User login
Caplacizumab improves outcomes in aTTP
ATLANTA—Caplacizumab can improve outcomes in patients with acquired thrombotic thrombocytopenic purpura (aTTP), according to research presented at the 2017 ASH Annual Meeting.
In the phase 3 HERCULES trial, researchers compared caplacizumab, an anti-von Willebrand factor nanobody, plus standard care (plasma exchange and immunosuppression) to placebo plus standard care in patients with aTTP.
Patients who received caplacizumab were significantly more likely to achieve platelet normalization and significantly less likely to experience aTTP-related death, aTTP recurrence, and major thromboembolic events.
Patients in the caplacizumab arm also required plasma exchange less frequently and spent less time in the hospital and intensive care unit (ICU).
Bleeding-related adverse events (AEs) were more common among patients who received caplacizumab than those who received placebo.
Marie Scully, MD, of the University College London Hospitals in London, UK, presented these results from HERCULES as a late-breaking abstract at the ASH Annual Meeting (abstract LBA-1). HERCULES was supported by Ablynx.
Patients and treatment
The study enrolled patients with an acute episode of aTTP. They were randomized to receive either caplacizumab (n=72) or placebo (n=73) in addition to standard care, which consisted of plasma exchange and immunosuppression.
Patients received a single intravenous bolus of 10 mg of caplacizumab or placebo followed by a daily subcutaneous dose of 10 mg of caplacizumab or placebo until 30 days after the last daily plasma exchange. If patients had a recurrence during the 30-day treatment period, they could go on to receive open-label caplacizumab.
If, at the end of the 30-day treatment period, there was evidence of persistent underlying disease activity indicative of an imminent risk for recurrence, caplacizumab or placebo could be extended for additional 7-day periods up to a maximum of 28 days. Patients were followed for a further 28 days after discontinuation of treatment.
In all, 71 patients received caplacizumab, and 58 (80.6%) of them completed the treatment. Seventy-three patients received placebo, and 50 of these patients (68.5%) completed treatment. Twenty-six patients in the placebo arm and 2 patients in the caplacizumab arm received open-label caplacizumab.
“If we look at the demographics, they’re relatively comparable to any data we normally see in patients with immune-mediated TTP,” Dr Scully said.
At baseline, the mean age was 44.9 in the caplacizumab arm and 47.3 in the placebo arm. Most patients in both arms were female—68.1% and 69.9%, respectively.
The proportion of patients with an initial aTTP episode was 66.7% in the caplacizumab arm and 46.6% in the placebo arm. The proportion with a recurrent episode was 33.3% and 53.4%, respectively.
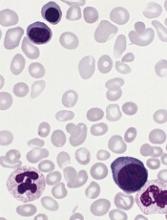
Most patients in both arms had ADAMTS13 activity below 10% at baseline—81.7% in the caplacizumab arm and 90.3% in the placebo arm.
The mean platelet count at baseline was 32.0 x 109/L in the caplacizumab arm and 39.1 x 109/L in the placebo arm.
Efficacy
The study’s primary endpoint was the time to normalization of platelet count response, which was defined as initial platelet count of at least 150 x 109/L with subsequent stop of daily plasma exchange within 5 days.
There was a significant reduction in time to platelet count response in the caplacizumab arm compared to the placebo arm. The platelet normalization rate ratio was 1.55 (P<0.01).
“Patients were 55% more likely to achieve normalization of their platelet count at any time in the caplacizumab group, and this was highly significant,” Dr Scully said.
A secondary endpoint was the combination of aTTP-related death, aTTP recurrence, and at least 1 major thromboembolic event during study treatment. The incidence of this combined endpoint was 12.7% (n=9) in the caplacizumab arm and 49.3% (n=36) in the placebo arm (P<0.0001).
The incidence of aTTP-related death was 0% (n=0) in the caplacizumab arm and 4.1% (n=3) in the placebo arm. The incidence of aTTP recurrence was 4.2% (n=3) and 38.4% (n=28), respectively. And the incidence of at least 1 major thromboembolic event was 8.5% (n=6) and 8.2% (n=6), respectively.
The researchers also assessed aTTP recurrence during the overall study period, which occurred in 12.7% (n=9) of patients in the caplacizumab arm and 38.4% (n=28) in the placebo arm (P<0.001).
During the follow-up period, there were 6 relapses (9.1%) in the caplacizumab arm but none in the placebo arm.
“This tells us something about the pathophysiology of TTP and the role of caplacizumab,” Dr Scully said. “All of these patients, on stopping caplacizumab, had ADAMTS13 levels less than 5%. Therefore, it was important that their treatment was continued to ensure removal of antibody.”
According to the International TTP Working Group consensus definition, none of the patients in the caplacizumab arm and 7.0% (n=5) of patients in the placebo arm had refractory aTTP (P=0.018).
The mean number of days of plasma exchange during the overall treatment period was 5.8 days in the caplacizumab arm and 9.4 days in the placebo arm (a 38% relative reduction). The mean volume of plasma used was 21.3L and 35.9L, respectively (a 41% relative reduction).
The mean duration of hospital stay was 9.9 days in the caplacizumab arm and 14.4 days in the placebo arm (a 31% relative reduction).
For patients admitted to the ICU (28 in the caplacizumab arm and 27 in the placebo arm), the mean number of days in the ICU was 3.4 days in the caplacizumab arm and 9.7 days in the placebo arm (a 65% relative reduction).
Safety
“The safety profile [of caplacizumab] was comparable to previous results and in keeping with the mechanism of action,” Dr Scully said.
The proportion of patients with at least 1 treatment-emergent AE was 97.2% in the caplacizumab arm and 97.3% in the placebo arm.
The proportion of patients with at least 1 study-drug-related AE was 57.7% in the caplacizumab arm and 43.8% in the placebo arm. The rate of discontinuation due to at least 1 AE was 7.0% and 12.3%, respectively.
The incidence of bleeding-related AEs was higher in the caplacizumab arm (45.6%) than the placebo arm (23.3%).
Bleeding-related AEs (in the caplacizumab and placebo arms, respectively) included epistaxis (23.9% and 1.4%), gingival bleeding (11.3% and 0%), bruising (7.0% and 4.1%), hematuria (5.6% and 1.4%), vaginal hemorrhage (4.2% and 1.4%), menorrhagia (2.8% and 1.4%), catheter site hemorrhage (2.8% and 4.1%), injection site bruising (2.8% and 2.7%), hematochezia (2.8% and 0%), and hematoma (2.8% and 0%).
The proportion of patients with at least 1 serious AE was 39.4% (n=28) in the caplacizumab arm and 53.4% (n=39) in the placebo arm. The proportion of patients with at least 1 study-drug-related serious AE was 14.1% (n=10) and 5.5% (n=4), respectively.
During the treatment period, there were no deaths in the caplacizumab arm and 3 deaths in the placebo arm. There was 1 death in the caplacizumab arm during the follow-up period, but it was considered unrelated to caplacizumab. ![]()
ATLANTA—Caplacizumab can improve outcomes in patients with acquired thrombotic thrombocytopenic purpura (aTTP), according to research presented at the 2017 ASH Annual Meeting.
In the phase 3 HERCULES trial, researchers compared caplacizumab, an anti-von Willebrand factor nanobody, plus standard care (plasma exchange and immunosuppression) to placebo plus standard care in patients with aTTP.
Patients who received caplacizumab were significantly more likely to achieve platelet normalization and significantly less likely to experience aTTP-related death, aTTP recurrence, and major thromboembolic events.
Patients in the caplacizumab arm also required plasma exchange less frequently and spent less time in the hospital and intensive care unit (ICU).
Bleeding-related adverse events (AEs) were more common among patients who received caplacizumab than those who received placebo.
Marie Scully, MD, of the University College London Hospitals in London, UK, presented these results from HERCULES as a late-breaking abstract at the ASH Annual Meeting (abstract LBA-1). HERCULES was supported by Ablynx.
Patients and treatment
The study enrolled patients with an acute episode of aTTP. They were randomized to receive either caplacizumab (n=72) or placebo (n=73) in addition to standard care, which consisted of plasma exchange and immunosuppression.
Patients received a single intravenous bolus of 10 mg of caplacizumab or placebo followed by a daily subcutaneous dose of 10 mg of caplacizumab or placebo until 30 days after the last daily plasma exchange. If patients had a recurrence during the 30-day treatment period, they could go on to receive open-label caplacizumab.
If, at the end of the 30-day treatment period, there was evidence of persistent underlying disease activity indicative of an imminent risk for recurrence, caplacizumab or placebo could be extended for additional 7-day periods up to a maximum of 28 days. Patients were followed for a further 28 days after discontinuation of treatment.
In all, 71 patients received caplacizumab, and 58 (80.6%) of them completed the treatment. Seventy-three patients received placebo, and 50 of these patients (68.5%) completed treatment. Twenty-six patients in the placebo arm and 2 patients in the caplacizumab arm received open-label caplacizumab.
“If we look at the demographics, they’re relatively comparable to any data we normally see in patients with immune-mediated TTP,” Dr Scully said.
At baseline, the mean age was 44.9 in the caplacizumab arm and 47.3 in the placebo arm. Most patients in both arms were female—68.1% and 69.9%, respectively.
The proportion of patients with an initial aTTP episode was 66.7% in the caplacizumab arm and 46.6% in the placebo arm. The proportion with a recurrent episode was 33.3% and 53.4%, respectively.
Most patients in both arms had ADAMTS13 activity below 10% at baseline—81.7% in the caplacizumab arm and 90.3% in the placebo arm.
The mean platelet count at baseline was 32.0 x 109/L in the caplacizumab arm and 39.1 x 109/L in the placebo arm.
Efficacy
The study’s primary endpoint was the time to normalization of platelet count response, which was defined as initial platelet count of at least 150 x 109/L with subsequent stop of daily plasma exchange within 5 days.
There was a significant reduction in time to platelet count response in the caplacizumab arm compared to the placebo arm. The platelet normalization rate ratio was 1.55 (P<0.01).
“Patients were 55% more likely to achieve normalization of their platelet count at any time in the caplacizumab group, and this was highly significant,” Dr Scully said.
A secondary endpoint was the combination of aTTP-related death, aTTP recurrence, and at least 1 major thromboembolic event during study treatment. The incidence of this combined endpoint was 12.7% (n=9) in the caplacizumab arm and 49.3% (n=36) in the placebo arm (P<0.0001).
The incidence of aTTP-related death was 0% (n=0) in the caplacizumab arm and 4.1% (n=3) in the placebo arm. The incidence of aTTP recurrence was 4.2% (n=3) and 38.4% (n=28), respectively. And the incidence of at least 1 major thromboembolic event was 8.5% (n=6) and 8.2% (n=6), respectively.
The researchers also assessed aTTP recurrence during the overall study period, which occurred in 12.7% (n=9) of patients in the caplacizumab arm and 38.4% (n=28) in the placebo arm (P<0.001).
During the follow-up period, there were 6 relapses (9.1%) in the caplacizumab arm but none in the placebo arm.
“This tells us something about the pathophysiology of TTP and the role of caplacizumab,” Dr Scully said. “All of these patients, on stopping caplacizumab, had ADAMTS13 levels less than 5%. Therefore, it was important that their treatment was continued to ensure removal of antibody.”
According to the International TTP Working Group consensus definition, none of the patients in the caplacizumab arm and 7.0% (n=5) of patients in the placebo arm had refractory aTTP (P=0.018).
The mean number of days of plasma exchange during the overall treatment period was 5.8 days in the caplacizumab arm and 9.4 days in the placebo arm (a 38% relative reduction). The mean volume of plasma used was 21.3L and 35.9L, respectively (a 41% relative reduction).
The mean duration of hospital stay was 9.9 days in the caplacizumab arm and 14.4 days in the placebo arm (a 31% relative reduction).
For patients admitted to the ICU (28 in the caplacizumab arm and 27 in the placebo arm), the mean number of days in the ICU was 3.4 days in the caplacizumab arm and 9.7 days in the placebo arm (a 65% relative reduction).
Safety
“The safety profile [of caplacizumab] was comparable to previous results and in keeping with the mechanism of action,” Dr Scully said.
The proportion of patients with at least 1 treatment-emergent AE was 97.2% in the caplacizumab arm and 97.3% in the placebo arm.
The proportion of patients with at least 1 study-drug-related AE was 57.7% in the caplacizumab arm and 43.8% in the placebo arm. The rate of discontinuation due to at least 1 AE was 7.0% and 12.3%, respectively.
The incidence of bleeding-related AEs was higher in the caplacizumab arm (45.6%) than the placebo arm (23.3%).
Bleeding-related AEs (in the caplacizumab and placebo arms, respectively) included epistaxis (23.9% and 1.4%), gingival bleeding (11.3% and 0%), bruising (7.0% and 4.1%), hematuria (5.6% and 1.4%), vaginal hemorrhage (4.2% and 1.4%), menorrhagia (2.8% and 1.4%), catheter site hemorrhage (2.8% and 4.1%), injection site bruising (2.8% and 2.7%), hematochezia (2.8% and 0%), and hematoma (2.8% and 0%).
The proportion of patients with at least 1 serious AE was 39.4% (n=28) in the caplacizumab arm and 53.4% (n=39) in the placebo arm. The proportion of patients with at least 1 study-drug-related serious AE was 14.1% (n=10) and 5.5% (n=4), respectively.
During the treatment period, there were no deaths in the caplacizumab arm and 3 deaths in the placebo arm. There was 1 death in the caplacizumab arm during the follow-up period, but it was considered unrelated to caplacizumab. ![]()
ATLANTA—Caplacizumab can improve outcomes in patients with acquired thrombotic thrombocytopenic purpura (aTTP), according to research presented at the 2017 ASH Annual Meeting.
In the phase 3 HERCULES trial, researchers compared caplacizumab, an anti-von Willebrand factor nanobody, plus standard care (plasma exchange and immunosuppression) to placebo plus standard care in patients with aTTP.
Patients who received caplacizumab were significantly more likely to achieve platelet normalization and significantly less likely to experience aTTP-related death, aTTP recurrence, and major thromboembolic events.
Patients in the caplacizumab arm also required plasma exchange less frequently and spent less time in the hospital and intensive care unit (ICU).
Bleeding-related adverse events (AEs) were more common among patients who received caplacizumab than those who received placebo.
Marie Scully, MD, of the University College London Hospitals in London, UK, presented these results from HERCULES as a late-breaking abstract at the ASH Annual Meeting (abstract LBA-1). HERCULES was supported by Ablynx.
Patients and treatment
The study enrolled patients with an acute episode of aTTP. They were randomized to receive either caplacizumab (n=72) or placebo (n=73) in addition to standard care, which consisted of plasma exchange and immunosuppression.
Patients received a single intravenous bolus of 10 mg of caplacizumab or placebo followed by a daily subcutaneous dose of 10 mg of caplacizumab or placebo until 30 days after the last daily plasma exchange. If patients had a recurrence during the 30-day treatment period, they could go on to receive open-label caplacizumab.
If, at the end of the 30-day treatment period, there was evidence of persistent underlying disease activity indicative of an imminent risk for recurrence, caplacizumab or placebo could be extended for additional 7-day periods up to a maximum of 28 days. Patients were followed for a further 28 days after discontinuation of treatment.
In all, 71 patients received caplacizumab, and 58 (80.6%) of them completed the treatment. Seventy-three patients received placebo, and 50 of these patients (68.5%) completed treatment. Twenty-six patients in the placebo arm and 2 patients in the caplacizumab arm received open-label caplacizumab.
“If we look at the demographics, they’re relatively comparable to any data we normally see in patients with immune-mediated TTP,” Dr Scully said.
At baseline, the mean age was 44.9 in the caplacizumab arm and 47.3 in the placebo arm. Most patients in both arms were female—68.1% and 69.9%, respectively.
The proportion of patients with an initial aTTP episode was 66.7% in the caplacizumab arm and 46.6% in the placebo arm. The proportion with a recurrent episode was 33.3% and 53.4%, respectively.
Most patients in both arms had ADAMTS13 activity below 10% at baseline—81.7% in the caplacizumab arm and 90.3% in the placebo arm.
The mean platelet count at baseline was 32.0 x 109/L in the caplacizumab arm and 39.1 x 109/L in the placebo arm.
Efficacy
The study’s primary endpoint was the time to normalization of platelet count response, which was defined as initial platelet count of at least 150 x 109/L with subsequent stop of daily plasma exchange within 5 days.
There was a significant reduction in time to platelet count response in the caplacizumab arm compared to the placebo arm. The platelet normalization rate ratio was 1.55 (P<0.01).
“Patients were 55% more likely to achieve normalization of their platelet count at any time in the caplacizumab group, and this was highly significant,” Dr Scully said.
A secondary endpoint was the combination of aTTP-related death, aTTP recurrence, and at least 1 major thromboembolic event during study treatment. The incidence of this combined endpoint was 12.7% (n=9) in the caplacizumab arm and 49.3% (n=36) in the placebo arm (P<0.0001).
The incidence of aTTP-related death was 0% (n=0) in the caplacizumab arm and 4.1% (n=3) in the placebo arm. The incidence of aTTP recurrence was 4.2% (n=3) and 38.4% (n=28), respectively. And the incidence of at least 1 major thromboembolic event was 8.5% (n=6) and 8.2% (n=6), respectively.
The researchers also assessed aTTP recurrence during the overall study period, which occurred in 12.7% (n=9) of patients in the caplacizumab arm and 38.4% (n=28) in the placebo arm (P<0.001).
During the follow-up period, there were 6 relapses (9.1%) in the caplacizumab arm but none in the placebo arm.
“This tells us something about the pathophysiology of TTP and the role of caplacizumab,” Dr Scully said. “All of these patients, on stopping caplacizumab, had ADAMTS13 levels less than 5%. Therefore, it was important that their treatment was continued to ensure removal of antibody.”
According to the International TTP Working Group consensus definition, none of the patients in the caplacizumab arm and 7.0% (n=5) of patients in the placebo arm had refractory aTTP (P=0.018).
The mean number of days of plasma exchange during the overall treatment period was 5.8 days in the caplacizumab arm and 9.4 days in the placebo arm (a 38% relative reduction). The mean volume of plasma used was 21.3L and 35.9L, respectively (a 41% relative reduction).
The mean duration of hospital stay was 9.9 days in the caplacizumab arm and 14.4 days in the placebo arm (a 31% relative reduction).
For patients admitted to the ICU (28 in the caplacizumab arm and 27 in the placebo arm), the mean number of days in the ICU was 3.4 days in the caplacizumab arm and 9.7 days in the placebo arm (a 65% relative reduction).
Safety
“The safety profile [of caplacizumab] was comparable to previous results and in keeping with the mechanism of action,” Dr Scully said.
The proportion of patients with at least 1 treatment-emergent AE was 97.2% in the caplacizumab arm and 97.3% in the placebo arm.
The proportion of patients with at least 1 study-drug-related AE was 57.7% in the caplacizumab arm and 43.8% in the placebo arm. The rate of discontinuation due to at least 1 AE was 7.0% and 12.3%, respectively.
The incidence of bleeding-related AEs was higher in the caplacizumab arm (45.6%) than the placebo arm (23.3%).
Bleeding-related AEs (in the caplacizumab and placebo arms, respectively) included epistaxis (23.9% and 1.4%), gingival bleeding (11.3% and 0%), bruising (7.0% and 4.1%), hematuria (5.6% and 1.4%), vaginal hemorrhage (4.2% and 1.4%), menorrhagia (2.8% and 1.4%), catheter site hemorrhage (2.8% and 4.1%), injection site bruising (2.8% and 2.7%), hematochezia (2.8% and 0%), and hematoma (2.8% and 0%).
The proportion of patients with at least 1 serious AE was 39.4% (n=28) in the caplacizumab arm and 53.4% (n=39) in the placebo arm. The proportion of patients with at least 1 study-drug-related serious AE was 14.1% (n=10) and 5.5% (n=4), respectively.
During the treatment period, there were no deaths in the caplacizumab arm and 3 deaths in the placebo arm. There was 1 death in the caplacizumab arm during the follow-up period, but it was considered unrelated to caplacizumab. ![]()
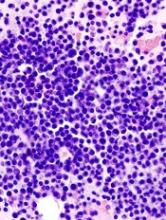
Chemo-free combo should be option for rel/ref CLL, doc says
ATLANTA—The combination of venetoclax and rituximab (VR) should be a standard treatment option for adults with relapsed/refractory chronic lymphocytic leukemia (CLL), according to a speaker at the 2017 ASH Annual Meeting.
Data from the phase 3 MURANO study showed that patients with relapsed/refractory CLL who received VR had significantly longer progression-free survival (PFS) than those who received bendamustine and rituximab (BR).
In addition, “secondary endpoints were consistently in favor of venetoclax-rituximab,” said study investigator John F. Seymour, MBBS, PhD, of Peter MacCallum Cancer Centre in Melbourne, Victoria, Australia.
Adverse events (AEs) were largely consistent with the known safety profiles of the drugs studied, but tumor lysis syndrome (TLS) was infrequent and occurred at a similar frequency in both treatment arms.
“Thus, overall, I believe venetoclax and rituximab should be considered as a suitable standard therapeutic option in patients with relapsed/refractory CLL,” Dr Seymour said.
It is important to note, however, that patients in the VR arm of this study could receive venetoclax for up to 2 years, whereas patients in the BR arm received study treatment for a maximum of six 28-day cycles.
Dr Seymour presented results from MURANO as a late-breaking abstract at ASH (LBA-2). The study was sponsored by Hoffman-La Roche and AbbVie.
MURANO enrolled 389 CLL patients who had received 1 to 3 prior therapies. Patients were randomized to receive VR (n=194) or BR (n=195). Baseline characteristics were similar between the treatment arms.
In both arms, patients received a single monthly dose of rituximab for 6 cycles. The first dose was 375 mg/m2, and all subsequent doses were 500 mg/m2.
In the VR arm, patients received a 4-week or 5-week dose ramp-up of venetoclax from 20 mg to 400 mg daily. This was intended to mitigate the risk of TLS, which has been observed in previous studies of venetoclax.
Patients in the VR arm continued with daily venetoclax at 400 mg for a maximum of 2 years or until disease progression or cessation due to toxicity. They started receiving rituximab after the ramp-up period (at week 6).
In the BR arm, patients received bendamustine at 70 mg/m2 on days 1 and 2 of each 28-day cycle for 6 cycles. Patients could proceed to subsequent therapy if they progressed.
The median follow-up was 23.8 months (range, 0-37.4 months).
Twenty-five percent of patients in the VR arm and 17% in the BR arm discontinued treatment ahead of schedule. Reasons for discontinuation (in the VR and BR arms, respectively) were disease progression (5% and 3%), AEs (12% and 6%), death (1% and 2%), and “other” (6% and 7%).
Survival
The study’s primary endpoint was investigator-assessed PFS. PFS according to an independent review committee (IRC) was a secondary endpoint.
According to investigators, the median PFS was not reached in the VR arm and was 17.0 months in the BR arm (hazard ratio [HR]=0.17, P<0.0001). According to the IRC, the median PFS was not reached in the VR arm and was 18.1 months in the BR arm (HR=0.17, P<0.0001).
According to investigators, the estimated PFS at 24 months was 84.9% in the VR arm and 36.3% in the BR arm. According to the IRC, the 24-month PFS was 82.8% and 37.4%, respectively.
The benefit with VR was consistent across subgroups. Patients had a PFS benefit regardless of their number of prior therapies, deletion 17p status, TP53 mutational status, baseline IGHV mutational status, and whether they had relapsed or refractory disease.
Dr Seymour acknowledged that the differences in treatment duration between the BR and VR arms may have affected the interpretation of these results.
“[T]he treatment duration differed, although, of course, the capacity to deliver more than 6 cycles of bendamustine-rituximab would have been problematic,” he said. “There is some data that antibody treatment may prolong progression-free survival. However, when this study was designed, in 2013, that data was certainly not available. And I believe, currently, maintenance antibody is not an accepted standard of treatment.”
The median overall survival (OS) was not reached in either treatment arm. The 1-year OS rate was 95.9% in the VR arm and 91.1% in the BR arm. The 2-year OS rate was 91.9% and 86.6%, respectively (HR=0.48, P=0.0186).
“[W]ith median follow-up of just on 2 years, there is already a clinically meaningful difference [in OS between the treatment arms],” Dr Seymour said.
“This is not attributable to any difference in availability of novel therapies. Of the 54 patients who received subsequent therapy after progression on the bendamustine-rituximab arm, 40 of those received novel targeted agents.”
Response and MRD
According to investigators, the overall response rate was 93.3% (181/194) in the VR arm and 67.7% (312/195) in the BR arm (P<0.0001). According to the IRC, the overall response rate was 92.3% (179/194) and 72.3% (141/195), respectively (P<0.0001).
According to investigators, the rate of complete response (CR) or CR with incomplete marrow recovery (CRi) was 26.8% (n=52) in the VR arm and 8.2% (n=16) in the BR arm. According to the IRC, the CR/CRi rate was 8.2% (n=16) and 3.6% (n=7), respectively.
Dr Seymour acknowledged the differences in CR/CRi between investigator and IRC assessments. He said 28 of the 42 discrepancies in the VR arm “were attributable to residual CT scan nodal abnormalities in the 16- to 30-mm size.” However, he also noted that 88% of these patients were negative for minimal residual disease (MRD) in the peripheral blood at that time point.
MRD was assessed every 3 months. Patients were counted as MRD-positive if they were positive by either allele-specific oligonucleotide polymerase chain reaction or multicolor flow cytometry. Patients were also counted as MRD-positive if there was a failure to collect a sample.
The proportion of patients who were MRD-negative in the VR and BR arms, respectively, was:
- 45% and 6% at 4 months
- 62% and 13% at 9 months
- 60% and 10% at 12 months
- 57% and 9% at 15 months
- 60% and 5% at 18 months.
Dr Seymour pointed out that 65 patients in the VR arm surpassed the maximum treatment duration for venetoclax (2 years) and therefore stopped receiving the drug, but only 12 of these patients have follow-up beyond 3 months.
“So information about the durability of response after cessation remains immature at the moment,” he said.
Safety
All patients in the VR arm and 98% in the BR arm had at least 1 AE. The rate of serious AEs was 46% and 43%, respectively. The rate of grade 3/4 AEs was 82% and 70%, respectively.
Grade 3/4 AEs with at least a 2% difference in incidence between the treatment arms (in the VR and BR arms, respectively) were neutropenia (58% and 39%), anemia (11% and 14%), thrombocytopenia (6% and 10%), febrile neutropenia (4% and 10%), pneumonia (5% and 8%), infusion-related reactions (2% and 5%), TLS (3% and 1%), hypotension (0% and 3%), hyperglycemia (2% and 0%), and hypogammaglobulinemia (2% and 0%).
The rate of grade 5 AEs was 5% in the VR arm and 6% in the BR arm.
Grade 5 AEs in the VR arm were pneumonia (n=3), sepsis (n=1), cardiac failure (n=1), myocardial infarction (n=1), sudden cardiac death (n=1), colorectal cancer (n=1), status epilepticus (n=1), and acute respiratory failure (n=1).
Grade 5 AEs in the BR arm included sepsis (n=2), lung cancer (n=2), Listeria sepsis (n=1), Scedosporium infection (n=1), lymphoma (n=1), hemorrhagic stroke (n=1), pulmonary embolism (n=1), acute myeloid leukemia (n=1), and sudden death (n=1). ![]()
ATLANTA—The combination of venetoclax and rituximab (VR) should be a standard treatment option for adults with relapsed/refractory chronic lymphocytic leukemia (CLL), according to a speaker at the 2017 ASH Annual Meeting.
Data from the phase 3 MURANO study showed that patients with relapsed/refractory CLL who received VR had significantly longer progression-free survival (PFS) than those who received bendamustine and rituximab (BR).
In addition, “secondary endpoints were consistently in favor of venetoclax-rituximab,” said study investigator John F. Seymour, MBBS, PhD, of Peter MacCallum Cancer Centre in Melbourne, Victoria, Australia.
Adverse events (AEs) were largely consistent with the known safety profiles of the drugs studied, but tumor lysis syndrome (TLS) was infrequent and occurred at a similar frequency in both treatment arms.
“Thus, overall, I believe venetoclax and rituximab should be considered as a suitable standard therapeutic option in patients with relapsed/refractory CLL,” Dr Seymour said.
It is important to note, however, that patients in the VR arm of this study could receive venetoclax for up to 2 years, whereas patients in the BR arm received study treatment for a maximum of six 28-day cycles.
Dr Seymour presented results from MURANO as a late-breaking abstract at ASH (LBA-2). The study was sponsored by Hoffman-La Roche and AbbVie.
MURANO enrolled 389 CLL patients who had received 1 to 3 prior therapies. Patients were randomized to receive VR (n=194) or BR (n=195). Baseline characteristics were similar between the treatment arms.
In both arms, patients received a single monthly dose of rituximab for 6 cycles. The first dose was 375 mg/m2, and all subsequent doses were 500 mg/m2.
In the VR arm, patients received a 4-week or 5-week dose ramp-up of venetoclax from 20 mg to 400 mg daily. This was intended to mitigate the risk of TLS, which has been observed in previous studies of venetoclax.
Patients in the VR arm continued with daily venetoclax at 400 mg for a maximum of 2 years or until disease progression or cessation due to toxicity. They started receiving rituximab after the ramp-up period (at week 6).
In the BR arm, patients received bendamustine at 70 mg/m2 on days 1 and 2 of each 28-day cycle for 6 cycles. Patients could proceed to subsequent therapy if they progressed.
The median follow-up was 23.8 months (range, 0-37.4 months).
Twenty-five percent of patients in the VR arm and 17% in the BR arm discontinued treatment ahead of schedule. Reasons for discontinuation (in the VR and BR arms, respectively) were disease progression (5% and 3%), AEs (12% and 6%), death (1% and 2%), and “other” (6% and 7%).
Survival
The study’s primary endpoint was investigator-assessed PFS. PFS according to an independent review committee (IRC) was a secondary endpoint.
According to investigators, the median PFS was not reached in the VR arm and was 17.0 months in the BR arm (hazard ratio [HR]=0.17, P<0.0001). According to the IRC, the median PFS was not reached in the VR arm and was 18.1 months in the BR arm (HR=0.17, P<0.0001).
According to investigators, the estimated PFS at 24 months was 84.9% in the VR arm and 36.3% in the BR arm. According to the IRC, the 24-month PFS was 82.8% and 37.4%, respectively.
The benefit with VR was consistent across subgroups. Patients had a PFS benefit regardless of their number of prior therapies, deletion 17p status, TP53 mutational status, baseline IGHV mutational status, and whether they had relapsed or refractory disease.
Dr Seymour acknowledged that the differences in treatment duration between the BR and VR arms may have affected the interpretation of these results.
“[T]he treatment duration differed, although, of course, the capacity to deliver more than 6 cycles of bendamustine-rituximab would have been problematic,” he said. “There is some data that antibody treatment may prolong progression-free survival. However, when this study was designed, in 2013, that data was certainly not available. And I believe, currently, maintenance antibody is not an accepted standard of treatment.”
The median overall survival (OS) was not reached in either treatment arm. The 1-year OS rate was 95.9% in the VR arm and 91.1% in the BR arm. The 2-year OS rate was 91.9% and 86.6%, respectively (HR=0.48, P=0.0186).
“[W]ith median follow-up of just on 2 years, there is already a clinically meaningful difference [in OS between the treatment arms],” Dr Seymour said.
“This is not attributable to any difference in availability of novel therapies. Of the 54 patients who received subsequent therapy after progression on the bendamustine-rituximab arm, 40 of those received novel targeted agents.”
Response and MRD
According to investigators, the overall response rate was 93.3% (181/194) in the VR arm and 67.7% (312/195) in the BR arm (P<0.0001). According to the IRC, the overall response rate was 92.3% (179/194) and 72.3% (141/195), respectively (P<0.0001).
According to investigators, the rate of complete response (CR) or CR with incomplete marrow recovery (CRi) was 26.8% (n=52) in the VR arm and 8.2% (n=16) in the BR arm. According to the IRC, the CR/CRi rate was 8.2% (n=16) and 3.6% (n=7), respectively.
Dr Seymour acknowledged the differences in CR/CRi between investigator and IRC assessments. He said 28 of the 42 discrepancies in the VR arm “were attributable to residual CT scan nodal abnormalities in the 16- to 30-mm size.” However, he also noted that 88% of these patients were negative for minimal residual disease (MRD) in the peripheral blood at that time point.
MRD was assessed every 3 months. Patients were counted as MRD-positive if they were positive by either allele-specific oligonucleotide polymerase chain reaction or multicolor flow cytometry. Patients were also counted as MRD-positive if there was a failure to collect a sample.
The proportion of patients who were MRD-negative in the VR and BR arms, respectively, was:
- 45% and 6% at 4 months
- 62% and 13% at 9 months
- 60% and 10% at 12 months
- 57% and 9% at 15 months
- 60% and 5% at 18 months.
Dr Seymour pointed out that 65 patients in the VR arm surpassed the maximum treatment duration for venetoclax (2 years) and therefore stopped receiving the drug, but only 12 of these patients have follow-up beyond 3 months.
“So information about the durability of response after cessation remains immature at the moment,” he said.
Safety
All patients in the VR arm and 98% in the BR arm had at least 1 AE. The rate of serious AEs was 46% and 43%, respectively. The rate of grade 3/4 AEs was 82% and 70%, respectively.
Grade 3/4 AEs with at least a 2% difference in incidence between the treatment arms (in the VR and BR arms, respectively) were neutropenia (58% and 39%), anemia (11% and 14%), thrombocytopenia (6% and 10%), febrile neutropenia (4% and 10%), pneumonia (5% and 8%), infusion-related reactions (2% and 5%), TLS (3% and 1%), hypotension (0% and 3%), hyperglycemia (2% and 0%), and hypogammaglobulinemia (2% and 0%).
The rate of grade 5 AEs was 5% in the VR arm and 6% in the BR arm.
Grade 5 AEs in the VR arm were pneumonia (n=3), sepsis (n=1), cardiac failure (n=1), myocardial infarction (n=1), sudden cardiac death (n=1), colorectal cancer (n=1), status epilepticus (n=1), and acute respiratory failure (n=1).
Grade 5 AEs in the BR arm included sepsis (n=2), lung cancer (n=2), Listeria sepsis (n=1), Scedosporium infection (n=1), lymphoma (n=1), hemorrhagic stroke (n=1), pulmonary embolism (n=1), acute myeloid leukemia (n=1), and sudden death (n=1). ![]()
ATLANTA—The combination of venetoclax and rituximab (VR) should be a standard treatment option for adults with relapsed/refractory chronic lymphocytic leukemia (CLL), according to a speaker at the 2017 ASH Annual Meeting.
Data from the phase 3 MURANO study showed that patients with relapsed/refractory CLL who received VR had significantly longer progression-free survival (PFS) than those who received bendamustine and rituximab (BR).
In addition, “secondary endpoints were consistently in favor of venetoclax-rituximab,” said study investigator John F. Seymour, MBBS, PhD, of Peter MacCallum Cancer Centre in Melbourne, Victoria, Australia.
Adverse events (AEs) were largely consistent with the known safety profiles of the drugs studied, but tumor lysis syndrome (TLS) was infrequent and occurred at a similar frequency in both treatment arms.
“Thus, overall, I believe venetoclax and rituximab should be considered as a suitable standard therapeutic option in patients with relapsed/refractory CLL,” Dr Seymour said.
It is important to note, however, that patients in the VR arm of this study could receive venetoclax for up to 2 years, whereas patients in the BR arm received study treatment for a maximum of six 28-day cycles.
Dr Seymour presented results from MURANO as a late-breaking abstract at ASH (LBA-2). The study was sponsored by Hoffman-La Roche and AbbVie.
MURANO enrolled 389 CLL patients who had received 1 to 3 prior therapies. Patients were randomized to receive VR (n=194) or BR (n=195). Baseline characteristics were similar between the treatment arms.
In both arms, patients received a single monthly dose of rituximab for 6 cycles. The first dose was 375 mg/m2, and all subsequent doses were 500 mg/m2.
In the VR arm, patients received a 4-week or 5-week dose ramp-up of venetoclax from 20 mg to 400 mg daily. This was intended to mitigate the risk of TLS, which has been observed in previous studies of venetoclax.
Patients in the VR arm continued with daily venetoclax at 400 mg for a maximum of 2 years or until disease progression or cessation due to toxicity. They started receiving rituximab after the ramp-up period (at week 6).
In the BR arm, patients received bendamustine at 70 mg/m2 on days 1 and 2 of each 28-day cycle for 6 cycles. Patients could proceed to subsequent therapy if they progressed.
The median follow-up was 23.8 months (range, 0-37.4 months).
Twenty-five percent of patients in the VR arm and 17% in the BR arm discontinued treatment ahead of schedule. Reasons for discontinuation (in the VR and BR arms, respectively) were disease progression (5% and 3%), AEs (12% and 6%), death (1% and 2%), and “other” (6% and 7%).
Survival
The study’s primary endpoint was investigator-assessed PFS. PFS according to an independent review committee (IRC) was a secondary endpoint.
According to investigators, the median PFS was not reached in the VR arm and was 17.0 months in the BR arm (hazard ratio [HR]=0.17, P<0.0001). According to the IRC, the median PFS was not reached in the VR arm and was 18.1 months in the BR arm (HR=0.17, P<0.0001).
According to investigators, the estimated PFS at 24 months was 84.9% in the VR arm and 36.3% in the BR arm. According to the IRC, the 24-month PFS was 82.8% and 37.4%, respectively.
The benefit with VR was consistent across subgroups. Patients had a PFS benefit regardless of their number of prior therapies, deletion 17p status, TP53 mutational status, baseline IGHV mutational status, and whether they had relapsed or refractory disease.
Dr Seymour acknowledged that the differences in treatment duration between the BR and VR arms may have affected the interpretation of these results.
“[T]he treatment duration differed, although, of course, the capacity to deliver more than 6 cycles of bendamustine-rituximab would have been problematic,” he said. “There is some data that antibody treatment may prolong progression-free survival. However, when this study was designed, in 2013, that data was certainly not available. And I believe, currently, maintenance antibody is not an accepted standard of treatment.”
The median overall survival (OS) was not reached in either treatment arm. The 1-year OS rate was 95.9% in the VR arm and 91.1% in the BR arm. The 2-year OS rate was 91.9% and 86.6%, respectively (HR=0.48, P=0.0186).
“[W]ith median follow-up of just on 2 years, there is already a clinically meaningful difference [in OS between the treatment arms],” Dr Seymour said.
“This is not attributable to any difference in availability of novel therapies. Of the 54 patients who received subsequent therapy after progression on the bendamustine-rituximab arm, 40 of those received novel targeted agents.”
Response and MRD
According to investigators, the overall response rate was 93.3% (181/194) in the VR arm and 67.7% (312/195) in the BR arm (P<0.0001). According to the IRC, the overall response rate was 92.3% (179/194) and 72.3% (141/195), respectively (P<0.0001).
According to investigators, the rate of complete response (CR) or CR with incomplete marrow recovery (CRi) was 26.8% (n=52) in the VR arm and 8.2% (n=16) in the BR arm. According to the IRC, the CR/CRi rate was 8.2% (n=16) and 3.6% (n=7), respectively.
Dr Seymour acknowledged the differences in CR/CRi between investigator and IRC assessments. He said 28 of the 42 discrepancies in the VR arm “were attributable to residual CT scan nodal abnormalities in the 16- to 30-mm size.” However, he also noted that 88% of these patients were negative for minimal residual disease (MRD) in the peripheral blood at that time point.
MRD was assessed every 3 months. Patients were counted as MRD-positive if they were positive by either allele-specific oligonucleotide polymerase chain reaction or multicolor flow cytometry. Patients were also counted as MRD-positive if there was a failure to collect a sample.
The proportion of patients who were MRD-negative in the VR and BR arms, respectively, was:
- 45% and 6% at 4 months
- 62% and 13% at 9 months
- 60% and 10% at 12 months
- 57% and 9% at 15 months
- 60% and 5% at 18 months.
Dr Seymour pointed out that 65 patients in the VR arm surpassed the maximum treatment duration for venetoclax (2 years) and therefore stopped receiving the drug, but only 12 of these patients have follow-up beyond 3 months.
“So information about the durability of response after cessation remains immature at the moment,” he said.
Safety
All patients in the VR arm and 98% in the BR arm had at least 1 AE. The rate of serious AEs was 46% and 43%, respectively. The rate of grade 3/4 AEs was 82% and 70%, respectively.
Grade 3/4 AEs with at least a 2% difference in incidence between the treatment arms (in the VR and BR arms, respectively) were neutropenia (58% and 39%), anemia (11% and 14%), thrombocytopenia (6% and 10%), febrile neutropenia (4% and 10%), pneumonia (5% and 8%), infusion-related reactions (2% and 5%), TLS (3% and 1%), hypotension (0% and 3%), hyperglycemia (2% and 0%), and hypogammaglobulinemia (2% and 0%).
The rate of grade 5 AEs was 5% in the VR arm and 6% in the BR arm.
Grade 5 AEs in the VR arm were pneumonia (n=3), sepsis (n=1), cardiac failure (n=1), myocardial infarction (n=1), sudden cardiac death (n=1), colorectal cancer (n=1), status epilepticus (n=1), and acute respiratory failure (n=1).
Grade 5 AEs in the BR arm included sepsis (n=2), lung cancer (n=2), Listeria sepsis (n=1), Scedosporium infection (n=1), lymphoma (n=1), hemorrhagic stroke (n=1), pulmonary embolism (n=1), acute myeloid leukemia (n=1), and sudden death (n=1). ![]()
Edoxaban noninferior to dalteparin for VTE in cancer
ATLANTA—Edoxaban is noninferior to dalteparin for the treatment of cancer-associated venous thromboembolism (VTE), a phase 3 study suggests.
In the Hokusai-VTE CANCER study, patients who received edoxaban had a lower rate of VTE recurrence but a higher rate of major bleeding than patients who received dalteparin.
Rates of VTE recurrence and major bleeding combined were similar between the treatment groups, as were rates of survival free from VTE or major bleeding.
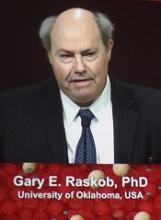
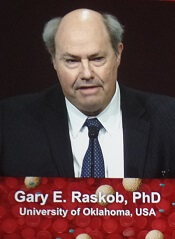
Gary E. Raskob, PhD, of the University of Oklahoma Health Sciences Center in Oklahoma City, presented these results at the 2017 ASH Annual Meeting (LBA-6).
Results were simultaneously published in NEJM. The study was funded by Daiichi Sankyo.
Patients and treatment
Hokusai-VTE CANCER enrolled 1050 adult cancer patients with acute VTE confirmed by imaging. Patients had either active cancer or had been diagnosed with cancer within 2 years from study enrollment. Patients with basal-cell or squamous-cell skin cancer were excluded.
Patients were randomized to receive edoxaban or dalteparin for at least 6 months and up to 12 months.
Edoxaban was given at 60 mg once daily (reduced to 30 mg for patients with creatinine clearance 30-50 mL/min, body weight ≤ 60 kg, or concomitant use of P-glycoprotein inhibitors), following treatment with low-molecular-weight heparin for at least 5 days.
Dalteparin was given at 200 IU/kg once daily for 30 days, then at 150 IU/kg once daily for the remainder of the study.
The median treatment duration was 211 days (interquartile range, 76 to 357) in the edoxaban arm and 184 days (interquartile range, 85 to 341) in the dalteparin arm.
Baseline characteristics were similar between the treatment arms. The median age was 64 in both arms, and about half of patients in each arm were male.
Roughly 98% of patients in each arm had active cancer, 53% had metastatic disease, 29% (dalteparin) and 31% (edoxaban) had recurrent cancer, and 72% (edoxaban) and 73% (dalteparin) had received cancer treatment in the previous 4 weeks.
About 63% of patients in each arm had pulmonary embolism (PE) with or without deep-vein thrombosis (DVT), and 37% had DVT only.
About 18% of patients had 0 risk factors for bleeding, 28% (edoxaban) and 29% (dalteparin) had 1 risk factor, 30% (dalteparin) and 33% (edoxaban) had 2 risk factors, and 21% (edoxaban) and 23% (dalteparin) had 3 or more risk factors for bleeding.
Results
The study’s primary outcome was a composite of first recurrent VTE and major bleeding event during the 12 months after randomization, regardless of treatment duration.
This outcome occurred in 12.8% (67/522) of patients in the edoxaban arm and 13.5% (71/524) of patients in the dalteparin arm. The hazard ratio (HR) with edoxaban was 0.97 (P=0.006 for non-inferiority, P=0.87 for superiority).
“Oral edoxaban is noninferior to subcutaneous dalteparin for the primary outcome of recurrent VTE or major bleeding,” Dr Raskob noted. “The lower rate of recurrent VTE observed with edoxaban was offset by a similar increase in the risk of major bleeding.”
The rate of recurrent VTE during the 12-month study period was 7.9% (n=41) in the edoxaban arm and 11.3% (n=59) in the dalteparin arm (HR=0.71, P=0.09). The rates of recurrent DVT were 3.6% and 6.7%, respectively (HR=0.56), and the rates of recurrent PE were 5.2% and 5.3%, respectively (HR=1.00).
The rate of major bleeding during the 12-month period was 6.9% (n=36) in the edoxaban arm and 4.0% (n=21) in the dalteparin arm (HR=1.77, P=0.04). The rates of clinically relevant nonmajor bleeding were 14.6% and 11.1%, respectively (HR=1.38), and the rates of major or clinically relevant nonmajor bleeding were 18.6% and 13.9%, respectively (HR=1.40).
“There was more upper GI [gastrointestinal] bleeding with edoxaban,” Dr Raskob noted. “It occurred predominantly in patients with GI cancer at the time of entry in the study.”
Death from any cause occurred in 39.5% of patients in the edoxaban arm and 36.6% of patients in the dalteparin arm (HR=1.12).
The rate of event-free survival (absence of recurrent VTE, major bleeding, and death) was 55.0% in the edoxaban arm and 56.5% in the dalteparin arm (HR=0.93).
“The bottom line for patients and oncologists is, ‘Does the patient survive free of these complications?’” Dr Raskob said. “Survival free of recurrent VTE or major bleeding was similar with these regimens.” ![]()
ATLANTA—Edoxaban is noninferior to dalteparin for the treatment of cancer-associated venous thromboembolism (VTE), a phase 3 study suggests.
In the Hokusai-VTE CANCER study, patients who received edoxaban had a lower rate of VTE recurrence but a higher rate of major bleeding than patients who received dalteparin.
Rates of VTE recurrence and major bleeding combined were similar between the treatment groups, as were rates of survival free from VTE or major bleeding.
Gary E. Raskob, PhD, of the University of Oklahoma Health Sciences Center in Oklahoma City, presented these results at the 2017 ASH Annual Meeting (LBA-6).
Results were simultaneously published in NEJM. The study was funded by Daiichi Sankyo.
Patients and treatment
Hokusai-VTE CANCER enrolled 1050 adult cancer patients with acute VTE confirmed by imaging. Patients had either active cancer or had been diagnosed with cancer within 2 years from study enrollment. Patients with basal-cell or squamous-cell skin cancer were excluded.
Patients were randomized to receive edoxaban or dalteparin for at least 6 months and up to 12 months.
Edoxaban was given at 60 mg once daily (reduced to 30 mg for patients with creatinine clearance 30-50 mL/min, body weight ≤ 60 kg, or concomitant use of P-glycoprotein inhibitors), following treatment with low-molecular-weight heparin for at least 5 days.
Dalteparin was given at 200 IU/kg once daily for 30 days, then at 150 IU/kg once daily for the remainder of the study.
The median treatment duration was 211 days (interquartile range, 76 to 357) in the edoxaban arm and 184 days (interquartile range, 85 to 341) in the dalteparin arm.
Baseline characteristics were similar between the treatment arms. The median age was 64 in both arms, and about half of patients in each arm were male.
Roughly 98% of patients in each arm had active cancer, 53% had metastatic disease, 29% (dalteparin) and 31% (edoxaban) had recurrent cancer, and 72% (edoxaban) and 73% (dalteparin) had received cancer treatment in the previous 4 weeks.
About 63% of patients in each arm had pulmonary embolism (PE) with or without deep-vein thrombosis (DVT), and 37% had DVT only.
About 18% of patients had 0 risk factors for bleeding, 28% (edoxaban) and 29% (dalteparin) had 1 risk factor, 30% (dalteparin) and 33% (edoxaban) had 2 risk factors, and 21% (edoxaban) and 23% (dalteparin) had 3 or more risk factors for bleeding.
Results
The study’s primary outcome was a composite of first recurrent VTE and major bleeding event during the 12 months after randomization, regardless of treatment duration.
This outcome occurred in 12.8% (67/522) of patients in the edoxaban arm and 13.5% (71/524) of patients in the dalteparin arm. The hazard ratio (HR) with edoxaban was 0.97 (P=0.006 for non-inferiority, P=0.87 for superiority).
“Oral edoxaban is noninferior to subcutaneous dalteparin for the primary outcome of recurrent VTE or major bleeding,” Dr Raskob noted. “The lower rate of recurrent VTE observed with edoxaban was offset by a similar increase in the risk of major bleeding.”
The rate of recurrent VTE during the 12-month study period was 7.9% (n=41) in the edoxaban arm and 11.3% (n=59) in the dalteparin arm (HR=0.71, P=0.09). The rates of recurrent DVT were 3.6% and 6.7%, respectively (HR=0.56), and the rates of recurrent PE were 5.2% and 5.3%, respectively (HR=1.00).
The rate of major bleeding during the 12-month period was 6.9% (n=36) in the edoxaban arm and 4.0% (n=21) in the dalteparin arm (HR=1.77, P=0.04). The rates of clinically relevant nonmajor bleeding were 14.6% and 11.1%, respectively (HR=1.38), and the rates of major or clinically relevant nonmajor bleeding were 18.6% and 13.9%, respectively (HR=1.40).
“There was more upper GI [gastrointestinal] bleeding with edoxaban,” Dr Raskob noted. “It occurred predominantly in patients with GI cancer at the time of entry in the study.”
Death from any cause occurred in 39.5% of patients in the edoxaban arm and 36.6% of patients in the dalteparin arm (HR=1.12).
The rate of event-free survival (absence of recurrent VTE, major bleeding, and death) was 55.0% in the edoxaban arm and 56.5% in the dalteparin arm (HR=0.93).
“The bottom line for patients and oncologists is, ‘Does the patient survive free of these complications?’” Dr Raskob said. “Survival free of recurrent VTE or major bleeding was similar with these regimens.” ![]()
ATLANTA—Edoxaban is noninferior to dalteparin for the treatment of cancer-associated venous thromboembolism (VTE), a phase 3 study suggests.
In the Hokusai-VTE CANCER study, patients who received edoxaban had a lower rate of VTE recurrence but a higher rate of major bleeding than patients who received dalteparin.
Rates of VTE recurrence and major bleeding combined were similar between the treatment groups, as were rates of survival free from VTE or major bleeding.
Gary E. Raskob, PhD, of the University of Oklahoma Health Sciences Center in Oklahoma City, presented these results at the 2017 ASH Annual Meeting (LBA-6).
Results were simultaneously published in NEJM. The study was funded by Daiichi Sankyo.
Patients and treatment
Hokusai-VTE CANCER enrolled 1050 adult cancer patients with acute VTE confirmed by imaging. Patients had either active cancer or had been diagnosed with cancer within 2 years from study enrollment. Patients with basal-cell or squamous-cell skin cancer were excluded.
Patients were randomized to receive edoxaban or dalteparin for at least 6 months and up to 12 months.
Edoxaban was given at 60 mg once daily (reduced to 30 mg for patients with creatinine clearance 30-50 mL/min, body weight ≤ 60 kg, or concomitant use of P-glycoprotein inhibitors), following treatment with low-molecular-weight heparin for at least 5 days.
Dalteparin was given at 200 IU/kg once daily for 30 days, then at 150 IU/kg once daily for the remainder of the study.
The median treatment duration was 211 days (interquartile range, 76 to 357) in the edoxaban arm and 184 days (interquartile range, 85 to 341) in the dalteparin arm.
Baseline characteristics were similar between the treatment arms. The median age was 64 in both arms, and about half of patients in each arm were male.
Roughly 98% of patients in each arm had active cancer, 53% had metastatic disease, 29% (dalteparin) and 31% (edoxaban) had recurrent cancer, and 72% (edoxaban) and 73% (dalteparin) had received cancer treatment in the previous 4 weeks.
About 63% of patients in each arm had pulmonary embolism (PE) with or without deep-vein thrombosis (DVT), and 37% had DVT only.
About 18% of patients had 0 risk factors for bleeding, 28% (edoxaban) and 29% (dalteparin) had 1 risk factor, 30% (dalteparin) and 33% (edoxaban) had 2 risk factors, and 21% (edoxaban) and 23% (dalteparin) had 3 or more risk factors for bleeding.
Results
The study’s primary outcome was a composite of first recurrent VTE and major bleeding event during the 12 months after randomization, regardless of treatment duration.
This outcome occurred in 12.8% (67/522) of patients in the edoxaban arm and 13.5% (71/524) of patients in the dalteparin arm. The hazard ratio (HR) with edoxaban was 0.97 (P=0.006 for non-inferiority, P=0.87 for superiority).
“Oral edoxaban is noninferior to subcutaneous dalteparin for the primary outcome of recurrent VTE or major bleeding,” Dr Raskob noted. “The lower rate of recurrent VTE observed with edoxaban was offset by a similar increase in the risk of major bleeding.”
The rate of recurrent VTE during the 12-month study period was 7.9% (n=41) in the edoxaban arm and 11.3% (n=59) in the dalteparin arm (HR=0.71, P=0.09). The rates of recurrent DVT were 3.6% and 6.7%, respectively (HR=0.56), and the rates of recurrent PE were 5.2% and 5.3%, respectively (HR=1.00).
The rate of major bleeding during the 12-month period was 6.9% (n=36) in the edoxaban arm and 4.0% (n=21) in the dalteparin arm (HR=1.77, P=0.04). The rates of clinically relevant nonmajor bleeding were 14.6% and 11.1%, respectively (HR=1.38), and the rates of major or clinically relevant nonmajor bleeding were 18.6% and 13.9%, respectively (HR=1.40).
“There was more upper GI [gastrointestinal] bleeding with edoxaban,” Dr Raskob noted. “It occurred predominantly in patients with GI cancer at the time of entry in the study.”
Death from any cause occurred in 39.5% of patients in the edoxaban arm and 36.6% of patients in the dalteparin arm (HR=1.12).
The rate of event-free survival (absence of recurrent VTE, major bleeding, and death) was 55.0% in the edoxaban arm and 56.5% in the dalteparin arm (HR=0.93).
“The bottom line for patients and oncologists is, ‘Does the patient survive free of these complications?’” Dr Raskob said. “Survival free of recurrent VTE or major bleeding was similar with these regimens.” ![]()
Combo should be standard in MM, doc says
ATLANTA—Study results “strongly support” a new standard of care for transplant-ineligible patients with newly diagnosed multiple myeloma (MM), according to a speaker at the 2017 ASH Annual Meeting.
The study, ALCYONE, suggests treatment with bortezomib, melphalan, and prednisone (VMP) can be improved by the addition of daratumumab (D).
D-VMP produced deeper responses and prolonged progression-free survival (PFS) when compared to VMP.
“In this first phase 3, randomized study with a monoclonal antibody in newly diagnosed multiple myeloma, daratumumab reduced the risk of progression or death by 50%,” said Maria-Victoria Mateos, MD, PhD, of University Hospital of Salamanca in Spain.
“No new safety signals were observed [with D-VMP], except for higher infectious events that resolved. I would say the results of this study strongly support daratumumab in combination with VMP as a standard of care in transplant-ineligible, newly diagnosed multiple myeloma.”
Dr Mateos presented results from ALCYONE as a late-breaking abstract (LBA-4) at the ASH Annual Meeting. The study was simultaneously published in NEJM. The research was supported by Janssen Research and Development.
Patients and treatment
ALCYONE enrolled 706 patients with newly diagnosed MM who were not eligible for high-dose chemotherapy with autologous stem cell transplant.
Patients were randomized to receive VMP or D-VMP. They were stratified by International Staging System (I, II, III), region (Europe vs other), and age (<75 vs ≥75 years).
All patients received up to 9 cycles of VMP:
- Bortezomib at 1.3 mg/m2 twice weekly on weeks 1, 2, 4, and 5 of cycle 1 and once weekly on weeks 1, 2, 4, and 5 of cycles 2 through 9
- Melphalan at 9 mg/m2 once daily on days 1 to 4 of each cycle
- Prednisone at 60 mg/m2 once daily on days 1 to 4 of each cycle.
Patients in the daratumumab arm received the drug at 16 mg/kg once-weekly for the first cycle, every 3 weeks for cycles 2 to 9, and every 4 weeks thereafter, until disease progression. These patients also received dexamethasone (to manage infusion reactions) at 20 mg on the same schedule.
Baseline characteristics were similar between the VMP (n=356) and D-VMP (n=350) arms. The median age was 71 in both arms (range, 50-91 in the VMP arm and 40-93 in the D-VMP arm). Males made up 47% of the VMP arm and 46% of the D-VMP arm.
Forty-nine percent of patients in the VMP arm and 52% in the D-VMP arm had an ECOG performance status of 1. Twenty-eight percent and 22%, respectively, had a status of 0.
The median follow-up was 16.5 months (range, 0.1-28.1). At the clinical cutoff date (June 12, 2017), 5% of patients in the VMP arm were still on study treatment, as were 71% of patients in the D-VMP arm.
Response and survival
“I would like to note that the benefit of the addition of daratumumab was observed since the beginning of the treatment,” Dr Mateos said.
The overall response rate was 74% in the VMP arm and 91% in the D-VMP arm (P<0.0001). The median duration of response was 21.3 months in the VMP arm and was not reached in the D-VMP arm.
The rate of complete response was 24% in the VMP arm and 43% in the D-VMP arm (P<0.0001). Six percent of patients in the VMP arm and 22% in the D-VMP arm were negative for minimal residual disease (P<0.0001).
The hazard ratio for disease progression or death in the D-VMP arm versus the VMP arm was 0.50 (P<0.0001).
The median PFS was 18.1 months in the VMP arm and was not reached in the D-VMP arm. The 12-month PFS was 76% and 87%, respectively. And the 18-month PFS was 50% and 72%, respectively.
D-VMP prolonged PFS regardless of patient sex, age, cytogenetic risk, ECOG performance status, baseline renal function, and other factors.
The median overall survival was not reached in either treatment arm. There were 48 deaths in the VMP arm and 45 in the D-VMP arm.
Adverse events
The most common treatment-emergent adverse events (TEAEs; in the D-VMP and VMP arms, respectively) were neutropenia (50% and 53%), thrombocytopenia (49% and 54%), anemia (28% and 38%), peripheral sensory neuropathy (28% and 34%), upper respiratory tract infection (26% and 14%), diarrhea (24% and 25%), pyrexia (23% and 21%), and nausea (21% and 22%).
The most common grade 3/4 TEAEs (in the D-VMP and VMP arms, respectively) were neutropenia (40% and 39%), thrombocytopenia (34% and 38%), and anemia (16% and 20%).
There were 6 deaths due to TEAEs in the D-VMP arm and 5 such deaths in the VMP arm.
The rate of grade 3/4 infections was higher in the D-VMP arm than the VMP arm—23% and 15%, respectively. The most common of these was pneumonia, with rates of 11% and 4%, respectively.
Infections resolved in 88% of cases in the D-VMP arm and 87% of cases in the VMP arm. Rates of treatment discontinuation due to infection were 0.9% and 1.4%, respectively. One patient in each group stopped treatment due to pneumonia.
Twenty-eight percent of patients in the D-VMP arm had infusion-related reactions (15% grade 3 and 2% grade 4). Most of these reactions occurred during the first infusion. Five patients (1.4%) discontinued daratumumab due to infusion-related reactions. ![]()
ATLANTA—Study results “strongly support” a new standard of care for transplant-ineligible patients with newly diagnosed multiple myeloma (MM), according to a speaker at the 2017 ASH Annual Meeting.
The study, ALCYONE, suggests treatment with bortezomib, melphalan, and prednisone (VMP) can be improved by the addition of daratumumab (D).
D-VMP produced deeper responses and prolonged progression-free survival (PFS) when compared to VMP.
“In this first phase 3, randomized study with a monoclonal antibody in newly diagnosed multiple myeloma, daratumumab reduced the risk of progression or death by 50%,” said Maria-Victoria Mateos, MD, PhD, of University Hospital of Salamanca in Spain.
“No new safety signals were observed [with D-VMP], except for higher infectious events that resolved. I would say the results of this study strongly support daratumumab in combination with VMP as a standard of care in transplant-ineligible, newly diagnosed multiple myeloma.”
Dr Mateos presented results from ALCYONE as a late-breaking abstract (LBA-4) at the ASH Annual Meeting. The study was simultaneously published in NEJM. The research was supported by Janssen Research and Development.
Patients and treatment
ALCYONE enrolled 706 patients with newly diagnosed MM who were not eligible for high-dose chemotherapy with autologous stem cell transplant.
Patients were randomized to receive VMP or D-VMP. They were stratified by International Staging System (I, II, III), region (Europe vs other), and age (<75 vs ≥75 years).
All patients received up to 9 cycles of VMP:
- Bortezomib at 1.3 mg/m2 twice weekly on weeks 1, 2, 4, and 5 of cycle 1 and once weekly on weeks 1, 2, 4, and 5 of cycles 2 through 9
- Melphalan at 9 mg/m2 once daily on days 1 to 4 of each cycle
- Prednisone at 60 mg/m2 once daily on days 1 to 4 of each cycle.
Patients in the daratumumab arm received the drug at 16 mg/kg once-weekly for the first cycle, every 3 weeks for cycles 2 to 9, and every 4 weeks thereafter, until disease progression. These patients also received dexamethasone (to manage infusion reactions) at 20 mg on the same schedule.
Baseline characteristics were similar between the VMP (n=356) and D-VMP (n=350) arms. The median age was 71 in both arms (range, 50-91 in the VMP arm and 40-93 in the D-VMP arm). Males made up 47% of the VMP arm and 46% of the D-VMP arm.
Forty-nine percent of patients in the VMP arm and 52% in the D-VMP arm had an ECOG performance status of 1. Twenty-eight percent and 22%, respectively, had a status of 0.
The median follow-up was 16.5 months (range, 0.1-28.1). At the clinical cutoff date (June 12, 2017), 5% of patients in the VMP arm were still on study treatment, as were 71% of patients in the D-VMP arm.
Response and survival
“I would like to note that the benefit of the addition of daratumumab was observed since the beginning of the treatment,” Dr Mateos said.
The overall response rate was 74% in the VMP arm and 91% in the D-VMP arm (P<0.0001). The median duration of response was 21.3 months in the VMP arm and was not reached in the D-VMP arm.
The rate of complete response was 24% in the VMP arm and 43% in the D-VMP arm (P<0.0001). Six percent of patients in the VMP arm and 22% in the D-VMP arm were negative for minimal residual disease (P<0.0001).
The hazard ratio for disease progression or death in the D-VMP arm versus the VMP arm was 0.50 (P<0.0001).
The median PFS was 18.1 months in the VMP arm and was not reached in the D-VMP arm. The 12-month PFS was 76% and 87%, respectively. And the 18-month PFS was 50% and 72%, respectively.
D-VMP prolonged PFS regardless of patient sex, age, cytogenetic risk, ECOG performance status, baseline renal function, and other factors.
The median overall survival was not reached in either treatment arm. There were 48 deaths in the VMP arm and 45 in the D-VMP arm.
Adverse events
The most common treatment-emergent adverse events (TEAEs; in the D-VMP and VMP arms, respectively) were neutropenia (50% and 53%), thrombocytopenia (49% and 54%), anemia (28% and 38%), peripheral sensory neuropathy (28% and 34%), upper respiratory tract infection (26% and 14%), diarrhea (24% and 25%), pyrexia (23% and 21%), and nausea (21% and 22%).
The most common grade 3/4 TEAEs (in the D-VMP and VMP arms, respectively) were neutropenia (40% and 39%), thrombocytopenia (34% and 38%), and anemia (16% and 20%).
There were 6 deaths due to TEAEs in the D-VMP arm and 5 such deaths in the VMP arm.
The rate of grade 3/4 infections was higher in the D-VMP arm than the VMP arm—23% and 15%, respectively. The most common of these was pneumonia, with rates of 11% and 4%, respectively.
Infections resolved in 88% of cases in the D-VMP arm and 87% of cases in the VMP arm. Rates of treatment discontinuation due to infection were 0.9% and 1.4%, respectively. One patient in each group stopped treatment due to pneumonia.
Twenty-eight percent of patients in the D-VMP arm had infusion-related reactions (15% grade 3 and 2% grade 4). Most of these reactions occurred during the first infusion. Five patients (1.4%) discontinued daratumumab due to infusion-related reactions. ![]()
ATLANTA—Study results “strongly support” a new standard of care for transplant-ineligible patients with newly diagnosed multiple myeloma (MM), according to a speaker at the 2017 ASH Annual Meeting.
The study, ALCYONE, suggests treatment with bortezomib, melphalan, and prednisone (VMP) can be improved by the addition of daratumumab (D).
D-VMP produced deeper responses and prolonged progression-free survival (PFS) when compared to VMP.
“In this first phase 3, randomized study with a monoclonal antibody in newly diagnosed multiple myeloma, daratumumab reduced the risk of progression or death by 50%,” said Maria-Victoria Mateos, MD, PhD, of University Hospital of Salamanca in Spain.
“No new safety signals were observed [with D-VMP], except for higher infectious events that resolved. I would say the results of this study strongly support daratumumab in combination with VMP as a standard of care in transplant-ineligible, newly diagnosed multiple myeloma.”
Dr Mateos presented results from ALCYONE as a late-breaking abstract (LBA-4) at the ASH Annual Meeting. The study was simultaneously published in NEJM. The research was supported by Janssen Research and Development.
Patients and treatment
ALCYONE enrolled 706 patients with newly diagnosed MM who were not eligible for high-dose chemotherapy with autologous stem cell transplant.
Patients were randomized to receive VMP or D-VMP. They were stratified by International Staging System (I, II, III), region (Europe vs other), and age (<75 vs ≥75 years).
All patients received up to 9 cycles of VMP:
- Bortezomib at 1.3 mg/m2 twice weekly on weeks 1, 2, 4, and 5 of cycle 1 and once weekly on weeks 1, 2, 4, and 5 of cycles 2 through 9
- Melphalan at 9 mg/m2 once daily on days 1 to 4 of each cycle
- Prednisone at 60 mg/m2 once daily on days 1 to 4 of each cycle.
Patients in the daratumumab arm received the drug at 16 mg/kg once-weekly for the first cycle, every 3 weeks for cycles 2 to 9, and every 4 weeks thereafter, until disease progression. These patients also received dexamethasone (to manage infusion reactions) at 20 mg on the same schedule.
Baseline characteristics were similar between the VMP (n=356) and D-VMP (n=350) arms. The median age was 71 in both arms (range, 50-91 in the VMP arm and 40-93 in the D-VMP arm). Males made up 47% of the VMP arm and 46% of the D-VMP arm.
Forty-nine percent of patients in the VMP arm and 52% in the D-VMP arm had an ECOG performance status of 1. Twenty-eight percent and 22%, respectively, had a status of 0.
The median follow-up was 16.5 months (range, 0.1-28.1). At the clinical cutoff date (June 12, 2017), 5% of patients in the VMP arm were still on study treatment, as were 71% of patients in the D-VMP arm.
Response and survival
“I would like to note that the benefit of the addition of daratumumab was observed since the beginning of the treatment,” Dr Mateos said.
The overall response rate was 74% in the VMP arm and 91% in the D-VMP arm (P<0.0001). The median duration of response was 21.3 months in the VMP arm and was not reached in the D-VMP arm.
The rate of complete response was 24% in the VMP arm and 43% in the D-VMP arm (P<0.0001). Six percent of patients in the VMP arm and 22% in the D-VMP arm were negative for minimal residual disease (P<0.0001).
The hazard ratio for disease progression or death in the D-VMP arm versus the VMP arm was 0.50 (P<0.0001).
The median PFS was 18.1 months in the VMP arm and was not reached in the D-VMP arm. The 12-month PFS was 76% and 87%, respectively. And the 18-month PFS was 50% and 72%, respectively.
D-VMP prolonged PFS regardless of patient sex, age, cytogenetic risk, ECOG performance status, baseline renal function, and other factors.
The median overall survival was not reached in either treatment arm. There were 48 deaths in the VMP arm and 45 in the D-VMP arm.
Adverse events
The most common treatment-emergent adverse events (TEAEs; in the D-VMP and VMP arms, respectively) were neutropenia (50% and 53%), thrombocytopenia (49% and 54%), anemia (28% and 38%), peripheral sensory neuropathy (28% and 34%), upper respiratory tract infection (26% and 14%), diarrhea (24% and 25%), pyrexia (23% and 21%), and nausea (21% and 22%).
The most common grade 3/4 TEAEs (in the D-VMP and VMP arms, respectively) were neutropenia (40% and 39%), thrombocytopenia (34% and 38%), and anemia (16% and 20%).
There were 6 deaths due to TEAEs in the D-VMP arm and 5 such deaths in the VMP arm.
The rate of grade 3/4 infections was higher in the D-VMP arm than the VMP arm—23% and 15%, respectively. The most common of these was pneumonia, with rates of 11% and 4%, respectively.
Infections resolved in 88% of cases in the D-VMP arm and 87% of cases in the VMP arm. Rates of treatment discontinuation due to infection were 0.9% and 1.4%, respectively. One patient in each group stopped treatment due to pneumonia.
Twenty-eight percent of patients in the D-VMP arm had infusion-related reactions (15% grade 3 and 2% grade 4). Most of these reactions occurred during the first infusion. Five patients (1.4%) discontinued daratumumab due to infusion-related reactions. ![]()
Emicizumab reduces bleeds in kids with hemophilia A and inhibitors
ATLANTA—Updated results from the HAVEN 2 trial have shown that emicizumab prophylaxis can reduce bleeds in children with hemophilia A and factor VIII inhibitors.
Sixty-five percent of all patients enrolled in HAVEN 2 had no bleeds while on emicizumab, and 95% had no treated bleeds.
Among patients who had been on emicizumab for at least 12 weeks, 35% had no bleeds, and 87% had no treated bleeds.
The most common adverse events (AEs) in this trial were viral upper respiratory tract infections and injection site reactions.
Guy Young, MD, of Children’s Hospital Los Angeles in California, presented these results at the 2017 ASH Annual Meeting (abstract 85). The trial was sponsored by Hoffmann-La Roche.
HAVEN 2 enrolled 60 patients, ages 1 to 17, who had hemophilia A and inhibitors. Most patients (95%) had severe hemophilia, 3.3% (n=2) had mild disease, and 1.7% (n=1) had moderate disease.
Nearly a quarter of patients (73.3%) had previously received prophylaxis, and 26.7% had previously received episodic treatment.
The median number of bleeds in the previous 24 weeks was 6.0 (range, 0-155), and 38.3% of patients had target joints.
Patients received emicizumab prophylaxis at 3 mg/kg/week for 4 weeks and 1.5 mg/kg/week thereafter. The median observation time was 9 weeks (range, 1.6 to 41.6 weeks).
Efficacy
The efficacy analysis included 57 patients who were younger than 12. The 3 older patients were only included in the safety analysis.
Of the 57 patients, 64.9% had 0 bleeds, 94.7% had 0 treated bleeds, and 98.2% had 0 treated spontaneous bleeds and 0 treated joint bleeds. None of the patients had treated target joint bleeds.
There were a total of 65 bleeds in 20 patients. Eight were joint bleeds, 2 were muscle bleeds, and the rest were classified as “other.” Of the 55 “other’’ bleeds, 26 (40.0%) were spontaneous, 36 (55.4%) were traumatic, and 3 (4.6%) were due to a procedure/surgery.
A subset of 23 patients received emicizumab for at least 12 weeks. They had a median treatment duration of 38.1 weeks (range, 12.7 to 41.6 weeks).
Of these patients, 34.8% had 0 bleeds, 87.0% had 0 treated bleeds, and 95.7% had 0 treated spontaneous bleeds and 0 treated joint bleeds. There were a total of 41 bleeds in 15 of these patients. Three bleeds (joint, muscle, and hip) were treated.
The median annualized bleeding rate (ABR) for the 23 patients was 1.5 for all bleeds and 0.0 for all types of treated bleeds.
There were 13 patients who had participated in a non-interventional study prior to enrolling in HAVEN 2, so these patients could serve as their own controls. The patients had an overall reduction in ABR of 99% with emicizumab.
Safety
All 60 patients were evaluated for safety. Forty patients had a total of 201 AEs. The most common AEs were viral upper respiratory tract infection (16.7%) and injection site reactions (16.7%)
There were 7 serious AEs in 6 patients—muscle hemorrhage (n=2), eye pain, catheter site injection, device-related infection, mouth hemorrhage, and appendicitis. None of these events were considered treatment-related.
There were no thromboembolic or thrombotic microangiopathy events, and none of the patients tested positive for anti-drug antibodies.
“The safety profile of emicizumab was favorable and well-tolerated,” Dr Young said. “And these updated results from the HAVEN 2 study confirm our prior efficacy results, presented at ISTH, that emicizumab successfully prevents or reduces bleeds.” ![]()
ATLANTA—Updated results from the HAVEN 2 trial have shown that emicizumab prophylaxis can reduce bleeds in children with hemophilia A and factor VIII inhibitors.
Sixty-five percent of all patients enrolled in HAVEN 2 had no bleeds while on emicizumab, and 95% had no treated bleeds.
Among patients who had been on emicizumab for at least 12 weeks, 35% had no bleeds, and 87% had no treated bleeds.
The most common adverse events (AEs) in this trial were viral upper respiratory tract infections and injection site reactions.
Guy Young, MD, of Children’s Hospital Los Angeles in California, presented these results at the 2017 ASH Annual Meeting (abstract 85). The trial was sponsored by Hoffmann-La Roche.
HAVEN 2 enrolled 60 patients, ages 1 to 17, who had hemophilia A and inhibitors. Most patients (95%) had severe hemophilia, 3.3% (n=2) had mild disease, and 1.7% (n=1) had moderate disease.
Nearly a quarter of patients (73.3%) had previously received prophylaxis, and 26.7% had previously received episodic treatment.
The median number of bleeds in the previous 24 weeks was 6.0 (range, 0-155), and 38.3% of patients had target joints.
Patients received emicizumab prophylaxis at 3 mg/kg/week for 4 weeks and 1.5 mg/kg/week thereafter. The median observation time was 9 weeks (range, 1.6 to 41.6 weeks).
Efficacy
The efficacy analysis included 57 patients who were younger than 12. The 3 older patients were only included in the safety analysis.
Of the 57 patients, 64.9% had 0 bleeds, 94.7% had 0 treated bleeds, and 98.2% had 0 treated spontaneous bleeds and 0 treated joint bleeds. None of the patients had treated target joint bleeds.
There were a total of 65 bleeds in 20 patients. Eight were joint bleeds, 2 were muscle bleeds, and the rest were classified as “other.” Of the 55 “other’’ bleeds, 26 (40.0%) were spontaneous, 36 (55.4%) were traumatic, and 3 (4.6%) were due to a procedure/surgery.
A subset of 23 patients received emicizumab for at least 12 weeks. They had a median treatment duration of 38.1 weeks (range, 12.7 to 41.6 weeks).
Of these patients, 34.8% had 0 bleeds, 87.0% had 0 treated bleeds, and 95.7% had 0 treated spontaneous bleeds and 0 treated joint bleeds. There were a total of 41 bleeds in 15 of these patients. Three bleeds (joint, muscle, and hip) were treated.
The median annualized bleeding rate (ABR) for the 23 patients was 1.5 for all bleeds and 0.0 for all types of treated bleeds.
There were 13 patients who had participated in a non-interventional study prior to enrolling in HAVEN 2, so these patients could serve as their own controls. The patients had an overall reduction in ABR of 99% with emicizumab.
Safety
All 60 patients were evaluated for safety. Forty patients had a total of 201 AEs. The most common AEs were viral upper respiratory tract infection (16.7%) and injection site reactions (16.7%)
There were 7 serious AEs in 6 patients—muscle hemorrhage (n=2), eye pain, catheter site injection, device-related infection, mouth hemorrhage, and appendicitis. None of these events were considered treatment-related.
There were no thromboembolic or thrombotic microangiopathy events, and none of the patients tested positive for anti-drug antibodies.
“The safety profile of emicizumab was favorable and well-tolerated,” Dr Young said. “And these updated results from the HAVEN 2 study confirm our prior efficacy results, presented at ISTH, that emicizumab successfully prevents or reduces bleeds.” ![]()
ATLANTA—Updated results from the HAVEN 2 trial have shown that emicizumab prophylaxis can reduce bleeds in children with hemophilia A and factor VIII inhibitors.
Sixty-five percent of all patients enrolled in HAVEN 2 had no bleeds while on emicizumab, and 95% had no treated bleeds.
Among patients who had been on emicizumab for at least 12 weeks, 35% had no bleeds, and 87% had no treated bleeds.
The most common adverse events (AEs) in this trial were viral upper respiratory tract infections and injection site reactions.
Guy Young, MD, of Children’s Hospital Los Angeles in California, presented these results at the 2017 ASH Annual Meeting (abstract 85). The trial was sponsored by Hoffmann-La Roche.
HAVEN 2 enrolled 60 patients, ages 1 to 17, who had hemophilia A and inhibitors. Most patients (95%) had severe hemophilia, 3.3% (n=2) had mild disease, and 1.7% (n=1) had moderate disease.
Nearly a quarter of patients (73.3%) had previously received prophylaxis, and 26.7% had previously received episodic treatment.
The median number of bleeds in the previous 24 weeks was 6.0 (range, 0-155), and 38.3% of patients had target joints.
Patients received emicizumab prophylaxis at 3 mg/kg/week for 4 weeks and 1.5 mg/kg/week thereafter. The median observation time was 9 weeks (range, 1.6 to 41.6 weeks).
Efficacy
The efficacy analysis included 57 patients who were younger than 12. The 3 older patients were only included in the safety analysis.
Of the 57 patients, 64.9% had 0 bleeds, 94.7% had 0 treated bleeds, and 98.2% had 0 treated spontaneous bleeds and 0 treated joint bleeds. None of the patients had treated target joint bleeds.
There were a total of 65 bleeds in 20 patients. Eight were joint bleeds, 2 were muscle bleeds, and the rest were classified as “other.” Of the 55 “other’’ bleeds, 26 (40.0%) were spontaneous, 36 (55.4%) were traumatic, and 3 (4.6%) were due to a procedure/surgery.
A subset of 23 patients received emicizumab for at least 12 weeks. They had a median treatment duration of 38.1 weeks (range, 12.7 to 41.6 weeks).
Of these patients, 34.8% had 0 bleeds, 87.0% had 0 treated bleeds, and 95.7% had 0 treated spontaneous bleeds and 0 treated joint bleeds. There were a total of 41 bleeds in 15 of these patients. Three bleeds (joint, muscle, and hip) were treated.
The median annualized bleeding rate (ABR) for the 23 patients was 1.5 for all bleeds and 0.0 for all types of treated bleeds.
There were 13 patients who had participated in a non-interventional study prior to enrolling in HAVEN 2, so these patients could serve as their own controls. The patients had an overall reduction in ABR of 99% with emicizumab.
Safety
All 60 patients were evaluated for safety. Forty patients had a total of 201 AEs. The most common AEs were viral upper respiratory tract infection (16.7%) and injection site reactions (16.7%)
There were 7 serious AEs in 6 patients—muscle hemorrhage (n=2), eye pain, catheter site injection, device-related infection, mouth hemorrhage, and appendicitis. None of these events were considered treatment-related.
There were no thromboembolic or thrombotic microangiopathy events, and none of the patients tested positive for anti-drug antibodies.
“The safety profile of emicizumab was favorable and well-tolerated,” Dr Young said. “And these updated results from the HAVEN 2 study confirm our prior efficacy results, presented at ISTH, that emicizumab successfully prevents or reduces bleeds.” ![]()
Team discovers oncogenic driver of T-ALL
Preclinical research suggests the TOX protein is an oncogenic driver of T-cell acute lymphoblastic leukemia (T-ALL).
Results indicate that TOX may be expressed in as many as 95% of human T-ALL cases, and the protein is required for the cancer’s growth and persistence.
“A major role for TOX in T-ALL is to elicit defects in DNA repair, leading to genetic changes that drive normal cells into cancer,” said study author David Langenau, PhD, of Massachusetts General Hospital in Boston.
“TOX then continues to be expressed within leukemic cells and is required for continued tumor growth. That means that, if we can successfully target TOX with small molecules in the future, the 95% of T-ALL patients whose tumors express TOX would have new treatment options for this aggressive leukemia.”
Dr Langenau and his colleagues described this new role for TOX in Cancer Discovery.
The team noted that T-ALL has several molecular subtypes, many of which are driven by common oncogenes such as MYC and NOTCH. However, evidence has suggested the cancer’s initiation is likely driven by aberrations in DNA repair.
To identify genes that might help drive T-ALL, the researchers performed a transgenic screen in zebrafish.
The team found that TOX collaborates with known oncogene pathways to transform T-cell precursors into leukemia cells by altering DNA repair and then expanding the population of transformed cells.
In human T-ALL cells, TOX was shown to suppress non-homologous end joining (NHEJ) repair, a pathway required for repairing double-strand DNA breaks that, when disrupted, is known to cause errant DNA repair and genomic instability.
Nearly all of the human T-ALL samples the researchers tested were found to express TOX. And TOX proved essential for the proliferation and survival of T-ALL.
Dr Langenau explained that TOX is known to have important roles in the development and maturation of several types of immune cells, yet its roles in leukemia initiation and genomic instability were not described until this work.
TOX belongs to a group of proteins known to regulate the configuration or expression of genes by binding to DNA molecules, yet its mechanism in T-ALL—blocking NHEJ repair by binding to DNA repair proteins rather than directly to DNA—was totally unexpected.
The researchers believe that, in addition to better understanding how TOX regulates the continued growth of T-ALL, it will be important to determine whether related proteins have similar molecular functions in other cancers. ![]()
Preclinical research suggests the TOX protein is an oncogenic driver of T-cell acute lymphoblastic leukemia (T-ALL).
Results indicate that TOX may be expressed in as many as 95% of human T-ALL cases, and the protein is required for the cancer’s growth and persistence.
“A major role for TOX in T-ALL is to elicit defects in DNA repair, leading to genetic changes that drive normal cells into cancer,” said study author David Langenau, PhD, of Massachusetts General Hospital in Boston.
“TOX then continues to be expressed within leukemic cells and is required for continued tumor growth. That means that, if we can successfully target TOX with small molecules in the future, the 95% of T-ALL patients whose tumors express TOX would have new treatment options for this aggressive leukemia.”
Dr Langenau and his colleagues described this new role for TOX in Cancer Discovery.
The team noted that T-ALL has several molecular subtypes, many of which are driven by common oncogenes such as MYC and NOTCH. However, evidence has suggested the cancer’s initiation is likely driven by aberrations in DNA repair.
To identify genes that might help drive T-ALL, the researchers performed a transgenic screen in zebrafish.
The team found that TOX collaborates with known oncogene pathways to transform T-cell precursors into leukemia cells by altering DNA repair and then expanding the population of transformed cells.
In human T-ALL cells, TOX was shown to suppress non-homologous end joining (NHEJ) repair, a pathway required for repairing double-strand DNA breaks that, when disrupted, is known to cause errant DNA repair and genomic instability.
Nearly all of the human T-ALL samples the researchers tested were found to express TOX. And TOX proved essential for the proliferation and survival of T-ALL.
Dr Langenau explained that TOX is known to have important roles in the development and maturation of several types of immune cells, yet its roles in leukemia initiation and genomic instability were not described until this work.
TOX belongs to a group of proteins known to regulate the configuration or expression of genes by binding to DNA molecules, yet its mechanism in T-ALL—blocking NHEJ repair by binding to DNA repair proteins rather than directly to DNA—was totally unexpected.
The researchers believe that, in addition to better understanding how TOX regulates the continued growth of T-ALL, it will be important to determine whether related proteins have similar molecular functions in other cancers. ![]()
Preclinical research suggests the TOX protein is an oncogenic driver of T-cell acute lymphoblastic leukemia (T-ALL).
Results indicate that TOX may be expressed in as many as 95% of human T-ALL cases, and the protein is required for the cancer’s growth and persistence.
“A major role for TOX in T-ALL is to elicit defects in DNA repair, leading to genetic changes that drive normal cells into cancer,” said study author David Langenau, PhD, of Massachusetts General Hospital in Boston.
“TOX then continues to be expressed within leukemic cells and is required for continued tumor growth. That means that, if we can successfully target TOX with small molecules in the future, the 95% of T-ALL patients whose tumors express TOX would have new treatment options for this aggressive leukemia.”
Dr Langenau and his colleagues described this new role for TOX in Cancer Discovery.
The team noted that T-ALL has several molecular subtypes, many of which are driven by common oncogenes such as MYC and NOTCH. However, evidence has suggested the cancer’s initiation is likely driven by aberrations in DNA repair.
To identify genes that might help drive T-ALL, the researchers performed a transgenic screen in zebrafish.
The team found that TOX collaborates with known oncogene pathways to transform T-cell precursors into leukemia cells by altering DNA repair and then expanding the population of transformed cells.
In human T-ALL cells, TOX was shown to suppress non-homologous end joining (NHEJ) repair, a pathway required for repairing double-strand DNA breaks that, when disrupted, is known to cause errant DNA repair and genomic instability.
Nearly all of the human T-ALL samples the researchers tested were found to express TOX. And TOX proved essential for the proliferation and survival of T-ALL.
Dr Langenau explained that TOX is known to have important roles in the development and maturation of several types of immune cells, yet its roles in leukemia initiation and genomic instability were not described until this work.
TOX belongs to a group of proteins known to regulate the configuration or expression of genes by binding to DNA molecules, yet its mechanism in T-ALL—blocking NHEJ repair by binding to DNA repair proteins rather than directly to DNA—was totally unexpected.
The researchers believe that, in addition to better understanding how TOX regulates the continued growth of T-ALL, it will be important to determine whether related proteins have similar molecular functions in other cancers. ![]()
FDA warns about risk of death with pembrolizumab in MM
The US Food and Drug Administration (FDA) has issued a statement warning about an increased risk of death associated with an unapproved use of pembrolizumab (Keytruda).
Results from 2 clinical trials have shown that combining pembrolizumab with dexamethasone and an immunomodulatory agent (lenalidomide or pomalidomide) increases the risk of death in patients with multiple myeloma (MM).
The FDA issued its statement to remind doctors and patients that pembrolizumab is not approved to treat MM and should not be given in combination with immunomodulatory agents to treat MM.
Pembrolizumab is currently FDA-approved to treat classical Hodgkin lymphoma, melanoma, lung cancer, head and neck cancer, urothelial carcinoma, and microsatellite instability-high cancer.
The FDA believes the benefits of taking pembrolizumab and other PD-1/PD-L1 inhibitors for their approved uses continue to outweigh the risks, according to Janet Woodcock, director of the FDA’s Center for Drug Evaluation and Research.
However, the FDA is investigating trials of pembrolizumab as well as trials of other PD-1/PD-L1 inhibitors.
Pembrolizumab in MM
The FDA’s warning is based on a review of data from 2 clinical trials—KEYNOTE-183 and KEYNOTE-185. The FDA placed a clinical hold on these trials—as well as KEYNOTE-023—in July.
KEYNOTE-183 is a phase 3 study of pomalidomide and low-dose dexamethasone, given with or without pembrolizumab, to patients with refractory or relapsed and refractory MM.
KEYNOTE-185 is a phase 3 study of lenalidomide and low-dose dexamethasone, given with or without pembrolizumab, to patients with newly diagnosed and treatment-naïve MM.
KEYNOTE-023 is a phase 1 trial of pembrolizumab in combination with backbone treatments. Cohort 1 of this trial was designed to evaluate pembrolizumab in combination with lenalidomide and dexamethasone in MM patients who received prior treatment with an immunomodulatory agent (lenalidomide, pomalidomide, or thalidomide).
Interim results from KEYNOTE-183 and KEYNOTE-185 revealed an increased risk of death for patients receiving pembrolizumab, when compared to patients receiving the control therapies.
Merck & Co., Inc., the company developing pembrolizumab, was informed of this risk by an external data monitoring committee. The company suspended enrollment in the trials and notified the FDA of the issue in June.
The following month, the FDA announced that all patients enrolled in KEYNOTE-183 and KEYNOTE-185, as well as patients in the pembrolizumab/lenalidomide/dexamethasone cohort of KEYNOTE-023, would discontinue investigational treatment with pembrolizumab.
FDA investigation
The FDA is examining data from the pembrolizumab trials and working with Merck to better understand the cause of the safety concerns, according to Woodcock.
The agency is also working with sponsors of other PD-1/PD-L1 inhibitors to examine other trials in which these drugs are being studied in combination with immunomodulatory agents and trials in which the inhibitors are being studied in combination with other classes of drugs in patients with hematologic malignancies.
Woodcock said the FDA will take appropriate action as warranted to ensure patients enrolled in these trials are protected and that doctors and researchers understand the risks associated with this investigational use.
The agency is also encouraging healthcare professionals and consumers to report any adverse events or side effects related to the use of pembrolizumab and other PD-1/PD-L1 inhibitors to FDA’s MedWatch Adverse Event Reporting Program. ![]()
The US Food and Drug Administration (FDA) has issued a statement warning about an increased risk of death associated with an unapproved use of pembrolizumab (Keytruda).
Results from 2 clinical trials have shown that combining pembrolizumab with dexamethasone and an immunomodulatory agent (lenalidomide or pomalidomide) increases the risk of death in patients with multiple myeloma (MM).
The FDA issued its statement to remind doctors and patients that pembrolizumab is not approved to treat MM and should not be given in combination with immunomodulatory agents to treat MM.
Pembrolizumab is currently FDA-approved to treat classical Hodgkin lymphoma, melanoma, lung cancer, head and neck cancer, urothelial carcinoma, and microsatellite instability-high cancer.
The FDA believes the benefits of taking pembrolizumab and other PD-1/PD-L1 inhibitors for their approved uses continue to outweigh the risks, according to Janet Woodcock, director of the FDA’s Center for Drug Evaluation and Research.
However, the FDA is investigating trials of pembrolizumab as well as trials of other PD-1/PD-L1 inhibitors.
Pembrolizumab in MM
The FDA’s warning is based on a review of data from 2 clinical trials—KEYNOTE-183 and KEYNOTE-185. The FDA placed a clinical hold on these trials—as well as KEYNOTE-023—in July.
KEYNOTE-183 is a phase 3 study of pomalidomide and low-dose dexamethasone, given with or without pembrolizumab, to patients with refractory or relapsed and refractory MM.
KEYNOTE-185 is a phase 3 study of lenalidomide and low-dose dexamethasone, given with or without pembrolizumab, to patients with newly diagnosed and treatment-naïve MM.
KEYNOTE-023 is a phase 1 trial of pembrolizumab in combination with backbone treatments. Cohort 1 of this trial was designed to evaluate pembrolizumab in combination with lenalidomide and dexamethasone in MM patients who received prior treatment with an immunomodulatory agent (lenalidomide, pomalidomide, or thalidomide).
Interim results from KEYNOTE-183 and KEYNOTE-185 revealed an increased risk of death for patients receiving pembrolizumab, when compared to patients receiving the control therapies.
Merck & Co., Inc., the company developing pembrolizumab, was informed of this risk by an external data monitoring committee. The company suspended enrollment in the trials and notified the FDA of the issue in June.
The following month, the FDA announced that all patients enrolled in KEYNOTE-183 and KEYNOTE-185, as well as patients in the pembrolizumab/lenalidomide/dexamethasone cohort of KEYNOTE-023, would discontinue investigational treatment with pembrolizumab.
FDA investigation
The FDA is examining data from the pembrolizumab trials and working with Merck to better understand the cause of the safety concerns, according to Woodcock.
The agency is also working with sponsors of other PD-1/PD-L1 inhibitors to examine other trials in which these drugs are being studied in combination with immunomodulatory agents and trials in which the inhibitors are being studied in combination with other classes of drugs in patients with hematologic malignancies.
Woodcock said the FDA will take appropriate action as warranted to ensure patients enrolled in these trials are protected and that doctors and researchers understand the risks associated with this investigational use.
The agency is also encouraging healthcare professionals and consumers to report any adverse events or side effects related to the use of pembrolizumab and other PD-1/PD-L1 inhibitors to FDA’s MedWatch Adverse Event Reporting Program. ![]()
The US Food and Drug Administration (FDA) has issued a statement warning about an increased risk of death associated with an unapproved use of pembrolizumab (Keytruda).
Results from 2 clinical trials have shown that combining pembrolizumab with dexamethasone and an immunomodulatory agent (lenalidomide or pomalidomide) increases the risk of death in patients with multiple myeloma (MM).
The FDA issued its statement to remind doctors and patients that pembrolizumab is not approved to treat MM and should not be given in combination with immunomodulatory agents to treat MM.
Pembrolizumab is currently FDA-approved to treat classical Hodgkin lymphoma, melanoma, lung cancer, head and neck cancer, urothelial carcinoma, and microsatellite instability-high cancer.
The FDA believes the benefits of taking pembrolizumab and other PD-1/PD-L1 inhibitors for their approved uses continue to outweigh the risks, according to Janet Woodcock, director of the FDA’s Center for Drug Evaluation and Research.
However, the FDA is investigating trials of pembrolizumab as well as trials of other PD-1/PD-L1 inhibitors.
Pembrolizumab in MM
The FDA’s warning is based on a review of data from 2 clinical trials—KEYNOTE-183 and KEYNOTE-185. The FDA placed a clinical hold on these trials—as well as KEYNOTE-023—in July.
KEYNOTE-183 is a phase 3 study of pomalidomide and low-dose dexamethasone, given with or without pembrolizumab, to patients with refractory or relapsed and refractory MM.
KEYNOTE-185 is a phase 3 study of lenalidomide and low-dose dexamethasone, given with or without pembrolizumab, to patients with newly diagnosed and treatment-naïve MM.
KEYNOTE-023 is a phase 1 trial of pembrolizumab in combination with backbone treatments. Cohort 1 of this trial was designed to evaluate pembrolizumab in combination with lenalidomide and dexamethasone in MM patients who received prior treatment with an immunomodulatory agent (lenalidomide, pomalidomide, or thalidomide).
Interim results from KEYNOTE-183 and KEYNOTE-185 revealed an increased risk of death for patients receiving pembrolizumab, when compared to patients receiving the control therapies.
Merck & Co., Inc., the company developing pembrolizumab, was informed of this risk by an external data monitoring committee. The company suspended enrollment in the trials and notified the FDA of the issue in June.
The following month, the FDA announced that all patients enrolled in KEYNOTE-183 and KEYNOTE-185, as well as patients in the pembrolizumab/lenalidomide/dexamethasone cohort of KEYNOTE-023, would discontinue investigational treatment with pembrolizumab.
FDA investigation
The FDA is examining data from the pembrolizumab trials and working with Merck to better understand the cause of the safety concerns, according to Woodcock.
The agency is also working with sponsors of other PD-1/PD-L1 inhibitors to examine other trials in which these drugs are being studied in combination with immunomodulatory agents and trials in which the inhibitors are being studied in combination with other classes of drugs in patients with hematologic malignancies.
Woodcock said the FDA will take appropriate action as warranted to ensure patients enrolled in these trials are protected and that doctors and researchers understand the risks associated with this investigational use.
The agency is also encouraging healthcare professionals and consumers to report any adverse events or side effects related to the use of pembrolizumab and other PD-1/PD-L1 inhibitors to FDA’s MedWatch Adverse Event Reporting Program.
Methotrexate could treat myeloproliferative neoplasms
Methotrexate (MTX) may be a feasible treatment option for myeloproliferative neoplasms (MPNs), according to preclinical research published in Haematologica.
Researchers tested low-dose MTX in mouse models that mimic human MPNs—essential thrombocythemia (ET) and polycythemia vera (PV).
The team found that MTX inhibited the JAK/STAT pathway, normalized some blood counts, and reduced splenomegaly in these mice.
“We have now shown pretty conclusively that we can use this approach to treat mouse models of human MPNs, results which provide a much more tangible prospect of success in humans,” said study author Martin Zeidler, PhD, of the University of Sheffield in Sheffield, UK.
Dr Zeidler and his colleagues tested MTX in transgenic mice whose endogenous JAK2 locus had been replaced by the human JAK2 V617F allele. These mice develop ET-like disease when heterozygous and PV-like disease when homozygous.
The researchers first treated wild-type mice and hJAK2 V617F age-matched littermates with either MTX or vehicle control for 28 days. The results indicated that low-dose MTX inhibits the JAK/STAT pathway.
The team then compared MTX and ruxolitinib in hJAK2 V617F-expressing mice.
MTX reduced hemoglobin levels, red blood cell counts, and hematocrit levels in heterozygous and homozygous hJAK2 V617F mice.
MTX also normalized white cell counts in heterozygous and homozygous mice, but platelet numbers and mean corpuscular volume were not significantly affected by treatment.
The researchers said MTX was as effective as ruxolitinib in these mice, but MTX treatment doesn’t result in general myelosuppression.
When the team analyzed bone marrow in the MTX-treated hJAK2 V617F mice, they found no reduction in cellularity or differentiation in any of the 3 hematopoietic lineages.
The researchers noted that homozygous mice have erythrocytic and megakaryocytic hyperplasia and polylobated nuclei in a proportion of megakaryocytes, and these phenotypes are subjectively reduced in MTX-treated mice. This suggests a disease-specific effect of MTX, rather than non-specific myelosuppression.
Both MTX and ruxolitinib reduced splenomegaly in hJAK2 V617F mice.
However, the researchers said they observed “modest increases” in reticulocyte numbers and spleen size in wild-type mice treated with MTX. These mice also had “slight increases” in pSTAT5 and PIM1 mRNA levels, but these same changes did not occur in hJAK2 V617F mice.
The researchers therefore concluded that a “detailed molecular analysis” of the interactions between MTX and wild-type JAK2 is needed.
The team is also hoping to start testing MTX in a clinical trial early next year, as these preclinical results suggest the drug could be effective in patients with ET or PV. And this might make MTX a low-cost alternative to therapies currently used to treat MPNs.
“Repurposing MTX has the potential to provide a new, molecularly targeted treatment for MPN patients within a budget accessible to healthcare systems throughout the world—a development that may ultimately provide substantial clinical and health economic benefits,” Dr Zeidler said.
Methotrexate (MTX) may be a feasible treatment option for myeloproliferative neoplasms (MPNs), according to preclinical research published in Haematologica.
Researchers tested low-dose MTX in mouse models that mimic human MPNs—essential thrombocythemia (ET) and polycythemia vera (PV).
The team found that MTX inhibited the JAK/STAT pathway, normalized some blood counts, and reduced splenomegaly in these mice.
“We have now shown pretty conclusively that we can use this approach to treat mouse models of human MPNs, results which provide a much more tangible prospect of success in humans,” said study author Martin Zeidler, PhD, of the University of Sheffield in Sheffield, UK.
Dr Zeidler and his colleagues tested MTX in transgenic mice whose endogenous JAK2 locus had been replaced by the human JAK2 V617F allele. These mice develop ET-like disease when heterozygous and PV-like disease when homozygous.
The researchers first treated wild-type mice and hJAK2 V617F age-matched littermates with either MTX or vehicle control for 28 days. The results indicated that low-dose MTX inhibits the JAK/STAT pathway.
The team then compared MTX and ruxolitinib in hJAK2 V617F-expressing mice.
MTX reduced hemoglobin levels, red blood cell counts, and hematocrit levels in heterozygous and homozygous hJAK2 V617F mice.
MTX also normalized white cell counts in heterozygous and homozygous mice, but platelet numbers and mean corpuscular volume were not significantly affected by treatment.
The researchers said MTX was as effective as ruxolitinib in these mice, but MTX treatment doesn’t result in general myelosuppression.
When the team analyzed bone marrow in the MTX-treated hJAK2 V617F mice, they found no reduction in cellularity or differentiation in any of the 3 hematopoietic lineages.
The researchers noted that homozygous mice have erythrocytic and megakaryocytic hyperplasia and polylobated nuclei in a proportion of megakaryocytes, and these phenotypes are subjectively reduced in MTX-treated mice. This suggests a disease-specific effect of MTX, rather than non-specific myelosuppression.
Both MTX and ruxolitinib reduced splenomegaly in hJAK2 V617F mice.
However, the researchers said they observed “modest increases” in reticulocyte numbers and spleen size in wild-type mice treated with MTX. These mice also had “slight increases” in pSTAT5 and PIM1 mRNA levels, but these same changes did not occur in hJAK2 V617F mice.
The researchers therefore concluded that a “detailed molecular analysis” of the interactions between MTX and wild-type JAK2 is needed.
The team is also hoping to start testing MTX in a clinical trial early next year, as these preclinical results suggest the drug could be effective in patients with ET or PV. And this might make MTX a low-cost alternative to therapies currently used to treat MPNs.
“Repurposing MTX has the potential to provide a new, molecularly targeted treatment for MPN patients within a budget accessible to healthcare systems throughout the world—a development that may ultimately provide substantial clinical and health economic benefits,” Dr Zeidler said.
Methotrexate (MTX) may be a feasible treatment option for myeloproliferative neoplasms (MPNs), according to preclinical research published in Haematologica.
Researchers tested low-dose MTX in mouse models that mimic human MPNs—essential thrombocythemia (ET) and polycythemia vera (PV).
The team found that MTX inhibited the JAK/STAT pathway, normalized some blood counts, and reduced splenomegaly in these mice.
“We have now shown pretty conclusively that we can use this approach to treat mouse models of human MPNs, results which provide a much more tangible prospect of success in humans,” said study author Martin Zeidler, PhD, of the University of Sheffield in Sheffield, UK.
Dr Zeidler and his colleagues tested MTX in transgenic mice whose endogenous JAK2 locus had been replaced by the human JAK2 V617F allele. These mice develop ET-like disease when heterozygous and PV-like disease when homozygous.
The researchers first treated wild-type mice and hJAK2 V617F age-matched littermates with either MTX or vehicle control for 28 days. The results indicated that low-dose MTX inhibits the JAK/STAT pathway.
The team then compared MTX and ruxolitinib in hJAK2 V617F-expressing mice.
MTX reduced hemoglobin levels, red blood cell counts, and hematocrit levels in heterozygous and homozygous hJAK2 V617F mice.
MTX also normalized white cell counts in heterozygous and homozygous mice, but platelet numbers and mean corpuscular volume were not significantly affected by treatment.
The researchers said MTX was as effective as ruxolitinib in these mice, but MTX treatment doesn’t result in general myelosuppression.
When the team analyzed bone marrow in the MTX-treated hJAK2 V617F mice, they found no reduction in cellularity or differentiation in any of the 3 hematopoietic lineages.
The researchers noted that homozygous mice have erythrocytic and megakaryocytic hyperplasia and polylobated nuclei in a proportion of megakaryocytes, and these phenotypes are subjectively reduced in MTX-treated mice. This suggests a disease-specific effect of MTX, rather than non-specific myelosuppression.
Both MTX and ruxolitinib reduced splenomegaly in hJAK2 V617F mice.
However, the researchers said they observed “modest increases” in reticulocyte numbers and spleen size in wild-type mice treated with MTX. These mice also had “slight increases” in pSTAT5 and PIM1 mRNA levels, but these same changes did not occur in hJAK2 V617F mice.
The researchers therefore concluded that a “detailed molecular analysis” of the interactions between MTX and wild-type JAK2 is needed.
The team is also hoping to start testing MTX in a clinical trial early next year, as these preclinical results suggest the drug could be effective in patients with ET or PV. And this might make MTX a low-cost alternative to therapies currently used to treat MPNs.
“Repurposing MTX has the potential to provide a new, molecularly targeted treatment for MPN patients within a budget accessible to healthcare systems throughout the world—a development that may ultimately provide substantial clinical and health economic benefits,” Dr Zeidler said.
Drug receives orphan designation for ocular GVHD
The US Food and Drug Administration (FDA) has granted orphan drug designation to OCU300 (brimonidine tartrate) for the treatment of ocular graft-versus-host disease (oGVHD) occurring after allogeneic hematopoietic stem cell transplant.
Brimonidine tartrate is an alpha adrenergic agonist that is already FDA-approved to lower intraocular pressure in patients with open-angle glaucoma or ocular hypertension.
Ocugen Inc. is repurposing the drug as OCU300 for the treatment of oGVHD under the FDA’s 505(b)(2) regulatory pathway.
“We are very excited to receive the first-ever orphan drug designation by the FDA for oGVHD, emphasizing the unmet medical need for patients with this disease,” said Shankar Musunuri, PhD, chairman, chief executive officer, and co-founder of Ocugen Inc.
“This is a significant milestone that will allow us to further advance the clinical development of OCU300, with a proprietary nanoemulsion, into a phase 3 clinical trial in the near future.”
According to Ocugen, OCU300 produced a beneficial effect in 90% of patients with oGVHD in an observational study, and the drug did not produce significant side effects.
About orphan designation
The FDA grants orphan designation to drugs and biologics intended to treat, diagnose, or prevent diseases/disorders that affect fewer than 200,000 people in the US.
The designation provides incentives for sponsors to develop products for rare diseases. This may include tax credits toward the cost of clinical trials, prescription drug user fee waivers, and 7 years of market exclusivity if the product is approved.
The US Food and Drug Administration (FDA) has granted orphan drug designation to OCU300 (brimonidine tartrate) for the treatment of ocular graft-versus-host disease (oGVHD) occurring after allogeneic hematopoietic stem cell transplant.
Brimonidine tartrate is an alpha adrenergic agonist that is already FDA-approved to lower intraocular pressure in patients with open-angle glaucoma or ocular hypertension.
Ocugen Inc. is repurposing the drug as OCU300 for the treatment of oGVHD under the FDA’s 505(b)(2) regulatory pathway.
“We are very excited to receive the first-ever orphan drug designation by the FDA for oGVHD, emphasizing the unmet medical need for patients with this disease,” said Shankar Musunuri, PhD, chairman, chief executive officer, and co-founder of Ocugen Inc.
“This is a significant milestone that will allow us to further advance the clinical development of OCU300, with a proprietary nanoemulsion, into a phase 3 clinical trial in the near future.”
According to Ocugen, OCU300 produced a beneficial effect in 90% of patients with oGVHD in an observational study, and the drug did not produce significant side effects.
About orphan designation
The FDA grants orphan designation to drugs and biologics intended to treat, diagnose, or prevent diseases/disorders that affect fewer than 200,000 people in the US.
The designation provides incentives for sponsors to develop products for rare diseases. This may include tax credits toward the cost of clinical trials, prescription drug user fee waivers, and 7 years of market exclusivity if the product is approved.
The US Food and Drug Administration (FDA) has granted orphan drug designation to OCU300 (brimonidine tartrate) for the treatment of ocular graft-versus-host disease (oGVHD) occurring after allogeneic hematopoietic stem cell transplant.
Brimonidine tartrate is an alpha adrenergic agonist that is already FDA-approved to lower intraocular pressure in patients with open-angle glaucoma or ocular hypertension.
Ocugen Inc. is repurposing the drug as OCU300 for the treatment of oGVHD under the FDA’s 505(b)(2) regulatory pathway.
“We are very excited to receive the first-ever orphan drug designation by the FDA for oGVHD, emphasizing the unmet medical need for patients with this disease,” said Shankar Musunuri, PhD, chairman, chief executive officer, and co-founder of Ocugen Inc.
“This is a significant milestone that will allow us to further advance the clinical development of OCU300, with a proprietary nanoemulsion, into a phase 3 clinical trial in the near future.”
According to Ocugen, OCU300 produced a beneficial effect in 90% of patients with oGVHD in an observational study, and the drug did not produce significant side effects.
About orphan designation
The FDA grants orphan designation to drugs and biologics intended to treat, diagnose, or prevent diseases/disorders that affect fewer than 200,000 people in the US.
The designation provides incentives for sponsors to develop products for rare diseases. This may include tax credits toward the cost of clinical trials, prescription drug user fee waivers, and 7 years of market exclusivity if the product is approved.
KRD appears more active, less safe than KCD in newly diagnosed MM
MADRID—New research suggests one triplet regimen may be more active but also more toxic than another in patients with newly diagnosed multiple myeloma (MM).
In the FORTE trial, the combination of carfilzomib, lenalidomide, and dexamethasone (KRD) produced higher response rates than carfilzomib, cyclophosphamide, and dexamethasone (KCD).
However, treatment with KRD also produced significantly more grade 3/4 non-hematologic adverse events (AEs) and serious AEs than the KCD regimen.
Francesca Gay, MD, PhD, of University of Torino in Italy, presented these results, from a planned interim analysis of FORTE, at the 22nd Congress of the European Hematology Association (EHA) as abstract S410.
The trial enrolled 477 MM patients younger than 65 years of age.
The patients were randomized to receive:
- Four 28-day KCD cycles (n=154)
Carfilzomib at 20 mg/m2 (for cycles 1 and 2) or 36 mg/m2 (for subsequent cycles) on days 1, 2, 8, 9, 15, and 16
Cyclophosphamide at 300 mg/m2 on days 1, 8, and 15
Dexamethasone at 20 mg on days 1, 2, 8, 9, 15, 16, 22, and 23
- Four 28-day KRD cycles (n=309)
Carfilzomib and dexamethasone as above
Lenalidomide at 25 mg on days 1-21
After the fourth induction cycle, all patients received cyclophosphamide at 2 g/m2, followed by peripheral blood stem cell (PBSC) collection for autologous stem cell transplant.
Patient characteristics
The median age was 57 (range, 52-62) in the KCD arm and the KRD arm (range, 51-62). In both arms, 55% of patients were male.
Roughly half of patients in both arms had an ISS stage of I (52% in the KCD arm and 51% in the KRD arm), 31% of patients in both arms were stage II, and 17% were stage III.
Fifty-eight percent of patients in the KCD arm and 59% in the KRD arm did not have t(4;14), t(14;16), or del17. Thirty-one percent and 26%, respectively, did have one of these cytogenetic abnormalities. (For the remaining patients, cytogenetic risk data were missing.)
PBSC mobilization and response
The median number of PBSCs collected was 8.6 x 106/kg in the KCD arm and 6.3 x 106/kg in the KRD arm. Plerixafor was required in 6% of patients in the KCD arm and 28% of patients in the KRD arm (P<0.001).
Ninety-two percent of patients in the KCD arm and 96% in the KRD arm had a partial response or better. Sixty-one percent and 74%, respectively, had a very good partial response (P=0.01). Six percent and 15%, respectively, had a complete response.
Safety
Grade 3/4 hematologic AEs and serious AEs (in the KRD and KCD arms, respectively) were thrombocytopenia (2% and 1%), neutropenia (6% and 5%), and anemia (2% and 3%). Seven percent of KRD patients and 6% of KCD patients had at least 1 grade 3/4 or serious hematologic AE.
Grade 3/4 non-hematologic AEs and serious AEs (in the KRD and KCD arms, respectively) included dermatologic events (8% and 1%, P<0.001), renal events (1% and 2%), fever (4% and 1%), infections (5% and 3%), gastrointestinal AEs (2% and 1%), hepatic events (8% and 1%, P<0.001), venous thromboembolism (1% and 0%), hypertension (3% and 2%), and cardiac events (1% and 2%).
Thirty-two percent of KRD patients and 16% of KCD patients had at least 1 grade 3/4 or serious non-hematologic AE (P<0.001).
Four percent of patients in the KRD arm and 2% in the KCD arm discontinued treatment due to AEs. Fifteen percent and 6%, respectively, reduced the dose of at least 1 drug (P=0.005).
One percent of patients in the KRD arm and 2% in the KCD arm died from AEs. In the KCD arm, 1 patient had a sudden death, and 1 died of pneumonia. In the KRD arm, there was 1 sudden death in a patient with sepsis, 1 patient died of infection, and 1 died of cardiac arrest (this patient previously discontinued treatment due to renal failure).
MADRID—New research suggests one triplet regimen may be more active but also more toxic than another in patients with newly diagnosed multiple myeloma (MM).
In the FORTE trial, the combination of carfilzomib, lenalidomide, and dexamethasone (KRD) produced higher response rates than carfilzomib, cyclophosphamide, and dexamethasone (KCD).
However, treatment with KRD also produced significantly more grade 3/4 non-hematologic adverse events (AEs) and serious AEs than the KCD regimen.
Francesca Gay, MD, PhD, of University of Torino in Italy, presented these results, from a planned interim analysis of FORTE, at the 22nd Congress of the European Hematology Association (EHA) as abstract S410.
The trial enrolled 477 MM patients younger than 65 years of age.
The patients were randomized to receive:
- Four 28-day KCD cycles (n=154)
Carfilzomib at 20 mg/m2 (for cycles 1 and 2) or 36 mg/m2 (for subsequent cycles) on days 1, 2, 8, 9, 15, and 16
Cyclophosphamide at 300 mg/m2 on days 1, 8, and 15
Dexamethasone at 20 mg on days 1, 2, 8, 9, 15, 16, 22, and 23
- Four 28-day KRD cycles (n=309)
Carfilzomib and dexamethasone as above
Lenalidomide at 25 mg on days 1-21
After the fourth induction cycle, all patients received cyclophosphamide at 2 g/m2, followed by peripheral blood stem cell (PBSC) collection for autologous stem cell transplant.
Patient characteristics
The median age was 57 (range, 52-62) in the KCD arm and the KRD arm (range, 51-62). In both arms, 55% of patients were male.
Roughly half of patients in both arms had an ISS stage of I (52% in the KCD arm and 51% in the KRD arm), 31% of patients in both arms were stage II, and 17% were stage III.
Fifty-eight percent of patients in the KCD arm and 59% in the KRD arm did not have t(4;14), t(14;16), or del17. Thirty-one percent and 26%, respectively, did have one of these cytogenetic abnormalities. (For the remaining patients, cytogenetic risk data were missing.)
PBSC mobilization and response
The median number of PBSCs collected was 8.6 x 106/kg in the KCD arm and 6.3 x 106/kg in the KRD arm. Plerixafor was required in 6% of patients in the KCD arm and 28% of patients in the KRD arm (P<0.001).
Ninety-two percent of patients in the KCD arm and 96% in the KRD arm had a partial response or better. Sixty-one percent and 74%, respectively, had a very good partial response (P=0.01). Six percent and 15%, respectively, had a complete response.
Safety
Grade 3/4 hematologic AEs and serious AEs (in the KRD and KCD arms, respectively) were thrombocytopenia (2% and 1%), neutropenia (6% and 5%), and anemia (2% and 3%). Seven percent of KRD patients and 6% of KCD patients had at least 1 grade 3/4 or serious hematologic AE.
Grade 3/4 non-hematologic AEs and serious AEs (in the KRD and KCD arms, respectively) included dermatologic events (8% and 1%, P<0.001), renal events (1% and 2%), fever (4% and 1%), infections (5% and 3%), gastrointestinal AEs (2% and 1%), hepatic events (8% and 1%, P<0.001), venous thromboembolism (1% and 0%), hypertension (3% and 2%), and cardiac events (1% and 2%).
Thirty-two percent of KRD patients and 16% of KCD patients had at least 1 grade 3/4 or serious non-hematologic AE (P<0.001).
Four percent of patients in the KRD arm and 2% in the KCD arm discontinued treatment due to AEs. Fifteen percent and 6%, respectively, reduced the dose of at least 1 drug (P=0.005).
One percent of patients in the KRD arm and 2% in the KCD arm died from AEs. In the KCD arm, 1 patient had a sudden death, and 1 died of pneumonia. In the KRD arm, there was 1 sudden death in a patient with sepsis, 1 patient died of infection, and 1 died of cardiac arrest (this patient previously discontinued treatment due to renal failure).
MADRID—New research suggests one triplet regimen may be more active but also more toxic than another in patients with newly diagnosed multiple myeloma (MM).
In the FORTE trial, the combination of carfilzomib, lenalidomide, and dexamethasone (KRD) produced higher response rates than carfilzomib, cyclophosphamide, and dexamethasone (KCD).
However, treatment with KRD also produced significantly more grade 3/4 non-hematologic adverse events (AEs) and serious AEs than the KCD regimen.
Francesca Gay, MD, PhD, of University of Torino in Italy, presented these results, from a planned interim analysis of FORTE, at the 22nd Congress of the European Hematology Association (EHA) as abstract S410.
The trial enrolled 477 MM patients younger than 65 years of age.
The patients were randomized to receive:
- Four 28-day KCD cycles (n=154)
Carfilzomib at 20 mg/m2 (for cycles 1 and 2) or 36 mg/m2 (for subsequent cycles) on days 1, 2, 8, 9, 15, and 16
Cyclophosphamide at 300 mg/m2 on days 1, 8, and 15
Dexamethasone at 20 mg on days 1, 2, 8, 9, 15, 16, 22, and 23
- Four 28-day KRD cycles (n=309)
Carfilzomib and dexamethasone as above
Lenalidomide at 25 mg on days 1-21
After the fourth induction cycle, all patients received cyclophosphamide at 2 g/m2, followed by peripheral blood stem cell (PBSC) collection for autologous stem cell transplant.
Patient characteristics
The median age was 57 (range, 52-62) in the KCD arm and the KRD arm (range, 51-62). In both arms, 55% of patients were male.
Roughly half of patients in both arms had an ISS stage of I (52% in the KCD arm and 51% in the KRD arm), 31% of patients in both arms were stage II, and 17% were stage III.
Fifty-eight percent of patients in the KCD arm and 59% in the KRD arm did not have t(4;14), t(14;16), or del17. Thirty-one percent and 26%, respectively, did have one of these cytogenetic abnormalities. (For the remaining patients, cytogenetic risk data were missing.)
PBSC mobilization and response
The median number of PBSCs collected was 8.6 x 106/kg in the KCD arm and 6.3 x 106/kg in the KRD arm. Plerixafor was required in 6% of patients in the KCD arm and 28% of patients in the KRD arm (P<0.001).
Ninety-two percent of patients in the KCD arm and 96% in the KRD arm had a partial response or better. Sixty-one percent and 74%, respectively, had a very good partial response (P=0.01). Six percent and 15%, respectively, had a complete response.
Safety
Grade 3/4 hematologic AEs and serious AEs (in the KRD and KCD arms, respectively) were thrombocytopenia (2% and 1%), neutropenia (6% and 5%), and anemia (2% and 3%). Seven percent of KRD patients and 6% of KCD patients had at least 1 grade 3/4 or serious hematologic AE.
Grade 3/4 non-hematologic AEs and serious AEs (in the KRD and KCD arms, respectively) included dermatologic events (8% and 1%, P<0.001), renal events (1% and 2%), fever (4% and 1%), infections (5% and 3%), gastrointestinal AEs (2% and 1%), hepatic events (8% and 1%, P<0.001), venous thromboembolism (1% and 0%), hypertension (3% and 2%), and cardiac events (1% and 2%).
Thirty-two percent of KRD patients and 16% of KCD patients had at least 1 grade 3/4 or serious non-hematologic AE (P<0.001).
Four percent of patients in the KRD arm and 2% in the KCD arm discontinued treatment due to AEs. Fifteen percent and 6%, respectively, reduced the dose of at least 1 drug (P=0.005).
One percent of patients in the KRD arm and 2% in the KCD arm died from AEs. In the KCD arm, 1 patient had a sudden death, and 1 died of pneumonia. In the KRD arm, there was 1 sudden death in a patient with sepsis, 1 patient died of infection, and 1 died of cardiac arrest (this patient previously discontinued treatment due to renal failure).