User login
Using Simulation to Enhance Care of Older Veterans
Enhancing patient-centered care is an important priority for caregivers in all settings but particularly in long-term care (LTC) where patients also are residents. Simulation is a potential strategy to effect cultural change for health care providers at LTC facilities. In a clinical setting, simulation is an educational model that allows staff to practice behaviors or skills without putting patients at risk. Due to limited time, staffing, and budget resources, the use of simulation for training is not common at LTC facilities.
Background
The simulation model is considered an effective teaching and learning strategy for replicating experiences in nursing practice.1,2 The interactive experience provides the learner with opportunities to engage with patients through psychomotor participation, critical thinking, reflection, and debriefing. Prelicensure nursing education programs and acute care hospitals are the most common users of simulation learning. However, there is a paucity of literature addressing the use of simulation in LTC.
One study was conducted in 2002 by P.K. Beville called the Virtual Dementia Tour, a program using evidence-based simulation. Beville found that study participants using the simulation model had a heightened awareness of the challenges of confused elderly as well as unrealistic expectations by caregivers.3 Although the Virtual Dementia Tour is available for a fee for training professional caregivers, lay people, family, and first responders, many LTC facilities do not have sufficient funding for simulation and simulation equipment, and many do not have dedicated staff for nursing education. Most staff in LTC facilities are unlicensed and may not have had simulation training experience. Additionally, due to staffing and budget constraints, staff education may be limited.
This article will describe the successful implementation of a simulation-based quality improvement project created by and used at the Louis Stokes Cleveland VA Medical Center (LSCVAMC) LTC facility. The LSCVAMC has acute care beds and is adjacent to its LTC facility. Also, a previously successful simulation educational program to improve delirium care was conducted at this acute care hospital.4
Experiential Learning Opportunity
Many residents in a LTC facility have been diagnosed with dementia. As part of a cultural transformation at LSCVAMC, a simulation program was used to help sensitize LTC caregivers to the many sensory changes that occur in older veterans with dementia. The program was guided by the Kolb model.5
The Kolb model of experiential learning includes 4 elements: abstract conceptualization (knowledge), active experimentation (application), concrete experience (engagement), and reflective observation (self-evaluation).5 A simulation program can touch all 4 elements of the Kolb model by providing an educational experience for all learning styles as well as facilitating critical thinking. Nursing homes that provide care to residents with dementia are required to include dementia education annually to staff.6 Long-term care facilities can take advantage of using simulation education along with their traditional educational programs to provide staff with exposure to realistic resident care conditions.7
Methods
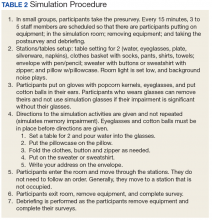
The simulation learning experience was provided to all nursing, recreation therapy, and rehabilitation services staff at the LTC facility. The goal was to create an affective, psychomotor learning experience that refreshed, reminded, and sensitized the staff to the challenges that many residents face. The LSCVAMC LTC leadership was supportive of this simulation model because it was not time intensive for direct care staff, and the materials needed were inexpensive. The only equipment that was purchased were several eyeglass readers, popcorn kernels, and Vaseline, resulting in a budget of about $10. The simulation program was scheduled on all shifts. In addition to the simulation experience, the model consists of pre- and postsurveys and a dementia review handout. Staff were able to complete a pre- and postsurvey as well as a debriefing all within a 30-minute time slot.
The pre- and posteducation surveys used were designed to measure learnings and provide data for future education planning. The surveys required only a yes/no and short answers. To reduce the total time of participants’ involvement in the simulation program, an online survey was used. Presurvey questions were designed to identify basic knowledge and experience with dementia, both at work and in personal life. The postsurvey questions sought to identify affective feelings about the participants experience as well as lessons learned and how that could impact future care.
The dementia review handout that was provided to staff 2 weeks before the simulation provided an overview of dementia. It included communication techniques and care planning suggestions.8 The time spent in the simulation room was about 10 to 15 minutes but depended on the activity. The total in-service time was about 30 minutes, depending on the time allotted for debriefing. Room choice was influenced by the number of participants performing the simulation at the same time. Activity stations/tables generally provided 1 experience at a time.
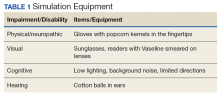
The room that was used had adjustable lighting with the ability to provide a low light setting. Activities were chosen based on the goals for the physical and cognitive disabilities to be simulated. Table 1 identifies equipment used with success and chosen with consideration for ease and expense in describing the disability.
Simulation activities were based on the staff learning needs determined by the presimulation survey. Simulated deficits impacted activities of daily living, mood, and cognition. Neuropathy, arthritis, paralysis, dementia, glaucoma, cataracts, and hearing loss are conditions that are easily represented in a simulation.
Participants also gained additional knowledge of dementia through the Kolb process, which was included in the debriefing. The survey followed the completion of the simulation session to identify knowledge deficits for general remediation and program development and expansion.
Discussion
During the dementia simulation, active experimentation or application learning may be counterintuitive. Staff do not apply their knowledge of dementia directly as in other education settings where they can practice or demonstrate a skill. Instead, participants experience care from the perspective of residents. This learning transitions well into reflective observation as the participants begin to understand the challenges of the cognitively impaired resident, which are manifested in the residents’ behaviors.
Debriefing and a postsimulation survey provide a guided reflection to assimilate new knowledge and revise presimulation attitudes about dementia.9 Reflective observation or self-evaluation is a learning activity that is not a routine part of staff education but can be a powerful learning tool. The postsimulation survey incorporated Bloom’s taxonomy: the affective domain of learning by challenging staff to organize their values with the experience and resolving in their mind any conflicts.10 The goal of the process is to help internalize the education by encouraging changes in behavior (in this case dementia care) and considering the new experience.
Survey Results
The 30-minute program allowed 155 staff to experience cognitive and physical impairment while completing tasks. The pre- and postsurveys were analyzed by 2 learning and dementia survey content experts. The survey questions were open-ended with the intention of eliciting affective behavior responses and staff could provide comments (See eTables 1 and 2 at www.mdedge.com/fedprac). All participants indicated they had knowledge of dementia before the simulation, but 70% acknowledged in the postsimulation survey that they did not have the dementia knowledge that they thought they had. Patience and understanding were most commonly reported in the reflective observation/affective domain (values are internalized leading to changes in behavior).
Participants also described success in closing the loop of experiential learning as a result of the simulation. Some participants verbalized experiencing emotional distress when they realized that their temporary, frustrating impairment was a permanent condition for the residents. Postexperience comments supported the success of the Kolb model experiential learning activity.
Conclusion
Dementia simulation can augment didactic education for improving the quality of dementia care. The virtual dementia simulation was an inexpensive educational program that did not adversely impact scheduling or patient care in a LTC facility. Care providers provided anecdotal feedback that suggested that the program increased their awareness of the difficulty of performing activities of daily living for patients with dementia. The simulation touched all 4 elements of the Kolb Model. The participants had gained new knowledge or reinforced existing knowledge. The simulation activities addressed the application and engagement parts of the model. Self-evaluation resulted from the debriefing time and postsurvey questions. The virtual dementia simulation will be repeated with additional debrief time and a long-term follow-up survey to identify additional learning needs and changes in professional practice.
Acknowledgments
The author thanks Nurse Educator Lisa Weber, MSN, RN-BC, for her contribution to the manuscript.
1. Aebersold M, Tschannen D. Simulation in nursing practice: the impact on patient care. Online J Issues Nurs. 2013;18(2):6.
2. Mariani B, Doolen J. Nursing simulation research: what are the perceived gaps? Clin Simulation in Nurs. 2016;12(1):30-36.
3. Beville PK. Virtual Dementia Tour helps sensitize health care providers. Am J Alzheimers Dis Other Demen. 2002;17(3):183-190.
4. Kresevic D, Heath B, Fine-Smilovich E, et al. Simulation training, coaching, and cue cards improve delirium care. Fed Pract. 2016;33(12):22-28.
5. Chmil JV, Turk M, Adamson K, Larew C. Effects of an experiential learning simulation design on clinical nursing judgment development. Nurse Educ. 2015;40(5):228-232.
6. Centers for Medicare & Medicaid Services. Medicare and Medicaid programs; reform of requirements for long-term care facilities, final rule. https://www.federalregister.gov/documents/2016/10/04/2016-23503/medicare-and-medicaid-programs-reform-of-requirements-for-long-term-care-facilities. Published October 4, 2016. Accessed May 22, 2018.
7. Donahoe J, Moon L, VanCleave K. Increasing student empathy toward older adults using the virtual dementia tour. J Baccalaureate Soc Work. 2014;19(1):S23-S40.
8. Coggins MD. Behavioral expressions in dementia patients. http://www.todaysgeriatricmedicine.com/archive/0115p6.shtml. Published 2015. Accessed May 10, 2018.
9. Al Sabei SD, Lasater K. Simulation debriefing for clinical judgment development: a concept analysis. Nurse Educ Today. 2016;45:42-47.
10. Anderson LW, Krathwohl DR, Bloom BS, eds. A Taxonomy for Learning, Teaching, and Assessing: A revision of Bloom’s Taxonomy of Educational Objectives. New York: Longman; 2001.
Enhancing patient-centered care is an important priority for caregivers in all settings but particularly in long-term care (LTC) where patients also are residents. Simulation is a potential strategy to effect cultural change for health care providers at LTC facilities. In a clinical setting, simulation is an educational model that allows staff to practice behaviors or skills without putting patients at risk. Due to limited time, staffing, and budget resources, the use of simulation for training is not common at LTC facilities.
Background
The simulation model is considered an effective teaching and learning strategy for replicating experiences in nursing practice.1,2 The interactive experience provides the learner with opportunities to engage with patients through psychomotor participation, critical thinking, reflection, and debriefing. Prelicensure nursing education programs and acute care hospitals are the most common users of simulation learning. However, there is a paucity of literature addressing the use of simulation in LTC.
One study was conducted in 2002 by P.K. Beville called the Virtual Dementia Tour, a program using evidence-based simulation. Beville found that study participants using the simulation model had a heightened awareness of the challenges of confused elderly as well as unrealistic expectations by caregivers.3 Although the Virtual Dementia Tour is available for a fee for training professional caregivers, lay people, family, and first responders, many LTC facilities do not have sufficient funding for simulation and simulation equipment, and many do not have dedicated staff for nursing education. Most staff in LTC facilities are unlicensed and may not have had simulation training experience. Additionally, due to staffing and budget constraints, staff education may be limited.
This article will describe the successful implementation of a simulation-based quality improvement project created by and used at the Louis Stokes Cleveland VA Medical Center (LSCVAMC) LTC facility. The LSCVAMC has acute care beds and is adjacent to its LTC facility. Also, a previously successful simulation educational program to improve delirium care was conducted at this acute care hospital.4
Experiential Learning Opportunity
Many residents in a LTC facility have been diagnosed with dementia. As part of a cultural transformation at LSCVAMC, a simulation program was used to help sensitize LTC caregivers to the many sensory changes that occur in older veterans with dementia. The program was guided by the Kolb model.5
The Kolb model of experiential learning includes 4 elements: abstract conceptualization (knowledge), active experimentation (application), concrete experience (engagement), and reflective observation (self-evaluation).5 A simulation program can touch all 4 elements of the Kolb model by providing an educational experience for all learning styles as well as facilitating critical thinking. Nursing homes that provide care to residents with dementia are required to include dementia education annually to staff.6 Long-term care facilities can take advantage of using simulation education along with their traditional educational programs to provide staff with exposure to realistic resident care conditions.7
Methods
The simulation learning experience was provided to all nursing, recreation therapy, and rehabilitation services staff at the LTC facility. The goal was to create an affective, psychomotor learning experience that refreshed, reminded, and sensitized the staff to the challenges that many residents face. The LSCVAMC LTC leadership was supportive of this simulation model because it was not time intensive for direct care staff, and the materials needed were inexpensive. The only equipment that was purchased were several eyeglass readers, popcorn kernels, and Vaseline, resulting in a budget of about $10. The simulation program was scheduled on all shifts. In addition to the simulation experience, the model consists of pre- and postsurveys and a dementia review handout. Staff were able to complete a pre- and postsurvey as well as a debriefing all within a 30-minute time slot.
The pre- and posteducation surveys used were designed to measure learnings and provide data for future education planning. The surveys required only a yes/no and short answers. To reduce the total time of participants’ involvement in the simulation program, an online survey was used. Presurvey questions were designed to identify basic knowledge and experience with dementia, both at work and in personal life. The postsurvey questions sought to identify affective feelings about the participants experience as well as lessons learned and how that could impact future care.
The dementia review handout that was provided to staff 2 weeks before the simulation provided an overview of dementia. It included communication techniques and care planning suggestions.8 The time spent in the simulation room was about 10 to 15 minutes but depended on the activity. The total in-service time was about 30 minutes, depending on the time allotted for debriefing. Room choice was influenced by the number of participants performing the simulation at the same time. Activity stations/tables generally provided 1 experience at a time.
The room that was used had adjustable lighting with the ability to provide a low light setting. Activities were chosen based on the goals for the physical and cognitive disabilities to be simulated. Table 1 identifies equipment used with success and chosen with consideration for ease and expense in describing the disability.
Simulation activities were based on the staff learning needs determined by the presimulation survey. Simulated deficits impacted activities of daily living, mood, and cognition. Neuropathy, arthritis, paralysis, dementia, glaucoma, cataracts, and hearing loss are conditions that are easily represented in a simulation.
Participants also gained additional knowledge of dementia through the Kolb process, which was included in the debriefing. The survey followed the completion of the simulation session to identify knowledge deficits for general remediation and program development and expansion.
Discussion
During the dementia simulation, active experimentation or application learning may be counterintuitive. Staff do not apply their knowledge of dementia directly as in other education settings where they can practice or demonstrate a skill. Instead, participants experience care from the perspective of residents. This learning transitions well into reflective observation as the participants begin to understand the challenges of the cognitively impaired resident, which are manifested in the residents’ behaviors.
Debriefing and a postsimulation survey provide a guided reflection to assimilate new knowledge and revise presimulation attitudes about dementia.9 Reflective observation or self-evaluation is a learning activity that is not a routine part of staff education but can be a powerful learning tool. The postsimulation survey incorporated Bloom’s taxonomy: the affective domain of learning by challenging staff to organize their values with the experience and resolving in their mind any conflicts.10 The goal of the process is to help internalize the education by encouraging changes in behavior (in this case dementia care) and considering the new experience.
Survey Results
The 30-minute program allowed 155 staff to experience cognitive and physical impairment while completing tasks. The pre- and postsurveys were analyzed by 2 learning and dementia survey content experts. The survey questions were open-ended with the intention of eliciting affective behavior responses and staff could provide comments (See eTables 1 and 2 at www.mdedge.com/fedprac). All participants indicated they had knowledge of dementia before the simulation, but 70% acknowledged in the postsimulation survey that they did not have the dementia knowledge that they thought they had. Patience and understanding were most commonly reported in the reflective observation/affective domain (values are internalized leading to changes in behavior).
Participants also described success in closing the loop of experiential learning as a result of the simulation. Some participants verbalized experiencing emotional distress when they realized that their temporary, frustrating impairment was a permanent condition for the residents. Postexperience comments supported the success of the Kolb model experiential learning activity.
Conclusion
Dementia simulation can augment didactic education for improving the quality of dementia care. The virtual dementia simulation was an inexpensive educational program that did not adversely impact scheduling or patient care in a LTC facility. Care providers provided anecdotal feedback that suggested that the program increased their awareness of the difficulty of performing activities of daily living for patients with dementia. The simulation touched all 4 elements of the Kolb Model. The participants had gained new knowledge or reinforced existing knowledge. The simulation activities addressed the application and engagement parts of the model. Self-evaluation resulted from the debriefing time and postsurvey questions. The virtual dementia simulation will be repeated with additional debrief time and a long-term follow-up survey to identify additional learning needs and changes in professional practice.
Acknowledgments
The author thanks Nurse Educator Lisa Weber, MSN, RN-BC, for her contribution to the manuscript.
Enhancing patient-centered care is an important priority for caregivers in all settings but particularly in long-term care (LTC) where patients also are residents. Simulation is a potential strategy to effect cultural change for health care providers at LTC facilities. In a clinical setting, simulation is an educational model that allows staff to practice behaviors or skills without putting patients at risk. Due to limited time, staffing, and budget resources, the use of simulation for training is not common at LTC facilities.
Background
The simulation model is considered an effective teaching and learning strategy for replicating experiences in nursing practice.1,2 The interactive experience provides the learner with opportunities to engage with patients through psychomotor participation, critical thinking, reflection, and debriefing. Prelicensure nursing education programs and acute care hospitals are the most common users of simulation learning. However, there is a paucity of literature addressing the use of simulation in LTC.
One study was conducted in 2002 by P.K. Beville called the Virtual Dementia Tour, a program using evidence-based simulation. Beville found that study participants using the simulation model had a heightened awareness of the challenges of confused elderly as well as unrealistic expectations by caregivers.3 Although the Virtual Dementia Tour is available for a fee for training professional caregivers, lay people, family, and first responders, many LTC facilities do not have sufficient funding for simulation and simulation equipment, and many do not have dedicated staff for nursing education. Most staff in LTC facilities are unlicensed and may not have had simulation training experience. Additionally, due to staffing and budget constraints, staff education may be limited.
This article will describe the successful implementation of a simulation-based quality improvement project created by and used at the Louis Stokes Cleveland VA Medical Center (LSCVAMC) LTC facility. The LSCVAMC has acute care beds and is adjacent to its LTC facility. Also, a previously successful simulation educational program to improve delirium care was conducted at this acute care hospital.4
Experiential Learning Opportunity
Many residents in a LTC facility have been diagnosed with dementia. As part of a cultural transformation at LSCVAMC, a simulation program was used to help sensitize LTC caregivers to the many sensory changes that occur in older veterans with dementia. The program was guided by the Kolb model.5
The Kolb model of experiential learning includes 4 elements: abstract conceptualization (knowledge), active experimentation (application), concrete experience (engagement), and reflective observation (self-evaluation).5 A simulation program can touch all 4 elements of the Kolb model by providing an educational experience for all learning styles as well as facilitating critical thinking. Nursing homes that provide care to residents with dementia are required to include dementia education annually to staff.6 Long-term care facilities can take advantage of using simulation education along with their traditional educational programs to provide staff with exposure to realistic resident care conditions.7
Methods
The simulation learning experience was provided to all nursing, recreation therapy, and rehabilitation services staff at the LTC facility. The goal was to create an affective, psychomotor learning experience that refreshed, reminded, and sensitized the staff to the challenges that many residents face. The LSCVAMC LTC leadership was supportive of this simulation model because it was not time intensive for direct care staff, and the materials needed were inexpensive. The only equipment that was purchased were several eyeglass readers, popcorn kernels, and Vaseline, resulting in a budget of about $10. The simulation program was scheduled on all shifts. In addition to the simulation experience, the model consists of pre- and postsurveys and a dementia review handout. Staff were able to complete a pre- and postsurvey as well as a debriefing all within a 30-minute time slot.
The pre- and posteducation surveys used were designed to measure learnings and provide data for future education planning. The surveys required only a yes/no and short answers. To reduce the total time of participants’ involvement in the simulation program, an online survey was used. Presurvey questions were designed to identify basic knowledge and experience with dementia, both at work and in personal life. The postsurvey questions sought to identify affective feelings about the participants experience as well as lessons learned and how that could impact future care.
The dementia review handout that was provided to staff 2 weeks before the simulation provided an overview of dementia. It included communication techniques and care planning suggestions.8 The time spent in the simulation room was about 10 to 15 minutes but depended on the activity. The total in-service time was about 30 minutes, depending on the time allotted for debriefing. Room choice was influenced by the number of participants performing the simulation at the same time. Activity stations/tables generally provided 1 experience at a time.
The room that was used had adjustable lighting with the ability to provide a low light setting. Activities were chosen based on the goals for the physical and cognitive disabilities to be simulated. Table 1 identifies equipment used with success and chosen with consideration for ease and expense in describing the disability.
Simulation activities were based on the staff learning needs determined by the presimulation survey. Simulated deficits impacted activities of daily living, mood, and cognition. Neuropathy, arthritis, paralysis, dementia, glaucoma, cataracts, and hearing loss are conditions that are easily represented in a simulation.
Participants also gained additional knowledge of dementia through the Kolb process, which was included in the debriefing. The survey followed the completion of the simulation session to identify knowledge deficits for general remediation and program development and expansion.
Discussion
During the dementia simulation, active experimentation or application learning may be counterintuitive. Staff do not apply their knowledge of dementia directly as in other education settings where they can practice or demonstrate a skill. Instead, participants experience care from the perspective of residents. This learning transitions well into reflective observation as the participants begin to understand the challenges of the cognitively impaired resident, which are manifested in the residents’ behaviors.
Debriefing and a postsimulation survey provide a guided reflection to assimilate new knowledge and revise presimulation attitudes about dementia.9 Reflective observation or self-evaluation is a learning activity that is not a routine part of staff education but can be a powerful learning tool. The postsimulation survey incorporated Bloom’s taxonomy: the affective domain of learning by challenging staff to organize their values with the experience and resolving in their mind any conflicts.10 The goal of the process is to help internalize the education by encouraging changes in behavior (in this case dementia care) and considering the new experience.
Survey Results
The 30-minute program allowed 155 staff to experience cognitive and physical impairment while completing tasks. The pre- and postsurveys were analyzed by 2 learning and dementia survey content experts. The survey questions were open-ended with the intention of eliciting affective behavior responses and staff could provide comments (See eTables 1 and 2 at www.mdedge.com/fedprac). All participants indicated they had knowledge of dementia before the simulation, but 70% acknowledged in the postsimulation survey that they did not have the dementia knowledge that they thought they had. Patience and understanding were most commonly reported in the reflective observation/affective domain (values are internalized leading to changes in behavior).
Participants also described success in closing the loop of experiential learning as a result of the simulation. Some participants verbalized experiencing emotional distress when they realized that their temporary, frustrating impairment was a permanent condition for the residents. Postexperience comments supported the success of the Kolb model experiential learning activity.
Conclusion
Dementia simulation can augment didactic education for improving the quality of dementia care. The virtual dementia simulation was an inexpensive educational program that did not adversely impact scheduling or patient care in a LTC facility. Care providers provided anecdotal feedback that suggested that the program increased their awareness of the difficulty of performing activities of daily living for patients with dementia. The simulation touched all 4 elements of the Kolb Model. The participants had gained new knowledge or reinforced existing knowledge. The simulation activities addressed the application and engagement parts of the model. Self-evaluation resulted from the debriefing time and postsurvey questions. The virtual dementia simulation will be repeated with additional debrief time and a long-term follow-up survey to identify additional learning needs and changes in professional practice.
Acknowledgments
The author thanks Nurse Educator Lisa Weber, MSN, RN-BC, for her contribution to the manuscript.
1. Aebersold M, Tschannen D. Simulation in nursing practice: the impact on patient care. Online J Issues Nurs. 2013;18(2):6.
2. Mariani B, Doolen J. Nursing simulation research: what are the perceived gaps? Clin Simulation in Nurs. 2016;12(1):30-36.
3. Beville PK. Virtual Dementia Tour helps sensitize health care providers. Am J Alzheimers Dis Other Demen. 2002;17(3):183-190.
4. Kresevic D, Heath B, Fine-Smilovich E, et al. Simulation training, coaching, and cue cards improve delirium care. Fed Pract. 2016;33(12):22-28.
5. Chmil JV, Turk M, Adamson K, Larew C. Effects of an experiential learning simulation design on clinical nursing judgment development. Nurse Educ. 2015;40(5):228-232.
6. Centers for Medicare & Medicaid Services. Medicare and Medicaid programs; reform of requirements for long-term care facilities, final rule. https://www.federalregister.gov/documents/2016/10/04/2016-23503/medicare-and-medicaid-programs-reform-of-requirements-for-long-term-care-facilities. Published October 4, 2016. Accessed May 22, 2018.
7. Donahoe J, Moon L, VanCleave K. Increasing student empathy toward older adults using the virtual dementia tour. J Baccalaureate Soc Work. 2014;19(1):S23-S40.
8. Coggins MD. Behavioral expressions in dementia patients. http://www.todaysgeriatricmedicine.com/archive/0115p6.shtml. Published 2015. Accessed May 10, 2018.
9. Al Sabei SD, Lasater K. Simulation debriefing for clinical judgment development: a concept analysis. Nurse Educ Today. 2016;45:42-47.
10. Anderson LW, Krathwohl DR, Bloom BS, eds. A Taxonomy for Learning, Teaching, and Assessing: A revision of Bloom’s Taxonomy of Educational Objectives. New York: Longman; 2001.
1. Aebersold M, Tschannen D. Simulation in nursing practice: the impact on patient care. Online J Issues Nurs. 2013;18(2):6.
2. Mariani B, Doolen J. Nursing simulation research: what are the perceived gaps? Clin Simulation in Nurs. 2016;12(1):30-36.
3. Beville PK. Virtual Dementia Tour helps sensitize health care providers. Am J Alzheimers Dis Other Demen. 2002;17(3):183-190.
4. Kresevic D, Heath B, Fine-Smilovich E, et al. Simulation training, coaching, and cue cards improve delirium care. Fed Pract. 2016;33(12):22-28.
5. Chmil JV, Turk M, Adamson K, Larew C. Effects of an experiential learning simulation design on clinical nursing judgment development. Nurse Educ. 2015;40(5):228-232.
6. Centers for Medicare & Medicaid Services. Medicare and Medicaid programs; reform of requirements for long-term care facilities, final rule. https://www.federalregister.gov/documents/2016/10/04/2016-23503/medicare-and-medicaid-programs-reform-of-requirements-for-long-term-care-facilities. Published October 4, 2016. Accessed May 22, 2018.
7. Donahoe J, Moon L, VanCleave K. Increasing student empathy toward older adults using the virtual dementia tour. J Baccalaureate Soc Work. 2014;19(1):S23-S40.
8. Coggins MD. Behavioral expressions in dementia patients. http://www.todaysgeriatricmedicine.com/archive/0115p6.shtml. Published 2015. Accessed May 10, 2018.
9. Al Sabei SD, Lasater K. Simulation debriefing for clinical judgment development: a concept analysis. Nurse Educ Today. 2016;45:42-47.
10. Anderson LW, Krathwohl DR, Bloom BS, eds. A Taxonomy for Learning, Teaching, and Assessing: A revision of Bloom’s Taxonomy of Educational Objectives. New York: Longman; 2001.