechanical thrombectomy and intravenous tissue plasminogen activator in acute ischemic stroke. Results of the multi mechanical embolus removal in cerebral ischemia (MERCI) trial, part I.AJNR Am J Neuroradiol.2006;27(6):1177–1182.
- ,,, et al.Safety and efficacy of mechanical embolectomy in acute ischemic stroke: results of the MERCI trial.Stroke.2005;36(7):1432–1438.
- ,,, et al.The Penumbra System: a mechanical device for the treatment of acute stroke due to thromboembolism.AJNR Am J Neuroradiol.2008;29(7):1409–1413.
- ,,, et al.Comparison of CT perfusion and angiography and MRI in selecting stroke patients for acute treatment.Neurology.2007;68(9):694–697.
- ,,, et al.Combined intravenous and intraarterial revascularization therapy using MRI perfusion/diffusion mismatch selection for acute ischemic stroke at 3–6 h after symptom onset.Neurocrit Care.2008;8(3):353–359.
- ,,, et al.Refining the perfusion‐diffusion mismatch hypothesis.Stroke.2005;36(6):1153–1159.
- . DIAS‐2: no benefit of desmoteplase in acute ischemic stroke. Available at: www.medscape.com/viewarticle/557663. Accessed May2009.
- ,,, et al.Effects of alteplase beyond 3 h after stroke in the Echoplanar Imaging Thrombolytic Evaluation Trial (EPITHET): a placebo‐controlled randomised trial.Lancet Neurol.2008;7(4):299–309.
- ,,.Magnetic resonance perfusion diffusion mismatch and thrombolysis in acute ischaemic stroke: a systematic review of the evidence to date.J Neurol Neurosurg Psychiatry.2007;78(5):485–491.
- ,,, et al.Optimal definition for PWI/DWI mismatch in acute ischemic stroke patients.J Cereb Blood Flow Metab.2008;28(5):887–891.
- ,,, et al.Rapid assessment of perfusion‐diffusion mismatch.Stroke.2008;39(1):75–81.
- CAST: randomised placebo‐controlled trial of early aspirin use in 20,000 patients with acute ischaemic stroke.CAST (Chinese Acute Stroke Trial) Collaborative Group.Lancet.1997;349(9066):1641–1649.
- The International Stroke Trial (IST): a randomised trial of aspirin, subcutaneous heparin, both, or neither among 19435 patients with acute ischaemic stroke.International Stroke Trial Collaborative Group.Lancet.1997;349(9065):1569–1581.
- ,,, et al.Dual antiplatelet therapy with clopidogrel and aspirin in symptomatic carotid stenosis evaluated using doppler embolic signal detection: the clopidogrel and aspirin for reduction of emboli in symptomatic carotid stenosis (CARESS) trial.Circulation.2005;111(17):2233–2240.
- ,,, et al.Effect of urgent treatment of transient ischaemic attack and minor stroke on early recurrent stroke (EXPRESS study): a prospective population‐based sequential comparison.Lancet.2007;370(9596):1432–1442.
- ,,,,,.Fast assessment of stroke and transient ischaemic attack to prevent early recurrence (FASTER): a randomised controlled pilot trial.Lancet Neurol.2007;6(11):961–969.
- ,,, et al.Antiplatelets versus anticoagulation in cervical artery dissection.Stroke.2007;38(9):2605–2611.
- ,,.Basilar artery occlusion.Neurocrit Care.2004;1(3):319–329.
- ,.Cerebral venous thrombosis: an update.Lancet Neurol.2007;6(2):162–170.
- ,,,,.Outcome in patients with basilar artery occlusion treated conventionally.J Neurol Neurosurg Psychiatry.2005;76(9):1238–1241.
- ,,, et al.Early decompressive surgery in malignant infarction of the middle cerebral artery: a pooled analysis of three randomised controlled trials.Lancet Neurol.2007;6(3):215–222.
- ,,,,,.‘Malignant’ middle cerebral artery territory infarction: clinical course and prognostic signs.Arch Neurol.1996;53(4):309–315.
- ,,,,.Predictors for malignant middle cerebral artery infarctions: a postmortem analysis.Neurology. 282006;66(6):815–820.
- ,,,,,.Poor outcomes in patients who do not receive intravenous tissue plasminogen activator because of mild or improving ischemic stroke.Stroke.2005;36(11):2497–2499.
- Organization WH. MONICA Manual, Part IV: Event Registration. Available at: http://www.ktl.fi/publications/monica/manual/part4/iv‐2.htm#s2. Accessed May2009.
- ,,, et al.Heart disease and stroke statistics 2008 update. A report from the American Heart Association Statistics Committee and Stroke Statistics Subcommittee.Circulation.200829;117(4):e25–e146.
- .Neurology in the next two decades: report of the Workforce Task Force of the American Academy of Neurology.Neurology.2000;54(4):787–789.
- ,,, et al.Guidelines for the early management of adults with ischemic stroke: a guideline from the American Heart Association/American Stroke Association Stroke Council, Clinical Cardiology Council, Cardiovascular Radiology and Intervention Council, and the Atherosclerotic Peripheral Vascular Disease and Quality of Care Outcomes in Research Interdisciplinary Working Groups: the American Academy of Neurology affirms the value of this guideline as an educational tool for neurologists.Stroke.2007;38(5):1655–1711.
- ,,,.Conditions that mimic stroke in the emergency department. Implications for acute stroke trials.Arch Neurol.1995;52(11):1119–1122.
- ,,,,.Distinguishing between stroke and mimic at the bedside: the brain attack study.Stroke.2006;37(3):769–775.
- ,,, et al.Stroke magnetic resonance imaging is accurate in hyperacute intracerebral hemorrhage: a multicenter study on the validity of stroke imaging.Stroke.2004;35(2):502–506.
- ,,, et al.Comparison of MRI and CT for detection of acute intracerebral hemorrhage.JAMA.2004;292(15):1823–1830.
- ,,, et al.Guidelines for the management of spontaneous intracerebral hemorrhage in adults: 2007 update: a guideline from the American Heart Association/American Stroke Association Stroke Council, High Blood Pressure Research Council, and the Quality of Care and Outcomes in Research Interdisciplinary Working Group.Stroke.2007;38(6):2001–2023.
- ,,.Aneurysmal subarachnoid hemorrhage.N Engl J Med.2006;354(4):387–396.
- ,,,.Subarachnoid haemorrhage.BMJ.2006;333(7561):235–240.
- ,,.Subarachnoid haemorrhage.Lancet.2007;369(9558):306–318.
- ,,.Intracerebral hemorrhage associated with oral anticoagulant therapy: current practices and unresolved questions.Stroke.2006;37(1):256–262.
- ,,, et al.Withdrawal of support in intracerebral hemorrhage may lead to self‐fulfilling prophecies.Neurology.2001;56(6):766–772.
- ,,,.Hospital usage of early do‐not‐resuscitate orders and outcome after intracerebral hemorrhage.Stroke.2004;35(5):1130–1134.
- ,,, et al.Early care limitations independently predict mortality after intracerebral hemorrhage.Neurology.2007;68(20):1651–1657.
- ,,,.Consent for intravenous thrombolysis in acute stroke: review and future directions.Arch Neurol.2007;64(6):785–792.
- .Thrombolysis (tissue plasminogen activator) in stroke: a medicolegal quagmire.Stroke.2006;37(7):1917–1922.
- Tissue plasminogen activator for acute ischemic stroke.The National Institute of Neurological Disorders and Stroke rt‐PA Stroke Study Group.N Engl J Med.1995;333(24):1581–1587.
- ,,, et al.Thrombolysis with alteplase for acute ischaemic stroke in the Safe Implementation of Thrombolysis in Stroke‐Monitoring Study (SITS‐MOST): an observational study.Lancet.2007;369(9558):275–282.
- American College of Emergency Physicians (ACEP). Use of Intravenous tPA for the Management of Acute Stroke in the Emergency Department. ACEP Policy Statement. February 2002. Available at: http://www.acep.org/practres.aspx?id=29834. Accessed May2009.
- American Academy of Emergency Medicine (AAEM). Position statement on the use of intravenous thrombolytic therapy in the treatment of stroke. January 2002. Available at: http://aaem.org/positionstatements/thrombolytictherapy.php. Accessed May2009.
- ,,, et al.Lack of clinical significance of early ischemic changes on computed tomography in acute stroke.JAMA.2001;286(22):2830–2838.
- ,,,,.Thrombolysis for acute stroke in routine clinical practice.Arch Intern Med.2002;162(17):1994–2001.
- ,,, et al.Thrombolysis with alteplase 3 to 4.5 hours after acute ischemic stroke.N Engl J Med.2008;359:1317–1329,1393–1395.
- ,,, et al.Intra‐arterial prourokinase for acute ischemic stroke. The PROACT II study: a randomized controlled trial. Prolyse in Acute Cerebral Thromboembolism.JAMA.1999;282(21):2003–2011.
- Modified MERCI Retriever FDA marketing approval letter. Available at: www.fda.gov/cdrh/pdf6/K062046.pdf. Accessed May2009.
- Penumbra System FDA marketing approval letter. Available at: www.fda.gov/cdrh/pdf7/K072718.pdf. Accessed May2009.
- .Safety of mechanical thrombectomy and intravenous tissue plasminogen activator in acute ischemic stroke. Results of the multi mechanical embolus removal in cerebral ischemia (MERCI) trial, part I.AJNR Am J Neuroradiol.2006;27(6):1177–1182.
- ,,, et al.Safety and efficacy of mechanical embolectomy in acute ischemic stroke: results of the MERCI trial.Stroke.2005;36(7):1432–1438.
- ,,, et al.The Penumbra System: a mechanical device for the treatment of acute stroke due to thromboembolism.AJNR Am J Neuroradiol.2008;29(7):1409–1413.
- ,,, et al.Comparison of CT perfusion and angiography and MRI in selecting stroke patients for acute treatment.Neurology.2007;68(9):694–697.
- ,,, et al.Combined intravenous and intraarterial revascularization therapy using MRI perfusion/diffusion mismatch selection for acute ischemic stroke at 3–6 h after symptom onset.Neurocrit Care.2008;8(3):353–359.
- ,,, et al.Refining the perfusion‐diffusion mismatch hypothesis.Stroke.2005;36(6):1153–1159.
- . DIAS‐2: no benefit of desmoteplase in acute ischemic stroke. Available at: www.medscape.com/viewarticle/557663. Accessed May2009.
- ,,, et al.Effects of alteplase beyond 3 h after stroke in the Echoplanar Imaging Thrombolytic Evaluation Trial (EPITHET): a placebo‐controlled randomised trial.Lancet Neurol.2008;7(4):299–309.
- ,,.Magnetic resonance perfusion diffusion mismatch and thrombolysis in acute ischaemic stroke: a systematic review of the evidence to date.J Neurol Neurosurg Psychiatry.2007;78(5):485–491.
- ,,, et al.Optimal definition for PWI/DWI mismatch in acute ischemic stroke patients.J Cereb Blood Flow Metab.2008;28(5):887–891.
- ,,, et al.Rapid assessment of perfusion‐diffusion mismatch.Stroke.2008;39(1):75–81.
- CAST: randomised placebo‐controlled trial of early aspirin use in 20,000 patients with acute ischaemic stroke.CAST (Chinese Acute Stroke Trial) Collaborative Group.Lancet.1997;349(9066):1641–1649.
- The International Stroke Trial (IST): a randomised trial of aspirin, subcutaneous heparin, both, or neither among 19435 patients with acute ischaemic stroke.International Stroke Trial Collaborative Group.Lancet.1997;349(9065):1569–1581.
- ,,, et al.Dual antiplatelet therapy with clopidogrel and aspirin in symptomatic carotid stenosis evaluated using doppler embolic signal detection: the clopidogrel and aspirin for reduction of emboli in symptomatic carotid stenosis (CARESS) trial.Circulation.2005;111(17):2233–2240.
- ,,, et al.Effect of urgent treatment of transient ischaemic attack and minor stroke on early recurrent stroke (EXPRESS study): a prospective population‐based sequential comparison.Lancet.2007;370(9596):1432–1442.
- ,,,,,.Fast assessment of stroke and transient ischaemic attack to prevent early recurrence (FASTER): a randomised controlled pilot trial.Lancet Neurol.2007;6(11):961–969.
- ,,, et al.Antiplatelets versus anticoagulation in cervical artery dissection.Stroke.2007;38(9):2605–2611.
- ,,.Basilar artery occlusion.Neurocrit Care.2004;1(3):319–329.
- ,.Cerebral venous thrombosis: an update.Lancet Neurol.2007;6(2):162–170.
- ,,,,.Outcome in patients with basilar artery occlusion treated conventionally.J Neurol Neurosurg Psychiatry.2005;76(9):1238–1241.
- ,,, et al.Early decompressive surgery in malignant infarction of the middle cerebral artery: a pooled analysis of three randomised controlled trials.Lancet Neurol.2007;6(3):215–222.
- ,,,,,.‘Malignant’ middle cerebral artery territory infarction: clinical course and prognostic signs.Arch Neurol.1996;53(4):309–315.
- ,,,,.Predictors for malignant middle cerebral artery infarctions: a postmortem analysis.Neurology. 282006;66(6):815–820.
- ,,,,,.Poor outcomes in patients who do not receive intravenous tissue plasminogen activator because of mild or improving ischemic stroke.Stroke.2005;36(11):2497–2499.