User login
Study supports sequencing in kids with cancer
SAN DIEGO—Comprehensive next-generation sequencing is both feasible and clinically useful in pediatric cancer patients, a new study suggests.
Researchers sequenced samples from 253 pediatric cancer patients and found that, in 79% of cases, there was at least one finding that could help guide care.
Scott Newman, PhD, of St. Jude Children’s Research Hospital in Memphis, Tennessee, presented these findings at the American Society of Human Genetics (ASHG) 2018 Annual Meeting (abstract 52).
The researchers conducted whole-genome, exome, and transcriptome sequencing of the patients’ tumors, as well as sequencing non-cancerous tissues from the same patients.
Of the 253 patients studied, 123 had hematologic malignancies.
The researchers found a mean of four pathogenic or likely pathogenic variants per patient (range, 0-18). This included prognostic (21.8%) and diagnostic (15.1%) variants as well as variants that could be targeted therapeutically (6.8%).
In all, 79% of the patients had at least one variant that was targetable, diagnostic, or prognostic. And test results were available within about 40 days, quickly enough that they could be used to guide care.
“With results available in a clinically relevant time frame, and pricing becoming increasingly comparable to the radiology and pathology tests, WGS [whole-genome sequencing] is becoming more accessible to pediatric oncology patients,” Dr. Newman said.
This work was part of the Genomes for Kids study (G4K), an effort to understand how best to use genetic data for pediatric cancer diagnosis and treatment. St. Jude has compiled the information from G4K into a publicly accessible online database.
The researchers have continued to perform sequencing on current patients, and, since the original study ended, have successfully used this method on roughly 300 additional patients. The team plans to continue studying sequencing methods in hopes of producing clinically applicable data more quickly.
G4K was sponsored by St. Jude.
SAN DIEGO—Comprehensive next-generation sequencing is both feasible and clinically useful in pediatric cancer patients, a new study suggests.
Researchers sequenced samples from 253 pediatric cancer patients and found that, in 79% of cases, there was at least one finding that could help guide care.
Scott Newman, PhD, of St. Jude Children’s Research Hospital in Memphis, Tennessee, presented these findings at the American Society of Human Genetics (ASHG) 2018 Annual Meeting (abstract 52).
The researchers conducted whole-genome, exome, and transcriptome sequencing of the patients’ tumors, as well as sequencing non-cancerous tissues from the same patients.
Of the 253 patients studied, 123 had hematologic malignancies.
The researchers found a mean of four pathogenic or likely pathogenic variants per patient (range, 0-18). This included prognostic (21.8%) and diagnostic (15.1%) variants as well as variants that could be targeted therapeutically (6.8%).
In all, 79% of the patients had at least one variant that was targetable, diagnostic, or prognostic. And test results were available within about 40 days, quickly enough that they could be used to guide care.
“With results available in a clinically relevant time frame, and pricing becoming increasingly comparable to the radiology and pathology tests, WGS [whole-genome sequencing] is becoming more accessible to pediatric oncology patients,” Dr. Newman said.
This work was part of the Genomes for Kids study (G4K), an effort to understand how best to use genetic data for pediatric cancer diagnosis and treatment. St. Jude has compiled the information from G4K into a publicly accessible online database.
The researchers have continued to perform sequencing on current patients, and, since the original study ended, have successfully used this method on roughly 300 additional patients. The team plans to continue studying sequencing methods in hopes of producing clinically applicable data more quickly.
G4K was sponsored by St. Jude.
SAN DIEGO—Comprehensive next-generation sequencing is both feasible and clinically useful in pediatric cancer patients, a new study suggests.
Researchers sequenced samples from 253 pediatric cancer patients and found that, in 79% of cases, there was at least one finding that could help guide care.
Scott Newman, PhD, of St. Jude Children’s Research Hospital in Memphis, Tennessee, presented these findings at the American Society of Human Genetics (ASHG) 2018 Annual Meeting (abstract 52).
The researchers conducted whole-genome, exome, and transcriptome sequencing of the patients’ tumors, as well as sequencing non-cancerous tissues from the same patients.
Of the 253 patients studied, 123 had hematologic malignancies.
The researchers found a mean of four pathogenic or likely pathogenic variants per patient (range, 0-18). This included prognostic (21.8%) and diagnostic (15.1%) variants as well as variants that could be targeted therapeutically (6.8%).
In all, 79% of the patients had at least one variant that was targetable, diagnostic, or prognostic. And test results were available within about 40 days, quickly enough that they could be used to guide care.
“With results available in a clinically relevant time frame, and pricing becoming increasingly comparable to the radiology and pathology tests, WGS [whole-genome sequencing] is becoming more accessible to pediatric oncology patients,” Dr. Newman said.
This work was part of the Genomes for Kids study (G4K), an effort to understand how best to use genetic data for pediatric cancer diagnosis and treatment. St. Jude has compiled the information from G4K into a publicly accessible online database.
The researchers have continued to perform sequencing on current patients, and, since the original study ended, have successfully used this method on roughly 300 additional patients. The team plans to continue studying sequencing methods in hopes of producing clinically applicable data more quickly.
G4K was sponsored by St. Jude.
‘Intense’ end-of-life care may be common in HSCT recipients
Patients who die within a year of allogeneic hematopoietic stem cell transplant (HSCT) tend to receive “medically intense” end-of-life care, an analysis suggests.
Researchers studied more than 2,000 patients who died within a year of allogeneic HSCT and found that a majority of the patients died in the hospital, and about half of them were admitted to the intensive care unit (ICU).
However, patient age, underlying diagnosis, and other factors influenced the likelihood of receiving intense end-of-life care.
For example, patients diagnosed with acute myeloid leukemia (AML) or myelodysplastic syndromes (MDS) were less likely than patients with acute lymphoblastic leukemia (ALL) to receive medically intense care.
Emily Johnston, MD, of the University of Alabama at Birmingham, and her colleagues reported these findings in the Journal of Clinical Oncology.
The researchers studied 2,135 patients in California who underwent inpatient HSCT and died within a year of the transplant (not as a result of peripartum events or trauma) between 2000 and 2013.
Fifty-three percent of the patients received some type of medically intense intervention, and 57% had at least two types of intense interventions.
Eighty-three percent of patients died in hospital, and 43% spent all of their last 30 days in the hospital.
Forty-nine percent of patients were admitted to the ICU, 45% were intubated, 22% underwent hemodialysis, and 8% received cardiopulmonary resuscitation.
Factors associated with intense care
The researchers said receipt of a medically intense intervention varied by age at death, underlying diagnosis, year of HSCT, location of care, and comorbidities. However, use of intense interventions did not vary according to sex, race/ethnicity, insurance type, or income.
Compared to patients age 60 and older, patients in the following age groups were more likely to receive medically intense interventions:
- Ages 15 to 21—odds ratio (OR)=2.6 (P<0.001)
- Ages 30 to 39—OR=1.8 (P<0.01)
- Ages 40 to 49—OR=1.4 (P<0.05).
Patients with comorbidities were more likely to receive intense interventions as well. The OR was 1.6 (P<0.01) for patients with one comorbidity and 2.5 (P<0.001) for patients with two or more comorbidities.
Patients with AML or MDS were less likely than patients with ALL to receive a medically intense intervention—OR=0.7 (P<0.05).
Patients who were transplanted between 2000 and 2004 were less likely to receive an intense intervention than patients transplanted between 2010 and 2013—OR=0.7 (P<0.01).
Patients who changed hospitals between HSCT and death were less likely to receive an intense intervention than patients who stayed at the same hospital. The OR was 0.3 if they transferred to a community hospital and 0.4 if they transferred to a specialty hospital (P<0.001 for both).
Patients living in rural areas were less likely than urban patients to receive a medically intense intervention—OR=0.6 (P<0.05).
“From our data, we understand there is a correlation with high-intensity end-of-life care in patients who die within one year after receiving a stem cell transplant, but we are still unsure if that was the care they wanted,” Dr. Johnston said.
“The findings suggest that, as oncologists, we need to start having end-of-life care conversations earlier with patients to determine if a high-intensity treatment plan is consistent with their goals or if a lower-intensity treatment plan is best. It’s not a one-size-fits-all approach in end-of-life care.”
This research was supported by Stanford University. One study author reported relationships with Corvus Pharmaceuticals, Shire Pharmaceuticals, and Adaptive Biotechnologies. All other authors reported no conflicts.
Patients who die within a year of allogeneic hematopoietic stem cell transplant (HSCT) tend to receive “medically intense” end-of-life care, an analysis suggests.
Researchers studied more than 2,000 patients who died within a year of allogeneic HSCT and found that a majority of the patients died in the hospital, and about half of them were admitted to the intensive care unit (ICU).
However, patient age, underlying diagnosis, and other factors influenced the likelihood of receiving intense end-of-life care.
For example, patients diagnosed with acute myeloid leukemia (AML) or myelodysplastic syndromes (MDS) were less likely than patients with acute lymphoblastic leukemia (ALL) to receive medically intense care.
Emily Johnston, MD, of the University of Alabama at Birmingham, and her colleagues reported these findings in the Journal of Clinical Oncology.
The researchers studied 2,135 patients in California who underwent inpatient HSCT and died within a year of the transplant (not as a result of peripartum events or trauma) between 2000 and 2013.
Fifty-three percent of the patients received some type of medically intense intervention, and 57% had at least two types of intense interventions.
Eighty-three percent of patients died in hospital, and 43% spent all of their last 30 days in the hospital.
Forty-nine percent of patients were admitted to the ICU, 45% were intubated, 22% underwent hemodialysis, and 8% received cardiopulmonary resuscitation.
Factors associated with intense care
The researchers said receipt of a medically intense intervention varied by age at death, underlying diagnosis, year of HSCT, location of care, and comorbidities. However, use of intense interventions did not vary according to sex, race/ethnicity, insurance type, or income.
Compared to patients age 60 and older, patients in the following age groups were more likely to receive medically intense interventions:
- Ages 15 to 21—odds ratio (OR)=2.6 (P<0.001)
- Ages 30 to 39—OR=1.8 (P<0.01)
- Ages 40 to 49—OR=1.4 (P<0.05).
Patients with comorbidities were more likely to receive intense interventions as well. The OR was 1.6 (P<0.01) for patients with one comorbidity and 2.5 (P<0.001) for patients with two or more comorbidities.
Patients with AML or MDS were less likely than patients with ALL to receive a medically intense intervention—OR=0.7 (P<0.05).
Patients who were transplanted between 2000 and 2004 were less likely to receive an intense intervention than patients transplanted between 2010 and 2013—OR=0.7 (P<0.01).
Patients who changed hospitals between HSCT and death were less likely to receive an intense intervention than patients who stayed at the same hospital. The OR was 0.3 if they transferred to a community hospital and 0.4 if they transferred to a specialty hospital (P<0.001 for both).
Patients living in rural areas were less likely than urban patients to receive a medically intense intervention—OR=0.6 (P<0.05).
“From our data, we understand there is a correlation with high-intensity end-of-life care in patients who die within one year after receiving a stem cell transplant, but we are still unsure if that was the care they wanted,” Dr. Johnston said.
“The findings suggest that, as oncologists, we need to start having end-of-life care conversations earlier with patients to determine if a high-intensity treatment plan is consistent with their goals or if a lower-intensity treatment plan is best. It’s not a one-size-fits-all approach in end-of-life care.”
This research was supported by Stanford University. One study author reported relationships with Corvus Pharmaceuticals, Shire Pharmaceuticals, and Adaptive Biotechnologies. All other authors reported no conflicts.
Patients who die within a year of allogeneic hematopoietic stem cell transplant (HSCT) tend to receive “medically intense” end-of-life care, an analysis suggests.
Researchers studied more than 2,000 patients who died within a year of allogeneic HSCT and found that a majority of the patients died in the hospital, and about half of them were admitted to the intensive care unit (ICU).
However, patient age, underlying diagnosis, and other factors influenced the likelihood of receiving intense end-of-life care.
For example, patients diagnosed with acute myeloid leukemia (AML) or myelodysplastic syndromes (MDS) were less likely than patients with acute lymphoblastic leukemia (ALL) to receive medically intense care.
Emily Johnston, MD, of the University of Alabama at Birmingham, and her colleagues reported these findings in the Journal of Clinical Oncology.
The researchers studied 2,135 patients in California who underwent inpatient HSCT and died within a year of the transplant (not as a result of peripartum events or trauma) between 2000 and 2013.
Fifty-three percent of the patients received some type of medically intense intervention, and 57% had at least two types of intense interventions.
Eighty-three percent of patients died in hospital, and 43% spent all of their last 30 days in the hospital.
Forty-nine percent of patients were admitted to the ICU, 45% were intubated, 22% underwent hemodialysis, and 8% received cardiopulmonary resuscitation.
Factors associated with intense care
The researchers said receipt of a medically intense intervention varied by age at death, underlying diagnosis, year of HSCT, location of care, and comorbidities. However, use of intense interventions did not vary according to sex, race/ethnicity, insurance type, or income.
Compared to patients age 60 and older, patients in the following age groups were more likely to receive medically intense interventions:
- Ages 15 to 21—odds ratio (OR)=2.6 (P<0.001)
- Ages 30 to 39—OR=1.8 (P<0.01)
- Ages 40 to 49—OR=1.4 (P<0.05).
Patients with comorbidities were more likely to receive intense interventions as well. The OR was 1.6 (P<0.01) for patients with one comorbidity and 2.5 (P<0.001) for patients with two or more comorbidities.
Patients with AML or MDS were less likely than patients with ALL to receive a medically intense intervention—OR=0.7 (P<0.05).
Patients who were transplanted between 2000 and 2004 were less likely to receive an intense intervention than patients transplanted between 2010 and 2013—OR=0.7 (P<0.01).
Patients who changed hospitals between HSCT and death were less likely to receive an intense intervention than patients who stayed at the same hospital. The OR was 0.3 if they transferred to a community hospital and 0.4 if they transferred to a specialty hospital (P<0.001 for both).
Patients living in rural areas were less likely than urban patients to receive a medically intense intervention—OR=0.6 (P<0.05).
“From our data, we understand there is a correlation with high-intensity end-of-life care in patients who die within one year after receiving a stem cell transplant, but we are still unsure if that was the care they wanted,” Dr. Johnston said.
“The findings suggest that, as oncologists, we need to start having end-of-life care conversations earlier with patients to determine if a high-intensity treatment plan is consistent with their goals or if a lower-intensity treatment plan is best. It’s not a one-size-fits-all approach in end-of-life care.”
This research was supported by Stanford University. One study author reported relationships with Corvus Pharmaceuticals, Shire Pharmaceuticals, and Adaptive Biotechnologies. All other authors reported no conflicts.
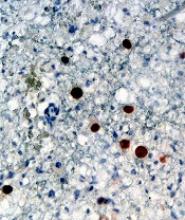
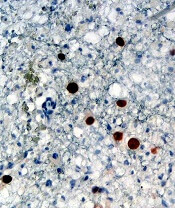
Adoptive T-cell therapy treats PML
Adoptive T-cell therapy has proven effective for treating progressive multifocal leukoencephalopathy (PML), according to research published in The New England Journal of Medicine.
Researchers observed substantial improvements in three PML patients infused with donor T cells targeting the BK virus.
Although one patient ultimately died, two had complete clearance of the JC virus and no clinical signs of PML after treatment.
“The JC and BK viruses are genetically similar and share proteins that can be targeted by the immune system,” said study author Katy Rezvani, MD, PhD, of The University of Texas MD Anderson Cancer Center in Houston.
“Because of these similarities, we hypothesized that T cells developed against BK virus may also be effective against JC virus infection.”
Dr. Rezvani’s team developed a novel approach for the generation of BK virus-specific T cells from healthy donors and established a bank of viral-specific T cells for immediate clinical use.
The researchers treated three patients with third-party, partially human leukocyte antigen (HLA)-matched, BK virus-specific T cells.
Patient 1 was a 32-year-old female with acute myeloid leukemia (AML) who previously received a double cord blood transplant.
Patient 2 was a 73-year-old female with JAK2-positive polycythemia rubra vera (PV) who had been treated with ruxolitinib.
Patient 3 was a 35-year-old man with AIDS who had discontinued highly active antiretroviral therapy due to side effects and who was no longer able to walk.
Following the first infusion, all three patients had a reduction in JC viral load in their cerebrospinal fluid. Viral loads dropped from:
- 700 to 78 copies in the AML patient
- 230,000 to 5,200 in the PV patient
- 4,300 to 1,300 in the AIDS patient.
“After infusion of viral-specific T cells, patients 1 and 3 had clinical improvement with significant reduction in JC virus in their cerebrospinal fluid,” Dr. Rezvani said.
“Both patients responded despite persistent T-cell immunodeficiency, supporting the concept that the response was mediated by the adoptively infused viral-specific T cells, and there were no infusion-related reactions.”
The AML patient received two additional infusions, which resulted in clearance of the virus in the cerebrospinal fluid and no signs of PML 27 months after the first infusion.
The PV patient received a second infusion that further reduced JC viral load, but no additional improvement was seen. The patient died 8 months after the first infusion.
The AIDS patient received additional infusions, resulting in complete clearance of the JC virus. This patient has regained mobility, and, 9 months after the first infusion, he is able to walk with a cane.
“We are encouraged that off-the-shelf, third-party, partially HLA-matched BK viral-specific T cells may provide a therapy for PML,” Dr. Rezvani said. “Further study in a larger group of patients is required to determine the success rate, durability, and longer-term adverse events with this treatment.”
This study was supported with funding from the Myelodysplastic Syndromes and Acute Myeloid Leukemia Moon Shot, part of MD Anderson’s Moon Shots Program, as well as the National Institutes of Health.
Adoptive T-cell therapy has proven effective for treating progressive multifocal leukoencephalopathy (PML), according to research published in The New England Journal of Medicine.
Researchers observed substantial improvements in three PML patients infused with donor T cells targeting the BK virus.
Although one patient ultimately died, two had complete clearance of the JC virus and no clinical signs of PML after treatment.
“The JC and BK viruses are genetically similar and share proteins that can be targeted by the immune system,” said study author Katy Rezvani, MD, PhD, of The University of Texas MD Anderson Cancer Center in Houston.
“Because of these similarities, we hypothesized that T cells developed against BK virus may also be effective against JC virus infection.”
Dr. Rezvani’s team developed a novel approach for the generation of BK virus-specific T cells from healthy donors and established a bank of viral-specific T cells for immediate clinical use.
The researchers treated three patients with third-party, partially human leukocyte antigen (HLA)-matched, BK virus-specific T cells.
Patient 1 was a 32-year-old female with acute myeloid leukemia (AML) who previously received a double cord blood transplant.
Patient 2 was a 73-year-old female with JAK2-positive polycythemia rubra vera (PV) who had been treated with ruxolitinib.
Patient 3 was a 35-year-old man with AIDS who had discontinued highly active antiretroviral therapy due to side effects and who was no longer able to walk.
Following the first infusion, all three patients had a reduction in JC viral load in their cerebrospinal fluid. Viral loads dropped from:
- 700 to 78 copies in the AML patient
- 230,000 to 5,200 in the PV patient
- 4,300 to 1,300 in the AIDS patient.
“After infusion of viral-specific T cells, patients 1 and 3 had clinical improvement with significant reduction in JC virus in their cerebrospinal fluid,” Dr. Rezvani said.
“Both patients responded despite persistent T-cell immunodeficiency, supporting the concept that the response was mediated by the adoptively infused viral-specific T cells, and there were no infusion-related reactions.”
The AML patient received two additional infusions, which resulted in clearance of the virus in the cerebrospinal fluid and no signs of PML 27 months after the first infusion.
The PV patient received a second infusion that further reduced JC viral load, but no additional improvement was seen. The patient died 8 months after the first infusion.
The AIDS patient received additional infusions, resulting in complete clearance of the JC virus. This patient has regained mobility, and, 9 months after the first infusion, he is able to walk with a cane.
“We are encouraged that off-the-shelf, third-party, partially HLA-matched BK viral-specific T cells may provide a therapy for PML,” Dr. Rezvani said. “Further study in a larger group of patients is required to determine the success rate, durability, and longer-term adverse events with this treatment.”
This study was supported with funding from the Myelodysplastic Syndromes and Acute Myeloid Leukemia Moon Shot, part of MD Anderson’s Moon Shots Program, as well as the National Institutes of Health.
Adoptive T-cell therapy has proven effective for treating progressive multifocal leukoencephalopathy (PML), according to research published in The New England Journal of Medicine.
Researchers observed substantial improvements in three PML patients infused with donor T cells targeting the BK virus.
Although one patient ultimately died, two had complete clearance of the JC virus and no clinical signs of PML after treatment.
“The JC and BK viruses are genetically similar and share proteins that can be targeted by the immune system,” said study author Katy Rezvani, MD, PhD, of The University of Texas MD Anderson Cancer Center in Houston.
“Because of these similarities, we hypothesized that T cells developed against BK virus may also be effective against JC virus infection.”
Dr. Rezvani’s team developed a novel approach for the generation of BK virus-specific T cells from healthy donors and established a bank of viral-specific T cells for immediate clinical use.
The researchers treated three patients with third-party, partially human leukocyte antigen (HLA)-matched, BK virus-specific T cells.
Patient 1 was a 32-year-old female with acute myeloid leukemia (AML) who previously received a double cord blood transplant.
Patient 2 was a 73-year-old female with JAK2-positive polycythemia rubra vera (PV) who had been treated with ruxolitinib.
Patient 3 was a 35-year-old man with AIDS who had discontinued highly active antiretroviral therapy due to side effects and who was no longer able to walk.
Following the first infusion, all three patients had a reduction in JC viral load in their cerebrospinal fluid. Viral loads dropped from:
- 700 to 78 copies in the AML patient
- 230,000 to 5,200 in the PV patient
- 4,300 to 1,300 in the AIDS patient.
“After infusion of viral-specific T cells, patients 1 and 3 had clinical improvement with significant reduction in JC virus in their cerebrospinal fluid,” Dr. Rezvani said.
“Both patients responded despite persistent T-cell immunodeficiency, supporting the concept that the response was mediated by the adoptively infused viral-specific T cells, and there were no infusion-related reactions.”
The AML patient received two additional infusions, which resulted in clearance of the virus in the cerebrospinal fluid and no signs of PML 27 months after the first infusion.
The PV patient received a second infusion that further reduced JC viral load, but no additional improvement was seen. The patient died 8 months after the first infusion.
The AIDS patient received additional infusions, resulting in complete clearance of the JC virus. This patient has regained mobility, and, 9 months after the first infusion, he is able to walk with a cane.
“We are encouraged that off-the-shelf, third-party, partially HLA-matched BK viral-specific T cells may provide a therapy for PML,” Dr. Rezvani said. “Further study in a larger group of patients is required to determine the success rate, durability, and longer-term adverse events with this treatment.”
This study was supported with funding from the Myelodysplastic Syndromes and Acute Myeloid Leukemia Moon Shot, part of MD Anderson’s Moon Shots Program, as well as the National Institutes of Health.
Dataset could reveal better therapies for AML
Researchers have released a dataset detailing the molecular makeup of tumor cells from more than 500 patients with acute myeloid leukemia (AML).
The team discovered mutations not previously observed in AML and found associations between mutations and responses to certain therapies.
For instance, AML cases with FLT3, NPM1, and DNMT3A mutations proved sensitive to the BTK inhibitor ibrutinib.
The researchers described their findings in Nature.
The team also made their dataset available via Vizome, an online data viewer. Other researchers can use Vizome to find out which targeted therapies might be most effective against specific subsets of AML cells.
“People can get online, search our database, and very quickly get answers to ‘Is this a good drug?’ or ‘Is there a patient population my drug can work in?’” said study author Brian Druker, MD, of Oregon Health & Science University (OHSU) in Portland, Oregon.
Newly identified mutations
For this study, part of the Beat AML initiative, Dr. Druker and his colleagues performed whole-exome and RNA sequencing on 672 samples from 562 AML patients.
The team identified mutations in 11 genes that were called in 1% or more of patients in this dataset but had not been observed in previous AML sequencing studies. The genes were:
- CUB and Sushi multiple domains 2 (CSMD2)
- NAC alpha domain containing (NACAD)
- Teneurin transmembrane protein 2 (TENM2)
- Aggrecan (ACAN)
- ADAM metallopeptidase with thrombospondin type 1 motif 7 (ADAMTS7)
- Immunoglobulin-like and fibronectin type III domain containing 1 (IGFN1)
- Neurobeachin-like 2 (NBEAL2)
- Poly(U) binding splicing factor 60 (PUF60)
- Zinc-finger protein 687 (ZNF687)
- Cadherin EGF LAG sevenpass G-type receptor 2 (CELSR2)
- Glutamate ionotropic receptor NMDA type subunit 2B (GRIN2B).
Testing therapies
The researchers also assessed how AML cells from 409 of the patient samples responded to each of 122 targeted therapies.
The team found that mutations in TP53, ASXL1, NRAS, and KRAS caused “a broad pattern of drug resistance.”
However, cases with TP53 mutations were sensitive to elesclomol (a drug that targets cancer cell metabolism), cases with ASXL1 mutations were sensitive to the HDAC inhibitor panobinostat, and cases with KRAS/NRAS mutations were sensitive to MAPK inhibitors (with NRAS-mutated cases demonstrating greater sensitivity).
The researchers also found that IDH2 mutations “conferred sensitivity to a broad spectrum of drugs,” but IDH1 mutations were associated with resistance to most drugs.
As previously mentioned, the researchers found a significant association between mutations in FLT3, NPM1, and DNMT3A and sensitivity to ibrutinib. However, the team found that cases with DNMT3A mutations alone or mutations in DNMT3A and FLT3 were not significantly different from cases with wild-type genes.
On the other hand, cases with FLT3-ITD alone or any combination with a mutation in NPM1 (including mutations in all three genes) were significantly more sensitive to ibrutinib than cases with wild-type genes.
Cases with FLT3-ITD and mutations in NPM1 were sensitive to another kinase inhibitor, entospletinib, as well.
The researchers also found that mutations in both BCOR and RUNX1 correlated with increased sensitivity to four JAK inhibitors—momelotinib, ruxolitinib, tofacitinib, and JAK inhibitor I.
However, cases with BCOR mutations alone or mutations in BCOR and DNMT3A or SRSF2 showed no difference in sensitivity to the JAK inhibitors from cases with wild-type genes.
Next steps
“We’re just starting to scratch the surface of what we can do when we analyze the data,” Dr. Druker said. “The real power comes when you start to integrate all that data. You can analyze what drug worked and why it worked.”
In fact, the researchers are already developing and initiating clinical trials to test hypotheses generated by this study.
“You can start to sense some momentum building with new, better therapeutics for AML patients, and, hopefully, this dataset will help fuel that momentum even further,” said study author Jeff Tyner, PhD, of the OHSU School of Medicine.
“We want to parlay this information into clinical trials as much as we can, and we also want the broader community to use this dataset to accelerate their own work.”
Funding for the current study was provided by grants from The Leukemia & Lymphoma Society, the National Cancer Institute, the National Library of Medicine, and other groups.
Researchers have released a dataset detailing the molecular makeup of tumor cells from more than 500 patients with acute myeloid leukemia (AML).
The team discovered mutations not previously observed in AML and found associations between mutations and responses to certain therapies.
For instance, AML cases with FLT3, NPM1, and DNMT3A mutations proved sensitive to the BTK inhibitor ibrutinib.
The researchers described their findings in Nature.
The team also made their dataset available via Vizome, an online data viewer. Other researchers can use Vizome to find out which targeted therapies might be most effective against specific subsets of AML cells.
“People can get online, search our database, and very quickly get answers to ‘Is this a good drug?’ or ‘Is there a patient population my drug can work in?’” said study author Brian Druker, MD, of Oregon Health & Science University (OHSU) in Portland, Oregon.
Newly identified mutations
For this study, part of the Beat AML initiative, Dr. Druker and his colleagues performed whole-exome and RNA sequencing on 672 samples from 562 AML patients.
The team identified mutations in 11 genes that were called in 1% or more of patients in this dataset but had not been observed in previous AML sequencing studies. The genes were:
- CUB and Sushi multiple domains 2 (CSMD2)
- NAC alpha domain containing (NACAD)
- Teneurin transmembrane protein 2 (TENM2)
- Aggrecan (ACAN)
- ADAM metallopeptidase with thrombospondin type 1 motif 7 (ADAMTS7)
- Immunoglobulin-like and fibronectin type III domain containing 1 (IGFN1)
- Neurobeachin-like 2 (NBEAL2)
- Poly(U) binding splicing factor 60 (PUF60)
- Zinc-finger protein 687 (ZNF687)
- Cadherin EGF LAG sevenpass G-type receptor 2 (CELSR2)
- Glutamate ionotropic receptor NMDA type subunit 2B (GRIN2B).
Testing therapies
The researchers also assessed how AML cells from 409 of the patient samples responded to each of 122 targeted therapies.
The team found that mutations in TP53, ASXL1, NRAS, and KRAS caused “a broad pattern of drug resistance.”
However, cases with TP53 mutations were sensitive to elesclomol (a drug that targets cancer cell metabolism), cases with ASXL1 mutations were sensitive to the HDAC inhibitor panobinostat, and cases with KRAS/NRAS mutations were sensitive to MAPK inhibitors (with NRAS-mutated cases demonstrating greater sensitivity).
The researchers also found that IDH2 mutations “conferred sensitivity to a broad spectrum of drugs,” but IDH1 mutations were associated with resistance to most drugs.
As previously mentioned, the researchers found a significant association between mutations in FLT3, NPM1, and DNMT3A and sensitivity to ibrutinib. However, the team found that cases with DNMT3A mutations alone or mutations in DNMT3A and FLT3 were not significantly different from cases with wild-type genes.
On the other hand, cases with FLT3-ITD alone or any combination with a mutation in NPM1 (including mutations in all three genes) were significantly more sensitive to ibrutinib than cases with wild-type genes.
Cases with FLT3-ITD and mutations in NPM1 were sensitive to another kinase inhibitor, entospletinib, as well.
The researchers also found that mutations in both BCOR and RUNX1 correlated with increased sensitivity to four JAK inhibitors—momelotinib, ruxolitinib, tofacitinib, and JAK inhibitor I.
However, cases with BCOR mutations alone or mutations in BCOR and DNMT3A or SRSF2 showed no difference in sensitivity to the JAK inhibitors from cases with wild-type genes.
Next steps
“We’re just starting to scratch the surface of what we can do when we analyze the data,” Dr. Druker said. “The real power comes when you start to integrate all that data. You can analyze what drug worked and why it worked.”
In fact, the researchers are already developing and initiating clinical trials to test hypotheses generated by this study.
“You can start to sense some momentum building with new, better therapeutics for AML patients, and, hopefully, this dataset will help fuel that momentum even further,” said study author Jeff Tyner, PhD, of the OHSU School of Medicine.
“We want to parlay this information into clinical trials as much as we can, and we also want the broader community to use this dataset to accelerate their own work.”
Funding for the current study was provided by grants from The Leukemia & Lymphoma Society, the National Cancer Institute, the National Library of Medicine, and other groups.
Researchers have released a dataset detailing the molecular makeup of tumor cells from more than 500 patients with acute myeloid leukemia (AML).
The team discovered mutations not previously observed in AML and found associations between mutations and responses to certain therapies.
For instance, AML cases with FLT3, NPM1, and DNMT3A mutations proved sensitive to the BTK inhibitor ibrutinib.
The researchers described their findings in Nature.
The team also made their dataset available via Vizome, an online data viewer. Other researchers can use Vizome to find out which targeted therapies might be most effective against specific subsets of AML cells.
“People can get online, search our database, and very quickly get answers to ‘Is this a good drug?’ or ‘Is there a patient population my drug can work in?’” said study author Brian Druker, MD, of Oregon Health & Science University (OHSU) in Portland, Oregon.
Newly identified mutations
For this study, part of the Beat AML initiative, Dr. Druker and his colleagues performed whole-exome and RNA sequencing on 672 samples from 562 AML patients.
The team identified mutations in 11 genes that were called in 1% or more of patients in this dataset but had not been observed in previous AML sequencing studies. The genes were:
- CUB and Sushi multiple domains 2 (CSMD2)
- NAC alpha domain containing (NACAD)
- Teneurin transmembrane protein 2 (TENM2)
- Aggrecan (ACAN)
- ADAM metallopeptidase with thrombospondin type 1 motif 7 (ADAMTS7)
- Immunoglobulin-like and fibronectin type III domain containing 1 (IGFN1)
- Neurobeachin-like 2 (NBEAL2)
- Poly(U) binding splicing factor 60 (PUF60)
- Zinc-finger protein 687 (ZNF687)
- Cadherin EGF LAG sevenpass G-type receptor 2 (CELSR2)
- Glutamate ionotropic receptor NMDA type subunit 2B (GRIN2B).
Testing therapies
The researchers also assessed how AML cells from 409 of the patient samples responded to each of 122 targeted therapies.
The team found that mutations in TP53, ASXL1, NRAS, and KRAS caused “a broad pattern of drug resistance.”
However, cases with TP53 mutations were sensitive to elesclomol (a drug that targets cancer cell metabolism), cases with ASXL1 mutations were sensitive to the HDAC inhibitor panobinostat, and cases with KRAS/NRAS mutations were sensitive to MAPK inhibitors (with NRAS-mutated cases demonstrating greater sensitivity).
The researchers also found that IDH2 mutations “conferred sensitivity to a broad spectrum of drugs,” but IDH1 mutations were associated with resistance to most drugs.
As previously mentioned, the researchers found a significant association between mutations in FLT3, NPM1, and DNMT3A and sensitivity to ibrutinib. However, the team found that cases with DNMT3A mutations alone or mutations in DNMT3A and FLT3 were not significantly different from cases with wild-type genes.
On the other hand, cases with FLT3-ITD alone or any combination with a mutation in NPM1 (including mutations in all three genes) were significantly more sensitive to ibrutinib than cases with wild-type genes.
Cases with FLT3-ITD and mutations in NPM1 were sensitive to another kinase inhibitor, entospletinib, as well.
The researchers also found that mutations in both BCOR and RUNX1 correlated with increased sensitivity to four JAK inhibitors—momelotinib, ruxolitinib, tofacitinib, and JAK inhibitor I.
However, cases with BCOR mutations alone or mutations in BCOR and DNMT3A or SRSF2 showed no difference in sensitivity to the JAK inhibitors from cases with wild-type genes.
Next steps
“We’re just starting to scratch the surface of what we can do when we analyze the data,” Dr. Druker said. “The real power comes when you start to integrate all that data. You can analyze what drug worked and why it worked.”
In fact, the researchers are already developing and initiating clinical trials to test hypotheses generated by this study.
“You can start to sense some momentum building with new, better therapeutics for AML patients, and, hopefully, this dataset will help fuel that momentum even further,” said study author Jeff Tyner, PhD, of the OHSU School of Medicine.
“We want to parlay this information into clinical trials as much as we can, and we also want the broader community to use this dataset to accelerate their own work.”
Funding for the current study was provided by grants from The Leukemia & Lymphoma Society, the National Cancer Institute, the National Library of Medicine, and other groups.
BTK inhibitor shows early promise for WM
NEW YORK—The BTK inhibitor zanubrutinib has demonstrated “robust activity” and “good tolerability” in patients with Waldenström’s macroglobulinemia (WM), according to an investigator.
In a phase 1 trial, zanubrutinib produced an overall response rate (ORR) of 92%, and the estimated 12-month progression-free survival (PFS) rate was 89%.
Most adverse events (AEs) in this trial were grade 1 or 2 in severity, although the incidence of serious AEs was 42%.
Constantine Tam, MD, of the Peter MacCallum Cancer Center in Victoria, Australia, presented these results at the 10th International Workshop on Waldenström’s Macroglobulinemia.
The trial is sponsored by BeiGene, Ltd., the company developing zanubrutinib.
The trial (NCT02343120) includes patients with WM and other B-cell malignancies. As of July 24, 2018, 77 patients with treatment-naïve or relapsed/refractory WM had been enrolled.
Seventy-three patients were evaluable for efficacy in this analysis, and the median follow-up time was 22.5 months (range, 4.1-43.9).
At the time of the data cutoff, 62 patients remained on study treatment. Four patients (3%) discontinued treatment due to disease progression, and one patient remains on treatment post-progression.
Efficacy
The median time to response was 85 days (range, 55-749).
The ORR was 92% (67/73), and the major response rate (MRR) was 82%. Forty-one percent of patients achieved a very good partial response (VGPR), defined as a greater than 90% reduction in baseline immunoglobulin M (IgM) levels and improvement of extramedullary disease by computed tomography.
The median IgM decreased from 32.7 g/L (range, 5.3-91.9) at baseline to 8.2 g/L (range, 0.3-57.8). The median hemoglobin increased from 8.85 g/dL (range, 6.3-9.8) to 13.4 g/dL (range, 7.7-17.0) among 32 patients with hemoglobin less than 10 g/dL at baseline.
MYD88 genotype was known in 63 patients. In the subset known to have the MYD88L265P mutation (n=54), the ORR was 94%, the MRR was 89%, and the VGPR rate was 46%.
In the nine patients known to have wild-type MYD88 (a genotype that, historically, has had sub-optimal response to BTK inhibition), the ORR was 89%, the MRR was 67%, and the VGPR rate was 22%.
The 12-month PFS was estimated to be 89%, and the median PFS had not been reached.
Safety
The most frequent AEs of any attribution were petechiae/purpura/contusion (43%), upper respiratory tract infection (42%), cough (17%), diarrhea (17%), constipation (16%), back pain (16%), and headache (16%).
Grade 3-4 AEs of any attribution reported in three or more patients included neutropenia (9%), anemia (7%), hypertension (5%), basal cell carcinoma (5%), renal and urinary disorders (4%), and pneumonia (4%).
Serious AEs were seen in 32 patients (42%). Events in five patients (7%) were considered possibly related to zanubrutinib treatment—febrile neutropenia, colitis, atrial fibrillation, hemothorax, and pneumonia.
Nine patients (12%) discontinued study treatment due to AEs, but all of these events were considered unrelated to treatment. The AEs (n=1 for each) included abdominal sepsis (fatal), gastric adenocarcinoma (fatal), septic shoulder, worsening bronchiectasis, scedosporium infection, prostate adenocarcinoma, metastatic neuroendocrine carcinoma, acute myeloid leukemia, and breast cancer.
Atrial fibrillation/flutter occurred in four patients (5%), and major hemorrhage was observed in two patients (3%).
“We are encouraged that additional data on zanubrutinib in patients with WM confirms the initially reported experience, with consistent demonstration of robust activity and good tolerability,” Dr. Tam said.
“We are hopeful that zanubrutinib, if approved, could potentially provide an important new treatment option to patients with WM and other hematologic malignancies.”
Dr. Tam reported financial relationships with BeiGene and other companies.
NEW YORK—The BTK inhibitor zanubrutinib has demonstrated “robust activity” and “good tolerability” in patients with Waldenström’s macroglobulinemia (WM), according to an investigator.
In a phase 1 trial, zanubrutinib produced an overall response rate (ORR) of 92%, and the estimated 12-month progression-free survival (PFS) rate was 89%.
Most adverse events (AEs) in this trial were grade 1 or 2 in severity, although the incidence of serious AEs was 42%.
Constantine Tam, MD, of the Peter MacCallum Cancer Center in Victoria, Australia, presented these results at the 10th International Workshop on Waldenström’s Macroglobulinemia.
The trial is sponsored by BeiGene, Ltd., the company developing zanubrutinib.
The trial (NCT02343120) includes patients with WM and other B-cell malignancies. As of July 24, 2018, 77 patients with treatment-naïve or relapsed/refractory WM had been enrolled.
Seventy-three patients were evaluable for efficacy in this analysis, and the median follow-up time was 22.5 months (range, 4.1-43.9).
At the time of the data cutoff, 62 patients remained on study treatment. Four patients (3%) discontinued treatment due to disease progression, and one patient remains on treatment post-progression.
Efficacy
The median time to response was 85 days (range, 55-749).
The ORR was 92% (67/73), and the major response rate (MRR) was 82%. Forty-one percent of patients achieved a very good partial response (VGPR), defined as a greater than 90% reduction in baseline immunoglobulin M (IgM) levels and improvement of extramedullary disease by computed tomography.
The median IgM decreased from 32.7 g/L (range, 5.3-91.9) at baseline to 8.2 g/L (range, 0.3-57.8). The median hemoglobin increased from 8.85 g/dL (range, 6.3-9.8) to 13.4 g/dL (range, 7.7-17.0) among 32 patients with hemoglobin less than 10 g/dL at baseline.
MYD88 genotype was known in 63 patients. In the subset known to have the MYD88L265P mutation (n=54), the ORR was 94%, the MRR was 89%, and the VGPR rate was 46%.
In the nine patients known to have wild-type MYD88 (a genotype that, historically, has had sub-optimal response to BTK inhibition), the ORR was 89%, the MRR was 67%, and the VGPR rate was 22%.
The 12-month PFS was estimated to be 89%, and the median PFS had not been reached.
Safety
The most frequent AEs of any attribution were petechiae/purpura/contusion (43%), upper respiratory tract infection (42%), cough (17%), diarrhea (17%), constipation (16%), back pain (16%), and headache (16%).
Grade 3-4 AEs of any attribution reported in three or more patients included neutropenia (9%), anemia (7%), hypertension (5%), basal cell carcinoma (5%), renal and urinary disorders (4%), and pneumonia (4%).
Serious AEs were seen in 32 patients (42%). Events in five patients (7%) were considered possibly related to zanubrutinib treatment—febrile neutropenia, colitis, atrial fibrillation, hemothorax, and pneumonia.
Nine patients (12%) discontinued study treatment due to AEs, but all of these events were considered unrelated to treatment. The AEs (n=1 for each) included abdominal sepsis (fatal), gastric adenocarcinoma (fatal), septic shoulder, worsening bronchiectasis, scedosporium infection, prostate adenocarcinoma, metastatic neuroendocrine carcinoma, acute myeloid leukemia, and breast cancer.
Atrial fibrillation/flutter occurred in four patients (5%), and major hemorrhage was observed in two patients (3%).
“We are encouraged that additional data on zanubrutinib in patients with WM confirms the initially reported experience, with consistent demonstration of robust activity and good tolerability,” Dr. Tam said.
“We are hopeful that zanubrutinib, if approved, could potentially provide an important new treatment option to patients with WM and other hematologic malignancies.”
Dr. Tam reported financial relationships with BeiGene and other companies.
NEW YORK—The BTK inhibitor zanubrutinib has demonstrated “robust activity” and “good tolerability” in patients with Waldenström’s macroglobulinemia (WM), according to an investigator.
In a phase 1 trial, zanubrutinib produced an overall response rate (ORR) of 92%, and the estimated 12-month progression-free survival (PFS) rate was 89%.
Most adverse events (AEs) in this trial were grade 1 or 2 in severity, although the incidence of serious AEs was 42%.
Constantine Tam, MD, of the Peter MacCallum Cancer Center in Victoria, Australia, presented these results at the 10th International Workshop on Waldenström’s Macroglobulinemia.
The trial is sponsored by BeiGene, Ltd., the company developing zanubrutinib.
The trial (NCT02343120) includes patients with WM and other B-cell malignancies. As of July 24, 2018, 77 patients with treatment-naïve or relapsed/refractory WM had been enrolled.
Seventy-three patients were evaluable for efficacy in this analysis, and the median follow-up time was 22.5 months (range, 4.1-43.9).
At the time of the data cutoff, 62 patients remained on study treatment. Four patients (3%) discontinued treatment due to disease progression, and one patient remains on treatment post-progression.
Efficacy
The median time to response was 85 days (range, 55-749).
The ORR was 92% (67/73), and the major response rate (MRR) was 82%. Forty-one percent of patients achieved a very good partial response (VGPR), defined as a greater than 90% reduction in baseline immunoglobulin M (IgM) levels and improvement of extramedullary disease by computed tomography.
The median IgM decreased from 32.7 g/L (range, 5.3-91.9) at baseline to 8.2 g/L (range, 0.3-57.8). The median hemoglobin increased from 8.85 g/dL (range, 6.3-9.8) to 13.4 g/dL (range, 7.7-17.0) among 32 patients with hemoglobin less than 10 g/dL at baseline.
MYD88 genotype was known in 63 patients. In the subset known to have the MYD88L265P mutation (n=54), the ORR was 94%, the MRR was 89%, and the VGPR rate was 46%.
In the nine patients known to have wild-type MYD88 (a genotype that, historically, has had sub-optimal response to BTK inhibition), the ORR was 89%, the MRR was 67%, and the VGPR rate was 22%.
The 12-month PFS was estimated to be 89%, and the median PFS had not been reached.
Safety
The most frequent AEs of any attribution were petechiae/purpura/contusion (43%), upper respiratory tract infection (42%), cough (17%), diarrhea (17%), constipation (16%), back pain (16%), and headache (16%).
Grade 3-4 AEs of any attribution reported in three or more patients included neutropenia (9%), anemia (7%), hypertension (5%), basal cell carcinoma (5%), renal and urinary disorders (4%), and pneumonia (4%).
Serious AEs were seen in 32 patients (42%). Events in five patients (7%) were considered possibly related to zanubrutinib treatment—febrile neutropenia, colitis, atrial fibrillation, hemothorax, and pneumonia.
Nine patients (12%) discontinued study treatment due to AEs, but all of these events were considered unrelated to treatment. The AEs (n=1 for each) included abdominal sepsis (fatal), gastric adenocarcinoma (fatal), septic shoulder, worsening bronchiectasis, scedosporium infection, prostate adenocarcinoma, metastatic neuroendocrine carcinoma, acute myeloid leukemia, and breast cancer.
Atrial fibrillation/flutter occurred in four patients (5%), and major hemorrhage was observed in two patients (3%).
“We are encouraged that additional data on zanubrutinib in patients with WM confirms the initially reported experience, with consistent demonstration of robust activity and good tolerability,” Dr. Tam said.
“We are hopeful that zanubrutinib, if approved, could potentially provide an important new treatment option to patients with WM and other hematologic malignancies.”
Dr. Tam reported financial relationships with BeiGene and other companies.
sNDA gets priority review for CLL/SLL
The U.S. Food and Drug Administration (FDA) has accepted for priority review a supplemental new drug application (sNDA) for ibrutinib (Imbruvica®).
With this sNDA, Pharmacyclics LLC (an AbbVie company) and Janssen Biotech, Inc., are seeking approval for ibrutinib in combination with obinutuzumab (Gazyva®) in previously untreated adults with chronic lymphocytic leukemia (CLL) or small lymphocytic lymphoma (SLL).
The FDA grants priority review to applications for products that may provide significant improvements in the treatment, diagnosis, or prevention of serious conditions.
The agency intends to take action on a priority review application within 6 months of receiving it rather than the standard 10 months.
Ibrutinib is already FDA-approved as monotherapy for adults with CLL/SLL (previously treated or untreated), with and without 17p deletion. Ibrutinib is also approved in combination with bendamustine and rituximab for adults with previously treated CLL/SLL.
Obinutuzumab is FDA-approved for use in combination with chlorambucil to treat previously untreated CLL.
The sNDA for ibrutinib in combination with obinutuzumab is based on results from the phase 3 iLLUMINATE trial (NCT02264574).
The trial is a comparison of ibrutinib plus obinutuzumab and chlorambucil plus obinutuzumab in patients with previously untreated CLL/SLL.
In May, AbbVie announced that the trial’s primary endpoint was met. Specifically, ibrutinib plus obinutuzumab was associated with significantly longer progression-free survival than chlorambucil plus obinutuzumab.
Data from the trial have not been released. Pharmacyclics and Janssen said they plan to present the data in a future publication or at a medical congress.
The U.S. Food and Drug Administration (FDA) has accepted for priority review a supplemental new drug application (sNDA) for ibrutinib (Imbruvica®).
With this sNDA, Pharmacyclics LLC (an AbbVie company) and Janssen Biotech, Inc., are seeking approval for ibrutinib in combination with obinutuzumab (Gazyva®) in previously untreated adults with chronic lymphocytic leukemia (CLL) or small lymphocytic lymphoma (SLL).
The FDA grants priority review to applications for products that may provide significant improvements in the treatment, diagnosis, or prevention of serious conditions.
The agency intends to take action on a priority review application within 6 months of receiving it rather than the standard 10 months.
Ibrutinib is already FDA-approved as monotherapy for adults with CLL/SLL (previously treated or untreated), with and without 17p deletion. Ibrutinib is also approved in combination with bendamustine and rituximab for adults with previously treated CLL/SLL.
Obinutuzumab is FDA-approved for use in combination with chlorambucil to treat previously untreated CLL.
The sNDA for ibrutinib in combination with obinutuzumab is based on results from the phase 3 iLLUMINATE trial (NCT02264574).
The trial is a comparison of ibrutinib plus obinutuzumab and chlorambucil plus obinutuzumab in patients with previously untreated CLL/SLL.
In May, AbbVie announced that the trial’s primary endpoint was met. Specifically, ibrutinib plus obinutuzumab was associated with significantly longer progression-free survival than chlorambucil plus obinutuzumab.
Data from the trial have not been released. Pharmacyclics and Janssen said they plan to present the data in a future publication or at a medical congress.
The U.S. Food and Drug Administration (FDA) has accepted for priority review a supplemental new drug application (sNDA) for ibrutinib (Imbruvica®).
With this sNDA, Pharmacyclics LLC (an AbbVie company) and Janssen Biotech, Inc., are seeking approval for ibrutinib in combination with obinutuzumab (Gazyva®) in previously untreated adults with chronic lymphocytic leukemia (CLL) or small lymphocytic lymphoma (SLL).
The FDA grants priority review to applications for products that may provide significant improvements in the treatment, diagnosis, or prevention of serious conditions.
The agency intends to take action on a priority review application within 6 months of receiving it rather than the standard 10 months.
Ibrutinib is already FDA-approved as monotherapy for adults with CLL/SLL (previously treated or untreated), with and without 17p deletion. Ibrutinib is also approved in combination with bendamustine and rituximab for adults with previously treated CLL/SLL.
Obinutuzumab is FDA-approved for use in combination with chlorambucil to treat previously untreated CLL.
The sNDA for ibrutinib in combination with obinutuzumab is based on results from the phase 3 iLLUMINATE trial (NCT02264574).
The trial is a comparison of ibrutinib plus obinutuzumab and chlorambucil plus obinutuzumab in patients with previously untreated CLL/SLL.
In May, AbbVie announced that the trial’s primary endpoint was met. Specifically, ibrutinib plus obinutuzumab was associated with significantly longer progression-free survival than chlorambucil plus obinutuzumab.
Data from the trial have not been released. Pharmacyclics and Janssen said they plan to present the data in a future publication or at a medical congress.
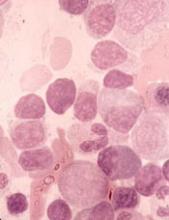
STRO-001 receives orphan designation for MM
The U.S. Food and Drug Administration (FDA) has granted orphan designation to STRO-001 for the treatment of multiple myeloma (MM).
STRO-001 is an antibody-drug conjugate targeting CD74, a protein highly expressed in MM and other B-cell malignancies.
Sutro Biopharma, Inc., is currently studying STRO-001 in a phase 1 trial enrolling separate dose-escalation cohorts for MM and B-cell lymphoma.
Preclinical research of STRO-001 in MM was presented at the 2017 ASH Annual Meeting.
Researchers examined bone marrow samples from MM patients and detected CD74 expression in 35 of the 36 samples, including specimens from patients who were treatment-naïve and patients who had been heavily pretreated with chemotherapy and stem cell transplant.
The researchers then found that STRO-001 demonstrated cytotoxicity in MM cell lines.
STRO-001 also reduced tumor burden in two disseminated xenograft models (ARP-1 and MM.1S) and prolonged survival in one of them (MM.1S).
About orphan designation
The FDA grants orphan designation to products intended to treat, diagnose, or prevent diseases/disorders that affect fewer than 200,000 people in the United States.
The designation provides incentives for sponsors to develop products for rare diseases. This may include tax credits toward the cost of clinical trials, prescription drug user fee waivers, and 7 years of market exclusivity if the product is approved.
The U.S. Food and Drug Administration (FDA) has granted orphan designation to STRO-001 for the treatment of multiple myeloma (MM).
STRO-001 is an antibody-drug conjugate targeting CD74, a protein highly expressed in MM and other B-cell malignancies.
Sutro Biopharma, Inc., is currently studying STRO-001 in a phase 1 trial enrolling separate dose-escalation cohorts for MM and B-cell lymphoma.
Preclinical research of STRO-001 in MM was presented at the 2017 ASH Annual Meeting.
Researchers examined bone marrow samples from MM patients and detected CD74 expression in 35 of the 36 samples, including specimens from patients who were treatment-naïve and patients who had been heavily pretreated with chemotherapy and stem cell transplant.
The researchers then found that STRO-001 demonstrated cytotoxicity in MM cell lines.
STRO-001 also reduced tumor burden in two disseminated xenograft models (ARP-1 and MM.1S) and prolonged survival in one of them (MM.1S).
About orphan designation
The FDA grants orphan designation to products intended to treat, diagnose, or prevent diseases/disorders that affect fewer than 200,000 people in the United States.
The designation provides incentives for sponsors to develop products for rare diseases. This may include tax credits toward the cost of clinical trials, prescription drug user fee waivers, and 7 years of market exclusivity if the product is approved.
The U.S. Food and Drug Administration (FDA) has granted orphan designation to STRO-001 for the treatment of multiple myeloma (MM).
STRO-001 is an antibody-drug conjugate targeting CD74, a protein highly expressed in MM and other B-cell malignancies.
Sutro Biopharma, Inc., is currently studying STRO-001 in a phase 1 trial enrolling separate dose-escalation cohorts for MM and B-cell lymphoma.
Preclinical research of STRO-001 in MM was presented at the 2017 ASH Annual Meeting.
Researchers examined bone marrow samples from MM patients and detected CD74 expression in 35 of the 36 samples, including specimens from patients who were treatment-naïve and patients who had been heavily pretreated with chemotherapy and stem cell transplant.
The researchers then found that STRO-001 demonstrated cytotoxicity in MM cell lines.
STRO-001 also reduced tumor burden in two disseminated xenograft models (ARP-1 and MM.1S) and prolonged survival in one of them (MM.1S).
About orphan designation
The FDA grants orphan designation to products intended to treat, diagnose, or prevent diseases/disorders that affect fewer than 200,000 people in the United States.
The designation provides incentives for sponsors to develop products for rare diseases. This may include tax credits toward the cost of clinical trials, prescription drug user fee waivers, and 7 years of market exclusivity if the product is approved.
FDA approves test to determine blood compatibility
The U.S. Food and Drug Administration (FDA) has approved ID CORE XT, a molecular-based assay used to determine blood donor and recipient compatibility.
ID CORE XT is a qualitative, polymerase chain reaction-based and hybridization-based genotyping test.
It is used for the simultaneous identification of multiple alleles encoding human erythrocyte antigens in genomic DNA extracted from whole blood specimens collected in ethylenediaminetetraacetic acid.
The test genotypes 29 polymorphisms determining 37 human erythrocyte antigen phenotypes of 10 blood group systems—Rh, Kell, Kidd, Duffy, MNS, Diego, Dombrock, Colton, Cartwright, and Lutheran.
ID CORE XT is the second molecular assay approved by the FDA for use in transfusion medicine and the first to report genotypes as final results.
The approval of ID CORE XT was granted to Progenika Biopharma S.A., a Grifols company.
According to Progenika, ID CORE XT will benefit patients who require ongoing transfusions, such as individuals with hemoglobinopathies.
ID CORE XT can also be used for cancer patients who require more thorough blood typing, patients with warm autoimmune hemolytic anemia, and patients taking daratumumab.
“The approval of the ID CORE XT test can streamline blood compatibility testing and provides an additional alternative to testing blood with antisera,” said Peter Marks, MD, PhD, director of the FDA’s Center for Biologics Evaluation and Research.
In a study published in Blood Transfusion this year, typing results with ID CORE XT were similar to results obtained with serology and molecular methods.
Researchers said there was 100% agreement between the positive results predicted by ID CORE XT and results obtained via serology (100% sensitivity).
For negative results, there was one discrepancy for E antigen (99.9% agreement) and 33 discrepancies for Fyb antigen (95.5% agreement). However, additional testing suggested that serology produced 34 false-negatives.
Both positive and negative results with ID CORE XT were in full agreement with results obtained via molecular methods (100% sensitivity and specificity).
The U.S. Food and Drug Administration (FDA) has approved ID CORE XT, a molecular-based assay used to determine blood donor and recipient compatibility.
ID CORE XT is a qualitative, polymerase chain reaction-based and hybridization-based genotyping test.
It is used for the simultaneous identification of multiple alleles encoding human erythrocyte antigens in genomic DNA extracted from whole blood specimens collected in ethylenediaminetetraacetic acid.
The test genotypes 29 polymorphisms determining 37 human erythrocyte antigen phenotypes of 10 blood group systems—Rh, Kell, Kidd, Duffy, MNS, Diego, Dombrock, Colton, Cartwright, and Lutheran.
ID CORE XT is the second molecular assay approved by the FDA for use in transfusion medicine and the first to report genotypes as final results.
The approval of ID CORE XT was granted to Progenika Biopharma S.A., a Grifols company.
According to Progenika, ID CORE XT will benefit patients who require ongoing transfusions, such as individuals with hemoglobinopathies.
ID CORE XT can also be used for cancer patients who require more thorough blood typing, patients with warm autoimmune hemolytic anemia, and patients taking daratumumab.
“The approval of the ID CORE XT test can streamline blood compatibility testing and provides an additional alternative to testing blood with antisera,” said Peter Marks, MD, PhD, director of the FDA’s Center for Biologics Evaluation and Research.
In a study published in Blood Transfusion this year, typing results with ID CORE XT were similar to results obtained with serology and molecular methods.
Researchers said there was 100% agreement between the positive results predicted by ID CORE XT and results obtained via serology (100% sensitivity).
For negative results, there was one discrepancy for E antigen (99.9% agreement) and 33 discrepancies for Fyb antigen (95.5% agreement). However, additional testing suggested that serology produced 34 false-negatives.
Both positive and negative results with ID CORE XT were in full agreement with results obtained via molecular methods (100% sensitivity and specificity).
The U.S. Food and Drug Administration (FDA) has approved ID CORE XT, a molecular-based assay used to determine blood donor and recipient compatibility.
ID CORE XT is a qualitative, polymerase chain reaction-based and hybridization-based genotyping test.
It is used for the simultaneous identification of multiple alleles encoding human erythrocyte antigens in genomic DNA extracted from whole blood specimens collected in ethylenediaminetetraacetic acid.
The test genotypes 29 polymorphisms determining 37 human erythrocyte antigen phenotypes of 10 blood group systems—Rh, Kell, Kidd, Duffy, MNS, Diego, Dombrock, Colton, Cartwright, and Lutheran.
ID CORE XT is the second molecular assay approved by the FDA for use in transfusion medicine and the first to report genotypes as final results.
The approval of ID CORE XT was granted to Progenika Biopharma S.A., a Grifols company.
According to Progenika, ID CORE XT will benefit patients who require ongoing transfusions, such as individuals with hemoglobinopathies.
ID CORE XT can also be used for cancer patients who require more thorough blood typing, patients with warm autoimmune hemolytic anemia, and patients taking daratumumab.
“The approval of the ID CORE XT test can streamline blood compatibility testing and provides an additional alternative to testing blood with antisera,” said Peter Marks, MD, PhD, director of the FDA’s Center for Biologics Evaluation and Research.
In a study published in Blood Transfusion this year, typing results with ID CORE XT were similar to results obtained with serology and molecular methods.
Researchers said there was 100% agreement between the positive results predicted by ID CORE XT and results obtained via serology (100% sensitivity).
For negative results, there was one discrepancy for E antigen (99.9% agreement) and 33 discrepancies for Fyb antigen (95.5% agreement). However, additional testing suggested that serology produced 34 false-negatives.
Both positive and negative results with ID CORE XT were in full agreement with results obtained via molecular methods (100% sensitivity and specificity).
Inhibitor receives orphan designation for PTCL
The U.S. Food and Drug Administration (FDA) has granted orphan drug designation to cerdulatinib for the treatment of peripheral T-cell lymphoma (PTCL).
Cerdulatinib is an oral Syk/JAK inhibitor being developed by Portola Pharmaceuticals, Inc.
Preclinical data have suggested an important role for Syk and JAK in PTCL tumor survival, and cerdulatinib is currently under evaluation in a phase 2a study of patients with PTCL and other non-Hodgkin lymphomas.
Results from this trial were presented at the 23rd Congress of the European Hematology Association (EHA) earlier this year.
At that time, the trial had enrolled 114 patients, 25 of them with PTCL. The patients received cerdulatinib at 25, 30, or 35 mg twice daily.
The objective response rate was 35% among the PTCL patients. All seven responders had a complete response, and 11 PTCL patients were still on cerdulatinib at the time of the presentation.
Grade 3 or higher adverse events observed in all evaluable patients included lipase increase (18%), neutropenia (17%), pneumonia/lung infection (11%), diarrhea (8%), fatigue (6%), amylase increase (5%), sepsis/septic shock (4%), hypertension (4%), anemia (4%), thrombocytopenia (4%), and hypophosphatemia (4%).
There were five deaths due to sepsis or septic shock (three of which were concomitant with pneumonia) that were considered related to cerdulatinib.
Three of the deaths occurred in patients with chronic lymphocytic leukemia, one in a patient with diffuse large B-cell lymphoma, and one in a patient with follicular lymphoma.
The deaths occurred early on in the trial, and researchers have since taken steps—dose reductions, monitoring, and antibiotic prophylaxis—to prevent additional deaths.
About orphan designation
The FDA grants orphan designation to products intended to treat, diagnose, or prevent diseases/disorders that affect fewer than 200,000 people in the United States.
The designation provides incentives for sponsors to develop products for rare diseases. This may include tax credits toward the cost of clinical trials, prescription drug user fee waivers, and 7 years of market exclusivity if the product is approved.
The U.S. Food and Drug Administration (FDA) has granted orphan drug designation to cerdulatinib for the treatment of peripheral T-cell lymphoma (PTCL).
Cerdulatinib is an oral Syk/JAK inhibitor being developed by Portola Pharmaceuticals, Inc.
Preclinical data have suggested an important role for Syk and JAK in PTCL tumor survival, and cerdulatinib is currently under evaluation in a phase 2a study of patients with PTCL and other non-Hodgkin lymphomas.
Results from this trial were presented at the 23rd Congress of the European Hematology Association (EHA) earlier this year.
At that time, the trial had enrolled 114 patients, 25 of them with PTCL. The patients received cerdulatinib at 25, 30, or 35 mg twice daily.
The objective response rate was 35% among the PTCL patients. All seven responders had a complete response, and 11 PTCL patients were still on cerdulatinib at the time of the presentation.
Grade 3 or higher adverse events observed in all evaluable patients included lipase increase (18%), neutropenia (17%), pneumonia/lung infection (11%), diarrhea (8%), fatigue (6%), amylase increase (5%), sepsis/septic shock (4%), hypertension (4%), anemia (4%), thrombocytopenia (4%), and hypophosphatemia (4%).
There were five deaths due to sepsis or septic shock (three of which were concomitant with pneumonia) that were considered related to cerdulatinib.
Three of the deaths occurred in patients with chronic lymphocytic leukemia, one in a patient with diffuse large B-cell lymphoma, and one in a patient with follicular lymphoma.
The deaths occurred early on in the trial, and researchers have since taken steps—dose reductions, monitoring, and antibiotic prophylaxis—to prevent additional deaths.
About orphan designation
The FDA grants orphan designation to products intended to treat, diagnose, or prevent diseases/disorders that affect fewer than 200,000 people in the United States.
The designation provides incentives for sponsors to develop products for rare diseases. This may include tax credits toward the cost of clinical trials, prescription drug user fee waivers, and 7 years of market exclusivity if the product is approved.
The U.S. Food and Drug Administration (FDA) has granted orphan drug designation to cerdulatinib for the treatment of peripheral T-cell lymphoma (PTCL).
Cerdulatinib is an oral Syk/JAK inhibitor being developed by Portola Pharmaceuticals, Inc.
Preclinical data have suggested an important role for Syk and JAK in PTCL tumor survival, and cerdulatinib is currently under evaluation in a phase 2a study of patients with PTCL and other non-Hodgkin lymphomas.
Results from this trial were presented at the 23rd Congress of the European Hematology Association (EHA) earlier this year.
At that time, the trial had enrolled 114 patients, 25 of them with PTCL. The patients received cerdulatinib at 25, 30, or 35 mg twice daily.
The objective response rate was 35% among the PTCL patients. All seven responders had a complete response, and 11 PTCL patients were still on cerdulatinib at the time of the presentation.
Grade 3 or higher adverse events observed in all evaluable patients included lipase increase (18%), neutropenia (17%), pneumonia/lung infection (11%), diarrhea (8%), fatigue (6%), amylase increase (5%), sepsis/septic shock (4%), hypertension (4%), anemia (4%), thrombocytopenia (4%), and hypophosphatemia (4%).
There were five deaths due to sepsis or septic shock (three of which were concomitant with pneumonia) that were considered related to cerdulatinib.
Three of the deaths occurred in patients with chronic lymphocytic leukemia, one in a patient with diffuse large B-cell lymphoma, and one in a patient with follicular lymphoma.
The deaths occurred early on in the trial, and researchers have since taken steps—dose reductions, monitoring, and antibiotic prophylaxis—to prevent additional deaths.
About orphan designation
The FDA grants orphan designation to products intended to treat, diagnose, or prevent diseases/disorders that affect fewer than 200,000 people in the United States.
The designation provides incentives for sponsors to develop products for rare diseases. This may include tax credits toward the cost of clinical trials, prescription drug user fee waivers, and 7 years of market exclusivity if the product is approved.
Phase 1 NHL, ALL trials placed on clinical hold
Update: On October 12, 2018, Affimed N.V. received a notification from the U.S. Food and Drug Administration (FDA) saying the agency concurred with Affimed’s decision and formally placed the investigational new drug application for AFM11 on full clinical hold. Affimed said it will comply with the FDA and other global health authorities’ requests for information to resolve the clinical hold.
Affimed N.V. has placed trials of AFM11 on clinical hold and notified the global health authorities of its decision.
AFM11 is a CD19/CD3-targeting T-cell engager being evaluated in two phase 1 trials—one in patients with relapsed or refractory, CD19-positive B-cell non-Hodgkin lymphoma (NHL) and one in adults with relapsed or refractory B-precursor acute lymphoblastic leukemia (ALL).
Affimed initiated the clinical hold on these trials after serious adverse events occurred in three patients treated with AFM11.
This included a death in the ALL study and two life-threatening events in the NHL study.
The serious adverse events occurred in patients enrolled in the highest dose cohorts of each study.
A total of 33 patients have been treated in the two studies (NCT02848911 and NCT02106091), and preliminary signs of clinical activity have been observed in several patients.
Affimed said it will be working closely with the global health authorities, safety monitoring committees, and the studies’ clinical investigators to review the adverse events, assess all the data, and determine next steps for the AFM11 program.
Affimed intends to provide an update on AFM11 upon completing the evaluation.
Update: On October 12, 2018, Affimed N.V. received a notification from the U.S. Food and Drug Administration (FDA) saying the agency concurred with Affimed’s decision and formally placed the investigational new drug application for AFM11 on full clinical hold. Affimed said it will comply with the FDA and other global health authorities’ requests for information to resolve the clinical hold.
Affimed N.V. has placed trials of AFM11 on clinical hold and notified the global health authorities of its decision.
AFM11 is a CD19/CD3-targeting T-cell engager being evaluated in two phase 1 trials—one in patients with relapsed or refractory, CD19-positive B-cell non-Hodgkin lymphoma (NHL) and one in adults with relapsed or refractory B-precursor acute lymphoblastic leukemia (ALL).
Affimed initiated the clinical hold on these trials after serious adverse events occurred in three patients treated with AFM11.
This included a death in the ALL study and two life-threatening events in the NHL study.
The serious adverse events occurred in patients enrolled in the highest dose cohorts of each study.
A total of 33 patients have been treated in the two studies (NCT02848911 and NCT02106091), and preliminary signs of clinical activity have been observed in several patients.
Affimed said it will be working closely with the global health authorities, safety monitoring committees, and the studies’ clinical investigators to review the adverse events, assess all the data, and determine next steps for the AFM11 program.
Affimed intends to provide an update on AFM11 upon completing the evaluation.
Update: On October 12, 2018, Affimed N.V. received a notification from the U.S. Food and Drug Administration (FDA) saying the agency concurred with Affimed’s decision and formally placed the investigational new drug application for AFM11 on full clinical hold. Affimed said it will comply with the FDA and other global health authorities’ requests for information to resolve the clinical hold.
Affimed N.V. has placed trials of AFM11 on clinical hold and notified the global health authorities of its decision.
AFM11 is a CD19/CD3-targeting T-cell engager being evaluated in two phase 1 trials—one in patients with relapsed or refractory, CD19-positive B-cell non-Hodgkin lymphoma (NHL) and one in adults with relapsed or refractory B-precursor acute lymphoblastic leukemia (ALL).
Affimed initiated the clinical hold on these trials after serious adverse events occurred in three patients treated with AFM11.
This included a death in the ALL study and two life-threatening events in the NHL study.
The serious adverse events occurred in patients enrolled in the highest dose cohorts of each study.
A total of 33 patients have been treated in the two studies (NCT02848911 and NCT02106091), and preliminary signs of clinical activity have been observed in several patients.
Affimed said it will be working closely with the global health authorities, safety monitoring committees, and the studies’ clinical investigators to review the adverse events, assess all the data, and determine next steps for the AFM11 program.
Affimed intends to provide an update on AFM11 upon completing the evaluation.