User login
Psychiatry trainees drive COVID-19 palliative care in New York
As SARS-CoV-2 cases surged in New York this past spring, one hospital system met the growing demand for palliative care in COVID-19 patients in acute care and emergency settings by training and redeploying psychiatry trainees, producing 100 consultations during a crisis period. Developers of this program wrote about their experience in the Journal of Pain and Symptom Management.
Research shows that psychiatrists can play an important, complementary role in palliative care, but not many models have explored this in practice. Over a 45-day period in March and April, New York Presbyterian/Columbia University Irving Medical Center saw an influx of 7,600 COVID-19 patients. Many were critically ill, and palliative care needs skyrocketed. Initial efforts to install a palliative care team at the emergency department and a proactive consultation model in the step-down units failed to meet demand for consults.
COVID-19 patients present unique challenges. Their clinical trajectory is less clear than those with cancer or other illnesses, Daniel Shalev, MD, a fellow in hospice and palliative medicine at Columbia University/New York State Psychiatric Institute, New York, and the study’s first author, said in an interview. “Ethical and systems issues around distribution of scarce resources may inflect patients’ and physicians’ responses,” Dr. Shalev said. “And families may not be able to be at the bedside with patients.”
To rapidly expand the palliative care workforce and meet patient needs, Dr. Shalev and colleagues recruited 16 psychiatry trainees from NYP, Columbia University Irving Medical Center, and Weill Cornell Medicine to work at NYP/Columbia University Irving Medical Center’s section of adult palliative medicine. Senior general psychiatry residents, child and adolescent psychiatry fellows, addiction psychiatry fellows, and postresidency T32 research fellows became part of a psychiatry-palliative care liaison team, offering psychosocial support and care goal strategies to patients and families.
Already well-versed in serious illness communication and psychosocial aspects of medical illness, the residents and fellows received additional training and education about SARS-CoV-2 and goals-of-care conversations. Child and adolescent psychiatry fellows participated in a communication workshop about the virus at Weill Cornell Medicine.
Working closely with the medical center’s palliative care service, the liaison team did consults around the clock at the ED under the supervision of a consultation-liaison (C-L) psychiatrist specializing in primary palliative care skills. The team managed 16 cases a day during the peak of New York’s COVID-19 outbreak, operating on a rotating schedule of one to three shifts weekly. Some shifts took place remotely to reduce exposure to the virus.
“We were fortunate that New York Presbyterian was early and aggressive in ensuring all clinical staff had personal protective equipment” in the treatment of COVID-19 patients, Dr. Shalev said.
The C-L psychiatry coordinator served as a traffic controller of sorts, overseeing daily staffing changes, maintaining a psychiatry–palliative care liaison team–shared patient list, and ensuring follow-up and continuity on patient care. The rotating schedule freed up time for trainees to meet other research and outpatient obligations.
The liaison team held a meeting each morning and accompanied the adult palliative care service on its daily virtual rounds to help streamline case management and care coordination among the various palliative care channels. Modifications in personnel took place as cases started to recede. Overall, the team participated in 100 consultations.
The findings show that there is significant overlap in psychiatry and palliative care skill sets, Dr. Shalev said. “Furthermore, many patients benefiting from palliative care services have mental health needs. But there are gaps between psychiatry and palliative care, including a lack of collaboration and cross-training. Our model showed how easily our disciplines can work together to improve the care available to all patients,” he added.
Some things could have gone more smoothly. Working under the duress of a pandemic, project leaders didn’t have enough time to train and supervise the team about advanced symptom management. Psychiatry staff members also weren’t as comfortable with nonpsychiatric symptom management as serious illness communication and psychiatric symptom management. Dr. Shalev expects these growth areas to improve over time.
The model could easily translate to other facilities, he believes. As of this writing, the liaison team was transitioning to a longer-term assignment involving patients on mechanical ventilation and their families.
The program increased access to care during a time of limited resources,and successfully combined psychiatric and palliative services – two specialties that, at times, can have conflicting recommendations, noted Maria I. Lapid, MD, a professor of psychiatry at the Mayo Clinic in Rochester, Minn., and a faculty member of the Mayo Clinic Center for Palliative Medicine, who was not part of the study. As urgent training for psychiatric trainees proved useful in the current crisis, long-term psychiatric programs will need to explore and consider how to integrate palliative care training into the psychiatric curriculum.
“Not only is this relevant in the current pandemic, but this will continue to be relevant in the context of the rapidly aging population” in the United States, said Dr. Lapid.
Dr. Shalev and colleagues declared no conflicts of interest in their study. Their research received no funds or grants from public, commercial, or nonprofit agencies.
SOURCE: Shalev D et al. J Pain Symptom Manage. 2020 Jun 13. doi.org/10.1016/j.jpainsymman.2020.06.009.
As SARS-CoV-2 cases surged in New York this past spring, one hospital system met the growing demand for palliative care in COVID-19 patients in acute care and emergency settings by training and redeploying psychiatry trainees, producing 100 consultations during a crisis period. Developers of this program wrote about their experience in the Journal of Pain and Symptom Management.
Research shows that psychiatrists can play an important, complementary role in palliative care, but not many models have explored this in practice. Over a 45-day period in March and April, New York Presbyterian/Columbia University Irving Medical Center saw an influx of 7,600 COVID-19 patients. Many were critically ill, and palliative care needs skyrocketed. Initial efforts to install a palliative care team at the emergency department and a proactive consultation model in the step-down units failed to meet demand for consults.
COVID-19 patients present unique challenges. Their clinical trajectory is less clear than those with cancer or other illnesses, Daniel Shalev, MD, a fellow in hospice and palliative medicine at Columbia University/New York State Psychiatric Institute, New York, and the study’s first author, said in an interview. “Ethical and systems issues around distribution of scarce resources may inflect patients’ and physicians’ responses,” Dr. Shalev said. “And families may not be able to be at the bedside with patients.”
To rapidly expand the palliative care workforce and meet patient needs, Dr. Shalev and colleagues recruited 16 psychiatry trainees from NYP, Columbia University Irving Medical Center, and Weill Cornell Medicine to work at NYP/Columbia University Irving Medical Center’s section of adult palliative medicine. Senior general psychiatry residents, child and adolescent psychiatry fellows, addiction psychiatry fellows, and postresidency T32 research fellows became part of a psychiatry-palliative care liaison team, offering psychosocial support and care goal strategies to patients and families.
Already well-versed in serious illness communication and psychosocial aspects of medical illness, the residents and fellows received additional training and education about SARS-CoV-2 and goals-of-care conversations. Child and adolescent psychiatry fellows participated in a communication workshop about the virus at Weill Cornell Medicine.
Working closely with the medical center’s palliative care service, the liaison team did consults around the clock at the ED under the supervision of a consultation-liaison (C-L) psychiatrist specializing in primary palliative care skills. The team managed 16 cases a day during the peak of New York’s COVID-19 outbreak, operating on a rotating schedule of one to three shifts weekly. Some shifts took place remotely to reduce exposure to the virus.
“We were fortunate that New York Presbyterian was early and aggressive in ensuring all clinical staff had personal protective equipment” in the treatment of COVID-19 patients, Dr. Shalev said.
The C-L psychiatry coordinator served as a traffic controller of sorts, overseeing daily staffing changes, maintaining a psychiatry–palliative care liaison team–shared patient list, and ensuring follow-up and continuity on patient care. The rotating schedule freed up time for trainees to meet other research and outpatient obligations.
The liaison team held a meeting each morning and accompanied the adult palliative care service on its daily virtual rounds to help streamline case management and care coordination among the various palliative care channels. Modifications in personnel took place as cases started to recede. Overall, the team participated in 100 consultations.
The findings show that there is significant overlap in psychiatry and palliative care skill sets, Dr. Shalev said. “Furthermore, many patients benefiting from palliative care services have mental health needs. But there are gaps between psychiatry and palliative care, including a lack of collaboration and cross-training. Our model showed how easily our disciplines can work together to improve the care available to all patients,” he added.
Some things could have gone more smoothly. Working under the duress of a pandemic, project leaders didn’t have enough time to train and supervise the team about advanced symptom management. Psychiatry staff members also weren’t as comfortable with nonpsychiatric symptom management as serious illness communication and psychiatric symptom management. Dr. Shalev expects these growth areas to improve over time.
The model could easily translate to other facilities, he believes. As of this writing, the liaison team was transitioning to a longer-term assignment involving patients on mechanical ventilation and their families.
The program increased access to care during a time of limited resources,and successfully combined psychiatric and palliative services – two specialties that, at times, can have conflicting recommendations, noted Maria I. Lapid, MD, a professor of psychiatry at the Mayo Clinic in Rochester, Minn., and a faculty member of the Mayo Clinic Center for Palliative Medicine, who was not part of the study. As urgent training for psychiatric trainees proved useful in the current crisis, long-term psychiatric programs will need to explore and consider how to integrate palliative care training into the psychiatric curriculum.
“Not only is this relevant in the current pandemic, but this will continue to be relevant in the context of the rapidly aging population” in the United States, said Dr. Lapid.
Dr. Shalev and colleagues declared no conflicts of interest in their study. Their research received no funds or grants from public, commercial, or nonprofit agencies.
SOURCE: Shalev D et al. J Pain Symptom Manage. 2020 Jun 13. doi.org/10.1016/j.jpainsymman.2020.06.009.
As SARS-CoV-2 cases surged in New York this past spring, one hospital system met the growing demand for palliative care in COVID-19 patients in acute care and emergency settings by training and redeploying psychiatry trainees, producing 100 consultations during a crisis period. Developers of this program wrote about their experience in the Journal of Pain and Symptom Management.
Research shows that psychiatrists can play an important, complementary role in palliative care, but not many models have explored this in practice. Over a 45-day period in March and April, New York Presbyterian/Columbia University Irving Medical Center saw an influx of 7,600 COVID-19 patients. Many were critically ill, and palliative care needs skyrocketed. Initial efforts to install a palliative care team at the emergency department and a proactive consultation model in the step-down units failed to meet demand for consults.
COVID-19 patients present unique challenges. Their clinical trajectory is less clear than those with cancer or other illnesses, Daniel Shalev, MD, a fellow in hospice and palliative medicine at Columbia University/New York State Psychiatric Institute, New York, and the study’s first author, said in an interview. “Ethical and systems issues around distribution of scarce resources may inflect patients’ and physicians’ responses,” Dr. Shalev said. “And families may not be able to be at the bedside with patients.”
To rapidly expand the palliative care workforce and meet patient needs, Dr. Shalev and colleagues recruited 16 psychiatry trainees from NYP, Columbia University Irving Medical Center, and Weill Cornell Medicine to work at NYP/Columbia University Irving Medical Center’s section of adult palliative medicine. Senior general psychiatry residents, child and adolescent psychiatry fellows, addiction psychiatry fellows, and postresidency T32 research fellows became part of a psychiatry-palliative care liaison team, offering psychosocial support and care goal strategies to patients and families.
Already well-versed in serious illness communication and psychosocial aspects of medical illness, the residents and fellows received additional training and education about SARS-CoV-2 and goals-of-care conversations. Child and adolescent psychiatry fellows participated in a communication workshop about the virus at Weill Cornell Medicine.
Working closely with the medical center’s palliative care service, the liaison team did consults around the clock at the ED under the supervision of a consultation-liaison (C-L) psychiatrist specializing in primary palliative care skills. The team managed 16 cases a day during the peak of New York’s COVID-19 outbreak, operating on a rotating schedule of one to three shifts weekly. Some shifts took place remotely to reduce exposure to the virus.
“We were fortunate that New York Presbyterian was early and aggressive in ensuring all clinical staff had personal protective equipment” in the treatment of COVID-19 patients, Dr. Shalev said.
The C-L psychiatry coordinator served as a traffic controller of sorts, overseeing daily staffing changes, maintaining a psychiatry–palliative care liaison team–shared patient list, and ensuring follow-up and continuity on patient care. The rotating schedule freed up time for trainees to meet other research and outpatient obligations.
The liaison team held a meeting each morning and accompanied the adult palliative care service on its daily virtual rounds to help streamline case management and care coordination among the various palliative care channels. Modifications in personnel took place as cases started to recede. Overall, the team participated in 100 consultations.
The findings show that there is significant overlap in psychiatry and palliative care skill sets, Dr. Shalev said. “Furthermore, many patients benefiting from palliative care services have mental health needs. But there are gaps between psychiatry and palliative care, including a lack of collaboration and cross-training. Our model showed how easily our disciplines can work together to improve the care available to all patients,” he added.
Some things could have gone more smoothly. Working under the duress of a pandemic, project leaders didn’t have enough time to train and supervise the team about advanced symptom management. Psychiatry staff members also weren’t as comfortable with nonpsychiatric symptom management as serious illness communication and psychiatric symptom management. Dr. Shalev expects these growth areas to improve over time.
The model could easily translate to other facilities, he believes. As of this writing, the liaison team was transitioning to a longer-term assignment involving patients on mechanical ventilation and their families.
The program increased access to care during a time of limited resources,and successfully combined psychiatric and palliative services – two specialties that, at times, can have conflicting recommendations, noted Maria I. Lapid, MD, a professor of psychiatry at the Mayo Clinic in Rochester, Minn., and a faculty member of the Mayo Clinic Center for Palliative Medicine, who was not part of the study. As urgent training for psychiatric trainees proved useful in the current crisis, long-term psychiatric programs will need to explore and consider how to integrate palliative care training into the psychiatric curriculum.
“Not only is this relevant in the current pandemic, but this will continue to be relevant in the context of the rapidly aging population” in the United States, said Dr. Lapid.
Dr. Shalev and colleagues declared no conflicts of interest in their study. Their research received no funds or grants from public, commercial, or nonprofit agencies.
SOURCE: Shalev D et al. J Pain Symptom Manage. 2020 Jun 13. doi.org/10.1016/j.jpainsymman.2020.06.009.
Pulmonary function tests can’t substitute for high-resolution CT in early systemic sclerosis ILD screening
Clinicians shouldn’t rely on pulmonary function tests (PFTs) alone to screen for interstitial lung disease (ILD). The tests performed poorly in a retrospective study of 212 patients with systemic sclerosis, reinforcing the findings of previous studies.
Any screening algorithm should include high-resolution CT (HRCT), which is good at prognosticating disease, the investigators wrote in Arthritis & Rheumatology. “I think all newly diagnosed systemic sclerosis patients should have a full set of PFTs (spirometry, lung volumes, and diffusion capacity) and an HRCT at baseline to evaluate for ILD,” the study’s lead author, Elana J. Bernstein, MD, said in an interview.
ILD is a leading cause of death in systemic sclerosis (SSc) patients, affecting 40%-60% of those with the disease. HRCT is currently the preferred option for detection of ILD. PFTs are commonly used to screen for ILD but haven’t performed well in previous studies. “Someone can have abnormalities on HRCT that are consistent with ILD but still have PFTs that are in the ‘normal’ range,” explained Dr. Bernstein of Columbia University, New York. One cross-sectional study of 102 SSc patients found that the test’s sensitivity for the detection of ILD on HRCT was just 37.5% when forced vital capacity (FVC) <80% predicted.
Investigators sought to assess performance characteristics of PFTs in patients with early diffuse cutaneous SSc, a cohort at high risk of developing ILD. The study enlisted patients from the Prospective Registry of Early Systemic Sclerosis (PRESS), a multicenter, prospective cohort study of adults with early diffuse cutaneous SSc. Overall, 212 patients at 11 U.S. academic medical centers participated in the study from April 2012 to January 2019.
All patients had spirometry (PFT) and HRCT chest scans. PFTs were conducted per American Thoracic Society/European Respiratory Society guidelines. The investigators calculated test characteristics for single PFT and combinations of PFT parameters for the detection of ILD on HRCT. The HRCTs were ordered at the discretion of treating physicians, and scrutinized for ILD features such as reticular changes, honeycombing, traction bronchiectasis, and ground-glass opacities. The investigators defined the lower limit of normal for FVC, total lung capacity, and diffusion capacity for carbon monoxide (DLCO) as 80% predicted.
Overall, Dr. Bernstein and her colleagues found that PFTs lacked sufficient sensitivity and negative predictive value for the detection of ILD on HRCT in these patients.
An FVC <80% predicted performed at only 63% sensitivity and an false negative rate of 37%. Total lung capacity or DLCO <80% predicted had a sensitivity of 46% and 80%, respectively. The combination of FVC or DLCO <80% predicted raised sensitivity to 85%. However, the addition of total lung capacity to this combination did not improve results.
Overall, PFTs had a positive predictive value of 64%-74% and an negative predictive value of 61%-70%. “This means that PFT alone will not accurately predict the presence of ILD in about 35%, and not be correctly negative in about 35%,” observed Daniel E. Furst, MD, professor of medicine (emeritus) at the University of California, Los Angeles, and professor of rheumatology at the University of California, Los Angeles.
While the combination of FVC <80% predicted or DLCO <80% predicted performed better than the other parameters, the sensitivity “is inadequate for an ILD screening test as it results in an false negative rate of 15%, thereby falsely reassuring 15% of patients that they do not have ILD when in fact they do,” the investigators observed.
“This study reinforces the notion that PFTs alone are ineffective screening tools for ILD in the presence of systemic sclerosis, particularly for patients with early systemic sclerosis,” said Elizabeth Volkmann, MD, MS, assistant professor and codirector of the CTD-ILD program in the division of rheumatology at the University of California, Los Angeles.
The study’s scope was relatively small, yet the results provide further evidence to show that HRCT should be performed in all SSc patients to screen for the presence of ILD, Dr. Volkmann said in an interview.
Other research has demonstrated the value of baseline HRCT as a prognosticator of ILD outcomes. The method provides useful information about the degree of fibrosis and degree of damage in early-stage disease, said Dr. Furst, also an adjunct professor at the University of Washington, Seattle, and a research professor at the University of Florence (Italy). “If there’s honeycombing, that’s a bad prognosis. If it’s ground glass or reticular changes, the prognosis is better.
“Once there’s a lot of damage, it’s much harder to interpret disease with HRCT,” he added.
HRCT and PFT work well together to assess what’s happening in patients, Dr. Furst explained. HRCT provides an idea of anatomic changes, whereas PFT outlines aspects of functional change to diagnose early ILD in early diffuse SSc. The study results should not apply to patients with later disease who have more developed ILD, he noted.
The investigators acknowledged that they weren’t able to categorize and analyze patients according to disease extent because they didn’t quantify the extent of ILD. Another limitation was that the HRCTs and PFTs were ordered at the discretion of individual physicians, which means that not all participants received the tests.
“Although the tests were done in 90% of the population, there is still a probability of a significant selection bias,” Dr. Furst said.
Dr. Bernstein and several other coauthors in the study received grants from the National Institute of Arthritis and Musculoskeletal and Skin Diseases to support their work. Dr. Furst disclosed receiving grant/research support from and/or consulting for AbbVie, Actelion, Amgen, Bristol-Myers Squibb, Corbus, the National Institutes of Health, Novartis, Pfizer, and Roche/Genentech. Dr. Volkmann disclosed consulting for and/or receiving grant support from Boehringer Ingelheim, Corbus, and Forbius.
SOURCE: Bernstein EJ et al. Arthritis Rheumatol. 2020 Jun 25. doi: 10.1002/art.41415.
Clinicians shouldn’t rely on pulmonary function tests (PFTs) alone to screen for interstitial lung disease (ILD). The tests performed poorly in a retrospective study of 212 patients with systemic sclerosis, reinforcing the findings of previous studies.
Any screening algorithm should include high-resolution CT (HRCT), which is good at prognosticating disease, the investigators wrote in Arthritis & Rheumatology. “I think all newly diagnosed systemic sclerosis patients should have a full set of PFTs (spirometry, lung volumes, and diffusion capacity) and an HRCT at baseline to evaluate for ILD,” the study’s lead author, Elana J. Bernstein, MD, said in an interview.
ILD is a leading cause of death in systemic sclerosis (SSc) patients, affecting 40%-60% of those with the disease. HRCT is currently the preferred option for detection of ILD. PFTs are commonly used to screen for ILD but haven’t performed well in previous studies. “Someone can have abnormalities on HRCT that are consistent with ILD but still have PFTs that are in the ‘normal’ range,” explained Dr. Bernstein of Columbia University, New York. One cross-sectional study of 102 SSc patients found that the test’s sensitivity for the detection of ILD on HRCT was just 37.5% when forced vital capacity (FVC) <80% predicted.
Investigators sought to assess performance characteristics of PFTs in patients with early diffuse cutaneous SSc, a cohort at high risk of developing ILD. The study enlisted patients from the Prospective Registry of Early Systemic Sclerosis (PRESS), a multicenter, prospective cohort study of adults with early diffuse cutaneous SSc. Overall, 212 patients at 11 U.S. academic medical centers participated in the study from April 2012 to January 2019.
All patients had spirometry (PFT) and HRCT chest scans. PFTs were conducted per American Thoracic Society/European Respiratory Society guidelines. The investigators calculated test characteristics for single PFT and combinations of PFT parameters for the detection of ILD on HRCT. The HRCTs were ordered at the discretion of treating physicians, and scrutinized for ILD features such as reticular changes, honeycombing, traction bronchiectasis, and ground-glass opacities. The investigators defined the lower limit of normal for FVC, total lung capacity, and diffusion capacity for carbon monoxide (DLCO) as 80% predicted.
Overall, Dr. Bernstein and her colleagues found that PFTs lacked sufficient sensitivity and negative predictive value for the detection of ILD on HRCT in these patients.
An FVC <80% predicted performed at only 63% sensitivity and an false negative rate of 37%. Total lung capacity or DLCO <80% predicted had a sensitivity of 46% and 80%, respectively. The combination of FVC or DLCO <80% predicted raised sensitivity to 85%. However, the addition of total lung capacity to this combination did not improve results.
Overall, PFTs had a positive predictive value of 64%-74% and an negative predictive value of 61%-70%. “This means that PFT alone will not accurately predict the presence of ILD in about 35%, and not be correctly negative in about 35%,” observed Daniel E. Furst, MD, professor of medicine (emeritus) at the University of California, Los Angeles, and professor of rheumatology at the University of California, Los Angeles.
While the combination of FVC <80% predicted or DLCO <80% predicted performed better than the other parameters, the sensitivity “is inadequate for an ILD screening test as it results in an false negative rate of 15%, thereby falsely reassuring 15% of patients that they do not have ILD when in fact they do,” the investigators observed.
“This study reinforces the notion that PFTs alone are ineffective screening tools for ILD in the presence of systemic sclerosis, particularly for patients with early systemic sclerosis,” said Elizabeth Volkmann, MD, MS, assistant professor and codirector of the CTD-ILD program in the division of rheumatology at the University of California, Los Angeles.
The study’s scope was relatively small, yet the results provide further evidence to show that HRCT should be performed in all SSc patients to screen for the presence of ILD, Dr. Volkmann said in an interview.
Other research has demonstrated the value of baseline HRCT as a prognosticator of ILD outcomes. The method provides useful information about the degree of fibrosis and degree of damage in early-stage disease, said Dr. Furst, also an adjunct professor at the University of Washington, Seattle, and a research professor at the University of Florence (Italy). “If there’s honeycombing, that’s a bad prognosis. If it’s ground glass or reticular changes, the prognosis is better.
“Once there’s a lot of damage, it’s much harder to interpret disease with HRCT,” he added.
HRCT and PFT work well together to assess what’s happening in patients, Dr. Furst explained. HRCT provides an idea of anatomic changes, whereas PFT outlines aspects of functional change to diagnose early ILD in early diffuse SSc. The study results should not apply to patients with later disease who have more developed ILD, he noted.
The investigators acknowledged that they weren’t able to categorize and analyze patients according to disease extent because they didn’t quantify the extent of ILD. Another limitation was that the HRCTs and PFTs were ordered at the discretion of individual physicians, which means that not all participants received the tests.
“Although the tests were done in 90% of the population, there is still a probability of a significant selection bias,” Dr. Furst said.
Dr. Bernstein and several other coauthors in the study received grants from the National Institute of Arthritis and Musculoskeletal and Skin Diseases to support their work. Dr. Furst disclosed receiving grant/research support from and/or consulting for AbbVie, Actelion, Amgen, Bristol-Myers Squibb, Corbus, the National Institutes of Health, Novartis, Pfizer, and Roche/Genentech. Dr. Volkmann disclosed consulting for and/or receiving grant support from Boehringer Ingelheim, Corbus, and Forbius.
SOURCE: Bernstein EJ et al. Arthritis Rheumatol. 2020 Jun 25. doi: 10.1002/art.41415.
Clinicians shouldn’t rely on pulmonary function tests (PFTs) alone to screen for interstitial lung disease (ILD). The tests performed poorly in a retrospective study of 212 patients with systemic sclerosis, reinforcing the findings of previous studies.
Any screening algorithm should include high-resolution CT (HRCT), which is good at prognosticating disease, the investigators wrote in Arthritis & Rheumatology. “I think all newly diagnosed systemic sclerosis patients should have a full set of PFTs (spirometry, lung volumes, and diffusion capacity) and an HRCT at baseline to evaluate for ILD,” the study’s lead author, Elana J. Bernstein, MD, said in an interview.
ILD is a leading cause of death in systemic sclerosis (SSc) patients, affecting 40%-60% of those with the disease. HRCT is currently the preferred option for detection of ILD. PFTs are commonly used to screen for ILD but haven’t performed well in previous studies. “Someone can have abnormalities on HRCT that are consistent with ILD but still have PFTs that are in the ‘normal’ range,” explained Dr. Bernstein of Columbia University, New York. One cross-sectional study of 102 SSc patients found that the test’s sensitivity for the detection of ILD on HRCT was just 37.5% when forced vital capacity (FVC) <80% predicted.
Investigators sought to assess performance characteristics of PFTs in patients with early diffuse cutaneous SSc, a cohort at high risk of developing ILD. The study enlisted patients from the Prospective Registry of Early Systemic Sclerosis (PRESS), a multicenter, prospective cohort study of adults with early diffuse cutaneous SSc. Overall, 212 patients at 11 U.S. academic medical centers participated in the study from April 2012 to January 2019.
All patients had spirometry (PFT) and HRCT chest scans. PFTs were conducted per American Thoracic Society/European Respiratory Society guidelines. The investigators calculated test characteristics for single PFT and combinations of PFT parameters for the detection of ILD on HRCT. The HRCTs were ordered at the discretion of treating physicians, and scrutinized for ILD features such as reticular changes, honeycombing, traction bronchiectasis, and ground-glass opacities. The investigators defined the lower limit of normal for FVC, total lung capacity, and diffusion capacity for carbon monoxide (DLCO) as 80% predicted.
Overall, Dr. Bernstein and her colleagues found that PFTs lacked sufficient sensitivity and negative predictive value for the detection of ILD on HRCT in these patients.
An FVC <80% predicted performed at only 63% sensitivity and an false negative rate of 37%. Total lung capacity or DLCO <80% predicted had a sensitivity of 46% and 80%, respectively. The combination of FVC or DLCO <80% predicted raised sensitivity to 85%. However, the addition of total lung capacity to this combination did not improve results.
Overall, PFTs had a positive predictive value of 64%-74% and an negative predictive value of 61%-70%. “This means that PFT alone will not accurately predict the presence of ILD in about 35%, and not be correctly negative in about 35%,” observed Daniel E. Furst, MD, professor of medicine (emeritus) at the University of California, Los Angeles, and professor of rheumatology at the University of California, Los Angeles.
While the combination of FVC <80% predicted or DLCO <80% predicted performed better than the other parameters, the sensitivity “is inadequate for an ILD screening test as it results in an false negative rate of 15%, thereby falsely reassuring 15% of patients that they do not have ILD when in fact they do,” the investigators observed.
“This study reinforces the notion that PFTs alone are ineffective screening tools for ILD in the presence of systemic sclerosis, particularly for patients with early systemic sclerosis,” said Elizabeth Volkmann, MD, MS, assistant professor and codirector of the CTD-ILD program in the division of rheumatology at the University of California, Los Angeles.
The study’s scope was relatively small, yet the results provide further evidence to show that HRCT should be performed in all SSc patients to screen for the presence of ILD, Dr. Volkmann said in an interview.
Other research has demonstrated the value of baseline HRCT as a prognosticator of ILD outcomes. The method provides useful information about the degree of fibrosis and degree of damage in early-stage disease, said Dr. Furst, also an adjunct professor at the University of Washington, Seattle, and a research professor at the University of Florence (Italy). “If there’s honeycombing, that’s a bad prognosis. If it’s ground glass or reticular changes, the prognosis is better.
“Once there’s a lot of damage, it’s much harder to interpret disease with HRCT,” he added.
HRCT and PFT work well together to assess what’s happening in patients, Dr. Furst explained. HRCT provides an idea of anatomic changes, whereas PFT outlines aspects of functional change to diagnose early ILD in early diffuse SSc. The study results should not apply to patients with later disease who have more developed ILD, he noted.
The investigators acknowledged that they weren’t able to categorize and analyze patients according to disease extent because they didn’t quantify the extent of ILD. Another limitation was that the HRCTs and PFTs were ordered at the discretion of individual physicians, which means that not all participants received the tests.
“Although the tests were done in 90% of the population, there is still a probability of a significant selection bias,” Dr. Furst said.
Dr. Bernstein and several other coauthors in the study received grants from the National Institute of Arthritis and Musculoskeletal and Skin Diseases to support their work. Dr. Furst disclosed receiving grant/research support from and/or consulting for AbbVie, Actelion, Amgen, Bristol-Myers Squibb, Corbus, the National Institutes of Health, Novartis, Pfizer, and Roche/Genentech. Dr. Volkmann disclosed consulting for and/or receiving grant support from Boehringer Ingelheim, Corbus, and Forbius.
SOURCE: Bernstein EJ et al. Arthritis Rheumatol. 2020 Jun 25. doi: 10.1002/art.41415.
FROM ARTHRITIS & RHEUMATOLOGY
Lifestyle changes may explain skin lesions in pandemic-era patients
such as lockdown conditions, which may be clarified with additional research.
Lindy P. Fox, MD, professor of dermatology at the University of California, San Francisco, who was not an author of either study, urged caution in interpreting these results. Data from the American Academy of Dermatology and a recent paper from the British Journal of Dermatology suggest a real association exists, at in least some patients. “It’s going to be true that most patients with toe lesions are PCR [polymerase chain reaction]-negative because it tends to be a late phenomenon when patients are no longer shedding virus,” Dr. Fox said in an interview.
Reports about chickenpox-like vesicles, urticaria, and other skin lesions in SARS-CoV-2 patients have circulated in the clinical literature and the media. Acute acro-ischemia has been cited as a potential sign of infection in adolescents and children.
One of the European studies, which was published in JAMA Dermatology, explored this association in 20 patients aged 1-18 years (mean age, 12.3 years), who presented with new-onset acral inflammatory lesions in their hands and feet at La Fe University Hospital, in Valencia, during the country’s peak quarantine period in April. Investigators conducted blood tests and reverse transcriptase–PCR (RT-PCR) for SARS-CoV-2, and six patients had skin biopsies.
Juncal Roca-Ginés, MD, of the department of dermatology, at the Hospital Universitario y Politécnico in La Fe, and coauthors, identified acral erythema in 6 (30%) of the cases, dactylitis in 4 (20%), purpuric maculopapules in 7 (35%), and a mixed pattern in 3 (15%). Serologic and viral testing yielded no positive results for SARS-CoV-2 or other viruses, and none of the patients exhibited COVID-19 symptoms such as fever, dry cough, sore throat, myalgia, or taste or smell disorders. In other findings, 45% of the patients had a history of vascular reactive disease of the hands, and 75% reported walking barefoot in their homes while staying at home. Only two patients reported taking medications.
In the six patients who had a biopsy, the findings were characteristic of chillblains, “confirming the clinical impression,” the authors wrote. Concluding that they could not show a relationship between acute acral skin changes and COVID-19, they noted that “other studies with improved microbiologic tests or molecular techniques aimed at demonstrating the presence of SARS-CoV-2 in the skin may help to clarify this problem.”
The other case series, which was also published in JAMA Dermatology and included 31 adults at a hospital in Brussels, who had recently developed chillblains, also looked for a connection between SARS-CoV-2 and chilblains, in April. Most of the participants were in their teens or 20s. Lesions had appeared on hands, feet, or on both extremities within 1-30 days of consultation, presenting as erythematous or purplish erythematous macules, occasionally with central vesicular or bullous lesions or necrotic areas. Patients reported pain, burning, and itching.
Skin biopsies were obtained in 22 patients and confirmed the diagnosis of chilblains; of the 15 with immunofluorescence analyses, 7 patients were found to have vasculitis of small-diameter vessels.
Of the 31 patients, 20 (64%) reported mild symptoms consistent with SARS-CoV-2, yet none of the RT-PCR or serologic test results showed signs of the virus in all 31 patients. “Because some patients had experienced chilblains for more than 15 days [under 30 days or less] at the time of inclusion, we can reasonably exclude the possibility that serologic testing was done too soon,” observed the authors. They also didn’t find eosinopenia, lymphopenia, and hyperferritinemia, which have been associated with COVID-19, they added.
Changes in lifestyle conditions during the pandemic may explain the appearance of these lesions, according to the authors of both studies, who mentioned that walking around in socks or bare feet and reduced physical activity could have indirectly led to the development of skin lesions.
It’s also possible that young people have less severe disease and a delayed reaction to the virus, Ignacio Torres-Navarro, MD, a dermatologist with La Fe University and the Spanish study’s corresponding author, said in an interview. Their feet may lack maturity in neurovascular regulation and/or the eccrine glands, which can happen in other diseases such as neutrophilic idiopathic eccrine hidradenitis. “In this context, perhaps there was an observational bias of the parents to the children when this manifestation was reported in the media. However, nothing has been demonstrated,” he said.
In an accompanying editor’s note, Claudia Hernandez, MD, of the departments of dermatology and pediatrics, Rush University Medical Center, Chicago, and Anna L. Bruckner, MD, of the departments of dermatology and pediatrics at the University of Colorado, Aurora, wrote that “it is still unclear whether a viral cytopathic process vs a viral reaction pattern or other mechanism is responsible for ‘COVID toes.’ ” Lack of confirmatory testing and reliance on indirect evidence of infection complicates this further, they noted, adding that “dermatologists must be aware of the protean cutaneous findings that are possibly associated with COVID-19, even if our understanding of their origins remains incomplete.”
In an interview, Dr. Fox, a member of the AAD’s’s COVID-19 Registry task force, offered other possible reasons for the negative antibody tests in the studies. The assay might not have been testing the correct antigen, or the timing of the test might not have been optimal. “More studies will help this become less controversial,” she said.
The authors of the two case series acknowledged potential limitations of their studies. Neither was large in scope: Both took place over a week’s time and included small cohorts. The Belgian study had no control group or long-term follow-up. Little is still known about the clinical manifestations and detection methods for SARS-CoV-2, noted the authors of the Spanish study.
The Spanish study received funding La Fe University Hospital’s department of dermatology, and the authors had no disclosures. The Belgian study received support from the Fondation Saint-Luc, which provided academic funding for its lead author, Marie Baeck, MD, PhD. Another author of this study received personal fees from the Fondation Saint-Luc and personal fees and nonfinancial support from Bioderma. The authors of the editor’s note had no disclosures.
SOURCES: Roca-Ginés J et al. JAMA Dermatol. 2020 Jun 25. doi: 10.1001/jamadermatol.2020.2340; Herman A et al. JAMA Dermatol. 2020 Jun 25. doi: 10.1001/jamadermatol.2020.2368.
such as lockdown conditions, which may be clarified with additional research.
Lindy P. Fox, MD, professor of dermatology at the University of California, San Francisco, who was not an author of either study, urged caution in interpreting these results. Data from the American Academy of Dermatology and a recent paper from the British Journal of Dermatology suggest a real association exists, at in least some patients. “It’s going to be true that most patients with toe lesions are PCR [polymerase chain reaction]-negative because it tends to be a late phenomenon when patients are no longer shedding virus,” Dr. Fox said in an interview.
Reports about chickenpox-like vesicles, urticaria, and other skin lesions in SARS-CoV-2 patients have circulated in the clinical literature and the media. Acute acro-ischemia has been cited as a potential sign of infection in adolescents and children.
One of the European studies, which was published in JAMA Dermatology, explored this association in 20 patients aged 1-18 years (mean age, 12.3 years), who presented with new-onset acral inflammatory lesions in their hands and feet at La Fe University Hospital, in Valencia, during the country’s peak quarantine period in April. Investigators conducted blood tests and reverse transcriptase–PCR (RT-PCR) for SARS-CoV-2, and six patients had skin biopsies.
Juncal Roca-Ginés, MD, of the department of dermatology, at the Hospital Universitario y Politécnico in La Fe, and coauthors, identified acral erythema in 6 (30%) of the cases, dactylitis in 4 (20%), purpuric maculopapules in 7 (35%), and a mixed pattern in 3 (15%). Serologic and viral testing yielded no positive results for SARS-CoV-2 or other viruses, and none of the patients exhibited COVID-19 symptoms such as fever, dry cough, sore throat, myalgia, or taste or smell disorders. In other findings, 45% of the patients had a history of vascular reactive disease of the hands, and 75% reported walking barefoot in their homes while staying at home. Only two patients reported taking medications.
In the six patients who had a biopsy, the findings were characteristic of chillblains, “confirming the clinical impression,” the authors wrote. Concluding that they could not show a relationship between acute acral skin changes and COVID-19, they noted that “other studies with improved microbiologic tests or molecular techniques aimed at demonstrating the presence of SARS-CoV-2 in the skin may help to clarify this problem.”
The other case series, which was also published in JAMA Dermatology and included 31 adults at a hospital in Brussels, who had recently developed chillblains, also looked for a connection between SARS-CoV-2 and chilblains, in April. Most of the participants were in their teens or 20s. Lesions had appeared on hands, feet, or on both extremities within 1-30 days of consultation, presenting as erythematous or purplish erythematous macules, occasionally with central vesicular or bullous lesions or necrotic areas. Patients reported pain, burning, and itching.
Skin biopsies were obtained in 22 patients and confirmed the diagnosis of chilblains; of the 15 with immunofluorescence analyses, 7 patients were found to have vasculitis of small-diameter vessels.
Of the 31 patients, 20 (64%) reported mild symptoms consistent with SARS-CoV-2, yet none of the RT-PCR or serologic test results showed signs of the virus in all 31 patients. “Because some patients had experienced chilblains for more than 15 days [under 30 days or less] at the time of inclusion, we can reasonably exclude the possibility that serologic testing was done too soon,” observed the authors. They also didn’t find eosinopenia, lymphopenia, and hyperferritinemia, which have been associated with COVID-19, they added.
Changes in lifestyle conditions during the pandemic may explain the appearance of these lesions, according to the authors of both studies, who mentioned that walking around in socks or bare feet and reduced physical activity could have indirectly led to the development of skin lesions.
It’s also possible that young people have less severe disease and a delayed reaction to the virus, Ignacio Torres-Navarro, MD, a dermatologist with La Fe University and the Spanish study’s corresponding author, said in an interview. Their feet may lack maturity in neurovascular regulation and/or the eccrine glands, which can happen in other diseases such as neutrophilic idiopathic eccrine hidradenitis. “In this context, perhaps there was an observational bias of the parents to the children when this manifestation was reported in the media. However, nothing has been demonstrated,” he said.
In an accompanying editor’s note, Claudia Hernandez, MD, of the departments of dermatology and pediatrics, Rush University Medical Center, Chicago, and Anna L. Bruckner, MD, of the departments of dermatology and pediatrics at the University of Colorado, Aurora, wrote that “it is still unclear whether a viral cytopathic process vs a viral reaction pattern or other mechanism is responsible for ‘COVID toes.’ ” Lack of confirmatory testing and reliance on indirect evidence of infection complicates this further, they noted, adding that “dermatologists must be aware of the protean cutaneous findings that are possibly associated with COVID-19, even if our understanding of their origins remains incomplete.”
In an interview, Dr. Fox, a member of the AAD’s’s COVID-19 Registry task force, offered other possible reasons for the negative antibody tests in the studies. The assay might not have been testing the correct antigen, or the timing of the test might not have been optimal. “More studies will help this become less controversial,” she said.
The authors of the two case series acknowledged potential limitations of their studies. Neither was large in scope: Both took place over a week’s time and included small cohorts. The Belgian study had no control group or long-term follow-up. Little is still known about the clinical manifestations and detection methods for SARS-CoV-2, noted the authors of the Spanish study.
The Spanish study received funding La Fe University Hospital’s department of dermatology, and the authors had no disclosures. The Belgian study received support from the Fondation Saint-Luc, which provided academic funding for its lead author, Marie Baeck, MD, PhD. Another author of this study received personal fees from the Fondation Saint-Luc and personal fees and nonfinancial support from Bioderma. The authors of the editor’s note had no disclosures.
SOURCES: Roca-Ginés J et al. JAMA Dermatol. 2020 Jun 25. doi: 10.1001/jamadermatol.2020.2340; Herman A et al. JAMA Dermatol. 2020 Jun 25. doi: 10.1001/jamadermatol.2020.2368.
such as lockdown conditions, which may be clarified with additional research.
Lindy P. Fox, MD, professor of dermatology at the University of California, San Francisco, who was not an author of either study, urged caution in interpreting these results. Data from the American Academy of Dermatology and a recent paper from the British Journal of Dermatology suggest a real association exists, at in least some patients. “It’s going to be true that most patients with toe lesions are PCR [polymerase chain reaction]-negative because it tends to be a late phenomenon when patients are no longer shedding virus,” Dr. Fox said in an interview.
Reports about chickenpox-like vesicles, urticaria, and other skin lesions in SARS-CoV-2 patients have circulated in the clinical literature and the media. Acute acro-ischemia has been cited as a potential sign of infection in adolescents and children.
One of the European studies, which was published in JAMA Dermatology, explored this association in 20 patients aged 1-18 years (mean age, 12.3 years), who presented with new-onset acral inflammatory lesions in their hands and feet at La Fe University Hospital, in Valencia, during the country’s peak quarantine period in April. Investigators conducted blood tests and reverse transcriptase–PCR (RT-PCR) for SARS-CoV-2, and six patients had skin biopsies.
Juncal Roca-Ginés, MD, of the department of dermatology, at the Hospital Universitario y Politécnico in La Fe, and coauthors, identified acral erythema in 6 (30%) of the cases, dactylitis in 4 (20%), purpuric maculopapules in 7 (35%), and a mixed pattern in 3 (15%). Serologic and viral testing yielded no positive results for SARS-CoV-2 or other viruses, and none of the patients exhibited COVID-19 symptoms such as fever, dry cough, sore throat, myalgia, or taste or smell disorders. In other findings, 45% of the patients had a history of vascular reactive disease of the hands, and 75% reported walking barefoot in their homes while staying at home. Only two patients reported taking medications.
In the six patients who had a biopsy, the findings were characteristic of chillblains, “confirming the clinical impression,” the authors wrote. Concluding that they could not show a relationship between acute acral skin changes and COVID-19, they noted that “other studies with improved microbiologic tests or molecular techniques aimed at demonstrating the presence of SARS-CoV-2 in the skin may help to clarify this problem.”
The other case series, which was also published in JAMA Dermatology and included 31 adults at a hospital in Brussels, who had recently developed chillblains, also looked for a connection between SARS-CoV-2 and chilblains, in April. Most of the participants were in their teens or 20s. Lesions had appeared on hands, feet, or on both extremities within 1-30 days of consultation, presenting as erythematous or purplish erythematous macules, occasionally with central vesicular or bullous lesions or necrotic areas. Patients reported pain, burning, and itching.
Skin biopsies were obtained in 22 patients and confirmed the diagnosis of chilblains; of the 15 with immunofluorescence analyses, 7 patients were found to have vasculitis of small-diameter vessels.
Of the 31 patients, 20 (64%) reported mild symptoms consistent with SARS-CoV-2, yet none of the RT-PCR or serologic test results showed signs of the virus in all 31 patients. “Because some patients had experienced chilblains for more than 15 days [under 30 days or less] at the time of inclusion, we can reasonably exclude the possibility that serologic testing was done too soon,” observed the authors. They also didn’t find eosinopenia, lymphopenia, and hyperferritinemia, which have been associated with COVID-19, they added.
Changes in lifestyle conditions during the pandemic may explain the appearance of these lesions, according to the authors of both studies, who mentioned that walking around in socks or bare feet and reduced physical activity could have indirectly led to the development of skin lesions.
It’s also possible that young people have less severe disease and a delayed reaction to the virus, Ignacio Torres-Navarro, MD, a dermatologist with La Fe University and the Spanish study’s corresponding author, said in an interview. Their feet may lack maturity in neurovascular regulation and/or the eccrine glands, which can happen in other diseases such as neutrophilic idiopathic eccrine hidradenitis. “In this context, perhaps there was an observational bias of the parents to the children when this manifestation was reported in the media. However, nothing has been demonstrated,” he said.
In an accompanying editor’s note, Claudia Hernandez, MD, of the departments of dermatology and pediatrics, Rush University Medical Center, Chicago, and Anna L. Bruckner, MD, of the departments of dermatology and pediatrics at the University of Colorado, Aurora, wrote that “it is still unclear whether a viral cytopathic process vs a viral reaction pattern or other mechanism is responsible for ‘COVID toes.’ ” Lack of confirmatory testing and reliance on indirect evidence of infection complicates this further, they noted, adding that “dermatologists must be aware of the protean cutaneous findings that are possibly associated with COVID-19, even if our understanding of their origins remains incomplete.”
In an interview, Dr. Fox, a member of the AAD’s’s COVID-19 Registry task force, offered other possible reasons for the negative antibody tests in the studies. The assay might not have been testing the correct antigen, or the timing of the test might not have been optimal. “More studies will help this become less controversial,” she said.
The authors of the two case series acknowledged potential limitations of their studies. Neither was large in scope: Both took place over a week’s time and included small cohorts. The Belgian study had no control group or long-term follow-up. Little is still known about the clinical manifestations and detection methods for SARS-CoV-2, noted the authors of the Spanish study.
The Spanish study received funding La Fe University Hospital’s department of dermatology, and the authors had no disclosures. The Belgian study received support from the Fondation Saint-Luc, which provided academic funding for its lead author, Marie Baeck, MD, PhD. Another author of this study received personal fees from the Fondation Saint-Luc and personal fees and nonfinancial support from Bioderma. The authors of the editor’s note had no disclosures.
SOURCES: Roca-Ginés J et al. JAMA Dermatol. 2020 Jun 25. doi: 10.1001/jamadermatol.2020.2340; Herman A et al. JAMA Dermatol. 2020 Jun 25. doi: 10.1001/jamadermatol.2020.2368.
For COVID-19 plus diabetes, glycemic control tops treatment list
Optimizing glycemic control “is the key to overall treatment in people with diabetes and COVID-19,” said Antonio Ceriello, MD, during a June 5 webinar sponsored by Harvard Medical School, Boston.
Dr. Ceriello, a research consultant with the Italian Ministry of Health, IRCCS Multi-Medica, Milan, highlighted a recent study that examined the association of blood glucose control and outcomes in COVID-19 patients with preexisting type 2 diabetes.
Among 7,000 cases of COVID-19, type 2 diabetes correlated with a higher death rate. However, those with well-controlled blood glucose (upper limit ≤10 mmol/L) had a survival rate of 98.9%, compared with just 11% among those with poorly controlled blood glucose (upper limit >10 mmol/L), a reduction in risk of 86% (adjusted hazard ratio, 0.14; Cell Metab. 2020 May 1. doi: 10.1016/j.cmet.2020.04.021).
Clinicians should also consider the possible side effects of hypoglycemic agents in the evolution of this disease. This is true of all patients, not just diabetes patients, Dr. Ceriello said. “We have data showing that ... hyperglycemia contributes directly to worsening the prognosis of COVID-19 independent of the presence of diabetes.”
One study found that the glycosylation of ACE-2 played an important role in allowing cellular entry of the virus (Am J Physiol Endocrinol Metab. 2020 Mar 31;318:E736-41). “This is something that could be related to hyperglycemia,” he added.
Another risk factor is thrombosis, a clear contributor to death rates in COVID-19. Research on thrombosis incidence in COVID-19 patients with diabetes reported higher levels of D-dimer levels in people with diabetes, especially among those who couldn’t manage their disease.
Tying all of these factors together, Dr. Ceriello discussed how ACE-2 glycosylation, in combination with other factors in SARS-CoV-2 infection, could lead to hyperglycemia, thrombosis, and subsequently multiorgan damage in diabetes patients.
Other research has associated higher HbA1c levels (mean HbA1c, 7.5%) with higher mortality risk in COVID-19 patients, said another speaker, Linong Ji, MD, director for endocrinology and metabolism at Peking University People’s Hospital, Beijing, and director of Peking University’s Diabetes Center. Proper guidance is key to ensuring early detection of hyperglycemic crisis in people with diabetes, advised Dr. Ji.
Global management of diabetes in SARS-CoV-2 patients is “quite challenging,” given that most patients don’t have their diabetes under control, said host and moderator A. Enrique Caballero, MD, an endocrinologist/investigator in the division of endocrinology, diabetes, and hypertension and division of global health equity at Brigham and Women’s Hospital, Boston. “They are not meeting treatment targets for cholesterol or glucose control. So we’re not managing optimal care. And now on top of this, we have COVID-19.”
Optimizing glycemic control “is the key to overall treatment in people with diabetes and COVID-19,” said Antonio Ceriello, MD, during a June 5 webinar sponsored by Harvard Medical School, Boston.
Dr. Ceriello, a research consultant with the Italian Ministry of Health, IRCCS Multi-Medica, Milan, highlighted a recent study that examined the association of blood glucose control and outcomes in COVID-19 patients with preexisting type 2 diabetes.
Among 7,000 cases of COVID-19, type 2 diabetes correlated with a higher death rate. However, those with well-controlled blood glucose (upper limit ≤10 mmol/L) had a survival rate of 98.9%, compared with just 11% among those with poorly controlled blood glucose (upper limit >10 mmol/L), a reduction in risk of 86% (adjusted hazard ratio, 0.14; Cell Metab. 2020 May 1. doi: 10.1016/j.cmet.2020.04.021).
Clinicians should also consider the possible side effects of hypoglycemic agents in the evolution of this disease. This is true of all patients, not just diabetes patients, Dr. Ceriello said. “We have data showing that ... hyperglycemia contributes directly to worsening the prognosis of COVID-19 independent of the presence of diabetes.”
One study found that the glycosylation of ACE-2 played an important role in allowing cellular entry of the virus (Am J Physiol Endocrinol Metab. 2020 Mar 31;318:E736-41). “This is something that could be related to hyperglycemia,” he added.
Another risk factor is thrombosis, a clear contributor to death rates in COVID-19. Research on thrombosis incidence in COVID-19 patients with diabetes reported higher levels of D-dimer levels in people with diabetes, especially among those who couldn’t manage their disease.
Tying all of these factors together, Dr. Ceriello discussed how ACE-2 glycosylation, in combination with other factors in SARS-CoV-2 infection, could lead to hyperglycemia, thrombosis, and subsequently multiorgan damage in diabetes patients.
Other research has associated higher HbA1c levels (mean HbA1c, 7.5%) with higher mortality risk in COVID-19 patients, said another speaker, Linong Ji, MD, director for endocrinology and metabolism at Peking University People’s Hospital, Beijing, and director of Peking University’s Diabetes Center. Proper guidance is key to ensuring early detection of hyperglycemic crisis in people with diabetes, advised Dr. Ji.
Global management of diabetes in SARS-CoV-2 patients is “quite challenging,” given that most patients don’t have their diabetes under control, said host and moderator A. Enrique Caballero, MD, an endocrinologist/investigator in the division of endocrinology, diabetes, and hypertension and division of global health equity at Brigham and Women’s Hospital, Boston. “They are not meeting treatment targets for cholesterol or glucose control. So we’re not managing optimal care. And now on top of this, we have COVID-19.”
Optimizing glycemic control “is the key to overall treatment in people with diabetes and COVID-19,” said Antonio Ceriello, MD, during a June 5 webinar sponsored by Harvard Medical School, Boston.
Dr. Ceriello, a research consultant with the Italian Ministry of Health, IRCCS Multi-Medica, Milan, highlighted a recent study that examined the association of blood glucose control and outcomes in COVID-19 patients with preexisting type 2 diabetes.
Among 7,000 cases of COVID-19, type 2 diabetes correlated with a higher death rate. However, those with well-controlled blood glucose (upper limit ≤10 mmol/L) had a survival rate of 98.9%, compared with just 11% among those with poorly controlled blood glucose (upper limit >10 mmol/L), a reduction in risk of 86% (adjusted hazard ratio, 0.14; Cell Metab. 2020 May 1. doi: 10.1016/j.cmet.2020.04.021).
Clinicians should also consider the possible side effects of hypoglycemic agents in the evolution of this disease. This is true of all patients, not just diabetes patients, Dr. Ceriello said. “We have data showing that ... hyperglycemia contributes directly to worsening the prognosis of COVID-19 independent of the presence of diabetes.”
One study found that the glycosylation of ACE-2 played an important role in allowing cellular entry of the virus (Am J Physiol Endocrinol Metab. 2020 Mar 31;318:E736-41). “This is something that could be related to hyperglycemia,” he added.
Another risk factor is thrombosis, a clear contributor to death rates in COVID-19. Research on thrombosis incidence in COVID-19 patients with diabetes reported higher levels of D-dimer levels in people with diabetes, especially among those who couldn’t manage their disease.
Tying all of these factors together, Dr. Ceriello discussed how ACE-2 glycosylation, in combination with other factors in SARS-CoV-2 infection, could lead to hyperglycemia, thrombosis, and subsequently multiorgan damage in diabetes patients.
Other research has associated higher HbA1c levels (mean HbA1c, 7.5%) with higher mortality risk in COVID-19 patients, said another speaker, Linong Ji, MD, director for endocrinology and metabolism at Peking University People’s Hospital, Beijing, and director of Peking University’s Diabetes Center. Proper guidance is key to ensuring early detection of hyperglycemic crisis in people with diabetes, advised Dr. Ji.
Global management of diabetes in SARS-CoV-2 patients is “quite challenging,” given that most patients don’t have their diabetes under control, said host and moderator A. Enrique Caballero, MD, an endocrinologist/investigator in the division of endocrinology, diabetes, and hypertension and division of global health equity at Brigham and Women’s Hospital, Boston. “They are not meeting treatment targets for cholesterol or glucose control. So we’re not managing optimal care. And now on top of this, we have COVID-19.”
Disparate study results on elective labor costs fuel debate
Cost concerns have circulated regarding elective induction of labor, a method that’s become increasingly popular in the United States. Two studies in Obstetrics & Gynecology, however, offer no consensus on the cost burden of this method.
A retrospective analysis of a large cohort in California reported higher costs for induction, compared with spontaneous labor, after accounting for variables such as parity, mode of delivery, and gestational age. A prospective study of five Utah hospitals found no significant cost differences between induction and expectant management.
The ARRIVE trial (A Randomized Trial of Induction versus Expectant Management), a multicenter study that compared elective labor induction at 39 weeks of gestation with spontaneous labor in low-risk nulliparous women, suggests that induction may have some benefits. While its researchers found no differences in perinatal outcomes, induction cases had fewer cesareans, fewer hypertensive disorders, and fewer newborns requiring respiratory support.
One key question that remains following ARRIVE is whether this practice should be implemented universally, Alyssa R. Hersh, MD, MPH, lead author of the California study, said in an interview. Quantifying the costs associated with elective labor is important because “health care in the United States is already much more expensive than in other countries, and [elective labor] could have a dramatic impact on annual health care costs.”
In a retrospective analysis, Dr. Hersh, of the Oregon Health & Science University, Portland, and her colleagues examined data from more than 1.2 million women in California with singleton, nonanomalous births. They excluded for multiple factors such as medically indicated induction of labor, placenta previa, breech presentation, or planned cesarean delivery.
Estimating cost differences between elective induction and spontaneous labor for mothers and neonates, they stratified results by vaginal or cesarean delivery, parity, gestational age at delivery, and geographic location. Elective induced labor represented 15% of the overall cohort of 1.2 million women.
Among vaginal deliveries, median maternal hospitalization costs were $10,175 in the induction group and $9,462 in the spontaneous labor group. For cesarean deliveries, the median costs were $20,294 with induction of labor and $18,812 with spontaneous labor.
Costs of maternal hospitalization with elective induction of labor were significantly higher than that of spontaneous labor, regardless of parity, mode of delivery, and gestational age at delivery, the authors reported. Comparing costs at rural and urban areas, the induction group saw higher maternal hospitalization costs and longer lengths of stay regardless of scenario.
Neonatal care was the one metric that incurred lower costs and lengths of stay in the induction group. Fewer adverse outcomes in this group could explain this outlier. “However, because this is observational data, we cannot elucidate what exactly contributed to these decreased costs,” Dr. Hersh and colleagues noted.
Timeliness was another limitation. “It is important to note that our study was conducted between 2007 and 2011, and the patients undergoing elective induction of labor during those years may differ from women undergoing elective induction of labor currently,” the authors acknowledged.
Another study by Brett D. Einerson, MD, MPH, of the University of Utah Health, Salt Lake City, and associates evaluated the actual hospital costs of patients undergoing elective induction and expectant management in a subset of patients from the ARRIVE trial.
“If, medically speaking, induction is equal to expectant management or has some benefit, as the larger ARRIVE trial suggests, we wanted to know: At what cost?” Dr. Einerson said in an interview.
Study participants hailed from five Utah hospitals within two health systems: the University of Utah Health and Intermountain Healthcare. Taking available data for 1,231 enrollees, investigators randomized 608 to labor induction and 623 to spontaneous labor. They measured actual hospital costs using advanced value-based analytics platforms at the Utah hospitals, comparing cost means and reporting the relative difference between induction and expectant management.
Overall, they found no significant differences between the mean total cost of elective induction and expectant management (adjusted mean difference, +4.7%). This was the case for other metrics: Costs did not vary among the five health systems or in most phases of care, including maternal inpatient postpartum care, maternal outpatient care after discharge, neonatal hospital care, and neonatal care after discharge.
The induction group did incur higher maternal inpatient intrapartum and delivery care costs (17%). However, these were offset by savings achieved during outpatient antenatal care (–47%). The assumption was additional costs of time spent on the labor ward might overwhelm cost savings elsewhere (reduced cesarean deliveries, fewer prenatal appointments and tests). “But this was not the case,” Dr. Einerson said.
Ultimately, the study was not large enough to find smaller differences in cost, he noted. It was only large enough to say that cost didn’t differentiate between arms with a margin of +/–7%. “A cost increase (or cost savings) with induction of 7% is meaningful over time and on a national scale,” Dr. Einerson explained.
Taken together, the two studies show that cost is not an insurmountable barrier to elective induced labor, Jeffrey L. Ecker, MD, and Mark A. Clapp, MD, MPH, wrote in an accompanying editorial (Obstet Gynecol. 2020;136[1]:6-7).
“This will be especially true if we are innovative and creatively adapt our facilities and spaces, thinking about where and how some of the required care can be appropriately and more economically offered,” they noted.
“Specifically, strategies to safely reduce labor and delivery time for inductions of labor, including considering and studying outpatient cervical ripening, may make elective induction of labor at 39 weeks of gestation even less costly and even more feasible to offer to all women,” suggested Dr. Ecker and Dr. Clapp, both at Massachusetts General Hospital and Harvard Medical School, both in Boston.
Dr. Hersh and coauthors had no relevant financial disclosures, and there was no external funding for their study. Dr. Einerson and most coauthors reported no relevant financial disclosures; one coauthor reported receiving funds from GestVision as a consultant, and another coauthor reported funds paid to her or her institution from some pharmaceutical companies when she was primary investigator on various trials or a consultant. This study was supported by grants from the Eunice Kennedy Shriver National Institute of Child Health and Human Development. Neither Dr. Ecker nor Dr Clapp had any relevant financial disclosures or received any funding.
SOURCES: Hersh AR et al. Obstet Gynecol. 2020. doi: 10.1097/AOG.0000000000003865; Einerson BD et al. Obstet Gynecol. 2020. doi: 10.1097/AOG.0000000000003930.
Cost concerns have circulated regarding elective induction of labor, a method that’s become increasingly popular in the United States. Two studies in Obstetrics & Gynecology, however, offer no consensus on the cost burden of this method.
A retrospective analysis of a large cohort in California reported higher costs for induction, compared with spontaneous labor, after accounting for variables such as parity, mode of delivery, and gestational age. A prospective study of five Utah hospitals found no significant cost differences between induction and expectant management.
The ARRIVE trial (A Randomized Trial of Induction versus Expectant Management), a multicenter study that compared elective labor induction at 39 weeks of gestation with spontaneous labor in low-risk nulliparous women, suggests that induction may have some benefits. While its researchers found no differences in perinatal outcomes, induction cases had fewer cesareans, fewer hypertensive disorders, and fewer newborns requiring respiratory support.
One key question that remains following ARRIVE is whether this practice should be implemented universally, Alyssa R. Hersh, MD, MPH, lead author of the California study, said in an interview. Quantifying the costs associated with elective labor is important because “health care in the United States is already much more expensive than in other countries, and [elective labor] could have a dramatic impact on annual health care costs.”
In a retrospective analysis, Dr. Hersh, of the Oregon Health & Science University, Portland, and her colleagues examined data from more than 1.2 million women in California with singleton, nonanomalous births. They excluded for multiple factors such as medically indicated induction of labor, placenta previa, breech presentation, or planned cesarean delivery.
Estimating cost differences between elective induction and spontaneous labor for mothers and neonates, they stratified results by vaginal or cesarean delivery, parity, gestational age at delivery, and geographic location. Elective induced labor represented 15% of the overall cohort of 1.2 million women.
Among vaginal deliveries, median maternal hospitalization costs were $10,175 in the induction group and $9,462 in the spontaneous labor group. For cesarean deliveries, the median costs were $20,294 with induction of labor and $18,812 with spontaneous labor.
Costs of maternal hospitalization with elective induction of labor were significantly higher than that of spontaneous labor, regardless of parity, mode of delivery, and gestational age at delivery, the authors reported. Comparing costs at rural and urban areas, the induction group saw higher maternal hospitalization costs and longer lengths of stay regardless of scenario.
Neonatal care was the one metric that incurred lower costs and lengths of stay in the induction group. Fewer adverse outcomes in this group could explain this outlier. “However, because this is observational data, we cannot elucidate what exactly contributed to these decreased costs,” Dr. Hersh and colleagues noted.
Timeliness was another limitation. “It is important to note that our study was conducted between 2007 and 2011, and the patients undergoing elective induction of labor during those years may differ from women undergoing elective induction of labor currently,” the authors acknowledged.
Another study by Brett D. Einerson, MD, MPH, of the University of Utah Health, Salt Lake City, and associates evaluated the actual hospital costs of patients undergoing elective induction and expectant management in a subset of patients from the ARRIVE trial.
“If, medically speaking, induction is equal to expectant management or has some benefit, as the larger ARRIVE trial suggests, we wanted to know: At what cost?” Dr. Einerson said in an interview.
Study participants hailed from five Utah hospitals within two health systems: the University of Utah Health and Intermountain Healthcare. Taking available data for 1,231 enrollees, investigators randomized 608 to labor induction and 623 to spontaneous labor. They measured actual hospital costs using advanced value-based analytics platforms at the Utah hospitals, comparing cost means and reporting the relative difference between induction and expectant management.
Overall, they found no significant differences between the mean total cost of elective induction and expectant management (adjusted mean difference, +4.7%). This was the case for other metrics: Costs did not vary among the five health systems or in most phases of care, including maternal inpatient postpartum care, maternal outpatient care after discharge, neonatal hospital care, and neonatal care after discharge.
The induction group did incur higher maternal inpatient intrapartum and delivery care costs (17%). However, these were offset by savings achieved during outpatient antenatal care (–47%). The assumption was additional costs of time spent on the labor ward might overwhelm cost savings elsewhere (reduced cesarean deliveries, fewer prenatal appointments and tests). “But this was not the case,” Dr. Einerson said.
Ultimately, the study was not large enough to find smaller differences in cost, he noted. It was only large enough to say that cost didn’t differentiate between arms with a margin of +/–7%. “A cost increase (or cost savings) with induction of 7% is meaningful over time and on a national scale,” Dr. Einerson explained.
Taken together, the two studies show that cost is not an insurmountable barrier to elective induced labor, Jeffrey L. Ecker, MD, and Mark A. Clapp, MD, MPH, wrote in an accompanying editorial (Obstet Gynecol. 2020;136[1]:6-7).
“This will be especially true if we are innovative and creatively adapt our facilities and spaces, thinking about where and how some of the required care can be appropriately and more economically offered,” they noted.
“Specifically, strategies to safely reduce labor and delivery time for inductions of labor, including considering and studying outpatient cervical ripening, may make elective induction of labor at 39 weeks of gestation even less costly and even more feasible to offer to all women,” suggested Dr. Ecker and Dr. Clapp, both at Massachusetts General Hospital and Harvard Medical School, both in Boston.
Dr. Hersh and coauthors had no relevant financial disclosures, and there was no external funding for their study. Dr. Einerson and most coauthors reported no relevant financial disclosures; one coauthor reported receiving funds from GestVision as a consultant, and another coauthor reported funds paid to her or her institution from some pharmaceutical companies when she was primary investigator on various trials or a consultant. This study was supported by grants from the Eunice Kennedy Shriver National Institute of Child Health and Human Development. Neither Dr. Ecker nor Dr Clapp had any relevant financial disclosures or received any funding.
SOURCES: Hersh AR et al. Obstet Gynecol. 2020. doi: 10.1097/AOG.0000000000003865; Einerson BD et al. Obstet Gynecol. 2020. doi: 10.1097/AOG.0000000000003930.
Cost concerns have circulated regarding elective induction of labor, a method that’s become increasingly popular in the United States. Two studies in Obstetrics & Gynecology, however, offer no consensus on the cost burden of this method.
A retrospective analysis of a large cohort in California reported higher costs for induction, compared with spontaneous labor, after accounting for variables such as parity, mode of delivery, and gestational age. A prospective study of five Utah hospitals found no significant cost differences between induction and expectant management.
The ARRIVE trial (A Randomized Trial of Induction versus Expectant Management), a multicenter study that compared elective labor induction at 39 weeks of gestation with spontaneous labor in low-risk nulliparous women, suggests that induction may have some benefits. While its researchers found no differences in perinatal outcomes, induction cases had fewer cesareans, fewer hypertensive disorders, and fewer newborns requiring respiratory support.
One key question that remains following ARRIVE is whether this practice should be implemented universally, Alyssa R. Hersh, MD, MPH, lead author of the California study, said in an interview. Quantifying the costs associated with elective labor is important because “health care in the United States is already much more expensive than in other countries, and [elective labor] could have a dramatic impact on annual health care costs.”
In a retrospective analysis, Dr. Hersh, of the Oregon Health & Science University, Portland, and her colleagues examined data from more than 1.2 million women in California with singleton, nonanomalous births. They excluded for multiple factors such as medically indicated induction of labor, placenta previa, breech presentation, or planned cesarean delivery.
Estimating cost differences between elective induction and spontaneous labor for mothers and neonates, they stratified results by vaginal or cesarean delivery, parity, gestational age at delivery, and geographic location. Elective induced labor represented 15% of the overall cohort of 1.2 million women.
Among vaginal deliveries, median maternal hospitalization costs were $10,175 in the induction group and $9,462 in the spontaneous labor group. For cesarean deliveries, the median costs were $20,294 with induction of labor and $18,812 with spontaneous labor.
Costs of maternal hospitalization with elective induction of labor were significantly higher than that of spontaneous labor, regardless of parity, mode of delivery, and gestational age at delivery, the authors reported. Comparing costs at rural and urban areas, the induction group saw higher maternal hospitalization costs and longer lengths of stay regardless of scenario.
Neonatal care was the one metric that incurred lower costs and lengths of stay in the induction group. Fewer adverse outcomes in this group could explain this outlier. “However, because this is observational data, we cannot elucidate what exactly contributed to these decreased costs,” Dr. Hersh and colleagues noted.
Timeliness was another limitation. “It is important to note that our study was conducted between 2007 and 2011, and the patients undergoing elective induction of labor during those years may differ from women undergoing elective induction of labor currently,” the authors acknowledged.
Another study by Brett D. Einerson, MD, MPH, of the University of Utah Health, Salt Lake City, and associates evaluated the actual hospital costs of patients undergoing elective induction and expectant management in a subset of patients from the ARRIVE trial.
“If, medically speaking, induction is equal to expectant management or has some benefit, as the larger ARRIVE trial suggests, we wanted to know: At what cost?” Dr. Einerson said in an interview.
Study participants hailed from five Utah hospitals within two health systems: the University of Utah Health and Intermountain Healthcare. Taking available data for 1,231 enrollees, investigators randomized 608 to labor induction and 623 to spontaneous labor. They measured actual hospital costs using advanced value-based analytics platforms at the Utah hospitals, comparing cost means and reporting the relative difference between induction and expectant management.
Overall, they found no significant differences between the mean total cost of elective induction and expectant management (adjusted mean difference, +4.7%). This was the case for other metrics: Costs did not vary among the five health systems or in most phases of care, including maternal inpatient postpartum care, maternal outpatient care after discharge, neonatal hospital care, and neonatal care after discharge.
The induction group did incur higher maternal inpatient intrapartum and delivery care costs (17%). However, these were offset by savings achieved during outpatient antenatal care (–47%). The assumption was additional costs of time spent on the labor ward might overwhelm cost savings elsewhere (reduced cesarean deliveries, fewer prenatal appointments and tests). “But this was not the case,” Dr. Einerson said.
Ultimately, the study was not large enough to find smaller differences in cost, he noted. It was only large enough to say that cost didn’t differentiate between arms with a margin of +/–7%. “A cost increase (or cost savings) with induction of 7% is meaningful over time and on a national scale,” Dr. Einerson explained.
Taken together, the two studies show that cost is not an insurmountable barrier to elective induced labor, Jeffrey L. Ecker, MD, and Mark A. Clapp, MD, MPH, wrote in an accompanying editorial (Obstet Gynecol. 2020;136[1]:6-7).
“This will be especially true if we are innovative and creatively adapt our facilities and spaces, thinking about where and how some of the required care can be appropriately and more economically offered,” they noted.
“Specifically, strategies to safely reduce labor and delivery time for inductions of labor, including considering and studying outpatient cervical ripening, may make elective induction of labor at 39 weeks of gestation even less costly and even more feasible to offer to all women,” suggested Dr. Ecker and Dr. Clapp, both at Massachusetts General Hospital and Harvard Medical School, both in Boston.
Dr. Hersh and coauthors had no relevant financial disclosures, and there was no external funding for their study. Dr. Einerson and most coauthors reported no relevant financial disclosures; one coauthor reported receiving funds from GestVision as a consultant, and another coauthor reported funds paid to her or her institution from some pharmaceutical companies when she was primary investigator on various trials or a consultant. This study was supported by grants from the Eunice Kennedy Shriver National Institute of Child Health and Human Development. Neither Dr. Ecker nor Dr Clapp had any relevant financial disclosures or received any funding.
SOURCES: Hersh AR et al. Obstet Gynecol. 2020. doi: 10.1097/AOG.0000000000003865; Einerson BD et al. Obstet Gynecol. 2020. doi: 10.1097/AOG.0000000000003930.
Biologics yield low rates of skin clearance in real-world psoriasis study
The study was published in May in the Journal of the European Academy of Dermatology and Venereology.
High efficacy rates, which include PASI 100 scores, have been reported in randomized trials of biologics that include anti–interleukin (IL)–17A therapies (secukinumab and ixekizumab), anti–IL-17A–receptor therapies (brodalumab), and anti–IL-23 therapies (guselkumab and risankizumab), but information on rates in real-world cohorts has been limited. “Real-world evidence provided by registries is only beginning to emerge, and efficacy data have mostly been derived from clinical trials,” senior author Kristian Reich, MD, PhD, professor for translational research in inflammatory skin diseases at the Institute for Health Services Research in Dermatology and Nursing, University Medical Center Hamburg-Eppendorf (Germany), said in an interview.
He and his coinvestigators conducted the PSO-BIO-REAL (Plaque Psoriasis Treated With Biologics in a Real World Setting) prospective trial in five countries, to evaluate the effectiveness of treatments in patients with moderate to severe plaque psoriasis over a year’s time following administration of a biologic therapy. Patients were 18 years of age or older and had either started a biologic for the first time (biologic-naive) or were transitioning to another biologic (biologic-experienced).
Among 846 participants, 32% were in the United States, followed by France (28%), Italy (22%), the United Kingdom (11%), and Germany (8%). Investigators estimated the proportion of patients achieving a PASI 100 (complete skin clearance) 6 months after starting a biologic as a primary objective, and as secondary objectives, PASI 100 scores at 1 year and PASI 100 maintenance from 6 to 12 months.
Nearly 200 patients withdrew during the course of the study, and 108 switched treatments. Therapies varied among patients: 61% received an anti–tumor necrosis factor agent such as etanercept, infliximab, adalimumab, or certolizumab pegol as an initial biologic treatment, 30% received an anti–IL-12/-23 agent (ustekinumab), and 9% received an anti-IL-17 agent (secukinumab). Additionally, 23% received a concomitant psoriasis medication.
PASI assessments were completed in 603 patients at 6 months, and 522 patients at 12 months. At 6 and 12 months respectively, 23% and 26% of the patients had achieved a PASI 100 score. Investigators noted that the rate of complete skin clearance declined as the number of baseline comorbidities and the number of prior biologics increased.
Biologic-experienced patients at study entry had lower PASI 100 response rates (about 20% at 6 and 12 months) than the biologic-naive patients (25% at 6 months, 30% at 12 months). Dr. Reich pointed out that many biologic-experienced patients often have active disease, despite previous use of biologics, and “they’re likely to represent a more difficult-to-treat population.” Factors such as convenience, safety, and the fact that more complicated patients – those with weight issues, more comorbidities and pretreatments, and lower compliance – are treated in real life than in clinical trials, are likely to influence lack of response in real-world data, Dr. Reich said.
The study’s enrollment period took place from 2014 to 2015, so it did not include patients on newer biologics such as brodalumab, guselkumab, ixekizumab, and tildrakizumab. “Some of these newer therapies have shown greater efficacy than drugs such as ustekinumab and etanercept in clinical trials, and patients are more likely to achieve complete skin clearance. Therefore, real-world rates of complete clearance may have improved since this study concluded,” the investigators pointed out.
Possible limitations of the study include selection bias and possible confounders, they noted.
The study was sponsored by Amgen/AstraZeneca; the manuscript was sponsored by LEO Pharma. One author was an AstraZeneca employee, two are LEO pharma employees, one author had no disclosures, and the remaining authors, including Dr. Reich, disclosed serving as an adviser, paid speaker, consultant, and/or investigator for multiple pharmaceutical companies.
SOURCE: Seneschal J et al. J Eur Acad Dermatol Venereol. 2020 May 4. doi: 10.1111/jdv.16568.
The study was published in May in the Journal of the European Academy of Dermatology and Venereology.
High efficacy rates, which include PASI 100 scores, have been reported in randomized trials of biologics that include anti–interleukin (IL)–17A therapies (secukinumab and ixekizumab), anti–IL-17A–receptor therapies (brodalumab), and anti–IL-23 therapies (guselkumab and risankizumab), but information on rates in real-world cohorts has been limited. “Real-world evidence provided by registries is only beginning to emerge, and efficacy data have mostly been derived from clinical trials,” senior author Kristian Reich, MD, PhD, professor for translational research in inflammatory skin diseases at the Institute for Health Services Research in Dermatology and Nursing, University Medical Center Hamburg-Eppendorf (Germany), said in an interview.
He and his coinvestigators conducted the PSO-BIO-REAL (Plaque Psoriasis Treated With Biologics in a Real World Setting) prospective trial in five countries, to evaluate the effectiveness of treatments in patients with moderate to severe plaque psoriasis over a year’s time following administration of a biologic therapy. Patients were 18 years of age or older and had either started a biologic for the first time (biologic-naive) or were transitioning to another biologic (biologic-experienced).
Among 846 participants, 32% were in the United States, followed by France (28%), Italy (22%), the United Kingdom (11%), and Germany (8%). Investigators estimated the proportion of patients achieving a PASI 100 (complete skin clearance) 6 months after starting a biologic as a primary objective, and as secondary objectives, PASI 100 scores at 1 year and PASI 100 maintenance from 6 to 12 months.
Nearly 200 patients withdrew during the course of the study, and 108 switched treatments. Therapies varied among patients: 61% received an anti–tumor necrosis factor agent such as etanercept, infliximab, adalimumab, or certolizumab pegol as an initial biologic treatment, 30% received an anti–IL-12/-23 agent (ustekinumab), and 9% received an anti-IL-17 agent (secukinumab). Additionally, 23% received a concomitant psoriasis medication.
PASI assessments were completed in 603 patients at 6 months, and 522 patients at 12 months. At 6 and 12 months respectively, 23% and 26% of the patients had achieved a PASI 100 score. Investigators noted that the rate of complete skin clearance declined as the number of baseline comorbidities and the number of prior biologics increased.
Biologic-experienced patients at study entry had lower PASI 100 response rates (about 20% at 6 and 12 months) than the biologic-naive patients (25% at 6 months, 30% at 12 months). Dr. Reich pointed out that many biologic-experienced patients often have active disease, despite previous use of biologics, and “they’re likely to represent a more difficult-to-treat population.” Factors such as convenience, safety, and the fact that more complicated patients – those with weight issues, more comorbidities and pretreatments, and lower compliance – are treated in real life than in clinical trials, are likely to influence lack of response in real-world data, Dr. Reich said.
The study’s enrollment period took place from 2014 to 2015, so it did not include patients on newer biologics such as brodalumab, guselkumab, ixekizumab, and tildrakizumab. “Some of these newer therapies have shown greater efficacy than drugs such as ustekinumab and etanercept in clinical trials, and patients are more likely to achieve complete skin clearance. Therefore, real-world rates of complete clearance may have improved since this study concluded,” the investigators pointed out.
Possible limitations of the study include selection bias and possible confounders, they noted.
The study was sponsored by Amgen/AstraZeneca; the manuscript was sponsored by LEO Pharma. One author was an AstraZeneca employee, two are LEO pharma employees, one author had no disclosures, and the remaining authors, including Dr. Reich, disclosed serving as an adviser, paid speaker, consultant, and/or investigator for multiple pharmaceutical companies.
SOURCE: Seneschal J et al. J Eur Acad Dermatol Venereol. 2020 May 4. doi: 10.1111/jdv.16568.
The study was published in May in the Journal of the European Academy of Dermatology and Venereology.
High efficacy rates, which include PASI 100 scores, have been reported in randomized trials of biologics that include anti–interleukin (IL)–17A therapies (secukinumab and ixekizumab), anti–IL-17A–receptor therapies (brodalumab), and anti–IL-23 therapies (guselkumab and risankizumab), but information on rates in real-world cohorts has been limited. “Real-world evidence provided by registries is only beginning to emerge, and efficacy data have mostly been derived from clinical trials,” senior author Kristian Reich, MD, PhD, professor for translational research in inflammatory skin diseases at the Institute for Health Services Research in Dermatology and Nursing, University Medical Center Hamburg-Eppendorf (Germany), said in an interview.
He and his coinvestigators conducted the PSO-BIO-REAL (Plaque Psoriasis Treated With Biologics in a Real World Setting) prospective trial in five countries, to evaluate the effectiveness of treatments in patients with moderate to severe plaque psoriasis over a year’s time following administration of a biologic therapy. Patients were 18 years of age or older and had either started a biologic for the first time (biologic-naive) or were transitioning to another biologic (biologic-experienced).
Among 846 participants, 32% were in the United States, followed by France (28%), Italy (22%), the United Kingdom (11%), and Germany (8%). Investigators estimated the proportion of patients achieving a PASI 100 (complete skin clearance) 6 months after starting a biologic as a primary objective, and as secondary objectives, PASI 100 scores at 1 year and PASI 100 maintenance from 6 to 12 months.
Nearly 200 patients withdrew during the course of the study, and 108 switched treatments. Therapies varied among patients: 61% received an anti–tumor necrosis factor agent such as etanercept, infliximab, adalimumab, or certolizumab pegol as an initial biologic treatment, 30% received an anti–IL-12/-23 agent (ustekinumab), and 9% received an anti-IL-17 agent (secukinumab). Additionally, 23% received a concomitant psoriasis medication.
PASI assessments were completed in 603 patients at 6 months, and 522 patients at 12 months. At 6 and 12 months respectively, 23% and 26% of the patients had achieved a PASI 100 score. Investigators noted that the rate of complete skin clearance declined as the number of baseline comorbidities and the number of prior biologics increased.
Biologic-experienced patients at study entry had lower PASI 100 response rates (about 20% at 6 and 12 months) than the biologic-naive patients (25% at 6 months, 30% at 12 months). Dr. Reich pointed out that many biologic-experienced patients often have active disease, despite previous use of biologics, and “they’re likely to represent a more difficult-to-treat population.” Factors such as convenience, safety, and the fact that more complicated patients – those with weight issues, more comorbidities and pretreatments, and lower compliance – are treated in real life than in clinical trials, are likely to influence lack of response in real-world data, Dr. Reich said.
The study’s enrollment period took place from 2014 to 2015, so it did not include patients on newer biologics such as brodalumab, guselkumab, ixekizumab, and tildrakizumab. “Some of these newer therapies have shown greater efficacy than drugs such as ustekinumab and etanercept in clinical trials, and patients are more likely to achieve complete skin clearance. Therefore, real-world rates of complete clearance may have improved since this study concluded,” the investigators pointed out.
Possible limitations of the study include selection bias and possible confounders, they noted.
The study was sponsored by Amgen/AstraZeneca; the manuscript was sponsored by LEO Pharma. One author was an AstraZeneca employee, two are LEO pharma employees, one author had no disclosures, and the remaining authors, including Dr. Reich, disclosed serving as an adviser, paid speaker, consultant, and/or investigator for multiple pharmaceutical companies.
SOURCE: Seneschal J et al. J Eur Acad Dermatol Venereol. 2020 May 4. doi: 10.1111/jdv.16568.
FROM THE JOURNAL OF THE EUROPEAN ACADEMY OF DERMATOLOGY AND VENEREOLOGY
Most e-consults not followed by specialist visit
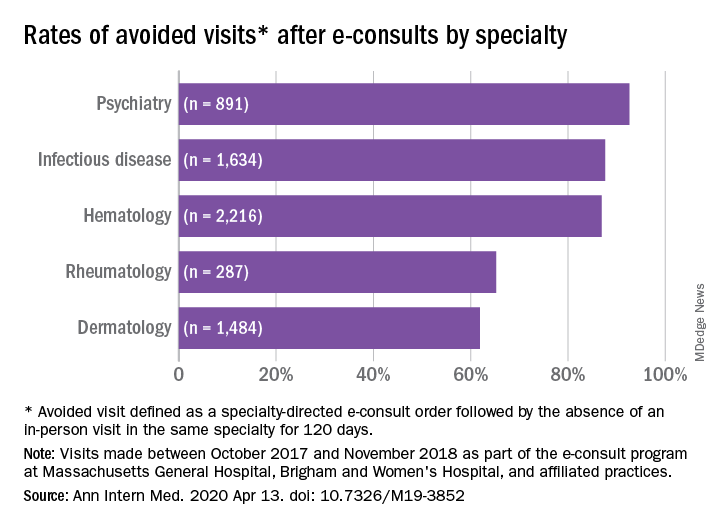
Studies have shown that e-consults increase access to specialist care and primary care physician (PCP) education, according to research published in the Annals of Internal Medicine (2020. Apr 14. doi: 10.7326/M19-3852) by Salman Ahmed, MD, and colleagues.
These resources are already being frequently used by physicians, but more often by general internists and hospitalists than by subspecialists, according to a recent survey by the American College of Physicians. That survey found that 42% of its respondents are using e-consults and that subspecialists’ use is less common primarily because of the lack of access to e-consult technology.
What hasn’t been widely researched are the effects of large-scale e-consult programs, said Dr. Ahmed, who is associate physician in the renal division at Brigham and Women’s Hospital, Boston, in an interview.
For frontline providers such as PCPs, e-consults are a way to quickly seek out answers to clinical questions from specialists. In turn, the specialist can help a wider pool of participants, he noted.
The findings of Dr. Ahmed’s study, which included several academic centers and hospitals affiliated with Partners HealthCare System, a nonprofit network in eastern Massachusetts that includes Brigham and Women’s Hospital, used several metrics to analyze the appropriateness and utility of e-consults across a range of specialties. An e-consult was considered useful if it resulted in the avoidance of a visit to a specialist, which was defined as the absence of an in-person visit to the type of specialist consulted electronically for 120 days. An e-consult was considered appropriate if it met the following four criteria.
- It could not be answered by referring to society guidelines or widely available, evidence-based summary sources.
- It did not seek logistic information, such as where to have a specific laboratory test done.
- It did not include a question of high urgency.
- The medical complexity of the clinical situation was not substantial enough to warrant an in-person consultation.
The investigators examined e-consult inquiries to mostly physician health care providers in five specialties – hematology, infectious disease, dermatology, rheumatology, and psychiatry – over a year.
High rates of appropriateness
The search spanned 6,512 eligible e-consults from 1,096 referring providers to 121 specialist consultants. Narrowing their search to 741 records with complete data, the investigators found that 70.2% of these consults met the criteria for appropriateness. In an analysis of four reviewers blinded to each other’s results, raters agreed on the appropriateness of 94% of e-consults.
Across specialties, more than 81% of e-consults were associated with avoided in-person visits.
The reasons for most e-consults were to seek answers to questions about diagnosis, therapeutics, or patient inquiries, or to request further education by PCPs.
“Across all specialties, the most common reasons an e-consult was not considered appropriate were failing the point-of-care resource test and asking a question of inappropriately high complexity,” the authors summarized.
Physicians and PCPs from tertiary care practices made up the majority of referring providers, with turnaround time for consults averaging 24 hours across specialties.
Rates of appropriateness, content, patient demographics, and timeliness of e-consult responses varied among the four specialties. Those with high avoidance of visits rates tended to have high appropriateness rates, indicating that some specialties may be more conducive to e-consults than others, the authors noted. Psychiatry and hematology had the highest proportion of appropriate e-consults (77.9% and 73.3% respectively). Rheumatology had the lowest proportion of appropriate e-consults and one of the lowest rates of avoided in-person visits, and dermatology had the lowest rate of avoided in-person visits, at 61.9%.
The majority (93%) of e-consults sought in psychiatry were therapy related, whereas 88.4% of the e-consult questions in rheumatology related to diagnosis.
“Questions about diagnosis were less likely to be answerable via e-consult, which suggests that to provide diagnoses, consultants may wish to engage with the patient directly,” Dr. Ahmed said in an interview.
Infectious disease specialists seemed to be the fastest responders, with nearly 90% of their consultations having been answered within a day. Dermatology specialists had the distinction of having the youngest e-consult patients (mean age, 38.6 years).
PCPs weigh in on results
Physicians said in interviews that the study data reflects their own positive experiences with e-consults.
“Although I don’t always think [an e-consult] is able to fully prevent the specialist visit, it does allow the specialist to provide recommendations for work-up that can be done prior to the specialist visit,” said Santina Wheat MD, a family physician at Erie Family Health Center in Chicago. This reduces the time in which the consult is placed to when effective treatment can take place.
Patients who may have to wait months or even years to see a specialty doctor, benefit from e-consults, said Dr. Wheat, who is also a member of the editorial advisory board of Family Practice News. “As part of an organization that does e-consults to another hospital with a different electronic medical record, the e-consult increases the likelihood that all of the clinical information reaches the specialists and prevents tests from being repeated.”
Starting an e-consult may also increase the likelihood that the patient quickly sees a specialist at the contracted hospital, she added.
Sarah G. Candler, MD, said in an interview that she also sees e-consults as an essential tool. “When patients present with rare, complex, or atypical pictures, I find it helpful to have specialists weigh in. The e-consult helps me ensure that I work to the top of my abilities as an internist,” said Dr. Candler, who is practice medical director and physician director of academic relations at Iora Primary Care, Northside Clinic, Houston. However, she did not agree with the study’s avoided in-person visits metric for assessing utility.
“In some cases, the end result of an e-consult is a referral for an in-person evaluation, and the role of the e-consult is to ensure that I have done my due diligence as a primary care doctor asking the correct questions, getting the appropriate work-up completed, and referring to the appropriate specialty for next steps, when necessary,” noted Dr. Candler, who also serves on the editorial advisory board of Internal Medicine News.
Financial considerations
The study’s authors suggested taking a closer look at standardizing payment for the use of e-consults and developing appropriateness criteria for them.
Health systems could use such criteria to study what makes an e-consult useful and how to best utilize this tool, Dr. Ahmed said in an interview.
“Compensation models that promote high-quality, effective, and efficient e-consults are needed to reinforce the ability of health systems to optimize the mix of e-consults and in-person visits,” Dr. Ahmed and colleagues suggested.
Because not all patient care requires e-consults, the model makes the most sense in practices that already participate in value-based payment programs. In these types of programs, the cost can be shared according to the variable risk and patient need for the service, Dr. Candler explained.
“I have been fortunate to work in two different systems that function in this way, which means that e-consults have been readily available and encouraged-both to improve patient care and decrease overall cost by decreasing unnecessary testing or specialist referral,” she said.
Dr. Wheat said that the managed care organization affiliated with her practice seems to be saving money with e-consults, as it decreases the need to pay for specialist visits in some instances and for repeated work-ups.
Future studies
The study’s cohort represented just one large health care system with a shared electronic health record. “Single-system descriptive studies, such as that of Ahmed and colleagues, are particularly useful for local evaluation and quality improvement efforts,” Varsha G. Vimalananda, MD, and B. Graeme Fincke, MD, both of the Center for Healthcare Organization and Implementation Research at Bedford (Mass.) Veterans Affairs Hospital, wrote in a related editorial.
“However, we need innovative approaches to evaluation that estimate the effect of e-consults on quality and cost of care across health care systems and over time. Implementation studies can help to identify key contributors to success,” the editorialists wrote.
One of the study authors, reported receiving personal fees from Bayer outside the submitted work. The other authors of the paper and the authors of the editorial reported no conflicts of interest. Dr. Candler said her employer contracts with an e-consult service, but that she is not compensated for use of the service. She is also a coeditor of Annals of Internal Medicine’s blog, “Fresh Look.”
SOURCE: Ahmed S et al. Ann Intern Med. 2020 Apr 14. doi: 10.7326/M19-3852.
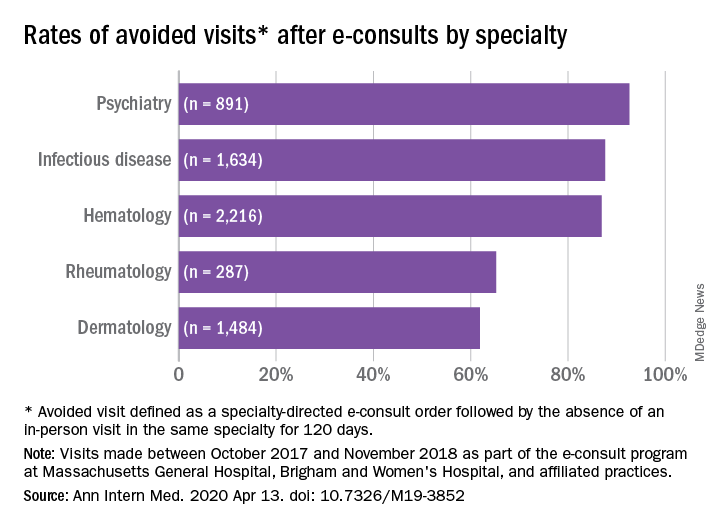
Studies have shown that e-consults increase access to specialist care and primary care physician (PCP) education, according to research published in the Annals of Internal Medicine (2020. Apr 14. doi: 10.7326/M19-3852) by Salman Ahmed, MD, and colleagues.
These resources are already being frequently used by physicians, but more often by general internists and hospitalists than by subspecialists, according to a recent survey by the American College of Physicians. That survey found that 42% of its respondents are using e-consults and that subspecialists’ use is less common primarily because of the lack of access to e-consult technology.
What hasn’t been widely researched are the effects of large-scale e-consult programs, said Dr. Ahmed, who is associate physician in the renal division at Brigham and Women’s Hospital, Boston, in an interview.
For frontline providers such as PCPs, e-consults are a way to quickly seek out answers to clinical questions from specialists. In turn, the specialist can help a wider pool of participants, he noted.
The findings of Dr. Ahmed’s study, which included several academic centers and hospitals affiliated with Partners HealthCare System, a nonprofit network in eastern Massachusetts that includes Brigham and Women’s Hospital, used several metrics to analyze the appropriateness and utility of e-consults across a range of specialties. An e-consult was considered useful if it resulted in the avoidance of a visit to a specialist, which was defined as the absence of an in-person visit to the type of specialist consulted electronically for 120 days. An e-consult was considered appropriate if it met the following four criteria.
- It could not be answered by referring to society guidelines or widely available, evidence-based summary sources.
- It did not seek logistic information, such as where to have a specific laboratory test done.
- It did not include a question of high urgency.
- The medical complexity of the clinical situation was not substantial enough to warrant an in-person consultation.
The investigators examined e-consult inquiries to mostly physician health care providers in five specialties – hematology, infectious disease, dermatology, rheumatology, and psychiatry – over a year.
High rates of appropriateness
The search spanned 6,512 eligible e-consults from 1,096 referring providers to 121 specialist consultants. Narrowing their search to 741 records with complete data, the investigators found that 70.2% of these consults met the criteria for appropriateness. In an analysis of four reviewers blinded to each other’s results, raters agreed on the appropriateness of 94% of e-consults.
Across specialties, more than 81% of e-consults were associated with avoided in-person visits.
The reasons for most e-consults were to seek answers to questions about diagnosis, therapeutics, or patient inquiries, or to request further education by PCPs.
“Across all specialties, the most common reasons an e-consult was not considered appropriate were failing the point-of-care resource test and asking a question of inappropriately high complexity,” the authors summarized.
Physicians and PCPs from tertiary care practices made up the majority of referring providers, with turnaround time for consults averaging 24 hours across specialties.
Rates of appropriateness, content, patient demographics, and timeliness of e-consult responses varied among the four specialties. Those with high avoidance of visits rates tended to have high appropriateness rates, indicating that some specialties may be more conducive to e-consults than others, the authors noted. Psychiatry and hematology had the highest proportion of appropriate e-consults (77.9% and 73.3% respectively). Rheumatology had the lowest proportion of appropriate e-consults and one of the lowest rates of avoided in-person visits, and dermatology had the lowest rate of avoided in-person visits, at 61.9%.
The majority (93%) of e-consults sought in psychiatry were therapy related, whereas 88.4% of the e-consult questions in rheumatology related to diagnosis.
“Questions about diagnosis were less likely to be answerable via e-consult, which suggests that to provide diagnoses, consultants may wish to engage with the patient directly,” Dr. Ahmed said in an interview.
Infectious disease specialists seemed to be the fastest responders, with nearly 90% of their consultations having been answered within a day. Dermatology specialists had the distinction of having the youngest e-consult patients (mean age, 38.6 years).
PCPs weigh in on results
Physicians said in interviews that the study data reflects their own positive experiences with e-consults.
“Although I don’t always think [an e-consult] is able to fully prevent the specialist visit, it does allow the specialist to provide recommendations for work-up that can be done prior to the specialist visit,” said Santina Wheat MD, a family physician at Erie Family Health Center in Chicago. This reduces the time in which the consult is placed to when effective treatment can take place.
Patients who may have to wait months or even years to see a specialty doctor, benefit from e-consults, said Dr. Wheat, who is also a member of the editorial advisory board of Family Practice News. “As part of an organization that does e-consults to another hospital with a different electronic medical record, the e-consult increases the likelihood that all of the clinical information reaches the specialists and prevents tests from being repeated.”
Starting an e-consult may also increase the likelihood that the patient quickly sees a specialist at the contracted hospital, she added.
Sarah G. Candler, MD, said in an interview that she also sees e-consults as an essential tool. “When patients present with rare, complex, or atypical pictures, I find it helpful to have specialists weigh in. The e-consult helps me ensure that I work to the top of my abilities as an internist,” said Dr. Candler, who is practice medical director and physician director of academic relations at Iora Primary Care, Northside Clinic, Houston. However, she did not agree with the study’s avoided in-person visits metric for assessing utility.
“In some cases, the end result of an e-consult is a referral for an in-person evaluation, and the role of the e-consult is to ensure that I have done my due diligence as a primary care doctor asking the correct questions, getting the appropriate work-up completed, and referring to the appropriate specialty for next steps, when necessary,” noted Dr. Candler, who also serves on the editorial advisory board of Internal Medicine News.
Financial considerations
The study’s authors suggested taking a closer look at standardizing payment for the use of e-consults and developing appropriateness criteria for them.
Health systems could use such criteria to study what makes an e-consult useful and how to best utilize this tool, Dr. Ahmed said in an interview.
“Compensation models that promote high-quality, effective, and efficient e-consults are needed to reinforce the ability of health systems to optimize the mix of e-consults and in-person visits,” Dr. Ahmed and colleagues suggested.
Because not all patient care requires e-consults, the model makes the most sense in practices that already participate in value-based payment programs. In these types of programs, the cost can be shared according to the variable risk and patient need for the service, Dr. Candler explained.
“I have been fortunate to work in two different systems that function in this way, which means that e-consults have been readily available and encouraged-both to improve patient care and decrease overall cost by decreasing unnecessary testing or specialist referral,” she said.
Dr. Wheat said that the managed care organization affiliated with her practice seems to be saving money with e-consults, as it decreases the need to pay for specialist visits in some instances and for repeated work-ups.
Future studies
The study’s cohort represented just one large health care system with a shared electronic health record. “Single-system descriptive studies, such as that of Ahmed and colleagues, are particularly useful for local evaluation and quality improvement efforts,” Varsha G. Vimalananda, MD, and B. Graeme Fincke, MD, both of the Center for Healthcare Organization and Implementation Research at Bedford (Mass.) Veterans Affairs Hospital, wrote in a related editorial.
“However, we need innovative approaches to evaluation that estimate the effect of e-consults on quality and cost of care across health care systems and over time. Implementation studies can help to identify key contributors to success,” the editorialists wrote.
One of the study authors, reported receiving personal fees from Bayer outside the submitted work. The other authors of the paper and the authors of the editorial reported no conflicts of interest. Dr. Candler said her employer contracts with an e-consult service, but that she is not compensated for use of the service. She is also a coeditor of Annals of Internal Medicine’s blog, “Fresh Look.”
SOURCE: Ahmed S et al. Ann Intern Med. 2020 Apr 14. doi: 10.7326/M19-3852.
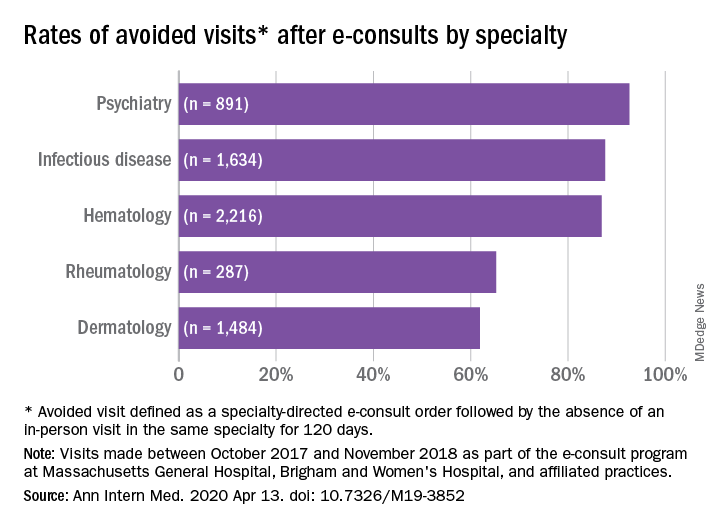
Studies have shown that e-consults increase access to specialist care and primary care physician (PCP) education, according to research published in the Annals of Internal Medicine (2020. Apr 14. doi: 10.7326/M19-3852) by Salman Ahmed, MD, and colleagues.
These resources are already being frequently used by physicians, but more often by general internists and hospitalists than by subspecialists, according to a recent survey by the American College of Physicians. That survey found that 42% of its respondents are using e-consults and that subspecialists’ use is less common primarily because of the lack of access to e-consult technology.
What hasn’t been widely researched are the effects of large-scale e-consult programs, said Dr. Ahmed, who is associate physician in the renal division at Brigham and Women’s Hospital, Boston, in an interview.
For frontline providers such as PCPs, e-consults are a way to quickly seek out answers to clinical questions from specialists. In turn, the specialist can help a wider pool of participants, he noted.
The findings of Dr. Ahmed’s study, which included several academic centers and hospitals affiliated with Partners HealthCare System, a nonprofit network in eastern Massachusetts that includes Brigham and Women’s Hospital, used several metrics to analyze the appropriateness and utility of e-consults across a range of specialties. An e-consult was considered useful if it resulted in the avoidance of a visit to a specialist, which was defined as the absence of an in-person visit to the type of specialist consulted electronically for 120 days. An e-consult was considered appropriate if it met the following four criteria.
- It could not be answered by referring to society guidelines or widely available, evidence-based summary sources.
- It did not seek logistic information, such as where to have a specific laboratory test done.
- It did not include a question of high urgency.
- The medical complexity of the clinical situation was not substantial enough to warrant an in-person consultation.
The investigators examined e-consult inquiries to mostly physician health care providers in five specialties – hematology, infectious disease, dermatology, rheumatology, and psychiatry – over a year.
High rates of appropriateness
The search spanned 6,512 eligible e-consults from 1,096 referring providers to 121 specialist consultants. Narrowing their search to 741 records with complete data, the investigators found that 70.2% of these consults met the criteria for appropriateness. In an analysis of four reviewers blinded to each other’s results, raters agreed on the appropriateness of 94% of e-consults.
Across specialties, more than 81% of e-consults were associated with avoided in-person visits.
The reasons for most e-consults were to seek answers to questions about diagnosis, therapeutics, or patient inquiries, or to request further education by PCPs.
“Across all specialties, the most common reasons an e-consult was not considered appropriate were failing the point-of-care resource test and asking a question of inappropriately high complexity,” the authors summarized.
Physicians and PCPs from tertiary care practices made up the majority of referring providers, with turnaround time for consults averaging 24 hours across specialties.
Rates of appropriateness, content, patient demographics, and timeliness of e-consult responses varied among the four specialties. Those with high avoidance of visits rates tended to have high appropriateness rates, indicating that some specialties may be more conducive to e-consults than others, the authors noted. Psychiatry and hematology had the highest proportion of appropriate e-consults (77.9% and 73.3% respectively). Rheumatology had the lowest proportion of appropriate e-consults and one of the lowest rates of avoided in-person visits, and dermatology had the lowest rate of avoided in-person visits, at 61.9%.
The majority (93%) of e-consults sought in psychiatry were therapy related, whereas 88.4% of the e-consult questions in rheumatology related to diagnosis.
“Questions about diagnosis were less likely to be answerable via e-consult, which suggests that to provide diagnoses, consultants may wish to engage with the patient directly,” Dr. Ahmed said in an interview.
Infectious disease specialists seemed to be the fastest responders, with nearly 90% of their consultations having been answered within a day. Dermatology specialists had the distinction of having the youngest e-consult patients (mean age, 38.6 years).
PCPs weigh in on results
Physicians said in interviews that the study data reflects their own positive experiences with e-consults.
“Although I don’t always think [an e-consult] is able to fully prevent the specialist visit, it does allow the specialist to provide recommendations for work-up that can be done prior to the specialist visit,” said Santina Wheat MD, a family physician at Erie Family Health Center in Chicago. This reduces the time in which the consult is placed to when effective treatment can take place.
Patients who may have to wait months or even years to see a specialty doctor, benefit from e-consults, said Dr. Wheat, who is also a member of the editorial advisory board of Family Practice News. “As part of an organization that does e-consults to another hospital with a different electronic medical record, the e-consult increases the likelihood that all of the clinical information reaches the specialists and prevents tests from being repeated.”
Starting an e-consult may also increase the likelihood that the patient quickly sees a specialist at the contracted hospital, she added.
Sarah G. Candler, MD, said in an interview that she also sees e-consults as an essential tool. “When patients present with rare, complex, or atypical pictures, I find it helpful to have specialists weigh in. The e-consult helps me ensure that I work to the top of my abilities as an internist,” said Dr. Candler, who is practice medical director and physician director of academic relations at Iora Primary Care, Northside Clinic, Houston. However, she did not agree with the study’s avoided in-person visits metric for assessing utility.
“In some cases, the end result of an e-consult is a referral for an in-person evaluation, and the role of the e-consult is to ensure that I have done my due diligence as a primary care doctor asking the correct questions, getting the appropriate work-up completed, and referring to the appropriate specialty for next steps, when necessary,” noted Dr. Candler, who also serves on the editorial advisory board of Internal Medicine News.
Financial considerations
The study’s authors suggested taking a closer look at standardizing payment for the use of e-consults and developing appropriateness criteria for them.
Health systems could use such criteria to study what makes an e-consult useful and how to best utilize this tool, Dr. Ahmed said in an interview.
“Compensation models that promote high-quality, effective, and efficient e-consults are needed to reinforce the ability of health systems to optimize the mix of e-consults and in-person visits,” Dr. Ahmed and colleagues suggested.
Because not all patient care requires e-consults, the model makes the most sense in practices that already participate in value-based payment programs. In these types of programs, the cost can be shared according to the variable risk and patient need for the service, Dr. Candler explained.
“I have been fortunate to work in two different systems that function in this way, which means that e-consults have been readily available and encouraged-both to improve patient care and decrease overall cost by decreasing unnecessary testing or specialist referral,” she said.
Dr. Wheat said that the managed care organization affiliated with her practice seems to be saving money with e-consults, as it decreases the need to pay for specialist visits in some instances and for repeated work-ups.
Future studies
The study’s cohort represented just one large health care system with a shared electronic health record. “Single-system descriptive studies, such as that of Ahmed and colleagues, are particularly useful for local evaluation and quality improvement efforts,” Varsha G. Vimalananda, MD, and B. Graeme Fincke, MD, both of the Center for Healthcare Organization and Implementation Research at Bedford (Mass.) Veterans Affairs Hospital, wrote in a related editorial.
“However, we need innovative approaches to evaluation that estimate the effect of e-consults on quality and cost of care across health care systems and over time. Implementation studies can help to identify key contributors to success,” the editorialists wrote.
One of the study authors, reported receiving personal fees from Bayer outside the submitted work. The other authors of the paper and the authors of the editorial reported no conflicts of interest. Dr. Candler said her employer contracts with an e-consult service, but that she is not compensated for use of the service. She is also a coeditor of Annals of Internal Medicine’s blog, “Fresh Look.”
SOURCE: Ahmed S et al. Ann Intern Med. 2020 Apr 14. doi: 10.7326/M19-3852.
FROM ANNALS OF INTERNAL MEDICINE
Milestone Match Day sees record highs; soar in DO applicants
Unifying allopathic (MD) and osteopathic (DO) applicants for the first time in a single matching program, 2020’s Match Day results underscored the continuing growth of DOs in the field, boosting numbers in primary care medicine and the Match as a whole.
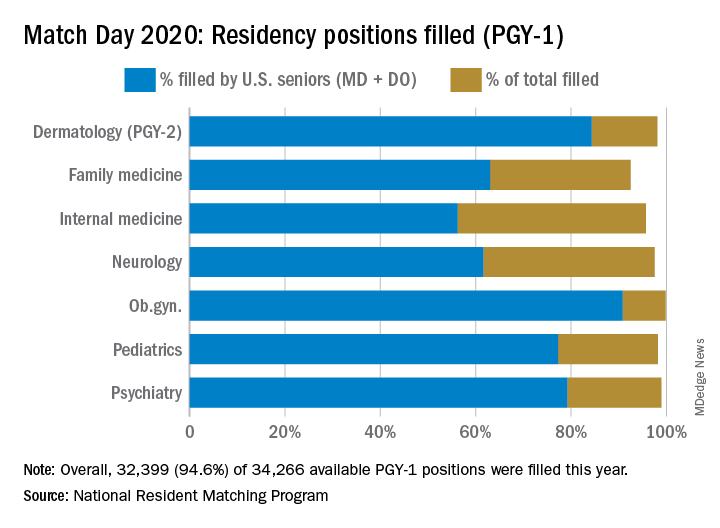
The 2020 Main Residency Match bested 2019’s record as the largest in the history of the National Resident Matching Program (NRMP), with 40,084 applicants submitting program choices for 37,256 positions. This compares with 38,376 applicants vying for 35,185 positions last year.
It’s the seventh consecutive year in which overall match numbers are up, according to the NRMP. Although the number of applicants increased, so did the number of positions, resulting in a slight drop in the percent of positions filled during 2019-2020.
Available first-year (PGY-1) positions rose to 34,266, an increase of 2,072 (6.4%) over 2019. “This was, in part, due to the last migration of osteopathic program positions into the Main Residency Match,” Donna L. Lamb, DHSc, NRMP president and CEO, said in an interview. An agreement the Accreditation Council for Graduate Medical Education, American Osteopathic Association and American Association of Colleges of Osteopathic Medicine reached in 2014 recognized ACGME as the primary accrediting body for graduate medical education programs by 2020.
This led to the first single match for U.S. MD and DO senior students and graduates and the inclusion of DO senior students as sponsored applicants in 2020, Dr. Lamb noted.
Gains, trends in 2020 match
Growth in U.S. DO senior participation also pushed this year’s Match to record highs. There were 6,581 U.S. DO medical school seniors who submitted rank order lists, 1,103 more than in 2019. Among those seniors, 90.7% matched to PGY-1 positions, driving the match rate for U.S. DO seniors up 2.6 percentage points from 2019.
Since 2016, the number of U.S. DO seniors seeking positions has risen by 3,599 or 120%. “Of course, the number of U.S. MD seniors who submitted program choices was also record-high: 19,326, an increase of 401 over 2019. The 93.7% match rate to first-year positions for this group has remained very consistent for many years,” Dr. Lamb said.
Among individual specialties, the NRMP reported extremely high fill rates for dermatology, medicine-emergency medicine, neurological surgery, physical medicine and rehabilitation (categorical), integrated plastic surgery, and thoracic surgery. Other competitive specialties included medicine-pediatrics, orthopedic surgery, otolaryngology, and vascular surgery.
Participation of international medical school students and graduates (IMGs) went up in 2020, breaking a 3-year cycle of decline. More than 61% matched to first-year positions, 2.5 percentage points higher than 2019 – and the highest match rate since 1990. “IMGs generally are having the most success matching to primary care specialties, including internal medicine, family medicine, and pediatrics,” Dr. Lamb said.
Primary care benefits from DO growth
DO candidates also helped drive up the numbers in primary care.
Internal medicine offered 8,697 categorical positions, 581 more than in 2019, reflecting a fill rate of 95.7%. More than 40% of these slots were filled by U.S. MD seniors, a category that’s seen decreases over the last 5 years, due in part to administrative and financial burdens associated with primary care internal medicine.
“In addition, the steady growth of internal medicine has increased the overall number of training positions available, and with the growth of other specialties in parallel, it has also likely had some effect on decreasing the percentage of U.S. graduates entering the field,” Phil Masters, MD, vice president of membership and global engagement at the American College of Physicians, said in an interview.
However, fill rates for U.S. DO seniors reached 16% in 2020, a notable rise from 6.9% in 2016. “As the number of osteopathic trainees increases, we are happy that more are choosing internal medicine as a career path,” Dr. Masters said, adding that the slightly different training and practice orientation of osteopathic physicians “complements that of their allopathic colleagues, and add richness to the many different practice settings that internal medicine encompasses.”
A record number of DO seniors also matched in family medicine (1,392), accounting for nearly 30% of all applicants. The single match led to an important net increase in filled family medicine residency positions, Clif Knight, MD, senior vice president for education at the American Academy of Family Physicians, said in an interview.
Overall, family medicine filled 92.5% of its 4,662 positions, 555 more than in 2019. The results show that family medicine and primary care are on solid footing, Dr. Knight said. “We are excited that the number of filled family medicine residency positions increased from last year. This is important as we work to meet the significant primary care workforce shortage,” he added.
In other specialties:
- Pediatrics filled more than 98% of its 2,864 categorical positions, 17 more than in 2019. U.S. MD seniors filled 1,731 (60.4%) of those slots. “We’re very excited about our newly matched pediatricians,” Sara “Sally” H. Goza, MD, president of the American Academy of Pediatrics, said in an interview. “The coronavirus outbreak has shown us how valuable the pediatric workforce is and how much we’re needed.’’
- Dermatology offered 478 positions, achieving a fill rate of 98.1%. “Looking at our own program’s Match results, I feel very satisfied that we are accomplishing our specific aim to serve rural populations and to create a diverse workforce in dermatology,” Erik Stratman, MD, an expert on dermatologic education in U.S. medical schools/residency programs, and a member of the American Academy of Dermatology, said in an interview. “It’s nice to see the fruits of the specialty’s expanding efforts to get the right people in the specialty who reflect those populations we serve.”
- Obstetrics-gynecology offered 1,433 first-year positions – 48 more than in 2019 – achieving a fill rate of 99.8%, with U.S. MD seniors filling more than 75% of those slots.
- Neurology filled more than 97.5% of 682 offered positions in 2020. However, U.S. MD seniors represented just under half of those filled positions (46.5%).
- Psychiatry offered 1,858 positions in 2020, achieving an overall fill rate of 98.9%, 61.2% for U.S. MD seniors.
- Emergency Medicine filled 99.5% of the 2,665 positions offered this year. In this profession, the U.S. MD fill rate was 64.3%. These new interns are sorely needed at a time when EM physicians are on the front lines of a pandemic, Hannah R. Hughes, MD, president of the Emergency Medicine Residents’ Association, said in an interview.
Unifying allopathic (MD) and osteopathic (DO) applicants for the first time in a single matching program, 2020’s Match Day results underscored the continuing growth of DOs in the field, boosting numbers in primary care medicine and the Match as a whole.
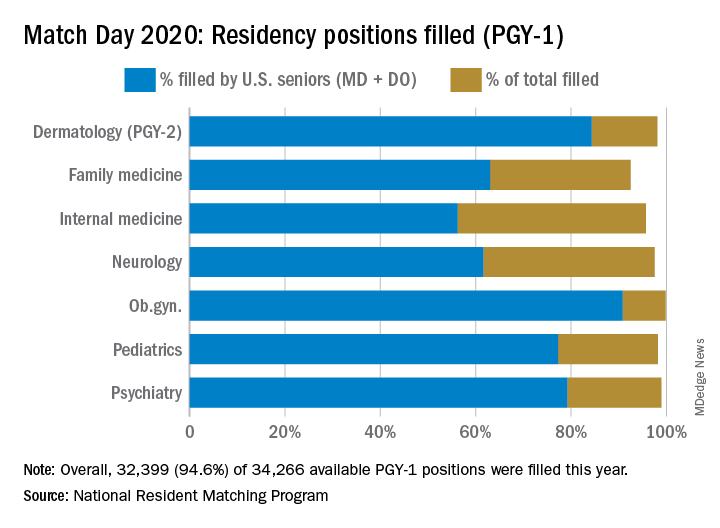
The 2020 Main Residency Match bested 2019’s record as the largest in the history of the National Resident Matching Program (NRMP), with 40,084 applicants submitting program choices for 37,256 positions. This compares with 38,376 applicants vying for 35,185 positions last year.
It’s the seventh consecutive year in which overall match numbers are up, according to the NRMP. Although the number of applicants increased, so did the number of positions, resulting in a slight drop in the percent of positions filled during 2019-2020.
Available first-year (PGY-1) positions rose to 34,266, an increase of 2,072 (6.4%) over 2019. “This was, in part, due to the last migration of osteopathic program positions into the Main Residency Match,” Donna L. Lamb, DHSc, NRMP president and CEO, said in an interview. An agreement the Accreditation Council for Graduate Medical Education, American Osteopathic Association and American Association of Colleges of Osteopathic Medicine reached in 2014 recognized ACGME as the primary accrediting body for graduate medical education programs by 2020.
This led to the first single match for U.S. MD and DO senior students and graduates and the inclusion of DO senior students as sponsored applicants in 2020, Dr. Lamb noted.
Gains, trends in 2020 match
Growth in U.S. DO senior participation also pushed this year’s Match to record highs. There were 6,581 U.S. DO medical school seniors who submitted rank order lists, 1,103 more than in 2019. Among those seniors, 90.7% matched to PGY-1 positions, driving the match rate for U.S. DO seniors up 2.6 percentage points from 2019.
Since 2016, the number of U.S. DO seniors seeking positions has risen by 3,599 or 120%. “Of course, the number of U.S. MD seniors who submitted program choices was also record-high: 19,326, an increase of 401 over 2019. The 93.7% match rate to first-year positions for this group has remained very consistent for many years,” Dr. Lamb said.
Among individual specialties, the NRMP reported extremely high fill rates for dermatology, medicine-emergency medicine, neurological surgery, physical medicine and rehabilitation (categorical), integrated plastic surgery, and thoracic surgery. Other competitive specialties included medicine-pediatrics, orthopedic surgery, otolaryngology, and vascular surgery.
Participation of international medical school students and graduates (IMGs) went up in 2020, breaking a 3-year cycle of decline. More than 61% matched to first-year positions, 2.5 percentage points higher than 2019 – and the highest match rate since 1990. “IMGs generally are having the most success matching to primary care specialties, including internal medicine, family medicine, and pediatrics,” Dr. Lamb said.
Primary care benefits from DO growth
DO candidates also helped drive up the numbers in primary care.
Internal medicine offered 8,697 categorical positions, 581 more than in 2019, reflecting a fill rate of 95.7%. More than 40% of these slots were filled by U.S. MD seniors, a category that’s seen decreases over the last 5 years, due in part to administrative and financial burdens associated with primary care internal medicine.
“In addition, the steady growth of internal medicine has increased the overall number of training positions available, and with the growth of other specialties in parallel, it has also likely had some effect on decreasing the percentage of U.S. graduates entering the field,” Phil Masters, MD, vice president of membership and global engagement at the American College of Physicians, said in an interview.
However, fill rates for U.S. DO seniors reached 16% in 2020, a notable rise from 6.9% in 2016. “As the number of osteopathic trainees increases, we are happy that more are choosing internal medicine as a career path,” Dr. Masters said, adding that the slightly different training and practice orientation of osteopathic physicians “complements that of their allopathic colleagues, and add richness to the many different practice settings that internal medicine encompasses.”
A record number of DO seniors also matched in family medicine (1,392), accounting for nearly 30% of all applicants. The single match led to an important net increase in filled family medicine residency positions, Clif Knight, MD, senior vice president for education at the American Academy of Family Physicians, said in an interview.
Overall, family medicine filled 92.5% of its 4,662 positions, 555 more than in 2019. The results show that family medicine and primary care are on solid footing, Dr. Knight said. “We are excited that the number of filled family medicine residency positions increased from last year. This is important as we work to meet the significant primary care workforce shortage,” he added.
In other specialties:
- Pediatrics filled more than 98% of its 2,864 categorical positions, 17 more than in 2019. U.S. MD seniors filled 1,731 (60.4%) of those slots. “We’re very excited about our newly matched pediatricians,” Sara “Sally” H. Goza, MD, president of the American Academy of Pediatrics, said in an interview. “The coronavirus outbreak has shown us how valuable the pediatric workforce is and how much we’re needed.’’
- Dermatology offered 478 positions, achieving a fill rate of 98.1%. “Looking at our own program’s Match results, I feel very satisfied that we are accomplishing our specific aim to serve rural populations and to create a diverse workforce in dermatology,” Erik Stratman, MD, an expert on dermatologic education in U.S. medical schools/residency programs, and a member of the American Academy of Dermatology, said in an interview. “It’s nice to see the fruits of the specialty’s expanding efforts to get the right people in the specialty who reflect those populations we serve.”
- Obstetrics-gynecology offered 1,433 first-year positions – 48 more than in 2019 – achieving a fill rate of 99.8%, with U.S. MD seniors filling more than 75% of those slots.
- Neurology filled more than 97.5% of 682 offered positions in 2020. However, U.S. MD seniors represented just under half of those filled positions (46.5%).
- Psychiatry offered 1,858 positions in 2020, achieving an overall fill rate of 98.9%, 61.2% for U.S. MD seniors.
- Emergency Medicine filled 99.5% of the 2,665 positions offered this year. In this profession, the U.S. MD fill rate was 64.3%. These new interns are sorely needed at a time when EM physicians are on the front lines of a pandemic, Hannah R. Hughes, MD, president of the Emergency Medicine Residents’ Association, said in an interview.
Unifying allopathic (MD) and osteopathic (DO) applicants for the first time in a single matching program, 2020’s Match Day results underscored the continuing growth of DOs in the field, boosting numbers in primary care medicine and the Match as a whole.
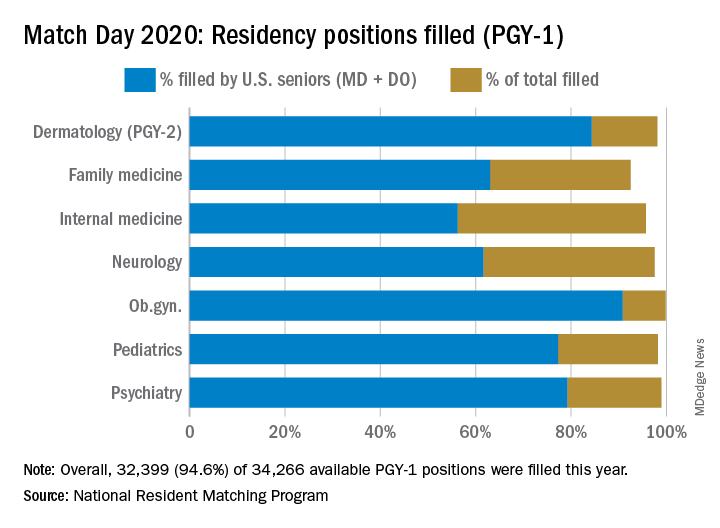
The 2020 Main Residency Match bested 2019’s record as the largest in the history of the National Resident Matching Program (NRMP), with 40,084 applicants submitting program choices for 37,256 positions. This compares with 38,376 applicants vying for 35,185 positions last year.
It’s the seventh consecutive year in which overall match numbers are up, according to the NRMP. Although the number of applicants increased, so did the number of positions, resulting in a slight drop in the percent of positions filled during 2019-2020.
Available first-year (PGY-1) positions rose to 34,266, an increase of 2,072 (6.4%) over 2019. “This was, in part, due to the last migration of osteopathic program positions into the Main Residency Match,” Donna L. Lamb, DHSc, NRMP president and CEO, said in an interview. An agreement the Accreditation Council for Graduate Medical Education, American Osteopathic Association and American Association of Colleges of Osteopathic Medicine reached in 2014 recognized ACGME as the primary accrediting body for graduate medical education programs by 2020.
This led to the first single match for U.S. MD and DO senior students and graduates and the inclusion of DO senior students as sponsored applicants in 2020, Dr. Lamb noted.
Gains, trends in 2020 match
Growth in U.S. DO senior participation also pushed this year’s Match to record highs. There were 6,581 U.S. DO medical school seniors who submitted rank order lists, 1,103 more than in 2019. Among those seniors, 90.7% matched to PGY-1 positions, driving the match rate for U.S. DO seniors up 2.6 percentage points from 2019.
Since 2016, the number of U.S. DO seniors seeking positions has risen by 3,599 or 120%. “Of course, the number of U.S. MD seniors who submitted program choices was also record-high: 19,326, an increase of 401 over 2019. The 93.7% match rate to first-year positions for this group has remained very consistent for many years,” Dr. Lamb said.
Among individual specialties, the NRMP reported extremely high fill rates for dermatology, medicine-emergency medicine, neurological surgery, physical medicine and rehabilitation (categorical), integrated plastic surgery, and thoracic surgery. Other competitive specialties included medicine-pediatrics, orthopedic surgery, otolaryngology, and vascular surgery.
Participation of international medical school students and graduates (IMGs) went up in 2020, breaking a 3-year cycle of decline. More than 61% matched to first-year positions, 2.5 percentage points higher than 2019 – and the highest match rate since 1990. “IMGs generally are having the most success matching to primary care specialties, including internal medicine, family medicine, and pediatrics,” Dr. Lamb said.
Primary care benefits from DO growth
DO candidates also helped drive up the numbers in primary care.
Internal medicine offered 8,697 categorical positions, 581 more than in 2019, reflecting a fill rate of 95.7%. More than 40% of these slots were filled by U.S. MD seniors, a category that’s seen decreases over the last 5 years, due in part to administrative and financial burdens associated with primary care internal medicine.
“In addition, the steady growth of internal medicine has increased the overall number of training positions available, and with the growth of other specialties in parallel, it has also likely had some effect on decreasing the percentage of U.S. graduates entering the field,” Phil Masters, MD, vice president of membership and global engagement at the American College of Physicians, said in an interview.
However, fill rates for U.S. DO seniors reached 16% in 2020, a notable rise from 6.9% in 2016. “As the number of osteopathic trainees increases, we are happy that more are choosing internal medicine as a career path,” Dr. Masters said, adding that the slightly different training and practice orientation of osteopathic physicians “complements that of their allopathic colleagues, and add richness to the many different practice settings that internal medicine encompasses.”
A record number of DO seniors also matched in family medicine (1,392), accounting for nearly 30% of all applicants. The single match led to an important net increase in filled family medicine residency positions, Clif Knight, MD, senior vice president for education at the American Academy of Family Physicians, said in an interview.
Overall, family medicine filled 92.5% of its 4,662 positions, 555 more than in 2019. The results show that family medicine and primary care are on solid footing, Dr. Knight said. “We are excited that the number of filled family medicine residency positions increased from last year. This is important as we work to meet the significant primary care workforce shortage,” he added.
In other specialties:
- Pediatrics filled more than 98% of its 2,864 categorical positions, 17 more than in 2019. U.S. MD seniors filled 1,731 (60.4%) of those slots. “We’re very excited about our newly matched pediatricians,” Sara “Sally” H. Goza, MD, president of the American Academy of Pediatrics, said in an interview. “The coronavirus outbreak has shown us how valuable the pediatric workforce is and how much we’re needed.’’
- Dermatology offered 478 positions, achieving a fill rate of 98.1%. “Looking at our own program’s Match results, I feel very satisfied that we are accomplishing our specific aim to serve rural populations and to create a diverse workforce in dermatology,” Erik Stratman, MD, an expert on dermatologic education in U.S. medical schools/residency programs, and a member of the American Academy of Dermatology, said in an interview. “It’s nice to see the fruits of the specialty’s expanding efforts to get the right people in the specialty who reflect those populations we serve.”
- Obstetrics-gynecology offered 1,433 first-year positions – 48 more than in 2019 – achieving a fill rate of 99.8%, with U.S. MD seniors filling more than 75% of those slots.
- Neurology filled more than 97.5% of 682 offered positions in 2020. However, U.S. MD seniors represented just under half of those filled positions (46.5%).
- Psychiatry offered 1,858 positions in 2020, achieving an overall fill rate of 98.9%, 61.2% for U.S. MD seniors.
- Emergency Medicine filled 99.5% of the 2,665 positions offered this year. In this profession, the U.S. MD fill rate was 64.3%. These new interns are sorely needed at a time when EM physicians are on the front lines of a pandemic, Hannah R. Hughes, MD, president of the Emergency Medicine Residents’ Association, said in an interview.
Match Day 2020: Online announcements replace celebrations, champagne
The third Friday in March usually marks a time when medical students across the United States participate in envelope-opening ceremonies with peers and family members. This year, the ruthless onslaught of coronavirus has forced residency programs to rethink their celebrations, leveraging social media platforms and other technologies to toast Match Day in cyberspace.
In the absence of ceremonies taking place due to restrictions on mass gatherings, “we anticipate that students may be more emotional than they expect,” Hannah R. Hughes, MD, president of the Emergency Medicine Residents’ Association (EMRA) said in an interview. To support these students on their journey to residency, EMRA has launched a social media campaign, asking medical students “to share with us their envelope-opening moments – either a selfie, photo, or video – that we can share with our online networks,” Dr. Hughes said.
EMRA is also asking program coordinators to forward photos and congratulatory messages to their new residents “so that we can share them with our networks at large,” she added.
Going virtual, it seems, has become the new norm.
At the University of California, San Francisco, the medical school decided to cancel its Match Day celebration for new interns, echoing many other programs across the United States. “We always send out a welcome email and make phone calls to all of our new interns,” said Rebecca Berman, MD, director of UCSF’s internal medicine residency program, which houses 63 medicine interns and 181 residents. Traditionally, the program has hosted the celebration for current residents. That, of course, had to change this year.
Current interns like to join in the fun, “since it means their internship is rapidly coming to a close,” said Dr. Berman, who at press time was considering a virtual toast via Zoom as a possible alternative. “These are difficult times for everyone, and we are doing our best to make our residents feel united and connected while they take care of patients in the era of social distancing.”
Melissa Held, MD, associate dean of medical student affairs at the University of Connecticut’s School of Medicine, Farmington, had been planning a celebration in the school’s academic rotunda with food and champagne. “Students typically come with their family members or significant others. The dean and I usually say a few words and then at noon, students get envelopes and can open them to find out where they matched for residency,” Dr. Held said. This year, the school will be uploading Match letters to its online system. Students can remotely find out where they matched at noon. “I plan to put together a slide show of pictures and congratulatory remarks from faculty and staff that will be sent to them around 11:30 a.m.,” Dr. Held said.
Mark Miceli, EdD, who oversees Match Day for the 130-plus medical students at the University of Massachusetts Medical School, Worcester, is inviting faculty and staff to submit short videos of congratulations, which it will post on its student affairs Match Day Instagram account. Like other schools, it will share results with students in an email, said Dr. Miceli, assistant vice provost of student life. “This message will be more personalized to our school than the NRMP [National Resident Matching Program] message, and will also include links to our match stats, a map of our matched student locations, and a list of where folks matched,” he said.
Students can opt out of the list if they want to. The communications department has also provided templates for signs students can print out. “They can write in where they matched, and take pictures for social media. We are encouraging the use of various hashtags to help build a virtual community,” Dr. Miceli said.
In a state hit particularly hard by coronavirus, the University of Washington School of Medicine is spreading Match Day cheer through online meeting platforms and celebratory graphics. This five-state school, representing students from Washington, Wyoming, Alaska, Montana, and Idaho, usually hosts several events across the different states and students have their pick of which to attend, according to Sarah Wood, associate director of student affairs.
In lieu of in-person events, some states are hosting a Zoom online celebration, others are using social media networking systems. “We’re inviting everyone to take part in an online event ... where we’ll do a slide show of photos that one of our students put together,” Ms. Wood said.
Students are disappointed in this change of plans, she said. To make things more festive, Ms. Wood is adding graphics such as fireworks and photos to the emails containing the Match results. “I want this to be more exciting for them than just a basic letter,” she said.
For now, Ms. Wood is trying to focus on the Match Day celebration, but admits that “my bigger fear is if we have to cancel graduation – and what that might look like.”
The third Friday in March usually marks a time when medical students across the United States participate in envelope-opening ceremonies with peers and family members. This year, the ruthless onslaught of coronavirus has forced residency programs to rethink their celebrations, leveraging social media platforms and other technologies to toast Match Day in cyberspace.
In the absence of ceremonies taking place due to restrictions on mass gatherings, “we anticipate that students may be more emotional than they expect,” Hannah R. Hughes, MD, president of the Emergency Medicine Residents’ Association (EMRA) said in an interview. To support these students on their journey to residency, EMRA has launched a social media campaign, asking medical students “to share with us their envelope-opening moments – either a selfie, photo, or video – that we can share with our online networks,” Dr. Hughes said.
EMRA is also asking program coordinators to forward photos and congratulatory messages to their new residents “so that we can share them with our networks at large,” she added.
Going virtual, it seems, has become the new norm.
At the University of California, San Francisco, the medical school decided to cancel its Match Day celebration for new interns, echoing many other programs across the United States. “We always send out a welcome email and make phone calls to all of our new interns,” said Rebecca Berman, MD, director of UCSF’s internal medicine residency program, which houses 63 medicine interns and 181 residents. Traditionally, the program has hosted the celebration for current residents. That, of course, had to change this year.
Current interns like to join in the fun, “since it means their internship is rapidly coming to a close,” said Dr. Berman, who at press time was considering a virtual toast via Zoom as a possible alternative. “These are difficult times for everyone, and we are doing our best to make our residents feel united and connected while they take care of patients in the era of social distancing.”
Melissa Held, MD, associate dean of medical student affairs at the University of Connecticut’s School of Medicine, Farmington, had been planning a celebration in the school’s academic rotunda with food and champagne. “Students typically come with their family members or significant others. The dean and I usually say a few words and then at noon, students get envelopes and can open them to find out where they matched for residency,” Dr. Held said. This year, the school will be uploading Match letters to its online system. Students can remotely find out where they matched at noon. “I plan to put together a slide show of pictures and congratulatory remarks from faculty and staff that will be sent to them around 11:30 a.m.,” Dr. Held said.
Mark Miceli, EdD, who oversees Match Day for the 130-plus medical students at the University of Massachusetts Medical School, Worcester, is inviting faculty and staff to submit short videos of congratulations, which it will post on its student affairs Match Day Instagram account. Like other schools, it will share results with students in an email, said Dr. Miceli, assistant vice provost of student life. “This message will be more personalized to our school than the NRMP [National Resident Matching Program] message, and will also include links to our match stats, a map of our matched student locations, and a list of where folks matched,” he said.
Students can opt out of the list if they want to. The communications department has also provided templates for signs students can print out. “They can write in where they matched, and take pictures for social media. We are encouraging the use of various hashtags to help build a virtual community,” Dr. Miceli said.
In a state hit particularly hard by coronavirus, the University of Washington School of Medicine is spreading Match Day cheer through online meeting platforms and celebratory graphics. This five-state school, representing students from Washington, Wyoming, Alaska, Montana, and Idaho, usually hosts several events across the different states and students have their pick of which to attend, according to Sarah Wood, associate director of student affairs.
In lieu of in-person events, some states are hosting a Zoom online celebration, others are using social media networking systems. “We’re inviting everyone to take part in an online event ... where we’ll do a slide show of photos that one of our students put together,” Ms. Wood said.
Students are disappointed in this change of plans, she said. To make things more festive, Ms. Wood is adding graphics such as fireworks and photos to the emails containing the Match results. “I want this to be more exciting for them than just a basic letter,” she said.
For now, Ms. Wood is trying to focus on the Match Day celebration, but admits that “my bigger fear is if we have to cancel graduation – and what that might look like.”
The third Friday in March usually marks a time when medical students across the United States participate in envelope-opening ceremonies with peers and family members. This year, the ruthless onslaught of coronavirus has forced residency programs to rethink their celebrations, leveraging social media platforms and other technologies to toast Match Day in cyberspace.
In the absence of ceremonies taking place due to restrictions on mass gatherings, “we anticipate that students may be more emotional than they expect,” Hannah R. Hughes, MD, president of the Emergency Medicine Residents’ Association (EMRA) said in an interview. To support these students on their journey to residency, EMRA has launched a social media campaign, asking medical students “to share with us their envelope-opening moments – either a selfie, photo, or video – that we can share with our online networks,” Dr. Hughes said.
EMRA is also asking program coordinators to forward photos and congratulatory messages to their new residents “so that we can share them with our networks at large,” she added.
Going virtual, it seems, has become the new norm.
At the University of California, San Francisco, the medical school decided to cancel its Match Day celebration for new interns, echoing many other programs across the United States. “We always send out a welcome email and make phone calls to all of our new interns,” said Rebecca Berman, MD, director of UCSF’s internal medicine residency program, which houses 63 medicine interns and 181 residents. Traditionally, the program has hosted the celebration for current residents. That, of course, had to change this year.
Current interns like to join in the fun, “since it means their internship is rapidly coming to a close,” said Dr. Berman, who at press time was considering a virtual toast via Zoom as a possible alternative. “These are difficult times for everyone, and we are doing our best to make our residents feel united and connected while they take care of patients in the era of social distancing.”
Melissa Held, MD, associate dean of medical student affairs at the University of Connecticut’s School of Medicine, Farmington, had been planning a celebration in the school’s academic rotunda with food and champagne. “Students typically come with their family members or significant others. The dean and I usually say a few words and then at noon, students get envelopes and can open them to find out where they matched for residency,” Dr. Held said. This year, the school will be uploading Match letters to its online system. Students can remotely find out where they matched at noon. “I plan to put together a slide show of pictures and congratulatory remarks from faculty and staff that will be sent to them around 11:30 a.m.,” Dr. Held said.
Mark Miceli, EdD, who oversees Match Day for the 130-plus medical students at the University of Massachusetts Medical School, Worcester, is inviting faculty and staff to submit short videos of congratulations, which it will post on its student affairs Match Day Instagram account. Like other schools, it will share results with students in an email, said Dr. Miceli, assistant vice provost of student life. “This message will be more personalized to our school than the NRMP [National Resident Matching Program] message, and will also include links to our match stats, a map of our matched student locations, and a list of where folks matched,” he said.
Students can opt out of the list if they want to. The communications department has also provided templates for signs students can print out. “They can write in where they matched, and take pictures for social media. We are encouraging the use of various hashtags to help build a virtual community,” Dr. Miceli said.
In a state hit particularly hard by coronavirus, the University of Washington School of Medicine is spreading Match Day cheer through online meeting platforms and celebratory graphics. This five-state school, representing students from Washington, Wyoming, Alaska, Montana, and Idaho, usually hosts several events across the different states and students have their pick of which to attend, according to Sarah Wood, associate director of student affairs.
In lieu of in-person events, some states are hosting a Zoom online celebration, others are using social media networking systems. “We’re inviting everyone to take part in an online event ... where we’ll do a slide show of photos that one of our students put together,” Ms. Wood said.
Students are disappointed in this change of plans, she said. To make things more festive, Ms. Wood is adding graphics such as fireworks and photos to the emails containing the Match results. “I want this to be more exciting for them than just a basic letter,” she said.
For now, Ms. Wood is trying to focus on the Match Day celebration, but admits that “my bigger fear is if we have to cancel graduation – and what that might look like.”
Policy & Practice
Wisconsin Doctors Want Cap Back
Wisconsin doctors hailed the state assembly's passage of a bill from Rep. Curt Gielow (R) that would reinstate a cap on noneconomic damages at $750,000. The 10-year-old cap was overturned by the Wisconsin Supreme Court in 2005, “throwing Wisconsin's once envied medical liability system into turmoil,” according to a statement issued by the Wisconsin Hospital Association and the Wisconsin Medical Society. Following the dissolution of the cap, physicians have cancelled their recruiting visits to the state, and premiums for the Injured Patients and Families Compensation Fund have increased by 25%, the associations claimed. “Four awards have already exceeded the previous cap, the number of lawsuits in excess of $1 million [increased] by over 22%, and a stunning $8.4 million verdict was handed down in Dane County,” the statement said. “This bill helps doctors concentrate on what concerns them the most: caring for patients,” said Dr. Susan Turney, chief executive officer and executive vice president of the Wisconsin Medical Society. “It doesn't change the fact that injured patients are fully compensated for their economic losses yet helps to maintain access to health care in Wisconsin.” The state's high court had ruled that the cap was unconstitutional beyond a reasonable doubt. A similar bill has been introduced in the state Senate.
Hospital Ethnicity Data
Most hospitals collect data about the race, ethnicity, and language preference of their patients, but few are using the data to improve health care quality, according to a study that was conducted by the National Public Health and Hospital Institute. Researchers surveyed 500 acute care hospitals and found that half collect information on patients' language, more than three-fourths collect information on patients' race, and half collect information on patients' ethnicity and language preference. Of the hospitals that did not collect this information, more than half said that they did not see the need to. “We are encouraged to know that so many hospitals already have quality data that enable them to develop and monitor interventions to eliminate racial and ethnic disparities in health care,” said Marsha Regenstein, Ph.D., the study's lead author and director of NPHHI. “Our challenge now is to work with hospital staff to make sure they recognize the importance of this quality data and that they put the data to use immediately.” The study was supported by the Robert Wood Johnson Foundation.
Assessing Pay for Performance
More than 100 pay-for-performance programs were operating around the country as of last September, according to a new report from the Alliance for Health Reform. Members of Congress and the Bush administration also are exploring methods for testing pay for performance within the Medicare program, including Medicare's voluntary physician reporting program which began earlier this year. So far, the private sector has taken the lead on pay for performance, according to the report. A prime example is the Bridges to Excellence program, sponsored by several large employers and operating in Cincinnati, Louisville, Ky., Massachusetts, and Albany/Schenectady, N.Y. The program is expanding into the District of Columbia/Maryland/Virginia area, Minnesota, and Georgia. The group offers payment incentives to high-performing physicians in the area of diabetes and cardiac care, and in the use of health information technology. But despite the success of the Bridges to Excellence model and some others, critics say that there are a number of unanswered questions. For example, proponents of pay for performance need to identify the size of the bonus or penalty needed to make a difference in quality, and to figure out what adjustments need to be made to payment systems across different medical specialties, according to the report.
Fighting Off Bad Bugs
Congress should be taking more aggressive steps to incentivize pharmaceutical and biotechnology industries to fight antibiotic resistance, physicians and other policy makers said during a press conference sponsored by the Infectious Diseases Society of America. The group released its “hit list” of the six most dangerous, drug-resistant microbes. “These are life-threatening drug-resistant infections, and we're seeing them every day,” explained Dr. Martin J. Blaser, IDSA president. “What is worse is that our ammunition is running out and there are no reinforcements in sight.” Another problem: “Some of the better drugs are more toxic,” he said. Robert Guidos, director of public policy with IDSA, noted that Congress has not taken any action to support the implementation of new incentives for drug companies to develop stronger antibiotics. Market exclusivity—a method that has worked favorably in the past for pediatric drugs—would be an option, he said. So would calling for tax credits for the manufacture or distribution of these products. Another option would be to establish an independent commission to identify which drugs are better at combating resistant microbes. “The superbugs are not waiting, and neither should we,” Dr. Blaser commented. The top “bad bugs” are methicillin-resistant Staphylococcus aureus; Escherichia coli and Klebsiella species; Acinetobacter baumannii; Aspergillus; vancomycin-resistant Enterococcus faecium; and Pseudomonas aeruginosa, according to the IDSA report.
Wisconsin Doctors Want Cap Back
Wisconsin doctors hailed the state assembly's passage of a bill from Rep. Curt Gielow (R) that would reinstate a cap on noneconomic damages at $750,000. The 10-year-old cap was overturned by the Wisconsin Supreme Court in 2005, “throwing Wisconsin's once envied medical liability system into turmoil,” according to a statement issued by the Wisconsin Hospital Association and the Wisconsin Medical Society. Following the dissolution of the cap, physicians have cancelled their recruiting visits to the state, and premiums for the Injured Patients and Families Compensation Fund have increased by 25%, the associations claimed. “Four awards have already exceeded the previous cap, the number of lawsuits in excess of $1 million [increased] by over 22%, and a stunning $8.4 million verdict was handed down in Dane County,” the statement said. “This bill helps doctors concentrate on what concerns them the most: caring for patients,” said Dr. Susan Turney, chief executive officer and executive vice president of the Wisconsin Medical Society. “It doesn't change the fact that injured patients are fully compensated for their economic losses yet helps to maintain access to health care in Wisconsin.” The state's high court had ruled that the cap was unconstitutional beyond a reasonable doubt. A similar bill has been introduced in the state Senate.
Hospital Ethnicity Data
Most hospitals collect data about the race, ethnicity, and language preference of their patients, but few are using the data to improve health care quality, according to a study that was conducted by the National Public Health and Hospital Institute. Researchers surveyed 500 acute care hospitals and found that half collect information on patients' language, more than three-fourths collect information on patients' race, and half collect information on patients' ethnicity and language preference. Of the hospitals that did not collect this information, more than half said that they did not see the need to. “We are encouraged to know that so many hospitals already have quality data that enable them to develop and monitor interventions to eliminate racial and ethnic disparities in health care,” said Marsha Regenstein, Ph.D., the study's lead author and director of NPHHI. “Our challenge now is to work with hospital staff to make sure they recognize the importance of this quality data and that they put the data to use immediately.” The study was supported by the Robert Wood Johnson Foundation.
Assessing Pay for Performance
More than 100 pay-for-performance programs were operating around the country as of last September, according to a new report from the Alliance for Health Reform. Members of Congress and the Bush administration also are exploring methods for testing pay for performance within the Medicare program, including Medicare's voluntary physician reporting program which began earlier this year. So far, the private sector has taken the lead on pay for performance, according to the report. A prime example is the Bridges to Excellence program, sponsored by several large employers and operating in Cincinnati, Louisville, Ky., Massachusetts, and Albany/Schenectady, N.Y. The program is expanding into the District of Columbia/Maryland/Virginia area, Minnesota, and Georgia. The group offers payment incentives to high-performing physicians in the area of diabetes and cardiac care, and in the use of health information technology. But despite the success of the Bridges to Excellence model and some others, critics say that there are a number of unanswered questions. For example, proponents of pay for performance need to identify the size of the bonus or penalty needed to make a difference in quality, and to figure out what adjustments need to be made to payment systems across different medical specialties, according to the report.
Fighting Off Bad Bugs
Congress should be taking more aggressive steps to incentivize pharmaceutical and biotechnology industries to fight antibiotic resistance, physicians and other policy makers said during a press conference sponsored by the Infectious Diseases Society of America. The group released its “hit list” of the six most dangerous, drug-resistant microbes. “These are life-threatening drug-resistant infections, and we're seeing them every day,” explained Dr. Martin J. Blaser, IDSA president. “What is worse is that our ammunition is running out and there are no reinforcements in sight.” Another problem: “Some of the better drugs are more toxic,” he said. Robert Guidos, director of public policy with IDSA, noted that Congress has not taken any action to support the implementation of new incentives for drug companies to develop stronger antibiotics. Market exclusivity—a method that has worked favorably in the past for pediatric drugs—would be an option, he said. So would calling for tax credits for the manufacture or distribution of these products. Another option would be to establish an independent commission to identify which drugs are better at combating resistant microbes. “The superbugs are not waiting, and neither should we,” Dr. Blaser commented. The top “bad bugs” are methicillin-resistant Staphylococcus aureus; Escherichia coli and Klebsiella species; Acinetobacter baumannii; Aspergillus; vancomycin-resistant Enterococcus faecium; and Pseudomonas aeruginosa, according to the IDSA report.
Wisconsin Doctors Want Cap Back
Wisconsin doctors hailed the state assembly's passage of a bill from Rep. Curt Gielow (R) that would reinstate a cap on noneconomic damages at $750,000. The 10-year-old cap was overturned by the Wisconsin Supreme Court in 2005, “throwing Wisconsin's once envied medical liability system into turmoil,” according to a statement issued by the Wisconsin Hospital Association and the Wisconsin Medical Society. Following the dissolution of the cap, physicians have cancelled their recruiting visits to the state, and premiums for the Injured Patients and Families Compensation Fund have increased by 25%, the associations claimed. “Four awards have already exceeded the previous cap, the number of lawsuits in excess of $1 million [increased] by over 22%, and a stunning $8.4 million verdict was handed down in Dane County,” the statement said. “This bill helps doctors concentrate on what concerns them the most: caring for patients,” said Dr. Susan Turney, chief executive officer and executive vice president of the Wisconsin Medical Society. “It doesn't change the fact that injured patients are fully compensated for their economic losses yet helps to maintain access to health care in Wisconsin.” The state's high court had ruled that the cap was unconstitutional beyond a reasonable doubt. A similar bill has been introduced in the state Senate.
Hospital Ethnicity Data
Most hospitals collect data about the race, ethnicity, and language preference of their patients, but few are using the data to improve health care quality, according to a study that was conducted by the National Public Health and Hospital Institute. Researchers surveyed 500 acute care hospitals and found that half collect information on patients' language, more than three-fourths collect information on patients' race, and half collect information on patients' ethnicity and language preference. Of the hospitals that did not collect this information, more than half said that they did not see the need to. “We are encouraged to know that so many hospitals already have quality data that enable them to develop and monitor interventions to eliminate racial and ethnic disparities in health care,” said Marsha Regenstein, Ph.D., the study's lead author and director of NPHHI. “Our challenge now is to work with hospital staff to make sure they recognize the importance of this quality data and that they put the data to use immediately.” The study was supported by the Robert Wood Johnson Foundation.
Assessing Pay for Performance
More than 100 pay-for-performance programs were operating around the country as of last September, according to a new report from the Alliance for Health Reform. Members of Congress and the Bush administration also are exploring methods for testing pay for performance within the Medicare program, including Medicare's voluntary physician reporting program which began earlier this year. So far, the private sector has taken the lead on pay for performance, according to the report. A prime example is the Bridges to Excellence program, sponsored by several large employers and operating in Cincinnati, Louisville, Ky., Massachusetts, and Albany/Schenectady, N.Y. The program is expanding into the District of Columbia/Maryland/Virginia area, Minnesota, and Georgia. The group offers payment incentives to high-performing physicians in the area of diabetes and cardiac care, and in the use of health information technology. But despite the success of the Bridges to Excellence model and some others, critics say that there are a number of unanswered questions. For example, proponents of pay for performance need to identify the size of the bonus or penalty needed to make a difference in quality, and to figure out what adjustments need to be made to payment systems across different medical specialties, according to the report.
Fighting Off Bad Bugs
Congress should be taking more aggressive steps to incentivize pharmaceutical and biotechnology industries to fight antibiotic resistance, physicians and other policy makers said during a press conference sponsored by the Infectious Diseases Society of America. The group released its “hit list” of the six most dangerous, drug-resistant microbes. “These are life-threatening drug-resistant infections, and we're seeing them every day,” explained Dr. Martin J. Blaser, IDSA president. “What is worse is that our ammunition is running out and there are no reinforcements in sight.” Another problem: “Some of the better drugs are more toxic,” he said. Robert Guidos, director of public policy with IDSA, noted that Congress has not taken any action to support the implementation of new incentives for drug companies to develop stronger antibiotics. Market exclusivity—a method that has worked favorably in the past for pediatric drugs—would be an option, he said. So would calling for tax credits for the manufacture or distribution of these products. Another option would be to establish an independent commission to identify which drugs are better at combating resistant microbes. “The superbugs are not waiting, and neither should we,” Dr. Blaser commented. The top “bad bugs” are methicillin-resistant Staphylococcus aureus; Escherichia coli and Klebsiella species; Acinetobacter baumannii; Aspergillus; vancomycin-resistant Enterococcus faecium; and Pseudomonas aeruginosa, according to the IDSA report.












