User login
The Bigger They Are ...
Editor’s note: This is the first of a two-part series addressing large HM group issues.
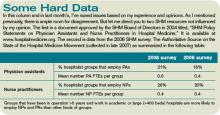
In the mid-1990s, when I first became interested in how other hospitalist groups were organized, I started surveying by phone all the groups I could find. It was really unusual to find a group larger than four or five full-time equivalent (FTE) hospitalists. Since then, the size of a typical hospitalist group has grown steadily, and data reported in SHM’s “2007-2008 Bi-Annual Survey on the State of Hospital Medicine” shows the median number of FTE physicians in HM groups is 8.0 (mean of 9.75). So in just a few years, our field has grown in such a way that half of all groups in operation now have more than eight physician FTEs. I think most future growth in numbers of hospitalists will be due to individual practices getting larger, rather than new practices starting up.
I work regularly with groups that have more than 20 FTEs, and I have found that large groups tend to have a number of attributes in common.
Separate Daytime Admitter and Rounder Functions
Large groups almost always staff admitter and rounder functions with separate doctors around the clock. That means patients arriving during regular business hours are admitted by a different doctor (the admitter) than the doctor who will provide their care on Day Two and beyond (the rounder).
Although such a system is popular, I suggest every group challenge itself to think about whether it really is the best system. Most groups, regardless of size, have about a quarter to a third of their new admits and consults arrive between 7 a.m. and 5 p.m. If the group did away with a separate admitter during the day and moved all daytime admitters into additional rounder positions, all the daytime admissions could be rotated among all of the daytime doctors, and those patients would typically be seen by the same hospitalist the next day. That would improve hospitalist-patient continuity for the patients who arrive during the day, which might improve the group’s overall efficiency as well as quality and patient satisfaction. Each rounder would become responsible for seeing up to three new consults or admissions during the course of the daytime rounding shift, and the list of new patients to take over each morning—patients admitted by the evening and night admitters—would be smaller.
Of course, one significant benefit of having a separate admitter shift during the day is relieving the rounding doctors of the stress of interrupting rounds for an unpredictable number of new admissions each day. And if the new admissions arrive in the morning, throughput may suffer as it might mean the rounding doctor may see “dischargeable” patients later in the day.
I think there is room for debate about whether it is best for large groups to have a separate admitter during the day, but whatever approach a group chooses, it should acknowledge the costs of that approach and not just assume that it is the only one that is feasible or reasonable.
Who Is Caring for Whom?
The larger the hospitalist group, the more difficulty nurses and other staff have understanding exactly how patients are distributed among the doctors. When one hospitalist rotates “off service” to be replaced by another the next day, or when overnight admissions are “picked up” by a rounding doctor the next morning, it can be difficult for nurses to know which hospitalist is responsible for the patient at a given moment.
All groups, regardless of size, should ensure that the hospitalist who picks up patients from a colleague who has rotated off the day before writes an order in the chart indicating “change attending to Dr. Jones,” or clearly communicates who the new hospitalist is by some other means, such as an electronic medical record or a phone call from a clerk. It isn’t enough that patients are assigned to a particular team—say, the “white team” or the “green team”—for their entire stay. Nurses and other staff need to know which hospitalist is covering that team each day.
One test of how well your system is working is to assess how the nurse answers when a patient or family asks, “Which doctor will be in to see me today?” It isn’t good enough for the nurse to just say, “The green-team doctor will see you, but I don’t know who that is today.” The nurse needs to be able to provide the name of the doctor who will be in. If nurses at your hospital regularly page the wrong hospitalist, or must call around just to figure out who the attending hospitalist is for a particular patient, then you have an opportunity to improve how you communicate this information to the nurse and others.
Even if you have a system in which it is clear to everyone which hospitalist has taken over for one who has rotated off-service, you need to ensure that nurses can easily determine the attending hospitalist for patients admitted the night before. Night-shift staff not knowing which doctor will take over in the morning is an all-too-common problem, and it results in too many staffers not knowing who is caring for the patient from the time the night doctor goes off (e.g., 7 a.m.) until the rounder taking over gets to that patient on rounds. Having evening/night admitters assign attending, or rounder, hospitalists at the time of each admission is a great solution, and I’ll provide ideas about how to do this in next month’s column.
I worry about patient satisfaction if the evening/night admitter can’t tell the patient the name of the hospitalist who will take over in the morning. How can the patient feel that they’re getting personalized care when they’re told, “I don’t know which of my partners will take over your care tomorrow. They all get together and divide up the patients each morning and will assign a doctor to you then”? It’s different if the admitter tells the patient, “I’m on call for our group tonight, but will be home sleeping tomorrow and my colleague, Dr. Clapton, will take over your care in the morning.” I usually go on to say with a wink that the patient is getting an upgrade, because Dr. Clapton is so much smarter and better-looking than me. I’ll understand if the embellishment doesn’t feel right for you, but I think there is value in the admitter, or a hospitalist rotating off-service, taking a minute to say something nice about the hospitalist who will take over next.
Next month, I will continue to explore issues that are particularly problematic for larger groups. TH
Dr. Nelson has been a practicing hospitalist since 1988 and is co-founder and past president of SHM. He is a principal in Nelson/Flores Associates, a national hospitalist practice management consulting firm. He also is part of the faculty for SHM’s “Best Practices in Managing a Hospital Medicine Program” course. This column represents his views and is not intended to reflect an official position of SHM.
Editor’s note: This is the first of a two-part series addressing large HM group issues.
In the mid-1990s, when I first became interested in how other hospitalist groups were organized, I started surveying by phone all the groups I could find. It was really unusual to find a group larger than four or five full-time equivalent (FTE) hospitalists. Since then, the size of a typical hospitalist group has grown steadily, and data reported in SHM’s “2007-2008 Bi-Annual Survey on the State of Hospital Medicine” shows the median number of FTE physicians in HM groups is 8.0 (mean of 9.75). So in just a few years, our field has grown in such a way that half of all groups in operation now have more than eight physician FTEs. I think most future growth in numbers of hospitalists will be due to individual practices getting larger, rather than new practices starting up.
I work regularly with groups that have more than 20 FTEs, and I have found that large groups tend to have a number of attributes in common.
Separate Daytime Admitter and Rounder Functions
Large groups almost always staff admitter and rounder functions with separate doctors around the clock. That means patients arriving during regular business hours are admitted by a different doctor (the admitter) than the doctor who will provide their care on Day Two and beyond (the rounder).
Although such a system is popular, I suggest every group challenge itself to think about whether it really is the best system. Most groups, regardless of size, have about a quarter to a third of their new admits and consults arrive between 7 a.m. and 5 p.m. If the group did away with a separate admitter during the day and moved all daytime admitters into additional rounder positions, all the daytime admissions could be rotated among all of the daytime doctors, and those patients would typically be seen by the same hospitalist the next day. That would improve hospitalist-patient continuity for the patients who arrive during the day, which might improve the group’s overall efficiency as well as quality and patient satisfaction. Each rounder would become responsible for seeing up to three new consults or admissions during the course of the daytime rounding shift, and the list of new patients to take over each morning—patients admitted by the evening and night admitters—would be smaller.
Of course, one significant benefit of having a separate admitter shift during the day is relieving the rounding doctors of the stress of interrupting rounds for an unpredictable number of new admissions each day. And if the new admissions arrive in the morning, throughput may suffer as it might mean the rounding doctor may see “dischargeable” patients later in the day.
I think there is room for debate about whether it is best for large groups to have a separate admitter during the day, but whatever approach a group chooses, it should acknowledge the costs of that approach and not just assume that it is the only one that is feasible or reasonable.
Who Is Caring for Whom?
The larger the hospitalist group, the more difficulty nurses and other staff have understanding exactly how patients are distributed among the doctors. When one hospitalist rotates “off service” to be replaced by another the next day, or when overnight admissions are “picked up” by a rounding doctor the next morning, it can be difficult for nurses to know which hospitalist is responsible for the patient at a given moment.
All groups, regardless of size, should ensure that the hospitalist who picks up patients from a colleague who has rotated off the day before writes an order in the chart indicating “change attending to Dr. Jones,” or clearly communicates who the new hospitalist is by some other means, such as an electronic medical record or a phone call from a clerk. It isn’t enough that patients are assigned to a particular team—say, the “white team” or the “green team”—for their entire stay. Nurses and other staff need to know which hospitalist is covering that team each day.
One test of how well your system is working is to assess how the nurse answers when a patient or family asks, “Which doctor will be in to see me today?” It isn’t good enough for the nurse to just say, “The green-team doctor will see you, but I don’t know who that is today.” The nurse needs to be able to provide the name of the doctor who will be in. If nurses at your hospital regularly page the wrong hospitalist, or must call around just to figure out who the attending hospitalist is for a particular patient, then you have an opportunity to improve how you communicate this information to the nurse and others.
Even if you have a system in which it is clear to everyone which hospitalist has taken over for one who has rotated off-service, you need to ensure that nurses can easily determine the attending hospitalist for patients admitted the night before. Night-shift staff not knowing which doctor will take over in the morning is an all-too-common problem, and it results in too many staffers not knowing who is caring for the patient from the time the night doctor goes off (e.g., 7 a.m.) until the rounder taking over gets to that patient on rounds. Having evening/night admitters assign attending, or rounder, hospitalists at the time of each admission is a great solution, and I’ll provide ideas about how to do this in next month’s column.
I worry about patient satisfaction if the evening/night admitter can’t tell the patient the name of the hospitalist who will take over in the morning. How can the patient feel that they’re getting personalized care when they’re told, “I don’t know which of my partners will take over your care tomorrow. They all get together and divide up the patients each morning and will assign a doctor to you then”? It’s different if the admitter tells the patient, “I’m on call for our group tonight, but will be home sleeping tomorrow and my colleague, Dr. Clapton, will take over your care in the morning.” I usually go on to say with a wink that the patient is getting an upgrade, because Dr. Clapton is so much smarter and better-looking than me. I’ll understand if the embellishment doesn’t feel right for you, but I think there is value in the admitter, or a hospitalist rotating off-service, taking a minute to say something nice about the hospitalist who will take over next.
Next month, I will continue to explore issues that are particularly problematic for larger groups. TH
Dr. Nelson has been a practicing hospitalist since 1988 and is co-founder and past president of SHM. He is a principal in Nelson/Flores Associates, a national hospitalist practice management consulting firm. He also is part of the faculty for SHM’s “Best Practices in Managing a Hospital Medicine Program” course. This column represents his views and is not intended to reflect an official position of SHM.
Editor’s note: This is the first of a two-part series addressing large HM group issues.
In the mid-1990s, when I first became interested in how other hospitalist groups were organized, I started surveying by phone all the groups I could find. It was really unusual to find a group larger than four or five full-time equivalent (FTE) hospitalists. Since then, the size of a typical hospitalist group has grown steadily, and data reported in SHM’s “2007-2008 Bi-Annual Survey on the State of Hospital Medicine” shows the median number of FTE physicians in HM groups is 8.0 (mean of 9.75). So in just a few years, our field has grown in such a way that half of all groups in operation now have more than eight physician FTEs. I think most future growth in numbers of hospitalists will be due to individual practices getting larger, rather than new practices starting up.
I work regularly with groups that have more than 20 FTEs, and I have found that large groups tend to have a number of attributes in common.
Separate Daytime Admitter and Rounder Functions
Large groups almost always staff admitter and rounder functions with separate doctors around the clock. That means patients arriving during regular business hours are admitted by a different doctor (the admitter) than the doctor who will provide their care on Day Two and beyond (the rounder).
Although such a system is popular, I suggest every group challenge itself to think about whether it really is the best system. Most groups, regardless of size, have about a quarter to a third of their new admits and consults arrive between 7 a.m. and 5 p.m. If the group did away with a separate admitter during the day and moved all daytime admitters into additional rounder positions, all the daytime admissions could be rotated among all of the daytime doctors, and those patients would typically be seen by the same hospitalist the next day. That would improve hospitalist-patient continuity for the patients who arrive during the day, which might improve the group’s overall efficiency as well as quality and patient satisfaction. Each rounder would become responsible for seeing up to three new consults or admissions during the course of the daytime rounding shift, and the list of new patients to take over each morning—patients admitted by the evening and night admitters—would be smaller.
Of course, one significant benefit of having a separate admitter shift during the day is relieving the rounding doctors of the stress of interrupting rounds for an unpredictable number of new admissions each day. And if the new admissions arrive in the morning, throughput may suffer as it might mean the rounding doctor may see “dischargeable” patients later in the day.
I think there is room for debate about whether it is best for large groups to have a separate admitter during the day, but whatever approach a group chooses, it should acknowledge the costs of that approach and not just assume that it is the only one that is feasible or reasonable.
Who Is Caring for Whom?
The larger the hospitalist group, the more difficulty nurses and other staff have understanding exactly how patients are distributed among the doctors. When one hospitalist rotates “off service” to be replaced by another the next day, or when overnight admissions are “picked up” by a rounding doctor the next morning, it can be difficult for nurses to know which hospitalist is responsible for the patient at a given moment.
All groups, regardless of size, should ensure that the hospitalist who picks up patients from a colleague who has rotated off the day before writes an order in the chart indicating “change attending to Dr. Jones,” or clearly communicates who the new hospitalist is by some other means, such as an electronic medical record or a phone call from a clerk. It isn’t enough that patients are assigned to a particular team—say, the “white team” or the “green team”—for their entire stay. Nurses and other staff need to know which hospitalist is covering that team each day.
One test of how well your system is working is to assess how the nurse answers when a patient or family asks, “Which doctor will be in to see me today?” It isn’t good enough for the nurse to just say, “The green-team doctor will see you, but I don’t know who that is today.” The nurse needs to be able to provide the name of the doctor who will be in. If nurses at your hospital regularly page the wrong hospitalist, or must call around just to figure out who the attending hospitalist is for a particular patient, then you have an opportunity to improve how you communicate this information to the nurse and others.
Even if you have a system in which it is clear to everyone which hospitalist has taken over for one who has rotated off-service, you need to ensure that nurses can easily determine the attending hospitalist for patients admitted the night before. Night-shift staff not knowing which doctor will take over in the morning is an all-too-common problem, and it results in too many staffers not knowing who is caring for the patient from the time the night doctor goes off (e.g., 7 a.m.) until the rounder taking over gets to that patient on rounds. Having evening/night admitters assign attending, or rounder, hospitalists at the time of each admission is a great solution, and I’ll provide ideas about how to do this in next month’s column.
I worry about patient satisfaction if the evening/night admitter can’t tell the patient the name of the hospitalist who will take over in the morning. How can the patient feel that they’re getting personalized care when they’re told, “I don’t know which of my partners will take over your care tomorrow. They all get together and divide up the patients each morning and will assign a doctor to you then”? It’s different if the admitter tells the patient, “I’m on call for our group tonight, but will be home sleeping tomorrow and my colleague, Dr. Clapton, will take over your care in the morning.” I usually go on to say with a wink that the patient is getting an upgrade, because Dr. Clapton is so much smarter and better-looking than me. I’ll understand if the embellishment doesn’t feel right for you, but I think there is value in the admitter, or a hospitalist rotating off-service, taking a minute to say something nice about the hospitalist who will take over next.
Next month, I will continue to explore issues that are particularly problematic for larger groups. TH
Dr. Nelson has been a practicing hospitalist since 1988 and is co-founder and past president of SHM. He is a principal in Nelson/Flores Associates, a national hospitalist practice management consulting firm. He also is part of the faculty for SHM’s “Best Practices in Managing a Hospital Medicine Program” course. This column represents his views and is not intended to reflect an official position of SHM.
Top o’ the Morning
In the what-have-you-done-for-me-lately category, many hospitalists are expected to really ramp up their efforts to improve their hospital’s throughput. So many hospital executives, who not long ago were dazzled by impressive reductions in lengths of stay and cost per case attributable to hospitalists, seem to have turned their attention to discharging patients early in the day. To some hospitalists who still expect gratitude for things done in the past, it seems terribly unfair that administrators now expect us to attend to this new metric. And, by the way, don’t let discharging patients early in the day interfere with improvements in quality metrics, patient satisfaction, and documentation.
Because of these increasing demands on hospitalists, we might feel sorry for ourselves. I do sometimes. But I also know that if we became hospital executives—and some of us have—we would expect the same of hospitalists in our institutions.
I’m struck by how often hospitalists, particularly those not in leadership positions, fail to understand why it matters so much to the execs that discharge orders are written early in the day. For them, I’ll try to provide a brief explanation.
Why It Matters
An increasing number of hospitals are operating with all of their staffed beds fully occupied. Many end up with patients boarding in the ED or ICU because no “regular” beds are available. And hospitals really suffer financially when they have to cancel elective admissions, such as surgeries, because no beds are available for the patient postop.
Hospitals could build more beds to increase their capacity, but that requires a long time and something along the lines of $1 million per bed. Where could they get the financing in today’s market? The other option is to shorten the length of time a patient occupies a bed so that more patients can be served using the existing inventory.
In nearly every hospital, the biggest bed crunch occurs in the afternoon. This is the time patients are ready to leave the post-anesthesia care unit or ED and move to their “floor” bed. If patients being discharged that day haven’t left yet, gridlock occurs. Costs of the gridlock are spread throughout the hospital, notably in the ED, which suffers because of the resulting increased lengths of stay and reduced throughput. This isn’t just an economic issue for the hospital; patients are adversely affected, too.
Even if your hospital has spare beds, early discharge still matters. If the discharge day isn’t managed well and patients routinely leave late in the afternoon, the hospital will have to spend more on evening-shift nursing staff.
It makes sense to look at every step that must occur prior to a patient vacating their room on the day of discharge. The time that the doctor actually writes the discharge order is one of the most critical, rate-limiting steps in the discharge process, so helpful executives suggest we organize our rounds to see the potential discharges first, then get around to seeing the patients who are really sick. I think most hospitalists, including me, find it really difficult to do this. If you’re in this category, you might consider starting your rounds earlier in the day.
Consider Rounding Earlier
Starting rounds earlier is usually an unpopular idea. Many groups refuse to consider it. If you are in a group that works day (rounding) shifts with specified start and stop times, coming in before the start of your shift to begin rounding is just donating uncompensated time to the practice. That is one of many reasons I think it is best for most practices to avoid specified start and stop times for their day shifts. Instead, I think it is reasonable for each doctor to decide when to start and stop work each day depending on the workload. So on days you have a higher-than-usual number of expected discharges or sick patients, you would probably choose to start earlier. And when patient volumes are low, you might choose to start later. The same is true of when you choose to leave for the day. Choosing to start earlier in the day should mean that you can wrap things up earlier on most days.
For a lot of hospitalists, routinely starting rounds earlier would be OK as long as they can finish earlier. But there are some for whom this is really tough or impossible, such as those who need to take their kids to school before work each morning. Rounding early won’t do any good if the hospital doesn’t ensure test results and other information is available early.
A practice could choose to undertake an initiative as simple as the following steps to support improvements in writing most discharge orders early in the day:
- Encourage starting rounds earlier (e.g., 7 a.m.) on most days;
- Whenever possible, prepare discharge summaries the day before;
- As often as possible, write in the order section “probable discharge tomorrow” one day before planned discharges;
- Keep routine morning conferences, such as signout, as short as possible; move it to later in the day, or eliminate it entirely, if feasible; and
- If you have routine, sit-down rounds with case managers each morning, think about whether they get in the way of early-in-the-day discharges. If so, consider moving them to the afternoons, and focus on discussing the next day’s potential discharges rather than discharges for the current day.
Consider establishing targets for each of these metrics and audit performance compared with a historical baseline. For example, the goal might be that the “probable discharge tomorrow” order appears the day before discharge in 50% of hospitalist patients, and the discharge summary is prepared the day before in 30%. These things help ensure other hospital staff members realize discharge is possible or likely and can significantly reduce discharges that are a surprise to nurses and others.
There is nothing magic about the bulleted protocol above. I’m offering it as only one potential idea to improve throughput, and you might want to pursue an entirely different strategy.
The Flip Side
Two closely related issues come up when working on getting discharge orders written early in the day. The first is that some late-afternoon discharges are in reality very early discharges that might have otherwise waited until the next day. It is important to stress that not all discharge orders are written early, and that hospitalists should not hold on to patients who could be discharged late in the day and instead release them the next morning to make their statistics look better.
The other related point is that a declining length of stay and discharging early in the day begin to compete with each other at some point. From a bed management perspective, the theoretical optimal length of stay means discharging patients the moment they are ready and not waiting until the next morning. This means discharging around the clock without regard to the time of day, and that would look terrible when analyzed from the perspective of the portion of discharge orders written early in the day—not to mention it would be very unpleasant for patients asked to leave at night. So I’m not suggesting that we should be discharging patients around the clock, but I just want to point out the tension between length of stay and writing discharge orders early in the day. TH
Dr. Nelson has been a practicing hospitalist since 1988 and is co-founder and past president of SHM. He is a principal in Nelson/Flores Associates, a national hospital practice management consulting firm. He is part of the faculty for SHM’s “Best Practices in Managing a Hospital Medicine Program” course. This column represents his views and is not intended to reflect an official SHM position.
In the what-have-you-done-for-me-lately category, many hospitalists are expected to really ramp up their efforts to improve their hospital’s throughput. So many hospital executives, who not long ago were dazzled by impressive reductions in lengths of stay and cost per case attributable to hospitalists, seem to have turned their attention to discharging patients early in the day. To some hospitalists who still expect gratitude for things done in the past, it seems terribly unfair that administrators now expect us to attend to this new metric. And, by the way, don’t let discharging patients early in the day interfere with improvements in quality metrics, patient satisfaction, and documentation.
Because of these increasing demands on hospitalists, we might feel sorry for ourselves. I do sometimes. But I also know that if we became hospital executives—and some of us have—we would expect the same of hospitalists in our institutions.
I’m struck by how often hospitalists, particularly those not in leadership positions, fail to understand why it matters so much to the execs that discharge orders are written early in the day. For them, I’ll try to provide a brief explanation.
Why It Matters
An increasing number of hospitals are operating with all of their staffed beds fully occupied. Many end up with patients boarding in the ED or ICU because no “regular” beds are available. And hospitals really suffer financially when they have to cancel elective admissions, such as surgeries, because no beds are available for the patient postop.
Hospitals could build more beds to increase their capacity, but that requires a long time and something along the lines of $1 million per bed. Where could they get the financing in today’s market? The other option is to shorten the length of time a patient occupies a bed so that more patients can be served using the existing inventory.
In nearly every hospital, the biggest bed crunch occurs in the afternoon. This is the time patients are ready to leave the post-anesthesia care unit or ED and move to their “floor” bed. If patients being discharged that day haven’t left yet, gridlock occurs. Costs of the gridlock are spread throughout the hospital, notably in the ED, which suffers because of the resulting increased lengths of stay and reduced throughput. This isn’t just an economic issue for the hospital; patients are adversely affected, too.
Even if your hospital has spare beds, early discharge still matters. If the discharge day isn’t managed well and patients routinely leave late in the afternoon, the hospital will have to spend more on evening-shift nursing staff.
It makes sense to look at every step that must occur prior to a patient vacating their room on the day of discharge. The time that the doctor actually writes the discharge order is one of the most critical, rate-limiting steps in the discharge process, so helpful executives suggest we organize our rounds to see the potential discharges first, then get around to seeing the patients who are really sick. I think most hospitalists, including me, find it really difficult to do this. If you’re in this category, you might consider starting your rounds earlier in the day.
Consider Rounding Earlier
Starting rounds earlier is usually an unpopular idea. Many groups refuse to consider it. If you are in a group that works day (rounding) shifts with specified start and stop times, coming in before the start of your shift to begin rounding is just donating uncompensated time to the practice. That is one of many reasons I think it is best for most practices to avoid specified start and stop times for their day shifts. Instead, I think it is reasonable for each doctor to decide when to start and stop work each day depending on the workload. So on days you have a higher-than-usual number of expected discharges or sick patients, you would probably choose to start earlier. And when patient volumes are low, you might choose to start later. The same is true of when you choose to leave for the day. Choosing to start earlier in the day should mean that you can wrap things up earlier on most days.
For a lot of hospitalists, routinely starting rounds earlier would be OK as long as they can finish earlier. But there are some for whom this is really tough or impossible, such as those who need to take their kids to school before work each morning. Rounding early won’t do any good if the hospital doesn’t ensure test results and other information is available early.
A practice could choose to undertake an initiative as simple as the following steps to support improvements in writing most discharge orders early in the day:
- Encourage starting rounds earlier (e.g., 7 a.m.) on most days;
- Whenever possible, prepare discharge summaries the day before;
- As often as possible, write in the order section “probable discharge tomorrow” one day before planned discharges;
- Keep routine morning conferences, such as signout, as short as possible; move it to later in the day, or eliminate it entirely, if feasible; and
- If you have routine, sit-down rounds with case managers each morning, think about whether they get in the way of early-in-the-day discharges. If so, consider moving them to the afternoons, and focus on discussing the next day’s potential discharges rather than discharges for the current day.
Consider establishing targets for each of these metrics and audit performance compared with a historical baseline. For example, the goal might be that the “probable discharge tomorrow” order appears the day before discharge in 50% of hospitalist patients, and the discharge summary is prepared the day before in 30%. These things help ensure other hospital staff members realize discharge is possible or likely and can significantly reduce discharges that are a surprise to nurses and others.
There is nothing magic about the bulleted protocol above. I’m offering it as only one potential idea to improve throughput, and you might want to pursue an entirely different strategy.
The Flip Side
Two closely related issues come up when working on getting discharge orders written early in the day. The first is that some late-afternoon discharges are in reality very early discharges that might have otherwise waited until the next day. It is important to stress that not all discharge orders are written early, and that hospitalists should not hold on to patients who could be discharged late in the day and instead release them the next morning to make their statistics look better.
The other related point is that a declining length of stay and discharging early in the day begin to compete with each other at some point. From a bed management perspective, the theoretical optimal length of stay means discharging patients the moment they are ready and not waiting until the next morning. This means discharging around the clock without regard to the time of day, and that would look terrible when analyzed from the perspective of the portion of discharge orders written early in the day—not to mention it would be very unpleasant for patients asked to leave at night. So I’m not suggesting that we should be discharging patients around the clock, but I just want to point out the tension between length of stay and writing discharge orders early in the day. TH
Dr. Nelson has been a practicing hospitalist since 1988 and is co-founder and past president of SHM. He is a principal in Nelson/Flores Associates, a national hospital practice management consulting firm. He is part of the faculty for SHM’s “Best Practices in Managing a Hospital Medicine Program” course. This column represents his views and is not intended to reflect an official SHM position.
In the what-have-you-done-for-me-lately category, many hospitalists are expected to really ramp up their efforts to improve their hospital’s throughput. So many hospital executives, who not long ago were dazzled by impressive reductions in lengths of stay and cost per case attributable to hospitalists, seem to have turned their attention to discharging patients early in the day. To some hospitalists who still expect gratitude for things done in the past, it seems terribly unfair that administrators now expect us to attend to this new metric. And, by the way, don’t let discharging patients early in the day interfere with improvements in quality metrics, patient satisfaction, and documentation.
Because of these increasing demands on hospitalists, we might feel sorry for ourselves. I do sometimes. But I also know that if we became hospital executives—and some of us have—we would expect the same of hospitalists in our institutions.
I’m struck by how often hospitalists, particularly those not in leadership positions, fail to understand why it matters so much to the execs that discharge orders are written early in the day. For them, I’ll try to provide a brief explanation.
Why It Matters
An increasing number of hospitals are operating with all of their staffed beds fully occupied. Many end up with patients boarding in the ED or ICU because no “regular” beds are available. And hospitals really suffer financially when they have to cancel elective admissions, such as surgeries, because no beds are available for the patient postop.
Hospitals could build more beds to increase their capacity, but that requires a long time and something along the lines of $1 million per bed. Where could they get the financing in today’s market? The other option is to shorten the length of time a patient occupies a bed so that more patients can be served using the existing inventory.
In nearly every hospital, the biggest bed crunch occurs in the afternoon. This is the time patients are ready to leave the post-anesthesia care unit or ED and move to their “floor” bed. If patients being discharged that day haven’t left yet, gridlock occurs. Costs of the gridlock are spread throughout the hospital, notably in the ED, which suffers because of the resulting increased lengths of stay and reduced throughput. This isn’t just an economic issue for the hospital; patients are adversely affected, too.
Even if your hospital has spare beds, early discharge still matters. If the discharge day isn’t managed well and patients routinely leave late in the afternoon, the hospital will have to spend more on evening-shift nursing staff.
It makes sense to look at every step that must occur prior to a patient vacating their room on the day of discharge. The time that the doctor actually writes the discharge order is one of the most critical, rate-limiting steps in the discharge process, so helpful executives suggest we organize our rounds to see the potential discharges first, then get around to seeing the patients who are really sick. I think most hospitalists, including me, find it really difficult to do this. If you’re in this category, you might consider starting your rounds earlier in the day.
Consider Rounding Earlier
Starting rounds earlier is usually an unpopular idea. Many groups refuse to consider it. If you are in a group that works day (rounding) shifts with specified start and stop times, coming in before the start of your shift to begin rounding is just donating uncompensated time to the practice. That is one of many reasons I think it is best for most practices to avoid specified start and stop times for their day shifts. Instead, I think it is reasonable for each doctor to decide when to start and stop work each day depending on the workload. So on days you have a higher-than-usual number of expected discharges or sick patients, you would probably choose to start earlier. And when patient volumes are low, you might choose to start later. The same is true of when you choose to leave for the day. Choosing to start earlier in the day should mean that you can wrap things up earlier on most days.
For a lot of hospitalists, routinely starting rounds earlier would be OK as long as they can finish earlier. But there are some for whom this is really tough or impossible, such as those who need to take their kids to school before work each morning. Rounding early won’t do any good if the hospital doesn’t ensure test results and other information is available early.
A practice could choose to undertake an initiative as simple as the following steps to support improvements in writing most discharge orders early in the day:
- Encourage starting rounds earlier (e.g., 7 a.m.) on most days;
- Whenever possible, prepare discharge summaries the day before;
- As often as possible, write in the order section “probable discharge tomorrow” one day before planned discharges;
- Keep routine morning conferences, such as signout, as short as possible; move it to later in the day, or eliminate it entirely, if feasible; and
- If you have routine, sit-down rounds with case managers each morning, think about whether they get in the way of early-in-the-day discharges. If so, consider moving them to the afternoons, and focus on discussing the next day’s potential discharges rather than discharges for the current day.
Consider establishing targets for each of these metrics and audit performance compared with a historical baseline. For example, the goal might be that the “probable discharge tomorrow” order appears the day before discharge in 50% of hospitalist patients, and the discharge summary is prepared the day before in 30%. These things help ensure other hospital staff members realize discharge is possible or likely and can significantly reduce discharges that are a surprise to nurses and others.
There is nothing magic about the bulleted protocol above. I’m offering it as only one potential idea to improve throughput, and you might want to pursue an entirely different strategy.
The Flip Side
Two closely related issues come up when working on getting discharge orders written early in the day. The first is that some late-afternoon discharges are in reality very early discharges that might have otherwise waited until the next day. It is important to stress that not all discharge orders are written early, and that hospitalists should not hold on to patients who could be discharged late in the day and instead release them the next morning to make their statistics look better.
The other related point is that a declining length of stay and discharging early in the day begin to compete with each other at some point. From a bed management perspective, the theoretical optimal length of stay means discharging patients the moment they are ready and not waiting until the next morning. This means discharging around the clock without regard to the time of day, and that would look terrible when analyzed from the perspective of the portion of discharge orders written early in the day—not to mention it would be very unpleasant for patients asked to leave at night. So I’m not suggesting that we should be discharging patients around the clock, but I just want to point out the tension between length of stay and writing discharge orders early in the day. TH
Dr. Nelson has been a practicing hospitalist since 1988 and is co-founder and past president of SHM. He is a principal in Nelson/Flores Associates, a national hospital practice management consulting firm. He is part of the faculty for SHM’s “Best Practices in Managing a Hospital Medicine Program” course. This column represents his views and is not intended to reflect an official SHM position.
Bonus-Pay Bonanza
Although there is a lot of debate about the effectiveness of pay-for-performance (P4P) plans, I think the plans are only going to increase in the foreseeable future.
We need more research to tell us the relative impact of public reporting of performance data and P4P programs. Most importantly, the details of how these plans are set up, how and what they measure, and the dollar amount involved will have everything to do with whether they are successful in improving the value of care we provide.
SHM’S Practice Management Committee conducted a mini-survey of hospitalist group leaders in 2006. Here are some of the key findings.
P4P Prevalence
Forty-one percent (60 out of 146) of hospital medicine group (HMG) leaders reported their groups have a quality-incentive program. Of those HMG leaders more likely to report participation in a quality-incentive program:
- 60% were at hospitals participating in a P4P program;
- 50% were at multispecialty/PCP medical groups; and
- 50% were in the Southern region.
Of those HMG leaders less likely to report participation in P4P programs, 28% were at academic programs and 31% were at local hospitalist-only groups.
Group vs. Individual Incentives
Of the HMG leaders participating in a quality-incentive program:
- 43% reported it was an individual incentive;
- 35% reported it was a group incentive;
- 10% reported the plan had elements of both individual and group incentives; and
- 12% were not sure if their plans had individual or group incentives.
Basis of Quality Targets
Of the HMG leaders reporting that they participate in a quality-incentive program (respondents could indicate one or more answers):
- 60% of the programs have targets based on national benchmarks;
- 23% have targets based on local or regional benchmarks;
- 37% have targets based on their hospital’s previous experience; and
- 47% have targets based on improvement over a baseline.
Maximum Impact of Incentives
Of the HMG leaders reporting that they participate in a quality-incentive program:
- 16% report the maximum impact is less than 3%;
- 24% report the maximum impact is from 3% to 7%;
- 35% report the maximum impact is from 8% to 10%;
- 17% report the maximum impact is from 11% to 20%;
- 3% report the maximum impact is more than 20%; and
- 5% report they do not know the maximum impact.
Group vs. Individual Incentives
Of the HMG leaders reporting that they participate in a quality-incentive program:
- 61% said they have received an incentive payment;
- 37% have not received an incentive payment; and
- 2% were unsure if they have received an incentive payment.
Quality Metrics
The most common metrics used in P4P programs, based on 29 responses to the SHM survey:
- 93% of HM programs have metrics based on The Joint Commission’s (JCAHO) heart failure measures;
- 86% have metrics based on JCAHO pneumonia measures;
- 79% have metrics based on JCAHO myocardial infarction measures;
- 28% have metrics based on a measure of medication reconciliation;
- 24% have metrics based on avoidance of unapproved abbreviations;
- 24% have metrics based on 100,000 Lives Campaign measures;
- 21% have metrics based on patient satisfaction measures;
- 17% have metrics based on transitions-of-care measures;
- 10% have metrics based on throughput measures;
- 7% have metrics based on end-of-life measures;
- 7% have metrics based on “good citizenship” measures;
- 7% have metrics based on mortality rate measures; and
- 7% have metrics based on readmission rate measures.
The most common metrics used in quality-incentive programs, based on 45 responses to SHM’s survey:
- 73% of programs use JCAHO heart failure measures;
- 73% use “good citizenship” measures;
- 73% use patient satisfaction measures;
- 67% use JCAHO pneumonia measures;
- 51% use transitions-of-care measures;
- 44% use JCAHO M.I. measures;
- 31% use throughput measures;
- 27% use avoidance of unapproved abbreviations;
- 24% use a measure based on medication reconciliation;
- 11% use 100,000 Lives Campaign measures;
- 9% use readmission rate measures;
- 7% use mortality rate measures; and
- 2% use end-of-life measures.
Recommendations
The prevalence of hospitalist quality-based compensation plans is continuing to grow rapidly, but the details of the plans’ structure will govern whether they benefit our patients, improve the overall value of the care we provide, and serve as a meaningful component of our compensation. I suggest each practice consider implementing plans with the following attributes:
A total dollar amount available for performance that is enough to influence hospitalist behavior. I think quality incentives should compose as much as 15% to 20% of a hospitalist’s annual income. Plans connecting quality performance to equal to or less than 7% of annual compensation (the case for 40% of groups in the above survey) rarely are effective.
Money vs. metrics. It usually is better to establish a plan based on a sliding scale of improved performance rather than a single threshold. For example, if all of the bonus money is available for a 10% improvement in performance, consider providing 10% of the total available money for each 1% improvement in performance.
Degree of difficulty. Performance thresholds should be set so that hospitalists need to change their practices to achieve them, but not so far out of reach that hospitalists give up on them. This can get tricky. Many practices set thresholds that are very easy to reach (e.g., they may be near the current level of performance).
Metrics for which trusted data is readily available. In most cases, this means using data already being collected. Avoid hard-to-track metrics, as they are likely to lead to disagreements about their accuracy.
Group vs. individual measures. Most performance metrics can’t be clearly attributed to one hospitalist as compared to another. For example, who gets the credit or blame for Ms. Smith getting or not getting a pneumovax? The majority of performance metrics are best measured and paid on a group basis. Some metrics, such as documenting medicine reconciliation on admission and discharge, can be effectively attributed to a single hospitalist and could be paid on an individual basis.
Small number of metrics, A meaningfully large amount of money should be connected to each one. Don’t make the mistake of having a $10,000 per doctor annual quality bonus pool divided among 20 metrics (each metric would pay a maximum of $500 per year).
Rotating metrics. Consider an annual meeting with members of your hospital’s administration to jointly establish the metrics used in the hospitalist quality incentive for that year. It is reasonable to change the metrics periodically.
It seems to me P4P programs are in their infancy, and will continue to evolve rapidly. Plans that fail to improve outcomes enough to justify the complexity of implementing, tracking, and paying for them will disappear slowly. (I wonder if payment for pneumovax administration during the hospital stay will be in this category.) And new, more effective, and more valuable programs will be developed.
Hospitalist practices will need to be nimble to keep pace with all of this change. Although SHM can alert you to how new P4P initiatives might affect your practice, and even recommend methods to improve your performance, you and your hospitalist colleagues still will have a lot of work to operationalize these programs in your practice. TH
Dr. Nelson has been a practicing hospitalist since 1988 and is co-founder and past president of SHM. He is a principal in Nelson/Flores Associates, a national hospitalist practice management consulting firm. He is part of the faculty for SHM’s “Best Practices in Managing a Hospital Medicine Program” course. This column represents his views and is not intended to reflect an official position of SHM.
Although there is a lot of debate about the effectiveness of pay-for-performance (P4P) plans, I think the plans are only going to increase in the foreseeable future.
We need more research to tell us the relative impact of public reporting of performance data and P4P programs. Most importantly, the details of how these plans are set up, how and what they measure, and the dollar amount involved will have everything to do with whether they are successful in improving the value of care we provide.
SHM’S Practice Management Committee conducted a mini-survey of hospitalist group leaders in 2006. Here are some of the key findings.
P4P Prevalence
Forty-one percent (60 out of 146) of hospital medicine group (HMG) leaders reported their groups have a quality-incentive program. Of those HMG leaders more likely to report participation in a quality-incentive program:
- 60% were at hospitals participating in a P4P program;
- 50% were at multispecialty/PCP medical groups; and
- 50% were in the Southern region.
Of those HMG leaders less likely to report participation in P4P programs, 28% were at academic programs and 31% were at local hospitalist-only groups.
Group vs. Individual Incentives
Of the HMG leaders participating in a quality-incentive program:
- 43% reported it was an individual incentive;
- 35% reported it was a group incentive;
- 10% reported the plan had elements of both individual and group incentives; and
- 12% were not sure if their plans had individual or group incentives.
Basis of Quality Targets
Of the HMG leaders reporting that they participate in a quality-incentive program (respondents could indicate one or more answers):
- 60% of the programs have targets based on national benchmarks;
- 23% have targets based on local or regional benchmarks;
- 37% have targets based on their hospital’s previous experience; and
- 47% have targets based on improvement over a baseline.
Maximum Impact of Incentives
Of the HMG leaders reporting that they participate in a quality-incentive program:
- 16% report the maximum impact is less than 3%;
- 24% report the maximum impact is from 3% to 7%;
- 35% report the maximum impact is from 8% to 10%;
- 17% report the maximum impact is from 11% to 20%;
- 3% report the maximum impact is more than 20%; and
- 5% report they do not know the maximum impact.
Group vs. Individual Incentives
Of the HMG leaders reporting that they participate in a quality-incentive program:
- 61% said they have received an incentive payment;
- 37% have not received an incentive payment; and
- 2% were unsure if they have received an incentive payment.
Quality Metrics
The most common metrics used in P4P programs, based on 29 responses to the SHM survey:
- 93% of HM programs have metrics based on The Joint Commission’s (JCAHO) heart failure measures;
- 86% have metrics based on JCAHO pneumonia measures;
- 79% have metrics based on JCAHO myocardial infarction measures;
- 28% have metrics based on a measure of medication reconciliation;
- 24% have metrics based on avoidance of unapproved abbreviations;
- 24% have metrics based on 100,000 Lives Campaign measures;
- 21% have metrics based on patient satisfaction measures;
- 17% have metrics based on transitions-of-care measures;
- 10% have metrics based on throughput measures;
- 7% have metrics based on end-of-life measures;
- 7% have metrics based on “good citizenship” measures;
- 7% have metrics based on mortality rate measures; and
- 7% have metrics based on readmission rate measures.
The most common metrics used in quality-incentive programs, based on 45 responses to SHM’s survey:
- 73% of programs use JCAHO heart failure measures;
- 73% use “good citizenship” measures;
- 73% use patient satisfaction measures;
- 67% use JCAHO pneumonia measures;
- 51% use transitions-of-care measures;
- 44% use JCAHO M.I. measures;
- 31% use throughput measures;
- 27% use avoidance of unapproved abbreviations;
- 24% use a measure based on medication reconciliation;
- 11% use 100,000 Lives Campaign measures;
- 9% use readmission rate measures;
- 7% use mortality rate measures; and
- 2% use end-of-life measures.
Recommendations
The prevalence of hospitalist quality-based compensation plans is continuing to grow rapidly, but the details of the plans’ structure will govern whether they benefit our patients, improve the overall value of the care we provide, and serve as a meaningful component of our compensation. I suggest each practice consider implementing plans with the following attributes:
A total dollar amount available for performance that is enough to influence hospitalist behavior. I think quality incentives should compose as much as 15% to 20% of a hospitalist’s annual income. Plans connecting quality performance to equal to or less than 7% of annual compensation (the case for 40% of groups in the above survey) rarely are effective.
Money vs. metrics. It usually is better to establish a plan based on a sliding scale of improved performance rather than a single threshold. For example, if all of the bonus money is available for a 10% improvement in performance, consider providing 10% of the total available money for each 1% improvement in performance.
Degree of difficulty. Performance thresholds should be set so that hospitalists need to change their practices to achieve them, but not so far out of reach that hospitalists give up on them. This can get tricky. Many practices set thresholds that are very easy to reach (e.g., they may be near the current level of performance).
Metrics for which trusted data is readily available. In most cases, this means using data already being collected. Avoid hard-to-track metrics, as they are likely to lead to disagreements about their accuracy.
Group vs. individual measures. Most performance metrics can’t be clearly attributed to one hospitalist as compared to another. For example, who gets the credit or blame for Ms. Smith getting or not getting a pneumovax? The majority of performance metrics are best measured and paid on a group basis. Some metrics, such as documenting medicine reconciliation on admission and discharge, can be effectively attributed to a single hospitalist and could be paid on an individual basis.
Small number of metrics, A meaningfully large amount of money should be connected to each one. Don’t make the mistake of having a $10,000 per doctor annual quality bonus pool divided among 20 metrics (each metric would pay a maximum of $500 per year).
Rotating metrics. Consider an annual meeting with members of your hospital’s administration to jointly establish the metrics used in the hospitalist quality incentive for that year. It is reasonable to change the metrics periodically.
It seems to me P4P programs are in their infancy, and will continue to evolve rapidly. Plans that fail to improve outcomes enough to justify the complexity of implementing, tracking, and paying for them will disappear slowly. (I wonder if payment for pneumovax administration during the hospital stay will be in this category.) And new, more effective, and more valuable programs will be developed.
Hospitalist practices will need to be nimble to keep pace with all of this change. Although SHM can alert you to how new P4P initiatives might affect your practice, and even recommend methods to improve your performance, you and your hospitalist colleagues still will have a lot of work to operationalize these programs in your practice. TH
Dr. Nelson has been a practicing hospitalist since 1988 and is co-founder and past president of SHM. He is a principal in Nelson/Flores Associates, a national hospitalist practice management consulting firm. He is part of the faculty for SHM’s “Best Practices in Managing a Hospital Medicine Program” course. This column represents his views and is not intended to reflect an official position of SHM.
Although there is a lot of debate about the effectiveness of pay-for-performance (P4P) plans, I think the plans are only going to increase in the foreseeable future.
We need more research to tell us the relative impact of public reporting of performance data and P4P programs. Most importantly, the details of how these plans are set up, how and what they measure, and the dollar amount involved will have everything to do with whether they are successful in improving the value of care we provide.
SHM’S Practice Management Committee conducted a mini-survey of hospitalist group leaders in 2006. Here are some of the key findings.
P4P Prevalence
Forty-one percent (60 out of 146) of hospital medicine group (HMG) leaders reported their groups have a quality-incentive program. Of those HMG leaders more likely to report participation in a quality-incentive program:
- 60% were at hospitals participating in a P4P program;
- 50% were at multispecialty/PCP medical groups; and
- 50% were in the Southern region.
Of those HMG leaders less likely to report participation in P4P programs, 28% were at academic programs and 31% were at local hospitalist-only groups.
Group vs. Individual Incentives
Of the HMG leaders participating in a quality-incentive program:
- 43% reported it was an individual incentive;
- 35% reported it was a group incentive;
- 10% reported the plan had elements of both individual and group incentives; and
- 12% were not sure if their plans had individual or group incentives.
Basis of Quality Targets
Of the HMG leaders reporting that they participate in a quality-incentive program (respondents could indicate one or more answers):
- 60% of the programs have targets based on national benchmarks;
- 23% have targets based on local or regional benchmarks;
- 37% have targets based on their hospital’s previous experience; and
- 47% have targets based on improvement over a baseline.
Maximum Impact of Incentives
Of the HMG leaders reporting that they participate in a quality-incentive program:
- 16% report the maximum impact is less than 3%;
- 24% report the maximum impact is from 3% to 7%;
- 35% report the maximum impact is from 8% to 10%;
- 17% report the maximum impact is from 11% to 20%;
- 3% report the maximum impact is more than 20%; and
- 5% report they do not know the maximum impact.
Group vs. Individual Incentives
Of the HMG leaders reporting that they participate in a quality-incentive program:
- 61% said they have received an incentive payment;
- 37% have not received an incentive payment; and
- 2% were unsure if they have received an incentive payment.
Quality Metrics
The most common metrics used in P4P programs, based on 29 responses to the SHM survey:
- 93% of HM programs have metrics based on The Joint Commission’s (JCAHO) heart failure measures;
- 86% have metrics based on JCAHO pneumonia measures;
- 79% have metrics based on JCAHO myocardial infarction measures;
- 28% have metrics based on a measure of medication reconciliation;
- 24% have metrics based on avoidance of unapproved abbreviations;
- 24% have metrics based on 100,000 Lives Campaign measures;
- 21% have metrics based on patient satisfaction measures;
- 17% have metrics based on transitions-of-care measures;
- 10% have metrics based on throughput measures;
- 7% have metrics based on end-of-life measures;
- 7% have metrics based on “good citizenship” measures;
- 7% have metrics based on mortality rate measures; and
- 7% have metrics based on readmission rate measures.
The most common metrics used in quality-incentive programs, based on 45 responses to SHM’s survey:
- 73% of programs use JCAHO heart failure measures;
- 73% use “good citizenship” measures;
- 73% use patient satisfaction measures;
- 67% use JCAHO pneumonia measures;
- 51% use transitions-of-care measures;
- 44% use JCAHO M.I. measures;
- 31% use throughput measures;
- 27% use avoidance of unapproved abbreviations;
- 24% use a measure based on medication reconciliation;
- 11% use 100,000 Lives Campaign measures;
- 9% use readmission rate measures;
- 7% use mortality rate measures; and
- 2% use end-of-life measures.
Recommendations
The prevalence of hospitalist quality-based compensation plans is continuing to grow rapidly, but the details of the plans’ structure will govern whether they benefit our patients, improve the overall value of the care we provide, and serve as a meaningful component of our compensation. I suggest each practice consider implementing plans with the following attributes:
A total dollar amount available for performance that is enough to influence hospitalist behavior. I think quality incentives should compose as much as 15% to 20% of a hospitalist’s annual income. Plans connecting quality performance to equal to or less than 7% of annual compensation (the case for 40% of groups in the above survey) rarely are effective.
Money vs. metrics. It usually is better to establish a plan based on a sliding scale of improved performance rather than a single threshold. For example, if all of the bonus money is available for a 10% improvement in performance, consider providing 10% of the total available money for each 1% improvement in performance.
Degree of difficulty. Performance thresholds should be set so that hospitalists need to change their practices to achieve them, but not so far out of reach that hospitalists give up on them. This can get tricky. Many practices set thresholds that are very easy to reach (e.g., they may be near the current level of performance).
Metrics for which trusted data is readily available. In most cases, this means using data already being collected. Avoid hard-to-track metrics, as they are likely to lead to disagreements about their accuracy.
Group vs. individual measures. Most performance metrics can’t be clearly attributed to one hospitalist as compared to another. For example, who gets the credit or blame for Ms. Smith getting or not getting a pneumovax? The majority of performance metrics are best measured and paid on a group basis. Some metrics, such as documenting medicine reconciliation on admission and discharge, can be effectively attributed to a single hospitalist and could be paid on an individual basis.
Small number of metrics, A meaningfully large amount of money should be connected to each one. Don’t make the mistake of having a $10,000 per doctor annual quality bonus pool divided among 20 metrics (each metric would pay a maximum of $500 per year).
Rotating metrics. Consider an annual meeting with members of your hospital’s administration to jointly establish the metrics used in the hospitalist quality incentive for that year. It is reasonable to change the metrics periodically.
It seems to me P4P programs are in their infancy, and will continue to evolve rapidly. Plans that fail to improve outcomes enough to justify the complexity of implementing, tracking, and paying for them will disappear slowly. (I wonder if payment for pneumovax administration during the hospital stay will be in this category.) And new, more effective, and more valuable programs will be developed.
Hospitalist practices will need to be nimble to keep pace with all of this change. Although SHM can alert you to how new P4P initiatives might affect your practice, and even recommend methods to improve your performance, you and your hospitalist colleagues still will have a lot of work to operationalize these programs in your practice. TH
Dr. Nelson has been a practicing hospitalist since 1988 and is co-founder and past president of SHM. He is a principal in Nelson/Flores Associates, a national hospitalist practice management consulting firm. He is part of the faculty for SHM’s “Best Practices in Managing a Hospital Medicine Program” course. This column represents his views and is not intended to reflect an official position of SHM.
Staffing Strategies
One of the most difficult challenges in staffing a hospitalist practice is handling the unpredictable daily fluctuations in patient volume. It isn’t difficult to decide how many hospitalists will work each day to handle the average number of daily visits (aka encounters), but the actual number of visits on any given day is almost always significantly different than the average. I think many groups could more effectively handle day-to-day variations in workload by eliminating predetermined lengths of the shifts that the doctors work. It isn’t a perfect strategy, but it is worth some consideration by nearly any practice. Let me explain.
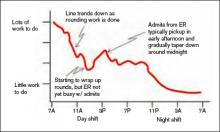
First, think about how the workload for a typical day might be represented. For many or most practices it often looks something like the wavy line in Figure 1. (See Figure 1, p. 52.)
Of course, the line representing a day’s work will be different every day, but I’ve tried to draw it in a way that represents a typical day.
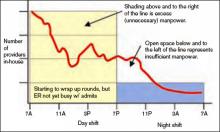
In Figure 2 (see p. 52), I’ve added horizontal bars to represent a common way that groups might schedule four daytime doctors who each work 7 a.m. to 7 p.m., and one night doctor working 7 p.m. to 7 a.m. The four horizontal bars represent the four day doctors, and the one horizontal bar at the bottom right represents the one night doctor. Ideally, the manpower (horizontal bars) should match the workload (wavy line) every hour of the day.
This graph shows that—at least for this particular day—there are many hours in the afternoon when there is excess manpower. The doctors may be sitting around waiting for their shift to end or waiting to see if it will suddenly get busy again. We all know that happens unpredictably. And from about 7 p.m. to about 11:30 p.m., the single night doctor has more work than he/she can reasonably handle.
In fact, there probably isn’t ever a day when the work that needs to be done is just the right amount for all four doctors from 7 a.m. to 7 p.m. with a sudden drop at 7 p.m. that is just right for one doctor for the next 12 hours. Because the doctors have scheduled themselves to work 12-hour shifts, they know in advance that their manpower will quite regularly fail to match the workload for that day.
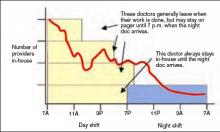
Groups have devised a number of strategies to try to get manpower to more closely match the unpredictable workload for a given day. These include having a member of the group available on standby (often called “jeopardy”) for that day; this physician comes in only if it is unusually busy. Some groups have a patient volume cap to prevent the practice from becoming too busy. I think a cap is a poor strategy that should be used only as a last resort, and I will discuss this in detail in a future column. Other groups have a swing shift from late in the afternoon until around 11 p.m. or so to help with evening admits and cross cover. And an often overlooked but potentially valuable strategy is to eliminate clearly specified start and stop times for the shifts that the doctors work. For an idea of what that might look like, see Figure 3 (p. 52).
Notice that the right-hand side of each yellow bar in Figures 2 and 3 is indistinct. That is meant to show that the precise time that the doctor leaves varies, depending on the day’s workload. That way the manpower can be adjusted from one day to the next to more closely match the workload than if the doctors work fixed shifts of a specified duration. On some days, all of the doctors may stay 12 hours or more, but on many days at least some of the doctors will end up leaving in less than 12 hours. If all day doctors work a 12-hour shift, they have provided 48 hours—four doctors at 12 hours each—of physician manpower, but if there is some flexibility about when the doctors leave, the same four day doctors could provide between about 34 and 52 hours of manpower, depending on the day’s workload.
If your practice is contracted to keep a doctor in the hospital around the clock, you will probably need the night doctor and at least one day doctor to stay around—even if it is a slow day. But the other doctors might be able to leave when their work is done. And it is also reasonable for some groups to eliminate precise times that the doctors start working in the morning each day, though they might be required to be available by pager by a specified time in the morning.
One common concern about such a system is how to handle issues that arise with the patients cared for by a doctor who has left. I think it is best for the doctor to stay available by pager and handle simple issues by phone. For more complicated issues (e.g., a patient who needs attention at the bedside) the doctor could either come back to the hospital or phone another member of the practice (e.g., the doctor required to stay at least 12 hours that day) and see if he or she can handle the emergency.
All of the specifics of a system that allows doctors to leave when their work is done rather than according to shifts of a predetermined number of hours would be too long for this column. But they aren’t complicated, and given the variability that exists in the number of daily patient visits to any hospitalist practice, the application of this kind of approach is well worth considering. TH
Dr. Nelson has been a practicing hospitalist since 1988 and is a co-founder and past-president of SHM. He is a principal in Nelson/Flores Associates, a national hospitalist practice management consulting firm. This column represents his views and is not intended to reflect an official position of SHM.
One of the most difficult challenges in staffing a hospitalist practice is handling the unpredictable daily fluctuations in patient volume. It isn’t difficult to decide how many hospitalists will work each day to handle the average number of daily visits (aka encounters), but the actual number of visits on any given day is almost always significantly different than the average. I think many groups could more effectively handle day-to-day variations in workload by eliminating predetermined lengths of the shifts that the doctors work. It isn’t a perfect strategy, but it is worth some consideration by nearly any practice. Let me explain.
First, think about how the workload for a typical day might be represented. For many or most practices it often looks something like the wavy line in Figure 1. (See Figure 1, p. 52.)
Of course, the line representing a day’s work will be different every day, but I’ve tried to draw it in a way that represents a typical day.
In Figure 2 (see p. 52), I’ve added horizontal bars to represent a common way that groups might schedule four daytime doctors who each work 7 a.m. to 7 p.m., and one night doctor working 7 p.m. to 7 a.m. The four horizontal bars represent the four day doctors, and the one horizontal bar at the bottom right represents the one night doctor. Ideally, the manpower (horizontal bars) should match the workload (wavy line) every hour of the day.
This graph shows that—at least for this particular day—there are many hours in the afternoon when there is excess manpower. The doctors may be sitting around waiting for their shift to end or waiting to see if it will suddenly get busy again. We all know that happens unpredictably. And from about 7 p.m. to about 11:30 p.m., the single night doctor has more work than he/she can reasonably handle.
In fact, there probably isn’t ever a day when the work that needs to be done is just the right amount for all four doctors from 7 a.m. to 7 p.m. with a sudden drop at 7 p.m. that is just right for one doctor for the next 12 hours. Because the doctors have scheduled themselves to work 12-hour shifts, they know in advance that their manpower will quite regularly fail to match the workload for that day.
Groups have devised a number of strategies to try to get manpower to more closely match the unpredictable workload for a given day. These include having a member of the group available on standby (often called “jeopardy”) for that day; this physician comes in only if it is unusually busy. Some groups have a patient volume cap to prevent the practice from becoming too busy. I think a cap is a poor strategy that should be used only as a last resort, and I will discuss this in detail in a future column. Other groups have a swing shift from late in the afternoon until around 11 p.m. or so to help with evening admits and cross cover. And an often overlooked but potentially valuable strategy is to eliminate clearly specified start and stop times for the shifts that the doctors work. For an idea of what that might look like, see Figure 3 (p. 52).
Notice that the right-hand side of each yellow bar in Figures 2 and 3 is indistinct. That is meant to show that the precise time that the doctor leaves varies, depending on the day’s workload. That way the manpower can be adjusted from one day to the next to more closely match the workload than if the doctors work fixed shifts of a specified duration. On some days, all of the doctors may stay 12 hours or more, but on many days at least some of the doctors will end up leaving in less than 12 hours. If all day doctors work a 12-hour shift, they have provided 48 hours—four doctors at 12 hours each—of physician manpower, but if there is some flexibility about when the doctors leave, the same four day doctors could provide between about 34 and 52 hours of manpower, depending on the day’s workload.
If your practice is contracted to keep a doctor in the hospital around the clock, you will probably need the night doctor and at least one day doctor to stay around—even if it is a slow day. But the other doctors might be able to leave when their work is done. And it is also reasonable for some groups to eliminate precise times that the doctors start working in the morning each day, though they might be required to be available by pager by a specified time in the morning.
One common concern about such a system is how to handle issues that arise with the patients cared for by a doctor who has left. I think it is best for the doctor to stay available by pager and handle simple issues by phone. For more complicated issues (e.g., a patient who needs attention at the bedside) the doctor could either come back to the hospital or phone another member of the practice (e.g., the doctor required to stay at least 12 hours that day) and see if he or she can handle the emergency.
All of the specifics of a system that allows doctors to leave when their work is done rather than according to shifts of a predetermined number of hours would be too long for this column. But they aren’t complicated, and given the variability that exists in the number of daily patient visits to any hospitalist practice, the application of this kind of approach is well worth considering. TH
Dr. Nelson has been a practicing hospitalist since 1988 and is a co-founder and past-president of SHM. He is a principal in Nelson/Flores Associates, a national hospitalist practice management consulting firm. This column represents his views and is not intended to reflect an official position of SHM.
One of the most difficult challenges in staffing a hospitalist practice is handling the unpredictable daily fluctuations in patient volume. It isn’t difficult to decide how many hospitalists will work each day to handle the average number of daily visits (aka encounters), but the actual number of visits on any given day is almost always significantly different than the average. I think many groups could more effectively handle day-to-day variations in workload by eliminating predetermined lengths of the shifts that the doctors work. It isn’t a perfect strategy, but it is worth some consideration by nearly any practice. Let me explain.
First, think about how the workload for a typical day might be represented. For many or most practices it often looks something like the wavy line in Figure 1. (See Figure 1, p. 52.)
Of course, the line representing a day’s work will be different every day, but I’ve tried to draw it in a way that represents a typical day.
In Figure 2 (see p. 52), I’ve added horizontal bars to represent a common way that groups might schedule four daytime doctors who each work 7 a.m. to 7 p.m., and one night doctor working 7 p.m. to 7 a.m. The four horizontal bars represent the four day doctors, and the one horizontal bar at the bottom right represents the one night doctor. Ideally, the manpower (horizontal bars) should match the workload (wavy line) every hour of the day.
This graph shows that—at least for this particular day—there are many hours in the afternoon when there is excess manpower. The doctors may be sitting around waiting for their shift to end or waiting to see if it will suddenly get busy again. We all know that happens unpredictably. And from about 7 p.m. to about 11:30 p.m., the single night doctor has more work than he/she can reasonably handle.
In fact, there probably isn’t ever a day when the work that needs to be done is just the right amount for all four doctors from 7 a.m. to 7 p.m. with a sudden drop at 7 p.m. that is just right for one doctor for the next 12 hours. Because the doctors have scheduled themselves to work 12-hour shifts, they know in advance that their manpower will quite regularly fail to match the workload for that day.
Groups have devised a number of strategies to try to get manpower to more closely match the unpredictable workload for a given day. These include having a member of the group available on standby (often called “jeopardy”) for that day; this physician comes in only if it is unusually busy. Some groups have a patient volume cap to prevent the practice from becoming too busy. I think a cap is a poor strategy that should be used only as a last resort, and I will discuss this in detail in a future column. Other groups have a swing shift from late in the afternoon until around 11 p.m. or so to help with evening admits and cross cover. And an often overlooked but potentially valuable strategy is to eliminate clearly specified start and stop times for the shifts that the doctors work. For an idea of what that might look like, see Figure 3 (p. 52).
Notice that the right-hand side of each yellow bar in Figures 2 and 3 is indistinct. That is meant to show that the precise time that the doctor leaves varies, depending on the day’s workload. That way the manpower can be adjusted from one day to the next to more closely match the workload than if the doctors work fixed shifts of a specified duration. On some days, all of the doctors may stay 12 hours or more, but on many days at least some of the doctors will end up leaving in less than 12 hours. If all day doctors work a 12-hour shift, they have provided 48 hours—four doctors at 12 hours each—of physician manpower, but if there is some flexibility about when the doctors leave, the same four day doctors could provide between about 34 and 52 hours of manpower, depending on the day’s workload.
If your practice is contracted to keep a doctor in the hospital around the clock, you will probably need the night doctor and at least one day doctor to stay around—even if it is a slow day. But the other doctors might be able to leave when their work is done. And it is also reasonable for some groups to eliminate precise times that the doctors start working in the morning each day, though they might be required to be available by pager by a specified time in the morning.
One common concern about such a system is how to handle issues that arise with the patients cared for by a doctor who has left. I think it is best for the doctor to stay available by pager and handle simple issues by phone. For more complicated issues (e.g., a patient who needs attention at the bedside) the doctor could either come back to the hospital or phone another member of the practice (e.g., the doctor required to stay at least 12 hours that day) and see if he or she can handle the emergency.
All of the specifics of a system that allows doctors to leave when their work is done rather than according to shifts of a predetermined number of hours would be too long for this column. But they aren’t complicated, and given the variability that exists in the number of daily patient visits to any hospitalist practice, the application of this kind of approach is well worth considering. TH
Dr. Nelson has been a practicing hospitalist since 1988 and is a co-founder and past-president of SHM. He is a principal in Nelson/Flores Associates, a national hospitalist practice management consulting firm. This column represents his views and is not intended to reflect an official position of SHM.
Satisfaction Scorecard
Patient satisfaction became a much more important issue earlier in 2008 when hospitals began reporting their performance on the Hospital Consumer Assessment of Healthcare Providers and Systems (HCAHPS) survey. The 18-item survey was developed by the Centers for Medicare and Medicaid Services (CMS) and the Agency for Healthcare Research and Quality, and is completed by patients to record their level of satisfaction with the hospital and the care they received.
If you don’t know your hospital’s publicly reported HCAHPS scores, you should make it your business to become familiar with them. Survey results from participating hospitals are updated periodically and available at www.hospitalcompare.hhs.gov.
I regularly hear hospitalists say they could more effectively direct their energy and resources in ways consistent with their hospital CEO’s goals, if they only knew what those goals were. If you find yourself in the same category, then you should know there is a really good chance the upper-level hospital leadership has a salary bonus in place for achieving certain patient safety and satisfaction goals. A recent survey in the Journal of Patient Safety showed this is the case for more than half of the nation’s hospital executives.1 Therefore, learning more about your hospital’s patient satisfaction scores, and your group’s contribution to the score, is worth the effort.
The publicly reported HCAHPS data does not address hospitalists’ effect on patient satisfaction separately from other doctors and hospital attributes. As a result, some hospitalist groups conduct their own survey. This may range from a very brief series of written questions, or a more-involved survey administered via phone. Since it is difficult to drill down to patient satisfaction with individual hospitalists, data from these surveys often times are collected for the entire hospitalist practice in aggregate, rather than by the individual doctor.
Incorporate Information
Investigate both internal and external resources, if you believe your group could benefit from an intervention (e.g., education or training to improve patient satisfaction). Many hospitals have someone on staff to provide employee training in this area; the trainer probably would be impressed and pleased if you initiate contact to learn more about available training. Resources external to your hospital include survey companies (e.g., Press Ganey, NCR Picker, among others). These companies can provide training and guidance, or put you in contact with firms with whom they work. I have seen something as simple as a one- or two-hour online or DVD course be a valuable tool for some practices.
I know some very efficient hospitalists who maintain incredibly high levels of patient satisfaction despite very high workloads. I think these doctors probably are outliers, and most of us will see satisfaction scores decline as workloads become unreasonably high. Each group should challenge itself continually to find the optimal point between patient volume and important outcomes like patient satisfaction.
Here are some strategies hospitalist groups could use to improve patient satisfaction:
- Call patients after discharge. This is a potent way to improve patient satisfaction. It is a valuable clinical encounter, since it offers a chance to reinforce discharge instructions (e.g, the value of smoking cessation, or the need to have ongoing INR monitoring), and to address any issues arising in the interim. The calls are most effective if done by the doctor who discharged the patient, but can be of some value if made by a nurse or other person connected to the practice. Note, it is best not to inform patients you will be making this call, since it will reduce the surprise and pleasure when the call comes, and could lead to frustration if a patient never gets the call they were told to expect.
- Provide referring doctors, emergency room doctors, and nurses at the hospital with a “script” to use when introducing or describing the hospitalist practice to patients. Without coaching, most of these people likely will say to the patient something like “your doctor [primary care physician] doesn’t come to the hospital anymore, so the hospitalist will see you.” Such a description may make the patient feel like they’re getting a second-class doctor. Instead, encourage these workers to say something like “Your doctor has decided to focus her practice on the office, to be more available to you there. As a result, she has decided to refer you to Dr. McCartney, a doctor who specializes in the care of hospitalized patients with problems like yours. Dr. McCartney will communicate with your primary doctor, and you should plan to follow up with her when you are discharged.”
- Communicate regularly, even daily, with family members of patients who have dementia or other cognitive impairment. This usually means calling the family.
- During initial and subsequent visits with a patient, shake hands or gently touch the patient in some way. Sit down and, while still sitting, conclude the conversation by asking if the patient has any questions and asking “Is there anything special I can do for you today?”
- Provide patients with a copy of their discharge summary. It can serve as a valuable education tool for the patient, their loved ones, visiting nurses, etc. Ideally, the summary should be transcribed on a stat basis, so it can be available for the nurse to give to the patient on the way out of the hospital. Alternatively, it could be mailed to the patient later.
- Track your ongoing satisfaction performance by regularly including available data from HCAHPS and/or other sources in the practice dashboard or report card.
- Ensure patients and their families are provided a copy of your group’s brochure. Brochures delivered to primary care offices rarely find their way into the hands of the patients, and often times are forgotten or misplaced by the time hospital care is needed. It usually is more effective to ensure hospital staff provides the brochure. This could be done via a standing protocol stating that a clerical person will provide all patients with a hospitalist as attending or consultant will get a copy. Or, ensure an order to this effect is written on every one of your patients. It’s best to do this via pre-printed order sets.
If you don’t have a group brochure, develop one. It should include the name of the group with a one- or two-line biography and photograph for each hospitalist (e.g., where they attended medical school and residency), and other key information about the practice. If you’d like a sample brochure, visit www.hospitalmedicine.org and search “sample brochure for hospitalist program.”
Each hospitalist in your group could carry business cards with the doctor’s picture next to their name and key info. One small study showed this enhanced patients’ ability to correctly identify their hospitalist and presumably increased their satisfaction, as well.
- Maximize hospitalist-patient continuity. Each group should adjust their work schedule to maximize continuity between patient and hospitalist while still providing a sustainable lifestyle. TH
Dr. Nelson has been a practicing hospitalist since 1988 and is co-founder and past president of SHM. He is a principal in Nelson/Flores Associates, a national hospitalist practice management consulting firm. He is part of the faculty for SHM’s “Best Practices in Managing a Hospital Medicine Program” course. This column represents his views and is not intended to reflect an official SHM position..
Reference
1. Vaughn T, Koepke M, Kroch E, et al. Engagement of leadership in quality improvement initiatives: executive quality improvement survey results. J Patient Saf. 2006;2(1):2-9.
Patient satisfaction became a much more important issue earlier in 2008 when hospitals began reporting their performance on the Hospital Consumer Assessment of Healthcare Providers and Systems (HCAHPS) survey. The 18-item survey was developed by the Centers for Medicare and Medicaid Services (CMS) and the Agency for Healthcare Research and Quality, and is completed by patients to record their level of satisfaction with the hospital and the care they received.
If you don’t know your hospital’s publicly reported HCAHPS scores, you should make it your business to become familiar with them. Survey results from participating hospitals are updated periodically and available at www.hospitalcompare.hhs.gov.
I regularly hear hospitalists say they could more effectively direct their energy and resources in ways consistent with their hospital CEO’s goals, if they only knew what those goals were. If you find yourself in the same category, then you should know there is a really good chance the upper-level hospital leadership has a salary bonus in place for achieving certain patient safety and satisfaction goals. A recent survey in the Journal of Patient Safety showed this is the case for more than half of the nation’s hospital executives.1 Therefore, learning more about your hospital’s patient satisfaction scores, and your group’s contribution to the score, is worth the effort.
The publicly reported HCAHPS data does not address hospitalists’ effect on patient satisfaction separately from other doctors and hospital attributes. As a result, some hospitalist groups conduct their own survey. This may range from a very brief series of written questions, or a more-involved survey administered via phone. Since it is difficult to drill down to patient satisfaction with individual hospitalists, data from these surveys often times are collected for the entire hospitalist practice in aggregate, rather than by the individual doctor.
Incorporate Information
Investigate both internal and external resources, if you believe your group could benefit from an intervention (e.g., education or training to improve patient satisfaction). Many hospitals have someone on staff to provide employee training in this area; the trainer probably would be impressed and pleased if you initiate contact to learn more about available training. Resources external to your hospital include survey companies (e.g., Press Ganey, NCR Picker, among others). These companies can provide training and guidance, or put you in contact with firms with whom they work. I have seen something as simple as a one- or two-hour online or DVD course be a valuable tool for some practices.
I know some very efficient hospitalists who maintain incredibly high levels of patient satisfaction despite very high workloads. I think these doctors probably are outliers, and most of us will see satisfaction scores decline as workloads become unreasonably high. Each group should challenge itself continually to find the optimal point between patient volume and important outcomes like patient satisfaction.
Here are some strategies hospitalist groups could use to improve patient satisfaction:
- Call patients after discharge. This is a potent way to improve patient satisfaction. It is a valuable clinical encounter, since it offers a chance to reinforce discharge instructions (e.g, the value of smoking cessation, or the need to have ongoing INR monitoring), and to address any issues arising in the interim. The calls are most effective if done by the doctor who discharged the patient, but can be of some value if made by a nurse or other person connected to the practice. Note, it is best not to inform patients you will be making this call, since it will reduce the surprise and pleasure when the call comes, and could lead to frustration if a patient never gets the call they were told to expect.
- Provide referring doctors, emergency room doctors, and nurses at the hospital with a “script” to use when introducing or describing the hospitalist practice to patients. Without coaching, most of these people likely will say to the patient something like “your doctor [primary care physician] doesn’t come to the hospital anymore, so the hospitalist will see you.” Such a description may make the patient feel like they’re getting a second-class doctor. Instead, encourage these workers to say something like “Your doctor has decided to focus her practice on the office, to be more available to you there. As a result, she has decided to refer you to Dr. McCartney, a doctor who specializes in the care of hospitalized patients with problems like yours. Dr. McCartney will communicate with your primary doctor, and you should plan to follow up with her when you are discharged.”
- Communicate regularly, even daily, with family members of patients who have dementia or other cognitive impairment. This usually means calling the family.
- During initial and subsequent visits with a patient, shake hands or gently touch the patient in some way. Sit down and, while still sitting, conclude the conversation by asking if the patient has any questions and asking “Is there anything special I can do for you today?”
- Provide patients with a copy of their discharge summary. It can serve as a valuable education tool for the patient, their loved ones, visiting nurses, etc. Ideally, the summary should be transcribed on a stat basis, so it can be available for the nurse to give to the patient on the way out of the hospital. Alternatively, it could be mailed to the patient later.
- Track your ongoing satisfaction performance by regularly including available data from HCAHPS and/or other sources in the practice dashboard or report card.
- Ensure patients and their families are provided a copy of your group’s brochure. Brochures delivered to primary care offices rarely find their way into the hands of the patients, and often times are forgotten or misplaced by the time hospital care is needed. It usually is more effective to ensure hospital staff provides the brochure. This could be done via a standing protocol stating that a clerical person will provide all patients with a hospitalist as attending or consultant will get a copy. Or, ensure an order to this effect is written on every one of your patients. It’s best to do this via pre-printed order sets.
If you don’t have a group brochure, develop one. It should include the name of the group with a one- or two-line biography and photograph for each hospitalist (e.g., where they attended medical school and residency), and other key information about the practice. If you’d like a sample brochure, visit www.hospitalmedicine.org and search “sample brochure for hospitalist program.”
Each hospitalist in your group could carry business cards with the doctor’s picture next to their name and key info. One small study showed this enhanced patients’ ability to correctly identify their hospitalist and presumably increased their satisfaction, as well.
- Maximize hospitalist-patient continuity. Each group should adjust their work schedule to maximize continuity between patient and hospitalist while still providing a sustainable lifestyle. TH
Dr. Nelson has been a practicing hospitalist since 1988 and is co-founder and past president of SHM. He is a principal in Nelson/Flores Associates, a national hospitalist practice management consulting firm. He is part of the faculty for SHM’s “Best Practices in Managing a Hospital Medicine Program” course. This column represents his views and is not intended to reflect an official SHM position..
Reference
1. Vaughn T, Koepke M, Kroch E, et al. Engagement of leadership in quality improvement initiatives: executive quality improvement survey results. J Patient Saf. 2006;2(1):2-9.
Patient satisfaction became a much more important issue earlier in 2008 when hospitals began reporting their performance on the Hospital Consumer Assessment of Healthcare Providers and Systems (HCAHPS) survey. The 18-item survey was developed by the Centers for Medicare and Medicaid Services (CMS) and the Agency for Healthcare Research and Quality, and is completed by patients to record their level of satisfaction with the hospital and the care they received.
If you don’t know your hospital’s publicly reported HCAHPS scores, you should make it your business to become familiar with them. Survey results from participating hospitals are updated periodically and available at www.hospitalcompare.hhs.gov.
I regularly hear hospitalists say they could more effectively direct their energy and resources in ways consistent with their hospital CEO’s goals, if they only knew what those goals were. If you find yourself in the same category, then you should know there is a really good chance the upper-level hospital leadership has a salary bonus in place for achieving certain patient safety and satisfaction goals. A recent survey in the Journal of Patient Safety showed this is the case for more than half of the nation’s hospital executives.1 Therefore, learning more about your hospital’s patient satisfaction scores, and your group’s contribution to the score, is worth the effort.
The publicly reported HCAHPS data does not address hospitalists’ effect on patient satisfaction separately from other doctors and hospital attributes. As a result, some hospitalist groups conduct their own survey. This may range from a very brief series of written questions, or a more-involved survey administered via phone. Since it is difficult to drill down to patient satisfaction with individual hospitalists, data from these surveys often times are collected for the entire hospitalist practice in aggregate, rather than by the individual doctor.
Incorporate Information
Investigate both internal and external resources, if you believe your group could benefit from an intervention (e.g., education or training to improve patient satisfaction). Many hospitals have someone on staff to provide employee training in this area; the trainer probably would be impressed and pleased if you initiate contact to learn more about available training. Resources external to your hospital include survey companies (e.g., Press Ganey, NCR Picker, among others). These companies can provide training and guidance, or put you in contact with firms with whom they work. I have seen something as simple as a one- or two-hour online or DVD course be a valuable tool for some practices.
I know some very efficient hospitalists who maintain incredibly high levels of patient satisfaction despite very high workloads. I think these doctors probably are outliers, and most of us will see satisfaction scores decline as workloads become unreasonably high. Each group should challenge itself continually to find the optimal point between patient volume and important outcomes like patient satisfaction.
Here are some strategies hospitalist groups could use to improve patient satisfaction:
- Call patients after discharge. This is a potent way to improve patient satisfaction. It is a valuable clinical encounter, since it offers a chance to reinforce discharge instructions (e.g, the value of smoking cessation, or the need to have ongoing INR monitoring), and to address any issues arising in the interim. The calls are most effective if done by the doctor who discharged the patient, but can be of some value if made by a nurse or other person connected to the practice. Note, it is best not to inform patients you will be making this call, since it will reduce the surprise and pleasure when the call comes, and could lead to frustration if a patient never gets the call they were told to expect.
- Provide referring doctors, emergency room doctors, and nurses at the hospital with a “script” to use when introducing or describing the hospitalist practice to patients. Without coaching, most of these people likely will say to the patient something like “your doctor [primary care physician] doesn’t come to the hospital anymore, so the hospitalist will see you.” Such a description may make the patient feel like they’re getting a second-class doctor. Instead, encourage these workers to say something like “Your doctor has decided to focus her practice on the office, to be more available to you there. As a result, she has decided to refer you to Dr. McCartney, a doctor who specializes in the care of hospitalized patients with problems like yours. Dr. McCartney will communicate with your primary doctor, and you should plan to follow up with her when you are discharged.”
- Communicate regularly, even daily, with family members of patients who have dementia or other cognitive impairment. This usually means calling the family.
- During initial and subsequent visits with a patient, shake hands or gently touch the patient in some way. Sit down and, while still sitting, conclude the conversation by asking if the patient has any questions and asking “Is there anything special I can do for you today?”
- Provide patients with a copy of their discharge summary. It can serve as a valuable education tool for the patient, their loved ones, visiting nurses, etc. Ideally, the summary should be transcribed on a stat basis, so it can be available for the nurse to give to the patient on the way out of the hospital. Alternatively, it could be mailed to the patient later.
- Track your ongoing satisfaction performance by regularly including available data from HCAHPS and/or other sources in the practice dashboard or report card.
- Ensure patients and their families are provided a copy of your group’s brochure. Brochures delivered to primary care offices rarely find their way into the hands of the patients, and often times are forgotten or misplaced by the time hospital care is needed. It usually is more effective to ensure hospital staff provides the brochure. This could be done via a standing protocol stating that a clerical person will provide all patients with a hospitalist as attending or consultant will get a copy. Or, ensure an order to this effect is written on every one of your patients. It’s best to do this via pre-printed order sets.
If you don’t have a group brochure, develop one. It should include the name of the group with a one- or two-line biography and photograph for each hospitalist (e.g., where they attended medical school and residency), and other key information about the practice. If you’d like a sample brochure, visit www.hospitalmedicine.org and search “sample brochure for hospitalist program.”
Each hospitalist in your group could carry business cards with the doctor’s picture next to their name and key info. One small study showed this enhanced patients’ ability to correctly identify their hospitalist and presumably increased their satisfaction, as well.
- Maximize hospitalist-patient continuity. Each group should adjust their work schedule to maximize continuity between patient and hospitalist while still providing a sustainable lifestyle. TH
Dr. Nelson has been a practicing hospitalist since 1988 and is co-founder and past president of SHM. He is a principal in Nelson/Flores Associates, a national hospitalist practice management consulting firm. He is part of the faculty for SHM’s “Best Practices in Managing a Hospital Medicine Program” course. This column represents his views and is not intended to reflect an official SHM position..
Reference
1. Vaughn T, Koepke M, Kroch E, et al. Engagement of leadership in quality improvement initiatives: executive quality improvement survey results. J Patient Saf. 2006;2(1):2-9.
Technological Advance or Workplace Setback?
Last month I discussed my concern regarding how often hospitalists are interrupted. In fact, I suspect frequent interruptions to our train of thought and workflow might lead to as many problems and errors as the sleep deprivation associated with long on-call shifts.
Every hospitalist group should think carefully about the effect their practice organization has on interruptions. Variables, such as the work schedule, the use of communication tools (or interruption tools) such as pagers, cell phones, and e-mail, and the use of clerical support staff, have an impact on the number of interruptions. This month, I will discuss the use of a “triage pager,” which is one example of practice organization that can have a huge impact on physician interruptions.
Worth the Interruptions?
Many large hospitalist groups have a pager to which all calls about new referrals go, and the pager is passed from one hospitalist to another each day or shift. This pager often is referred to as the “triage” or “hot” pager. It makes it easy for emergency room (ER) doctors and others to know how to reach the correct hospitalist about a new referral–they always call the same number. Typically, the hospitalist holding the pager calls the ER doctor back, learns about the patient, and then pages whichever hospitalist actually will care for the patient. The second hospitalist calls back and learns about the new patient from the “triage” hospitalist.
Although this is a valuable service for ER doctors and others referring patients to the hospitalists, it is terribly disruptive for the hospitalist carrying the pager. The unlucky person is interrupted constantly, and likely will have a very hard time providing patient care. Is there a better way to handle the triage function? Is there an alternative triage method, one that reduces hospitalist interruptions and switch tasking? There are three potential adjustments to the triage system you may want to consider (and remember, this is an issue only for larger groups–say more than 15 or 20 hospitalists).
Clerical Assistance
During business hours, Mondays through Fridays, have incoming referral calls go to a clerical person working for the hospitalists. A call received by this person might go something like:
- Phone rings;
- Clerical staff answers: “Hospitalist referral line;”
- ER doctor (or ER secretary): “I have a patient to be admitted to the hospitalist service;”
- Staff looks at the roster and determines the appropriate hospitalist for the next new patient;
- Staff: “That patient will go to Dr. Lovett. Give me the patient’s name and I’ll page Dr. Lovett, who will call you back to discuss the case in a couple minutes.”
This system preserves the easiest way to call referrals to the hospitalists, but decreases hospitalist interruptions and prevents the daisy chain of communication between the ER doctor, the triage doctor, and, finally, the hospitalist who actually will see the patient. Outside of regular business hours, these calls could go to another clerical person on duty in the hospital, or, perhaps, the ER secretary could field the calls and keep track of which hospitalist is up for referral.
On-Duty Hospitalist
If your group can’t, or doesn’t, want to have such calls funneled through a clerical person, the calls could go to an on-duty hospitalist. Rather than calling the ER to learn the details of a new patient who will be cared for by a different hospitalist, the “triage” hospitalist simply looks at a list to determine which hospitalist is up for the next new referral, then sends a page to the physician to call the ER. The triage doctor is interrupted, but immediately hands off the burden of communicating with the ER doctor to the hospitalist who actually will care for the patient.
A New Position
Or, instead of the two approaches above, you might take a 180-degree approach. You could create a new triage doctor position. This hospitalist would have no other responsibilities. In other words, while on triage, a doctor does not have a list of patients to round on and manage. The triage doctor’s only duty is to maximize ED throughput by quickly providing an opinion about whether a patient is appropriate for admission to the hospitalist service, and to assist moving them out of the ED and to the floor quickly. Eric Howell, MD, director, Zieve Medical Services, Johns Hopkins Bayview Medical Center at Johns Hopkins University in Baltimore has studied this third option, the use of a triage hospitalist who has no other clinical responsibilities, in a teaching hospital setting. Dr. Howell first implemented this as a daytime-only service, however, it proved so invaluable to improving emergency department throughput that it is now in place 24/7. He has published a study of this system and described the evolution in the following post on the SHM list serve:1
“Until 2006, when our gen-med service admission numbers were lower (approximately24 a day), we had the triage hospitalist carry a 50% clinical load, so that they could dedicate 50% time to triage. As our volume increased, and after we expanded the triage service to the ICUs and specialty floors, we dedicated one doc 24-7 (two, 12-hours shifts, actually) to the sole task of triage.
“It initially sounded like a large amount of resources just to triage, but at our 330-bed hospital, it has increased ED capacity substantially. The effect has been not to just increase ED visits and department of medicine admissions, but to increase surgical admissions through the ED, as well. The effect has been to dramatically reduce ambulance diversion. So, now the hospital funds the 24/7 triage position without a second thought.
“We have had enormous success and even expanded the hospitalist triage role to non-hospitalist wards showing dramatic decrease (25%) in ED length of stay. ”
Practical Measures
I’m skeptical a triage pager system, such as Dr. Howell describes above, is a good idea for most hospitalist practices. It is very expensive for a practice to devote physician manpower solely to non-billable services. The payoff, as measured in more productive or less-stressed hospitalists, would not justify the investment. Instead, as Dr. Howell did, you would have to look for a return on the investment outside the hospitalist practice itself, such as improvements in ED throughput.
Remember, Dr. Howell’s study was done in a teaching setting, and I suspect the reason a dedicated triage doctor proved so beneficial was it kept interns from setting up camp in the ED to complete the time-consuming admission process and delaying the patients’ transfer out of the ED. The triage doctor ensures nearly all ED admissions quickly move to the floor where the admitting team will make the time-consuming, initial (admitting) visit. In a non-teaching setting, that process isn’t burdened with trainees who take so long to admit patients, therefore, a dedicated triage hospitalist system probably would not result in such dramatic improvements in ED throughput.
Recommendations
I’ll finish by offering a summary and recommendations, based on my reasonably extensive experience, but almost no research data.
- For practices smaller than 10 hospitalists, the decision to use a triage pager can be based on preference. It won’t have significant impact on interruptions or work flow.
- Larger practices, especially those with more than 20 hospitalists, should first try to use a clerical person to field incoming referral calls during weekday business hours. The clerical employee would then page the hospitalist due to get the next new patient, and that hospitalist would call the referring doctor to learn about the patient directly.
- Large practices in teaching hospitals should think about whether it would be worthwhile to dedicate a hospitalist solely to the task of triage in hopes of reaping benefits elsewhere in the hospital, such as ED throughput. TH
Dr. Nelson has been a practicing hospitalist since 1988 and is co-founder and past president of SHM. He is a principal in Nelson/Flores Associates, a national hospitalist practice management consulting firm. He is part of the faculty for SHM’s “Best Practices in Managing a Hospital Medicine Program” course. This column represents his views and is not intended to reflect an official position of SHM.
Reference
1. Howell EE, Bessman ES, Rubin HR. Hospitalists and an innovative emergency department admission process. J Gen Intern Med. 2004.19(3):266-268.
Last month I discussed my concern regarding how often hospitalists are interrupted. In fact, I suspect frequent interruptions to our train of thought and workflow might lead to as many problems and errors as the sleep deprivation associated with long on-call shifts.
Every hospitalist group should think carefully about the effect their practice organization has on interruptions. Variables, such as the work schedule, the use of communication tools (or interruption tools) such as pagers, cell phones, and e-mail, and the use of clerical support staff, have an impact on the number of interruptions. This month, I will discuss the use of a “triage pager,” which is one example of practice organization that can have a huge impact on physician interruptions.
Worth the Interruptions?
Many large hospitalist groups have a pager to which all calls about new referrals go, and the pager is passed from one hospitalist to another each day or shift. This pager often is referred to as the “triage” or “hot” pager. It makes it easy for emergency room (ER) doctors and others to know how to reach the correct hospitalist about a new referral–they always call the same number. Typically, the hospitalist holding the pager calls the ER doctor back, learns about the patient, and then pages whichever hospitalist actually will care for the patient. The second hospitalist calls back and learns about the new patient from the “triage” hospitalist.
Although this is a valuable service for ER doctors and others referring patients to the hospitalists, it is terribly disruptive for the hospitalist carrying the pager. The unlucky person is interrupted constantly, and likely will have a very hard time providing patient care. Is there a better way to handle the triage function? Is there an alternative triage method, one that reduces hospitalist interruptions and switch tasking? There are three potential adjustments to the triage system you may want to consider (and remember, this is an issue only for larger groups–say more than 15 or 20 hospitalists).
Clerical Assistance
During business hours, Mondays through Fridays, have incoming referral calls go to a clerical person working for the hospitalists. A call received by this person might go something like:
- Phone rings;
- Clerical staff answers: “Hospitalist referral line;”
- ER doctor (or ER secretary): “I have a patient to be admitted to the hospitalist service;”
- Staff looks at the roster and determines the appropriate hospitalist for the next new patient;
- Staff: “That patient will go to Dr. Lovett. Give me the patient’s name and I’ll page Dr. Lovett, who will call you back to discuss the case in a couple minutes.”
This system preserves the easiest way to call referrals to the hospitalists, but decreases hospitalist interruptions and prevents the daisy chain of communication between the ER doctor, the triage doctor, and, finally, the hospitalist who actually will see the patient. Outside of regular business hours, these calls could go to another clerical person on duty in the hospital, or, perhaps, the ER secretary could field the calls and keep track of which hospitalist is up for referral.
On-Duty Hospitalist
If your group can’t, or doesn’t, want to have such calls funneled through a clerical person, the calls could go to an on-duty hospitalist. Rather than calling the ER to learn the details of a new patient who will be cared for by a different hospitalist, the “triage” hospitalist simply looks at a list to determine which hospitalist is up for the next new referral, then sends a page to the physician to call the ER. The triage doctor is interrupted, but immediately hands off the burden of communicating with the ER doctor to the hospitalist who actually will care for the patient.
A New Position
Or, instead of the two approaches above, you might take a 180-degree approach. You could create a new triage doctor position. This hospitalist would have no other responsibilities. In other words, while on triage, a doctor does not have a list of patients to round on and manage. The triage doctor’s only duty is to maximize ED throughput by quickly providing an opinion about whether a patient is appropriate for admission to the hospitalist service, and to assist moving them out of the ED and to the floor quickly. Eric Howell, MD, director, Zieve Medical Services, Johns Hopkins Bayview Medical Center at Johns Hopkins University in Baltimore has studied this third option, the use of a triage hospitalist who has no other clinical responsibilities, in a teaching hospital setting. Dr. Howell first implemented this as a daytime-only service, however, it proved so invaluable to improving emergency department throughput that it is now in place 24/7. He has published a study of this system and described the evolution in the following post on the SHM list serve:1
“Until 2006, when our gen-med service admission numbers were lower (approximately24 a day), we had the triage hospitalist carry a 50% clinical load, so that they could dedicate 50% time to triage. As our volume increased, and after we expanded the triage service to the ICUs and specialty floors, we dedicated one doc 24-7 (two, 12-hours shifts, actually) to the sole task of triage.
“It initially sounded like a large amount of resources just to triage, but at our 330-bed hospital, it has increased ED capacity substantially. The effect has been not to just increase ED visits and department of medicine admissions, but to increase surgical admissions through the ED, as well. The effect has been to dramatically reduce ambulance diversion. So, now the hospital funds the 24/7 triage position without a second thought.
“We have had enormous success and even expanded the hospitalist triage role to non-hospitalist wards showing dramatic decrease (25%) in ED length of stay. ”
Practical Measures
I’m skeptical a triage pager system, such as Dr. Howell describes above, is a good idea for most hospitalist practices. It is very expensive for a practice to devote physician manpower solely to non-billable services. The payoff, as measured in more productive or less-stressed hospitalists, would not justify the investment. Instead, as Dr. Howell did, you would have to look for a return on the investment outside the hospitalist practice itself, such as improvements in ED throughput.
Remember, Dr. Howell’s study was done in a teaching setting, and I suspect the reason a dedicated triage doctor proved so beneficial was it kept interns from setting up camp in the ED to complete the time-consuming admission process and delaying the patients’ transfer out of the ED. The triage doctor ensures nearly all ED admissions quickly move to the floor where the admitting team will make the time-consuming, initial (admitting) visit. In a non-teaching setting, that process isn’t burdened with trainees who take so long to admit patients, therefore, a dedicated triage hospitalist system probably would not result in such dramatic improvements in ED throughput.
Recommendations
I’ll finish by offering a summary and recommendations, based on my reasonably extensive experience, but almost no research data.
- For practices smaller than 10 hospitalists, the decision to use a triage pager can be based on preference. It won’t have significant impact on interruptions or work flow.
- Larger practices, especially those with more than 20 hospitalists, should first try to use a clerical person to field incoming referral calls during weekday business hours. The clerical employee would then page the hospitalist due to get the next new patient, and that hospitalist would call the referring doctor to learn about the patient directly.
- Large practices in teaching hospitals should think about whether it would be worthwhile to dedicate a hospitalist solely to the task of triage in hopes of reaping benefits elsewhere in the hospital, such as ED throughput. TH
Dr. Nelson has been a practicing hospitalist since 1988 and is co-founder and past president of SHM. He is a principal in Nelson/Flores Associates, a national hospitalist practice management consulting firm. He is part of the faculty for SHM’s “Best Practices in Managing a Hospital Medicine Program” course. This column represents his views and is not intended to reflect an official position of SHM.
Reference
1. Howell EE, Bessman ES, Rubin HR. Hospitalists and an innovative emergency department admission process. J Gen Intern Med. 2004.19(3):266-268.
Last month I discussed my concern regarding how often hospitalists are interrupted. In fact, I suspect frequent interruptions to our train of thought and workflow might lead to as many problems and errors as the sleep deprivation associated with long on-call shifts.
Every hospitalist group should think carefully about the effect their practice organization has on interruptions. Variables, such as the work schedule, the use of communication tools (or interruption tools) such as pagers, cell phones, and e-mail, and the use of clerical support staff, have an impact on the number of interruptions. This month, I will discuss the use of a “triage pager,” which is one example of practice organization that can have a huge impact on physician interruptions.
Worth the Interruptions?
Many large hospitalist groups have a pager to which all calls about new referrals go, and the pager is passed from one hospitalist to another each day or shift. This pager often is referred to as the “triage” or “hot” pager. It makes it easy for emergency room (ER) doctors and others to know how to reach the correct hospitalist about a new referral–they always call the same number. Typically, the hospitalist holding the pager calls the ER doctor back, learns about the patient, and then pages whichever hospitalist actually will care for the patient. The second hospitalist calls back and learns about the new patient from the “triage” hospitalist.
Although this is a valuable service for ER doctors and others referring patients to the hospitalists, it is terribly disruptive for the hospitalist carrying the pager. The unlucky person is interrupted constantly, and likely will have a very hard time providing patient care. Is there a better way to handle the triage function? Is there an alternative triage method, one that reduces hospitalist interruptions and switch tasking? There are three potential adjustments to the triage system you may want to consider (and remember, this is an issue only for larger groups–say more than 15 or 20 hospitalists).
Clerical Assistance
During business hours, Mondays through Fridays, have incoming referral calls go to a clerical person working for the hospitalists. A call received by this person might go something like:
- Phone rings;
- Clerical staff answers: “Hospitalist referral line;”
- ER doctor (or ER secretary): “I have a patient to be admitted to the hospitalist service;”
- Staff looks at the roster and determines the appropriate hospitalist for the next new patient;
- Staff: “That patient will go to Dr. Lovett. Give me the patient’s name and I’ll page Dr. Lovett, who will call you back to discuss the case in a couple minutes.”
This system preserves the easiest way to call referrals to the hospitalists, but decreases hospitalist interruptions and prevents the daisy chain of communication between the ER doctor, the triage doctor, and, finally, the hospitalist who actually will see the patient. Outside of regular business hours, these calls could go to another clerical person on duty in the hospital, or, perhaps, the ER secretary could field the calls and keep track of which hospitalist is up for referral.
On-Duty Hospitalist
If your group can’t, or doesn’t, want to have such calls funneled through a clerical person, the calls could go to an on-duty hospitalist. Rather than calling the ER to learn the details of a new patient who will be cared for by a different hospitalist, the “triage” hospitalist simply looks at a list to determine which hospitalist is up for the next new referral, then sends a page to the physician to call the ER. The triage doctor is interrupted, but immediately hands off the burden of communicating with the ER doctor to the hospitalist who actually will care for the patient.
A New Position
Or, instead of the two approaches above, you might take a 180-degree approach. You could create a new triage doctor position. This hospitalist would have no other responsibilities. In other words, while on triage, a doctor does not have a list of patients to round on and manage. The triage doctor’s only duty is to maximize ED throughput by quickly providing an opinion about whether a patient is appropriate for admission to the hospitalist service, and to assist moving them out of the ED and to the floor quickly. Eric Howell, MD, director, Zieve Medical Services, Johns Hopkins Bayview Medical Center at Johns Hopkins University in Baltimore has studied this third option, the use of a triage hospitalist who has no other clinical responsibilities, in a teaching hospital setting. Dr. Howell first implemented this as a daytime-only service, however, it proved so invaluable to improving emergency department throughput that it is now in place 24/7. He has published a study of this system and described the evolution in the following post on the SHM list serve:1
“Until 2006, when our gen-med service admission numbers were lower (approximately24 a day), we had the triage hospitalist carry a 50% clinical load, so that they could dedicate 50% time to triage. As our volume increased, and after we expanded the triage service to the ICUs and specialty floors, we dedicated one doc 24-7 (two, 12-hours shifts, actually) to the sole task of triage.
“It initially sounded like a large amount of resources just to triage, but at our 330-bed hospital, it has increased ED capacity substantially. The effect has been not to just increase ED visits and department of medicine admissions, but to increase surgical admissions through the ED, as well. The effect has been to dramatically reduce ambulance diversion. So, now the hospital funds the 24/7 triage position without a second thought.
“We have had enormous success and even expanded the hospitalist triage role to non-hospitalist wards showing dramatic decrease (25%) in ED length of stay. ”
Practical Measures
I’m skeptical a triage pager system, such as Dr. Howell describes above, is a good idea for most hospitalist practices. It is very expensive for a practice to devote physician manpower solely to non-billable services. The payoff, as measured in more productive or less-stressed hospitalists, would not justify the investment. Instead, as Dr. Howell did, you would have to look for a return on the investment outside the hospitalist practice itself, such as improvements in ED throughput.
Remember, Dr. Howell’s study was done in a teaching setting, and I suspect the reason a dedicated triage doctor proved so beneficial was it kept interns from setting up camp in the ED to complete the time-consuming admission process and delaying the patients’ transfer out of the ED. The triage doctor ensures nearly all ED admissions quickly move to the floor where the admitting team will make the time-consuming, initial (admitting) visit. In a non-teaching setting, that process isn’t burdened with trainees who take so long to admit patients, therefore, a dedicated triage hospitalist system probably would not result in such dramatic improvements in ED throughput.
Recommendations
I’ll finish by offering a summary and recommendations, based on my reasonably extensive experience, but almost no research data.
- For practices smaller than 10 hospitalists, the decision to use a triage pager can be based on preference. It won’t have significant impact on interruptions or work flow.
- Larger practices, especially those with more than 20 hospitalists, should first try to use a clerical person to field incoming referral calls during weekday business hours. The clerical employee would then page the hospitalist due to get the next new patient, and that hospitalist would call the referring doctor to learn about the patient directly.
- Large practices in teaching hospitals should think about whether it would be worthwhile to dedicate a hospitalist solely to the task of triage in hopes of reaping benefits elsewhere in the hospital, such as ED throughput. TH
Dr. Nelson has been a practicing hospitalist since 1988 and is co-founder and past president of SHM. He is a principal in Nelson/Flores Associates, a national hospitalist practice management consulting firm. He is part of the faculty for SHM’s “Best Practices in Managing a Hospital Medicine Program” course. This column represents his views and is not intended to reflect an official position of SHM.
Reference
1. Howell EE, Bessman ES, Rubin HR. Hospitalists and an innovative emergency department admission process. J Gen Intern Med. 2004.19(3):266-268.
Really, It’s Switch Tasking
It’s fitting that I’ve been interrupted many times while I’ve been writing this column. My topic is interruptions in the work of a hospitalist. I’ll leave it to you to judge whether the interruptions I suffered while writing have adversely affected the quality of this column. The more important question is how much the quality, efficiency and patient safety of hospitalists’ work suffers because of interruptions.
For the most part, the hospital where I worked as an orderly (how is that for an antiquated term!) in the 1970s was like a library; nursing stations usually were quiet and slow paced, well suited for concentration and focus. Today, the nursing station in a typical hospital looks more like the floor of the stock exchange, with many people trying to talk over each other and jostling for a position at a computer. People who study this kind of thing would say that we increasingly work in high-tempo settings with a high communication burden, and, as a result, our work has become increasingly “interrupt driven.”
It is tempting to say hospitalists (and emergency room doctors and others) have to do a lot of multitasking. But I think that we’re really “switch tasking” most of the time, rather than multitasking.1 Switch tasking means frequently changing tasks. With some regularity we stop in the middle of one task and switch our attention to another—and incur two costs in the process. One cost is the mental energy consumed and stress of frequently shifting our attention.
The other cost is that it is reasonably common that we fail to return to the original task, so it remains uncompleted. How often have you promised a patient you’d write a PRN order for a sleeping pill, but got interrupted and never circled back to write the order? And it is easy for most of us to think of similar errors with more significant consequences.
Kevin O’Leary and colleagues at Northwestern University in Evanston, Ill., conducted a time-motion study of hospitalists. It found hospitalists were interrupted by pages an average of 3.4 times per hour (+/- 1.5).2 Emergency room (ER) doctors face an environment similar to hospitalists, and one study found ER doctors were interrupted an average of once every 5 minutes, and two-thirds of the time did not return to the prior task.3
Interruptions vs. Sleep Depravation
I’ve found it difficult to adjust my work style and habits to keep up with the pace of change and the increasing frequency of interruptions. My first, and generally ineffective, impulse is to try and decrease the noise and interruptions by doing things like asking others to page me less often, and only for time-sensitive clinical issues and not for routine things. But the problem is that promptly addressing many of these interruptions is our job, not simply a distraction.
Even if we can’t make the interruptions go away, we can try to manage them. In 2005, I was thrilled to learn of an emerging field known as “interruption science.” For a really engaging look at this field, search the Internet for “Meet the Life Hackers,” an article by Clive Owen in the New York Times [Sunday] Magazine, October 16, 2005. It describes people who are devoting their research careers to understanding the best ways to manage interruptions and where our attention shifts next.
One workplace that has been studied extensively is the cockpit of fighter jets. They’re full of remarkable gadgets that provide constant information via lights and noisemaking devices, including one that sounds like the female voice on your car’s GPS navigator. But research showed that during times of high pilot workload, some of these alarms distracted the pilots from more important tasks and increased errors. One strategy has been to suppress some alarms when the jet is configured for a complex operation, such as dropping a precision bomb or landing.
Although I have absolutely no data to prove it, I suspect hospitalists’ high volume of interruptions increases the errors we make. In fact, frequent interruptions might lead to more problems and errors than the sleep deprivation that has received so much attention in the past few years.
Fixing the problem of sleep deprivation seems easy, at first. Just eliminate the long work periods. But that means moving toward more shift work, which decreases continuity and increases the potential for new problems, like fumbled handoffs. It is really tough to figure out how to optimally balance the competing needs of preventing sleep deprivation and maximizing continuity to the point that minimizes the errors and problems caused by each. And I think it’s even tougher to find solutions to reduce hospitalist interruptions and the adverse consequences.
Proactive Measures
Two strategies to minimize hospitalist interruptions have been used in a handful of places with some success. Neither is perfect, and both are difficult to implement. But each can serve as a starting place for brainstorming about where you could or should direct your efforts.
The first is to have a rounding assistant accompany each hospitalist throughout the day. This person:
- Doesn’t need any medical training and functions much like a mobile receptionist.
- Would hold the doctor’s pager and keep track of all incoming calls, some of which would be handled without involving the doctor. As an example, this assistant should be able to handle the “family is anxious and wants to know when you will be here” call without interrupting the doctor.
- Could find charts, look up test results on the computer, page consultants, etc.
All these things could decrease the hospitalist’s interruptions with little impact on others.
Although it sounds wonderful, a rounding assistant ends up being very expensive and few practices use them. Some practices have case managers dedicated to the hospitalists, which provide some rounding assistant functions in addition to their case management work.
A second strategy that can significantly influence interruptions is to implement a system of unit-based hospitalists, in which a given hospitalist has most patients on a single unit of the hospital. This can decrease the number of pages to the hospitalist, as well as influencing communication in other ways that impact interruptions. TH
Dr. Nelson has been a practicing hospitalist since 1988 and is co-founder and past president of SHM. He is a principal in Nelson/Flores Associates, a national hospitalist practice management consulting firm. He is also part of the faculty for SHM’s “Best Practices in Managing a Hospital Medicine Program” course. This column represents his views and is not intended to reflect an official position of SHM.
References
1. Crenshaw D. The Myth of Multitasking: How Doing it All Gets Nothing Done. Hoboken, NJ. Jossey-Boss; 2008.
2. O’Leary, KJ, Liebovitz DM, Baker, DW. How hospitalists spend their time: Insights on efficiency and safety. J Hosp Med. 2006;11(2);88-93.
3. Chisolm et. al. Emergency department workplace interruptions: Are emergency physicians “interrupt-driven” and “multitasking?” Acad Emerg Med. 2000;7:1239-1243.
It’s fitting that I’ve been interrupted many times while I’ve been writing this column. My topic is interruptions in the work of a hospitalist. I’ll leave it to you to judge whether the interruptions I suffered while writing have adversely affected the quality of this column. The more important question is how much the quality, efficiency and patient safety of hospitalists’ work suffers because of interruptions.
For the most part, the hospital where I worked as an orderly (how is that for an antiquated term!) in the 1970s was like a library; nursing stations usually were quiet and slow paced, well suited for concentration and focus. Today, the nursing station in a typical hospital looks more like the floor of the stock exchange, with many people trying to talk over each other and jostling for a position at a computer. People who study this kind of thing would say that we increasingly work in high-tempo settings with a high communication burden, and, as a result, our work has become increasingly “interrupt driven.”
It is tempting to say hospitalists (and emergency room doctors and others) have to do a lot of multitasking. But I think that we’re really “switch tasking” most of the time, rather than multitasking.1 Switch tasking means frequently changing tasks. With some regularity we stop in the middle of one task and switch our attention to another—and incur two costs in the process. One cost is the mental energy consumed and stress of frequently shifting our attention.
The other cost is that it is reasonably common that we fail to return to the original task, so it remains uncompleted. How often have you promised a patient you’d write a PRN order for a sleeping pill, but got interrupted and never circled back to write the order? And it is easy for most of us to think of similar errors with more significant consequences.
Kevin O’Leary and colleagues at Northwestern University in Evanston, Ill., conducted a time-motion study of hospitalists. It found hospitalists were interrupted by pages an average of 3.4 times per hour (+/- 1.5).2 Emergency room (ER) doctors face an environment similar to hospitalists, and one study found ER doctors were interrupted an average of once every 5 minutes, and two-thirds of the time did not return to the prior task.3
Interruptions vs. Sleep Depravation
I’ve found it difficult to adjust my work style and habits to keep up with the pace of change and the increasing frequency of interruptions. My first, and generally ineffective, impulse is to try and decrease the noise and interruptions by doing things like asking others to page me less often, and only for time-sensitive clinical issues and not for routine things. But the problem is that promptly addressing many of these interruptions is our job, not simply a distraction.
Even if we can’t make the interruptions go away, we can try to manage them. In 2005, I was thrilled to learn of an emerging field known as “interruption science.” For a really engaging look at this field, search the Internet for “Meet the Life Hackers,” an article by Clive Owen in the New York Times [Sunday] Magazine, October 16, 2005. It describes people who are devoting their research careers to understanding the best ways to manage interruptions and where our attention shifts next.
One workplace that has been studied extensively is the cockpit of fighter jets. They’re full of remarkable gadgets that provide constant information via lights and noisemaking devices, including one that sounds like the female voice on your car’s GPS navigator. But research showed that during times of high pilot workload, some of these alarms distracted the pilots from more important tasks and increased errors. One strategy has been to suppress some alarms when the jet is configured for a complex operation, such as dropping a precision bomb or landing.
Although I have absolutely no data to prove it, I suspect hospitalists’ high volume of interruptions increases the errors we make. In fact, frequent interruptions might lead to more problems and errors than the sleep deprivation that has received so much attention in the past few years.
Fixing the problem of sleep deprivation seems easy, at first. Just eliminate the long work periods. But that means moving toward more shift work, which decreases continuity and increases the potential for new problems, like fumbled handoffs. It is really tough to figure out how to optimally balance the competing needs of preventing sleep deprivation and maximizing continuity to the point that minimizes the errors and problems caused by each. And I think it’s even tougher to find solutions to reduce hospitalist interruptions and the adverse consequences.
Proactive Measures
Two strategies to minimize hospitalist interruptions have been used in a handful of places with some success. Neither is perfect, and both are difficult to implement. But each can serve as a starting place for brainstorming about where you could or should direct your efforts.
The first is to have a rounding assistant accompany each hospitalist throughout the day. This person:
- Doesn’t need any medical training and functions much like a mobile receptionist.
- Would hold the doctor’s pager and keep track of all incoming calls, some of which would be handled without involving the doctor. As an example, this assistant should be able to handle the “family is anxious and wants to know when you will be here” call without interrupting the doctor.
- Could find charts, look up test results on the computer, page consultants, etc.
All these things could decrease the hospitalist’s interruptions with little impact on others.
Although it sounds wonderful, a rounding assistant ends up being very expensive and few practices use them. Some practices have case managers dedicated to the hospitalists, which provide some rounding assistant functions in addition to their case management work.
A second strategy that can significantly influence interruptions is to implement a system of unit-based hospitalists, in which a given hospitalist has most patients on a single unit of the hospital. This can decrease the number of pages to the hospitalist, as well as influencing communication in other ways that impact interruptions. TH
Dr. Nelson has been a practicing hospitalist since 1988 and is co-founder and past president of SHM. He is a principal in Nelson/Flores Associates, a national hospitalist practice management consulting firm. He is also part of the faculty for SHM’s “Best Practices in Managing a Hospital Medicine Program” course. This column represents his views and is not intended to reflect an official position of SHM.
References
1. Crenshaw D. The Myth of Multitasking: How Doing it All Gets Nothing Done. Hoboken, NJ. Jossey-Boss; 2008.
2. O’Leary, KJ, Liebovitz DM, Baker, DW. How hospitalists spend their time: Insights on efficiency and safety. J Hosp Med. 2006;11(2);88-93.
3. Chisolm et. al. Emergency department workplace interruptions: Are emergency physicians “interrupt-driven” and “multitasking?” Acad Emerg Med. 2000;7:1239-1243.
It’s fitting that I’ve been interrupted many times while I’ve been writing this column. My topic is interruptions in the work of a hospitalist. I’ll leave it to you to judge whether the interruptions I suffered while writing have adversely affected the quality of this column. The more important question is how much the quality, efficiency and patient safety of hospitalists’ work suffers because of interruptions.
For the most part, the hospital where I worked as an orderly (how is that for an antiquated term!) in the 1970s was like a library; nursing stations usually were quiet and slow paced, well suited for concentration and focus. Today, the nursing station in a typical hospital looks more like the floor of the stock exchange, with many people trying to talk over each other and jostling for a position at a computer. People who study this kind of thing would say that we increasingly work in high-tempo settings with a high communication burden, and, as a result, our work has become increasingly “interrupt driven.”
It is tempting to say hospitalists (and emergency room doctors and others) have to do a lot of multitasking. But I think that we’re really “switch tasking” most of the time, rather than multitasking.1 Switch tasking means frequently changing tasks. With some regularity we stop in the middle of one task and switch our attention to another—and incur two costs in the process. One cost is the mental energy consumed and stress of frequently shifting our attention.
The other cost is that it is reasonably common that we fail to return to the original task, so it remains uncompleted. How often have you promised a patient you’d write a PRN order for a sleeping pill, but got interrupted and never circled back to write the order? And it is easy for most of us to think of similar errors with more significant consequences.
Kevin O’Leary and colleagues at Northwestern University in Evanston, Ill., conducted a time-motion study of hospitalists. It found hospitalists were interrupted by pages an average of 3.4 times per hour (+/- 1.5).2 Emergency room (ER) doctors face an environment similar to hospitalists, and one study found ER doctors were interrupted an average of once every 5 minutes, and two-thirds of the time did not return to the prior task.3
Interruptions vs. Sleep Depravation
I’ve found it difficult to adjust my work style and habits to keep up with the pace of change and the increasing frequency of interruptions. My first, and generally ineffective, impulse is to try and decrease the noise and interruptions by doing things like asking others to page me less often, and only for time-sensitive clinical issues and not for routine things. But the problem is that promptly addressing many of these interruptions is our job, not simply a distraction.
Even if we can’t make the interruptions go away, we can try to manage them. In 2005, I was thrilled to learn of an emerging field known as “interruption science.” For a really engaging look at this field, search the Internet for “Meet the Life Hackers,” an article by Clive Owen in the New York Times [Sunday] Magazine, October 16, 2005. It describes people who are devoting their research careers to understanding the best ways to manage interruptions and where our attention shifts next.
One workplace that has been studied extensively is the cockpit of fighter jets. They’re full of remarkable gadgets that provide constant information via lights and noisemaking devices, including one that sounds like the female voice on your car’s GPS navigator. But research showed that during times of high pilot workload, some of these alarms distracted the pilots from more important tasks and increased errors. One strategy has been to suppress some alarms when the jet is configured for a complex operation, such as dropping a precision bomb or landing.
Although I have absolutely no data to prove it, I suspect hospitalists’ high volume of interruptions increases the errors we make. In fact, frequent interruptions might lead to more problems and errors than the sleep deprivation that has received so much attention in the past few years.
Fixing the problem of sleep deprivation seems easy, at first. Just eliminate the long work periods. But that means moving toward more shift work, which decreases continuity and increases the potential for new problems, like fumbled handoffs. It is really tough to figure out how to optimally balance the competing needs of preventing sleep deprivation and maximizing continuity to the point that minimizes the errors and problems caused by each. And I think it’s even tougher to find solutions to reduce hospitalist interruptions and the adverse consequences.
Proactive Measures
Two strategies to minimize hospitalist interruptions have been used in a handful of places with some success. Neither is perfect, and both are difficult to implement. But each can serve as a starting place for brainstorming about where you could or should direct your efforts.
The first is to have a rounding assistant accompany each hospitalist throughout the day. This person:
- Doesn’t need any medical training and functions much like a mobile receptionist.
- Would hold the doctor’s pager and keep track of all incoming calls, some of which would be handled without involving the doctor. As an example, this assistant should be able to handle the “family is anxious and wants to know when you will be here” call without interrupting the doctor.
- Could find charts, look up test results on the computer, page consultants, etc.
All these things could decrease the hospitalist’s interruptions with little impact on others.
Although it sounds wonderful, a rounding assistant ends up being very expensive and few practices use them. Some practices have case managers dedicated to the hospitalists, which provide some rounding assistant functions in addition to their case management work.
A second strategy that can significantly influence interruptions is to implement a system of unit-based hospitalists, in which a given hospitalist has most patients on a single unit of the hospital. This can decrease the number of pages to the hospitalist, as well as influencing communication in other ways that impact interruptions. TH
Dr. Nelson has been a practicing hospitalist since 1988 and is co-founder and past president of SHM. He is a principal in Nelson/Flores Associates, a national hospitalist practice management consulting firm. He is also part of the faculty for SHM’s “Best Practices in Managing a Hospital Medicine Program” course. This column represents his views and is not intended to reflect an official position of SHM.
References
1. Crenshaw D. The Myth of Multitasking: How Doing it All Gets Nothing Done. Hoboken, NJ. Jossey-Boss; 2008.
2. O’Leary, KJ, Liebovitz DM, Baker, DW. How hospitalists spend their time: Insights on efficiency and safety. J Hosp Med. 2006;11(2);88-93.
3. Chisolm et. al. Emergency department workplace interruptions: Are emergency physicians “interrupt-driven” and “multitasking?” Acad Emerg Med. 2000;7:1239-1243.
Maximizing NPPs in Hospitalist Practices
Last month, I recommended considering new and innovative roles for the non-physician providers (NPPs) (see The Hospitalist, September 2008, p. 61.). In this column I’ll discuss the economic and patient satisfaction issues related to NPPs in hospitalist practice.
Economics of NPPs
My experience suggests many practices follow a similar line of reasoning when adding NPPs: “We have six physician hospitalist FTEs and need to expand further, yet recruiting additional MDs is difficult. Perhaps we should add one or more NPPs instead. That should work out well economically since NPPs have lower salaries. After all, it seems to work for heart surgeons and orthopedists.”
This kind of reasoning has two flaws. The practice is, in essence, deciding to add NPPs because that process may be easier than finding additional MDs. The practice should instead consider what work needs to be done and decide whether there is a genuinely valuable role for an NPP.
Secondly, just because it makes financial sense for some specialties to add NPPs doesn’t mean it does for hospitalist groups. The salary gap between orthopedists or cardiac surgeons and NPPs is huge. The salary difference between a physician hospitalist and an NPP is much more modest.
From a strictly financial analysis, which ignores the many benefits of NPPs that don’t appear on financial statements, an NPP needs to increase the efficiency of an orthopedist or cardiac surgeon by only 10% to 20%. That same NPP would need to increase the efficiency of a hospitalist by more like 50%. (I estimated the percentages to illustrate the point. You should conduct a more-detailed analysis of your own situation to determine accurate percentages.)
I’ve worked with practices that have incorporated NPPs but failed to think carefully about their optimal roles. These staff end up functioning in a mostly clerical role, doing tasks such as faxing discharge information to PCPs, retrieving records from outside facilities, or handling billing functions for the doctors. Those practices should either change the NPPs’ roles or use the money to instead hire clerical help. That would leave money for other purposes, such as creating a more aggressive physician recruiting effort or hiring MDs to moonlight.
Local Factors Govern Economics, Practice
In addition to financial considerations surrounding NPPs, keep in mind licensure. Nurse practitioners are licensed as independent practitioners. Physician assistants are not. The laws governing scope of practice for both of these professionals vary from state to state. Additionally, hospital bylaws govern the boundaries of what NPPs can do without supervision. Two hospitals in the same community might have completely different rules. It is important to understand the state and individual hospital regulations that govern NPPs where you practice.
A PA’s work will nearly always require a physician being physically present during some portion of the patient visit and co-signing chart notes and orders. Nurse practitioners, on the other hand, may be able to perform certain patient-care activities independently. In the latter case, Medicare and other payers typically reimburse at 85% of the rate customarily paid to MDs for the same service.
Patient Perception of NPPs
Patients are increasingly more accepting of NPs and PAs. This seems especially true in settings with clear distinctions between the role of NPP and MD.
For example, my wife is perfectly happy to see a nurse practitioner for routine gynecological care, such as Pap smears. She knows the obstetrician handled the delivery of our children and is available anytime she’s needed.
My neighbor was pleased with his open-heart surgery experience and spoke glowingly of the NP who made rounds daily and assisted during the surgery. He knew the MD surgeon performed most of the operation but left the perioperative care up to the NP.
Patients on a hospitalist service may not see things the same way. My neighbor understood he was hospitalized for the purpose of open-heart surgery done by the MD. He looked at the perioperative care outside of the operation as a secondary issue.
Most medical admissions managed by hospitalists don’t have such clear marquee events in patients’ eyes. So it may be less natural for patients to feel OK about how the hospitalist and NPP divide up care responsibilities. Look at it this way: As hospitalists, we have limited face time with patients, and must make good use of it to establish trust and rapport. When we add an NPP to the care team, we ask patients to develop trust and rapport with two providers instead of just one.
Imagine a patient recently discharged from a hospitalist practice. Her friend asks how it went and which doctor she saw. The patient responds, “I couldn’t figure out who was really in charge of my care. Dr. Nelson’s name was on my armband, but I rarely saw him. Instead, I saw his assistant (the NPP) most of the time.” I suspect that patient will be much less likely to report high levels of satisfaction with her care than one who just saw a hospitalist.
Though I’m concerned that it might be more difficult to keep patients happy when NPPs are part of a hospitalist practice, most practices report this hasn’t been a problem. I’m not suggesting that concern about patient satisfaction means you shouldn’t use NPPs in your hospitalist practices. However, patient satisfaction is an issue to consider when organizing your practice—and an NPP’s role in it—to provide the greatest benefit to your patients. TH
Dr. Nelson has been a practicing hospitalist since 1988 and is co-founder and past president of SHM. He is a principal in Nelson/Flores Associates, a national hospitalist practice management consulting firm. He is also part of the faculty for SHM’s “Best Practices in Managing a Hospital Medicine Program” course. This column represents his views and is not intended to reflect an official position of SHM.
Last month, I recommended considering new and innovative roles for the non-physician providers (NPPs) (see The Hospitalist, September 2008, p. 61.). In this column I’ll discuss the economic and patient satisfaction issues related to NPPs in hospitalist practice.
Economics of NPPs
My experience suggests many practices follow a similar line of reasoning when adding NPPs: “We have six physician hospitalist FTEs and need to expand further, yet recruiting additional MDs is difficult. Perhaps we should add one or more NPPs instead. That should work out well economically since NPPs have lower salaries. After all, it seems to work for heart surgeons and orthopedists.”
This kind of reasoning has two flaws. The practice is, in essence, deciding to add NPPs because that process may be easier than finding additional MDs. The practice should instead consider what work needs to be done and decide whether there is a genuinely valuable role for an NPP.
Secondly, just because it makes financial sense for some specialties to add NPPs doesn’t mean it does for hospitalist groups. The salary gap between orthopedists or cardiac surgeons and NPPs is huge. The salary difference between a physician hospitalist and an NPP is much more modest.
From a strictly financial analysis, which ignores the many benefits of NPPs that don’t appear on financial statements, an NPP needs to increase the efficiency of an orthopedist or cardiac surgeon by only 10% to 20%. That same NPP would need to increase the efficiency of a hospitalist by more like 50%. (I estimated the percentages to illustrate the point. You should conduct a more-detailed analysis of your own situation to determine accurate percentages.)
I’ve worked with practices that have incorporated NPPs but failed to think carefully about their optimal roles. These staff end up functioning in a mostly clerical role, doing tasks such as faxing discharge information to PCPs, retrieving records from outside facilities, or handling billing functions for the doctors. Those practices should either change the NPPs’ roles or use the money to instead hire clerical help. That would leave money for other purposes, such as creating a more aggressive physician recruiting effort or hiring MDs to moonlight.
Local Factors Govern Economics, Practice
In addition to financial considerations surrounding NPPs, keep in mind licensure. Nurse practitioners are licensed as independent practitioners. Physician assistants are not. The laws governing scope of practice for both of these professionals vary from state to state. Additionally, hospital bylaws govern the boundaries of what NPPs can do without supervision. Two hospitals in the same community might have completely different rules. It is important to understand the state and individual hospital regulations that govern NPPs where you practice.
A PA’s work will nearly always require a physician being physically present during some portion of the patient visit and co-signing chart notes and orders. Nurse practitioners, on the other hand, may be able to perform certain patient-care activities independently. In the latter case, Medicare and other payers typically reimburse at 85% of the rate customarily paid to MDs for the same service.
Patient Perception of NPPs
Patients are increasingly more accepting of NPs and PAs. This seems especially true in settings with clear distinctions between the role of NPP and MD.
For example, my wife is perfectly happy to see a nurse practitioner for routine gynecological care, such as Pap smears. She knows the obstetrician handled the delivery of our children and is available anytime she’s needed.
My neighbor was pleased with his open-heart surgery experience and spoke glowingly of the NP who made rounds daily and assisted during the surgery. He knew the MD surgeon performed most of the operation but left the perioperative care up to the NP.
Patients on a hospitalist service may not see things the same way. My neighbor understood he was hospitalized for the purpose of open-heart surgery done by the MD. He looked at the perioperative care outside of the operation as a secondary issue.
Most medical admissions managed by hospitalists don’t have such clear marquee events in patients’ eyes. So it may be less natural for patients to feel OK about how the hospitalist and NPP divide up care responsibilities. Look at it this way: As hospitalists, we have limited face time with patients, and must make good use of it to establish trust and rapport. When we add an NPP to the care team, we ask patients to develop trust and rapport with two providers instead of just one.
Imagine a patient recently discharged from a hospitalist practice. Her friend asks how it went and which doctor she saw. The patient responds, “I couldn’t figure out who was really in charge of my care. Dr. Nelson’s name was on my armband, but I rarely saw him. Instead, I saw his assistant (the NPP) most of the time.” I suspect that patient will be much less likely to report high levels of satisfaction with her care than one who just saw a hospitalist.
Though I’m concerned that it might be more difficult to keep patients happy when NPPs are part of a hospitalist practice, most practices report this hasn’t been a problem. I’m not suggesting that concern about patient satisfaction means you shouldn’t use NPPs in your hospitalist practices. However, patient satisfaction is an issue to consider when organizing your practice—and an NPP’s role in it—to provide the greatest benefit to your patients. TH
Dr. Nelson has been a practicing hospitalist since 1988 and is co-founder and past president of SHM. He is a principal in Nelson/Flores Associates, a national hospitalist practice management consulting firm. He is also part of the faculty for SHM’s “Best Practices in Managing a Hospital Medicine Program” course. This column represents his views and is not intended to reflect an official position of SHM.
Last month, I recommended considering new and innovative roles for the non-physician providers (NPPs) (see The Hospitalist, September 2008, p. 61.). In this column I’ll discuss the economic and patient satisfaction issues related to NPPs in hospitalist practice.
Economics of NPPs
My experience suggests many practices follow a similar line of reasoning when adding NPPs: “We have six physician hospitalist FTEs and need to expand further, yet recruiting additional MDs is difficult. Perhaps we should add one or more NPPs instead. That should work out well economically since NPPs have lower salaries. After all, it seems to work for heart surgeons and orthopedists.”
This kind of reasoning has two flaws. The practice is, in essence, deciding to add NPPs because that process may be easier than finding additional MDs. The practice should instead consider what work needs to be done and decide whether there is a genuinely valuable role for an NPP.
Secondly, just because it makes financial sense for some specialties to add NPPs doesn’t mean it does for hospitalist groups. The salary gap between orthopedists or cardiac surgeons and NPPs is huge. The salary difference between a physician hospitalist and an NPP is much more modest.
From a strictly financial analysis, which ignores the many benefits of NPPs that don’t appear on financial statements, an NPP needs to increase the efficiency of an orthopedist or cardiac surgeon by only 10% to 20%. That same NPP would need to increase the efficiency of a hospitalist by more like 50%. (I estimated the percentages to illustrate the point. You should conduct a more-detailed analysis of your own situation to determine accurate percentages.)
I’ve worked with practices that have incorporated NPPs but failed to think carefully about their optimal roles. These staff end up functioning in a mostly clerical role, doing tasks such as faxing discharge information to PCPs, retrieving records from outside facilities, or handling billing functions for the doctors. Those practices should either change the NPPs’ roles or use the money to instead hire clerical help. That would leave money for other purposes, such as creating a more aggressive physician recruiting effort or hiring MDs to moonlight.
Local Factors Govern Economics, Practice
In addition to financial considerations surrounding NPPs, keep in mind licensure. Nurse practitioners are licensed as independent practitioners. Physician assistants are not. The laws governing scope of practice for both of these professionals vary from state to state. Additionally, hospital bylaws govern the boundaries of what NPPs can do without supervision. Two hospitals in the same community might have completely different rules. It is important to understand the state and individual hospital regulations that govern NPPs where you practice.
A PA’s work will nearly always require a physician being physically present during some portion of the patient visit and co-signing chart notes and orders. Nurse practitioners, on the other hand, may be able to perform certain patient-care activities independently. In the latter case, Medicare and other payers typically reimburse at 85% of the rate customarily paid to MDs for the same service.
Patient Perception of NPPs
Patients are increasingly more accepting of NPs and PAs. This seems especially true in settings with clear distinctions between the role of NPP and MD.
For example, my wife is perfectly happy to see a nurse practitioner for routine gynecological care, such as Pap smears. She knows the obstetrician handled the delivery of our children and is available anytime she’s needed.
My neighbor was pleased with his open-heart surgery experience and spoke glowingly of the NP who made rounds daily and assisted during the surgery. He knew the MD surgeon performed most of the operation but left the perioperative care up to the NP.
Patients on a hospitalist service may not see things the same way. My neighbor understood he was hospitalized for the purpose of open-heart surgery done by the MD. He looked at the perioperative care outside of the operation as a secondary issue.
Most medical admissions managed by hospitalists don’t have such clear marquee events in patients’ eyes. So it may be less natural for patients to feel OK about how the hospitalist and NPP divide up care responsibilities. Look at it this way: As hospitalists, we have limited face time with patients, and must make good use of it to establish trust and rapport. When we add an NPP to the care team, we ask patients to develop trust and rapport with two providers instead of just one.
Imagine a patient recently discharged from a hospitalist practice. Her friend asks how it went and which doctor she saw. The patient responds, “I couldn’t figure out who was really in charge of my care. Dr. Nelson’s name was on my armband, but I rarely saw him. Instead, I saw his assistant (the NPP) most of the time.” I suspect that patient will be much less likely to report high levels of satisfaction with her care than one who just saw a hospitalist.
Though I’m concerned that it might be more difficult to keep patients happy when NPPs are part of a hospitalist practice, most practices report this hasn’t been a problem. I’m not suggesting that concern about patient satisfaction means you shouldn’t use NPPs in your hospitalist practices. However, patient satisfaction is an issue to consider when organizing your practice—and an NPP’s role in it—to provide the greatest benefit to your patients. TH
Dr. Nelson has been a practicing hospitalist since 1988 and is co-founder and past president of SHM. He is a principal in Nelson/Flores Associates, a national hospitalist practice management consulting firm. He is also part of the faculty for SHM’s “Best Practices in Managing a Hospital Medicine Program” course. This column represents his views and is not intended to reflect an official position of SHM.
The 4-1-1 on NPPs
I’m convinced it is smart for many hospitalist practices to include nurse practitioners and/or physician assistants. The most common problem I see is that a practice doesn’t execute this idea well. They may have the right idea to add these providers, but they fail to create the right job description, support, and management oversight.
While there are a variety of terms in common use, such as “mid-level” and “allied health professional,” I will use “non-physician provider” (NPP) to refer to both NPs and PAs.
The two most common reasons to add NPPs are a strategy to manage growth in the difficult physician recruiting environment and as a way to optimize practice value (provide the best care at the lowest provider cost).
Valuable Roles?
My anecdotal experience suggests most practices have the NPP function in ways that may not be optimal. Most commonly, the NPP works much like another hospitalist in the practice, admitting and “carrying” their own patient caseload. There is often an attempt to have the NPP care for patients that are somewhat less sick and complicated, or care for a smaller patient volume (though this varies a lot).
This is a great concept, but often proves difficult to implement well. The NPPs in such practices often say their caseload—and amount of supervision and interaction with the physician hospitalists—varies a great deal, depending on which hospitalist is on duty. At times, they may have little interaction, leading to a defacto independent practice. At other times, work done by the NPP is repeated by the physician hospitalist. In either case, the NPP is unable to contribute optimally to the practice.
NPPs in this situation often express uncertainty about their job description and who serves as their physician supervisor. If the NPPs in your practice say their job varies, depending on which doctor is on duty, you’re probably limiting the NPP’s contribution to the practice.
Some practices have the NPP manage only the discharge process (and not provide ongoing patient care), including dictation of the discharge summary, for most or all hospitalist patients. In such a system, the NPP may have had little or no involvement with the patient prior to discharge. A variation on this system is to transfer a patient to the care of the NPP (with physician oversight) a day or two before the anticipated day of discharge and when the acute illness has improved.
While reasonable people can disagree, the problem I see with an NPP dedicated to managing the discharge process is that discharge is often the most complicated visit. Managing it well requires knowing a great deal about the patient’s medical and social situation. Asking any provider, including a physician, to step in on the last day and handle this, and prepare a meaningful discharge summary, is very challenging.
While that is unavoidable in some cases, it seems to me a poor idea to create a system in which it happens routinely for all (or nearly all) patients. I worry that referring doctors may not be pleased if they routinely get discharge summaries prepared by someone who had little or no involvement with the patient prior to the day of discharge. How informative and reliable could such a summary be?
New Alternatives
A few practices have begun asking NPPs to function in less common roles, but ones that may contribute more to the practice and provide the NPP with greater satisfaction.
A common scenario is for the several, day-shift doctors to end their work around 7 p.m. when they’re replaced by a single night doctor. And the number of admissions and “crosscover” burdens tend to be greatest in the late afternoon and early night hours around this shift change. This regularly overwhelms the night doctor for the first few hours of the shift (and the ED gets backed up, and so on).
Relief in the form of an NPP functioning in a “swing shift” role—working from the mid-afternoon until around midnight—may make more sense for some practices than having a physician hospitalist work this shift. The NPP would be responsible for admitting patients (all of whom would be seen by the in-house supervising MD that night) and functioning as the first responder for all “crosscover” issues. The practice could have an NPP work this shift seven days a week, and all other patient visits could be made by the MD hospitalists (i.e., the NPP would not have their own “service” of patients to round on daily).
An NPP could also be put in charge of a consult service, such as serving as the main hospitalist consultant on orthopedic patients that need medical consultants. In this role, the NPP would work nearly all his/her time on a single floor, such as the orthopedic floor, and get to know the orthopedic physicians and nursing staff well. This close communication and working relationship would make the NPP well accepted and effective. While physician oversight would still be required, the NPP would likely take mental ownership of issues, such as response times to consult requests, rates of VTE prophylaxis, perioperative beta-blocker use, etc. This could lead to a rewarding role for the NPP and might result in better clinical performance because it would be “owned” by a single person. It is easy to envision a role like this on other units, such as psychiatry or an in-hospital skilled nursing unit.
Lastly, the NPP might be asked to own issues, such as glycemic control or CMS core measure performance for all hospitalist patients (or all patients in the hospital). He or she might see all diabetic patients daily and adjust glycemic therapy as appropriate, but all of those patients would have a separate MD hospitalist see them daily to care for all other problems.
Room for Opinions
There aren’t much data to guide decisions about the right or best role for NPPs in hospitalist practice. For various reasons including local culture, some practices may function best without including NPPs. Yet, many, or most, practices should thoughtfully consider high value roles for NPPs. I think it is important to avoid a knee-jerk response of simply adding NPPs in the role of additional hospitalists, and instead considering less traditional or novel roles. That is just my opinion (informed by considerable experience with a lot of practices) and reasonable people can see it differently. I’m interested in hearing from anyone with an opinion about optimal NPP roles within hospitalist practices.
Next month I’ll offer comments on the economics of NPPs and thoughts about patient satisfaction with NPPs. TH
Dr. Nelson has been a practicing hospitalist since 1988 and is co-founder and past president of SHM. He is a principal in Nelson/Flores Associates, a national hospitalist practice management consulting firm. He is also part of the faculty for SHM’s “Best Practices in Managing a Hospital Medicine Program” course. This column represents his views and is not intended to reflect an official position of SHM.
I’m convinced it is smart for many hospitalist practices to include nurse practitioners and/or physician assistants. The most common problem I see is that a practice doesn’t execute this idea well. They may have the right idea to add these providers, but they fail to create the right job description, support, and management oversight.
While there are a variety of terms in common use, such as “mid-level” and “allied health professional,” I will use “non-physician provider” (NPP) to refer to both NPs and PAs.
The two most common reasons to add NPPs are a strategy to manage growth in the difficult physician recruiting environment and as a way to optimize practice value (provide the best care at the lowest provider cost).
Valuable Roles?
My anecdotal experience suggests most practices have the NPP function in ways that may not be optimal. Most commonly, the NPP works much like another hospitalist in the practice, admitting and “carrying” their own patient caseload. There is often an attempt to have the NPP care for patients that are somewhat less sick and complicated, or care for a smaller patient volume (though this varies a lot).
This is a great concept, but often proves difficult to implement well. The NPPs in such practices often say their caseload—and amount of supervision and interaction with the physician hospitalists—varies a great deal, depending on which hospitalist is on duty. At times, they may have little interaction, leading to a defacto independent practice. At other times, work done by the NPP is repeated by the physician hospitalist. In either case, the NPP is unable to contribute optimally to the practice.
NPPs in this situation often express uncertainty about their job description and who serves as their physician supervisor. If the NPPs in your practice say their job varies, depending on which doctor is on duty, you’re probably limiting the NPP’s contribution to the practice.
Some practices have the NPP manage only the discharge process (and not provide ongoing patient care), including dictation of the discharge summary, for most or all hospitalist patients. In such a system, the NPP may have had little or no involvement with the patient prior to discharge. A variation on this system is to transfer a patient to the care of the NPP (with physician oversight) a day or two before the anticipated day of discharge and when the acute illness has improved.
While reasonable people can disagree, the problem I see with an NPP dedicated to managing the discharge process is that discharge is often the most complicated visit. Managing it well requires knowing a great deal about the patient’s medical and social situation. Asking any provider, including a physician, to step in on the last day and handle this, and prepare a meaningful discharge summary, is very challenging.
While that is unavoidable in some cases, it seems to me a poor idea to create a system in which it happens routinely for all (or nearly all) patients. I worry that referring doctors may not be pleased if they routinely get discharge summaries prepared by someone who had little or no involvement with the patient prior to the day of discharge. How informative and reliable could such a summary be?
New Alternatives
A few practices have begun asking NPPs to function in less common roles, but ones that may contribute more to the practice and provide the NPP with greater satisfaction.
A common scenario is for the several, day-shift doctors to end their work around 7 p.m. when they’re replaced by a single night doctor. And the number of admissions and “crosscover” burdens tend to be greatest in the late afternoon and early night hours around this shift change. This regularly overwhelms the night doctor for the first few hours of the shift (and the ED gets backed up, and so on).
Relief in the form of an NPP functioning in a “swing shift” role—working from the mid-afternoon until around midnight—may make more sense for some practices than having a physician hospitalist work this shift. The NPP would be responsible for admitting patients (all of whom would be seen by the in-house supervising MD that night) and functioning as the first responder for all “crosscover” issues. The practice could have an NPP work this shift seven days a week, and all other patient visits could be made by the MD hospitalists (i.e., the NPP would not have their own “service” of patients to round on daily).
An NPP could also be put in charge of a consult service, such as serving as the main hospitalist consultant on orthopedic patients that need medical consultants. In this role, the NPP would work nearly all his/her time on a single floor, such as the orthopedic floor, and get to know the orthopedic physicians and nursing staff well. This close communication and working relationship would make the NPP well accepted and effective. While physician oversight would still be required, the NPP would likely take mental ownership of issues, such as response times to consult requests, rates of VTE prophylaxis, perioperative beta-blocker use, etc. This could lead to a rewarding role for the NPP and might result in better clinical performance because it would be “owned” by a single person. It is easy to envision a role like this on other units, such as psychiatry or an in-hospital skilled nursing unit.
Lastly, the NPP might be asked to own issues, such as glycemic control or CMS core measure performance for all hospitalist patients (or all patients in the hospital). He or she might see all diabetic patients daily and adjust glycemic therapy as appropriate, but all of those patients would have a separate MD hospitalist see them daily to care for all other problems.
Room for Opinions
There aren’t much data to guide decisions about the right or best role for NPPs in hospitalist practice. For various reasons including local culture, some practices may function best without including NPPs. Yet, many, or most, practices should thoughtfully consider high value roles for NPPs. I think it is important to avoid a knee-jerk response of simply adding NPPs in the role of additional hospitalists, and instead considering less traditional or novel roles. That is just my opinion (informed by considerable experience with a lot of practices) and reasonable people can see it differently. I’m interested in hearing from anyone with an opinion about optimal NPP roles within hospitalist practices.
Next month I’ll offer comments on the economics of NPPs and thoughts about patient satisfaction with NPPs. TH
Dr. Nelson has been a practicing hospitalist since 1988 and is co-founder and past president of SHM. He is a principal in Nelson/Flores Associates, a national hospitalist practice management consulting firm. He is also part of the faculty for SHM’s “Best Practices in Managing a Hospital Medicine Program” course. This column represents his views and is not intended to reflect an official position of SHM.
I’m convinced it is smart for many hospitalist practices to include nurse practitioners and/or physician assistants. The most common problem I see is that a practice doesn’t execute this idea well. They may have the right idea to add these providers, but they fail to create the right job description, support, and management oversight.
While there are a variety of terms in common use, such as “mid-level” and “allied health professional,” I will use “non-physician provider” (NPP) to refer to both NPs and PAs.
The two most common reasons to add NPPs are a strategy to manage growth in the difficult physician recruiting environment and as a way to optimize practice value (provide the best care at the lowest provider cost).
Valuable Roles?
My anecdotal experience suggests most practices have the NPP function in ways that may not be optimal. Most commonly, the NPP works much like another hospitalist in the practice, admitting and “carrying” their own patient caseload. There is often an attempt to have the NPP care for patients that are somewhat less sick and complicated, or care for a smaller patient volume (though this varies a lot).
This is a great concept, but often proves difficult to implement well. The NPPs in such practices often say their caseload—and amount of supervision and interaction with the physician hospitalists—varies a great deal, depending on which hospitalist is on duty. At times, they may have little interaction, leading to a defacto independent practice. At other times, work done by the NPP is repeated by the physician hospitalist. In either case, the NPP is unable to contribute optimally to the practice.
NPPs in this situation often express uncertainty about their job description and who serves as their physician supervisor. If the NPPs in your practice say their job varies, depending on which doctor is on duty, you’re probably limiting the NPP’s contribution to the practice.
Some practices have the NPP manage only the discharge process (and not provide ongoing patient care), including dictation of the discharge summary, for most or all hospitalist patients. In such a system, the NPP may have had little or no involvement with the patient prior to discharge. A variation on this system is to transfer a patient to the care of the NPP (with physician oversight) a day or two before the anticipated day of discharge and when the acute illness has improved.
While reasonable people can disagree, the problem I see with an NPP dedicated to managing the discharge process is that discharge is often the most complicated visit. Managing it well requires knowing a great deal about the patient’s medical and social situation. Asking any provider, including a physician, to step in on the last day and handle this, and prepare a meaningful discharge summary, is very challenging.
While that is unavoidable in some cases, it seems to me a poor idea to create a system in which it happens routinely for all (or nearly all) patients. I worry that referring doctors may not be pleased if they routinely get discharge summaries prepared by someone who had little or no involvement with the patient prior to the day of discharge. How informative and reliable could such a summary be?
New Alternatives
A few practices have begun asking NPPs to function in less common roles, but ones that may contribute more to the practice and provide the NPP with greater satisfaction.
A common scenario is for the several, day-shift doctors to end their work around 7 p.m. when they’re replaced by a single night doctor. And the number of admissions and “crosscover” burdens tend to be greatest in the late afternoon and early night hours around this shift change. This regularly overwhelms the night doctor for the first few hours of the shift (and the ED gets backed up, and so on).
Relief in the form of an NPP functioning in a “swing shift” role—working from the mid-afternoon until around midnight—may make more sense for some practices than having a physician hospitalist work this shift. The NPP would be responsible for admitting patients (all of whom would be seen by the in-house supervising MD that night) and functioning as the first responder for all “crosscover” issues. The practice could have an NPP work this shift seven days a week, and all other patient visits could be made by the MD hospitalists (i.e., the NPP would not have their own “service” of patients to round on daily).
An NPP could also be put in charge of a consult service, such as serving as the main hospitalist consultant on orthopedic patients that need medical consultants. In this role, the NPP would work nearly all his/her time on a single floor, such as the orthopedic floor, and get to know the orthopedic physicians and nursing staff well. This close communication and working relationship would make the NPP well accepted and effective. While physician oversight would still be required, the NPP would likely take mental ownership of issues, such as response times to consult requests, rates of VTE prophylaxis, perioperative beta-blocker use, etc. This could lead to a rewarding role for the NPP and might result in better clinical performance because it would be “owned” by a single person. It is easy to envision a role like this on other units, such as psychiatry or an in-hospital skilled nursing unit.
Lastly, the NPP might be asked to own issues, such as glycemic control or CMS core measure performance for all hospitalist patients (or all patients in the hospital). He or she might see all diabetic patients daily and adjust glycemic therapy as appropriate, but all of those patients would have a separate MD hospitalist see them daily to care for all other problems.
Room for Opinions
There aren’t much data to guide decisions about the right or best role for NPPs in hospitalist practice. For various reasons including local culture, some practices may function best without including NPPs. Yet, many, or most, practices should thoughtfully consider high value roles for NPPs. I think it is important to avoid a knee-jerk response of simply adding NPPs in the role of additional hospitalists, and instead considering less traditional or novel roles. That is just my opinion (informed by considerable experience with a lot of practices) and reasonable people can see it differently. I’m interested in hearing from anyone with an opinion about optimal NPP roles within hospitalist practices.
Next month I’ll offer comments on the economics of NPPs and thoughts about patient satisfaction with NPPs. TH
Dr. Nelson has been a practicing hospitalist since 1988 and is co-founder and past president of SHM. He is a principal in Nelson/Flores Associates, a national hospitalist practice management consulting firm. He is also part of the faculty for SHM’s “Best Practices in Managing a Hospital Medicine Program” course. This column represents his views and is not intended to reflect an official position of SHM.
Play by the Rules
How does your hospitalist group make decisions on important issues? There are many reasonable approaches. The best method will vary significantly depending on the group’s size and whether the doctors own their own private practice or are employees of a hospital or large multisite private hospitalist group.
Because many doctors are drawn to the profession in part seeking autonomy and independence, there is often a tension between their desire to make many decisions about business and practice operations independently and the need to set aside some personal interests in order for the group to function well. This can become apparent when the group reaches an agreement regarding a difficult issue for which there are different points of view.
Consider a hospitalist group made up of internists occasionally asked to admit teenagers younger than 17. There might be a variety of opinions about whether this is appropriate, but it will be best for everyone in the group to follow the same policy. If the majority decision is that it is reasonable to admit patients as long as they’re post-pubertal, everyone in the group should abide by this policy.
But when called by the emergency department about such a patient, a dissenting hospitalist might feel entitled to decline the admission despite the group’s decision. For this doctor, autonomy trumps cohesive group functioning.
The best approach to individual doctors not feeling bound by the group’s decisions is complex and will vary depending on the situation. But it can be mitigated by ensuring that the group has a clear governance structure and method for reaching controversial decisions.
Group Size Matters
A look at hospitalist groups of varying sizes illustrates the growing complexity of decision-making processes.
Small groups (eight or fewer individuals): Hospitalist groups nearly always start with a small number of doctors (often between one and three at the group’s inception) and find little need for a formal governance structure. They tend to make all important decisions based on consensus.
One risk of making decisions by consensus is that the group may be limited by the lowest common denominator. Even if most doctors in the group want to change something to avoid disadvantaging a doctor with a different point of view, the group may be held back and not make the change. In essence, the group can be ruled by the minority. This may not happen often, and as long as the group keeps this risk in mind it is usually fine to operate on consensus.
Medium-size groups (nine-14): A group this size probably needs to acknowledge that it will be unable to reach consensus on a number of issues and will need a voting system. It can be uncomfortable to jump from a culture of consensus to one of majority rule because the latter means there will be winners and losers. A clear set of rules or bylaws can increase the likelihood that those on the losing end of the issue will comply with the majority.
Large groups (more than 14): A large group usuallys face more complex decisions and has a wider range of opinions. Meetings may drag on as an issue is debated and all members have their say.
For this reason, large groups should consider forming a small executive committee consisting of the group’s leader and several representatives elected by a vote of the whole group. This can be a much more efficient way for the group to reach decisions. The executive committee researches issues and forms recommendations for the whole group. For some issues it might be reasonable for the executive committee’s decisions to be final. For others, the decisions of the executive committee might be presented to the whole group as a recommendation and put to a vote of all members.
It is important for a group of any size to have a clearly designated leader to oversee its operations and meetings and represent the group to external constituents. It’s critical that all groups have a culture of physician ownership even if they are contractual employees of another entity, such as the hospital.
It is best if the leader is not viewed as a boss others work for. That will lead to an employee—not an owner—mentality on the part of the others. TH
Dr. Nelson has been a practicing hospitalist since 1988 and is co-founder and past president of SHM. He is a principal in Nelson/Flores Associates, a national hospitalist practice management consulting firm. He also on the faculty of SHM’s “Best Practices in Managing a Hospital Medicine Program.” This column represents his views and is not intended to reflect an official position of SHM.
How does your hospitalist group make decisions on important issues? There are many reasonable approaches. The best method will vary significantly depending on the group’s size and whether the doctors own their own private practice or are employees of a hospital or large multisite private hospitalist group.
Because many doctors are drawn to the profession in part seeking autonomy and independence, there is often a tension between their desire to make many decisions about business and practice operations independently and the need to set aside some personal interests in order for the group to function well. This can become apparent when the group reaches an agreement regarding a difficult issue for which there are different points of view.
Consider a hospitalist group made up of internists occasionally asked to admit teenagers younger than 17. There might be a variety of opinions about whether this is appropriate, but it will be best for everyone in the group to follow the same policy. If the majority decision is that it is reasonable to admit patients as long as they’re post-pubertal, everyone in the group should abide by this policy.
But when called by the emergency department about such a patient, a dissenting hospitalist might feel entitled to decline the admission despite the group’s decision. For this doctor, autonomy trumps cohesive group functioning.
The best approach to individual doctors not feeling bound by the group’s decisions is complex and will vary depending on the situation. But it can be mitigated by ensuring that the group has a clear governance structure and method for reaching controversial decisions.
Group Size Matters
A look at hospitalist groups of varying sizes illustrates the growing complexity of decision-making processes.
Small groups (eight or fewer individuals): Hospitalist groups nearly always start with a small number of doctors (often between one and three at the group’s inception) and find little need for a formal governance structure. They tend to make all important decisions based on consensus.
One risk of making decisions by consensus is that the group may be limited by the lowest common denominator. Even if most doctors in the group want to change something to avoid disadvantaging a doctor with a different point of view, the group may be held back and not make the change. In essence, the group can be ruled by the minority. This may not happen often, and as long as the group keeps this risk in mind it is usually fine to operate on consensus.
Medium-size groups (nine-14): A group this size probably needs to acknowledge that it will be unable to reach consensus on a number of issues and will need a voting system. It can be uncomfortable to jump from a culture of consensus to one of majority rule because the latter means there will be winners and losers. A clear set of rules or bylaws can increase the likelihood that those on the losing end of the issue will comply with the majority.
Large groups (more than 14): A large group usuallys face more complex decisions and has a wider range of opinions. Meetings may drag on as an issue is debated and all members have their say.
For this reason, large groups should consider forming a small executive committee consisting of the group’s leader and several representatives elected by a vote of the whole group. This can be a much more efficient way for the group to reach decisions. The executive committee researches issues and forms recommendations for the whole group. For some issues it might be reasonable for the executive committee’s decisions to be final. For others, the decisions of the executive committee might be presented to the whole group as a recommendation and put to a vote of all members.
It is important for a group of any size to have a clearly designated leader to oversee its operations and meetings and represent the group to external constituents. It’s critical that all groups have a culture of physician ownership even if they are contractual employees of another entity, such as the hospital.
It is best if the leader is not viewed as a boss others work for. That will lead to an employee—not an owner—mentality on the part of the others. TH
Dr. Nelson has been a practicing hospitalist since 1988 and is co-founder and past president of SHM. He is a principal in Nelson/Flores Associates, a national hospitalist practice management consulting firm. He also on the faculty of SHM’s “Best Practices in Managing a Hospital Medicine Program.” This column represents his views and is not intended to reflect an official position of SHM.
How does your hospitalist group make decisions on important issues? There are many reasonable approaches. The best method will vary significantly depending on the group’s size and whether the doctors own their own private practice or are employees of a hospital or large multisite private hospitalist group.
Because many doctors are drawn to the profession in part seeking autonomy and independence, there is often a tension between their desire to make many decisions about business and practice operations independently and the need to set aside some personal interests in order for the group to function well. This can become apparent when the group reaches an agreement regarding a difficult issue for which there are different points of view.
Consider a hospitalist group made up of internists occasionally asked to admit teenagers younger than 17. There might be a variety of opinions about whether this is appropriate, but it will be best for everyone in the group to follow the same policy. If the majority decision is that it is reasonable to admit patients as long as they’re post-pubertal, everyone in the group should abide by this policy.
But when called by the emergency department about such a patient, a dissenting hospitalist might feel entitled to decline the admission despite the group’s decision. For this doctor, autonomy trumps cohesive group functioning.
The best approach to individual doctors not feeling bound by the group’s decisions is complex and will vary depending on the situation. But it can be mitigated by ensuring that the group has a clear governance structure and method for reaching controversial decisions.
Group Size Matters
A look at hospitalist groups of varying sizes illustrates the growing complexity of decision-making processes.
Small groups (eight or fewer individuals): Hospitalist groups nearly always start with a small number of doctors (often between one and three at the group’s inception) and find little need for a formal governance structure. They tend to make all important decisions based on consensus.
One risk of making decisions by consensus is that the group may be limited by the lowest common denominator. Even if most doctors in the group want to change something to avoid disadvantaging a doctor with a different point of view, the group may be held back and not make the change. In essence, the group can be ruled by the minority. This may not happen often, and as long as the group keeps this risk in mind it is usually fine to operate on consensus.
Medium-size groups (nine-14): A group this size probably needs to acknowledge that it will be unable to reach consensus on a number of issues and will need a voting system. It can be uncomfortable to jump from a culture of consensus to one of majority rule because the latter means there will be winners and losers. A clear set of rules or bylaws can increase the likelihood that those on the losing end of the issue will comply with the majority.
Large groups (more than 14): A large group usuallys face more complex decisions and has a wider range of opinions. Meetings may drag on as an issue is debated and all members have their say.
For this reason, large groups should consider forming a small executive committee consisting of the group’s leader and several representatives elected by a vote of the whole group. This can be a much more efficient way for the group to reach decisions. The executive committee researches issues and forms recommendations for the whole group. For some issues it might be reasonable for the executive committee’s decisions to be final. For others, the decisions of the executive committee might be presented to the whole group as a recommendation and put to a vote of all members.
It is important for a group of any size to have a clearly designated leader to oversee its operations and meetings and represent the group to external constituents. It’s critical that all groups have a culture of physician ownership even if they are contractual employees of another entity, such as the hospital.
It is best if the leader is not viewed as a boss others work for. That will lead to an employee—not an owner—mentality on the part of the others. TH
Dr. Nelson has been a practicing hospitalist since 1988 and is co-founder and past president of SHM. He is a principal in Nelson/Flores Associates, a national hospitalist practice management consulting firm. He also on the faculty of SHM’s “Best Practices in Managing a Hospital Medicine Program.” This column represents his views and is not intended to reflect an official position of SHM.