User login
Continuity Conundrum
Editor’s note: Third of a three-part series.
In the two monthly columns preceding this one, I’ve provided an overview of some ways hospitalist groups distribute new referrals among the providers. This month, I’ll review things that cause some groups to make exceptions to their typical method of distributing patients, and turn from how patients are distributed over 24 hours to thoughts about how they might be assigned over the course of consecutive days worked by a doctor.
Equitable Exceptions
There are a number of reasons groups decide to depart from their typical method of assigning patients. These include:
- “Bouncebacks”;
- One hospitalist is at the cap, others aren’t;
- Consult requested of a specific hospitalist;
- Hospitalists with unique skills (e.g., ICU expertise); and
- A patient “fires” the hospitalist.
There isn’t a standard “hospitalist way” of dealing with these issues, and each group will need to work out its own system. The most common of these issues is “bouncebacks.” Every group should try to have patients readmitted within three or four days of discharge go back to the discharging hospitalist. However, this proves difficult in many cases for several reasons, most commonly because the original discharging doctor might not be working when the patient returns.
The Alpha & Omega
Nearly every hospitalist practice makes some effort to maximize continuity between a single hospitalist and patient over the course of a hospital stay. But the effect of the method of patient assignment on continuity often is overlooked.
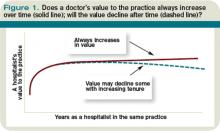
A reasonable way to think about or measure continuity is to estimate the portion of patients seen by the group that see the same hospitalist for each daytime visit over the course of their stay. (Assume that in most HM groups the same hospitalist can’t make both day and night visits over the course of the hospital stay. So, just for simplicity, I’ve intentionally left night visits, including an initial admission visit at night, out of the continuity calculation.) Plug the numbers for your practice into the formula (see Figure 1, right) and see what you get.
If a hospitalist always works seven consecutive day shifts (e.g., a seven-on/seven-off schedule) and the hospitalist’s patients have an average LOS of 4.2 days, then 54% of patients will see the same hospitalist for all daytime visits, and 46% will experience at least one handoff. (To keep things simple, I’m ignoring the effect on continuity of patients being admitted by an “admitter” or nocturnist who doesn’t see the patient subsequently.)
Changing the number of consecutive day shifts a hospitalist works has the most significant impact on continuity, but just how many consecutive days can one work routinely before fatigue and burnout—not too mention increased errors and decreased patient satisfaction—become a problem? (Many hospitalists make the mistake of trying to stuff what might be a reasonable annual workload into the smallest number of shifts possible with the goal of maximizing the number of days off. That means each worked day will be very busy, making it really hard to work many consecutive days. But you always have the option of titrating out that same annual workload over more days so that each day is less busy and it becomes easier to work more consecutive days.)
An often-overlooked way to improve continuity without having to work more consecutive day shifts is to have a hospitalist who is early in their series of worked days take on more new admissions and consults, and perhaps exempt that doctor from taking on new referrals for the last day or two he or she is on service. Eric Howell, MD, FHM, an SHM board member, calls this method “slam and dwindle.” This has been the approach I’ve experienced my whole career, and it is hard for me to imagine doing it any other way.
Here’s how it might work: Let’s say Dr. Petty always works seven consecutive day shifts, and on the first day he picks up a list of patients remaining from the doctor he’s replacing. To keep things simple, let’s assume he’s not in a large group, and during his first day of seven days on service he accepts and “keeps” all new referrals to the practice. On each successive day, he might assume the care of some new patients, but none on days six and seven. This means he takes on a disproportionately large number of new referrals at the beginning of his consecutive worked days, or “front-loads” new referrals. And because many of these patients will discharge before the end of his seven days and he takes on no new patients on days six and seven, his census will drop a lot before he rotates off, which in turn means there will be few patients who will have to get to know a new doctor on the first day Dr. Petty starts his seven-off schedule.
This system of patient distribution means continuity improved without requiring Dr. Petty to work more consecutive day shifts. Even though he works seven consecutive days and his average (or median) LOS is 4.2, as in the example above, his continuity will be much better than 54%. In fact, as many as 70% to 80% of Dr. Petty’s patients will see him for every daytime visit during their stay.
Other benefits of assigning more patients early and none late in a series of worked days are that on his last day of service, he will have more time to “tee up” patients for the next doctor, including preparing for patients anticipated to discharge the next day (e.g., dictate discharge summary, complete paperwork, etc.), and might be able to wrap up a little earlier that day. And when rotating back on service, he will pick up a small list of patients left by Dr. Tench, maybe fewer than eight, rather than the group’s average daily load of 15 patients per doctor, so he will have the capacity to admit a lot of patients that day.
I think there are three main reasons this isn’t a more common approach:
- Many HM groups just haven’t considered it.
- HM groups might have a schedule that has all doctors rotate off/on the same days each week. For example, all doctors rotate off on Tuesdays and are replaced by new doctors on Wednesday. That makes it impossible to exempt a doctor from taking on new referrals on the last day of service because all of the group’s doctors have their last day on Tuesday. These groups could stagger the day each doctor rotates off—one on Monday, one on Tuesday, and so on.
- Every doctor is so busy each day that it wouldn’t be feasible to exempt any individual doctor from taking on new patients, even if they are off the next day.
Despite the difficulties implementing a system of front-loading new referrals, I think most hospitalists would find that they like it. Because it reduces handoffs, it reduces, at least modestly, the group’s overall workload and probably benefits the group’s quality and patient satisfaction. TH
Dr. Nelson has been a practicing hospitalist since 1988 and is co-founder and past president of SHM. He is a principal in Nelson Flores Hospital Medicine Consultants, a national hospitalist practice management consulting firm (www.nelsonflores.com). He is also course co-director and faculty for SHM’s “Best Practices in Managing a Hospital Medicine Program” course. This column represents his views and is not intended to reflect an official position of SHM.
Editor’s note: Third of a three-part series.
In the two monthly columns preceding this one, I’ve provided an overview of some ways hospitalist groups distribute new referrals among the providers. This month, I’ll review things that cause some groups to make exceptions to their typical method of distributing patients, and turn from how patients are distributed over 24 hours to thoughts about how they might be assigned over the course of consecutive days worked by a doctor.
Equitable Exceptions
There are a number of reasons groups decide to depart from their typical method of assigning patients. These include:
- “Bouncebacks”;
- One hospitalist is at the cap, others aren’t;
- Consult requested of a specific hospitalist;
- Hospitalists with unique skills (e.g., ICU expertise); and
- A patient “fires” the hospitalist.
There isn’t a standard “hospitalist way” of dealing with these issues, and each group will need to work out its own system. The most common of these issues is “bouncebacks.” Every group should try to have patients readmitted within three or four days of discharge go back to the discharging hospitalist. However, this proves difficult in many cases for several reasons, most commonly because the original discharging doctor might not be working when the patient returns.
The Alpha & Omega
Nearly every hospitalist practice makes some effort to maximize continuity between a single hospitalist and patient over the course of a hospital stay. But the effect of the method of patient assignment on continuity often is overlooked.
A reasonable way to think about or measure continuity is to estimate the portion of patients seen by the group that see the same hospitalist for each daytime visit over the course of their stay. (Assume that in most HM groups the same hospitalist can’t make both day and night visits over the course of the hospital stay. So, just for simplicity, I’ve intentionally left night visits, including an initial admission visit at night, out of the continuity calculation.) Plug the numbers for your practice into the formula (see Figure 1, right) and see what you get.
If a hospitalist always works seven consecutive day shifts (e.g., a seven-on/seven-off schedule) and the hospitalist’s patients have an average LOS of 4.2 days, then 54% of patients will see the same hospitalist for all daytime visits, and 46% will experience at least one handoff. (To keep things simple, I’m ignoring the effect on continuity of patients being admitted by an “admitter” or nocturnist who doesn’t see the patient subsequently.)
Changing the number of consecutive day shifts a hospitalist works has the most significant impact on continuity, but just how many consecutive days can one work routinely before fatigue and burnout—not too mention increased errors and decreased patient satisfaction—become a problem? (Many hospitalists make the mistake of trying to stuff what might be a reasonable annual workload into the smallest number of shifts possible with the goal of maximizing the number of days off. That means each worked day will be very busy, making it really hard to work many consecutive days. But you always have the option of titrating out that same annual workload over more days so that each day is less busy and it becomes easier to work more consecutive days.)
An often-overlooked way to improve continuity without having to work more consecutive day shifts is to have a hospitalist who is early in their series of worked days take on more new admissions and consults, and perhaps exempt that doctor from taking on new referrals for the last day or two he or she is on service. Eric Howell, MD, FHM, an SHM board member, calls this method “slam and dwindle.” This has been the approach I’ve experienced my whole career, and it is hard for me to imagine doing it any other way.
Here’s how it might work: Let’s say Dr. Petty always works seven consecutive day shifts, and on the first day he picks up a list of patients remaining from the doctor he’s replacing. To keep things simple, let’s assume he’s not in a large group, and during his first day of seven days on service he accepts and “keeps” all new referrals to the practice. On each successive day, he might assume the care of some new patients, but none on days six and seven. This means he takes on a disproportionately large number of new referrals at the beginning of his consecutive worked days, or “front-loads” new referrals. And because many of these patients will discharge before the end of his seven days and he takes on no new patients on days six and seven, his census will drop a lot before he rotates off, which in turn means there will be few patients who will have to get to know a new doctor on the first day Dr. Petty starts his seven-off schedule.
This system of patient distribution means continuity improved without requiring Dr. Petty to work more consecutive day shifts. Even though he works seven consecutive days and his average (or median) LOS is 4.2, as in the example above, his continuity will be much better than 54%. In fact, as many as 70% to 80% of Dr. Petty’s patients will see him for every daytime visit during their stay.
Other benefits of assigning more patients early and none late in a series of worked days are that on his last day of service, he will have more time to “tee up” patients for the next doctor, including preparing for patients anticipated to discharge the next day (e.g., dictate discharge summary, complete paperwork, etc.), and might be able to wrap up a little earlier that day. And when rotating back on service, he will pick up a small list of patients left by Dr. Tench, maybe fewer than eight, rather than the group’s average daily load of 15 patients per doctor, so he will have the capacity to admit a lot of patients that day.
I think there are three main reasons this isn’t a more common approach:
- Many HM groups just haven’t considered it.
- HM groups might have a schedule that has all doctors rotate off/on the same days each week. For example, all doctors rotate off on Tuesdays and are replaced by new doctors on Wednesday. That makes it impossible to exempt a doctor from taking on new referrals on the last day of service because all of the group’s doctors have their last day on Tuesday. These groups could stagger the day each doctor rotates off—one on Monday, one on Tuesday, and so on.
- Every doctor is so busy each day that it wouldn’t be feasible to exempt any individual doctor from taking on new patients, even if they are off the next day.
Despite the difficulties implementing a system of front-loading new referrals, I think most hospitalists would find that they like it. Because it reduces handoffs, it reduces, at least modestly, the group’s overall workload and probably benefits the group’s quality and patient satisfaction. TH
Dr. Nelson has been a practicing hospitalist since 1988 and is co-founder and past president of SHM. He is a principal in Nelson Flores Hospital Medicine Consultants, a national hospitalist practice management consulting firm (www.nelsonflores.com). He is also course co-director and faculty for SHM’s “Best Practices in Managing a Hospital Medicine Program” course. This column represents his views and is not intended to reflect an official position of SHM.
Editor’s note: Third of a three-part series.
In the two monthly columns preceding this one, I’ve provided an overview of some ways hospitalist groups distribute new referrals among the providers. This month, I’ll review things that cause some groups to make exceptions to their typical method of distributing patients, and turn from how patients are distributed over 24 hours to thoughts about how they might be assigned over the course of consecutive days worked by a doctor.
Equitable Exceptions
There are a number of reasons groups decide to depart from their typical method of assigning patients. These include:
- “Bouncebacks”;
- One hospitalist is at the cap, others aren’t;
- Consult requested of a specific hospitalist;
- Hospitalists with unique skills (e.g., ICU expertise); and
- A patient “fires” the hospitalist.
There isn’t a standard “hospitalist way” of dealing with these issues, and each group will need to work out its own system. The most common of these issues is “bouncebacks.” Every group should try to have patients readmitted within three or four days of discharge go back to the discharging hospitalist. However, this proves difficult in many cases for several reasons, most commonly because the original discharging doctor might not be working when the patient returns.
The Alpha & Omega
Nearly every hospitalist practice makes some effort to maximize continuity between a single hospitalist and patient over the course of a hospital stay. But the effect of the method of patient assignment on continuity often is overlooked.
A reasonable way to think about or measure continuity is to estimate the portion of patients seen by the group that see the same hospitalist for each daytime visit over the course of their stay. (Assume that in most HM groups the same hospitalist can’t make both day and night visits over the course of the hospital stay. So, just for simplicity, I’ve intentionally left night visits, including an initial admission visit at night, out of the continuity calculation.) Plug the numbers for your practice into the formula (see Figure 1, right) and see what you get.
If a hospitalist always works seven consecutive day shifts (e.g., a seven-on/seven-off schedule) and the hospitalist’s patients have an average LOS of 4.2 days, then 54% of patients will see the same hospitalist for all daytime visits, and 46% will experience at least one handoff. (To keep things simple, I’m ignoring the effect on continuity of patients being admitted by an “admitter” or nocturnist who doesn’t see the patient subsequently.)
Changing the number of consecutive day shifts a hospitalist works has the most significant impact on continuity, but just how many consecutive days can one work routinely before fatigue and burnout—not too mention increased errors and decreased patient satisfaction—become a problem? (Many hospitalists make the mistake of trying to stuff what might be a reasonable annual workload into the smallest number of shifts possible with the goal of maximizing the number of days off. That means each worked day will be very busy, making it really hard to work many consecutive days. But you always have the option of titrating out that same annual workload over more days so that each day is less busy and it becomes easier to work more consecutive days.)
An often-overlooked way to improve continuity without having to work more consecutive day shifts is to have a hospitalist who is early in their series of worked days take on more new admissions and consults, and perhaps exempt that doctor from taking on new referrals for the last day or two he or she is on service. Eric Howell, MD, FHM, an SHM board member, calls this method “slam and dwindle.” This has been the approach I’ve experienced my whole career, and it is hard for me to imagine doing it any other way.
Here’s how it might work: Let’s say Dr. Petty always works seven consecutive day shifts, and on the first day he picks up a list of patients remaining from the doctor he’s replacing. To keep things simple, let’s assume he’s not in a large group, and during his first day of seven days on service he accepts and “keeps” all new referrals to the practice. On each successive day, he might assume the care of some new patients, but none on days six and seven. This means he takes on a disproportionately large number of new referrals at the beginning of his consecutive worked days, or “front-loads” new referrals. And because many of these patients will discharge before the end of his seven days and he takes on no new patients on days six and seven, his census will drop a lot before he rotates off, which in turn means there will be few patients who will have to get to know a new doctor on the first day Dr. Petty starts his seven-off schedule.
This system of patient distribution means continuity improved without requiring Dr. Petty to work more consecutive day shifts. Even though he works seven consecutive days and his average (or median) LOS is 4.2, as in the example above, his continuity will be much better than 54%. In fact, as many as 70% to 80% of Dr. Petty’s patients will see him for every daytime visit during their stay.
Other benefits of assigning more patients early and none late in a series of worked days are that on his last day of service, he will have more time to “tee up” patients for the next doctor, including preparing for patients anticipated to discharge the next day (e.g., dictate discharge summary, complete paperwork, etc.), and might be able to wrap up a little earlier that day. And when rotating back on service, he will pick up a small list of patients left by Dr. Tench, maybe fewer than eight, rather than the group’s average daily load of 15 patients per doctor, so he will have the capacity to admit a lot of patients that day.
I think there are three main reasons this isn’t a more common approach:
- Many HM groups just haven’t considered it.
- HM groups might have a schedule that has all doctors rotate off/on the same days each week. For example, all doctors rotate off on Tuesdays and are replaced by new doctors on Wednesday. That makes it impossible to exempt a doctor from taking on new referrals on the last day of service because all of the group’s doctors have their last day on Tuesday. These groups could stagger the day each doctor rotates off—one on Monday, one on Tuesday, and so on.
- Every doctor is so busy each day that it wouldn’t be feasible to exempt any individual doctor from taking on new patients, even if they are off the next day.
Despite the difficulties implementing a system of front-loading new referrals, I think most hospitalists would find that they like it. Because it reduces handoffs, it reduces, at least modestly, the group’s overall workload and probably benefits the group’s quality and patient satisfaction. TH
Dr. Nelson has been a practicing hospitalist since 1988 and is co-founder and past president of SHM. He is a principal in Nelson Flores Hospital Medicine Consultants, a national hospitalist practice management consulting firm (www.nelsonflores.com). He is also course co-director and faculty for SHM’s “Best Practices in Managing a Hospital Medicine Program” course. This column represents his views and is not intended to reflect an official position of SHM.
New Referral Distribution
Editor’s note: Second of a three-part series.
As I mentioned last month, there isn’t a proven best method to use when distributing new referrals among your group’s providers. The popular methods fall along a continuum of being focused on daily, or continuous, leveling of patient loads between providers (“load leveling”) at one end; at the other end of the continuum is having a doctor be “on” for all new referrals for a predetermined time period, and accepting that patient volumes might be uneven day to day but tend to even out over long periods.
There might not be any reason to change your group’s approach to patient assignment, but you should always be thinking about how your own methods might be changed or improved. I have shared (“Bigger Isn’t Always Better,” June 2009, p. 46) my concern that some groups invest far too much time in a morning load-leveling and handoff conference. Make sure your group is using only as much time as needed.
Air-Traffic Controllers
Many large groups (e.g., more than 15 full-time equivalents) that assign patients to providers in sequence, like dealing a deck of cards, have a designated provider who holds the triage pager and serves as “air-traffic controller.” This person typically takes incoming calls about all new referrals, jots down the relevant clinical data, keeps track of which hospitalist is due to take the next patient, pages that person, and repeats the clinical information. As I’ve written before (“How to Hire and Use Clerical Staff,” June 2007, p. 73), many practices have found that during business hours, they can hand this role to a clerical person who simply takes down the name and phone number of the doctor making the referral, then pages that information to the hospitalist due to get the next patient. The hospitalist then calls and speaks directly with the referring doctor.
Small- to medium-sized groups can eliminate entirely the need for any such “air-traffic control” function if they assign all new referrals to a single doctor for specified periods of time. For example, from 7 a.m. to 3 p.m. today, all new referrals go to Dr. Glass, and from 3 p.m. to 11 p.m., they go to Dr. Cage.
Admitter-Rounder Duties
Many—maybe most?—large groups separate daytime admitter and rounder functions so that on any given day, a hospitalist does one but not both. The principal advantages of this approach are reducing the stress on, and possibly increasing the efficiency of, rounding doctors by shielding them from the unpredictable and time-consuming interruption of needing to admit a new patient. And a daytime doctor who only does admissions might be able to start seeing a patient in the ED more quickly than one who is busy making rounds.
Any increased availability of admitters to the ED could be offset by their lack of surge capacity leading to a bottleneck in ED throughput when there are many patients to admit at the same time and a limited number of admitters (often only one). Such a bottleneck would be much less likely if all daytime doctors (i.e., the rounders) were available to see admissions rather than just admitters.
Continuity of care suffers when a group has separate admitters and rounders, because no patients will be seen by the same doctor on the day of admission and the day following. This method requires a handoff from the day of admission to the next day. Such a handoff might be unavoidable for patients admitted during the night, but this doesn’t have to occur when patients are admitted during the daytime.
Who’s Seeing this Patient?
It seems to make sense to wait until each morning to distribute patients. That allows the practice to know just how many new patients there are, and they can be distributed according to complexity and whether a hospitalist has formed a previous relationship with that patient. But it means that no one at the hospital will know which hospitalist is caring for the patient until later in the morning. For example, if the radiologist is over-reading a study done during the night and finds something worthy of a phone call to the hospitalist, no one is sure who should get the call. A patient might develop hypoglycemia shortly after the hospitalist night shift is over, but the nurse doesn’t know which hospitalist to call.
And, perhaps most importantly, if patients aren’t distributed until the start of the day shift, the night hospitalist can’t tell the patient and family which hospitalist to expect the next morning. To test the significance of this issue, I conducted an experiment while working our group’s late-evening admitter shift. I concluded my visit with each admitted patient by explaining, “I am on-call for our group tonight, so I will be off recovering tomorrow. Therefore, I won’t see you again, but one of my partners will take over in the morning. Do you have any questions for me?” Every patient I admitted had the same question. “What is that doctor’s name?”
How does your group answer a patient who asks which hospitalist will be in the next day? If your method is load-leveling in the morning, then the best answer your night admitting doctor can give is probably to say: “I don’t know which of my partners will be in. There are several working tomorrow, and at the start of the day, they will divide up the patients who come in tonight depending on how busy each of them is. But all the doctors in our group are terrific and will take good care of you.”
I’m told the same thing when I get my hair cut: You’ll get whichever “hair artist” is up next. I put up with it at the hair place because it costs less than $15. But I still find it a little irritating. I’m sure all the barbers aren’t equally skilled or diligent, and I want the best one. (Maybe I shouldn’t care since there isn’t much that can be done with my hair.) I’m pretty sure patients feel the same way about which doctor they get. The public is convinced there is a wide variety in the quality of doctors, and they want a good one. If you have to tell them theirs is being assigned by lottery, they won’t be as happy than if you can provide the name and a little information about the doctor they can expect to see the next day.
When the patients I admit late last evening ask who would see them the next day, I’m glad when I can provide a name and a little more information. I say something like, “I won’t see you after tonight, but my partner, Dr. Shawn Lee, will be instead. That means you’re getting an upgrade! Not only is he a really nice guy, he’s voted one of Seattle’s best doctors every year. He’ll do a great job for you.”
To make this communication effective, the night doctor has to know which hospitalist takes over the next morning and has a list indicating which day doctor will get the first, second, third new patient, and so on, admitted during the night. This is possible if patients are assigned by a predetermined algorithm, or if the day doctors have their load-leveling meeting at the end of each day shift, rather than in the morning, to create a list telling the night doctor which day hospitalist he should admit the first and subsequent patents to. That way, the night doctor can write in the admitting orders at 1 a.m. “admit to Dr. X.” This eliminates confusion on the part of other hospital staff who need to know who to call about a patient after the start of the day shift.
Next month I will look at special circumstances, and some pros and cons of having an individual hospitalist take on the care of more patients at the beginning of consecutive day shifts, and exempting them from taking on new patients on the last day or two before rotating off. TH
Dr. Nelson has been a practicing hospitalist since 1988 and is co-founder and past president of SHM. He is a principal in Nelson Flores Hospital Medicine Consultants, a national hospitalist practice management consulting firm (www.nelsonflores.com). He is also course co-director and faculty for SHM’s “Best Practices in Managing a Hospital Medicine Program” course. This column represents his views and is not intended to reflect an official position of SHM.
Editor’s note: Second of a three-part series.
As I mentioned last month, there isn’t a proven best method to use when distributing new referrals among your group’s providers. The popular methods fall along a continuum of being focused on daily, or continuous, leveling of patient loads between providers (“load leveling”) at one end; at the other end of the continuum is having a doctor be “on” for all new referrals for a predetermined time period, and accepting that patient volumes might be uneven day to day but tend to even out over long periods.
There might not be any reason to change your group’s approach to patient assignment, but you should always be thinking about how your own methods might be changed or improved. I have shared (“Bigger Isn’t Always Better,” June 2009, p. 46) my concern that some groups invest far too much time in a morning load-leveling and handoff conference. Make sure your group is using only as much time as needed.
Air-Traffic Controllers
Many large groups (e.g., more than 15 full-time equivalents) that assign patients to providers in sequence, like dealing a deck of cards, have a designated provider who holds the triage pager and serves as “air-traffic controller.” This person typically takes incoming calls about all new referrals, jots down the relevant clinical data, keeps track of which hospitalist is due to take the next patient, pages that person, and repeats the clinical information. As I’ve written before (“How to Hire and Use Clerical Staff,” June 2007, p. 73), many practices have found that during business hours, they can hand this role to a clerical person who simply takes down the name and phone number of the doctor making the referral, then pages that information to the hospitalist due to get the next patient. The hospitalist then calls and speaks directly with the referring doctor.
Small- to medium-sized groups can eliminate entirely the need for any such “air-traffic control” function if they assign all new referrals to a single doctor for specified periods of time. For example, from 7 a.m. to 3 p.m. today, all new referrals go to Dr. Glass, and from 3 p.m. to 11 p.m., they go to Dr. Cage.
Admitter-Rounder Duties
Many—maybe most?—large groups separate daytime admitter and rounder functions so that on any given day, a hospitalist does one but not both. The principal advantages of this approach are reducing the stress on, and possibly increasing the efficiency of, rounding doctors by shielding them from the unpredictable and time-consuming interruption of needing to admit a new patient. And a daytime doctor who only does admissions might be able to start seeing a patient in the ED more quickly than one who is busy making rounds.
Any increased availability of admitters to the ED could be offset by their lack of surge capacity leading to a bottleneck in ED throughput when there are many patients to admit at the same time and a limited number of admitters (often only one). Such a bottleneck would be much less likely if all daytime doctors (i.e., the rounders) were available to see admissions rather than just admitters.
Continuity of care suffers when a group has separate admitters and rounders, because no patients will be seen by the same doctor on the day of admission and the day following. This method requires a handoff from the day of admission to the next day. Such a handoff might be unavoidable for patients admitted during the night, but this doesn’t have to occur when patients are admitted during the daytime.
Who’s Seeing this Patient?
It seems to make sense to wait until each morning to distribute patients. That allows the practice to know just how many new patients there are, and they can be distributed according to complexity and whether a hospitalist has formed a previous relationship with that patient. But it means that no one at the hospital will know which hospitalist is caring for the patient until later in the morning. For example, if the radiologist is over-reading a study done during the night and finds something worthy of a phone call to the hospitalist, no one is sure who should get the call. A patient might develop hypoglycemia shortly after the hospitalist night shift is over, but the nurse doesn’t know which hospitalist to call.
And, perhaps most importantly, if patients aren’t distributed until the start of the day shift, the night hospitalist can’t tell the patient and family which hospitalist to expect the next morning. To test the significance of this issue, I conducted an experiment while working our group’s late-evening admitter shift. I concluded my visit with each admitted patient by explaining, “I am on-call for our group tonight, so I will be off recovering tomorrow. Therefore, I won’t see you again, but one of my partners will take over in the morning. Do you have any questions for me?” Every patient I admitted had the same question. “What is that doctor’s name?”
How does your group answer a patient who asks which hospitalist will be in the next day? If your method is load-leveling in the morning, then the best answer your night admitting doctor can give is probably to say: “I don’t know which of my partners will be in. There are several working tomorrow, and at the start of the day, they will divide up the patients who come in tonight depending on how busy each of them is. But all the doctors in our group are terrific and will take good care of you.”
I’m told the same thing when I get my hair cut: You’ll get whichever “hair artist” is up next. I put up with it at the hair place because it costs less than $15. But I still find it a little irritating. I’m sure all the barbers aren’t equally skilled or diligent, and I want the best one. (Maybe I shouldn’t care since there isn’t much that can be done with my hair.) I’m pretty sure patients feel the same way about which doctor they get. The public is convinced there is a wide variety in the quality of doctors, and they want a good one. If you have to tell them theirs is being assigned by lottery, they won’t be as happy than if you can provide the name and a little information about the doctor they can expect to see the next day.
When the patients I admit late last evening ask who would see them the next day, I’m glad when I can provide a name and a little more information. I say something like, “I won’t see you after tonight, but my partner, Dr. Shawn Lee, will be instead. That means you’re getting an upgrade! Not only is he a really nice guy, he’s voted one of Seattle’s best doctors every year. He’ll do a great job for you.”
To make this communication effective, the night doctor has to know which hospitalist takes over the next morning and has a list indicating which day doctor will get the first, second, third new patient, and so on, admitted during the night. This is possible if patients are assigned by a predetermined algorithm, or if the day doctors have their load-leveling meeting at the end of each day shift, rather than in the morning, to create a list telling the night doctor which day hospitalist he should admit the first and subsequent patents to. That way, the night doctor can write in the admitting orders at 1 a.m. “admit to Dr. X.” This eliminates confusion on the part of other hospital staff who need to know who to call about a patient after the start of the day shift.
Next month I will look at special circumstances, and some pros and cons of having an individual hospitalist take on the care of more patients at the beginning of consecutive day shifts, and exempting them from taking on new patients on the last day or two before rotating off. TH
Dr. Nelson has been a practicing hospitalist since 1988 and is co-founder and past president of SHM. He is a principal in Nelson Flores Hospital Medicine Consultants, a national hospitalist practice management consulting firm (www.nelsonflores.com). He is also course co-director and faculty for SHM’s “Best Practices in Managing a Hospital Medicine Program” course. This column represents his views and is not intended to reflect an official position of SHM.
Editor’s note: Second of a three-part series.
As I mentioned last month, there isn’t a proven best method to use when distributing new referrals among your group’s providers. The popular methods fall along a continuum of being focused on daily, or continuous, leveling of patient loads between providers (“load leveling”) at one end; at the other end of the continuum is having a doctor be “on” for all new referrals for a predetermined time period, and accepting that patient volumes might be uneven day to day but tend to even out over long periods.
There might not be any reason to change your group’s approach to patient assignment, but you should always be thinking about how your own methods might be changed or improved. I have shared (“Bigger Isn’t Always Better,” June 2009, p. 46) my concern that some groups invest far too much time in a morning load-leveling and handoff conference. Make sure your group is using only as much time as needed.
Air-Traffic Controllers
Many large groups (e.g., more than 15 full-time equivalents) that assign patients to providers in sequence, like dealing a deck of cards, have a designated provider who holds the triage pager and serves as “air-traffic controller.” This person typically takes incoming calls about all new referrals, jots down the relevant clinical data, keeps track of which hospitalist is due to take the next patient, pages that person, and repeats the clinical information. As I’ve written before (“How to Hire and Use Clerical Staff,” June 2007, p. 73), many practices have found that during business hours, they can hand this role to a clerical person who simply takes down the name and phone number of the doctor making the referral, then pages that information to the hospitalist due to get the next patient. The hospitalist then calls and speaks directly with the referring doctor.
Small- to medium-sized groups can eliminate entirely the need for any such “air-traffic control” function if they assign all new referrals to a single doctor for specified periods of time. For example, from 7 a.m. to 3 p.m. today, all new referrals go to Dr. Glass, and from 3 p.m. to 11 p.m., they go to Dr. Cage.
Admitter-Rounder Duties
Many—maybe most?—large groups separate daytime admitter and rounder functions so that on any given day, a hospitalist does one but not both. The principal advantages of this approach are reducing the stress on, and possibly increasing the efficiency of, rounding doctors by shielding them from the unpredictable and time-consuming interruption of needing to admit a new patient. And a daytime doctor who only does admissions might be able to start seeing a patient in the ED more quickly than one who is busy making rounds.
Any increased availability of admitters to the ED could be offset by their lack of surge capacity leading to a bottleneck in ED throughput when there are many patients to admit at the same time and a limited number of admitters (often only one). Such a bottleneck would be much less likely if all daytime doctors (i.e., the rounders) were available to see admissions rather than just admitters.
Continuity of care suffers when a group has separate admitters and rounders, because no patients will be seen by the same doctor on the day of admission and the day following. This method requires a handoff from the day of admission to the next day. Such a handoff might be unavoidable for patients admitted during the night, but this doesn’t have to occur when patients are admitted during the daytime.
Who’s Seeing this Patient?
It seems to make sense to wait until each morning to distribute patients. That allows the practice to know just how many new patients there are, and they can be distributed according to complexity and whether a hospitalist has formed a previous relationship with that patient. But it means that no one at the hospital will know which hospitalist is caring for the patient until later in the morning. For example, if the radiologist is over-reading a study done during the night and finds something worthy of a phone call to the hospitalist, no one is sure who should get the call. A patient might develop hypoglycemia shortly after the hospitalist night shift is over, but the nurse doesn’t know which hospitalist to call.
And, perhaps most importantly, if patients aren’t distributed until the start of the day shift, the night hospitalist can’t tell the patient and family which hospitalist to expect the next morning. To test the significance of this issue, I conducted an experiment while working our group’s late-evening admitter shift. I concluded my visit with each admitted patient by explaining, “I am on-call for our group tonight, so I will be off recovering tomorrow. Therefore, I won’t see you again, but one of my partners will take over in the morning. Do you have any questions for me?” Every patient I admitted had the same question. “What is that doctor’s name?”
How does your group answer a patient who asks which hospitalist will be in the next day? If your method is load-leveling in the morning, then the best answer your night admitting doctor can give is probably to say: “I don’t know which of my partners will be in. There are several working tomorrow, and at the start of the day, they will divide up the patients who come in tonight depending on how busy each of them is. But all the doctors in our group are terrific and will take good care of you.”
I’m told the same thing when I get my hair cut: You’ll get whichever “hair artist” is up next. I put up with it at the hair place because it costs less than $15. But I still find it a little irritating. I’m sure all the barbers aren’t equally skilled or diligent, and I want the best one. (Maybe I shouldn’t care since there isn’t much that can be done with my hair.) I’m pretty sure patients feel the same way about which doctor they get. The public is convinced there is a wide variety in the quality of doctors, and they want a good one. If you have to tell them theirs is being assigned by lottery, they won’t be as happy than if you can provide the name and a little information about the doctor they can expect to see the next day.
When the patients I admit late last evening ask who would see them the next day, I’m glad when I can provide a name and a little more information. I say something like, “I won’t see you after tonight, but my partner, Dr. Shawn Lee, will be instead. That means you’re getting an upgrade! Not only is he a really nice guy, he’s voted one of Seattle’s best doctors every year. He’ll do a great job for you.”
To make this communication effective, the night doctor has to know which hospitalist takes over the next morning and has a list indicating which day doctor will get the first, second, third new patient, and so on, admitted during the night. This is possible if patients are assigned by a predetermined algorithm, or if the day doctors have their load-leveling meeting at the end of each day shift, rather than in the morning, to create a list telling the night doctor which day hospitalist he should admit the first and subsequent patents to. That way, the night doctor can write in the admitting orders at 1 a.m. “admit to Dr. X.” This eliminates confusion on the part of other hospital staff who need to know who to call about a patient after the start of the day shift.
Next month I will look at special circumstances, and some pros and cons of having an individual hospitalist take on the care of more patients at the beginning of consecutive day shifts, and exempting them from taking on new patients on the last day or two before rotating off. TH
Dr. Nelson has been a practicing hospitalist since 1988 and is co-founder and past president of SHM. He is a principal in Nelson Flores Hospital Medicine Consultants, a national hospitalist practice management consulting firm (www.nelsonflores.com). He is also course co-director and faculty for SHM’s “Best Practices in Managing a Hospital Medicine Program” course. This column represents his views and is not intended to reflect an official position of SHM.
Patient Distribution
Editor’s note: This is the first of a three-part series.
My experience is that some, maybe even most, hospitalists tend to assume there is a standard or “right” way to organize things like work schedules, compensation, or even the assignment of patients among the group’s providers. Some will say things like “SHM says the best hospitalist schedule is …” or “The best way to compensate hospitalists is …”
But there really isn’t a “best” way to manage any particular attribute of a practice. Don’t make the mistake of assuming your method is best, or that it’s the way “everybody else does it.” Although scheduling and compensation are marquee issues for hospitalists, approaches to distributing new patients is much less visible. Many groups tend to assume their method is the only reasonable approach. The best approach, however, varies from one practice to the next. You should be open to hearing approaches to scheduling that are different from your own.
Assign Patients by “Load Leveling”
I’ve come across a lot—and I mean a lot—of different approaches to distributing new patients in HM groups around the country, but it seems pretty clear that the most common method is to undertake “load leveling” on a daily or ongoing basis.
For example, groups that have a separate night shift (the night doctor performs no daytime work the day before or the day after a night shift) typically distribute the night’s new patients with the intent of having each daytime doctor start with the same number of patients. The group might more heavily weight some patients, such as those in the ICU (e.g., each ICU patient counts as 1.5 or two non-ICU patients), but most groups don’t. Over the course of the day shift, new referrals will be distributed evenly among the doctors one at a time, sort of like dealing a deck of cards.
This approach aims to avoid significant imbalances in patient loads and has the potential cultural benefit of everyone sharing equally in busy and slow days. Groups that use it tend to see it as the best option because it is the fairest way to divide up the workload.
Practices that use load-leveling almost always use a schedule built on shifts of a predetermined and fixed duration. For example, say the day shift always works from 7 a.m. to 7 p.m. This schedule usually has the majority of compensation paid via a fixed annual salary or fixed shift rate. One potential problem with this approach is that the doctor who is efficient and discharges a lot of patients today is “rewarded” with more new patients tomorrow. Hospitalists who are allergic to work might have an incentive to have a patient wait until tomorrow to discharge to avoid having to assume the care of yet another patient tomorrow morning. Hospital executives who are focused on length-of-stay management might be concerned if they knew this was a potential issue. Of course, the reverse is true as well. In a practice that doesn’t aggressively undertake load-leveling, a less-than-admirable hospitalist could push patients to discharge earlier than optimal just to have one less patient the next day.
Another cost of this approach is that the distribution of patients can be time-consuming each morning. It also offers the opportunity for some in the group to decide they’re treated unfairly. For instance, you might hear the occasional “just last Tuesday, I started with 16 patients, compared with 15 for everyone else. Now you want me to do it again? You’re being unfair to me; it’s someone else’s turn to take the extra patient.”
Assignment by Location
Groups that use “unit-based” hospitalists distribute patients according to the unit the patient is admitted to—and the hospitalist covering that unit. The pros and cons of unit-based hospitalists are many (see “A Unit-Based Approach,” September 2007), but there is an obvious tension between keeping patient loads even among hospitalists and ensuring that all of a hospitalist’s patients are on “their” unit. Practicality usually requires a compromise between pure unit-based assignment and load-leveling.
Uneven Assignments
Some groups assign patients according to a predetermined algorithm and employ load-leveling only when patient loads become extremely unbalanced. For example, Dr. Jones gets all the new referrals today, and Dr. James gets them tomorrow. The idea is that patient loads end up close to even over time, even if they’re unbalanced on any given day.
A system like this allows everyone, including the hospitalists themselves, ED staff, etc., to know who will take the next patient. It decreases the need to communicate the “who’s next” information time after time during the course of the day. In small- to medium-sized practices, it could mean no one needs to function as the triage doctor (i.e., the person who inefficiently answers the service calls, scribbles down clinical information, then calls the hospitalist who is due to take the next patient and relays all the pertinent patient info). This system allows the
hospitalists to know which days will be harder (e.g., taking on the care of new patients) and which days will be easier (e.g., rounding but not assuming care of new patients). Allowing uneven loads also eliminates the need to spend energy working to even the loads and risking that some in the group feel as if they aren’t being treated fairly.
Uncommon yet Intriguing Approaches
Pair referring primary-care physicians (PCPs) with specific hospitalists. I’ve encountered two groups that had hospitalists always admit patients from the same PCPs. In other words, hospitalist Dr. Hancock always serves as attending for patients referred by the same nine PCPs, and hospitalist Dr. Franklin always attends to patients from a different set of PCPs. It seems to me that there could be tremendous benefit in working closely with the same PCPs, most notably getting to know the PCPs’ office staff. But this system raises the risk of creating out-of-balance patient loads, among other problems. It is really attractive to me, but most groups will decide its costs outweigh its benefits.
Hospitalist and patient stay connected during admission. I’m not aware of any group that uses this method (let me know if you do!), but there could be benefits to having each patient see the same hospitalist during each hospital stay. Of course, that is assuming the hospitalist is on duty. Hospitalist and patient could be paired upon the patient’s first admission. The hospitalist could form an excellent relationship with the patient and family; the time spent by the hospitalist getting to know patients on admission would be reduced, and I suspect there might be some benefit in the quality of care.
This method, however, likely results in the most uneven patient loads, and load-leveling would be difficult, if not impossible. Even if hospitalist and patient did form a tight bond, there is a high probability that the hospitalist would be off for the duration of the patient’s next admission. So despite what I suspect are tremendous benefits, this approach may not be feasible for any group.
In next month’s column, I will discuss issues related to the way patients are distributed. TH
Dr. Nelson has been a practicing hospitalist since 1988 and is co-founder and past president of SHM. He is a principal in Nelson Flores Hospital Medicine Consultants, a national hospitalist practice management consulting firm (www.nelsonflores.com). He is co-director and faculty for SHM’s “Best Practices in Managing a Hospital Medicine Program” course. This column represents his views and is not intended to reflect an official position of SHM.
Editor’s note: This is the first of a three-part series.
My experience is that some, maybe even most, hospitalists tend to assume there is a standard or “right” way to organize things like work schedules, compensation, or even the assignment of patients among the group’s providers. Some will say things like “SHM says the best hospitalist schedule is …” or “The best way to compensate hospitalists is …”
But there really isn’t a “best” way to manage any particular attribute of a practice. Don’t make the mistake of assuming your method is best, or that it’s the way “everybody else does it.” Although scheduling and compensation are marquee issues for hospitalists, approaches to distributing new patients is much less visible. Many groups tend to assume their method is the only reasonable approach. The best approach, however, varies from one practice to the next. You should be open to hearing approaches to scheduling that are different from your own.
Assign Patients by “Load Leveling”
I’ve come across a lot—and I mean a lot—of different approaches to distributing new patients in HM groups around the country, but it seems pretty clear that the most common method is to undertake “load leveling” on a daily or ongoing basis.
For example, groups that have a separate night shift (the night doctor performs no daytime work the day before or the day after a night shift) typically distribute the night’s new patients with the intent of having each daytime doctor start with the same number of patients. The group might more heavily weight some patients, such as those in the ICU (e.g., each ICU patient counts as 1.5 or two non-ICU patients), but most groups don’t. Over the course of the day shift, new referrals will be distributed evenly among the doctors one at a time, sort of like dealing a deck of cards.
This approach aims to avoid significant imbalances in patient loads and has the potential cultural benefit of everyone sharing equally in busy and slow days. Groups that use it tend to see it as the best option because it is the fairest way to divide up the workload.
Practices that use load-leveling almost always use a schedule built on shifts of a predetermined and fixed duration. For example, say the day shift always works from 7 a.m. to 7 p.m. This schedule usually has the majority of compensation paid via a fixed annual salary or fixed shift rate. One potential problem with this approach is that the doctor who is efficient and discharges a lot of patients today is “rewarded” with more new patients tomorrow. Hospitalists who are allergic to work might have an incentive to have a patient wait until tomorrow to discharge to avoid having to assume the care of yet another patient tomorrow morning. Hospital executives who are focused on length-of-stay management might be concerned if they knew this was a potential issue. Of course, the reverse is true as well. In a practice that doesn’t aggressively undertake load-leveling, a less-than-admirable hospitalist could push patients to discharge earlier than optimal just to have one less patient the next day.
Another cost of this approach is that the distribution of patients can be time-consuming each morning. It also offers the opportunity for some in the group to decide they’re treated unfairly. For instance, you might hear the occasional “just last Tuesday, I started with 16 patients, compared with 15 for everyone else. Now you want me to do it again? You’re being unfair to me; it’s someone else’s turn to take the extra patient.”
Assignment by Location
Groups that use “unit-based” hospitalists distribute patients according to the unit the patient is admitted to—and the hospitalist covering that unit. The pros and cons of unit-based hospitalists are many (see “A Unit-Based Approach,” September 2007), but there is an obvious tension between keeping patient loads even among hospitalists and ensuring that all of a hospitalist’s patients are on “their” unit. Practicality usually requires a compromise between pure unit-based assignment and load-leveling.
Uneven Assignments
Some groups assign patients according to a predetermined algorithm and employ load-leveling only when patient loads become extremely unbalanced. For example, Dr. Jones gets all the new referrals today, and Dr. James gets them tomorrow. The idea is that patient loads end up close to even over time, even if they’re unbalanced on any given day.
A system like this allows everyone, including the hospitalists themselves, ED staff, etc., to know who will take the next patient. It decreases the need to communicate the “who’s next” information time after time during the course of the day. In small- to medium-sized practices, it could mean no one needs to function as the triage doctor (i.e., the person who inefficiently answers the service calls, scribbles down clinical information, then calls the hospitalist who is due to take the next patient and relays all the pertinent patient info). This system allows the
hospitalists to know which days will be harder (e.g., taking on the care of new patients) and which days will be easier (e.g., rounding but not assuming care of new patients). Allowing uneven loads also eliminates the need to spend energy working to even the loads and risking that some in the group feel as if they aren’t being treated fairly.
Uncommon yet Intriguing Approaches
Pair referring primary-care physicians (PCPs) with specific hospitalists. I’ve encountered two groups that had hospitalists always admit patients from the same PCPs. In other words, hospitalist Dr. Hancock always serves as attending for patients referred by the same nine PCPs, and hospitalist Dr. Franklin always attends to patients from a different set of PCPs. It seems to me that there could be tremendous benefit in working closely with the same PCPs, most notably getting to know the PCPs’ office staff. But this system raises the risk of creating out-of-balance patient loads, among other problems. It is really attractive to me, but most groups will decide its costs outweigh its benefits.
Hospitalist and patient stay connected during admission. I’m not aware of any group that uses this method (let me know if you do!), but there could be benefits to having each patient see the same hospitalist during each hospital stay. Of course, that is assuming the hospitalist is on duty. Hospitalist and patient could be paired upon the patient’s first admission. The hospitalist could form an excellent relationship with the patient and family; the time spent by the hospitalist getting to know patients on admission would be reduced, and I suspect there might be some benefit in the quality of care.
This method, however, likely results in the most uneven patient loads, and load-leveling would be difficult, if not impossible. Even if hospitalist and patient did form a tight bond, there is a high probability that the hospitalist would be off for the duration of the patient’s next admission. So despite what I suspect are tremendous benefits, this approach may not be feasible for any group.
In next month’s column, I will discuss issues related to the way patients are distributed. TH
Dr. Nelson has been a practicing hospitalist since 1988 and is co-founder and past president of SHM. He is a principal in Nelson Flores Hospital Medicine Consultants, a national hospitalist practice management consulting firm (www.nelsonflores.com). He is co-director and faculty for SHM’s “Best Practices in Managing a Hospital Medicine Program” course. This column represents his views and is not intended to reflect an official position of SHM.
Editor’s note: This is the first of a three-part series.
My experience is that some, maybe even most, hospitalists tend to assume there is a standard or “right” way to organize things like work schedules, compensation, or even the assignment of patients among the group’s providers. Some will say things like “SHM says the best hospitalist schedule is …” or “The best way to compensate hospitalists is …”
But there really isn’t a “best” way to manage any particular attribute of a practice. Don’t make the mistake of assuming your method is best, or that it’s the way “everybody else does it.” Although scheduling and compensation are marquee issues for hospitalists, approaches to distributing new patients is much less visible. Many groups tend to assume their method is the only reasonable approach. The best approach, however, varies from one practice to the next. You should be open to hearing approaches to scheduling that are different from your own.
Assign Patients by “Load Leveling”
I’ve come across a lot—and I mean a lot—of different approaches to distributing new patients in HM groups around the country, but it seems pretty clear that the most common method is to undertake “load leveling” on a daily or ongoing basis.
For example, groups that have a separate night shift (the night doctor performs no daytime work the day before or the day after a night shift) typically distribute the night’s new patients with the intent of having each daytime doctor start with the same number of patients. The group might more heavily weight some patients, such as those in the ICU (e.g., each ICU patient counts as 1.5 or two non-ICU patients), but most groups don’t. Over the course of the day shift, new referrals will be distributed evenly among the doctors one at a time, sort of like dealing a deck of cards.
This approach aims to avoid significant imbalances in patient loads and has the potential cultural benefit of everyone sharing equally in busy and slow days. Groups that use it tend to see it as the best option because it is the fairest way to divide up the workload.
Practices that use load-leveling almost always use a schedule built on shifts of a predetermined and fixed duration. For example, say the day shift always works from 7 a.m. to 7 p.m. This schedule usually has the majority of compensation paid via a fixed annual salary or fixed shift rate. One potential problem with this approach is that the doctor who is efficient and discharges a lot of patients today is “rewarded” with more new patients tomorrow. Hospitalists who are allergic to work might have an incentive to have a patient wait until tomorrow to discharge to avoid having to assume the care of yet another patient tomorrow morning. Hospital executives who are focused on length-of-stay management might be concerned if they knew this was a potential issue. Of course, the reverse is true as well. In a practice that doesn’t aggressively undertake load-leveling, a less-than-admirable hospitalist could push patients to discharge earlier than optimal just to have one less patient the next day.
Another cost of this approach is that the distribution of patients can be time-consuming each morning. It also offers the opportunity for some in the group to decide they’re treated unfairly. For instance, you might hear the occasional “just last Tuesday, I started with 16 patients, compared with 15 for everyone else. Now you want me to do it again? You’re being unfair to me; it’s someone else’s turn to take the extra patient.”
Assignment by Location
Groups that use “unit-based” hospitalists distribute patients according to the unit the patient is admitted to—and the hospitalist covering that unit. The pros and cons of unit-based hospitalists are many (see “A Unit-Based Approach,” September 2007), but there is an obvious tension between keeping patient loads even among hospitalists and ensuring that all of a hospitalist’s patients are on “their” unit. Practicality usually requires a compromise between pure unit-based assignment and load-leveling.
Uneven Assignments
Some groups assign patients according to a predetermined algorithm and employ load-leveling only when patient loads become extremely unbalanced. For example, Dr. Jones gets all the new referrals today, and Dr. James gets them tomorrow. The idea is that patient loads end up close to even over time, even if they’re unbalanced on any given day.
A system like this allows everyone, including the hospitalists themselves, ED staff, etc., to know who will take the next patient. It decreases the need to communicate the “who’s next” information time after time during the course of the day. In small- to medium-sized practices, it could mean no one needs to function as the triage doctor (i.e., the person who inefficiently answers the service calls, scribbles down clinical information, then calls the hospitalist who is due to take the next patient and relays all the pertinent patient info). This system allows the
hospitalists to know which days will be harder (e.g., taking on the care of new patients) and which days will be easier (e.g., rounding but not assuming care of new patients). Allowing uneven loads also eliminates the need to spend energy working to even the loads and risking that some in the group feel as if they aren’t being treated fairly.
Uncommon yet Intriguing Approaches
Pair referring primary-care physicians (PCPs) with specific hospitalists. I’ve encountered two groups that had hospitalists always admit patients from the same PCPs. In other words, hospitalist Dr. Hancock always serves as attending for patients referred by the same nine PCPs, and hospitalist Dr. Franklin always attends to patients from a different set of PCPs. It seems to me that there could be tremendous benefit in working closely with the same PCPs, most notably getting to know the PCPs’ office staff. But this system raises the risk of creating out-of-balance patient loads, among other problems. It is really attractive to me, but most groups will decide its costs outweigh its benefits.
Hospitalist and patient stay connected during admission. I’m not aware of any group that uses this method (let me know if you do!), but there could be benefits to having each patient see the same hospitalist during each hospital stay. Of course, that is assuming the hospitalist is on duty. Hospitalist and patient could be paired upon the patient’s first admission. The hospitalist could form an excellent relationship with the patient and family; the time spent by the hospitalist getting to know patients on admission would be reduced, and I suspect there might be some benefit in the quality of care.
This method, however, likely results in the most uneven patient loads, and load-leveling would be difficult, if not impossible. Even if hospitalist and patient did form a tight bond, there is a high probability that the hospitalist would be off for the duration of the patient’s next admission. So despite what I suspect are tremendous benefits, this approach may not be feasible for any group.
In next month’s column, I will discuss issues related to the way patients are distributed. TH
Dr. Nelson has been a practicing hospitalist since 1988 and is co-founder and past president of SHM. He is a principal in Nelson Flores Hospital Medicine Consultants, a national hospitalist practice management consulting firm (www.nelsonflores.com). He is co-director and faculty for SHM’s “Best Practices in Managing a Hospital Medicine Program” course. This column represents his views and is not intended to reflect an official position of SHM.
Necessary Evil: Change
The amount and complexity of medical knowledge we need to keep up with is changing and growing at a remarkable rate. I was trained in an era in which it was taken as a given that congestive heart failure patients should not receive beta-blockers; now it is a big mistake if we don’t prescribe them in most cases. But even before starting medical school, most of us realize that things will change a lot, and many of us see that as a good thing. It keeps our work interesting. Just recently, our hospital had a guest speaker who talked about potential medical applications of nanotechnology. It was way over my head, but it sounded pretty cool.
While I was prepared for ongoing changes in medical knowledge, I failed to anticipate how quickly the business of medicine would change during my career. I think the need to keep up with ever-increasing financial and regulatory issues siphons a lot of time and energy that could be used to keep up with the medical knowledge base. I wasn’t prepared for this when I started my career.
Because it is the start of a new year, I thought I would highlight one issue related to CPT coding: Medicare stopped recognizing consult codes as of Jan. 1 (see “Consultation Elimination,” p. 31).
What It Means for Hospitalists
The good news is that we can just use initial hospital visit codes, inpatient or observation, for all new visits. For example, it won’t matter anymore whether I’m admitting and serving as attending for a patient, or whether a surgeon admitted the patient and asked me to consult for preoperative medical evaluation (“clearance”). I should use the same CPT code in either situation, simply appending a modifier if I’m the admitting physician. And for billing purposes, we won’t have to worry about documenting which doctor requested that we see the patient, though it is a good idea to document it as part of the clinical record anyway.
But it gets a little more complicated. The codes aren’t going away or being removed from the CPT “bible” published by the American Medical Association (AMA). Instead, Medicare simply won’t recognize them anymore. Other payors probably will follow suit within a few months, but that isn’t certain. So it is possible that when asked by a surgeon to provide a preoperative evaluation, you will need to bill an initial hospital (or office or nursing facility) care visit if the patient is on Medicare but bill a consult code if the patient has other insurance. You should check with your billers to ensure you’re doing this correctly.
Medicare-paid consults are at a slightly higher rate than the equivalent service billed as initial hospital care (e.g., when the hospitalist is attending). So a higher reimbursing code has been replaced with one that pays a little less. For example, a 99253 consultation code requires a detailed history, detailed examination, and medical decision-making of low complexity; last year, 99253 was reimbursed by Medicare at an average rate of $114.69. The equivalent admission code for a detailed history, detailed examination, and low-complexity medical decision-making is a 99221 code, for which Medicare pays about $99.90. This represents a difference of about 14%.
However, the net financial impact of this change probably will be positive for most HM groups because you probably bill very few initial consult codes, and instead were stuck billing a follow-up visit code when seeing co-management “consults” (i.e., a patient admitted by a surgeon who asks you to follow and manage diabetes and other medical issues). Now, at least in the case of Medicare, it is appropriate for us to bill an initial hospital visit code, which provides significantly higher reimbursement than follow-up codes.
In addition, there is a modest (about 0.3%) proposed increase in work relative value units attached to the initial hospital visit codes, which will benefit us not only when we’re consulting, but also when we admit and serve as a patient’s attending.
Some specialists may be less interested in consulting on our patients because the initial visit codes will reimburse a little less than similar consultation codes. I don’t anticipate this will be a significant problem for most of us, particularly since many specialists bill the highest level of consultation code (99255), which pays about the same as the equivalent admission code (99223).
Although I think elimination of the use of consultation codes seems like a reasonable step toward simplifying how hospitalists bill for our services, keeping up with these frequent coding changes requires a high level of diligence on our part, and on the part of our administrative and clerical staffs. And it consumes time and resources that I—and my team—could better spend keeping up with changes in clinical practice.
Perhaps when all the dust settles around the healthcare reform debate, we will begin to move toward new, more creative payment models that will allow us to focus on what we do best. TH
Dr. Nelson has been a practicing hospitalist since 1988 and is cofounder and past president of SHM. He is a principal in Nelson Flores Hospital Medicine Consultants, a national hospitalist practice management consulting firm (www.nelsonflores.com). He is also course co-director and faculty for SHM’s “Best Practices in Managing a Hospital Medicine Program” course. This column represents his views and is not intended to reflect an official position of SHM.
The amount and complexity of medical knowledge we need to keep up with is changing and growing at a remarkable rate. I was trained in an era in which it was taken as a given that congestive heart failure patients should not receive beta-blockers; now it is a big mistake if we don’t prescribe them in most cases. But even before starting medical school, most of us realize that things will change a lot, and many of us see that as a good thing. It keeps our work interesting. Just recently, our hospital had a guest speaker who talked about potential medical applications of nanotechnology. It was way over my head, but it sounded pretty cool.
While I was prepared for ongoing changes in medical knowledge, I failed to anticipate how quickly the business of medicine would change during my career. I think the need to keep up with ever-increasing financial and regulatory issues siphons a lot of time and energy that could be used to keep up with the medical knowledge base. I wasn’t prepared for this when I started my career.
Because it is the start of a new year, I thought I would highlight one issue related to CPT coding: Medicare stopped recognizing consult codes as of Jan. 1 (see “Consultation Elimination,” p. 31).
What It Means for Hospitalists
The good news is that we can just use initial hospital visit codes, inpatient or observation, for all new visits. For example, it won’t matter anymore whether I’m admitting and serving as attending for a patient, or whether a surgeon admitted the patient and asked me to consult for preoperative medical evaluation (“clearance”). I should use the same CPT code in either situation, simply appending a modifier if I’m the admitting physician. And for billing purposes, we won’t have to worry about documenting which doctor requested that we see the patient, though it is a good idea to document it as part of the clinical record anyway.
But it gets a little more complicated. The codes aren’t going away or being removed from the CPT “bible” published by the American Medical Association (AMA). Instead, Medicare simply won’t recognize them anymore. Other payors probably will follow suit within a few months, but that isn’t certain. So it is possible that when asked by a surgeon to provide a preoperative evaluation, you will need to bill an initial hospital (or office or nursing facility) care visit if the patient is on Medicare but bill a consult code if the patient has other insurance. You should check with your billers to ensure you’re doing this correctly.
Medicare-paid consults are at a slightly higher rate than the equivalent service billed as initial hospital care (e.g., when the hospitalist is attending). So a higher reimbursing code has been replaced with one that pays a little less. For example, a 99253 consultation code requires a detailed history, detailed examination, and medical decision-making of low complexity; last year, 99253 was reimbursed by Medicare at an average rate of $114.69. The equivalent admission code for a detailed history, detailed examination, and low-complexity medical decision-making is a 99221 code, for which Medicare pays about $99.90. This represents a difference of about 14%.
However, the net financial impact of this change probably will be positive for most HM groups because you probably bill very few initial consult codes, and instead were stuck billing a follow-up visit code when seeing co-management “consults” (i.e., a patient admitted by a surgeon who asks you to follow and manage diabetes and other medical issues). Now, at least in the case of Medicare, it is appropriate for us to bill an initial hospital visit code, which provides significantly higher reimbursement than follow-up codes.
In addition, there is a modest (about 0.3%) proposed increase in work relative value units attached to the initial hospital visit codes, which will benefit us not only when we’re consulting, but also when we admit and serve as a patient’s attending.
Some specialists may be less interested in consulting on our patients because the initial visit codes will reimburse a little less than similar consultation codes. I don’t anticipate this will be a significant problem for most of us, particularly since many specialists bill the highest level of consultation code (99255), which pays about the same as the equivalent admission code (99223).
Although I think elimination of the use of consultation codes seems like a reasonable step toward simplifying how hospitalists bill for our services, keeping up with these frequent coding changes requires a high level of diligence on our part, and on the part of our administrative and clerical staffs. And it consumes time and resources that I—and my team—could better spend keeping up with changes in clinical practice.
Perhaps when all the dust settles around the healthcare reform debate, we will begin to move toward new, more creative payment models that will allow us to focus on what we do best. TH
Dr. Nelson has been a practicing hospitalist since 1988 and is cofounder and past president of SHM. He is a principal in Nelson Flores Hospital Medicine Consultants, a national hospitalist practice management consulting firm (www.nelsonflores.com). He is also course co-director and faculty for SHM’s “Best Practices in Managing a Hospital Medicine Program” course. This column represents his views and is not intended to reflect an official position of SHM.
The amount and complexity of medical knowledge we need to keep up with is changing and growing at a remarkable rate. I was trained in an era in which it was taken as a given that congestive heart failure patients should not receive beta-blockers; now it is a big mistake if we don’t prescribe them in most cases. But even before starting medical school, most of us realize that things will change a lot, and many of us see that as a good thing. It keeps our work interesting. Just recently, our hospital had a guest speaker who talked about potential medical applications of nanotechnology. It was way over my head, but it sounded pretty cool.
While I was prepared for ongoing changes in medical knowledge, I failed to anticipate how quickly the business of medicine would change during my career. I think the need to keep up with ever-increasing financial and regulatory issues siphons a lot of time and energy that could be used to keep up with the medical knowledge base. I wasn’t prepared for this when I started my career.
Because it is the start of a new year, I thought I would highlight one issue related to CPT coding: Medicare stopped recognizing consult codes as of Jan. 1 (see “Consultation Elimination,” p. 31).
What It Means for Hospitalists
The good news is that we can just use initial hospital visit codes, inpatient or observation, for all new visits. For example, it won’t matter anymore whether I’m admitting and serving as attending for a patient, or whether a surgeon admitted the patient and asked me to consult for preoperative medical evaluation (“clearance”). I should use the same CPT code in either situation, simply appending a modifier if I’m the admitting physician. And for billing purposes, we won’t have to worry about documenting which doctor requested that we see the patient, though it is a good idea to document it as part of the clinical record anyway.
But it gets a little more complicated. The codes aren’t going away or being removed from the CPT “bible” published by the American Medical Association (AMA). Instead, Medicare simply won’t recognize them anymore. Other payors probably will follow suit within a few months, but that isn’t certain. So it is possible that when asked by a surgeon to provide a preoperative evaluation, you will need to bill an initial hospital (or office or nursing facility) care visit if the patient is on Medicare but bill a consult code if the patient has other insurance. You should check with your billers to ensure you’re doing this correctly.
Medicare-paid consults are at a slightly higher rate than the equivalent service billed as initial hospital care (e.g., when the hospitalist is attending). So a higher reimbursing code has been replaced with one that pays a little less. For example, a 99253 consultation code requires a detailed history, detailed examination, and medical decision-making of low complexity; last year, 99253 was reimbursed by Medicare at an average rate of $114.69. The equivalent admission code for a detailed history, detailed examination, and low-complexity medical decision-making is a 99221 code, for which Medicare pays about $99.90. This represents a difference of about 14%.
However, the net financial impact of this change probably will be positive for most HM groups because you probably bill very few initial consult codes, and instead were stuck billing a follow-up visit code when seeing co-management “consults” (i.e., a patient admitted by a surgeon who asks you to follow and manage diabetes and other medical issues). Now, at least in the case of Medicare, it is appropriate for us to bill an initial hospital visit code, which provides significantly higher reimbursement than follow-up codes.
In addition, there is a modest (about 0.3%) proposed increase in work relative value units attached to the initial hospital visit codes, which will benefit us not only when we’re consulting, but also when we admit and serve as a patient’s attending.
Some specialists may be less interested in consulting on our patients because the initial visit codes will reimburse a little less than similar consultation codes. I don’t anticipate this will be a significant problem for most of us, particularly since many specialists bill the highest level of consultation code (99255), which pays about the same as the equivalent admission code (99223).
Although I think elimination of the use of consultation codes seems like a reasonable step toward simplifying how hospitalists bill for our services, keeping up with these frequent coding changes requires a high level of diligence on our part, and on the part of our administrative and clerical staffs. And it consumes time and resources that I—and my team—could better spend keeping up with changes in clinical practice.
Perhaps when all the dust settles around the healthcare reform debate, we will begin to move toward new, more creative payment models that will allow us to focus on what we do best. TH
Dr. Nelson has been a practicing hospitalist since 1988 and is cofounder and past president of SHM. He is a principal in Nelson Flores Hospital Medicine Consultants, a national hospitalist practice management consulting firm (www.nelsonflores.com). He is also course co-director and faculty for SHM’s “Best Practices in Managing a Hospital Medicine Program” course. This column represents his views and is not intended to reflect an official position of SHM.
Compensation Conundrum
Should hospitalist compensation increase automatically based on how long the physician has been in the practice (i.e., tenure)? Should hospitalist compensation have a cost-of-living provision, in which compensation goes up based on some external measure, such as the consumer price index?
I’m in favor of ever-increasing hospitalist incomes, including mine. And, fortunately, surveys done by SHM and others show hospitalist incomes have been increasing much faster than the cost of living. A portion of this increase can be explained by inflation and the fact that the average productivity for a full-time hospitalist has been increasing. We’re either working harder or more efficiently, but either way, the average full-time hospitalist is seeing more billable encounters than ever before.
But inflation and workload account for only a portion of the historical increase in hospitalist salaries. Market forces—principally, the demand for hospitalists exceeding the supply—probably are the biggest factors leading to rising salaries.
When Is a Hospitalist Most Valuable?
In this column, I’m going to discuss compensation philosophy for standard work as a staff hospitalist. That is mostly direct patient care, with the typical amount of such additional work as committee participation, protocol development, etc. A hospitalist who takes on a new role, such as group leader, medical director of the quality department, chief medical officer, etc., should expect his or her salary to change as a result of the promotion, and I’m excluding that situation from this article.
So back to my original question. If surveys demonstrate hospitalist salaries are increasing, then it is reasonable for your practice to ensure your hospitalist salaries keep up with established market rates. But independent of changes in the market, should hospitalist salaries in your group go up based on years of service in the group or years of experience as a hospitalist, even if some of that time was in another practice?
There are a number of ways to approach this question, but for me the key question is, at what point in an HM career is the hospitalist most valuable to the practice? Is it the first year out of residency? What about five years into your practice as a hospitalist? Maybe 10 years? Longer? I think it makes the most sense for salary to increase as long as the hospitalist’s value to the practice is increasing, but routine increases beyond that probably don’t make sense.
A hospitalist straight out of residency is almost always less valuable than someone with experience in your practice. But one point of view is that the new residency grad usually catches up to experienced hospitalists within six to 18 months. This is often followed by a long plateau phase, and, eventually, some of the more “senior” physicians become a little less valuable than those with just a few years of experience. One orthopedist told me, “New hospitalists are so eager to help and are flexible and are committed to the success of the team. But after a while, a lot of them tend to ossify and become more difficult to work with.”
For very understandable reasons, physicians who are more established in their careers could have less scheduling flexibility and might be less willing to adjust their scope of practice to take on new roles. Some senior hospitalists—like doctors in any specialty—lose value if they don’t adequately keep up with advances in medicine. Offsetting this potential decline in value with tenure are the increase in institutional knowledge as well as relationships that a hospitalist develops by staying in the same practice for years (see Figure 1).
This point of view matches a compensation structure that might have a new residency grad start at a lower salary that increases to the “mature” level after 12 to 18 months, and remains there without future tenure-based increases—that is, a single step up in salary based on tenure. I think this makes sense for most practices.
Exceptions to the Rule
I can think of two reasonably common situations in which a group might deviate from a single tenure-based salary increase. The first is private groups in which the physicians are the contractual owners of their practice (i.e., they’re employed by a corporation they own, and not employed by the hospital or another large entity). In this structure, new physicians typically have a lower salary until they become a partner, usually after a year or two with the group. Becoming partner could require buying into the practice with tens of thousands of dollars, and might include the opportunity to share in future profit distributions. (Although buying into physician practices has been a common and appropriate model for decades, I think a new hospitalist should think carefully about whether what they will own after buying in is really worth the cost of the buy-in.)
Another exception is when hospitalists are part of a large multi-specialty physician group that offers multiple tenure-based salary increases for all physicians in all specialties. It probably makes sense to structure the hospitalist compensation plan the same way. But remember, it might take several years for primary-care physicians and surgeons to build robust patient populations and referral streams, and annual increases in salary for the first five years might mirror the pace by which a typical doctor builds his or her practice.
A new hospitalist, even one just out of residency, has an essentially mature referral stream within days of starting. So a five-year, tenure-based increase in salary could look more like the practice is simply underpaying the hospitalist until their fifth anniversary with the practice.
Automatic Increases
Some hospitalists have automatic cost-of-living salary increases. In some cases, the increases are tied to an external benchmark (e.g., the consumer price index), but it is probably more common that the future increase is simply estimated and compensation is contractually assured of increasing by a few percentage points annually.
Most hospitalists don’t have such a provision in their contracts. Indeed, most working Americans with salaries in the hospitalist range and higher don’t have cost-of-living increases. Instead, future salary adjustments are made based on market data, such as the results of salary surveys. TH
Dr. Nelson has been a hospitalist since 1988 and is co-founder and past president of SHM. He is a principal in Nelson Flores Hospital Medicine Consultants, a national hospitalist practice management consulting firm (www.nelsonflores.com). He is also course co-director and faculty for SHM’s “Best Practices in Managing a Hospital Medicine Program” course. This column represents his views and is not intended to reflect an official position of SHM.
Should hospitalist compensation increase automatically based on how long the physician has been in the practice (i.e., tenure)? Should hospitalist compensation have a cost-of-living provision, in which compensation goes up based on some external measure, such as the consumer price index?
I’m in favor of ever-increasing hospitalist incomes, including mine. And, fortunately, surveys done by SHM and others show hospitalist incomes have been increasing much faster than the cost of living. A portion of this increase can be explained by inflation and the fact that the average productivity for a full-time hospitalist has been increasing. We’re either working harder or more efficiently, but either way, the average full-time hospitalist is seeing more billable encounters than ever before.
But inflation and workload account for only a portion of the historical increase in hospitalist salaries. Market forces—principally, the demand for hospitalists exceeding the supply—probably are the biggest factors leading to rising salaries.
When Is a Hospitalist Most Valuable?
In this column, I’m going to discuss compensation philosophy for standard work as a staff hospitalist. That is mostly direct patient care, with the typical amount of such additional work as committee participation, protocol development, etc. A hospitalist who takes on a new role, such as group leader, medical director of the quality department, chief medical officer, etc., should expect his or her salary to change as a result of the promotion, and I’m excluding that situation from this article.
So back to my original question. If surveys demonstrate hospitalist salaries are increasing, then it is reasonable for your practice to ensure your hospitalist salaries keep up with established market rates. But independent of changes in the market, should hospitalist salaries in your group go up based on years of service in the group or years of experience as a hospitalist, even if some of that time was in another practice?
There are a number of ways to approach this question, but for me the key question is, at what point in an HM career is the hospitalist most valuable to the practice? Is it the first year out of residency? What about five years into your practice as a hospitalist? Maybe 10 years? Longer? I think it makes the most sense for salary to increase as long as the hospitalist’s value to the practice is increasing, but routine increases beyond that probably don’t make sense.
A hospitalist straight out of residency is almost always less valuable than someone with experience in your practice. But one point of view is that the new residency grad usually catches up to experienced hospitalists within six to 18 months. This is often followed by a long plateau phase, and, eventually, some of the more “senior” physicians become a little less valuable than those with just a few years of experience. One orthopedist told me, “New hospitalists are so eager to help and are flexible and are committed to the success of the team. But after a while, a lot of them tend to ossify and become more difficult to work with.”
For very understandable reasons, physicians who are more established in their careers could have less scheduling flexibility and might be less willing to adjust their scope of practice to take on new roles. Some senior hospitalists—like doctors in any specialty—lose value if they don’t adequately keep up with advances in medicine. Offsetting this potential decline in value with tenure are the increase in institutional knowledge as well as relationships that a hospitalist develops by staying in the same practice for years (see Figure 1).
This point of view matches a compensation structure that might have a new residency grad start at a lower salary that increases to the “mature” level after 12 to 18 months, and remains there without future tenure-based increases—that is, a single step up in salary based on tenure. I think this makes sense for most practices.
Exceptions to the Rule
I can think of two reasonably common situations in which a group might deviate from a single tenure-based salary increase. The first is private groups in which the physicians are the contractual owners of their practice (i.e., they’re employed by a corporation they own, and not employed by the hospital or another large entity). In this structure, new physicians typically have a lower salary until they become a partner, usually after a year or two with the group. Becoming partner could require buying into the practice with tens of thousands of dollars, and might include the opportunity to share in future profit distributions. (Although buying into physician practices has been a common and appropriate model for decades, I think a new hospitalist should think carefully about whether what they will own after buying in is really worth the cost of the buy-in.)
Another exception is when hospitalists are part of a large multi-specialty physician group that offers multiple tenure-based salary increases for all physicians in all specialties. It probably makes sense to structure the hospitalist compensation plan the same way. But remember, it might take several years for primary-care physicians and surgeons to build robust patient populations and referral streams, and annual increases in salary for the first five years might mirror the pace by which a typical doctor builds his or her practice.
A new hospitalist, even one just out of residency, has an essentially mature referral stream within days of starting. So a five-year, tenure-based increase in salary could look more like the practice is simply underpaying the hospitalist until their fifth anniversary with the practice.
Automatic Increases
Some hospitalists have automatic cost-of-living salary increases. In some cases, the increases are tied to an external benchmark (e.g., the consumer price index), but it is probably more common that the future increase is simply estimated and compensation is contractually assured of increasing by a few percentage points annually.
Most hospitalists don’t have such a provision in their contracts. Indeed, most working Americans with salaries in the hospitalist range and higher don’t have cost-of-living increases. Instead, future salary adjustments are made based on market data, such as the results of salary surveys. TH
Dr. Nelson has been a hospitalist since 1988 and is co-founder and past president of SHM. He is a principal in Nelson Flores Hospital Medicine Consultants, a national hospitalist practice management consulting firm (www.nelsonflores.com). He is also course co-director and faculty for SHM’s “Best Practices in Managing a Hospital Medicine Program” course. This column represents his views and is not intended to reflect an official position of SHM.
Should hospitalist compensation increase automatically based on how long the physician has been in the practice (i.e., tenure)? Should hospitalist compensation have a cost-of-living provision, in which compensation goes up based on some external measure, such as the consumer price index?
I’m in favor of ever-increasing hospitalist incomes, including mine. And, fortunately, surveys done by SHM and others show hospitalist incomes have been increasing much faster than the cost of living. A portion of this increase can be explained by inflation and the fact that the average productivity for a full-time hospitalist has been increasing. We’re either working harder or more efficiently, but either way, the average full-time hospitalist is seeing more billable encounters than ever before.
But inflation and workload account for only a portion of the historical increase in hospitalist salaries. Market forces—principally, the demand for hospitalists exceeding the supply—probably are the biggest factors leading to rising salaries.
When Is a Hospitalist Most Valuable?
In this column, I’m going to discuss compensation philosophy for standard work as a staff hospitalist. That is mostly direct patient care, with the typical amount of such additional work as committee participation, protocol development, etc. A hospitalist who takes on a new role, such as group leader, medical director of the quality department, chief medical officer, etc., should expect his or her salary to change as a result of the promotion, and I’m excluding that situation from this article.
So back to my original question. If surveys demonstrate hospitalist salaries are increasing, then it is reasonable for your practice to ensure your hospitalist salaries keep up with established market rates. But independent of changes in the market, should hospitalist salaries in your group go up based on years of service in the group or years of experience as a hospitalist, even if some of that time was in another practice?
There are a number of ways to approach this question, but for me the key question is, at what point in an HM career is the hospitalist most valuable to the practice? Is it the first year out of residency? What about five years into your practice as a hospitalist? Maybe 10 years? Longer? I think it makes the most sense for salary to increase as long as the hospitalist’s value to the practice is increasing, but routine increases beyond that probably don’t make sense.
A hospitalist straight out of residency is almost always less valuable than someone with experience in your practice. But one point of view is that the new residency grad usually catches up to experienced hospitalists within six to 18 months. This is often followed by a long plateau phase, and, eventually, some of the more “senior” physicians become a little less valuable than those with just a few years of experience. One orthopedist told me, “New hospitalists are so eager to help and are flexible and are committed to the success of the team. But after a while, a lot of them tend to ossify and become more difficult to work with.”
For very understandable reasons, physicians who are more established in their careers could have less scheduling flexibility and might be less willing to adjust their scope of practice to take on new roles. Some senior hospitalists—like doctors in any specialty—lose value if they don’t adequately keep up with advances in medicine. Offsetting this potential decline in value with tenure are the increase in institutional knowledge as well as relationships that a hospitalist develops by staying in the same practice for years (see Figure 1).
This point of view matches a compensation structure that might have a new residency grad start at a lower salary that increases to the “mature” level after 12 to 18 months, and remains there without future tenure-based increases—that is, a single step up in salary based on tenure. I think this makes sense for most practices.
Exceptions to the Rule
I can think of two reasonably common situations in which a group might deviate from a single tenure-based salary increase. The first is private groups in which the physicians are the contractual owners of their practice (i.e., they’re employed by a corporation they own, and not employed by the hospital or another large entity). In this structure, new physicians typically have a lower salary until they become a partner, usually after a year or two with the group. Becoming partner could require buying into the practice with tens of thousands of dollars, and might include the opportunity to share in future profit distributions. (Although buying into physician practices has been a common and appropriate model for decades, I think a new hospitalist should think carefully about whether what they will own after buying in is really worth the cost of the buy-in.)
Another exception is when hospitalists are part of a large multi-specialty physician group that offers multiple tenure-based salary increases for all physicians in all specialties. It probably makes sense to structure the hospitalist compensation plan the same way. But remember, it might take several years for primary-care physicians and surgeons to build robust patient populations and referral streams, and annual increases in salary for the first five years might mirror the pace by which a typical doctor builds his or her practice.
A new hospitalist, even one just out of residency, has an essentially mature referral stream within days of starting. So a five-year, tenure-based increase in salary could look more like the practice is simply underpaying the hospitalist until their fifth anniversary with the practice.
Automatic Increases
Some hospitalists have automatic cost-of-living salary increases. In some cases, the increases are tied to an external benchmark (e.g., the consumer price index), but it is probably more common that the future increase is simply estimated and compensation is contractually assured of increasing by a few percentage points annually.
Most hospitalists don’t have such a provision in their contracts. Indeed, most working Americans with salaries in the hospitalist range and higher don’t have cost-of-living increases. Instead, future salary adjustments are made based on market data, such as the results of salary surveys. TH
Dr. Nelson has been a hospitalist since 1988 and is co-founder and past president of SHM. He is a principal in Nelson Flores Hospital Medicine Consultants, a national hospitalist practice management consulting firm (www.nelsonflores.com). He is also course co-director and faculty for SHM’s “Best Practices in Managing a Hospital Medicine Program” course. This column represents his views and is not intended to reflect an official position of SHM.
Fiduciary Responsibility
Editor’s note: Second of a two-part series.
Many issues that influence hospitalist budgets, specifically the amount of financial support provided by the hospital, are common in most HM practices. Last month I addressed issues related to collecting professional fee revenue (see “Budget Checkup,” October 2009, p. 54). This month I’ll turn to operations that have a significant influence on the practice’s financial picture.
Staffing and Scheduling
My experience is that hospitalists think carefully about the effect of their chosen schedule on a physician’s lifestyle (e.g., make HM a career path and minimize the risk of burnout) and patient-hospitalist continuity. But rarely do I find evidence that the group has acknowledged the effect of their schedules on the budget.
Here’s a common example. As patient volume grows, most groups find that the volume of admissions from late in the afternoon to around 10 or 11 p.m. is too high for one doctor to manage. So the group decides to add an evening shift (often called a “swing shift”). And because all previous shifts in the practice have been 12 hours long, they decide to make the evening shift last 12 hours as well. Many groups adhere to this physician schedule even if patient volume only requires evening-shift coverage from 5 p.m. until around 10 or 11 at night. By choosing a 12-hour evening shift, rather than the five or six hours that are really needed, the practice may be paying for about six hours of unnecessary coverage each day. Six hours more per day is 42 hours per week; I don’t have to tell you that this system can get really expensive very quickly.
Another common example: A group that uses a seven-on/seven-off schedule will add two new full-time equivalent (FTE) employees at the same time to preserve the symmetry required by the schedule, even if patient volume justifies adding only 0.5 to 1.0 FTE.
My point in these examples is not to suggest the right schedule for your group, but to provide a reminder that the schedule has a significant impact on the budget (see “Staffing Strategies,” January 2007, p. 50).
NPP Roles
Physician assistants and nurse practitioners, which I refer to collectively as non-physician providers (NPPs), can make valuable contributions to hospitalist practices. Just as it would do for an MD hospitalist, a practice should assess NPP contribution to important metrics, such as quality of care, throughput, stakeholder satisfaction, and practice economics. I have worked with practices that never give much thought to whether their NPPs occupy the right roles in the practice—positions that allow NPPs to make significant, cost-effective, and career-satisfying contributions.
A simple exercise that can be very helpful is to determine the total cost to employ NPPs (salary and benefits) and think about whether the practice would be better off if those dollars were spent on physicians. If the return on investing in NPPs is less than the return on investing in physicians, the practice should consider adjusting the NPPs’ roles and/or schedules (see “Role Refinement,” September 2009, p. 53).
I’m not suggesting that the only measure of NPP value is in dollars or professional fee revenue billed. Instead, the group’s return on investment should be viewed broadly and include things that don’t appear in financial statements, such as quality, efficiency, patient satisfaction, etc.
Arbitrary Definitions
SHM’s “2007-2008 Bi-Annual Survey on the State of the Hospital Medicine Movement” shows full-time hospitalists work an average of 2,172 hours annually. This might not be a reliable figure. Even so, many practices define full-time work based on annual hours (or shifts), but the doctors regularly adjust actual number of hours worked depending on that day’s workload, and few practices rigorously track actual hours worked. So I think data on hours worked annually (from SHM or other sources) should not be used as reliable or valid target for a practice.
Annual number of shifts worked can be reported by a practice more reliably but usually isn’t included in surveys because shift lengths can vary significantly from one place to the next. Ultimately, the number of hours or shifts that define full-time work for a given practice is arbitrary. And it has an impact on the budget.
Many—maybe most—practices arrive at a definition of full-time work based on annual hours, and any provider who works more than that number is paid for “extra” hours or shifts. If the number of hours or shifts that define full-time work is set low, the practice will end up paying for a lot of extra hours or shifts. Payment beyond the projected salary allowance can cause the practice budget to balloon.
One test to see if this might be an issue in your practice is to total the compensation and productivity (e.g., work relative value units, or wRVUs, or billable encounters) for each doctor in the practice. Analyze how the compensation per wRVU or encounter compares with survey data. If your group is higher than survey data, then the definition of full-time work might be unreasonably low, and vice versa.
Night-Shift Costs
Hospitalist night shifts tend to result in low productivity until the practice has grown enough that there are six to eight daytime hospitalists (rounder/admitter) for every night-shift doctor. Still, most small practices find that it is worthwhile to schedule a separate in-house night shift. The cost of the additional FTEs required to staff a separate night shift can be significant, and is a reason many very small practices require more financial support per FTE hospitalist from the hospital than larger practices.
In most cases, I think it is in the hospital’s best interest to provide support for a separate night shift (see “Finding and Keeping Dedicated Noctornists,” February 2008, p. 61). If the practice budget, or amount of support required of the hospital, is seen as excessive, it is worth estimating how much of the excess is attributable to the expensive night shift.
One simple way to do this is to think about the amount of hospital support that goes to each doctor during each shift. For example, if a hospitalist works 182 shifts a year and is compensated $230,000 (salary and bonus at $200,000, and benefits at $30,000 annually), then the doctor costs the practice $1,264 per shift. You might conduct an analysis and learn that the doctor averages $900 in collected professional fees during a day shift and $500 during a night shift. That means more hospital support goes to cover a night shift ($764) than a day shift ($364). Put another way, in this example, each night shift worked by a doctor requires $400 more hospital support per shift than the day-shift hospitalist ($764 vs. $364). In most cases, the hospital realizes a significant return on spending the extra money on the night shifts.
Hospitalist Productivity
Some hospitals have systems of care that interfere with hospitalist productivity. These could be such things as a poorly organized medical record, an IT system that requires logging into multiple programs to retrieve data on a single patient, or hospitalists being required to do clerical work. Productivity also is influenced by time spent on nonclinical activities, which leads to decreasing professional fee revenue. Every practice should think carefully about the systems and activities that might be getting in the way of efficiency. TH
Dr. Nelson has been a practicing hospitalist since 1988 and is co-founder and past president of SHM. He is a principal in Nelson Flores Hospital Medicine Consultants, a national hospitalist practice management consulting firm (www.nelsonflores.com). He is co-director and faculty for SHM’s “Best Practices in Managing a Hospital Medicine Program” course. This column represents his views and is not intended to reflect an official position of SHM.
Editor’s note: Second of a two-part series.
Many issues that influence hospitalist budgets, specifically the amount of financial support provided by the hospital, are common in most HM practices. Last month I addressed issues related to collecting professional fee revenue (see “Budget Checkup,” October 2009, p. 54). This month I’ll turn to operations that have a significant influence on the practice’s financial picture.
Staffing and Scheduling
My experience is that hospitalists think carefully about the effect of their chosen schedule on a physician’s lifestyle (e.g., make HM a career path and minimize the risk of burnout) and patient-hospitalist continuity. But rarely do I find evidence that the group has acknowledged the effect of their schedules on the budget.
Here’s a common example. As patient volume grows, most groups find that the volume of admissions from late in the afternoon to around 10 or 11 p.m. is too high for one doctor to manage. So the group decides to add an evening shift (often called a “swing shift”). And because all previous shifts in the practice have been 12 hours long, they decide to make the evening shift last 12 hours as well. Many groups adhere to this physician schedule even if patient volume only requires evening-shift coverage from 5 p.m. until around 10 or 11 at night. By choosing a 12-hour evening shift, rather than the five or six hours that are really needed, the practice may be paying for about six hours of unnecessary coverage each day. Six hours more per day is 42 hours per week; I don’t have to tell you that this system can get really expensive very quickly.
Another common example: A group that uses a seven-on/seven-off schedule will add two new full-time equivalent (FTE) employees at the same time to preserve the symmetry required by the schedule, even if patient volume justifies adding only 0.5 to 1.0 FTE.
My point in these examples is not to suggest the right schedule for your group, but to provide a reminder that the schedule has a significant impact on the budget (see “Staffing Strategies,” January 2007, p. 50).
NPP Roles
Physician assistants and nurse practitioners, which I refer to collectively as non-physician providers (NPPs), can make valuable contributions to hospitalist practices. Just as it would do for an MD hospitalist, a practice should assess NPP contribution to important metrics, such as quality of care, throughput, stakeholder satisfaction, and practice economics. I have worked with practices that never give much thought to whether their NPPs occupy the right roles in the practice—positions that allow NPPs to make significant, cost-effective, and career-satisfying contributions.
A simple exercise that can be very helpful is to determine the total cost to employ NPPs (salary and benefits) and think about whether the practice would be better off if those dollars were spent on physicians. If the return on investing in NPPs is less than the return on investing in physicians, the practice should consider adjusting the NPPs’ roles and/or schedules (see “Role Refinement,” September 2009, p. 53).
I’m not suggesting that the only measure of NPP value is in dollars or professional fee revenue billed. Instead, the group’s return on investment should be viewed broadly and include things that don’t appear in financial statements, such as quality, efficiency, patient satisfaction, etc.
Arbitrary Definitions
SHM’s “2007-2008 Bi-Annual Survey on the State of the Hospital Medicine Movement” shows full-time hospitalists work an average of 2,172 hours annually. This might not be a reliable figure. Even so, many practices define full-time work based on annual hours (or shifts), but the doctors regularly adjust actual number of hours worked depending on that day’s workload, and few practices rigorously track actual hours worked. So I think data on hours worked annually (from SHM or other sources) should not be used as reliable or valid target for a practice.
Annual number of shifts worked can be reported by a practice more reliably but usually isn’t included in surveys because shift lengths can vary significantly from one place to the next. Ultimately, the number of hours or shifts that define full-time work for a given practice is arbitrary. And it has an impact on the budget.
Many—maybe most—practices arrive at a definition of full-time work based on annual hours, and any provider who works more than that number is paid for “extra” hours or shifts. If the number of hours or shifts that define full-time work is set low, the practice will end up paying for a lot of extra hours or shifts. Payment beyond the projected salary allowance can cause the practice budget to balloon.
One test to see if this might be an issue in your practice is to total the compensation and productivity (e.g., work relative value units, or wRVUs, or billable encounters) for each doctor in the practice. Analyze how the compensation per wRVU or encounter compares with survey data. If your group is higher than survey data, then the definition of full-time work might be unreasonably low, and vice versa.
Night-Shift Costs
Hospitalist night shifts tend to result in low productivity until the practice has grown enough that there are six to eight daytime hospitalists (rounder/admitter) for every night-shift doctor. Still, most small practices find that it is worthwhile to schedule a separate in-house night shift. The cost of the additional FTEs required to staff a separate night shift can be significant, and is a reason many very small practices require more financial support per FTE hospitalist from the hospital than larger practices.
In most cases, I think it is in the hospital’s best interest to provide support for a separate night shift (see “Finding and Keeping Dedicated Noctornists,” February 2008, p. 61). If the practice budget, or amount of support required of the hospital, is seen as excessive, it is worth estimating how much of the excess is attributable to the expensive night shift.
One simple way to do this is to think about the amount of hospital support that goes to each doctor during each shift. For example, if a hospitalist works 182 shifts a year and is compensated $230,000 (salary and bonus at $200,000, and benefits at $30,000 annually), then the doctor costs the practice $1,264 per shift. You might conduct an analysis and learn that the doctor averages $900 in collected professional fees during a day shift and $500 during a night shift. That means more hospital support goes to cover a night shift ($764) than a day shift ($364). Put another way, in this example, each night shift worked by a doctor requires $400 more hospital support per shift than the day-shift hospitalist ($764 vs. $364). In most cases, the hospital realizes a significant return on spending the extra money on the night shifts.
Hospitalist Productivity
Some hospitals have systems of care that interfere with hospitalist productivity. These could be such things as a poorly organized medical record, an IT system that requires logging into multiple programs to retrieve data on a single patient, or hospitalists being required to do clerical work. Productivity also is influenced by time spent on nonclinical activities, which leads to decreasing professional fee revenue. Every practice should think carefully about the systems and activities that might be getting in the way of efficiency. TH
Dr. Nelson has been a practicing hospitalist since 1988 and is co-founder and past president of SHM. He is a principal in Nelson Flores Hospital Medicine Consultants, a national hospitalist practice management consulting firm (www.nelsonflores.com). He is co-director and faculty for SHM’s “Best Practices in Managing a Hospital Medicine Program” course. This column represents his views and is not intended to reflect an official position of SHM.
Editor’s note: Second of a two-part series.
Many issues that influence hospitalist budgets, specifically the amount of financial support provided by the hospital, are common in most HM practices. Last month I addressed issues related to collecting professional fee revenue (see “Budget Checkup,” October 2009, p. 54). This month I’ll turn to operations that have a significant influence on the practice’s financial picture.
Staffing and Scheduling
My experience is that hospitalists think carefully about the effect of their chosen schedule on a physician’s lifestyle (e.g., make HM a career path and minimize the risk of burnout) and patient-hospitalist continuity. But rarely do I find evidence that the group has acknowledged the effect of their schedules on the budget.
Here’s a common example. As patient volume grows, most groups find that the volume of admissions from late in the afternoon to around 10 or 11 p.m. is too high for one doctor to manage. So the group decides to add an evening shift (often called a “swing shift”). And because all previous shifts in the practice have been 12 hours long, they decide to make the evening shift last 12 hours as well. Many groups adhere to this physician schedule even if patient volume only requires evening-shift coverage from 5 p.m. until around 10 or 11 at night. By choosing a 12-hour evening shift, rather than the five or six hours that are really needed, the practice may be paying for about six hours of unnecessary coverage each day. Six hours more per day is 42 hours per week; I don’t have to tell you that this system can get really expensive very quickly.
Another common example: A group that uses a seven-on/seven-off schedule will add two new full-time equivalent (FTE) employees at the same time to preserve the symmetry required by the schedule, even if patient volume justifies adding only 0.5 to 1.0 FTE.
My point in these examples is not to suggest the right schedule for your group, but to provide a reminder that the schedule has a significant impact on the budget (see “Staffing Strategies,” January 2007, p. 50).
NPP Roles
Physician assistants and nurse practitioners, which I refer to collectively as non-physician providers (NPPs), can make valuable contributions to hospitalist practices. Just as it would do for an MD hospitalist, a practice should assess NPP contribution to important metrics, such as quality of care, throughput, stakeholder satisfaction, and practice economics. I have worked with practices that never give much thought to whether their NPPs occupy the right roles in the practice—positions that allow NPPs to make significant, cost-effective, and career-satisfying contributions.
A simple exercise that can be very helpful is to determine the total cost to employ NPPs (salary and benefits) and think about whether the practice would be better off if those dollars were spent on physicians. If the return on investing in NPPs is less than the return on investing in physicians, the practice should consider adjusting the NPPs’ roles and/or schedules (see “Role Refinement,” September 2009, p. 53).
I’m not suggesting that the only measure of NPP value is in dollars or professional fee revenue billed. Instead, the group’s return on investment should be viewed broadly and include things that don’t appear in financial statements, such as quality, efficiency, patient satisfaction, etc.
Arbitrary Definitions
SHM’s “2007-2008 Bi-Annual Survey on the State of the Hospital Medicine Movement” shows full-time hospitalists work an average of 2,172 hours annually. This might not be a reliable figure. Even so, many practices define full-time work based on annual hours (or shifts), but the doctors regularly adjust actual number of hours worked depending on that day’s workload, and few practices rigorously track actual hours worked. So I think data on hours worked annually (from SHM or other sources) should not be used as reliable or valid target for a practice.
Annual number of shifts worked can be reported by a practice more reliably but usually isn’t included in surveys because shift lengths can vary significantly from one place to the next. Ultimately, the number of hours or shifts that define full-time work for a given practice is arbitrary. And it has an impact on the budget.
Many—maybe most—practices arrive at a definition of full-time work based on annual hours, and any provider who works more than that number is paid for “extra” hours or shifts. If the number of hours or shifts that define full-time work is set low, the practice will end up paying for a lot of extra hours or shifts. Payment beyond the projected salary allowance can cause the practice budget to balloon.
One test to see if this might be an issue in your practice is to total the compensation and productivity (e.g., work relative value units, or wRVUs, or billable encounters) for each doctor in the practice. Analyze how the compensation per wRVU or encounter compares with survey data. If your group is higher than survey data, then the definition of full-time work might be unreasonably low, and vice versa.
Night-Shift Costs
Hospitalist night shifts tend to result in low productivity until the practice has grown enough that there are six to eight daytime hospitalists (rounder/admitter) for every night-shift doctor. Still, most small practices find that it is worthwhile to schedule a separate in-house night shift. The cost of the additional FTEs required to staff a separate night shift can be significant, and is a reason many very small practices require more financial support per FTE hospitalist from the hospital than larger practices.
In most cases, I think it is in the hospital’s best interest to provide support for a separate night shift (see “Finding and Keeping Dedicated Noctornists,” February 2008, p. 61). If the practice budget, or amount of support required of the hospital, is seen as excessive, it is worth estimating how much of the excess is attributable to the expensive night shift.
One simple way to do this is to think about the amount of hospital support that goes to each doctor during each shift. For example, if a hospitalist works 182 shifts a year and is compensated $230,000 (salary and bonus at $200,000, and benefits at $30,000 annually), then the doctor costs the practice $1,264 per shift. You might conduct an analysis and learn that the doctor averages $900 in collected professional fees during a day shift and $500 during a night shift. That means more hospital support goes to cover a night shift ($764) than a day shift ($364). Put another way, in this example, each night shift worked by a doctor requires $400 more hospital support per shift than the day-shift hospitalist ($764 vs. $364). In most cases, the hospital realizes a significant return on spending the extra money on the night shifts.
Hospitalist Productivity
Some hospitals have systems of care that interfere with hospitalist productivity. These could be such things as a poorly organized medical record, an IT system that requires logging into multiple programs to retrieve data on a single patient, or hospitalists being required to do clerical work. Productivity also is influenced by time spent on nonclinical activities, which leads to decreasing professional fee revenue. Every practice should think carefully about the systems and activities that might be getting in the way of efficiency. TH
Dr. Nelson has been a practicing hospitalist since 1988 and is co-founder and past president of SHM. He is a principal in Nelson Flores Hospital Medicine Consultants, a national hospitalist practice management consulting firm (www.nelsonflores.com). He is co-director and faculty for SHM’s “Best Practices in Managing a Hospital Medicine Program” course. This column represents his views and is not intended to reflect an official position of SHM.
Budget Checkup
Editor’s note: Part one of a two-part series.
Why does a particular hospitalist practice require more than the typical amount of financial support from a hospital? This is one of the most common questions I am asked. This month and next, I will provide a thorough list of potential answers.
SHM’s “2007-2008 Bi-annual Survey on the State of the Hospital Medicine Movement” showed that hospitals pay an average of $97,400 per year in support per full-time hospitalist. I suspect that amount is higher now. Nevertheless, hospital executives and hospitalists should understand the reasons why the hospital support that is required for their practice might be more or less.
A comprehensive list of potential reasons would include dozens of factors, and my intent is only to highlight some of the most common and significant ones.
Documentation, Coding, Billing, and Collecting
This is an area in which many, if not most, practices have room for improvement. One very simple way to estimate how your group is doing on these things is to think about how you’re performing on the following tasks:
- Do the hospitalists really understand the documentation requirements for each CPT code, and is their performance in selecting CPT codes audited regularly (e.g., annually)?1
- Does the group have a reliable method of charge capture that minimizes problems like lost charges? Is there an established “chain of custody” of this information, from the hospitalist to the biller?
- Is there a rigorous review or audit of the biller’s performance? Does the group monitor metrics, such as days in accounts receivable, collection rate, etc.? Is there a periodic audit of the biller? An audit could be as simple as tracking down five to 10 billed encounters from six months prior for each doctor in the practice, and reviewing the status of each bill (e.g., paid, written off, or perhaps the bill has vanished or never made it into the billing system).
- Is revenue appropriately applied to the hospitalist cost center? For many hospital-employed hospitalists, payors might be including their professional fee payments on the same remittance advice as hospital inpatient payments (due to same tax ID number). The hospital’s business office might be unable or unwilling to break these payments into hospital and professional fee portions and apply them correctly. Hospital-employed hospitalists should know whether their collections are being applied to their revenue center accurately.
Payor Mix
The two factors that govern the amount of professional fee revenues a hospitalist practice will collect are the integrity of the billing process (described above) and the payor mix. The payor mix for most hospitalist practices is roughly 55% to 60% Medicare, 5% to 10% self-pay, 5% to 10% Medicaid, and commercial insurance for the rest.
A hospitalist practice that is significantly different from this example should expect professional fee collections to vary accordingly.
Hospitalist Fee Schedule
My experience is that very few hospitalists know their own fee schedule. The term “fee schedule” is generally used to mean the billed charge for each type of service provided. A hospitalist fee schedule usually fits on a single page, with a list of CPT codes (admits, consults, followups, etc.) down one column and the charge for that service in a second column to the right. It would be reasonable to post the fee schedule in hospitalists’ offices.
Groups that use electronic charge capture, in which the doctor enters into a computer the CPT code to bill for each patient daily, can often see the related charge for each code as it is entered.
Someone connected to the practice, often in the billing office, should review the fee schedule—at least annually—to ensure that services aren’t being billed below the rate allowed by payors.
Negotiated Rates Paid by Commercial Insurance
Some hospitalist groups are able to negotiate higher payments than the typical rates paid by commercial payors. Because commercial insurance is a relatively small portion of most hospitalists’ payor mix, this might not have a large impact on the overall practice finances. So my sense is that most groups don’t pursue this opportunity.
Groups in markets with significant managed care are an exception. They usually are aggressive in negotiations for commercial payor rates.
Some hospital-employed HM groups might end up with lower commercial rates than they could have. Here is how it might happen: A hospital negotiates with Aetna to pay rates for hospital services (the bills submitted by the hospital, not the physician bills) that are attractive to the hospital. To make this proposal more palatable to Aetna, the hospital says it will accept lower rates for its employed physicians, including hospitalists. So the hospitalists’ collections end up lower, and the support paid by the hospital to the hospitalist group is correspondingly higher. The hospital ends up fine in this scenario, because it is being paid an attractive rate by Aetna for hospital services, but the hospitalist practice appears to be underperforming financially.
It is worth knowing if this is an issue at your practice, but in most cases it won’t explain larger problems in the hospitalist budget or amount of support required from the hospital.
Accounting Issues
Budgets and financial statements can be confusing, and revenues and expenses might not be what you expect. For example, in my practice, auditors told our accountants that we needed to accrue an extra month of salary into this year’s budget. So when looking at our fiscal year-end financial statement, the salary expense is for 13 months instead of 12 months. This quirk made it appear that we required more than the budgeted amount of support from our hospital, when in fact we performed better than budget this year.
I certainly can’t explain all the reasons for unusual accounting issues, and I still struggle to understand why accrual accounting is better than cash-basis accounting. My best advice is to have the lead hospitalist in your group get to know the accountant who handles your budget and financial statements. The accountant should explain all of these issues clearly.
In next month’s column, I’ll review how a hospitalist practice’s internal operations, such as staffing and scheduling, can have a major influence on the budget and the amount of support required from the hospital. TH
Dr. Nelson has been a practicing hospitalist since 1988 and is co-founder and past president of SHM. He is a principal in Nelson Flores Hospital Medicine Consultants, a national hospitalist practice management consulting firm (www.nelsonflores.com). He is also course co-director and faculty for SHM’s “Best Practices in Managing a Hospital Medicine Program.” This column represents his views and is not intended to reflect an official position of SHM.
Reference
- Centers for Medicare and Medicaid Services. Improper medicare fee-for-service payments report, November 2006: long report. CMS Web site. Available at: www.cms.hhs.gov/apps/er_report/preview_er_report_print.asp?from=public&which=long&reportID=5. Accessed Sept. 1, 2009.
Editor’s note: Part one of a two-part series.
Why does a particular hospitalist practice require more than the typical amount of financial support from a hospital? This is one of the most common questions I am asked. This month and next, I will provide a thorough list of potential answers.
SHM’s “2007-2008 Bi-annual Survey on the State of the Hospital Medicine Movement” showed that hospitals pay an average of $97,400 per year in support per full-time hospitalist. I suspect that amount is higher now. Nevertheless, hospital executives and hospitalists should understand the reasons why the hospital support that is required for their practice might be more or less.
A comprehensive list of potential reasons would include dozens of factors, and my intent is only to highlight some of the most common and significant ones.
Documentation, Coding, Billing, and Collecting
This is an area in which many, if not most, practices have room for improvement. One very simple way to estimate how your group is doing on these things is to think about how you’re performing on the following tasks:
- Do the hospitalists really understand the documentation requirements for each CPT code, and is their performance in selecting CPT codes audited regularly (e.g., annually)?1
- Does the group have a reliable method of charge capture that minimizes problems like lost charges? Is there an established “chain of custody” of this information, from the hospitalist to the biller?
- Is there a rigorous review or audit of the biller’s performance? Does the group monitor metrics, such as days in accounts receivable, collection rate, etc.? Is there a periodic audit of the biller? An audit could be as simple as tracking down five to 10 billed encounters from six months prior for each doctor in the practice, and reviewing the status of each bill (e.g., paid, written off, or perhaps the bill has vanished or never made it into the billing system).
- Is revenue appropriately applied to the hospitalist cost center? For many hospital-employed hospitalists, payors might be including their professional fee payments on the same remittance advice as hospital inpatient payments (due to same tax ID number). The hospital’s business office might be unable or unwilling to break these payments into hospital and professional fee portions and apply them correctly. Hospital-employed hospitalists should know whether their collections are being applied to their revenue center accurately.
Payor Mix
The two factors that govern the amount of professional fee revenues a hospitalist practice will collect are the integrity of the billing process (described above) and the payor mix. The payor mix for most hospitalist practices is roughly 55% to 60% Medicare, 5% to 10% self-pay, 5% to 10% Medicaid, and commercial insurance for the rest.
A hospitalist practice that is significantly different from this example should expect professional fee collections to vary accordingly.
Hospitalist Fee Schedule
My experience is that very few hospitalists know their own fee schedule. The term “fee schedule” is generally used to mean the billed charge for each type of service provided. A hospitalist fee schedule usually fits on a single page, with a list of CPT codes (admits, consults, followups, etc.) down one column and the charge for that service in a second column to the right. It would be reasonable to post the fee schedule in hospitalists’ offices.
Groups that use electronic charge capture, in which the doctor enters into a computer the CPT code to bill for each patient daily, can often see the related charge for each code as it is entered.
Someone connected to the practice, often in the billing office, should review the fee schedule—at least annually—to ensure that services aren’t being billed below the rate allowed by payors.
Negotiated Rates Paid by Commercial Insurance
Some hospitalist groups are able to negotiate higher payments than the typical rates paid by commercial payors. Because commercial insurance is a relatively small portion of most hospitalists’ payor mix, this might not have a large impact on the overall practice finances. So my sense is that most groups don’t pursue this opportunity.
Groups in markets with significant managed care are an exception. They usually are aggressive in negotiations for commercial payor rates.
Some hospital-employed HM groups might end up with lower commercial rates than they could have. Here is how it might happen: A hospital negotiates with Aetna to pay rates for hospital services (the bills submitted by the hospital, not the physician bills) that are attractive to the hospital. To make this proposal more palatable to Aetna, the hospital says it will accept lower rates for its employed physicians, including hospitalists. So the hospitalists’ collections end up lower, and the support paid by the hospital to the hospitalist group is correspondingly higher. The hospital ends up fine in this scenario, because it is being paid an attractive rate by Aetna for hospital services, but the hospitalist practice appears to be underperforming financially.
It is worth knowing if this is an issue at your practice, but in most cases it won’t explain larger problems in the hospitalist budget or amount of support required from the hospital.
Accounting Issues
Budgets and financial statements can be confusing, and revenues and expenses might not be what you expect. For example, in my practice, auditors told our accountants that we needed to accrue an extra month of salary into this year’s budget. So when looking at our fiscal year-end financial statement, the salary expense is for 13 months instead of 12 months. This quirk made it appear that we required more than the budgeted amount of support from our hospital, when in fact we performed better than budget this year.
I certainly can’t explain all the reasons for unusual accounting issues, and I still struggle to understand why accrual accounting is better than cash-basis accounting. My best advice is to have the lead hospitalist in your group get to know the accountant who handles your budget and financial statements. The accountant should explain all of these issues clearly.
In next month’s column, I’ll review how a hospitalist practice’s internal operations, such as staffing and scheduling, can have a major influence on the budget and the amount of support required from the hospital. TH
Dr. Nelson has been a practicing hospitalist since 1988 and is co-founder and past president of SHM. He is a principal in Nelson Flores Hospital Medicine Consultants, a national hospitalist practice management consulting firm (www.nelsonflores.com). He is also course co-director and faculty for SHM’s “Best Practices in Managing a Hospital Medicine Program.” This column represents his views and is not intended to reflect an official position of SHM.
Reference
- Centers for Medicare and Medicaid Services. Improper medicare fee-for-service payments report, November 2006: long report. CMS Web site. Available at: www.cms.hhs.gov/apps/er_report/preview_er_report_print.asp?from=public&which=long&reportID=5. Accessed Sept. 1, 2009.
Editor’s note: Part one of a two-part series.
Why does a particular hospitalist practice require more than the typical amount of financial support from a hospital? This is one of the most common questions I am asked. This month and next, I will provide a thorough list of potential answers.
SHM’s “2007-2008 Bi-annual Survey on the State of the Hospital Medicine Movement” showed that hospitals pay an average of $97,400 per year in support per full-time hospitalist. I suspect that amount is higher now. Nevertheless, hospital executives and hospitalists should understand the reasons why the hospital support that is required for their practice might be more or less.
A comprehensive list of potential reasons would include dozens of factors, and my intent is only to highlight some of the most common and significant ones.
Documentation, Coding, Billing, and Collecting
This is an area in which many, if not most, practices have room for improvement. One very simple way to estimate how your group is doing on these things is to think about how you’re performing on the following tasks:
- Do the hospitalists really understand the documentation requirements for each CPT code, and is their performance in selecting CPT codes audited regularly (e.g., annually)?1
- Does the group have a reliable method of charge capture that minimizes problems like lost charges? Is there an established “chain of custody” of this information, from the hospitalist to the biller?
- Is there a rigorous review or audit of the biller’s performance? Does the group monitor metrics, such as days in accounts receivable, collection rate, etc.? Is there a periodic audit of the biller? An audit could be as simple as tracking down five to 10 billed encounters from six months prior for each doctor in the practice, and reviewing the status of each bill (e.g., paid, written off, or perhaps the bill has vanished or never made it into the billing system).
- Is revenue appropriately applied to the hospitalist cost center? For many hospital-employed hospitalists, payors might be including their professional fee payments on the same remittance advice as hospital inpatient payments (due to same tax ID number). The hospital’s business office might be unable or unwilling to break these payments into hospital and professional fee portions and apply them correctly. Hospital-employed hospitalists should know whether their collections are being applied to their revenue center accurately.
Payor Mix
The two factors that govern the amount of professional fee revenues a hospitalist practice will collect are the integrity of the billing process (described above) and the payor mix. The payor mix for most hospitalist practices is roughly 55% to 60% Medicare, 5% to 10% self-pay, 5% to 10% Medicaid, and commercial insurance for the rest.
A hospitalist practice that is significantly different from this example should expect professional fee collections to vary accordingly.
Hospitalist Fee Schedule
My experience is that very few hospitalists know their own fee schedule. The term “fee schedule” is generally used to mean the billed charge for each type of service provided. A hospitalist fee schedule usually fits on a single page, with a list of CPT codes (admits, consults, followups, etc.) down one column and the charge for that service in a second column to the right. It would be reasonable to post the fee schedule in hospitalists’ offices.
Groups that use electronic charge capture, in which the doctor enters into a computer the CPT code to bill for each patient daily, can often see the related charge for each code as it is entered.
Someone connected to the practice, often in the billing office, should review the fee schedule—at least annually—to ensure that services aren’t being billed below the rate allowed by payors.
Negotiated Rates Paid by Commercial Insurance
Some hospitalist groups are able to negotiate higher payments than the typical rates paid by commercial payors. Because commercial insurance is a relatively small portion of most hospitalists’ payor mix, this might not have a large impact on the overall practice finances. So my sense is that most groups don’t pursue this opportunity.
Groups in markets with significant managed care are an exception. They usually are aggressive in negotiations for commercial payor rates.
Some hospital-employed HM groups might end up with lower commercial rates than they could have. Here is how it might happen: A hospital negotiates with Aetna to pay rates for hospital services (the bills submitted by the hospital, not the physician bills) that are attractive to the hospital. To make this proposal more palatable to Aetna, the hospital says it will accept lower rates for its employed physicians, including hospitalists. So the hospitalists’ collections end up lower, and the support paid by the hospital to the hospitalist group is correspondingly higher. The hospital ends up fine in this scenario, because it is being paid an attractive rate by Aetna for hospital services, but the hospitalist practice appears to be underperforming financially.
It is worth knowing if this is an issue at your practice, but in most cases it won’t explain larger problems in the hospitalist budget or amount of support required from the hospital.
Accounting Issues
Budgets and financial statements can be confusing, and revenues and expenses might not be what you expect. For example, in my practice, auditors told our accountants that we needed to accrue an extra month of salary into this year’s budget. So when looking at our fiscal year-end financial statement, the salary expense is for 13 months instead of 12 months. This quirk made it appear that we required more than the budgeted amount of support from our hospital, when in fact we performed better than budget this year.
I certainly can’t explain all the reasons for unusual accounting issues, and I still struggle to understand why accrual accounting is better than cash-basis accounting. My best advice is to have the lead hospitalist in your group get to know the accountant who handles your budget and financial statements. The accountant should explain all of these issues clearly.
In next month’s column, I’ll review how a hospitalist practice’s internal operations, such as staffing and scheduling, can have a major influence on the budget and the amount of support required from the hospital. TH
Dr. Nelson has been a practicing hospitalist since 1988 and is co-founder and past president of SHM. He is a principal in Nelson Flores Hospital Medicine Consultants, a national hospitalist practice management consulting firm (www.nelsonflores.com). He is also course co-director and faculty for SHM’s “Best Practices in Managing a Hospital Medicine Program.” This column represents his views and is not intended to reflect an official position of SHM.
Reference
- Centers for Medicare and Medicaid Services. Improper medicare fee-for-service payments report, November 2006: long report. CMS Web site. Available at: www.cms.hhs.gov/apps/er_report/preview_er_report_print.asp?from=public&which=long&reportID=5. Accessed Sept. 1, 2009.
Role Refinement
Physician assistants (PAs) and nurse practitioners (NPs), which I will refer to as non-physician providers (NPPs), are popular members of hospitalist practices and have a lot to offer. I think HM groups without NPPs should think about whether adding them would be valuable.
My experience suggests there are many different ways NPPs can contribute to an effective practice. But the optimal NPP role, one that is good for patient care, economically sound for the practice, and satisfying for both the NPP and the MD hospitalists, varies significantly from one practice to the next. I’ve worked with a number of practices that fail to achieve all these goals for a variety of reasons, but a common theme is that the MD hospitalists seem to think the NPPs have been provided for free. As a result, the MDs, and perhaps to some degree the NPPs, feel little or no obligation to develop the optimal NPP job description.
A popular role for NPPs is one very similar to that of the MD hospitalist (e.g., the NPP has a team of patients and rounds and admits daily). That might work well, but for reasons I’ve discussed previously (see “The 411 on NPPs,” September 2008, p. 61), many practices should at least consider other roles for NPPs. One alternative would be to have the NPP work an afternoon-to-night shift (e.g., 3 to 11 p.m.) to handle admissions and “crosscover.” Another option is for the NPP to essentially “own” a component of the practice, such as medical consults for orthopedic patients.
Whatever role is chosen, it must be one that provides the NPP career satisfaction. Over the last few years, I’ve had the pleasure of connecting with Ryan Genzink, PA-C, at various SHM meetings. He essentially is a career hospitalist, and I’ve found him to be a thoughtful guy. At HM09 in Chicago, he and I spoke for a while about NPP roles that provide value and career satisfaction. So I’ve invited him to share his thoughts here.
(Editor’s note: The following is written by Ryan Genzink, PA-C, of Hospitalists of West Michigan in Grand Rapids. He is the AAPA medical liaison to SHM.)
Dr. Nelson correctly observes that while NPPs can be beneficial to HM, there is no “one size fits all” model. However, I think finding the right model for your group sometimes is presented as being more difficult than it really needs to be. Over the years, I have had the opportunity to talk with a number of physicians, PAs, and NPs who work in HM. While models vary, those identified as successful seem to share some common elements.
My story is typical of a lot of PAs working in HM. When I was hired in 2000, my hospital was addressing a workforce shortage. Medical resident workloads were capped, private attending physicians wanted help admitting patients, and the ED was anxious to transfer admitted patients. The hospital was intent on not making our patients wait.
I joined a small group of PAs whose job description included addressing these issues. Like the residents we worked alongside, we took initial calls from the ED, performed histories and physicals, then staffed those with our attending physicians. As a new graduate, I was green and enthusiastic.
The hospitalists were fairly new to working with PAs, too. They had spent years teaching residents, but PAs had joined the group only a year prior. Even so, the group had developed a successful supervision model based on their experiences teaching residents. Patients I saw were cared for by attendings who reviewed the history, asked key questions, performed essential exam elements, and gave the final word on the treatment plan. Teaching naturally flowed from these interactions.
This model continues today. And like the interns who needed less attending input as they transitioned into chief residents, I also required less physician input over time. As our professional relationship grew, the hospitalists became more familiar with my work and exam skills, and I became proficient with our common treatment plans. We functioned together as a team. Of course, this process was no small investment on the part of the hospitalists I worked with. It took time—sometimes with detailed discussions of treatment protocols, or re-examining the patient together to make sure our exams were on the same page. Nonetheless, I think all involved agree the payoff was worth the effort. For our physicians, it made the transition from a resident-based program to one staffed with NPPs favorable. Granted, a residency program has different goals, but because the NPPs don’t rotate off service every six weeks, there is more time to develop collaborative, professional relationships. The investment the attending physicians made stuck.
As work volume increased, PAs in our group expanded into other roles. Our two academic rounding teams, each consisting of one hospitalist and a few residents, added a third team staffed with a hospitalist and a PA. When the residents left, all three teams were staffed with a physician and a PA. NPs later joined the group. And while NPs had slightly different state supervision rules, they functioned in the same roles as the PAs in our facility.
This team approach to rounding works well for our group. The hospitalists and NPPs work together to care for a set group of patients. The hospitalist and the NPP meet in the morning to divide the workload based on acuity, geographic location, and urgency. Sharing a common patient load helps with the common hospitalist dilemma of having to be in two places at the same time. I can see a patient who is ready for discharge (e.g., their ride is on the way), allowing my attending to dedicate his time to another patient’s family conference. In every case, the physician is involved. It is the extent of the involvement that varies. This model gives us flexibility and offers availability to our common patients.
Again, this is one of many successful models. Some, including Dr. Nelson, have suggested that a successful integration model might limit NPPs’ role in the group so that they can have ownership (e.g., post-op consult services). I think there is some merit to this, but this system also has potential unintended consequences.
When we look at what makes hospitalists successful at caring for post-operative patients, we often cite the experience gained from the wide variety of complex medical problems that we address on a daily basis. It is our frequent experience with patients with chronic heart failure that helps us identify the patient in early fluid overload. Our knowledge of diabetic ketoacidosis improves our routine diabetes management.
In my experience, rarely does a patient present with a single, narrowly defined problem. I think that limiting NPPs to the care of specific patient problems will result in limiting their effectiveness and possibly decrease their job satisfaction. I also think HM groups can err on the side of having unrealistic expectations for NPPs. Some groups have them perform the same role as an attending—with an NPP taking the spot of an off-service attending, and vice versa. This can work, if the NPP is experienced. Few would expect a new intern to perform like an attending. Conversely, restricting an NPP to collecting labs and paperwork is not an efficient use of resources.
As Dr. Nelson suggests, successful NPP integration depends on physician leaders being dedicated to the collaborative model and understanding that NPP success is tied to group success. And while admittedly not a perfect test, when in doubt about how an NPP could function in your group, I think asking if a resident would work in the same role is a good starting point. TH
Dr. Nelson has been a practicing hospitalist since 1988 and is co-founder and past president of SHM. He is a principal in Nelson Flores Hospital Medicine Consultants, a national hospitalist practice management consulting firm (www.nelson flores.com). He is co-director and faculty for SHM’s “Best Practices in Managing a Hospital Medicine Program” course. This column represents his views and is not intended to reflect an official position of SHM.
Physician assistants (PAs) and nurse practitioners (NPs), which I will refer to as non-physician providers (NPPs), are popular members of hospitalist practices and have a lot to offer. I think HM groups without NPPs should think about whether adding them would be valuable.
My experience suggests there are many different ways NPPs can contribute to an effective practice. But the optimal NPP role, one that is good for patient care, economically sound for the practice, and satisfying for both the NPP and the MD hospitalists, varies significantly from one practice to the next. I’ve worked with a number of practices that fail to achieve all these goals for a variety of reasons, but a common theme is that the MD hospitalists seem to think the NPPs have been provided for free. As a result, the MDs, and perhaps to some degree the NPPs, feel little or no obligation to develop the optimal NPP job description.
A popular role for NPPs is one very similar to that of the MD hospitalist (e.g., the NPP has a team of patients and rounds and admits daily). That might work well, but for reasons I’ve discussed previously (see “The 411 on NPPs,” September 2008, p. 61), many practices should at least consider other roles for NPPs. One alternative would be to have the NPP work an afternoon-to-night shift (e.g., 3 to 11 p.m.) to handle admissions and “crosscover.” Another option is for the NPP to essentially “own” a component of the practice, such as medical consults for orthopedic patients.
Whatever role is chosen, it must be one that provides the NPP career satisfaction. Over the last few years, I’ve had the pleasure of connecting with Ryan Genzink, PA-C, at various SHM meetings. He essentially is a career hospitalist, and I’ve found him to be a thoughtful guy. At HM09 in Chicago, he and I spoke for a while about NPP roles that provide value and career satisfaction. So I’ve invited him to share his thoughts here.
(Editor’s note: The following is written by Ryan Genzink, PA-C, of Hospitalists of West Michigan in Grand Rapids. He is the AAPA medical liaison to SHM.)
Dr. Nelson correctly observes that while NPPs can be beneficial to HM, there is no “one size fits all” model. However, I think finding the right model for your group sometimes is presented as being more difficult than it really needs to be. Over the years, I have had the opportunity to talk with a number of physicians, PAs, and NPs who work in HM. While models vary, those identified as successful seem to share some common elements.
My story is typical of a lot of PAs working in HM. When I was hired in 2000, my hospital was addressing a workforce shortage. Medical resident workloads were capped, private attending physicians wanted help admitting patients, and the ED was anxious to transfer admitted patients. The hospital was intent on not making our patients wait.
I joined a small group of PAs whose job description included addressing these issues. Like the residents we worked alongside, we took initial calls from the ED, performed histories and physicals, then staffed those with our attending physicians. As a new graduate, I was green and enthusiastic.
The hospitalists were fairly new to working with PAs, too. They had spent years teaching residents, but PAs had joined the group only a year prior. Even so, the group had developed a successful supervision model based on their experiences teaching residents. Patients I saw were cared for by attendings who reviewed the history, asked key questions, performed essential exam elements, and gave the final word on the treatment plan. Teaching naturally flowed from these interactions.
This model continues today. And like the interns who needed less attending input as they transitioned into chief residents, I also required less physician input over time. As our professional relationship grew, the hospitalists became more familiar with my work and exam skills, and I became proficient with our common treatment plans. We functioned together as a team. Of course, this process was no small investment on the part of the hospitalists I worked with. It took time—sometimes with detailed discussions of treatment protocols, or re-examining the patient together to make sure our exams were on the same page. Nonetheless, I think all involved agree the payoff was worth the effort. For our physicians, it made the transition from a resident-based program to one staffed with NPPs favorable. Granted, a residency program has different goals, but because the NPPs don’t rotate off service every six weeks, there is more time to develop collaborative, professional relationships. The investment the attending physicians made stuck.
As work volume increased, PAs in our group expanded into other roles. Our two academic rounding teams, each consisting of one hospitalist and a few residents, added a third team staffed with a hospitalist and a PA. When the residents left, all three teams were staffed with a physician and a PA. NPs later joined the group. And while NPs had slightly different state supervision rules, they functioned in the same roles as the PAs in our facility.
This team approach to rounding works well for our group. The hospitalists and NPPs work together to care for a set group of patients. The hospitalist and the NPP meet in the morning to divide the workload based on acuity, geographic location, and urgency. Sharing a common patient load helps with the common hospitalist dilemma of having to be in two places at the same time. I can see a patient who is ready for discharge (e.g., their ride is on the way), allowing my attending to dedicate his time to another patient’s family conference. In every case, the physician is involved. It is the extent of the involvement that varies. This model gives us flexibility and offers availability to our common patients.
Again, this is one of many successful models. Some, including Dr. Nelson, have suggested that a successful integration model might limit NPPs’ role in the group so that they can have ownership (e.g., post-op consult services). I think there is some merit to this, but this system also has potential unintended consequences.
When we look at what makes hospitalists successful at caring for post-operative patients, we often cite the experience gained from the wide variety of complex medical problems that we address on a daily basis. It is our frequent experience with patients with chronic heart failure that helps us identify the patient in early fluid overload. Our knowledge of diabetic ketoacidosis improves our routine diabetes management.
In my experience, rarely does a patient present with a single, narrowly defined problem. I think that limiting NPPs to the care of specific patient problems will result in limiting their effectiveness and possibly decrease their job satisfaction. I also think HM groups can err on the side of having unrealistic expectations for NPPs. Some groups have them perform the same role as an attending—with an NPP taking the spot of an off-service attending, and vice versa. This can work, if the NPP is experienced. Few would expect a new intern to perform like an attending. Conversely, restricting an NPP to collecting labs and paperwork is not an efficient use of resources.
As Dr. Nelson suggests, successful NPP integration depends on physician leaders being dedicated to the collaborative model and understanding that NPP success is tied to group success. And while admittedly not a perfect test, when in doubt about how an NPP could function in your group, I think asking if a resident would work in the same role is a good starting point. TH
Dr. Nelson has been a practicing hospitalist since 1988 and is co-founder and past president of SHM. He is a principal in Nelson Flores Hospital Medicine Consultants, a national hospitalist practice management consulting firm (www.nelson flores.com). He is co-director and faculty for SHM’s “Best Practices in Managing a Hospital Medicine Program” course. This column represents his views and is not intended to reflect an official position of SHM.
Physician assistants (PAs) and nurse practitioners (NPs), which I will refer to as non-physician providers (NPPs), are popular members of hospitalist practices and have a lot to offer. I think HM groups without NPPs should think about whether adding them would be valuable.
My experience suggests there are many different ways NPPs can contribute to an effective practice. But the optimal NPP role, one that is good for patient care, economically sound for the practice, and satisfying for both the NPP and the MD hospitalists, varies significantly from one practice to the next. I’ve worked with a number of practices that fail to achieve all these goals for a variety of reasons, but a common theme is that the MD hospitalists seem to think the NPPs have been provided for free. As a result, the MDs, and perhaps to some degree the NPPs, feel little or no obligation to develop the optimal NPP job description.
A popular role for NPPs is one very similar to that of the MD hospitalist (e.g., the NPP has a team of patients and rounds and admits daily). That might work well, but for reasons I’ve discussed previously (see “The 411 on NPPs,” September 2008, p. 61), many practices should at least consider other roles for NPPs. One alternative would be to have the NPP work an afternoon-to-night shift (e.g., 3 to 11 p.m.) to handle admissions and “crosscover.” Another option is for the NPP to essentially “own” a component of the practice, such as medical consults for orthopedic patients.
Whatever role is chosen, it must be one that provides the NPP career satisfaction. Over the last few years, I’ve had the pleasure of connecting with Ryan Genzink, PA-C, at various SHM meetings. He essentially is a career hospitalist, and I’ve found him to be a thoughtful guy. At HM09 in Chicago, he and I spoke for a while about NPP roles that provide value and career satisfaction. So I’ve invited him to share his thoughts here.
(Editor’s note: The following is written by Ryan Genzink, PA-C, of Hospitalists of West Michigan in Grand Rapids. He is the AAPA medical liaison to SHM.)
Dr. Nelson correctly observes that while NPPs can be beneficial to HM, there is no “one size fits all” model. However, I think finding the right model for your group sometimes is presented as being more difficult than it really needs to be. Over the years, I have had the opportunity to talk with a number of physicians, PAs, and NPs who work in HM. While models vary, those identified as successful seem to share some common elements.
My story is typical of a lot of PAs working in HM. When I was hired in 2000, my hospital was addressing a workforce shortage. Medical resident workloads were capped, private attending physicians wanted help admitting patients, and the ED was anxious to transfer admitted patients. The hospital was intent on not making our patients wait.
I joined a small group of PAs whose job description included addressing these issues. Like the residents we worked alongside, we took initial calls from the ED, performed histories and physicals, then staffed those with our attending physicians. As a new graduate, I was green and enthusiastic.
The hospitalists were fairly new to working with PAs, too. They had spent years teaching residents, but PAs had joined the group only a year prior. Even so, the group had developed a successful supervision model based on their experiences teaching residents. Patients I saw were cared for by attendings who reviewed the history, asked key questions, performed essential exam elements, and gave the final word on the treatment plan. Teaching naturally flowed from these interactions.
This model continues today. And like the interns who needed less attending input as they transitioned into chief residents, I also required less physician input over time. As our professional relationship grew, the hospitalists became more familiar with my work and exam skills, and I became proficient with our common treatment plans. We functioned together as a team. Of course, this process was no small investment on the part of the hospitalists I worked with. It took time—sometimes with detailed discussions of treatment protocols, or re-examining the patient together to make sure our exams were on the same page. Nonetheless, I think all involved agree the payoff was worth the effort. For our physicians, it made the transition from a resident-based program to one staffed with NPPs favorable. Granted, a residency program has different goals, but because the NPPs don’t rotate off service every six weeks, there is more time to develop collaborative, professional relationships. The investment the attending physicians made stuck.
As work volume increased, PAs in our group expanded into other roles. Our two academic rounding teams, each consisting of one hospitalist and a few residents, added a third team staffed with a hospitalist and a PA. When the residents left, all three teams were staffed with a physician and a PA. NPs later joined the group. And while NPs had slightly different state supervision rules, they functioned in the same roles as the PAs in our facility.
This team approach to rounding works well for our group. The hospitalists and NPPs work together to care for a set group of patients. The hospitalist and the NPP meet in the morning to divide the workload based on acuity, geographic location, and urgency. Sharing a common patient load helps with the common hospitalist dilemma of having to be in two places at the same time. I can see a patient who is ready for discharge (e.g., their ride is on the way), allowing my attending to dedicate his time to another patient’s family conference. In every case, the physician is involved. It is the extent of the involvement that varies. This model gives us flexibility and offers availability to our common patients.
Again, this is one of many successful models. Some, including Dr. Nelson, have suggested that a successful integration model might limit NPPs’ role in the group so that they can have ownership (e.g., post-op consult services). I think there is some merit to this, but this system also has potential unintended consequences.
When we look at what makes hospitalists successful at caring for post-operative patients, we often cite the experience gained from the wide variety of complex medical problems that we address on a daily basis. It is our frequent experience with patients with chronic heart failure that helps us identify the patient in early fluid overload. Our knowledge of diabetic ketoacidosis improves our routine diabetes management.
In my experience, rarely does a patient present with a single, narrowly defined problem. I think that limiting NPPs to the care of specific patient problems will result in limiting their effectiveness and possibly decrease their job satisfaction. I also think HM groups can err on the side of having unrealistic expectations for NPPs. Some groups have them perform the same role as an attending—with an NPP taking the spot of an off-service attending, and vice versa. This can work, if the NPP is experienced. Few would expect a new intern to perform like an attending. Conversely, restricting an NPP to collecting labs and paperwork is not an efficient use of resources.
As Dr. Nelson suggests, successful NPP integration depends on physician leaders being dedicated to the collaborative model and understanding that NPP success is tied to group success. And while admittedly not a perfect test, when in doubt about how an NPP could function in your group, I think asking if a resident would work in the same role is a good starting point. TH
Dr. Nelson has been a practicing hospitalist since 1988 and is co-founder and past president of SHM. He is a principal in Nelson Flores Hospital Medicine Consultants, a national hospitalist practice management consulting firm (www.nelson flores.com). He is co-director and faculty for SHM’s “Best Practices in Managing a Hospital Medicine Program” course. This column represents his views and is not intended to reflect an official position of SHM.
Volume Variables
At sold-out HM09 in Chicago in May, I had the pleasure of moderating a panel discussion titled “Who Says 15 Patients a Day is the Right Number?” As you might guess, each panelist (including me) said, in effect, “No one says 15 patients a day is the right number.”
Despite being a very important issue to SHM, the society doesn’t have an official position on the “right” or optimal daily patient volume or workload for a hospitalist. SHM generates and disseminates a lot of information to help each practice make decisions about workload, including SHM’s 2007-2008 “Bi-annual Survey on the State of the Hospital Medicine Movement,” articles available at www.hospitalmedicine.org, and articles in The Hospitalist. But all practices, and individual hospitalists, will have to decide what level of patient volume enables safe care, a sustainable and satisfying workload, and reasonable economic performance.
Workload Metrics
A problem that makes any workload discussion difficult is that many terms are sometimes used to mean different things. For example, “daily census” is used when comparing workloads between practices, but “daily encounters” is nearly always a more informative metric. Remember, daily encounters for a practice will always be higher (though on rare occasion, the same) than daily census.
The only definition of encounters that can be reliably compared between practices is billable encounters. Confusion arises when one person is reporting billable encounters, and another person is counting as one encounter each time a hospitalist interacted with a patient (e.g., went into the patient’s room or made a chart entry) and reports a higher encounter volume despite having the same workload and patient volume. Of course, billable encounters fail to perfectly describe our workloads, but until someone comes up with a better metric that is universally understood and applicable across all settings, billable encounters is the best metric we have.
Both billable encounters and census can be tricky. We might be convinced that because she averages 17 billable encounters per day, Dr. Krause has a higher workload than Dr. Palmer, who averages 15. But it turns out that Dr. Palmer works 210 shifts annually, generating 3,150 annual encounters; Dr. Krause’s 181 annual shifts generate 3,077 encounters. So while Dr. Krause does indeed work harder on the average day, she has lower annual productivity. My experience is that by failing to compare workloads over long periods, such as a year, many attempts to compare workloads yield misleading conclusions.
Comparing encounter volume from one practice to the next fails to capture other ways workloads differ. Dr. Krause may be the principal caregiver for a number of ICU patients; Dr. Plant might turn such patients over to intensivists. For this reason, work relative value units (wRVUs), which attempt to capture the complexity of each encounter, usually are a more meaningful—though still imperfect—metric.
Apples vs. Apples
Any truly valid method of comparing workloads should sum the annual workload for the entire practice and divide by the total provider full-time equivalents (FTEs). Yet problems arise because night shifts usually are less productive than day shifts. Consider a practice that has a distinct night shift worked by a doctor who does no day-shift work the day before or after. There is a tendency to leave this night shift out of the analysis of average workload per FTE, which makes the practice appear more productive than it really is.
For example, the practice I am part of has dedicated nocturnists who don’t work day shifts. So when thinking about how hard we’re working, we tend to sum each “day” doctor’s wRVUs for the year and divide by the number of day doctors. Calculated this way, our day doctors appear to be more productive than SHM data might indicate, but when including our nocturnists’ production and FTEs in the analysis, the overall workload per FTE in the practice is similar to the data.
Productivity Per FTE
While I think productivity per FTE per year is the best metric to use when comparing a practice to external survey data or comparing one practice to another, it is confounded by two sticky problems: inconsistent definitions of what constitutes an FTE, and the lack of an agreed-upon method of accounting for the contribution of nonphysician providers.
The most common definitions of what constitutes an FTE are based on the number of hours or shifts worked. One practice might define an FTE as 2,000 hours of work annually; another might use 180 annual shifts. Unless each shift has a clearly defined duration, it will be very difficult to reach conclusions. Although each practice might make sound decisions about how they define an FTE, they’re ultimately making arbitrary choices that aren’t consistent from one practice to the next. Controlling for this issue is very difficult.
Even trickier is how to compare the contributions of physician assistants (PAs) and nurse practitioners (NPs) from one practice to the next. In the above example, Dr. Plant’s practice has eight physician FTEs and four NPPs, and Dr. Krause’s group has eight MDs and no NPPs. How much more productive should we expect Dr. Plant’s practice to be? (NPPs make many valuable contributions, in addition to increasing productivity, but these are outside the scope of this article.)
Though survey data offer some clues, there is no established standard for increased productivity expected of PAs and NPs. One approach I use is to compare an NPP’s total compensation (salary and benefits) with that of the average physician FTE. If the cost of each NPP is 60% of an MD, then one could say that each NPP represents 0.6 “physician FTE equivalents” and could be expected to increase the productivity of the practice proportionately. So Dr. Plant’s group might be expected to have the productivity of 10.2 physician FTEs (4 NPPs X 0.6 = 2.2 “physician FTE equivalents,” added to the eight physician FTEs). (Note: While I think converting NPP FTEs into “physician equivalents” is useful in analyzing the effect of workloads on budgets, there are clearly many other very important issues when trying to quantify the contribution of NPPs to a practice.)
Judgment Rules
There are dozens of additional issues, such as the effect on productivity resulting from inefficient hospital systems (e.g., a clunky electronic health record, typed admit notes aren’t available for a few days compared with records available within two to four hours of dictation), activities such as attending Rapid Response Team activations, and differences in the social complexity of the patient population. None of these would show up in wRVU reports, so they are missing from the analysis I’ve described above.
I think it is impossible to control for all of the differences between practices that influence the definition of appropriate workload. This is the main reason SHM probably will never have a firm position on exactly what is the right or optimal number.
Although 15 patients a day is a reasonable starting point (I prefer to see fewer patients daily, but work more days/shifts annually), things get complicated in a hurry, and there will always be significant variation. TH
Dr. Nelson has been a practicing hospitalist since 1988 and is co-founder and past president of SHM. He is a principal in Nelson/Flores Associates, a national hospitalist practice management consulting firm. He also is faculty for SHM’s “Best Practices in Managing a Hospital Medicine Program” course. This column represents his views and is not intended to reflect an official position of SHM.
At sold-out HM09 in Chicago in May, I had the pleasure of moderating a panel discussion titled “Who Says 15 Patients a Day is the Right Number?” As you might guess, each panelist (including me) said, in effect, “No one says 15 patients a day is the right number.”
Despite being a very important issue to SHM, the society doesn’t have an official position on the “right” or optimal daily patient volume or workload for a hospitalist. SHM generates and disseminates a lot of information to help each practice make decisions about workload, including SHM’s 2007-2008 “Bi-annual Survey on the State of the Hospital Medicine Movement,” articles available at www.hospitalmedicine.org, and articles in The Hospitalist. But all practices, and individual hospitalists, will have to decide what level of patient volume enables safe care, a sustainable and satisfying workload, and reasonable economic performance.
Workload Metrics
A problem that makes any workload discussion difficult is that many terms are sometimes used to mean different things. For example, “daily census” is used when comparing workloads between practices, but “daily encounters” is nearly always a more informative metric. Remember, daily encounters for a practice will always be higher (though on rare occasion, the same) than daily census.
The only definition of encounters that can be reliably compared between practices is billable encounters. Confusion arises when one person is reporting billable encounters, and another person is counting as one encounter each time a hospitalist interacted with a patient (e.g., went into the patient’s room or made a chart entry) and reports a higher encounter volume despite having the same workload and patient volume. Of course, billable encounters fail to perfectly describe our workloads, but until someone comes up with a better metric that is universally understood and applicable across all settings, billable encounters is the best metric we have.
Both billable encounters and census can be tricky. We might be convinced that because she averages 17 billable encounters per day, Dr. Krause has a higher workload than Dr. Palmer, who averages 15. But it turns out that Dr. Palmer works 210 shifts annually, generating 3,150 annual encounters; Dr. Krause’s 181 annual shifts generate 3,077 encounters. So while Dr. Krause does indeed work harder on the average day, she has lower annual productivity. My experience is that by failing to compare workloads over long periods, such as a year, many attempts to compare workloads yield misleading conclusions.
Comparing encounter volume from one practice to the next fails to capture other ways workloads differ. Dr. Krause may be the principal caregiver for a number of ICU patients; Dr. Plant might turn such patients over to intensivists. For this reason, work relative value units (wRVUs), which attempt to capture the complexity of each encounter, usually are a more meaningful—though still imperfect—metric.
Apples vs. Apples
Any truly valid method of comparing workloads should sum the annual workload for the entire practice and divide by the total provider full-time equivalents (FTEs). Yet problems arise because night shifts usually are less productive than day shifts. Consider a practice that has a distinct night shift worked by a doctor who does no day-shift work the day before or after. There is a tendency to leave this night shift out of the analysis of average workload per FTE, which makes the practice appear more productive than it really is.
For example, the practice I am part of has dedicated nocturnists who don’t work day shifts. So when thinking about how hard we’re working, we tend to sum each “day” doctor’s wRVUs for the year and divide by the number of day doctors. Calculated this way, our day doctors appear to be more productive than SHM data might indicate, but when including our nocturnists’ production and FTEs in the analysis, the overall workload per FTE in the practice is similar to the data.
Productivity Per FTE
While I think productivity per FTE per year is the best metric to use when comparing a practice to external survey data or comparing one practice to another, it is confounded by two sticky problems: inconsistent definitions of what constitutes an FTE, and the lack of an agreed-upon method of accounting for the contribution of nonphysician providers.
The most common definitions of what constitutes an FTE are based on the number of hours or shifts worked. One practice might define an FTE as 2,000 hours of work annually; another might use 180 annual shifts. Unless each shift has a clearly defined duration, it will be very difficult to reach conclusions. Although each practice might make sound decisions about how they define an FTE, they’re ultimately making arbitrary choices that aren’t consistent from one practice to the next. Controlling for this issue is very difficult.
Even trickier is how to compare the contributions of physician assistants (PAs) and nurse practitioners (NPs) from one practice to the next. In the above example, Dr. Plant’s practice has eight physician FTEs and four NPPs, and Dr. Krause’s group has eight MDs and no NPPs. How much more productive should we expect Dr. Plant’s practice to be? (NPPs make many valuable contributions, in addition to increasing productivity, but these are outside the scope of this article.)
Though survey data offer some clues, there is no established standard for increased productivity expected of PAs and NPs. One approach I use is to compare an NPP’s total compensation (salary and benefits) with that of the average physician FTE. If the cost of each NPP is 60% of an MD, then one could say that each NPP represents 0.6 “physician FTE equivalents” and could be expected to increase the productivity of the practice proportionately. So Dr. Plant’s group might be expected to have the productivity of 10.2 physician FTEs (4 NPPs X 0.6 = 2.2 “physician FTE equivalents,” added to the eight physician FTEs). (Note: While I think converting NPP FTEs into “physician equivalents” is useful in analyzing the effect of workloads on budgets, there are clearly many other very important issues when trying to quantify the contribution of NPPs to a practice.)
Judgment Rules
There are dozens of additional issues, such as the effect on productivity resulting from inefficient hospital systems (e.g., a clunky electronic health record, typed admit notes aren’t available for a few days compared with records available within two to four hours of dictation), activities such as attending Rapid Response Team activations, and differences in the social complexity of the patient population. None of these would show up in wRVU reports, so they are missing from the analysis I’ve described above.
I think it is impossible to control for all of the differences between practices that influence the definition of appropriate workload. This is the main reason SHM probably will never have a firm position on exactly what is the right or optimal number.
Although 15 patients a day is a reasonable starting point (I prefer to see fewer patients daily, but work more days/shifts annually), things get complicated in a hurry, and there will always be significant variation. TH
Dr. Nelson has been a practicing hospitalist since 1988 and is co-founder and past president of SHM. He is a principal in Nelson/Flores Associates, a national hospitalist practice management consulting firm. He also is faculty for SHM’s “Best Practices in Managing a Hospital Medicine Program” course. This column represents his views and is not intended to reflect an official position of SHM.
At sold-out HM09 in Chicago in May, I had the pleasure of moderating a panel discussion titled “Who Says 15 Patients a Day is the Right Number?” As you might guess, each panelist (including me) said, in effect, “No one says 15 patients a day is the right number.”
Despite being a very important issue to SHM, the society doesn’t have an official position on the “right” or optimal daily patient volume or workload for a hospitalist. SHM generates and disseminates a lot of information to help each practice make decisions about workload, including SHM’s 2007-2008 “Bi-annual Survey on the State of the Hospital Medicine Movement,” articles available at www.hospitalmedicine.org, and articles in The Hospitalist. But all practices, and individual hospitalists, will have to decide what level of patient volume enables safe care, a sustainable and satisfying workload, and reasonable economic performance.
Workload Metrics
A problem that makes any workload discussion difficult is that many terms are sometimes used to mean different things. For example, “daily census” is used when comparing workloads between practices, but “daily encounters” is nearly always a more informative metric. Remember, daily encounters for a practice will always be higher (though on rare occasion, the same) than daily census.
The only definition of encounters that can be reliably compared between practices is billable encounters. Confusion arises when one person is reporting billable encounters, and another person is counting as one encounter each time a hospitalist interacted with a patient (e.g., went into the patient’s room or made a chart entry) and reports a higher encounter volume despite having the same workload and patient volume. Of course, billable encounters fail to perfectly describe our workloads, but until someone comes up with a better metric that is universally understood and applicable across all settings, billable encounters is the best metric we have.
Both billable encounters and census can be tricky. We might be convinced that because she averages 17 billable encounters per day, Dr. Krause has a higher workload than Dr. Palmer, who averages 15. But it turns out that Dr. Palmer works 210 shifts annually, generating 3,150 annual encounters; Dr. Krause’s 181 annual shifts generate 3,077 encounters. So while Dr. Krause does indeed work harder on the average day, she has lower annual productivity. My experience is that by failing to compare workloads over long periods, such as a year, many attempts to compare workloads yield misleading conclusions.
Comparing encounter volume from one practice to the next fails to capture other ways workloads differ. Dr. Krause may be the principal caregiver for a number of ICU patients; Dr. Plant might turn such patients over to intensivists. For this reason, work relative value units (wRVUs), which attempt to capture the complexity of each encounter, usually are a more meaningful—though still imperfect—metric.
Apples vs. Apples
Any truly valid method of comparing workloads should sum the annual workload for the entire practice and divide by the total provider full-time equivalents (FTEs). Yet problems arise because night shifts usually are less productive than day shifts. Consider a practice that has a distinct night shift worked by a doctor who does no day-shift work the day before or after. There is a tendency to leave this night shift out of the analysis of average workload per FTE, which makes the practice appear more productive than it really is.
For example, the practice I am part of has dedicated nocturnists who don’t work day shifts. So when thinking about how hard we’re working, we tend to sum each “day” doctor’s wRVUs for the year and divide by the number of day doctors. Calculated this way, our day doctors appear to be more productive than SHM data might indicate, but when including our nocturnists’ production and FTEs in the analysis, the overall workload per FTE in the practice is similar to the data.
Productivity Per FTE
While I think productivity per FTE per year is the best metric to use when comparing a practice to external survey data or comparing one practice to another, it is confounded by two sticky problems: inconsistent definitions of what constitutes an FTE, and the lack of an agreed-upon method of accounting for the contribution of nonphysician providers.
The most common definitions of what constitutes an FTE are based on the number of hours or shifts worked. One practice might define an FTE as 2,000 hours of work annually; another might use 180 annual shifts. Unless each shift has a clearly defined duration, it will be very difficult to reach conclusions. Although each practice might make sound decisions about how they define an FTE, they’re ultimately making arbitrary choices that aren’t consistent from one practice to the next. Controlling for this issue is very difficult.
Even trickier is how to compare the contributions of physician assistants (PAs) and nurse practitioners (NPs) from one practice to the next. In the above example, Dr. Plant’s practice has eight physician FTEs and four NPPs, and Dr. Krause’s group has eight MDs and no NPPs. How much more productive should we expect Dr. Plant’s practice to be? (NPPs make many valuable contributions, in addition to increasing productivity, but these are outside the scope of this article.)
Though survey data offer some clues, there is no established standard for increased productivity expected of PAs and NPs. One approach I use is to compare an NPP’s total compensation (salary and benefits) with that of the average physician FTE. If the cost of each NPP is 60% of an MD, then one could say that each NPP represents 0.6 “physician FTE equivalents” and could be expected to increase the productivity of the practice proportionately. So Dr. Plant’s group might be expected to have the productivity of 10.2 physician FTEs (4 NPPs X 0.6 = 2.2 “physician FTE equivalents,” added to the eight physician FTEs). (Note: While I think converting NPP FTEs into “physician equivalents” is useful in analyzing the effect of workloads on budgets, there are clearly many other very important issues when trying to quantify the contribution of NPPs to a practice.)
Judgment Rules
There are dozens of additional issues, such as the effect on productivity resulting from inefficient hospital systems (e.g., a clunky electronic health record, typed admit notes aren’t available for a few days compared with records available within two to four hours of dictation), activities such as attending Rapid Response Team activations, and differences in the social complexity of the patient population. None of these would show up in wRVU reports, so they are missing from the analysis I’ve described above.
I think it is impossible to control for all of the differences between practices that influence the definition of appropriate workload. This is the main reason SHM probably will never have a firm position on exactly what is the right or optimal number.
Although 15 patients a day is a reasonable starting point (I prefer to see fewer patients daily, but work more days/shifts annually), things get complicated in a hurry, and there will always be significant variation. TH
Dr. Nelson has been a practicing hospitalist since 1988 and is co-founder and past president of SHM. He is a principal in Nelson/Flores Associates, a national hospitalist practice management consulting firm. He also is faculty for SHM’s “Best Practices in Managing a Hospital Medicine Program” course. This column represents his views and is not intended to reflect an official position of SHM.
Internal Peer Review
As far as I can tell, few hospitalist groups conduct any sort of formal peer review. Most seem to rely on the hospital’s medical staff peer review to encourage quality of care and address shortcomings; the review is often coupled with a salary incentive paid for good performance on certain quality metrics. While these reviews are of some value, I think they are pretty blunt instruments. Every hospitalist practice should think about developing a more robust system of peer review for their group.
Review Categories
Assessment of each provider’s individual performance, whether they are an MD, nurse practitioner, or physician assistant, can be divided into three general categories. The first is the traditional “human resources” category of performance, which includes whether the person gets along well with others in the practice as well as other hospital staff, patients, and families. Does the person arrive at work when scheduled, manage time effectively, and work efficiently? Do nurses and other hospital staff have compliments or complaints about this doctor?
The second category of performance can encompass the hospitalist’s business and operational contributions to the practice. Do they document, code, and bill visits correctly? Do they attend and participate in meetings and serve on one or more hospital committees?
The third category assesses measurable quality of care. This could include an assessment of mortality, readmission rate, performance on such quality metrics as core measures, and performance on selected initiatives (e.g., appropriate VTE prophylaxis). Aggregate data for these measures can be difficult to attribute to a single hospitalist, so this may require a review of individual charts instead of relying on reports generated by the hospital’s data systems.
A number of metrics might apply to more than one of the three categories. For example, documenting accurate medicine reconciliation can be thought of as both a quality issue (good for patients) and a business issue (e.g., your hospital might provide a financial reward to your group for good performance). Ensuring the referring physician is “CC’d” on all dictated reports is both a quality and business issue. It really doesn’t matter which category you put these in.
The categories I have listed, and the sample items in each, are intended as examples. You should think about the unique attributes of your practice and its current priorities in order to develop the best internal peer review system for your group. You probably will want to change metrics periodically. For example, you may choose to focus on VTE prophylaxis for now, but at some point it may make sense to replace it with a new metric, such as glycemic control.
Manage the Review
There is no single right approach to conducting your own peer review. Just make sure that the process is fair and meaningful for all involved. The process probably will be more valuable if most of the data on each hospitalist can be reviewed by the whole group, or at least by a designated peer review committee. The main exceptions to such transparency are issues in the first human resources category. If a nurse or another hospitalist has specific criticisms of one hospitalist, it is best not to share that information with the whole group. But it should be fine for everyone in the group to know who is best and worst at things like documenting and coding visits or ordering VTE prophylaxis when needed. Beyond these general principles, the specific process your group uses for peer review can take many forms.
It may make sense to form a peer review committee that performs all the reviews on everyone in the group, including the members of the committee itself. Each member of the committee should have a specified term, such as one or two years. It might not make sense for some groups, especially ones with less than 10 hospitalists, to have a formal committee. In that case, every member of the group could serve as a reviewer for all other doctors except themselves.
The group should hold formal peer review sessions quarterly or semi-annually. The group for which I serve as medical director reviews about one-fourth of the doctors at a roughly two-hour meeting each quarter. Prior to each meeting, we conduct a survey (see Figure 1) using a free Web-based tool to collect opinions about the doctors under review. We use SurveyMonkey.com, though there are many other options. The tool makes it easy to send reminders to get everyone to complete the survey and to collect and analyze the results. At the beginning of the meeting, the medical director of the practice reviews the results with the doctor being surveyed; they are not shared with others.
Most of the meeting time is spent assessing 10 charts for the doctor under review. Using the billing system, we select patients the doctor saw for many consecutive days. We want to avoid pulling charts at random only to find that the doctor only made one visit and there isn’t much to review. We assess a number of measures:
- Was VTE prophylaxis addressed appropriately?
- Was the referring doctor CC’d in the dictated reports?
- Did the doctor choose the appropriate CPT code for each visit?
- Was there a good plan for transition of care at discharge?
The doctor is provided a summary of all the findings of the peer review session, and a copy is kept on file. TH
Dr. Nelson has been a practicing hospitalist since 1988 and is co-founder and past president of SHM. He is a principal in Nelson/Flores Associates, a national hospitalist practice management consulting firm. He also is part of the faculty for SHM’s “Best Practices in Managing a Hospital Medicine Program” course. This column represents his views and is not intended to reflect an official position of SHM.
As far as I can tell, few hospitalist groups conduct any sort of formal peer review. Most seem to rely on the hospital’s medical staff peer review to encourage quality of care and address shortcomings; the review is often coupled with a salary incentive paid for good performance on certain quality metrics. While these reviews are of some value, I think they are pretty blunt instruments. Every hospitalist practice should think about developing a more robust system of peer review for their group.
Review Categories
Assessment of each provider’s individual performance, whether they are an MD, nurse practitioner, or physician assistant, can be divided into three general categories. The first is the traditional “human resources” category of performance, which includes whether the person gets along well with others in the practice as well as other hospital staff, patients, and families. Does the person arrive at work when scheduled, manage time effectively, and work efficiently? Do nurses and other hospital staff have compliments or complaints about this doctor?
The second category of performance can encompass the hospitalist’s business and operational contributions to the practice. Do they document, code, and bill visits correctly? Do they attend and participate in meetings and serve on one or more hospital committees?
The third category assesses measurable quality of care. This could include an assessment of mortality, readmission rate, performance on such quality metrics as core measures, and performance on selected initiatives (e.g., appropriate VTE prophylaxis). Aggregate data for these measures can be difficult to attribute to a single hospitalist, so this may require a review of individual charts instead of relying on reports generated by the hospital’s data systems.
A number of metrics might apply to more than one of the three categories. For example, documenting accurate medicine reconciliation can be thought of as both a quality issue (good for patients) and a business issue (e.g., your hospital might provide a financial reward to your group for good performance). Ensuring the referring physician is “CC’d” on all dictated reports is both a quality and business issue. It really doesn’t matter which category you put these in.
The categories I have listed, and the sample items in each, are intended as examples. You should think about the unique attributes of your practice and its current priorities in order to develop the best internal peer review system for your group. You probably will want to change metrics periodically. For example, you may choose to focus on VTE prophylaxis for now, but at some point it may make sense to replace it with a new metric, such as glycemic control.
Manage the Review
There is no single right approach to conducting your own peer review. Just make sure that the process is fair and meaningful for all involved. The process probably will be more valuable if most of the data on each hospitalist can be reviewed by the whole group, or at least by a designated peer review committee. The main exceptions to such transparency are issues in the first human resources category. If a nurse or another hospitalist has specific criticisms of one hospitalist, it is best not to share that information with the whole group. But it should be fine for everyone in the group to know who is best and worst at things like documenting and coding visits or ordering VTE prophylaxis when needed. Beyond these general principles, the specific process your group uses for peer review can take many forms.
It may make sense to form a peer review committee that performs all the reviews on everyone in the group, including the members of the committee itself. Each member of the committee should have a specified term, such as one or two years. It might not make sense for some groups, especially ones with less than 10 hospitalists, to have a formal committee. In that case, every member of the group could serve as a reviewer for all other doctors except themselves.
The group should hold formal peer review sessions quarterly or semi-annually. The group for which I serve as medical director reviews about one-fourth of the doctors at a roughly two-hour meeting each quarter. Prior to each meeting, we conduct a survey (see Figure 1) using a free Web-based tool to collect opinions about the doctors under review. We use SurveyMonkey.com, though there are many other options. The tool makes it easy to send reminders to get everyone to complete the survey and to collect and analyze the results. At the beginning of the meeting, the medical director of the practice reviews the results with the doctor being surveyed; they are not shared with others.
Most of the meeting time is spent assessing 10 charts for the doctor under review. Using the billing system, we select patients the doctor saw for many consecutive days. We want to avoid pulling charts at random only to find that the doctor only made one visit and there isn’t much to review. We assess a number of measures:
- Was VTE prophylaxis addressed appropriately?
- Was the referring doctor CC’d in the dictated reports?
- Did the doctor choose the appropriate CPT code for each visit?
- Was there a good plan for transition of care at discharge?
The doctor is provided a summary of all the findings of the peer review session, and a copy is kept on file. TH
Dr. Nelson has been a practicing hospitalist since 1988 and is co-founder and past president of SHM. He is a principal in Nelson/Flores Associates, a national hospitalist practice management consulting firm. He also is part of the faculty for SHM’s “Best Practices in Managing a Hospital Medicine Program” course. This column represents his views and is not intended to reflect an official position of SHM.
As far as I can tell, few hospitalist groups conduct any sort of formal peer review. Most seem to rely on the hospital’s medical staff peer review to encourage quality of care and address shortcomings; the review is often coupled with a salary incentive paid for good performance on certain quality metrics. While these reviews are of some value, I think they are pretty blunt instruments. Every hospitalist practice should think about developing a more robust system of peer review for their group.
Review Categories
Assessment of each provider’s individual performance, whether they are an MD, nurse practitioner, or physician assistant, can be divided into three general categories. The first is the traditional “human resources” category of performance, which includes whether the person gets along well with others in the practice as well as other hospital staff, patients, and families. Does the person arrive at work when scheduled, manage time effectively, and work efficiently? Do nurses and other hospital staff have compliments or complaints about this doctor?
The second category of performance can encompass the hospitalist’s business and operational contributions to the practice. Do they document, code, and bill visits correctly? Do they attend and participate in meetings and serve on one or more hospital committees?
The third category assesses measurable quality of care. This could include an assessment of mortality, readmission rate, performance on such quality metrics as core measures, and performance on selected initiatives (e.g., appropriate VTE prophylaxis). Aggregate data for these measures can be difficult to attribute to a single hospitalist, so this may require a review of individual charts instead of relying on reports generated by the hospital’s data systems.
A number of metrics might apply to more than one of the three categories. For example, documenting accurate medicine reconciliation can be thought of as both a quality issue (good for patients) and a business issue (e.g., your hospital might provide a financial reward to your group for good performance). Ensuring the referring physician is “CC’d” on all dictated reports is both a quality and business issue. It really doesn’t matter which category you put these in.
The categories I have listed, and the sample items in each, are intended as examples. You should think about the unique attributes of your practice and its current priorities in order to develop the best internal peer review system for your group. You probably will want to change metrics periodically. For example, you may choose to focus on VTE prophylaxis for now, but at some point it may make sense to replace it with a new metric, such as glycemic control.
Manage the Review
There is no single right approach to conducting your own peer review. Just make sure that the process is fair and meaningful for all involved. The process probably will be more valuable if most of the data on each hospitalist can be reviewed by the whole group, or at least by a designated peer review committee. The main exceptions to such transparency are issues in the first human resources category. If a nurse or another hospitalist has specific criticisms of one hospitalist, it is best not to share that information with the whole group. But it should be fine for everyone in the group to know who is best and worst at things like documenting and coding visits or ordering VTE prophylaxis when needed. Beyond these general principles, the specific process your group uses for peer review can take many forms.
It may make sense to form a peer review committee that performs all the reviews on everyone in the group, including the members of the committee itself. Each member of the committee should have a specified term, such as one or two years. It might not make sense for some groups, especially ones with less than 10 hospitalists, to have a formal committee. In that case, every member of the group could serve as a reviewer for all other doctors except themselves.
The group should hold formal peer review sessions quarterly or semi-annually. The group for which I serve as medical director reviews about one-fourth of the doctors at a roughly two-hour meeting each quarter. Prior to each meeting, we conduct a survey (see Figure 1) using a free Web-based tool to collect opinions about the doctors under review. We use SurveyMonkey.com, though there are many other options. The tool makes it easy to send reminders to get everyone to complete the survey and to collect and analyze the results. At the beginning of the meeting, the medical director of the practice reviews the results with the doctor being surveyed; they are not shared with others.
Most of the meeting time is spent assessing 10 charts for the doctor under review. Using the billing system, we select patients the doctor saw for many consecutive days. We want to avoid pulling charts at random only to find that the doctor only made one visit and there isn’t much to review. We assess a number of measures:
- Was VTE prophylaxis addressed appropriately?
- Was the referring doctor CC’d in the dictated reports?
- Did the doctor choose the appropriate CPT code for each visit?
- Was there a good plan for transition of care at discharge?
The doctor is provided a summary of all the findings of the peer review session, and a copy is kept on file. TH
Dr. Nelson has been a practicing hospitalist since 1988 and is co-founder and past president of SHM. He is a principal in Nelson/Flores Associates, a national hospitalist practice management consulting firm. He also is part of the faculty for SHM’s “Best Practices in Managing a Hospital Medicine Program” course. This column represents his views and is not intended to reflect an official position of SHM.