User login
A Shooting in the Hospital: When Domestic Violence Occurs in the Hospital, Reflection, and Response
On September 12, 2017, a son walked into his mother’s room in the surgical intensive care unit (ICU) of Dartmouth-Hitchcock Medical Center (DHMC) in Lebanon, New Hampshire, and shot her with a handgun. As an actively practicing hospitalist and the Chief Clinical Officer for DHMC, I immediately became involved with our hospitals’ response to domestic violence, a homicide, and an issue that to this point we felt lived outside our walls.
Several hospital systems are struggling with violence entering their institutions, particularly in their psychiatry and emergency service areas, fueled in part by untreated mental health and the rising opioid epidemic. Although gun violence in hospitals is indeed rare, inside the hospital, it occurs often in the emergency department.1 In New Hampshire, we suffer from a woefully underfunded state mental health infrastructure and one of the highest opioid death rates in the United States.2
DHMC is a 400-bed academic medical center, level 1 trauma center, and a National Cancer Institute (NCI)-designated cancer center that serves New Hampshire and eastern Vermont with its community and critical access hospitals and community group practices across the two states. With a wide geographic catchment area, our academic hospital at DHMC has one of the highest case-mix indices in the northeastern United States and is in the top 30 among hospitals of >300 beds in the United States.
After the shooting, the patient’s son left the ICU without targeting anyone else, and despite video surveillance systems, he was not seen leaving the hospital. At the same time, a Code Blue was called to address the victim and her needs. The Critical Care staff struggled to attend to and resuscitate the victim, and my Medicine team, on call that day, was paged and rushed to the ICU to assist. In a unit trained to manage the sequelae of trauma, this event was painfully surreal. Ultimately, the surgical critical-care physician, attending to the patient, ended the resuscitation efforts when it was clear that the patient, now a homicide victim, could not be saved.
With the shooter’s whereabouts unknown, a Code Silver (Active Shooter alert) was called. Then, following our “Run-Hide-Fight” training protocol, staff, patients, and visitors exited the building in large numbers and those that could not, sheltered in place. The operating room and the emergency department were secured and continued to function.
More than 160 law enforcement officers, including trained tactical and SWAT teams, from 13 different agencies arrived on scene. Ninety minutes after the shooting, the son was apprehended at a police traffic checkpoint, attempting to leave the hospital campus.
Our involvement in this event did not end at this point. Concerned about the possibility of other suspects or devices left in the hospital, the law enforcement officers swept our hospital. With a 1.2 million square foot campus, this would take another two hours, during which we still provided care to our patients and asked the staff and families to continue to seek safe shelter.
The shock of this terrible day was immediate and profound, leading to a thorough debrief and systematic analysis of how we might improve our processes and in turn help other organizations that might unfortunately face similar situations.
We reflected on how to better secure our hospital and to strengthen our coordination and collaboration with law enforcement. We increased our security presence not only in the ICU but also in our emergency department and developed individual unit-based security measures. We fast-tracked a unit-based shutdown plan that was already in process and increased our commitments to plan and drill for larger scenarios in conjunction with law enforcement agencies.
The physical location of our hospital was important in how our response unfolded. DHMC’s unique rural location in northern New England added challenges specific to our location, which may provide an opportunity for other hospitals to consider. Although we were able to provide care, water, and transport during this tragedy on a warm day in September, caring for thousands of people outside a hospital during a typical subzero February would be a different story.
Communication during the event and how specifically to ask people to act were identified as a key area of improvement. We realized that our language and training around the various codes lacked clarity and specificity. As is familiar to many, in our hospital with Red, Blue, Black, Purple, and White codes, some staff (and certainly families and visitors) were not sure what to do in a “Code Silver.” We worked to better define our language so that in a future event or in a drill, we would state in plain language that we have “an active shooter” or a “violence with weapons” event in progress with clear instructions on next steps. Our term “Run-Hide-Fight” was changed to “Avoid-Hide-Fight” to better reflect updated training and best practice for a future event. We revised our teaching and training materials and protocols, so that in the event of a similar situation, we could provide information in plain language, across numerous formats, and with some frequency to keep people apprised, even if the situation is not changing.
Our methods of ongoing communications were also reassessed. In our reviews, it became clear that the notification systems and the computer-based alerts seen on the computers of hospital staff were different from those at the medical school. Communication protocols on pagers and mobile phones and across social media such as Facebook and Twitter were redesigned. Though our institution has long had the ability to provide cell phone notifications during emergencies, not all employees and staff had elected to activate this feature. We also improved our speaker systems so that overhead paging and alerts could be heard outside the building.
Having improved personal reference materials on hand is important. We updated the cards attached to our ID badges with clear instructions about “active shooter” or “violence with weapon” situations. We also developed different response scenarios dependent on the campus location. An event in the ICU, for example, might require leaving the scene, although sheltering-in-place might be more appropriate for an offsite administrative building.
A significant challenge to our active-shooter situation was making sure that our staff, patients, visitors, and their families were adequately supported following the event. Learning from the experiences of other hospitals and communities, we undertook a deliberate process of preparedness and healing.3 From our surgical ICU to our distant community group practices, we provided communication and avenues for personal support. Our Employee Assistance Program provided 24/7 support in a conference room in the surgical ICU and in other areas, on and off site, for all staff at Dartmouth-Hitchcock. The shooting affected those in the vicinity, as well as far away. Staff who had experienced domestic and other violence in their past were impacted in ways that required special care and attention. Some who were in adjacent rooms during the event were able to return to work immediately, whereas other staff, in separate units and more distant clinics, struggled and required leaves of absence. Through this event, we witnessed the personal and deep psychological impact of such violence. We held town halls, updated daily communications from our Incident Command Team, and maintained an open dialog across the organization.
In reflection, it is challenging to face this experience without the greater context of what we unfortunately experience all too often in America today. We have seen the spectrum from the shootings at Marjory Stoneman Douglas High School in Parkland, Florida, to the isolated events that rarely reach our national news and collective consciousness. It seems that we have already experienced a shooting at a school every week in the US.
There is even an overlap seen in domestic and mass shootings as we saw in the Sandy Hook Elementary School shootings in 2012, in which the tragic event was preceded by the shooter murdering his mother in her home.4 Today, in the US, women are disproportionally the subject of domestic violence, and more than half of all killed are done so by a male family member. The presence of a gun in domestic violence situations increases the risk for homicide for women by 500%.5- 7 Our experience indeed mirrored this reality.
Many readers of this piece will recognize how similar their situation is to that of our hospital, that this happens elsewhere, not here. Although my institution has faced this as a tragedy that has tested our organization, one cannot also be deeply troubled by the greater impact of domestic and gun violence on healthcare and the American society today. Our staff and physicians have been witness and at times subject to such violence, and this experience has now made it even more poignant. Ultimately, and sadly, we feel that we are more prepared.
Disclosures
The author has nothing to disclose.
1. Kelen GD, Catlett CL, Kunitz JG, Hsieh YH. Hospital-based shootings in the United States: 2000 to 2011. Ann Emerg Med. 2012;60(6):790-798. doi: 10.1016/j.annemergmed.2012.08.012. PubMed
2. Center for Disease Control and Preventions (CDC) Drug Overdose Death Data. https://www.cdc.gov/drugoverdose/data/statedeaths.html. Accessed April 10, 2018
3. Van Den Bos J, Creten N, Davenport S, Roberts, M. Cost of community violence to hospitals and health systems. Report for the American Hospital Association. July 26, 2017
4. Krouse WJ, Richardson DJ. Mass murder with firearms: incidents and victims, 1999-2013. Congressional Research Service. https://fas.org/sgp/crs/misc/R44126.pdf. Accessed April 10, 2018
5. Campbell JC, Webster D, Koziol-McLain J, et al. Risk factors for femicide within physically abusive intimate relationships. Am J Public Health. 2003;93(7):1089-1097. https:/doi.org/10.2105/AJPH.93.7.1089.
6. Fox JA, Zawitz MW. Homicide trends in the United States: Bureau of Justice Statistics; 2009.
7. Federal Bureau of Investigation. 2014 Crime in their United States. https://ucr.fbi.gov/crime-in-the-u.s/2014/crime-in-the-u.s.-2014/cius-home. Accessed April 10, 2018
On September 12, 2017, a son walked into his mother’s room in the surgical intensive care unit (ICU) of Dartmouth-Hitchcock Medical Center (DHMC) in Lebanon, New Hampshire, and shot her with a handgun. As an actively practicing hospitalist and the Chief Clinical Officer for DHMC, I immediately became involved with our hospitals’ response to domestic violence, a homicide, and an issue that to this point we felt lived outside our walls.
Several hospital systems are struggling with violence entering their institutions, particularly in their psychiatry and emergency service areas, fueled in part by untreated mental health and the rising opioid epidemic. Although gun violence in hospitals is indeed rare, inside the hospital, it occurs often in the emergency department.1 In New Hampshire, we suffer from a woefully underfunded state mental health infrastructure and one of the highest opioid death rates in the United States.2
DHMC is a 400-bed academic medical center, level 1 trauma center, and a National Cancer Institute (NCI)-designated cancer center that serves New Hampshire and eastern Vermont with its community and critical access hospitals and community group practices across the two states. With a wide geographic catchment area, our academic hospital at DHMC has one of the highest case-mix indices in the northeastern United States and is in the top 30 among hospitals of >300 beds in the United States.
After the shooting, the patient’s son left the ICU without targeting anyone else, and despite video surveillance systems, he was not seen leaving the hospital. At the same time, a Code Blue was called to address the victim and her needs. The Critical Care staff struggled to attend to and resuscitate the victim, and my Medicine team, on call that day, was paged and rushed to the ICU to assist. In a unit trained to manage the sequelae of trauma, this event was painfully surreal. Ultimately, the surgical critical-care physician, attending to the patient, ended the resuscitation efforts when it was clear that the patient, now a homicide victim, could not be saved.
With the shooter’s whereabouts unknown, a Code Silver (Active Shooter alert) was called. Then, following our “Run-Hide-Fight” training protocol, staff, patients, and visitors exited the building in large numbers and those that could not, sheltered in place. The operating room and the emergency department were secured and continued to function.
More than 160 law enforcement officers, including trained tactical and SWAT teams, from 13 different agencies arrived on scene. Ninety minutes after the shooting, the son was apprehended at a police traffic checkpoint, attempting to leave the hospital campus.
Our involvement in this event did not end at this point. Concerned about the possibility of other suspects or devices left in the hospital, the law enforcement officers swept our hospital. With a 1.2 million square foot campus, this would take another two hours, during which we still provided care to our patients and asked the staff and families to continue to seek safe shelter.
The shock of this terrible day was immediate and profound, leading to a thorough debrief and systematic analysis of how we might improve our processes and in turn help other organizations that might unfortunately face similar situations.
We reflected on how to better secure our hospital and to strengthen our coordination and collaboration with law enforcement. We increased our security presence not only in the ICU but also in our emergency department and developed individual unit-based security measures. We fast-tracked a unit-based shutdown plan that was already in process and increased our commitments to plan and drill for larger scenarios in conjunction with law enforcement agencies.
The physical location of our hospital was important in how our response unfolded. DHMC’s unique rural location in northern New England added challenges specific to our location, which may provide an opportunity for other hospitals to consider. Although we were able to provide care, water, and transport during this tragedy on a warm day in September, caring for thousands of people outside a hospital during a typical subzero February would be a different story.
Communication during the event and how specifically to ask people to act were identified as a key area of improvement. We realized that our language and training around the various codes lacked clarity and specificity. As is familiar to many, in our hospital with Red, Blue, Black, Purple, and White codes, some staff (and certainly families and visitors) were not sure what to do in a “Code Silver.” We worked to better define our language so that in a future event or in a drill, we would state in plain language that we have “an active shooter” or a “violence with weapons” event in progress with clear instructions on next steps. Our term “Run-Hide-Fight” was changed to “Avoid-Hide-Fight” to better reflect updated training and best practice for a future event. We revised our teaching and training materials and protocols, so that in the event of a similar situation, we could provide information in plain language, across numerous formats, and with some frequency to keep people apprised, even if the situation is not changing.
Our methods of ongoing communications were also reassessed. In our reviews, it became clear that the notification systems and the computer-based alerts seen on the computers of hospital staff were different from those at the medical school. Communication protocols on pagers and mobile phones and across social media such as Facebook and Twitter were redesigned. Though our institution has long had the ability to provide cell phone notifications during emergencies, not all employees and staff had elected to activate this feature. We also improved our speaker systems so that overhead paging and alerts could be heard outside the building.
Having improved personal reference materials on hand is important. We updated the cards attached to our ID badges with clear instructions about “active shooter” or “violence with weapon” situations. We also developed different response scenarios dependent on the campus location. An event in the ICU, for example, might require leaving the scene, although sheltering-in-place might be more appropriate for an offsite administrative building.
A significant challenge to our active-shooter situation was making sure that our staff, patients, visitors, and their families were adequately supported following the event. Learning from the experiences of other hospitals and communities, we undertook a deliberate process of preparedness and healing.3 From our surgical ICU to our distant community group practices, we provided communication and avenues for personal support. Our Employee Assistance Program provided 24/7 support in a conference room in the surgical ICU and in other areas, on and off site, for all staff at Dartmouth-Hitchcock. The shooting affected those in the vicinity, as well as far away. Staff who had experienced domestic and other violence in their past were impacted in ways that required special care and attention. Some who were in adjacent rooms during the event were able to return to work immediately, whereas other staff, in separate units and more distant clinics, struggled and required leaves of absence. Through this event, we witnessed the personal and deep psychological impact of such violence. We held town halls, updated daily communications from our Incident Command Team, and maintained an open dialog across the organization.
In reflection, it is challenging to face this experience without the greater context of what we unfortunately experience all too often in America today. We have seen the spectrum from the shootings at Marjory Stoneman Douglas High School in Parkland, Florida, to the isolated events that rarely reach our national news and collective consciousness. It seems that we have already experienced a shooting at a school every week in the US.
There is even an overlap seen in domestic and mass shootings as we saw in the Sandy Hook Elementary School shootings in 2012, in which the tragic event was preceded by the shooter murdering his mother in her home.4 Today, in the US, women are disproportionally the subject of domestic violence, and more than half of all killed are done so by a male family member. The presence of a gun in domestic violence situations increases the risk for homicide for women by 500%.5- 7 Our experience indeed mirrored this reality.
Many readers of this piece will recognize how similar their situation is to that of our hospital, that this happens elsewhere, not here. Although my institution has faced this as a tragedy that has tested our organization, one cannot also be deeply troubled by the greater impact of domestic and gun violence on healthcare and the American society today. Our staff and physicians have been witness and at times subject to such violence, and this experience has now made it even more poignant. Ultimately, and sadly, we feel that we are more prepared.
Disclosures
The author has nothing to disclose.
On September 12, 2017, a son walked into his mother’s room in the surgical intensive care unit (ICU) of Dartmouth-Hitchcock Medical Center (DHMC) in Lebanon, New Hampshire, and shot her with a handgun. As an actively practicing hospitalist and the Chief Clinical Officer for DHMC, I immediately became involved with our hospitals’ response to domestic violence, a homicide, and an issue that to this point we felt lived outside our walls.
Several hospital systems are struggling with violence entering their institutions, particularly in their psychiatry and emergency service areas, fueled in part by untreated mental health and the rising opioid epidemic. Although gun violence in hospitals is indeed rare, inside the hospital, it occurs often in the emergency department.1 In New Hampshire, we suffer from a woefully underfunded state mental health infrastructure and one of the highest opioid death rates in the United States.2
DHMC is a 400-bed academic medical center, level 1 trauma center, and a National Cancer Institute (NCI)-designated cancer center that serves New Hampshire and eastern Vermont with its community and critical access hospitals and community group practices across the two states. With a wide geographic catchment area, our academic hospital at DHMC has one of the highest case-mix indices in the northeastern United States and is in the top 30 among hospitals of >300 beds in the United States.
After the shooting, the patient’s son left the ICU without targeting anyone else, and despite video surveillance systems, he was not seen leaving the hospital. At the same time, a Code Blue was called to address the victim and her needs. The Critical Care staff struggled to attend to and resuscitate the victim, and my Medicine team, on call that day, was paged and rushed to the ICU to assist. In a unit trained to manage the sequelae of trauma, this event was painfully surreal. Ultimately, the surgical critical-care physician, attending to the patient, ended the resuscitation efforts when it was clear that the patient, now a homicide victim, could not be saved.
With the shooter’s whereabouts unknown, a Code Silver (Active Shooter alert) was called. Then, following our “Run-Hide-Fight” training protocol, staff, patients, and visitors exited the building in large numbers and those that could not, sheltered in place. The operating room and the emergency department were secured and continued to function.
More than 160 law enforcement officers, including trained tactical and SWAT teams, from 13 different agencies arrived on scene. Ninety minutes after the shooting, the son was apprehended at a police traffic checkpoint, attempting to leave the hospital campus.
Our involvement in this event did not end at this point. Concerned about the possibility of other suspects or devices left in the hospital, the law enforcement officers swept our hospital. With a 1.2 million square foot campus, this would take another two hours, during which we still provided care to our patients and asked the staff and families to continue to seek safe shelter.
The shock of this terrible day was immediate and profound, leading to a thorough debrief and systematic analysis of how we might improve our processes and in turn help other organizations that might unfortunately face similar situations.
We reflected on how to better secure our hospital and to strengthen our coordination and collaboration with law enforcement. We increased our security presence not only in the ICU but also in our emergency department and developed individual unit-based security measures. We fast-tracked a unit-based shutdown plan that was already in process and increased our commitments to plan and drill for larger scenarios in conjunction with law enforcement agencies.
The physical location of our hospital was important in how our response unfolded. DHMC’s unique rural location in northern New England added challenges specific to our location, which may provide an opportunity for other hospitals to consider. Although we were able to provide care, water, and transport during this tragedy on a warm day in September, caring for thousands of people outside a hospital during a typical subzero February would be a different story.
Communication during the event and how specifically to ask people to act were identified as a key area of improvement. We realized that our language and training around the various codes lacked clarity and specificity. As is familiar to many, in our hospital with Red, Blue, Black, Purple, and White codes, some staff (and certainly families and visitors) were not sure what to do in a “Code Silver.” We worked to better define our language so that in a future event or in a drill, we would state in plain language that we have “an active shooter” or a “violence with weapons” event in progress with clear instructions on next steps. Our term “Run-Hide-Fight” was changed to “Avoid-Hide-Fight” to better reflect updated training and best practice for a future event. We revised our teaching and training materials and protocols, so that in the event of a similar situation, we could provide information in plain language, across numerous formats, and with some frequency to keep people apprised, even if the situation is not changing.
Our methods of ongoing communications were also reassessed. In our reviews, it became clear that the notification systems and the computer-based alerts seen on the computers of hospital staff were different from those at the medical school. Communication protocols on pagers and mobile phones and across social media such as Facebook and Twitter were redesigned. Though our institution has long had the ability to provide cell phone notifications during emergencies, not all employees and staff had elected to activate this feature. We also improved our speaker systems so that overhead paging and alerts could be heard outside the building.
Having improved personal reference materials on hand is important. We updated the cards attached to our ID badges with clear instructions about “active shooter” or “violence with weapon” situations. We also developed different response scenarios dependent on the campus location. An event in the ICU, for example, might require leaving the scene, although sheltering-in-place might be more appropriate for an offsite administrative building.
A significant challenge to our active-shooter situation was making sure that our staff, patients, visitors, and their families were adequately supported following the event. Learning from the experiences of other hospitals and communities, we undertook a deliberate process of preparedness and healing.3 From our surgical ICU to our distant community group practices, we provided communication and avenues for personal support. Our Employee Assistance Program provided 24/7 support in a conference room in the surgical ICU and in other areas, on and off site, for all staff at Dartmouth-Hitchcock. The shooting affected those in the vicinity, as well as far away. Staff who had experienced domestic and other violence in their past were impacted in ways that required special care and attention. Some who were in adjacent rooms during the event were able to return to work immediately, whereas other staff, in separate units and more distant clinics, struggled and required leaves of absence. Through this event, we witnessed the personal and deep psychological impact of such violence. We held town halls, updated daily communications from our Incident Command Team, and maintained an open dialog across the organization.
In reflection, it is challenging to face this experience without the greater context of what we unfortunately experience all too often in America today. We have seen the spectrum from the shootings at Marjory Stoneman Douglas High School in Parkland, Florida, to the isolated events that rarely reach our national news and collective consciousness. It seems that we have already experienced a shooting at a school every week in the US.
There is even an overlap seen in domestic and mass shootings as we saw in the Sandy Hook Elementary School shootings in 2012, in which the tragic event was preceded by the shooter murdering his mother in her home.4 Today, in the US, women are disproportionally the subject of domestic violence, and more than half of all killed are done so by a male family member. The presence of a gun in domestic violence situations increases the risk for homicide for women by 500%.5- 7 Our experience indeed mirrored this reality.
Many readers of this piece will recognize how similar their situation is to that of our hospital, that this happens elsewhere, not here. Although my institution has faced this as a tragedy that has tested our organization, one cannot also be deeply troubled by the greater impact of domestic and gun violence on healthcare and the American society today. Our staff and physicians have been witness and at times subject to such violence, and this experience has now made it even more poignant. Ultimately, and sadly, we feel that we are more prepared.
Disclosures
The author has nothing to disclose.
1. Kelen GD, Catlett CL, Kunitz JG, Hsieh YH. Hospital-based shootings in the United States: 2000 to 2011. Ann Emerg Med. 2012;60(6):790-798. doi: 10.1016/j.annemergmed.2012.08.012. PubMed
2. Center for Disease Control and Preventions (CDC) Drug Overdose Death Data. https://www.cdc.gov/drugoverdose/data/statedeaths.html. Accessed April 10, 2018
3. Van Den Bos J, Creten N, Davenport S, Roberts, M. Cost of community violence to hospitals and health systems. Report for the American Hospital Association. July 26, 2017
4. Krouse WJ, Richardson DJ. Mass murder with firearms: incidents and victims, 1999-2013. Congressional Research Service. https://fas.org/sgp/crs/misc/R44126.pdf. Accessed April 10, 2018
5. Campbell JC, Webster D, Koziol-McLain J, et al. Risk factors for femicide within physically abusive intimate relationships. Am J Public Health. 2003;93(7):1089-1097. https:/doi.org/10.2105/AJPH.93.7.1089.
6. Fox JA, Zawitz MW. Homicide trends in the United States: Bureau of Justice Statistics; 2009.
7. Federal Bureau of Investigation. 2014 Crime in their United States. https://ucr.fbi.gov/crime-in-the-u.s/2014/crime-in-the-u.s.-2014/cius-home. Accessed April 10, 2018
1. Kelen GD, Catlett CL, Kunitz JG, Hsieh YH. Hospital-based shootings in the United States: 2000 to 2011. Ann Emerg Med. 2012;60(6):790-798. doi: 10.1016/j.annemergmed.2012.08.012. PubMed
2. Center for Disease Control and Preventions (CDC) Drug Overdose Death Data. https://www.cdc.gov/drugoverdose/data/statedeaths.html. Accessed April 10, 2018
3. Van Den Bos J, Creten N, Davenport S, Roberts, M. Cost of community violence to hospitals and health systems. Report for the American Hospital Association. July 26, 2017
4. Krouse WJ, Richardson DJ. Mass murder with firearms: incidents and victims, 1999-2013. Congressional Research Service. https://fas.org/sgp/crs/misc/R44126.pdf. Accessed April 10, 2018
5. Campbell JC, Webster D, Koziol-McLain J, et al. Risk factors for femicide within physically abusive intimate relationships. Am J Public Health. 2003;93(7):1089-1097. https:/doi.org/10.2105/AJPH.93.7.1089.
6. Fox JA, Zawitz MW. Homicide trends in the United States: Bureau of Justice Statistics; 2009.
7. Federal Bureau of Investigation. 2014 Crime in their United States. https://ucr.fbi.gov/crime-in-the-u.s/2014/crime-in-the-u.s.-2014/cius-home. Accessed April 10, 2018
© 2018 Society of Hospital Medicine
Acute Pancreatitis
A 55‐year‐old man presents with colicky right upper quadrant pain radiating to his back for 12 hours. He does not use ethanol and has no familial or personal history of pancreatic disease. Pertinent laboratory values include: white blood cell count 23.6 103/L; hemoglobin 16.2 g/dL; blood urea nitrogen (BUN) 52 mg/dL; aspartate aminotransferase 110 U/L; alanine aminotransferase 272 U/L; alkaline phosphatase 432 U/L; total bilirubin 4.3 mg/dL; amylase 2230 U/L; lipase 1623 U/L. He is afebrile, normotensive, and not hypoxic, but his respiratory rate is 30. He has voluntary guarding with palpation of the abdomen, decreased bowel sounds, and decreased breath sounds at the left lung base. A transabdominal ultrasound of the right upper quadrant reveals cholelithiaisis without choledocholithiasis. There is mild peripancreatic stranding and the head is slightly edematous.
NATURAL HISTORY
Acute pancreatitis (AP) is a common cause for emergency room presentation, resulting in over 280,000 hospital admissions in the United States at a cost of nearly $3 billion dollars annually.[1] In its mildest form it may require a 2‐ to 5‐day hospital stay and an uncomplicated discharge. In more severe cases, such as in the setting of pancreatic necrosis and/or the development of organ failure, hospitalization can feature a much longer and complicated hospital course.[2]
|
| AP is now classified as mild, moderately acute, or severe based on the presence of local complications and/or persistent organ failure. |
| Lactated Ringer's solution should be used in all patients as the resuscitative fluid in AP |
| Aggressive fluid resuscitation is critical (defined as 250500 mL/h), especially in the first 24 hours of admission. |
| Enteric feeding should be attempted within the first 72 hours of admission and can be given orally with a low‐fat diet. |
| Antibiotics should not be used unless there is documented infection; prophylactic antibiotics to treat necrotizing AP are not beneficial. |
| New definitions of pancreatic fluid collections determine optimal therapy. |
| Medical therapy for infected pancreatic necrosis should be attempted prior to necrosectomy. |
| Alternatives to open necrosectomy, such as endoscopic or retroperitoneal debridement, are preferred in cases of unstable infected pancreatic necrosis. |
DIAGNOSTIC CRITERIA AND CLASSIFICATION
AP is diagnosed by the patient having 2 out of the following 3 criteria: (1) classic clinical symptoms with abdominal pain consistent with AP (2) serum amylase and/or lipase greater than 3 times the upper limit of normal, and/or (3) characteristic findings from abdominal imaging.[3] It is important for the hospitalist to recognize that patients can have AP with normal serum amylase and/or lipase levels, as long as their clinical symptoms and imaging exam are consistent with the disease.[4] It is also important to recognize that amylase and/or lipase elevation is not 100% specific for pancreatitis; alternate conditions that elevate amylase levels include renal insufficiency, intestinal ischemia and obstruction, macroamylasemia, and multiple medications, whereas lipase elevations can be seen in spontaneous bacterial peritonitis, intestinal ischemia, and esophagitis.[5]
AP is classified as either mild (absence of organ failure or local complications), moderate (local complications and/or transient organ failure 48 hours) or severe (persistent organ failure >48 hours).[3] Organ failure is defined by the modified Marshall score, and local complications include pancreatic fluid collections, pancreatic and peripancreatic necrosis, and vascular thrombosis (Table 2).[6]
| Organ System Score | 0 | 1 | 2 | 3 | 4 |
|---|---|---|---|---|---|
| |||||
| Respiratory (PaO2/FiO2) | >400 | 301400 | 201300 | 101200 | 101 |
| Renal serum creatinine (mg/dL) | 1.4 | 1.41.8 | 1.93.6 | 3.74.9 | >4.9 |
| Cardiovascular systolic blood pressure (mm Hg) | >90 | 90, fluid responsive | 90, not fluid responsive | 90, pH 7.3 | 90, pH 7.2 |
ETIOLOGY
Transiently obstructing gallstones, thought to account for about 50% of cases, are the most common cause of AP. The rising prevalence of obesity, which is a known risk factor for AP due to the corresponding increase in the frequency of gallstones, suggests that this will continue to be the leading cause going forward.[7] Alcohol use is associated with both acute and chronic pancreatitis; however, the extent to which it is a primary cause of AP is uncertain.[8] Trauma, medications, hypercalcemia, and hypertriglyceridemia must also be considered; however, they are much less common. AP from endoscopic retrograde cholangiopancreatography (ERCP) occurs following 5% of procedures and from endoscopic ultrasound (EUS) fine‐needle aspiration following 1%. Although several medications are clearly associated with AP, many that were previously invoked seem less likely.[9] Immunoglobulin G (IgG) 4related systemic disease, although rare, is becoming more recognized and should be considered when the more common etiologies are ruled out. Finally, it is controversial whether anatomic findings such as pancreatic divisum and functional disorders such as sphincter of Oddi dysfunction cause AP.[10]
Identifying the cause of an acute episode remains important, as subsequent treatment strategies can be tailored to help prevent recurrence. A thorough personal history, including prior gallbladder disease, alcohol use, and medications is strongly recommended. Basic laboratory studies including liver function tests, serum calcium and triglycerides, as well as a right upper quadrant ultrasound are indicated in all patients presenting with AP.[1] Idiopathic AP is not uncommon. Given the increasing awareness of genetic factors, potential role of advanced endoscopy, and higher risk of recurrence in this group, patients with idiopathic AP should be referred to specialized centers of expertise.[4]
PROGNOSTICATION
Most cases of AP are mild and do not require prolonged hospitalization; however, because 5% of hospitalized patients will die from this disease, prognostic criteria are needed to determine high‐risk cases.[11] Multiple systems have been developed (Bedside Index for Severity in Acute Pancreatitis, Ranson's, Acute Physiology and Chronic Health Evaluation II, Computed Tomography Severity Index), but all have had difficulty achieving accuracy in a user‐friendly tool; because of this, hospitalists should instead focus on the individual laboratory parameters that correlate with pathophysiologic derangement. Elevations in BUN and hematocrit indicate hypovolemia, leukocytosis, and fluid sequestration are indicators of the inflammatory cascade. Creatinine, elevated liver tests, and hypoxia are indicators of organ damage. Low calcium is reflective of fat necrosis saponification (endorgan damage) and also an indicator of hypovolemia. Essentially, the prediction of severity depends on identifying indications of endorgan damage in a timely manner and can be performed through a combination of age, known comorbidities, physical exam, and basic laboratory testing.[12]
ADDITIONAL INITIAL IMAGING
Although sensitive and specific for AP, routine computed tomography (CT) imaging for all patients presenting with suspected AP is not indicated. The diagnosis is often clear on a clinical and lab basis alone, and most patients with AP will improve within 48 hours.[13] CT or magnetic resonance imaging (MRI) can be considered for patients with an unclear diagnosis and indeterminate ultrasound or in those who are not improving within the first 48 to72 hours after presentation. This additional imaging can help make an alternative diagnosis or detect an early complication such as pancreatic necrosis. CT is preferred; however, MRI may be utilized if there is a high suspicion for biliary stones that were not seen on ultrasound or when CT is indicated but impaired renal function precludes its use.[4] In patients presenting with recurrent idiopathic AP, EUS is recommended to evaluate for an occult malignancy or microlithiasis.[14]
INITIAL CLINICAL MANAGEMENT
Without evidence of either (1) ascending cholangitis or (2) proven choledocholithiasis with clinical decompensation and worsening liver tests, ERCP should not be performed and management should be focused on supportive care, pain control, and monitoring prognostic information regarding severity. The initial management of AP should include fluid replacement with lactated Ringer's (LR) solution at 5‐10 mL/kg/h to achieve noninvasive parameters of a heart rate 120, mean arterial pressure 65 to 85 mm Hg, and urine output >0.5 to 1 mL/kg/h. LR decreases the incidence of the systemic inflammatory response syndrome (SIRS) by 80% compared with normal saline.[4, 15] Early and sufficient fluid replacement is associated with decreased rates of SIRS and organ failure, whereas under‐resuscitation has been associated with necrosis and increased mortality. In the first 48 to 72 hours of admission, frequent assessment of hemoglobin (HgB) and BUN, as well as urine output measurements, should be obtained to make sure fluid resuscitation is adequate.[4] Intravenous fluid replacement should continue in the hospital until the patient can adequately maintain appropriate fluid intake orally. Prophylactic antimicrobial therapy is not indicated in initial cases of AP, unless there are clear signs of an underlying infection. Pain control is essential, and efforts at reintroducing oral feeding should be initiated once the pain is decreasing. There are no randomized trials that have identified an optimal narcotic‐based pain regimen. On a daily basis, a complete blood count, renal function, and liver function should be measured. There is no reason to continue measuring serum amylase or lipase, as it may not be elevated in some instances in AP, and its fluctuation is not indicative of a change in clinical status.
Case Management Strategy
The patient has mild AP based on lack of organ failure and local complications and is admitted to the regular medical floor. The etiology appears to be due to cholelithiasis, but the patient does not have cholangitis, so ERCP was not considered, and antibiotics were not started. Aggressive fluid resuscitation with lactated Ringer's is started at a rate of 350 mL/h, and BUN and HgB are monitored every 8 hours to make sure that these levels are decreasing. The patient is placed on a low‐fat diet and encouraged to eat as tolerated. Further imaging is not ordered at this time.
Hospital Day 3
The patient's liver tests have normalized, but the BUN continues to rise (82 mg/dL) despite aggressive fluid resuscitation with LR. He remains afebrile and normotensive, but is now hypoxic and requiring nasal cannula oxygen at 4 L/min to maintain his oxygen saturation above 90%. His abdominal pain is controlled with intravenous opiates, but he is not hungry or able to eat. With these changes in his clinical course, a CT scan is performed, which demonstrates acute peripancreatic necrosis centered on the head of the pancreas.
PERSISTENT ORGAN FAILURE AND PANCREATIC NECROSIS
Generally, patients with severe AP (persistent organ failure >48 hours following admission) should be followed in the intensive care unit for effective monitoring and support.
Pancreatic necrosis is defined as a diffuse or focal area of nonviable pancreatic parenchyma >3 cm in size or >30% of the pancreas.[1] Extrapancreatic necrosis can also be present, and is associated with adverse outcomes such as organ failure.[16] Pancreatic and extrapancreatic necrosis can be sterile or infected. The presence of infection does not necessarily increase the risk of subsequent organ failure.
FEEDING
In patients with mild pancreatitis, oral feeding with a low‐fat solid diet can be initiated when nausea, vomiting, and pain have resolved.[1] A randomized controlled trial demonstrated that patients who receive oral feeding earlier in the course of their stay have a shorter length of stay and fewer complications.[17] In patients with evolving AP who unable to tolerate oral feeding, enteral tube feeding either via nasogastric or nasojejunal routes should be initiated to support the intestinal biome and prevent bacterial translocation from the gut to the pancreas. Nasogastric feeding appears to be as safe as nasojejunal feeding.[18] Parenteral nutrition should only be used as a second‐line therapy if adequate caloric requirements cannot be maintained via an enteral route given the increased rate of infections and mortality when compared with nasoenteric feeding.[19] The most recent study on when to start enteric feeding in patients at high risk for complications demonstrates no benefit from starting nasoenteric feeding within the first 24 hours of admission compared to starting an oral diet at 72 hours.[20]
INTRA‐ABDOMINAL COMPARTMENT SYNDROME
A sometimes overlooked consequence of aggressive fluid resuscitation can be the development of intra‐abdominal compartment syndrome, which is defined as new organ dysfunction with concomitant intra‐abdominal pressure measurements >20 mm Hg. Patients with an increasingly tense abdomen, oliguria, or increasing ventilator requirements should have intravesical pressures measured with a urinary catheter. Initial treatment consists of decreasing the fluid resuscitation rate along with supportive measures such as reducing ventilator tidal volume and placing nasogastric and rectal tubes; if not successful, surgical decompression is indicated.
SUBSPECIALIST INVOLVEMENT
The majority of mild AP cases can effectively be managed by hospitalists, and there is no evidence that subspecialist involvement improves important clinical outcomes in mild disease. The need for subspecialty input should be based on the need for a procedure such as ERCP or collaborative care if the patient develops more acute complications requiring ongoing critical care support or decisions centered on sampling of fluid collections and/or necrosectomy.
Case Management Strategy
The patient is transferred to the intensive care unit for closer monitoring of his hemodynamic and respiratory status. His LR is held at 250 mL/h and his BUN is checked every 8 hours. He undergoes serial abdominal exams and twice‐daily bladder pressure measurements to evaluate for intra‐abdominal compartment syndrome. Antibiotics continue to be held as there is no evidence of pancreatic or extrapancreatic infection. A nasogastric tube is placed and enteral feeding begun with a low‐fat formulation and advanced as tolerated. The gastroenterology service is consulted to assist in management.
Hospital Day 17
With optimal intensive care unit monitoring of fluid status, early initiation of enteral feeding, and management of pain, the patient's vital signs have normalized and is he is transferred to the medical ward and is tolerating a clear liquid diet. In the next 48 hours, he becomes febrile. Urinalysis is unremarkable and blood cultures show no growth. Given continued fevers without a clear source, a CT scan of the abdomen is obtained. It demonstrates formation of a necrotic collection.
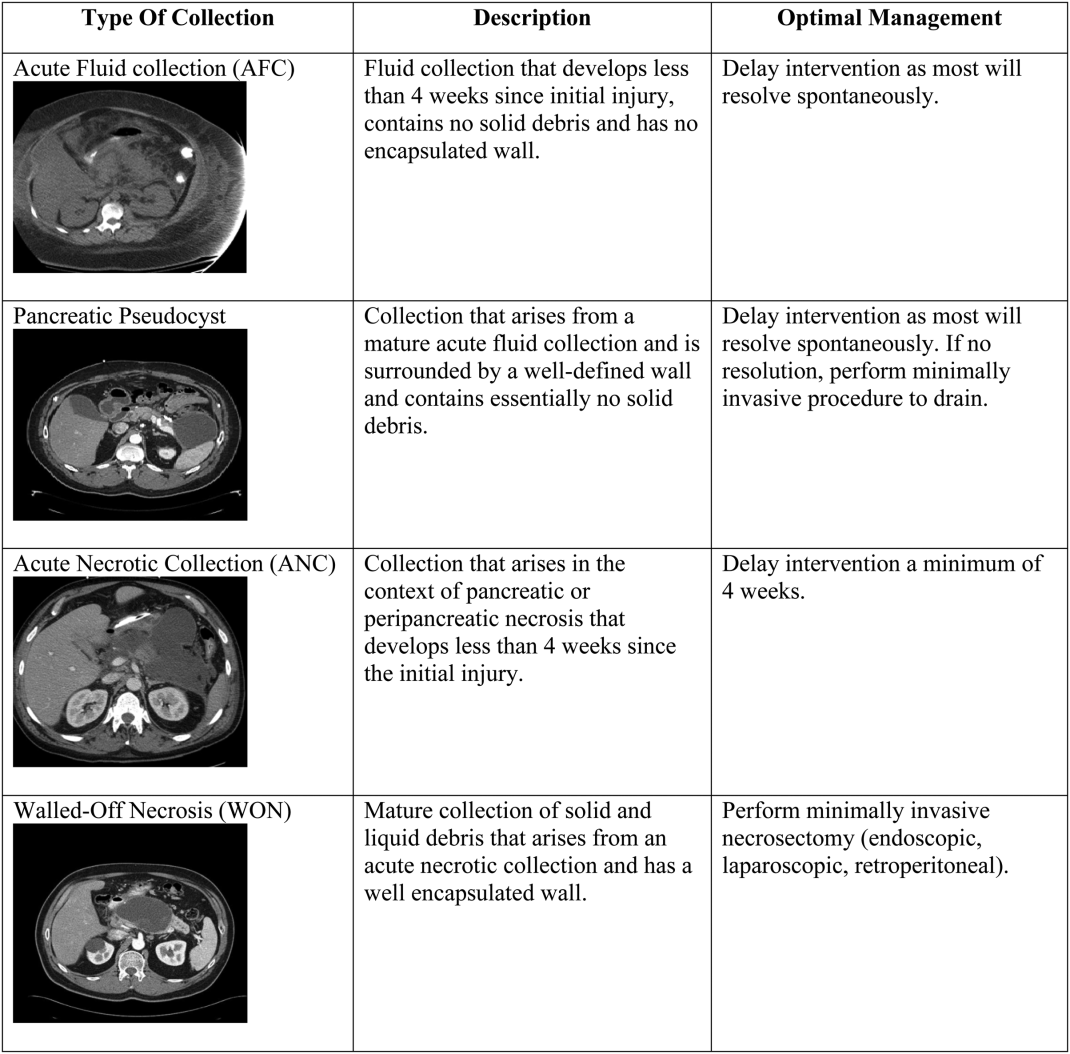
DEFINITION AND MANAGEMENT OF PANCREATIC FLUID COLLECTIONS
There are 4 main types of pancreatic collections, which include acute fluid collections, acute necrotic collections, pseudocysts, and walled off necrosis (Figure 1).[3] Acute fluid collections (AFC) develop less than 4 weeks after an episode of interstitial pancreatitis. They are found in the pancreatic parenchyma or peripancreatic tissue and usually resolve without requiring intervention. When a fluid collection develops in the context of pancreatic necrosis, it is known as an acute necrotic collection. If an AFC does not resolve in 4 weeks and develops an encapsulated wall that lacks solid debris, it is characterized as a pseudocyst. Pseudocysts are usually extrapancreatic, but occasionally can be intrapancreatic as a result of a disrupted pancreatic duct. Walled off necrosis (WON) occurs after 4 weeks, contains solid debris, and occurs only in the context of necrotizing pancreatitis.
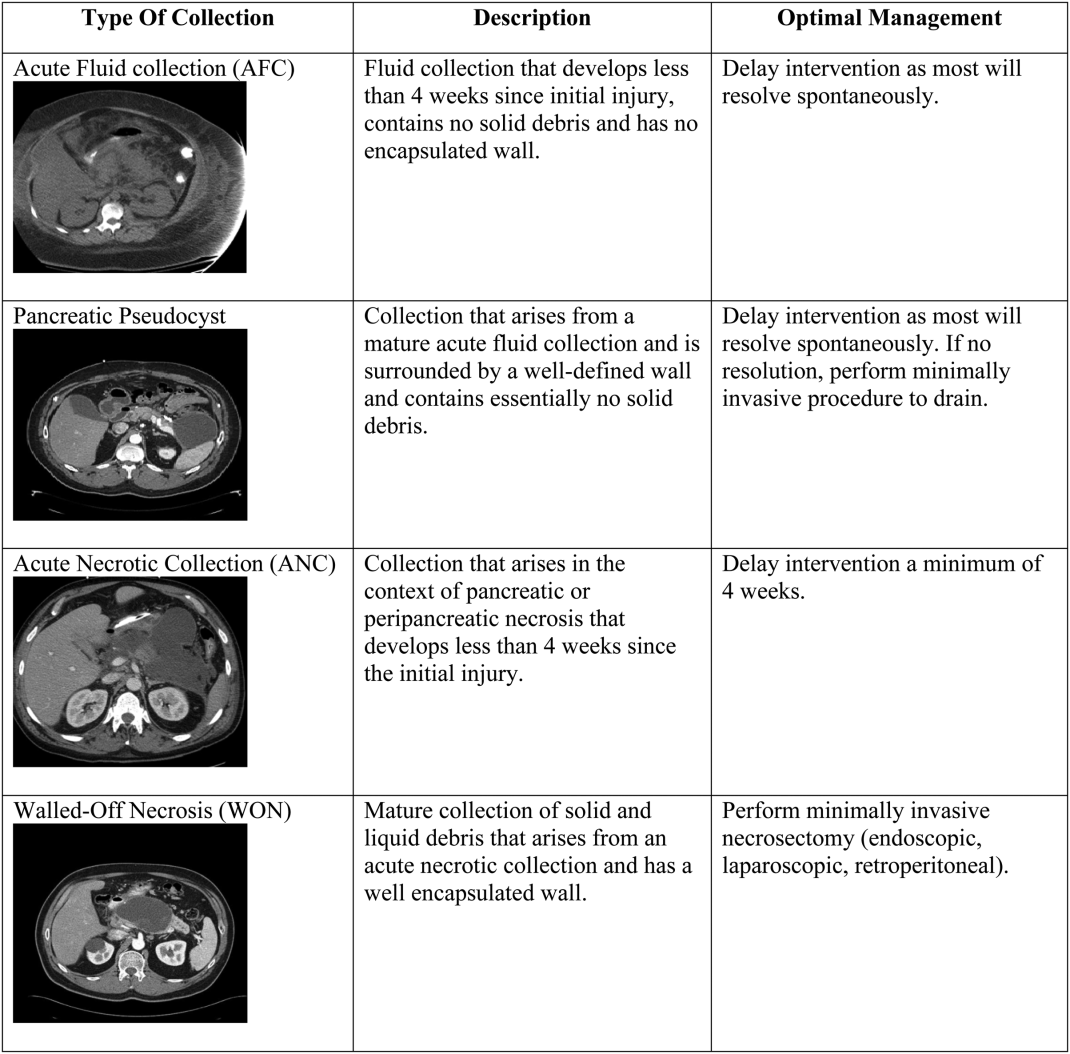
The most important strategy for the hospitalist in managing AFC is to delay intervention as long as possible.[14, 21, 22] This decision generally requires multidisciplinary input (for example with gastroenterology, surgical, and infectious diseases consultative services), as any intervention performed prematurely may lead to significant morbidity and occasional mortality. The vast majority of AFCs and pseudocysts will resolve spontaneously. In addition, most ANCs can be allowed to mature beyond the time of the initial hospitalization and can be managed as an outpatient if/when they proceed to WON.
INFECTED PANCREATIC NECROSIS
In the last decade, the paradigm for managing infected pancreatic necrosis has shifted dramatically. It is no longer necessary to sample the pancreas to make the diagnosis of infected pancreatic necrosis. In most cases, a careful history, clinical examination, and imaging should be able to make the diagnosis.[1, 23] Historically, open necrosectomy/debridement was the standard for the treatment of infected necrosis, but due to increased mortality, this practice has been abandoned. Currently, it is recommended that in stable patients, a course of pancreas‐penetrating antibiotics (such as meropenem) can be tried to allow for better organization of the inflammatory reaction. Subsequently, if the patient remains ill and the infected necrosis has not resolved, minimally invasive necrosectomy, via a variety of techniques such as endoscopy, laparoscopy, or a video‐assisted retroperitoneal approach, should be employed before considering any open surgery. Minimally invasive techniques have the advantages of not only being as successful as open surgery, but also have lower complication rates.[24]
Case Management Strategy
In the setting of fevers and a necrotic fluid collection, the patient is empirically started on meropenem. The pancreatic fluid collection has caused pressure on the stomach, which has led to nausea and vomiting, but he has tolerated continued enteral feeding via a nasogastric tube.
Hospital Day 29
The patient undergoes successful direct endoscopic necrosectomy on hospital day 29 after a repeat CT scan demonstrates complete maturation of the walled off pancreatic necrosis. Following the procedure, his nausea resolves and he is able to tolerate transition to a low‐fat diet.
OTHER COMPLICATIONS
Prior to discharge, it is important to consider other possible complications that may have arisen. New onset glucose intolerance or diabetes, thrombosis of the portal vasculature, and/or splenic aneurysm development can all occur several weeks into the hospitalization. The hospitalist must be aware of clinical clues such as new‐onset ascites due to thrombosis of the superior mesenteric vein.
PREVENTING READMISSIONS
Patients presenting with acute pancreatitis have a 30‐day readmission rate around 20%.[25] Prognostic factors that reduce the risk of readmission include patient tolerating a solid diet, absence of other gastrointestinal symptoms (nausea, vomiting, or diarrhea), and well‐controlled pain. The presence of pancreatic necrosis and the necessity for antimicrobial therapy increase the risk of readmission.[25] In terms of modifiable risk factors, risk of readmission has been correlated with alcohol as etiology of index hospitalization and tobacco abuse. Careful attention to addressing alcohol use and abuse as well as the challenging transition from acute to chronic pain control for patients with chronic pancreatitis is essential, as it is often recurrent pain and possibly not pancreatitis per se that may be the most common reason for hospital readmission. Finally, cholecystectomy for biliary AP should be performed prior to discharge; if this is not feasible, short‐interval outpatient follow‐up for surgery is imperative.
Management Strategy
The patient undergoes an uneventful laparoscopic cholecystectomy on hospital day 35. He is discharged to a skilled nursing facility with physical and occupational rehabilitation services. He has follow‐up scheduled with the gastroenterology service in 2 weeks. His case highlights many of the potential complications of acute pancreatitis and the major updates to management of this common illness (Table 1).
Disclosure
Nothing to report.
- , , , et al. American college of gastroenterology guideline: management of acute pancreatitis. Am J Gastroenterol. 2013;108:1400–1415.
- , , . Acute pancreatitis. BMJ. 2014;349:g4859.
- , , , et al. Classification of acute pancreatitis‐2012: revision of Atlanta classification and definitions by international consensus. Gut. 2013;62:102–111.
- , . Clinical management of patients with acute pancreatitis. Gastroenterology. 2013;144:1272–1281.
- , , , et al. Acute pancreatitis and normoamylasemia. Not an uncommon combination. Ann Surg. 1989;2010:614–620.
- , , , et al. Acute pancreatitis with normal serum lipase: a case series. JOP. 2010;11:369–372.
- , , , et al. Body mass index and the risk and prognosis of acute pancreatitis: a meta‐analysis. Eur J Gastroenterol Hepatol. 2011;23(12):1136–1143.
- , , , et al. Alcohol consumption on pancreatic diseases. World J Gastroenterol. 2013;19(5):638–647.
- , , , et al. Drug‐induced pancreatitis. Curr Gastroenterol Rep. 2012;14:131–138.
- , . Pancreas divisum does not cause pancreatitis, but associates with CFTR mutations. Am J Gastroenterol. 2012;107:318–320.
- , , , et al. Association between early systemic inflammatory response, severity of multiorgan dysfunction and death in acute pancreatitis. Br J Surg. 2006;93:738–744.
- , . Practice guidelines in acute pancreatitis. Am J Gastroenterol. 2006;101(10):2379–2400.
- , , . Natural history following the first attack of acute pancreatitis. Am J Gastroenterol. 2012;107:1096–1103.
- Working Group IAP/APA Acute Pancreatitis Guidelines. IAP/APA Evidence‐based guidelines for the management of acute pancreatitis. Pancreatology. 2013;13:e1–e15.
- , , , et al. Interventions for necrotizing pancreatitis: summary of a multidisciplinary consensus conference. Pancreas. 2012;41(8):1176–1194.
- , , , et al. Extrapancreatic necrosis without pancreatic parenchymal necrosis: a separate entity in necrotising pancreatitis? Gut. 2013;62(10):1475–1480.
- , , . A randomized controlled trial of enteral versus parenteral feeding in patients with predicted severe acute pancreatitis shows a significant reduction in mortality and in infected pancreatic complications with total enteral nutrition. Dig Surg. 2006;23:336–345.
- , , , et al. Evaluation of early enteral feeding through nasogastric and nasojejunal tube in severe acute pancreatitis. A non‐inferiority randomized controlled trial. Pancreas. 2012;41:153–159.
- , , , . Enteral versus parenteral nutrition for acute pancreatitis. Cochrane Database Syst Rev. 2010;1:CD002837.
- , , , et al. Early versus on‐demand nasoenteric tube feeding in acute pancreatitis. N Engl J Med. 2014;371(21):1983–1993.
- , , , et al. A conservative and minimally invasive approach to necrotizing pancreatitis improves outcome. Gastroenterology. 2011;141:1254–1263.
- , , , et al. Endoscopic necrosectomy in necrotizing pancreatitis: indication is the key. Gut. 2010;59:1587.
- , , . Management of acute pancreatitis. Expert Rev Gastroenterol Hepatol. 2014;8(6):1–8.
- , . Evidence‐based management of acute pancreatitis. Curr Treat Options Gastroenterol. 2014;9(2):175–180.
- , , , et al. A scoring system to predict readmission of patients with acute pancreatitis to the hospital within thirty days of discharge. Clin Gastroenterol Hepatol. 2011;9(2):175–180.
A 55‐year‐old man presents with colicky right upper quadrant pain radiating to his back for 12 hours. He does not use ethanol and has no familial or personal history of pancreatic disease. Pertinent laboratory values include: white blood cell count 23.6 103/L; hemoglobin 16.2 g/dL; blood urea nitrogen (BUN) 52 mg/dL; aspartate aminotransferase 110 U/L; alanine aminotransferase 272 U/L; alkaline phosphatase 432 U/L; total bilirubin 4.3 mg/dL; amylase 2230 U/L; lipase 1623 U/L. He is afebrile, normotensive, and not hypoxic, but his respiratory rate is 30. He has voluntary guarding with palpation of the abdomen, decreased bowel sounds, and decreased breath sounds at the left lung base. A transabdominal ultrasound of the right upper quadrant reveals cholelithiaisis without choledocholithiasis. There is mild peripancreatic stranding and the head is slightly edematous.
NATURAL HISTORY
Acute pancreatitis (AP) is a common cause for emergency room presentation, resulting in over 280,000 hospital admissions in the United States at a cost of nearly $3 billion dollars annually.[1] In its mildest form it may require a 2‐ to 5‐day hospital stay and an uncomplicated discharge. In more severe cases, such as in the setting of pancreatic necrosis and/or the development of organ failure, hospitalization can feature a much longer and complicated hospital course.[2]
|
| AP is now classified as mild, moderately acute, or severe based on the presence of local complications and/or persistent organ failure. |
| Lactated Ringer's solution should be used in all patients as the resuscitative fluid in AP |
| Aggressive fluid resuscitation is critical (defined as 250500 mL/h), especially in the first 24 hours of admission. |
| Enteric feeding should be attempted within the first 72 hours of admission and can be given orally with a low‐fat diet. |
| Antibiotics should not be used unless there is documented infection; prophylactic antibiotics to treat necrotizing AP are not beneficial. |
| New definitions of pancreatic fluid collections determine optimal therapy. |
| Medical therapy for infected pancreatic necrosis should be attempted prior to necrosectomy. |
| Alternatives to open necrosectomy, such as endoscopic or retroperitoneal debridement, are preferred in cases of unstable infected pancreatic necrosis. |
DIAGNOSTIC CRITERIA AND CLASSIFICATION
AP is diagnosed by the patient having 2 out of the following 3 criteria: (1) classic clinical symptoms with abdominal pain consistent with AP (2) serum amylase and/or lipase greater than 3 times the upper limit of normal, and/or (3) characteristic findings from abdominal imaging.[3] It is important for the hospitalist to recognize that patients can have AP with normal serum amylase and/or lipase levels, as long as their clinical symptoms and imaging exam are consistent with the disease.[4] It is also important to recognize that amylase and/or lipase elevation is not 100% specific for pancreatitis; alternate conditions that elevate amylase levels include renal insufficiency, intestinal ischemia and obstruction, macroamylasemia, and multiple medications, whereas lipase elevations can be seen in spontaneous bacterial peritonitis, intestinal ischemia, and esophagitis.[5]
AP is classified as either mild (absence of organ failure or local complications), moderate (local complications and/or transient organ failure 48 hours) or severe (persistent organ failure >48 hours).[3] Organ failure is defined by the modified Marshall score, and local complications include pancreatic fluid collections, pancreatic and peripancreatic necrosis, and vascular thrombosis (Table 2).[6]
| Organ System Score | 0 | 1 | 2 | 3 | 4 |
|---|---|---|---|---|---|
| |||||
| Respiratory (PaO2/FiO2) | >400 | 301400 | 201300 | 101200 | 101 |
| Renal serum creatinine (mg/dL) | 1.4 | 1.41.8 | 1.93.6 | 3.74.9 | >4.9 |
| Cardiovascular systolic blood pressure (mm Hg) | >90 | 90, fluid responsive | 90, not fluid responsive | 90, pH 7.3 | 90, pH 7.2 |
ETIOLOGY
Transiently obstructing gallstones, thought to account for about 50% of cases, are the most common cause of AP. The rising prevalence of obesity, which is a known risk factor for AP due to the corresponding increase in the frequency of gallstones, suggests that this will continue to be the leading cause going forward.[7] Alcohol use is associated with both acute and chronic pancreatitis; however, the extent to which it is a primary cause of AP is uncertain.[8] Trauma, medications, hypercalcemia, and hypertriglyceridemia must also be considered; however, they are much less common. AP from endoscopic retrograde cholangiopancreatography (ERCP) occurs following 5% of procedures and from endoscopic ultrasound (EUS) fine‐needle aspiration following 1%. Although several medications are clearly associated with AP, many that were previously invoked seem less likely.[9] Immunoglobulin G (IgG) 4related systemic disease, although rare, is becoming more recognized and should be considered when the more common etiologies are ruled out. Finally, it is controversial whether anatomic findings such as pancreatic divisum and functional disorders such as sphincter of Oddi dysfunction cause AP.[10]
Identifying the cause of an acute episode remains important, as subsequent treatment strategies can be tailored to help prevent recurrence. A thorough personal history, including prior gallbladder disease, alcohol use, and medications is strongly recommended. Basic laboratory studies including liver function tests, serum calcium and triglycerides, as well as a right upper quadrant ultrasound are indicated in all patients presenting with AP.[1] Idiopathic AP is not uncommon. Given the increasing awareness of genetic factors, potential role of advanced endoscopy, and higher risk of recurrence in this group, patients with idiopathic AP should be referred to specialized centers of expertise.[4]
PROGNOSTICATION
Most cases of AP are mild and do not require prolonged hospitalization; however, because 5% of hospitalized patients will die from this disease, prognostic criteria are needed to determine high‐risk cases.[11] Multiple systems have been developed (Bedside Index for Severity in Acute Pancreatitis, Ranson's, Acute Physiology and Chronic Health Evaluation II, Computed Tomography Severity Index), but all have had difficulty achieving accuracy in a user‐friendly tool; because of this, hospitalists should instead focus on the individual laboratory parameters that correlate with pathophysiologic derangement. Elevations in BUN and hematocrit indicate hypovolemia, leukocytosis, and fluid sequestration are indicators of the inflammatory cascade. Creatinine, elevated liver tests, and hypoxia are indicators of organ damage. Low calcium is reflective of fat necrosis saponification (endorgan damage) and also an indicator of hypovolemia. Essentially, the prediction of severity depends on identifying indications of endorgan damage in a timely manner and can be performed through a combination of age, known comorbidities, physical exam, and basic laboratory testing.[12]
ADDITIONAL INITIAL IMAGING
Although sensitive and specific for AP, routine computed tomography (CT) imaging for all patients presenting with suspected AP is not indicated. The diagnosis is often clear on a clinical and lab basis alone, and most patients with AP will improve within 48 hours.[13] CT or magnetic resonance imaging (MRI) can be considered for patients with an unclear diagnosis and indeterminate ultrasound or in those who are not improving within the first 48 to72 hours after presentation. This additional imaging can help make an alternative diagnosis or detect an early complication such as pancreatic necrosis. CT is preferred; however, MRI may be utilized if there is a high suspicion for biliary stones that were not seen on ultrasound or when CT is indicated but impaired renal function precludes its use.[4] In patients presenting with recurrent idiopathic AP, EUS is recommended to evaluate for an occult malignancy or microlithiasis.[14]
INITIAL CLINICAL MANAGEMENT
Without evidence of either (1) ascending cholangitis or (2) proven choledocholithiasis with clinical decompensation and worsening liver tests, ERCP should not be performed and management should be focused on supportive care, pain control, and monitoring prognostic information regarding severity. The initial management of AP should include fluid replacement with lactated Ringer's (LR) solution at 5‐10 mL/kg/h to achieve noninvasive parameters of a heart rate 120, mean arterial pressure 65 to 85 mm Hg, and urine output >0.5 to 1 mL/kg/h. LR decreases the incidence of the systemic inflammatory response syndrome (SIRS) by 80% compared with normal saline.[4, 15] Early and sufficient fluid replacement is associated with decreased rates of SIRS and organ failure, whereas under‐resuscitation has been associated with necrosis and increased mortality. In the first 48 to 72 hours of admission, frequent assessment of hemoglobin (HgB) and BUN, as well as urine output measurements, should be obtained to make sure fluid resuscitation is adequate.[4] Intravenous fluid replacement should continue in the hospital until the patient can adequately maintain appropriate fluid intake orally. Prophylactic antimicrobial therapy is not indicated in initial cases of AP, unless there are clear signs of an underlying infection. Pain control is essential, and efforts at reintroducing oral feeding should be initiated once the pain is decreasing. There are no randomized trials that have identified an optimal narcotic‐based pain regimen. On a daily basis, a complete blood count, renal function, and liver function should be measured. There is no reason to continue measuring serum amylase or lipase, as it may not be elevated in some instances in AP, and its fluctuation is not indicative of a change in clinical status.
Case Management Strategy
The patient has mild AP based on lack of organ failure and local complications and is admitted to the regular medical floor. The etiology appears to be due to cholelithiasis, but the patient does not have cholangitis, so ERCP was not considered, and antibiotics were not started. Aggressive fluid resuscitation with lactated Ringer's is started at a rate of 350 mL/h, and BUN and HgB are monitored every 8 hours to make sure that these levels are decreasing. The patient is placed on a low‐fat diet and encouraged to eat as tolerated. Further imaging is not ordered at this time.
Hospital Day 3
The patient's liver tests have normalized, but the BUN continues to rise (82 mg/dL) despite aggressive fluid resuscitation with LR. He remains afebrile and normotensive, but is now hypoxic and requiring nasal cannula oxygen at 4 L/min to maintain his oxygen saturation above 90%. His abdominal pain is controlled with intravenous opiates, but he is not hungry or able to eat. With these changes in his clinical course, a CT scan is performed, which demonstrates acute peripancreatic necrosis centered on the head of the pancreas.
PERSISTENT ORGAN FAILURE AND PANCREATIC NECROSIS
Generally, patients with severe AP (persistent organ failure >48 hours following admission) should be followed in the intensive care unit for effective monitoring and support.
Pancreatic necrosis is defined as a diffuse or focal area of nonviable pancreatic parenchyma >3 cm in size or >30% of the pancreas.[1] Extrapancreatic necrosis can also be present, and is associated with adverse outcomes such as organ failure.[16] Pancreatic and extrapancreatic necrosis can be sterile or infected. The presence of infection does not necessarily increase the risk of subsequent organ failure.
FEEDING
In patients with mild pancreatitis, oral feeding with a low‐fat solid diet can be initiated when nausea, vomiting, and pain have resolved.[1] A randomized controlled trial demonstrated that patients who receive oral feeding earlier in the course of their stay have a shorter length of stay and fewer complications.[17] In patients with evolving AP who unable to tolerate oral feeding, enteral tube feeding either via nasogastric or nasojejunal routes should be initiated to support the intestinal biome and prevent bacterial translocation from the gut to the pancreas. Nasogastric feeding appears to be as safe as nasojejunal feeding.[18] Parenteral nutrition should only be used as a second‐line therapy if adequate caloric requirements cannot be maintained via an enteral route given the increased rate of infections and mortality when compared with nasoenteric feeding.[19] The most recent study on when to start enteric feeding in patients at high risk for complications demonstrates no benefit from starting nasoenteric feeding within the first 24 hours of admission compared to starting an oral diet at 72 hours.[20]
INTRA‐ABDOMINAL COMPARTMENT SYNDROME
A sometimes overlooked consequence of aggressive fluid resuscitation can be the development of intra‐abdominal compartment syndrome, which is defined as new organ dysfunction with concomitant intra‐abdominal pressure measurements >20 mm Hg. Patients with an increasingly tense abdomen, oliguria, or increasing ventilator requirements should have intravesical pressures measured with a urinary catheter. Initial treatment consists of decreasing the fluid resuscitation rate along with supportive measures such as reducing ventilator tidal volume and placing nasogastric and rectal tubes; if not successful, surgical decompression is indicated.
SUBSPECIALIST INVOLVEMENT
The majority of mild AP cases can effectively be managed by hospitalists, and there is no evidence that subspecialist involvement improves important clinical outcomes in mild disease. The need for subspecialty input should be based on the need for a procedure such as ERCP or collaborative care if the patient develops more acute complications requiring ongoing critical care support or decisions centered on sampling of fluid collections and/or necrosectomy.
Case Management Strategy
The patient is transferred to the intensive care unit for closer monitoring of his hemodynamic and respiratory status. His LR is held at 250 mL/h and his BUN is checked every 8 hours. He undergoes serial abdominal exams and twice‐daily bladder pressure measurements to evaluate for intra‐abdominal compartment syndrome. Antibiotics continue to be held as there is no evidence of pancreatic or extrapancreatic infection. A nasogastric tube is placed and enteral feeding begun with a low‐fat formulation and advanced as tolerated. The gastroenterology service is consulted to assist in management.
Hospital Day 17
With optimal intensive care unit monitoring of fluid status, early initiation of enteral feeding, and management of pain, the patient's vital signs have normalized and is he is transferred to the medical ward and is tolerating a clear liquid diet. In the next 48 hours, he becomes febrile. Urinalysis is unremarkable and blood cultures show no growth. Given continued fevers without a clear source, a CT scan of the abdomen is obtained. It demonstrates formation of a necrotic collection.
DEFINITION AND MANAGEMENT OF PANCREATIC FLUID COLLECTIONS
There are 4 main types of pancreatic collections, which include acute fluid collections, acute necrotic collections, pseudocysts, and walled off necrosis (Figure 1).[3] Acute fluid collections (AFC) develop less than 4 weeks after an episode of interstitial pancreatitis. They are found in the pancreatic parenchyma or peripancreatic tissue and usually resolve without requiring intervention. When a fluid collection develops in the context of pancreatic necrosis, it is known as an acute necrotic collection. If an AFC does not resolve in 4 weeks and develops an encapsulated wall that lacks solid debris, it is characterized as a pseudocyst. Pseudocysts are usually extrapancreatic, but occasionally can be intrapancreatic as a result of a disrupted pancreatic duct. Walled off necrosis (WON) occurs after 4 weeks, contains solid debris, and occurs only in the context of necrotizing pancreatitis.
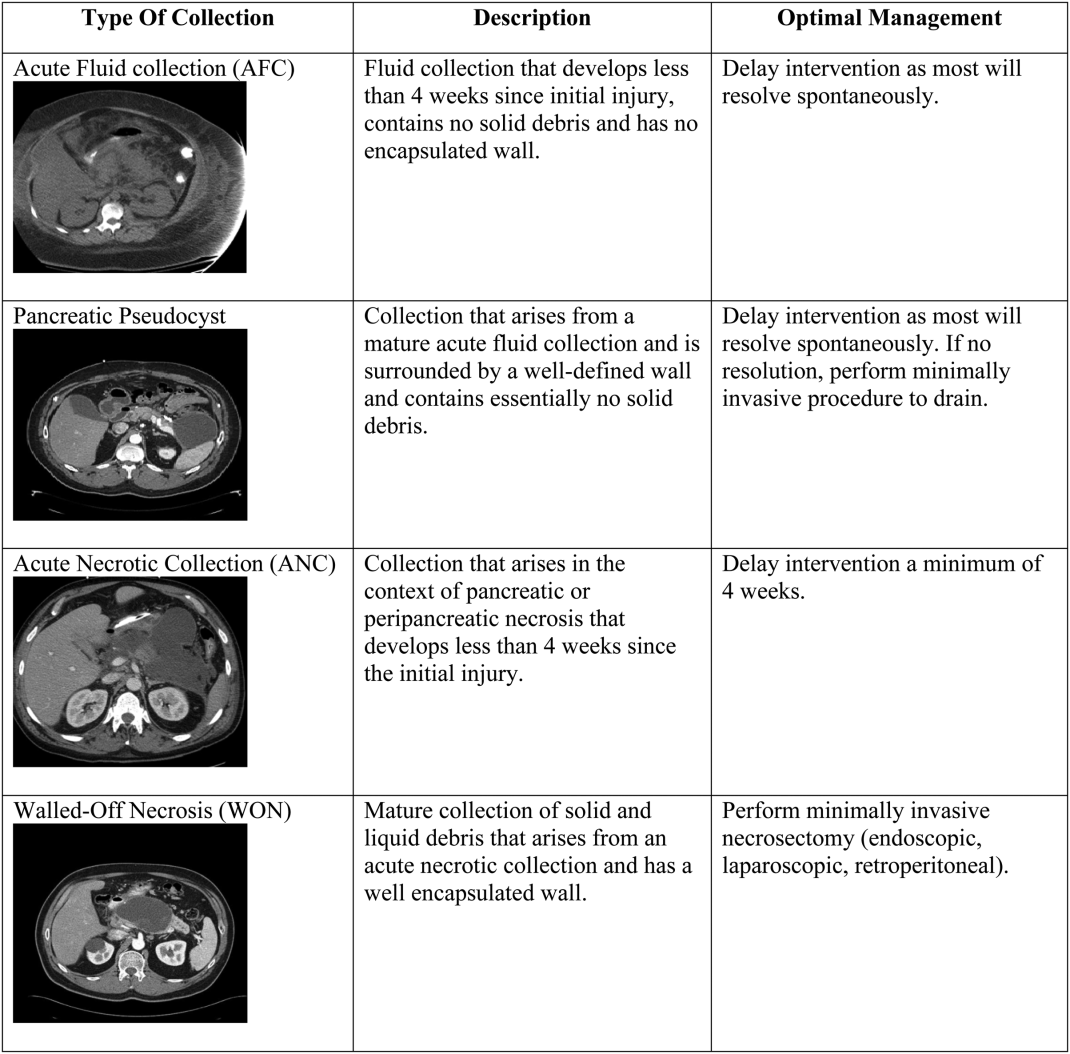
The most important strategy for the hospitalist in managing AFC is to delay intervention as long as possible.[14, 21, 22] This decision generally requires multidisciplinary input (for example with gastroenterology, surgical, and infectious diseases consultative services), as any intervention performed prematurely may lead to significant morbidity and occasional mortality. The vast majority of AFCs and pseudocysts will resolve spontaneously. In addition, most ANCs can be allowed to mature beyond the time of the initial hospitalization and can be managed as an outpatient if/when they proceed to WON.
INFECTED PANCREATIC NECROSIS
In the last decade, the paradigm for managing infected pancreatic necrosis has shifted dramatically. It is no longer necessary to sample the pancreas to make the diagnosis of infected pancreatic necrosis. In most cases, a careful history, clinical examination, and imaging should be able to make the diagnosis.[1, 23] Historically, open necrosectomy/debridement was the standard for the treatment of infected necrosis, but due to increased mortality, this practice has been abandoned. Currently, it is recommended that in stable patients, a course of pancreas‐penetrating antibiotics (such as meropenem) can be tried to allow for better organization of the inflammatory reaction. Subsequently, if the patient remains ill and the infected necrosis has not resolved, minimally invasive necrosectomy, via a variety of techniques such as endoscopy, laparoscopy, or a video‐assisted retroperitoneal approach, should be employed before considering any open surgery. Minimally invasive techniques have the advantages of not only being as successful as open surgery, but also have lower complication rates.[24]
Case Management Strategy
In the setting of fevers and a necrotic fluid collection, the patient is empirically started on meropenem. The pancreatic fluid collection has caused pressure on the stomach, which has led to nausea and vomiting, but he has tolerated continued enteral feeding via a nasogastric tube.
Hospital Day 29
The patient undergoes successful direct endoscopic necrosectomy on hospital day 29 after a repeat CT scan demonstrates complete maturation of the walled off pancreatic necrosis. Following the procedure, his nausea resolves and he is able to tolerate transition to a low‐fat diet.
OTHER COMPLICATIONS
Prior to discharge, it is important to consider other possible complications that may have arisen. New onset glucose intolerance or diabetes, thrombosis of the portal vasculature, and/or splenic aneurysm development can all occur several weeks into the hospitalization. The hospitalist must be aware of clinical clues such as new‐onset ascites due to thrombosis of the superior mesenteric vein.
PREVENTING READMISSIONS
Patients presenting with acute pancreatitis have a 30‐day readmission rate around 20%.[25] Prognostic factors that reduce the risk of readmission include patient tolerating a solid diet, absence of other gastrointestinal symptoms (nausea, vomiting, or diarrhea), and well‐controlled pain. The presence of pancreatic necrosis and the necessity for antimicrobial therapy increase the risk of readmission.[25] In terms of modifiable risk factors, risk of readmission has been correlated with alcohol as etiology of index hospitalization and tobacco abuse. Careful attention to addressing alcohol use and abuse as well as the challenging transition from acute to chronic pain control for patients with chronic pancreatitis is essential, as it is often recurrent pain and possibly not pancreatitis per se that may be the most common reason for hospital readmission. Finally, cholecystectomy for biliary AP should be performed prior to discharge; if this is not feasible, short‐interval outpatient follow‐up for surgery is imperative.
Management Strategy
The patient undergoes an uneventful laparoscopic cholecystectomy on hospital day 35. He is discharged to a skilled nursing facility with physical and occupational rehabilitation services. He has follow‐up scheduled with the gastroenterology service in 2 weeks. His case highlights many of the potential complications of acute pancreatitis and the major updates to management of this common illness (Table 1).
Disclosure
Nothing to report.
A 55‐year‐old man presents with colicky right upper quadrant pain radiating to his back for 12 hours. He does not use ethanol and has no familial or personal history of pancreatic disease. Pertinent laboratory values include: white blood cell count 23.6 103/L; hemoglobin 16.2 g/dL; blood urea nitrogen (BUN) 52 mg/dL; aspartate aminotransferase 110 U/L; alanine aminotransferase 272 U/L; alkaline phosphatase 432 U/L; total bilirubin 4.3 mg/dL; amylase 2230 U/L; lipase 1623 U/L. He is afebrile, normotensive, and not hypoxic, but his respiratory rate is 30. He has voluntary guarding with palpation of the abdomen, decreased bowel sounds, and decreased breath sounds at the left lung base. A transabdominal ultrasound of the right upper quadrant reveals cholelithiaisis without choledocholithiasis. There is mild peripancreatic stranding and the head is slightly edematous.
NATURAL HISTORY
Acute pancreatitis (AP) is a common cause for emergency room presentation, resulting in over 280,000 hospital admissions in the United States at a cost of nearly $3 billion dollars annually.[1] In its mildest form it may require a 2‐ to 5‐day hospital stay and an uncomplicated discharge. In more severe cases, such as in the setting of pancreatic necrosis and/or the development of organ failure, hospitalization can feature a much longer and complicated hospital course.[2]
|
| AP is now classified as mild, moderately acute, or severe based on the presence of local complications and/or persistent organ failure. |
| Lactated Ringer's solution should be used in all patients as the resuscitative fluid in AP |
| Aggressive fluid resuscitation is critical (defined as 250500 mL/h), especially in the first 24 hours of admission. |
| Enteric feeding should be attempted within the first 72 hours of admission and can be given orally with a low‐fat diet. |
| Antibiotics should not be used unless there is documented infection; prophylactic antibiotics to treat necrotizing AP are not beneficial. |
| New definitions of pancreatic fluid collections determine optimal therapy. |
| Medical therapy for infected pancreatic necrosis should be attempted prior to necrosectomy. |
| Alternatives to open necrosectomy, such as endoscopic or retroperitoneal debridement, are preferred in cases of unstable infected pancreatic necrosis. |
DIAGNOSTIC CRITERIA AND CLASSIFICATION
AP is diagnosed by the patient having 2 out of the following 3 criteria: (1) classic clinical symptoms with abdominal pain consistent with AP (2) serum amylase and/or lipase greater than 3 times the upper limit of normal, and/or (3) characteristic findings from abdominal imaging.[3] It is important for the hospitalist to recognize that patients can have AP with normal serum amylase and/or lipase levels, as long as their clinical symptoms and imaging exam are consistent with the disease.[4] It is also important to recognize that amylase and/or lipase elevation is not 100% specific for pancreatitis; alternate conditions that elevate amylase levels include renal insufficiency, intestinal ischemia and obstruction, macroamylasemia, and multiple medications, whereas lipase elevations can be seen in spontaneous bacterial peritonitis, intestinal ischemia, and esophagitis.[5]
AP is classified as either mild (absence of organ failure or local complications), moderate (local complications and/or transient organ failure 48 hours) or severe (persistent organ failure >48 hours).[3] Organ failure is defined by the modified Marshall score, and local complications include pancreatic fluid collections, pancreatic and peripancreatic necrosis, and vascular thrombosis (Table 2).[6]
| Organ System Score | 0 | 1 | 2 | 3 | 4 |
|---|---|---|---|---|---|
| |||||
| Respiratory (PaO2/FiO2) | >400 | 301400 | 201300 | 101200 | 101 |
| Renal serum creatinine (mg/dL) | 1.4 | 1.41.8 | 1.93.6 | 3.74.9 | >4.9 |
| Cardiovascular systolic blood pressure (mm Hg) | >90 | 90, fluid responsive | 90, not fluid responsive | 90, pH 7.3 | 90, pH 7.2 |
ETIOLOGY
Transiently obstructing gallstones, thought to account for about 50% of cases, are the most common cause of AP. The rising prevalence of obesity, which is a known risk factor for AP due to the corresponding increase in the frequency of gallstones, suggests that this will continue to be the leading cause going forward.[7] Alcohol use is associated with both acute and chronic pancreatitis; however, the extent to which it is a primary cause of AP is uncertain.[8] Trauma, medications, hypercalcemia, and hypertriglyceridemia must also be considered; however, they are much less common. AP from endoscopic retrograde cholangiopancreatography (ERCP) occurs following 5% of procedures and from endoscopic ultrasound (EUS) fine‐needle aspiration following 1%. Although several medications are clearly associated with AP, many that were previously invoked seem less likely.[9] Immunoglobulin G (IgG) 4related systemic disease, although rare, is becoming more recognized and should be considered when the more common etiologies are ruled out. Finally, it is controversial whether anatomic findings such as pancreatic divisum and functional disorders such as sphincter of Oddi dysfunction cause AP.[10]
Identifying the cause of an acute episode remains important, as subsequent treatment strategies can be tailored to help prevent recurrence. A thorough personal history, including prior gallbladder disease, alcohol use, and medications is strongly recommended. Basic laboratory studies including liver function tests, serum calcium and triglycerides, as well as a right upper quadrant ultrasound are indicated in all patients presenting with AP.[1] Idiopathic AP is not uncommon. Given the increasing awareness of genetic factors, potential role of advanced endoscopy, and higher risk of recurrence in this group, patients with idiopathic AP should be referred to specialized centers of expertise.[4]
PROGNOSTICATION
Most cases of AP are mild and do not require prolonged hospitalization; however, because 5% of hospitalized patients will die from this disease, prognostic criteria are needed to determine high‐risk cases.[11] Multiple systems have been developed (Bedside Index for Severity in Acute Pancreatitis, Ranson's, Acute Physiology and Chronic Health Evaluation II, Computed Tomography Severity Index), but all have had difficulty achieving accuracy in a user‐friendly tool; because of this, hospitalists should instead focus on the individual laboratory parameters that correlate with pathophysiologic derangement. Elevations in BUN and hematocrit indicate hypovolemia, leukocytosis, and fluid sequestration are indicators of the inflammatory cascade. Creatinine, elevated liver tests, and hypoxia are indicators of organ damage. Low calcium is reflective of fat necrosis saponification (endorgan damage) and also an indicator of hypovolemia. Essentially, the prediction of severity depends on identifying indications of endorgan damage in a timely manner and can be performed through a combination of age, known comorbidities, physical exam, and basic laboratory testing.[12]
ADDITIONAL INITIAL IMAGING
Although sensitive and specific for AP, routine computed tomography (CT) imaging for all patients presenting with suspected AP is not indicated. The diagnosis is often clear on a clinical and lab basis alone, and most patients with AP will improve within 48 hours.[13] CT or magnetic resonance imaging (MRI) can be considered for patients with an unclear diagnosis and indeterminate ultrasound or in those who are not improving within the first 48 to72 hours after presentation. This additional imaging can help make an alternative diagnosis or detect an early complication such as pancreatic necrosis. CT is preferred; however, MRI may be utilized if there is a high suspicion for biliary stones that were not seen on ultrasound or when CT is indicated but impaired renal function precludes its use.[4] In patients presenting with recurrent idiopathic AP, EUS is recommended to evaluate for an occult malignancy or microlithiasis.[14]
INITIAL CLINICAL MANAGEMENT
Without evidence of either (1) ascending cholangitis or (2) proven choledocholithiasis with clinical decompensation and worsening liver tests, ERCP should not be performed and management should be focused on supportive care, pain control, and monitoring prognostic information regarding severity. The initial management of AP should include fluid replacement with lactated Ringer's (LR) solution at 5‐10 mL/kg/h to achieve noninvasive parameters of a heart rate 120, mean arterial pressure 65 to 85 mm Hg, and urine output >0.5 to 1 mL/kg/h. LR decreases the incidence of the systemic inflammatory response syndrome (SIRS) by 80% compared with normal saline.[4, 15] Early and sufficient fluid replacement is associated with decreased rates of SIRS and organ failure, whereas under‐resuscitation has been associated with necrosis and increased mortality. In the first 48 to 72 hours of admission, frequent assessment of hemoglobin (HgB) and BUN, as well as urine output measurements, should be obtained to make sure fluid resuscitation is adequate.[4] Intravenous fluid replacement should continue in the hospital until the patient can adequately maintain appropriate fluid intake orally. Prophylactic antimicrobial therapy is not indicated in initial cases of AP, unless there are clear signs of an underlying infection. Pain control is essential, and efforts at reintroducing oral feeding should be initiated once the pain is decreasing. There are no randomized trials that have identified an optimal narcotic‐based pain regimen. On a daily basis, a complete blood count, renal function, and liver function should be measured. There is no reason to continue measuring serum amylase or lipase, as it may not be elevated in some instances in AP, and its fluctuation is not indicative of a change in clinical status.
Case Management Strategy
The patient has mild AP based on lack of organ failure and local complications and is admitted to the regular medical floor. The etiology appears to be due to cholelithiasis, but the patient does not have cholangitis, so ERCP was not considered, and antibiotics were not started. Aggressive fluid resuscitation with lactated Ringer's is started at a rate of 350 mL/h, and BUN and HgB are monitored every 8 hours to make sure that these levels are decreasing. The patient is placed on a low‐fat diet and encouraged to eat as tolerated. Further imaging is not ordered at this time.
Hospital Day 3
The patient's liver tests have normalized, but the BUN continues to rise (82 mg/dL) despite aggressive fluid resuscitation with LR. He remains afebrile and normotensive, but is now hypoxic and requiring nasal cannula oxygen at 4 L/min to maintain his oxygen saturation above 90%. His abdominal pain is controlled with intravenous opiates, but he is not hungry or able to eat. With these changes in his clinical course, a CT scan is performed, which demonstrates acute peripancreatic necrosis centered on the head of the pancreas.
PERSISTENT ORGAN FAILURE AND PANCREATIC NECROSIS
Generally, patients with severe AP (persistent organ failure >48 hours following admission) should be followed in the intensive care unit for effective monitoring and support.
Pancreatic necrosis is defined as a diffuse or focal area of nonviable pancreatic parenchyma >3 cm in size or >30% of the pancreas.[1] Extrapancreatic necrosis can also be present, and is associated with adverse outcomes such as organ failure.[16] Pancreatic and extrapancreatic necrosis can be sterile or infected. The presence of infection does not necessarily increase the risk of subsequent organ failure.
FEEDING
In patients with mild pancreatitis, oral feeding with a low‐fat solid diet can be initiated when nausea, vomiting, and pain have resolved.[1] A randomized controlled trial demonstrated that patients who receive oral feeding earlier in the course of their stay have a shorter length of stay and fewer complications.[17] In patients with evolving AP who unable to tolerate oral feeding, enteral tube feeding either via nasogastric or nasojejunal routes should be initiated to support the intestinal biome and prevent bacterial translocation from the gut to the pancreas. Nasogastric feeding appears to be as safe as nasojejunal feeding.[18] Parenteral nutrition should only be used as a second‐line therapy if adequate caloric requirements cannot be maintained via an enteral route given the increased rate of infections and mortality when compared with nasoenteric feeding.[19] The most recent study on when to start enteric feeding in patients at high risk for complications demonstrates no benefit from starting nasoenteric feeding within the first 24 hours of admission compared to starting an oral diet at 72 hours.[20]
INTRA‐ABDOMINAL COMPARTMENT SYNDROME
A sometimes overlooked consequence of aggressive fluid resuscitation can be the development of intra‐abdominal compartment syndrome, which is defined as new organ dysfunction with concomitant intra‐abdominal pressure measurements >20 mm Hg. Patients with an increasingly tense abdomen, oliguria, or increasing ventilator requirements should have intravesical pressures measured with a urinary catheter. Initial treatment consists of decreasing the fluid resuscitation rate along with supportive measures such as reducing ventilator tidal volume and placing nasogastric and rectal tubes; if not successful, surgical decompression is indicated.
SUBSPECIALIST INVOLVEMENT
The majority of mild AP cases can effectively be managed by hospitalists, and there is no evidence that subspecialist involvement improves important clinical outcomes in mild disease. The need for subspecialty input should be based on the need for a procedure such as ERCP or collaborative care if the patient develops more acute complications requiring ongoing critical care support or decisions centered on sampling of fluid collections and/or necrosectomy.
Case Management Strategy
The patient is transferred to the intensive care unit for closer monitoring of his hemodynamic and respiratory status. His LR is held at 250 mL/h and his BUN is checked every 8 hours. He undergoes serial abdominal exams and twice‐daily bladder pressure measurements to evaluate for intra‐abdominal compartment syndrome. Antibiotics continue to be held as there is no evidence of pancreatic or extrapancreatic infection. A nasogastric tube is placed and enteral feeding begun with a low‐fat formulation and advanced as tolerated. The gastroenterology service is consulted to assist in management.
Hospital Day 17
With optimal intensive care unit monitoring of fluid status, early initiation of enteral feeding, and management of pain, the patient's vital signs have normalized and is he is transferred to the medical ward and is tolerating a clear liquid diet. In the next 48 hours, he becomes febrile. Urinalysis is unremarkable and blood cultures show no growth. Given continued fevers without a clear source, a CT scan of the abdomen is obtained. It demonstrates formation of a necrotic collection.
DEFINITION AND MANAGEMENT OF PANCREATIC FLUID COLLECTIONS
There are 4 main types of pancreatic collections, which include acute fluid collections, acute necrotic collections, pseudocysts, and walled off necrosis (Figure 1).[3] Acute fluid collections (AFC) develop less than 4 weeks after an episode of interstitial pancreatitis. They are found in the pancreatic parenchyma or peripancreatic tissue and usually resolve without requiring intervention. When a fluid collection develops in the context of pancreatic necrosis, it is known as an acute necrotic collection. If an AFC does not resolve in 4 weeks and develops an encapsulated wall that lacks solid debris, it is characterized as a pseudocyst. Pseudocysts are usually extrapancreatic, but occasionally can be intrapancreatic as a result of a disrupted pancreatic duct. Walled off necrosis (WON) occurs after 4 weeks, contains solid debris, and occurs only in the context of necrotizing pancreatitis.
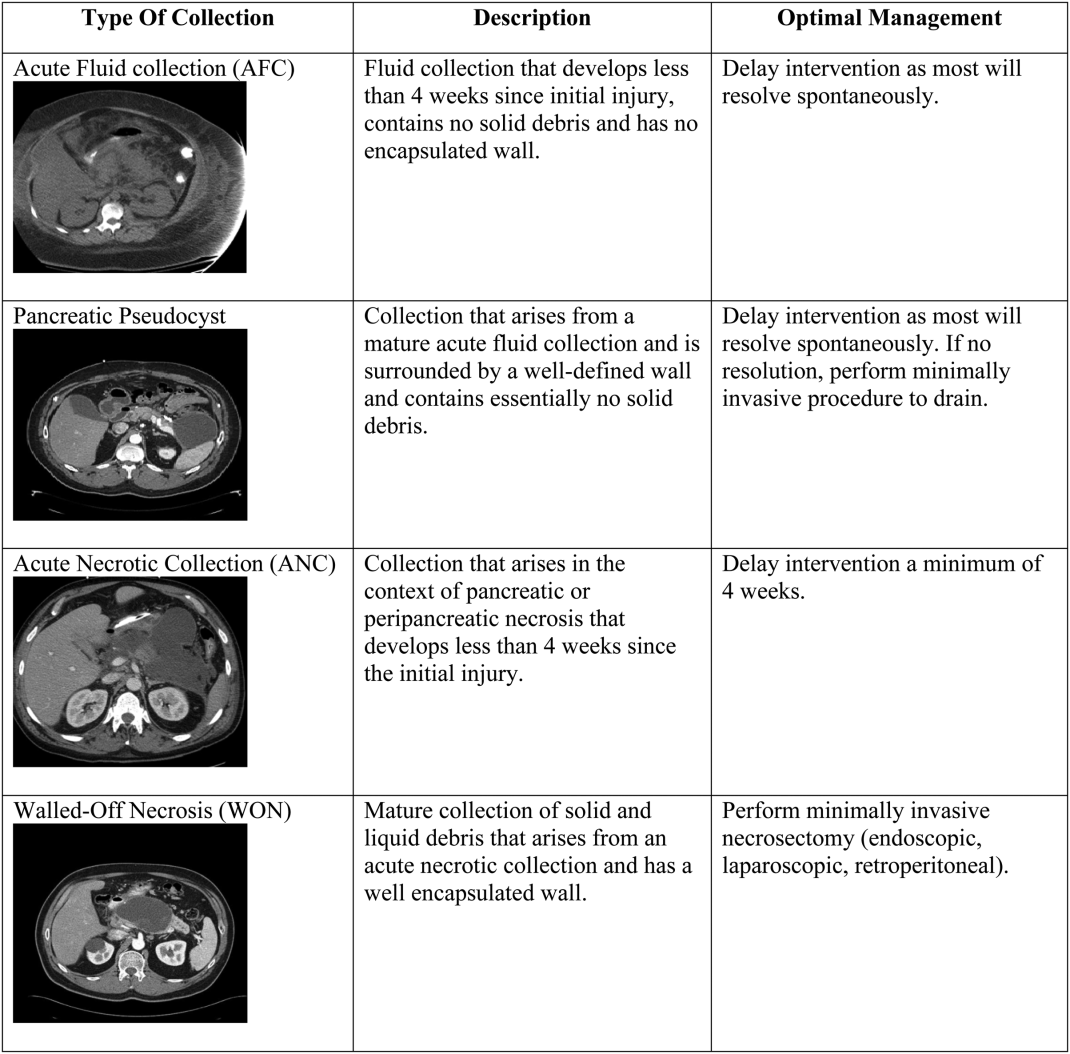
The most important strategy for the hospitalist in managing AFC is to delay intervention as long as possible.[14, 21, 22] This decision generally requires multidisciplinary input (for example with gastroenterology, surgical, and infectious diseases consultative services), as any intervention performed prematurely may lead to significant morbidity and occasional mortality. The vast majority of AFCs and pseudocysts will resolve spontaneously. In addition, most ANCs can be allowed to mature beyond the time of the initial hospitalization and can be managed as an outpatient if/when they proceed to WON.
INFECTED PANCREATIC NECROSIS
In the last decade, the paradigm for managing infected pancreatic necrosis has shifted dramatically. It is no longer necessary to sample the pancreas to make the diagnosis of infected pancreatic necrosis. In most cases, a careful history, clinical examination, and imaging should be able to make the diagnosis.[1, 23] Historically, open necrosectomy/debridement was the standard for the treatment of infected necrosis, but due to increased mortality, this practice has been abandoned. Currently, it is recommended that in stable patients, a course of pancreas‐penetrating antibiotics (such as meropenem) can be tried to allow for better organization of the inflammatory reaction. Subsequently, if the patient remains ill and the infected necrosis has not resolved, minimally invasive necrosectomy, via a variety of techniques such as endoscopy, laparoscopy, or a video‐assisted retroperitoneal approach, should be employed before considering any open surgery. Minimally invasive techniques have the advantages of not only being as successful as open surgery, but also have lower complication rates.[24]
Case Management Strategy
In the setting of fevers and a necrotic fluid collection, the patient is empirically started on meropenem. The pancreatic fluid collection has caused pressure on the stomach, which has led to nausea and vomiting, but he has tolerated continued enteral feeding via a nasogastric tube.
Hospital Day 29
The patient undergoes successful direct endoscopic necrosectomy on hospital day 29 after a repeat CT scan demonstrates complete maturation of the walled off pancreatic necrosis. Following the procedure, his nausea resolves and he is able to tolerate transition to a low‐fat diet.
OTHER COMPLICATIONS
Prior to discharge, it is important to consider other possible complications that may have arisen. New onset glucose intolerance or diabetes, thrombosis of the portal vasculature, and/or splenic aneurysm development can all occur several weeks into the hospitalization. The hospitalist must be aware of clinical clues such as new‐onset ascites due to thrombosis of the superior mesenteric vein.
PREVENTING READMISSIONS
Patients presenting with acute pancreatitis have a 30‐day readmission rate around 20%.[25] Prognostic factors that reduce the risk of readmission include patient tolerating a solid diet, absence of other gastrointestinal symptoms (nausea, vomiting, or diarrhea), and well‐controlled pain. The presence of pancreatic necrosis and the necessity for antimicrobial therapy increase the risk of readmission.[25] In terms of modifiable risk factors, risk of readmission has been correlated with alcohol as etiology of index hospitalization and tobacco abuse. Careful attention to addressing alcohol use and abuse as well as the challenging transition from acute to chronic pain control for patients with chronic pancreatitis is essential, as it is often recurrent pain and possibly not pancreatitis per se that may be the most common reason for hospital readmission. Finally, cholecystectomy for biliary AP should be performed prior to discharge; if this is not feasible, short‐interval outpatient follow‐up for surgery is imperative.
Management Strategy
The patient undergoes an uneventful laparoscopic cholecystectomy on hospital day 35. He is discharged to a skilled nursing facility with physical and occupational rehabilitation services. He has follow‐up scheduled with the gastroenterology service in 2 weeks. His case highlights many of the potential complications of acute pancreatitis and the major updates to management of this common illness (Table 1).
Disclosure
Nothing to report.
- , , , et al. American college of gastroenterology guideline: management of acute pancreatitis. Am J Gastroenterol. 2013;108:1400–1415.
- , , . Acute pancreatitis. BMJ. 2014;349:g4859.
- , , , et al. Classification of acute pancreatitis‐2012: revision of Atlanta classification and definitions by international consensus. Gut. 2013;62:102–111.
- , . Clinical management of patients with acute pancreatitis. Gastroenterology. 2013;144:1272–1281.
- , , , et al. Acute pancreatitis and normoamylasemia. Not an uncommon combination. Ann Surg. 1989;2010:614–620.
- , , , et al. Acute pancreatitis with normal serum lipase: a case series. JOP. 2010;11:369–372.
- , , , et al. Body mass index and the risk and prognosis of acute pancreatitis: a meta‐analysis. Eur J Gastroenterol Hepatol. 2011;23(12):1136–1143.
- , , , et al. Alcohol consumption on pancreatic diseases. World J Gastroenterol. 2013;19(5):638–647.
- , , , et al. Drug‐induced pancreatitis. Curr Gastroenterol Rep. 2012;14:131–138.
- , . Pancreas divisum does not cause pancreatitis, but associates with CFTR mutations. Am J Gastroenterol. 2012;107:318–320.
- , , , et al. Association between early systemic inflammatory response, severity of multiorgan dysfunction and death in acute pancreatitis. Br J Surg. 2006;93:738–744.
- , . Practice guidelines in acute pancreatitis. Am J Gastroenterol. 2006;101(10):2379–2400.
- , , . Natural history following the first attack of acute pancreatitis. Am J Gastroenterol. 2012;107:1096–1103.
- Working Group IAP/APA Acute Pancreatitis Guidelines. IAP/APA Evidence‐based guidelines for the management of acute pancreatitis. Pancreatology. 2013;13:e1–e15.
- , , , et al. Interventions for necrotizing pancreatitis: summary of a multidisciplinary consensus conference. Pancreas. 2012;41(8):1176–1194.
- , , , et al. Extrapancreatic necrosis without pancreatic parenchymal necrosis: a separate entity in necrotising pancreatitis? Gut. 2013;62(10):1475–1480.
- , , . A randomized controlled trial of enteral versus parenteral feeding in patients with predicted severe acute pancreatitis shows a significant reduction in mortality and in infected pancreatic complications with total enteral nutrition. Dig Surg. 2006;23:336–345.
- , , , et al. Evaluation of early enteral feeding through nasogastric and nasojejunal tube in severe acute pancreatitis. A non‐inferiority randomized controlled trial. Pancreas. 2012;41:153–159.
- , , , . Enteral versus parenteral nutrition for acute pancreatitis. Cochrane Database Syst Rev. 2010;1:CD002837.
- , , , et al. Early versus on‐demand nasoenteric tube feeding in acute pancreatitis. N Engl J Med. 2014;371(21):1983–1993.
- , , , et al. A conservative and minimally invasive approach to necrotizing pancreatitis improves outcome. Gastroenterology. 2011;141:1254–1263.
- , , , et al. Endoscopic necrosectomy in necrotizing pancreatitis: indication is the key. Gut. 2010;59:1587.
- , , . Management of acute pancreatitis. Expert Rev Gastroenterol Hepatol. 2014;8(6):1–8.
- , . Evidence‐based management of acute pancreatitis. Curr Treat Options Gastroenterol. 2014;9(2):175–180.
- , , , et al. A scoring system to predict readmission of patients with acute pancreatitis to the hospital within thirty days of discharge. Clin Gastroenterol Hepatol. 2011;9(2):175–180.
- , , , et al. American college of gastroenterology guideline: management of acute pancreatitis. Am J Gastroenterol. 2013;108:1400–1415.
- , , . Acute pancreatitis. BMJ. 2014;349:g4859.
- , , , et al. Classification of acute pancreatitis‐2012: revision of Atlanta classification and definitions by international consensus. Gut. 2013;62:102–111.
- , . Clinical management of patients with acute pancreatitis. Gastroenterology. 2013;144:1272–1281.
- , , , et al. Acute pancreatitis and normoamylasemia. Not an uncommon combination. Ann Surg. 1989;2010:614–620.
- , , , et al. Acute pancreatitis with normal serum lipase: a case series. JOP. 2010;11:369–372.
- , , , et al. Body mass index and the risk and prognosis of acute pancreatitis: a meta‐analysis. Eur J Gastroenterol Hepatol. 2011;23(12):1136–1143.
- , , , et al. Alcohol consumption on pancreatic diseases. World J Gastroenterol. 2013;19(5):638–647.
- , , , et al. Drug‐induced pancreatitis. Curr Gastroenterol Rep. 2012;14:131–138.
- , . Pancreas divisum does not cause pancreatitis, but associates with CFTR mutations. Am J Gastroenterol. 2012;107:318–320.
- , , , et al. Association between early systemic inflammatory response, severity of multiorgan dysfunction and death in acute pancreatitis. Br J Surg. 2006;93:738–744.
- , . Practice guidelines in acute pancreatitis. Am J Gastroenterol. 2006;101(10):2379–2400.
- , , . Natural history following the first attack of acute pancreatitis. Am J Gastroenterol. 2012;107:1096–1103.
- Working Group IAP/APA Acute Pancreatitis Guidelines. IAP/APA Evidence‐based guidelines for the management of acute pancreatitis. Pancreatology. 2013;13:e1–e15.
- , , , et al. Interventions for necrotizing pancreatitis: summary of a multidisciplinary consensus conference. Pancreas. 2012;41(8):1176–1194.
- , , , et al. Extrapancreatic necrosis without pancreatic parenchymal necrosis: a separate entity in necrotising pancreatitis? Gut. 2013;62(10):1475–1480.
- , , . A randomized controlled trial of enteral versus parenteral feeding in patients with predicted severe acute pancreatitis shows a significant reduction in mortality and in infected pancreatic complications with total enteral nutrition. Dig Surg. 2006;23:336–345.
- , , , et al. Evaluation of early enteral feeding through nasogastric and nasojejunal tube in severe acute pancreatitis. A non‐inferiority randomized controlled trial. Pancreas. 2012;41:153–159.
- , , , . Enteral versus parenteral nutrition for acute pancreatitis. Cochrane Database Syst Rev. 2010;1:CD002837.
- , , , et al. Early versus on‐demand nasoenteric tube feeding in acute pancreatitis. N Engl J Med. 2014;371(21):1983–1993.
- , , , et al. A conservative and minimally invasive approach to necrotizing pancreatitis improves outcome. Gastroenterology. 2011;141:1254–1263.
- , , , et al. Endoscopic necrosectomy in necrotizing pancreatitis: indication is the key. Gut. 2010;59:1587.
- , , . Management of acute pancreatitis. Expert Rev Gastroenterol Hepatol. 2014;8(6):1–8.
- , . Evidence‐based management of acute pancreatitis. Curr Treat Options Gastroenterol. 2014;9(2):175–180.
- , , , et al. A scoring system to predict readmission of patients with acute pancreatitis to the hospital within thirty days of discharge. Clin Gastroenterol Hepatol. 2011;9(2):175–180.