User login
Tongue necrosis from temporal arteritis
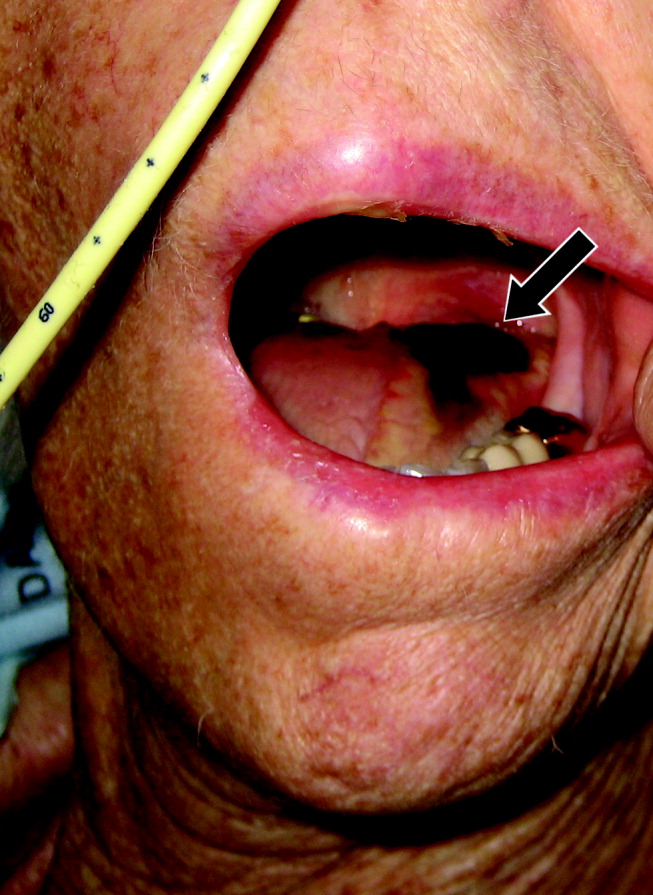
A 77‐year‐old woman with hypothyroidism presented with a 2‐week history of head, neck, jaw, and tongue pain. She had also developed slurred speech and difficulty chewing. On examination she had a temperature of 38.0C. She was without neurological deficits. However, she did have difficulty protruding her tongue, which had a cyanotic appearance and was painful. Laboratory findings showed an erythrocyte sedimentation rate of 68 mm/hr. Temporal arteritis was suspected, and the patient was started on corticosteroids. A subsequent temporal artery biopsy revealed inflammation and thrombus formation consistent with temporal arteritis. On hospital day 3, she developed unilateral ischemia in her tongue, which eventually became necrotic (Fig. 1). Although tongue necrosis is rare, temporal arteritis is the most frequent cause. It is usually unilateral and caused by compromised blood supply as a result of vasculitis in one of the lingual arteries. Other causes of tongue necrosis such as embolus, abscess, syphilis, tongue carcinoma, and Hodgkin's disease should be excluded.1, 2 Although necrotic tongue tissue must sometimes be extensively debrided or resected, our patient required minimal debridement. At follow‐up 1 month later, she was recovering at home with ongoing speech therapy and a corticosteroid taper.
- ,,.Lingual infarction: a review of the literature.Ann Vasc Surg.1992;6:450–452.
- ,.The ESR in the diagnosis and management of the polymyalgia rheumatica/giant cell arteritis syndrome.Ann Rheum Dis.1983;42:168–170.
A 77‐year‐old woman with hypothyroidism presented with a 2‐week history of head, neck, jaw, and tongue pain. She had also developed slurred speech and difficulty chewing. On examination she had a temperature of 38.0C. She was without neurological deficits. However, she did have difficulty protruding her tongue, which had a cyanotic appearance and was painful. Laboratory findings showed an erythrocyte sedimentation rate of 68 mm/hr. Temporal arteritis was suspected, and the patient was started on corticosteroids. A subsequent temporal artery biopsy revealed inflammation and thrombus formation consistent with temporal arteritis. On hospital day 3, she developed unilateral ischemia in her tongue, which eventually became necrotic (Fig. 1). Although tongue necrosis is rare, temporal arteritis is the most frequent cause. It is usually unilateral and caused by compromised blood supply as a result of vasculitis in one of the lingual arteries. Other causes of tongue necrosis such as embolus, abscess, syphilis, tongue carcinoma, and Hodgkin's disease should be excluded.1, 2 Although necrotic tongue tissue must sometimes be extensively debrided or resected, our patient required minimal debridement. At follow‐up 1 month later, she was recovering at home with ongoing speech therapy and a corticosteroid taper.
A 77‐year‐old woman with hypothyroidism presented with a 2‐week history of head, neck, jaw, and tongue pain. She had also developed slurred speech and difficulty chewing. On examination she had a temperature of 38.0C. She was without neurological deficits. However, she did have difficulty protruding her tongue, which had a cyanotic appearance and was painful. Laboratory findings showed an erythrocyte sedimentation rate of 68 mm/hr. Temporal arteritis was suspected, and the patient was started on corticosteroids. A subsequent temporal artery biopsy revealed inflammation and thrombus formation consistent with temporal arteritis. On hospital day 3, she developed unilateral ischemia in her tongue, which eventually became necrotic (Fig. 1). Although tongue necrosis is rare, temporal arteritis is the most frequent cause. It is usually unilateral and caused by compromised blood supply as a result of vasculitis in one of the lingual arteries. Other causes of tongue necrosis such as embolus, abscess, syphilis, tongue carcinoma, and Hodgkin's disease should be excluded.1, 2 Although necrotic tongue tissue must sometimes be extensively debrided or resected, our patient required minimal debridement. At follow‐up 1 month later, she was recovering at home with ongoing speech therapy and a corticosteroid taper.
- ,,.Lingual infarction: a review of the literature.Ann Vasc Surg.1992;6:450–452.
- ,.The ESR in the diagnosis and management of the polymyalgia rheumatica/giant cell arteritis syndrome.Ann Rheum Dis.1983;42:168–170.
- ,,.Lingual infarction: a review of the literature.Ann Vasc Surg.1992;6:450–452.
- ,.The ESR in the diagnosis and management of the polymyalgia rheumatica/giant cell arteritis syndrome.Ann Rheum Dis.1983;42:168–170.