User login
Long-term management of patients with unstable angina and NSTEMI
- Immediately upon presentation of non-ST-elevation myocardial infarction (NSTEMI), aspirin therapy (81–325 mg) should be initiated (A). If aspirin is contraindicated, clopidogrel (300-mg loading dose followed by 75 mg/d) should be administered (A).
- In patients for whom an early noninterventional approach is planned, or for patients not at high risk of bleeding for whom percutaneous coronary intervention (PCI) is planned, clopidogrel 75 mg (once daily) should be added to aspirin therapy as quickly as possible and continued for up to 9 months (B).
- Aggressive low-density lipoprotein (LDL) cholesterol-lowering therapy and general cardiovascular risk reduction are important in long-term management of these patients. Thus, a fibrate or niacin should be administered if the high-density lipoprotein (HDL) cholesterol is <40 mg/dL (B).
- In patients with LDL cholesterol >100 mg/dL, HMG-CoA reductase inhibitors (statins) and diet should be started during admission and continued after discharge (B).
In the long-term care of patients with acute coronary syndrome, recently published w that prognostic benefits improve with more aggressive antiplatelet therapy for those at high risk for recurrent events. Moreover, long-term care should include aggressive LDL cholesterol-lowering therapy and use of beta-blockers and angiotensin-converting enzyme (ACE) inhibitors, in addition to diet modification and exercise.
STEMI and NSTEMI: The new nomenclature
Coronary artery disease, the leading cause of death in the United States,1 can manifest in many ways involving a constellation of symptoms, electrocardiogram changes, and serum markers. These acute coronary syndromes result from decreased coronary blood flow and cause chest discomfort, usually at rest, with or without characteristic radiation, or such comparable anginal equivalents as weakness, dyspnea, and diaphoresis.
STEMI. An elevated ST-segment with elevated levels of such cardiac markers as creatine kinase myocardial band or troponin I or troponin T are consistent with a diagnosis of ST-elevation myocardial infarction (STEMI). The old term, acute myocardial infarction, was defined by the presence of pathological Q waves (Q wave MI).
NSTEMI. Patients with elevated serum levels of creatine kinase myocardial band or troponin I or troponin T, but no ST-segment elevation, are said to have non-ST-elevation myocardial infarction (NSTEMI).
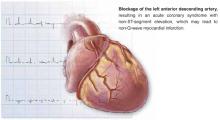
Unstable angina. Normal levels of serum cardiac markers and an absence of ST-elevation are consistent with a diagnosis of unstable angina (Figure). Of patients with STEMI, most will ultimately experience a Q-wave MI; a minority will have a non–Q-wave MI. Of patients with NSTEMI, most will sustain a non–Q-wave MI, while a minority will sustain a Q-wave MI.
Unstable angina and NSTEMI are urgent and life-threatening problems. Chest pain and related symptoms account for 5.3 million visits to US emergency departments per year2 and account for 1.4 million hospitalizations annually.3 Approximately 15% of those presenting with unstable angina and NSTEMI go on to (re)infarct or die within 30 days.4
FIGURE
Unstable angina and NSTEMI
FIGURE
Nomenclature of acute coronary syndrome
ACC/AHA Guidelines
In 2000 the American College of Cardiology and the American Heart Association (ACC/AHA) Task Force on Practice Guidelines published their evidence-based recommendations for treatment of unstable angina/NSTEMI following an exhaustive review of the literature.
New trials in acute coronary syndromes
Since 2000, knowledge of acute coronary syndromes advanced considerably with results of large pivotal randomized controlled studies, which necessitated updating the ACC/AHA guidelines just 21 months after their completion. The most notable of these studies were the Clopidogrel in Unstable Angina to Prevent Recurrent Ischemic Events (CURE) trial,6 the Percutaneous Coronary Intervention (PCI)-CURE7 subset analysis, and the Myocardial Ischemia Reduction with Aggressive Cholesterol Lowering (MIRACL) trial.8
Although incorporation of antiplatelet therapy is the focus of this article, the ultimate objective of the new revised guidelines is improved clinical outcomes for patients with acute coronary syndromes by improving early risk assessment, using revascularization procedures aggressively when risk for future cardiac events is high, using short- and long-term antiplatelet and antithrombotic agents, and modifying long-term risk.
2002 revised guidelines
The studies reviewed in the 2002 revised guidelines assessed multiple therapies in the reduction of recurrent MI, stroke, and other cardiovascular events following patients’ presentation with unstable angina and NSTEMI. The studies also evaluated traditional therapies for acute coronary syndromes, such as unfractionated heparin, beta-blockers, and aspirin, as well as more recent therapies, including low-molecular-weight heparin, antiplatelet therapy (parenteral glycoprotein IIb/IIIa [GP IIb/IIIa] antagonists and ADP-receptor antagonists [thienopyridines]), lipid-lowering therapy (HMG-CoA reductase inhibitors, or statins), and antihypertensive agents.2
The results of these trials have lead to changes in the initial management of patients following an new ischemic event, as well as the choice of medical therapy begun in the hospital and continued following discharge. Patients are given an individualized medical regimen based on specific needs that include in-hospital findings relating to the type of recent procedure, risk factors for subsequent ischemic events and drug tolerability. Such a regimen, although beyond the scope of this discussion, can be recalled as “ABCDE,” for Anti-platelet agents/ACE inhibitors, Beta-blockers, Blood pressure control, Cholesterol (lipid)-lowering agents, Cigarette cessation, Diet modification, Diabetes control, Exercise, and Education.
Important changes in long-term management
For most primary care physicians—with the possible exception of those in rural areas, who are faced with the burden of emergent care—the most important aspect of the revised guidelines is the changes in recommendations for long-term management of patients with unstable angina and NSTEMI. The goal of these new recommendations is to reduce the risk of subsequent cardiovascular events, such as death, recurrent MI, congestive heart failure, and stroke. Based on the results of the groundbreaking studies reviewed by the ACC/AHA panel, major changes to the original guidelines were necessary for the areas of long-term antiplatelet therapy and risk reduction.
TABLE
ACC/AHA task force classifications on patient evaluation and therapy
| Levels of evidence | ||
|---|---|---|
| A (highest) | B (intermediate) | C (lowest) |
| Data derived from multiple randomized clinical trials involving large numbers of patients. | Data derived from limited number of randomized clinical trials involving small numbers of patients or from analyses of nonrandomized trials or observation registries. | Basis of recommendation from expert opinion. large numbers of patients. |
| Recommendations made were based on expert analyses of published data. | ||
Antiplatelet therapy
Antiplatelet therapy—aspirin, GP IIb/IIIa antagonists, or an ADP-receptor antagonist (eg, clopidogrel)—is critical in the treatment and management of patients with unstable angina/NSTEMI.2 Based on the ACC/AHA Task Force classification (Table), aspirin (81–325 mg) should be initiated as quickly as possible after the condition is recognized, and continued indefinitely (SOR: A).
Clopidogrel (300-mg loading dose followed by 75 mg/d) should be administered to patients unable to take aspirin (SOR: A). In addition, clopidogrel 75 mg (once daily) should be added to aspirin therapy as quickly as possible and continued for up to 9 months in patients for whom an early noninterventional approach is planned (SOR: A), or for patients with a planned PCI who are not at high risk of bleeding (SOR: B).2
The CURE trial: clopidogrel and aspirin
The principal studies underlying the new recommendations for long-term antiplatelet therapy are the CURE trial6 and the PCI-CURE7 subset analysis. In the CURE trial, 12,562 patients who presented with unstable angina/NSTEMI within 24 hours following the onset of symptoms were randomized to receive clopidogrel (loading dose of 300 mg followed by 75 mg/d) with aspirin or placebo with aspirin for 3 to 12 months (mean follow-up, 9 months).
The relative risk (RR) of the primary composite outcome including incidence of cardiovascular death, nonfatal MI, or stroke was lower by 20% (RR=0.80; 95% confidence interval [CI], 0.72–0.90; P<.001) in the clopidogrel arm. Similarly, a composite outcome also including revascularization was lower by 14% (RR=0.86; P<.001) for those who received clopidogrel. Benefits were seen in all risk groups. A significant increase in bleeding events was observed in the group that received clopidogrel plus aspirin compared with aspirin alone (major bleeding, P=.001; minor bleeding, P<.001).6
CURE patients were followed for up to 1 year, with a mean follow-up period of 9 months. In addition to the early benefits seen, from day 31 up to 1 year there was a highly significant incremental reduction of 18% in the primary outcome (P<.001) with clopidogrel.7
The PCI-CURE subset: Percutaneous coronary interventions
In the PCI-CURE trial, a subset of patients recruited for CURE who underwent PCI was pretreated with aspirin 325 mg and clopidogrel 75 mg for a median of 10 days. These patients received either clopidogrel or ticlopidine for 4 weeks, and then were restarted on either clopidogrel 75 mg (80%) or placebo in addition to aspirin for an additional mean of 8 months with up to 1 year of follow-up.
Long-term administration of clopidogrel 75 mg following PCI resulted in a 30% reduction (RR=0.70; 95% CI, 0.50–0.70; P=.03) in cardiovascular death, MI, and any revascularization, with a 31% reduction in cardiovascular death or MI (P=.002) compared with placebo. Major bleeding rates were similar between groups (P=.64).9
The CREDO study
The new guidelines for long-term antiplatelet therapy are further supported by the subsequently published Clopidogrel for the Reduction of Events During Observation (CREDO) study.10 CREDO demonstrated a 26.9% relative risk reduction in the combined risk of death, MI, or stroke (95% CI, 3.9%–44.4%; P=.02) in patients with long-term (12 months) aspirin plus clopidogrel 75 mg therapy compared with aspirin plus placebo in 2116 patients undergoing elective PCI or deemed at high likelihood of undergoing PCI. There was no significant increase in the risk of major bleeding (P=.07) between the placebo and clopidogrel arms.
Risk reduction
The revised guidelines also included updated recommendations for risk reduction. It is now recommended that a fibrate or niacin be administered if the HDL cholesterol level is <40 mg/dL (SOR: B).2 Further, statins and a heart-healthy diet should be started during admission and continued after discharge for patients with LDL cholesterol >100 mg/dL (SOR: B).2
This recommendation is based in part on the MIRACL trial, in which 3086 acute coronary syndrome patients treated with atorvastatin, 24 to 96 hours after hospital admission, demonstrated a significant reduction in the composite rate of death, nonfatal MI, resuscitated cardiac arrest, or recurrent ischemia compared with those who received placebo (14.8% vs 17.4%) (RR=0.84; 95% CI, 0.70–1.00; P=.048). Patients were followed for up to 16 weeks after starting therapy. Abnormal liver transaminases (>3 times upper limit of normal) occurred more often in the atorvastatin group than the placebo group (2.5% vs 0.6%; P<.001).8
- Atorvastatin • Lipitor
- Clopidogrel • Plavix
- Ticlopidine • Ticlid
Correspondence
John S. Banas, MD, FACC, Morristown Memorial Hospital, 100 Madison Ave, Morristown, NJ 07960. E-mail: [email protected].
1. American Heart Association. Heart and Stroke Statistical Update. Available at: www.americanheart.org. Accessed on March 31, 2004.
2. Braunwald E, Antman EM, Beasley JW, et al. ACC/AHA guideline update for the management of patients with unstable angina and non-ST-segment elevation myocardial infarction—2002: summary article: report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. Circulation 2002;106:1893-1900.
3. Graves EJ, Kozak LJ. Detailed diagnoses and procedures, National Hospital Discharge Survey, 1996. National Center for Health Statistics. Vital Health Stat 1998;13:i-iii,1-151.
4. The Pursuit Trial Investigators. Inhibition of platelet glycoprotein IIb/IIIa with eptifibatide in patients with acute coronary syndromes. N Engl J Med 1998;339:436-443.
5. Braunwald E, Antman EM, Beasley JW, et al. ACC/AHA guidelines for the management of patients with unstable angina and non-ST-segment elevation myocardial infarction: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Committee on the Management of Patients With Unstable Angina). J Am Coll Cardiol 2000;36:970-1062.
6. Yusuf S, Zhao F, Mehta SR, Chrolavicius S, Tognoni G, Fox KK. Effects of clopidogrel in addition to aspirin in patients with acute coronary syndromes without ST-segment elevation. N Eng J Med 2001;345:494-502.
7. Mehta SR, Yusuf S. Short- and long-term oral antiplatelet therapy in acute coronary syndromes and percutaneous coronary interventions. J Am Coll Cardiol 2003;41:79S-88S.
8. Schwartz GG, Olsson AG, Ezekowitz MD, et al. Effects of atorvastatin on early recurrent ischemic events in acute coronary syndromes: the MIRACL study, a randomized controlled trial. JAMA 2001;285:1711-1718.
9. Mehta SR, Yusuf S, Peters RJ, et al. Effects of pretreatment with clopidogrel and aspirin followed by long-term therapy in patients undergoing percutaneous coronary intervention: the PCI-CURE study. Lancet 2001;358:527-533.
10. Steinhubl SR, Berger PB. Mann JT for the CREDO Investigators. Early and sustained dual oral antiplatelet therapy following percutaneous coronary intervention. A randomized controlled trial. JAMA 2002;288:2411-2420.
11. Antman EM, Braunwald E. Acute myocardial infarction. In: Braunwald E, ed. Heart Disease: A Textbook of Cardiovascular Medicine. Philadelphia, Pa: WB Saunders, 1997.
- Immediately upon presentation of non-ST-elevation myocardial infarction (NSTEMI), aspirin therapy (81–325 mg) should be initiated (A). If aspirin is contraindicated, clopidogrel (300-mg loading dose followed by 75 mg/d) should be administered (A).
- In patients for whom an early noninterventional approach is planned, or for patients not at high risk of bleeding for whom percutaneous coronary intervention (PCI) is planned, clopidogrel 75 mg (once daily) should be added to aspirin therapy as quickly as possible and continued for up to 9 months (B).
- Aggressive low-density lipoprotein (LDL) cholesterol-lowering therapy and general cardiovascular risk reduction are important in long-term management of these patients. Thus, a fibrate or niacin should be administered if the high-density lipoprotein (HDL) cholesterol is <40 mg/dL (B).
- In patients with LDL cholesterol >100 mg/dL, HMG-CoA reductase inhibitors (statins) and diet should be started during admission and continued after discharge (B).
In the long-term care of patients with acute coronary syndrome, recently published w that prognostic benefits improve with more aggressive antiplatelet therapy for those at high risk for recurrent events. Moreover, long-term care should include aggressive LDL cholesterol-lowering therapy and use of beta-blockers and angiotensin-converting enzyme (ACE) inhibitors, in addition to diet modification and exercise.
STEMI and NSTEMI: The new nomenclature
Coronary artery disease, the leading cause of death in the United States,1 can manifest in many ways involving a constellation of symptoms, electrocardiogram changes, and serum markers. These acute coronary syndromes result from decreased coronary blood flow and cause chest discomfort, usually at rest, with or without characteristic radiation, or such comparable anginal equivalents as weakness, dyspnea, and diaphoresis.
STEMI. An elevated ST-segment with elevated levels of such cardiac markers as creatine kinase myocardial band or troponin I or troponin T are consistent with a diagnosis of ST-elevation myocardial infarction (STEMI). The old term, acute myocardial infarction, was defined by the presence of pathological Q waves (Q wave MI).
NSTEMI. Patients with elevated serum levels of creatine kinase myocardial band or troponin I or troponin T, but no ST-segment elevation, are said to have non-ST-elevation myocardial infarction (NSTEMI).
Unstable angina. Normal levels of serum cardiac markers and an absence of ST-elevation are consistent with a diagnosis of unstable angina (Figure). Of patients with STEMI, most will ultimately experience a Q-wave MI; a minority will have a non–Q-wave MI. Of patients with NSTEMI, most will sustain a non–Q-wave MI, while a minority will sustain a Q-wave MI.
Unstable angina and NSTEMI are urgent and life-threatening problems. Chest pain and related symptoms account for 5.3 million visits to US emergency departments per year2 and account for 1.4 million hospitalizations annually.3 Approximately 15% of those presenting with unstable angina and NSTEMI go on to (re)infarct or die within 30 days.4
FIGURE
Unstable angina and NSTEMI
FIGURE
Nomenclature of acute coronary syndrome
ACC/AHA Guidelines
In 2000 the American College of Cardiology and the American Heart Association (ACC/AHA) Task Force on Practice Guidelines published their evidence-based recommendations for treatment of unstable angina/NSTEMI following an exhaustive review of the literature.
New trials in acute coronary syndromes
Since 2000, knowledge of acute coronary syndromes advanced considerably with results of large pivotal randomized controlled studies, which necessitated updating the ACC/AHA guidelines just 21 months after their completion. The most notable of these studies were the Clopidogrel in Unstable Angina to Prevent Recurrent Ischemic Events (CURE) trial,6 the Percutaneous Coronary Intervention (PCI)-CURE7 subset analysis, and the Myocardial Ischemia Reduction with Aggressive Cholesterol Lowering (MIRACL) trial.8
Although incorporation of antiplatelet therapy is the focus of this article, the ultimate objective of the new revised guidelines is improved clinical outcomes for patients with acute coronary syndromes by improving early risk assessment, using revascularization procedures aggressively when risk for future cardiac events is high, using short- and long-term antiplatelet and antithrombotic agents, and modifying long-term risk.
2002 revised guidelines
The studies reviewed in the 2002 revised guidelines assessed multiple therapies in the reduction of recurrent MI, stroke, and other cardiovascular events following patients’ presentation with unstable angina and NSTEMI. The studies also evaluated traditional therapies for acute coronary syndromes, such as unfractionated heparin, beta-blockers, and aspirin, as well as more recent therapies, including low-molecular-weight heparin, antiplatelet therapy (parenteral glycoprotein IIb/IIIa [GP IIb/IIIa] antagonists and ADP-receptor antagonists [thienopyridines]), lipid-lowering therapy (HMG-CoA reductase inhibitors, or statins), and antihypertensive agents.2
The results of these trials have lead to changes in the initial management of patients following an new ischemic event, as well as the choice of medical therapy begun in the hospital and continued following discharge. Patients are given an individualized medical regimen based on specific needs that include in-hospital findings relating to the type of recent procedure, risk factors for subsequent ischemic events and drug tolerability. Such a regimen, although beyond the scope of this discussion, can be recalled as “ABCDE,” for Anti-platelet agents/ACE inhibitors, Beta-blockers, Blood pressure control, Cholesterol (lipid)-lowering agents, Cigarette cessation, Diet modification, Diabetes control, Exercise, and Education.
Important changes in long-term management
For most primary care physicians—with the possible exception of those in rural areas, who are faced with the burden of emergent care—the most important aspect of the revised guidelines is the changes in recommendations for long-term management of patients with unstable angina and NSTEMI. The goal of these new recommendations is to reduce the risk of subsequent cardiovascular events, such as death, recurrent MI, congestive heart failure, and stroke. Based on the results of the groundbreaking studies reviewed by the ACC/AHA panel, major changes to the original guidelines were necessary for the areas of long-term antiplatelet therapy and risk reduction.
TABLE
ACC/AHA task force classifications on patient evaluation and therapy
| Levels of evidence | ||
|---|---|---|
| A (highest) | B (intermediate) | C (lowest) |
| Data derived from multiple randomized clinical trials involving large numbers of patients. | Data derived from limited number of randomized clinical trials involving small numbers of patients or from analyses of nonrandomized trials or observation registries. | Basis of recommendation from expert opinion. large numbers of patients. |
| Recommendations made were based on expert analyses of published data. | ||
Antiplatelet therapy
Antiplatelet therapy—aspirin, GP IIb/IIIa antagonists, or an ADP-receptor antagonist (eg, clopidogrel)—is critical in the treatment and management of patients with unstable angina/NSTEMI.2 Based on the ACC/AHA Task Force classification (Table), aspirin (81–325 mg) should be initiated as quickly as possible after the condition is recognized, and continued indefinitely (SOR: A).
Clopidogrel (300-mg loading dose followed by 75 mg/d) should be administered to patients unable to take aspirin (SOR: A). In addition, clopidogrel 75 mg (once daily) should be added to aspirin therapy as quickly as possible and continued for up to 9 months in patients for whom an early noninterventional approach is planned (SOR: A), or for patients with a planned PCI who are not at high risk of bleeding (SOR: B).2
The CURE trial: clopidogrel and aspirin
The principal studies underlying the new recommendations for long-term antiplatelet therapy are the CURE trial6 and the PCI-CURE7 subset analysis. In the CURE trial, 12,562 patients who presented with unstable angina/NSTEMI within 24 hours following the onset of symptoms were randomized to receive clopidogrel (loading dose of 300 mg followed by 75 mg/d) with aspirin or placebo with aspirin for 3 to 12 months (mean follow-up, 9 months).
The relative risk (RR) of the primary composite outcome including incidence of cardiovascular death, nonfatal MI, or stroke was lower by 20% (RR=0.80; 95% confidence interval [CI], 0.72–0.90; P<.001) in the clopidogrel arm. Similarly, a composite outcome also including revascularization was lower by 14% (RR=0.86; P<.001) for those who received clopidogrel. Benefits were seen in all risk groups. A significant increase in bleeding events was observed in the group that received clopidogrel plus aspirin compared with aspirin alone (major bleeding, P=.001; minor bleeding, P<.001).6
CURE patients were followed for up to 1 year, with a mean follow-up period of 9 months. In addition to the early benefits seen, from day 31 up to 1 year there was a highly significant incremental reduction of 18% in the primary outcome (P<.001) with clopidogrel.7
The PCI-CURE subset: Percutaneous coronary interventions
In the PCI-CURE trial, a subset of patients recruited for CURE who underwent PCI was pretreated with aspirin 325 mg and clopidogrel 75 mg for a median of 10 days. These patients received either clopidogrel or ticlopidine for 4 weeks, and then were restarted on either clopidogrel 75 mg (80%) or placebo in addition to aspirin for an additional mean of 8 months with up to 1 year of follow-up.
Long-term administration of clopidogrel 75 mg following PCI resulted in a 30% reduction (RR=0.70; 95% CI, 0.50–0.70; P=.03) in cardiovascular death, MI, and any revascularization, with a 31% reduction in cardiovascular death or MI (P=.002) compared with placebo. Major bleeding rates were similar between groups (P=.64).9
The CREDO study
The new guidelines for long-term antiplatelet therapy are further supported by the subsequently published Clopidogrel for the Reduction of Events During Observation (CREDO) study.10 CREDO demonstrated a 26.9% relative risk reduction in the combined risk of death, MI, or stroke (95% CI, 3.9%–44.4%; P=.02) in patients with long-term (12 months) aspirin plus clopidogrel 75 mg therapy compared with aspirin plus placebo in 2116 patients undergoing elective PCI or deemed at high likelihood of undergoing PCI. There was no significant increase in the risk of major bleeding (P=.07) between the placebo and clopidogrel arms.
Risk reduction
The revised guidelines also included updated recommendations for risk reduction. It is now recommended that a fibrate or niacin be administered if the HDL cholesterol level is <40 mg/dL (SOR: B).2 Further, statins and a heart-healthy diet should be started during admission and continued after discharge for patients with LDL cholesterol >100 mg/dL (SOR: B).2
This recommendation is based in part on the MIRACL trial, in which 3086 acute coronary syndrome patients treated with atorvastatin, 24 to 96 hours after hospital admission, demonstrated a significant reduction in the composite rate of death, nonfatal MI, resuscitated cardiac arrest, or recurrent ischemia compared with those who received placebo (14.8% vs 17.4%) (RR=0.84; 95% CI, 0.70–1.00; P=.048). Patients were followed for up to 16 weeks after starting therapy. Abnormal liver transaminases (>3 times upper limit of normal) occurred more often in the atorvastatin group than the placebo group (2.5% vs 0.6%; P<.001).8
- Atorvastatin • Lipitor
- Clopidogrel • Plavix
- Ticlopidine • Ticlid
Correspondence
John S. Banas, MD, FACC, Morristown Memorial Hospital, 100 Madison Ave, Morristown, NJ 07960. E-mail: [email protected].
- Immediately upon presentation of non-ST-elevation myocardial infarction (NSTEMI), aspirin therapy (81–325 mg) should be initiated (A). If aspirin is contraindicated, clopidogrel (300-mg loading dose followed by 75 mg/d) should be administered (A).
- In patients for whom an early noninterventional approach is planned, or for patients not at high risk of bleeding for whom percutaneous coronary intervention (PCI) is planned, clopidogrel 75 mg (once daily) should be added to aspirin therapy as quickly as possible and continued for up to 9 months (B).
- Aggressive low-density lipoprotein (LDL) cholesterol-lowering therapy and general cardiovascular risk reduction are important in long-term management of these patients. Thus, a fibrate or niacin should be administered if the high-density lipoprotein (HDL) cholesterol is <40 mg/dL (B).
- In patients with LDL cholesterol >100 mg/dL, HMG-CoA reductase inhibitors (statins) and diet should be started during admission and continued after discharge (B).
In the long-term care of patients with acute coronary syndrome, recently published w that prognostic benefits improve with more aggressive antiplatelet therapy for those at high risk for recurrent events. Moreover, long-term care should include aggressive LDL cholesterol-lowering therapy and use of beta-blockers and angiotensin-converting enzyme (ACE) inhibitors, in addition to diet modification and exercise.
STEMI and NSTEMI: The new nomenclature
Coronary artery disease, the leading cause of death in the United States,1 can manifest in many ways involving a constellation of symptoms, electrocardiogram changes, and serum markers. These acute coronary syndromes result from decreased coronary blood flow and cause chest discomfort, usually at rest, with or without characteristic radiation, or such comparable anginal equivalents as weakness, dyspnea, and diaphoresis.
STEMI. An elevated ST-segment with elevated levels of such cardiac markers as creatine kinase myocardial band or troponin I or troponin T are consistent with a diagnosis of ST-elevation myocardial infarction (STEMI). The old term, acute myocardial infarction, was defined by the presence of pathological Q waves (Q wave MI).
NSTEMI. Patients with elevated serum levels of creatine kinase myocardial band or troponin I or troponin T, but no ST-segment elevation, are said to have non-ST-elevation myocardial infarction (NSTEMI).
Unstable angina. Normal levels of serum cardiac markers and an absence of ST-elevation are consistent with a diagnosis of unstable angina (Figure). Of patients with STEMI, most will ultimately experience a Q-wave MI; a minority will have a non–Q-wave MI. Of patients with NSTEMI, most will sustain a non–Q-wave MI, while a minority will sustain a Q-wave MI.
Unstable angina and NSTEMI are urgent and life-threatening problems. Chest pain and related symptoms account for 5.3 million visits to US emergency departments per year2 and account for 1.4 million hospitalizations annually.3 Approximately 15% of those presenting with unstable angina and NSTEMI go on to (re)infarct or die within 30 days.4
FIGURE
Unstable angina and NSTEMI
FIGURE
Nomenclature of acute coronary syndrome
ACC/AHA Guidelines
In 2000 the American College of Cardiology and the American Heart Association (ACC/AHA) Task Force on Practice Guidelines published their evidence-based recommendations for treatment of unstable angina/NSTEMI following an exhaustive review of the literature.
New trials in acute coronary syndromes
Since 2000, knowledge of acute coronary syndromes advanced considerably with results of large pivotal randomized controlled studies, which necessitated updating the ACC/AHA guidelines just 21 months after their completion. The most notable of these studies were the Clopidogrel in Unstable Angina to Prevent Recurrent Ischemic Events (CURE) trial,6 the Percutaneous Coronary Intervention (PCI)-CURE7 subset analysis, and the Myocardial Ischemia Reduction with Aggressive Cholesterol Lowering (MIRACL) trial.8
Although incorporation of antiplatelet therapy is the focus of this article, the ultimate objective of the new revised guidelines is improved clinical outcomes for patients with acute coronary syndromes by improving early risk assessment, using revascularization procedures aggressively when risk for future cardiac events is high, using short- and long-term antiplatelet and antithrombotic agents, and modifying long-term risk.
2002 revised guidelines
The studies reviewed in the 2002 revised guidelines assessed multiple therapies in the reduction of recurrent MI, stroke, and other cardiovascular events following patients’ presentation with unstable angina and NSTEMI. The studies also evaluated traditional therapies for acute coronary syndromes, such as unfractionated heparin, beta-blockers, and aspirin, as well as more recent therapies, including low-molecular-weight heparin, antiplatelet therapy (parenteral glycoprotein IIb/IIIa [GP IIb/IIIa] antagonists and ADP-receptor antagonists [thienopyridines]), lipid-lowering therapy (HMG-CoA reductase inhibitors, or statins), and antihypertensive agents.2
The results of these trials have lead to changes in the initial management of patients following an new ischemic event, as well as the choice of medical therapy begun in the hospital and continued following discharge. Patients are given an individualized medical regimen based on specific needs that include in-hospital findings relating to the type of recent procedure, risk factors for subsequent ischemic events and drug tolerability. Such a regimen, although beyond the scope of this discussion, can be recalled as “ABCDE,” for Anti-platelet agents/ACE inhibitors, Beta-blockers, Blood pressure control, Cholesterol (lipid)-lowering agents, Cigarette cessation, Diet modification, Diabetes control, Exercise, and Education.
Important changes in long-term management
For most primary care physicians—with the possible exception of those in rural areas, who are faced with the burden of emergent care—the most important aspect of the revised guidelines is the changes in recommendations for long-term management of patients with unstable angina and NSTEMI. The goal of these new recommendations is to reduce the risk of subsequent cardiovascular events, such as death, recurrent MI, congestive heart failure, and stroke. Based on the results of the groundbreaking studies reviewed by the ACC/AHA panel, major changes to the original guidelines were necessary for the areas of long-term antiplatelet therapy and risk reduction.
TABLE
ACC/AHA task force classifications on patient evaluation and therapy
| Levels of evidence | ||
|---|---|---|
| A (highest) | B (intermediate) | C (lowest) |
| Data derived from multiple randomized clinical trials involving large numbers of patients. | Data derived from limited number of randomized clinical trials involving small numbers of patients or from analyses of nonrandomized trials or observation registries. | Basis of recommendation from expert opinion. large numbers of patients. |
| Recommendations made were based on expert analyses of published data. | ||
Antiplatelet therapy
Antiplatelet therapy—aspirin, GP IIb/IIIa antagonists, or an ADP-receptor antagonist (eg, clopidogrel)—is critical in the treatment and management of patients with unstable angina/NSTEMI.2 Based on the ACC/AHA Task Force classification (Table), aspirin (81–325 mg) should be initiated as quickly as possible after the condition is recognized, and continued indefinitely (SOR: A).
Clopidogrel (300-mg loading dose followed by 75 mg/d) should be administered to patients unable to take aspirin (SOR: A). In addition, clopidogrel 75 mg (once daily) should be added to aspirin therapy as quickly as possible and continued for up to 9 months in patients for whom an early noninterventional approach is planned (SOR: A), or for patients with a planned PCI who are not at high risk of bleeding (SOR: B).2
The CURE trial: clopidogrel and aspirin
The principal studies underlying the new recommendations for long-term antiplatelet therapy are the CURE trial6 and the PCI-CURE7 subset analysis. In the CURE trial, 12,562 patients who presented with unstable angina/NSTEMI within 24 hours following the onset of symptoms were randomized to receive clopidogrel (loading dose of 300 mg followed by 75 mg/d) with aspirin or placebo with aspirin for 3 to 12 months (mean follow-up, 9 months).
The relative risk (RR) of the primary composite outcome including incidence of cardiovascular death, nonfatal MI, or stroke was lower by 20% (RR=0.80; 95% confidence interval [CI], 0.72–0.90; P<.001) in the clopidogrel arm. Similarly, a composite outcome also including revascularization was lower by 14% (RR=0.86; P<.001) for those who received clopidogrel. Benefits were seen in all risk groups. A significant increase in bleeding events was observed in the group that received clopidogrel plus aspirin compared with aspirin alone (major bleeding, P=.001; minor bleeding, P<.001).6
CURE patients were followed for up to 1 year, with a mean follow-up period of 9 months. In addition to the early benefits seen, from day 31 up to 1 year there was a highly significant incremental reduction of 18% in the primary outcome (P<.001) with clopidogrel.7
The PCI-CURE subset: Percutaneous coronary interventions
In the PCI-CURE trial, a subset of patients recruited for CURE who underwent PCI was pretreated with aspirin 325 mg and clopidogrel 75 mg for a median of 10 days. These patients received either clopidogrel or ticlopidine for 4 weeks, and then were restarted on either clopidogrel 75 mg (80%) or placebo in addition to aspirin for an additional mean of 8 months with up to 1 year of follow-up.
Long-term administration of clopidogrel 75 mg following PCI resulted in a 30% reduction (RR=0.70; 95% CI, 0.50–0.70; P=.03) in cardiovascular death, MI, and any revascularization, with a 31% reduction in cardiovascular death or MI (P=.002) compared with placebo. Major bleeding rates were similar between groups (P=.64).9
The CREDO study
The new guidelines for long-term antiplatelet therapy are further supported by the subsequently published Clopidogrel for the Reduction of Events During Observation (CREDO) study.10 CREDO demonstrated a 26.9% relative risk reduction in the combined risk of death, MI, or stroke (95% CI, 3.9%–44.4%; P=.02) in patients with long-term (12 months) aspirin plus clopidogrel 75 mg therapy compared with aspirin plus placebo in 2116 patients undergoing elective PCI or deemed at high likelihood of undergoing PCI. There was no significant increase in the risk of major bleeding (P=.07) between the placebo and clopidogrel arms.
Risk reduction
The revised guidelines also included updated recommendations for risk reduction. It is now recommended that a fibrate or niacin be administered if the HDL cholesterol level is <40 mg/dL (SOR: B).2 Further, statins and a heart-healthy diet should be started during admission and continued after discharge for patients with LDL cholesterol >100 mg/dL (SOR: B).2
This recommendation is based in part on the MIRACL trial, in which 3086 acute coronary syndrome patients treated with atorvastatin, 24 to 96 hours after hospital admission, demonstrated a significant reduction in the composite rate of death, nonfatal MI, resuscitated cardiac arrest, or recurrent ischemia compared with those who received placebo (14.8% vs 17.4%) (RR=0.84; 95% CI, 0.70–1.00; P=.048). Patients were followed for up to 16 weeks after starting therapy. Abnormal liver transaminases (>3 times upper limit of normal) occurred more often in the atorvastatin group than the placebo group (2.5% vs 0.6%; P<.001).8
- Atorvastatin • Lipitor
- Clopidogrel • Plavix
- Ticlopidine • Ticlid
Correspondence
John S. Banas, MD, FACC, Morristown Memorial Hospital, 100 Madison Ave, Morristown, NJ 07960. E-mail: [email protected].
1. American Heart Association. Heart and Stroke Statistical Update. Available at: www.americanheart.org. Accessed on March 31, 2004.
2. Braunwald E, Antman EM, Beasley JW, et al. ACC/AHA guideline update for the management of patients with unstable angina and non-ST-segment elevation myocardial infarction—2002: summary article: report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. Circulation 2002;106:1893-1900.
3. Graves EJ, Kozak LJ. Detailed diagnoses and procedures, National Hospital Discharge Survey, 1996. National Center for Health Statistics. Vital Health Stat 1998;13:i-iii,1-151.
4. The Pursuit Trial Investigators. Inhibition of platelet glycoprotein IIb/IIIa with eptifibatide in patients with acute coronary syndromes. N Engl J Med 1998;339:436-443.
5. Braunwald E, Antman EM, Beasley JW, et al. ACC/AHA guidelines for the management of patients with unstable angina and non-ST-segment elevation myocardial infarction: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Committee on the Management of Patients With Unstable Angina). J Am Coll Cardiol 2000;36:970-1062.
6. Yusuf S, Zhao F, Mehta SR, Chrolavicius S, Tognoni G, Fox KK. Effects of clopidogrel in addition to aspirin in patients with acute coronary syndromes without ST-segment elevation. N Eng J Med 2001;345:494-502.
7. Mehta SR, Yusuf S. Short- and long-term oral antiplatelet therapy in acute coronary syndromes and percutaneous coronary interventions. J Am Coll Cardiol 2003;41:79S-88S.
8. Schwartz GG, Olsson AG, Ezekowitz MD, et al. Effects of atorvastatin on early recurrent ischemic events in acute coronary syndromes: the MIRACL study, a randomized controlled trial. JAMA 2001;285:1711-1718.
9. Mehta SR, Yusuf S, Peters RJ, et al. Effects of pretreatment with clopidogrel and aspirin followed by long-term therapy in patients undergoing percutaneous coronary intervention: the PCI-CURE study. Lancet 2001;358:527-533.
10. Steinhubl SR, Berger PB. Mann JT for the CREDO Investigators. Early and sustained dual oral antiplatelet therapy following percutaneous coronary intervention. A randomized controlled trial. JAMA 2002;288:2411-2420.
11. Antman EM, Braunwald E. Acute myocardial infarction. In: Braunwald E, ed. Heart Disease: A Textbook of Cardiovascular Medicine. Philadelphia, Pa: WB Saunders, 1997.
1. American Heart Association. Heart and Stroke Statistical Update. Available at: www.americanheart.org. Accessed on March 31, 2004.
2. Braunwald E, Antman EM, Beasley JW, et al. ACC/AHA guideline update for the management of patients with unstable angina and non-ST-segment elevation myocardial infarction—2002: summary article: report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. Circulation 2002;106:1893-1900.
3. Graves EJ, Kozak LJ. Detailed diagnoses and procedures, National Hospital Discharge Survey, 1996. National Center for Health Statistics. Vital Health Stat 1998;13:i-iii,1-151.
4. The Pursuit Trial Investigators. Inhibition of platelet glycoprotein IIb/IIIa with eptifibatide in patients with acute coronary syndromes. N Engl J Med 1998;339:436-443.
5. Braunwald E, Antman EM, Beasley JW, et al. ACC/AHA guidelines for the management of patients with unstable angina and non-ST-segment elevation myocardial infarction: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Committee on the Management of Patients With Unstable Angina). J Am Coll Cardiol 2000;36:970-1062.
6. Yusuf S, Zhao F, Mehta SR, Chrolavicius S, Tognoni G, Fox KK. Effects of clopidogrel in addition to aspirin in patients with acute coronary syndromes without ST-segment elevation. N Eng J Med 2001;345:494-502.
7. Mehta SR, Yusuf S. Short- and long-term oral antiplatelet therapy in acute coronary syndromes and percutaneous coronary interventions. J Am Coll Cardiol 2003;41:79S-88S.
8. Schwartz GG, Olsson AG, Ezekowitz MD, et al. Effects of atorvastatin on early recurrent ischemic events in acute coronary syndromes: the MIRACL study, a randomized controlled trial. JAMA 2001;285:1711-1718.
9. Mehta SR, Yusuf S, Peters RJ, et al. Effects of pretreatment with clopidogrel and aspirin followed by long-term therapy in patients undergoing percutaneous coronary intervention: the PCI-CURE study. Lancet 2001;358:527-533.
10. Steinhubl SR, Berger PB. Mann JT for the CREDO Investigators. Early and sustained dual oral antiplatelet therapy following percutaneous coronary intervention. A randomized controlled trial. JAMA 2002;288:2411-2420.
11. Antman EM, Braunwald E. Acute myocardial infarction. In: Braunwald E, ed. Heart Disease: A Textbook of Cardiovascular Medicine. Philadelphia, Pa: WB Saunders, 1997.