User login
Evaluation of suspected left ventricular systolic dysfunction
- Heart failure is an increasingly common problem in primary care, with a mortality rate higher than that of most cancers.
- The absence of dyspnea on exertion or a normal electrocardiogram (ECG) result indicates that heart failure is unlikely; a gallop rhythm or laterally displaced apical rhythm is strong evidence in favor of heart failure.
- The history and physical examination and ECG alone are usually inadequate to confirm diagnosis of left ventricular systolic dysfunction, and echocardiography remains the gold standard to confirm the diagnosis.
Heart failure is increasing in incidence and prevalence; it currently affects 0.4% to 2% of the general population and 8% to 10% of the elderly.1,2 In the United States, heart failure is the second most common cardiovascular reason for an outpatient visit in the ambulatory care setting and remains the most common cause for hospitalization among patients older than 65 years.3 The total cost for heart failure management in 1999 was estimated to approach $56 billion.4 Those suffering with this illness experience high levels of morbidity and mortality5 that are reflected in the workloads of both primary and secondary care. Heart failure admission rates are rising, and the prognosis of heart failure has been compared with that of malignancy, with a 6-year mortality rate of 84% in men and 77% in women.6,7
A number of heart failure guidelines8-14 provide direction regarding “best practice” with regard to diagnosis and management. These guidelines have all been produced by expert panels and base their evidence on systematic critical reviews of the literature, plus expert consensus opinion. The evidence underlying the development of these guidelines ranges from well-conducted randomized controlled trials to expert opinion. These guidelines all emphasize the ways in which approaches to the diagnosis and management of heart failure have altered substantially in recent years and are continuing to change rapidly. The need to detect heart failure at an early stage to slow the progression of left ventricular systolic dysfunction (LVSD) is now well accepted.15
The following provides an overview of the current recommended approaches to diagnosis, focusing specifically on LVSD, the most common type of heart failure and also the usual focus of most guidelines. Accurate diagnosis of LVSD is the single most important step in management.16 An adequate diagnosis should establish the existence of heart failure, differentiate systolic from diastolic dysfunction, and identify the main underlying cause and any subsidiary diagnoses that may exacerbate heart failure. The etiology of heart failure and the presence of exacerbating factors or other diseases need to be carefully considered in all patients. Coronary artery disease remains the most common potentially reversible etiologic factor in heart failure.8
Using the history and physical examination
The major symptoms of heart failure are fatigue, exercise intolerance, exertional dyspnea, orthopnea, paroxysmal nocturnal dyspnea, and dependent edema. However, such symptoms are similar to those of many other diseases, particularly pulmonary diseases. For example, exertional dypsnea is a common symptom in heart failure but can be due to a wide range of other causes, such as chronic obstructive pulmonary disease, interstitial lung disease, asthma, respiratory infection, deconditioning, or obesity. Many patients with impaired left ventricular function may have no obvious symptoms.17 This highlights the importance of exploring past medical and medication history as these contribute to the overall clinical assessment.
Physical findings that may support a diagnosis of heart failure include raised jugular venous pressure, peripheral edema not due to venous insufficiency, presence of a third heart sound, gallop rhythm, laterally displaced apical impulse, tachycardia, and pulmonary rales that do not clear with coughing. Although clinical findings are particularly useful in acute severe heart failure at the time of hospitalization,18 it is difficult to accurately diagnose mild heart failure in the community on the basis of clinical grounds alone.2,9 The value of different symptoms and aspects of the medical history and use of medications in the evaluation of potential heart failure patients have been examined by researchers.18, 20-23 Similarly, the utility of physical examination has also undergone investigation.18,20,22-28Table 1 summarizes the study findings with regard to clinical symptoms and signs.
Davie and colleagues20 assessed the value of symptoms, past history, medications, and signs in the evaluation of patients who may have LVSD. No one clinical feature predicted LVSD, as assessed by echocardiography with sensitivity, specificity, and a high positive and negative predictive value. Absence of dyspnea on exertion essentially ruled out heart failure (negative likelihood ratio [LR-] = 0.06), while gallop rhythm (positive likelihood ratio [LR+] = 24.0), laterally displaced apical impulse (LR+ 16.4), and elevated jugular venous pulsation (LR+ = 8.9) are strong evidence in favor of the diagnosis. Furthermore, the combination of history of myocardial infarction and displaced apex on physical examination, although not particularly sensitive (39% sensitivity) was very specific (99% specificity) with high positive (89%) and negative (89%) predictive values. The authors also suggest that a breathless patient with a past history of myocardial infarction and a displaced apex beat on physical examination will almost certainly have heart failure and, if resources are limited, may not need echocardiography to confirm the diagnosis. However, less than 50% of breathless patients will have this combination, and the other half would therefore need echocardiography as the gold standard diagnostic tool for LVSD.
Morgan and coworkers28 assessed the prevalence and clinical characteristics of LVSD among elderly patients (those aged 70 years to 84 years) in a primary care setting by echocardiographic assessment of ventricular function. They found that no single clinical symptom or sign was both sensitive and specific, and concluded that diagnosis should not be based on clinical history and examination alone. They found that a substantial number of elderly individuals had asymptomatic or misdiagnosed LVSD, and suggested this might be due to the extremely limited sensitivity and specificity of clinical history taking and examination. For example, only 11% of patients with LVSD had a raised jugular venous pressure, and bilateral ankle edema was common but nonspecific. Researchers have therefore concluded that although these clinical findings are useful in acute severe heart failure, they have only a small role in detecting LVSD in the community.18
TABLE 1
The use of clinical symptoms and signs to diagnose heart failure, by study
| Sign or symptom | N | Setting* | Study quality (1a-5)† | Sensitivity (%) | Specificity (%) | LR+ | LR- | PV+(%) | PV-(%) |
|---|---|---|---|---|---|---|---|---|---|
| Previous myocardial infarction | |||||||||
| Davie, 199720 | 259 | R | 2b | 59 | 86 | 4.1 | 0.48 | 44 | 92 |
| Morgan, 199928 | 817 | P | 2b | 39 | 91 | 4.3 | 0.67 | ||
| Dyspnea on exertion | |||||||||
| Davie, 199720 | 259 | R | 2b | 100 | 17 | 1.20 | 0.06 | 18 | 100 |
| Morgan, 199928 | 817 | P | 2b | 15 | 97 | 5.4 | 0.88 | ||
| Orthopnea | |||||||||
| Davie, 199720 | 259 | R | 2b | 22 | 74 | 0.85 | 1.05 | 14 | 83 |
| Paroxysmal nocturnal dyspnea | |||||||||
| Davie, 199720 | 259 | R | 2b | 39 | 80 | 1.95 | 0.76 | 27 | 87 |
| History of peripheral edema | |||||||||
| Davie, 199720 | 259 | R | 2b | 49 | 47 | 0.92 | 1.09 | 15 | 83 |
| Tachycardia | |||||||||
| Davie, 199720 | 259 | R | 2b | 22 | 92 | 2.75 | 0.85 | 33 | 86 |
| Elevated JVP | |||||||||
| Davie, 199720 | 259 | R | 2b | 17 | 98 | 8.95 | 0.84 | 64 | 86 |
| Morgan, 199928 | 817 | R | 2b | 11 | 97 | 3.6 | 0.92 | ||
| Gallop rhythm | |||||||||
| Davie, 199720 | 259 | P | 2b | 24 | 99 | 24.0 | 0.77 | 77 | 87 |
| 3rd heart sound | |||||||||
| Rihal, 199524 | 554 | H | 2b | 9 | 97 | 3.00 | 0.94 | 54 | 78 |
| Laterally displaced apical impulse | |||||||||
| Davie, 199720 | 259 | R | 2b | 66 | 96 | 16.4 | 0.35 | 75 | 94 |
| Pulmonary rales | |||||||||
| Davie, 199720 | 259 | R | 2b | 29 | 77 | 1.26 | 0.92 | 19 | 85 |
| Morgan, 199928 | 817 | P | 2b | 44 | 82 | 2.4 | 0.68 | ||
| Peripheral edema on examination | |||||||||
| Davie, 199720 | 259 | R | 2b | 20 | 86 | 1.43 | 0.93 | 21 | 85 |
| Morgan, 199928 | 817 | P | 2b | 18 | 91 | 2.0 | 0.90 | ||
| NOTE: Pretest probability = 50%. | |||||||||
| *P denotes cross-sectional primary care population; R, primary care patients referred for suspected heart failure; H, hospitalized patients undergoing angiography. | |||||||||
| † Level 1a is the most rigorous; level 5 is the least rigorous. | |||||||||
| LR+ denotes positive likelihood ratio; LR-, negative likelihood ratio; PV+, positive predictive value; PV-, negative predictive value. | |||||||||
Laboratory and imaging evaluation
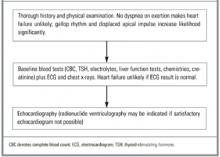
Although an important and valuable part of the evaluation, the history and physical examination alone are insufficient to confirm a diagnosis in most cases. Recommended initial tests for patients with signs or symptoms of heart failure include complete blood count (CBC), serum electrolytes, serum creatinine, serum albumin, liver function tests, urinalysis, electrocardiogram, and chest x-ray (Figure).
Blood tests. For those older than 65 years or with atrial fibrillation or evidence of thyroid disease, thyroid function tests should also be performed because heart failure due to thyrotoxicosis is frequently associated with rapid atrial fibrillation and hypothyroidism may also present as heart failure.8,10 The other routine blood tests are important as a way to exclude alternative diagnoses; they also help with the search for predisposing or exacerbating causes of the heart failure. These baseline tests also help guide future therapeutic decision making. For example, electrolyte and renal function results are pertinent when initiating angiotensin-converting enzyme (ACE) inhibitors. Anemia can exacerbate pre-existing heart failure, and measurement of renal function is essential to distinguish fluid overload due to heart failure from renal failure. Liver enzymes may be affected by hepatic congestion. Urinalysis is valuable in the detection of underlying renal disease or diabetes.8
Electrocardiography. An electrocardiogram (ECG) is another recommended part of the evaluation of the suspected heart failure patient.8-14 Considerable attention has been paid to examining the value of this test in the diagnosis of LVSD.29-32 Davie and colleagues29 assessed the value of the ECG in identifying patients with possible heart failure by examining referrals for echocardiography by primary care practitioners. A total of 534 patients were referred for echocardiography for possible heart failure, of whom 18% (n = 96) had LVSD. They showed that LVSD was extremely unlikely if the ECG result was normal, but that 1 in 3 patients with an abnormal result had significant LVSD. Thus, a normal ECG result virtually excludes chronic heart failure due to LVSD. However, the ECG is not a substitute for echocardiography, as an abnormal result does not accurately predict the presence of LVSD (Table 2).
Others have confirmed these findings.30,32 Talreja and colleagues30 found that of 330 consecutive in-patients referred for echocardiographic assessment of left ventricular function, 124 (41%) had LVSD. Only 2 of 124 patients with LVSD had a normal electrocardiogram result. When the ECG result is normal, the authors suggest that echocardiography is not needed. However, they concede that physicians are unlikely to adhere to this because many may not be as sophisticated in interpreting the ECG and may feel it important to get an accurate measure of ejection fraction. Guidelines published by the European Society of Cardiology10 state that a normal ECG result in patients with suspected heart failure should lead us to doubt the accuracy of the diagnosis.
Chest x-ray. The chest x-ray is most valuable as a test to exclude pulmonary causes. However, the existing evidence suggests it is not a reliable way to exclude LVSD.24,26,33,34 (Table 2) provides information about the value of radiography in predicting LVSD. A systematic review of the literature concluded that redistribution and cardiomegaly were the best chest radiographic findings for diagnosing increased preload and reduced ejection fraction, respectively.34 However, neither finding alone could adequately exclude or confirm LVSD. Studies published since that review have confirmed this finding.33 Although part of the evaluation of the heart failure patient, radiography is only one part of the diagnostic process and cannot be used to provide definitive diagnostic information.
Echocardiography. The most important step in the evaluation of the heart failure patient is the assessment of left ventricular systolic function. Both echocardiography and radionuclide ventriculography have been advocated.8-14 However, echocardiography is preferred as it is widely available, simple, noninvasive, safe, usually less expensive, and provides more information about valve function and left ventricular hypertrophy. Table 2 demonstrates the high sensitivity and specificity of echocardiography.35 In view of this, it is recommended as a standard adjunct to the clinical diagnosis of patients with dyspnea on exertion and suspected heart failure. Between 8% and 18% of patients will have inadequate echocardiograms, in which case radionuclide ventriculography is advocated.8
Neurohormonal markers. In recent years there has been increasing interest in the potential role of neurohormonal markers, such as B-type natriuretic peptide (BNP), atrial natriuretic peptide (ANP), N-terminal pro-ANP (N-ANP), and N-terminal pro-BNP (N-BNP) as indices of LVSD.36-42 Most of the data relating to these markers are relatively recent; therefore their use is not addressed in any detail in any of the aforementioned guidelines.
Some studies41,42 suggest that BNP and N-BNP are useful for diagnosing LVSD even when the positive predictive values are low, because of their high negative predictive values. One of the most recent studies44 examined the utility of BNP in an urgent care setting and suggested that BNP was an extremely reliable indicator of LVSD. In this population of patients with acute dyspnea where 39% had a final diagnosis of heart failure, 90% with a positive BNP had heart failure and 98% of those with a negative BNP did not. Although there appears to be a growing body of evidence supporting the role of these neurohormonal markers in the evaluation of the patient with LVSD, Table 2 illustrates that there have also been conflicting findings. This is partly because of differences in study design, study populations, cut-off points for ANP and BNP, and the definition of LVSD. Most studies agree that assessment of BNP, in particular, may be a cost-effective method for initial screening for LVSD, but should still be followed by an echocardiogram to confirm the diagnosis.
Management follows diagnosis. Making the correct diagnosis is the crucial first step in the management of chronic heart failure. Figure 1 summarizes the steps currently recommended for the evaluation of the patient with LVSD. A confirmation of a diagnosis of LVSD, however, is not the end of the story. Management will then need to include initiation of appropriate therapies and consideration of treatable and reversible etiologies, a subject to be addressed in the June 2002 issue of this journal.
TABLE 2
Key investigations used for the diagnosis of left ventricular systolic dysfunction
| Test | N | Setting* | Study quality † | Sensitivity (%) | Specificity(%) | LR+ | LR- | PV+ (%) | PV- (%) |
|---|---|---|---|---|---|---|---|---|---|
| Electrocardiogram | |||||||||
| Davie, 199729 | 534 | R | 1c | 94 | 61 | 2.43 | 0.10 | 35 | 98 |
| Lindsay, 200043 | 416 | R | 1c | 90 | 65 | 2.59 | 2.76 | 43 | 90 |
| Mosterd, 199732 | 1980 | R | 1c | 54 | 79 | 2.55 | 0.58 | 7 | 98 |
| Electrocardiogram (patient older than 70 years) | |||||||||
| Mosterd, 199732 | 1980 | R | 1c | 67 | 64 | 1.88 | 0.52 | 7 | 98 |
| Talreja, 200030 | 330 | H | 1c | 65 | 98 | 38.2 | 0.36 | 98 | 64 |
| Chest x-ray | |||||||||
| Badgett, 199634 | 29 studies | 2a | 51 | 79 | 2.43 | 0.62 | 71 | 62 | |
| Rihal, 199524 | 554 | H | 2b | 20 | 89 | 1.82 | 0.90 | 34 | 79 |
| Echocardiogram | |||||||||
| Erbel, 198435 | 110 | H | 1c | 80 | 100 | 80.0 | 0.20 | 100 | 85 |
| N-terminal ANP > 4.4 ng/mL | |||||||||
| McClure, 199840 | 134 | M | 2b | — | — | 1.08 | 0.96 | 52 | 51 |
| N-terminal pro-BNP > 275 fmol/mL | |||||||||
| Talwar, 199942 | 249 | R | 2b | 94 | 55 | 2.09 | 011 | 58 | 93 |
| BNP > 75 pg/mL | |||||||||
| Maisel, 200137 | 200 | R | 1c | 86 | 98 | 43.0 | 0.14 | 98 | 89 |
| Dao, 200144 | 250 | U | 1b | 98 | 92 | 12.2 | 0.02 | 92 | 98 |
| BNP > 46 pg/mL | |||||||||
| McClure, 199840 | 134 | M | 2b | — | — | 2.25 | 0.83 | 69 | 55 |
| BNP > 17.9 pg/mL | |||||||||
| McDonagh, 199841 | 1653 | P | 2b | 76 | 87 | 5.85 | 0.28 | 16 | 97 |
| NOTE: Pretest probability = 50%. | |||||||||
| *P denotes cross-sectional primary care population; R, primary care patients referred for suspected heart failure; H, hospitalized patients undergoing angiography; U, urgent care center; M, long-term myocardial infarction survivors recalled by their family physician. | |||||||||
| † Level 1a is the most rigorous; level 5 is the least rigorous. | |||||||||
| ANP, atrial natriuretic peptide; BNP, B-type natriuretic peptide; LR+, positive likelihood ratio; LR-, negative likelihood ratio; PV+, positive predictive value; PV-, negative predictive value. | |||||||||
Figure
Steps in the assessment of the patient with suspected heart failure
ACKNOWLEDGMENTS
We wish to thank Mr Chris Shiels at the Department of Primary Care, University of Liverpool, for his valuable advice regarding this manuscript.
1. Mair FS, Crowley TS, Bundred PE. Prevalence, aetiology and management of heart failure in general practice. Br J Gen Pract 1996;46:77-9.
2. Wheeldon NM, MacDonald TM, Flucker CJ, McDermitt DG, Struthers AD. An electrocardiographic study of chronic heart failure in the community. QJM 1993;86:17-23.
3. O’Connell JB, Bristow MR. Economic impact of heart failure in the United States: time for a different approach. J Heart Lung Transplan 1994;13:S107-112.
4. O’Connell JB. The economic burden of heart failure. Clin Cardiol 2000;23 (3 Suppl):III6-10.
5. English MA, Mastrean MB. Congestive heart failure: public and private burden. Crit Care Nurs Q 1995;18:1-6.
6. Croft JB, Giles WH, Pollard RA, Keenan NL, Casper ML, Anda RF. Heart failure survival among older adults in the United States: a poor prognosis for an emerging epidemic in the Medicare population. Arch Intern Med 1999;159:505-10.
7. Stewart S, MacIntyre K, Hole DJ, Capewell S, McMurray JJV. More ‘malignant’ than cancer? Five-year survival following a first admission for heart failure. Eur J Heart Fail 2001;3:315-22.
8. Konstam M, Dracup K, Baker D, et al. Heart failure: evaluation and care of patients with left-ventricular systolic dysfunction. Clinical Practice Guideline No. 11. AHCPR Publication No. 94-0612. Agency for Health Care Policy and Research, Public Health Service, US Department of Health and Human Services, Rockville, Md.
9. Guidelines for the evaluation and management of heart failure. Report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Committee on Evaluation and Management of Heart Failure). Circulation 1995;92:2764-84.
10. The Task Force on Heart Failure of the European Society of Cardiology. Guidelines for the diagnosis of heart failure. Eur Heart J 1995;16:741-51.
11. Heart failure —systolic dysfunction. University of Michigan Health System. August 1999. (Available at http://cme.med.umich.edu/pdf/guideline/heart.pdf)
12. The Task Force of the Working Group on Heart Failure of the European Society of Cardiolog. The treatment of heart failure. Eur Heart J 1997;18:736-53.
13. Diagnosis and treatment of heart failure due to left ventricular systolic dysfunction. A national clinical guideline. Scottish Intercollegiate Guidelines Network (SIGN); SIGN publication; no. 35. Feb 1999; 68.
14. Anonymous. Heart Failure Society of America (HFSA) practice guidelines. HFSA guidelines for management of patients with heart failure caused by left ventricular systolic dysfunction—pharmacological approaches [published erratum appears in J Card Fail 2000 Mar; 6:74]. J Card Fail 5:357-82.
15. McMurray JJV, Dargie HJ. Diagnosis and management of heart failure. BMJ 1994;308:321-8.
16. Mair FS. Management of heart failure. Am Fam Phys 1996;54:245-54.
17. Marantz PR, Tobin JN, Wassertheil-Smoller S, et al. The relationship between left ventricular systolic function and congestive heart failure diagnosed by clinical criteria. Circulation 1988;77:607-12.
18. Gillespie ND, McNeill G, Pringle T, Ogston S, Struthers AD, Pringle SD. Cross sectional study of contribution of clinical assessment and simple cardiac investigations to diagnosis of left ventricular systolic dysfunction in patients admitted with acute dyspnoea. BMJ 1997;314:936-40.
19. Remes J, Miettinen H, Reunanen A, Pyorala K. Validity of clinical diagnosis of heart failure in primary health care. Eur Heart J 1991;12:315-21.
20. Davie AP, Francis CM, Caruana L, Sutherland GR, McMurray JJV. Assessing diagnosis in heart failure: which features are of any use? QJM 1997;90:335-9.
21. Gadsboll N, Hoilund-Carlsen PF, Nielsen GG, et al. Symptoms and signs of heart failure in patients with myocardial infarction: reproducibility and relationship to chest X-ray, radionuclide ventriculog-raphy, and right heart catheterisation. Eur Heart J 1989;10:1017-28.
22. Stevenson LW, Perloff JK. The limited reliability of physical signs for estimating hemodynamics in chronic heart failure. JAMA 1989;261:884-8.
23. Ishmail AA, Wing S, Ferguson J, Hutchinson TA, Magder S, Flegel KM. Interobserver agreement by auscultation in the presence of a third heart sound in patients with congestive heart failure. Chest 1987;91:870-3.
24. Rihal CS, Davis KB, Kennedy W, Gersh BJ. The utility of clinical, electrocardiographic and roentgenographic variables in the prediction of left ventricular function. Am J Cardiol 1995;752:220-3.
25. Harlan WR, Oberman A, Grimm R, Rosati RA. Chronic congestive heart failure in coronary artery disease: clinical criteria. Ann Intern Med 1977;86:133-8.
26. Chakko S, Woska D, Martinez H, et al. Clinical, radiographic, and hemodynamic correlations in chronic congestive heart failure: conflicting results may lead to inappropriate care. Am J Med 1991;90:353-9.
27. Mattleman SJ, Hakki A, Iskandrian AS, Segal BL, Kane SA. Reliability of bedside evaluation in determining left ventricular function: correlation with left ventricular ejection fraction determined by radionuclide ventriculography. J Am Coll Cardio 1983;1:417-20.
28. Morgan S, Smith H, Simpson I, et al. Prevalence and clinical characteristics of left ventricular dysfunction among elderly patients in general practice setting: cross sectional survey. BMJ 1999;318:368-72.
29. Davie AP, Francis CM, Love MP, et al. Value of electrocardiogram in identifying heart failure due to left ventricular systolic dysfunction. BMJ 1996;312:222-3.
30. Talreja D, Gruver C, Sklenar J, Dent J, Kaul S. Efficient utilization of echocardiography for the assessment of left ventricular systolic function. Am Heart J 2000;139:394-8.
31. Murkofsky RL, Dangas G, Diamond JA, et al. A prolonged QRS duration on surface electrocardiogram is a specific indicator of left ventricular dysfunction. J Am Coll Cardiol 1998;32:476-82.
32. Mosterd A, de Bruijne MC, Hoes AW, et al. Usefulness of echocardiography in detecting left ventricular dysfunction in population-based studies (The Rotterdam Study). Am J Cardiol 1997;79:103-4.
33. Clark AL, Coats ALS. Unreliability of cardiothoracic ratio as a marker of left ventricular impairment: comparison with radionuclide ventriculography and echocardiography. Postgrad Med J 2000;76:289-91.
34. Badgett RG, Mulrow CD, Otto PM, Ramirez G. How well can the chest radiograph diagnose left ventricular dysfunction? J Gen Intern Med 1996;11:625-34.
35. Erbel R, Schweizer P, Drebs W, Meyer J, Effert S. Sensitivity and specificity of two-dimensional echocardiography in detection of impaired left ventricular function. Eur Heart J 1984;5:477-89.
36. Davis M, Espiner E, Richards G, et al. Plasma brain natriuretic peptide in assessment of acute dyspnoea. Lancet 1994;343:440-4.
37. Maisel AS, Koon J, Krishnaswamy P, et al. Utility of B-natriuretic peptide as a rapid, point-of-care test for screening patients undergoing echocardiography to determine left ventricular dysfunction. Am Heart J 2001;141:367-74.
38. Schirmer H, Omland T. Circulating N-terminal pro-atrial natriuretic peptide is an independent predictor of left ventricular hypertrophy in the general population. The Tromsø Study. Eur Heart J 1999;20:755-63.
39. Lerman A, Gibbons RJ, Rodeheffer RJ, et al. Circulating N-terminal atrial natriuretic peptide as a marker for symptomless left-ventricular dysfunction. Lancet 1993;341:1105-9.
40. McClure SJ, Davie AP, Goldthorp S, et al. Cohort study of plasma natriuretic peptides for identifying left ventricular systolic dysfunction in primary care. BMJ 1998;317:516-9.
41. McDonagh TA, Robb SD, Murdoch DR, et al. Biochemical detection of left-ventricular systolic dysfunction. Lancet 1998;351:9-13,
42. Talwar S, Squire IB, Davies JE, et al. Plasma N-terminal pro-brain natriuretic peptide and the ECG in the assessment of left-ventricular systolic dysfunction in a high risk population. Eur Heart J 1999;20:1736-1744.
43. Lindsay MM, Goodfield NER, Hogg KJ, Dunn EG. Optimising direct access echo referral in suspected heart failure. Scot Med J 2000;45:043-044.
44. Dao Q, Krishnaswamy P, Kazanegra R, et al. Utility of B-Type natriuretic peptide in the diagnosis of congestive heart failure in an urgent care setting. J Am Coll Cardiol 2001;37:379-85.
- Heart failure is an increasingly common problem in primary care, with a mortality rate higher than that of most cancers.
- The absence of dyspnea on exertion or a normal electrocardiogram (ECG) result indicates that heart failure is unlikely; a gallop rhythm or laterally displaced apical rhythm is strong evidence in favor of heart failure.
- The history and physical examination and ECG alone are usually inadequate to confirm diagnosis of left ventricular systolic dysfunction, and echocardiography remains the gold standard to confirm the diagnosis.
Heart failure is increasing in incidence and prevalence; it currently affects 0.4% to 2% of the general population and 8% to 10% of the elderly.1,2 In the United States, heart failure is the second most common cardiovascular reason for an outpatient visit in the ambulatory care setting and remains the most common cause for hospitalization among patients older than 65 years.3 The total cost for heart failure management in 1999 was estimated to approach $56 billion.4 Those suffering with this illness experience high levels of morbidity and mortality5 that are reflected in the workloads of both primary and secondary care. Heart failure admission rates are rising, and the prognosis of heart failure has been compared with that of malignancy, with a 6-year mortality rate of 84% in men and 77% in women.6,7
A number of heart failure guidelines8-14 provide direction regarding “best practice” with regard to diagnosis and management. These guidelines have all been produced by expert panels and base their evidence on systematic critical reviews of the literature, plus expert consensus opinion. The evidence underlying the development of these guidelines ranges from well-conducted randomized controlled trials to expert opinion. These guidelines all emphasize the ways in which approaches to the diagnosis and management of heart failure have altered substantially in recent years and are continuing to change rapidly. The need to detect heart failure at an early stage to slow the progression of left ventricular systolic dysfunction (LVSD) is now well accepted.15
The following provides an overview of the current recommended approaches to diagnosis, focusing specifically on LVSD, the most common type of heart failure and also the usual focus of most guidelines. Accurate diagnosis of LVSD is the single most important step in management.16 An adequate diagnosis should establish the existence of heart failure, differentiate systolic from diastolic dysfunction, and identify the main underlying cause and any subsidiary diagnoses that may exacerbate heart failure. The etiology of heart failure and the presence of exacerbating factors or other diseases need to be carefully considered in all patients. Coronary artery disease remains the most common potentially reversible etiologic factor in heart failure.8
Using the history and physical examination
The major symptoms of heart failure are fatigue, exercise intolerance, exertional dyspnea, orthopnea, paroxysmal nocturnal dyspnea, and dependent edema. However, such symptoms are similar to those of many other diseases, particularly pulmonary diseases. For example, exertional dypsnea is a common symptom in heart failure but can be due to a wide range of other causes, such as chronic obstructive pulmonary disease, interstitial lung disease, asthma, respiratory infection, deconditioning, or obesity. Many patients with impaired left ventricular function may have no obvious symptoms.17 This highlights the importance of exploring past medical and medication history as these contribute to the overall clinical assessment.
Physical findings that may support a diagnosis of heart failure include raised jugular venous pressure, peripheral edema not due to venous insufficiency, presence of a third heart sound, gallop rhythm, laterally displaced apical impulse, tachycardia, and pulmonary rales that do not clear with coughing. Although clinical findings are particularly useful in acute severe heart failure at the time of hospitalization,18 it is difficult to accurately diagnose mild heart failure in the community on the basis of clinical grounds alone.2,9 The value of different symptoms and aspects of the medical history and use of medications in the evaluation of potential heart failure patients have been examined by researchers.18, 20-23 Similarly, the utility of physical examination has also undergone investigation.18,20,22-28Table 1 summarizes the study findings with regard to clinical symptoms and signs.
Davie and colleagues20 assessed the value of symptoms, past history, medications, and signs in the evaluation of patients who may have LVSD. No one clinical feature predicted LVSD, as assessed by echocardiography with sensitivity, specificity, and a high positive and negative predictive value. Absence of dyspnea on exertion essentially ruled out heart failure (negative likelihood ratio [LR-] = 0.06), while gallop rhythm (positive likelihood ratio [LR+] = 24.0), laterally displaced apical impulse (LR+ 16.4), and elevated jugular venous pulsation (LR+ = 8.9) are strong evidence in favor of the diagnosis. Furthermore, the combination of history of myocardial infarction and displaced apex on physical examination, although not particularly sensitive (39% sensitivity) was very specific (99% specificity) with high positive (89%) and negative (89%) predictive values. The authors also suggest that a breathless patient with a past history of myocardial infarction and a displaced apex beat on physical examination will almost certainly have heart failure and, if resources are limited, may not need echocardiography to confirm the diagnosis. However, less than 50% of breathless patients will have this combination, and the other half would therefore need echocardiography as the gold standard diagnostic tool for LVSD.
Morgan and coworkers28 assessed the prevalence and clinical characteristics of LVSD among elderly patients (those aged 70 years to 84 years) in a primary care setting by echocardiographic assessment of ventricular function. They found that no single clinical symptom or sign was both sensitive and specific, and concluded that diagnosis should not be based on clinical history and examination alone. They found that a substantial number of elderly individuals had asymptomatic or misdiagnosed LVSD, and suggested this might be due to the extremely limited sensitivity and specificity of clinical history taking and examination. For example, only 11% of patients with LVSD had a raised jugular venous pressure, and bilateral ankle edema was common but nonspecific. Researchers have therefore concluded that although these clinical findings are useful in acute severe heart failure, they have only a small role in detecting LVSD in the community.18
TABLE 1
The use of clinical symptoms and signs to diagnose heart failure, by study
| Sign or symptom | N | Setting* | Study quality (1a-5)† | Sensitivity (%) | Specificity (%) | LR+ | LR- | PV+(%) | PV-(%) |
|---|---|---|---|---|---|---|---|---|---|
| Previous myocardial infarction | |||||||||
| Davie, 199720 | 259 | R | 2b | 59 | 86 | 4.1 | 0.48 | 44 | 92 |
| Morgan, 199928 | 817 | P | 2b | 39 | 91 | 4.3 | 0.67 | ||
| Dyspnea on exertion | |||||||||
| Davie, 199720 | 259 | R | 2b | 100 | 17 | 1.20 | 0.06 | 18 | 100 |
| Morgan, 199928 | 817 | P | 2b | 15 | 97 | 5.4 | 0.88 | ||
| Orthopnea | |||||||||
| Davie, 199720 | 259 | R | 2b | 22 | 74 | 0.85 | 1.05 | 14 | 83 |
| Paroxysmal nocturnal dyspnea | |||||||||
| Davie, 199720 | 259 | R | 2b | 39 | 80 | 1.95 | 0.76 | 27 | 87 |
| History of peripheral edema | |||||||||
| Davie, 199720 | 259 | R | 2b | 49 | 47 | 0.92 | 1.09 | 15 | 83 |
| Tachycardia | |||||||||
| Davie, 199720 | 259 | R | 2b | 22 | 92 | 2.75 | 0.85 | 33 | 86 |
| Elevated JVP | |||||||||
| Davie, 199720 | 259 | R | 2b | 17 | 98 | 8.95 | 0.84 | 64 | 86 |
| Morgan, 199928 | 817 | R | 2b | 11 | 97 | 3.6 | 0.92 | ||
| Gallop rhythm | |||||||||
| Davie, 199720 | 259 | P | 2b | 24 | 99 | 24.0 | 0.77 | 77 | 87 |
| 3rd heart sound | |||||||||
| Rihal, 199524 | 554 | H | 2b | 9 | 97 | 3.00 | 0.94 | 54 | 78 |
| Laterally displaced apical impulse | |||||||||
| Davie, 199720 | 259 | R | 2b | 66 | 96 | 16.4 | 0.35 | 75 | 94 |
| Pulmonary rales | |||||||||
| Davie, 199720 | 259 | R | 2b | 29 | 77 | 1.26 | 0.92 | 19 | 85 |
| Morgan, 199928 | 817 | P | 2b | 44 | 82 | 2.4 | 0.68 | ||
| Peripheral edema on examination | |||||||||
| Davie, 199720 | 259 | R | 2b | 20 | 86 | 1.43 | 0.93 | 21 | 85 |
| Morgan, 199928 | 817 | P | 2b | 18 | 91 | 2.0 | 0.90 | ||
| NOTE: Pretest probability = 50%. | |||||||||
| *P denotes cross-sectional primary care population; R, primary care patients referred for suspected heart failure; H, hospitalized patients undergoing angiography. | |||||||||
| † Level 1a is the most rigorous; level 5 is the least rigorous. | |||||||||
| LR+ denotes positive likelihood ratio; LR-, negative likelihood ratio; PV+, positive predictive value; PV-, negative predictive value. | |||||||||
Laboratory and imaging evaluation
Although an important and valuable part of the evaluation, the history and physical examination alone are insufficient to confirm a diagnosis in most cases. Recommended initial tests for patients with signs or symptoms of heart failure include complete blood count (CBC), serum electrolytes, serum creatinine, serum albumin, liver function tests, urinalysis, electrocardiogram, and chest x-ray (Figure).
Blood tests. For those older than 65 years or with atrial fibrillation or evidence of thyroid disease, thyroid function tests should also be performed because heart failure due to thyrotoxicosis is frequently associated with rapid atrial fibrillation and hypothyroidism may also present as heart failure.8,10 The other routine blood tests are important as a way to exclude alternative diagnoses; they also help with the search for predisposing or exacerbating causes of the heart failure. These baseline tests also help guide future therapeutic decision making. For example, electrolyte and renal function results are pertinent when initiating angiotensin-converting enzyme (ACE) inhibitors. Anemia can exacerbate pre-existing heart failure, and measurement of renal function is essential to distinguish fluid overload due to heart failure from renal failure. Liver enzymes may be affected by hepatic congestion. Urinalysis is valuable in the detection of underlying renal disease or diabetes.8
Electrocardiography. An electrocardiogram (ECG) is another recommended part of the evaluation of the suspected heart failure patient.8-14 Considerable attention has been paid to examining the value of this test in the diagnosis of LVSD.29-32 Davie and colleagues29 assessed the value of the ECG in identifying patients with possible heart failure by examining referrals for echocardiography by primary care practitioners. A total of 534 patients were referred for echocardiography for possible heart failure, of whom 18% (n = 96) had LVSD. They showed that LVSD was extremely unlikely if the ECG result was normal, but that 1 in 3 patients with an abnormal result had significant LVSD. Thus, a normal ECG result virtually excludes chronic heart failure due to LVSD. However, the ECG is not a substitute for echocardiography, as an abnormal result does not accurately predict the presence of LVSD (Table 2).
Others have confirmed these findings.30,32 Talreja and colleagues30 found that of 330 consecutive in-patients referred for echocardiographic assessment of left ventricular function, 124 (41%) had LVSD. Only 2 of 124 patients with LVSD had a normal electrocardiogram result. When the ECG result is normal, the authors suggest that echocardiography is not needed. However, they concede that physicians are unlikely to adhere to this because many may not be as sophisticated in interpreting the ECG and may feel it important to get an accurate measure of ejection fraction. Guidelines published by the European Society of Cardiology10 state that a normal ECG result in patients with suspected heart failure should lead us to doubt the accuracy of the diagnosis.
Chest x-ray. The chest x-ray is most valuable as a test to exclude pulmonary causes. However, the existing evidence suggests it is not a reliable way to exclude LVSD.24,26,33,34 (Table 2) provides information about the value of radiography in predicting LVSD. A systematic review of the literature concluded that redistribution and cardiomegaly were the best chest radiographic findings for diagnosing increased preload and reduced ejection fraction, respectively.34 However, neither finding alone could adequately exclude or confirm LVSD. Studies published since that review have confirmed this finding.33 Although part of the evaluation of the heart failure patient, radiography is only one part of the diagnostic process and cannot be used to provide definitive diagnostic information.
Echocardiography. The most important step in the evaluation of the heart failure patient is the assessment of left ventricular systolic function. Both echocardiography and radionuclide ventriculography have been advocated.8-14 However, echocardiography is preferred as it is widely available, simple, noninvasive, safe, usually less expensive, and provides more information about valve function and left ventricular hypertrophy. Table 2 demonstrates the high sensitivity and specificity of echocardiography.35 In view of this, it is recommended as a standard adjunct to the clinical diagnosis of patients with dyspnea on exertion and suspected heart failure. Between 8% and 18% of patients will have inadequate echocardiograms, in which case radionuclide ventriculography is advocated.8
Neurohormonal markers. In recent years there has been increasing interest in the potential role of neurohormonal markers, such as B-type natriuretic peptide (BNP), atrial natriuretic peptide (ANP), N-terminal pro-ANP (N-ANP), and N-terminal pro-BNP (N-BNP) as indices of LVSD.36-42 Most of the data relating to these markers are relatively recent; therefore their use is not addressed in any detail in any of the aforementioned guidelines.
Some studies41,42 suggest that BNP and N-BNP are useful for diagnosing LVSD even when the positive predictive values are low, because of their high negative predictive values. One of the most recent studies44 examined the utility of BNP in an urgent care setting and suggested that BNP was an extremely reliable indicator of LVSD. In this population of patients with acute dyspnea where 39% had a final diagnosis of heart failure, 90% with a positive BNP had heart failure and 98% of those with a negative BNP did not. Although there appears to be a growing body of evidence supporting the role of these neurohormonal markers in the evaluation of the patient with LVSD, Table 2 illustrates that there have also been conflicting findings. This is partly because of differences in study design, study populations, cut-off points for ANP and BNP, and the definition of LVSD. Most studies agree that assessment of BNP, in particular, may be a cost-effective method for initial screening for LVSD, but should still be followed by an echocardiogram to confirm the diagnosis.
Management follows diagnosis. Making the correct diagnosis is the crucial first step in the management of chronic heart failure. Figure 1 summarizes the steps currently recommended for the evaluation of the patient with LVSD. A confirmation of a diagnosis of LVSD, however, is not the end of the story. Management will then need to include initiation of appropriate therapies and consideration of treatable and reversible etiologies, a subject to be addressed in the June 2002 issue of this journal.
TABLE 2
Key investigations used for the diagnosis of left ventricular systolic dysfunction
| Test | N | Setting* | Study quality † | Sensitivity (%) | Specificity(%) | LR+ | LR- | PV+ (%) | PV- (%) |
|---|---|---|---|---|---|---|---|---|---|
| Electrocardiogram | |||||||||
| Davie, 199729 | 534 | R | 1c | 94 | 61 | 2.43 | 0.10 | 35 | 98 |
| Lindsay, 200043 | 416 | R | 1c | 90 | 65 | 2.59 | 2.76 | 43 | 90 |
| Mosterd, 199732 | 1980 | R | 1c | 54 | 79 | 2.55 | 0.58 | 7 | 98 |
| Electrocardiogram (patient older than 70 years) | |||||||||
| Mosterd, 199732 | 1980 | R | 1c | 67 | 64 | 1.88 | 0.52 | 7 | 98 |
| Talreja, 200030 | 330 | H | 1c | 65 | 98 | 38.2 | 0.36 | 98 | 64 |
| Chest x-ray | |||||||||
| Badgett, 199634 | 29 studies | 2a | 51 | 79 | 2.43 | 0.62 | 71 | 62 | |
| Rihal, 199524 | 554 | H | 2b | 20 | 89 | 1.82 | 0.90 | 34 | 79 |
| Echocardiogram | |||||||||
| Erbel, 198435 | 110 | H | 1c | 80 | 100 | 80.0 | 0.20 | 100 | 85 |
| N-terminal ANP > 4.4 ng/mL | |||||||||
| McClure, 199840 | 134 | M | 2b | — | — | 1.08 | 0.96 | 52 | 51 |
| N-terminal pro-BNP > 275 fmol/mL | |||||||||
| Talwar, 199942 | 249 | R | 2b | 94 | 55 | 2.09 | 011 | 58 | 93 |
| BNP > 75 pg/mL | |||||||||
| Maisel, 200137 | 200 | R | 1c | 86 | 98 | 43.0 | 0.14 | 98 | 89 |
| Dao, 200144 | 250 | U | 1b | 98 | 92 | 12.2 | 0.02 | 92 | 98 |
| BNP > 46 pg/mL | |||||||||
| McClure, 199840 | 134 | M | 2b | — | — | 2.25 | 0.83 | 69 | 55 |
| BNP > 17.9 pg/mL | |||||||||
| McDonagh, 199841 | 1653 | P | 2b | 76 | 87 | 5.85 | 0.28 | 16 | 97 |
| NOTE: Pretest probability = 50%. | |||||||||
| *P denotes cross-sectional primary care population; R, primary care patients referred for suspected heart failure; H, hospitalized patients undergoing angiography; U, urgent care center; M, long-term myocardial infarction survivors recalled by their family physician. | |||||||||
| † Level 1a is the most rigorous; level 5 is the least rigorous. | |||||||||
| ANP, atrial natriuretic peptide; BNP, B-type natriuretic peptide; LR+, positive likelihood ratio; LR-, negative likelihood ratio; PV+, positive predictive value; PV-, negative predictive value. | |||||||||
Figure
Steps in the assessment of the patient with suspected heart failure
ACKNOWLEDGMENTS
We wish to thank Mr Chris Shiels at the Department of Primary Care, University of Liverpool, for his valuable advice regarding this manuscript.
- Heart failure is an increasingly common problem in primary care, with a mortality rate higher than that of most cancers.
- The absence of dyspnea on exertion or a normal electrocardiogram (ECG) result indicates that heart failure is unlikely; a gallop rhythm or laterally displaced apical rhythm is strong evidence in favor of heart failure.
- The history and physical examination and ECG alone are usually inadequate to confirm diagnosis of left ventricular systolic dysfunction, and echocardiography remains the gold standard to confirm the diagnosis.
Heart failure is increasing in incidence and prevalence; it currently affects 0.4% to 2% of the general population and 8% to 10% of the elderly.1,2 In the United States, heart failure is the second most common cardiovascular reason for an outpatient visit in the ambulatory care setting and remains the most common cause for hospitalization among patients older than 65 years.3 The total cost for heart failure management in 1999 was estimated to approach $56 billion.4 Those suffering with this illness experience high levels of morbidity and mortality5 that are reflected in the workloads of both primary and secondary care. Heart failure admission rates are rising, and the prognosis of heart failure has been compared with that of malignancy, with a 6-year mortality rate of 84% in men and 77% in women.6,7
A number of heart failure guidelines8-14 provide direction regarding “best practice” with regard to diagnosis and management. These guidelines have all been produced by expert panels and base their evidence on systematic critical reviews of the literature, plus expert consensus opinion. The evidence underlying the development of these guidelines ranges from well-conducted randomized controlled trials to expert opinion. These guidelines all emphasize the ways in which approaches to the diagnosis and management of heart failure have altered substantially in recent years and are continuing to change rapidly. The need to detect heart failure at an early stage to slow the progression of left ventricular systolic dysfunction (LVSD) is now well accepted.15
The following provides an overview of the current recommended approaches to diagnosis, focusing specifically on LVSD, the most common type of heart failure and also the usual focus of most guidelines. Accurate diagnosis of LVSD is the single most important step in management.16 An adequate diagnosis should establish the existence of heart failure, differentiate systolic from diastolic dysfunction, and identify the main underlying cause and any subsidiary diagnoses that may exacerbate heart failure. The etiology of heart failure and the presence of exacerbating factors or other diseases need to be carefully considered in all patients. Coronary artery disease remains the most common potentially reversible etiologic factor in heart failure.8
Using the history and physical examination
The major symptoms of heart failure are fatigue, exercise intolerance, exertional dyspnea, orthopnea, paroxysmal nocturnal dyspnea, and dependent edema. However, such symptoms are similar to those of many other diseases, particularly pulmonary diseases. For example, exertional dypsnea is a common symptom in heart failure but can be due to a wide range of other causes, such as chronic obstructive pulmonary disease, interstitial lung disease, asthma, respiratory infection, deconditioning, or obesity. Many patients with impaired left ventricular function may have no obvious symptoms.17 This highlights the importance of exploring past medical and medication history as these contribute to the overall clinical assessment.
Physical findings that may support a diagnosis of heart failure include raised jugular venous pressure, peripheral edema not due to venous insufficiency, presence of a third heart sound, gallop rhythm, laterally displaced apical impulse, tachycardia, and pulmonary rales that do not clear with coughing. Although clinical findings are particularly useful in acute severe heart failure at the time of hospitalization,18 it is difficult to accurately diagnose mild heart failure in the community on the basis of clinical grounds alone.2,9 The value of different symptoms and aspects of the medical history and use of medications in the evaluation of potential heart failure patients have been examined by researchers.18, 20-23 Similarly, the utility of physical examination has also undergone investigation.18,20,22-28Table 1 summarizes the study findings with regard to clinical symptoms and signs.
Davie and colleagues20 assessed the value of symptoms, past history, medications, and signs in the evaluation of patients who may have LVSD. No one clinical feature predicted LVSD, as assessed by echocardiography with sensitivity, specificity, and a high positive and negative predictive value. Absence of dyspnea on exertion essentially ruled out heart failure (negative likelihood ratio [LR-] = 0.06), while gallop rhythm (positive likelihood ratio [LR+] = 24.0), laterally displaced apical impulse (LR+ 16.4), and elevated jugular venous pulsation (LR+ = 8.9) are strong evidence in favor of the diagnosis. Furthermore, the combination of history of myocardial infarction and displaced apex on physical examination, although not particularly sensitive (39% sensitivity) was very specific (99% specificity) with high positive (89%) and negative (89%) predictive values. The authors also suggest that a breathless patient with a past history of myocardial infarction and a displaced apex beat on physical examination will almost certainly have heart failure and, if resources are limited, may not need echocardiography to confirm the diagnosis. However, less than 50% of breathless patients will have this combination, and the other half would therefore need echocardiography as the gold standard diagnostic tool for LVSD.
Morgan and coworkers28 assessed the prevalence and clinical characteristics of LVSD among elderly patients (those aged 70 years to 84 years) in a primary care setting by echocardiographic assessment of ventricular function. They found that no single clinical symptom or sign was both sensitive and specific, and concluded that diagnosis should not be based on clinical history and examination alone. They found that a substantial number of elderly individuals had asymptomatic or misdiagnosed LVSD, and suggested this might be due to the extremely limited sensitivity and specificity of clinical history taking and examination. For example, only 11% of patients with LVSD had a raised jugular venous pressure, and bilateral ankle edema was common but nonspecific. Researchers have therefore concluded that although these clinical findings are useful in acute severe heart failure, they have only a small role in detecting LVSD in the community.18
TABLE 1
The use of clinical symptoms and signs to diagnose heart failure, by study
| Sign or symptom | N | Setting* | Study quality (1a-5)† | Sensitivity (%) | Specificity (%) | LR+ | LR- | PV+(%) | PV-(%) |
|---|---|---|---|---|---|---|---|---|---|
| Previous myocardial infarction | |||||||||
| Davie, 199720 | 259 | R | 2b | 59 | 86 | 4.1 | 0.48 | 44 | 92 |
| Morgan, 199928 | 817 | P | 2b | 39 | 91 | 4.3 | 0.67 | ||
| Dyspnea on exertion | |||||||||
| Davie, 199720 | 259 | R | 2b | 100 | 17 | 1.20 | 0.06 | 18 | 100 |
| Morgan, 199928 | 817 | P | 2b | 15 | 97 | 5.4 | 0.88 | ||
| Orthopnea | |||||||||
| Davie, 199720 | 259 | R | 2b | 22 | 74 | 0.85 | 1.05 | 14 | 83 |
| Paroxysmal nocturnal dyspnea | |||||||||
| Davie, 199720 | 259 | R | 2b | 39 | 80 | 1.95 | 0.76 | 27 | 87 |
| History of peripheral edema | |||||||||
| Davie, 199720 | 259 | R | 2b | 49 | 47 | 0.92 | 1.09 | 15 | 83 |
| Tachycardia | |||||||||
| Davie, 199720 | 259 | R | 2b | 22 | 92 | 2.75 | 0.85 | 33 | 86 |
| Elevated JVP | |||||||||
| Davie, 199720 | 259 | R | 2b | 17 | 98 | 8.95 | 0.84 | 64 | 86 |
| Morgan, 199928 | 817 | R | 2b | 11 | 97 | 3.6 | 0.92 | ||
| Gallop rhythm | |||||||||
| Davie, 199720 | 259 | P | 2b | 24 | 99 | 24.0 | 0.77 | 77 | 87 |
| 3rd heart sound | |||||||||
| Rihal, 199524 | 554 | H | 2b | 9 | 97 | 3.00 | 0.94 | 54 | 78 |
| Laterally displaced apical impulse | |||||||||
| Davie, 199720 | 259 | R | 2b | 66 | 96 | 16.4 | 0.35 | 75 | 94 |
| Pulmonary rales | |||||||||
| Davie, 199720 | 259 | R | 2b | 29 | 77 | 1.26 | 0.92 | 19 | 85 |
| Morgan, 199928 | 817 | P | 2b | 44 | 82 | 2.4 | 0.68 | ||
| Peripheral edema on examination | |||||||||
| Davie, 199720 | 259 | R | 2b | 20 | 86 | 1.43 | 0.93 | 21 | 85 |
| Morgan, 199928 | 817 | P | 2b | 18 | 91 | 2.0 | 0.90 | ||
| NOTE: Pretest probability = 50%. | |||||||||
| *P denotes cross-sectional primary care population; R, primary care patients referred for suspected heart failure; H, hospitalized patients undergoing angiography. | |||||||||
| † Level 1a is the most rigorous; level 5 is the least rigorous. | |||||||||
| LR+ denotes positive likelihood ratio; LR-, negative likelihood ratio; PV+, positive predictive value; PV-, negative predictive value. | |||||||||
Laboratory and imaging evaluation
Although an important and valuable part of the evaluation, the history and physical examination alone are insufficient to confirm a diagnosis in most cases. Recommended initial tests for patients with signs or symptoms of heart failure include complete blood count (CBC), serum electrolytes, serum creatinine, serum albumin, liver function tests, urinalysis, electrocardiogram, and chest x-ray (Figure).
Blood tests. For those older than 65 years or with atrial fibrillation or evidence of thyroid disease, thyroid function tests should also be performed because heart failure due to thyrotoxicosis is frequently associated with rapid atrial fibrillation and hypothyroidism may also present as heart failure.8,10 The other routine blood tests are important as a way to exclude alternative diagnoses; they also help with the search for predisposing or exacerbating causes of the heart failure. These baseline tests also help guide future therapeutic decision making. For example, electrolyte and renal function results are pertinent when initiating angiotensin-converting enzyme (ACE) inhibitors. Anemia can exacerbate pre-existing heart failure, and measurement of renal function is essential to distinguish fluid overload due to heart failure from renal failure. Liver enzymes may be affected by hepatic congestion. Urinalysis is valuable in the detection of underlying renal disease or diabetes.8
Electrocardiography. An electrocardiogram (ECG) is another recommended part of the evaluation of the suspected heart failure patient.8-14 Considerable attention has been paid to examining the value of this test in the diagnosis of LVSD.29-32 Davie and colleagues29 assessed the value of the ECG in identifying patients with possible heart failure by examining referrals for echocardiography by primary care practitioners. A total of 534 patients were referred for echocardiography for possible heart failure, of whom 18% (n = 96) had LVSD. They showed that LVSD was extremely unlikely if the ECG result was normal, but that 1 in 3 patients with an abnormal result had significant LVSD. Thus, a normal ECG result virtually excludes chronic heart failure due to LVSD. However, the ECG is not a substitute for echocardiography, as an abnormal result does not accurately predict the presence of LVSD (Table 2).
Others have confirmed these findings.30,32 Talreja and colleagues30 found that of 330 consecutive in-patients referred for echocardiographic assessment of left ventricular function, 124 (41%) had LVSD. Only 2 of 124 patients with LVSD had a normal electrocardiogram result. When the ECG result is normal, the authors suggest that echocardiography is not needed. However, they concede that physicians are unlikely to adhere to this because many may not be as sophisticated in interpreting the ECG and may feel it important to get an accurate measure of ejection fraction. Guidelines published by the European Society of Cardiology10 state that a normal ECG result in patients with suspected heart failure should lead us to doubt the accuracy of the diagnosis.
Chest x-ray. The chest x-ray is most valuable as a test to exclude pulmonary causes. However, the existing evidence suggests it is not a reliable way to exclude LVSD.24,26,33,34 (Table 2) provides information about the value of radiography in predicting LVSD. A systematic review of the literature concluded that redistribution and cardiomegaly were the best chest radiographic findings for diagnosing increased preload and reduced ejection fraction, respectively.34 However, neither finding alone could adequately exclude or confirm LVSD. Studies published since that review have confirmed this finding.33 Although part of the evaluation of the heart failure patient, radiography is only one part of the diagnostic process and cannot be used to provide definitive diagnostic information.
Echocardiography. The most important step in the evaluation of the heart failure patient is the assessment of left ventricular systolic function. Both echocardiography and radionuclide ventriculography have been advocated.8-14 However, echocardiography is preferred as it is widely available, simple, noninvasive, safe, usually less expensive, and provides more information about valve function and left ventricular hypertrophy. Table 2 demonstrates the high sensitivity and specificity of echocardiography.35 In view of this, it is recommended as a standard adjunct to the clinical diagnosis of patients with dyspnea on exertion and suspected heart failure. Between 8% and 18% of patients will have inadequate echocardiograms, in which case radionuclide ventriculography is advocated.8
Neurohormonal markers. In recent years there has been increasing interest in the potential role of neurohormonal markers, such as B-type natriuretic peptide (BNP), atrial natriuretic peptide (ANP), N-terminal pro-ANP (N-ANP), and N-terminal pro-BNP (N-BNP) as indices of LVSD.36-42 Most of the data relating to these markers are relatively recent; therefore their use is not addressed in any detail in any of the aforementioned guidelines.
Some studies41,42 suggest that BNP and N-BNP are useful for diagnosing LVSD even when the positive predictive values are low, because of their high negative predictive values. One of the most recent studies44 examined the utility of BNP in an urgent care setting and suggested that BNP was an extremely reliable indicator of LVSD. In this population of patients with acute dyspnea where 39% had a final diagnosis of heart failure, 90% with a positive BNP had heart failure and 98% of those with a negative BNP did not. Although there appears to be a growing body of evidence supporting the role of these neurohormonal markers in the evaluation of the patient with LVSD, Table 2 illustrates that there have also been conflicting findings. This is partly because of differences in study design, study populations, cut-off points for ANP and BNP, and the definition of LVSD. Most studies agree that assessment of BNP, in particular, may be a cost-effective method for initial screening for LVSD, but should still be followed by an echocardiogram to confirm the diagnosis.
Management follows diagnosis. Making the correct diagnosis is the crucial first step in the management of chronic heart failure. Figure 1 summarizes the steps currently recommended for the evaluation of the patient with LVSD. A confirmation of a diagnosis of LVSD, however, is not the end of the story. Management will then need to include initiation of appropriate therapies and consideration of treatable and reversible etiologies, a subject to be addressed in the June 2002 issue of this journal.
TABLE 2
Key investigations used for the diagnosis of left ventricular systolic dysfunction
| Test | N | Setting* | Study quality † | Sensitivity (%) | Specificity(%) | LR+ | LR- | PV+ (%) | PV- (%) |
|---|---|---|---|---|---|---|---|---|---|
| Electrocardiogram | |||||||||
| Davie, 199729 | 534 | R | 1c | 94 | 61 | 2.43 | 0.10 | 35 | 98 |
| Lindsay, 200043 | 416 | R | 1c | 90 | 65 | 2.59 | 2.76 | 43 | 90 |
| Mosterd, 199732 | 1980 | R | 1c | 54 | 79 | 2.55 | 0.58 | 7 | 98 |
| Electrocardiogram (patient older than 70 years) | |||||||||
| Mosterd, 199732 | 1980 | R | 1c | 67 | 64 | 1.88 | 0.52 | 7 | 98 |
| Talreja, 200030 | 330 | H | 1c | 65 | 98 | 38.2 | 0.36 | 98 | 64 |
| Chest x-ray | |||||||||
| Badgett, 199634 | 29 studies | 2a | 51 | 79 | 2.43 | 0.62 | 71 | 62 | |
| Rihal, 199524 | 554 | H | 2b | 20 | 89 | 1.82 | 0.90 | 34 | 79 |
| Echocardiogram | |||||||||
| Erbel, 198435 | 110 | H | 1c | 80 | 100 | 80.0 | 0.20 | 100 | 85 |
| N-terminal ANP > 4.4 ng/mL | |||||||||
| McClure, 199840 | 134 | M | 2b | — | — | 1.08 | 0.96 | 52 | 51 |
| N-terminal pro-BNP > 275 fmol/mL | |||||||||
| Talwar, 199942 | 249 | R | 2b | 94 | 55 | 2.09 | 011 | 58 | 93 |
| BNP > 75 pg/mL | |||||||||
| Maisel, 200137 | 200 | R | 1c | 86 | 98 | 43.0 | 0.14 | 98 | 89 |
| Dao, 200144 | 250 | U | 1b | 98 | 92 | 12.2 | 0.02 | 92 | 98 |
| BNP > 46 pg/mL | |||||||||
| McClure, 199840 | 134 | M | 2b | — | — | 2.25 | 0.83 | 69 | 55 |
| BNP > 17.9 pg/mL | |||||||||
| McDonagh, 199841 | 1653 | P | 2b | 76 | 87 | 5.85 | 0.28 | 16 | 97 |
| NOTE: Pretest probability = 50%. | |||||||||
| *P denotes cross-sectional primary care population; R, primary care patients referred for suspected heart failure; H, hospitalized patients undergoing angiography; U, urgent care center; M, long-term myocardial infarction survivors recalled by their family physician. | |||||||||
| † Level 1a is the most rigorous; level 5 is the least rigorous. | |||||||||
| ANP, atrial natriuretic peptide; BNP, B-type natriuretic peptide; LR+, positive likelihood ratio; LR-, negative likelihood ratio; PV+, positive predictive value; PV-, negative predictive value. | |||||||||
Figure
Steps in the assessment of the patient with suspected heart failure
ACKNOWLEDGMENTS
We wish to thank Mr Chris Shiels at the Department of Primary Care, University of Liverpool, for his valuable advice regarding this manuscript.
1. Mair FS, Crowley TS, Bundred PE. Prevalence, aetiology and management of heart failure in general practice. Br J Gen Pract 1996;46:77-9.
2. Wheeldon NM, MacDonald TM, Flucker CJ, McDermitt DG, Struthers AD. An electrocardiographic study of chronic heart failure in the community. QJM 1993;86:17-23.
3. O’Connell JB, Bristow MR. Economic impact of heart failure in the United States: time for a different approach. J Heart Lung Transplan 1994;13:S107-112.
4. O’Connell JB. The economic burden of heart failure. Clin Cardiol 2000;23 (3 Suppl):III6-10.
5. English MA, Mastrean MB. Congestive heart failure: public and private burden. Crit Care Nurs Q 1995;18:1-6.
6. Croft JB, Giles WH, Pollard RA, Keenan NL, Casper ML, Anda RF. Heart failure survival among older adults in the United States: a poor prognosis for an emerging epidemic in the Medicare population. Arch Intern Med 1999;159:505-10.
7. Stewart S, MacIntyre K, Hole DJ, Capewell S, McMurray JJV. More ‘malignant’ than cancer? Five-year survival following a first admission for heart failure. Eur J Heart Fail 2001;3:315-22.
8. Konstam M, Dracup K, Baker D, et al. Heart failure: evaluation and care of patients with left-ventricular systolic dysfunction. Clinical Practice Guideline No. 11. AHCPR Publication No. 94-0612. Agency for Health Care Policy and Research, Public Health Service, US Department of Health and Human Services, Rockville, Md.
9. Guidelines for the evaluation and management of heart failure. Report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Committee on Evaluation and Management of Heart Failure). Circulation 1995;92:2764-84.
10. The Task Force on Heart Failure of the European Society of Cardiology. Guidelines for the diagnosis of heart failure. Eur Heart J 1995;16:741-51.
11. Heart failure —systolic dysfunction. University of Michigan Health System. August 1999. (Available at http://cme.med.umich.edu/pdf/guideline/heart.pdf)
12. The Task Force of the Working Group on Heart Failure of the European Society of Cardiolog. The treatment of heart failure. Eur Heart J 1997;18:736-53.
13. Diagnosis and treatment of heart failure due to left ventricular systolic dysfunction. A national clinical guideline. Scottish Intercollegiate Guidelines Network (SIGN); SIGN publication; no. 35. Feb 1999; 68.
14. Anonymous. Heart Failure Society of America (HFSA) practice guidelines. HFSA guidelines for management of patients with heart failure caused by left ventricular systolic dysfunction—pharmacological approaches [published erratum appears in J Card Fail 2000 Mar; 6:74]. J Card Fail 5:357-82.
15. McMurray JJV, Dargie HJ. Diagnosis and management of heart failure. BMJ 1994;308:321-8.
16. Mair FS. Management of heart failure. Am Fam Phys 1996;54:245-54.
17. Marantz PR, Tobin JN, Wassertheil-Smoller S, et al. The relationship between left ventricular systolic function and congestive heart failure diagnosed by clinical criteria. Circulation 1988;77:607-12.
18. Gillespie ND, McNeill G, Pringle T, Ogston S, Struthers AD, Pringle SD. Cross sectional study of contribution of clinical assessment and simple cardiac investigations to diagnosis of left ventricular systolic dysfunction in patients admitted with acute dyspnoea. BMJ 1997;314:936-40.
19. Remes J, Miettinen H, Reunanen A, Pyorala K. Validity of clinical diagnosis of heart failure in primary health care. Eur Heart J 1991;12:315-21.
20. Davie AP, Francis CM, Caruana L, Sutherland GR, McMurray JJV. Assessing diagnosis in heart failure: which features are of any use? QJM 1997;90:335-9.
21. Gadsboll N, Hoilund-Carlsen PF, Nielsen GG, et al. Symptoms and signs of heart failure in patients with myocardial infarction: reproducibility and relationship to chest X-ray, radionuclide ventriculog-raphy, and right heart catheterisation. Eur Heart J 1989;10:1017-28.
22. Stevenson LW, Perloff JK. The limited reliability of physical signs for estimating hemodynamics in chronic heart failure. JAMA 1989;261:884-8.
23. Ishmail AA, Wing S, Ferguson J, Hutchinson TA, Magder S, Flegel KM. Interobserver agreement by auscultation in the presence of a third heart sound in patients with congestive heart failure. Chest 1987;91:870-3.
24. Rihal CS, Davis KB, Kennedy W, Gersh BJ. The utility of clinical, electrocardiographic and roentgenographic variables in the prediction of left ventricular function. Am J Cardiol 1995;752:220-3.
25. Harlan WR, Oberman A, Grimm R, Rosati RA. Chronic congestive heart failure in coronary artery disease: clinical criteria. Ann Intern Med 1977;86:133-8.
26. Chakko S, Woska D, Martinez H, et al. Clinical, radiographic, and hemodynamic correlations in chronic congestive heart failure: conflicting results may lead to inappropriate care. Am J Med 1991;90:353-9.
27. Mattleman SJ, Hakki A, Iskandrian AS, Segal BL, Kane SA. Reliability of bedside evaluation in determining left ventricular function: correlation with left ventricular ejection fraction determined by radionuclide ventriculography. J Am Coll Cardio 1983;1:417-20.
28. Morgan S, Smith H, Simpson I, et al. Prevalence and clinical characteristics of left ventricular dysfunction among elderly patients in general practice setting: cross sectional survey. BMJ 1999;318:368-72.
29. Davie AP, Francis CM, Love MP, et al. Value of electrocardiogram in identifying heart failure due to left ventricular systolic dysfunction. BMJ 1996;312:222-3.
30. Talreja D, Gruver C, Sklenar J, Dent J, Kaul S. Efficient utilization of echocardiography for the assessment of left ventricular systolic function. Am Heart J 2000;139:394-8.
31. Murkofsky RL, Dangas G, Diamond JA, et al. A prolonged QRS duration on surface electrocardiogram is a specific indicator of left ventricular dysfunction. J Am Coll Cardiol 1998;32:476-82.
32. Mosterd A, de Bruijne MC, Hoes AW, et al. Usefulness of echocardiography in detecting left ventricular dysfunction in population-based studies (The Rotterdam Study). Am J Cardiol 1997;79:103-4.
33. Clark AL, Coats ALS. Unreliability of cardiothoracic ratio as a marker of left ventricular impairment: comparison with radionuclide ventriculography and echocardiography. Postgrad Med J 2000;76:289-91.
34. Badgett RG, Mulrow CD, Otto PM, Ramirez G. How well can the chest radiograph diagnose left ventricular dysfunction? J Gen Intern Med 1996;11:625-34.
35. Erbel R, Schweizer P, Drebs W, Meyer J, Effert S. Sensitivity and specificity of two-dimensional echocardiography in detection of impaired left ventricular function. Eur Heart J 1984;5:477-89.
36. Davis M, Espiner E, Richards G, et al. Plasma brain natriuretic peptide in assessment of acute dyspnoea. Lancet 1994;343:440-4.
37. Maisel AS, Koon J, Krishnaswamy P, et al. Utility of B-natriuretic peptide as a rapid, point-of-care test for screening patients undergoing echocardiography to determine left ventricular dysfunction. Am Heart J 2001;141:367-74.
38. Schirmer H, Omland T. Circulating N-terminal pro-atrial natriuretic peptide is an independent predictor of left ventricular hypertrophy in the general population. The Tromsø Study. Eur Heart J 1999;20:755-63.
39. Lerman A, Gibbons RJ, Rodeheffer RJ, et al. Circulating N-terminal atrial natriuretic peptide as a marker for symptomless left-ventricular dysfunction. Lancet 1993;341:1105-9.
40. McClure SJ, Davie AP, Goldthorp S, et al. Cohort study of plasma natriuretic peptides for identifying left ventricular systolic dysfunction in primary care. BMJ 1998;317:516-9.
41. McDonagh TA, Robb SD, Murdoch DR, et al. Biochemical detection of left-ventricular systolic dysfunction. Lancet 1998;351:9-13,
42. Talwar S, Squire IB, Davies JE, et al. Plasma N-terminal pro-brain natriuretic peptide and the ECG in the assessment of left-ventricular systolic dysfunction in a high risk population. Eur Heart J 1999;20:1736-1744.
43. Lindsay MM, Goodfield NER, Hogg KJ, Dunn EG. Optimising direct access echo referral in suspected heart failure. Scot Med J 2000;45:043-044.
44. Dao Q, Krishnaswamy P, Kazanegra R, et al. Utility of B-Type natriuretic peptide in the diagnosis of congestive heart failure in an urgent care setting. J Am Coll Cardiol 2001;37:379-85.
1. Mair FS, Crowley TS, Bundred PE. Prevalence, aetiology and management of heart failure in general practice. Br J Gen Pract 1996;46:77-9.
2. Wheeldon NM, MacDonald TM, Flucker CJ, McDermitt DG, Struthers AD. An electrocardiographic study of chronic heart failure in the community. QJM 1993;86:17-23.
3. O’Connell JB, Bristow MR. Economic impact of heart failure in the United States: time for a different approach. J Heart Lung Transplan 1994;13:S107-112.
4. O’Connell JB. The economic burden of heart failure. Clin Cardiol 2000;23 (3 Suppl):III6-10.
5. English MA, Mastrean MB. Congestive heart failure: public and private burden. Crit Care Nurs Q 1995;18:1-6.
6. Croft JB, Giles WH, Pollard RA, Keenan NL, Casper ML, Anda RF. Heart failure survival among older adults in the United States: a poor prognosis for an emerging epidemic in the Medicare population. Arch Intern Med 1999;159:505-10.
7. Stewart S, MacIntyre K, Hole DJ, Capewell S, McMurray JJV. More ‘malignant’ than cancer? Five-year survival following a first admission for heart failure. Eur J Heart Fail 2001;3:315-22.
8. Konstam M, Dracup K, Baker D, et al. Heart failure: evaluation and care of patients with left-ventricular systolic dysfunction. Clinical Practice Guideline No. 11. AHCPR Publication No. 94-0612. Agency for Health Care Policy and Research, Public Health Service, US Department of Health and Human Services, Rockville, Md.
9. Guidelines for the evaluation and management of heart failure. Report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Committee on Evaluation and Management of Heart Failure). Circulation 1995;92:2764-84.
10. The Task Force on Heart Failure of the European Society of Cardiology. Guidelines for the diagnosis of heart failure. Eur Heart J 1995;16:741-51.
11. Heart failure —systolic dysfunction. University of Michigan Health System. August 1999. (Available at http://cme.med.umich.edu/pdf/guideline/heart.pdf)
12. The Task Force of the Working Group on Heart Failure of the European Society of Cardiolog. The treatment of heart failure. Eur Heart J 1997;18:736-53.
13. Diagnosis and treatment of heart failure due to left ventricular systolic dysfunction. A national clinical guideline. Scottish Intercollegiate Guidelines Network (SIGN); SIGN publication; no. 35. Feb 1999; 68.
14. Anonymous. Heart Failure Society of America (HFSA) practice guidelines. HFSA guidelines for management of patients with heart failure caused by left ventricular systolic dysfunction—pharmacological approaches [published erratum appears in J Card Fail 2000 Mar; 6:74]. J Card Fail 5:357-82.
15. McMurray JJV, Dargie HJ. Diagnosis and management of heart failure. BMJ 1994;308:321-8.
16. Mair FS. Management of heart failure. Am Fam Phys 1996;54:245-54.
17. Marantz PR, Tobin JN, Wassertheil-Smoller S, et al. The relationship between left ventricular systolic function and congestive heart failure diagnosed by clinical criteria. Circulation 1988;77:607-12.
18. Gillespie ND, McNeill G, Pringle T, Ogston S, Struthers AD, Pringle SD. Cross sectional study of contribution of clinical assessment and simple cardiac investigations to diagnosis of left ventricular systolic dysfunction in patients admitted with acute dyspnoea. BMJ 1997;314:936-40.
19. Remes J, Miettinen H, Reunanen A, Pyorala K. Validity of clinical diagnosis of heart failure in primary health care. Eur Heart J 1991;12:315-21.
20. Davie AP, Francis CM, Caruana L, Sutherland GR, McMurray JJV. Assessing diagnosis in heart failure: which features are of any use? QJM 1997;90:335-9.
21. Gadsboll N, Hoilund-Carlsen PF, Nielsen GG, et al. Symptoms and signs of heart failure in patients with myocardial infarction: reproducibility and relationship to chest X-ray, radionuclide ventriculog-raphy, and right heart catheterisation. Eur Heart J 1989;10:1017-28.
22. Stevenson LW, Perloff JK. The limited reliability of physical signs for estimating hemodynamics in chronic heart failure. JAMA 1989;261:884-8.
23. Ishmail AA, Wing S, Ferguson J, Hutchinson TA, Magder S, Flegel KM. Interobserver agreement by auscultation in the presence of a third heart sound in patients with congestive heart failure. Chest 1987;91:870-3.
24. Rihal CS, Davis KB, Kennedy W, Gersh BJ. The utility of clinical, electrocardiographic and roentgenographic variables in the prediction of left ventricular function. Am J Cardiol 1995;752:220-3.
25. Harlan WR, Oberman A, Grimm R, Rosati RA. Chronic congestive heart failure in coronary artery disease: clinical criteria. Ann Intern Med 1977;86:133-8.
26. Chakko S, Woska D, Martinez H, et al. Clinical, radiographic, and hemodynamic correlations in chronic congestive heart failure: conflicting results may lead to inappropriate care. Am J Med 1991;90:353-9.
27. Mattleman SJ, Hakki A, Iskandrian AS, Segal BL, Kane SA. Reliability of bedside evaluation in determining left ventricular function: correlation with left ventricular ejection fraction determined by radionuclide ventriculography. J Am Coll Cardio 1983;1:417-20.
28. Morgan S, Smith H, Simpson I, et al. Prevalence and clinical characteristics of left ventricular dysfunction among elderly patients in general practice setting: cross sectional survey. BMJ 1999;318:368-72.
29. Davie AP, Francis CM, Love MP, et al. Value of electrocardiogram in identifying heart failure due to left ventricular systolic dysfunction. BMJ 1996;312:222-3.
30. Talreja D, Gruver C, Sklenar J, Dent J, Kaul S. Efficient utilization of echocardiography for the assessment of left ventricular systolic function. Am Heart J 2000;139:394-8.
31. Murkofsky RL, Dangas G, Diamond JA, et al. A prolonged QRS duration on surface electrocardiogram is a specific indicator of left ventricular dysfunction. J Am Coll Cardiol 1998;32:476-82.
32. Mosterd A, de Bruijne MC, Hoes AW, et al. Usefulness of echocardiography in detecting left ventricular dysfunction in population-based studies (The Rotterdam Study). Am J Cardiol 1997;79:103-4.
33. Clark AL, Coats ALS. Unreliability of cardiothoracic ratio as a marker of left ventricular impairment: comparison with radionuclide ventriculography and echocardiography. Postgrad Med J 2000;76:289-91.
34. Badgett RG, Mulrow CD, Otto PM, Ramirez G. How well can the chest radiograph diagnose left ventricular dysfunction? J Gen Intern Med 1996;11:625-34.
35. Erbel R, Schweizer P, Drebs W, Meyer J, Effert S. Sensitivity and specificity of two-dimensional echocardiography in detection of impaired left ventricular function. Eur Heart J 1984;5:477-89.
36. Davis M, Espiner E, Richards G, et al. Plasma brain natriuretic peptide in assessment of acute dyspnoea. Lancet 1994;343:440-4.
37. Maisel AS, Koon J, Krishnaswamy P, et al. Utility of B-natriuretic peptide as a rapid, point-of-care test for screening patients undergoing echocardiography to determine left ventricular dysfunction. Am Heart J 2001;141:367-74.
38. Schirmer H, Omland T. Circulating N-terminal pro-atrial natriuretic peptide is an independent predictor of left ventricular hypertrophy in the general population. The Tromsø Study. Eur Heart J 1999;20:755-63.
39. Lerman A, Gibbons RJ, Rodeheffer RJ, et al. Circulating N-terminal atrial natriuretic peptide as a marker for symptomless left-ventricular dysfunction. Lancet 1993;341:1105-9.
40. McClure SJ, Davie AP, Goldthorp S, et al. Cohort study of plasma natriuretic peptides for identifying left ventricular systolic dysfunction in primary care. BMJ 1998;317:516-9.
41. McDonagh TA, Robb SD, Murdoch DR, et al. Biochemical detection of left-ventricular systolic dysfunction. Lancet 1998;351:9-13,
42. Talwar S, Squire IB, Davies JE, et al. Plasma N-terminal pro-brain natriuretic peptide and the ECG in the assessment of left-ventricular systolic dysfunction in a high risk population. Eur Heart J 1999;20:1736-1744.
43. Lindsay MM, Goodfield NER, Hogg KJ, Dunn EG. Optimising direct access echo referral in suspected heart failure. Scot Med J 2000;45:043-044.
44. Dao Q, Krishnaswamy P, Kazanegra R, et al. Utility of B-Type natriuretic peptide in the diagnosis of congestive heart failure in an urgent care setting. J Am Coll Cardiol 2001;37:379-85.