User login
Selinexor receives priority review for penta-refractory MM
The U.S. Food and Drug Administration (FDA) has accepted for priority review the new drug application (NDA) for selinexor.
With this NDA, Karyopharm Therapeutics Inc., is seeking accelerated approval for selinexor, an oral selective inhibitor of nuclear export compound, as a treatment for penta-refractory multiple myeloma (MM).
The FDA grants priority review to applications for products that may provide significant improvements in the treatment, diagnosis, or prevention of serious conditions.
The agency intends to take action on a priority review application within 6 months of receiving it rather than the standard 10 months.
The FDA plans to make a decision on the NDA for selinexor by April 6, 2019.
Selinexor also has orphan drug and fast track designations from the FDA for the treatment of penta-refractory MM.
Selinexor has demonstrated a clinical benefit in penta-refractory MM patients in the phase 2 STORM trial, according to researchers.
Results from this trial were recently presented at the Society of Hematologic Oncology (SOHO) 2018 Annual Meeting.
STORM included 122 patients with penta-refractory MM. They received selinexor at 80 mg twice weekly plus dexamethasone at 20 mg twice weekly until disease progression.
Two patients (1.6%) achieved stringent complete responses (with minimal residual disease negativity), six patients (4.9%) had very good partial responses, 24 (19.7%) had partial responses, and 16 (13.1%) had minimal responses.
Forty-eight patients (39.3%) had stable disease, 16 (13.1%) had progressive disease, and 10 (8.2%) were not evaluable for response.
The median progression-free survival was 3.7 months, and the median overall survival was 8.6 months.
Common treatment-related adverse events included fatigue/asthenia (69.9%), nausea (69.1%), thrombocytopenia (67.5%), anorexia (52.0%), anemia (48.0%), weight loss (47.2%), neutropenia (35.8%), vomiting (35.0%), diarrhea (33.3%), hyponatremia (30.9%), leukopenia (29.3%), and lymphopenia (13.8%).
Trials of selinexor were placed on partial clinical hold in March 2017 due to a lack of information about serious adverse events. However, the hold was lifted for trials of patients with hematologic malignancies at the end of that same month.
The U.S. Food and Drug Administration (FDA) has accepted for priority review the new drug application (NDA) for selinexor.
With this NDA, Karyopharm Therapeutics Inc., is seeking accelerated approval for selinexor, an oral selective inhibitor of nuclear export compound, as a treatment for penta-refractory multiple myeloma (MM).
The FDA grants priority review to applications for products that may provide significant improvements in the treatment, diagnosis, or prevention of serious conditions.
The agency intends to take action on a priority review application within 6 months of receiving it rather than the standard 10 months.
The FDA plans to make a decision on the NDA for selinexor by April 6, 2019.
Selinexor also has orphan drug and fast track designations from the FDA for the treatment of penta-refractory MM.
Selinexor has demonstrated a clinical benefit in penta-refractory MM patients in the phase 2 STORM trial, according to researchers.
Results from this trial were recently presented at the Society of Hematologic Oncology (SOHO) 2018 Annual Meeting.
STORM included 122 patients with penta-refractory MM. They received selinexor at 80 mg twice weekly plus dexamethasone at 20 mg twice weekly until disease progression.
Two patients (1.6%) achieved stringent complete responses (with minimal residual disease negativity), six patients (4.9%) had very good partial responses, 24 (19.7%) had partial responses, and 16 (13.1%) had minimal responses.
Forty-eight patients (39.3%) had stable disease, 16 (13.1%) had progressive disease, and 10 (8.2%) were not evaluable for response.
The median progression-free survival was 3.7 months, and the median overall survival was 8.6 months.
Common treatment-related adverse events included fatigue/asthenia (69.9%), nausea (69.1%), thrombocytopenia (67.5%), anorexia (52.0%), anemia (48.0%), weight loss (47.2%), neutropenia (35.8%), vomiting (35.0%), diarrhea (33.3%), hyponatremia (30.9%), leukopenia (29.3%), and lymphopenia (13.8%).
Trials of selinexor were placed on partial clinical hold in March 2017 due to a lack of information about serious adverse events. However, the hold was lifted for trials of patients with hematologic malignancies at the end of that same month.
The U.S. Food and Drug Administration (FDA) has accepted for priority review the new drug application (NDA) for selinexor.
With this NDA, Karyopharm Therapeutics Inc., is seeking accelerated approval for selinexor, an oral selective inhibitor of nuclear export compound, as a treatment for penta-refractory multiple myeloma (MM).
The FDA grants priority review to applications for products that may provide significant improvements in the treatment, diagnosis, or prevention of serious conditions.
The agency intends to take action on a priority review application within 6 months of receiving it rather than the standard 10 months.
The FDA plans to make a decision on the NDA for selinexor by April 6, 2019.
Selinexor also has orphan drug and fast track designations from the FDA for the treatment of penta-refractory MM.
Selinexor has demonstrated a clinical benefit in penta-refractory MM patients in the phase 2 STORM trial, according to researchers.
Results from this trial were recently presented at the Society of Hematologic Oncology (SOHO) 2018 Annual Meeting.
STORM included 122 patients with penta-refractory MM. They received selinexor at 80 mg twice weekly plus dexamethasone at 20 mg twice weekly until disease progression.
Two patients (1.6%) achieved stringent complete responses (with minimal residual disease negativity), six patients (4.9%) had very good partial responses, 24 (19.7%) had partial responses, and 16 (13.1%) had minimal responses.
Forty-eight patients (39.3%) had stable disease, 16 (13.1%) had progressive disease, and 10 (8.2%) were not evaluable for response.
The median progression-free survival was 3.7 months, and the median overall survival was 8.6 months.
Common treatment-related adverse events included fatigue/asthenia (69.9%), nausea (69.1%), thrombocytopenia (67.5%), anorexia (52.0%), anemia (48.0%), weight loss (47.2%), neutropenia (35.8%), vomiting (35.0%), diarrhea (33.3%), hyponatremia (30.9%), leukopenia (29.3%), and lymphopenia (13.8%).
Trials of selinexor were placed on partial clinical hold in March 2017 due to a lack of information about serious adverse events. However, the hold was lifted for trials of patients with hematologic malignancies at the end of that same month.
Researchers say rethink ‘arbitrary categorization’ of VTE risk
Danish researchers conducted a large, 16-year study of patients with venous thromboembolism (VTE) and found a high recurrence risk in all types of VTE.
At 6 months of follow-up, patients with unprovoked and provoked VTE had similar risk of recurrence, lower than that for patients with cancer-related VTE.
But at a 10-year follow-up, patients with unprovoked VTE had a recurrence risk similar to cancer-related VTE.
Based on these findings, the investigators concluded that risk stratification for these patients needs to be optimized.
“Our findings indicate that we may need to rethink arbitrary categorization, considering the heterogeneity of patients with venous thromboembolism,” they wrote.
They published their findings in The American Journal of Medicine.
The investigators used data from 3 nationwide Danish registries to analyze the risk of recurrent VTE in 73,993 patients with incident VTE. They stratified the patients according to whether the VTE was unprovoked, provoked, or cancer-related.
Provoked VTE occurs in patients without cancer but with other contributing factors such as surgery or trauma, and unprovoked VTE occurs without well-known provoking risk factors. Investigators did not include non-melanoma skin cancer in the cancer-related VTE classification.
Median age of the study population was 62.3 years and 54.1% were women.
During a median follow-up of 3.7 years, 9,205 patients experienced a recurrent event.
At the 6-month follow-up, the recurrence rates per 100 person-years were 6.92 for provoked, 6.80 for unprovoked, and 9.06 for cancer-related VTE.
And at the 10-year follow-up, recurrence rates were 2.22 (provoked), 2.84 (unprovoked), and 3.70 (cancer-related). This corresponded to an 18% higher adjusted relative risk of recurrence for patients with unprovoked VTE than patients with provoked VTE.
The investigators observed that at 10 years, the recurrence risk following an unprovoked VTE resembled the risk of patients with cancer-related VTE.
They suggested the mechanism for this could be a “rebound thrombosis” caused by a discontinuation of oral anticoagulants after an unprovoked VTE.
The investigators noted that the findings persisted through various sensitivity analyses “conducted to challenge the robustness of our finding.”
Two areas of concern, they wrote, arise from these findings: how long to anticoagulate patients and which patients to treat.
"Optimal duration of anticoagulation is a pivotal and an ongoing scientific and clinical concern," explained lead investigator Ida Ehlers Albertsen, MD, of Aalborg University in Denmark.
"The emergence of the non-vitamin K antagonist oral anticoagulants has changed the landscape for prevention of thrombosis, and contemporary risk stratification approaches may need to be adjusted according to these effective and safer agents."
Danish researchers conducted a large, 16-year study of patients with venous thromboembolism (VTE) and found a high recurrence risk in all types of VTE.
At 6 months of follow-up, patients with unprovoked and provoked VTE had similar risk of recurrence, lower than that for patients with cancer-related VTE.
But at a 10-year follow-up, patients with unprovoked VTE had a recurrence risk similar to cancer-related VTE.
Based on these findings, the investigators concluded that risk stratification for these patients needs to be optimized.
“Our findings indicate that we may need to rethink arbitrary categorization, considering the heterogeneity of patients with venous thromboembolism,” they wrote.
They published their findings in The American Journal of Medicine.
The investigators used data from 3 nationwide Danish registries to analyze the risk of recurrent VTE in 73,993 patients with incident VTE. They stratified the patients according to whether the VTE was unprovoked, provoked, or cancer-related.
Provoked VTE occurs in patients without cancer but with other contributing factors such as surgery or trauma, and unprovoked VTE occurs without well-known provoking risk factors. Investigators did not include non-melanoma skin cancer in the cancer-related VTE classification.
Median age of the study population was 62.3 years and 54.1% were women.
During a median follow-up of 3.7 years, 9,205 patients experienced a recurrent event.
At the 6-month follow-up, the recurrence rates per 100 person-years were 6.92 for provoked, 6.80 for unprovoked, and 9.06 for cancer-related VTE.
And at the 10-year follow-up, recurrence rates were 2.22 (provoked), 2.84 (unprovoked), and 3.70 (cancer-related). This corresponded to an 18% higher adjusted relative risk of recurrence for patients with unprovoked VTE than patients with provoked VTE.
The investigators observed that at 10 years, the recurrence risk following an unprovoked VTE resembled the risk of patients with cancer-related VTE.
They suggested the mechanism for this could be a “rebound thrombosis” caused by a discontinuation of oral anticoagulants after an unprovoked VTE.
The investigators noted that the findings persisted through various sensitivity analyses “conducted to challenge the robustness of our finding.”
Two areas of concern, they wrote, arise from these findings: how long to anticoagulate patients and which patients to treat.
"Optimal duration of anticoagulation is a pivotal and an ongoing scientific and clinical concern," explained lead investigator Ida Ehlers Albertsen, MD, of Aalborg University in Denmark.
"The emergence of the non-vitamin K antagonist oral anticoagulants has changed the landscape for prevention of thrombosis, and contemporary risk stratification approaches may need to be adjusted according to these effective and safer agents."
Danish researchers conducted a large, 16-year study of patients with venous thromboembolism (VTE) and found a high recurrence risk in all types of VTE.
At 6 months of follow-up, patients with unprovoked and provoked VTE had similar risk of recurrence, lower than that for patients with cancer-related VTE.
But at a 10-year follow-up, patients with unprovoked VTE had a recurrence risk similar to cancer-related VTE.
Based on these findings, the investigators concluded that risk stratification for these patients needs to be optimized.
“Our findings indicate that we may need to rethink arbitrary categorization, considering the heterogeneity of patients with venous thromboembolism,” they wrote.
They published their findings in The American Journal of Medicine.
The investigators used data from 3 nationwide Danish registries to analyze the risk of recurrent VTE in 73,993 patients with incident VTE. They stratified the patients according to whether the VTE was unprovoked, provoked, or cancer-related.
Provoked VTE occurs in patients without cancer but with other contributing factors such as surgery or trauma, and unprovoked VTE occurs without well-known provoking risk factors. Investigators did not include non-melanoma skin cancer in the cancer-related VTE classification.
Median age of the study population was 62.3 years and 54.1% were women.
During a median follow-up of 3.7 years, 9,205 patients experienced a recurrent event.
At the 6-month follow-up, the recurrence rates per 100 person-years were 6.92 for provoked, 6.80 for unprovoked, and 9.06 for cancer-related VTE.
And at the 10-year follow-up, recurrence rates were 2.22 (provoked), 2.84 (unprovoked), and 3.70 (cancer-related). This corresponded to an 18% higher adjusted relative risk of recurrence for patients with unprovoked VTE than patients with provoked VTE.
The investigators observed that at 10 years, the recurrence risk following an unprovoked VTE resembled the risk of patients with cancer-related VTE.
They suggested the mechanism for this could be a “rebound thrombosis” caused by a discontinuation of oral anticoagulants after an unprovoked VTE.
The investigators noted that the findings persisted through various sensitivity analyses “conducted to challenge the robustness of our finding.”
Two areas of concern, they wrote, arise from these findings: how long to anticoagulate patients and which patients to treat.
"Optimal duration of anticoagulation is a pivotal and an ongoing scientific and clinical concern," explained lead investigator Ida Ehlers Albertsen, MD, of Aalborg University in Denmark.
"The emergence of the non-vitamin K antagonist oral anticoagulants has changed the landscape for prevention of thrombosis, and contemporary risk stratification approaches may need to be adjusted according to these effective and safer agents."
Duvelisib bests ofatumumab as monotherapy for treatment of CLL/SLL
Final analysis of the phase 3 DUO trial has shown monotherapy with oral duvelisib results in a statistically significant improvement in progression-free survival (PFS) and overall response rate (ORR) compared to monotherapy with ofatumumab for patients with relapsed or refractory chronic lymphocytic leukemia/small lympchocytic lymphoma (CLL/SLL).
PFS for all patients as assessed by Independent Review Committee (IRC) was a median 13.3 months with duvelisib compared to 9.9 months with ofatumumab (P<0.0001).
ORR was significantly higher with duvelisib, 74% compared to 45%, P<0.0001, regardless of deletion 17p status.
Duvelisib (Copiktra™) was recently approved by the U.S. Food and Drug Administration for CLL/SLL based in part on this head-to-head trial.
The investigators reported the results in Blood.
"The way we treat patients with CLL is changing rapidly as we move from standard chemotherapy-based approaches to more targeted therapies," said principal investigator Ian W. Flinn, MD, PhD, of Sarah Cannon Research Institute in Nashville.
"Based on these data, duvelisib may offer a new treatment option for patients who otherwise may have limited options."
Duvelisib is an oral, dual inhibitor of phosphoinositide 3-kinase (PI3K)-δ and -γ, which means it blocks the survival and proliferation of malignant B cells and also disrupts the recruitment and differentiation of T cells and macrophages within the tumor microenvironment.
Ofatumumab is a humanized anti-CD20 antibody with single-agent efficacy in refractory CLL. It is approved by the FDA as a treatment option in CLL.
Study design
Investigators randomized 319 relapsed or refractory CLL/SLL patients, 160 to the duvelisib arm and 159 to the ofatumumab arm.
Patients in the duvelisib arm self-administered 25 mg capsules twice daily continuously in 28-day cycles. They could take duvelisib for up to 18 cycles, until disease progression or unacceptable toxicity.
Ofatumumab-treated patients received infusions as approved in the product labeling for monotherapy in relapsed CLL. Dosing of ofatumumab could not exceed 12 doses in 7 cycles.
Prophylaxis for Pneumocystis jirovecci was required for all patients on both treatment arms.
Patients were allowed to crossover to a separate extension study to receive the opposite therapy if they had progressive disease.
They were followed for a median of 22.4 months.
Patient characteristics
According to the investigators, patient characteristics were well balanced between the arms.
The majority (60%) were male and the median age in both arms was 69. Most had an ECOG performance status of 0 or 1; 7% in the duvelisib arm and 10% in the ofatumumab arm had a performance status of 2.
Other patient characteristics in the duvelisib and ofatumumab arms, respectively, were:
- Time from initial diagnosis: 7.5 years, 6.7 years
- CLL/SLL, %: 97/5, 99/2
- Bulky disease: 46%, 45%
- Baseline lymphocyte counts: 38x109/L, 35x109/L
- Deletion 17p and/or TP53 mutation: 31%, 33%
- Median number of prior therapies: 2 in each arm
- Previous alkylating agent: 93%, 95%
- Previous monoclonal antibody: 78%, 83%
- Prior purine analog: 60%, 71%
Of the total patients enrolled, 158 patients in the duvelisib arm and 155 in the ofatumumab arm received treatment, for a median exposure of 50 weeks and 23 weeks, respectively.
Efficacy
In addition to the significantly improved overall PFS and ORR with duvelisib, further analysis revealed that PFS also improved for all predefined subgroups.
High-risk patients with deletion 17p/TP53 mutations also experienced a significant improvement in PFS with duvelisib of 12.7 months compared to 9.0 months with ofatumumab by IRC (P=0.0002).
The estimated probability of being progression-free for these patients at 6 and 12 moths was 73% and 55% with duvelisib and 63% and 30% with ofatumumab.
The investigators pointed out that duvelisib treatment was particularly effective in eliciting a lymph node response—85.0% compared to 15.7% with ofatumumab as assessed by IRC (P<0.0001).
Median overall survival was not reached in either arm. The 12-month probability of survival was 86% for both treatments.
Safety
Median treatment exposure was almost twice as long in the duvelisib arm because ofatumumab treatment was not allowed to exceed 12 doses as specified in the prescribing information.
The investigators explained this resulted in a longer adverse event (AE) reporting period for duvelisib.
One hundred twenty-four duvelisib-treated patients discontinued treatment, most commonly due to AEs (35%), disease progression (22%), subject withdrawal (8%), and death (8%).
All ofatumumab-treated patients discontinued treatment by the time of data cutoff, and 67% had completed treatment as per protocol. Others discontinued due to disease progression (20%), subject withdrawal (5%), and AEs (4%).
Eight (5%) duvelisib patients crossed over to ofatumumab therapy at the time of disease progression, and 89 (57%) ofatumumab-treated patients crossed over to duvelisib.
Nearly all patients in both arms experienced an AE.
The most common hematologic malignancies with duvelisib and ofatumumab, respectively, occurring in 10% or more patients were neutropenia (33%, 21%), anemia (23%, 10%), and thrombocytopenia (15%, 6%).
The most common nonhematologic AES with duvelisib were diarrhea (51%), pyrexia (29%), nausea (23%), and cough (21%).
With ofatumumab, the most common nonhematologic AES were infusion-related reaction (19%), cough (14%), and diarrhea, rash, and fatigue (12% each).
Grade 3 or greater AEs occurred in 87% of duvelisib-treated patients and 48% in the ofatumumab arm.
The most common grade 3 or greater events with duvelisib were neutropenia (30%), diarrhea (15%), pneumonia (14%), and anemia (13%).
With ofatumumab, only neutropenia (17%) of grade 3 or higher occurred in 10% or more patients.
Severe immune-related toxicities with duvelisib included colitis (12%) and pneumonitis, alanine transaminase (ALT) or aspartate transaminase (AST) increase (3% each). The events were managed with dose interruptions and steroid therapy for pneumonitis or colitis. All reported events resolved, and none was fatal.
Infectious AEs occurred more frequently with duvelisib, 69% compared to 43% in the ofatumumab arm. Pneumonia (18%) and upper respiratory tract infection (16%) were the most common events.
Three patients in the duvelisib arm and 1 in the ofatumumab arm contracted Pneumocystis jirovecii.
The most frequently reported serious AE was pneumonia (duvelisib 15%; ofatumumab 3%).
Nineteen fatal AEs occurred in patients on the duvelisib arm, 4 of which were related to the study drug: staphylococcal pneumonia (n = 2), sepsis (n=1), and general health deterioration (n = 1).
Seven fatal AEs occurred in patients on the ofatumumab arm, although none was attributed to ofatumumab.
The DUO trial was sponsored by Verastem Oncology and Infinity Pharmaceuticals , Inc.
Final analysis of the phase 3 DUO trial has shown monotherapy with oral duvelisib results in a statistically significant improvement in progression-free survival (PFS) and overall response rate (ORR) compared to monotherapy with ofatumumab for patients with relapsed or refractory chronic lymphocytic leukemia/small lympchocytic lymphoma (CLL/SLL).
PFS for all patients as assessed by Independent Review Committee (IRC) was a median 13.3 months with duvelisib compared to 9.9 months with ofatumumab (P<0.0001).
ORR was significantly higher with duvelisib, 74% compared to 45%, P<0.0001, regardless of deletion 17p status.
Duvelisib (Copiktra™) was recently approved by the U.S. Food and Drug Administration for CLL/SLL based in part on this head-to-head trial.
The investigators reported the results in Blood.
"The way we treat patients with CLL is changing rapidly as we move from standard chemotherapy-based approaches to more targeted therapies," said principal investigator Ian W. Flinn, MD, PhD, of Sarah Cannon Research Institute in Nashville.
"Based on these data, duvelisib may offer a new treatment option for patients who otherwise may have limited options."
Duvelisib is an oral, dual inhibitor of phosphoinositide 3-kinase (PI3K)-δ and -γ, which means it blocks the survival and proliferation of malignant B cells and also disrupts the recruitment and differentiation of T cells and macrophages within the tumor microenvironment.
Ofatumumab is a humanized anti-CD20 antibody with single-agent efficacy in refractory CLL. It is approved by the FDA as a treatment option in CLL.
Study design
Investigators randomized 319 relapsed or refractory CLL/SLL patients, 160 to the duvelisib arm and 159 to the ofatumumab arm.
Patients in the duvelisib arm self-administered 25 mg capsules twice daily continuously in 28-day cycles. They could take duvelisib for up to 18 cycles, until disease progression or unacceptable toxicity.
Ofatumumab-treated patients received infusions as approved in the product labeling for monotherapy in relapsed CLL. Dosing of ofatumumab could not exceed 12 doses in 7 cycles.
Prophylaxis for Pneumocystis jirovecci was required for all patients on both treatment arms.
Patients were allowed to crossover to a separate extension study to receive the opposite therapy if they had progressive disease.
They were followed for a median of 22.4 months.
Patient characteristics
According to the investigators, patient characteristics were well balanced between the arms.
The majority (60%) were male and the median age in both arms was 69. Most had an ECOG performance status of 0 or 1; 7% in the duvelisib arm and 10% in the ofatumumab arm had a performance status of 2.
Other patient characteristics in the duvelisib and ofatumumab arms, respectively, were:
- Time from initial diagnosis: 7.5 years, 6.7 years
- CLL/SLL, %: 97/5, 99/2
- Bulky disease: 46%, 45%
- Baseline lymphocyte counts: 38x109/L, 35x109/L
- Deletion 17p and/or TP53 mutation: 31%, 33%
- Median number of prior therapies: 2 in each arm
- Previous alkylating agent: 93%, 95%
- Previous monoclonal antibody: 78%, 83%
- Prior purine analog: 60%, 71%
Of the total patients enrolled, 158 patients in the duvelisib arm and 155 in the ofatumumab arm received treatment, for a median exposure of 50 weeks and 23 weeks, respectively.
Efficacy
In addition to the significantly improved overall PFS and ORR with duvelisib, further analysis revealed that PFS also improved for all predefined subgroups.
High-risk patients with deletion 17p/TP53 mutations also experienced a significant improvement in PFS with duvelisib of 12.7 months compared to 9.0 months with ofatumumab by IRC (P=0.0002).
The estimated probability of being progression-free for these patients at 6 and 12 moths was 73% and 55% with duvelisib and 63% and 30% with ofatumumab.
The investigators pointed out that duvelisib treatment was particularly effective in eliciting a lymph node response—85.0% compared to 15.7% with ofatumumab as assessed by IRC (P<0.0001).
Median overall survival was not reached in either arm. The 12-month probability of survival was 86% for both treatments.
Safety
Median treatment exposure was almost twice as long in the duvelisib arm because ofatumumab treatment was not allowed to exceed 12 doses as specified in the prescribing information.
The investigators explained this resulted in a longer adverse event (AE) reporting period for duvelisib.
One hundred twenty-four duvelisib-treated patients discontinued treatment, most commonly due to AEs (35%), disease progression (22%), subject withdrawal (8%), and death (8%).
All ofatumumab-treated patients discontinued treatment by the time of data cutoff, and 67% had completed treatment as per protocol. Others discontinued due to disease progression (20%), subject withdrawal (5%), and AEs (4%).
Eight (5%) duvelisib patients crossed over to ofatumumab therapy at the time of disease progression, and 89 (57%) ofatumumab-treated patients crossed over to duvelisib.
Nearly all patients in both arms experienced an AE.
The most common hematologic malignancies with duvelisib and ofatumumab, respectively, occurring in 10% or more patients were neutropenia (33%, 21%), anemia (23%, 10%), and thrombocytopenia (15%, 6%).
The most common nonhematologic AES with duvelisib were diarrhea (51%), pyrexia (29%), nausea (23%), and cough (21%).
With ofatumumab, the most common nonhematologic AES were infusion-related reaction (19%), cough (14%), and diarrhea, rash, and fatigue (12% each).
Grade 3 or greater AEs occurred in 87% of duvelisib-treated patients and 48% in the ofatumumab arm.
The most common grade 3 or greater events with duvelisib were neutropenia (30%), diarrhea (15%), pneumonia (14%), and anemia (13%).
With ofatumumab, only neutropenia (17%) of grade 3 or higher occurred in 10% or more patients.
Severe immune-related toxicities with duvelisib included colitis (12%) and pneumonitis, alanine transaminase (ALT) or aspartate transaminase (AST) increase (3% each). The events were managed with dose interruptions and steroid therapy for pneumonitis or colitis. All reported events resolved, and none was fatal.
Infectious AEs occurred more frequently with duvelisib, 69% compared to 43% in the ofatumumab arm. Pneumonia (18%) and upper respiratory tract infection (16%) were the most common events.
Three patients in the duvelisib arm and 1 in the ofatumumab arm contracted Pneumocystis jirovecii.
The most frequently reported serious AE was pneumonia (duvelisib 15%; ofatumumab 3%).
Nineteen fatal AEs occurred in patients on the duvelisib arm, 4 of which were related to the study drug: staphylococcal pneumonia (n = 2), sepsis (n=1), and general health deterioration (n = 1).
Seven fatal AEs occurred in patients on the ofatumumab arm, although none was attributed to ofatumumab.
The DUO trial was sponsored by Verastem Oncology and Infinity Pharmaceuticals , Inc.
Final analysis of the phase 3 DUO trial has shown monotherapy with oral duvelisib results in a statistically significant improvement in progression-free survival (PFS) and overall response rate (ORR) compared to monotherapy with ofatumumab for patients with relapsed or refractory chronic lymphocytic leukemia/small lympchocytic lymphoma (CLL/SLL).
PFS for all patients as assessed by Independent Review Committee (IRC) was a median 13.3 months with duvelisib compared to 9.9 months with ofatumumab (P<0.0001).
ORR was significantly higher with duvelisib, 74% compared to 45%, P<0.0001, regardless of deletion 17p status.
Duvelisib (Copiktra™) was recently approved by the U.S. Food and Drug Administration for CLL/SLL based in part on this head-to-head trial.
The investigators reported the results in Blood.
"The way we treat patients with CLL is changing rapidly as we move from standard chemotherapy-based approaches to more targeted therapies," said principal investigator Ian W. Flinn, MD, PhD, of Sarah Cannon Research Institute in Nashville.
"Based on these data, duvelisib may offer a new treatment option for patients who otherwise may have limited options."
Duvelisib is an oral, dual inhibitor of phosphoinositide 3-kinase (PI3K)-δ and -γ, which means it blocks the survival and proliferation of malignant B cells and also disrupts the recruitment and differentiation of T cells and macrophages within the tumor microenvironment.
Ofatumumab is a humanized anti-CD20 antibody with single-agent efficacy in refractory CLL. It is approved by the FDA as a treatment option in CLL.
Study design
Investigators randomized 319 relapsed or refractory CLL/SLL patients, 160 to the duvelisib arm and 159 to the ofatumumab arm.
Patients in the duvelisib arm self-administered 25 mg capsules twice daily continuously in 28-day cycles. They could take duvelisib for up to 18 cycles, until disease progression or unacceptable toxicity.
Ofatumumab-treated patients received infusions as approved in the product labeling for monotherapy in relapsed CLL. Dosing of ofatumumab could not exceed 12 doses in 7 cycles.
Prophylaxis for Pneumocystis jirovecci was required for all patients on both treatment arms.
Patients were allowed to crossover to a separate extension study to receive the opposite therapy if they had progressive disease.
They were followed for a median of 22.4 months.
Patient characteristics
According to the investigators, patient characteristics were well balanced between the arms.
The majority (60%) were male and the median age in both arms was 69. Most had an ECOG performance status of 0 or 1; 7% in the duvelisib arm and 10% in the ofatumumab arm had a performance status of 2.
Other patient characteristics in the duvelisib and ofatumumab arms, respectively, were:
- Time from initial diagnosis: 7.5 years, 6.7 years
- CLL/SLL, %: 97/5, 99/2
- Bulky disease: 46%, 45%
- Baseline lymphocyte counts: 38x109/L, 35x109/L
- Deletion 17p and/or TP53 mutation: 31%, 33%
- Median number of prior therapies: 2 in each arm
- Previous alkylating agent: 93%, 95%
- Previous monoclonal antibody: 78%, 83%
- Prior purine analog: 60%, 71%
Of the total patients enrolled, 158 patients in the duvelisib arm and 155 in the ofatumumab arm received treatment, for a median exposure of 50 weeks and 23 weeks, respectively.
Efficacy
In addition to the significantly improved overall PFS and ORR with duvelisib, further analysis revealed that PFS also improved for all predefined subgroups.
High-risk patients with deletion 17p/TP53 mutations also experienced a significant improvement in PFS with duvelisib of 12.7 months compared to 9.0 months with ofatumumab by IRC (P=0.0002).
The estimated probability of being progression-free for these patients at 6 and 12 moths was 73% and 55% with duvelisib and 63% and 30% with ofatumumab.
The investigators pointed out that duvelisib treatment was particularly effective in eliciting a lymph node response—85.0% compared to 15.7% with ofatumumab as assessed by IRC (P<0.0001).
Median overall survival was not reached in either arm. The 12-month probability of survival was 86% for both treatments.
Safety
Median treatment exposure was almost twice as long in the duvelisib arm because ofatumumab treatment was not allowed to exceed 12 doses as specified in the prescribing information.
The investigators explained this resulted in a longer adverse event (AE) reporting period for duvelisib.
One hundred twenty-four duvelisib-treated patients discontinued treatment, most commonly due to AEs (35%), disease progression (22%), subject withdrawal (8%), and death (8%).
All ofatumumab-treated patients discontinued treatment by the time of data cutoff, and 67% had completed treatment as per protocol. Others discontinued due to disease progression (20%), subject withdrawal (5%), and AEs (4%).
Eight (5%) duvelisib patients crossed over to ofatumumab therapy at the time of disease progression, and 89 (57%) ofatumumab-treated patients crossed over to duvelisib.
Nearly all patients in both arms experienced an AE.
The most common hematologic malignancies with duvelisib and ofatumumab, respectively, occurring in 10% or more patients were neutropenia (33%, 21%), anemia (23%, 10%), and thrombocytopenia (15%, 6%).
The most common nonhematologic AES with duvelisib were diarrhea (51%), pyrexia (29%), nausea (23%), and cough (21%).
With ofatumumab, the most common nonhematologic AES were infusion-related reaction (19%), cough (14%), and diarrhea, rash, and fatigue (12% each).
Grade 3 or greater AEs occurred in 87% of duvelisib-treated patients and 48% in the ofatumumab arm.
The most common grade 3 or greater events with duvelisib were neutropenia (30%), diarrhea (15%), pneumonia (14%), and anemia (13%).
With ofatumumab, only neutropenia (17%) of grade 3 or higher occurred in 10% or more patients.
Severe immune-related toxicities with duvelisib included colitis (12%) and pneumonitis, alanine transaminase (ALT) or aspartate transaminase (AST) increase (3% each). The events were managed with dose interruptions and steroid therapy for pneumonitis or colitis. All reported events resolved, and none was fatal.
Infectious AEs occurred more frequently with duvelisib, 69% compared to 43% in the ofatumumab arm. Pneumonia (18%) and upper respiratory tract infection (16%) were the most common events.
Three patients in the duvelisib arm and 1 in the ofatumumab arm contracted Pneumocystis jirovecii.
The most frequently reported serious AE was pneumonia (duvelisib 15%; ofatumumab 3%).
Nineteen fatal AEs occurred in patients on the duvelisib arm, 4 of which were related to the study drug: staphylococcal pneumonia (n = 2), sepsis (n=1), and general health deterioration (n = 1).
Seven fatal AEs occurred in patients on the ofatumumab arm, although none was attributed to ofatumumab.
The DUO trial was sponsored by Verastem Oncology and Infinity Pharmaceuticals , Inc.
Emicizumab now also approved for hemophilia A without inhibitors
The U.S. Food and Drug Administration (FDA) approved emicizumab-kxwh (Hemlibra) for prophylaxis to prevent or reduce the frequency of bleeding episodes in adult and pediatric patients, including newborns, with hemophilia A with or without factor VIII (FVIII) inhibitors.
Emicizumab is a humanized bispecific factor IXa- and factor X-directed antibody for patients with congenital FVIII deficiency.
It was first approved in 2017 for hemophilia A patients with FVIII inhibitors.
The current approval expands the indication to include patients without FVIII inhibitors and provides new dosing regimens.
The FDA based the current approval on the HAVEN 3 and HAVEN 4 trials.
HAVEN 3 (NCT02847637)
This multicenter trial randomized 89 patients with severe hemophilia A without FVIII inhibitors to receive emicizumab prophylaxis at one of 3 dose levels: 1.5 mg/kg once weekly (ARM A), 3 mg/kg once every two weeks (Arm B), or no prophylaxis (Arm C). Patients had previously received on-demand treatment with FVIII.
Before the start of the trial, investigators stratified patients by 24-week bleed rate—fewer than 9 bleeds and 9 or more bleeds.
Patients were treated with emicizumab for a minimum of 24 weeks.
Patients in Arm A experienced a 96% reduction in annualized bleed rate (ABR) compared to patients with no prophylaxis (ABR ratio=0.04; P<0.0001).
Patients in Arm B had a 97% reduction in ABR compared to patients with no prophylaxis (ABR ratio=0.03; P<0.0001).
The trial met all bleed-related secondary endpoints, such as all bleeds, treated spontaneous bleeds, treated joint bleeds, and treated target joint bleeds.
HAVEN 4 (NCT03020160)
This was a single-arm multicenter trial in 48 adult and adolescent males with hemophilia A with or without FVIII inhibitors. The patients had previously received on-demand or prophylactic treatment with FVIII or bypassing agents.
The study was conducted in two parts: a run-in of 7 patients to determine the pharmacokinetics after a single 6 mg/kg dose in four weeks. This was followed by the same dose once every four weeks for at least 24 weeks.
The second part was an expansion cohort of 41 patients who received emicizumab at 3 mg/kg once weekly for the first four weeks followed by 6 mg/kg once every four weeks for at least 24 weeks.
The ABR for treated bleeds was 2.4 (95% CI: 1.38, 4.28) and the median ABR was 0.0 (interquartile range: 0.00, 2.08).
The recommended loading dose is 3 mg/kg once weekly for the first four weeks for all prophylactic regimens.
Safety
The prescribing information for emicizumab includes a warning about thrombotic microangiopathy and thromboembolism.
These events were reported on average when a cumulative amount of >100 U/kg/24 hours of activated prothrombin complex concentrate (aPCC) was administered for 24 hours or more to patients receiving emicizumab prophylaxis.
According to the warning box, patients should be monitored for these events if aPCC is administered. If symptoms occur, aPCC should be discontinued and emicizumab dosing suspended.
The most common adverse reactions reported for emicizumab with an incidence ≥10% were injection site reactions (22%), headache (15%), and arthralgia (15%).
Emicizumab is manufactured by Genentech, Inc., a member of the Roche Group.
Additional data on emicizumab can be found in an earlier Roche media release.
The U.S. Food and Drug Administration (FDA) approved emicizumab-kxwh (Hemlibra) for prophylaxis to prevent or reduce the frequency of bleeding episodes in adult and pediatric patients, including newborns, with hemophilia A with or without factor VIII (FVIII) inhibitors.
Emicizumab is a humanized bispecific factor IXa- and factor X-directed antibody for patients with congenital FVIII deficiency.
It was first approved in 2017 for hemophilia A patients with FVIII inhibitors.
The current approval expands the indication to include patients without FVIII inhibitors and provides new dosing regimens.
The FDA based the current approval on the HAVEN 3 and HAVEN 4 trials.
HAVEN 3 (NCT02847637)
This multicenter trial randomized 89 patients with severe hemophilia A without FVIII inhibitors to receive emicizumab prophylaxis at one of 3 dose levels: 1.5 mg/kg once weekly (ARM A), 3 mg/kg once every two weeks (Arm B), or no prophylaxis (Arm C). Patients had previously received on-demand treatment with FVIII.
Before the start of the trial, investigators stratified patients by 24-week bleed rate—fewer than 9 bleeds and 9 or more bleeds.
Patients were treated with emicizumab for a minimum of 24 weeks.
Patients in Arm A experienced a 96% reduction in annualized bleed rate (ABR) compared to patients with no prophylaxis (ABR ratio=0.04; P<0.0001).
Patients in Arm B had a 97% reduction in ABR compared to patients with no prophylaxis (ABR ratio=0.03; P<0.0001).
The trial met all bleed-related secondary endpoints, such as all bleeds, treated spontaneous bleeds, treated joint bleeds, and treated target joint bleeds.
HAVEN 4 (NCT03020160)
This was a single-arm multicenter trial in 48 adult and adolescent males with hemophilia A with or without FVIII inhibitors. The patients had previously received on-demand or prophylactic treatment with FVIII or bypassing agents.
The study was conducted in two parts: a run-in of 7 patients to determine the pharmacokinetics after a single 6 mg/kg dose in four weeks. This was followed by the same dose once every four weeks for at least 24 weeks.
The second part was an expansion cohort of 41 patients who received emicizumab at 3 mg/kg once weekly for the first four weeks followed by 6 mg/kg once every four weeks for at least 24 weeks.
The ABR for treated bleeds was 2.4 (95% CI: 1.38, 4.28) and the median ABR was 0.0 (interquartile range: 0.00, 2.08).
The recommended loading dose is 3 mg/kg once weekly for the first four weeks for all prophylactic regimens.
Safety
The prescribing information for emicizumab includes a warning about thrombotic microangiopathy and thromboembolism.
These events were reported on average when a cumulative amount of >100 U/kg/24 hours of activated prothrombin complex concentrate (aPCC) was administered for 24 hours or more to patients receiving emicizumab prophylaxis.
According to the warning box, patients should be monitored for these events if aPCC is administered. If symptoms occur, aPCC should be discontinued and emicizumab dosing suspended.
The most common adverse reactions reported for emicizumab with an incidence ≥10% were injection site reactions (22%), headache (15%), and arthralgia (15%).
Emicizumab is manufactured by Genentech, Inc., a member of the Roche Group.
Additional data on emicizumab can be found in an earlier Roche media release.
The U.S. Food and Drug Administration (FDA) approved emicizumab-kxwh (Hemlibra) for prophylaxis to prevent or reduce the frequency of bleeding episodes in adult and pediatric patients, including newborns, with hemophilia A with or without factor VIII (FVIII) inhibitors.
Emicizumab is a humanized bispecific factor IXa- and factor X-directed antibody for patients with congenital FVIII deficiency.
It was first approved in 2017 for hemophilia A patients with FVIII inhibitors.
The current approval expands the indication to include patients without FVIII inhibitors and provides new dosing regimens.
The FDA based the current approval on the HAVEN 3 and HAVEN 4 trials.
HAVEN 3 (NCT02847637)
This multicenter trial randomized 89 patients with severe hemophilia A without FVIII inhibitors to receive emicizumab prophylaxis at one of 3 dose levels: 1.5 mg/kg once weekly (ARM A), 3 mg/kg once every two weeks (Arm B), or no prophylaxis (Arm C). Patients had previously received on-demand treatment with FVIII.
Before the start of the trial, investigators stratified patients by 24-week bleed rate—fewer than 9 bleeds and 9 or more bleeds.
Patients were treated with emicizumab for a minimum of 24 weeks.
Patients in Arm A experienced a 96% reduction in annualized bleed rate (ABR) compared to patients with no prophylaxis (ABR ratio=0.04; P<0.0001).
Patients in Arm B had a 97% reduction in ABR compared to patients with no prophylaxis (ABR ratio=0.03; P<0.0001).
The trial met all bleed-related secondary endpoints, such as all bleeds, treated spontaneous bleeds, treated joint bleeds, and treated target joint bleeds.
HAVEN 4 (NCT03020160)
This was a single-arm multicenter trial in 48 adult and adolescent males with hemophilia A with or without FVIII inhibitors. The patients had previously received on-demand or prophylactic treatment with FVIII or bypassing agents.
The study was conducted in two parts: a run-in of 7 patients to determine the pharmacokinetics after a single 6 mg/kg dose in four weeks. This was followed by the same dose once every four weeks for at least 24 weeks.
The second part was an expansion cohort of 41 patients who received emicizumab at 3 mg/kg once weekly for the first four weeks followed by 6 mg/kg once every four weeks for at least 24 weeks.
The ABR for treated bleeds was 2.4 (95% CI: 1.38, 4.28) and the median ABR was 0.0 (interquartile range: 0.00, 2.08).
The recommended loading dose is 3 mg/kg once weekly for the first four weeks for all prophylactic regimens.
Safety
The prescribing information for emicizumab includes a warning about thrombotic microangiopathy and thromboembolism.
These events were reported on average when a cumulative amount of >100 U/kg/24 hours of activated prothrombin complex concentrate (aPCC) was administered for 24 hours or more to patients receiving emicizumab prophylaxis.
According to the warning box, patients should be monitored for these events if aPCC is administered. If symptoms occur, aPCC should be discontinued and emicizumab dosing suspended.
The most common adverse reactions reported for emicizumab with an incidence ≥10% were injection site reactions (22%), headache (15%), and arthralgia (15%).
Emicizumab is manufactured by Genentech, Inc., a member of the Roche Group.
Additional data on emicizumab can be found in an earlier Roche media release.
Researchers develop genetics-based prognostic tool for MDS
Researchers have developed a new risk model for primary myelodysplastic syndromes (MDS) that integrates genetic and clinical information.
The research team considered the current standard for prognostication—the revised International Prognostic Scoring System (IPSS-R)—to be too complex, limited to newly diagnosed cases, and missing information on mutations and age.
So they devised a “simpler and more contemporary” prognostic system, the Mayo Alliance Prognostic Model for MDS.
The team, from the Mayo Clinic in Rochester, Minnesota, and the National Taiwan University Hospital (NTUH), described the new model in Mayo Clinic Proceedings.
Lead author Ayalew Tefferi, MD, of the Mayo Clinic, said the new model “is not an enhancement of the international prognostic scoring system tool, it's a complete makeover."
The team analyzed mutation information from 357 patients with primary MDS or leukemic transformation treated at the Mayo Clinic from the end of December 1994 through mid-December 2017.
The patients were a median age of 74 and 70% were males.
They compared the Mayo patients to 328 NTUH patients, who were a median age of 66 and 65% were males.
Multivariate analysis of the Mayo cohort identified the following as predictors of inferior overall survival:
- Monosomal karyotype (hazard ratio [HR], 5.2; 95% CI, 3.1-8.6)
- Non-monosomal karyotype abnormalities other than single/double del(5q) (HR, 1.8; 95% CI, 1.3-2.6)
- RUNX1 (HR, 2.0; 95% CI, 1.2-3.1)
- ASXL1 (HR, 1.7; 95% CI, 1.2-2.3) mutations
- Absence of SF3B1 mutations (HR, 1.6; 95% CI, 1.1-2.4)
- Age greater than 70 years (HR, 2.2; 95% CI, 1.6-3.1)
- Hemoglobin level less than 8 g/dL in women or less than 9 g/dL in men (HR, 2.3; 95% CI, 1.7-3.1)
- Platelet count less than 75 x 109/L (HR, 1.5; 95% CI, 1.1-2.1)
- 10% or more bone marrow blasts (HR, 1.7; 95% CI, 1.1-2.8)
They then provided values to reflect the prognostic contribution of each of the above predictors and devised the new 4-tiered Mayo prognostic model.
Median 5-year overall survival rates in the 4 categories in the Mayo model were 73% (low risk), 34% (intermediate-1), 7% (intermediate-2), and 0% (high risk; 9-month median survival).
The team then validated the Mayo alliance model by using the NTUH cohort and compared it to the IPSS-R.
The investigators were able to confirm superior predictive accuracy of their model and a substantial discordance between the the Mayo model and the IPSS-R in terms of the pattern of risk distribution.
Examples of discordance included:
- More than 25% of patients belonging to the high-risk category according to the Mayo alliance model were classified as IPSS-R low or intermediate risk
- Almost 50% of patients with intermediate-2 risk category according to the Mayo alliance model were classified as IPSS-R very low or low risk
- Almost 50% of patients with IPSS-R very low risk were classified as intermediate-2 or intermediate-1 risk according to the Mayo alliance model
The authors wrote that this “suggests a fundamental and not incremental advantage for the new Mayo alliance model.”
Researchers have developed a new risk model for primary myelodysplastic syndromes (MDS) that integrates genetic and clinical information.
The research team considered the current standard for prognostication—the revised International Prognostic Scoring System (IPSS-R)—to be too complex, limited to newly diagnosed cases, and missing information on mutations and age.
So they devised a “simpler and more contemporary” prognostic system, the Mayo Alliance Prognostic Model for MDS.
The team, from the Mayo Clinic in Rochester, Minnesota, and the National Taiwan University Hospital (NTUH), described the new model in Mayo Clinic Proceedings.
Lead author Ayalew Tefferi, MD, of the Mayo Clinic, said the new model “is not an enhancement of the international prognostic scoring system tool, it's a complete makeover."
The team analyzed mutation information from 357 patients with primary MDS or leukemic transformation treated at the Mayo Clinic from the end of December 1994 through mid-December 2017.
The patients were a median age of 74 and 70% were males.
They compared the Mayo patients to 328 NTUH patients, who were a median age of 66 and 65% were males.
Multivariate analysis of the Mayo cohort identified the following as predictors of inferior overall survival:
- Monosomal karyotype (hazard ratio [HR], 5.2; 95% CI, 3.1-8.6)
- Non-monosomal karyotype abnormalities other than single/double del(5q) (HR, 1.8; 95% CI, 1.3-2.6)
- RUNX1 (HR, 2.0; 95% CI, 1.2-3.1)
- ASXL1 (HR, 1.7; 95% CI, 1.2-2.3) mutations
- Absence of SF3B1 mutations (HR, 1.6; 95% CI, 1.1-2.4)
- Age greater than 70 years (HR, 2.2; 95% CI, 1.6-3.1)
- Hemoglobin level less than 8 g/dL in women or less than 9 g/dL in men (HR, 2.3; 95% CI, 1.7-3.1)
- Platelet count less than 75 x 109/L (HR, 1.5; 95% CI, 1.1-2.1)
- 10% or more bone marrow blasts (HR, 1.7; 95% CI, 1.1-2.8)
They then provided values to reflect the prognostic contribution of each of the above predictors and devised the new 4-tiered Mayo prognostic model.
Median 5-year overall survival rates in the 4 categories in the Mayo model were 73% (low risk), 34% (intermediate-1), 7% (intermediate-2), and 0% (high risk; 9-month median survival).
The team then validated the Mayo alliance model by using the NTUH cohort and compared it to the IPSS-R.
The investigators were able to confirm superior predictive accuracy of their model and a substantial discordance between the the Mayo model and the IPSS-R in terms of the pattern of risk distribution.
Examples of discordance included:
- More than 25% of patients belonging to the high-risk category according to the Mayo alliance model were classified as IPSS-R low or intermediate risk
- Almost 50% of patients with intermediate-2 risk category according to the Mayo alliance model were classified as IPSS-R very low or low risk
- Almost 50% of patients with IPSS-R very low risk were classified as intermediate-2 or intermediate-1 risk according to the Mayo alliance model
The authors wrote that this “suggests a fundamental and not incremental advantage for the new Mayo alliance model.”
Researchers have developed a new risk model for primary myelodysplastic syndromes (MDS) that integrates genetic and clinical information.
The research team considered the current standard for prognostication—the revised International Prognostic Scoring System (IPSS-R)—to be too complex, limited to newly diagnosed cases, and missing information on mutations and age.
So they devised a “simpler and more contemporary” prognostic system, the Mayo Alliance Prognostic Model for MDS.
The team, from the Mayo Clinic in Rochester, Minnesota, and the National Taiwan University Hospital (NTUH), described the new model in Mayo Clinic Proceedings.
Lead author Ayalew Tefferi, MD, of the Mayo Clinic, said the new model “is not an enhancement of the international prognostic scoring system tool, it's a complete makeover."
The team analyzed mutation information from 357 patients with primary MDS or leukemic transformation treated at the Mayo Clinic from the end of December 1994 through mid-December 2017.
The patients were a median age of 74 and 70% were males.
They compared the Mayo patients to 328 NTUH patients, who were a median age of 66 and 65% were males.
Multivariate analysis of the Mayo cohort identified the following as predictors of inferior overall survival:
- Monosomal karyotype (hazard ratio [HR], 5.2; 95% CI, 3.1-8.6)
- Non-monosomal karyotype abnormalities other than single/double del(5q) (HR, 1.8; 95% CI, 1.3-2.6)
- RUNX1 (HR, 2.0; 95% CI, 1.2-3.1)
- ASXL1 (HR, 1.7; 95% CI, 1.2-2.3) mutations
- Absence of SF3B1 mutations (HR, 1.6; 95% CI, 1.1-2.4)
- Age greater than 70 years (HR, 2.2; 95% CI, 1.6-3.1)
- Hemoglobin level less than 8 g/dL in women or less than 9 g/dL in men (HR, 2.3; 95% CI, 1.7-3.1)
- Platelet count less than 75 x 109/L (HR, 1.5; 95% CI, 1.1-2.1)
- 10% or more bone marrow blasts (HR, 1.7; 95% CI, 1.1-2.8)
They then provided values to reflect the prognostic contribution of each of the above predictors and devised the new 4-tiered Mayo prognostic model.
Median 5-year overall survival rates in the 4 categories in the Mayo model were 73% (low risk), 34% (intermediate-1), 7% (intermediate-2), and 0% (high risk; 9-month median survival).
The team then validated the Mayo alliance model by using the NTUH cohort and compared it to the IPSS-R.
The investigators were able to confirm superior predictive accuracy of their model and a substantial discordance between the the Mayo model and the IPSS-R in terms of the pattern of risk distribution.
Examples of discordance included:
- More than 25% of patients belonging to the high-risk category according to the Mayo alliance model were classified as IPSS-R low or intermediate risk
- Almost 50% of patients with intermediate-2 risk category according to the Mayo alliance model were classified as IPSS-R very low or low risk
- Almost 50% of patients with IPSS-R very low risk were classified as intermediate-2 or intermediate-1 risk according to the Mayo alliance model
The authors wrote that this “suggests a fundamental and not incremental advantage for the new Mayo alliance model.”
Carfilzomib receives approval for once-weekly dosing
The U.S. Food and Drug Administration (FDA) has approved carfilzomib (Kyprolis) for a once-weekly dosing option in combination with dexamethasone for patients with relapsed or refractory multiple myeloma (MM).
Carfilzomib administered once-weekly at 70 mg/m2 with dexamethasone achieved a superior progression-free survival (PFS) and overall response rates (ORR) compared to twice-weekly carfilzomib at doses of 27 mg/m2.
Carfilzomib is not, however, approved for the twice-weekly 27 mg/m2 dose with dexamethasone alone, but with dexamethasone and lenalidomide.
The FDA based its approval on data from the phase 3 ARROW trial.
The FDA reviewed and approved the supplemental New Drug Application under its Oncology Center of Excellence Real-Time Oncology Review and Assessment Aid pilot program. The program is exploring a more efficient review process to ensure that safe and effective treatments are available to patients as soon as possible.
The FDA approved the carfilzomib application in just over a month.
ARROW
The ARROW study, reported at the 2018 ASCO annual meeting and published in The Lancet, evaluated 478 patients with relapsed or refractory MM who had received at least two but no more than three prior therapies. Prior therapies could include bortezomib and an immunomodulatory drug.
Patients randomized to the investigational arm receive a 30-minute infusion of once-weekly carfilzomib (20 mg/m2 on day 1 of cycle 1; 70 mg/m2 on days 8 and 15 of cycle 1; and 70 mg/m2 on days 1, 8 and 15 of subsequent cycles) with 40 mg of dexamethasone.
Patients randomized to the comparator arm received a 10-minute infusion of twice-weekly carfilzomib (20 mg/m2 on days 1 and 2 of cycle 1; 27 mg/m2 on days 8, 9, 15 and 16 of cycle 1; and 27 mg/m2 on days 1, 2, 8, 9, 15 and 16 of subsequent cycles) with 40 mg of dexamethasone.
Patients in the once-weekly arm achieved a statistically significant 3.7-month improvement in PFS compared to the twice-weekly regimen. Median PFS was 11.2 months for the once-weekly patients and 7.6 months for the twice-weekly group (P=0.0014).
Patients in the once-weekly group had a 62.9% ORR compared to 40.8% for those treated twice weekly (P<0.0001).
More patients (7.1%) in the once-weekly group had complete responses or better than those in the twice-weekly arm (1.7%).
The safety profile of the two arms were comparable, with no new safety risks identified in the once-weekly arm.
Treatment-emergent adverse events occurring in 20% or more patients in either arm included anemia, diarrhea, fatigue, hypertension, insomnia, and pyrexia.
First approved in 2012, carfilzomib has indications for the following in the U.S.:
- Treatment of patients with relapsed or refractory multiple myeloma who have received one to three lines of therapy in combination with dexamethasone or with lenalidomide plus dexamethasone.
- As a single agent for the treatment of patients with relapsed or refractory multiple myeloma who have received one or more lines of therapy.
Amgen manufactures carfilzomib for Onyx Pharmaceuticals, Inc.
Prescribing information for carfilzomib is available online.
The U.S. Food and Drug Administration (FDA) has approved carfilzomib (Kyprolis) for a once-weekly dosing option in combination with dexamethasone for patients with relapsed or refractory multiple myeloma (MM).
Carfilzomib administered once-weekly at 70 mg/m2 with dexamethasone achieved a superior progression-free survival (PFS) and overall response rates (ORR) compared to twice-weekly carfilzomib at doses of 27 mg/m2.
Carfilzomib is not, however, approved for the twice-weekly 27 mg/m2 dose with dexamethasone alone, but with dexamethasone and lenalidomide.
The FDA based its approval on data from the phase 3 ARROW trial.
The FDA reviewed and approved the supplemental New Drug Application under its Oncology Center of Excellence Real-Time Oncology Review and Assessment Aid pilot program. The program is exploring a more efficient review process to ensure that safe and effective treatments are available to patients as soon as possible.
The FDA approved the carfilzomib application in just over a month.
ARROW
The ARROW study, reported at the 2018 ASCO annual meeting and published in The Lancet, evaluated 478 patients with relapsed or refractory MM who had received at least two but no more than three prior therapies. Prior therapies could include bortezomib and an immunomodulatory drug.
Patients randomized to the investigational arm receive a 30-minute infusion of once-weekly carfilzomib (20 mg/m2 on day 1 of cycle 1; 70 mg/m2 on days 8 and 15 of cycle 1; and 70 mg/m2 on days 1, 8 and 15 of subsequent cycles) with 40 mg of dexamethasone.
Patients randomized to the comparator arm received a 10-minute infusion of twice-weekly carfilzomib (20 mg/m2 on days 1 and 2 of cycle 1; 27 mg/m2 on days 8, 9, 15 and 16 of cycle 1; and 27 mg/m2 on days 1, 2, 8, 9, 15 and 16 of subsequent cycles) with 40 mg of dexamethasone.
Patients in the once-weekly arm achieved a statistically significant 3.7-month improvement in PFS compared to the twice-weekly regimen. Median PFS was 11.2 months for the once-weekly patients and 7.6 months for the twice-weekly group (P=0.0014).
Patients in the once-weekly group had a 62.9% ORR compared to 40.8% for those treated twice weekly (P<0.0001).
More patients (7.1%) in the once-weekly group had complete responses or better than those in the twice-weekly arm (1.7%).
The safety profile of the two arms were comparable, with no new safety risks identified in the once-weekly arm.
Treatment-emergent adverse events occurring in 20% or more patients in either arm included anemia, diarrhea, fatigue, hypertension, insomnia, and pyrexia.
First approved in 2012, carfilzomib has indications for the following in the U.S.:
- Treatment of patients with relapsed or refractory multiple myeloma who have received one to three lines of therapy in combination with dexamethasone or with lenalidomide plus dexamethasone.
- As a single agent for the treatment of patients with relapsed or refractory multiple myeloma who have received one or more lines of therapy.
Amgen manufactures carfilzomib for Onyx Pharmaceuticals, Inc.
Prescribing information for carfilzomib is available online.
The U.S. Food and Drug Administration (FDA) has approved carfilzomib (Kyprolis) for a once-weekly dosing option in combination with dexamethasone for patients with relapsed or refractory multiple myeloma (MM).
Carfilzomib administered once-weekly at 70 mg/m2 with dexamethasone achieved a superior progression-free survival (PFS) and overall response rates (ORR) compared to twice-weekly carfilzomib at doses of 27 mg/m2.
Carfilzomib is not, however, approved for the twice-weekly 27 mg/m2 dose with dexamethasone alone, but with dexamethasone and lenalidomide.
The FDA based its approval on data from the phase 3 ARROW trial.
The FDA reviewed and approved the supplemental New Drug Application under its Oncology Center of Excellence Real-Time Oncology Review and Assessment Aid pilot program. The program is exploring a more efficient review process to ensure that safe and effective treatments are available to patients as soon as possible.
The FDA approved the carfilzomib application in just over a month.
ARROW
The ARROW study, reported at the 2018 ASCO annual meeting and published in The Lancet, evaluated 478 patients with relapsed or refractory MM who had received at least two but no more than three prior therapies. Prior therapies could include bortezomib and an immunomodulatory drug.
Patients randomized to the investigational arm receive a 30-minute infusion of once-weekly carfilzomib (20 mg/m2 on day 1 of cycle 1; 70 mg/m2 on days 8 and 15 of cycle 1; and 70 mg/m2 on days 1, 8 and 15 of subsequent cycles) with 40 mg of dexamethasone.
Patients randomized to the comparator arm received a 10-minute infusion of twice-weekly carfilzomib (20 mg/m2 on days 1 and 2 of cycle 1; 27 mg/m2 on days 8, 9, 15 and 16 of cycle 1; and 27 mg/m2 on days 1, 2, 8, 9, 15 and 16 of subsequent cycles) with 40 mg of dexamethasone.
Patients in the once-weekly arm achieved a statistically significant 3.7-month improvement in PFS compared to the twice-weekly regimen. Median PFS was 11.2 months for the once-weekly patients and 7.6 months for the twice-weekly group (P=0.0014).
Patients in the once-weekly group had a 62.9% ORR compared to 40.8% for those treated twice weekly (P<0.0001).
More patients (7.1%) in the once-weekly group had complete responses or better than those in the twice-weekly arm (1.7%).
The safety profile of the two arms were comparable, with no new safety risks identified in the once-weekly arm.
Treatment-emergent adverse events occurring in 20% or more patients in either arm included anemia, diarrhea, fatigue, hypertension, insomnia, and pyrexia.
First approved in 2012, carfilzomib has indications for the following in the U.S.:
- Treatment of patients with relapsed or refractory multiple myeloma who have received one to three lines of therapy in combination with dexamethasone or with lenalidomide plus dexamethasone.
- As a single agent for the treatment of patients with relapsed or refractory multiple myeloma who have received one or more lines of therapy.
Amgen manufactures carfilzomib for Onyx Pharmaceuticals, Inc.
Prescribing information for carfilzomib is available online.
Single leukemic cell can contaminate CAR T-cell product
Investigators report that a single leukemic cell unintentionally engineered into the chimeric antigen receptor (CAR) T-cell product can mask it from recognition and confer resistance to CAR T-cell therapy.
They described the case of a 20-year-old male who received the anti-CD19 CAR tisagenlecleucel (Kymriah) and relapsed at day 252 after the infusion.
The transduction of a leukemic cell during manufacture of the CAR T-cell product “is a rare event,” they wrote, and indicated that “this is the only case out of 369 patients reported worldwide at the time of publication.”
Lead author Marco Ruella, MD, of the University of Pennsylvania, and colleagues described the case in a Brief Communication published in Nature Medicine.
"In this case,” Dr. Ruella said, “we found that 100 percent of relapsed leukemic cells carried the CAR that we use to genetically modify T cells."
The patient had B-cell acute lymphoblastic leukemia (B-ALL) and relapsed three times after chemotherapy and a cord blood transplant before enrolling in the phase 1 trial of CTL019 (NCT 01626495).
The investigators reported that the infused CAR cells “displayed the typical pattern of in vivo engraftment and expansion.” At day 28 after the infusion, the patient was in complete remission.
But by day 252, he experienced a second expansion of CAR cells that did not correspond to the re-expansion of CAR+ T cells.
At day 261, the patient relapsed with more than 90% CD10+CD19- leukemic cells in the bone marrow and circulating blasts. The cells were CAR-transduced B-cell leukemia (CARB) cells.
The CARB cells continued to expand, and the patient died of progressive leukemia.
The investigators tracked the origin of the CARB cells by analyzing the relapsed CAR19+ cells using next-generation sequencing.
They hypothesized that the CAR19+ leukemia relapse occurred through lentiviral transduction during the manufacturing process, since they detected no replication-competent lentivirus when testing the patient’s peripheral blood at numerous time points after CTL019 infusion.
Further analysis confirmed the CARB cells were a byproduct made during CTL019 cell manufacturing.
To confirm that the leukemia relapse originated from a single clone, the investigators expanded in mice blast cells detected in the patient at month 9. Nine of 71 cells analyzed were positive for vector-host junctions. This confirmed that the relapsed cells originated from a single blast clone.
The investigators also excluded other possible reasons for the loss of CD19, including mutations, splicing variants, and structural alteration of the B-cell receptor complex.
They found that expression of the CAR in cis on B-ALL blasts masked the CAR target epitope.
The investigators concluded that their results “provide a direct confirmation of the cancer stem cell hypothesis in humans, given that clonal analysis indicated that the relapse and subsequent death of the patient were attributed to the progeny of a single leukemic blast cell with extensive replicative capacity, both in culture and in vivo.”
They called for improved manufacturing technologies that can eliminate contamination by residual tumor cells from engineered T cells.
Interestingly, this case developed not long after a case that showed essentially the opposite situation—a patient with chronic lymphocytic leukemia went into remission because of a single CAR T cell that reproduced and fought off the disease.
Investigators report that a single leukemic cell unintentionally engineered into the chimeric antigen receptor (CAR) T-cell product can mask it from recognition and confer resistance to CAR T-cell therapy.
They described the case of a 20-year-old male who received the anti-CD19 CAR tisagenlecleucel (Kymriah) and relapsed at day 252 after the infusion.
The transduction of a leukemic cell during manufacture of the CAR T-cell product “is a rare event,” they wrote, and indicated that “this is the only case out of 369 patients reported worldwide at the time of publication.”
Lead author Marco Ruella, MD, of the University of Pennsylvania, and colleagues described the case in a Brief Communication published in Nature Medicine.
"In this case,” Dr. Ruella said, “we found that 100 percent of relapsed leukemic cells carried the CAR that we use to genetically modify T cells."
The patient had B-cell acute lymphoblastic leukemia (B-ALL) and relapsed three times after chemotherapy and a cord blood transplant before enrolling in the phase 1 trial of CTL019 (NCT 01626495).
The investigators reported that the infused CAR cells “displayed the typical pattern of in vivo engraftment and expansion.” At day 28 after the infusion, the patient was in complete remission.
But by day 252, he experienced a second expansion of CAR cells that did not correspond to the re-expansion of CAR+ T cells.
At day 261, the patient relapsed with more than 90% CD10+CD19- leukemic cells in the bone marrow and circulating blasts. The cells were CAR-transduced B-cell leukemia (CARB) cells.
The CARB cells continued to expand, and the patient died of progressive leukemia.
The investigators tracked the origin of the CARB cells by analyzing the relapsed CAR19+ cells using next-generation sequencing.
They hypothesized that the CAR19+ leukemia relapse occurred through lentiviral transduction during the manufacturing process, since they detected no replication-competent lentivirus when testing the patient’s peripheral blood at numerous time points after CTL019 infusion.
Further analysis confirmed the CARB cells were a byproduct made during CTL019 cell manufacturing.
To confirm that the leukemia relapse originated from a single clone, the investigators expanded in mice blast cells detected in the patient at month 9. Nine of 71 cells analyzed were positive for vector-host junctions. This confirmed that the relapsed cells originated from a single blast clone.
The investigators also excluded other possible reasons for the loss of CD19, including mutations, splicing variants, and structural alteration of the B-cell receptor complex.
They found that expression of the CAR in cis on B-ALL blasts masked the CAR target epitope.
The investigators concluded that their results “provide a direct confirmation of the cancer stem cell hypothesis in humans, given that clonal analysis indicated that the relapse and subsequent death of the patient were attributed to the progeny of a single leukemic blast cell with extensive replicative capacity, both in culture and in vivo.”
They called for improved manufacturing technologies that can eliminate contamination by residual tumor cells from engineered T cells.
Interestingly, this case developed not long after a case that showed essentially the opposite situation—a patient with chronic lymphocytic leukemia went into remission because of a single CAR T cell that reproduced and fought off the disease.
Investigators report that a single leukemic cell unintentionally engineered into the chimeric antigen receptor (CAR) T-cell product can mask it from recognition and confer resistance to CAR T-cell therapy.
They described the case of a 20-year-old male who received the anti-CD19 CAR tisagenlecleucel (Kymriah) and relapsed at day 252 after the infusion.
The transduction of a leukemic cell during manufacture of the CAR T-cell product “is a rare event,” they wrote, and indicated that “this is the only case out of 369 patients reported worldwide at the time of publication.”
Lead author Marco Ruella, MD, of the University of Pennsylvania, and colleagues described the case in a Brief Communication published in Nature Medicine.
"In this case,” Dr. Ruella said, “we found that 100 percent of relapsed leukemic cells carried the CAR that we use to genetically modify T cells."
The patient had B-cell acute lymphoblastic leukemia (B-ALL) and relapsed three times after chemotherapy and a cord blood transplant before enrolling in the phase 1 trial of CTL019 (NCT 01626495).
The investigators reported that the infused CAR cells “displayed the typical pattern of in vivo engraftment and expansion.” At day 28 after the infusion, the patient was in complete remission.
But by day 252, he experienced a second expansion of CAR cells that did not correspond to the re-expansion of CAR+ T cells.
At day 261, the patient relapsed with more than 90% CD10+CD19- leukemic cells in the bone marrow and circulating blasts. The cells were CAR-transduced B-cell leukemia (CARB) cells.
The CARB cells continued to expand, and the patient died of progressive leukemia.
The investigators tracked the origin of the CARB cells by analyzing the relapsed CAR19+ cells using next-generation sequencing.
They hypothesized that the CAR19+ leukemia relapse occurred through lentiviral transduction during the manufacturing process, since they detected no replication-competent lentivirus when testing the patient’s peripheral blood at numerous time points after CTL019 infusion.
Further analysis confirmed the CARB cells were a byproduct made during CTL019 cell manufacturing.
To confirm that the leukemia relapse originated from a single clone, the investigators expanded in mice blast cells detected in the patient at month 9. Nine of 71 cells analyzed were positive for vector-host junctions. This confirmed that the relapsed cells originated from a single blast clone.
The investigators also excluded other possible reasons for the loss of CD19, including mutations, splicing variants, and structural alteration of the B-cell receptor complex.
They found that expression of the CAR in cis on B-ALL blasts masked the CAR target epitope.
The investigators concluded that their results “provide a direct confirmation of the cancer stem cell hypothesis in humans, given that clonal analysis indicated that the relapse and subsequent death of the patient were attributed to the progeny of a single leukemic blast cell with extensive replicative capacity, both in culture and in vivo.”
They called for improved manufacturing technologies that can eliminate contamination by residual tumor cells from engineered T cells.
Interestingly, this case developed not long after a case that showed essentially the opposite situation—a patient with chronic lymphocytic leukemia went into remission because of a single CAR T cell that reproduced and fought off the disease.
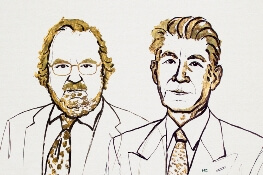
Two immunologists receive Nobel Prize in medicine
Two immunologists have been awarded the Nobel Prize in Physiology or Medicine for discoveries that represent a “paradigmatic shift in the fight against cancer,” the Nobel committee said.
James P. Allison, PhD, of MD Anderson Cancer Center, and Tasuku Honjo, MD, PhD, of Kyoto University, shared the prize for their discovery of cancer therapies that work by inhibiting negative immune regulation.
Dr. Allison studied the protein CTLA-4 found on T cells, which acts as a T-cell brake, and Dr. Honjo discovered a protein on immune cells called PD-1 that also acts as a T-cell brake.
In addition to sharing the honor, the scientists will split the 9 million Swedish kronor ($1.01 million) that comes with the prize.
Drs. Allison and Honjo, working in parallel, pursued different strategies for inhibiting the brakes on the immune system. Both strategies produced effective checkpoint inhibitors in the treatment of cancer.
James P. Allison
Dr. Allison was one of several scientists during the 1990s who noticed that CTLA-4 functions as a brake on T cells. Unlike other scientists, however, he set out to investigate whether blocking CTLA-4 with an antibody he had already developed could release the brake on the immune system.
The antibody had “spectacular” effects in curing mice with cancer. Despite little interest from the pharmaceutical industry, Dr. Allison continued efforts to develop the antibody therapy for humans.
The antibody turned out to be ipilimumab, which was approved in 2011 by the U.S. Food and Drug Administration (FDA) for the treatment of advanced melanoma.
Tasuko Honjo
A few years prior to Dr. Allison’s finding, Dr. Honjo discovered PD-1 and set out to determine its function. PD-1 also operates as a T-cell brake, but it uses a different mechanism than does CTLA-4.
Dr. Honjo and others demonstrated in animal experiments that PD-1 blockade could be an effective anticancer therapy. Over the years he demonstrated the efficacy of targeting PD-1 in different types of human cancers.
The first two PD-1 checkpoint inhibitors—pembrolizumab and nivolumab—were approved by the FDA in 2014 for the treatment of melanoma.
Nivolumab is also approved to treat classical Hodgkin lymphoma (HL), non-small cell lung cancer (NSCLC), small cell lung cancer, squamous cell carcinoma of the head and neck, colorectal cancer, hepatocellular carcinoma, renal cell carcinoma, urothelial carcinoma, and microsatellite instability-high or mismatch repair deficient colorectal cancer.
Pembrolizumab is also approved to treat primary mediastinal large B-cell lymphoma, advanced NSCLC, classical HL, advanced gastric cancer, advanced cervical cancer, head and neck squamous cell cancer, advanced urothelial bladder cancer, and microsatellite instability-high cancer.
And targeting both CTLA-4 and PD-1 in combination therapy together may prove to be even more effective in eliminating cancer cells than either strategy alone, as is being demonstrated in patients with melanoma.
The Nobel organization wrote in a press release, “Checkpoint therapy has now revolutionized cancer treatment and has fundamentally changed the way we view how cancer can be managed.”
Two immunologists have been awarded the Nobel Prize in Physiology or Medicine for discoveries that represent a “paradigmatic shift in the fight against cancer,” the Nobel committee said.
James P. Allison, PhD, of MD Anderson Cancer Center, and Tasuku Honjo, MD, PhD, of Kyoto University, shared the prize for their discovery of cancer therapies that work by inhibiting negative immune regulation.
Dr. Allison studied the protein CTLA-4 found on T cells, which acts as a T-cell brake, and Dr. Honjo discovered a protein on immune cells called PD-1 that also acts as a T-cell brake.
In addition to sharing the honor, the scientists will split the 9 million Swedish kronor ($1.01 million) that comes with the prize.
Drs. Allison and Honjo, working in parallel, pursued different strategies for inhibiting the brakes on the immune system. Both strategies produced effective checkpoint inhibitors in the treatment of cancer.
James P. Allison
Dr. Allison was one of several scientists during the 1990s who noticed that CTLA-4 functions as a brake on T cells. Unlike other scientists, however, he set out to investigate whether blocking CTLA-4 with an antibody he had already developed could release the brake on the immune system.
The antibody had “spectacular” effects in curing mice with cancer. Despite little interest from the pharmaceutical industry, Dr. Allison continued efforts to develop the antibody therapy for humans.
The antibody turned out to be ipilimumab, which was approved in 2011 by the U.S. Food and Drug Administration (FDA) for the treatment of advanced melanoma.
Tasuko Honjo
A few years prior to Dr. Allison’s finding, Dr. Honjo discovered PD-1 and set out to determine its function. PD-1 also operates as a T-cell brake, but it uses a different mechanism than does CTLA-4.
Dr. Honjo and others demonstrated in animal experiments that PD-1 blockade could be an effective anticancer therapy. Over the years he demonstrated the efficacy of targeting PD-1 in different types of human cancers.
The first two PD-1 checkpoint inhibitors—pembrolizumab and nivolumab—were approved by the FDA in 2014 for the treatment of melanoma.
Nivolumab is also approved to treat classical Hodgkin lymphoma (HL), non-small cell lung cancer (NSCLC), small cell lung cancer, squamous cell carcinoma of the head and neck, colorectal cancer, hepatocellular carcinoma, renal cell carcinoma, urothelial carcinoma, and microsatellite instability-high or mismatch repair deficient colorectal cancer.
Pembrolizumab is also approved to treat primary mediastinal large B-cell lymphoma, advanced NSCLC, classical HL, advanced gastric cancer, advanced cervical cancer, head and neck squamous cell cancer, advanced urothelial bladder cancer, and microsatellite instability-high cancer.
And targeting both CTLA-4 and PD-1 in combination therapy together may prove to be even more effective in eliminating cancer cells than either strategy alone, as is being demonstrated in patients with melanoma.
The Nobel organization wrote in a press release, “Checkpoint therapy has now revolutionized cancer treatment and has fundamentally changed the way we view how cancer can be managed.”
Two immunologists have been awarded the Nobel Prize in Physiology or Medicine for discoveries that represent a “paradigmatic shift in the fight against cancer,” the Nobel committee said.
James P. Allison, PhD, of MD Anderson Cancer Center, and Tasuku Honjo, MD, PhD, of Kyoto University, shared the prize for their discovery of cancer therapies that work by inhibiting negative immune regulation.
Dr. Allison studied the protein CTLA-4 found on T cells, which acts as a T-cell brake, and Dr. Honjo discovered a protein on immune cells called PD-1 that also acts as a T-cell brake.
In addition to sharing the honor, the scientists will split the 9 million Swedish kronor ($1.01 million) that comes with the prize.
Drs. Allison and Honjo, working in parallel, pursued different strategies for inhibiting the brakes on the immune system. Both strategies produced effective checkpoint inhibitors in the treatment of cancer.
James P. Allison
Dr. Allison was one of several scientists during the 1990s who noticed that CTLA-4 functions as a brake on T cells. Unlike other scientists, however, he set out to investigate whether blocking CTLA-4 with an antibody he had already developed could release the brake on the immune system.
The antibody had “spectacular” effects in curing mice with cancer. Despite little interest from the pharmaceutical industry, Dr. Allison continued efforts to develop the antibody therapy for humans.
The antibody turned out to be ipilimumab, which was approved in 2011 by the U.S. Food and Drug Administration (FDA) for the treatment of advanced melanoma.
Tasuko Honjo
A few years prior to Dr. Allison’s finding, Dr. Honjo discovered PD-1 and set out to determine its function. PD-1 also operates as a T-cell brake, but it uses a different mechanism than does CTLA-4.
Dr. Honjo and others demonstrated in animal experiments that PD-1 blockade could be an effective anticancer therapy. Over the years he demonstrated the efficacy of targeting PD-1 in different types of human cancers.
The first two PD-1 checkpoint inhibitors—pembrolizumab and nivolumab—were approved by the FDA in 2014 for the treatment of melanoma.
Nivolumab is also approved to treat classical Hodgkin lymphoma (HL), non-small cell lung cancer (NSCLC), small cell lung cancer, squamous cell carcinoma of the head and neck, colorectal cancer, hepatocellular carcinoma, renal cell carcinoma, urothelial carcinoma, and microsatellite instability-high or mismatch repair deficient colorectal cancer.
Pembrolizumab is also approved to treat primary mediastinal large B-cell lymphoma, advanced NSCLC, classical HL, advanced gastric cancer, advanced cervical cancer, head and neck squamous cell cancer, advanced urothelial bladder cancer, and microsatellite instability-high cancer.
And targeting both CTLA-4 and PD-1 in combination therapy together may prove to be even more effective in eliminating cancer cells than either strategy alone, as is being demonstrated in patients with melanoma.
The Nobel organization wrote in a press release, “Checkpoint therapy has now revolutionized cancer treatment and has fundamentally changed the way we view how cancer can be managed.”
First NGS assay approved for MRD detection in ALL or MM
The U.S. Food and Drug Administration has authorized the first next-generation sequencing (NGS)-based assay to be marketed for minimal residual disease (MRD) testing in patients with acute lymphoblastic leukemia (ALL) or multiple myeloma (MM).
The assay, called clonoSEQ®, uses both polymerase chain reaction (PCR) and NGS to identify and quantify gene sequences in DNA from patients’ bone marrow.
ClonoSEQ Assay can detect MRD levels below 1 in 1 million cells. By comparison flow cytometry assays or PCR-based assays are capable of measuring MRD down to 1 in 10,000 or 1 in 100,000 cells.
The clonoSEQ Assay is marketed by Adaptive Biotechnologies.
The FDA based its authorization on data from three clinical studies, one with 273 ALL patients, an ongoing study of 323 MM patients, and another MM trial with 706 patients.
Validation in ALL
As described in the clonoSEQ Assay Technical Information, a subset of 273 patients originally enrolled in the Children’s Oncology Group AALL0232 (NCT00075725) and AALL0331 (NCT00103285) studies had left-over bone marrow specimens to evaluate the performance of the clonoSEQ Assay.
MRD as determined by MRD negativity at less than 10-4 predicted improved event-free survival (EFS) irrespective of age. MRD-positive patients had a 2.74 higher event risk compared to MRD-negative patients.
Similar findings between MRD negativity and EFS in pediatric ALL using an earlier version of the assay were published in Blood.
Validation in MM
The ongoing phase 3 DFCI Study 10-106 (NCT01208662) is comparing conventional treatment with lenalidomide, bortezomib and dexamethasone to high-dose treatment with stem cell transplant as initial management of MM patients less than 65 years.
According to clonoSEQ’s technical information, bone marrow samples from 323 of the 720 patients originally enrolled were available and evaluable for MRD assessment.
ClonoSEQ measurements demonstrated that MRD status at a threshold of 10-5 significantly predicts progression-free survival (PFS) in all patients (P=0.027).
And samples from 75 patients who had achieved complete remission (CR) showed a modest association with disease-free survival (DFS) and lower MRD levels (P=0.064).
In the phase 3 ALCYONE trial, investigators randomly assigned 706 treatment-naïve MM patients ineligible for hematopoietic stem cell transplant to bortezomib, melphalan, and prednisone with or without daratumumab.
MRD assessments were made using the clonoSEQ Assay at screening, at confirmation of CR or stringent CR, and at intervals after patients achieved a CR.
Patients who did not achieve CR were considered MRD positive. The threshold for the MRD analysis was 10-5.
Investigators found that patients who were MRD negative by the clonoSEQ Assay had longer PFS compared to MRD-positive patients, regardless of treatment group.
For additional information on the clonoSEQ Assay consult the Technical Information available online.
The U.S. Food and Drug Administration has authorized the first next-generation sequencing (NGS)-based assay to be marketed for minimal residual disease (MRD) testing in patients with acute lymphoblastic leukemia (ALL) or multiple myeloma (MM).
The assay, called clonoSEQ®, uses both polymerase chain reaction (PCR) and NGS to identify and quantify gene sequences in DNA from patients’ bone marrow.
ClonoSEQ Assay can detect MRD levels below 1 in 1 million cells. By comparison flow cytometry assays or PCR-based assays are capable of measuring MRD down to 1 in 10,000 or 1 in 100,000 cells.
The clonoSEQ Assay is marketed by Adaptive Biotechnologies.
The FDA based its authorization on data from three clinical studies, one with 273 ALL patients, an ongoing study of 323 MM patients, and another MM trial with 706 patients.
Validation in ALL
As described in the clonoSEQ Assay Technical Information, a subset of 273 patients originally enrolled in the Children’s Oncology Group AALL0232 (NCT00075725) and AALL0331 (NCT00103285) studies had left-over bone marrow specimens to evaluate the performance of the clonoSEQ Assay.
MRD as determined by MRD negativity at less than 10-4 predicted improved event-free survival (EFS) irrespective of age. MRD-positive patients had a 2.74 higher event risk compared to MRD-negative patients.
Similar findings between MRD negativity and EFS in pediatric ALL using an earlier version of the assay were published in Blood.
Validation in MM
The ongoing phase 3 DFCI Study 10-106 (NCT01208662) is comparing conventional treatment with lenalidomide, bortezomib and dexamethasone to high-dose treatment with stem cell transplant as initial management of MM patients less than 65 years.
According to clonoSEQ’s technical information, bone marrow samples from 323 of the 720 patients originally enrolled were available and evaluable for MRD assessment.
ClonoSEQ measurements demonstrated that MRD status at a threshold of 10-5 significantly predicts progression-free survival (PFS) in all patients (P=0.027).
And samples from 75 patients who had achieved complete remission (CR) showed a modest association with disease-free survival (DFS) and lower MRD levels (P=0.064).
In the phase 3 ALCYONE trial, investigators randomly assigned 706 treatment-naïve MM patients ineligible for hematopoietic stem cell transplant to bortezomib, melphalan, and prednisone with or without daratumumab.
MRD assessments were made using the clonoSEQ Assay at screening, at confirmation of CR or stringent CR, and at intervals after patients achieved a CR.
Patients who did not achieve CR were considered MRD positive. The threshold for the MRD analysis was 10-5.
Investigators found that patients who were MRD negative by the clonoSEQ Assay had longer PFS compared to MRD-positive patients, regardless of treatment group.
For additional information on the clonoSEQ Assay consult the Technical Information available online.
The U.S. Food and Drug Administration has authorized the first next-generation sequencing (NGS)-based assay to be marketed for minimal residual disease (MRD) testing in patients with acute lymphoblastic leukemia (ALL) or multiple myeloma (MM).
The assay, called clonoSEQ®, uses both polymerase chain reaction (PCR) and NGS to identify and quantify gene sequences in DNA from patients’ bone marrow.
ClonoSEQ Assay can detect MRD levels below 1 in 1 million cells. By comparison flow cytometry assays or PCR-based assays are capable of measuring MRD down to 1 in 10,000 or 1 in 100,000 cells.
The clonoSEQ Assay is marketed by Adaptive Biotechnologies.
The FDA based its authorization on data from three clinical studies, one with 273 ALL patients, an ongoing study of 323 MM patients, and another MM trial with 706 patients.
Validation in ALL
As described in the clonoSEQ Assay Technical Information, a subset of 273 patients originally enrolled in the Children’s Oncology Group AALL0232 (NCT00075725) and AALL0331 (NCT00103285) studies had left-over bone marrow specimens to evaluate the performance of the clonoSEQ Assay.
MRD as determined by MRD negativity at less than 10-4 predicted improved event-free survival (EFS) irrespective of age. MRD-positive patients had a 2.74 higher event risk compared to MRD-negative patients.
Similar findings between MRD negativity and EFS in pediatric ALL using an earlier version of the assay were published in Blood.
Validation in MM
The ongoing phase 3 DFCI Study 10-106 (NCT01208662) is comparing conventional treatment with lenalidomide, bortezomib and dexamethasone to high-dose treatment with stem cell transplant as initial management of MM patients less than 65 years.
According to clonoSEQ’s technical information, bone marrow samples from 323 of the 720 patients originally enrolled were available and evaluable for MRD assessment.
ClonoSEQ measurements demonstrated that MRD status at a threshold of 10-5 significantly predicts progression-free survival (PFS) in all patients (P=0.027).
And samples from 75 patients who had achieved complete remission (CR) showed a modest association with disease-free survival (DFS) and lower MRD levels (P=0.064).
In the phase 3 ALCYONE trial, investigators randomly assigned 706 treatment-naïve MM patients ineligible for hematopoietic stem cell transplant to bortezomib, melphalan, and prednisone with or without daratumumab.
MRD assessments were made using the clonoSEQ Assay at screening, at confirmation of CR or stringent CR, and at intervals after patients achieved a CR.
Patients who did not achieve CR were considered MRD positive. The threshold for the MRD analysis was 10-5.
Investigators found that patients who were MRD negative by the clonoSEQ Assay had longer PFS compared to MRD-positive patients, regardless of treatment group.
For additional information on the clonoSEQ Assay consult the Technical Information available online.
Auto-FMT restores gut microbiota after HSCT
A randomized, controlled study of 25 patients has demonstrated that an autologous fecal microbiota transplant (auto-FMT) can restore beneficial gut bacteria depleted during allogeneic hematopoietic stem cell transplant (auto-HSCT), according to researchers.
Antibiotics given to prevent and treat bacterial infections during HSCT can also destroy patients’ beneficial intestinal bacteria, increasing their risk for infections and graft-versus-host disease.
The researchers reported that auto-FMT is a safe and effective way to help replenish the beneficial bacteria to near baseline levels within days.
Study patients receiving HSCT at Memorial Sloan Kettering Cancer Center (MSKCC) in New York provided fecal samples collected before transplant conditioning, which were frozen and stored before undergoing transplant.
Between 1 and 5 weeks, when physicians could confirm that patients’ stem cells had engrafted, they collected another fecal sample from patients and randomized the first 25 who lacked known beneficial bacteria to one of two groups.
Eleven control patients received standard of care without fecal transplant and 14 received auto-FMT by enema.
Researchers followed the subjects for 1 year after randomization, with fecal samples collected during this time.
Eleven of the 14 patients (79%) in the auto-FMT group recovered 75% or more of their initial good gut bacteria within days. This helped restore their digestive, immune, and other essential functions.
The beneficial microbial groups restored included Lachnospiraceae (family), Ruminococcaceae (family), and Bacteroidetes (phylum).
Patients in the standard care group took many weeks to replenish the beneficial bacteria destroyed during antibiotic treatment. Only 3 of 11 (27%) control patients had regained 75% or more of the microbiota in their initial fecal sample.
The investigators acknowledge a few study limitations, including that it was conducted at a single institution. Therefore, they say, the findings may not apply to patients undergoing allo-HSCT at other institutions.
In addition, auto-FMT patients may have been treated previously for cancer and depleted of some good bacteria as a result of prior antibiotic therapy.
Nevertheless, the investigators believe their study demonstrated the potential of auto-FMT as a clinical intervention, “thereby reversing the disruptive effects of broad-spectrum antibiotic treatment for patients undergoing allo-HSCT transplant,” they wrote.
Lead author Ying Taur, MD, MPH, of MSKCC, and colleagues published their paper in Science Translational Medicine.
The trial, supported in part by the National Institute of Allergy and Infectious Diseases (NIAID) of the National Institutes of Health, is ongoing and continues to accrue patients (NCT02269150).
“This important study suggests that clinical intervention using auto-FMT can safely reverse the disruptive effects of broad-spectrum antibiotic treatment,” said Anthony S. Fauci, MD, director of NIAID.
“If validated in larger studies, this approach may prove to be a relatively simple way to quickly restore a person’s healthy microbiome following intensive antimicrobial therapy.”
A randomized, controlled study of 25 patients has demonstrated that an autologous fecal microbiota transplant (auto-FMT) can restore beneficial gut bacteria depleted during allogeneic hematopoietic stem cell transplant (auto-HSCT), according to researchers.
Antibiotics given to prevent and treat bacterial infections during HSCT can also destroy patients’ beneficial intestinal bacteria, increasing their risk for infections and graft-versus-host disease.
The researchers reported that auto-FMT is a safe and effective way to help replenish the beneficial bacteria to near baseline levels within days.
Study patients receiving HSCT at Memorial Sloan Kettering Cancer Center (MSKCC) in New York provided fecal samples collected before transplant conditioning, which were frozen and stored before undergoing transplant.
Between 1 and 5 weeks, when physicians could confirm that patients’ stem cells had engrafted, they collected another fecal sample from patients and randomized the first 25 who lacked known beneficial bacteria to one of two groups.
Eleven control patients received standard of care without fecal transplant and 14 received auto-FMT by enema.
Researchers followed the subjects for 1 year after randomization, with fecal samples collected during this time.
Eleven of the 14 patients (79%) in the auto-FMT group recovered 75% or more of their initial good gut bacteria within days. This helped restore their digestive, immune, and other essential functions.
The beneficial microbial groups restored included Lachnospiraceae (family), Ruminococcaceae (family), and Bacteroidetes (phylum).
Patients in the standard care group took many weeks to replenish the beneficial bacteria destroyed during antibiotic treatment. Only 3 of 11 (27%) control patients had regained 75% or more of the microbiota in their initial fecal sample.
The investigators acknowledge a few study limitations, including that it was conducted at a single institution. Therefore, they say, the findings may not apply to patients undergoing allo-HSCT at other institutions.
In addition, auto-FMT patients may have been treated previously for cancer and depleted of some good bacteria as a result of prior antibiotic therapy.
Nevertheless, the investigators believe their study demonstrated the potential of auto-FMT as a clinical intervention, “thereby reversing the disruptive effects of broad-spectrum antibiotic treatment for patients undergoing allo-HSCT transplant,” they wrote.
Lead author Ying Taur, MD, MPH, of MSKCC, and colleagues published their paper in Science Translational Medicine.
The trial, supported in part by the National Institute of Allergy and Infectious Diseases (NIAID) of the National Institutes of Health, is ongoing and continues to accrue patients (NCT02269150).
“This important study suggests that clinical intervention using auto-FMT can safely reverse the disruptive effects of broad-spectrum antibiotic treatment,” said Anthony S. Fauci, MD, director of NIAID.
“If validated in larger studies, this approach may prove to be a relatively simple way to quickly restore a person’s healthy microbiome following intensive antimicrobial therapy.”
A randomized, controlled study of 25 patients has demonstrated that an autologous fecal microbiota transplant (auto-FMT) can restore beneficial gut bacteria depleted during allogeneic hematopoietic stem cell transplant (auto-HSCT), according to researchers.
Antibiotics given to prevent and treat bacterial infections during HSCT can also destroy patients’ beneficial intestinal bacteria, increasing their risk for infections and graft-versus-host disease.
The researchers reported that auto-FMT is a safe and effective way to help replenish the beneficial bacteria to near baseline levels within days.
Study patients receiving HSCT at Memorial Sloan Kettering Cancer Center (MSKCC) in New York provided fecal samples collected before transplant conditioning, which were frozen and stored before undergoing transplant.
Between 1 and 5 weeks, when physicians could confirm that patients’ stem cells had engrafted, they collected another fecal sample from patients and randomized the first 25 who lacked known beneficial bacteria to one of two groups.
Eleven control patients received standard of care without fecal transplant and 14 received auto-FMT by enema.
Researchers followed the subjects for 1 year after randomization, with fecal samples collected during this time.
Eleven of the 14 patients (79%) in the auto-FMT group recovered 75% or more of their initial good gut bacteria within days. This helped restore their digestive, immune, and other essential functions.
The beneficial microbial groups restored included Lachnospiraceae (family), Ruminococcaceae (family), and Bacteroidetes (phylum).
Patients in the standard care group took many weeks to replenish the beneficial bacteria destroyed during antibiotic treatment. Only 3 of 11 (27%) control patients had regained 75% or more of the microbiota in their initial fecal sample.
The investigators acknowledge a few study limitations, including that it was conducted at a single institution. Therefore, they say, the findings may not apply to patients undergoing allo-HSCT at other institutions.
In addition, auto-FMT patients may have been treated previously for cancer and depleted of some good bacteria as a result of prior antibiotic therapy.
Nevertheless, the investigators believe their study demonstrated the potential of auto-FMT as a clinical intervention, “thereby reversing the disruptive effects of broad-spectrum antibiotic treatment for patients undergoing allo-HSCT transplant,” they wrote.
Lead author Ying Taur, MD, MPH, of MSKCC, and colleagues published their paper in Science Translational Medicine.
The trial, supported in part by the National Institute of Allergy and Infectious Diseases (NIAID) of the National Institutes of Health, is ongoing and continues to accrue patients (NCT02269150).
“This important study suggests that clinical intervention using auto-FMT can safely reverse the disruptive effects of broad-spectrum antibiotic treatment,” said Anthony S. Fauci, MD, director of NIAID.
“If validated in larger studies, this approach may prove to be a relatively simple way to quickly restore a person’s healthy microbiome following intensive antimicrobial therapy.”