User login
Academic Hospitalist Groups Lag Behind in Admissions, Discharges
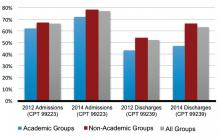
In 2012, SHM reported increasing numbers of hospital encounters coded for high-level evaluation and management services, as reported by the 2012 State of Hospital Medicine (SOHM) survey respondents. The 2014 SOHM report shows a solid continuation of this trend, with high-level CPT codes predominating in admission and discharge services by wider margins than ever before.
The 2014 report provides CPT code data from 173 hospitalist groups, who reported the number of inpatient admissions with CPT codes corresponding to Level 1, Level 2, or Level 3. Inpatient discharges have codes corresponding to either Level 1 or Level 2.
Compared to 2012, Level 3 admissions (CPT 99223) increased by 14% in 2014 and now account for 77% of all admissions (see Figure 1). Level 2 discharges (CPT 99239) have increased by 17% since 2012 and now account for 63% of discharges.
In 2014, SOHM added CPT code distribution data for observation care. Observation admissions and inpatient and observation subsequent care are also reported as Level 1, 2, or 3 by the corresponding CPT codes. Observation discharges, which have only one code level, are also reported, in addition to the three levels of same-day admit/discharge encounters.
The rate of Level 3 CPT codes reported for observation admissions, which was 72%, roughly approximated that of inpatient admissions. For subsequent care, Level 2 accounts for the majority of both observation and inpatient codes.
Despite the general predominance of Level 3 admissions and now Level 2 inpatient discharges, not all hospitalist groups deal equally in these higher billing evaluation and management services. Groups in the West region previously dominated the high-level encounters in both admissions and discharges; in 2014, the South took the lead in high-level admissions.

One factor that has consistently signaled lower rates of high-level coding, however, is academic status. A likely reason, as alluded to in a previous “Survey Insights” column, relates to the fact that residents’ time is not billable. This is particularly important in the discharge coding, in which the higher Level 2 code is strictly based on the statement by an attending that discharge services were personally provided for more than 30 minutes. Understandably, this happens less often when a resident’s education includes providing discharge services.
If attending face-to-face time is a major factor in the discharge coding differential, it does not explain where academic groups are missing the boat on the admission side, where residents’ documentation is incorporated by attendings—and can have a substantial effect on accurate billing. This assumes that academic groups are not treating far fewer sick patients, less comprehensively, across the board.
In my own public academic hospital, I see reviewing the required elements of the history and physical examination (H&P) as survival for our hospital and our mission, as well as an opportunity to educate residents simultaneously in patient interviewing skills and system-based practice.
But before I get too far into waxing altruistic, let me recognize another factor suggested by the SOHM report: I am not 100% salaried. That means thorough documentation and accurate coding directly impact my personal compensation.
The 2014 SOHM report shows, as it did in 2012, an inverse correlation between high-level admissions and percent salaried compensation. Although this relationship remains less clear in follow-ups and discharges, perhaps hospitalists pay more attention to coding criteria when it’s bread on the table…and if time permits.
Dr. Creamer is medical director of the short-stay unit at MetroHealth Medical Center in Cleveland and a member of SHM’s Practice Analysis Committee.
In 2012, SHM reported increasing numbers of hospital encounters coded for high-level evaluation and management services, as reported by the 2012 State of Hospital Medicine (SOHM) survey respondents. The 2014 SOHM report shows a solid continuation of this trend, with high-level CPT codes predominating in admission and discharge services by wider margins than ever before.
The 2014 report provides CPT code data from 173 hospitalist groups, who reported the number of inpatient admissions with CPT codes corresponding to Level 1, Level 2, or Level 3. Inpatient discharges have codes corresponding to either Level 1 or Level 2.
Compared to 2012, Level 3 admissions (CPT 99223) increased by 14% in 2014 and now account for 77% of all admissions (see Figure 1). Level 2 discharges (CPT 99239) have increased by 17% since 2012 and now account for 63% of discharges.
In 2014, SOHM added CPT code distribution data for observation care. Observation admissions and inpatient and observation subsequent care are also reported as Level 1, 2, or 3 by the corresponding CPT codes. Observation discharges, which have only one code level, are also reported, in addition to the three levels of same-day admit/discharge encounters.
The rate of Level 3 CPT codes reported for observation admissions, which was 72%, roughly approximated that of inpatient admissions. For subsequent care, Level 2 accounts for the majority of both observation and inpatient codes.
Despite the general predominance of Level 3 admissions and now Level 2 inpatient discharges, not all hospitalist groups deal equally in these higher billing evaluation and management services. Groups in the West region previously dominated the high-level encounters in both admissions and discharges; in 2014, the South took the lead in high-level admissions.

One factor that has consistently signaled lower rates of high-level coding, however, is academic status. A likely reason, as alluded to in a previous “Survey Insights” column, relates to the fact that residents’ time is not billable. This is particularly important in the discharge coding, in which the higher Level 2 code is strictly based on the statement by an attending that discharge services were personally provided for more than 30 minutes. Understandably, this happens less often when a resident’s education includes providing discharge services.
If attending face-to-face time is a major factor in the discharge coding differential, it does not explain where academic groups are missing the boat on the admission side, where residents’ documentation is incorporated by attendings—and can have a substantial effect on accurate billing. This assumes that academic groups are not treating far fewer sick patients, less comprehensively, across the board.
In my own public academic hospital, I see reviewing the required elements of the history and physical examination (H&P) as survival for our hospital and our mission, as well as an opportunity to educate residents simultaneously in patient interviewing skills and system-based practice.
But before I get too far into waxing altruistic, let me recognize another factor suggested by the SOHM report: I am not 100% salaried. That means thorough documentation and accurate coding directly impact my personal compensation.
The 2014 SOHM report shows, as it did in 2012, an inverse correlation between high-level admissions and percent salaried compensation. Although this relationship remains less clear in follow-ups and discharges, perhaps hospitalists pay more attention to coding criteria when it’s bread on the table…and if time permits.
Dr. Creamer is medical director of the short-stay unit at MetroHealth Medical Center in Cleveland and a member of SHM’s Practice Analysis Committee.
In 2012, SHM reported increasing numbers of hospital encounters coded for high-level evaluation and management services, as reported by the 2012 State of Hospital Medicine (SOHM) survey respondents. The 2014 SOHM report shows a solid continuation of this trend, with high-level CPT codes predominating in admission and discharge services by wider margins than ever before.
The 2014 report provides CPT code data from 173 hospitalist groups, who reported the number of inpatient admissions with CPT codes corresponding to Level 1, Level 2, or Level 3. Inpatient discharges have codes corresponding to either Level 1 or Level 2.
Compared to 2012, Level 3 admissions (CPT 99223) increased by 14% in 2014 and now account for 77% of all admissions (see Figure 1). Level 2 discharges (CPT 99239) have increased by 17% since 2012 and now account for 63% of discharges.
In 2014, SOHM added CPT code distribution data for observation care. Observation admissions and inpatient and observation subsequent care are also reported as Level 1, 2, or 3 by the corresponding CPT codes. Observation discharges, which have only one code level, are also reported, in addition to the three levels of same-day admit/discharge encounters.
The rate of Level 3 CPT codes reported for observation admissions, which was 72%, roughly approximated that of inpatient admissions. For subsequent care, Level 2 accounts for the majority of both observation and inpatient codes.
Despite the general predominance of Level 3 admissions and now Level 2 inpatient discharges, not all hospitalist groups deal equally in these higher billing evaluation and management services. Groups in the West region previously dominated the high-level encounters in both admissions and discharges; in 2014, the South took the lead in high-level admissions.

One factor that has consistently signaled lower rates of high-level coding, however, is academic status. A likely reason, as alluded to in a previous “Survey Insights” column, relates to the fact that residents’ time is not billable. This is particularly important in the discharge coding, in which the higher Level 2 code is strictly based on the statement by an attending that discharge services were personally provided for more than 30 minutes. Understandably, this happens less often when a resident’s education includes providing discharge services.
If attending face-to-face time is a major factor in the discharge coding differential, it does not explain where academic groups are missing the boat on the admission side, where residents’ documentation is incorporated by attendings—and can have a substantial effect on accurate billing. This assumes that academic groups are not treating far fewer sick patients, less comprehensively, across the board.
In my own public academic hospital, I see reviewing the required elements of the history and physical examination (H&P) as survival for our hospital and our mission, as well as an opportunity to educate residents simultaneously in patient interviewing skills and system-based practice.
But before I get too far into waxing altruistic, let me recognize another factor suggested by the SOHM report: I am not 100% salaried. That means thorough documentation and accurate coding directly impact my personal compensation.
The 2014 SOHM report shows, as it did in 2012, an inverse correlation between high-level admissions and percent salaried compensation. Although this relationship remains less clear in follow-ups and discharges, perhaps hospitalists pay more attention to coding criteria when it’s bread on the table…and if time permits.
Dr. Creamer is medical director of the short-stay unit at MetroHealth Medical Center in Cleveland and a member of SHM’s Practice Analysis Committee.
SHM Tallies Ratio of Hospital Respondents' Observation Admissions to Inpatient Admission Encounters
SHM added a new item to its 2012 State of Hospital Medicine report: the ratio of respondents’ observation admissions to inpatient admission encounters. This metric was added because observation encounters have been increasing, with financial effects on hospitals and patients. SHM survey respondents reported a 20% observation rate for both adult and pediatric practice groups (see Figure 1).
Under observation status, services that used to be billed as inpatient status (e.g. chest pain evaluation, treatment of asthma exacerbation) must be billed by the hospital at much lower outpatient rates. Some hospitals have responded to this financial pressure by creating observation units or making other operational adjustments. One recent analysis suggested that nationwide adoption of such efforts could save billions of dollars.1
Becoming lean enough to do short work in short time, though, does not address all of the observation-related issues facing hospitals. When the Centers for Medicare & Medicaid Services’ (CMS) Recovery Audit Contractors (RACs) determine retrospectively that an inpatient admission should have been an observation encounter, the hospital’s payment is not downgraded but forfeited.2 This development has prompted hospitals to preemptively opt for observation status for certain patients. Case managers and providers increasingly are spending time reviewing inpatient versus observation status throughout a patient’s stay. Many hospitals have turned to third-party contractors to help review observation status.
Observation status has financial implications for patients as well. In the past year, USA Today, The Wall Street Journal, and CNN Money all have reported on patients hit with unexpected out-of-pocket expenses related to observation care.3,4,5 A common theme: Medicare patient hospitalized with an acute fracture, managed nonoperatively but requiring rehabilitation prior to returning home. These patients found out too late that observation, a status they were often unaware of, did not qualify for CMS’ three-day inpatient requirement to cover rehabilitation costs. Some patients were charged exorbitant prices for noncovered “outpatient” services, such as providing their routine medications.
Advocacy groups have joined the fray on patients’ behalf, and legal challenges have ensued. AARP and others are educating patients about observation status—and their right to challenge it. The Center for Medicare Advocacy (www.kslaw.com/Library/publication/HH111411_Bagnall.pdf) has filed a lawsuit against the U.S. Department of Health and Human Services on behalf of patients hit with uncovered rehabilitation costs, and the American Hospital Association has teamed with several hospitals to sue over funds forfeited in RAC audits (www.aha.org/content/12/121101-aha-hhs-medicare-com.pdf). Both houses of Congress have legislation (H.R. 1543 and S. 818) seeking to count observation days toward the Medicare three-day rule. For its part, CMS has promised to review observation status and, hopefully, clarify the rules.
Hospitalists, meanwhile, are gearing up for more observation care. The 2012 State of Hospital Medicine report shows that 37% of adult groups and 28% of pediatric groups reported having primary responsibility for observation or short-stay units. My own hospital runs both a clinical decision unit in the ED and a short-stay unit staffed by our hospitalist group. As SHM tracks observation status in future surveys, HM groups will be able to follow this phenomenon among their colleagues and benchmark their own rates of observation encounters.
Dr. Creamer is medical director of the short-stay unit at MetroHealth Medical Center in Cleveland and a member of SHM’s Practice Analysis Committee.
References
- Feng Z, Wright DB, Mor V. Sharp rise in Medicare enrollees being held in hospitals for observation raises concerns about causes and consequences. Health Aff (Millwood). 2012;31(6):1251-1259.
- Baugh CW, Venkatesh AK, Hilton JA, Samuel PA, Schuur JD, Bohan JS. Making greater use of dedicated hospital observation units for many short-stay patients could save $3.1 billion a year. Health Aff (Millwood). 2012;31(10):2314-2323.
- Gengler A. The painful new trend in Medicare. CNN Money website. Available at: http://money.cnn.com/2012/08/07/pf/medicare-rehab-costs.moneymag/index.htm. Accessed March 6, 2013.
- Jaffe S. Patients held for observation can face steep drug bills. USA Today website. Available at: http://usatoday30.usatoday.com/money/industries/health/drugs/story/2012-04-30/drugs-can-be-expensive-in-observation-care/54646378/1. Accessed March 6, 2013.
- Landro L. Filling a gap between ERs and inpatient rooms. The Wall Street Journal website. Available at: http://online.wsj.com/article/SB10001424052970204349404578101060863887052.html. Accessed March 6, 2013.
SHM added a new item to its 2012 State of Hospital Medicine report: the ratio of respondents’ observation admissions to inpatient admission encounters. This metric was added because observation encounters have been increasing, with financial effects on hospitals and patients. SHM survey respondents reported a 20% observation rate for both adult and pediatric practice groups (see Figure 1).
Under observation status, services that used to be billed as inpatient status (e.g. chest pain evaluation, treatment of asthma exacerbation) must be billed by the hospital at much lower outpatient rates. Some hospitals have responded to this financial pressure by creating observation units or making other operational adjustments. One recent analysis suggested that nationwide adoption of such efforts could save billions of dollars.1
Becoming lean enough to do short work in short time, though, does not address all of the observation-related issues facing hospitals. When the Centers for Medicare & Medicaid Services’ (CMS) Recovery Audit Contractors (RACs) determine retrospectively that an inpatient admission should have been an observation encounter, the hospital’s payment is not downgraded but forfeited.2 This development has prompted hospitals to preemptively opt for observation status for certain patients. Case managers and providers increasingly are spending time reviewing inpatient versus observation status throughout a patient’s stay. Many hospitals have turned to third-party contractors to help review observation status.
Observation status has financial implications for patients as well. In the past year, USA Today, The Wall Street Journal, and CNN Money all have reported on patients hit with unexpected out-of-pocket expenses related to observation care.3,4,5 A common theme: Medicare patient hospitalized with an acute fracture, managed nonoperatively but requiring rehabilitation prior to returning home. These patients found out too late that observation, a status they were often unaware of, did not qualify for CMS’ three-day inpatient requirement to cover rehabilitation costs. Some patients were charged exorbitant prices for noncovered “outpatient” services, such as providing their routine medications.
Advocacy groups have joined the fray on patients’ behalf, and legal challenges have ensued. AARP and others are educating patients about observation status—and their right to challenge it. The Center for Medicare Advocacy (www.kslaw.com/Library/publication/HH111411_Bagnall.pdf) has filed a lawsuit against the U.S. Department of Health and Human Services on behalf of patients hit with uncovered rehabilitation costs, and the American Hospital Association has teamed with several hospitals to sue over funds forfeited in RAC audits (www.aha.org/content/12/121101-aha-hhs-medicare-com.pdf). Both houses of Congress have legislation (H.R. 1543 and S. 818) seeking to count observation days toward the Medicare three-day rule. For its part, CMS has promised to review observation status and, hopefully, clarify the rules.
Hospitalists, meanwhile, are gearing up for more observation care. The 2012 State of Hospital Medicine report shows that 37% of adult groups and 28% of pediatric groups reported having primary responsibility for observation or short-stay units. My own hospital runs both a clinical decision unit in the ED and a short-stay unit staffed by our hospitalist group. As SHM tracks observation status in future surveys, HM groups will be able to follow this phenomenon among their colleagues and benchmark their own rates of observation encounters.
Dr. Creamer is medical director of the short-stay unit at MetroHealth Medical Center in Cleveland and a member of SHM’s Practice Analysis Committee.
References
- Feng Z, Wright DB, Mor V. Sharp rise in Medicare enrollees being held in hospitals for observation raises concerns about causes and consequences. Health Aff (Millwood). 2012;31(6):1251-1259.
- Baugh CW, Venkatesh AK, Hilton JA, Samuel PA, Schuur JD, Bohan JS. Making greater use of dedicated hospital observation units for many short-stay patients could save $3.1 billion a year. Health Aff (Millwood). 2012;31(10):2314-2323.
- Gengler A. The painful new trend in Medicare. CNN Money website. Available at: http://money.cnn.com/2012/08/07/pf/medicare-rehab-costs.moneymag/index.htm. Accessed March 6, 2013.
- Jaffe S. Patients held for observation can face steep drug bills. USA Today website. Available at: http://usatoday30.usatoday.com/money/industries/health/drugs/story/2012-04-30/drugs-can-be-expensive-in-observation-care/54646378/1. Accessed March 6, 2013.
- Landro L. Filling a gap between ERs and inpatient rooms. The Wall Street Journal website. Available at: http://online.wsj.com/article/SB10001424052970204349404578101060863887052.html. Accessed March 6, 2013.
SHM added a new item to its 2012 State of Hospital Medicine report: the ratio of respondents’ observation admissions to inpatient admission encounters. This metric was added because observation encounters have been increasing, with financial effects on hospitals and patients. SHM survey respondents reported a 20% observation rate for both adult and pediatric practice groups (see Figure 1).
Under observation status, services that used to be billed as inpatient status (e.g. chest pain evaluation, treatment of asthma exacerbation) must be billed by the hospital at much lower outpatient rates. Some hospitals have responded to this financial pressure by creating observation units or making other operational adjustments. One recent analysis suggested that nationwide adoption of such efforts could save billions of dollars.1
Becoming lean enough to do short work in short time, though, does not address all of the observation-related issues facing hospitals. When the Centers for Medicare & Medicaid Services’ (CMS) Recovery Audit Contractors (RACs) determine retrospectively that an inpatient admission should have been an observation encounter, the hospital’s payment is not downgraded but forfeited.2 This development has prompted hospitals to preemptively opt for observation status for certain patients. Case managers and providers increasingly are spending time reviewing inpatient versus observation status throughout a patient’s stay. Many hospitals have turned to third-party contractors to help review observation status.
Observation status has financial implications for patients as well. In the past year, USA Today, The Wall Street Journal, and CNN Money all have reported on patients hit with unexpected out-of-pocket expenses related to observation care.3,4,5 A common theme: Medicare patient hospitalized with an acute fracture, managed nonoperatively but requiring rehabilitation prior to returning home. These patients found out too late that observation, a status they were often unaware of, did not qualify for CMS’ three-day inpatient requirement to cover rehabilitation costs. Some patients were charged exorbitant prices for noncovered “outpatient” services, such as providing their routine medications.
Advocacy groups have joined the fray on patients’ behalf, and legal challenges have ensued. AARP and others are educating patients about observation status—and their right to challenge it. The Center for Medicare Advocacy (www.kslaw.com/Library/publication/HH111411_Bagnall.pdf) has filed a lawsuit against the U.S. Department of Health and Human Services on behalf of patients hit with uncovered rehabilitation costs, and the American Hospital Association has teamed with several hospitals to sue over funds forfeited in RAC audits (www.aha.org/content/12/121101-aha-hhs-medicare-com.pdf). Both houses of Congress have legislation (H.R. 1543 and S. 818) seeking to count observation days toward the Medicare three-day rule. For its part, CMS has promised to review observation status and, hopefully, clarify the rules.
Hospitalists, meanwhile, are gearing up for more observation care. The 2012 State of Hospital Medicine report shows that 37% of adult groups and 28% of pediatric groups reported having primary responsibility for observation or short-stay units. My own hospital runs both a clinical decision unit in the ED and a short-stay unit staffed by our hospitalist group. As SHM tracks observation status in future surveys, HM groups will be able to follow this phenomenon among their colleagues and benchmark their own rates of observation encounters.
Dr. Creamer is medical director of the short-stay unit at MetroHealth Medical Center in Cleveland and a member of SHM’s Practice Analysis Committee.
References
- Feng Z, Wright DB, Mor V. Sharp rise in Medicare enrollees being held in hospitals for observation raises concerns about causes and consequences. Health Aff (Millwood). 2012;31(6):1251-1259.
- Baugh CW, Venkatesh AK, Hilton JA, Samuel PA, Schuur JD, Bohan JS. Making greater use of dedicated hospital observation units for many short-stay patients could save $3.1 billion a year. Health Aff (Millwood). 2012;31(10):2314-2323.
- Gengler A. The painful new trend in Medicare. CNN Money website. Available at: http://money.cnn.com/2012/08/07/pf/medicare-rehab-costs.moneymag/index.htm. Accessed March 6, 2013.
- Jaffe S. Patients held for observation can face steep drug bills. USA Today website. Available at: http://usatoday30.usatoday.com/money/industries/health/drugs/story/2012-04-30/drugs-can-be-expensive-in-observation-care/54646378/1. Accessed March 6, 2013.
- Landro L. Filling a gap between ERs and inpatient rooms. The Wall Street Journal website. Available at: http://online.wsj.com/article/SB10001424052970204349404578101060863887052.html. Accessed March 6, 2013.