User login
Using Stroke Order Sets to Improve Compliance With Quality Measures for Ischemic Stroke Admissions
Stroke and cardiovascular disease (CVD) create a heavy economic burden on the health care system in the US.1 About 795,000 people have a stroke in the US each year. In 2013, stroke was the cause of 1 in every 20 deaths in the US.2 On average, someone in the US has a stroke every 40 seconds, and someone dies of one about every 4 minutes.3 Stroke also accounts for 889,000 hospitalizations per year.4,5
Stroke has been studied widely, and evidence-based guidelines have been created for the management of stroke. Despite these published guidelines for stroke care, inconsistencies in stroke management of veterans still exist. These inconsistencies led to the creation of guidelines that include quality measurements for the care of veterans with stroke.
Several campaigns have been mounted to bolster quality care for veterans with ischemic stroke. These include the Primary Stroke Center Certification by The Joint Commission (JC),6 Get With the Guidelines by the American Stroke Association,7 the Paul Coverdell Registry by the Centers for Disease Control and Prevention,8 and other efforts by the National Quality Forum (NQF) and the Centers for Medicare and Medicaid Services.9 These organizations have independently and collaboratively established quality metrics associated with health care delivery for the care of veterans with stroke. Some of these metrics have been distinguished as performance measures, or metrics that are suitable for public reporting, and may be used for comparing institutions and rewarding those who meet specific thresholds (ie, pay for performance).10
The aim of this project was to increase compliance at the Atlanta VA Medical Center (VAMC) in Decatur, Georgia, with JC National Quality Measures for the care of veterans with ischemic stroke, thus providing optimal care for veterans admitted for ischemic stroke management.
There are 3 phases in the management of a patient with a stroke: stroke presentation, admission/management, and discharge. This project focused on the admission/management phase. The stroke presentation phase is completed in the emergency department (ED), and the discharge phase has a check list for stroke, including atrial fibrillation (AF) and counseling prior to discharge. Data from the check list and counseling were not included in this project.
Specific attention was given to the following JC measures: stroke (STK) 1, STK 5, and STK 10 because the Atlanta VAMC was below the national average for these core measures for fiscal year 2015. Compliance was accomplished by creating order sets for the admission and subsequent care of veterans with ischemic stroke, tracking order set usage, and reporting regularly to the medicine/admitting team members on use rates and meeting quality measures. This project underwent the quality vs research review process and was determined to be a quality improvement (QI) project, so the project did not require institutional review board approval.
Methods
At the Atlanta VAMC, all patients admitted for stroke workup or management are admitted to the medicine service. The medicine admitting teams are composed of an attending physician, a medicine resident, a nurse practitioner (NP), a pharmacist, and 2 interns; and the hospitalist team composed of a hospitalist. The project began January 1, 2016, and ended December 31, 2016.
The hospitalist created evidence-based admission orders for all patients admitted for stroke or transient ischemic attack (TIA).The measures used were from the JC Specification Manual for Joint Commission National Quality as well as The American College of Cardiology/American Heart Association classification of care metrics.5
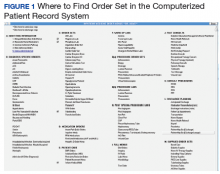
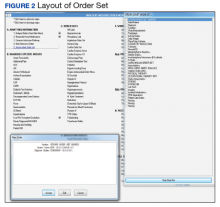
The order sets were reviewed and confirmed by a neurologist. The JC quality measures required for the care of patients admitted for stroke management were embedded in these order sets. These order sets were placed directly under the general admission orders in the Computerized Patient Record System (CPRS)
The quality measures included:
- STK 1: Veteran admitted for stroke received venous thromboembolic (VTE) prophylaxis in a timely manner. Pharmacologic management for VTE prophylaxis with subcutaneous low-molecular weight heparin and/or application of bilateral sequential compression devices were tracked.
- STK 5: Veteran admitted for stroke administered antithrombotic therapy by end of hospital day 2. Aspirin, aspirin/dipyridamole, and ticlopidine were tracked.
- STK 10: Veteran admitted for stroke assessed for rehabilitation services during admission. Physical therapy and occupational therapy consult placements were tracked. Quality measures, such as administration of tissue plasminogen activator (tPA), were not embedded in the order set because veterans who met the criteria for tPA were immediately administered tPA in the ED or transferred to the closest stroke center.
In this QI project, only quality measures that had to be completed in the inpatient setting were included. Quality measures such as tPA administration, National Institutes of Health (NIH) Stroke Scale timely documentation, swallow screen prior to po intake, and stroke transfers were completed in the ED prior to clearance for admission, so these were not included in the project. The Atlanta VAMC ED has protocols to care for these patients, but they do not have order sets with markers that could trace their usage.
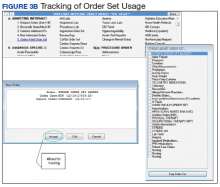
All admission orders placed were reviewed by a QI team to check whether the stroke order set had been used. The ability to determine order set use was accomplished by adding the unique identifier Stroke Order Set Marker, which allowed for querying using structured query language (SQL) within the Corporate Data Warehouse.
Next, all admissions were checked through chart review for compliance with quality measures. Admissions that had not been completed for all quality measures were identified, and the physicians or NPs caring for those veterans were alerted. These order sets were supposed to be used during admission of all patients admitted for stroke management or workup; however, some patients were admitted without the use of the order sets.
The successful completion of the quality measures were then compared between the groups of patients admitted using the order set and the group of patients in which the order set was not used at their admission. The physicians were provided acceptable reasons, including contraindications to certain medications such as patient history of allergy. The admitting physician made decisions on the antiplatelet medications to use or on neurology recommendations. The neurology department was consulted on all patients who had acute or subacute ischemic stroke findings on magnetic resonance imaging (MRI).
At the beginning of the month, internal medicine residents from Emory University and Morehouse School of Medicine received orientation on the use of the stroke order set from the team NP and chief resident. Tips on how to use the CPRS and how to access the stroke order sets also were created.
One challenge the project faced was the continuous change in the admitting team pool: Some residents did not remember to use the stroke order sets.
Results
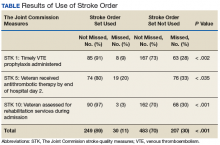
Of 323 admitted patients with stroke, 93 admissions were entered using the stroke order set. Out of these completed orders, 85 (91%) veterans admitted for ischemic stroke or TIA management received timely VTE prophylaxis, and 8 (9%) veterans did not. Of the 230 admissions completed without using the stroke order set, 167 (73%) veterans received timely VTE prophylaxis, and 63 (28%) veterans did not. Additionally out of the 93 veterans admitted using the stroke order set, 74 (80%) veterans admitted for the management of ischemic stroke received antithrombotic therapy by end of hospital day 2, whereas 19 (20%) veterans did not, and there were no clear contraindications documented as to why.
For veterans admitted without using the order set, 167 (73%) veterans admitted for the management of ischemic stroke received antithrombotic therapy by the end of hospital day 2, whereas 76 (33%) veterans did not. Last, 90 (97%) of the 93 veterans admitted for stroke workup using the order set were assessed for rehabilitation services during admission, whereas 3 (3%) were not. For the veterans who were admitted without using the stroke order set, 162 (70%) were assessed for rehabilitation services during admission, whereas 68 (30%) were not.
Out of 969 compliance measures looked at, 237 measures were missed and 732 measures were appropriately completed irrespective of whether the stroke order set was used. Out of the 279 admissions where the stroke order set was used, 249 (89%) quality measures were met.
The study threshold for meeting the standards was the national average for 2015, which was 91.1% for the administration of VTE prophylaxis in a timely manner, 97.9% for administering antithrombotic therapy by end of hospital day 2, and 94.2% for assessment of the patient by rehabilitation services during the admission.
Discussion
Despite the repeated training and orientation, compliance to the order set usage was not optimal, likely secondary to a frequent change in the pool of admitting physicians using the order set. Also, the order set was new to staff, thus, admitting physicians sometimes forgot to use them. The next step in this project will be to create an order set for the ED with markers for tracing usage. These order sets will include all quality measures that need to be completed in the ED, such as the NIH Stroke Scale timely documentation, tPA administration data, swallow screen prior to po intake, and stroke transfers.
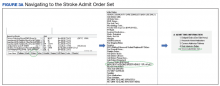
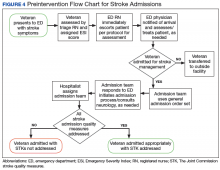
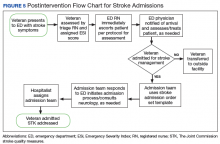
This QI project also streamlined the process for stroke admissions. With the creation of the order set, all orders needed for stroke were available to the admitting physician, resulting in less need for searching the order individually from a large pool of orders (Figures 3 and 4).
Several reputable institutions have quality metrics and performance measures typically focused on processes of care based on specific clinical guidelines recommendations. Clinical guidelines are usually based on sufficient evidence that failure to provide the recommended care is likely to result in suboptimal clinical outcomes. Stroke quality measure compliance is part of the Reporting Hospital Quality Data for Annual Payment Update (RHQDAPU) initiative, and most hospitals will be required to report these measures in order to receive full Medicare payments.11
Limitations
Limitations of this study relate to CPRS functions, which must be specifically activated at different VA sites in order to enable the use of these functions. Also, the successful creation of these order sets depended on the information specialist’s knowledge of the capabilities of the CPRS.
Conclusion
Gaps in practice and recommended guidelines can be bridged by creating standardized admission orders embedded with required quality measures. The Atlanta VAMC project showed that the use of a standardized stroke admission order set significantly improved compliance to quality measures for veterans admitted for ischemic stroke management. This is consistent with a study completed in the ED, which showed that for veterans hospitalized for acute ischemic stroke, electronic order set use was associated with increased use of IV tPA.12 Creating order sets can be challenging, but if these barriers can be overcome, with the first order set, similar templates can be used to create order sets for other clinical conditions, such as heart failure, sepsis, and chronic obstructive pulmonary disease exacerbation.
1. Writing Group Members, Mozaffarian D, Benjamin EJ, Go AS, et al; American Heart Association Statistics Committee; Stroke Statistics Subcommittee. Executive summary: heart disease and stroke statistics—2016 update: a report from the American Heart Association. Circulation. 2016;133(4):447-454.
2. Centers for Disease Control and Prevention. Vital signs: recent trends in stroke death rates–United States, 2000-2015. https://www.cdc.gov/mmwr/volumes/66/wr/mm6635e1.htm. Published September 8, 2017. Accessed June 14, 2018.
3. Benjamin EJ, Blaha MJ, Chiuve SE, et al; American Heart Association Statistics Committee and Stroke Statistics Subcommittee. Heart disease and stroke statistics—2017 update: a report from the American Heart Association. Circulation. 2017;135(10):e229-e445.
4. Lloyd-Jones D, Adams R, Carnethon M, et al; American Heart Association Statistics Committee and Stroke Statistics Subcommittee. Heart disease and stroke statistics—2009 update: a report from the American heart association statistics committee and stroke statistics subcommittee. Circulation. 2009;119(3):480-486.
5. Poisson SN, Josephson SA. Quality measures in stroke. Neurohospitalist. 2011;1(2):71-77.
6. The Joint Commission. Primary Stroke Centers—Stroke Performance Measurement. https://www.jointcommission.org/performance_ measurement.aspx. Accessed June 14, 2018.
7. American Stroke Association. Get with the guidelines–stroke. http://www.heart.org/HEARTORG/Professional/GetWithTheGuidelines/GetWithTheGuidelines-Stroke/Get-With-The-Guidelines-Stroke-Overview_UCM_308021_Article.jsp#.WyKre1VKiUk. Accessed June 14, 2018.
8. Centers for Disease Control and Prevention. The Paul Coverdell National Acute Stroke Registry. www.cdc.gov/DHDSP/stroke_registry.htm. Published March 13, 2008.
9. Reeves MJ, Parker C, Fonarow GC, Smith EE, Schwamm LH. Development of stroke performance measures: definitions, methods, and current measures. Stroke. 2010;41(7):1573-1578.
10. American College of Cardiology/American Heart Association Task Force on Performance Measures, Bonow RO, Masoudi FA, et al. ACC/AHA classification of care metrics: performance measures and quality metrics: a report of the American College of Cardiology/American Heart Association Task Force on performance measures. Circulation. 2008;118(24):2662-2666.
11. Centers for Medicare and Medicaid Services. Reporting Hospital Quality Data for Annual Payment Update https://www.cms.gov/Medicare/Quality-Initiatives-Patient-Assessment-Instruments/HospitalQualityInits/downloads/HospitalFactSheetAP.pdf. Published November 2004. Accessed June 14, 2018.
12. Ballard DW, Kim AS, Huang J, et al; KP CREST Network Investigators. Implementation of computerized physician order entry is associated with increased thrombolytic administration for emergency department veterans with acute ischemic stroke. Ann Emerg Med. 2015;66(6):601-610.
Stroke and cardiovascular disease (CVD) create a heavy economic burden on the health care system in the US.1 About 795,000 people have a stroke in the US each year. In 2013, stroke was the cause of 1 in every 20 deaths in the US.2 On average, someone in the US has a stroke every 40 seconds, and someone dies of one about every 4 minutes.3 Stroke also accounts for 889,000 hospitalizations per year.4,5
Stroke has been studied widely, and evidence-based guidelines have been created for the management of stroke. Despite these published guidelines for stroke care, inconsistencies in stroke management of veterans still exist. These inconsistencies led to the creation of guidelines that include quality measurements for the care of veterans with stroke.
Several campaigns have been mounted to bolster quality care for veterans with ischemic stroke. These include the Primary Stroke Center Certification by The Joint Commission (JC),6 Get With the Guidelines by the American Stroke Association,7 the Paul Coverdell Registry by the Centers for Disease Control and Prevention,8 and other efforts by the National Quality Forum (NQF) and the Centers for Medicare and Medicaid Services.9 These organizations have independently and collaboratively established quality metrics associated with health care delivery for the care of veterans with stroke. Some of these metrics have been distinguished as performance measures, or metrics that are suitable for public reporting, and may be used for comparing institutions and rewarding those who meet specific thresholds (ie, pay for performance).10
The aim of this project was to increase compliance at the Atlanta VA Medical Center (VAMC) in Decatur, Georgia, with JC National Quality Measures for the care of veterans with ischemic stroke, thus providing optimal care for veterans admitted for ischemic stroke management.
There are 3 phases in the management of a patient with a stroke: stroke presentation, admission/management, and discharge. This project focused on the admission/management phase. The stroke presentation phase is completed in the emergency department (ED), and the discharge phase has a check list for stroke, including atrial fibrillation (AF) and counseling prior to discharge. Data from the check list and counseling were not included in this project.
Specific attention was given to the following JC measures: stroke (STK) 1, STK 5, and STK 10 because the Atlanta VAMC was below the national average for these core measures for fiscal year 2015. Compliance was accomplished by creating order sets for the admission and subsequent care of veterans with ischemic stroke, tracking order set usage, and reporting regularly to the medicine/admitting team members on use rates and meeting quality measures. This project underwent the quality vs research review process and was determined to be a quality improvement (QI) project, so the project did not require institutional review board approval.
Methods
At the Atlanta VAMC, all patients admitted for stroke workup or management are admitted to the medicine service. The medicine admitting teams are composed of an attending physician, a medicine resident, a nurse practitioner (NP), a pharmacist, and 2 interns; and the hospitalist team composed of a hospitalist. The project began January 1, 2016, and ended December 31, 2016.
The hospitalist created evidence-based admission orders for all patients admitted for stroke or transient ischemic attack (TIA).The measures used were from the JC Specification Manual for Joint Commission National Quality as well as The American College of Cardiology/American Heart Association classification of care metrics.5
The order sets were reviewed and confirmed by a neurologist. The JC quality measures required for the care of patients admitted for stroke management were embedded in these order sets. These order sets were placed directly under the general admission orders in the Computerized Patient Record System (CPRS)
The quality measures included:
- STK 1: Veteran admitted for stroke received venous thromboembolic (VTE) prophylaxis in a timely manner. Pharmacologic management for VTE prophylaxis with subcutaneous low-molecular weight heparin and/or application of bilateral sequential compression devices were tracked.
- STK 5: Veteran admitted for stroke administered antithrombotic therapy by end of hospital day 2. Aspirin, aspirin/dipyridamole, and ticlopidine were tracked.
- STK 10: Veteran admitted for stroke assessed for rehabilitation services during admission. Physical therapy and occupational therapy consult placements were tracked. Quality measures, such as administration of tissue plasminogen activator (tPA), were not embedded in the order set because veterans who met the criteria for tPA were immediately administered tPA in the ED or transferred to the closest stroke center.
In this QI project, only quality measures that had to be completed in the inpatient setting were included. Quality measures such as tPA administration, National Institutes of Health (NIH) Stroke Scale timely documentation, swallow screen prior to po intake, and stroke transfers were completed in the ED prior to clearance for admission, so these were not included in the project. The Atlanta VAMC ED has protocols to care for these patients, but they do not have order sets with markers that could trace their usage.
All admission orders placed were reviewed by a QI team to check whether the stroke order set had been used. The ability to determine order set use was accomplished by adding the unique identifier Stroke Order Set Marker, which allowed for querying using structured query language (SQL) within the Corporate Data Warehouse.
Next, all admissions were checked through chart review for compliance with quality measures. Admissions that had not been completed for all quality measures were identified, and the physicians or NPs caring for those veterans were alerted. These order sets were supposed to be used during admission of all patients admitted for stroke management or workup; however, some patients were admitted without the use of the order sets.
The successful completion of the quality measures were then compared between the groups of patients admitted using the order set and the group of patients in which the order set was not used at their admission. The physicians were provided acceptable reasons, including contraindications to certain medications such as patient history of allergy. The admitting physician made decisions on the antiplatelet medications to use or on neurology recommendations. The neurology department was consulted on all patients who had acute or subacute ischemic stroke findings on magnetic resonance imaging (MRI).
At the beginning of the month, internal medicine residents from Emory University and Morehouse School of Medicine received orientation on the use of the stroke order set from the team NP and chief resident. Tips on how to use the CPRS and how to access the stroke order sets also were created.
One challenge the project faced was the continuous change in the admitting team pool: Some residents did not remember to use the stroke order sets.
Results
Of 323 admitted patients with stroke, 93 admissions were entered using the stroke order set. Out of these completed orders, 85 (91%) veterans admitted for ischemic stroke or TIA management received timely VTE prophylaxis, and 8 (9%) veterans did not. Of the 230 admissions completed without using the stroke order set, 167 (73%) veterans received timely VTE prophylaxis, and 63 (28%) veterans did not. Additionally out of the 93 veterans admitted using the stroke order set, 74 (80%) veterans admitted for the management of ischemic stroke received antithrombotic therapy by end of hospital day 2, whereas 19 (20%) veterans did not, and there were no clear contraindications documented as to why.
For veterans admitted without using the order set, 167 (73%) veterans admitted for the management of ischemic stroke received antithrombotic therapy by the end of hospital day 2, whereas 76 (33%) veterans did not. Last, 90 (97%) of the 93 veterans admitted for stroke workup using the order set were assessed for rehabilitation services during admission, whereas 3 (3%) were not. For the veterans who were admitted without using the stroke order set, 162 (70%) were assessed for rehabilitation services during admission, whereas 68 (30%) were not.
Out of 969 compliance measures looked at, 237 measures were missed and 732 measures were appropriately completed irrespective of whether the stroke order set was used. Out of the 279 admissions where the stroke order set was used, 249 (89%) quality measures were met.
The study threshold for meeting the standards was the national average for 2015, which was 91.1% for the administration of VTE prophylaxis in a timely manner, 97.9% for administering antithrombotic therapy by end of hospital day 2, and 94.2% for assessment of the patient by rehabilitation services during the admission.
Discussion
Despite the repeated training and orientation, compliance to the order set usage was not optimal, likely secondary to a frequent change in the pool of admitting physicians using the order set. Also, the order set was new to staff, thus, admitting physicians sometimes forgot to use them. The next step in this project will be to create an order set for the ED with markers for tracing usage. These order sets will include all quality measures that need to be completed in the ED, such as the NIH Stroke Scale timely documentation, tPA administration data, swallow screen prior to po intake, and stroke transfers.
This QI project also streamlined the process for stroke admissions. With the creation of the order set, all orders needed for stroke were available to the admitting physician, resulting in less need for searching the order individually from a large pool of orders (Figures 3 and 4).
Several reputable institutions have quality metrics and performance measures typically focused on processes of care based on specific clinical guidelines recommendations. Clinical guidelines are usually based on sufficient evidence that failure to provide the recommended care is likely to result in suboptimal clinical outcomes. Stroke quality measure compliance is part of the Reporting Hospital Quality Data for Annual Payment Update (RHQDAPU) initiative, and most hospitals will be required to report these measures in order to receive full Medicare payments.11
Limitations
Limitations of this study relate to CPRS functions, which must be specifically activated at different VA sites in order to enable the use of these functions. Also, the successful creation of these order sets depended on the information specialist’s knowledge of the capabilities of the CPRS.
Conclusion
Gaps in practice and recommended guidelines can be bridged by creating standardized admission orders embedded with required quality measures. The Atlanta VAMC project showed that the use of a standardized stroke admission order set significantly improved compliance to quality measures for veterans admitted for ischemic stroke management. This is consistent with a study completed in the ED, which showed that for veterans hospitalized for acute ischemic stroke, electronic order set use was associated with increased use of IV tPA.12 Creating order sets can be challenging, but if these barriers can be overcome, with the first order set, similar templates can be used to create order sets for other clinical conditions, such as heart failure, sepsis, and chronic obstructive pulmonary disease exacerbation.
Stroke and cardiovascular disease (CVD) create a heavy economic burden on the health care system in the US.1 About 795,000 people have a stroke in the US each year. In 2013, stroke was the cause of 1 in every 20 deaths in the US.2 On average, someone in the US has a stroke every 40 seconds, and someone dies of one about every 4 minutes.3 Stroke also accounts for 889,000 hospitalizations per year.4,5
Stroke has been studied widely, and evidence-based guidelines have been created for the management of stroke. Despite these published guidelines for stroke care, inconsistencies in stroke management of veterans still exist. These inconsistencies led to the creation of guidelines that include quality measurements for the care of veterans with stroke.
Several campaigns have been mounted to bolster quality care for veterans with ischemic stroke. These include the Primary Stroke Center Certification by The Joint Commission (JC),6 Get With the Guidelines by the American Stroke Association,7 the Paul Coverdell Registry by the Centers for Disease Control and Prevention,8 and other efforts by the National Quality Forum (NQF) and the Centers for Medicare and Medicaid Services.9 These organizations have independently and collaboratively established quality metrics associated with health care delivery for the care of veterans with stroke. Some of these metrics have been distinguished as performance measures, or metrics that are suitable for public reporting, and may be used for comparing institutions and rewarding those who meet specific thresholds (ie, pay for performance).10
The aim of this project was to increase compliance at the Atlanta VA Medical Center (VAMC) in Decatur, Georgia, with JC National Quality Measures for the care of veterans with ischemic stroke, thus providing optimal care for veterans admitted for ischemic stroke management.
There are 3 phases in the management of a patient with a stroke: stroke presentation, admission/management, and discharge. This project focused on the admission/management phase. The stroke presentation phase is completed in the emergency department (ED), and the discharge phase has a check list for stroke, including atrial fibrillation (AF) and counseling prior to discharge. Data from the check list and counseling were not included in this project.
Specific attention was given to the following JC measures: stroke (STK) 1, STK 5, and STK 10 because the Atlanta VAMC was below the national average for these core measures for fiscal year 2015. Compliance was accomplished by creating order sets for the admission and subsequent care of veterans with ischemic stroke, tracking order set usage, and reporting regularly to the medicine/admitting team members on use rates and meeting quality measures. This project underwent the quality vs research review process and was determined to be a quality improvement (QI) project, so the project did not require institutional review board approval.
Methods
At the Atlanta VAMC, all patients admitted for stroke workup or management are admitted to the medicine service. The medicine admitting teams are composed of an attending physician, a medicine resident, a nurse practitioner (NP), a pharmacist, and 2 interns; and the hospitalist team composed of a hospitalist. The project began January 1, 2016, and ended December 31, 2016.
The hospitalist created evidence-based admission orders for all patients admitted for stroke or transient ischemic attack (TIA).The measures used were from the JC Specification Manual for Joint Commission National Quality as well as The American College of Cardiology/American Heart Association classification of care metrics.5
The order sets were reviewed and confirmed by a neurologist. The JC quality measures required for the care of patients admitted for stroke management were embedded in these order sets. These order sets were placed directly under the general admission orders in the Computerized Patient Record System (CPRS)
The quality measures included:
- STK 1: Veteran admitted for stroke received venous thromboembolic (VTE) prophylaxis in a timely manner. Pharmacologic management for VTE prophylaxis with subcutaneous low-molecular weight heparin and/or application of bilateral sequential compression devices were tracked.
- STK 5: Veteran admitted for stroke administered antithrombotic therapy by end of hospital day 2. Aspirin, aspirin/dipyridamole, and ticlopidine were tracked.
- STK 10: Veteran admitted for stroke assessed for rehabilitation services during admission. Physical therapy and occupational therapy consult placements were tracked. Quality measures, such as administration of tissue plasminogen activator (tPA), were not embedded in the order set because veterans who met the criteria for tPA were immediately administered tPA in the ED or transferred to the closest stroke center.
In this QI project, only quality measures that had to be completed in the inpatient setting were included. Quality measures such as tPA administration, National Institutes of Health (NIH) Stroke Scale timely documentation, swallow screen prior to po intake, and stroke transfers were completed in the ED prior to clearance for admission, so these were not included in the project. The Atlanta VAMC ED has protocols to care for these patients, but they do not have order sets with markers that could trace their usage.
All admission orders placed were reviewed by a QI team to check whether the stroke order set had been used. The ability to determine order set use was accomplished by adding the unique identifier Stroke Order Set Marker, which allowed for querying using structured query language (SQL) within the Corporate Data Warehouse.
Next, all admissions were checked through chart review for compliance with quality measures. Admissions that had not been completed for all quality measures were identified, and the physicians or NPs caring for those veterans were alerted. These order sets were supposed to be used during admission of all patients admitted for stroke management or workup; however, some patients were admitted without the use of the order sets.
The successful completion of the quality measures were then compared between the groups of patients admitted using the order set and the group of patients in which the order set was not used at their admission. The physicians were provided acceptable reasons, including contraindications to certain medications such as patient history of allergy. The admitting physician made decisions on the antiplatelet medications to use or on neurology recommendations. The neurology department was consulted on all patients who had acute or subacute ischemic stroke findings on magnetic resonance imaging (MRI).
At the beginning of the month, internal medicine residents from Emory University and Morehouse School of Medicine received orientation on the use of the stroke order set from the team NP and chief resident. Tips on how to use the CPRS and how to access the stroke order sets also were created.
One challenge the project faced was the continuous change in the admitting team pool: Some residents did not remember to use the stroke order sets.
Results
Of 323 admitted patients with stroke, 93 admissions were entered using the stroke order set. Out of these completed orders, 85 (91%) veterans admitted for ischemic stroke or TIA management received timely VTE prophylaxis, and 8 (9%) veterans did not. Of the 230 admissions completed without using the stroke order set, 167 (73%) veterans received timely VTE prophylaxis, and 63 (28%) veterans did not. Additionally out of the 93 veterans admitted using the stroke order set, 74 (80%) veterans admitted for the management of ischemic stroke received antithrombotic therapy by end of hospital day 2, whereas 19 (20%) veterans did not, and there were no clear contraindications documented as to why.
For veterans admitted without using the order set, 167 (73%) veterans admitted for the management of ischemic stroke received antithrombotic therapy by the end of hospital day 2, whereas 76 (33%) veterans did not. Last, 90 (97%) of the 93 veterans admitted for stroke workup using the order set were assessed for rehabilitation services during admission, whereas 3 (3%) were not. For the veterans who were admitted without using the stroke order set, 162 (70%) were assessed for rehabilitation services during admission, whereas 68 (30%) were not.
Out of 969 compliance measures looked at, 237 measures were missed and 732 measures were appropriately completed irrespective of whether the stroke order set was used. Out of the 279 admissions where the stroke order set was used, 249 (89%) quality measures were met.
The study threshold for meeting the standards was the national average for 2015, which was 91.1% for the administration of VTE prophylaxis in a timely manner, 97.9% for administering antithrombotic therapy by end of hospital day 2, and 94.2% for assessment of the patient by rehabilitation services during the admission.
Discussion
Despite the repeated training and orientation, compliance to the order set usage was not optimal, likely secondary to a frequent change in the pool of admitting physicians using the order set. Also, the order set was new to staff, thus, admitting physicians sometimes forgot to use them. The next step in this project will be to create an order set for the ED with markers for tracing usage. These order sets will include all quality measures that need to be completed in the ED, such as the NIH Stroke Scale timely documentation, tPA administration data, swallow screen prior to po intake, and stroke transfers.
This QI project also streamlined the process for stroke admissions. With the creation of the order set, all orders needed for stroke were available to the admitting physician, resulting in less need for searching the order individually from a large pool of orders (Figures 3 and 4).
Several reputable institutions have quality metrics and performance measures typically focused on processes of care based on specific clinical guidelines recommendations. Clinical guidelines are usually based on sufficient evidence that failure to provide the recommended care is likely to result in suboptimal clinical outcomes. Stroke quality measure compliance is part of the Reporting Hospital Quality Data for Annual Payment Update (RHQDAPU) initiative, and most hospitals will be required to report these measures in order to receive full Medicare payments.11
Limitations
Limitations of this study relate to CPRS functions, which must be specifically activated at different VA sites in order to enable the use of these functions. Also, the successful creation of these order sets depended on the information specialist’s knowledge of the capabilities of the CPRS.
Conclusion
Gaps in practice and recommended guidelines can be bridged by creating standardized admission orders embedded with required quality measures. The Atlanta VAMC project showed that the use of a standardized stroke admission order set significantly improved compliance to quality measures for veterans admitted for ischemic stroke management. This is consistent with a study completed in the ED, which showed that for veterans hospitalized for acute ischemic stroke, electronic order set use was associated with increased use of IV tPA.12 Creating order sets can be challenging, but if these barriers can be overcome, with the first order set, similar templates can be used to create order sets for other clinical conditions, such as heart failure, sepsis, and chronic obstructive pulmonary disease exacerbation.
1. Writing Group Members, Mozaffarian D, Benjamin EJ, Go AS, et al; American Heart Association Statistics Committee; Stroke Statistics Subcommittee. Executive summary: heart disease and stroke statistics—2016 update: a report from the American Heart Association. Circulation. 2016;133(4):447-454.
2. Centers for Disease Control and Prevention. Vital signs: recent trends in stroke death rates–United States, 2000-2015. https://www.cdc.gov/mmwr/volumes/66/wr/mm6635e1.htm. Published September 8, 2017. Accessed June 14, 2018.
3. Benjamin EJ, Blaha MJ, Chiuve SE, et al; American Heart Association Statistics Committee and Stroke Statistics Subcommittee. Heart disease and stroke statistics—2017 update: a report from the American Heart Association. Circulation. 2017;135(10):e229-e445.
4. Lloyd-Jones D, Adams R, Carnethon M, et al; American Heart Association Statistics Committee and Stroke Statistics Subcommittee. Heart disease and stroke statistics—2009 update: a report from the American heart association statistics committee and stroke statistics subcommittee. Circulation. 2009;119(3):480-486.
5. Poisson SN, Josephson SA. Quality measures in stroke. Neurohospitalist. 2011;1(2):71-77.
6. The Joint Commission. Primary Stroke Centers—Stroke Performance Measurement. https://www.jointcommission.org/performance_ measurement.aspx. Accessed June 14, 2018.
7. American Stroke Association. Get with the guidelines–stroke. http://www.heart.org/HEARTORG/Professional/GetWithTheGuidelines/GetWithTheGuidelines-Stroke/Get-With-The-Guidelines-Stroke-Overview_UCM_308021_Article.jsp#.WyKre1VKiUk. Accessed June 14, 2018.
8. Centers for Disease Control and Prevention. The Paul Coverdell National Acute Stroke Registry. www.cdc.gov/DHDSP/stroke_registry.htm. Published March 13, 2008.
9. Reeves MJ, Parker C, Fonarow GC, Smith EE, Schwamm LH. Development of stroke performance measures: definitions, methods, and current measures. Stroke. 2010;41(7):1573-1578.
10. American College of Cardiology/American Heart Association Task Force on Performance Measures, Bonow RO, Masoudi FA, et al. ACC/AHA classification of care metrics: performance measures and quality metrics: a report of the American College of Cardiology/American Heart Association Task Force on performance measures. Circulation. 2008;118(24):2662-2666.
11. Centers for Medicare and Medicaid Services. Reporting Hospital Quality Data for Annual Payment Update https://www.cms.gov/Medicare/Quality-Initiatives-Patient-Assessment-Instruments/HospitalQualityInits/downloads/HospitalFactSheetAP.pdf. Published November 2004. Accessed June 14, 2018.
12. Ballard DW, Kim AS, Huang J, et al; KP CREST Network Investigators. Implementation of computerized physician order entry is associated with increased thrombolytic administration for emergency department veterans with acute ischemic stroke. Ann Emerg Med. 2015;66(6):601-610.
1. Writing Group Members, Mozaffarian D, Benjamin EJ, Go AS, et al; American Heart Association Statistics Committee; Stroke Statistics Subcommittee. Executive summary: heart disease and stroke statistics—2016 update: a report from the American Heart Association. Circulation. 2016;133(4):447-454.
2. Centers for Disease Control and Prevention. Vital signs: recent trends in stroke death rates–United States, 2000-2015. https://www.cdc.gov/mmwr/volumes/66/wr/mm6635e1.htm. Published September 8, 2017. Accessed June 14, 2018.
3. Benjamin EJ, Blaha MJ, Chiuve SE, et al; American Heart Association Statistics Committee and Stroke Statistics Subcommittee. Heart disease and stroke statistics—2017 update: a report from the American Heart Association. Circulation. 2017;135(10):e229-e445.
4. Lloyd-Jones D, Adams R, Carnethon M, et al; American Heart Association Statistics Committee and Stroke Statistics Subcommittee. Heart disease and stroke statistics—2009 update: a report from the American heart association statistics committee and stroke statistics subcommittee. Circulation. 2009;119(3):480-486.
5. Poisson SN, Josephson SA. Quality measures in stroke. Neurohospitalist. 2011;1(2):71-77.
6. The Joint Commission. Primary Stroke Centers—Stroke Performance Measurement. https://www.jointcommission.org/performance_ measurement.aspx. Accessed June 14, 2018.
7. American Stroke Association. Get with the guidelines–stroke. http://www.heart.org/HEARTORG/Professional/GetWithTheGuidelines/GetWithTheGuidelines-Stroke/Get-With-The-Guidelines-Stroke-Overview_UCM_308021_Article.jsp#.WyKre1VKiUk. Accessed June 14, 2018.
8. Centers for Disease Control and Prevention. The Paul Coverdell National Acute Stroke Registry. www.cdc.gov/DHDSP/stroke_registry.htm. Published March 13, 2008.
9. Reeves MJ, Parker C, Fonarow GC, Smith EE, Schwamm LH. Development of stroke performance measures: definitions, methods, and current measures. Stroke. 2010;41(7):1573-1578.
10. American College of Cardiology/American Heart Association Task Force on Performance Measures, Bonow RO, Masoudi FA, et al. ACC/AHA classification of care metrics: performance measures and quality metrics: a report of the American College of Cardiology/American Heart Association Task Force on performance measures. Circulation. 2008;118(24):2662-2666.
11. Centers for Medicare and Medicaid Services. Reporting Hospital Quality Data for Annual Payment Update https://www.cms.gov/Medicare/Quality-Initiatives-Patient-Assessment-Instruments/HospitalQualityInits/downloads/HospitalFactSheetAP.pdf. Published November 2004. Accessed June 14, 2018.
12. Ballard DW, Kim AS, Huang J, et al; KP CREST Network Investigators. Implementation of computerized physician order entry is associated with increased thrombolytic administration for emergency department veterans with acute ischemic stroke. Ann Emerg Med. 2015;66(6):601-610.