User login
Health Care for Refugees Resettled in the US
It is estimated that three million refugees from all over the world—forced to flee their native countries for various reasons—have entered the United States since 1980.1,2 Prior to resettling in the US, refugees undergo health screenings for high-risk infectious diseases that preclude emigration; those free of such diseases may enter. However, the civil surgeon who conducts a refugee’s medical examination does not screen for chronic diseases that are not considered a threat to public health. Other infectious illnesses, previous traumatic injuries, and mental health issues may also go undetected at this exam.
Refugees may have had little or no access to health care before their arrival in the US, lived in conditions that increased their risk for exposure to various illnesses, and experienced traumatic events before fleeing their native lands. After their arrival, refugees may face access issues, including language and cultural barriers, health care ineligibility, and lack of transportation. This article seeks to increase awareness among primary care practitioners of the needs and issues of refugees who may be seen in their practices for conditions that developed before their arrival in the US and others emerging since their resettlement.
This activity will begin with an overview of who refugees are, how they come to reside in the US, and the medical process they undergo before resettlement. Next follows a discussion of medical issues that practitioners should be aware of among refugees, including conditions not commonly seen in the US. Finally, language and cultural issues will be addressed, including an explanatory model3 to help bridge discrepancies between practitioners of Western medicine and patients of non-Western traditions.
Man, 58, from Burundi
At age 55, the patient was resettled to the US with his family. Since then, he has had trouble holding a job, and his difficulties have been attributed to the stress of transition to life in the US. His current employer has sent him for an occupational examination. Findings are within normal limits except for visual acuity, which is tested at 20/25 in his right eye and 20/200 in his left. When asked, the patient reports having had “river blindness,” that is, onchocerciasis, as a child. Onchocerciasis is an uncommon cause of permanent blindness.
BACKGROUND AND DEFINITIONS
Refugees are defined by US Citizenship and Immigration Services4 as “people who have been persecuted or fear they will be persecuted on account of race, religion, nationality, and/or membership in a particular social group or political opinion.” The United Nations High Commission for Refugees (UNHCR)5 adds that a refugee “is outside the country of his nationality, and is unable to, or owing to such fear, is unwilling to, avail himself of the protection of that country.”
The man from Burundi came to the US through a long, complicated process. His family fled genocide in their native country to a refugee camp in Tanzania. Once there, they attained official refugee status, an essential part of the resettlement process. Refugees must fall into one of three processing priority categories:
(1) those referred by UNHCR, a US embassy, or a designated voluntary agency
(2) persons designated by a US refugee program as belonging to a “special humanitarian concern” group
(3) certain family members of refugees who currently reside in the US.6
The application generally involves biographical information and a family tree.7 Because they had fled their home, the family from Burundi had limited paperwork but were referred by UNHCR to the US for resettlement.
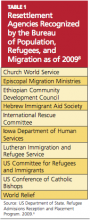
Once refugees become eligible for resettlement in the US, they undergo medical screening, security clearance, and cultural orientation. They are then placed by one of the sponsoring resettlement agencies listed in Table 1.8 This process can take from two months to several years.9 The medical screening may be performed by a panel physician, an overseas practitioner who examines refugees prior to their resettlement; or by a civil surgeon, who examines refugees after their arrival in the US—generally when the refugee applies for status adjustment.10
The man from Burundi represents a relatively common issue among refugees in the US. Many chronic conditions go untreated within this population because follow-up may be inadequate or absent, patients’ access to health care is insufficient, or the health care provider is unfamiliar with refugee issues. In this case, evaluation of the man’s vision was not part of the routine examination conducted in all refugees. Because he was never offered a subsequent vision check, his blindness went unnoticed, and his work difficulties were attributed to language and adjustment issues.
His visual problem could not be corrected, but once it was identified, accommodations were made in the workplace that facilitated his adjustment to the new work environment.
Girl, 16, from Liberia
This patient, who is being seen in your office for a sports physical, arrived in the US three years ago. Her medical screening at the time of immigration indicated “good health,” and she has had no health problems since then. Her exam seems unremarkable except for a low-pitched, rumbling, diastolic murmur best heard with the bell of the stethoscope near the apex when she lies in the left lateral decubitus position.
HEALTH SCREENINGS
Before coming to the US, refugees must undergo a health evaluation that includes a thorough medical history, full physical examination, chest x-ray, if indicated, for tuberculosis (TB), vaccination verification, and laboratory work as needed to identify specific infectious diseases.11 Screenings included in this evaluation target problems that are considered important from a public health perspective, including TB and certain sexually transmitted illnesses. Many infectious diseases are not considered a threat to public health because the requisite vector is not present in the US (eg, malaria, schistosomiasis).12
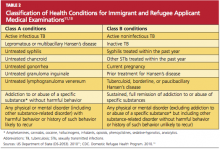
Public health conditions are categorized as Class A or Class B (see Table 2,11,13). Typically, refugees with a Class A condition are considered ineligible for admission to the US. Presence of a Class B condition must be brought to the attention of consular authorities, as it may indicate future disability or need for medical treatment.13,14
It is important for practitioners to know that if an illness or medical condition is discovered during the panel physician’s examination but is not considered “relevant to the visa medical examination,” the panel physician does not treat the patient. Rather, he or she recommends that the patient seek care from a medical provider.15 Essentially, refugees with a condition that is not considered a public health threat are allowed into the US, whether or not the condition has been addressed—as in the case of the diastolic heart murmur in the girl from Liberia.
This heart murmur could be a complication of rheumatic fever secondary to untreated group A streptococcal infection. In developing nations, rheumatic heart disease is the most commonly acquired heart condition, frequently exceeding congenital heart disease as a cause of hospitalization among children, adolescents, and teens.16 The risks associated with pregnancy in women with rheumatic heart disease have long been known,17 but as rheumatic heart disease has become less common in the developed nations, so has the sequela of mitral valve stenosis.
Clinicians need to become familiar with other illnesses commonly found in the developing nations, such as malaria and measles.12 Furthermore, practitioners should be aware that refugees may be immunologically susceptible to pathogens endemic to the countries of resettlement.
Woman, 65, from Bhutan
Forcibly deported from Bhutan to Nepal, this patient resettled to the US four years ago. She neither reads nor writes in her first language (Nepali) nor in English. She has been attending English language classes since her arrival in the US but has made little progress. The woman visits a health fair, bringing with her nine medications, including two bottles of insulin and three empty bottles for three different antihypertensive medications. Through an interpreter, you learn that the woman is not taking any of these medications regularly. She is also unaware that she should neither reuse needles nor share her medications with her son, who is also diabetic. She cannot afford to refill her prescriptions.
THE PROCESS, THE BARRIERS
Upon their arrival in the US, refugees receive 30 to 90 days’ support for “housing, essential furnishings, food, clothing, community orientation, and referral to other social, medical, and employment services.”8 In addition to the predeparture medical screening, refugees receive assistance for travel arrangements and a loan to pay for travel to the US.18 Refugees must sign a promissory note indicating that they will begin repayment of the loan within six months of their arrival and will complete repayment within 42months.19
At the time of their arrival, refugees apply for a Social Security number, register their children for school, undergo another medical evaluation, and receive English language training, if needed.8 Within six months of their arrival, refugees of working age are expected to have obtained employment.7 After one year in the US, refugees must apply for Legal Permanent Resident Status; after five years, they can apply for citizenship.8,20,21
In the case of the woman from Bhutan, neither diabetes nor hypertension precluded her resettlement; however, several factors now complicate her health care. Although she has access to health care providers, she cannot afford copayments for her medications, nor does she understand the instructions for their use. That she is not literate in any language complicates the challenge for her to learn to speak English. Her lack of linguistic and health literacy adds to the financial burden of the medications she needs.
The use of formally trained medical interpreters can alleviate some, but not all, of these problems. The refugee who does not become a citizen within seven years risks losing all benefits, including Medicare and Medicaid. This is particularly problematic for older refugees with multiple health problems. The process of becoming a US citizen is arduous, including lessons in civics and a required level of language fluency that is difficult to attain, particularly for those who are not literate in any language.
The Office of Refugee Resettlement22 recommends that refugees undergo a second medical screening after their arrival to identify any conditions that were not addressed by the panel physician. This examination, according to the CDC, “provides an opportunity to identify important causes of morbidity among resettled refugees that might not have been discovered previously, and enables early referral for treatment and follow-up care.”1 This screening also offers refugees the chance to establish a medical home and to begin to become familiar with the US health care system, potential barriers notwithstanding.
Girl, 15, from Sudan
A cough is the presenting symptom in this girl, who resettled to the US three years ago. She has no other upper respiratory symptoms. Results of laboratory testing indicate eosinophilia and mild anemia.
COMMON HEALTH ISSUES
Health conditions that refugees face but that may not be found in other immigrants or nonimmigrants include TB, hepatitis, parasites, HIV and other sexually transmitted infections, and mental health issues.23,24 For some refugees, female genital mutilation/cutting (FGM/C)23 or lead exposure25 may be a significant concern. Additionally, the traumatic events that led refugees to flee their homes may have resulted in musculoskeletal or neurologic injuries with a wide array of manifestations.
Parasites
Parasitic infections are common among refugees, and these can lead to anemia resulting from blood loss and iron deficiency, malnutrition, growth retardation, invasive illnesses, and death.26,27 According to Carlsten and Jackson,28 immigrants can be infected by multiple pathogens simultaneously, and some parasites may survive for as long as decades.
The most common parasitic infections among refugees are hookworm, whipworm, roundworm, and Giardia lamblia.23 In a screening performed five years after the arrival in the US of the “Lost Boys and Girls of Sudan,” 64% of a cohort of the boys living in Atlanta tested positive for Schistosoma mansoni or Schistosoma haematobium, and 25% tested positive for Strongyloides stercoralis—the organisms responsible for schistosomiasis and strongyloidiasis, respectively.26 In 2005, the CDC recommended presumptive treatment for both illnesses in Sudanese refugees who were not treated for these infections before their resettlement.29
Despite treatment and prophylaxis prior to refugees’ departure for the US, parasitic infections remain common in the refugee population.23 Practitioners should be aware that a cough could indicate the presence of roundworms that have entered the body through the skin and spread to the lungs via the blood.30,31 All refugees should be screened for eosinophilia to detect parasitic infections.23 An absolute eosinophil count exceeding 400 cells/L warrants further investigation.27
Because of presumptive treatment for malaria given to nonpregnant refugees, this disease is rarely seen after refugees’ arrival in the US.23 However, practitioners should not overlook the possibility of malaria when they examine refugee patients, as malaria may take time to manifest clinically.24
Tuberculosis
While refugees cannot be admitted into the US with active, infectious TB (a Class A disease), the majority of cases of TB in the US occur among foreign-born individuals, with prevalence 10 times that in the US-born population.32 Refugees are at particular risk for TB.33
When examining refugee patients, especially those recently arrived in the US, clinicians should be aware of the potential for extrapulmonary TB, which accounted for 20% of TB cases in the US in 2008.32 Extrapulmonary TB can be found anywhere in the body, with more common sites including the lymph nodes, pleura, and osteoarticular areas. Skeletal TB accounts for 35% of extrapulmonary TB cases—most commonly Pott’s disease, or spinal TB.34
Use of bacille Calmette-Guerin (BCG), a vaccine given in various countries to prevent childhood tuberculous meningitis and miliary disease, often leads to confusion when the tuberculin skin test (TST, previously known as the purified protein derivative, or PPD) is used to screen for TB.35 While BCG can increase the number of false-positive TST results, TST reaction following BCG decreases with time and generally is not seen longer than 10 years postvaccination.36
Furthermore, the immunity produced by BCG weakens over time; thus, an adult, though immunized as an infant, is at risk for TB infection. The CDC currently recommends the same testing for TB, whether or not patients have undergone BCG vaccination. Similarly, TST results should be interpreted in the same way for BCG-vaccinated patients and nonvaccinated patients alike.35
Finally, BCG does not affect results of blood tests for TB. However, these tests are new, expensive, and not available everywhere.35
Hepatitis
Among the forms of hepatitis, hepatitis B virus (HBV) is of greatest concern within the refugee community, as it is endemic to much of the world.37 Between 2003 and 2007, 10.7% of refugees screened in DeKalb County, Georgia, for HBsAg (the hepatitis B surface antigen that indicates exposure to the virus) tested positive, accounting for 43.3% of HBsAg-positive test results in the county during that period. Chronic HBV infection can lead to end-stage liver disease, cirrhosis, and hepatocellular carcinoma.37
Museru et al37 recommend that health care providers ascertain the hepatitis B–serological status of resettled refugees from areas that are highly endemic for HBV infection. In addition, Adams and colleagues23 recommend screening patients who have undergone blood transfusions, female genital surgery, or other surgical procedures in their countries of origin, as well as patients from Africa or southeast Asia, for hepatitis C.23
Mutilation or Cutting of the Female Genitalia
Ritual FGM/C is the practice of injuring or removing part or all of the external female genitalia for cultural and other nonmedical reasons.38 FGM/C is primarily practiced in Africa (see Figure,39,40) but may occur also in Asia, the Middle East, and Central and South America.38 It is often practiced by informally trained individuals, with “inexact surgical outcomes.”23 FGM/C has been outlawed in the US and other countries with large immigrant populations; some nations grant asylum to women who fear being subjected to FGM/C if they return to their country of origin.39
Practitioners who care for female refugees should be aware of both the short-term sequelae (pain, bleeding, trauma, sepsis) and additional long-term sequelae (dyspareunia, urinary retention and recurrent urinary tract infections, chronic pelvic inflammatory disease, keloid scar formation, childbirth complications) of FGM/C, in addition to psychological sequelae.23,38,41 It is important to approach affected patients with sympathy and without judgment, as the decision to undergo FGM/C may not have been theirs.41
The Royal College of Obstetricians and Gynaecologists in the United Kingdom has produced a helpful set of guidelines, Female Genital Mutilation and its Management,41 for clinicians working with patients who have undergone FGM/C.
Sexually Transmitted Infections
In light of a new law allowing refugees with HIV to be resettled in the US,42 practitioners must now be aware of the possibility of HIV infection in a refugee patient, whether documented or not. Practitioners should follow the same guidelines for refugees as they do for all patients regarding HIV screening and counseling, including allowing patients the opportunity to decline testing.43 However, they should also be aware of countries in which HIV prevalence rates are high.43
Additionally, while HIV-1 is the world’s predominant strain of the disease, refugees from West African countries have been at increased risk for exposure to HIV-2 and should be tested accordingly.43,44 Refugees may also be at increased risk for HIV and other sexually transmitted infections attributable to physical or sexual violence.43,45
All screening for HIV and other sexually transmitted infections should be performed in a culturally appropriate manner, with the use of trained interpreters as needed, to ensure that all patients receive accurate information and counseling.43
Exposure to Lead
Refugee children are at high risk for lead exposure both before and after their arrival in the US—the latter as a result of their families’ living conditions after resettlement, despite the ban on lead-based paint.25 A study in Minnesota from 2000 to 2002 showed that among refugee children younger than 6, prevalence of lead poisoning was 14 times that found in American children in their age-group.25 In New York City, Asian children have been shown to be at particular risk for lead poisoning—including the case of a year-old Cambodian child who was evidently exposed to an amulet with leaded beads. Sources of lead other than paint may include imported food, spices, cosmetics, pottery, and health remedies.46
Where children were born and where they have lived throughout their lives appear to be the greatest predictors of lead poisoning risk.25 One primary risk factor for lead poisoning is malnutrition, associated with increased absorption of lead in the intestines and the resulting micronutrient deficiencies.25
The CDC recommends:
• Screening for lead in all children from age 6 months to 16 years at the time of their arrival in the US
• Follow-up blood lead testing of children ages 6 months to 6 years, 3 to 6 months after they have moved into a permanent residence25
• Nutritional assessments for children younger than 6 years, as well as measurement of hemoglobin/hematocrit levels, including at least one of the following measurements: mean corpuscular volume with red-cell distribution width, ferritin, transferrin saturation, or reticulocyte hemoglobin content
• Daily multivitamins with iron for refugee children ages 6 months to approximately 5 years.
Lead poisoning, as indicated by a blood lead level (BLL) exceeding 10 g/dL, is known to have neurodevelopmental and cognitive sequelae. In children with a significantly higher BLL, manifestations may include headaches, abdominal pain, anorexia, constipation, clumsiness, agitation, and lethargy in the acute phase.25
Woman, 48, from Afghanistan
Through an interpreter, you learn that this visitor to a local health fair has been experiencing left arm pain since she and her family fled Kabul. When her house there was hit by a rocket, she ran back in, despite a fire, to save her infant daughter. Although she received care as a refugee in Pakistan for burns to her arms and body, she has scarring and strictures the length of her arm. Thanks to the efforts of a volunteer physical therapist, use of the woman’s injured arm has been preserved. She is diagnosed with posttraumatic stress syndrome and referred to a local mental health clinic whose staff specializes in working with survivors of trauma and torture.
Mental Health Issues
Mental health issues are a significant component of refugee health. MacDuff et al47 report that 36% of complementary and alternative medicine use among refugees targets mental health issues resulting from trauma. Because refugees were forced by dangerous conditions to flee their home countries, they are particularly susceptible to mental health concerns. They may have witnessed violence, undergone torture, or been subjected to unsafe or unsanitary conditions in refugee camps. Many have had trouble adjusting to their new culture.23,24,28
As a result, refugees are at increased risk for depression, posttraumatic stress disorder, substance abuse, somatization, psychosis, and suicide.23,28 Mental health issues among refugees are also complicated by the cultural and communication barriers that often exist between refugees and practitioners.23 Thus, practitioners need to take careful histories with sensitivity to their patients’ previous experiences.
While the acuity of these issues begins to decrease around three years after refugees’ arrival in their country of resettlement, the burden of mental health problems often persists for many years.28 Adams et al23 recommend that refugees be referred to social workers, cultural case mediators, and community organizations. Clinicians who do not feel comfortable managing mental health conditions should refer refugee patients to appropriate mental health practitioners and follow up to make sure that patients’ needs are being met.
Musculoskeletal and Neurologic Injuries
Traumatic events can lead to a wide variety of musculoskeletal and neurologic injuries—for example, wounds inflicted by weapons, amputations following land mine injuries, crush injuries from collapsing buildings, or burns sustained in rocket attacks. The array of possibilities necessitates a thorough history and complete musculoskeletal and neurologic assessments.
LANGUAGE AND CULTURAL ISSUES
In addition to being aware of the potential health issues that arise within the refugee population, primary care providers need to be prepared to confront language and cultural issues that may arise. The National Standards on Culturally and Linguistically Appropriate Services (CLAS)48 offer appropriate guidance in 14 key areas.
Refugees frequently have limited or no working knowledge of English. Whenever possible, practitioners should use medically trained interpreters to help them receive and convey accurate information and thus provide comprehensive care. When professional interpreters are not available, telephone interpreter services are available for purchase by the facility or practice. Children or other family members should not be relied on for accurate interpretation.48
As for cultural differences, it is important to note that a refugee’s concept of family may differ from that found in Western culture.49 For example, it is not uncommon to find extended families living together, with members referring to nieces and nephews as their children, or aunts and uncles as their parents. A thorough exploration of the relationships among patients and their families is important, particularly during the family history.
Regardless of where resettled refugees come from, it is probable that their cultural and personal beliefs about medicine differ from those of practitioners with years of Western medicine training. In addition to implementing CLAS guidelines,48 practitioners should be familiar with Kleinman’s3explanatory model, which explores the differences between the patient and practitioner models—not necessarily differences in levels of knowledge, but rather of “values and interests.”3 Thus, people unfamiliar with or resistant to the Western model of medicine are often seen as ignorant, whereas an issue of values may be at play.
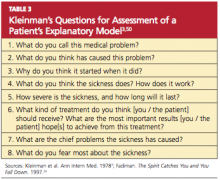
Identifying the differences between the patient’s and the clinician’s explanatory models allows the clinician to anticipate and address potential misunderstandings, understand patients’ perceived needs, and involve patients in management strategies that will motivate them to comply with treatment. To help clinicians assess the explanatory models of their patients, Kleinman provides eight questions (shown in Table 3,3,50).
CONCLUSION
As the world becomes more of a global village, increasing numbers of primary care providers will see refugee patients. Practitioners need to be aware of the physical, socioeconomic, and psychological issues that affect refugees during and after resettlement in the US. Refugees may have conditions that could not be addressed in their home country or refugee camp. They may have illnesses with which US practitioners are ordinarily unfamiliar, poorly treated or untreated traumatic injuries, or psychological trauma resulting from conditions that forced them to flee their native lands.
Clinicians who work with refugees should be familiar with the resettlement process and perform a thorough examination after the refugee’s resettlement, managing previously unaddressed health issues. Complete histories must be taken and physical examinations performed in a culturally appropriate manner and an atmosphere of mutual trust.
Finally, it is vital for providers to explore the explanatory models from which patients view their illnesses. Such an understanding facilitates culturally appropriate care with patient participation, and ultimately more positive clinical outcomes.
Authors’ note: The patients portrayed in this article are all composites. While the issues described are real, these “patients” were developed from multiple cases to protect individual patient privacy. None is real, and any resemblance to any real persons is purely accidental.
REFERENCES
1. Ramos M, Orozovich P, Moser K, et al. Health of resettled Iraqi refugees: San Diego County, California, October 2007–September 2009. MMWR Morb Mortal Wkly Rep. 2010;59(49):1614-1618.
2. US Department of State. FY 2010 cumulative summary of refugee admissions. www.wrapsnet .org/reports/archives/tabid/215/language/en-us/default.aspx. Accessed February 17, 2011.
3. Kleinman A, Eisenberg L, Good B. Culture, illness, and care: clinical lessons from anthropologic and cross-cultural research. Ann Intern Med. 1978;88(2):251-258.
4. US Citizenship and Immigration Services. Refugees and asylum. www.uscis.gov/portal/site/uscis/menuitem.eb1d4c2a3e5b9ac89243c6a7543f6d1a/?vgnextoid=1f1c3e4d77d73210VgnVCM100000082ca60aRCRD&vgnextchannel=1f1c3e4d77d73210VgnVCM100000082ca60aRCRD. Accessed February 17, 2011.
5. United Nations High Commissioner for Refugees. Refugees: flowing across borders. www .unhcr.org/pages/49c3646c125.html. Accessed February 17, 2011.
6. US Citizenship and Immigration Services. The United States Refugee Admissions Program (USRAP) consultation and worldwide processing priorities. www.uscis.gov/portal/site/uscis/menuitem.5af9bb95919f35e66f614176543f6d1a/?vgnextoid=796b0eb389683210VgnVCM100000082ca60aRCRD&vgnextchannel=385d3e4d77d73210VgnVCM100000082ca60aRCRD. Accessed February 17, 2011.
7. US Committee for Refugees and Immigrants. Frequently asked questions. www.refugees.org/about-us/faqs.html. Accessed February 17, 2011.
8. US Department of State. Refugee Admissions Reception and Placement Program. www.state
.gov/g/prm/rls/125478.htm. Accessed February 17, 2011.
9. Office of Refugee Resettlement. Report to Congress: FY 2007. www.acf.hhs.gov/programs/orr/data/ORR_2007_report.pdf. Accessed February 17, 2011.
10. CDC. Medical examination: frequently asked questions (FAQs). www.cdc.gov/immigrant
refugeehealth/exams/medical-examination-faqs .html#9. Accessed February 17, 2011.
11. US Department of State. Medical Examination for Immigrant or Refugee Applicant (DS-2053, OMB No. 1405-0113, expiration date 04/30/2012. http://bangkok.usembassy.gov/root/pdfs/med forms_043012.pdf. Accessed February 17, 2011.
12. Cohen J, Powderly WG, Opal SM, eds. Infectious Diseases. 3rd ed. Philadelphia, PA: Elsevier; 2010.
13. CDC. Domestic Refugee Health Program: Frequently Asked Questions (2010). www.cdc.gov/immigrantrefugeehealth/guidelines/domestic/domestic-refugee-questions.html. Accessed February 17, 2011.
14. CDC. Technical Instructions: guidance for HIV for panel physicians and civil surgeons (2010). www.cdc.gov/immigrantrefugeehealth/exams/ti/hiv-guidance-panel-civil.html. Accessed February 17, 2011.
15. CDC. Medical history and physical examination: technical instructions for medical examination of aliens. www.cdc.gov/immigrantrefugee health/exams/ti/panel/technical-instructions/panel-physicians/medical-history-physical-exam .html. Accessed February 17, 2011.
16. Lee JL, Naguwa SM, Cheema GS, Gershwin ME. Acute rheumatic fever and its consequences: a persistent threat to developing nations in the 21st century. Autoimmun Rev. 2009;9(2):117-123.
17. Henderson DN. Pregnancy complicated by rheumatic heart disease. Can Med Assoc J. 1936; 35(4):394-398.
18. US Citizenship and Immigration Services. Refugees. www.uscis.gov/portal/site/uscis/menu item.eb1d4c2a3e5b9ac89243c6a7543f6d1a/?vgnextoid=385d3e4d77d73210VgnVCM100000082ca60aRCRD&vgnextchannel=385d3e4d77d73210VgnVCM100000082ca60aRCRD. Accessed February 17, 2011.
19. US Department of State. 9 FAM appendix O, exhibit II: Promissory note (2007). In: Foreign Affairs Manual Volume 9: Visas. www.state.gov/documents/organization/88070.pdf. Accessed February 17, 2011.
20. United States Department of State. US Refugee Admissions Program. www.state.gov/g/prm/c26471.htm. Accessed February 17, 2011.
21. J. Kernan, Community Relations Officer, US Citizenship and Immigration Services, personal communication, March 29, 2010.
22. Office of Refugee Resettlement. Health. www.acf.hhs.gov/programs/orr/benefits/health .htm. Accessed February 17, 2011.
23. Adams KM, Gardiner LD, Assefi N. Healthcare challenges from the developing world: post-immigration refugee medicine. BMJ. 2004;328(7455): 1548-1552.
24. Walker PF, Jaranson J. Refugee and immigrant health care. Med Clin North Am. 1999; 83(4):1103-1120.
25. CDC. Screening for lead at the domestic refugee medical examination (2005). www.cdc.gov/immigrantrefugeehealth/pdf/lead.pdf. Accessed February 17, 2011.
26. Franco-Paredes C, Dismukes R, Nicolls D, et al. Short report: persistent and untreated tropical infectious diseases among Sudanese refugees in the United States. Am J Trop Med Hyg. 2007;77 (4):633-635.
27. CDC. Immigrant and Refugee Health: Domestic Refugee Health Guidelines: Intestinal Parasites. www.cdc.gov/immigrantrefugeehealth/guidelines/ip/intestinal-parasites-domestic.html#asympto matic2. Accessed February 17, 2011.
28. Carlsten C, Jackson C. Refugee and immigrant health care. EthnoMed. http://ethnomed.org/clinical/refugee-health/carlsten.pdf. Accessed February 17, 2011.
29. Conly JM, Johnston BL. The infectious diseases implications of the “Lost Boys and Girls of Sudan.” Can J Infect Dis Med Microbiol. 2008;19 (3):215-216.
30. Aggarwal B, Sharma M, Singh T. Acute eosinophilic pneumonia due to round worm infestation. Indian J Pediatr. 2008;75(3):296-297.
31. Tsai HC, Lee SS, Liu YC, et al. Clinical manifestations of strongyloidiasis in southern Taiwan.
J Microbiol Immunol Infect. 2002;35(1):29-36.
32. CDC. Reported tuberculosis in the United States, 2008. www.cdc.gov/tb/statistics/reports/2008/pdf/2008report.pdf. Accessed February 17, 2011.
33. Oeltmann JE, Varma JK, Ortega L, et al. Multidrug-resistant tuberculosis outbreak among US-bound Hmong refugees, Thailand, 2005. Emerg Infect Dis. 2008;14(11):1715-1721.
34. Golden MP, Vikram H. Extrapulmonary tuberculosis: an overview. Am Fam Physician. 2005; 72(9):1761-1768.
35. CDC. Tuberculosis (TB) Fact Sheets: BCG Vaccine. www.cdc.gov/tb/publications/factsheets/prevention/BCG.htm. Accessed February 17, 2011.
36. The role of BCG vaccine in the prevention and control of tuberculosis in the United States: a joint statement by the Advisory Council for the Elimination of Tuberculosis and the Advisory Committee on Immunization Practices. MMWR Recomm Rep. 1996;45(RR-4):1-18.
37. Museru OI, Vargas M, Kinyua M, et al. Hepatitis B virus infection among refugees resettled in the US: high prevalence and challenges in access to health care. J Immigr Minor Health. 2010;12 (6):823-827.
38. World Health Organization, UNAIDS, UNDP, UNECA, UNESO, UNFPA, UNHCHR, UNHCR, UNICEF, UNIFEM. Eliminating Female Genital Mutilation: An Interagency Statement (2008). http://whqlibdoc.who.int/publications/2008/ 9789241596442_eng.pdf. Accessed February 17, 2010.
39. United Nations Children’s Fund. Female Genital Mutilation/Cutting: A Statistical Exploration (2005). www.unicef.org/publications/files/FGM-C_final_10_October.pdf. Accessed February 17, 2011.
40. Yoder PS, Abderrahim N, Zhuzhuni A. DHS Comparative Reports No. 7: Female Genital Cutting in the Demographic and Health Surveys: A Critical and Comparative Analysis. Calverton, MD: ORC Macro. September 2004.
41. Royal College of Obstetricians and Gynaecologists. Female Genital Mutilation and its Management (Green-top Guideline No. 53; 2009). www .rcog.org.uk/files/rcog-corp/GreenTop53Female GenitalMutilation.pdf. Accessed February 17, 2011.
42. CDC. Final Rule Removing HIV Infection from U.S. Immigration Screening: Revision of 42 CFR Part 34 (Medical Examination of Aliens) Removal of Human Immunodeficiency Virus (HIV) from Definition of Communicable Disease of Public Health Significance—Final Rule. www.cdc.gov/immigrantrefugeehealth/laws-regs/hiv-ban-removal/final-rule.html. Accessed February 17, 2011.
43. CDC. Immigrant and Refugee Health: Screening for HIV-infection during the refugee domestic medical examination. www.cdc.gov/immigrant
refugeehealth/guidelines/domestic/screening-
hiv-infection-domestic.html. Accessed February 17, 2011.
44. CDC. Human Immunodeficiency Virus Type 2: HIV/AIDS Fact Sheets. Atlanta: Centers for Disease Control and Prevention; 2007.
45. Mills EJ, Nachega JB. HIV infection as a weapon of war. Lancet Infect Dis. 2006;6(12):752-753.
46. CDC. Lead poisoning of a child associated with use of a Cambodian amulet—New York City, 2009. MMWR Morb Mortal Wkly Rep. 2011;60(3): 69-71.
47. MacDuff S, Grodin MA, Gardiner P. The use of complementary and alternative medicine among refugees: a systematic review. J Immigr Minor Health. 2010 Mar 12 [Epub ahead of print].
48. US Department of Health and Human Services, Office of Minority Health. National standards on culturally and linguistically appropriate services (CLAS). http://minorityhealth.hhs.gov/templates/browse.aspx?lvl=2&lvlID=15. Accessed February 17, 2011.
49. Haviland WA, Prins HEL, Walrath D, McBride B, eds. Cultural Anthropology: The Human Challenge. 12th ed. Belmont, CA: Wadsworth Publishing; 2008.
50. Fadiman A. The Spirit Catches You and You Fall Down: A Hmong Child, Her American Doctors, and the Collision of Two Cultures. New York, NY: Farrar, Straus and Giroux; 1997.
It is estimated that three million refugees from all over the world—forced to flee their native countries for various reasons—have entered the United States since 1980.1,2 Prior to resettling in the US, refugees undergo health screenings for high-risk infectious diseases that preclude emigration; those free of such diseases may enter. However, the civil surgeon who conducts a refugee’s medical examination does not screen for chronic diseases that are not considered a threat to public health. Other infectious illnesses, previous traumatic injuries, and mental health issues may also go undetected at this exam.
Refugees may have had little or no access to health care before their arrival in the US, lived in conditions that increased their risk for exposure to various illnesses, and experienced traumatic events before fleeing their native lands. After their arrival, refugees may face access issues, including language and cultural barriers, health care ineligibility, and lack of transportation. This article seeks to increase awareness among primary care practitioners of the needs and issues of refugees who may be seen in their practices for conditions that developed before their arrival in the US and others emerging since their resettlement.
This activity will begin with an overview of who refugees are, how they come to reside in the US, and the medical process they undergo before resettlement. Next follows a discussion of medical issues that practitioners should be aware of among refugees, including conditions not commonly seen in the US. Finally, language and cultural issues will be addressed, including an explanatory model3 to help bridge discrepancies between practitioners of Western medicine and patients of non-Western traditions.
Man, 58, from Burundi
At age 55, the patient was resettled to the US with his family. Since then, he has had trouble holding a job, and his difficulties have been attributed to the stress of transition to life in the US. His current employer has sent him for an occupational examination. Findings are within normal limits except for visual acuity, which is tested at 20/25 in his right eye and 20/200 in his left. When asked, the patient reports having had “river blindness,” that is, onchocerciasis, as a child. Onchocerciasis is an uncommon cause of permanent blindness.
BACKGROUND AND DEFINITIONS
Refugees are defined by US Citizenship and Immigration Services4 as “people who have been persecuted or fear they will be persecuted on account of race, religion, nationality, and/or membership in a particular social group or political opinion.” The United Nations High Commission for Refugees (UNHCR)5 adds that a refugee “is outside the country of his nationality, and is unable to, or owing to such fear, is unwilling to, avail himself of the protection of that country.”
The man from Burundi came to the US through a long, complicated process. His family fled genocide in their native country to a refugee camp in Tanzania. Once there, they attained official refugee status, an essential part of the resettlement process. Refugees must fall into one of three processing priority categories:
(1) those referred by UNHCR, a US embassy, or a designated voluntary agency
(2) persons designated by a US refugee program as belonging to a “special humanitarian concern” group
(3) certain family members of refugees who currently reside in the US.6
The application generally involves biographical information and a family tree.7 Because they had fled their home, the family from Burundi had limited paperwork but were referred by UNHCR to the US for resettlement.
Once refugees become eligible for resettlement in the US, they undergo medical screening, security clearance, and cultural orientation. They are then placed by one of the sponsoring resettlement agencies listed in Table 1.8 This process can take from two months to several years.9 The medical screening may be performed by a panel physician, an overseas practitioner who examines refugees prior to their resettlement; or by a civil surgeon, who examines refugees after their arrival in the US—generally when the refugee applies for status adjustment.10
The man from Burundi represents a relatively common issue among refugees in the US. Many chronic conditions go untreated within this population because follow-up may be inadequate or absent, patients’ access to health care is insufficient, or the health care provider is unfamiliar with refugee issues. In this case, evaluation of the man’s vision was not part of the routine examination conducted in all refugees. Because he was never offered a subsequent vision check, his blindness went unnoticed, and his work difficulties were attributed to language and adjustment issues.
His visual problem could not be corrected, but once it was identified, accommodations were made in the workplace that facilitated his adjustment to the new work environment.
Girl, 16, from Liberia
This patient, who is being seen in your office for a sports physical, arrived in the US three years ago. Her medical screening at the time of immigration indicated “good health,” and she has had no health problems since then. Her exam seems unremarkable except for a low-pitched, rumbling, diastolic murmur best heard with the bell of the stethoscope near the apex when she lies in the left lateral decubitus position.
HEALTH SCREENINGS
Before coming to the US, refugees must undergo a health evaluation that includes a thorough medical history, full physical examination, chest x-ray, if indicated, for tuberculosis (TB), vaccination verification, and laboratory work as needed to identify specific infectious diseases.11 Screenings included in this evaluation target problems that are considered important from a public health perspective, including TB and certain sexually transmitted illnesses. Many infectious diseases are not considered a threat to public health because the requisite vector is not present in the US (eg, malaria, schistosomiasis).12
Public health conditions are categorized as Class A or Class B (see Table 2,11,13). Typically, refugees with a Class A condition are considered ineligible for admission to the US. Presence of a Class B condition must be brought to the attention of consular authorities, as it may indicate future disability or need for medical treatment.13,14
It is important for practitioners to know that if an illness or medical condition is discovered during the panel physician’s examination but is not considered “relevant to the visa medical examination,” the panel physician does not treat the patient. Rather, he or she recommends that the patient seek care from a medical provider.15 Essentially, refugees with a condition that is not considered a public health threat are allowed into the US, whether or not the condition has been addressed—as in the case of the diastolic heart murmur in the girl from Liberia.
This heart murmur could be a complication of rheumatic fever secondary to untreated group A streptococcal infection. In developing nations, rheumatic heart disease is the most commonly acquired heart condition, frequently exceeding congenital heart disease as a cause of hospitalization among children, adolescents, and teens.16 The risks associated with pregnancy in women with rheumatic heart disease have long been known,17 but as rheumatic heart disease has become less common in the developed nations, so has the sequela of mitral valve stenosis.
Clinicians need to become familiar with other illnesses commonly found in the developing nations, such as malaria and measles.12 Furthermore, practitioners should be aware that refugees may be immunologically susceptible to pathogens endemic to the countries of resettlement.
Woman, 65, from Bhutan
Forcibly deported from Bhutan to Nepal, this patient resettled to the US four years ago. She neither reads nor writes in her first language (Nepali) nor in English. She has been attending English language classes since her arrival in the US but has made little progress. The woman visits a health fair, bringing with her nine medications, including two bottles of insulin and three empty bottles for three different antihypertensive medications. Through an interpreter, you learn that the woman is not taking any of these medications regularly. She is also unaware that she should neither reuse needles nor share her medications with her son, who is also diabetic. She cannot afford to refill her prescriptions.
THE PROCESS, THE BARRIERS
Upon their arrival in the US, refugees receive 30 to 90 days’ support for “housing, essential furnishings, food, clothing, community orientation, and referral to other social, medical, and employment services.”8 In addition to the predeparture medical screening, refugees receive assistance for travel arrangements and a loan to pay for travel to the US.18 Refugees must sign a promissory note indicating that they will begin repayment of the loan within six months of their arrival and will complete repayment within 42months.19
At the time of their arrival, refugees apply for a Social Security number, register their children for school, undergo another medical evaluation, and receive English language training, if needed.8 Within six months of their arrival, refugees of working age are expected to have obtained employment.7 After one year in the US, refugees must apply for Legal Permanent Resident Status; after five years, they can apply for citizenship.8,20,21
In the case of the woman from Bhutan, neither diabetes nor hypertension precluded her resettlement; however, several factors now complicate her health care. Although she has access to health care providers, she cannot afford copayments for her medications, nor does she understand the instructions for their use. That she is not literate in any language complicates the challenge for her to learn to speak English. Her lack of linguistic and health literacy adds to the financial burden of the medications she needs.
The use of formally trained medical interpreters can alleviate some, but not all, of these problems. The refugee who does not become a citizen within seven years risks losing all benefits, including Medicare and Medicaid. This is particularly problematic for older refugees with multiple health problems. The process of becoming a US citizen is arduous, including lessons in civics and a required level of language fluency that is difficult to attain, particularly for those who are not literate in any language.
The Office of Refugee Resettlement22 recommends that refugees undergo a second medical screening after their arrival to identify any conditions that were not addressed by the panel physician. This examination, according to the CDC, “provides an opportunity to identify important causes of morbidity among resettled refugees that might not have been discovered previously, and enables early referral for treatment and follow-up care.”1 This screening also offers refugees the chance to establish a medical home and to begin to become familiar with the US health care system, potential barriers notwithstanding.
Girl, 15, from Sudan
A cough is the presenting symptom in this girl, who resettled to the US three years ago. She has no other upper respiratory symptoms. Results of laboratory testing indicate eosinophilia and mild anemia.
COMMON HEALTH ISSUES
Health conditions that refugees face but that may not be found in other immigrants or nonimmigrants include TB, hepatitis, parasites, HIV and other sexually transmitted infections, and mental health issues.23,24 For some refugees, female genital mutilation/cutting (FGM/C)23 or lead exposure25 may be a significant concern. Additionally, the traumatic events that led refugees to flee their homes may have resulted in musculoskeletal or neurologic injuries with a wide array of manifestations.
Parasites
Parasitic infections are common among refugees, and these can lead to anemia resulting from blood loss and iron deficiency, malnutrition, growth retardation, invasive illnesses, and death.26,27 According to Carlsten and Jackson,28 immigrants can be infected by multiple pathogens simultaneously, and some parasites may survive for as long as decades.
The most common parasitic infections among refugees are hookworm, whipworm, roundworm, and Giardia lamblia.23 In a screening performed five years after the arrival in the US of the “Lost Boys and Girls of Sudan,” 64% of a cohort of the boys living in Atlanta tested positive for Schistosoma mansoni or Schistosoma haematobium, and 25% tested positive for Strongyloides stercoralis—the organisms responsible for schistosomiasis and strongyloidiasis, respectively.26 In 2005, the CDC recommended presumptive treatment for both illnesses in Sudanese refugees who were not treated for these infections before their resettlement.29
Despite treatment and prophylaxis prior to refugees’ departure for the US, parasitic infections remain common in the refugee population.23 Practitioners should be aware that a cough could indicate the presence of roundworms that have entered the body through the skin and spread to the lungs via the blood.30,31 All refugees should be screened for eosinophilia to detect parasitic infections.23 An absolute eosinophil count exceeding 400 cells/L warrants further investigation.27
Because of presumptive treatment for malaria given to nonpregnant refugees, this disease is rarely seen after refugees’ arrival in the US.23 However, practitioners should not overlook the possibility of malaria when they examine refugee patients, as malaria may take time to manifest clinically.24
Tuberculosis
While refugees cannot be admitted into the US with active, infectious TB (a Class A disease), the majority of cases of TB in the US occur among foreign-born individuals, with prevalence 10 times that in the US-born population.32 Refugees are at particular risk for TB.33
When examining refugee patients, especially those recently arrived in the US, clinicians should be aware of the potential for extrapulmonary TB, which accounted for 20% of TB cases in the US in 2008.32 Extrapulmonary TB can be found anywhere in the body, with more common sites including the lymph nodes, pleura, and osteoarticular areas. Skeletal TB accounts for 35% of extrapulmonary TB cases—most commonly Pott’s disease, or spinal TB.34
Use of bacille Calmette-Guerin (BCG), a vaccine given in various countries to prevent childhood tuberculous meningitis and miliary disease, often leads to confusion when the tuberculin skin test (TST, previously known as the purified protein derivative, or PPD) is used to screen for TB.35 While BCG can increase the number of false-positive TST results, TST reaction following BCG decreases with time and generally is not seen longer than 10 years postvaccination.36
Furthermore, the immunity produced by BCG weakens over time; thus, an adult, though immunized as an infant, is at risk for TB infection. The CDC currently recommends the same testing for TB, whether or not patients have undergone BCG vaccination. Similarly, TST results should be interpreted in the same way for BCG-vaccinated patients and nonvaccinated patients alike.35
Finally, BCG does not affect results of blood tests for TB. However, these tests are new, expensive, and not available everywhere.35
Hepatitis
Among the forms of hepatitis, hepatitis B virus (HBV) is of greatest concern within the refugee community, as it is endemic to much of the world.37 Between 2003 and 2007, 10.7% of refugees screened in DeKalb County, Georgia, for HBsAg (the hepatitis B surface antigen that indicates exposure to the virus) tested positive, accounting for 43.3% of HBsAg-positive test results in the county during that period. Chronic HBV infection can lead to end-stage liver disease, cirrhosis, and hepatocellular carcinoma.37
Museru et al37 recommend that health care providers ascertain the hepatitis B–serological status of resettled refugees from areas that are highly endemic for HBV infection. In addition, Adams and colleagues23 recommend screening patients who have undergone blood transfusions, female genital surgery, or other surgical procedures in their countries of origin, as well as patients from Africa or southeast Asia, for hepatitis C.23
Mutilation or Cutting of the Female Genitalia
Ritual FGM/C is the practice of injuring or removing part or all of the external female genitalia for cultural and other nonmedical reasons.38 FGM/C is primarily practiced in Africa (see Figure,39,40) but may occur also in Asia, the Middle East, and Central and South America.38 It is often practiced by informally trained individuals, with “inexact surgical outcomes.”23 FGM/C has been outlawed in the US and other countries with large immigrant populations; some nations grant asylum to women who fear being subjected to FGM/C if they return to their country of origin.39
Practitioners who care for female refugees should be aware of both the short-term sequelae (pain, bleeding, trauma, sepsis) and additional long-term sequelae (dyspareunia, urinary retention and recurrent urinary tract infections, chronic pelvic inflammatory disease, keloid scar formation, childbirth complications) of FGM/C, in addition to psychological sequelae.23,38,41 It is important to approach affected patients with sympathy and without judgment, as the decision to undergo FGM/C may not have been theirs.41
The Royal College of Obstetricians and Gynaecologists in the United Kingdom has produced a helpful set of guidelines, Female Genital Mutilation and its Management,41 for clinicians working with patients who have undergone FGM/C.
Sexually Transmitted Infections
In light of a new law allowing refugees with HIV to be resettled in the US,42 practitioners must now be aware of the possibility of HIV infection in a refugee patient, whether documented or not. Practitioners should follow the same guidelines for refugees as they do for all patients regarding HIV screening and counseling, including allowing patients the opportunity to decline testing.43 However, they should also be aware of countries in which HIV prevalence rates are high.43
Additionally, while HIV-1 is the world’s predominant strain of the disease, refugees from West African countries have been at increased risk for exposure to HIV-2 and should be tested accordingly.43,44 Refugees may also be at increased risk for HIV and other sexually transmitted infections attributable to physical or sexual violence.43,45
All screening for HIV and other sexually transmitted infections should be performed in a culturally appropriate manner, with the use of trained interpreters as needed, to ensure that all patients receive accurate information and counseling.43
Exposure to Lead
Refugee children are at high risk for lead exposure both before and after their arrival in the US—the latter as a result of their families’ living conditions after resettlement, despite the ban on lead-based paint.25 A study in Minnesota from 2000 to 2002 showed that among refugee children younger than 6, prevalence of lead poisoning was 14 times that found in American children in their age-group.25 In New York City, Asian children have been shown to be at particular risk for lead poisoning—including the case of a year-old Cambodian child who was evidently exposed to an amulet with leaded beads. Sources of lead other than paint may include imported food, spices, cosmetics, pottery, and health remedies.46
Where children were born and where they have lived throughout their lives appear to be the greatest predictors of lead poisoning risk.25 One primary risk factor for lead poisoning is malnutrition, associated with increased absorption of lead in the intestines and the resulting micronutrient deficiencies.25
The CDC recommends:
• Screening for lead in all children from age 6 months to 16 years at the time of their arrival in the US
• Follow-up blood lead testing of children ages 6 months to 6 years, 3 to 6 months after they have moved into a permanent residence25
• Nutritional assessments for children younger than 6 years, as well as measurement of hemoglobin/hematocrit levels, including at least one of the following measurements: mean corpuscular volume with red-cell distribution width, ferritin, transferrin saturation, or reticulocyte hemoglobin content
• Daily multivitamins with iron for refugee children ages 6 months to approximately 5 years.
Lead poisoning, as indicated by a blood lead level (BLL) exceeding 10 g/dL, is known to have neurodevelopmental and cognitive sequelae. In children with a significantly higher BLL, manifestations may include headaches, abdominal pain, anorexia, constipation, clumsiness, agitation, and lethargy in the acute phase.25
Woman, 48, from Afghanistan
Through an interpreter, you learn that this visitor to a local health fair has been experiencing left arm pain since she and her family fled Kabul. When her house there was hit by a rocket, she ran back in, despite a fire, to save her infant daughter. Although she received care as a refugee in Pakistan for burns to her arms and body, she has scarring and strictures the length of her arm. Thanks to the efforts of a volunteer physical therapist, use of the woman’s injured arm has been preserved. She is diagnosed with posttraumatic stress syndrome and referred to a local mental health clinic whose staff specializes in working with survivors of trauma and torture.
Mental Health Issues
Mental health issues are a significant component of refugee health. MacDuff et al47 report that 36% of complementary and alternative medicine use among refugees targets mental health issues resulting from trauma. Because refugees were forced by dangerous conditions to flee their home countries, they are particularly susceptible to mental health concerns. They may have witnessed violence, undergone torture, or been subjected to unsafe or unsanitary conditions in refugee camps. Many have had trouble adjusting to their new culture.23,24,28
As a result, refugees are at increased risk for depression, posttraumatic stress disorder, substance abuse, somatization, psychosis, and suicide.23,28 Mental health issues among refugees are also complicated by the cultural and communication barriers that often exist between refugees and practitioners.23 Thus, practitioners need to take careful histories with sensitivity to their patients’ previous experiences.
While the acuity of these issues begins to decrease around three years after refugees’ arrival in their country of resettlement, the burden of mental health problems often persists for many years.28 Adams et al23 recommend that refugees be referred to social workers, cultural case mediators, and community organizations. Clinicians who do not feel comfortable managing mental health conditions should refer refugee patients to appropriate mental health practitioners and follow up to make sure that patients’ needs are being met.
Musculoskeletal and Neurologic Injuries
Traumatic events can lead to a wide variety of musculoskeletal and neurologic injuries—for example, wounds inflicted by weapons, amputations following land mine injuries, crush injuries from collapsing buildings, or burns sustained in rocket attacks. The array of possibilities necessitates a thorough history and complete musculoskeletal and neurologic assessments.
LANGUAGE AND CULTURAL ISSUES
In addition to being aware of the potential health issues that arise within the refugee population, primary care providers need to be prepared to confront language and cultural issues that may arise. The National Standards on Culturally and Linguistically Appropriate Services (CLAS)48 offer appropriate guidance in 14 key areas.
Refugees frequently have limited or no working knowledge of English. Whenever possible, practitioners should use medically trained interpreters to help them receive and convey accurate information and thus provide comprehensive care. When professional interpreters are not available, telephone interpreter services are available for purchase by the facility or practice. Children or other family members should not be relied on for accurate interpretation.48
As for cultural differences, it is important to note that a refugee’s concept of family may differ from that found in Western culture.49 For example, it is not uncommon to find extended families living together, with members referring to nieces and nephews as their children, or aunts and uncles as their parents. A thorough exploration of the relationships among patients and their families is important, particularly during the family history.
Regardless of where resettled refugees come from, it is probable that their cultural and personal beliefs about medicine differ from those of practitioners with years of Western medicine training. In addition to implementing CLAS guidelines,48 practitioners should be familiar with Kleinman’s3explanatory model, which explores the differences between the patient and practitioner models—not necessarily differences in levels of knowledge, but rather of “values and interests.”3 Thus, people unfamiliar with or resistant to the Western model of medicine are often seen as ignorant, whereas an issue of values may be at play.
Identifying the differences between the patient’s and the clinician’s explanatory models allows the clinician to anticipate and address potential misunderstandings, understand patients’ perceived needs, and involve patients in management strategies that will motivate them to comply with treatment. To help clinicians assess the explanatory models of their patients, Kleinman provides eight questions (shown in Table 3,3,50).
CONCLUSION
As the world becomes more of a global village, increasing numbers of primary care providers will see refugee patients. Practitioners need to be aware of the physical, socioeconomic, and psychological issues that affect refugees during and after resettlement in the US. Refugees may have conditions that could not be addressed in their home country or refugee camp. They may have illnesses with which US practitioners are ordinarily unfamiliar, poorly treated or untreated traumatic injuries, or psychological trauma resulting from conditions that forced them to flee their native lands.
Clinicians who work with refugees should be familiar with the resettlement process and perform a thorough examination after the refugee’s resettlement, managing previously unaddressed health issues. Complete histories must be taken and physical examinations performed in a culturally appropriate manner and an atmosphere of mutual trust.
Finally, it is vital for providers to explore the explanatory models from which patients view their illnesses. Such an understanding facilitates culturally appropriate care with patient participation, and ultimately more positive clinical outcomes.
Authors’ note: The patients portrayed in this article are all composites. While the issues described are real, these “patients” were developed from multiple cases to protect individual patient privacy. None is real, and any resemblance to any real persons is purely accidental.
REFERENCES
1. Ramos M, Orozovich P, Moser K, et al. Health of resettled Iraqi refugees: San Diego County, California, October 2007–September 2009. MMWR Morb Mortal Wkly Rep. 2010;59(49):1614-1618.
2. US Department of State. FY 2010 cumulative summary of refugee admissions. www.wrapsnet .org/reports/archives/tabid/215/language/en-us/default.aspx. Accessed February 17, 2011.
3. Kleinman A, Eisenberg L, Good B. Culture, illness, and care: clinical lessons from anthropologic and cross-cultural research. Ann Intern Med. 1978;88(2):251-258.
4. US Citizenship and Immigration Services. Refugees and asylum. www.uscis.gov/portal/site/uscis/menuitem.eb1d4c2a3e5b9ac89243c6a7543f6d1a/?vgnextoid=1f1c3e4d77d73210VgnVCM100000082ca60aRCRD&vgnextchannel=1f1c3e4d77d73210VgnVCM100000082ca60aRCRD. Accessed February 17, 2011.
5. United Nations High Commissioner for Refugees. Refugees: flowing across borders. www .unhcr.org/pages/49c3646c125.html. Accessed February 17, 2011.
6. US Citizenship and Immigration Services. The United States Refugee Admissions Program (USRAP) consultation and worldwide processing priorities. www.uscis.gov/portal/site/uscis/menuitem.5af9bb95919f35e66f614176543f6d1a/?vgnextoid=796b0eb389683210VgnVCM100000082ca60aRCRD&vgnextchannel=385d3e4d77d73210VgnVCM100000082ca60aRCRD. Accessed February 17, 2011.
7. US Committee for Refugees and Immigrants. Frequently asked questions. www.refugees.org/about-us/faqs.html. Accessed February 17, 2011.
8. US Department of State. Refugee Admissions Reception and Placement Program. www.state
.gov/g/prm/rls/125478.htm. Accessed February 17, 2011.
9. Office of Refugee Resettlement. Report to Congress: FY 2007. www.acf.hhs.gov/programs/orr/data/ORR_2007_report.pdf. Accessed February 17, 2011.
10. CDC. Medical examination: frequently asked questions (FAQs). www.cdc.gov/immigrant
refugeehealth/exams/medical-examination-faqs .html#9. Accessed February 17, 2011.
11. US Department of State. Medical Examination for Immigrant or Refugee Applicant (DS-2053, OMB No. 1405-0113, expiration date 04/30/2012. http://bangkok.usembassy.gov/root/pdfs/med forms_043012.pdf. Accessed February 17, 2011.
12. Cohen J, Powderly WG, Opal SM, eds. Infectious Diseases. 3rd ed. Philadelphia, PA: Elsevier; 2010.
13. CDC. Domestic Refugee Health Program: Frequently Asked Questions (2010). www.cdc.gov/immigrantrefugeehealth/guidelines/domestic/domestic-refugee-questions.html. Accessed February 17, 2011.
14. CDC. Technical Instructions: guidance for HIV for panel physicians and civil surgeons (2010). www.cdc.gov/immigrantrefugeehealth/exams/ti/hiv-guidance-panel-civil.html. Accessed February 17, 2011.
15. CDC. Medical history and physical examination: technical instructions for medical examination of aliens. www.cdc.gov/immigrantrefugee health/exams/ti/panel/technical-instructions/panel-physicians/medical-history-physical-exam .html. Accessed February 17, 2011.
16. Lee JL, Naguwa SM, Cheema GS, Gershwin ME. Acute rheumatic fever and its consequences: a persistent threat to developing nations in the 21st century. Autoimmun Rev. 2009;9(2):117-123.
17. Henderson DN. Pregnancy complicated by rheumatic heart disease. Can Med Assoc J. 1936; 35(4):394-398.
18. US Citizenship and Immigration Services. Refugees. www.uscis.gov/portal/site/uscis/menu item.eb1d4c2a3e5b9ac89243c6a7543f6d1a/?vgnextoid=385d3e4d77d73210VgnVCM100000082ca60aRCRD&vgnextchannel=385d3e4d77d73210VgnVCM100000082ca60aRCRD. Accessed February 17, 2011.
19. US Department of State. 9 FAM appendix O, exhibit II: Promissory note (2007). In: Foreign Affairs Manual Volume 9: Visas. www.state.gov/documents/organization/88070.pdf. Accessed February 17, 2011.
20. United States Department of State. US Refugee Admissions Program. www.state.gov/g/prm/c26471.htm. Accessed February 17, 2011.
21. J. Kernan, Community Relations Officer, US Citizenship and Immigration Services, personal communication, March 29, 2010.
22. Office of Refugee Resettlement. Health. www.acf.hhs.gov/programs/orr/benefits/health .htm. Accessed February 17, 2011.
23. Adams KM, Gardiner LD, Assefi N. Healthcare challenges from the developing world: post-immigration refugee medicine. BMJ. 2004;328(7455): 1548-1552.
24. Walker PF, Jaranson J. Refugee and immigrant health care. Med Clin North Am. 1999; 83(4):1103-1120.
25. CDC. Screening for lead at the domestic refugee medical examination (2005). www.cdc.gov/immigrantrefugeehealth/pdf/lead.pdf. Accessed February 17, 2011.
26. Franco-Paredes C, Dismukes R, Nicolls D, et al. Short report: persistent and untreated tropical infectious diseases among Sudanese refugees in the United States. Am J Trop Med Hyg. 2007;77 (4):633-635.
27. CDC. Immigrant and Refugee Health: Domestic Refugee Health Guidelines: Intestinal Parasites. www.cdc.gov/immigrantrefugeehealth/guidelines/ip/intestinal-parasites-domestic.html#asympto matic2. Accessed February 17, 2011.
28. Carlsten C, Jackson C. Refugee and immigrant health care. EthnoMed. http://ethnomed.org/clinical/refugee-health/carlsten.pdf. Accessed February 17, 2011.
29. Conly JM, Johnston BL. The infectious diseases implications of the “Lost Boys and Girls of Sudan.” Can J Infect Dis Med Microbiol. 2008;19 (3):215-216.
30. Aggarwal B, Sharma M, Singh T. Acute eosinophilic pneumonia due to round worm infestation. Indian J Pediatr. 2008;75(3):296-297.
31. Tsai HC, Lee SS, Liu YC, et al. Clinical manifestations of strongyloidiasis in southern Taiwan.
J Microbiol Immunol Infect. 2002;35(1):29-36.
32. CDC. Reported tuberculosis in the United States, 2008. www.cdc.gov/tb/statistics/reports/2008/pdf/2008report.pdf. Accessed February 17, 2011.
33. Oeltmann JE, Varma JK, Ortega L, et al. Multidrug-resistant tuberculosis outbreak among US-bound Hmong refugees, Thailand, 2005. Emerg Infect Dis. 2008;14(11):1715-1721.
34. Golden MP, Vikram H. Extrapulmonary tuberculosis: an overview. Am Fam Physician. 2005; 72(9):1761-1768.
35. CDC. Tuberculosis (TB) Fact Sheets: BCG Vaccine. www.cdc.gov/tb/publications/factsheets/prevention/BCG.htm. Accessed February 17, 2011.
36. The role of BCG vaccine in the prevention and control of tuberculosis in the United States: a joint statement by the Advisory Council for the Elimination of Tuberculosis and the Advisory Committee on Immunization Practices. MMWR Recomm Rep. 1996;45(RR-4):1-18.
37. Museru OI, Vargas M, Kinyua M, et al. Hepatitis B virus infection among refugees resettled in the US: high prevalence and challenges in access to health care. J Immigr Minor Health. 2010;12 (6):823-827.
38. World Health Organization, UNAIDS, UNDP, UNECA, UNESO, UNFPA, UNHCHR, UNHCR, UNICEF, UNIFEM. Eliminating Female Genital Mutilation: An Interagency Statement (2008). http://whqlibdoc.who.int/publications/2008/ 9789241596442_eng.pdf. Accessed February 17, 2010.
39. United Nations Children’s Fund. Female Genital Mutilation/Cutting: A Statistical Exploration (2005). www.unicef.org/publications/files/FGM-C_final_10_October.pdf. Accessed February 17, 2011.
40. Yoder PS, Abderrahim N, Zhuzhuni A. DHS Comparative Reports No. 7: Female Genital Cutting in the Demographic and Health Surveys: A Critical and Comparative Analysis. Calverton, MD: ORC Macro. September 2004.
41. Royal College of Obstetricians and Gynaecologists. Female Genital Mutilation and its Management (Green-top Guideline No. 53; 2009). www .rcog.org.uk/files/rcog-corp/GreenTop53Female GenitalMutilation.pdf. Accessed February 17, 2011.
42. CDC. Final Rule Removing HIV Infection from U.S. Immigration Screening: Revision of 42 CFR Part 34 (Medical Examination of Aliens) Removal of Human Immunodeficiency Virus (HIV) from Definition of Communicable Disease of Public Health Significance—Final Rule. www.cdc.gov/immigrantrefugeehealth/laws-regs/hiv-ban-removal/final-rule.html. Accessed February 17, 2011.
43. CDC. Immigrant and Refugee Health: Screening for HIV-infection during the refugee domestic medical examination. www.cdc.gov/immigrant
refugeehealth/guidelines/domestic/screening-
hiv-infection-domestic.html. Accessed February 17, 2011.
44. CDC. Human Immunodeficiency Virus Type 2: HIV/AIDS Fact Sheets. Atlanta: Centers for Disease Control and Prevention; 2007.
45. Mills EJ, Nachega JB. HIV infection as a weapon of war. Lancet Infect Dis. 2006;6(12):752-753.
46. CDC. Lead poisoning of a child associated with use of a Cambodian amulet—New York City, 2009. MMWR Morb Mortal Wkly Rep. 2011;60(3): 69-71.
47. MacDuff S, Grodin MA, Gardiner P. The use of complementary and alternative medicine among refugees: a systematic review. J Immigr Minor Health. 2010 Mar 12 [Epub ahead of print].
48. US Department of Health and Human Services, Office of Minority Health. National standards on culturally and linguistically appropriate services (CLAS). http://minorityhealth.hhs.gov/templates/browse.aspx?lvl=2&lvlID=15. Accessed February 17, 2011.
49. Haviland WA, Prins HEL, Walrath D, McBride B, eds. Cultural Anthropology: The Human Challenge. 12th ed. Belmont, CA: Wadsworth Publishing; 2008.
50. Fadiman A. The Spirit Catches You and You Fall Down: A Hmong Child, Her American Doctors, and the Collision of Two Cultures. New York, NY: Farrar, Straus and Giroux; 1997.
It is estimated that three million refugees from all over the world—forced to flee their native countries for various reasons—have entered the United States since 1980.1,2 Prior to resettling in the US, refugees undergo health screenings for high-risk infectious diseases that preclude emigration; those free of such diseases may enter. However, the civil surgeon who conducts a refugee’s medical examination does not screen for chronic diseases that are not considered a threat to public health. Other infectious illnesses, previous traumatic injuries, and mental health issues may also go undetected at this exam.
Refugees may have had little or no access to health care before their arrival in the US, lived in conditions that increased their risk for exposure to various illnesses, and experienced traumatic events before fleeing their native lands. After their arrival, refugees may face access issues, including language and cultural barriers, health care ineligibility, and lack of transportation. This article seeks to increase awareness among primary care practitioners of the needs and issues of refugees who may be seen in their practices for conditions that developed before their arrival in the US and others emerging since their resettlement.
This activity will begin with an overview of who refugees are, how they come to reside in the US, and the medical process they undergo before resettlement. Next follows a discussion of medical issues that practitioners should be aware of among refugees, including conditions not commonly seen in the US. Finally, language and cultural issues will be addressed, including an explanatory model3 to help bridge discrepancies between practitioners of Western medicine and patients of non-Western traditions.
Man, 58, from Burundi
At age 55, the patient was resettled to the US with his family. Since then, he has had trouble holding a job, and his difficulties have been attributed to the stress of transition to life in the US. His current employer has sent him for an occupational examination. Findings are within normal limits except for visual acuity, which is tested at 20/25 in his right eye and 20/200 in his left. When asked, the patient reports having had “river blindness,” that is, onchocerciasis, as a child. Onchocerciasis is an uncommon cause of permanent blindness.
BACKGROUND AND DEFINITIONS
Refugees are defined by US Citizenship and Immigration Services4 as “people who have been persecuted or fear they will be persecuted on account of race, religion, nationality, and/or membership in a particular social group or political opinion.” The United Nations High Commission for Refugees (UNHCR)5 adds that a refugee “is outside the country of his nationality, and is unable to, or owing to such fear, is unwilling to, avail himself of the protection of that country.”
The man from Burundi came to the US through a long, complicated process. His family fled genocide in their native country to a refugee camp in Tanzania. Once there, they attained official refugee status, an essential part of the resettlement process. Refugees must fall into one of three processing priority categories:
(1) those referred by UNHCR, a US embassy, or a designated voluntary agency
(2) persons designated by a US refugee program as belonging to a “special humanitarian concern” group
(3) certain family members of refugees who currently reside in the US.6
The application generally involves biographical information and a family tree.7 Because they had fled their home, the family from Burundi had limited paperwork but were referred by UNHCR to the US for resettlement.
Once refugees become eligible for resettlement in the US, they undergo medical screening, security clearance, and cultural orientation. They are then placed by one of the sponsoring resettlement agencies listed in Table 1.8 This process can take from two months to several years.9 The medical screening may be performed by a panel physician, an overseas practitioner who examines refugees prior to their resettlement; or by a civil surgeon, who examines refugees after their arrival in the US—generally when the refugee applies for status adjustment.10
The man from Burundi represents a relatively common issue among refugees in the US. Many chronic conditions go untreated within this population because follow-up may be inadequate or absent, patients’ access to health care is insufficient, or the health care provider is unfamiliar with refugee issues. In this case, evaluation of the man’s vision was not part of the routine examination conducted in all refugees. Because he was never offered a subsequent vision check, his blindness went unnoticed, and his work difficulties were attributed to language and adjustment issues.
His visual problem could not be corrected, but once it was identified, accommodations were made in the workplace that facilitated his adjustment to the new work environment.
Girl, 16, from Liberia
This patient, who is being seen in your office for a sports physical, arrived in the US three years ago. Her medical screening at the time of immigration indicated “good health,” and she has had no health problems since then. Her exam seems unremarkable except for a low-pitched, rumbling, diastolic murmur best heard with the bell of the stethoscope near the apex when she lies in the left lateral decubitus position.
HEALTH SCREENINGS
Before coming to the US, refugees must undergo a health evaluation that includes a thorough medical history, full physical examination, chest x-ray, if indicated, for tuberculosis (TB), vaccination verification, and laboratory work as needed to identify specific infectious diseases.11 Screenings included in this evaluation target problems that are considered important from a public health perspective, including TB and certain sexually transmitted illnesses. Many infectious diseases are not considered a threat to public health because the requisite vector is not present in the US (eg, malaria, schistosomiasis).12
Public health conditions are categorized as Class A or Class B (see Table 2,11,13). Typically, refugees with a Class A condition are considered ineligible for admission to the US. Presence of a Class B condition must be brought to the attention of consular authorities, as it may indicate future disability or need for medical treatment.13,14
It is important for practitioners to know that if an illness or medical condition is discovered during the panel physician’s examination but is not considered “relevant to the visa medical examination,” the panel physician does not treat the patient. Rather, he or she recommends that the patient seek care from a medical provider.15 Essentially, refugees with a condition that is not considered a public health threat are allowed into the US, whether or not the condition has been addressed—as in the case of the diastolic heart murmur in the girl from Liberia.
This heart murmur could be a complication of rheumatic fever secondary to untreated group A streptococcal infection. In developing nations, rheumatic heart disease is the most commonly acquired heart condition, frequently exceeding congenital heart disease as a cause of hospitalization among children, adolescents, and teens.16 The risks associated with pregnancy in women with rheumatic heart disease have long been known,17 but as rheumatic heart disease has become less common in the developed nations, so has the sequela of mitral valve stenosis.
Clinicians need to become familiar with other illnesses commonly found in the developing nations, such as malaria and measles.12 Furthermore, practitioners should be aware that refugees may be immunologically susceptible to pathogens endemic to the countries of resettlement.
Woman, 65, from Bhutan
Forcibly deported from Bhutan to Nepal, this patient resettled to the US four years ago. She neither reads nor writes in her first language (Nepali) nor in English. She has been attending English language classes since her arrival in the US but has made little progress. The woman visits a health fair, bringing with her nine medications, including two bottles of insulin and three empty bottles for three different antihypertensive medications. Through an interpreter, you learn that the woman is not taking any of these medications regularly. She is also unaware that she should neither reuse needles nor share her medications with her son, who is also diabetic. She cannot afford to refill her prescriptions.
THE PROCESS, THE BARRIERS
Upon their arrival in the US, refugees receive 30 to 90 days’ support for “housing, essential furnishings, food, clothing, community orientation, and referral to other social, medical, and employment services.”8 In addition to the predeparture medical screening, refugees receive assistance for travel arrangements and a loan to pay for travel to the US.18 Refugees must sign a promissory note indicating that they will begin repayment of the loan within six months of their arrival and will complete repayment within 42months.19
At the time of their arrival, refugees apply for a Social Security number, register their children for school, undergo another medical evaluation, and receive English language training, if needed.8 Within six months of their arrival, refugees of working age are expected to have obtained employment.7 After one year in the US, refugees must apply for Legal Permanent Resident Status; after five years, they can apply for citizenship.8,20,21
In the case of the woman from Bhutan, neither diabetes nor hypertension precluded her resettlement; however, several factors now complicate her health care. Although she has access to health care providers, she cannot afford copayments for her medications, nor does she understand the instructions for their use. That she is not literate in any language complicates the challenge for her to learn to speak English. Her lack of linguistic and health literacy adds to the financial burden of the medications she needs.
The use of formally trained medical interpreters can alleviate some, but not all, of these problems. The refugee who does not become a citizen within seven years risks losing all benefits, including Medicare and Medicaid. This is particularly problematic for older refugees with multiple health problems. The process of becoming a US citizen is arduous, including lessons in civics and a required level of language fluency that is difficult to attain, particularly for those who are not literate in any language.
The Office of Refugee Resettlement22 recommends that refugees undergo a second medical screening after their arrival to identify any conditions that were not addressed by the panel physician. This examination, according to the CDC, “provides an opportunity to identify important causes of morbidity among resettled refugees that might not have been discovered previously, and enables early referral for treatment and follow-up care.”1 This screening also offers refugees the chance to establish a medical home and to begin to become familiar with the US health care system, potential barriers notwithstanding.
Girl, 15, from Sudan
A cough is the presenting symptom in this girl, who resettled to the US three years ago. She has no other upper respiratory symptoms. Results of laboratory testing indicate eosinophilia and mild anemia.
COMMON HEALTH ISSUES
Health conditions that refugees face but that may not be found in other immigrants or nonimmigrants include TB, hepatitis, parasites, HIV and other sexually transmitted infections, and mental health issues.23,24 For some refugees, female genital mutilation/cutting (FGM/C)23 or lead exposure25 may be a significant concern. Additionally, the traumatic events that led refugees to flee their homes may have resulted in musculoskeletal or neurologic injuries with a wide array of manifestations.
Parasites
Parasitic infections are common among refugees, and these can lead to anemia resulting from blood loss and iron deficiency, malnutrition, growth retardation, invasive illnesses, and death.26,27 According to Carlsten and Jackson,28 immigrants can be infected by multiple pathogens simultaneously, and some parasites may survive for as long as decades.
The most common parasitic infections among refugees are hookworm, whipworm, roundworm, and Giardia lamblia.23 In a screening performed five years after the arrival in the US of the “Lost Boys and Girls of Sudan,” 64% of a cohort of the boys living in Atlanta tested positive for Schistosoma mansoni or Schistosoma haematobium, and 25% tested positive for Strongyloides stercoralis—the organisms responsible for schistosomiasis and strongyloidiasis, respectively.26 In 2005, the CDC recommended presumptive treatment for both illnesses in Sudanese refugees who were not treated for these infections before their resettlement.29
Despite treatment and prophylaxis prior to refugees’ departure for the US, parasitic infections remain common in the refugee population.23 Practitioners should be aware that a cough could indicate the presence of roundworms that have entered the body through the skin and spread to the lungs via the blood.30,31 All refugees should be screened for eosinophilia to detect parasitic infections.23 An absolute eosinophil count exceeding 400 cells/L warrants further investigation.27
Because of presumptive treatment for malaria given to nonpregnant refugees, this disease is rarely seen after refugees’ arrival in the US.23 However, practitioners should not overlook the possibility of malaria when they examine refugee patients, as malaria may take time to manifest clinically.24
Tuberculosis
While refugees cannot be admitted into the US with active, infectious TB (a Class A disease), the majority of cases of TB in the US occur among foreign-born individuals, with prevalence 10 times that in the US-born population.32 Refugees are at particular risk for TB.33
When examining refugee patients, especially those recently arrived in the US, clinicians should be aware of the potential for extrapulmonary TB, which accounted for 20% of TB cases in the US in 2008.32 Extrapulmonary TB can be found anywhere in the body, with more common sites including the lymph nodes, pleura, and osteoarticular areas. Skeletal TB accounts for 35% of extrapulmonary TB cases—most commonly Pott’s disease, or spinal TB.34
Use of bacille Calmette-Guerin (BCG), a vaccine given in various countries to prevent childhood tuberculous meningitis and miliary disease, often leads to confusion when the tuberculin skin test (TST, previously known as the purified protein derivative, or PPD) is used to screen for TB.35 While BCG can increase the number of false-positive TST results, TST reaction following BCG decreases with time and generally is not seen longer than 10 years postvaccination.36
Furthermore, the immunity produced by BCG weakens over time; thus, an adult, though immunized as an infant, is at risk for TB infection. The CDC currently recommends the same testing for TB, whether or not patients have undergone BCG vaccination. Similarly, TST results should be interpreted in the same way for BCG-vaccinated patients and nonvaccinated patients alike.35
Finally, BCG does not affect results of blood tests for TB. However, these tests are new, expensive, and not available everywhere.35
Hepatitis
Among the forms of hepatitis, hepatitis B virus (HBV) is of greatest concern within the refugee community, as it is endemic to much of the world.37 Between 2003 and 2007, 10.7% of refugees screened in DeKalb County, Georgia, for HBsAg (the hepatitis B surface antigen that indicates exposure to the virus) tested positive, accounting for 43.3% of HBsAg-positive test results in the county during that period. Chronic HBV infection can lead to end-stage liver disease, cirrhosis, and hepatocellular carcinoma.37
Museru et al37 recommend that health care providers ascertain the hepatitis B–serological status of resettled refugees from areas that are highly endemic for HBV infection. In addition, Adams and colleagues23 recommend screening patients who have undergone blood transfusions, female genital surgery, or other surgical procedures in their countries of origin, as well as patients from Africa or southeast Asia, for hepatitis C.23
Mutilation or Cutting of the Female Genitalia
Ritual FGM/C is the practice of injuring or removing part or all of the external female genitalia for cultural and other nonmedical reasons.38 FGM/C is primarily practiced in Africa (see Figure,39,40) but may occur also in Asia, the Middle East, and Central and South America.38 It is often practiced by informally trained individuals, with “inexact surgical outcomes.”23 FGM/C has been outlawed in the US and other countries with large immigrant populations; some nations grant asylum to women who fear being subjected to FGM/C if they return to their country of origin.39
Practitioners who care for female refugees should be aware of both the short-term sequelae (pain, bleeding, trauma, sepsis) and additional long-term sequelae (dyspareunia, urinary retention and recurrent urinary tract infections, chronic pelvic inflammatory disease, keloid scar formation, childbirth complications) of FGM/C, in addition to psychological sequelae.23,38,41 It is important to approach affected patients with sympathy and without judgment, as the decision to undergo FGM/C may not have been theirs.41
The Royal College of Obstetricians and Gynaecologists in the United Kingdom has produced a helpful set of guidelines, Female Genital Mutilation and its Management,41 for clinicians working with patients who have undergone FGM/C.
Sexually Transmitted Infections
In light of a new law allowing refugees with HIV to be resettled in the US,42 practitioners must now be aware of the possibility of HIV infection in a refugee patient, whether documented or not. Practitioners should follow the same guidelines for refugees as they do for all patients regarding HIV screening and counseling, including allowing patients the opportunity to decline testing.43 However, they should also be aware of countries in which HIV prevalence rates are high.43
Additionally, while HIV-1 is the world’s predominant strain of the disease, refugees from West African countries have been at increased risk for exposure to HIV-2 and should be tested accordingly.43,44 Refugees may also be at increased risk for HIV and other sexually transmitted infections attributable to physical or sexual violence.43,45
All screening for HIV and other sexually transmitted infections should be performed in a culturally appropriate manner, with the use of trained interpreters as needed, to ensure that all patients receive accurate information and counseling.43
Exposure to Lead
Refugee children are at high risk for lead exposure both before and after their arrival in the US—the latter as a result of their families’ living conditions after resettlement, despite the ban on lead-based paint.25 A study in Minnesota from 2000 to 2002 showed that among refugee children younger than 6, prevalence of lead poisoning was 14 times that found in American children in their age-group.25 In New York City, Asian children have been shown to be at particular risk for lead poisoning—including the case of a year-old Cambodian child who was evidently exposed to an amulet with leaded beads. Sources of lead other than paint may include imported food, spices, cosmetics, pottery, and health remedies.46
Where children were born and where they have lived throughout their lives appear to be the greatest predictors of lead poisoning risk.25 One primary risk factor for lead poisoning is malnutrition, associated with increased absorption of lead in the intestines and the resulting micronutrient deficiencies.25
The CDC recommends:
• Screening for lead in all children from age 6 months to 16 years at the time of their arrival in the US
• Follow-up blood lead testing of children ages 6 months to 6 years, 3 to 6 months after they have moved into a permanent residence25
• Nutritional assessments for children younger than 6 years, as well as measurement of hemoglobin/hematocrit levels, including at least one of the following measurements: mean corpuscular volume with red-cell distribution width, ferritin, transferrin saturation, or reticulocyte hemoglobin content
• Daily multivitamins with iron for refugee children ages 6 months to approximately 5 years.
Lead poisoning, as indicated by a blood lead level (BLL) exceeding 10 g/dL, is known to have neurodevelopmental and cognitive sequelae. In children with a significantly higher BLL, manifestations may include headaches, abdominal pain, anorexia, constipation, clumsiness, agitation, and lethargy in the acute phase.25
Woman, 48, from Afghanistan
Through an interpreter, you learn that this visitor to a local health fair has been experiencing left arm pain since she and her family fled Kabul. When her house there was hit by a rocket, she ran back in, despite a fire, to save her infant daughter. Although she received care as a refugee in Pakistan for burns to her arms and body, she has scarring and strictures the length of her arm. Thanks to the efforts of a volunteer physical therapist, use of the woman’s injured arm has been preserved. She is diagnosed with posttraumatic stress syndrome and referred to a local mental health clinic whose staff specializes in working with survivors of trauma and torture.
Mental Health Issues
Mental health issues are a significant component of refugee health. MacDuff et al47 report that 36% of complementary and alternative medicine use among refugees targets mental health issues resulting from trauma. Because refugees were forced by dangerous conditions to flee their home countries, they are particularly susceptible to mental health concerns. They may have witnessed violence, undergone torture, or been subjected to unsafe or unsanitary conditions in refugee camps. Many have had trouble adjusting to their new culture.23,24,28
As a result, refugees are at increased risk for depression, posttraumatic stress disorder, substance abuse, somatization, psychosis, and suicide.23,28 Mental health issues among refugees are also complicated by the cultural and communication barriers that often exist between refugees and practitioners.23 Thus, practitioners need to take careful histories with sensitivity to their patients’ previous experiences.
While the acuity of these issues begins to decrease around three years after refugees’ arrival in their country of resettlement, the burden of mental health problems often persists for many years.28 Adams et al23 recommend that refugees be referred to social workers, cultural case mediators, and community organizations. Clinicians who do not feel comfortable managing mental health conditions should refer refugee patients to appropriate mental health practitioners and follow up to make sure that patients’ needs are being met.
Musculoskeletal and Neurologic Injuries
Traumatic events can lead to a wide variety of musculoskeletal and neurologic injuries—for example, wounds inflicted by weapons, amputations following land mine injuries, crush injuries from collapsing buildings, or burns sustained in rocket attacks. The array of possibilities necessitates a thorough history and complete musculoskeletal and neurologic assessments.
LANGUAGE AND CULTURAL ISSUES
In addition to being aware of the potential health issues that arise within the refugee population, primary care providers need to be prepared to confront language and cultural issues that may arise. The National Standards on Culturally and Linguistically Appropriate Services (CLAS)48 offer appropriate guidance in 14 key areas.
Refugees frequently have limited or no working knowledge of English. Whenever possible, practitioners should use medically trained interpreters to help them receive and convey accurate information and thus provide comprehensive care. When professional interpreters are not available, telephone interpreter services are available for purchase by the facility or practice. Children or other family members should not be relied on for accurate interpretation.48
As for cultural differences, it is important to note that a refugee’s concept of family may differ from that found in Western culture.49 For example, it is not uncommon to find extended families living together, with members referring to nieces and nephews as their children, or aunts and uncles as their parents. A thorough exploration of the relationships among patients and their families is important, particularly during the family history.
Regardless of where resettled refugees come from, it is probable that their cultural and personal beliefs about medicine differ from those of practitioners with years of Western medicine training. In addition to implementing CLAS guidelines,48 practitioners should be familiar with Kleinman’s3explanatory model, which explores the differences between the patient and practitioner models—not necessarily differences in levels of knowledge, but rather of “values and interests.”3 Thus, people unfamiliar with or resistant to the Western model of medicine are often seen as ignorant, whereas an issue of values may be at play.
Identifying the differences between the patient’s and the clinician’s explanatory models allows the clinician to anticipate and address potential misunderstandings, understand patients’ perceived needs, and involve patients in management strategies that will motivate them to comply with treatment. To help clinicians assess the explanatory models of their patients, Kleinman provides eight questions (shown in Table 3,3,50).
CONCLUSION
As the world becomes more of a global village, increasing numbers of primary care providers will see refugee patients. Practitioners need to be aware of the physical, socioeconomic, and psychological issues that affect refugees during and after resettlement in the US. Refugees may have conditions that could not be addressed in their home country or refugee camp. They may have illnesses with which US practitioners are ordinarily unfamiliar, poorly treated or untreated traumatic injuries, or psychological trauma resulting from conditions that forced them to flee their native lands.
Clinicians who work with refugees should be familiar with the resettlement process and perform a thorough examination after the refugee’s resettlement, managing previously unaddressed health issues. Complete histories must be taken and physical examinations performed in a culturally appropriate manner and an atmosphere of mutual trust.
Finally, it is vital for providers to explore the explanatory models from which patients view their illnesses. Such an understanding facilitates culturally appropriate care with patient participation, and ultimately more positive clinical outcomes.
Authors’ note: The patients portrayed in this article are all composites. While the issues described are real, these “patients” were developed from multiple cases to protect individual patient privacy. None is real, and any resemblance to any real persons is purely accidental.
REFERENCES
1. Ramos M, Orozovich P, Moser K, et al. Health of resettled Iraqi refugees: San Diego County, California, October 2007–September 2009. MMWR Morb Mortal Wkly Rep. 2010;59(49):1614-1618.
2. US Department of State. FY 2010 cumulative summary of refugee admissions. www.wrapsnet .org/reports/archives/tabid/215/language/en-us/default.aspx. Accessed February 17, 2011.
3. Kleinman A, Eisenberg L, Good B. Culture, illness, and care: clinical lessons from anthropologic and cross-cultural research. Ann Intern Med. 1978;88(2):251-258.
4. US Citizenship and Immigration Services. Refugees and asylum. www.uscis.gov/portal/site/uscis/menuitem.eb1d4c2a3e5b9ac89243c6a7543f6d1a/?vgnextoid=1f1c3e4d77d73210VgnVCM100000082ca60aRCRD&vgnextchannel=1f1c3e4d77d73210VgnVCM100000082ca60aRCRD. Accessed February 17, 2011.
5. United Nations High Commissioner for Refugees. Refugees: flowing across borders. www .unhcr.org/pages/49c3646c125.html. Accessed February 17, 2011.
6. US Citizenship and Immigration Services. The United States Refugee Admissions Program (USRAP) consultation and worldwide processing priorities. www.uscis.gov/portal/site/uscis/menuitem.5af9bb95919f35e66f614176543f6d1a/?vgnextoid=796b0eb389683210VgnVCM100000082ca60aRCRD&vgnextchannel=385d3e4d77d73210VgnVCM100000082ca60aRCRD. Accessed February 17, 2011.
7. US Committee for Refugees and Immigrants. Frequently asked questions. www.refugees.org/about-us/faqs.html. Accessed February 17, 2011.
8. US Department of State. Refugee Admissions Reception and Placement Program. www.state
.gov/g/prm/rls/125478.htm. Accessed February 17, 2011.
9. Office of Refugee Resettlement. Report to Congress: FY 2007. www.acf.hhs.gov/programs/orr/data/ORR_2007_report.pdf. Accessed February 17, 2011.
10. CDC. Medical examination: frequently asked questions (FAQs). www.cdc.gov/immigrant
refugeehealth/exams/medical-examination-faqs .html#9. Accessed February 17, 2011.
11. US Department of State. Medical Examination for Immigrant or Refugee Applicant (DS-2053, OMB No. 1405-0113, expiration date 04/30/2012. http://bangkok.usembassy.gov/root/pdfs/med forms_043012.pdf. Accessed February 17, 2011.
12. Cohen J, Powderly WG, Opal SM, eds. Infectious Diseases. 3rd ed. Philadelphia, PA: Elsevier; 2010.
13. CDC. Domestic Refugee Health Program: Frequently Asked Questions (2010). www.cdc.gov/immigrantrefugeehealth/guidelines/domestic/domestic-refugee-questions.html. Accessed February 17, 2011.
14. CDC. Technical Instructions: guidance for HIV for panel physicians and civil surgeons (2010). www.cdc.gov/immigrantrefugeehealth/exams/ti/hiv-guidance-panel-civil.html. Accessed February 17, 2011.
15. CDC. Medical history and physical examination: technical instructions for medical examination of aliens. www.cdc.gov/immigrantrefugee health/exams/ti/panel/technical-instructions/panel-physicians/medical-history-physical-exam .html. Accessed February 17, 2011.
16. Lee JL, Naguwa SM, Cheema GS, Gershwin ME. Acute rheumatic fever and its consequences: a persistent threat to developing nations in the 21st century. Autoimmun Rev. 2009;9(2):117-123.
17. Henderson DN. Pregnancy complicated by rheumatic heart disease. Can Med Assoc J. 1936; 35(4):394-398.
18. US Citizenship and Immigration Services. Refugees. www.uscis.gov/portal/site/uscis/menu item.eb1d4c2a3e5b9ac89243c6a7543f6d1a/?vgnextoid=385d3e4d77d73210VgnVCM100000082ca60aRCRD&vgnextchannel=385d3e4d77d73210VgnVCM100000082ca60aRCRD. Accessed February 17, 2011.
19. US Department of State. 9 FAM appendix O, exhibit II: Promissory note (2007). In: Foreign Affairs Manual Volume 9: Visas. www.state.gov/documents/organization/88070.pdf. Accessed February 17, 2011.
20. United States Department of State. US Refugee Admissions Program. www.state.gov/g/prm/c26471.htm. Accessed February 17, 2011.
21. J. Kernan, Community Relations Officer, US Citizenship and Immigration Services, personal communication, March 29, 2010.
22. Office of Refugee Resettlement. Health. www.acf.hhs.gov/programs/orr/benefits/health .htm. Accessed February 17, 2011.
23. Adams KM, Gardiner LD, Assefi N. Healthcare challenges from the developing world: post-immigration refugee medicine. BMJ. 2004;328(7455): 1548-1552.
24. Walker PF, Jaranson J. Refugee and immigrant health care. Med Clin North Am. 1999; 83(4):1103-1120.
25. CDC. Screening for lead at the domestic refugee medical examination (2005). www.cdc.gov/immigrantrefugeehealth/pdf/lead.pdf. Accessed February 17, 2011.
26. Franco-Paredes C, Dismukes R, Nicolls D, et al. Short report: persistent and untreated tropical infectious diseases among Sudanese refugees in the United States. Am J Trop Med Hyg. 2007;77 (4):633-635.
27. CDC. Immigrant and Refugee Health: Domestic Refugee Health Guidelines: Intestinal Parasites. www.cdc.gov/immigrantrefugeehealth/guidelines/ip/intestinal-parasites-domestic.html#asympto matic2. Accessed February 17, 2011.
28. Carlsten C, Jackson C. Refugee and immigrant health care. EthnoMed. http://ethnomed.org/clinical/refugee-health/carlsten.pdf. Accessed February 17, 2011.
29. Conly JM, Johnston BL. The infectious diseases implications of the “Lost Boys and Girls of Sudan.” Can J Infect Dis Med Microbiol. 2008;19 (3):215-216.
30. Aggarwal B, Sharma M, Singh T. Acute eosinophilic pneumonia due to round worm infestation. Indian J Pediatr. 2008;75(3):296-297.
31. Tsai HC, Lee SS, Liu YC, et al. Clinical manifestations of strongyloidiasis in southern Taiwan.
J Microbiol Immunol Infect. 2002;35(1):29-36.
32. CDC. Reported tuberculosis in the United States, 2008. www.cdc.gov/tb/statistics/reports/2008/pdf/2008report.pdf. Accessed February 17, 2011.
33. Oeltmann JE, Varma JK, Ortega L, et al. Multidrug-resistant tuberculosis outbreak among US-bound Hmong refugees, Thailand, 2005. Emerg Infect Dis. 2008;14(11):1715-1721.
34. Golden MP, Vikram H. Extrapulmonary tuberculosis: an overview. Am Fam Physician. 2005; 72(9):1761-1768.
35. CDC. Tuberculosis (TB) Fact Sheets: BCG Vaccine. www.cdc.gov/tb/publications/factsheets/prevention/BCG.htm. Accessed February 17, 2011.
36. The role of BCG vaccine in the prevention and control of tuberculosis in the United States: a joint statement by the Advisory Council for the Elimination of Tuberculosis and the Advisory Committee on Immunization Practices. MMWR Recomm Rep. 1996;45(RR-4):1-18.
37. Museru OI, Vargas M, Kinyua M, et al. Hepatitis B virus infection among refugees resettled in the US: high prevalence and challenges in access to health care. J Immigr Minor Health. 2010;12 (6):823-827.
38. World Health Organization, UNAIDS, UNDP, UNECA, UNESO, UNFPA, UNHCHR, UNHCR, UNICEF, UNIFEM. Eliminating Female Genital Mutilation: An Interagency Statement (2008). http://whqlibdoc.who.int/publications/2008/ 9789241596442_eng.pdf. Accessed February 17, 2010.
39. United Nations Children’s Fund. Female Genital Mutilation/Cutting: A Statistical Exploration (2005). www.unicef.org/publications/files/FGM-C_final_10_October.pdf. Accessed February 17, 2011.
40. Yoder PS, Abderrahim N, Zhuzhuni A. DHS Comparative Reports No. 7: Female Genital Cutting in the Demographic and Health Surveys: A Critical and Comparative Analysis. Calverton, MD: ORC Macro. September 2004.
41. Royal College of Obstetricians and Gynaecologists. Female Genital Mutilation and its Management (Green-top Guideline No. 53; 2009). www .rcog.org.uk/files/rcog-corp/GreenTop53Female GenitalMutilation.pdf. Accessed February 17, 2011.
42. CDC. Final Rule Removing HIV Infection from U.S. Immigration Screening: Revision of 42 CFR Part 34 (Medical Examination of Aliens) Removal of Human Immunodeficiency Virus (HIV) from Definition of Communicable Disease of Public Health Significance—Final Rule. www.cdc.gov/immigrantrefugeehealth/laws-regs/hiv-ban-removal/final-rule.html. Accessed February 17, 2011.
43. CDC. Immigrant and Refugee Health: Screening for HIV-infection during the refugee domestic medical examination. www.cdc.gov/immigrant
refugeehealth/guidelines/domestic/screening-
hiv-infection-domestic.html. Accessed February 17, 2011.
44. CDC. Human Immunodeficiency Virus Type 2: HIV/AIDS Fact Sheets. Atlanta: Centers for Disease Control and Prevention; 2007.
45. Mills EJ, Nachega JB. HIV infection as a weapon of war. Lancet Infect Dis. 2006;6(12):752-753.
46. CDC. Lead poisoning of a child associated with use of a Cambodian amulet—New York City, 2009. MMWR Morb Mortal Wkly Rep. 2011;60(3): 69-71.
47. MacDuff S, Grodin MA, Gardiner P. The use of complementary and alternative medicine among refugees: a systematic review. J Immigr Minor Health. 2010 Mar 12 [Epub ahead of print].
48. US Department of Health and Human Services, Office of Minority Health. National standards on culturally and linguistically appropriate services (CLAS). http://minorityhealth.hhs.gov/templates/browse.aspx?lvl=2&lvlID=15. Accessed February 17, 2011.
49. Haviland WA, Prins HEL, Walrath D, McBride B, eds. Cultural Anthropology: The Human Challenge. 12th ed. Belmont, CA: Wadsworth Publishing; 2008.
50. Fadiman A. The Spirit Catches You and You Fall Down: A Hmong Child, Her American Doctors, and the Collision of Two Cultures. New York, NY: Farrar, Straus and Giroux; 1997.