User login
Patient-centric pain management decision aid reduces opioid use posthysterectomy
Investigators at the University of Michigan, Ann Arbor, found that a simple patient decision aid can be a useful tool in providing adequate postsurgical pain control to patients while reducing the number of opioid tablets in the community. The shared decision-making aid focuses on educating the patient about opioid use and engages her in an appropriate postoperative pain management plan. Results from this prospective quality improvement study were presented in a poster at the 47th AAGL Global Congress on Minimally Invasive Gynecology (Las Vegas, Nevada, November 11–15, 2018).1
Annmarie Vilkins, DO, and colleagues’ aim was to evaluate the impact of shared decision-making through the use of a patient decision aid targeting posthysterectomy pain management and opioid use. Can such a targeted strategy help decrease posthysterectomy opioid distribution in the community without compromising patient pain control or satisfaction?
The authors noted that more than 46 people die each day from an overdose involving prescription opioids.2 Studies have shown that patients actually use significantly fewer opioid tablets than the amount clinicians generally prescribe following ObGyn surgeries.3,4 Unused prescription opioid availability has the potential for accidental use or intentional misuse of the unneeded drugs by others.
Study methods
The investigators included all English-speaking patients undergoing hysterectomy for benign disease at their institution from March 1 through July 31, 2018. Data were analyzed from women undergoing laparoscopic, vaginal, or abdominal hysterectomy before (n = 195) and after (n = 177) the decision aid was implemented.
Preoperative education. In the preoperative area, patients were uniformly educated regarding postoperative pain expectations (for example, it is normal to have some pain; the goal is to manage your pain so you can function; some women do not require opioid medications after surgery), risks of opioid medications (such as dependence or addiction; misuse of leftover pills by others), adverse effects (drowsiness; confusion), and the recommended postoperative pain management schedule.
Postoperatively, pain medications included ibuprofen around the clock, acetaminophen as needed (used with caution when hydrocodone with acetaminophen was also prescribed), and opioids only if needed.
Discharge medication planning. Using a visual scale, the investigators then educated patients regarding the maximum number of opioid tablets permitted to be prescribed according to department guidelines and the average number of opioid tablets that a typical patient uses. The number of opioid tablets prescribed varied based on route of hysterectomy (laparoscopic, abdominal, or vaginal). For example, for a laparoscopic hysterectomy, the maximum allowed prescription for oxycodone was 20 tablets, while patients used an average number of 10 tablets.
The patient was then asked to choose her desired number of tablets with which she would like to be discharged.
Structured telephone calls were made to patients 2 weeks postoperatively.
Impact of the decision aid on opioid prescribing
Before implementation of the decision aid, the average number of opioid pills prescribed at discharge was 25 (median, 20–35), while that number dropped to 10 (median, 10–15) after the aid’s implementation. Similarly, the average oral morphine equivalents (OMEs) at time of discharge was 150 (interquartile range [IQR], 120–200) before decision aid implementation and 75 (IQR, 25–150) after decision aid implementation. Similar reductions in average OMEs were observed before and after the aid’s implementation across the 3 hysterectomy routes.
Continue to: According to the type of opioid...
According to the type of opioid prescribed at discharge, hydrocodone 5 mg was prescribed in 99 cases (50.8%) before decision aid implementation and in 14 cases (7.9%) after implementation. By contrast, oxycodone 5 mg was prescribed in 85 cases (43.6%) before implementation and in 149 cases (84.2%) after implementation.
The number of refill requests was similar before (n = 11 [5.6%]) and after (n = 12 [6.8%]) the aid’s implementation.
Tool reduced opioid availability in the community
The use of a simple patient decision aid—which focuses on opioid education and engages patients in an appropriate postoperative pain management plan—can result in fewer opioid tablets in the community while still providing adequate pain control, the authors concluded.
Online resource. For more on targeted strategies to optimize opioid prescribing after surgery, visit the University of Michigan’s Opioid Prescribing Engagement Network (OPEN) at http://michigan-open.org.
- Vilkins A, Till S, Lim R, et al. The impact of shared decision making on post-hysterectomy opioid prescribing. Poster presented at: 47th AAGL Global Congress on Minimally Invasive Gynecology; November 11-15, 2018; Las Vegas, NV.
- Seth P, Scholl L, Rudd RA, et al. Overdose deaths involving opioids, cocaine, and psychostimulants—United States, 2015–2016. MMWR Morb Mortal Wkly Rep. 2018;67:349-358.
- Bateman BT, Cole NM, Maeda A, et al. Patterns of opioid prescription and use after cesarean delivery. Obstet Gynecol. 2017;130:29-35.
- As-Sanie S, Till S, Mowers EL, et al. Opioid prescribing patterns, patient use, and postoperative pain after hysterectomy for benign indications. Obstet Gynecol. 2017;130:1261-1268.
Investigators at the University of Michigan, Ann Arbor, found that a simple patient decision aid can be a useful tool in providing adequate postsurgical pain control to patients while reducing the number of opioid tablets in the community. The shared decision-making aid focuses on educating the patient about opioid use and engages her in an appropriate postoperative pain management plan. Results from this prospective quality improvement study were presented in a poster at the 47th AAGL Global Congress on Minimally Invasive Gynecology (Las Vegas, Nevada, November 11–15, 2018).1
Annmarie Vilkins, DO, and colleagues’ aim was to evaluate the impact of shared decision-making through the use of a patient decision aid targeting posthysterectomy pain management and opioid use. Can such a targeted strategy help decrease posthysterectomy opioid distribution in the community without compromising patient pain control or satisfaction?
The authors noted that more than 46 people die each day from an overdose involving prescription opioids.2 Studies have shown that patients actually use significantly fewer opioid tablets than the amount clinicians generally prescribe following ObGyn surgeries.3,4 Unused prescription opioid availability has the potential for accidental use or intentional misuse of the unneeded drugs by others.
Study methods
The investigators included all English-speaking patients undergoing hysterectomy for benign disease at their institution from March 1 through July 31, 2018. Data were analyzed from women undergoing laparoscopic, vaginal, or abdominal hysterectomy before (n = 195) and after (n = 177) the decision aid was implemented.
Preoperative education. In the preoperative area, patients were uniformly educated regarding postoperative pain expectations (for example, it is normal to have some pain; the goal is to manage your pain so you can function; some women do not require opioid medications after surgery), risks of opioid medications (such as dependence or addiction; misuse of leftover pills by others), adverse effects (drowsiness; confusion), and the recommended postoperative pain management schedule.
Postoperatively, pain medications included ibuprofen around the clock, acetaminophen as needed (used with caution when hydrocodone with acetaminophen was also prescribed), and opioids only if needed.
Discharge medication planning. Using a visual scale, the investigators then educated patients regarding the maximum number of opioid tablets permitted to be prescribed according to department guidelines and the average number of opioid tablets that a typical patient uses. The number of opioid tablets prescribed varied based on route of hysterectomy (laparoscopic, abdominal, or vaginal). For example, for a laparoscopic hysterectomy, the maximum allowed prescription for oxycodone was 20 tablets, while patients used an average number of 10 tablets.
The patient was then asked to choose her desired number of tablets with which she would like to be discharged.
Structured telephone calls were made to patients 2 weeks postoperatively.
Impact of the decision aid on opioid prescribing
Before implementation of the decision aid, the average number of opioid pills prescribed at discharge was 25 (median, 20–35), while that number dropped to 10 (median, 10–15) after the aid’s implementation. Similarly, the average oral morphine equivalents (OMEs) at time of discharge was 150 (interquartile range [IQR], 120–200) before decision aid implementation and 75 (IQR, 25–150) after decision aid implementation. Similar reductions in average OMEs were observed before and after the aid’s implementation across the 3 hysterectomy routes.
Continue to: According to the type of opioid...
According to the type of opioid prescribed at discharge, hydrocodone 5 mg was prescribed in 99 cases (50.8%) before decision aid implementation and in 14 cases (7.9%) after implementation. By contrast, oxycodone 5 mg was prescribed in 85 cases (43.6%) before implementation and in 149 cases (84.2%) after implementation.
The number of refill requests was similar before (n = 11 [5.6%]) and after (n = 12 [6.8%]) the aid’s implementation.
Tool reduced opioid availability in the community
The use of a simple patient decision aid—which focuses on opioid education and engages patients in an appropriate postoperative pain management plan—can result in fewer opioid tablets in the community while still providing adequate pain control, the authors concluded.
Online resource. For more on targeted strategies to optimize opioid prescribing after surgery, visit the University of Michigan’s Opioid Prescribing Engagement Network (OPEN) at http://michigan-open.org.
Investigators at the University of Michigan, Ann Arbor, found that a simple patient decision aid can be a useful tool in providing adequate postsurgical pain control to patients while reducing the number of opioid tablets in the community. The shared decision-making aid focuses on educating the patient about opioid use and engages her in an appropriate postoperative pain management plan. Results from this prospective quality improvement study were presented in a poster at the 47th AAGL Global Congress on Minimally Invasive Gynecology (Las Vegas, Nevada, November 11–15, 2018).1
Annmarie Vilkins, DO, and colleagues’ aim was to evaluate the impact of shared decision-making through the use of a patient decision aid targeting posthysterectomy pain management and opioid use. Can such a targeted strategy help decrease posthysterectomy opioid distribution in the community without compromising patient pain control or satisfaction?
The authors noted that more than 46 people die each day from an overdose involving prescription opioids.2 Studies have shown that patients actually use significantly fewer opioid tablets than the amount clinicians generally prescribe following ObGyn surgeries.3,4 Unused prescription opioid availability has the potential for accidental use or intentional misuse of the unneeded drugs by others.
Study methods
The investigators included all English-speaking patients undergoing hysterectomy for benign disease at their institution from March 1 through July 31, 2018. Data were analyzed from women undergoing laparoscopic, vaginal, or abdominal hysterectomy before (n = 195) and after (n = 177) the decision aid was implemented.
Preoperative education. In the preoperative area, patients were uniformly educated regarding postoperative pain expectations (for example, it is normal to have some pain; the goal is to manage your pain so you can function; some women do not require opioid medications after surgery), risks of opioid medications (such as dependence or addiction; misuse of leftover pills by others), adverse effects (drowsiness; confusion), and the recommended postoperative pain management schedule.
Postoperatively, pain medications included ibuprofen around the clock, acetaminophen as needed (used with caution when hydrocodone with acetaminophen was also prescribed), and opioids only if needed.
Discharge medication planning. Using a visual scale, the investigators then educated patients regarding the maximum number of opioid tablets permitted to be prescribed according to department guidelines and the average number of opioid tablets that a typical patient uses. The number of opioid tablets prescribed varied based on route of hysterectomy (laparoscopic, abdominal, or vaginal). For example, for a laparoscopic hysterectomy, the maximum allowed prescription for oxycodone was 20 tablets, while patients used an average number of 10 tablets.
The patient was then asked to choose her desired number of tablets with which she would like to be discharged.
Structured telephone calls were made to patients 2 weeks postoperatively.
Impact of the decision aid on opioid prescribing
Before implementation of the decision aid, the average number of opioid pills prescribed at discharge was 25 (median, 20–35), while that number dropped to 10 (median, 10–15) after the aid’s implementation. Similarly, the average oral morphine equivalents (OMEs) at time of discharge was 150 (interquartile range [IQR], 120–200) before decision aid implementation and 75 (IQR, 25–150) after decision aid implementation. Similar reductions in average OMEs were observed before and after the aid’s implementation across the 3 hysterectomy routes.
Continue to: According to the type of opioid...
According to the type of opioid prescribed at discharge, hydrocodone 5 mg was prescribed in 99 cases (50.8%) before decision aid implementation and in 14 cases (7.9%) after implementation. By contrast, oxycodone 5 mg was prescribed in 85 cases (43.6%) before implementation and in 149 cases (84.2%) after implementation.
The number of refill requests was similar before (n = 11 [5.6%]) and after (n = 12 [6.8%]) the aid’s implementation.
Tool reduced opioid availability in the community
The use of a simple patient decision aid—which focuses on opioid education and engages patients in an appropriate postoperative pain management plan—can result in fewer opioid tablets in the community while still providing adequate pain control, the authors concluded.
Online resource. For more on targeted strategies to optimize opioid prescribing after surgery, visit the University of Michigan’s Opioid Prescribing Engagement Network (OPEN) at http://michigan-open.org.
- Vilkins A, Till S, Lim R, et al. The impact of shared decision making on post-hysterectomy opioid prescribing. Poster presented at: 47th AAGL Global Congress on Minimally Invasive Gynecology; November 11-15, 2018; Las Vegas, NV.
- Seth P, Scholl L, Rudd RA, et al. Overdose deaths involving opioids, cocaine, and psychostimulants—United States, 2015–2016. MMWR Morb Mortal Wkly Rep. 2018;67:349-358.
- Bateman BT, Cole NM, Maeda A, et al. Patterns of opioid prescription and use after cesarean delivery. Obstet Gynecol. 2017;130:29-35.
- As-Sanie S, Till S, Mowers EL, et al. Opioid prescribing patterns, patient use, and postoperative pain after hysterectomy for benign indications. Obstet Gynecol. 2017;130:1261-1268.
- Vilkins A, Till S, Lim R, et al. The impact of shared decision making on post-hysterectomy opioid prescribing. Poster presented at: 47th AAGL Global Congress on Minimally Invasive Gynecology; November 11-15, 2018; Las Vegas, NV.
- Seth P, Scholl L, Rudd RA, et al. Overdose deaths involving opioids, cocaine, and psychostimulants—United States, 2015–2016. MMWR Morb Mortal Wkly Rep. 2018;67:349-358.
- Bateman BT, Cole NM, Maeda A, et al. Patterns of opioid prescription and use after cesarean delivery. Obstet Gynecol. 2017;130:29-35.
- As-Sanie S, Till S, Mowers EL, et al. Opioid prescribing patterns, patient use, and postoperative pain after hysterectomy for benign indications. Obstet Gynecol. 2017;130:1261-1268.
Making a difference: ACOG’s guidance on low-dose aspirin for preventing superimposed preeclampsia
Investigators at Thomas Jefferson University found that low-dose aspirin therapy in pregnant women with chronic hypertension—as recommended by the American College of Obstetricians and Gynecologists (ACOG) in 20161—was associated with a 57% decrease in superimposed preeclampsia. Chaitra Banala, BS, presented the study’s results in a poster presentation at the ACOG 2018 annual meeting (April 27–30, 2018, Austin, Texas).2
The study’s goal was to evaluate the incidence of superimposed preeclampsia in women with chronic hypertension in the periods before and after the ACOG recommendation was published.
Study participants. Pregnant women with chronic hypertension who delivered at Thomas Jefferson University Hospital from January 2008 to July 2017 were included in this retrospective cohort study. Women with multiple gestations were excluded.
The cohort included 715 pregnant patients with chronic hypertension divided into 2 groups: 635 pre-ACOG patients and 80 post-ACOG patients (that is, patients who delivered before and after the ACOG recommendation). The investigators offered daily low-dose (81 mg) aspirin.
The cohort was further stratified by additional risk factors for superimposed preeclampsia, including a history of preeclampsia and pregestational diabetes.
Outcomes. The primary outcome was the incidence of superimposed preeclampsia. Secondary outcomes included the incidence of superimposed preeclampsia with severe features (SIPSF), small for gestational age, and preterm birth.
Findings. The incidence of superimposed preeclampsia in women with chronic hypertension was 20 (25%) in the post-ACOG group versus 232 (37%) in the pre-ACOG group (odds ratio [OR], 0.43; 95% confidence interval [CI], 0.26–0.73).
In the subgroup of women with chronic hypertension who did not have other risk factors, superimposed preeclampsia and SIPSF were significantly decreased: 4/41 (10%) versus 106/355 (30%) (OR, 0.25 [95% CI, 0.08–0.73]) and 2/41 (5%) versus 65/355 (18%) (OR, 0.22 [95% CI, 0.54–0.97]), respectively. The maternal demographics and secondary outcomes did not differ significantly.
After the ACOG guidance was released, low-dose aspirin decreased superimposed preeclampsia by 57% in all women with chronic hypertension. Of those with chronic hypertension without other risk factors, there were decreases of 75% in superimposed preeclampsia and 78% in SIPSF.
Final thoughts. Ms. Banala said in an interview with OBG Management following her presentation, “When we stratified the cohort based on their risk factors, we found that aspirin had the highest benefit in patients with only chronic hypertension, so without other risk factors. And we found that there was a benefit in patients with chronic hypertension who were not on antihypertensive medication. So overall our study concluded that this guideline has made a significant impact in decreasing the frequency of superimposed preeclampsia.”
Share your thoughts! Send your Letter to the Editor to [email protected]. Please include your name and the city and state in which you practice.
- American College of Obstetricians and Gynecologists. Practice advisory on low-dose aspirin and prevention of preeclampsia: updated recommendations. https://www.acog.org/Clinical-Guidance-and-Publications/Practice-Advisories/Practice-Advisory-Low-Dose-Aspirin-and-Prevention-of-Preeclampsia-Updated-Recommendations. Published July 11, 2016. Accessed May 3, 2018.
- Banala C, Cruz Y, Moreno C, Schoen C, Berghella V, Roman A. Impact of ACOG guideline regarding low dose aspirin for prevention of superimposed preeclampsia [abstract 27O]. Obstet Gynecol. 2018;131(suppl 1):170S.
Investigators at Thomas Jefferson University found that low-dose aspirin therapy in pregnant women with chronic hypertension—as recommended by the American College of Obstetricians and Gynecologists (ACOG) in 20161—was associated with a 57% decrease in superimposed preeclampsia. Chaitra Banala, BS, presented the study’s results in a poster presentation at the ACOG 2018 annual meeting (April 27–30, 2018, Austin, Texas).2
The study’s goal was to evaluate the incidence of superimposed preeclampsia in women with chronic hypertension in the periods before and after the ACOG recommendation was published.
Study participants. Pregnant women with chronic hypertension who delivered at Thomas Jefferson University Hospital from January 2008 to July 2017 were included in this retrospective cohort study. Women with multiple gestations were excluded.
The cohort included 715 pregnant patients with chronic hypertension divided into 2 groups: 635 pre-ACOG patients and 80 post-ACOG patients (that is, patients who delivered before and after the ACOG recommendation). The investigators offered daily low-dose (81 mg) aspirin.
The cohort was further stratified by additional risk factors for superimposed preeclampsia, including a history of preeclampsia and pregestational diabetes.
Outcomes. The primary outcome was the incidence of superimposed preeclampsia. Secondary outcomes included the incidence of superimposed preeclampsia with severe features (SIPSF), small for gestational age, and preterm birth.
Findings. The incidence of superimposed preeclampsia in women with chronic hypertension was 20 (25%) in the post-ACOG group versus 232 (37%) in the pre-ACOG group (odds ratio [OR], 0.43; 95% confidence interval [CI], 0.26–0.73).
In the subgroup of women with chronic hypertension who did not have other risk factors, superimposed preeclampsia and SIPSF were significantly decreased: 4/41 (10%) versus 106/355 (30%) (OR, 0.25 [95% CI, 0.08–0.73]) and 2/41 (5%) versus 65/355 (18%) (OR, 0.22 [95% CI, 0.54–0.97]), respectively. The maternal demographics and secondary outcomes did not differ significantly.
After the ACOG guidance was released, low-dose aspirin decreased superimposed preeclampsia by 57% in all women with chronic hypertension. Of those with chronic hypertension without other risk factors, there were decreases of 75% in superimposed preeclampsia and 78% in SIPSF.
Final thoughts. Ms. Banala said in an interview with OBG Management following her presentation, “When we stratified the cohort based on their risk factors, we found that aspirin had the highest benefit in patients with only chronic hypertension, so without other risk factors. And we found that there was a benefit in patients with chronic hypertension who were not on antihypertensive medication. So overall our study concluded that this guideline has made a significant impact in decreasing the frequency of superimposed preeclampsia.”
Share your thoughts! Send your Letter to the Editor to [email protected]. Please include your name and the city and state in which you practice.
Investigators at Thomas Jefferson University found that low-dose aspirin therapy in pregnant women with chronic hypertension—as recommended by the American College of Obstetricians and Gynecologists (ACOG) in 20161—was associated with a 57% decrease in superimposed preeclampsia. Chaitra Banala, BS, presented the study’s results in a poster presentation at the ACOG 2018 annual meeting (April 27–30, 2018, Austin, Texas).2
The study’s goal was to evaluate the incidence of superimposed preeclampsia in women with chronic hypertension in the periods before and after the ACOG recommendation was published.
Study participants. Pregnant women with chronic hypertension who delivered at Thomas Jefferson University Hospital from January 2008 to July 2017 were included in this retrospective cohort study. Women with multiple gestations were excluded.
The cohort included 715 pregnant patients with chronic hypertension divided into 2 groups: 635 pre-ACOG patients and 80 post-ACOG patients (that is, patients who delivered before and after the ACOG recommendation). The investigators offered daily low-dose (81 mg) aspirin.
The cohort was further stratified by additional risk factors for superimposed preeclampsia, including a history of preeclampsia and pregestational diabetes.
Outcomes. The primary outcome was the incidence of superimposed preeclampsia. Secondary outcomes included the incidence of superimposed preeclampsia with severe features (SIPSF), small for gestational age, and preterm birth.
Findings. The incidence of superimposed preeclampsia in women with chronic hypertension was 20 (25%) in the post-ACOG group versus 232 (37%) in the pre-ACOG group (odds ratio [OR], 0.43; 95% confidence interval [CI], 0.26–0.73).
In the subgroup of women with chronic hypertension who did not have other risk factors, superimposed preeclampsia and SIPSF were significantly decreased: 4/41 (10%) versus 106/355 (30%) (OR, 0.25 [95% CI, 0.08–0.73]) and 2/41 (5%) versus 65/355 (18%) (OR, 0.22 [95% CI, 0.54–0.97]), respectively. The maternal demographics and secondary outcomes did not differ significantly.
After the ACOG guidance was released, low-dose aspirin decreased superimposed preeclampsia by 57% in all women with chronic hypertension. Of those with chronic hypertension without other risk factors, there were decreases of 75% in superimposed preeclampsia and 78% in SIPSF.
Final thoughts. Ms. Banala said in an interview with OBG Management following her presentation, “When we stratified the cohort based on their risk factors, we found that aspirin had the highest benefit in patients with only chronic hypertension, so without other risk factors. And we found that there was a benefit in patients with chronic hypertension who were not on antihypertensive medication. So overall our study concluded that this guideline has made a significant impact in decreasing the frequency of superimposed preeclampsia.”
Share your thoughts! Send your Letter to the Editor to [email protected]. Please include your name and the city and state in which you practice.
- American College of Obstetricians and Gynecologists. Practice advisory on low-dose aspirin and prevention of preeclampsia: updated recommendations. https://www.acog.org/Clinical-Guidance-and-Publications/Practice-Advisories/Practice-Advisory-Low-Dose-Aspirin-and-Prevention-of-Preeclampsia-Updated-Recommendations. Published July 11, 2016. Accessed May 3, 2018.
- Banala C, Cruz Y, Moreno C, Schoen C, Berghella V, Roman A. Impact of ACOG guideline regarding low dose aspirin for prevention of superimposed preeclampsia [abstract 27O]. Obstet Gynecol. 2018;131(suppl 1):170S.
- American College of Obstetricians and Gynecologists. Practice advisory on low-dose aspirin and prevention of preeclampsia: updated recommendations. https://www.acog.org/Clinical-Guidance-and-Publications/Practice-Advisories/Practice-Advisory-Low-Dose-Aspirin-and-Prevention-of-Preeclampsia-Updated-Recommendations. Published July 11, 2016. Accessed May 3, 2018.
- Banala C, Cruz Y, Moreno C, Schoen C, Berghella V, Roman A. Impact of ACOG guideline regarding low dose aspirin for prevention of superimposed preeclampsia [abstract 27O]. Obstet Gynecol. 2018;131(suppl 1):170S.
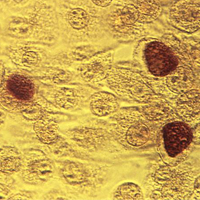
Chlamydia infection: Common, and consequential to women's health
Dispensing hormonal contraceptives in 1-year supplies saves state $43 million and avoids 15,000 unintended pregnancies
Recent insurance coverage legislation enacted in California is expected to result in 15,000 fewer unintended pregnancies, 2,000 fewer miscarriages, and 7,000 fewer abortions, according to an analysis of the mandate’s potential impact by investigators at the University of California.1
Enacted in September 2016, the contraceptive supply legislation known as SB 999 requires health plans and insurers to cover a year-long supply of hormonal contraceptive pills, patches, and rings (formulations approved by the US Food and Drug Administration). Clinicians can now prescribe and pharmacists can dispense up to a 12-month supply at one time. California joins 5 other states and Washington, DC, that have such mandates.
Having a year’s worth of contraceptives on hand is anticipated to reduce the interruption in contraception use that may occur with a 30- or 90-day supply that needs frequent refilling and thereby lower the unplanned pregnancy rate as well as associated health care costs.
Understanding the legislation’s impact on the population’s health outcomes will be useful for other states considering similar proposed legislation.
Details of the study
In a short communication published in Contraception, McMenamin and colleagues described how University of California faculty and researchers, engaged by the California Health Benefits Review Program, assessed the utilization and cost implications of SB 999 and arrived at their estimated projections.1
The assessment was based on a literature review (including current use of hormonal contraceptives, unintended pregnancy rates among contraceptive users, and assumptions about shifts in dispensing patterns for contraceptive supplies), a survey of the state’s 5 largest health insurance providers, and a claims database review of the utilization and cost implications of SB 999.
Two scenarios. Projections for the use and costs of hormonal contraceptives were made for 2 situations: whether SB 999 was enacted into law or not. Approximately 25 million Californians would be affected by the legislation, including 744,000 who used hormonal contraceptives in 2016.
To calculate their projections, the researchers used a baseline estimate of a 9% unintended pregnancy rate among current users of hormonal contraceptives (or 67,000 unintended pregnancies leading to 28,000 live births, 9,000 miscarriages, and 30,000 abortions).2 They also used a previously reported 30% reduction in the odds of unintended pregnancy with 12-month dispensing.3
Impact of shift in dispensing patterns
With SB 999 versus without SB 999, a 30% reduction in the odds of unintended pregnancies would lead to 6,000 fewer live births, 2,000 fewer miscarriages, and 7,000 fewer abortions.
The legislation would also reduce projected health care expenditures. Total net health care costs would decrease by 0.03%, for a savings of about $43 million, due to avoidance of unintended pregnancies and related medical costs.
Benefits will be even greater over time
The authors noted that the reductions in unintended pregnancies and associated health care costs with the implementation of SB 999 may be even greater in later years as beneficial health outcomes and cost savings accrue over time.
This study’s findings provide support for the implementation of similar legislation in other states.
- McMenamin SB, Charles SA, Tabatabaeepour N, Shigekawa E, Corbett G. Implications of dispensing self-administered hormonal contraceptives in a 1-year supply: a California case study. Contraception. 2017;95(5):449–451.
- Trussel J. Contraceptive failure in the United States. Contraception. 2011;83(5):397–404.
- Foster DG, Hulett D, Bradsberry M, Darney P, Policar M. Number of oral contraceptive pill packages dispensed and subsequent unintended pregnancies. Obstet Gynecol. 2011;117(3):566–572.
Recent insurance coverage legislation enacted in California is expected to result in 15,000 fewer unintended pregnancies, 2,000 fewer miscarriages, and 7,000 fewer abortions, according to an analysis of the mandate’s potential impact by investigators at the University of California.1
Enacted in September 2016, the contraceptive supply legislation known as SB 999 requires health plans and insurers to cover a year-long supply of hormonal contraceptive pills, patches, and rings (formulations approved by the US Food and Drug Administration). Clinicians can now prescribe and pharmacists can dispense up to a 12-month supply at one time. California joins 5 other states and Washington, DC, that have such mandates.
Having a year’s worth of contraceptives on hand is anticipated to reduce the interruption in contraception use that may occur with a 30- or 90-day supply that needs frequent refilling and thereby lower the unplanned pregnancy rate as well as associated health care costs.
Understanding the legislation’s impact on the population’s health outcomes will be useful for other states considering similar proposed legislation.
Details of the study
In a short communication published in Contraception, McMenamin and colleagues described how University of California faculty and researchers, engaged by the California Health Benefits Review Program, assessed the utilization and cost implications of SB 999 and arrived at their estimated projections.1
The assessment was based on a literature review (including current use of hormonal contraceptives, unintended pregnancy rates among contraceptive users, and assumptions about shifts in dispensing patterns for contraceptive supplies), a survey of the state’s 5 largest health insurance providers, and a claims database review of the utilization and cost implications of SB 999.
Two scenarios. Projections for the use and costs of hormonal contraceptives were made for 2 situations: whether SB 999 was enacted into law or not. Approximately 25 million Californians would be affected by the legislation, including 744,000 who used hormonal contraceptives in 2016.
To calculate their projections, the researchers used a baseline estimate of a 9% unintended pregnancy rate among current users of hormonal contraceptives (or 67,000 unintended pregnancies leading to 28,000 live births, 9,000 miscarriages, and 30,000 abortions).2 They also used a previously reported 30% reduction in the odds of unintended pregnancy with 12-month dispensing.3
Impact of shift in dispensing patterns
With SB 999 versus without SB 999, a 30% reduction in the odds of unintended pregnancies would lead to 6,000 fewer live births, 2,000 fewer miscarriages, and 7,000 fewer abortions.
The legislation would also reduce projected health care expenditures. Total net health care costs would decrease by 0.03%, for a savings of about $43 million, due to avoidance of unintended pregnancies and related medical costs.
Benefits will be even greater over time
The authors noted that the reductions in unintended pregnancies and associated health care costs with the implementation of SB 999 may be even greater in later years as beneficial health outcomes and cost savings accrue over time.
This study’s findings provide support for the implementation of similar legislation in other states.
Recent insurance coverage legislation enacted in California is expected to result in 15,000 fewer unintended pregnancies, 2,000 fewer miscarriages, and 7,000 fewer abortions, according to an analysis of the mandate’s potential impact by investigators at the University of California.1
Enacted in September 2016, the contraceptive supply legislation known as SB 999 requires health plans and insurers to cover a year-long supply of hormonal contraceptive pills, patches, and rings (formulations approved by the US Food and Drug Administration). Clinicians can now prescribe and pharmacists can dispense up to a 12-month supply at one time. California joins 5 other states and Washington, DC, that have such mandates.
Having a year’s worth of contraceptives on hand is anticipated to reduce the interruption in contraception use that may occur with a 30- or 90-day supply that needs frequent refilling and thereby lower the unplanned pregnancy rate as well as associated health care costs.
Understanding the legislation’s impact on the population’s health outcomes will be useful for other states considering similar proposed legislation.
Details of the study
In a short communication published in Contraception, McMenamin and colleagues described how University of California faculty and researchers, engaged by the California Health Benefits Review Program, assessed the utilization and cost implications of SB 999 and arrived at their estimated projections.1
The assessment was based on a literature review (including current use of hormonal contraceptives, unintended pregnancy rates among contraceptive users, and assumptions about shifts in dispensing patterns for contraceptive supplies), a survey of the state’s 5 largest health insurance providers, and a claims database review of the utilization and cost implications of SB 999.
Two scenarios. Projections for the use and costs of hormonal contraceptives were made for 2 situations: whether SB 999 was enacted into law or not. Approximately 25 million Californians would be affected by the legislation, including 744,000 who used hormonal contraceptives in 2016.
To calculate their projections, the researchers used a baseline estimate of a 9% unintended pregnancy rate among current users of hormonal contraceptives (or 67,000 unintended pregnancies leading to 28,000 live births, 9,000 miscarriages, and 30,000 abortions).2 They also used a previously reported 30% reduction in the odds of unintended pregnancy with 12-month dispensing.3
Impact of shift in dispensing patterns
With SB 999 versus without SB 999, a 30% reduction in the odds of unintended pregnancies would lead to 6,000 fewer live births, 2,000 fewer miscarriages, and 7,000 fewer abortions.
The legislation would also reduce projected health care expenditures. Total net health care costs would decrease by 0.03%, for a savings of about $43 million, due to avoidance of unintended pregnancies and related medical costs.
Benefits will be even greater over time
The authors noted that the reductions in unintended pregnancies and associated health care costs with the implementation of SB 999 may be even greater in later years as beneficial health outcomes and cost savings accrue over time.
This study’s findings provide support for the implementation of similar legislation in other states.
- McMenamin SB, Charles SA, Tabatabaeepour N, Shigekawa E, Corbett G. Implications of dispensing self-administered hormonal contraceptives in a 1-year supply: a California case study. Contraception. 2017;95(5):449–451.
- Trussel J. Contraceptive failure in the United States. Contraception. 2011;83(5):397–404.
- Foster DG, Hulett D, Bradsberry M, Darney P, Policar M. Number of oral contraceptive pill packages dispensed and subsequent unintended pregnancies. Obstet Gynecol. 2011;117(3):566–572.
- McMenamin SB, Charles SA, Tabatabaeepour N, Shigekawa E, Corbett G. Implications of dispensing self-administered hormonal contraceptives in a 1-year supply: a California case study. Contraception. 2017;95(5):449–451.
- Trussel J. Contraceptive failure in the United States. Contraception. 2011;83(5):397–404.
- Foster DG, Hulett D, Bradsberry M, Darney P, Policar M. Number of oral contraceptive pill packages dispensed and subsequent unintended pregnancies. Obstet Gynecol. 2011;117(3):566–572.
Educate patients about dense breasts and cancer risk
Monica Saini, MD, a radiologist in Santa Fe, New Mexico, and JoAnn Pushkin, executive director of the nonprofit educational website DenseBreast-info.org, engaged ObGyn attendees on “Breast density: Why it matters and what to do” at the American College of Obstetricians and Gynecologists (ACOG) 2017 Annual Clinical and Scientific Meeting (May 6–9, 2017) in San Diego, California. The program was sponsored by GE Healthcare.
DENSE BREASTS ARE A RISK FACTOR FOR CANCER
Breast density is the second largest risk factor for breast cancer after radiation treatment to the chest, so it is important to identify patients with dense breasts, according to Dr. Saini. The American College of Radiology’s Breast Imaging Reporting and Data System (BI-RADS) classifies breast density into 4 groups: 1) almost entirely fatty, 2) scattered fibroglandular densities, 3) heterogeneously dense, and 4) extremely dense. A woman whose mammograms show heterogeneously dense or extremely dense breasts is considered to have “dense breasts.”
Cancer is often difficult to identify with mammography in dense breasts because masses or lumps appear as white on a white (dense tissue) background; by contrast, a tumor in a nondense (fatty) breast would appear as white on a dark, fatty tissue background. Approximately one-third of cancers in dense breasts have a delayed diagnosis on mammography, and 70% of cancers occur in dense breasts, said Dr. Saini.
Having dense breasts is not an abnormal condition, however, and is actually common—about 40% of women aged 40 or older have dense breasts.
Supplement mammography with other screening modalities
While screening mammograms can save lives, mammography should not be viewed as a one-size-fits-all modality. Screening for breast cancer should be personalized, based on, among other factors, a woman’s personal and family history, age, genetic risk, lifestyle factors, and breast density.
Key point. Women with dense breasts should continue to have screening mammograms. In addition, mammography for these patients should be supplemented with other technologies, such as 3D mammography (digital tomosynthesis), handheld ultrasound, or automated breast ultrasound (ABUS). In women at higher risk (presence of BRCA1 or BRCA2 gene mutation, strong family history of breast cancer, or radiation treatment to the chest) magnetic resonance imaging (MRI) may be considered.
Data on adjunct screening modalities. Dr. Saini discussed the results of the ASTOUND trial, a prospective multicenter study that compared ultrasound and tomosynthesis for the detection of breast cancer in mammography-negative dense breasts.1 Among the 3,231 asymptomatic women included in the trial, 13 breast cancers were detected with tomosynthesis (incremental cancer detection rate [CDR], 4 per 1,000 screens; 95% confidence interval [CI], 1.8–6.2) and 23 were detected with ultrasound (incremental CDR, 7.1 per 1,000 screens; 95% CI, 4.4–10.0), P = .006. There were 107 false-positive results: 53 with tomosynthesis and 65 with ultrasound, a difference that was not statistically significant. The study authors noted that while ultrasound had better incremental breast cancer detection than tomosynthesis, and at a similar false-positive recall rate, tomosynthesis did detect more than half of the additional breast cancers in these women.1
Make screening easier for the patient
Dr. Saini noted that for women with dense breasts, performing mammography and adjunctive screening at the same visit is convenient for the patient. Physicians can also write prescriptions for follow-up based on density findings, for example, “3D mammography if available, if dense, order ultrasound.”
Read how to answer patient questions about breast density
ARE YOU READY TO ANSWER PATIENT QUESTIONS ABOUT BREAST DENSITY?
That is the question JoAnn Pushkin, executive director of DenseBreast-info.org, asked in her presentation. You should discuss with patients exactly what it means to have dense breasts, breast density as an independent risk factor for cancer, the breast imaging technologies available for screening (mammography, tomosynthesis, ultrasound, contrast-enhanced MRI), the risks and benefits of each screening modality, and surveillance intervals for women with dense breasts. Good communication with the patient’s radiology team assists in formulating an individualized screening strategy.
Patients may have concerns about the information provided—or not provided—in their state’s breast density notification letter after a mammogram. Currently, 31 states mandate some type of breast density notification, while 4 states have efforts for density reporting or education that do not require notification. The information given to patients and how they will be informed varies by state. Some states, for example, require that patients who have heterogeneously or extremely dense breasts be informed of this by letter, while other states require that all patients receive the same notification with information about dense breasts but does not tell them whether or not they have dense breasts.
A go-to resource for ObGyns and patients
The website of the nonprofit DenseBreast-Info.org (http://densebreast-info.org/), co-founded by Wendie Berg, MD, PhD, who serves as Chief Scientific Advisor to the organization and is Professor of Radiology at the University of Pittsburgh School of Medicine/Magee-Women’s Hospital of UPMC, provides an interactive US map that features state-by-state breast density reporting guidelines so you can stay up-to-date on notification legislation in your area.
Sections for patients offer comprehensive and clearly written information on categories of breast density, a patient risk checklist, screening test descriptions, frequently asked questions, educational videos, and a patient brochure in English and Spanish.
For health care providers, resources include:
- a screening decision support tool flowchart to help assess which patients need more screening
- a table summarizing the cancer detection rates for mammography alone and mammography plus another screening modality (tomosynthesis, ultrasound, MRI)
- a comparison of breast cancer screening guidelines from various medical societies, including the American College of Radiology/Society of Breast Imaging, the American Cancer Society, the American College of Obstetricians and Gynecologists, and the US Preventive Services Task Force.
A special section covers screening technology, and each page includes descriptions, benefits, and considerations for use. Photos of the equipment and images of breast scans with explanatory captions enhance understanding.
Screening for high-risk women
Ms. Pushkin noted that for high-risk patients with dense breasts, mammography plus MRI annually would be an appropriate option.
- Tagliafico AS, Calabrese M, Mariscotti G, et al. Adjunct screening with tomosynthesis or ultrasound in women with mammography-negative dense breasts: interim report of a prospective comparative trial [published online ahead of print March 9, 2015]. J Clin Oncol. doi:10.1200/JCO.2015.63.4147.
Monica Saini, MD, a radiologist in Santa Fe, New Mexico, and JoAnn Pushkin, executive director of the nonprofit educational website DenseBreast-info.org, engaged ObGyn attendees on “Breast density: Why it matters and what to do” at the American College of Obstetricians and Gynecologists (ACOG) 2017 Annual Clinical and Scientific Meeting (May 6–9, 2017) in San Diego, California. The program was sponsored by GE Healthcare.
DENSE BREASTS ARE A RISK FACTOR FOR CANCER
Breast density is the second largest risk factor for breast cancer after radiation treatment to the chest, so it is important to identify patients with dense breasts, according to Dr. Saini. The American College of Radiology’s Breast Imaging Reporting and Data System (BI-RADS) classifies breast density into 4 groups: 1) almost entirely fatty, 2) scattered fibroglandular densities, 3) heterogeneously dense, and 4) extremely dense. A woman whose mammograms show heterogeneously dense or extremely dense breasts is considered to have “dense breasts.”
Cancer is often difficult to identify with mammography in dense breasts because masses or lumps appear as white on a white (dense tissue) background; by contrast, a tumor in a nondense (fatty) breast would appear as white on a dark, fatty tissue background. Approximately one-third of cancers in dense breasts have a delayed diagnosis on mammography, and 70% of cancers occur in dense breasts, said Dr. Saini.
Having dense breasts is not an abnormal condition, however, and is actually common—about 40% of women aged 40 or older have dense breasts.
Supplement mammography with other screening modalities
While screening mammograms can save lives, mammography should not be viewed as a one-size-fits-all modality. Screening for breast cancer should be personalized, based on, among other factors, a woman’s personal and family history, age, genetic risk, lifestyle factors, and breast density.
Key point. Women with dense breasts should continue to have screening mammograms. In addition, mammography for these patients should be supplemented with other technologies, such as 3D mammography (digital tomosynthesis), handheld ultrasound, or automated breast ultrasound (ABUS). In women at higher risk (presence of BRCA1 or BRCA2 gene mutation, strong family history of breast cancer, or radiation treatment to the chest) magnetic resonance imaging (MRI) may be considered.
Data on adjunct screening modalities. Dr. Saini discussed the results of the ASTOUND trial, a prospective multicenter study that compared ultrasound and tomosynthesis for the detection of breast cancer in mammography-negative dense breasts.1 Among the 3,231 asymptomatic women included in the trial, 13 breast cancers were detected with tomosynthesis (incremental cancer detection rate [CDR], 4 per 1,000 screens; 95% confidence interval [CI], 1.8–6.2) and 23 were detected with ultrasound (incremental CDR, 7.1 per 1,000 screens; 95% CI, 4.4–10.0), P = .006. There were 107 false-positive results: 53 with tomosynthesis and 65 with ultrasound, a difference that was not statistically significant. The study authors noted that while ultrasound had better incremental breast cancer detection than tomosynthesis, and at a similar false-positive recall rate, tomosynthesis did detect more than half of the additional breast cancers in these women.1
Make screening easier for the patient
Dr. Saini noted that for women with dense breasts, performing mammography and adjunctive screening at the same visit is convenient for the patient. Physicians can also write prescriptions for follow-up based on density findings, for example, “3D mammography if available, if dense, order ultrasound.”
Read how to answer patient questions about breast density
ARE YOU READY TO ANSWER PATIENT QUESTIONS ABOUT BREAST DENSITY?
That is the question JoAnn Pushkin, executive director of DenseBreast-info.org, asked in her presentation. You should discuss with patients exactly what it means to have dense breasts, breast density as an independent risk factor for cancer, the breast imaging technologies available for screening (mammography, tomosynthesis, ultrasound, contrast-enhanced MRI), the risks and benefits of each screening modality, and surveillance intervals for women with dense breasts. Good communication with the patient’s radiology team assists in formulating an individualized screening strategy.
Patients may have concerns about the information provided—or not provided—in their state’s breast density notification letter after a mammogram. Currently, 31 states mandate some type of breast density notification, while 4 states have efforts for density reporting or education that do not require notification. The information given to patients and how they will be informed varies by state. Some states, for example, require that patients who have heterogeneously or extremely dense breasts be informed of this by letter, while other states require that all patients receive the same notification with information about dense breasts but does not tell them whether or not they have dense breasts.
A go-to resource for ObGyns and patients
The website of the nonprofit DenseBreast-Info.org (http://densebreast-info.org/), co-founded by Wendie Berg, MD, PhD, who serves as Chief Scientific Advisor to the organization and is Professor of Radiology at the University of Pittsburgh School of Medicine/Magee-Women’s Hospital of UPMC, provides an interactive US map that features state-by-state breast density reporting guidelines so you can stay up-to-date on notification legislation in your area.
Sections for patients offer comprehensive and clearly written information on categories of breast density, a patient risk checklist, screening test descriptions, frequently asked questions, educational videos, and a patient brochure in English and Spanish.
For health care providers, resources include:
- a screening decision support tool flowchart to help assess which patients need more screening
- a table summarizing the cancer detection rates for mammography alone and mammography plus another screening modality (tomosynthesis, ultrasound, MRI)
- a comparison of breast cancer screening guidelines from various medical societies, including the American College of Radiology/Society of Breast Imaging, the American Cancer Society, the American College of Obstetricians and Gynecologists, and the US Preventive Services Task Force.
A special section covers screening technology, and each page includes descriptions, benefits, and considerations for use. Photos of the equipment and images of breast scans with explanatory captions enhance understanding.
Screening for high-risk women
Ms. Pushkin noted that for high-risk patients with dense breasts, mammography plus MRI annually would be an appropriate option.
Monica Saini, MD, a radiologist in Santa Fe, New Mexico, and JoAnn Pushkin, executive director of the nonprofit educational website DenseBreast-info.org, engaged ObGyn attendees on “Breast density: Why it matters and what to do” at the American College of Obstetricians and Gynecologists (ACOG) 2017 Annual Clinical and Scientific Meeting (May 6–9, 2017) in San Diego, California. The program was sponsored by GE Healthcare.
DENSE BREASTS ARE A RISK FACTOR FOR CANCER
Breast density is the second largest risk factor for breast cancer after radiation treatment to the chest, so it is important to identify patients with dense breasts, according to Dr. Saini. The American College of Radiology’s Breast Imaging Reporting and Data System (BI-RADS) classifies breast density into 4 groups: 1) almost entirely fatty, 2) scattered fibroglandular densities, 3) heterogeneously dense, and 4) extremely dense. A woman whose mammograms show heterogeneously dense or extremely dense breasts is considered to have “dense breasts.”
Cancer is often difficult to identify with mammography in dense breasts because masses or lumps appear as white on a white (dense tissue) background; by contrast, a tumor in a nondense (fatty) breast would appear as white on a dark, fatty tissue background. Approximately one-third of cancers in dense breasts have a delayed diagnosis on mammography, and 70% of cancers occur in dense breasts, said Dr. Saini.
Having dense breasts is not an abnormal condition, however, and is actually common—about 40% of women aged 40 or older have dense breasts.
Supplement mammography with other screening modalities
While screening mammograms can save lives, mammography should not be viewed as a one-size-fits-all modality. Screening for breast cancer should be personalized, based on, among other factors, a woman’s personal and family history, age, genetic risk, lifestyle factors, and breast density.
Key point. Women with dense breasts should continue to have screening mammograms. In addition, mammography for these patients should be supplemented with other technologies, such as 3D mammography (digital tomosynthesis), handheld ultrasound, or automated breast ultrasound (ABUS). In women at higher risk (presence of BRCA1 or BRCA2 gene mutation, strong family history of breast cancer, or radiation treatment to the chest) magnetic resonance imaging (MRI) may be considered.
Data on adjunct screening modalities. Dr. Saini discussed the results of the ASTOUND trial, a prospective multicenter study that compared ultrasound and tomosynthesis for the detection of breast cancer in mammography-negative dense breasts.1 Among the 3,231 asymptomatic women included in the trial, 13 breast cancers were detected with tomosynthesis (incremental cancer detection rate [CDR], 4 per 1,000 screens; 95% confidence interval [CI], 1.8–6.2) and 23 were detected with ultrasound (incremental CDR, 7.1 per 1,000 screens; 95% CI, 4.4–10.0), P = .006. There were 107 false-positive results: 53 with tomosynthesis and 65 with ultrasound, a difference that was not statistically significant. The study authors noted that while ultrasound had better incremental breast cancer detection than tomosynthesis, and at a similar false-positive recall rate, tomosynthesis did detect more than half of the additional breast cancers in these women.1
Make screening easier for the patient
Dr. Saini noted that for women with dense breasts, performing mammography and adjunctive screening at the same visit is convenient for the patient. Physicians can also write prescriptions for follow-up based on density findings, for example, “3D mammography if available, if dense, order ultrasound.”
Read how to answer patient questions about breast density
ARE YOU READY TO ANSWER PATIENT QUESTIONS ABOUT BREAST DENSITY?
That is the question JoAnn Pushkin, executive director of DenseBreast-info.org, asked in her presentation. You should discuss with patients exactly what it means to have dense breasts, breast density as an independent risk factor for cancer, the breast imaging technologies available for screening (mammography, tomosynthesis, ultrasound, contrast-enhanced MRI), the risks and benefits of each screening modality, and surveillance intervals for women with dense breasts. Good communication with the patient’s radiology team assists in formulating an individualized screening strategy.
Patients may have concerns about the information provided—or not provided—in their state’s breast density notification letter after a mammogram. Currently, 31 states mandate some type of breast density notification, while 4 states have efforts for density reporting or education that do not require notification. The information given to patients and how they will be informed varies by state. Some states, for example, require that patients who have heterogeneously or extremely dense breasts be informed of this by letter, while other states require that all patients receive the same notification with information about dense breasts but does not tell them whether or not they have dense breasts.
A go-to resource for ObGyns and patients
The website of the nonprofit DenseBreast-Info.org (http://densebreast-info.org/), co-founded by Wendie Berg, MD, PhD, who serves as Chief Scientific Advisor to the organization and is Professor of Radiology at the University of Pittsburgh School of Medicine/Magee-Women’s Hospital of UPMC, provides an interactive US map that features state-by-state breast density reporting guidelines so you can stay up-to-date on notification legislation in your area.
Sections for patients offer comprehensive and clearly written information on categories of breast density, a patient risk checklist, screening test descriptions, frequently asked questions, educational videos, and a patient brochure in English and Spanish.
For health care providers, resources include:
- a screening decision support tool flowchart to help assess which patients need more screening
- a table summarizing the cancer detection rates for mammography alone and mammography plus another screening modality (tomosynthesis, ultrasound, MRI)
- a comparison of breast cancer screening guidelines from various medical societies, including the American College of Radiology/Society of Breast Imaging, the American Cancer Society, the American College of Obstetricians and Gynecologists, and the US Preventive Services Task Force.
A special section covers screening technology, and each page includes descriptions, benefits, and considerations for use. Photos of the equipment and images of breast scans with explanatory captions enhance understanding.
Screening for high-risk women
Ms. Pushkin noted that for high-risk patients with dense breasts, mammography plus MRI annually would be an appropriate option.
- Tagliafico AS, Calabrese M, Mariscotti G, et al. Adjunct screening with tomosynthesis or ultrasound in women with mammography-negative dense breasts: interim report of a prospective comparative trial [published online ahead of print March 9, 2015]. J Clin Oncol. doi:10.1200/JCO.2015.63.4147.
- Tagliafico AS, Calabrese M, Mariscotti G, et al. Adjunct screening with tomosynthesis or ultrasound in women with mammography-negative dense breasts: interim report of a prospective comparative trial [published online ahead of print March 9, 2015]. J Clin Oncol. doi:10.1200/JCO.2015.63.4147.