User login
Camplyobacter Empyema
A 72‐year‐old man had been suffering from low‐grade fever, minimally productive cough, and shortness of breath for 1 week when he experienced sudden, moderately severe right‐sided chest pain. His local primary care physician found no abnormalities on physical exam and laboratory testing. A chest x‐ray, however, did reveal a small right‐sided pleural effusion. The patient was empirically started on levofloxacin but noticed no improvement. Two weeks into his illness, he was referred to our institution for further management. By this time, he reported a rapid 10‐pound weight loss and a daily low‐grade fever. Chest examination revealed dullness to percussion along with decreased breath sounds in the right posterior lung fields. A complete blood count showed an elevated white count of 17,000/mL with 14,000 neutrophils. Hemoglobin was 13.5 g/dL. A repeat chest x‐ ray and then a CT scan showed a multiloculated pleural effusion in the right lower hemithorax. Ultrasound‐guided tap of this effusion showed cloudy fluid consistent with pus, with a protein of 4.8 g/dL and total nucleated cells of 6000/mL. A gram stain on this fluid was negative.
The patient had a history remarkable for severe underlying chronic obstructive pulmonary disease (COPD). His forced expiratory volume in 1 second (FEV1) was 21%, and his diffusing capacity of carbon monoxide (DLCO) was 27%. Therefore, decortication under general anesthesia was not an option. So the largest pus pocket was drained under CT guidance, and the patient was dismissed home on levofloxacin.
He returned for follow‐up after 3 weeks and reported daily low‐grade fever, night sweats, and an additional weight loss of 14 pounds. His white count had risen to 18,300/mL with a neutrophil count of 16,600. Hemoglobin had fallen to 11.9 g/dL. A repeat CT scan showed that although the previously drained fluid pocket had resolved, a moderate amount of fluid had reaccumulated in other pockets. Delayed anaerobic culture results from the hospitalization 3 weeks earlier were now available and, interestingly, showed 2+ growth of Campylobacter jejuni, broadly sensitive to all antibiotics including penicillin. Piperacillin/tazobactam was started intravenously, and CT‐guided drainage of the largest pus pocket was again performed.
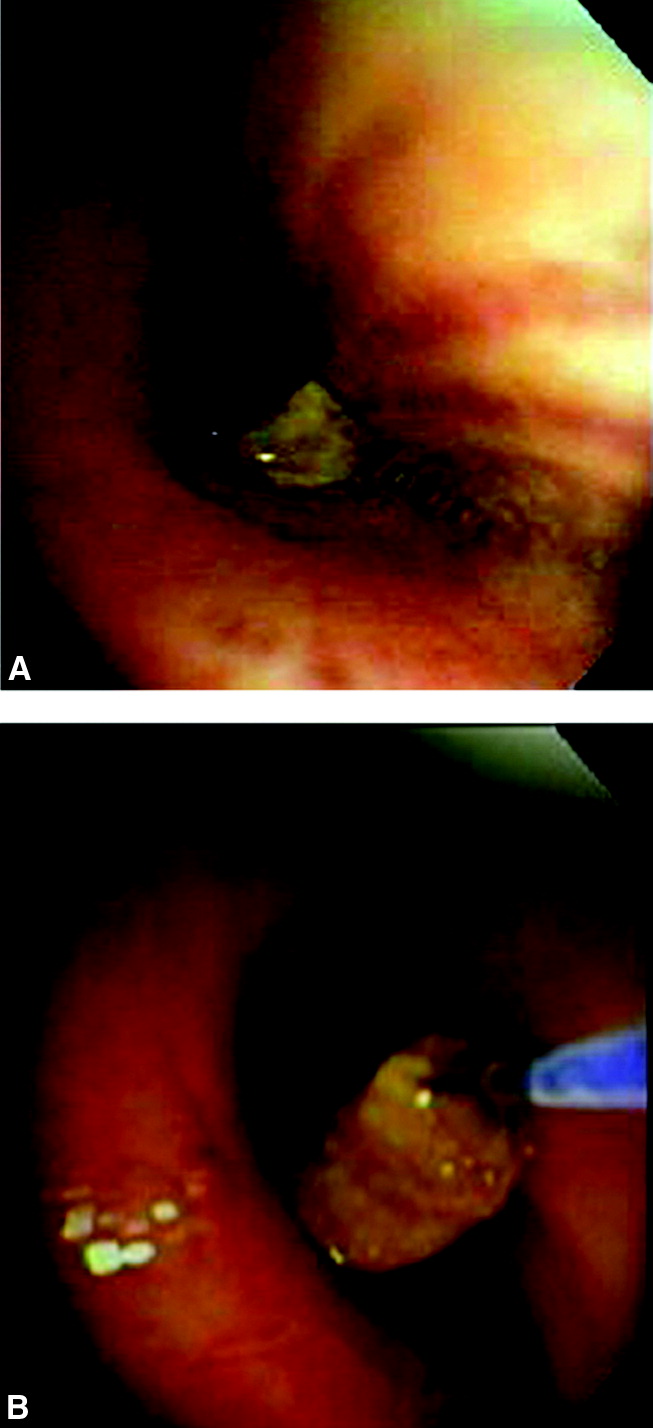
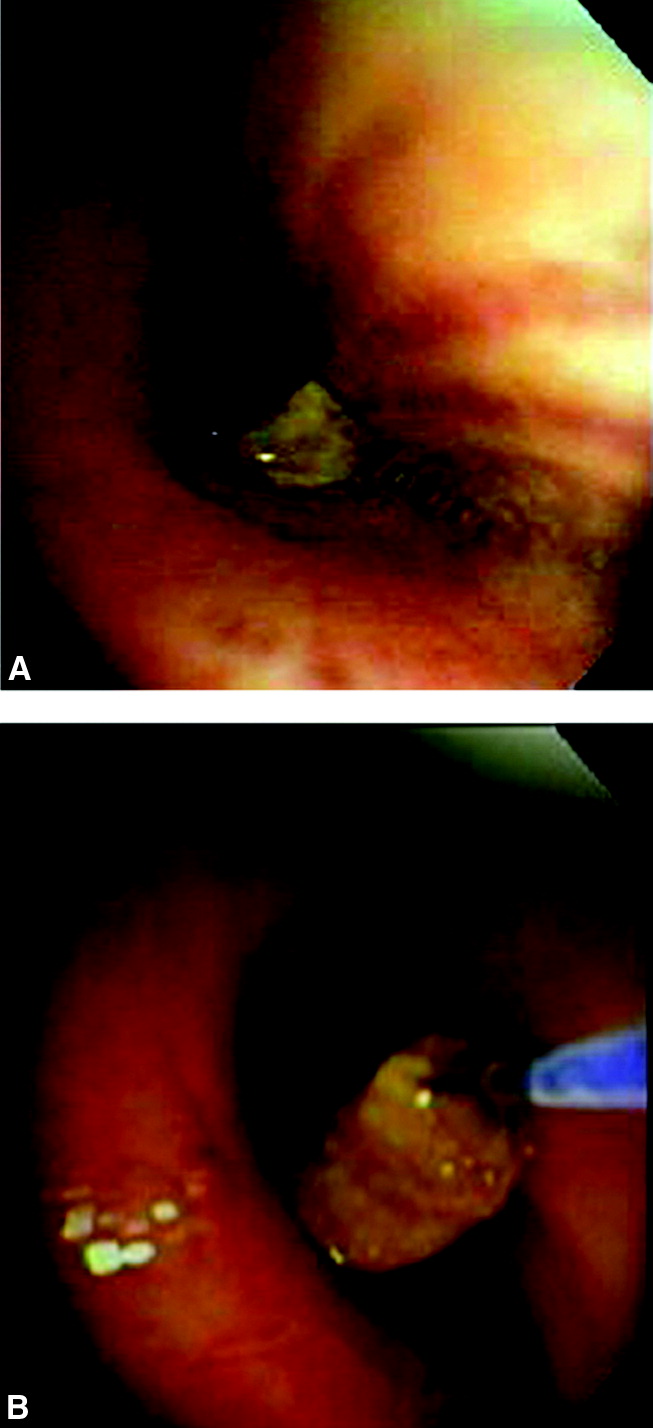
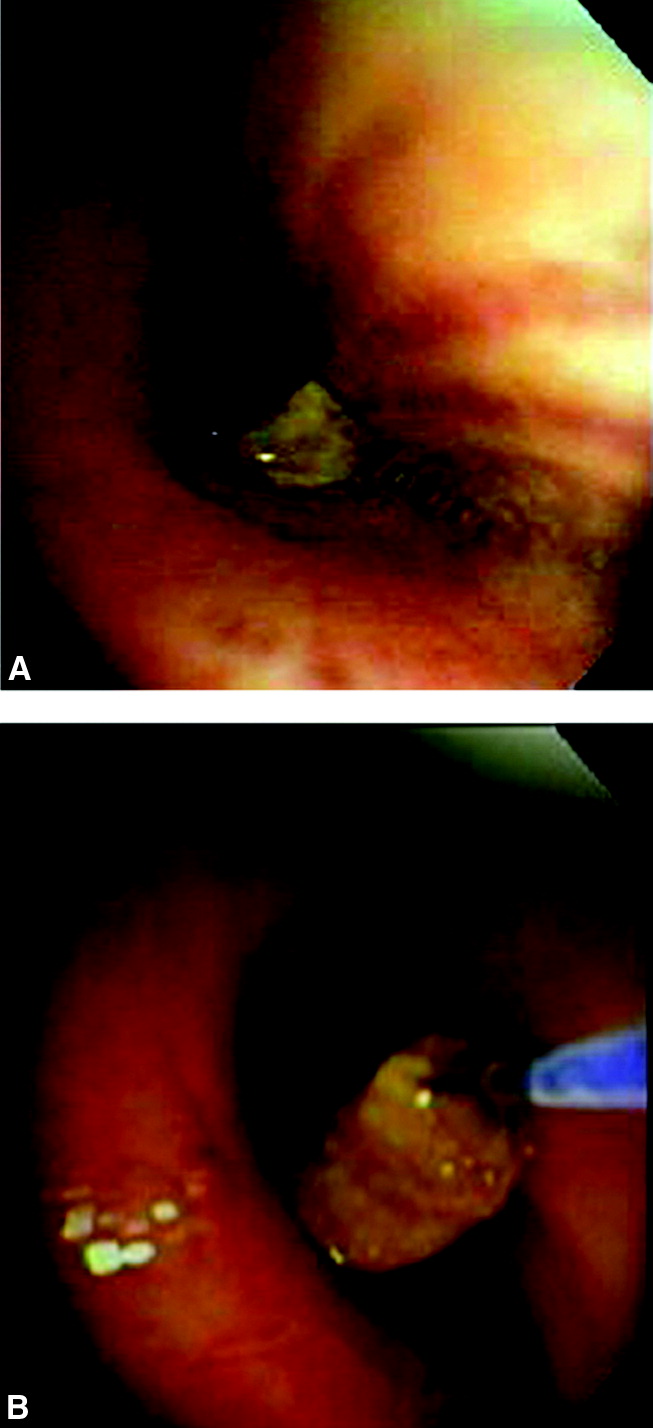
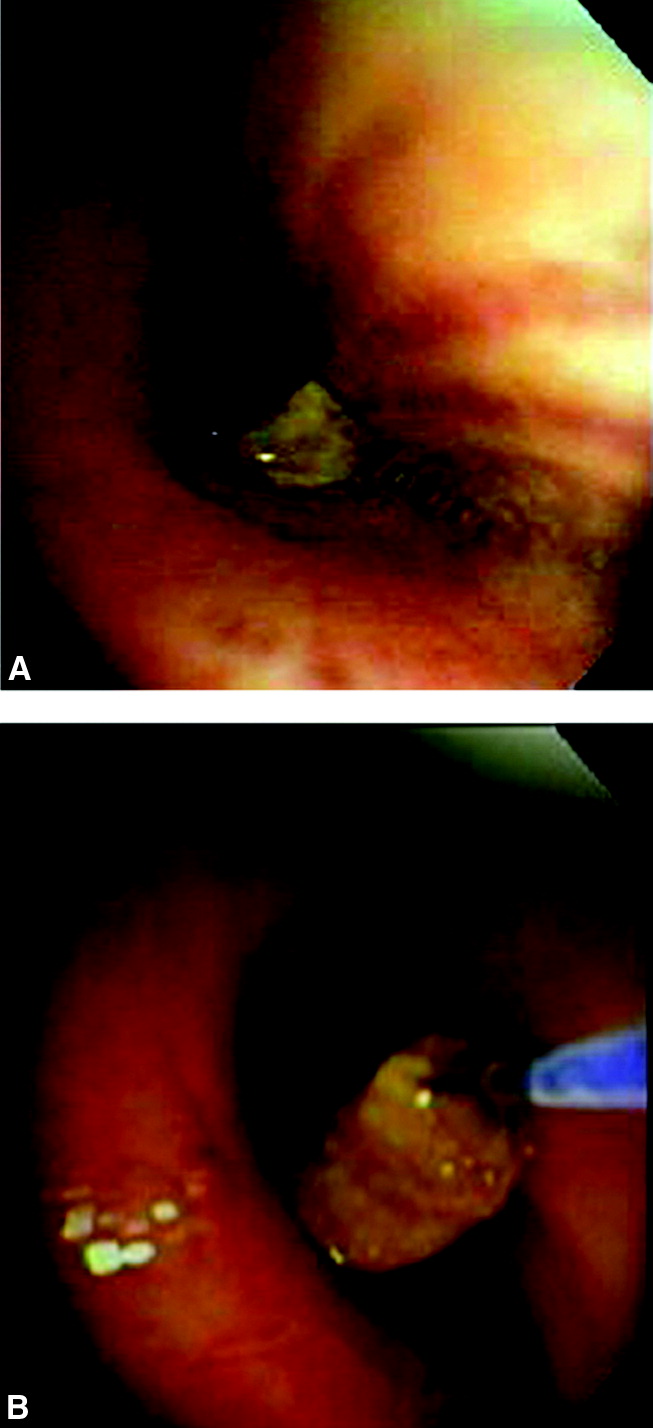
We carefully reexamined the patient's CT scan, and there appeared to be a lesion in the right main‐stem bronchus. We decided to perform a bronchoscopy, which revealed a foreign body in the right main‐stem bronchus. The foreign body turned out to be a piece of chicken and a peanut. On specific questioning of the patient again, he admitted that at times he coughed after eating too quickly. Specifically, he remembered that a few days before falling sick he was at a village fair, where he had had chicken, and he thought he might have coughed after eating it. He denied any diarrheal illness in the recent past. We obtained a swallow study and upper gastrointestinal endoscopy, both of which were unremarkable.
He improved remarkably after removal of the foreign body and was sent home on amoxicillin‐clavulanic acid for 3 weeks.
DISCUSSION
Campylobacter is one of the most common zoonoses in the world.1 Commercially raised poultry is nearly always colonized with Campylobacter jejuni, and therefore, not surprisingly, 50% to 70% of C. jejuni infection in humans is caused by undercooked poultry.2 The most common presentation of C. jejuni in humans is acute enteritis or colitis, but it can have numerous extraintestinal manifestations.3 Bacteremia occurs in fewer than 1% of patients, but C. jejuni meningitis and endocarditis have been reported. Hepatitis, interstitial nephritis, hemolytic‐uremic syndrome, and IgA nephropathy are other reported complications. Our patient probably aspirated a piece of undercooked chicken that likely was the source of the C. jejuni, causing a persistent empyema.
Most patients fully recover from C. jejuni infections without medications, but if illness is severe or prolonged, antibiotics are recommended. Macrolides are usually the first‐line treatment, but their increasing veterinary use is leading to their being resistant to these drugs.4 Most isolates are not susceptible to cephalosporins or penicillins, except amoxicillin or ticarcillin plus clavulanic acid. The C. jejuni isolated in culture in our lab from this patient was unusual in being broadly sensitive.
Our patient aspirated a foreign body in the form of chicken and a peanut without even realizing it. This is extremely uncommon, although foreign‐body aspiration in otherwise healthy and alert adults sometimes does occur. The most common presentation is sudden choking, coughing, and vomiting, followed by wheezing and breathlessness. Patients may also present with persistent cough, hemoptysis, fever, breathlessness, or wheezing. Children may present with cyanosis.
Inorganic foreign bodies tend to be from dental accidents, and organic aspirated foreign bodies tend to depend on the types of food eaten in a particular population, with bones, nuts, and apple pips the most common. In adults, all foreign bodies tend to lodge in the right bronchial tree. Aspiration of organic material is usually diagnosed later than aspiration of nonorganic material.5 In either case, airway foreign‐body aspiration is a common cause of recurrent bacterial pneumonia, and long delays in diagnosis are quite typical.6
Plain x‐rays may be entirely normal. A CT may demonstrate an aspirated foreign body in the lumen of the tracheobronchial tree. Other common findings are atelectasis, hyperlucency, bronchiectasis, lobar consolidation, ipsilateral pleural effusion, and lymphadenopathy and a thickened bronchial wall adjacent to the foreign body.7 Newer methods such as CT virtual bronchoscopy are being evaluated for use in selected cases when clinical suspicion is high.8 0
- ,,,.Campylobacter jejuni—an emerging foodborne pathogen.Emerg Infect Dis.1999;5(1):28–35.
- ,.Sources of Campylobacter colonization in broiler chickens.Appl Environ Microbiol.2003;69:4343–4351.
- .Clinical aspects of Campylobacter jejuni infections in adults.West J Med.1994;161(2):148–152.
- ,.Macrolide resistance in Campylobacter jejuni and Campylobacter coli.J Antimicrob Chemother.2006;58:243–255.
- ,,,.Bronchoscopic removal of foreign bodies in adults: experience with 62 patients from 1974–1998.Eur Respir J.1999;14:792–795.
- ,,,,.Foreign body aspiration into the lower airway in Chinese adults.Chest.1997;112(1):129–133.
- ,,,,,.CT findings of the chest in adults with aspirated foreign bodies.Eur Radiol.2001;11:606–611.
- ,,, et al.CT virtual bronchoscopy in the evaluation of children with suspected foreign body aspiration.Eur J Radiol.2003;48:188–192.
A 72‐year‐old man had been suffering from low‐grade fever, minimally productive cough, and shortness of breath for 1 week when he experienced sudden, moderately severe right‐sided chest pain. His local primary care physician found no abnormalities on physical exam and laboratory testing. A chest x‐ray, however, did reveal a small right‐sided pleural effusion. The patient was empirically started on levofloxacin but noticed no improvement. Two weeks into his illness, he was referred to our institution for further management. By this time, he reported a rapid 10‐pound weight loss and a daily low‐grade fever. Chest examination revealed dullness to percussion along with decreased breath sounds in the right posterior lung fields. A complete blood count showed an elevated white count of 17,000/mL with 14,000 neutrophils. Hemoglobin was 13.5 g/dL. A repeat chest x‐ ray and then a CT scan showed a multiloculated pleural effusion in the right lower hemithorax. Ultrasound‐guided tap of this effusion showed cloudy fluid consistent with pus, with a protein of 4.8 g/dL and total nucleated cells of 6000/mL. A gram stain on this fluid was negative.
The patient had a history remarkable for severe underlying chronic obstructive pulmonary disease (COPD). His forced expiratory volume in 1 second (FEV1) was 21%, and his diffusing capacity of carbon monoxide (DLCO) was 27%. Therefore, decortication under general anesthesia was not an option. So the largest pus pocket was drained under CT guidance, and the patient was dismissed home on levofloxacin.
He returned for follow‐up after 3 weeks and reported daily low‐grade fever, night sweats, and an additional weight loss of 14 pounds. His white count had risen to 18,300/mL with a neutrophil count of 16,600. Hemoglobin had fallen to 11.9 g/dL. A repeat CT scan showed that although the previously drained fluid pocket had resolved, a moderate amount of fluid had reaccumulated in other pockets. Delayed anaerobic culture results from the hospitalization 3 weeks earlier were now available and, interestingly, showed 2+ growth of Campylobacter jejuni, broadly sensitive to all antibiotics including penicillin. Piperacillin/tazobactam was started intravenously, and CT‐guided drainage of the largest pus pocket was again performed.
We carefully reexamined the patient's CT scan, and there appeared to be a lesion in the right main‐stem bronchus. We decided to perform a bronchoscopy, which revealed a foreign body in the right main‐stem bronchus. The foreign body turned out to be a piece of chicken and a peanut. On specific questioning of the patient again, he admitted that at times he coughed after eating too quickly. Specifically, he remembered that a few days before falling sick he was at a village fair, where he had had chicken, and he thought he might have coughed after eating it. He denied any diarrheal illness in the recent past. We obtained a swallow study and upper gastrointestinal endoscopy, both of which were unremarkable.
He improved remarkably after removal of the foreign body and was sent home on amoxicillin‐clavulanic acid for 3 weeks.
DISCUSSION
Campylobacter is one of the most common zoonoses in the world.1 Commercially raised poultry is nearly always colonized with Campylobacter jejuni, and therefore, not surprisingly, 50% to 70% of C. jejuni infection in humans is caused by undercooked poultry.2 The most common presentation of C. jejuni in humans is acute enteritis or colitis, but it can have numerous extraintestinal manifestations.3 Bacteremia occurs in fewer than 1% of patients, but C. jejuni meningitis and endocarditis have been reported. Hepatitis, interstitial nephritis, hemolytic‐uremic syndrome, and IgA nephropathy are other reported complications. Our patient probably aspirated a piece of undercooked chicken that likely was the source of the C. jejuni, causing a persistent empyema.
Most patients fully recover from C. jejuni infections without medications, but if illness is severe or prolonged, antibiotics are recommended. Macrolides are usually the first‐line treatment, but their increasing veterinary use is leading to their being resistant to these drugs.4 Most isolates are not susceptible to cephalosporins or penicillins, except amoxicillin or ticarcillin plus clavulanic acid. The C. jejuni isolated in culture in our lab from this patient was unusual in being broadly sensitive.
Our patient aspirated a foreign body in the form of chicken and a peanut without even realizing it. This is extremely uncommon, although foreign‐body aspiration in otherwise healthy and alert adults sometimes does occur. The most common presentation is sudden choking, coughing, and vomiting, followed by wheezing and breathlessness. Patients may also present with persistent cough, hemoptysis, fever, breathlessness, or wheezing. Children may present with cyanosis.
Inorganic foreign bodies tend to be from dental accidents, and organic aspirated foreign bodies tend to depend on the types of food eaten in a particular population, with bones, nuts, and apple pips the most common. In adults, all foreign bodies tend to lodge in the right bronchial tree. Aspiration of organic material is usually diagnosed later than aspiration of nonorganic material.5 In either case, airway foreign‐body aspiration is a common cause of recurrent bacterial pneumonia, and long delays in diagnosis are quite typical.6
Plain x‐rays may be entirely normal. A CT may demonstrate an aspirated foreign body in the lumen of the tracheobronchial tree. Other common findings are atelectasis, hyperlucency, bronchiectasis, lobar consolidation, ipsilateral pleural effusion, and lymphadenopathy and a thickened bronchial wall adjacent to the foreign body.7 Newer methods such as CT virtual bronchoscopy are being evaluated for use in selected cases when clinical suspicion is high.8 0
A 72‐year‐old man had been suffering from low‐grade fever, minimally productive cough, and shortness of breath for 1 week when he experienced sudden, moderately severe right‐sided chest pain. His local primary care physician found no abnormalities on physical exam and laboratory testing. A chest x‐ray, however, did reveal a small right‐sided pleural effusion. The patient was empirically started on levofloxacin but noticed no improvement. Two weeks into his illness, he was referred to our institution for further management. By this time, he reported a rapid 10‐pound weight loss and a daily low‐grade fever. Chest examination revealed dullness to percussion along with decreased breath sounds in the right posterior lung fields. A complete blood count showed an elevated white count of 17,000/mL with 14,000 neutrophils. Hemoglobin was 13.5 g/dL. A repeat chest x‐ ray and then a CT scan showed a multiloculated pleural effusion in the right lower hemithorax. Ultrasound‐guided tap of this effusion showed cloudy fluid consistent with pus, with a protein of 4.8 g/dL and total nucleated cells of 6000/mL. A gram stain on this fluid was negative.
The patient had a history remarkable for severe underlying chronic obstructive pulmonary disease (COPD). His forced expiratory volume in 1 second (FEV1) was 21%, and his diffusing capacity of carbon monoxide (DLCO) was 27%. Therefore, decortication under general anesthesia was not an option. So the largest pus pocket was drained under CT guidance, and the patient was dismissed home on levofloxacin.
He returned for follow‐up after 3 weeks and reported daily low‐grade fever, night sweats, and an additional weight loss of 14 pounds. His white count had risen to 18,300/mL with a neutrophil count of 16,600. Hemoglobin had fallen to 11.9 g/dL. A repeat CT scan showed that although the previously drained fluid pocket had resolved, a moderate amount of fluid had reaccumulated in other pockets. Delayed anaerobic culture results from the hospitalization 3 weeks earlier were now available and, interestingly, showed 2+ growth of Campylobacter jejuni, broadly sensitive to all antibiotics including penicillin. Piperacillin/tazobactam was started intravenously, and CT‐guided drainage of the largest pus pocket was again performed.
We carefully reexamined the patient's CT scan, and there appeared to be a lesion in the right main‐stem bronchus. We decided to perform a bronchoscopy, which revealed a foreign body in the right main‐stem bronchus. The foreign body turned out to be a piece of chicken and a peanut. On specific questioning of the patient again, he admitted that at times he coughed after eating too quickly. Specifically, he remembered that a few days before falling sick he was at a village fair, where he had had chicken, and he thought he might have coughed after eating it. He denied any diarrheal illness in the recent past. We obtained a swallow study and upper gastrointestinal endoscopy, both of which were unremarkable.
He improved remarkably after removal of the foreign body and was sent home on amoxicillin‐clavulanic acid for 3 weeks.
DISCUSSION
Campylobacter is one of the most common zoonoses in the world.1 Commercially raised poultry is nearly always colonized with Campylobacter jejuni, and therefore, not surprisingly, 50% to 70% of C. jejuni infection in humans is caused by undercooked poultry.2 The most common presentation of C. jejuni in humans is acute enteritis or colitis, but it can have numerous extraintestinal manifestations.3 Bacteremia occurs in fewer than 1% of patients, but C. jejuni meningitis and endocarditis have been reported. Hepatitis, interstitial nephritis, hemolytic‐uremic syndrome, and IgA nephropathy are other reported complications. Our patient probably aspirated a piece of undercooked chicken that likely was the source of the C. jejuni, causing a persistent empyema.
Most patients fully recover from C. jejuni infections without medications, but if illness is severe or prolonged, antibiotics are recommended. Macrolides are usually the first‐line treatment, but their increasing veterinary use is leading to their being resistant to these drugs.4 Most isolates are not susceptible to cephalosporins or penicillins, except amoxicillin or ticarcillin plus clavulanic acid. The C. jejuni isolated in culture in our lab from this patient was unusual in being broadly sensitive.
Our patient aspirated a foreign body in the form of chicken and a peanut without even realizing it. This is extremely uncommon, although foreign‐body aspiration in otherwise healthy and alert adults sometimes does occur. The most common presentation is sudden choking, coughing, and vomiting, followed by wheezing and breathlessness. Patients may also present with persistent cough, hemoptysis, fever, breathlessness, or wheezing. Children may present with cyanosis.
Inorganic foreign bodies tend to be from dental accidents, and organic aspirated foreign bodies tend to depend on the types of food eaten in a particular population, with bones, nuts, and apple pips the most common. In adults, all foreign bodies tend to lodge in the right bronchial tree. Aspiration of organic material is usually diagnosed later than aspiration of nonorganic material.5 In either case, airway foreign‐body aspiration is a common cause of recurrent bacterial pneumonia, and long delays in diagnosis are quite typical.6
Plain x‐rays may be entirely normal. A CT may demonstrate an aspirated foreign body in the lumen of the tracheobronchial tree. Other common findings are atelectasis, hyperlucency, bronchiectasis, lobar consolidation, ipsilateral pleural effusion, and lymphadenopathy and a thickened bronchial wall adjacent to the foreign body.7 Newer methods such as CT virtual bronchoscopy are being evaluated for use in selected cases when clinical suspicion is high.8 0
- ,,,.Campylobacter jejuni—an emerging foodborne pathogen.Emerg Infect Dis.1999;5(1):28–35.
- ,.Sources of Campylobacter colonization in broiler chickens.Appl Environ Microbiol.2003;69:4343–4351.
- .Clinical aspects of Campylobacter jejuni infections in adults.West J Med.1994;161(2):148–152.
- ,.Macrolide resistance in Campylobacter jejuni and Campylobacter coli.J Antimicrob Chemother.2006;58:243–255.
- ,,,.Bronchoscopic removal of foreign bodies in adults: experience with 62 patients from 1974–1998.Eur Respir J.1999;14:792–795.
- ,,,,.Foreign body aspiration into the lower airway in Chinese adults.Chest.1997;112(1):129–133.
- ,,,,,.CT findings of the chest in adults with aspirated foreign bodies.Eur Radiol.2001;11:606–611.
- ,,, et al.CT virtual bronchoscopy in the evaluation of children with suspected foreign body aspiration.Eur J Radiol.2003;48:188–192.
- ,,,.Campylobacter jejuni—an emerging foodborne pathogen.Emerg Infect Dis.1999;5(1):28–35.
- ,.Sources of Campylobacter colonization in broiler chickens.Appl Environ Microbiol.2003;69:4343–4351.
- .Clinical aspects of Campylobacter jejuni infections in adults.West J Med.1994;161(2):148–152.
- ,.Macrolide resistance in Campylobacter jejuni and Campylobacter coli.J Antimicrob Chemother.2006;58:243–255.
- ,,,.Bronchoscopic removal of foreign bodies in adults: experience with 62 patients from 1974–1998.Eur Respir J.1999;14:792–795.
- ,,,,.Foreign body aspiration into the lower airway in Chinese adults.Chest.1997;112(1):129–133.
- ,,,,,.CT findings of the chest in adults with aspirated foreign bodies.Eur Radiol.2001;11:606–611.
- ,,, et al.CT virtual bronchoscopy in the evaluation of children with suspected foreign body aspiration.Eur J Radiol.2003;48:188–192.
A Case of Palpebral Purpura and Trouble Swallowing
A48-year-old female was admitted to the hospital with atrial fibrillation. Her medical history was significant for systemic lupus erythematosus (SLE) diagnosed 28 years ago, with low dose prednisone treatment for the past 15 years.
In the past year, the patient had experienced progressive difficulty swallowing and often choked on her food, resulting in a 35-pound weight loss. She also mentioned that she had been bruising easily.
On examination, the patient had bruising around her eyes and a thick, enlarged tongue with clear marks of her teeth visible on the surface.
Which test will most likely lead to a diagnosis?
- Magnetic resonance imaging (MRI) of pituitary gland;
- Abdominal fat pad biopsy;
- Thyroid stimulating hormone (TSH) level;
- Serum Angiotensin converting enzyme (ACE) levels
- Tongue biopsy
Discussion
The answer is B: abdominal fat pad biopsy. Macroglossia, especially in adults, is a rare clinical finding and is most often associated with amyloidosis.1 It has also been rarely described in association with acromegaly, hypothyroidism, and sarcoidosis. In children, macroglossia may be seen in a variety of conditions including cretinism, Down syndrome, Beckwith-Wiedemann syndrome, and various storage diseases.2 Lymphangioma of the tongue may also present with macroglossia.3
Another finding classically seen in amyloidosis is palpebral purpura.4 The occurrence of these two physical findings together in this patient strongly suggests the diagnosis of amyloidosis. The amyloidoses are now considered a group of diseases characterized by extracellular deposition of insoluble fibrillar proteins in various organs secondary to misfolding of proteins.
They include not only primary and secondary amyloidosis but also Alzheimer’s, prion diseases, many other neurodegenerative disorders, and some types of cystic fibroses.5
Traditionally, amyloidosis was described as one of three types: primary, secondary, and heritable. Primary amyloidosis is the most common type and results from deposition of fragments of light chain immunoglobulin deposits. It is most frequently associated with plasma cell dyscrasias. Secondary, or AA, amyloidosis occurs in association with inflammatory conditions and results from deposition of fragments of the acute phase reactant serum amyloid A. Familial amyloidoses or the ATTR amyloidoses are a fairly heterogeneous group with different proteins associated with different disorders.5
The typical findings seen in this case are associated with primary amyloidosis.4 The presence of primary amyloidosis was confirmed in this case by a bone marrow biopsy. This patient had SLE, but SLE is usually not complicated by the development of amyloidosis, although rare cases in literature have been described.6 Also, as mentioned above, secondary amyloidosis is usually characterized by AA rather than AL amyloidosis.
The diagnosis of amyloidosis is made pathologically when an involved organ is biopsied. When clinical suspicion is high and no organ has been biopsied, the simplest procedure is to obtain an abdominal fat pad biopsy and stain it with Congo red. This test is 85% sensitive in patients with primary amyloidosis.4 TH
References
- Xavier SD, Bussoloti IF, Muller H. Macroglossia secondary to systemic amyloidosis: case report and literature review. Ear Nose Throat J. 2005 Jun;84(6):358-361.
- Wolford LM, Cottrell DA. Diagnosis of macroglossia and indications for reduction glossectomy. Am J Orthod Dentofacial Orthop. 1996 Aug;110:170-177.
- Gulemann M, Katz J. Macroglossia combined with lymphangioma: a case report. J Clin Pediatr Dent. 2003 Winter;27(2):167-169.
- Falk RH, Comenzo RL, Skinner M. The systemic amyloidoses. N Engl J Med 1997; 337: 898-909.
- Merlini G, Bellotti V. Mechanisms of disease: molecular mechanisms of amyloidosis. N Engl J Med. 2003; 349:583-596.
- Al-Hoqail I, Naddaf H, Al-Rikabi A, et al. Systemic lupus erythematosus and amyloidosis. Clin Rheumatol. 1997 Jun;16(4):422-424.on.
A48-year-old female was admitted to the hospital with atrial fibrillation. Her medical history was significant for systemic lupus erythematosus (SLE) diagnosed 28 years ago, with low dose prednisone treatment for the past 15 years.
In the past year, the patient had experienced progressive difficulty swallowing and often choked on her food, resulting in a 35-pound weight loss. She also mentioned that she had been bruising easily.
On examination, the patient had bruising around her eyes and a thick, enlarged tongue with clear marks of her teeth visible on the surface.
Which test will most likely lead to a diagnosis?
- Magnetic resonance imaging (MRI) of pituitary gland;
- Abdominal fat pad biopsy;
- Thyroid stimulating hormone (TSH) level;
- Serum Angiotensin converting enzyme (ACE) levels
- Tongue biopsy
Discussion
The answer is B: abdominal fat pad biopsy. Macroglossia, especially in adults, is a rare clinical finding and is most often associated with amyloidosis.1 It has also been rarely described in association with acromegaly, hypothyroidism, and sarcoidosis. In children, macroglossia may be seen in a variety of conditions including cretinism, Down syndrome, Beckwith-Wiedemann syndrome, and various storage diseases.2 Lymphangioma of the tongue may also present with macroglossia.3
Another finding classically seen in amyloidosis is palpebral purpura.4 The occurrence of these two physical findings together in this patient strongly suggests the diagnosis of amyloidosis. The amyloidoses are now considered a group of diseases characterized by extracellular deposition of insoluble fibrillar proteins in various organs secondary to misfolding of proteins.
They include not only primary and secondary amyloidosis but also Alzheimer’s, prion diseases, many other neurodegenerative disorders, and some types of cystic fibroses.5
Traditionally, amyloidosis was described as one of three types: primary, secondary, and heritable. Primary amyloidosis is the most common type and results from deposition of fragments of light chain immunoglobulin deposits. It is most frequently associated with plasma cell dyscrasias. Secondary, or AA, amyloidosis occurs in association with inflammatory conditions and results from deposition of fragments of the acute phase reactant serum amyloid A. Familial amyloidoses or the ATTR amyloidoses are a fairly heterogeneous group with different proteins associated with different disorders.5
The typical findings seen in this case are associated with primary amyloidosis.4 The presence of primary amyloidosis was confirmed in this case by a bone marrow biopsy. This patient had SLE, but SLE is usually not complicated by the development of amyloidosis, although rare cases in literature have been described.6 Also, as mentioned above, secondary amyloidosis is usually characterized by AA rather than AL amyloidosis.
The diagnosis of amyloidosis is made pathologically when an involved organ is biopsied. When clinical suspicion is high and no organ has been biopsied, the simplest procedure is to obtain an abdominal fat pad biopsy and stain it with Congo red. This test is 85% sensitive in patients with primary amyloidosis.4 TH
References
- Xavier SD, Bussoloti IF, Muller H. Macroglossia secondary to systemic amyloidosis: case report and literature review. Ear Nose Throat J. 2005 Jun;84(6):358-361.
- Wolford LM, Cottrell DA. Diagnosis of macroglossia and indications for reduction glossectomy. Am J Orthod Dentofacial Orthop. 1996 Aug;110:170-177.
- Gulemann M, Katz J. Macroglossia combined with lymphangioma: a case report. J Clin Pediatr Dent. 2003 Winter;27(2):167-169.
- Falk RH, Comenzo RL, Skinner M. The systemic amyloidoses. N Engl J Med 1997; 337: 898-909.
- Merlini G, Bellotti V. Mechanisms of disease: molecular mechanisms of amyloidosis. N Engl J Med. 2003; 349:583-596.
- Al-Hoqail I, Naddaf H, Al-Rikabi A, et al. Systemic lupus erythematosus and amyloidosis. Clin Rheumatol. 1997 Jun;16(4):422-424.on.
A48-year-old female was admitted to the hospital with atrial fibrillation. Her medical history was significant for systemic lupus erythematosus (SLE) diagnosed 28 years ago, with low dose prednisone treatment for the past 15 years.
In the past year, the patient had experienced progressive difficulty swallowing and often choked on her food, resulting in a 35-pound weight loss. She also mentioned that she had been bruising easily.
On examination, the patient had bruising around her eyes and a thick, enlarged tongue with clear marks of her teeth visible on the surface.
Which test will most likely lead to a diagnosis?
- Magnetic resonance imaging (MRI) of pituitary gland;
- Abdominal fat pad biopsy;
- Thyroid stimulating hormone (TSH) level;
- Serum Angiotensin converting enzyme (ACE) levels
- Tongue biopsy
Discussion
The answer is B: abdominal fat pad biopsy. Macroglossia, especially in adults, is a rare clinical finding and is most often associated with amyloidosis.1 It has also been rarely described in association with acromegaly, hypothyroidism, and sarcoidosis. In children, macroglossia may be seen in a variety of conditions including cretinism, Down syndrome, Beckwith-Wiedemann syndrome, and various storage diseases.2 Lymphangioma of the tongue may also present with macroglossia.3
Another finding classically seen in amyloidosis is palpebral purpura.4 The occurrence of these two physical findings together in this patient strongly suggests the diagnosis of amyloidosis. The amyloidoses are now considered a group of diseases characterized by extracellular deposition of insoluble fibrillar proteins in various organs secondary to misfolding of proteins.
They include not only primary and secondary amyloidosis but also Alzheimer’s, prion diseases, many other neurodegenerative disorders, and some types of cystic fibroses.5
Traditionally, amyloidosis was described as one of three types: primary, secondary, and heritable. Primary amyloidosis is the most common type and results from deposition of fragments of light chain immunoglobulin deposits. It is most frequently associated with plasma cell dyscrasias. Secondary, or AA, amyloidosis occurs in association with inflammatory conditions and results from deposition of fragments of the acute phase reactant serum amyloid A. Familial amyloidoses or the ATTR amyloidoses are a fairly heterogeneous group with different proteins associated with different disorders.5
The typical findings seen in this case are associated with primary amyloidosis.4 The presence of primary amyloidosis was confirmed in this case by a bone marrow biopsy. This patient had SLE, but SLE is usually not complicated by the development of amyloidosis, although rare cases in literature have been described.6 Also, as mentioned above, secondary amyloidosis is usually characterized by AA rather than AL amyloidosis.
The diagnosis of amyloidosis is made pathologically when an involved organ is biopsied. When clinical suspicion is high and no organ has been biopsied, the simplest procedure is to obtain an abdominal fat pad biopsy and stain it with Congo red. This test is 85% sensitive in patients with primary amyloidosis.4 TH
References
- Xavier SD, Bussoloti IF, Muller H. Macroglossia secondary to systemic amyloidosis: case report and literature review. Ear Nose Throat J. 2005 Jun;84(6):358-361.
- Wolford LM, Cottrell DA. Diagnosis of macroglossia and indications for reduction glossectomy. Am J Orthod Dentofacial Orthop. 1996 Aug;110:170-177.
- Gulemann M, Katz J. Macroglossia combined with lymphangioma: a case report. J Clin Pediatr Dent. 2003 Winter;27(2):167-169.
- Falk RH, Comenzo RL, Skinner M. The systemic amyloidoses. N Engl J Med 1997; 337: 898-909.
- Merlini G, Bellotti V. Mechanisms of disease: molecular mechanisms of amyloidosis. N Engl J Med. 2003; 349:583-596.
- Al-Hoqail I, Naddaf H, Al-Rikabi A, et al. Systemic lupus erythematosus and amyloidosis. Clin Rheumatol. 1997 Jun;16(4):422-424.on.