User login
Method may enable eradication of LSCs in AML
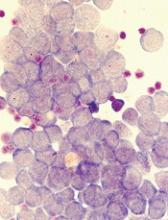
Disrupting mitophagy may be a “promising strategy” for eliminating leukemia stem cells (LSCs) in acute myeloid leukemia (AML), according to researchers.
The team found that AML LSCs depend on mitophagy to maintain their “stemness,” but targeting the central metabolic stress regulator AMPK or the mitochondrial dynamics regulator FIS1 can disrupt mitophagy and impair LSC function.
Craig T. Jordan, PhD, of the University of Colorado in Aurora, and his colleagues reported these findings in Cell Stem Cell.
The researchers said in vitro experiments showed that LSCs have elevated levels of FIS1 and “distinct mitochondrial morphology.”
When the team inhibited FIS1 in the AML cell line MOLM-13 and primary AML cells, they observed disruption of mitochondrial dynamics. Experiments in mouse models indicated that FIS1 is required for LSC self-renewal.
Specifically, the researchers said they found that depletion of FIS1 hinders mitophagy and leads to inactivation of GSK3, myeloid differentiation, cell-cycle arrest, and loss of LSC function.
Dr Jordan and his colleagues also found that AMPK is an upstream regulator of FIS1, and targeting AMPK produces similar effects as targeting FIS1—namely, disrupting mitophagy and impairing LSC self-renewal.
The researchers said their findings suggest that mitochondrial stress generated from oncogenic transformation may activate AMPK signaling in LSCs. And the AMPK signaling drives FIS1-mediated mitophagy, which eliminates stressed mitochondria and allows LSCs to thrive.
However, when AMPK or FIS1 is inhibited, the damaged mitochondria are not eliminated. This leads to “GSK3 inhibition and other unknown events” that prompt differentiation and hinder LSC function.
“Leukemia stem cells require AMPK for their survival, but normal hematopoietic cells can do without it,” Dr Jordan noted. “The reason this study is so important is that, so far, nobody’s come up with a good way to kill leukemia stem cells while sparing normal blood-forming cells. If we can translate this concept to patients, the potential for improved therapy is very exciting.”
Disrupting mitophagy may be a “promising strategy” for eliminating leukemia stem cells (LSCs) in acute myeloid leukemia (AML), according to researchers.
The team found that AML LSCs depend on mitophagy to maintain their “stemness,” but targeting the central metabolic stress regulator AMPK or the mitochondrial dynamics regulator FIS1 can disrupt mitophagy and impair LSC function.
Craig T. Jordan, PhD, of the University of Colorado in Aurora, and his colleagues reported these findings in Cell Stem Cell.
The researchers said in vitro experiments showed that LSCs have elevated levels of FIS1 and “distinct mitochondrial morphology.”
When the team inhibited FIS1 in the AML cell line MOLM-13 and primary AML cells, they observed disruption of mitochondrial dynamics. Experiments in mouse models indicated that FIS1 is required for LSC self-renewal.
Specifically, the researchers said they found that depletion of FIS1 hinders mitophagy and leads to inactivation of GSK3, myeloid differentiation, cell-cycle arrest, and loss of LSC function.
Dr Jordan and his colleagues also found that AMPK is an upstream regulator of FIS1, and targeting AMPK produces similar effects as targeting FIS1—namely, disrupting mitophagy and impairing LSC self-renewal.
The researchers said their findings suggest that mitochondrial stress generated from oncogenic transformation may activate AMPK signaling in LSCs. And the AMPK signaling drives FIS1-mediated mitophagy, which eliminates stressed mitochondria and allows LSCs to thrive.
However, when AMPK or FIS1 is inhibited, the damaged mitochondria are not eliminated. This leads to “GSK3 inhibition and other unknown events” that prompt differentiation and hinder LSC function.
“Leukemia stem cells require AMPK for their survival, but normal hematopoietic cells can do without it,” Dr Jordan noted. “The reason this study is so important is that, so far, nobody’s come up with a good way to kill leukemia stem cells while sparing normal blood-forming cells. If we can translate this concept to patients, the potential for improved therapy is very exciting.”
Disrupting mitophagy may be a “promising strategy” for eliminating leukemia stem cells (LSCs) in acute myeloid leukemia (AML), according to researchers.
The team found that AML LSCs depend on mitophagy to maintain their “stemness,” but targeting the central metabolic stress regulator AMPK or the mitochondrial dynamics regulator FIS1 can disrupt mitophagy and impair LSC function.
Craig T. Jordan, PhD, of the University of Colorado in Aurora, and his colleagues reported these findings in Cell Stem Cell.
The researchers said in vitro experiments showed that LSCs have elevated levels of FIS1 and “distinct mitochondrial morphology.”
When the team inhibited FIS1 in the AML cell line MOLM-13 and primary AML cells, they observed disruption of mitochondrial dynamics. Experiments in mouse models indicated that FIS1 is required for LSC self-renewal.
Specifically, the researchers said they found that depletion of FIS1 hinders mitophagy and leads to inactivation of GSK3, myeloid differentiation, cell-cycle arrest, and loss of LSC function.
Dr Jordan and his colleagues also found that AMPK is an upstream regulator of FIS1, and targeting AMPK produces similar effects as targeting FIS1—namely, disrupting mitophagy and impairing LSC self-renewal.
The researchers said their findings suggest that mitochondrial stress generated from oncogenic transformation may activate AMPK signaling in LSCs. And the AMPK signaling drives FIS1-mediated mitophagy, which eliminates stressed mitochondria and allows LSCs to thrive.
However, when AMPK or FIS1 is inhibited, the damaged mitochondria are not eliminated. This leads to “GSK3 inhibition and other unknown events” that prompt differentiation and hinder LSC function.
“Leukemia stem cells require AMPK for their survival, but normal hematopoietic cells can do without it,” Dr Jordan noted. “The reason this study is so important is that, so far, nobody’s come up with a good way to kill leukemia stem cells while sparing normal blood-forming cells. If we can translate this concept to patients, the potential for improved therapy is very exciting.”
Protein ‘atlas’ could aid study, treatment of diseases
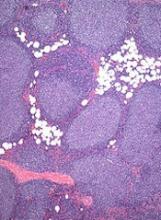
New technology has enabled researchers to create a “genomic atlas of the human plasma proteome,” according to an article published in Nature.
The researchers identified nearly 2000 genetic associations with close to 1500 proteins, and they believe these discoveries will improve our understanding of diseases and aid drug development.
“Compared to genes, proteins have been relatively understudied in human blood, even though they are the ‘effectors’ of human biology, are disrupted in many diseases, and are the targets of most medicines,” said study author Adam Butterworth, PhD, of the University of Cambridge in the UK.
“Novel technologies are now allowing us to start addressing this gap in our knowledge.”
Dr Butterworth and his colleagues used an assay called SOMAscan (developed by the company SomaLogic) to measure 3622 proteins in the blood of 3301 people. The team then analyzed the DNA of these individuals to see which regions of their genomes were associated with protein levels.
In this way, the researchers found 1927 significant associations between 1478 proteins and 764 genomic regions. These findings are publicly available via the University of Cambridge website.
The researchers said one way to use this information is to identify biological pathways that cause diseases.
“Thanks to the genomics revolution over the past decade, we’ve been good at finding statistical associations between the genome and disease, but the difficulty has been then identifying the disease-causing genes and pathways,” said study author James Peters, PhD, of the University of Cambridge.
“Now, by combining our database with what we know about associations between genetic variants and disease, we are able to say a lot more about the biology of disease.”
In some cases, the researchers identified multiple genetic variants influencing levels of a protein. By combining these variants into a “score” for that protein, they were able to identify new associations between proteins and disease.
The team also said the proteomic genetic data can be used to aid drug development. In addition to highlighting potential side effects of drugs, the findings can provide insights on protein targets of new and existing drugs.
By linking drugs, proteins, genetic variation, and diseases, the researchers have already suggested existing drugs that could potentially be used to treat different diseases and increased confidence that certain drugs currently in development might be successful in clinical trials.
“Our database is really just a starting point,” said study author Benjamin Sun, an MB/PhD student at the University of Cambridge.
“We’ve given some examples in this study of how it might be used, but now it’s over to the research community to begin using it and finding new applications.”
The research was funded by MSD, National Institute for Health Research, NHS Blood and Transplant, British Heart Foundation, Medical Research Council, UK Research and Innovation, and SomaLogic.
New technology has enabled researchers to create a “genomic atlas of the human plasma proteome,” according to an article published in Nature.
The researchers identified nearly 2000 genetic associations with close to 1500 proteins, and they believe these discoveries will improve our understanding of diseases and aid drug development.
“Compared to genes, proteins have been relatively understudied in human blood, even though they are the ‘effectors’ of human biology, are disrupted in many diseases, and are the targets of most medicines,” said study author Adam Butterworth, PhD, of the University of Cambridge in the UK.
“Novel technologies are now allowing us to start addressing this gap in our knowledge.”
Dr Butterworth and his colleagues used an assay called SOMAscan (developed by the company SomaLogic) to measure 3622 proteins in the blood of 3301 people. The team then analyzed the DNA of these individuals to see which regions of their genomes were associated with protein levels.
In this way, the researchers found 1927 significant associations between 1478 proteins and 764 genomic regions. These findings are publicly available via the University of Cambridge website.
The researchers said one way to use this information is to identify biological pathways that cause diseases.
“Thanks to the genomics revolution over the past decade, we’ve been good at finding statistical associations between the genome and disease, but the difficulty has been then identifying the disease-causing genes and pathways,” said study author James Peters, PhD, of the University of Cambridge.
“Now, by combining our database with what we know about associations between genetic variants and disease, we are able to say a lot more about the biology of disease.”
In some cases, the researchers identified multiple genetic variants influencing levels of a protein. By combining these variants into a “score” for that protein, they were able to identify new associations between proteins and disease.
The team also said the proteomic genetic data can be used to aid drug development. In addition to highlighting potential side effects of drugs, the findings can provide insights on protein targets of new and existing drugs.
By linking drugs, proteins, genetic variation, and diseases, the researchers have already suggested existing drugs that could potentially be used to treat different diseases and increased confidence that certain drugs currently in development might be successful in clinical trials.
“Our database is really just a starting point,” said study author Benjamin Sun, an MB/PhD student at the University of Cambridge.
“We’ve given some examples in this study of how it might be used, but now it’s over to the research community to begin using it and finding new applications.”
The research was funded by MSD, National Institute for Health Research, NHS Blood and Transplant, British Heart Foundation, Medical Research Council, UK Research and Innovation, and SomaLogic.
New technology has enabled researchers to create a “genomic atlas of the human plasma proteome,” according to an article published in Nature.
The researchers identified nearly 2000 genetic associations with close to 1500 proteins, and they believe these discoveries will improve our understanding of diseases and aid drug development.
“Compared to genes, proteins have been relatively understudied in human blood, even though they are the ‘effectors’ of human biology, are disrupted in many diseases, and are the targets of most medicines,” said study author Adam Butterworth, PhD, of the University of Cambridge in the UK.
“Novel technologies are now allowing us to start addressing this gap in our knowledge.”
Dr Butterworth and his colleagues used an assay called SOMAscan (developed by the company SomaLogic) to measure 3622 proteins in the blood of 3301 people. The team then analyzed the DNA of these individuals to see which regions of their genomes were associated with protein levels.
In this way, the researchers found 1927 significant associations between 1478 proteins and 764 genomic regions. These findings are publicly available via the University of Cambridge website.
The researchers said one way to use this information is to identify biological pathways that cause diseases.
“Thanks to the genomics revolution over the past decade, we’ve been good at finding statistical associations between the genome and disease, but the difficulty has been then identifying the disease-causing genes and pathways,” said study author James Peters, PhD, of the University of Cambridge.
“Now, by combining our database with what we know about associations between genetic variants and disease, we are able to say a lot more about the biology of disease.”
In some cases, the researchers identified multiple genetic variants influencing levels of a protein. By combining these variants into a “score” for that protein, they were able to identify new associations between proteins and disease.
The team also said the proteomic genetic data can be used to aid drug development. In addition to highlighting potential side effects of drugs, the findings can provide insights on protein targets of new and existing drugs.
By linking drugs, proteins, genetic variation, and diseases, the researchers have already suggested existing drugs that could potentially be used to treat different diseases and increased confidence that certain drugs currently in development might be successful in clinical trials.
“Our database is really just a starting point,” said study author Benjamin Sun, an MB/PhD student at the University of Cambridge.
“We’ve given some examples in this study of how it might be used, but now it’s over to the research community to begin using it and finding new applications.”
The research was funded by MSD, National Institute for Health Research, NHS Blood and Transplant, British Heart Foundation, Medical Research Council, UK Research and Innovation, and SomaLogic.
Treatment improves PFS in early stage FL
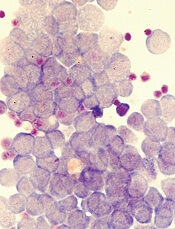
A multidrug regimen can improve upon involved-field radiotherapy (IFRT) in patients with early stage follicular lymphoma (FL), according to research published in the Journal of Clinical Oncology.
FL patients who received IFRT plus cyclophosphamide, vincristine, and prednisolone (CVP)—with or without rituximab—had a significant improvement in progression-free survival (PFS) compared to patients who received standard treatment with IFRT alone.
However, there was no significant difference in overall survival (OS) between the treatment arms.
“This is the first successful randomized study ever to be conducted in early stage follicular lymphoma comparing standard therapy to standard therapy plus effective chemotherapy or immunochemotherapy,” said Michael MacManus, MBBCh, of Peter MacCallum Cancer Centre in Melbourne, Victoria, Australia.
“It shows that the initial treatment received by patients can significantly affect their long-term chance of staying free from disease. Moving forward, we are interested in determining whether there is a benefit in overall long-term survival for patients treated with the combination with further follow-up, and if there is any way to predict if a person will benefit from combined treatment based on analyses of blood or biopsy specimens.”
Dr MacManus and his colleagues studied 150 patients with stage I to II, low-grade FL who were enrolled in this trial between 2000 and 2012.
At randomization, the patients’ median age was 57, 52% were male, 75% had stage I disease, and 48% had PET staging.
Half of patients (n=75) were randomized to receive IFRT (30-36 Gy) alone, and half were randomized to IFRT (30-36 Gy) plus 6 cycles of CVP. From 2006 on, patients in the CVP arm received rituximab (R) as well (n=31).
Baseline characteristics were well-balanced between the treatment arms.
Efficacy
The median follow-up was 9.6 years (range, 3.1 to 15.8 years).
PFS was significantly better among patients randomized to receive CVP±R (hazard ratio [HR]=0.57; P=0.033). The estimated 10-year PFS rate was 41% in the IFRT arm and 59% in the CVP±R arm.
Patients randomized to receive CVP plus R (n=31) had significantly better PFS than patients randomized to receive IFRT alone (n=31) over the same time period (HR=0.26; P=0.045).
There were 10 deaths in the IRFT arm and 5 in the CVP±R arm, but there was no significant difference in OS between the arms (HR=0.62; P=0.40). The 10-year OS rate was 86% in the IFRT arm and 95% in the CVP±R arm.
There was no significant between-arm difference in transformation to aggressive lymphoma (P=0.1). Transformation occurred in 10 patients in the IFRT arm and 4 in the CVP±R arm.
Safety
There were 148 patients from both arms who ultimately received IFRT, and 69 patients who received CVP±R.
Grade 2 toxicities occurring in more than 10% of IFRT recipients included upper gastrointestinal (n=27; 18%), skin (n=21; 14%), and mucous membrane (n=19; 12%) toxicity. One IFRT recipient had grade 3 mucositis, and 1 had grade 4 esophageal/pharyngeal mucosal toxicity.
Grade 3 toxicities occurring in at least 2 patients in the CVP±R arm included neutropenia (n=10; 14%), infection (n=8; 12%), diarrhea (n=3; 4%), elevated gamma-glutamyl transferase (n=3; 4%), fatigue (n=3; 4%), and febrile neutropenia (n=3; 4%).
Three patients (4%) in the CVP±R arm had acute grade 3 neuropathy related to vincristine. Ten patients (14%) had grade 4 neutropenia.
The most common late toxicities for the entire patient cohort were salivary gland (n=8; 5%) and skin (n=4; 3%) toxicities.
Grade 3 lung and menopausal toxicities occurred in 1 patient each. Two patients had late grade 3 vincristine neuropathy. One patient who had grade 3 neuropathy during chemotherapy progressed to grade 4.
A multidrug regimen can improve upon involved-field radiotherapy (IFRT) in patients with early stage follicular lymphoma (FL), according to research published in the Journal of Clinical Oncology.
FL patients who received IFRT plus cyclophosphamide, vincristine, and prednisolone (CVP)—with or without rituximab—had a significant improvement in progression-free survival (PFS) compared to patients who received standard treatment with IFRT alone.
However, there was no significant difference in overall survival (OS) between the treatment arms.
“This is the first successful randomized study ever to be conducted in early stage follicular lymphoma comparing standard therapy to standard therapy plus effective chemotherapy or immunochemotherapy,” said Michael MacManus, MBBCh, of Peter MacCallum Cancer Centre in Melbourne, Victoria, Australia.
“It shows that the initial treatment received by patients can significantly affect their long-term chance of staying free from disease. Moving forward, we are interested in determining whether there is a benefit in overall long-term survival for patients treated with the combination with further follow-up, and if there is any way to predict if a person will benefit from combined treatment based on analyses of blood or biopsy specimens.”
Dr MacManus and his colleagues studied 150 patients with stage I to II, low-grade FL who were enrolled in this trial between 2000 and 2012.
At randomization, the patients’ median age was 57, 52% were male, 75% had stage I disease, and 48% had PET staging.
Half of patients (n=75) were randomized to receive IFRT (30-36 Gy) alone, and half were randomized to IFRT (30-36 Gy) plus 6 cycles of CVP. From 2006 on, patients in the CVP arm received rituximab (R) as well (n=31).
Baseline characteristics were well-balanced between the treatment arms.
Efficacy
The median follow-up was 9.6 years (range, 3.1 to 15.8 years).
PFS was significantly better among patients randomized to receive CVP±R (hazard ratio [HR]=0.57; P=0.033). The estimated 10-year PFS rate was 41% in the IFRT arm and 59% in the CVP±R arm.
Patients randomized to receive CVP plus R (n=31) had significantly better PFS than patients randomized to receive IFRT alone (n=31) over the same time period (HR=0.26; P=0.045).
There were 10 deaths in the IRFT arm and 5 in the CVP±R arm, but there was no significant difference in OS between the arms (HR=0.62; P=0.40). The 10-year OS rate was 86% in the IFRT arm and 95% in the CVP±R arm.
There was no significant between-arm difference in transformation to aggressive lymphoma (P=0.1). Transformation occurred in 10 patients in the IFRT arm and 4 in the CVP±R arm.
Safety
There were 148 patients from both arms who ultimately received IFRT, and 69 patients who received CVP±R.
Grade 2 toxicities occurring in more than 10% of IFRT recipients included upper gastrointestinal (n=27; 18%), skin (n=21; 14%), and mucous membrane (n=19; 12%) toxicity. One IFRT recipient had grade 3 mucositis, and 1 had grade 4 esophageal/pharyngeal mucosal toxicity.
Grade 3 toxicities occurring in at least 2 patients in the CVP±R arm included neutropenia (n=10; 14%), infection (n=8; 12%), diarrhea (n=3; 4%), elevated gamma-glutamyl transferase (n=3; 4%), fatigue (n=3; 4%), and febrile neutropenia (n=3; 4%).
Three patients (4%) in the CVP±R arm had acute grade 3 neuropathy related to vincristine. Ten patients (14%) had grade 4 neutropenia.
The most common late toxicities for the entire patient cohort were salivary gland (n=8; 5%) and skin (n=4; 3%) toxicities.
Grade 3 lung and menopausal toxicities occurred in 1 patient each. Two patients had late grade 3 vincristine neuropathy. One patient who had grade 3 neuropathy during chemotherapy progressed to grade 4.
A multidrug regimen can improve upon involved-field radiotherapy (IFRT) in patients with early stage follicular lymphoma (FL), according to research published in the Journal of Clinical Oncology.
FL patients who received IFRT plus cyclophosphamide, vincristine, and prednisolone (CVP)—with or without rituximab—had a significant improvement in progression-free survival (PFS) compared to patients who received standard treatment with IFRT alone.
However, there was no significant difference in overall survival (OS) between the treatment arms.
“This is the first successful randomized study ever to be conducted in early stage follicular lymphoma comparing standard therapy to standard therapy plus effective chemotherapy or immunochemotherapy,” said Michael MacManus, MBBCh, of Peter MacCallum Cancer Centre in Melbourne, Victoria, Australia.
“It shows that the initial treatment received by patients can significantly affect their long-term chance of staying free from disease. Moving forward, we are interested in determining whether there is a benefit in overall long-term survival for patients treated with the combination with further follow-up, and if there is any way to predict if a person will benefit from combined treatment based on analyses of blood or biopsy specimens.”
Dr MacManus and his colleagues studied 150 patients with stage I to II, low-grade FL who were enrolled in this trial between 2000 and 2012.
At randomization, the patients’ median age was 57, 52% were male, 75% had stage I disease, and 48% had PET staging.
Half of patients (n=75) were randomized to receive IFRT (30-36 Gy) alone, and half were randomized to IFRT (30-36 Gy) plus 6 cycles of CVP. From 2006 on, patients in the CVP arm received rituximab (R) as well (n=31).
Baseline characteristics were well-balanced between the treatment arms.
Efficacy
The median follow-up was 9.6 years (range, 3.1 to 15.8 years).
PFS was significantly better among patients randomized to receive CVP±R (hazard ratio [HR]=0.57; P=0.033). The estimated 10-year PFS rate was 41% in the IFRT arm and 59% in the CVP±R arm.
Patients randomized to receive CVP plus R (n=31) had significantly better PFS than patients randomized to receive IFRT alone (n=31) over the same time period (HR=0.26; P=0.045).
There were 10 deaths in the IRFT arm and 5 in the CVP±R arm, but there was no significant difference in OS between the arms (HR=0.62; P=0.40). The 10-year OS rate was 86% in the IFRT arm and 95% in the CVP±R arm.
There was no significant between-arm difference in transformation to aggressive lymphoma (P=0.1). Transformation occurred in 10 patients in the IFRT arm and 4 in the CVP±R arm.
Safety
There were 148 patients from both arms who ultimately received IFRT, and 69 patients who received CVP±R.
Grade 2 toxicities occurring in more than 10% of IFRT recipients included upper gastrointestinal (n=27; 18%), skin (n=21; 14%), and mucous membrane (n=19; 12%) toxicity. One IFRT recipient had grade 3 mucositis, and 1 had grade 4 esophageal/pharyngeal mucosal toxicity.
Grade 3 toxicities occurring in at least 2 patients in the CVP±R arm included neutropenia (n=10; 14%), infection (n=8; 12%), diarrhea (n=3; 4%), elevated gamma-glutamyl transferase (n=3; 4%), fatigue (n=3; 4%), and febrile neutropenia (n=3; 4%).
Three patients (4%) in the CVP±R arm had acute grade 3 neuropathy related to vincristine. Ten patients (14%) had grade 4 neutropenia.
The most common late toxicities for the entire patient cohort were salivary gland (n=8; 5%) and skin (n=4; 3%) toxicities.
Grade 3 lung and menopausal toxicities occurred in 1 patient each. Two patients had late grade 3 vincristine neuropathy. One patient who had grade 3 neuropathy during chemotherapy progressed to grade 4.
Adult CCSs report financial hardships
Health-related financial hardship is common among adult survivors of childhood cancer, according to a study published in the Journal of the National Cancer Institute.
Researchers analyzed more than 2800 long-term childhood cancer survivors (CCSs) and found that 65% had financial challenges related to their cancer diagnosis.
“These findings suggest primary care doctors and oncologists should routinely screen childhood cancer survivors for possible financial hardship,” said I-Chan Huang, PhD, of St. Jude Children’s Research Hospital in Memphis, Tennessee.
Specifically, Dr Huang recommends that healthcare providers routinely ask CCSs if they are unable to purchase medications, ever skip appointments for economic reasons, or worry about how to pay their medical bills.
For this study, Dr Huang and his colleagues analyzed data from 2811 CCSs. The subjects had a mean age of 31.8 (range, 18 to 65) and were a mean of 23.6 years from cancer diagnosis. Most (57.8%) had been diagnosed with hematologic malignancies, 32.0% with solid tumors, and 10.1% with central nervous system malignancies.
All subjects had been treated at St. Jude and enrolled in the St. Jude LIFE study. Participants return to St. Jude periodically for several days of clinical and functional assessments. Data for this study were collected during the CCSs’ first St. Jude LIFE evaluations.
Assessing hardship
The researchers measured 3 types of financial hardship—material, psychological, and coping/behavioral.
About 1 in 5 CCSs (22.4%) reported material financial hardship. In other words, their cancer had an impact on their financial situation.
More than half of CCSs (51.1%) reported psychological hardship—concern about their ability to pay for medical expenses.
And 33% of CCSs reported coping/behavioral hardship—an inability to see a doctor or go to the hospital due to finances.
Roughly 65% of CCSs reported at least 1 type of financial hardship.
All 3 types of hardship were significantly associated with somatization (all P<0.001), anxiety (all P<0.001), depression (all P<0.001), suicidal thoughts (all P<0.05), and difficulty in retirement planning (all P<0.001).
Furthermore, CCSs who reported financial hardship had significantly lower health-related quality of life (P<0.001 for all 3 domains), sensation abnormality (all P<0.001), pulmonary symptoms (all P<0.05), and cardiac symptoms (all P<0.05).
Predicting hardship
Intensive cancer treatment, chronic health conditions, second cancers, age at the time of study evaluation, education level, and annual household income were all significantly associated with a greater risk of financial hardship.
CCSs age 40 and older had an increased risk of psychological and coping/behavioral hardship (P<0.001 for both domains).
CCSs with an annual household income of less than $40,000 had an increased risk of material, psychological, and coping/behavioral hardship, compared to CCSs with an income of $80,000 or more (P<0.001 for all domains).
CCSs who did not obtain a high school diploma had an increased risk of material (P<0.001), psychological (P<0.01), and coping/behavioral hardship (P<0.001) compared to college graduates.
CCSs who received cancer treatments associated with a high-risk disease burden (vs low-risk) had an increased risk of material (P=0.01) and psychological (P=0.004) hardship.
Health conditions associated with material financial hardship included grade 2-4 myocardial infarction (P<0.001), peripheral neuropathy (P<0.001), subsequent neoplasm (P<0.001), seizure (P=0.007), reproductive disorders (P=0.01), stroke (P=0.02), amputation (P=0.02), upper gastrointestinal disease (P=0.04), and hearing loss (P=0.05).
Grade 2-4 myocardial infarction and reproductive disorders were significantly associated with psychological financial hardship (P=0.02 for both).
“Severe late effects that emerge early in life and disrupt education and training opportunities are a double hit for survivors,” Dr Huang said. “These health problems decrease the survivors’ earning mobility and financial security later in life. The phenomenon leaves them at risk for poor health and psychological outcomes compared to healthier survivors.”
Health-related financial hardship is common among adult survivors of childhood cancer, according to a study published in the Journal of the National Cancer Institute.
Researchers analyzed more than 2800 long-term childhood cancer survivors (CCSs) and found that 65% had financial challenges related to their cancer diagnosis.
“These findings suggest primary care doctors and oncologists should routinely screen childhood cancer survivors for possible financial hardship,” said I-Chan Huang, PhD, of St. Jude Children’s Research Hospital in Memphis, Tennessee.
Specifically, Dr Huang recommends that healthcare providers routinely ask CCSs if they are unable to purchase medications, ever skip appointments for economic reasons, or worry about how to pay their medical bills.
For this study, Dr Huang and his colleagues analyzed data from 2811 CCSs. The subjects had a mean age of 31.8 (range, 18 to 65) and were a mean of 23.6 years from cancer diagnosis. Most (57.8%) had been diagnosed with hematologic malignancies, 32.0% with solid tumors, and 10.1% with central nervous system malignancies.
All subjects had been treated at St. Jude and enrolled in the St. Jude LIFE study. Participants return to St. Jude periodically for several days of clinical and functional assessments. Data for this study were collected during the CCSs’ first St. Jude LIFE evaluations.
Assessing hardship
The researchers measured 3 types of financial hardship—material, psychological, and coping/behavioral.
About 1 in 5 CCSs (22.4%) reported material financial hardship. In other words, their cancer had an impact on their financial situation.
More than half of CCSs (51.1%) reported psychological hardship—concern about their ability to pay for medical expenses.
And 33% of CCSs reported coping/behavioral hardship—an inability to see a doctor or go to the hospital due to finances.
Roughly 65% of CCSs reported at least 1 type of financial hardship.
All 3 types of hardship were significantly associated with somatization (all P<0.001), anxiety (all P<0.001), depression (all P<0.001), suicidal thoughts (all P<0.05), and difficulty in retirement planning (all P<0.001).
Furthermore, CCSs who reported financial hardship had significantly lower health-related quality of life (P<0.001 for all 3 domains), sensation abnormality (all P<0.001), pulmonary symptoms (all P<0.05), and cardiac symptoms (all P<0.05).
Predicting hardship
Intensive cancer treatment, chronic health conditions, second cancers, age at the time of study evaluation, education level, and annual household income were all significantly associated with a greater risk of financial hardship.
CCSs age 40 and older had an increased risk of psychological and coping/behavioral hardship (P<0.001 for both domains).
CCSs with an annual household income of less than $40,000 had an increased risk of material, psychological, and coping/behavioral hardship, compared to CCSs with an income of $80,000 or more (P<0.001 for all domains).
CCSs who did not obtain a high school diploma had an increased risk of material (P<0.001), psychological (P<0.01), and coping/behavioral hardship (P<0.001) compared to college graduates.
CCSs who received cancer treatments associated with a high-risk disease burden (vs low-risk) had an increased risk of material (P=0.01) and psychological (P=0.004) hardship.
Health conditions associated with material financial hardship included grade 2-4 myocardial infarction (P<0.001), peripheral neuropathy (P<0.001), subsequent neoplasm (P<0.001), seizure (P=0.007), reproductive disorders (P=0.01), stroke (P=0.02), amputation (P=0.02), upper gastrointestinal disease (P=0.04), and hearing loss (P=0.05).
Grade 2-4 myocardial infarction and reproductive disorders were significantly associated with psychological financial hardship (P=0.02 for both).
“Severe late effects that emerge early in life and disrupt education and training opportunities are a double hit for survivors,” Dr Huang said. “These health problems decrease the survivors’ earning mobility and financial security later in life. The phenomenon leaves them at risk for poor health and psychological outcomes compared to healthier survivors.”
Health-related financial hardship is common among adult survivors of childhood cancer, according to a study published in the Journal of the National Cancer Institute.
Researchers analyzed more than 2800 long-term childhood cancer survivors (CCSs) and found that 65% had financial challenges related to their cancer diagnosis.
“These findings suggest primary care doctors and oncologists should routinely screen childhood cancer survivors for possible financial hardship,” said I-Chan Huang, PhD, of St. Jude Children’s Research Hospital in Memphis, Tennessee.
Specifically, Dr Huang recommends that healthcare providers routinely ask CCSs if they are unable to purchase medications, ever skip appointments for economic reasons, or worry about how to pay their medical bills.
For this study, Dr Huang and his colleagues analyzed data from 2811 CCSs. The subjects had a mean age of 31.8 (range, 18 to 65) and were a mean of 23.6 years from cancer diagnosis. Most (57.8%) had been diagnosed with hematologic malignancies, 32.0% with solid tumors, and 10.1% with central nervous system malignancies.
All subjects had been treated at St. Jude and enrolled in the St. Jude LIFE study. Participants return to St. Jude periodically for several days of clinical and functional assessments. Data for this study were collected during the CCSs’ first St. Jude LIFE evaluations.
Assessing hardship
The researchers measured 3 types of financial hardship—material, psychological, and coping/behavioral.
About 1 in 5 CCSs (22.4%) reported material financial hardship. In other words, their cancer had an impact on their financial situation.
More than half of CCSs (51.1%) reported psychological hardship—concern about their ability to pay for medical expenses.
And 33% of CCSs reported coping/behavioral hardship—an inability to see a doctor or go to the hospital due to finances.
Roughly 65% of CCSs reported at least 1 type of financial hardship.
All 3 types of hardship were significantly associated with somatization (all P<0.001), anxiety (all P<0.001), depression (all P<0.001), suicidal thoughts (all P<0.05), and difficulty in retirement planning (all P<0.001).
Furthermore, CCSs who reported financial hardship had significantly lower health-related quality of life (P<0.001 for all 3 domains), sensation abnormality (all P<0.001), pulmonary symptoms (all P<0.05), and cardiac symptoms (all P<0.05).
Predicting hardship
Intensive cancer treatment, chronic health conditions, second cancers, age at the time of study evaluation, education level, and annual household income were all significantly associated with a greater risk of financial hardship.
CCSs age 40 and older had an increased risk of psychological and coping/behavioral hardship (P<0.001 for both domains).
CCSs with an annual household income of less than $40,000 had an increased risk of material, psychological, and coping/behavioral hardship, compared to CCSs with an income of $80,000 or more (P<0.001 for all domains).
CCSs who did not obtain a high school diploma had an increased risk of material (P<0.001), psychological (P<0.01), and coping/behavioral hardship (P<0.001) compared to college graduates.
CCSs who received cancer treatments associated with a high-risk disease burden (vs low-risk) had an increased risk of material (P=0.01) and psychological (P=0.004) hardship.
Health conditions associated with material financial hardship included grade 2-4 myocardial infarction (P<0.001), peripheral neuropathy (P<0.001), subsequent neoplasm (P<0.001), seizure (P=0.007), reproductive disorders (P=0.01), stroke (P=0.02), amputation (P=0.02), upper gastrointestinal disease (P=0.04), and hearing loss (P=0.05).
Grade 2-4 myocardial infarction and reproductive disorders were significantly associated with psychological financial hardship (P=0.02 for both).
“Severe late effects that emerge early in life and disrupt education and training opportunities are a double hit for survivors,” Dr Huang said. “These health problems decrease the survivors’ earning mobility and financial security later in life. The phenomenon leaves them at risk for poor health and psychological outcomes compared to healthier survivors.”
Inhibitor receives breakthrough designation for AML
The US Food and Drug Administration (FDA) has granted breakthrough therapy designation to quizartinib, an investigational FLT3 inhibitor, for the treatment of adults with relapsed/refractory FLT3-ITD acute myeloid leukemia (AML).
The FDA granted quizartinib breakthrough designation based on results from the phase 3 QuANTUM-R study, which were presented at the 23rd Congress of the European Hematology Association in June.
QuANTUM-R enrolled adults with FLT3-ITD AML (at least 3% FLT3-ITD allelic ratio) who had refractory disease or had relapsed within 6 months of their first complete remission.
Patients were randomized to receive once-daily treatment with quizartinib (n=245) or a salvage chemotherapy regimen (n=122)—low-dose cytarabine (LoDAC, n=29); combination mitoxantrone, etoposide, and cytarabine (MEC, n=40); or combination fludarabine, cytarabine, and idarubicin (FLAG-IDA, n=53).
Responders could proceed to hematopoietic stem cell transplant (HSCT), and those in the quizartinib arm could resume quizartinib after HSCT. Thirty-two percent of quizartinib-treated patients and 12% of the chemotherapy group went on to HSCT.
The median follow-up was 23.5 months. The efficacy results include all randomized patients.
The overall response rate was 69% in the quizartinib arm and 30% in the chemotherapy arm. The complete response (CR) rate was 4% and 1%, respectively; the rate of CR with incomplete platelet recovery was 4% and 0%, respectively; and the rate of CR with incomplete hematologic recovery was 40% and 26%, respectively.
The median overall survival was 6.2 months in the quizartinib arm and 4.7 months in the chemotherapy arm (hazard ratio=0.76, P=0.0177). The 1-year overall survival rate was 27% and 20%, respectively.
The median event-free survival was 6.0 weeks in the quizartinib arm and 3.7 weeks in the chemotherapy arm (hazard ratio=0.90, P=0.1071).
The safety results include only patients who received their assigned treatment—241 patients who received quizartinib and 94 who received salvage chemotherapy (22 on LoDAC, 25 on MEC, and 47 on FLAG-IDA).
Grade 3 or higher hematologic treatment-emergent adverse events occurring in at least 5% of patients (in the quizartinib and chemotherapy groups, respectively) included thrombocytopenia (35% and 34%), anemia (30% and 29%), neutropenia (32% and 25%), febrile neutropenia (31% and 21%), and leukopenia (17% and 16%).
Grade 3 or higher nonhematologic treatment-emergent adverse events occurring in at least 5% of patients (in the quizartinib and chemotherapy groups, respectively) included fatigue (8% and 1%), hypokalemia (12% and 9%), sepsis/septic shock (16% and 18%), dyspnea (5% for both), hypophosphatemia (5% for both), and pneumonia (12% and 9%).
Three percent of patients in the quizartinib arm had grade 3 QTcF prolongation, and 2 patients discontinued quizartinib due to QTcF prolongation.
About breakthrough designation
Breakthrough designation is intended to expedite the development and review of new treatments for serious or life-threatening conditions.
The designation entitles the company developing a therapy to more intensive FDA guidance on an efficient and accelerated development program, as well as eligibility for other actions to expedite FDA review, such as rolling submission and priority review.
To earn breakthrough designation, a treatment must show encouraging early clinical results demonstrating substantial improvement over available therapies with regard to a clinically significant endpoint, or it must fulfill an unmet need.
Other designations for quizartinib
In addition to breakthrough therapy designation, quizartinib has fast track and orphan drug designations from the FDA.
The FDA’s fast track development program is designed to expedite clinical development and submission of applications for products with the potential to treat serious or life-threatening conditions and address unmet medical needs.
Fast track designation facilitates frequent interactions with the FDA review team, including meetings to discuss the product’s development plan and written communications about issues such as trial design and use of biomarkers.
Products that receive fast track designation may be eligible for accelerated approval and priority review if relevant criteria are met. Such products may also be eligible for rolling review, which allows a developer to submit individual sections of a product’s application for review as they are ready, rather than waiting until all sections are complete.
The FDA grants orphan designation to products intended to treat, diagnose, or prevent diseases/disorders that affect fewer than 200,000 people in the US.
Orphan designation provides incentives for sponsors to develop products for rare diseases. This may include tax credits toward the cost of clinical trials, prescription drug user fee waivers, and 7 years of market exclusivity if the product is approved.
The US Food and Drug Administration (FDA) has granted breakthrough therapy designation to quizartinib, an investigational FLT3 inhibitor, for the treatment of adults with relapsed/refractory FLT3-ITD acute myeloid leukemia (AML).
The FDA granted quizartinib breakthrough designation based on results from the phase 3 QuANTUM-R study, which were presented at the 23rd Congress of the European Hematology Association in June.
QuANTUM-R enrolled adults with FLT3-ITD AML (at least 3% FLT3-ITD allelic ratio) who had refractory disease or had relapsed within 6 months of their first complete remission.
Patients were randomized to receive once-daily treatment with quizartinib (n=245) or a salvage chemotherapy regimen (n=122)—low-dose cytarabine (LoDAC, n=29); combination mitoxantrone, etoposide, and cytarabine (MEC, n=40); or combination fludarabine, cytarabine, and idarubicin (FLAG-IDA, n=53).
Responders could proceed to hematopoietic stem cell transplant (HSCT), and those in the quizartinib arm could resume quizartinib after HSCT. Thirty-two percent of quizartinib-treated patients and 12% of the chemotherapy group went on to HSCT.
The median follow-up was 23.5 months. The efficacy results include all randomized patients.
The overall response rate was 69% in the quizartinib arm and 30% in the chemotherapy arm. The complete response (CR) rate was 4% and 1%, respectively; the rate of CR with incomplete platelet recovery was 4% and 0%, respectively; and the rate of CR with incomplete hematologic recovery was 40% and 26%, respectively.
The median overall survival was 6.2 months in the quizartinib arm and 4.7 months in the chemotherapy arm (hazard ratio=0.76, P=0.0177). The 1-year overall survival rate was 27% and 20%, respectively.
The median event-free survival was 6.0 weeks in the quizartinib arm and 3.7 weeks in the chemotherapy arm (hazard ratio=0.90, P=0.1071).
The safety results include only patients who received their assigned treatment—241 patients who received quizartinib and 94 who received salvage chemotherapy (22 on LoDAC, 25 on MEC, and 47 on FLAG-IDA).
Grade 3 or higher hematologic treatment-emergent adverse events occurring in at least 5% of patients (in the quizartinib and chemotherapy groups, respectively) included thrombocytopenia (35% and 34%), anemia (30% and 29%), neutropenia (32% and 25%), febrile neutropenia (31% and 21%), and leukopenia (17% and 16%).
Grade 3 or higher nonhematologic treatment-emergent adverse events occurring in at least 5% of patients (in the quizartinib and chemotherapy groups, respectively) included fatigue (8% and 1%), hypokalemia (12% and 9%), sepsis/septic shock (16% and 18%), dyspnea (5% for both), hypophosphatemia (5% for both), and pneumonia (12% and 9%).
Three percent of patients in the quizartinib arm had grade 3 QTcF prolongation, and 2 patients discontinued quizartinib due to QTcF prolongation.
About breakthrough designation
Breakthrough designation is intended to expedite the development and review of new treatments for serious or life-threatening conditions.
The designation entitles the company developing a therapy to more intensive FDA guidance on an efficient and accelerated development program, as well as eligibility for other actions to expedite FDA review, such as rolling submission and priority review.
To earn breakthrough designation, a treatment must show encouraging early clinical results demonstrating substantial improvement over available therapies with regard to a clinically significant endpoint, or it must fulfill an unmet need.
Other designations for quizartinib
In addition to breakthrough therapy designation, quizartinib has fast track and orphan drug designations from the FDA.
The FDA’s fast track development program is designed to expedite clinical development and submission of applications for products with the potential to treat serious or life-threatening conditions and address unmet medical needs.
Fast track designation facilitates frequent interactions with the FDA review team, including meetings to discuss the product’s development plan and written communications about issues such as trial design and use of biomarkers.
Products that receive fast track designation may be eligible for accelerated approval and priority review if relevant criteria are met. Such products may also be eligible for rolling review, which allows a developer to submit individual sections of a product’s application for review as they are ready, rather than waiting until all sections are complete.
The FDA grants orphan designation to products intended to treat, diagnose, or prevent diseases/disorders that affect fewer than 200,000 people in the US.
Orphan designation provides incentives for sponsors to develop products for rare diseases. This may include tax credits toward the cost of clinical trials, prescription drug user fee waivers, and 7 years of market exclusivity if the product is approved.
The US Food and Drug Administration (FDA) has granted breakthrough therapy designation to quizartinib, an investigational FLT3 inhibitor, for the treatment of adults with relapsed/refractory FLT3-ITD acute myeloid leukemia (AML).
The FDA granted quizartinib breakthrough designation based on results from the phase 3 QuANTUM-R study, which were presented at the 23rd Congress of the European Hematology Association in June.
QuANTUM-R enrolled adults with FLT3-ITD AML (at least 3% FLT3-ITD allelic ratio) who had refractory disease or had relapsed within 6 months of their first complete remission.
Patients were randomized to receive once-daily treatment with quizartinib (n=245) or a salvage chemotherapy regimen (n=122)—low-dose cytarabine (LoDAC, n=29); combination mitoxantrone, etoposide, and cytarabine (MEC, n=40); or combination fludarabine, cytarabine, and idarubicin (FLAG-IDA, n=53).
Responders could proceed to hematopoietic stem cell transplant (HSCT), and those in the quizartinib arm could resume quizartinib after HSCT. Thirty-two percent of quizartinib-treated patients and 12% of the chemotherapy group went on to HSCT.
The median follow-up was 23.5 months. The efficacy results include all randomized patients.
The overall response rate was 69% in the quizartinib arm and 30% in the chemotherapy arm. The complete response (CR) rate was 4% and 1%, respectively; the rate of CR with incomplete platelet recovery was 4% and 0%, respectively; and the rate of CR with incomplete hematologic recovery was 40% and 26%, respectively.
The median overall survival was 6.2 months in the quizartinib arm and 4.7 months in the chemotherapy arm (hazard ratio=0.76, P=0.0177). The 1-year overall survival rate was 27% and 20%, respectively.
The median event-free survival was 6.0 weeks in the quizartinib arm and 3.7 weeks in the chemotherapy arm (hazard ratio=0.90, P=0.1071).
The safety results include only patients who received their assigned treatment—241 patients who received quizartinib and 94 who received salvage chemotherapy (22 on LoDAC, 25 on MEC, and 47 on FLAG-IDA).
Grade 3 or higher hematologic treatment-emergent adverse events occurring in at least 5% of patients (in the quizartinib and chemotherapy groups, respectively) included thrombocytopenia (35% and 34%), anemia (30% and 29%), neutropenia (32% and 25%), febrile neutropenia (31% and 21%), and leukopenia (17% and 16%).
Grade 3 or higher nonhematologic treatment-emergent adverse events occurring in at least 5% of patients (in the quizartinib and chemotherapy groups, respectively) included fatigue (8% and 1%), hypokalemia (12% and 9%), sepsis/septic shock (16% and 18%), dyspnea (5% for both), hypophosphatemia (5% for both), and pneumonia (12% and 9%).
Three percent of patients in the quizartinib arm had grade 3 QTcF prolongation, and 2 patients discontinued quizartinib due to QTcF prolongation.
About breakthrough designation
Breakthrough designation is intended to expedite the development and review of new treatments for serious or life-threatening conditions.
The designation entitles the company developing a therapy to more intensive FDA guidance on an efficient and accelerated development program, as well as eligibility for other actions to expedite FDA review, such as rolling submission and priority review.
To earn breakthrough designation, a treatment must show encouraging early clinical results demonstrating substantial improvement over available therapies with regard to a clinically significant endpoint, or it must fulfill an unmet need.
Other designations for quizartinib
In addition to breakthrough therapy designation, quizartinib has fast track and orphan drug designations from the FDA.
The FDA’s fast track development program is designed to expedite clinical development and submission of applications for products with the potential to treat serious or life-threatening conditions and address unmet medical needs.
Fast track designation facilitates frequent interactions with the FDA review team, including meetings to discuss the product’s development plan and written communications about issues such as trial design and use of biomarkers.
Products that receive fast track designation may be eligible for accelerated approval and priority review if relevant criteria are met. Such products may also be eligible for rolling review, which allows a developer to submit individual sections of a product’s application for review as they are ready, rather than waiting until all sections are complete.
The FDA grants orphan designation to products intended to treat, diagnose, or prevent diseases/disorders that affect fewer than 200,000 people in the US.
Orphan designation provides incentives for sponsors to develop products for rare diseases. This may include tax credits toward the cost of clinical trials, prescription drug user fee waivers, and 7 years of market exclusivity if the product is approved.
FA pathway key to DNA repair after CRISPR cutting
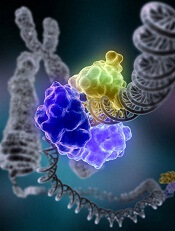
New research suggests the Fanconi anemia (FA) pathway plays a key role in repairing double-strand breaks (DSBs) created by CRISPR-Cas9 genome editing.
Researchers said they found that Cas9-induced single-strand template repair requires the FA pathway, and the protein FANCD2 localizes to Cas9-induced DSBs.
The team said this research provides insight into why CRISPR-Cas9 does not produce equal success in all cells.
Furthermore, the work might help researchers boost the efficiency with which cells insert new DNA into the genome and generally tweak CRISPR-Cas9 editing to get the desired outcome.
“If you want to treat sickle cell anemia, your chances of success are inextricably tied to the efficiency with which you can replace the mutated sickle cell gene with the correct one,” said study author Chris Richardson, PhD, formerly of the University of California, Berkeley, but now at Spotlight Therapeutics in Hayward, California.
“If you harvest a million cells from a patient and you have a 10% insertion rate, that is not as good as if you have 30% to 40%. Being able to manipulate those cells to increase the frequency of this process, called homology-directed repair, is exciting.”
Dr Richardson and his colleagues described this work in Nature Genetics.
CRISPR relies on DNA repair
The researchers noted that CRISPR-Cas9 creates targeted DSBs, and it’s up to the cell to repair the DNA.
This can happen in 2 ways. Enzymes can stitch the dangling ends back together, which often results in one or more bases being added or deleted, disrupting the function of the gene.
Alternatively, other enzymes can patch the break with a single strand of DNA that matches the DNA sequence upstream and downstream of the cut. A complementary DNA strand is created to complete the double-strand repair.
The former method, called non-homologous end-joining, appears to be the most common outcome after CRISPR cutting.
The latter method, homology-directed repair, happens more frequently in some cells than others and requires the presence of DNA that can be used to patch the break. Researchers often supply a single-stranded piece of DNA and hope the cell uses it to replace the faulty sequence with the new one.
Both processes are a bit mysterious, however, and no one knows why some cells readily patch in DNA while others do so infrequently.
“The enthusiasm for using CRISPR-Cas9 for medical or synthetic biology applications is great, but no one really knows what happens after you put it into cells,” Dr Richardson said. “It goes and creates these breaks, and you count on the cells to fix them, but people don’t really understand how that process works.”
To find out which DNA repair enzymes are critical to homology-directed repair after CRISPR cutting, Dr Richardson and his colleagues used a technique called CRISPR interference. They knocked out, one at a time, more than 2000 genes known or suspected to be involved in DNA repair.
The researchers were surprised to find that many of the genes that proved important—homology-directed repair dropped dramatically when they were silenced—were involved in the FA pathway.
FA pathway
The FA pathway was largely understood to repair DNA interstrand crosslinks, where a nucleotide on one strand of DNA bonds tightly with a nucleotide on the adjacent strand, interfering with DNA replication and often killing the cell.
“Based on our work, we believe that the Fanconi anemia pathway plays a major role in fixing other types of lesions as well, but is best understood as the pathway that repairs double-strand breaks,” Dr Richardson said. “After Cas9 editing, the Fanconi anemia pathway is required if you want to insert new DNA.”
The importance of the FA pathway in repairing DSBs casts doubt on some planned CRISPR treatments for Fanconi anemia itself.
Without an active FA pathway, cells may not be able to replace their mutated genes with normal genes after Cas9 makes a cut. In fact, the activity level of the FA pathway may affect how efficiently CRISPR can insert DNA in a specific cell.
The researchers concluded that, while end-joining is the default repair mechanism after a DSB, the FA pathway competes with it, and that higher activity results in more homology-directed repair and less end-joining.
Dr Richardson and his colleagues also found that 1 of the 21 proteins in the FA pathway, FANCD2, always homes in on the site of the DSB created by CRISPR-Cas9. This suggests FANCD2 plays an important role in regulating the insertion of new DNA at the cut site.
The researchers therefore believe FANCD2 could be tweaked to boost the frequency with which a cell inserts DNA via homology-directed repair.
“Also, since FANCD2 localizes to the site of Cas9 breaks, you can use FANCD2 to map where Cas9 is cutting in any cell type,” Dr Richardson said. “If you edit a population of cells and you want to know where the on- and off-target cuts are, you can just map where FANCD2 was found in the genome and you can find the cuts.”
New research suggests the Fanconi anemia (FA) pathway plays a key role in repairing double-strand breaks (DSBs) created by CRISPR-Cas9 genome editing.
Researchers said they found that Cas9-induced single-strand template repair requires the FA pathway, and the protein FANCD2 localizes to Cas9-induced DSBs.
The team said this research provides insight into why CRISPR-Cas9 does not produce equal success in all cells.
Furthermore, the work might help researchers boost the efficiency with which cells insert new DNA into the genome and generally tweak CRISPR-Cas9 editing to get the desired outcome.
“If you want to treat sickle cell anemia, your chances of success are inextricably tied to the efficiency with which you can replace the mutated sickle cell gene with the correct one,” said study author Chris Richardson, PhD, formerly of the University of California, Berkeley, but now at Spotlight Therapeutics in Hayward, California.
“If you harvest a million cells from a patient and you have a 10% insertion rate, that is not as good as if you have 30% to 40%. Being able to manipulate those cells to increase the frequency of this process, called homology-directed repair, is exciting.”
Dr Richardson and his colleagues described this work in Nature Genetics.
CRISPR relies on DNA repair
The researchers noted that CRISPR-Cas9 creates targeted DSBs, and it’s up to the cell to repair the DNA.
This can happen in 2 ways. Enzymes can stitch the dangling ends back together, which often results in one or more bases being added or deleted, disrupting the function of the gene.
Alternatively, other enzymes can patch the break with a single strand of DNA that matches the DNA sequence upstream and downstream of the cut. A complementary DNA strand is created to complete the double-strand repair.
The former method, called non-homologous end-joining, appears to be the most common outcome after CRISPR cutting.
The latter method, homology-directed repair, happens more frequently in some cells than others and requires the presence of DNA that can be used to patch the break. Researchers often supply a single-stranded piece of DNA and hope the cell uses it to replace the faulty sequence with the new one.
Both processes are a bit mysterious, however, and no one knows why some cells readily patch in DNA while others do so infrequently.
“The enthusiasm for using CRISPR-Cas9 for medical or synthetic biology applications is great, but no one really knows what happens after you put it into cells,” Dr Richardson said. “It goes and creates these breaks, and you count on the cells to fix them, but people don’t really understand how that process works.”
To find out which DNA repair enzymes are critical to homology-directed repair after CRISPR cutting, Dr Richardson and his colleagues used a technique called CRISPR interference. They knocked out, one at a time, more than 2000 genes known or suspected to be involved in DNA repair.
The researchers were surprised to find that many of the genes that proved important—homology-directed repair dropped dramatically when they were silenced—were involved in the FA pathway.
FA pathway
The FA pathway was largely understood to repair DNA interstrand crosslinks, where a nucleotide on one strand of DNA bonds tightly with a nucleotide on the adjacent strand, interfering with DNA replication and often killing the cell.
“Based on our work, we believe that the Fanconi anemia pathway plays a major role in fixing other types of lesions as well, but is best understood as the pathway that repairs double-strand breaks,” Dr Richardson said. “After Cas9 editing, the Fanconi anemia pathway is required if you want to insert new DNA.”
The importance of the FA pathway in repairing DSBs casts doubt on some planned CRISPR treatments for Fanconi anemia itself.
Without an active FA pathway, cells may not be able to replace their mutated genes with normal genes after Cas9 makes a cut. In fact, the activity level of the FA pathway may affect how efficiently CRISPR can insert DNA in a specific cell.
The researchers concluded that, while end-joining is the default repair mechanism after a DSB, the FA pathway competes with it, and that higher activity results in more homology-directed repair and less end-joining.
Dr Richardson and his colleagues also found that 1 of the 21 proteins in the FA pathway, FANCD2, always homes in on the site of the DSB created by CRISPR-Cas9. This suggests FANCD2 plays an important role in regulating the insertion of new DNA at the cut site.
The researchers therefore believe FANCD2 could be tweaked to boost the frequency with which a cell inserts DNA via homology-directed repair.
“Also, since FANCD2 localizes to the site of Cas9 breaks, you can use FANCD2 to map where Cas9 is cutting in any cell type,” Dr Richardson said. “If you edit a population of cells and you want to know where the on- and off-target cuts are, you can just map where FANCD2 was found in the genome and you can find the cuts.”
New research suggests the Fanconi anemia (FA) pathway plays a key role in repairing double-strand breaks (DSBs) created by CRISPR-Cas9 genome editing.
Researchers said they found that Cas9-induced single-strand template repair requires the FA pathway, and the protein FANCD2 localizes to Cas9-induced DSBs.
The team said this research provides insight into why CRISPR-Cas9 does not produce equal success in all cells.
Furthermore, the work might help researchers boost the efficiency with which cells insert new DNA into the genome and generally tweak CRISPR-Cas9 editing to get the desired outcome.
“If you want to treat sickle cell anemia, your chances of success are inextricably tied to the efficiency with which you can replace the mutated sickle cell gene with the correct one,” said study author Chris Richardson, PhD, formerly of the University of California, Berkeley, but now at Spotlight Therapeutics in Hayward, California.
“If you harvest a million cells from a patient and you have a 10% insertion rate, that is not as good as if you have 30% to 40%. Being able to manipulate those cells to increase the frequency of this process, called homology-directed repair, is exciting.”
Dr Richardson and his colleagues described this work in Nature Genetics.
CRISPR relies on DNA repair
The researchers noted that CRISPR-Cas9 creates targeted DSBs, and it’s up to the cell to repair the DNA.
This can happen in 2 ways. Enzymes can stitch the dangling ends back together, which often results in one or more bases being added or deleted, disrupting the function of the gene.
Alternatively, other enzymes can patch the break with a single strand of DNA that matches the DNA sequence upstream and downstream of the cut. A complementary DNA strand is created to complete the double-strand repair.
The former method, called non-homologous end-joining, appears to be the most common outcome after CRISPR cutting.
The latter method, homology-directed repair, happens more frequently in some cells than others and requires the presence of DNA that can be used to patch the break. Researchers often supply a single-stranded piece of DNA and hope the cell uses it to replace the faulty sequence with the new one.
Both processes are a bit mysterious, however, and no one knows why some cells readily patch in DNA while others do so infrequently.
“The enthusiasm for using CRISPR-Cas9 for medical or synthetic biology applications is great, but no one really knows what happens after you put it into cells,” Dr Richardson said. “It goes and creates these breaks, and you count on the cells to fix them, but people don’t really understand how that process works.”
To find out which DNA repair enzymes are critical to homology-directed repair after CRISPR cutting, Dr Richardson and his colleagues used a technique called CRISPR interference. They knocked out, one at a time, more than 2000 genes known or suspected to be involved in DNA repair.
The researchers were surprised to find that many of the genes that proved important—homology-directed repair dropped dramatically when they were silenced—were involved in the FA pathway.
FA pathway
The FA pathway was largely understood to repair DNA interstrand crosslinks, where a nucleotide on one strand of DNA bonds tightly with a nucleotide on the adjacent strand, interfering with DNA replication and often killing the cell.
“Based on our work, we believe that the Fanconi anemia pathway plays a major role in fixing other types of lesions as well, but is best understood as the pathway that repairs double-strand breaks,” Dr Richardson said. “After Cas9 editing, the Fanconi anemia pathway is required if you want to insert new DNA.”
The importance of the FA pathway in repairing DSBs casts doubt on some planned CRISPR treatments for Fanconi anemia itself.
Without an active FA pathway, cells may not be able to replace their mutated genes with normal genes after Cas9 makes a cut. In fact, the activity level of the FA pathway may affect how efficiently CRISPR can insert DNA in a specific cell.
The researchers concluded that, while end-joining is the default repair mechanism after a DSB, the FA pathway competes with it, and that higher activity results in more homology-directed repair and less end-joining.
Dr Richardson and his colleagues also found that 1 of the 21 proteins in the FA pathway, FANCD2, always homes in on the site of the DSB created by CRISPR-Cas9. This suggests FANCD2 plays an important role in regulating the insertion of new DNA at the cut site.
The researchers therefore believe FANCD2 could be tweaked to boost the frequency with which a cell inserts DNA via homology-directed repair.
“Also, since FANCD2 localizes to the site of Cas9 breaks, you can use FANCD2 to map where Cas9 is cutting in any cell type,” Dr Richardson said. “If you edit a population of cells and you want to know where the on- and off-target cuts are, you can just map where FANCD2 was found in the genome and you can find the cuts.”
Drug receives orphan designation for MM
The US Food and Drug Administration (FDA) has granted orphan drug designation to SRF231 for the treatment of multiple myeloma (MM).
SRF231 is a fully human antibody that inhibits the activity of CD47, a protein that is overexpressed on many cancer cells and prevents them from being engulfed and eliminated by macrophages.
Surface Oncology, the company developing SRF231, is currently conducting a phase 1 trial (NCT03512340) of SRF231 in patients with solid tumors and hematologic malignancies.
Preclinical research on SRF231 was presented at the 2016 ASH Annual Meeting.
SRF231 demonstrated “potent” activity against hematologic malignancies, according to researchers.
The team said SRF231 promoted macrophage-mediated phagocytic clearance of several hematologic primary tumor samples and cell lines in vitro.
SRF231 also demonstrated activity in murine xenograft models of hematologic malignancies. Specifically, the researchers observed “profound tumor growth inhibition” in models of MM, diffuse large B-cell lymphoma, and Burkitt lymphoma.
The team said SRF231 demonstrated activity when given alone or in combination with opsonizing antibodies.
Results also showed that SRF231 did not induce hemagglutination or phagocytosis of red blood cells in vitro.
About orphan designation
The FDA grants orphan designation to products intended to treat, diagnose, or prevent diseases/disorders that affect fewer than 200,000 people in the US.
Orphan designation provides incentives for sponsors to develop products for rare diseases. This may include tax credits toward the cost of clinical trials, prescription drug user fee waivers, and 7 years of market exclusivity if the product is approved.
The US Food and Drug Administration (FDA) has granted orphan drug designation to SRF231 for the treatment of multiple myeloma (MM).
SRF231 is a fully human antibody that inhibits the activity of CD47, a protein that is overexpressed on many cancer cells and prevents them from being engulfed and eliminated by macrophages.
Surface Oncology, the company developing SRF231, is currently conducting a phase 1 trial (NCT03512340) of SRF231 in patients with solid tumors and hematologic malignancies.
Preclinical research on SRF231 was presented at the 2016 ASH Annual Meeting.
SRF231 demonstrated “potent” activity against hematologic malignancies, according to researchers.
The team said SRF231 promoted macrophage-mediated phagocytic clearance of several hematologic primary tumor samples and cell lines in vitro.
SRF231 also demonstrated activity in murine xenograft models of hematologic malignancies. Specifically, the researchers observed “profound tumor growth inhibition” in models of MM, diffuse large B-cell lymphoma, and Burkitt lymphoma.
The team said SRF231 demonstrated activity when given alone or in combination with opsonizing antibodies.
Results also showed that SRF231 did not induce hemagglutination or phagocytosis of red blood cells in vitro.
About orphan designation
The FDA grants orphan designation to products intended to treat, diagnose, or prevent diseases/disorders that affect fewer than 200,000 people in the US.
Orphan designation provides incentives for sponsors to develop products for rare diseases. This may include tax credits toward the cost of clinical trials, prescription drug user fee waivers, and 7 years of market exclusivity if the product is approved.
The US Food and Drug Administration (FDA) has granted orphan drug designation to SRF231 for the treatment of multiple myeloma (MM).
SRF231 is a fully human antibody that inhibits the activity of CD47, a protein that is overexpressed on many cancer cells and prevents them from being engulfed and eliminated by macrophages.
Surface Oncology, the company developing SRF231, is currently conducting a phase 1 trial (NCT03512340) of SRF231 in patients with solid tumors and hematologic malignancies.
Preclinical research on SRF231 was presented at the 2016 ASH Annual Meeting.
SRF231 demonstrated “potent” activity against hematologic malignancies, according to researchers.
The team said SRF231 promoted macrophage-mediated phagocytic clearance of several hematologic primary tumor samples and cell lines in vitro.
SRF231 also demonstrated activity in murine xenograft models of hematologic malignancies. Specifically, the researchers observed “profound tumor growth inhibition” in models of MM, diffuse large B-cell lymphoma, and Burkitt lymphoma.
The team said SRF231 demonstrated activity when given alone or in combination with opsonizing antibodies.
Results also showed that SRF231 did not induce hemagglutination or phagocytosis of red blood cells in vitro.
About orphan designation
The FDA grants orphan designation to products intended to treat, diagnose, or prevent diseases/disorders that affect fewer than 200,000 people in the US.
Orphan designation provides incentives for sponsors to develop products for rare diseases. This may include tax credits toward the cost of clinical trials, prescription drug user fee waivers, and 7 years of market exclusivity if the product is approved.
CHMP recommends generic deferiprone
The European Medicines Agency’s Committee for Medicinal Products for Human Use (CHMP) has recommended approval for Deferiprone Lipomed to treat iron overload in patients with thalassemia major.
Deferiprone Lipomed is a generic version of the iron chelating agent Ferriprox, which has been authorized in the European Union since August 1999.
According to the CHMP, studies have shown that Deferiprone Lipomed is of satisfactory quality and bioequivalent to Ferriprox.
The CHMP’s recommendation for Deferiprone Lipomed will be reviewed by the European Commission, which has the authority to approve medicines for use in the European Union, Norway, Iceland, and Liechtenstein.
The European Commission usually makes a decision within 67 days of the CHMP’s recommendation.
If approved, Deferiprone Lipomed will be available as 500-mg film-coated tablets.
The drug will be authorized for the following uses:
- As monotherapy to treat iron overload in patients with thalassemia major when current chelation therapy is contraindicated or inadequate
- In combination with another chelator in patients with thalassemia major when monotherapy with any iron chelator is ineffective or when prevention or treatment of life-threatening consequences of iron overload justifies rapid or intensive correction.
According to the prescribing information for Ferriprox, the combination of iron chelators should be considered on a case-by-case basis, and patients should be monitored for response and adverse events.
Fatalities and life-threatening situations (caused by agranulocytosis) have been reported with the combination of deferiprone and deferoxamine.
Combination therapy is not recommended when monotherapy with either chelator is adequate or when serum ferritin falls below 500 μg/l. Additionally, there are limited data on the combined use of Ferriprox and deferasirox.
The applicant for Deferiprone Lipomed is Lipomed GmbH.
The European Medicines Agency’s Committee for Medicinal Products for Human Use (CHMP) has recommended approval for Deferiprone Lipomed to treat iron overload in patients with thalassemia major.
Deferiprone Lipomed is a generic version of the iron chelating agent Ferriprox, which has been authorized in the European Union since August 1999.
According to the CHMP, studies have shown that Deferiprone Lipomed is of satisfactory quality and bioequivalent to Ferriprox.
The CHMP’s recommendation for Deferiprone Lipomed will be reviewed by the European Commission, which has the authority to approve medicines for use in the European Union, Norway, Iceland, and Liechtenstein.
The European Commission usually makes a decision within 67 days of the CHMP’s recommendation.
If approved, Deferiprone Lipomed will be available as 500-mg film-coated tablets.
The drug will be authorized for the following uses:
- As monotherapy to treat iron overload in patients with thalassemia major when current chelation therapy is contraindicated or inadequate
- In combination with another chelator in patients with thalassemia major when monotherapy with any iron chelator is ineffective or when prevention or treatment of life-threatening consequences of iron overload justifies rapid or intensive correction.
According to the prescribing information for Ferriprox, the combination of iron chelators should be considered on a case-by-case basis, and patients should be monitored for response and adverse events.
Fatalities and life-threatening situations (caused by agranulocytosis) have been reported with the combination of deferiprone and deferoxamine.
Combination therapy is not recommended when monotherapy with either chelator is adequate or when serum ferritin falls below 500 μg/l. Additionally, there are limited data on the combined use of Ferriprox and deferasirox.
The applicant for Deferiprone Lipomed is Lipomed GmbH.
The European Medicines Agency’s Committee for Medicinal Products for Human Use (CHMP) has recommended approval for Deferiprone Lipomed to treat iron overload in patients with thalassemia major.
Deferiprone Lipomed is a generic version of the iron chelating agent Ferriprox, which has been authorized in the European Union since August 1999.
According to the CHMP, studies have shown that Deferiprone Lipomed is of satisfactory quality and bioequivalent to Ferriprox.
The CHMP’s recommendation for Deferiprone Lipomed will be reviewed by the European Commission, which has the authority to approve medicines for use in the European Union, Norway, Iceland, and Liechtenstein.
The European Commission usually makes a decision within 67 days of the CHMP’s recommendation.
If approved, Deferiprone Lipomed will be available as 500-mg film-coated tablets.
The drug will be authorized for the following uses:
- As monotherapy to treat iron overload in patients with thalassemia major when current chelation therapy is contraindicated or inadequate
- In combination with another chelator in patients with thalassemia major when monotherapy with any iron chelator is ineffective or when prevention or treatment of life-threatening consequences of iron overload justifies rapid or intensive correction.
According to the prescribing information for Ferriprox, the combination of iron chelators should be considered on a case-by-case basis, and patients should be monitored for response and adverse events.
Fatalities and life-threatening situations (caused by agranulocytosis) have been reported with the combination of deferiprone and deferoxamine.
Combination therapy is not recommended when monotherapy with either chelator is adequate or when serum ferritin falls below 500 μg/l. Additionally, there are limited data on the combined use of Ferriprox and deferasirox.
The applicant for Deferiprone Lipomed is Lipomed GmbH.
CHMP backs generic lenalidomide
The European Medicines Agency’s Committee for Medicinal Products for Human Use (CHMP) has recommended approval for Lenalidomide Accord as a treatment for multiple myeloma (MM).
Lenalidomide Accord is a generic version of the immunomodulatory agent Revlimid, which has been authorized in the European Union since June 2007.
The CHMP said studies have demonstrated the satisfactory quality of Lenalidomide Accord and its bioequivalence to Revlimid.
The CHMP’s recommendation for Lenalidomide Accord will be reviewed by the European Commission, which has the authority to approve medicines for use in the European Union, Norway, Iceland, and Liechtenstein.
The European Commission usually makes a decision within 67 days of the CHMP’s recommendation.
If approved, Lenalidomide Accord will be available as capsules (2.5 mg, 5 mg, 7.5 mg, 10 mg, 15 mg, 20 mg, and 25 mg) and authorized for the following uses:
- As monotherapy for the maintenance treatment of adults with newly diagnosed MM who have undergone autologous stem cell transplant
- In combination with melphalan and prednisone followed by lenalidomide maintenance in adults with previously untreated MM who are not eligible for transplant
- In combination with dexamethasone to treat MM in adults who have received at least 1 prior therapy.
The applicant for Lenalidomide Accord is Accord Healthcare Limited.
The European Medicines Agency’s Committee for Medicinal Products for Human Use (CHMP) has recommended approval for Lenalidomide Accord as a treatment for multiple myeloma (MM).
Lenalidomide Accord is a generic version of the immunomodulatory agent Revlimid, which has been authorized in the European Union since June 2007.
The CHMP said studies have demonstrated the satisfactory quality of Lenalidomide Accord and its bioequivalence to Revlimid.
The CHMP’s recommendation for Lenalidomide Accord will be reviewed by the European Commission, which has the authority to approve medicines for use in the European Union, Norway, Iceland, and Liechtenstein.
The European Commission usually makes a decision within 67 days of the CHMP’s recommendation.
If approved, Lenalidomide Accord will be available as capsules (2.5 mg, 5 mg, 7.5 mg, 10 mg, 15 mg, 20 mg, and 25 mg) and authorized for the following uses:
- As monotherapy for the maintenance treatment of adults with newly diagnosed MM who have undergone autologous stem cell transplant
- In combination with melphalan and prednisone followed by lenalidomide maintenance in adults with previously untreated MM who are not eligible for transplant
- In combination with dexamethasone to treat MM in adults who have received at least 1 prior therapy.
The applicant for Lenalidomide Accord is Accord Healthcare Limited.
The European Medicines Agency’s Committee for Medicinal Products for Human Use (CHMP) has recommended approval for Lenalidomide Accord as a treatment for multiple myeloma (MM).
Lenalidomide Accord is a generic version of the immunomodulatory agent Revlimid, which has been authorized in the European Union since June 2007.
The CHMP said studies have demonstrated the satisfactory quality of Lenalidomide Accord and its bioequivalence to Revlimid.
The CHMP’s recommendation for Lenalidomide Accord will be reviewed by the European Commission, which has the authority to approve medicines for use in the European Union, Norway, Iceland, and Liechtenstein.
The European Commission usually makes a decision within 67 days of the CHMP’s recommendation.
If approved, Lenalidomide Accord will be available as capsules (2.5 mg, 5 mg, 7.5 mg, 10 mg, 15 mg, 20 mg, and 25 mg) and authorized for the following uses:
- As monotherapy for the maintenance treatment of adults with newly diagnosed MM who have undergone autologous stem cell transplant
- In combination with melphalan and prednisone followed by lenalidomide maintenance in adults with previously untreated MM who are not eligible for transplant
- In combination with dexamethasone to treat MM in adults who have received at least 1 prior therapy.
The applicant for Lenalidomide Accord is Accord Healthcare Limited.
CHMP recommends expanded approval for daratumumab
The European Medicines Agency’s Committee for Medicinal Products for Human Use (CHMP) has recommended broadening the existing marketing authorization for daratumumab (Darzalex).
The CHMP is recommending approval for daratumumab in combination with bortezomib, melphalan, and prednisone (VMP) for the treatment of adults with newly diagnosed multiple myeloma (MM) who are ineligible for autologous stem cell transplant.
The CHMP’s recommendation will be reviewed by the European Commission (EC), which has the authority to approve medicines for use in the European Union, Norway, Iceland, and Liechtenstein.
The EC usually makes a decision within 67 days of the CHMP’s recommendation.
Daratumumab already has EC approval for the following indications:
- For use in combination with lenalidomide and dexamethasone, or bortezomib and dexamethasone, to treat adults with MM who have received at least 1 prior therapy
- As monotherapy for adults with relapsed and refractory MM whose prior therapy included a proteasome inhibitor and an immunomodulatory agent and who have demonstrated disease progression on their last therapy.
The CHMP’s recommendation to expand the existing marketing authorization for daratumumab is based on results from the phase 3 ALCYONE (MMY3007) study.
Results from this study were presented at the 2017 ASH Annual Meeting and simultaneously published in NEJM.
ALCYONE enrolled 706 patients with newly diagnosed MM who were not eligible for high-dose chemotherapy with autologous stem cell transplant. Patients were randomized to receive VMP or daratumumab plus VMP (D-VMP).
The overall response rates were 91% in the D-VMP arm and 74% in the VMP arm (P<0.0001). Rates of complete response were 43% and 24%, respectively. Rates of minimal residual disease negativity were 22% and 6%, respectively.
The median progression-free survival (PFS) was not reached in the D-VMP arm and was 18.1 months in the VMP arm. The 12-month PFS was 87% and 76%, respectively. The 18-month PFS was 72% and 50%, respectively.
The most common treatment-emergent adverse events (in the D-VMP and VMP arms, respectively) were neutropenia (50% and 53%), thrombocytopenia (49% and 54%), anemia (28% and 38%), peripheral sensory neuropathy (28% and 34%), upper respiratory tract infection (26% and 14%), diarrhea (24% and 25%), pyrexia (23% and 21%), and nausea (21% and 22%).
Infusion-related reactions occurred in 28% of patients in the D-VMP arm and 0% of those in the VMP arm.
The rate of grade 3/4 infections was higher in the D-VMP arm than the VMP arm—23% and 15%, respectively. In both arms, most infections resolved.
The most common grade 3/4 treatment-emergent adverse events (in the D-VMP and VMP arms, respectively) were neutropenia (40% and 39%), thrombocytopenia (34% and 38%), and anemia (16% and 20%).
The rate of discontinuation due to adverse events was 5% in the D-VMP arm and 9% in the VMP arm.
The European Medicines Agency’s Committee for Medicinal Products for Human Use (CHMP) has recommended broadening the existing marketing authorization for daratumumab (Darzalex).
The CHMP is recommending approval for daratumumab in combination with bortezomib, melphalan, and prednisone (VMP) for the treatment of adults with newly diagnosed multiple myeloma (MM) who are ineligible for autologous stem cell transplant.
The CHMP’s recommendation will be reviewed by the European Commission (EC), which has the authority to approve medicines for use in the European Union, Norway, Iceland, and Liechtenstein.
The EC usually makes a decision within 67 days of the CHMP’s recommendation.
Daratumumab already has EC approval for the following indications:
- For use in combination with lenalidomide and dexamethasone, or bortezomib and dexamethasone, to treat adults with MM who have received at least 1 prior therapy
- As monotherapy for adults with relapsed and refractory MM whose prior therapy included a proteasome inhibitor and an immunomodulatory agent and who have demonstrated disease progression on their last therapy.
The CHMP’s recommendation to expand the existing marketing authorization for daratumumab is based on results from the phase 3 ALCYONE (MMY3007) study.
Results from this study were presented at the 2017 ASH Annual Meeting and simultaneously published in NEJM.
ALCYONE enrolled 706 patients with newly diagnosed MM who were not eligible for high-dose chemotherapy with autologous stem cell transplant. Patients were randomized to receive VMP or daratumumab plus VMP (D-VMP).
The overall response rates were 91% in the D-VMP arm and 74% in the VMP arm (P<0.0001). Rates of complete response were 43% and 24%, respectively. Rates of minimal residual disease negativity were 22% and 6%, respectively.
The median progression-free survival (PFS) was not reached in the D-VMP arm and was 18.1 months in the VMP arm. The 12-month PFS was 87% and 76%, respectively. The 18-month PFS was 72% and 50%, respectively.
The most common treatment-emergent adverse events (in the D-VMP and VMP arms, respectively) were neutropenia (50% and 53%), thrombocytopenia (49% and 54%), anemia (28% and 38%), peripheral sensory neuropathy (28% and 34%), upper respiratory tract infection (26% and 14%), diarrhea (24% and 25%), pyrexia (23% and 21%), and nausea (21% and 22%).
Infusion-related reactions occurred in 28% of patients in the D-VMP arm and 0% of those in the VMP arm.
The rate of grade 3/4 infections was higher in the D-VMP arm than the VMP arm—23% and 15%, respectively. In both arms, most infections resolved.
The most common grade 3/4 treatment-emergent adverse events (in the D-VMP and VMP arms, respectively) were neutropenia (40% and 39%), thrombocytopenia (34% and 38%), and anemia (16% and 20%).
The rate of discontinuation due to adverse events was 5% in the D-VMP arm and 9% in the VMP arm.
The European Medicines Agency’s Committee for Medicinal Products for Human Use (CHMP) has recommended broadening the existing marketing authorization for daratumumab (Darzalex).
The CHMP is recommending approval for daratumumab in combination with bortezomib, melphalan, and prednisone (VMP) for the treatment of adults with newly diagnosed multiple myeloma (MM) who are ineligible for autologous stem cell transplant.
The CHMP’s recommendation will be reviewed by the European Commission (EC), which has the authority to approve medicines for use in the European Union, Norway, Iceland, and Liechtenstein.
The EC usually makes a decision within 67 days of the CHMP’s recommendation.
Daratumumab already has EC approval for the following indications:
- For use in combination with lenalidomide and dexamethasone, or bortezomib and dexamethasone, to treat adults with MM who have received at least 1 prior therapy
- As monotherapy for adults with relapsed and refractory MM whose prior therapy included a proteasome inhibitor and an immunomodulatory agent and who have demonstrated disease progression on their last therapy.
The CHMP’s recommendation to expand the existing marketing authorization for daratumumab is based on results from the phase 3 ALCYONE (MMY3007) study.
Results from this study were presented at the 2017 ASH Annual Meeting and simultaneously published in NEJM.
ALCYONE enrolled 706 patients with newly diagnosed MM who were not eligible for high-dose chemotherapy with autologous stem cell transplant. Patients were randomized to receive VMP or daratumumab plus VMP (D-VMP).
The overall response rates were 91% in the D-VMP arm and 74% in the VMP arm (P<0.0001). Rates of complete response were 43% and 24%, respectively. Rates of minimal residual disease negativity were 22% and 6%, respectively.
The median progression-free survival (PFS) was not reached in the D-VMP arm and was 18.1 months in the VMP arm. The 12-month PFS was 87% and 76%, respectively. The 18-month PFS was 72% and 50%, respectively.
The most common treatment-emergent adverse events (in the D-VMP and VMP arms, respectively) were neutropenia (50% and 53%), thrombocytopenia (49% and 54%), anemia (28% and 38%), peripheral sensory neuropathy (28% and 34%), upper respiratory tract infection (26% and 14%), diarrhea (24% and 25%), pyrexia (23% and 21%), and nausea (21% and 22%).
Infusion-related reactions occurred in 28% of patients in the D-VMP arm and 0% of those in the VMP arm.
The rate of grade 3/4 infections was higher in the D-VMP arm than the VMP arm—23% and 15%, respectively. In both arms, most infections resolved.
The most common grade 3/4 treatment-emergent adverse events (in the D-VMP and VMP arms, respectively) were neutropenia (40% and 39%), thrombocytopenia (34% and 38%), and anemia (16% and 20%).
The rate of discontinuation due to adverse events was 5% in the D-VMP arm and 9% in the VMP arm.