User login
The Role of Hospital Medicine in Emergency Preparedness: A Framework for Hospitalist Leadership in Disaster Preparedness, Response, and Recovery
Recent events, domestically and globally, have highlighted the numerous complex challenges that disasters and mass casualty incidents (MCIs) impose on hospitals. Mass casualty events result from natural phenomena (eg, hurricanes, tornadoes, and wildfires), accidents (eg, plane crashes, building collapses, and toxic waste spills), or man-made crises (eg, terrorism).1-4 These events feature the potential to cause an acute surge of patients, which can overwhelm available hospital resources and personnel. Mass effect incidents are sustained crises, which often occur due to loss of infrastructure, epidemic infectious diseases, or need for hospital evacuations, and can completely overtax local and regional resources, thus requiring federal and state coordination.5
Hospital disaster response plans have traditionally centered on responses by the emergency department (ED) and associated surgical services to mass trauma-type events, without commensurate involvement of other hospital departments in either incident management operations or the planning process for mass effect incidents.6,7 In particular, the role of hospitalists in the leadership structure of various hospital disaster command structures remains undefined.8 However, recent disasters suggest that hospitalist involvement will highly benefit hospital emergency preparedness.9 Hospitalists possess specialized expertise in patient triage and disposition; medical comanagement with surgical services; coordination of complex medical care (usually with continuous 24/7 in-house coverage); integration with the full spectrum of affiliated services, such as case management or patient rehabilitation; and quality improvement research.10-12 At our institution, hospitalists are involved in the direct care of over 60% of the patients admitted across all medical and surgical services. Thus, we believe that hospitalists are uniquely qualified to offer leadership in disaster preparation, response, and recovery if integrated into hospitals’ incident command architectures. For example, although numerous acute patient surges are due to trauma MCIs, hospitalists may nevertheless act as the primary care providers in disasters that are medical in nature or that require rapid hospital evacuation and patient transfer (Table 1).
Although truly large-scale disasters are uncommon, several recent incidents exemplify scenarios with remarkably extreme acute patient surges (defined as >20% of normal patient volumes), which completely overwhelm a hospital’s capacity to maintain normal operations and require response from all available medical personnel, ideally in a preplanned and organized manner.13 The Las Vegas shooting on October 1, 2017, for example, resulted in 546 trauma victims, inundating two local hospitals and one regional facility.14,15 In another case, the deadliest tornado in modern US history struck Joplin, Missouri on May 22, 2011, destroying one of the two hospitals in the city and leaving an estimated 1,371 people injured, many of whom were presented to the one remaining area hospital.16 One of our team members (J.P.), a storm chaser from out-of-town, reported to the remaining functioning hospital and oversaw an impromptu hospital unit that received patients from the damaged hospital, ultimately caring for approximately 40 patients with a combination of medical and surgical issues from presentation through eventual disposition or transfer to outlying hospitals.17 Such incidents illustrate that during trauma events, hospitalists play critical roles for continuity of care for hospitalized disaster victims.
Therefore, we propose a means for incorporating hospitalists into the coordinated hospital disaster response effort, first by providing hospitalists with an overview of disaster management principles to allow their engagement with hospitals’ disaster management system with working fluency and second, by proposing a framework for hospitalist involvement in hospital emergency response. These recommendations stem from our experience and from similar recommendations from a number of evidence-based articles on intensive care medicine, disaster preparedness, and emergency medicine literature cited in this article. To our knowledge, no evidence-based literature discusses hospital medicine or internal medicine specific to emergency preparedness. We aim to change such condition with this article.
KEY PRINCIPLES OF INCIDENT MANAGEMENT AND PREPAREDNESS: A PRIMER FOR HOSPITALISTS
Effective participation in disaster response and planning requires a basic understanding of the organizational structures for incident management.18,19 Overall disaster response within the United States is guided by the National Response Framework, a national-level strategy that directs coordination between military and civilian response efforts, the latter of which are structured by the National Incident Management System (NIMS).20 NIMS organizes emergency management across all government levels (federal, state, and local) and the private sector under a common operational language and command structure. Both systems grew out of analyses of the September 11, 2001 attacks and Hurricane Katrina, indicating the need for a wider systemic organization to response efforts.1 State-level efforts are designed to mobilize resources to assist in community-level operations. Incident management always falls to the local authorities. At this local level, discrete hospitals often take part in healthcare coalitions that act in conjunction with other health entities, local public health departments, and emergency medical services, forming a multiagency coordination system.5 This healthcare coalition (emergency support function #8 health and medical), in support of emergency managers of city and county governments, forms the core of the medical response. One commonality to all emergency management is the concept of an “all-hazards” approach, which aims to develop a broad and flexible strategy for efficient management of nearly any type of incident. This “all-hazards” approach allows effective management through each of the four phases of incident management: preparation, response, recovery, and ongoing mitigation.
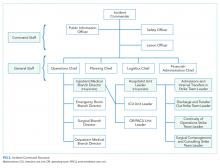
Direct supervision over incident management is achieved through an Incident Command System (ICS), a hierarchical organization of positions involved in response. The top supervisory structure of ICS (Incident Command and General Staff) is the same regardless of the locale in which it operates, allowing coherent interoperability with other agencies. Incidents of any size are managed with a scalable approach; subordinate ICS positions, which are tailored according to specific needs, can be activated as needed. Healthcare implementation of the ICS structure led to the development of the Hospital Incident Command System (HICS), which now serves as the national standard for hospital-based incident management and facilitates the capacity of individual hospitals to coordinate with other resources regionally and is a part of NIMS for emergency response (Figure 1).21 The success of HICS-led regulatory agencies (namely the Centers for Medicare and Medicaid Services and the Joint Commission) to require ICS/HICS in-hospital incident response plans.22 The most recent HICS (Version V) excludes physician involvement in the overall management chart. However, we demonstrate how the inherent flexibility in ICS can adapt to involve hospitalists. Although HICS serves as a backbone that requires institutionally specific modifications, other institutions, such as ours, commonly have entire branches or positions renamed, reapportioned, or created to fill their specific needs. Specialized training in ICS, NIMS, and other aspects of hospital emergency response is beyond the scope of this article but is available for free through the Department of Homeland Security and FEMA.23
Perhaps, the defining feature of ICS/HICS is its expandability, allowing the response efforts to be scaled and tailored in size, scope, and complexity of that of the incident.24 At the same time, the principles of span of control and unity of command promote efficient command structure by mandating each participant within the disaster response process to report to only one superior, whereas these superiors are limited to a manageable number of subordinates. For example, in Figure 2, all Strike Team Leaders
PROPOSED FRAMEWORK FOR HOSPITALIST INVOLVEMENT
Although incidents vary in terms of their severity, acuity of onset, duration, and composition of patients, a defining feature of MCIs is the rapid surge of patients with acute needs. Many MCIs are easily absorbed by local facilities. However, smaller hospitals or hospitals receiving patients from larger-scale incidents may become overwhelmed, in which larger incidents may result in an acute surge of over 20% of hospital capacity.13 Moreover, hospital surge capabilities have markedly diminished over the past decade due to overcrowding of emergency rooms, in part by admitted patients occupying the room space within the ED (“boarding”), further decreasing the hospitals’ capacities to accept new patients.25
Our proposed framework for hospitalist involvement in MCI disaster response focuses on such a situation, with emphasis on augmentation of hospital surge capacity and facilitation of patient throughput and discharge. Notably, these goals are modified from the standard HICS architecture (Figures 1-2 and Table 2). In this framework, hospitalists can play a critical role in decompressing the emergency room through admitting medical patients as rapidly as possible (even if preliminary workup is still pending), facilitating rapid discharge of patients to allow newer admissions to reach the floor, and prioritizing patients that could be transferred to other facilities or services and thus opening additional beds for admission (eg, accepting patients from the ICU or surgical floors to increase capacities on those services). Additionally, hospitalists can comanage surgical patients while surgeons are operating, assist intensivists with medical issues, and facilitate care of patients with minor injuries.
Using the HICS framework, each of those domains would be handled by a Strike Team led by one Team Leader whose goal is to operationalize various assets into a cohesive team specializing in those goals. Table 2 summarizes these goals, as presented in the context of patient examples.
To keep up with the ICS fundamentals, Hospitalist Unit Leaders may address a large MCI with all four strike teams or may only activate the strike teams needed for a less intensive MCI. For example, a bombing may result in a patient surge of 30% more than normal operations and thus demand a full response that includes all the strike teams noted above. By contrast, a bus accident with 20 injured patients may only require a Hospitalist Unit Leader to activate the “Admissions and Internal Transfers In” Strike Team to help offload a busy emergency room.
HOSPITALIST LEADERSHIP IN HOSPITAL EMERGENCY OPERATION PLAN DEVELOPMENT
Emergency management is comprised of four phases: preparation, response, recovery, and mitigation. The latter two phases are beyond the scope of this paper. Although most of our review has focused on modeling disaster response, hospitalist leadership remains critical in preparing for disasters. A disaster often psychologically overwhelms care providers, who feel compelled to help but are uncertain where to begin. To aid the members of a disaster response team, a state-of-the-art hospitalist group creates Job Action Sheets (JASs) for each position in their HICS organizational chart; these sheets codify how to respond and what roles are needed. These formal, protocolized sheets provide individuals assigned to these positions a description of their roles and responsibilities, including to whom they report and over whom they supervise, and include detailed checklists to aid in reaching critical milestones during the response phase. For example, the “Surgical Comanagement and Consulting” Strike Team Leader JAS would likely include the expectations of surgeons for assisting in patient management (ie, auto-consulting on all postoperative patients) and whether nursing phone calls on surgical patients would be temporarily routed to the Strike Team during periods of OR surge.
Hospitalists are well suited as leaders in disaster preparation given their ability to coordinate care among a large spectrum of stakeholders. For example, case managers and social workers are essential members of a well-structured Discharge Strike Team. Their input is critical to ensure that disaster tactics – such as care coordination contracts with local skilled nursing facilities willing to expedite discharge in emergencies to their facilities – are in-place before a real MCI. During Hurricane Sandy, mass evacuation of affected hospitals was effective through the Healthcare Facility Evacuation Center (a healthcare coalition of the New York Hospital Association) but nevertheless plagued with issues regarding situational awareness, poor communication between facilities, and difficulty bundling patients with medical records to receiving facilities – items which can be identified, anticipated, and thoroughly vetted by hospitalists well in advance of a real-world evacuation.26, 27
As the Joint Commission mandates regular exercises of the emergency plan, protocols must be drilled regularly to uncover deficiencies and areas for improvement.18 The most common failure patterns in Emergency Operation Plans (EOPs) include unrealistic and ineffective expectations and poor communication between different personnel and groups, resulting in confusion and obfuscation.28-30 Therefore, EOPs need to be both comprehensive and realistic – characteristics that can only be tested through repeated drills. These characteristics can be tested during tabletop exercises, where hospitalists assume the role of a part of the ICS structure and with JAS in hand, attempt to reason how to respond to a given scenario.31 Our experience is that small-scale drills conducted more frequently than the bare minimum mandated by the Joint Commission are far more effective for success in real-life situations.
Although no hospital EOP can anticipate every contingency, hospitalists can proactively practice contingency planning for sustained system-wide mass effect incidents, in which hospitals are unable to maintain normal operations and shift from standard to crisis conventions of care. For example, mass effect incidents (ie, hospital damage from an earthquake or a massive and persistent regional power failure), require planning for how a hospital-wide mass evacuation would unfold and how efforts from multiple ancillary hospital services (engineering, nursing, security, and patient transport) would be integrated. As of 2015, over 90% of hospitals have adopted an electronic health record, but only two-thirds of hospitals feature EOPs for information technology failures.32,33 Given the large footprint of hospitalists in clinical practice, HICS principles appear ripe for application in IT outages and through development of ICS positions structured specifically to this type of contingency.34
CONCLUSION
Disasters unfold rapidly with marked patient surges and the potential to strain healthcare systems over an extended period. However, in both instances, hospitalists are possibly some of the most qualified clinicians to prepare for and respond to such events. Hospitalists need to assume a leadership role in emergency preparedness to integrate seamlessly into hospital incident command structures and to shape the interdepartmental relationships vital to success – skills at which hospitalists excel. Although no plan can address all possible disasters, familiarity with HICS and well-prepared and well-written JASs should help groups respond and succeed in almost all hazards.
Disclosures
None of the authors have any conflicts of interest to report.
1. Homeland Security Presidential Directive-5. 2003.
2. Born CT, Briggs SM, Ciraulo DL, et al. Disasters and mass casualties: I. General principles of response and management. J Am Acad Orthop Surg. 2007;15(7):388-396. doi: 10.5435/00124635-200707000-00004. PubMed
3. Born CT, Briggs SM, Ciraulo DL, et al. Disasters and mass casualties: II. explosive, biologic, chemical, and nuclear agents. J Am Acad Orthop Surg. 2007;15(8):461-473. PubMed
4. Christian MD, Hawryluck L, Wax RS, et al., Development of a triage protocol for critical care during an influenza pandemic. CMAJ. 2006;175(11):1377-1381. doi: 10.1503/cmaj.060911. PubMed
5. Barbera JA, Macintyre AG. Medical Surge Capacity and Capability: The Healthcare Coalition in Emergency Response and Recovery. In: Knebel A, Trabert E, eds. Department of Health and Human Services. 2007.
6. Roccaforte JD, Cushman JG. Disaster preparation and management for the intensive care unit. Curr Opin Crit Care. 2002;8(6):607-615. PubMed
7. Roccaforte JD, Cushman JG. Disaster preparedness, triage, and surge capacity for hospital definitive care areas: optimizing outcomes when demands exceed resources. Anesthesiol Clin. 2007;25(1):161-177, xi. doi: 10.1016/j.anclin.2007.01.002. PubMed
8. Emergency Medical Services of California. Hospital Incident Command System V. 2014 [cited 2018 February 14th]. https://emsa.ca.gov/wp-content/uploads/sites/47/2017/09/HICS_Guidebook_2014_11.pdf. Accessed June 1, 2018.
9. Sprung CL, Zimmerman JL, Christian MD, et al. Recommendations for intensive care unit and hospital preparations for an influenza epidemic or mass disaster: Summary report of the European Society of Intensive Care Medicine’s Task Force for intensive care unit triage during an influenza epidemic or mass disaster. Intensive Care Med. 2010;36(3):428-443. doi: 10.1007/s00134-010-1759-y. PubMed
10. Inpatient specialists help cut costs, reduce LOS. Hospitalists partner with case managers. Hosp Case Manag. 1997;5(5):79-81. PubMed
11. Thompson RE, Pfeifer K, Grant PJ, et al. Hospital medicine and perioperative care: A framework for high-quality, high-value collaborative care. J Hosp Med. 2017;12(4):277-282. doi: 10.12788/jhm.2717. PubMed
12. Gupta R, Moriates C, Harrison JD, et al. Development of a high-value care culture survey: A modified Delphi process and psychometric evaluation. BMJ Qual Saf. 2017;26(6):475-483. doi: 10.1136/bmjqs-2016-005612. PubMed
13. Tadmor B, McManus J, Koenig KL. The art and science of surge: Experience from Israel and the U.S. military. Acad Emerg Med. 2006;13(11):1130-1134. doi: 10.1197/j.aem.2006.06.043. PubMed
14. Myers AL. Vegas Hospitals Swamped With Victims After High-Rise Attack. Associated Press; 2017. https://www.msn.com/en-us/news/breakingnews/vegas-hospitals-swamped-with-victims-after-high-rise-attack/ar-AAsQyZ8?ocid=HPCDHP. Las Vegas. Accessed June 1, 2018.
15. Craig T. As the Wounded Kept Coming, Las Vegas Hospitals Dealt With Injuries Rarely Seen in the US. In: Mello F, Sun L, eds. Washington Post: Washington Post; Oct 3, 2017.
16. Porth L. Preparedness and Partnerships: Lessons learned from the Missouri disasters of 2011. A Focus on Joplin. 2012, Missouri Hospital Association. PubMed
17. Persoff J. First Response Mode: May 22, 2011, Joplin Tornado. June 5, 2011; Available from: http://stormdoctor.blogspot.com/2011/06/first-response-mode-may-22-2011-joplin.html. Accessed June 1, 2018.
18. Dichter JR, Kanter RK, Dries D, et al. System-level planning, coordination, and communication: care of the critically ill and injured during pandemics and disasters: CHEST consensus statement. Chest. 2014;146(4 Suppl):e87S-e102S. doi: 10.1378/chest.14-0738. PubMed
19. Thomas TL, Hsu EB, Kim HK, Colli S, Arana G, Green GB. The incident command system in disasters: Evaluation methods for a hospital-based exercise. Prehosp Disaster Med. 2005;20(1):14-23. doi: 10.1017/S1049023X00002090. PubMed
20. FEMA. The Historical Contex of Emergency Management. [cited 2018 February 14th]; Available from: https://training.fema.gov/emi.aspx. Accessed June 1, 2018.
21. Backer H. Hospital Incident Command System Guidebook 5th Edition. In: Smiley D, Schoenthal L, eds. California Emergency Medical Services Authority, 2014. Accessed June 1, 2018.
22. Emergency Management Resources. Available from: https://www.jointcommission.org/emergency_management.aspx. Accessed June 1, 2018.
23. Incident Command System Training Program. Available from: https://training.fema.gov/emiweb/is/icsresource/trainingmaterials.htm.
24. Agency, F.E.M. NIMS and the Incident Command System. Nov 23, 2004; Available from: https://www.fema.gov/txt/nims/nims_ics_position_paper.txt. Accessed June 1, 2018.
25. Peleg K, Kellermann AL. Enhancing hospital surge capacity for mass casualty events. JAMA. 2009;302(5):565-567. doi: 10.1001/jama.2009.1119. PubMed
26. Adalja AA, Watson M, Bouri N, et al. Absorbing citywide patient surge during Hurricane Sandy: a case study in accommodating multiple hospital evacuations. Ann Emerg Med. 2014;64(1):66-73.e1. doi: 10.1016/j.annemergmed.2013.12.010. PubMed
27. Adalja AA, Watson M, Wollner S, Rambhia KJ, Toner ES. Response to the sudden closure of St. Vincent’s Hospital: learning from a real, no-notice, prolonged surge event. Biosecur Bioterror. 2011;9(2):153-161. doi: 10.1089/bsp.2011.0002. PubMed
28. Klein JS, Weigelt JA. Disaster management. Lessons learned. Surg Clin North Am. 1991;71(2):257-266. PubMed
29. Frykberg ER. Medical management of disasters and mass casualties from terrorist bombings: How can we cope? J Trauma. 2002;53(2):201-212. doi: 10.1097/00005373-200208000-00001. PubMed
30. Lynn M, Gurr D, Memon A, Kaliff J. Management of conventional mass casualty incidents: Ten commandments for hospital planning. J Burn Care Res. 2006;27(5):649-658. doi: 10.1097/01.BCR.0000238119.29269.2B. PubMed
31. Williams J, Nocera M, Casteel C. The effectiveness of disaster training for health care workers: A systematic review. Ann Emerg Med. 2008;52(3):211-22, 222.e1-2. doi: 10.1016/j.annemergmed.2007.09.030. PubMed
32. Percent of Hospitals, By Type, that Possess Certified Health IT. 2015, US Department of Health and Human Services: Office of the National Coordinator for Health Information Technology.
33. Lee C, Robinson KM, Wendt K, Williamson D, et al. The preparedness of hospital Health Information Services for system failures due to internal disasters. Health Inf Manag. 2009;38(2):18-25. doi: 10.1177/183335830903800203. PubMed
34. Situations, C.o.G.f.E.C.S.o.C.f.U.i.D. and I.o. Medicine, Crisis Standards of Care: A Systems Framework for Catastrophic Disaster Response. Mar 21, 2012, Washington (DC): National Academies Press (US). PubMed
Recent events, domestically and globally, have highlighted the numerous complex challenges that disasters and mass casualty incidents (MCIs) impose on hospitals. Mass casualty events result from natural phenomena (eg, hurricanes, tornadoes, and wildfires), accidents (eg, plane crashes, building collapses, and toxic waste spills), or man-made crises (eg, terrorism).1-4 These events feature the potential to cause an acute surge of patients, which can overwhelm available hospital resources and personnel. Mass effect incidents are sustained crises, which often occur due to loss of infrastructure, epidemic infectious diseases, or need for hospital evacuations, and can completely overtax local and regional resources, thus requiring federal and state coordination.5
Hospital disaster response plans have traditionally centered on responses by the emergency department (ED) and associated surgical services to mass trauma-type events, without commensurate involvement of other hospital departments in either incident management operations or the planning process for mass effect incidents.6,7 In particular, the role of hospitalists in the leadership structure of various hospital disaster command structures remains undefined.8 However, recent disasters suggest that hospitalist involvement will highly benefit hospital emergency preparedness.9 Hospitalists possess specialized expertise in patient triage and disposition; medical comanagement with surgical services; coordination of complex medical care (usually with continuous 24/7 in-house coverage); integration with the full spectrum of affiliated services, such as case management or patient rehabilitation; and quality improvement research.10-12 At our institution, hospitalists are involved in the direct care of over 60% of the patients admitted across all medical and surgical services. Thus, we believe that hospitalists are uniquely qualified to offer leadership in disaster preparation, response, and recovery if integrated into hospitals’ incident command architectures. For example, although numerous acute patient surges are due to trauma MCIs, hospitalists may nevertheless act as the primary care providers in disasters that are medical in nature or that require rapid hospital evacuation and patient transfer (Table 1).
Although truly large-scale disasters are uncommon, several recent incidents exemplify scenarios with remarkably extreme acute patient surges (defined as >20% of normal patient volumes), which completely overwhelm a hospital’s capacity to maintain normal operations and require response from all available medical personnel, ideally in a preplanned and organized manner.13 The Las Vegas shooting on October 1, 2017, for example, resulted in 546 trauma victims, inundating two local hospitals and one regional facility.14,15 In another case, the deadliest tornado in modern US history struck Joplin, Missouri on May 22, 2011, destroying one of the two hospitals in the city and leaving an estimated 1,371 people injured, many of whom were presented to the one remaining area hospital.16 One of our team members (J.P.), a storm chaser from out-of-town, reported to the remaining functioning hospital and oversaw an impromptu hospital unit that received patients from the damaged hospital, ultimately caring for approximately 40 patients with a combination of medical and surgical issues from presentation through eventual disposition or transfer to outlying hospitals.17 Such incidents illustrate that during trauma events, hospitalists play critical roles for continuity of care for hospitalized disaster victims.
Therefore, we propose a means for incorporating hospitalists into the coordinated hospital disaster response effort, first by providing hospitalists with an overview of disaster management principles to allow their engagement with hospitals’ disaster management system with working fluency and second, by proposing a framework for hospitalist involvement in hospital emergency response. These recommendations stem from our experience and from similar recommendations from a number of evidence-based articles on intensive care medicine, disaster preparedness, and emergency medicine literature cited in this article. To our knowledge, no evidence-based literature discusses hospital medicine or internal medicine specific to emergency preparedness. We aim to change such condition with this article.
KEY PRINCIPLES OF INCIDENT MANAGEMENT AND PREPAREDNESS: A PRIMER FOR HOSPITALISTS
Effective participation in disaster response and planning requires a basic understanding of the organizational structures for incident management.18,19 Overall disaster response within the United States is guided by the National Response Framework, a national-level strategy that directs coordination between military and civilian response efforts, the latter of which are structured by the National Incident Management System (NIMS).20 NIMS organizes emergency management across all government levels (federal, state, and local) and the private sector under a common operational language and command structure. Both systems grew out of analyses of the September 11, 2001 attacks and Hurricane Katrina, indicating the need for a wider systemic organization to response efforts.1 State-level efforts are designed to mobilize resources to assist in community-level operations. Incident management always falls to the local authorities. At this local level, discrete hospitals often take part in healthcare coalitions that act in conjunction with other health entities, local public health departments, and emergency medical services, forming a multiagency coordination system.5 This healthcare coalition (emergency support function #8 health and medical), in support of emergency managers of city and county governments, forms the core of the medical response. One commonality to all emergency management is the concept of an “all-hazards” approach, which aims to develop a broad and flexible strategy for efficient management of nearly any type of incident. This “all-hazards” approach allows effective management through each of the four phases of incident management: preparation, response, recovery, and ongoing mitigation.
Direct supervision over incident management is achieved through an Incident Command System (ICS), a hierarchical organization of positions involved in response. The top supervisory structure of ICS (Incident Command and General Staff) is the same regardless of the locale in which it operates, allowing coherent interoperability with other agencies. Incidents of any size are managed with a scalable approach; subordinate ICS positions, which are tailored according to specific needs, can be activated as needed. Healthcare implementation of the ICS structure led to the development of the Hospital Incident Command System (HICS), which now serves as the national standard for hospital-based incident management and facilitates the capacity of individual hospitals to coordinate with other resources regionally and is a part of NIMS for emergency response (Figure 1).21 The success of HICS-led regulatory agencies (namely the Centers for Medicare and Medicaid Services and the Joint Commission) to require ICS/HICS in-hospital incident response plans.22 The most recent HICS (Version V) excludes physician involvement in the overall management chart. However, we demonstrate how the inherent flexibility in ICS can adapt to involve hospitalists. Although HICS serves as a backbone that requires institutionally specific modifications, other institutions, such as ours, commonly have entire branches or positions renamed, reapportioned, or created to fill their specific needs. Specialized training in ICS, NIMS, and other aspects of hospital emergency response is beyond the scope of this article but is available for free through the Department of Homeland Security and FEMA.23
Perhaps, the defining feature of ICS/HICS is its expandability, allowing the response efforts to be scaled and tailored in size, scope, and complexity of that of the incident.24 At the same time, the principles of span of control and unity of command promote efficient command structure by mandating each participant within the disaster response process to report to only one superior, whereas these superiors are limited to a manageable number of subordinates. For example, in Figure 2, all Strike Team Leaders
PROPOSED FRAMEWORK FOR HOSPITALIST INVOLVEMENT
Although incidents vary in terms of their severity, acuity of onset, duration, and composition of patients, a defining feature of MCIs is the rapid surge of patients with acute needs. Many MCIs are easily absorbed by local facilities. However, smaller hospitals or hospitals receiving patients from larger-scale incidents may become overwhelmed, in which larger incidents may result in an acute surge of over 20% of hospital capacity.13 Moreover, hospital surge capabilities have markedly diminished over the past decade due to overcrowding of emergency rooms, in part by admitted patients occupying the room space within the ED (“boarding”), further decreasing the hospitals’ capacities to accept new patients.25
Our proposed framework for hospitalist involvement in MCI disaster response focuses on such a situation, with emphasis on augmentation of hospital surge capacity and facilitation of patient throughput and discharge. Notably, these goals are modified from the standard HICS architecture (Figures 1-2 and Table 2). In this framework, hospitalists can play a critical role in decompressing the emergency room through admitting medical patients as rapidly as possible (even if preliminary workup is still pending), facilitating rapid discharge of patients to allow newer admissions to reach the floor, and prioritizing patients that could be transferred to other facilities or services and thus opening additional beds for admission (eg, accepting patients from the ICU or surgical floors to increase capacities on those services). Additionally, hospitalists can comanage surgical patients while surgeons are operating, assist intensivists with medical issues, and facilitate care of patients with minor injuries.
Using the HICS framework, each of those domains would be handled by a Strike Team led by one Team Leader whose goal is to operationalize various assets into a cohesive team specializing in those goals. Table 2 summarizes these goals, as presented in the context of patient examples.
To keep up with the ICS fundamentals, Hospitalist Unit Leaders may address a large MCI with all four strike teams or may only activate the strike teams needed for a less intensive MCI. For example, a bombing may result in a patient surge of 30% more than normal operations and thus demand a full response that includes all the strike teams noted above. By contrast, a bus accident with 20 injured patients may only require a Hospitalist Unit Leader to activate the “Admissions and Internal Transfers In” Strike Team to help offload a busy emergency room.
HOSPITALIST LEADERSHIP IN HOSPITAL EMERGENCY OPERATION PLAN DEVELOPMENT
Emergency management is comprised of four phases: preparation, response, recovery, and mitigation. The latter two phases are beyond the scope of this paper. Although most of our review has focused on modeling disaster response, hospitalist leadership remains critical in preparing for disasters. A disaster often psychologically overwhelms care providers, who feel compelled to help but are uncertain where to begin. To aid the members of a disaster response team, a state-of-the-art hospitalist group creates Job Action Sheets (JASs) for each position in their HICS organizational chart; these sheets codify how to respond and what roles are needed. These formal, protocolized sheets provide individuals assigned to these positions a description of their roles and responsibilities, including to whom they report and over whom they supervise, and include detailed checklists to aid in reaching critical milestones during the response phase. For example, the “Surgical Comanagement and Consulting” Strike Team Leader JAS would likely include the expectations of surgeons for assisting in patient management (ie, auto-consulting on all postoperative patients) and whether nursing phone calls on surgical patients would be temporarily routed to the Strike Team during periods of OR surge.
Hospitalists are well suited as leaders in disaster preparation given their ability to coordinate care among a large spectrum of stakeholders. For example, case managers and social workers are essential members of a well-structured Discharge Strike Team. Their input is critical to ensure that disaster tactics – such as care coordination contracts with local skilled nursing facilities willing to expedite discharge in emergencies to their facilities – are in-place before a real MCI. During Hurricane Sandy, mass evacuation of affected hospitals was effective through the Healthcare Facility Evacuation Center (a healthcare coalition of the New York Hospital Association) but nevertheless plagued with issues regarding situational awareness, poor communication between facilities, and difficulty bundling patients with medical records to receiving facilities – items which can be identified, anticipated, and thoroughly vetted by hospitalists well in advance of a real-world evacuation.26, 27
As the Joint Commission mandates regular exercises of the emergency plan, protocols must be drilled regularly to uncover deficiencies and areas for improvement.18 The most common failure patterns in Emergency Operation Plans (EOPs) include unrealistic and ineffective expectations and poor communication between different personnel and groups, resulting in confusion and obfuscation.28-30 Therefore, EOPs need to be both comprehensive and realistic – characteristics that can only be tested through repeated drills. These characteristics can be tested during tabletop exercises, where hospitalists assume the role of a part of the ICS structure and with JAS in hand, attempt to reason how to respond to a given scenario.31 Our experience is that small-scale drills conducted more frequently than the bare minimum mandated by the Joint Commission are far more effective for success in real-life situations.
Although no hospital EOP can anticipate every contingency, hospitalists can proactively practice contingency planning for sustained system-wide mass effect incidents, in which hospitals are unable to maintain normal operations and shift from standard to crisis conventions of care. For example, mass effect incidents (ie, hospital damage from an earthquake or a massive and persistent regional power failure), require planning for how a hospital-wide mass evacuation would unfold and how efforts from multiple ancillary hospital services (engineering, nursing, security, and patient transport) would be integrated. As of 2015, over 90% of hospitals have adopted an electronic health record, but only two-thirds of hospitals feature EOPs for information technology failures.32,33 Given the large footprint of hospitalists in clinical practice, HICS principles appear ripe for application in IT outages and through development of ICS positions structured specifically to this type of contingency.34
CONCLUSION
Disasters unfold rapidly with marked patient surges and the potential to strain healthcare systems over an extended period. However, in both instances, hospitalists are possibly some of the most qualified clinicians to prepare for and respond to such events. Hospitalists need to assume a leadership role in emergency preparedness to integrate seamlessly into hospital incident command structures and to shape the interdepartmental relationships vital to success – skills at which hospitalists excel. Although no plan can address all possible disasters, familiarity with HICS and well-prepared and well-written JASs should help groups respond and succeed in almost all hazards.
Disclosures
None of the authors have any conflicts of interest to report.
Recent events, domestically and globally, have highlighted the numerous complex challenges that disasters and mass casualty incidents (MCIs) impose on hospitals. Mass casualty events result from natural phenomena (eg, hurricanes, tornadoes, and wildfires), accidents (eg, plane crashes, building collapses, and toxic waste spills), or man-made crises (eg, terrorism).1-4 These events feature the potential to cause an acute surge of patients, which can overwhelm available hospital resources and personnel. Mass effect incidents are sustained crises, which often occur due to loss of infrastructure, epidemic infectious diseases, or need for hospital evacuations, and can completely overtax local and regional resources, thus requiring federal and state coordination.5
Hospital disaster response plans have traditionally centered on responses by the emergency department (ED) and associated surgical services to mass trauma-type events, without commensurate involvement of other hospital departments in either incident management operations or the planning process for mass effect incidents.6,7 In particular, the role of hospitalists in the leadership structure of various hospital disaster command structures remains undefined.8 However, recent disasters suggest that hospitalist involvement will highly benefit hospital emergency preparedness.9 Hospitalists possess specialized expertise in patient triage and disposition; medical comanagement with surgical services; coordination of complex medical care (usually with continuous 24/7 in-house coverage); integration with the full spectrum of affiliated services, such as case management or patient rehabilitation; and quality improvement research.10-12 At our institution, hospitalists are involved in the direct care of over 60% of the patients admitted across all medical and surgical services. Thus, we believe that hospitalists are uniquely qualified to offer leadership in disaster preparation, response, and recovery if integrated into hospitals’ incident command architectures. For example, although numerous acute patient surges are due to trauma MCIs, hospitalists may nevertheless act as the primary care providers in disasters that are medical in nature or that require rapid hospital evacuation and patient transfer (Table 1).
Although truly large-scale disasters are uncommon, several recent incidents exemplify scenarios with remarkably extreme acute patient surges (defined as >20% of normal patient volumes), which completely overwhelm a hospital’s capacity to maintain normal operations and require response from all available medical personnel, ideally in a preplanned and organized manner.13 The Las Vegas shooting on October 1, 2017, for example, resulted in 546 trauma victims, inundating two local hospitals and one regional facility.14,15 In another case, the deadliest tornado in modern US history struck Joplin, Missouri on May 22, 2011, destroying one of the two hospitals in the city and leaving an estimated 1,371 people injured, many of whom were presented to the one remaining area hospital.16 One of our team members (J.P.), a storm chaser from out-of-town, reported to the remaining functioning hospital and oversaw an impromptu hospital unit that received patients from the damaged hospital, ultimately caring for approximately 40 patients with a combination of medical and surgical issues from presentation through eventual disposition or transfer to outlying hospitals.17 Such incidents illustrate that during trauma events, hospitalists play critical roles for continuity of care for hospitalized disaster victims.
Therefore, we propose a means for incorporating hospitalists into the coordinated hospital disaster response effort, first by providing hospitalists with an overview of disaster management principles to allow their engagement with hospitals’ disaster management system with working fluency and second, by proposing a framework for hospitalist involvement in hospital emergency response. These recommendations stem from our experience and from similar recommendations from a number of evidence-based articles on intensive care medicine, disaster preparedness, and emergency medicine literature cited in this article. To our knowledge, no evidence-based literature discusses hospital medicine or internal medicine specific to emergency preparedness. We aim to change such condition with this article.
KEY PRINCIPLES OF INCIDENT MANAGEMENT AND PREPAREDNESS: A PRIMER FOR HOSPITALISTS
Effective participation in disaster response and planning requires a basic understanding of the organizational structures for incident management.18,19 Overall disaster response within the United States is guided by the National Response Framework, a national-level strategy that directs coordination between military and civilian response efforts, the latter of which are structured by the National Incident Management System (NIMS).20 NIMS organizes emergency management across all government levels (federal, state, and local) and the private sector under a common operational language and command structure. Both systems grew out of analyses of the September 11, 2001 attacks and Hurricane Katrina, indicating the need for a wider systemic organization to response efforts.1 State-level efforts are designed to mobilize resources to assist in community-level operations. Incident management always falls to the local authorities. At this local level, discrete hospitals often take part in healthcare coalitions that act in conjunction with other health entities, local public health departments, and emergency medical services, forming a multiagency coordination system.5 This healthcare coalition (emergency support function #8 health and medical), in support of emergency managers of city and county governments, forms the core of the medical response. One commonality to all emergency management is the concept of an “all-hazards” approach, which aims to develop a broad and flexible strategy for efficient management of nearly any type of incident. This “all-hazards” approach allows effective management through each of the four phases of incident management: preparation, response, recovery, and ongoing mitigation.
Direct supervision over incident management is achieved through an Incident Command System (ICS), a hierarchical organization of positions involved in response. The top supervisory structure of ICS (Incident Command and General Staff) is the same regardless of the locale in which it operates, allowing coherent interoperability with other agencies. Incidents of any size are managed with a scalable approach; subordinate ICS positions, which are tailored according to specific needs, can be activated as needed. Healthcare implementation of the ICS structure led to the development of the Hospital Incident Command System (HICS), which now serves as the national standard for hospital-based incident management and facilitates the capacity of individual hospitals to coordinate with other resources regionally and is a part of NIMS for emergency response (Figure 1).21 The success of HICS-led regulatory agencies (namely the Centers for Medicare and Medicaid Services and the Joint Commission) to require ICS/HICS in-hospital incident response plans.22 The most recent HICS (Version V) excludes physician involvement in the overall management chart. However, we demonstrate how the inherent flexibility in ICS can adapt to involve hospitalists. Although HICS serves as a backbone that requires institutionally specific modifications, other institutions, such as ours, commonly have entire branches or positions renamed, reapportioned, or created to fill their specific needs. Specialized training in ICS, NIMS, and other aspects of hospital emergency response is beyond the scope of this article but is available for free through the Department of Homeland Security and FEMA.23
Perhaps, the defining feature of ICS/HICS is its expandability, allowing the response efforts to be scaled and tailored in size, scope, and complexity of that of the incident.24 At the same time, the principles of span of control and unity of command promote efficient command structure by mandating each participant within the disaster response process to report to only one superior, whereas these superiors are limited to a manageable number of subordinates. For example, in Figure 2, all Strike Team Leaders
PROPOSED FRAMEWORK FOR HOSPITALIST INVOLVEMENT
Although incidents vary in terms of their severity, acuity of onset, duration, and composition of patients, a defining feature of MCIs is the rapid surge of patients with acute needs. Many MCIs are easily absorbed by local facilities. However, smaller hospitals or hospitals receiving patients from larger-scale incidents may become overwhelmed, in which larger incidents may result in an acute surge of over 20% of hospital capacity.13 Moreover, hospital surge capabilities have markedly diminished over the past decade due to overcrowding of emergency rooms, in part by admitted patients occupying the room space within the ED (“boarding”), further decreasing the hospitals’ capacities to accept new patients.25
Our proposed framework for hospitalist involvement in MCI disaster response focuses on such a situation, with emphasis on augmentation of hospital surge capacity and facilitation of patient throughput and discharge. Notably, these goals are modified from the standard HICS architecture (Figures 1-2 and Table 2). In this framework, hospitalists can play a critical role in decompressing the emergency room through admitting medical patients as rapidly as possible (even if preliminary workup is still pending), facilitating rapid discharge of patients to allow newer admissions to reach the floor, and prioritizing patients that could be transferred to other facilities or services and thus opening additional beds for admission (eg, accepting patients from the ICU or surgical floors to increase capacities on those services). Additionally, hospitalists can comanage surgical patients while surgeons are operating, assist intensivists with medical issues, and facilitate care of patients with minor injuries.
Using the HICS framework, each of those domains would be handled by a Strike Team led by one Team Leader whose goal is to operationalize various assets into a cohesive team specializing in those goals. Table 2 summarizes these goals, as presented in the context of patient examples.
To keep up with the ICS fundamentals, Hospitalist Unit Leaders may address a large MCI with all four strike teams or may only activate the strike teams needed for a less intensive MCI. For example, a bombing may result in a patient surge of 30% more than normal operations and thus demand a full response that includes all the strike teams noted above. By contrast, a bus accident with 20 injured patients may only require a Hospitalist Unit Leader to activate the “Admissions and Internal Transfers In” Strike Team to help offload a busy emergency room.
HOSPITALIST LEADERSHIP IN HOSPITAL EMERGENCY OPERATION PLAN DEVELOPMENT
Emergency management is comprised of four phases: preparation, response, recovery, and mitigation. The latter two phases are beyond the scope of this paper. Although most of our review has focused on modeling disaster response, hospitalist leadership remains critical in preparing for disasters. A disaster often psychologically overwhelms care providers, who feel compelled to help but are uncertain where to begin. To aid the members of a disaster response team, a state-of-the-art hospitalist group creates Job Action Sheets (JASs) for each position in their HICS organizational chart; these sheets codify how to respond and what roles are needed. These formal, protocolized sheets provide individuals assigned to these positions a description of their roles and responsibilities, including to whom they report and over whom they supervise, and include detailed checklists to aid in reaching critical milestones during the response phase. For example, the “Surgical Comanagement and Consulting” Strike Team Leader JAS would likely include the expectations of surgeons for assisting in patient management (ie, auto-consulting on all postoperative patients) and whether nursing phone calls on surgical patients would be temporarily routed to the Strike Team during periods of OR surge.
Hospitalists are well suited as leaders in disaster preparation given their ability to coordinate care among a large spectrum of stakeholders. For example, case managers and social workers are essential members of a well-structured Discharge Strike Team. Their input is critical to ensure that disaster tactics – such as care coordination contracts with local skilled nursing facilities willing to expedite discharge in emergencies to their facilities – are in-place before a real MCI. During Hurricane Sandy, mass evacuation of affected hospitals was effective through the Healthcare Facility Evacuation Center (a healthcare coalition of the New York Hospital Association) but nevertheless plagued with issues regarding situational awareness, poor communication between facilities, and difficulty bundling patients with medical records to receiving facilities – items which can be identified, anticipated, and thoroughly vetted by hospitalists well in advance of a real-world evacuation.26, 27
As the Joint Commission mandates regular exercises of the emergency plan, protocols must be drilled regularly to uncover deficiencies and areas for improvement.18 The most common failure patterns in Emergency Operation Plans (EOPs) include unrealistic and ineffective expectations and poor communication between different personnel and groups, resulting in confusion and obfuscation.28-30 Therefore, EOPs need to be both comprehensive and realistic – characteristics that can only be tested through repeated drills. These characteristics can be tested during tabletop exercises, where hospitalists assume the role of a part of the ICS structure and with JAS in hand, attempt to reason how to respond to a given scenario.31 Our experience is that small-scale drills conducted more frequently than the bare minimum mandated by the Joint Commission are far more effective for success in real-life situations.
Although no hospital EOP can anticipate every contingency, hospitalists can proactively practice contingency planning for sustained system-wide mass effect incidents, in which hospitals are unable to maintain normal operations and shift from standard to crisis conventions of care. For example, mass effect incidents (ie, hospital damage from an earthquake or a massive and persistent regional power failure), require planning for how a hospital-wide mass evacuation would unfold and how efforts from multiple ancillary hospital services (engineering, nursing, security, and patient transport) would be integrated. As of 2015, over 90% of hospitals have adopted an electronic health record, but only two-thirds of hospitals feature EOPs for information technology failures.32,33 Given the large footprint of hospitalists in clinical practice, HICS principles appear ripe for application in IT outages and through development of ICS positions structured specifically to this type of contingency.34
CONCLUSION
Disasters unfold rapidly with marked patient surges and the potential to strain healthcare systems over an extended period. However, in both instances, hospitalists are possibly some of the most qualified clinicians to prepare for and respond to such events. Hospitalists need to assume a leadership role in emergency preparedness to integrate seamlessly into hospital incident command structures and to shape the interdepartmental relationships vital to success – skills at which hospitalists excel. Although no plan can address all possible disasters, familiarity with HICS and well-prepared and well-written JASs should help groups respond and succeed in almost all hazards.
Disclosures
None of the authors have any conflicts of interest to report.
1. Homeland Security Presidential Directive-5. 2003.
2. Born CT, Briggs SM, Ciraulo DL, et al. Disasters and mass casualties: I. General principles of response and management. J Am Acad Orthop Surg. 2007;15(7):388-396. doi: 10.5435/00124635-200707000-00004. PubMed
3. Born CT, Briggs SM, Ciraulo DL, et al. Disasters and mass casualties: II. explosive, biologic, chemical, and nuclear agents. J Am Acad Orthop Surg. 2007;15(8):461-473. PubMed
4. Christian MD, Hawryluck L, Wax RS, et al., Development of a triage protocol for critical care during an influenza pandemic. CMAJ. 2006;175(11):1377-1381. doi: 10.1503/cmaj.060911. PubMed
5. Barbera JA, Macintyre AG. Medical Surge Capacity and Capability: The Healthcare Coalition in Emergency Response and Recovery. In: Knebel A, Trabert E, eds. Department of Health and Human Services. 2007.
6. Roccaforte JD, Cushman JG. Disaster preparation and management for the intensive care unit. Curr Opin Crit Care. 2002;8(6):607-615. PubMed
7. Roccaforte JD, Cushman JG. Disaster preparedness, triage, and surge capacity for hospital definitive care areas: optimizing outcomes when demands exceed resources. Anesthesiol Clin. 2007;25(1):161-177, xi. doi: 10.1016/j.anclin.2007.01.002. PubMed
8. Emergency Medical Services of California. Hospital Incident Command System V. 2014 [cited 2018 February 14th]. https://emsa.ca.gov/wp-content/uploads/sites/47/2017/09/HICS_Guidebook_2014_11.pdf. Accessed June 1, 2018.
9. Sprung CL, Zimmerman JL, Christian MD, et al. Recommendations for intensive care unit and hospital preparations for an influenza epidemic or mass disaster: Summary report of the European Society of Intensive Care Medicine’s Task Force for intensive care unit triage during an influenza epidemic or mass disaster. Intensive Care Med. 2010;36(3):428-443. doi: 10.1007/s00134-010-1759-y. PubMed
10. Inpatient specialists help cut costs, reduce LOS. Hospitalists partner with case managers. Hosp Case Manag. 1997;5(5):79-81. PubMed
11. Thompson RE, Pfeifer K, Grant PJ, et al. Hospital medicine and perioperative care: A framework for high-quality, high-value collaborative care. J Hosp Med. 2017;12(4):277-282. doi: 10.12788/jhm.2717. PubMed
12. Gupta R, Moriates C, Harrison JD, et al. Development of a high-value care culture survey: A modified Delphi process and psychometric evaluation. BMJ Qual Saf. 2017;26(6):475-483. doi: 10.1136/bmjqs-2016-005612. PubMed
13. Tadmor B, McManus J, Koenig KL. The art and science of surge: Experience from Israel and the U.S. military. Acad Emerg Med. 2006;13(11):1130-1134. doi: 10.1197/j.aem.2006.06.043. PubMed
14. Myers AL. Vegas Hospitals Swamped With Victims After High-Rise Attack. Associated Press; 2017. https://www.msn.com/en-us/news/breakingnews/vegas-hospitals-swamped-with-victims-after-high-rise-attack/ar-AAsQyZ8?ocid=HPCDHP. Las Vegas. Accessed June 1, 2018.
15. Craig T. As the Wounded Kept Coming, Las Vegas Hospitals Dealt With Injuries Rarely Seen in the US. In: Mello F, Sun L, eds. Washington Post: Washington Post; Oct 3, 2017.
16. Porth L. Preparedness and Partnerships: Lessons learned from the Missouri disasters of 2011. A Focus on Joplin. 2012, Missouri Hospital Association. PubMed
17. Persoff J. First Response Mode: May 22, 2011, Joplin Tornado. June 5, 2011; Available from: http://stormdoctor.blogspot.com/2011/06/first-response-mode-may-22-2011-joplin.html. Accessed June 1, 2018.
18. Dichter JR, Kanter RK, Dries D, et al. System-level planning, coordination, and communication: care of the critically ill and injured during pandemics and disasters: CHEST consensus statement. Chest. 2014;146(4 Suppl):e87S-e102S. doi: 10.1378/chest.14-0738. PubMed
19. Thomas TL, Hsu EB, Kim HK, Colli S, Arana G, Green GB. The incident command system in disasters: Evaluation methods for a hospital-based exercise. Prehosp Disaster Med. 2005;20(1):14-23. doi: 10.1017/S1049023X00002090. PubMed
20. FEMA. The Historical Contex of Emergency Management. [cited 2018 February 14th]; Available from: https://training.fema.gov/emi.aspx. Accessed June 1, 2018.
21. Backer H. Hospital Incident Command System Guidebook 5th Edition. In: Smiley D, Schoenthal L, eds. California Emergency Medical Services Authority, 2014. Accessed June 1, 2018.
22. Emergency Management Resources. Available from: https://www.jointcommission.org/emergency_management.aspx. Accessed June 1, 2018.
23. Incident Command System Training Program. Available from: https://training.fema.gov/emiweb/is/icsresource/trainingmaterials.htm.
24. Agency, F.E.M. NIMS and the Incident Command System. Nov 23, 2004; Available from: https://www.fema.gov/txt/nims/nims_ics_position_paper.txt. Accessed June 1, 2018.
25. Peleg K, Kellermann AL. Enhancing hospital surge capacity for mass casualty events. JAMA. 2009;302(5):565-567. doi: 10.1001/jama.2009.1119. PubMed
26. Adalja AA, Watson M, Bouri N, et al. Absorbing citywide patient surge during Hurricane Sandy: a case study in accommodating multiple hospital evacuations. Ann Emerg Med. 2014;64(1):66-73.e1. doi: 10.1016/j.annemergmed.2013.12.010. PubMed
27. Adalja AA, Watson M, Wollner S, Rambhia KJ, Toner ES. Response to the sudden closure of St. Vincent’s Hospital: learning from a real, no-notice, prolonged surge event. Biosecur Bioterror. 2011;9(2):153-161. doi: 10.1089/bsp.2011.0002. PubMed
28. Klein JS, Weigelt JA. Disaster management. Lessons learned. Surg Clin North Am. 1991;71(2):257-266. PubMed
29. Frykberg ER. Medical management of disasters and mass casualties from terrorist bombings: How can we cope? J Trauma. 2002;53(2):201-212. doi: 10.1097/00005373-200208000-00001. PubMed
30. Lynn M, Gurr D, Memon A, Kaliff J. Management of conventional mass casualty incidents: Ten commandments for hospital planning. J Burn Care Res. 2006;27(5):649-658. doi: 10.1097/01.BCR.0000238119.29269.2B. PubMed
31. Williams J, Nocera M, Casteel C. The effectiveness of disaster training for health care workers: A systematic review. Ann Emerg Med. 2008;52(3):211-22, 222.e1-2. doi: 10.1016/j.annemergmed.2007.09.030. PubMed
32. Percent of Hospitals, By Type, that Possess Certified Health IT. 2015, US Department of Health and Human Services: Office of the National Coordinator for Health Information Technology.
33. Lee C, Robinson KM, Wendt K, Williamson D, et al. The preparedness of hospital Health Information Services for system failures due to internal disasters. Health Inf Manag. 2009;38(2):18-25. doi: 10.1177/183335830903800203. PubMed
34. Situations, C.o.G.f.E.C.S.o.C.f.U.i.D. and I.o. Medicine, Crisis Standards of Care: A Systems Framework for Catastrophic Disaster Response. Mar 21, 2012, Washington (DC): National Academies Press (US). PubMed
1. Homeland Security Presidential Directive-5. 2003.
2. Born CT, Briggs SM, Ciraulo DL, et al. Disasters and mass casualties: I. General principles of response and management. J Am Acad Orthop Surg. 2007;15(7):388-396. doi: 10.5435/00124635-200707000-00004. PubMed
3. Born CT, Briggs SM, Ciraulo DL, et al. Disasters and mass casualties: II. explosive, biologic, chemical, and nuclear agents. J Am Acad Orthop Surg. 2007;15(8):461-473. PubMed
4. Christian MD, Hawryluck L, Wax RS, et al., Development of a triage protocol for critical care during an influenza pandemic. CMAJ. 2006;175(11):1377-1381. doi: 10.1503/cmaj.060911. PubMed
5. Barbera JA, Macintyre AG. Medical Surge Capacity and Capability: The Healthcare Coalition in Emergency Response and Recovery. In: Knebel A, Trabert E, eds. Department of Health and Human Services. 2007.
6. Roccaforte JD, Cushman JG. Disaster preparation and management for the intensive care unit. Curr Opin Crit Care. 2002;8(6):607-615. PubMed
7. Roccaforte JD, Cushman JG. Disaster preparedness, triage, and surge capacity for hospital definitive care areas: optimizing outcomes when demands exceed resources. Anesthesiol Clin. 2007;25(1):161-177, xi. doi: 10.1016/j.anclin.2007.01.002. PubMed
8. Emergency Medical Services of California. Hospital Incident Command System V. 2014 [cited 2018 February 14th]. https://emsa.ca.gov/wp-content/uploads/sites/47/2017/09/HICS_Guidebook_2014_11.pdf. Accessed June 1, 2018.
9. Sprung CL, Zimmerman JL, Christian MD, et al. Recommendations for intensive care unit and hospital preparations for an influenza epidemic or mass disaster: Summary report of the European Society of Intensive Care Medicine’s Task Force for intensive care unit triage during an influenza epidemic or mass disaster. Intensive Care Med. 2010;36(3):428-443. doi: 10.1007/s00134-010-1759-y. PubMed
10. Inpatient specialists help cut costs, reduce LOS. Hospitalists partner with case managers. Hosp Case Manag. 1997;5(5):79-81. PubMed
11. Thompson RE, Pfeifer K, Grant PJ, et al. Hospital medicine and perioperative care: A framework for high-quality, high-value collaborative care. J Hosp Med. 2017;12(4):277-282. doi: 10.12788/jhm.2717. PubMed
12. Gupta R, Moriates C, Harrison JD, et al. Development of a high-value care culture survey: A modified Delphi process and psychometric evaluation. BMJ Qual Saf. 2017;26(6):475-483. doi: 10.1136/bmjqs-2016-005612. PubMed
13. Tadmor B, McManus J, Koenig KL. The art and science of surge: Experience from Israel and the U.S. military. Acad Emerg Med. 2006;13(11):1130-1134. doi: 10.1197/j.aem.2006.06.043. PubMed
14. Myers AL. Vegas Hospitals Swamped With Victims After High-Rise Attack. Associated Press; 2017. https://www.msn.com/en-us/news/breakingnews/vegas-hospitals-swamped-with-victims-after-high-rise-attack/ar-AAsQyZ8?ocid=HPCDHP. Las Vegas. Accessed June 1, 2018.
15. Craig T. As the Wounded Kept Coming, Las Vegas Hospitals Dealt With Injuries Rarely Seen in the US. In: Mello F, Sun L, eds. Washington Post: Washington Post; Oct 3, 2017.
16. Porth L. Preparedness and Partnerships: Lessons learned from the Missouri disasters of 2011. A Focus on Joplin. 2012, Missouri Hospital Association. PubMed
17. Persoff J. First Response Mode: May 22, 2011, Joplin Tornado. June 5, 2011; Available from: http://stormdoctor.blogspot.com/2011/06/first-response-mode-may-22-2011-joplin.html. Accessed June 1, 2018.
18. Dichter JR, Kanter RK, Dries D, et al. System-level planning, coordination, and communication: care of the critically ill and injured during pandemics and disasters: CHEST consensus statement. Chest. 2014;146(4 Suppl):e87S-e102S. doi: 10.1378/chest.14-0738. PubMed
19. Thomas TL, Hsu EB, Kim HK, Colli S, Arana G, Green GB. The incident command system in disasters: Evaluation methods for a hospital-based exercise. Prehosp Disaster Med. 2005;20(1):14-23. doi: 10.1017/S1049023X00002090. PubMed
20. FEMA. The Historical Contex of Emergency Management. [cited 2018 February 14th]; Available from: https://training.fema.gov/emi.aspx. Accessed June 1, 2018.
21. Backer H. Hospital Incident Command System Guidebook 5th Edition. In: Smiley D, Schoenthal L, eds. California Emergency Medical Services Authority, 2014. Accessed June 1, 2018.
22. Emergency Management Resources. Available from: https://www.jointcommission.org/emergency_management.aspx. Accessed June 1, 2018.
23. Incident Command System Training Program. Available from: https://training.fema.gov/emiweb/is/icsresource/trainingmaterials.htm.
24. Agency, F.E.M. NIMS and the Incident Command System. Nov 23, 2004; Available from: https://www.fema.gov/txt/nims/nims_ics_position_paper.txt. Accessed June 1, 2018.
25. Peleg K, Kellermann AL. Enhancing hospital surge capacity for mass casualty events. JAMA. 2009;302(5):565-567. doi: 10.1001/jama.2009.1119. PubMed
26. Adalja AA, Watson M, Bouri N, et al. Absorbing citywide patient surge during Hurricane Sandy: a case study in accommodating multiple hospital evacuations. Ann Emerg Med. 2014;64(1):66-73.e1. doi: 10.1016/j.annemergmed.2013.12.010. PubMed
27. Adalja AA, Watson M, Wollner S, Rambhia KJ, Toner ES. Response to the sudden closure of St. Vincent’s Hospital: learning from a real, no-notice, prolonged surge event. Biosecur Bioterror. 2011;9(2):153-161. doi: 10.1089/bsp.2011.0002. PubMed
28. Klein JS, Weigelt JA. Disaster management. Lessons learned. Surg Clin North Am. 1991;71(2):257-266. PubMed
29. Frykberg ER. Medical management of disasters and mass casualties from terrorist bombings: How can we cope? J Trauma. 2002;53(2):201-212. doi: 10.1097/00005373-200208000-00001. PubMed
30. Lynn M, Gurr D, Memon A, Kaliff J. Management of conventional mass casualty incidents: Ten commandments for hospital planning. J Burn Care Res. 2006;27(5):649-658. doi: 10.1097/01.BCR.0000238119.29269.2B. PubMed
31. Williams J, Nocera M, Casteel C. The effectiveness of disaster training for health care workers: A systematic review. Ann Emerg Med. 2008;52(3):211-22, 222.e1-2. doi: 10.1016/j.annemergmed.2007.09.030. PubMed
32. Percent of Hospitals, By Type, that Possess Certified Health IT. 2015, US Department of Health and Human Services: Office of the National Coordinator for Health Information Technology.
33. Lee C, Robinson KM, Wendt K, Williamson D, et al. The preparedness of hospital Health Information Services for system failures due to internal disasters. Health Inf Manag. 2009;38(2):18-25. doi: 10.1177/183335830903800203. PubMed
34. Situations, C.o.G.f.E.C.S.o.C.f.U.i.D. and I.o. Medicine, Crisis Standards of Care: A Systems Framework for Catastrophic Disaster Response. Mar 21, 2012, Washington (DC): National Academies Press (US). PubMed
© 2018 Society of Hospital Medicine
In the Literature
In This Edition
- C-reactive protein levels predict death from cardiac causes after MI.
- SSRIs reduce risk for recurrent cardiac events in acute coronary syndrome.
- Vancomycin is as effective as metronidazole in routine treatment of C. difficile and superior in severe infection.
- Prevalence and severity of C. difficile are increasing in hospitalized patients in the U.S.
- Deviations in recommended enoxaparin dosing in NSTEMI result in worse outcomes.
- Most outpatient VTE events occur in recently hospitalized patients.
- Poor health literacy predicts mortality in older adults.
- A validated model predicts the risk for delirium at hospital discharge.
Do C-reactive Protein Levels Predict Death from Heart Failure?
Background: Ultra-sensitive quantitative assessment of C-reactive protein (CRP), a surrogate marker of systemic inflammation, has previously been shown to predict plaque instability in acute coronary syndromes. Data are lacking as to whether this blood test can also predict subsequent risk of heart failure or death on presentation in patients admitted for acute myocardial infarction (MI).
Study design: Prospec-tive observational study.
Setting: Olmstead County, Minn.
Synopsis: Ultra-sensitive quantitative serum CRP levels were obtained a median of 6.1 hours following onset of symptoms in 329 patients admitted with acute MI. The patients were stratified into tertiles based levels of CRP less than 3 mg/L, 3-15 mg/L, and more than 15 mg/L.
Tertiles were similar in respect to age, male-predominance, most cardiac risk factors, body mass index, and electrocardiographic (EKG) changes. However, there were statistically significant differences between groups, particularly the frequency of diabetes (10.7%, 31.2%, and 38.0%), previous MI history (2.7%, 4.6%, and 9.3%), Killip class greater than one (15.2%, 31.2%, and 39.8%), peak cardiac enzyme levels (both were higher in the bottom tertile, and lowest in the top tertile), and likelihood of significant comorbidities (lower likelihood in the bottom tertile, higher likelihood in the top tertile).
One-year survival was highly correlated with CRP tertile (93%, 84%, and 62% respectively). Once corrected for age, gender, peak cardiac enzymes, Killip class, coronary history, and recurring ischemic events, there remained a robust hazard ratio for heart failure and death at one year based on CRP tertile (1.00, 1.73, and 3.96, respectively).
Bottom line: Ultra-sensitive quantitative CRP levels obtained on admission for acute MI predict one-year risk for heart failure or death. The ability to generalize these results into clinical practice may be limited due to heterogeneity of the studied groups with a higher frequency of diabetes, prior coronary disease, and higher comorbidities in the group that had the highest CRP levels and thus more mortality and heart failure.
Citation: Bursi F, Weston SA, Killian JM, et al. C-reactive protein and heart failure after myocardial infarction in the community. Am J Med. 2007;120(7):616-622.
Do Selective Serotonin Reuptake Inhibitors Confer Cardiac Benefit?
Background: Selective serotonin reuptake inhibitors (SSRIs) theoretically lead to qualitative platelet dysfunction due to inhibition of serotonin-induced platelet activation (and thus resultant inhibition of platelet aggregation and vasoconstriction).
Study design: Retrospective observational study.
Setting: Large teaching hospital in Baltimore.
Synopsis: Of 1,254 patients admitted during the three-year study, 158 patients were on an SSRI at the time of admission. Of the remaining 1,096 patients, a cohort of 158 propensity-matched patients was identified who were statistically similar to the study group in all comorbidities (except for depression, which was higher in the SSRI group).
There were no statistically significant differences between the SSRI group and the propensity-matched group in regards to treatment for acute coronary syndrome (ACS). Almost all received aspirin (98.7% versus 99.4%), clopidogrel (95.6% versus 93.7%), unfractionated heparin (96.8% versus 99.4%), and a glycoprotein IIb/IIIa inhibitor (100% in both).
Patients in the SSRI group had a statistically lower incidence of minor adverse cardiac events (7.0% versus 13.9%), but had increased bleeding events (37.3% versus 26.6%). Minor cardiac events were defined as recurrent EKG findings of ischemia without resultant cardiac enzyme increase, new heart failure, or asymptomatic cardiac enzyme elevation without EKG changes.
Bottom line: Patients taking SSRIs when admitted with an ACS (for an unknown duration) appear to be at lower risk for minor cardiac complications compared with patients not taking an SSRI on admission. These patients also appear to be at elevated risk for bleeding in the setting of maximum antiplatelet and heparin therapy typical in management of ACS.
Citation: Ziegelstein RC, Meuchel J, Kim TJ, et al. Selective serotonin reuptake inhibitor use by patients with acute coronary syndromes. Am J Med. 2007;120(6):525-530.
When Is Vancomycin Superior in Treating C. difficile-Associated Diarrhea?
Background: Epidemic strains of C. difficile raise issues about which antibiotic treatment for C. difficile-associated diarrhea (CDAD) may be superior, particularly due to the availability of more potent antibiotics that can wipe out the protective flora of the intestinal tract.
Study design: Prospec-tive, randomized, double-blind, placebo-controlled trial over 7.5 years.
Setting: A teaching hospital in Chicago.
Synopsis: One hundred seventy-two patients with diarrhea were stratified into mild (fewer than two risks) or severe (two or more risks) disease groups within 48 hours of randomization. These patients were older than 60, with temperature greater than 38.3°C, albumin level lower than 2.5 mg/dL, or peripheral white blood count greater than 15,000 cells/mm. Patients requiring intensive care unit treatment or those with colonscopic evidence of pseudomembranous colitis received an additional risk score of two.
One hundred fifty patients completed the study, 71 in the vancomycin group (125 mg orally, four times a day) and 79 in the metronidazole group (250 mg orally, four times a day). Both groups were similar in composition and numbers of patients with mild and severe CDAD. Patients received placebo plus either vancomycin or metronidazole.
Cure was defined as resolution of diarrhea by day six of therapy and negative C. difficile toxin A assays on days six and 10 of therapy. Results were statistically similar in both treatment groups with mild disease (98% vancomycin versus 90% metronidazole), but favored vancomycin in severe disease (97% versus 76%).
Relapse were not statistically different in either group (7% versus 14%). An albumin level less than 2.5 mg/dL or the presence of colonoscopy-confirmed pseudomembranous colitis showed statistically significant correlation with metronidazole treatment failure (relative risks of 12.70 and 6.67, respectively).
Bottom line: Oral vancomycin, with its commensurate potential for inducing vancomycin-resistant Enterococcus, proved to be equally effective as metronidazole in treating mild CDAD. It was statistically superior to metronidazole in severe disease with hypoalbuminemia and pseudomembranous colitis predicting failure of metronidazole therapy.
Citation: Zar FA, Bakkanagari SR, Moorthi KM, et al. A comparison of vancomycin and metronidazole for the treatment of C. difficile-associated diarrhea, stratified by disease severity. Clin Infect Dis. 2007;45(3):302-307.
What Risk Factors Affect VTE Development in Outpatients?
Background: Decreasing lengths of stay have raised concern that treatments that previously would have continued during the longer hospital stays in the past, such as deep vein thrombosis prophylaxis, may result in unintended adverse consequences after discharge.
Study design: Retrospective observational study
Setting: Worcester, Mass., in 1999, 2001, and 2003, comprising residents who had diagnosis of venous thromboembolism (VTE) at any one of the 12 hospitals in the region
Synopsis: VTE was diagnosed in 1,897 residents (71.1%, 15.0% had pulmonary embolism [PE], and 13.9% had both). Further, 73.7% of the patients presented as an outpatient or were diagnosed within one day of hospital admission.
Compared with inpatients with VTE, outpatients were younger (63.3 years versus 67.4), were less likely to have had a recent infection (18.6% versus 46.8%), central venous catheter (10.4% versus 41.0%), recent fracture (7.3% versus 18.7%), heart failure (4.2% versus 16.5%), cardiac procedures (2.9% versus 7.8%), or recent intensive care unit care stay (8.7% versus 38.2%), but were more likely to have had a prior episode of VTE (19.9% versus 10.2%) or to be taking hormonal therapy (8.0% versus 3.0%).
The prevalence of malignancy was similar in both groups (29.0% versus 32.3%). Most outpatients diagnosed with VTE (59.9%) had been hospitalized in the preceding three months with a majority of VTEs diagnosed within 30 days of discharge. Only 59.7% of those previously hospitalized had any DVT prophylaxis (42.8% received anticoagulants, 16.9% had mechanical prophylaxis).
Bottom line: In an era of decreasing lengths of stay, the possible high level of outpatient VTE attributable to recent hospitalization may be at least partially due to inadequate inpatient pharmacologic VTE prophylaxis in more than 50% of the patients.
Citation: Spencer FA, Lessard D, Emery C, et al. Venous thromboembolism in the outpatient setting. Arch Intern Med. 2007;167(14):1471-1475.
How Has C. difficile Colitis Changed in Severity and Prevalence?
Background: Recent epidemic strains of Clostridium difficile have been reported with several studies suggesting that C. difficile infection has become more serious with risks for sepsis, colectomy, and death.
Study design: Cohort analysis of nationwide inpatient sample (NIS) discharge data for 11 years.
Synopsis: Of the more than 78 million discharge abstracts available for analysis, 299,453 patients were discharged with either a principle or secondary diagnosis of Clostridium difficile colitis (CDC). Demographics trends comparing the early period (1993-1996) versus the middle period (1997-2000) versus the late period (2001-2003) showed CDC incidence:
- Increased in older groups (65.6 years, 66.9 years, 67.6 years);
- Decreased in females (59.8%, 59.1%, 58.9%); and
- Decreased in Caucasians (70.90%, 67.20%, 59.10%).
From 1993 to 2003, the prevalence of CDC discharge diagnoses increased from 261 to 546 cases per 100,000; the colectomy rate due to CDC increased from 1.2 up to 3.4 per 1000, and the case fatality rate statistically significantly increased from 7.84% to 9.26%.
Bottom line: Despite the limitations of using discharge coding abstracts, this study confirms the significantly increasing prevalence (particularly in older, non-Caucasian men) and severity of CDC over the previous decade. This has resulted in a higher incidence of colectomy and death.
Citation: Ricciardi R, Rothenberger DA, Madoff RD. Increasing prevalence and severity of Clostridium difficile colitis in hospitalized patients in the United States. Arch Surg. 2007;142(7):624-631.
How Often Do Clinicians Deviate from Recommended Enoxaparin Doses?
Background: Low molecular heparins have been increasingly utilized in the setting of non-ST-segment elevation myocardial infarctions (NSTEMI) in place of unfractionated heparin. They require careful dose adjustment to ensure appropriate therapeutic effect and prevent bleeding and thrombotic complications.
Study design: Retrospective observational cohort study.
Setting: Medical centers throughout the U.S. that participated in the Can Rapid Risk Stratification of Unstable Angina Patients Suppress Adverse Outcomes with Early Implementation of the ACC/AHA Guidelines (CRUSADE) initiative.
Synopsis: A total of 10,687 patients from 332 hospitals received enoxaparin for NSTEMI as part of CRUSADE. Patients were stratified by whether they received:
- The recommended dose of enoxaparin (1 mg/kg twice daily for glomerular filtration rate (GFR) more than 30 mL/min versus 0.5 mg/kg twice daily for estimated GFR of 30 mL/min or less; 52.1%);
- An excess dose (more than 10 mg/day over recommended dose; 18.7%); or
- A lower-than-recommended dose (more than 10 mg/day less than the recommended dose; 29.2%).
Those receiving an excess dose were more likely to be older, have lower body-mass indexes (BMI), weigh less, be female, have estimated GFRs less than 60 mL/min, and smoke. Those receiving less-than-recommended dosing were more likely to have a higher BMI, weigh more, and be male. Major bleeding episodes (14.2%) and deaths (5.6%) were more common statistically in the excess dose group compared with the recommended dose group (7.3% and 2.4%, respectively). Deaths, but not bleeding, also were higher in the lower-than-recommended dose group (3.3% versus 2.4%).
Bottom line: A little more than half of patients received the correct dose of enoxaparin in NSTEMIs. Those who received too high a dose had marked increases in risk of bleeding and death, and those receiving subtherapeutic doses suffered increased mortality.
Citation: LaPointe NMA, Chen AY, Alexander KP, et al. Enoxaparin dosing and associated risk of in-hospital bleeding and death in patients with non-ST-segment elevation acute coronary syndromes. Arch Intern Med. 2007;167(14):1539-1344.
Does Poor Health Literacy Predict Mortality?
Background: Prior studies have shown increased hospitalization rates in patients with poor health literacy (e.g., inability to comprehend prescriptions or educational materials). At least one study has shown an increase in mortality in 70-to-79-year-olds with impaired health literacy.
Study design: Prospective cohort study.
Setting: Four U.S. metropolitan areas.
Synopsis: Poor health literacy predicts patients’ inability to understand basic health information, such as prescription information, drug dosing intervals, or follow-up schedules. In 1997, 3,260 patients age 65 or older were included in the study, which used a face-to-face standardized test to quantify health literacy.
Patients were tracked via the National Death Index through 2003. Patients were stratified as having adequate, marginal, or inadequate health literacy (64.2%, 11.2%, and 24.5% of patients, respectively). Marginal and inadequate health literacy were strongly associated with increasing age, African American race, lower incomes, lower levels of education, worse physical and mental health, limitations in activities of daily living (ADLs), and lower BMIs. These patients were also less likely to perform vigorous exercise, and less likely to have smoked or used alcohol.
Health literacy (adequate, marginal, or inadequate) predicted unadjusted mortality rates (18.9%, 28.7%, and 39.4%, respectively). Adjusting for socioeconomic status, demographics, and baseline health, all-cause mortality hazard ratios of marginal and inadequate literacy (compared with adequate health literacy) were 1.13 (0.90-1.41 not statistically significant) and 1.52 (1.26-1.83, statistically significant).
Bottom line: Limited data exists regarding how to improve health literacy, and there is no easy bedside test to identify patients with varying levels of literacy. But there appears to be a strong, independent correlation to health literacy and mortality. Physicians need to remain vigilant in their patients’ understanding of their disease, treatment, and follow-up.
Citation: Baker DW, Wolf MS, Feinglass J, et al. Health literacy and mortality among elderly persons. Arch Intern Med. 2007;167(14):1503-1509.
Which Factors Predict Delirium at Discharge?
Background: Delirium at hospital discharge, which can persist for months following hospitalization, may be a contributing factor to dementia, results in increased medical errors during the traditionally high-risk period between discharge and follow-up. Further, it results in serious complications, and, if unrecognized, a high mortality rate.
Study design: Prospective validation model.
Synopsis: A model to predict delirium at hospital discharge was studied in a development cohort of 491 patients age 70 or older who had no evidence of delirium on admission. Of twenty-two different candidate factors, five factors correlated with high odds ratios of delirium at discharge in the 106 (21.6%) of those in the study group who developed delirium: dementia, vision impairment, inability to perform more than one ADL, multiple comorbidities (based on a Charlson score of four or more), and restraint use during delirium.
Patients were stratified into low-risk (zero-one factors), intermediate risk (two-three factors), or high risk (four or more factors) for delirium at hospital discharge. Relative risks (RR) for each group were 1, 4.4, and 15.3, respectively; RR for nursing home placement or death (NHPOD) at one year was 1, 2.4, and 3.4, respectively. A validation cohort of 461 statistically similar patients showed RR for development in the low-, intermediate-, and high-risk groups of 1, 5.4, 10.2, respectively; and RR at one year for NHPOD was 1, 2.7, and 4.4, respectively.
Bottom line: Dementia, vision impairment, inability to perform at least one ADL, multiple comorbidities, and use of restraints are risk factors that can stratify patients into low, intermediate, and high risk for delirium at hospital discharge. Commensurate risks exist for nursing home placement or death at one year.
Citation: Inouye SK, Zhang Y, Jones RN. Risk factors for delirium at discharge. Arch Intern Med. 2007;167(13):1406-1413.
In This Edition
- C-reactive protein levels predict death from cardiac causes after MI.
- SSRIs reduce risk for recurrent cardiac events in acute coronary syndrome.
- Vancomycin is as effective as metronidazole in routine treatment of C. difficile and superior in severe infection.
- Prevalence and severity of C. difficile are increasing in hospitalized patients in the U.S.
- Deviations in recommended enoxaparin dosing in NSTEMI result in worse outcomes.
- Most outpatient VTE events occur in recently hospitalized patients.
- Poor health literacy predicts mortality in older adults.
- A validated model predicts the risk for delirium at hospital discharge.
Do C-reactive Protein Levels Predict Death from Heart Failure?
Background: Ultra-sensitive quantitative assessment of C-reactive protein (CRP), a surrogate marker of systemic inflammation, has previously been shown to predict plaque instability in acute coronary syndromes. Data are lacking as to whether this blood test can also predict subsequent risk of heart failure or death on presentation in patients admitted for acute myocardial infarction (MI).
Study design: Prospec-tive observational study.
Setting: Olmstead County, Minn.
Synopsis: Ultra-sensitive quantitative serum CRP levels were obtained a median of 6.1 hours following onset of symptoms in 329 patients admitted with acute MI. The patients were stratified into tertiles based levels of CRP less than 3 mg/L, 3-15 mg/L, and more than 15 mg/L.
Tertiles were similar in respect to age, male-predominance, most cardiac risk factors, body mass index, and electrocardiographic (EKG) changes. However, there were statistically significant differences between groups, particularly the frequency of diabetes (10.7%, 31.2%, and 38.0%), previous MI history (2.7%, 4.6%, and 9.3%), Killip class greater than one (15.2%, 31.2%, and 39.8%), peak cardiac enzyme levels (both were higher in the bottom tertile, and lowest in the top tertile), and likelihood of significant comorbidities (lower likelihood in the bottom tertile, higher likelihood in the top tertile).
One-year survival was highly correlated with CRP tertile (93%, 84%, and 62% respectively). Once corrected for age, gender, peak cardiac enzymes, Killip class, coronary history, and recurring ischemic events, there remained a robust hazard ratio for heart failure and death at one year based on CRP tertile (1.00, 1.73, and 3.96, respectively).
Bottom line: Ultra-sensitive quantitative CRP levels obtained on admission for acute MI predict one-year risk for heart failure or death. The ability to generalize these results into clinical practice may be limited due to heterogeneity of the studied groups with a higher frequency of diabetes, prior coronary disease, and higher comorbidities in the group that had the highest CRP levels and thus more mortality and heart failure.
Citation: Bursi F, Weston SA, Killian JM, et al. C-reactive protein and heart failure after myocardial infarction in the community. Am J Med. 2007;120(7):616-622.
Do Selective Serotonin Reuptake Inhibitors Confer Cardiac Benefit?
Background: Selective serotonin reuptake inhibitors (SSRIs) theoretically lead to qualitative platelet dysfunction due to inhibition of serotonin-induced platelet activation (and thus resultant inhibition of platelet aggregation and vasoconstriction).
Study design: Retrospective observational study.
Setting: Large teaching hospital in Baltimore.
Synopsis: Of 1,254 patients admitted during the three-year study, 158 patients were on an SSRI at the time of admission. Of the remaining 1,096 patients, a cohort of 158 propensity-matched patients was identified who were statistically similar to the study group in all comorbidities (except for depression, which was higher in the SSRI group).
There were no statistically significant differences between the SSRI group and the propensity-matched group in regards to treatment for acute coronary syndrome (ACS). Almost all received aspirin (98.7% versus 99.4%), clopidogrel (95.6% versus 93.7%), unfractionated heparin (96.8% versus 99.4%), and a glycoprotein IIb/IIIa inhibitor (100% in both).
Patients in the SSRI group had a statistically lower incidence of minor adverse cardiac events (7.0% versus 13.9%), but had increased bleeding events (37.3% versus 26.6%). Minor cardiac events were defined as recurrent EKG findings of ischemia without resultant cardiac enzyme increase, new heart failure, or asymptomatic cardiac enzyme elevation without EKG changes.
Bottom line: Patients taking SSRIs when admitted with an ACS (for an unknown duration) appear to be at lower risk for minor cardiac complications compared with patients not taking an SSRI on admission. These patients also appear to be at elevated risk for bleeding in the setting of maximum antiplatelet and heparin therapy typical in management of ACS.
Citation: Ziegelstein RC, Meuchel J, Kim TJ, et al. Selective serotonin reuptake inhibitor use by patients with acute coronary syndromes. Am J Med. 2007;120(6):525-530.
When Is Vancomycin Superior in Treating C. difficile-Associated Diarrhea?
Background: Epidemic strains of C. difficile raise issues about which antibiotic treatment for C. difficile-associated diarrhea (CDAD) may be superior, particularly due to the availability of more potent antibiotics that can wipe out the protective flora of the intestinal tract.
Study design: Prospec-tive, randomized, double-blind, placebo-controlled trial over 7.5 years.
Setting: A teaching hospital in Chicago.
Synopsis: One hundred seventy-two patients with diarrhea were stratified into mild (fewer than two risks) or severe (two or more risks) disease groups within 48 hours of randomization. These patients were older than 60, with temperature greater than 38.3°C, albumin level lower than 2.5 mg/dL, or peripheral white blood count greater than 15,000 cells/mm. Patients requiring intensive care unit treatment or those with colonscopic evidence of pseudomembranous colitis received an additional risk score of two.
One hundred fifty patients completed the study, 71 in the vancomycin group (125 mg orally, four times a day) and 79 in the metronidazole group (250 mg orally, four times a day). Both groups were similar in composition and numbers of patients with mild and severe CDAD. Patients received placebo plus either vancomycin or metronidazole.
Cure was defined as resolution of diarrhea by day six of therapy and negative C. difficile toxin A assays on days six and 10 of therapy. Results were statistically similar in both treatment groups with mild disease (98% vancomycin versus 90% metronidazole), but favored vancomycin in severe disease (97% versus 76%).
Relapse were not statistically different in either group (7% versus 14%). An albumin level less than 2.5 mg/dL or the presence of colonoscopy-confirmed pseudomembranous colitis showed statistically significant correlation with metronidazole treatment failure (relative risks of 12.70 and 6.67, respectively).
Bottom line: Oral vancomycin, with its commensurate potential for inducing vancomycin-resistant Enterococcus, proved to be equally effective as metronidazole in treating mild CDAD. It was statistically superior to metronidazole in severe disease with hypoalbuminemia and pseudomembranous colitis predicting failure of metronidazole therapy.
Citation: Zar FA, Bakkanagari SR, Moorthi KM, et al. A comparison of vancomycin and metronidazole for the treatment of C. difficile-associated diarrhea, stratified by disease severity. Clin Infect Dis. 2007;45(3):302-307.
What Risk Factors Affect VTE Development in Outpatients?
Background: Decreasing lengths of stay have raised concern that treatments that previously would have continued during the longer hospital stays in the past, such as deep vein thrombosis prophylaxis, may result in unintended adverse consequences after discharge.
Study design: Retrospective observational study
Setting: Worcester, Mass., in 1999, 2001, and 2003, comprising residents who had diagnosis of venous thromboembolism (VTE) at any one of the 12 hospitals in the region
Synopsis: VTE was diagnosed in 1,897 residents (71.1%, 15.0% had pulmonary embolism [PE], and 13.9% had both). Further, 73.7% of the patients presented as an outpatient or were diagnosed within one day of hospital admission.
Compared with inpatients with VTE, outpatients were younger (63.3 years versus 67.4), were less likely to have had a recent infection (18.6% versus 46.8%), central venous catheter (10.4% versus 41.0%), recent fracture (7.3% versus 18.7%), heart failure (4.2% versus 16.5%), cardiac procedures (2.9% versus 7.8%), or recent intensive care unit care stay (8.7% versus 38.2%), but were more likely to have had a prior episode of VTE (19.9% versus 10.2%) or to be taking hormonal therapy (8.0% versus 3.0%).
The prevalence of malignancy was similar in both groups (29.0% versus 32.3%). Most outpatients diagnosed with VTE (59.9%) had been hospitalized in the preceding three months with a majority of VTEs diagnosed within 30 days of discharge. Only 59.7% of those previously hospitalized had any DVT prophylaxis (42.8% received anticoagulants, 16.9% had mechanical prophylaxis).
Bottom line: In an era of decreasing lengths of stay, the possible high level of outpatient VTE attributable to recent hospitalization may be at least partially due to inadequate inpatient pharmacologic VTE prophylaxis in more than 50% of the patients.
Citation: Spencer FA, Lessard D, Emery C, et al. Venous thromboembolism in the outpatient setting. Arch Intern Med. 2007;167(14):1471-1475.
How Has C. difficile Colitis Changed in Severity and Prevalence?
Background: Recent epidemic strains of Clostridium difficile have been reported with several studies suggesting that C. difficile infection has become more serious with risks for sepsis, colectomy, and death.
Study design: Cohort analysis of nationwide inpatient sample (NIS) discharge data for 11 years.
Synopsis: Of the more than 78 million discharge abstracts available for analysis, 299,453 patients were discharged with either a principle or secondary diagnosis of Clostridium difficile colitis (CDC). Demographics trends comparing the early period (1993-1996) versus the middle period (1997-2000) versus the late period (2001-2003) showed CDC incidence:
- Increased in older groups (65.6 years, 66.9 years, 67.6 years);
- Decreased in females (59.8%, 59.1%, 58.9%); and
- Decreased in Caucasians (70.90%, 67.20%, 59.10%).
From 1993 to 2003, the prevalence of CDC discharge diagnoses increased from 261 to 546 cases per 100,000; the colectomy rate due to CDC increased from 1.2 up to 3.4 per 1000, and the case fatality rate statistically significantly increased from 7.84% to 9.26%.
Bottom line: Despite the limitations of using discharge coding abstracts, this study confirms the significantly increasing prevalence (particularly in older, non-Caucasian men) and severity of CDC over the previous decade. This has resulted in a higher incidence of colectomy and death.
Citation: Ricciardi R, Rothenberger DA, Madoff RD. Increasing prevalence and severity of Clostridium difficile colitis in hospitalized patients in the United States. Arch Surg. 2007;142(7):624-631.
How Often Do Clinicians Deviate from Recommended Enoxaparin Doses?
Background: Low molecular heparins have been increasingly utilized in the setting of non-ST-segment elevation myocardial infarctions (NSTEMI) in place of unfractionated heparin. They require careful dose adjustment to ensure appropriate therapeutic effect and prevent bleeding and thrombotic complications.
Study design: Retrospective observational cohort study.
Setting: Medical centers throughout the U.S. that participated in the Can Rapid Risk Stratification of Unstable Angina Patients Suppress Adverse Outcomes with Early Implementation of the ACC/AHA Guidelines (CRUSADE) initiative.
Synopsis: A total of 10,687 patients from 332 hospitals received enoxaparin for NSTEMI as part of CRUSADE. Patients were stratified by whether they received:
- The recommended dose of enoxaparin (1 mg/kg twice daily for glomerular filtration rate (GFR) more than 30 mL/min versus 0.5 mg/kg twice daily for estimated GFR of 30 mL/min or less; 52.1%);
- An excess dose (more than 10 mg/day over recommended dose; 18.7%); or
- A lower-than-recommended dose (more than 10 mg/day less than the recommended dose; 29.2%).
Those receiving an excess dose were more likely to be older, have lower body-mass indexes (BMI), weigh less, be female, have estimated GFRs less than 60 mL/min, and smoke. Those receiving less-than-recommended dosing were more likely to have a higher BMI, weigh more, and be male. Major bleeding episodes (14.2%) and deaths (5.6%) were more common statistically in the excess dose group compared with the recommended dose group (7.3% and 2.4%, respectively). Deaths, but not bleeding, also were higher in the lower-than-recommended dose group (3.3% versus 2.4%).
Bottom line: A little more than half of patients received the correct dose of enoxaparin in NSTEMIs. Those who received too high a dose had marked increases in risk of bleeding and death, and those receiving subtherapeutic doses suffered increased mortality.
Citation: LaPointe NMA, Chen AY, Alexander KP, et al. Enoxaparin dosing and associated risk of in-hospital bleeding and death in patients with non-ST-segment elevation acute coronary syndromes. Arch Intern Med. 2007;167(14):1539-1344.
Does Poor Health Literacy Predict Mortality?
Background: Prior studies have shown increased hospitalization rates in patients with poor health literacy (e.g., inability to comprehend prescriptions or educational materials). At least one study has shown an increase in mortality in 70-to-79-year-olds with impaired health literacy.
Study design: Prospective cohort study.
Setting: Four U.S. metropolitan areas.
Synopsis: Poor health literacy predicts patients’ inability to understand basic health information, such as prescription information, drug dosing intervals, or follow-up schedules. In 1997, 3,260 patients age 65 or older were included in the study, which used a face-to-face standardized test to quantify health literacy.
Patients were tracked via the National Death Index through 2003. Patients were stratified as having adequate, marginal, or inadequate health literacy (64.2%, 11.2%, and 24.5% of patients, respectively). Marginal and inadequate health literacy were strongly associated with increasing age, African American race, lower incomes, lower levels of education, worse physical and mental health, limitations in activities of daily living (ADLs), and lower BMIs. These patients were also less likely to perform vigorous exercise, and less likely to have smoked or used alcohol.
Health literacy (adequate, marginal, or inadequate) predicted unadjusted mortality rates (18.9%, 28.7%, and 39.4%, respectively). Adjusting for socioeconomic status, demographics, and baseline health, all-cause mortality hazard ratios of marginal and inadequate literacy (compared with adequate health literacy) were 1.13 (0.90-1.41 not statistically significant) and 1.52 (1.26-1.83, statistically significant).
Bottom line: Limited data exists regarding how to improve health literacy, and there is no easy bedside test to identify patients with varying levels of literacy. But there appears to be a strong, independent correlation to health literacy and mortality. Physicians need to remain vigilant in their patients’ understanding of their disease, treatment, and follow-up.
Citation: Baker DW, Wolf MS, Feinglass J, et al. Health literacy and mortality among elderly persons. Arch Intern Med. 2007;167(14):1503-1509.
Which Factors Predict Delirium at Discharge?
Background: Delirium at hospital discharge, which can persist for months following hospitalization, may be a contributing factor to dementia, results in increased medical errors during the traditionally high-risk period between discharge and follow-up. Further, it results in serious complications, and, if unrecognized, a high mortality rate.
Study design: Prospective validation model.
Synopsis: A model to predict delirium at hospital discharge was studied in a development cohort of 491 patients age 70 or older who had no evidence of delirium on admission. Of twenty-two different candidate factors, five factors correlated with high odds ratios of delirium at discharge in the 106 (21.6%) of those in the study group who developed delirium: dementia, vision impairment, inability to perform more than one ADL, multiple comorbidities (based on a Charlson score of four or more), and restraint use during delirium.
Patients were stratified into low-risk (zero-one factors), intermediate risk (two-three factors), or high risk (four or more factors) for delirium at hospital discharge. Relative risks (RR) for each group were 1, 4.4, and 15.3, respectively; RR for nursing home placement or death (NHPOD) at one year was 1, 2.4, and 3.4, respectively. A validation cohort of 461 statistically similar patients showed RR for development in the low-, intermediate-, and high-risk groups of 1, 5.4, 10.2, respectively; and RR at one year for NHPOD was 1, 2.7, and 4.4, respectively.
Bottom line: Dementia, vision impairment, inability to perform at least one ADL, multiple comorbidities, and use of restraints are risk factors that can stratify patients into low, intermediate, and high risk for delirium at hospital discharge. Commensurate risks exist for nursing home placement or death at one year.
Citation: Inouye SK, Zhang Y, Jones RN. Risk factors for delirium at discharge. Arch Intern Med. 2007;167(13):1406-1413.
In This Edition
- C-reactive protein levels predict death from cardiac causes after MI.
- SSRIs reduce risk for recurrent cardiac events in acute coronary syndrome.
- Vancomycin is as effective as metronidazole in routine treatment of C. difficile and superior in severe infection.
- Prevalence and severity of C. difficile are increasing in hospitalized patients in the U.S.
- Deviations in recommended enoxaparin dosing in NSTEMI result in worse outcomes.
- Most outpatient VTE events occur in recently hospitalized patients.
- Poor health literacy predicts mortality in older adults.
- A validated model predicts the risk for delirium at hospital discharge.
Do C-reactive Protein Levels Predict Death from Heart Failure?
Background: Ultra-sensitive quantitative assessment of C-reactive protein (CRP), a surrogate marker of systemic inflammation, has previously been shown to predict plaque instability in acute coronary syndromes. Data are lacking as to whether this blood test can also predict subsequent risk of heart failure or death on presentation in patients admitted for acute myocardial infarction (MI).
Study design: Prospec-tive observational study.
Setting: Olmstead County, Minn.
Synopsis: Ultra-sensitive quantitative serum CRP levels were obtained a median of 6.1 hours following onset of symptoms in 329 patients admitted with acute MI. The patients were stratified into tertiles based levels of CRP less than 3 mg/L, 3-15 mg/L, and more than 15 mg/L.
Tertiles were similar in respect to age, male-predominance, most cardiac risk factors, body mass index, and electrocardiographic (EKG) changes. However, there were statistically significant differences between groups, particularly the frequency of diabetes (10.7%, 31.2%, and 38.0%), previous MI history (2.7%, 4.6%, and 9.3%), Killip class greater than one (15.2%, 31.2%, and 39.8%), peak cardiac enzyme levels (both were higher in the bottom tertile, and lowest in the top tertile), and likelihood of significant comorbidities (lower likelihood in the bottom tertile, higher likelihood in the top tertile).
One-year survival was highly correlated with CRP tertile (93%, 84%, and 62% respectively). Once corrected for age, gender, peak cardiac enzymes, Killip class, coronary history, and recurring ischemic events, there remained a robust hazard ratio for heart failure and death at one year based on CRP tertile (1.00, 1.73, and 3.96, respectively).
Bottom line: Ultra-sensitive quantitative CRP levels obtained on admission for acute MI predict one-year risk for heart failure or death. The ability to generalize these results into clinical practice may be limited due to heterogeneity of the studied groups with a higher frequency of diabetes, prior coronary disease, and higher comorbidities in the group that had the highest CRP levels and thus more mortality and heart failure.
Citation: Bursi F, Weston SA, Killian JM, et al. C-reactive protein and heart failure after myocardial infarction in the community. Am J Med. 2007;120(7):616-622.
Do Selective Serotonin Reuptake Inhibitors Confer Cardiac Benefit?
Background: Selective serotonin reuptake inhibitors (SSRIs) theoretically lead to qualitative platelet dysfunction due to inhibition of serotonin-induced platelet activation (and thus resultant inhibition of platelet aggregation and vasoconstriction).
Study design: Retrospective observational study.
Setting: Large teaching hospital in Baltimore.
Synopsis: Of 1,254 patients admitted during the three-year study, 158 patients were on an SSRI at the time of admission. Of the remaining 1,096 patients, a cohort of 158 propensity-matched patients was identified who were statistically similar to the study group in all comorbidities (except for depression, which was higher in the SSRI group).
There were no statistically significant differences between the SSRI group and the propensity-matched group in regards to treatment for acute coronary syndrome (ACS). Almost all received aspirin (98.7% versus 99.4%), clopidogrel (95.6% versus 93.7%), unfractionated heparin (96.8% versus 99.4%), and a glycoprotein IIb/IIIa inhibitor (100% in both).
Patients in the SSRI group had a statistically lower incidence of minor adverse cardiac events (7.0% versus 13.9%), but had increased bleeding events (37.3% versus 26.6%). Minor cardiac events were defined as recurrent EKG findings of ischemia without resultant cardiac enzyme increase, new heart failure, or asymptomatic cardiac enzyme elevation without EKG changes.
Bottom line: Patients taking SSRIs when admitted with an ACS (for an unknown duration) appear to be at lower risk for minor cardiac complications compared with patients not taking an SSRI on admission. These patients also appear to be at elevated risk for bleeding in the setting of maximum antiplatelet and heparin therapy typical in management of ACS.
Citation: Ziegelstein RC, Meuchel J, Kim TJ, et al. Selective serotonin reuptake inhibitor use by patients with acute coronary syndromes. Am J Med. 2007;120(6):525-530.
When Is Vancomycin Superior in Treating C. difficile-Associated Diarrhea?
Background: Epidemic strains of C. difficile raise issues about which antibiotic treatment for C. difficile-associated diarrhea (CDAD) may be superior, particularly due to the availability of more potent antibiotics that can wipe out the protective flora of the intestinal tract.
Study design: Prospec-tive, randomized, double-blind, placebo-controlled trial over 7.5 years.
Setting: A teaching hospital in Chicago.
Synopsis: One hundred seventy-two patients with diarrhea were stratified into mild (fewer than two risks) or severe (two or more risks) disease groups within 48 hours of randomization. These patients were older than 60, with temperature greater than 38.3°C, albumin level lower than 2.5 mg/dL, or peripheral white blood count greater than 15,000 cells/mm. Patients requiring intensive care unit treatment or those with colonscopic evidence of pseudomembranous colitis received an additional risk score of two.
One hundred fifty patients completed the study, 71 in the vancomycin group (125 mg orally, four times a day) and 79 in the metronidazole group (250 mg orally, four times a day). Both groups were similar in composition and numbers of patients with mild and severe CDAD. Patients received placebo plus either vancomycin or metronidazole.
Cure was defined as resolution of diarrhea by day six of therapy and negative C. difficile toxin A assays on days six and 10 of therapy. Results were statistically similar in both treatment groups with mild disease (98% vancomycin versus 90% metronidazole), but favored vancomycin in severe disease (97% versus 76%).
Relapse were not statistically different in either group (7% versus 14%). An albumin level less than 2.5 mg/dL or the presence of colonoscopy-confirmed pseudomembranous colitis showed statistically significant correlation with metronidazole treatment failure (relative risks of 12.70 and 6.67, respectively).
Bottom line: Oral vancomycin, with its commensurate potential for inducing vancomycin-resistant Enterococcus, proved to be equally effective as metronidazole in treating mild CDAD. It was statistically superior to metronidazole in severe disease with hypoalbuminemia and pseudomembranous colitis predicting failure of metronidazole therapy.
Citation: Zar FA, Bakkanagari SR, Moorthi KM, et al. A comparison of vancomycin and metronidazole for the treatment of C. difficile-associated diarrhea, stratified by disease severity. Clin Infect Dis. 2007;45(3):302-307.
What Risk Factors Affect VTE Development in Outpatients?
Background: Decreasing lengths of stay have raised concern that treatments that previously would have continued during the longer hospital stays in the past, such as deep vein thrombosis prophylaxis, may result in unintended adverse consequences after discharge.
Study design: Retrospective observational study
Setting: Worcester, Mass., in 1999, 2001, and 2003, comprising residents who had diagnosis of venous thromboembolism (VTE) at any one of the 12 hospitals in the region
Synopsis: VTE was diagnosed in 1,897 residents (71.1%, 15.0% had pulmonary embolism [PE], and 13.9% had both). Further, 73.7% of the patients presented as an outpatient or were diagnosed within one day of hospital admission.
Compared with inpatients with VTE, outpatients were younger (63.3 years versus 67.4), were less likely to have had a recent infection (18.6% versus 46.8%), central venous catheter (10.4% versus 41.0%), recent fracture (7.3% versus 18.7%), heart failure (4.2% versus 16.5%), cardiac procedures (2.9% versus 7.8%), or recent intensive care unit care stay (8.7% versus 38.2%), but were more likely to have had a prior episode of VTE (19.9% versus 10.2%) or to be taking hormonal therapy (8.0% versus 3.0%).
The prevalence of malignancy was similar in both groups (29.0% versus 32.3%). Most outpatients diagnosed with VTE (59.9%) had been hospitalized in the preceding three months with a majority of VTEs diagnosed within 30 days of discharge. Only 59.7% of those previously hospitalized had any DVT prophylaxis (42.8% received anticoagulants, 16.9% had mechanical prophylaxis).
Bottom line: In an era of decreasing lengths of stay, the possible high level of outpatient VTE attributable to recent hospitalization may be at least partially due to inadequate inpatient pharmacologic VTE prophylaxis in more than 50% of the patients.
Citation: Spencer FA, Lessard D, Emery C, et al. Venous thromboembolism in the outpatient setting. Arch Intern Med. 2007;167(14):1471-1475.
How Has C. difficile Colitis Changed in Severity and Prevalence?
Background: Recent epidemic strains of Clostridium difficile have been reported with several studies suggesting that C. difficile infection has become more serious with risks for sepsis, colectomy, and death.
Study design: Cohort analysis of nationwide inpatient sample (NIS) discharge data for 11 years.
Synopsis: Of the more than 78 million discharge abstracts available for analysis, 299,453 patients were discharged with either a principle or secondary diagnosis of Clostridium difficile colitis (CDC). Demographics trends comparing the early period (1993-1996) versus the middle period (1997-2000) versus the late period (2001-2003) showed CDC incidence:
- Increased in older groups (65.6 years, 66.9 years, 67.6 years);
- Decreased in females (59.8%, 59.1%, 58.9%); and
- Decreased in Caucasians (70.90%, 67.20%, 59.10%).
From 1993 to 2003, the prevalence of CDC discharge diagnoses increased from 261 to 546 cases per 100,000; the colectomy rate due to CDC increased from 1.2 up to 3.4 per 1000, and the case fatality rate statistically significantly increased from 7.84% to 9.26%.
Bottom line: Despite the limitations of using discharge coding abstracts, this study confirms the significantly increasing prevalence (particularly in older, non-Caucasian men) and severity of CDC over the previous decade. This has resulted in a higher incidence of colectomy and death.
Citation: Ricciardi R, Rothenberger DA, Madoff RD. Increasing prevalence and severity of Clostridium difficile colitis in hospitalized patients in the United States. Arch Surg. 2007;142(7):624-631.
How Often Do Clinicians Deviate from Recommended Enoxaparin Doses?
Background: Low molecular heparins have been increasingly utilized in the setting of non-ST-segment elevation myocardial infarctions (NSTEMI) in place of unfractionated heparin. They require careful dose adjustment to ensure appropriate therapeutic effect and prevent bleeding and thrombotic complications.
Study design: Retrospective observational cohort study.
Setting: Medical centers throughout the U.S. that participated in the Can Rapid Risk Stratification of Unstable Angina Patients Suppress Adverse Outcomes with Early Implementation of the ACC/AHA Guidelines (CRUSADE) initiative.
Synopsis: A total of 10,687 patients from 332 hospitals received enoxaparin for NSTEMI as part of CRUSADE. Patients were stratified by whether they received:
- The recommended dose of enoxaparin (1 mg/kg twice daily for glomerular filtration rate (GFR) more than 30 mL/min versus 0.5 mg/kg twice daily for estimated GFR of 30 mL/min or less; 52.1%);
- An excess dose (more than 10 mg/day over recommended dose; 18.7%); or
- A lower-than-recommended dose (more than 10 mg/day less than the recommended dose; 29.2%).
Those receiving an excess dose were more likely to be older, have lower body-mass indexes (BMI), weigh less, be female, have estimated GFRs less than 60 mL/min, and smoke. Those receiving less-than-recommended dosing were more likely to have a higher BMI, weigh more, and be male. Major bleeding episodes (14.2%) and deaths (5.6%) were more common statistically in the excess dose group compared with the recommended dose group (7.3% and 2.4%, respectively). Deaths, but not bleeding, also were higher in the lower-than-recommended dose group (3.3% versus 2.4%).
Bottom line: A little more than half of patients received the correct dose of enoxaparin in NSTEMIs. Those who received too high a dose had marked increases in risk of bleeding and death, and those receiving subtherapeutic doses suffered increased mortality.
Citation: LaPointe NMA, Chen AY, Alexander KP, et al. Enoxaparin dosing and associated risk of in-hospital bleeding and death in patients with non-ST-segment elevation acute coronary syndromes. Arch Intern Med. 2007;167(14):1539-1344.
Does Poor Health Literacy Predict Mortality?
Background: Prior studies have shown increased hospitalization rates in patients with poor health literacy (e.g., inability to comprehend prescriptions or educational materials). At least one study has shown an increase in mortality in 70-to-79-year-olds with impaired health literacy.
Study design: Prospective cohort study.
Setting: Four U.S. metropolitan areas.
Synopsis: Poor health literacy predicts patients’ inability to understand basic health information, such as prescription information, drug dosing intervals, or follow-up schedules. In 1997, 3,260 patients age 65 or older were included in the study, which used a face-to-face standardized test to quantify health literacy.
Patients were tracked via the National Death Index through 2003. Patients were stratified as having adequate, marginal, or inadequate health literacy (64.2%, 11.2%, and 24.5% of patients, respectively). Marginal and inadequate health literacy were strongly associated with increasing age, African American race, lower incomes, lower levels of education, worse physical and mental health, limitations in activities of daily living (ADLs), and lower BMIs. These patients were also less likely to perform vigorous exercise, and less likely to have smoked or used alcohol.
Health literacy (adequate, marginal, or inadequate) predicted unadjusted mortality rates (18.9%, 28.7%, and 39.4%, respectively). Adjusting for socioeconomic status, demographics, and baseline health, all-cause mortality hazard ratios of marginal and inadequate literacy (compared with adequate health literacy) were 1.13 (0.90-1.41 not statistically significant) and 1.52 (1.26-1.83, statistically significant).
Bottom line: Limited data exists regarding how to improve health literacy, and there is no easy bedside test to identify patients with varying levels of literacy. But there appears to be a strong, independent correlation to health literacy and mortality. Physicians need to remain vigilant in their patients’ understanding of their disease, treatment, and follow-up.
Citation: Baker DW, Wolf MS, Feinglass J, et al. Health literacy and mortality among elderly persons. Arch Intern Med. 2007;167(14):1503-1509.
Which Factors Predict Delirium at Discharge?
Background: Delirium at hospital discharge, which can persist for months following hospitalization, may be a contributing factor to dementia, results in increased medical errors during the traditionally high-risk period between discharge and follow-up. Further, it results in serious complications, and, if unrecognized, a high mortality rate.
Study design: Prospective validation model.
Synopsis: A model to predict delirium at hospital discharge was studied in a development cohort of 491 patients age 70 or older who had no evidence of delirium on admission. Of twenty-two different candidate factors, five factors correlated with high odds ratios of delirium at discharge in the 106 (21.6%) of those in the study group who developed delirium: dementia, vision impairment, inability to perform more than one ADL, multiple comorbidities (based on a Charlson score of four or more), and restraint use during delirium.
Patients were stratified into low-risk (zero-one factors), intermediate risk (two-three factors), or high risk (four or more factors) for delirium at hospital discharge. Relative risks (RR) for each group were 1, 4.4, and 15.3, respectively; RR for nursing home placement or death (NHPOD) at one year was 1, 2.4, and 3.4, respectively. A validation cohort of 461 statistically similar patients showed RR for development in the low-, intermediate-, and high-risk groups of 1, 5.4, 10.2, respectively; and RR at one year for NHPOD was 1, 2.7, and 4.4, respectively.
Bottom line: Dementia, vision impairment, inability to perform at least one ADL, multiple comorbidities, and use of restraints are risk factors that can stratify patients into low, intermediate, and high risk for delirium at hospital discharge. Commensurate risks exist for nursing home placement or death at one year.
Citation: Inouye SK, Zhang Y, Jones RN. Risk factors for delirium at discharge. Arch Intern Med. 2007;167(13):1406-1413.
Sixth Annual Southern Regional Meeting Recap
Distinguished by the high quality that has become the trademark of the Society of Hospital Medicine’s meetings, the Sixth Annual Southern Regional Meeting began with a Practice Management pre-course directed by Joseph Miller. The course served as a template of SHM’s prospective educational efforts and generated immense enthusiasm from aTendees. Addressing the spectrum of hospital practices, pioneers of the specialty including Drs. Win Whitcomb and John Nelson presented topics ranging from recruitment to retention. Roger A. Heroux, PhD and Mr. Martin B. Buser emphasized practical means by which hospitalists can demonstrate value and how best to offer “proof” of return-on-investment in hospital practices.
For the first time the Southern Regional Meeting took place outside of Atlanta and with a new co-sponsor, Mayo Clinic. Orlando played host to the near‑record attendance conference that occurred on Walt Disney World property at the Wyndham Palace. The conference also included a new emphasis on families, offering a new spouse/family program that gave attendees and their families discounted tickets to parks and ideas for outings. The overwhelming success of the program suggested this may be a productive addition to other SHM meetings.
Day one of the main conference stressed the latest evidence in hospital medicine. The first plenary sessions focused on the most common cardiac hospital admissions: acute coronary syndromes (Dr. Keith Oken), atrial fibrillation (Dr. Joseph Blackshear), and diastolic heart failure (Dr. Eugene Page).
Given the increasing importance of the hospitalist in management of patients in the perioperative period, the conference then focused on unique aspects of pre-operative and intra-operative care. Perennial favorite Dr. Geno Merli presented data on the (lack of) evidence supporting most preoperative testing, while newcomers Drs. Neil Feinglass and Bruce Leone presented anesthesiologists’ perspectives on the impact of hospitalists on the surgical patient.
Hospitalists are increasingly on the frontlines of trying to minimize error and improve outcomes. Accordingly, early aaernoon topics looked at two issues in this regard: Heparin-Induced Thrombocytopenia (Dr. Jay Herman) and Improving Outcomes in Cardiac Arrest (Dr. Jason Persoff). Then attendees were able to choose from a spectrum of breakout sessions and workshops that ranged from the integration of nurse practitioners/PAs (Dr. Mitchell Wilson) to performing clinical research (Dr. Mike Picco). Dr. Merli held his popular discussion on anticoagulation in the perioperative period. Dr. Bruce Mitchell and Dr. Jared Morton spearheaded two sessions focusing on minorities in hospital medicine and on the unique aspects of hospitalists on physicians in training, respectively. Finally, Dr. Larry Wellikson provided practical information on how to get a job in hospital medicine as one of the closing sessions of the day.
Dr. Beril Cakir chaired the abstract competition at the end of the first day. Thirteen abstracts from over 6 institutions were presented. Dr. Greg Pendell, from Mayo Clinic Jacksonville, was awarded first place and the opportunity to present in April at the Annual Session in Chicago.
Day two built on the theme of hospital medicine’s diversity, with topics ranged from Emerging Infectious Threats (Dr. Walter Hellinger) and the CDC’s Mandate to Reduce Antimicrobial Resistance (Dr. Dan Dressler) to Status Epilepticus (Dr. David Chabolla). Dr. Amir Jaffer spoke about the Cleveland Clinic’s successful preoperative care clinic, while Dr. Archana Roy reviewed the most infl uential research articles to impact the specialty over the past year.
As a leader in advocating tighter glucose control in inpatients, Dr. Guillermo Umpierrez spoke about the paradigm change regarding what is truly considered “good” control of blood sugar in inpatients with diabetes, emphasizing how glucose control can impact mortality. The plenary session closed with an exciting update on the emergence of the specialty of Hospital Medicine by Dr. Larry Wellikson, SHM’s CEO.
Emphasizing the humanity of hospitalists, afternoon workshops included a special workshop by pediatrician Dr. Susie Gerik about the Spiritual Review of Systems, followed by Dr. James Lyman’s workshop on End-of-Life Opportunities for Hospitalists. Both spoke about the emotional aspects of caring for adult patients with severe illness and in those for whom hospice care is the mainstay of therapy.
Dr. Jeff Garland led a standing room only group through various approaches to oxygenation and ventilation in acutely ill patients. Dr. Solomon Tafari presented an evidence-based approach to the unconscious patient, and Dr. Mellena Bridges went over several CT scan case studies. Dr. Mike Picco reviewed the complexity of medical statistics, while Dr. Guillermo Umpierrez gave his perennially popular workshop on endocrine emergencies.
The success of any conference lies not only in the contribution of those who stand before podium, but in the countless movements and machinations that occur behind the scenes to allow a conference to operate so flawlessly. To that end, I would like to commend the herculean job performed by the SHM staff, particularly Angela Musial, Erica Pearson, and Jane Mihelic, whose savvy and dedication gave conference goers a highly organized, orchestrated CME event. The sheer breadth and scope of the speakers and topics presented stem from the creativity and enthusiasm of the conference’s committee members, with special mention to Drs. Donna Dean (the highly under recognized but not under appreciated assistant course director), Ryan McNamara, Mitchell Wilson, Patrick Cawley, Beril Cakir, and Ron Angus.
I would like to close with special acknowledgement of those whose great vision and leadership have guided this annual event and served as a focal point for SHM’s emergence: Dr. Mark Williams and Dr. Larry Wellikson. I thank you both.
Dr. Williams and Emory University plan to continue the annual autumn meeting, which will return to Atlanta in November, 2005.
Distinguished by the high quality that has become the trademark of the Society of Hospital Medicine’s meetings, the Sixth Annual Southern Regional Meeting began with a Practice Management pre-course directed by Joseph Miller. The course served as a template of SHM’s prospective educational efforts and generated immense enthusiasm from aTendees. Addressing the spectrum of hospital practices, pioneers of the specialty including Drs. Win Whitcomb and John Nelson presented topics ranging from recruitment to retention. Roger A. Heroux, PhD and Mr. Martin B. Buser emphasized practical means by which hospitalists can demonstrate value and how best to offer “proof” of return-on-investment in hospital practices.
For the first time the Southern Regional Meeting took place outside of Atlanta and with a new co-sponsor, Mayo Clinic. Orlando played host to the near‑record attendance conference that occurred on Walt Disney World property at the Wyndham Palace. The conference also included a new emphasis on families, offering a new spouse/family program that gave attendees and their families discounted tickets to parks and ideas for outings. The overwhelming success of the program suggested this may be a productive addition to other SHM meetings.
Day one of the main conference stressed the latest evidence in hospital medicine. The first plenary sessions focused on the most common cardiac hospital admissions: acute coronary syndromes (Dr. Keith Oken), atrial fibrillation (Dr. Joseph Blackshear), and diastolic heart failure (Dr. Eugene Page).
Given the increasing importance of the hospitalist in management of patients in the perioperative period, the conference then focused on unique aspects of pre-operative and intra-operative care. Perennial favorite Dr. Geno Merli presented data on the (lack of) evidence supporting most preoperative testing, while newcomers Drs. Neil Feinglass and Bruce Leone presented anesthesiologists’ perspectives on the impact of hospitalists on the surgical patient.
Hospitalists are increasingly on the frontlines of trying to minimize error and improve outcomes. Accordingly, early aaernoon topics looked at two issues in this regard: Heparin-Induced Thrombocytopenia (Dr. Jay Herman) and Improving Outcomes in Cardiac Arrest (Dr. Jason Persoff). Then attendees were able to choose from a spectrum of breakout sessions and workshops that ranged from the integration of nurse practitioners/PAs (Dr. Mitchell Wilson) to performing clinical research (Dr. Mike Picco). Dr. Merli held his popular discussion on anticoagulation in the perioperative period. Dr. Bruce Mitchell and Dr. Jared Morton spearheaded two sessions focusing on minorities in hospital medicine and on the unique aspects of hospitalists on physicians in training, respectively. Finally, Dr. Larry Wellikson provided practical information on how to get a job in hospital medicine as one of the closing sessions of the day.
Dr. Beril Cakir chaired the abstract competition at the end of the first day. Thirteen abstracts from over 6 institutions were presented. Dr. Greg Pendell, from Mayo Clinic Jacksonville, was awarded first place and the opportunity to present in April at the Annual Session in Chicago.
Day two built on the theme of hospital medicine’s diversity, with topics ranged from Emerging Infectious Threats (Dr. Walter Hellinger) and the CDC’s Mandate to Reduce Antimicrobial Resistance (Dr. Dan Dressler) to Status Epilepticus (Dr. David Chabolla). Dr. Amir Jaffer spoke about the Cleveland Clinic’s successful preoperative care clinic, while Dr. Archana Roy reviewed the most infl uential research articles to impact the specialty over the past year.
As a leader in advocating tighter glucose control in inpatients, Dr. Guillermo Umpierrez spoke about the paradigm change regarding what is truly considered “good” control of blood sugar in inpatients with diabetes, emphasizing how glucose control can impact mortality. The plenary session closed with an exciting update on the emergence of the specialty of Hospital Medicine by Dr. Larry Wellikson, SHM’s CEO.
Emphasizing the humanity of hospitalists, afternoon workshops included a special workshop by pediatrician Dr. Susie Gerik about the Spiritual Review of Systems, followed by Dr. James Lyman’s workshop on End-of-Life Opportunities for Hospitalists. Both spoke about the emotional aspects of caring for adult patients with severe illness and in those for whom hospice care is the mainstay of therapy.
Dr. Jeff Garland led a standing room only group through various approaches to oxygenation and ventilation in acutely ill patients. Dr. Solomon Tafari presented an evidence-based approach to the unconscious patient, and Dr. Mellena Bridges went over several CT scan case studies. Dr. Mike Picco reviewed the complexity of medical statistics, while Dr. Guillermo Umpierrez gave his perennially popular workshop on endocrine emergencies.
The success of any conference lies not only in the contribution of those who stand before podium, but in the countless movements and machinations that occur behind the scenes to allow a conference to operate so flawlessly. To that end, I would like to commend the herculean job performed by the SHM staff, particularly Angela Musial, Erica Pearson, and Jane Mihelic, whose savvy and dedication gave conference goers a highly organized, orchestrated CME event. The sheer breadth and scope of the speakers and topics presented stem from the creativity and enthusiasm of the conference’s committee members, with special mention to Drs. Donna Dean (the highly under recognized but not under appreciated assistant course director), Ryan McNamara, Mitchell Wilson, Patrick Cawley, Beril Cakir, and Ron Angus.
I would like to close with special acknowledgement of those whose great vision and leadership have guided this annual event and served as a focal point for SHM’s emergence: Dr. Mark Williams and Dr. Larry Wellikson. I thank you both.
Dr. Williams and Emory University plan to continue the annual autumn meeting, which will return to Atlanta in November, 2005.
Distinguished by the high quality that has become the trademark of the Society of Hospital Medicine’s meetings, the Sixth Annual Southern Regional Meeting began with a Practice Management pre-course directed by Joseph Miller. The course served as a template of SHM’s prospective educational efforts and generated immense enthusiasm from aTendees. Addressing the spectrum of hospital practices, pioneers of the specialty including Drs. Win Whitcomb and John Nelson presented topics ranging from recruitment to retention. Roger A. Heroux, PhD and Mr. Martin B. Buser emphasized practical means by which hospitalists can demonstrate value and how best to offer “proof” of return-on-investment in hospital practices.
For the first time the Southern Regional Meeting took place outside of Atlanta and with a new co-sponsor, Mayo Clinic. Orlando played host to the near‑record attendance conference that occurred on Walt Disney World property at the Wyndham Palace. The conference also included a new emphasis on families, offering a new spouse/family program that gave attendees and their families discounted tickets to parks and ideas for outings. The overwhelming success of the program suggested this may be a productive addition to other SHM meetings.
Day one of the main conference stressed the latest evidence in hospital medicine. The first plenary sessions focused on the most common cardiac hospital admissions: acute coronary syndromes (Dr. Keith Oken), atrial fibrillation (Dr. Joseph Blackshear), and diastolic heart failure (Dr. Eugene Page).
Given the increasing importance of the hospitalist in management of patients in the perioperative period, the conference then focused on unique aspects of pre-operative and intra-operative care. Perennial favorite Dr. Geno Merli presented data on the (lack of) evidence supporting most preoperative testing, while newcomers Drs. Neil Feinglass and Bruce Leone presented anesthesiologists’ perspectives on the impact of hospitalists on the surgical patient.
Hospitalists are increasingly on the frontlines of trying to minimize error and improve outcomes. Accordingly, early aaernoon topics looked at two issues in this regard: Heparin-Induced Thrombocytopenia (Dr. Jay Herman) and Improving Outcomes in Cardiac Arrest (Dr. Jason Persoff). Then attendees were able to choose from a spectrum of breakout sessions and workshops that ranged from the integration of nurse practitioners/PAs (Dr. Mitchell Wilson) to performing clinical research (Dr. Mike Picco). Dr. Merli held his popular discussion on anticoagulation in the perioperative period. Dr. Bruce Mitchell and Dr. Jared Morton spearheaded two sessions focusing on minorities in hospital medicine and on the unique aspects of hospitalists on physicians in training, respectively. Finally, Dr. Larry Wellikson provided practical information on how to get a job in hospital medicine as one of the closing sessions of the day.
Dr. Beril Cakir chaired the abstract competition at the end of the first day. Thirteen abstracts from over 6 institutions were presented. Dr. Greg Pendell, from Mayo Clinic Jacksonville, was awarded first place and the opportunity to present in April at the Annual Session in Chicago.
Day two built on the theme of hospital medicine’s diversity, with topics ranged from Emerging Infectious Threats (Dr. Walter Hellinger) and the CDC’s Mandate to Reduce Antimicrobial Resistance (Dr. Dan Dressler) to Status Epilepticus (Dr. David Chabolla). Dr. Amir Jaffer spoke about the Cleveland Clinic’s successful preoperative care clinic, while Dr. Archana Roy reviewed the most infl uential research articles to impact the specialty over the past year.
As a leader in advocating tighter glucose control in inpatients, Dr. Guillermo Umpierrez spoke about the paradigm change regarding what is truly considered “good” control of blood sugar in inpatients with diabetes, emphasizing how glucose control can impact mortality. The plenary session closed with an exciting update on the emergence of the specialty of Hospital Medicine by Dr. Larry Wellikson, SHM’s CEO.
Emphasizing the humanity of hospitalists, afternoon workshops included a special workshop by pediatrician Dr. Susie Gerik about the Spiritual Review of Systems, followed by Dr. James Lyman’s workshop on End-of-Life Opportunities for Hospitalists. Both spoke about the emotional aspects of caring for adult patients with severe illness and in those for whom hospice care is the mainstay of therapy.
Dr. Jeff Garland led a standing room only group through various approaches to oxygenation and ventilation in acutely ill patients. Dr. Solomon Tafari presented an evidence-based approach to the unconscious patient, and Dr. Mellena Bridges went over several CT scan case studies. Dr. Mike Picco reviewed the complexity of medical statistics, while Dr. Guillermo Umpierrez gave his perennially popular workshop on endocrine emergencies.
The success of any conference lies not only in the contribution of those who stand before podium, but in the countless movements and machinations that occur behind the scenes to allow a conference to operate so flawlessly. To that end, I would like to commend the herculean job performed by the SHM staff, particularly Angela Musial, Erica Pearson, and Jane Mihelic, whose savvy and dedication gave conference goers a highly organized, orchestrated CME event. The sheer breadth and scope of the speakers and topics presented stem from the creativity and enthusiasm of the conference’s committee members, with special mention to Drs. Donna Dean (the highly under recognized but not under appreciated assistant course director), Ryan McNamara, Mitchell Wilson, Patrick Cawley, Beril Cakir, and Ron Angus.
I would like to close with special acknowledgement of those whose great vision and leadership have guided this annual event and served as a focal point for SHM’s emergence: Dr. Mark Williams and Dr. Larry Wellikson. I thank you both.
Dr. Williams and Emory University plan to continue the annual autumn meeting, which will return to Atlanta in November, 2005.