User login
ACOG’s push for medical liability reform: What’s the latest?
It’s a conundrum. There seems to be no doubt about the need for medical liability reform—in fact, there is wide-spread support for it. And yet....
Four years after Captain Chesley “Sully” Sullenberger saved a planeload of passengers during an emergency landing—the “miracle on the Hudson”—he’s become a national champion of medical liability reform. In a recent interview with Politico, Sullenberger equated the 200,000 lives estimated to be lost each year due to medical errors to “20 jetliners crashing per week,” a situation he insists would close airports and ground flights until the problem was solved. But these 200,000 deaths cause little more than a ripple of concern, he claims.1
Among the solutions he proposes is “a whole different approach to reviewing medical errors, figuring out what’s behind them, not just blaming doctors and nurses.”1
Captain Sullenberger is discovering the difficult reality we’ve experienced for too many years: Solutions just don’t come very fast to medical liability reform, despite wide-spread support for it.
At the American Congress of Obstetricians and Gynecologists (ACOG), our campaign for medical liability reform has focused, as always, on patients, using the campaign line: “Who will delivery my baby?” ACOG supports caps on noneconomic damages and other reforms, such as those contained in the California Medical Injury Compensation Reform Act (MICRA), the gold standard for medical liability reform. We will continue to push for national MICRA reform until we’ve won that important protection for all ObGyns and their patients.
Until we reach that goal, we’re working to accomplish meaningful steps to liability reform where we can, including testing state alternatives. And our colleague organizations? Many of them, once insisting on federal adoption of MICRA or nothing at all, now actively support meaningful alternatives, too.
What do we want?
Proposals for tort reform, based on California’s MICRA statute, include:
- mandatory periodic payments of all future damages exceeding $100,000
- a $250,000 ceiling on noneconomic damage awards
- a requirement that claims must be filed within 2 years of the date by which the alleged injury reasonably should have been discovered but in no event more than 4 years from the time of the alleged injury. In the case of alleged injury to children under 4 years of age, claims must be filed by the child’s 8th birthday.
- limits on punitive damages, with 50% of punitive damage awards going to a state disciplinary fund
- limits on attorney contingency fees
- reductions in awards based on the amount paid from another source, such as health or disability insurance
- a requirement for “clear and convincing evidence” rather than the usual “preponderance of evidence” when a health-care professional who provided delivery services but not prenatal care is sued
- alternative systems for dispute resolution.
10 alternative reforms
Good ideas include:
1. Require a certificate of merit from the plaintiff
This proposal would require the plaintiff to file an affidavit with the court to demonstrate that the case has merit before the complaint can move forward. Certificates would necessitate the written opinion of a legally qualified health-care provider affirming that the defendant failed to meet the care standards that would be followed by a reasonably prudent health-care provider—and that this failure caused or directly contributed to the damages claimed.
2. Facilitate early settlement offers
Under this idea, a physician or hospital would be allowed to offer economic damages to an injured party without involving the courts. This offer would not constitute an admission of liability and would be inadmissible if a lawsuit were later filed in the case. Physicians would have an incentive to make a good-faith offer as early as possible after the injury is discovered, and patients would have an incentive to accept legitimate offers of compensation. Early-offer programs would require the injured party to meet a higher burden of proof for alleged negligence if that party chooses to reject the offer and file a lawsuit.
3. Create health-care courts
Health-care courts would allow for a bench or jury trial presided over by a specially trained judge to exclusively hear medical liability cases. Such courts have the potential to correct severe deficiencies in the current medical justice system and to reduce health-system errors and improve patient safety.
4. Allow a physician to say, “I’m sorry”
This proposal would encourage physicians to directly discuss errors and injuries with patients, to apologize and outline corrective action. Such discussions would be inadmissible if a patient later files a lawsuit.
5. Establish medical review panels
Any claim against a physician would be reviewed by a panel of experts who would provide an opinion on whether the physician failed to act within the relevant standards of care.
6. Require a claim to be screened and mediated
A plaintiff ’s claim would have to be evaluated by a screening panel before it could proceed to litigation. The panel would identify claims hat merit compensation and encourage early resolution of those claims. It also would encourage withdrawal or dismissal of non-meritorious claims.
7. Protect physicians who follow evidence-based guidelines
Health-care providers who follow guidelines based on solid evidence, and those who have legitimate justifications for departing from guidelines, would be protected from liability claims.
8. Allow the voluntary resolution of disputes
This proposal would motivate states to encourage the creation of other innovative systems to compensate individuals who are injured in the course of receiving health-care services.
9. Require expert witnesses to meet certain standards
This alternative would limit expert-witness standing to individuals who:
- are licensed and trained in the same specialty as the defendant
- have particular expertise in the disease process or procedure performed in the case
- have been in active medical practice in the same specialty as the defendant within 5 years of the claim or who have been taught at an accredited medical school on the care and type of treatment at issue.
10. Create catastrophic injury systems
These systems would establish a fund for individuals who have experienced bad outcomes. Birth injury funds are an example of this model.
Who’s on our side?
Congressional policy wonks give liability reform a thumbs up
In early 2010, the Medicare Payment Advisory Commission (MedPAC), a nonpartisan advisory counsel to the US Congress, identified three important ways that our current malpractice system harms the Medicare program and Medicare beneficiaries, the aged, and disabled:
- Medicare payments to providers include some liability costs (folded into hospital diagnosis-related group [DRG] payments; factored into physician fee schedule calculation)
- Defensive medicine drives up costs for Medicare
- Malpractice impairs the quality and safety of care to beneficiaries. That is, the current system does not improve patient safety.
MedPAC staff recommended that the commissioners urge Congress to pass government-subsidized malpractice reinsurance for providers who meet certain safety criteria or create a federal administrative adjudication process. The commissioners expressed an interest in alternatives to address the costs of medical malpractice, including ways to encourage states and providers to address medical malpractice in a manner most appropriate for them. However, when MedPAC returned to this topic at its next meeting later the same year, the commissioners mentioned medical liability only to dismiss it as an incidental issue in opening remarks.
The Congressional Budget Office (CBO) estimates that medical malpractice costs our health-care system $35 billion in direct costs, with billions more as a result of defensive medicine.
CBO has scored these medical liability reform proposals as providing significant savings to our federal budget:
- a $250,000 cap on subjective, noneconomic damages (with no limit on economic damages)
- collateral source rule allowing evidence of outside payments to be submitted in court
- a ban on subrogation by certain collateral sources
- caps on attorney contingency fees
- periodic payments of future damages
- a reasonable statute of limitations.
In addition, in 2011, CBO scored comprehensive medical liability reform as saving the federal government $62.4 billion over 10 years. As longtime Illinois Senator Everett Dirksen was known to say, “A billion here, a billion there, and pretty soon you’re talking real money.”
Many Republican congressional leaders “walk the walk”
Republicans have long claimed medical liability reform as their issue. And they walk the walk.
Representative Phil Gingrey, MD, of Georgia, an ACOG Fellow, has led the medical liability reform fight on Capitol Hill for a number of years. His bill, the Protecting Access to Healthcare Act (HR 5), which would have brought MICRA to the national level, was repeatedly passed by the Republican majority of the House of Representatives, only to be ignored by the Democrats controlling the Senate.
Again this year, Dr. Gingrey introduced legislation to protect physicians from unexpected liability. His Standard of Care Protection Act (HR 1473) would ensure that provisions of the Affordable Care Act (ACA) cannot be used to create new causes of action against medical professionals. HR 1473 would ensure that Medicare, Medicaid, and other federal programs that establish government standards and guidelines for health-care providers cannot be used to create new causes of action.
Federal health-care programs are changing to ensure that payment reflects quality of care. As a result, new payment rules, guidelines, and standards are being written into federal laws and regulations. HR 1473 would make clear that these cannot be used to define the applicable standard of care or duty of care in a medical liability lawsuit.
ACOG supports Dr. Gingrey’s bill, as well as a second, companion approach that would ensure that ObGyns who follow guidelines and standards of care developed by their medical society are protected from liability, with sensible exceptions for egregious harm and negligence.
Representative Charlie Dent, Republican of Pennsylvania, also has introduced ACOG-supported medical liability legislation. The Health Care Safety Net Enhancement Act (HR 36) would provide federal liability protection for physicians providing care under the Emergency Medical Treatment and Active Labor Act (EMTALA). HR 36 is commonly referred to as Good Samaritan legislation, intended to protect doctors who rush to the aid of a sick individual. The likelihood of any of these bills getting enacted into law is slim. Even some conservative Republicans oppose federal liability reform as an intrusion into states’ rights.
Some Democrats have said good things
In his proposed budget for fiscal year 2012, President Barack Obama asked Congress for funding to address medical liability issues.
He proposed “to restrain health-care costs” through “a more aggressive effort to reform our medical malpractice system to reduce defensive medicine, promote patient safety, and improve patient outcomes.” He encouraged Republicans to work constructively with him on medical malpractice as part of an overall effort to restrain health-care costs.2
The President asked Congress for “$250 million in grants to states to reform the way they resolve medical malpractice disputes,” including health courts, safe harbors, early disclosure and offer, and other legal reforms such as joint and several liability and collateral source rules.2
Congress never funded the President’s request.
President Obama repeated his request in his fiscal year 2013 budget proposal. Congress didn’t fund it then, either.
Earlier, in March 2009, in remarks to the Business Roundtable, President Obama noted that “the cost issue is the thing that we actually think is the big driver in this whole debate...things like comparative effectiveness, health IT, prevention, figuring out how our reimbursement structures are designed under Medicare and Medicaid. Medical liability issues—I think all those things have to be on the table.”3
In an interview the same month, Senator Ron Wyden, Democrat of Oregon, said, “I think [medical liability reform is] an essential piece for there to be enduring reform, reform that will stick and will get a significant bipar-tisan vote in the United States Senate.”4
Senator Wyden’s Healthy Americans Act (S 391) included incentives to get states to enact malpractice reforms as a key to overhauling the health-care system.
Also in March 2009, Representative Rob Andrews, Democrat of New Jersey, Chairman of the House Education and Labor, Health Subcommittee, pointed to the need for medical liability reform.
“It’s hard for me to imagine a [health-care reform] result that gets to the president’s desk that doesn’t deal with the medical mal-practice issue in some way.”4
And Senator Max Baucus, Democrat of Montana, Chairman of the Senate Finance Committee, proposed providing states grant money to develop alternative litigation models, such as encouraging disclosure and compensation in the case of error, and establishing health courts whose judges have health-care expertise.
As early as May 2006, President Obama (then a Senator from Illinois) and Senator Hillary Rodham Clinton, Democrat of New York, urged a focus on patient safety.
“Instead of focusing on the few areas of intense disagreement,” they wrote in the New England Journal of Medicine, “such as the possibility of mandating caps on the financial damages awarded to patients, we believe that the discussion should center on a more fundamental issue: the need to improve patient safety....”
“To improve both patient safety and the medical liability climate, the tort system must achieve four goals: reduce the rates of preventable patient injuries, promote open communication between physicians and patients, ensure patients access to fair compensation for legitimate medical injuries, and reduce liability insurance premiums for health-care providers. Addressing just one of these issues is not sufficient.”5
And then there are the trial lawyers
Readers of OBG Management know all too well that the role of trial lawyers in medical liability reform has been to block meaningful reforms from passing and to repeal reforms currently in place. The Association of Trial Lawyers of America, now known as the American Association for Justice, tries to portray itself as defending vulnerable patients against a few bad apples. Its Web site (www.justice.org) points to recent National Practitioner Data Bank (NPDB) figures indicating that “just 6% of doctors are responsible for 58% of all negligence incidents. The civil justice system seeks to weed out those few doctors whose actions have such devastating impact on patients.”
The Web site includes these bullet points:
- 6% of doctors have been responsible for 58% of all malpractice payments since 1991
- 2% of doctors having three or more mal-practice payments were responsible for 33% of all payments
- 1% of doctors having four or more malprac-tice payments were responsible for 20% of all payments
- 82% of doctors have never had a medical malpractice payment.
Tell that to ObGyns, who, in 2012, paid an average of 12.4% of their gross income for liability insurance premiums in 2012, and nearly 60% of whom changed their practices based on the risk or fear of professional liability claims or litigation. And this despite the fact that 43.9% of claims were dropped or settled without any payment on behalf of the ObGyn.
Action at the state level
We need a federal solution, but since that isn’t within reach, we’re looking to the states for action. And there’s a lot of action in some states, including Connecticut, Florida, Georgia, Hawaii, Illinois, Iowa, Missouri, Oregon, Rhode Island, Tennessee, and Utah.
Advocates in these states are trying a number of different approaches, hoping that some type of meaningful reform will be signed into law. Here’s a sampling of what’s under way.
Connecticut
HB 6687, amend certificates of merit in medical liability actions. Status: April 1, 2013: Joint Committee on Judiciary hearing. The bill would eliminate the need for a detailed basis for the formation of an opinion and replace it with a lower threshold stating the appearance of one or more specific breaches of the prevailing professional standard of care.
In addition, HB 6687 would allow any expert who may testify in court to satisfy the certificate of merit requirement, but at trial the “expert,” in order to testify, needs to have the court determine him or her to be qualified to testify based on discovery and evidentiary issues that are decided at trial. This expert then could sign a certificate of merit but have the court determine that he or she is indeed not an expert for that case. HB 6687 delays the challenging of qualifications of an expert only after the completion of discovery, adding substantial time and cost to defending meritless suits. Finally, the bill allows for a second bite of the apple for cases that did not meet this watered down standard for certificate of merit and would eliminate the automatic dismissal of cases filed with inadequate certificates that did not meet the rules of the court.
SB 1154, amend Connecticut’s failure of suit statute to allow a plaintiff whose lawsuit was dismissed due to a failure to file a certificate of good faith as required by statute, to commence a new action.
HB 5229, limit noneconomic damages in medical liability cases to $250,000 for each health-care provider and institution per event, and $750,000 overall for each event.
HB 5270, establish peer-review panels in medical liability actions. The panels would consist of physicians, medical professionals, and individuals outside the medical profession who would review claims of alleged negligence and determine whether there is probable cause that the medical liability claims have been made in good faith prior to the action being referred to mandatory mediation.
SB 97, extend the statute of limitations in medical liability cases, allowing for an action to be brought no more than 10 years from the date of the act or omission that serves as the basis for the claim.
Florida
The Birth-Related Neurological Injury Compensation Association (NICA). NICA is a statutory organization that manages the compensation plan used to pay for the care of infants born with certain neurological injuries. This plan is available to eligible families statewide without litigation. By eliminating costly legal proceedings, and through professional management of its disbursements, NICA ensures that birth-injured infants receive the care they need while reducing the financial burden on medical providers and families. Defensive work continues on the NICA Board and trial bar.
HB 7015, expert witness. Status: March 28, 2013, the House Justice Appropriations Subcommittee reported favorably. This bill would adopt the Daubert standard for expert witness testimony. It provides that a witness qualified as an expert by knowledge, skill, experience, training, or education may testify in the form of an opinion as to the facts at issue in a case.
Georgia
HB 499, Provider Shield Act. Georgia is the first state to introduce legislation based on the American Medical Association’s model bill, “The Provider Shield Act,” which clarifies language in the Affordable Care Act by providing that a physician’s failure to comply with, or a breach of, any federal statute, regulation, program, guideline, or other provision shall not: (1) be admissible; (2) be used to determine the standard of care; or (3) be the legal basis for a presumption of negligence.
Status: Enacted May 6, 2013. The law prohibits the use of payer guidelines and quality criteria outlined in federal law as a legal basis for negligence or standard of care in determining medical liability. Physicians are concerned that without such protections, the medical profession could be exposed to charges of negligence that aren’t based on clinical standards or the patient’s unique medical needs. Implementation of any guideline by any public or private payor, or the establishment of any payment standard or reimbursement criteria under any federal laws or regulations related to health care, shall not be construed, without competent expert testimony establishing the appropriate standard of care, to establish a legal basis for negligence or the standard of care or duty of care owed by a health-care provider to a patient in any civil action for medical malpractice or product liability.
This first-of-its-kind legislation reinforces the concept that medical decisions should be based on a patient’s unique medical needs. HB 499 makes it clear that federal standards or guidelines designed to enhance access to high-quality health care cannot be used to invent new legal actions against physicians.
Hawaii
SB 1308, health-care provider benevolent gesture legislation.
Illinois
On March 22, 2013, several pieces of tort-reform legislation were re-referred to the House Committee on Rules, effectively killing the bills for the session. The House Speaker would have to choose to “release” any of the bills in order for them to move again; this is highly unlikely.
HB 138 would have deleted existing-venue language providing that an action may commence in any county if all defendants are nonresidents of the state, and replaced it with language providing that, if no defendants that are joined in good faith and with probable cause for the purpose of obtaining a judgment against them are residents of the state, an action may be commenced only in the county in which the transaction or some part thereof occurred out of which the cause of action arose.
HB 2220 and HB 2222 provided that, with respect to certain types of actions, for any defendant whose fault is less than 25% of the total fault attributable to the plaintiff, the defendants sued by the plaintiff, and any third-party defendant who could have been sued by the plaintiff (instead of any third-party defendant except the plaintiff’s employer), shall be severally liable for all other damages. In addition, these bills provided that, for any defendant whose fault is 25% or greater of the total fault attributable to the plaintiff, the defendants sued by the plaintiff, and any third-party defendants who could have been sued by the plaintiff (instead of any third-party defendants except the plaintiff’s employer), shall be jointly and severally liable for all other damages.
HB 2221 created requirements regarding qualifications, testimony, disclosure and compensation of expert testimony and standards for reviewing courts to follow in ruling on the admissibility of expert testimony.
Iowa
SSB 1054 and HSB 36, expert’s certificate of merit affidavit and noneconomic cap. These bills provide that in any medical liability action, the plaintiff is required, within 180 days of the defendant’s answer, to serve the defendant with an expert’s certificate of merit affidavit for each expert scheduled to testify. They also would limit noneconomic damage awards in medical liability cases to $1 million.
Missouri
HJR 6 proposes a constitutional amendment allowing the legislature to cap noneconomic damages in medical liability cases.
SJR 1 grants the legislature the power to limit, by statute, jury awards for noneconomic damages.
SB 64 changes the evidentiary standard in medical liability cases to “clear and convincing” for noneconomic damages.
Oregon
SB 483, early discussion and resolution. Status: Passed by the legislature. This bill establishes an early discussion and resolution (EDC) process within the Oregon Patient Safety Commission. This voluntary process is intended to facilitate open communication about all outcomes of care, including serious events, between the provider, health-care facility, and the patient. When an adverse health-care incident occurs, the patient, health-care provider or health-care facility where the incident occurred may file a notice of adverse health-care incident with the Commission. This notice triggers discussion of the health-care incident and, if appropriate, an offer of compensation. If discussion does not result in the resolution of the claim, the bill gives the parties the option of participating in Commission-facilitated mediation. The entire process is voluntary.
SJR 30, proposed amendment to constitution, $1 million limit on noneconomic awards in medical liability cases. Slated for next general election.
Rhode Island
HB 5380, apology bill. Status: Heard in House Judiciary Committee on March 27, 2013; no action was taken. This bill provides that statements by a health-care provider to a patient or to the patient’s family regarding the outcome of such patient’s medical care and treatment, such as an apology or expression of sympathy, shall be inadmissible as evidence or an admission of liability in any claim or action against the provider.
Tennessee
Joint and several liability. Status: On March 26, 2013, the House Civil Justice Subcommittee reported favorably. This bill would codify current state law by providing that if multiple defendants are found liable in a civil action governed by comparative fault, a defendant shall only be severally liable for the percentage of damages for which fault is attributed to such defendant by the trier of fact, and no defendant shall be held jointly liable for any damages.
SB 274, medical liability expert witness reform.
Utah
HB 135, rules, arbitration. Status: March 21, 2013, sent to Governor Gary Herbert for his approval. HB 135 provides that a party in a medical liability action or arbitration may not attempt to allocate fault to any health-care provider unless a certificate of compliance has been issued. HB 135 also requires that evidence from a medical review panel remain unreportable to a health-care facility or health insurance plan.
Summing up
Medical liability reform—the obvious need for it, the good reasons to do it, and the fact that it remains beyond reach—is a constant source of frustration among many ObGyns. Maybe Captain Sully can save the day.
How medical liability affects the ObGyn specialty
ACOG’s 2012 Survey on Professional Liability, our 11th survey since 1983, assessed the effects of professional liability litigation and insurance issues on the practice of obstetrics and gynecology.6 The survey, conducted under the direction of ACOG’s Vice President for Fellowship and Deputy Executive Vice President Albert Strunk, MD, JD, included segments on demographics, patient care, liability claims experience, and practice changes associated with the cost of liability insurance and the fear of litigation. The survey went to 32,238 Fellows and Junior Fellows. Of these, 9,006 completed the questionnaire. Here are major findings.
Provider profiles
A total of 72.5% of respondents provided both obstetric and gynecologic care, slightly lower than the percentage identified in the 2009 survey, which was 74.3%. Fewer than 7% of respondents provided obstetric care only; 19.8% provided gynecologic care only. Of those restricting their services to gynecology, 88.9% had previously offered obstetric care. The average age at which these physicians stopped practicing obstetrics was 49 years.
Cost of liability insurance
ObGyns spent an average of 12.4% of their gross income on liability insurance premiums in 2012, down from 18% in 2009.
How liability issues affected practice
Since the previous survey in 2009, 57.9% of respondents made one or more changes to their practice to mitigate the risk or fear of professional liability claims or litigation.
Obstetric practice. Among respondents who made changes to their obstetric practice, 27.4% decreased the number of high-risk patients they see, 23.8% increased the number of cesarean deliveries they perform, 18.9% stopped offering and performing vaginal birth after cesarean (VBAC), 11.5% reduced the total number of deliveries, and 6.2% stopped practicing obstetrics altogether.
Gynecologic practice. Respondents who changed their gynecologic practice cut back on surgical procedures (18.9%), stopped performing major gynecologic surgery (6.7%), and stopped performing all surgery (1.8%).
Other changes. Medical liability issues contributed to the decisions of 12.3% of respondents to choose salaried employment with a hospital, government, or other institution.
Claims experience
Obstetric claims were likely to involve a neurologically impaired infant (28.8%) as the primary allegation, followed by stillbirth or neonatal death (14.4%).
Other variables involved in obstetric claims included electronic fetal monitoring (20.9%), shoulder dystocia and/or brachial plexus injury (15.5%), and actions of ObGyn residents (11.4%).
Gynecologic claims. Survey respondents reported a total of 1,496 gynecologic claims. Major injury to the patient was the primary allegation of 29.1% of these claims. A delay in diagnosis or failure to diagnose was the second most common primary allegation (22.1%), followed by minor injury to the patient (20.7%).Of the claims involving a delayed or missed diagnosis, 41.8% involved cancer. Of these, breast cancer was the most frequent type of cancer (39.1%), followed by uterine cancer (20.3%), ovarian cancer (14.5%), and cervical cancer (10.9%).
Many gynecologic claims (44.4%) involved surgical complications arising from hysterectomy (28.7%) and laparoscopic procedures (14.6%).
Claims outcomes. A total of 43.9% of claims were dropped or settled without any payment on behalf of the ObGyn. Of these, 29.0% were dropped by the plaintiff, 11.2% were dismissed by the court, and 3.7% were settled without payment on behalf of the ObGyn.The average for all paid claims was $510,473.
The average payment for claims involving a neurologically impaired infant was $982,051. Other average payments for obstetric claims include $364,794 for “other infant injury–major” and $271,149 for stillbirth or neonatal death.
Average payments for gynecologic claims include $407,500 for a failure to diagnose breast cancer and $315,633 for “patient injury–major.”
Most challenging locales. It will come as no surprise to many readers that average medical liability payouts are especially high in six states:
New York - $677,866,050
Pennsylvania - $319,710,250
Illinois - $242,108,800
New Jersey - $221,170,750
Florida - $218,123,050
California - $215,519,200.
Fifty-eight percent of payouts nationwide were for female patients.7
Tell us what you think, at [email protected]. Please include your name and city and state.
1.Cheney K. ‘Miracle’ pilot on mission against medical errors. Politico.com. August 1, 2013. http://www.politico.com/story/2013/08/sully-sullenberger-mission-medical-erros-95009.html. Accessed August 6, 2013.
2.Office of Management and Budget. Fiscal Year 2012 Budget of the US Government. http://www.whitehouse.gov/files/documents/budget_2012.pdf. Accessed August 8, 2013.
3.Obama’s remarks to the Business Roundtable, March 12, 2009. Wall Street Journal: Washington Wire. http://blogs.wsj.com/washwire/2009/03/12/obamas-remarks-to-the-business-roundtable/. Accessed August 8, 2013.
4.Werner E. Health debate could spur malpractice changes. Salt Lake Tribune. March 17, 2009. http://www.sltrib.com/ci_11933162. Accessed August 8, 2013.
5.Clinton HR, Obama B. Perspective: Making patient safety the centerpiece of medical liability reform. N Engl J Med. 2006;354(21):2205–2208.
6.American Congress of Obstetricians and Gynecologists. Survey on Professional Liability. 2012 Survey Results. http://www.acog.org/About_ACOG/ACOG_Departments/Professional_Liability/2012_Survey_Results. Accessed August 7, 2013.
7. Latner AW. Six states account for 50% of malpractice payouts. Clinical Advisor. April 17, 2012. http://www.clinicaladvisor.com/six-states-account-for-50-of-malpractice-payouts/article/236931. Accessed August 7, 2013.
It’s a conundrum. There seems to be no doubt about the need for medical liability reform—in fact, there is wide-spread support for it. And yet....
Four years after Captain Chesley “Sully” Sullenberger saved a planeload of passengers during an emergency landing—the “miracle on the Hudson”—he’s become a national champion of medical liability reform. In a recent interview with Politico, Sullenberger equated the 200,000 lives estimated to be lost each year due to medical errors to “20 jetliners crashing per week,” a situation he insists would close airports and ground flights until the problem was solved. But these 200,000 deaths cause little more than a ripple of concern, he claims.1
Among the solutions he proposes is “a whole different approach to reviewing medical errors, figuring out what’s behind them, not just blaming doctors and nurses.”1
Captain Sullenberger is discovering the difficult reality we’ve experienced for too many years: Solutions just don’t come very fast to medical liability reform, despite wide-spread support for it.
At the American Congress of Obstetricians and Gynecologists (ACOG), our campaign for medical liability reform has focused, as always, on patients, using the campaign line: “Who will delivery my baby?” ACOG supports caps on noneconomic damages and other reforms, such as those contained in the California Medical Injury Compensation Reform Act (MICRA), the gold standard for medical liability reform. We will continue to push for national MICRA reform until we’ve won that important protection for all ObGyns and their patients.
Until we reach that goal, we’re working to accomplish meaningful steps to liability reform where we can, including testing state alternatives. And our colleague organizations? Many of them, once insisting on federal adoption of MICRA or nothing at all, now actively support meaningful alternatives, too.
What do we want?
Proposals for tort reform, based on California’s MICRA statute, include:
- mandatory periodic payments of all future damages exceeding $100,000
- a $250,000 ceiling on noneconomic damage awards
- a requirement that claims must be filed within 2 years of the date by which the alleged injury reasonably should have been discovered but in no event more than 4 years from the time of the alleged injury. In the case of alleged injury to children under 4 years of age, claims must be filed by the child’s 8th birthday.
- limits on punitive damages, with 50% of punitive damage awards going to a state disciplinary fund
- limits on attorney contingency fees
- reductions in awards based on the amount paid from another source, such as health or disability insurance
- a requirement for “clear and convincing evidence” rather than the usual “preponderance of evidence” when a health-care professional who provided delivery services but not prenatal care is sued
- alternative systems for dispute resolution.
10 alternative reforms
Good ideas include:
1. Require a certificate of merit from the plaintiff
This proposal would require the plaintiff to file an affidavit with the court to demonstrate that the case has merit before the complaint can move forward. Certificates would necessitate the written opinion of a legally qualified health-care provider affirming that the defendant failed to meet the care standards that would be followed by a reasonably prudent health-care provider—and that this failure caused or directly contributed to the damages claimed.
2. Facilitate early settlement offers
Under this idea, a physician or hospital would be allowed to offer economic damages to an injured party without involving the courts. This offer would not constitute an admission of liability and would be inadmissible if a lawsuit were later filed in the case. Physicians would have an incentive to make a good-faith offer as early as possible after the injury is discovered, and patients would have an incentive to accept legitimate offers of compensation. Early-offer programs would require the injured party to meet a higher burden of proof for alleged negligence if that party chooses to reject the offer and file a lawsuit.
3. Create health-care courts
Health-care courts would allow for a bench or jury trial presided over by a specially trained judge to exclusively hear medical liability cases. Such courts have the potential to correct severe deficiencies in the current medical justice system and to reduce health-system errors and improve patient safety.
4. Allow a physician to say, “I’m sorry”
This proposal would encourage physicians to directly discuss errors and injuries with patients, to apologize and outline corrective action. Such discussions would be inadmissible if a patient later files a lawsuit.
5. Establish medical review panels
Any claim against a physician would be reviewed by a panel of experts who would provide an opinion on whether the physician failed to act within the relevant standards of care.
6. Require a claim to be screened and mediated
A plaintiff ’s claim would have to be evaluated by a screening panel before it could proceed to litigation. The panel would identify claims hat merit compensation and encourage early resolution of those claims. It also would encourage withdrawal or dismissal of non-meritorious claims.
7. Protect physicians who follow evidence-based guidelines
Health-care providers who follow guidelines based on solid evidence, and those who have legitimate justifications for departing from guidelines, would be protected from liability claims.
8. Allow the voluntary resolution of disputes
This proposal would motivate states to encourage the creation of other innovative systems to compensate individuals who are injured in the course of receiving health-care services.
9. Require expert witnesses to meet certain standards
This alternative would limit expert-witness standing to individuals who:
- are licensed and trained in the same specialty as the defendant
- have particular expertise in the disease process or procedure performed in the case
- have been in active medical practice in the same specialty as the defendant within 5 years of the claim or who have been taught at an accredited medical school on the care and type of treatment at issue.
10. Create catastrophic injury systems
These systems would establish a fund for individuals who have experienced bad outcomes. Birth injury funds are an example of this model.
Who’s on our side?
Congressional policy wonks give liability reform a thumbs up
In early 2010, the Medicare Payment Advisory Commission (MedPAC), a nonpartisan advisory counsel to the US Congress, identified three important ways that our current malpractice system harms the Medicare program and Medicare beneficiaries, the aged, and disabled:
- Medicare payments to providers include some liability costs (folded into hospital diagnosis-related group [DRG] payments; factored into physician fee schedule calculation)
- Defensive medicine drives up costs for Medicare
- Malpractice impairs the quality and safety of care to beneficiaries. That is, the current system does not improve patient safety.
MedPAC staff recommended that the commissioners urge Congress to pass government-subsidized malpractice reinsurance for providers who meet certain safety criteria or create a federal administrative adjudication process. The commissioners expressed an interest in alternatives to address the costs of medical malpractice, including ways to encourage states and providers to address medical malpractice in a manner most appropriate for them. However, when MedPAC returned to this topic at its next meeting later the same year, the commissioners mentioned medical liability only to dismiss it as an incidental issue in opening remarks.
The Congressional Budget Office (CBO) estimates that medical malpractice costs our health-care system $35 billion in direct costs, with billions more as a result of defensive medicine.
CBO has scored these medical liability reform proposals as providing significant savings to our federal budget:
- a $250,000 cap on subjective, noneconomic damages (with no limit on economic damages)
- collateral source rule allowing evidence of outside payments to be submitted in court
- a ban on subrogation by certain collateral sources
- caps on attorney contingency fees
- periodic payments of future damages
- a reasonable statute of limitations.
In addition, in 2011, CBO scored comprehensive medical liability reform as saving the federal government $62.4 billion over 10 years. As longtime Illinois Senator Everett Dirksen was known to say, “A billion here, a billion there, and pretty soon you’re talking real money.”
Many Republican congressional leaders “walk the walk”
Republicans have long claimed medical liability reform as their issue. And they walk the walk.
Representative Phil Gingrey, MD, of Georgia, an ACOG Fellow, has led the medical liability reform fight on Capitol Hill for a number of years. His bill, the Protecting Access to Healthcare Act (HR 5), which would have brought MICRA to the national level, was repeatedly passed by the Republican majority of the House of Representatives, only to be ignored by the Democrats controlling the Senate.
Again this year, Dr. Gingrey introduced legislation to protect physicians from unexpected liability. His Standard of Care Protection Act (HR 1473) would ensure that provisions of the Affordable Care Act (ACA) cannot be used to create new causes of action against medical professionals. HR 1473 would ensure that Medicare, Medicaid, and other federal programs that establish government standards and guidelines for health-care providers cannot be used to create new causes of action.
Federal health-care programs are changing to ensure that payment reflects quality of care. As a result, new payment rules, guidelines, and standards are being written into federal laws and regulations. HR 1473 would make clear that these cannot be used to define the applicable standard of care or duty of care in a medical liability lawsuit.
ACOG supports Dr. Gingrey’s bill, as well as a second, companion approach that would ensure that ObGyns who follow guidelines and standards of care developed by their medical society are protected from liability, with sensible exceptions for egregious harm and negligence.
Representative Charlie Dent, Republican of Pennsylvania, also has introduced ACOG-supported medical liability legislation. The Health Care Safety Net Enhancement Act (HR 36) would provide federal liability protection for physicians providing care under the Emergency Medical Treatment and Active Labor Act (EMTALA). HR 36 is commonly referred to as Good Samaritan legislation, intended to protect doctors who rush to the aid of a sick individual. The likelihood of any of these bills getting enacted into law is slim. Even some conservative Republicans oppose federal liability reform as an intrusion into states’ rights.
Some Democrats have said good things
In his proposed budget for fiscal year 2012, President Barack Obama asked Congress for funding to address medical liability issues.
He proposed “to restrain health-care costs” through “a more aggressive effort to reform our medical malpractice system to reduce defensive medicine, promote patient safety, and improve patient outcomes.” He encouraged Republicans to work constructively with him on medical malpractice as part of an overall effort to restrain health-care costs.2
The President asked Congress for “$250 million in grants to states to reform the way they resolve medical malpractice disputes,” including health courts, safe harbors, early disclosure and offer, and other legal reforms such as joint and several liability and collateral source rules.2
Congress never funded the President’s request.
President Obama repeated his request in his fiscal year 2013 budget proposal. Congress didn’t fund it then, either.
Earlier, in March 2009, in remarks to the Business Roundtable, President Obama noted that “the cost issue is the thing that we actually think is the big driver in this whole debate...things like comparative effectiveness, health IT, prevention, figuring out how our reimbursement structures are designed under Medicare and Medicaid. Medical liability issues—I think all those things have to be on the table.”3
In an interview the same month, Senator Ron Wyden, Democrat of Oregon, said, “I think [medical liability reform is] an essential piece for there to be enduring reform, reform that will stick and will get a significant bipar-tisan vote in the United States Senate.”4
Senator Wyden’s Healthy Americans Act (S 391) included incentives to get states to enact malpractice reforms as a key to overhauling the health-care system.
Also in March 2009, Representative Rob Andrews, Democrat of New Jersey, Chairman of the House Education and Labor, Health Subcommittee, pointed to the need for medical liability reform.
“It’s hard for me to imagine a [health-care reform] result that gets to the president’s desk that doesn’t deal with the medical mal-practice issue in some way.”4
And Senator Max Baucus, Democrat of Montana, Chairman of the Senate Finance Committee, proposed providing states grant money to develop alternative litigation models, such as encouraging disclosure and compensation in the case of error, and establishing health courts whose judges have health-care expertise.
As early as May 2006, President Obama (then a Senator from Illinois) and Senator Hillary Rodham Clinton, Democrat of New York, urged a focus on patient safety.
“Instead of focusing on the few areas of intense disagreement,” they wrote in the New England Journal of Medicine, “such as the possibility of mandating caps on the financial damages awarded to patients, we believe that the discussion should center on a more fundamental issue: the need to improve patient safety....”
“To improve both patient safety and the medical liability climate, the tort system must achieve four goals: reduce the rates of preventable patient injuries, promote open communication between physicians and patients, ensure patients access to fair compensation for legitimate medical injuries, and reduce liability insurance premiums for health-care providers. Addressing just one of these issues is not sufficient.”5
And then there are the trial lawyers
Readers of OBG Management know all too well that the role of trial lawyers in medical liability reform has been to block meaningful reforms from passing and to repeal reforms currently in place. The Association of Trial Lawyers of America, now known as the American Association for Justice, tries to portray itself as defending vulnerable patients against a few bad apples. Its Web site (www.justice.org) points to recent National Practitioner Data Bank (NPDB) figures indicating that “just 6% of doctors are responsible for 58% of all negligence incidents. The civil justice system seeks to weed out those few doctors whose actions have such devastating impact on patients.”
The Web site includes these bullet points:
- 6% of doctors have been responsible for 58% of all malpractice payments since 1991
- 2% of doctors having three or more mal-practice payments were responsible for 33% of all payments
- 1% of doctors having four or more malprac-tice payments were responsible for 20% of all payments
- 82% of doctors have never had a medical malpractice payment.
Tell that to ObGyns, who, in 2012, paid an average of 12.4% of their gross income for liability insurance premiums in 2012, and nearly 60% of whom changed their practices based on the risk or fear of professional liability claims or litigation. And this despite the fact that 43.9% of claims were dropped or settled without any payment on behalf of the ObGyn.
Action at the state level
We need a federal solution, but since that isn’t within reach, we’re looking to the states for action. And there’s a lot of action in some states, including Connecticut, Florida, Georgia, Hawaii, Illinois, Iowa, Missouri, Oregon, Rhode Island, Tennessee, and Utah.
Advocates in these states are trying a number of different approaches, hoping that some type of meaningful reform will be signed into law. Here’s a sampling of what’s under way.
Connecticut
HB 6687, amend certificates of merit in medical liability actions. Status: April 1, 2013: Joint Committee on Judiciary hearing. The bill would eliminate the need for a detailed basis for the formation of an opinion and replace it with a lower threshold stating the appearance of one or more specific breaches of the prevailing professional standard of care.
In addition, HB 6687 would allow any expert who may testify in court to satisfy the certificate of merit requirement, but at trial the “expert,” in order to testify, needs to have the court determine him or her to be qualified to testify based on discovery and evidentiary issues that are decided at trial. This expert then could sign a certificate of merit but have the court determine that he or she is indeed not an expert for that case. HB 6687 delays the challenging of qualifications of an expert only after the completion of discovery, adding substantial time and cost to defending meritless suits. Finally, the bill allows for a second bite of the apple for cases that did not meet this watered down standard for certificate of merit and would eliminate the automatic dismissal of cases filed with inadequate certificates that did not meet the rules of the court.
SB 1154, amend Connecticut’s failure of suit statute to allow a plaintiff whose lawsuit was dismissed due to a failure to file a certificate of good faith as required by statute, to commence a new action.
HB 5229, limit noneconomic damages in medical liability cases to $250,000 for each health-care provider and institution per event, and $750,000 overall for each event.
HB 5270, establish peer-review panels in medical liability actions. The panels would consist of physicians, medical professionals, and individuals outside the medical profession who would review claims of alleged negligence and determine whether there is probable cause that the medical liability claims have been made in good faith prior to the action being referred to mandatory mediation.
SB 97, extend the statute of limitations in medical liability cases, allowing for an action to be brought no more than 10 years from the date of the act or omission that serves as the basis for the claim.
Florida
The Birth-Related Neurological Injury Compensation Association (NICA). NICA is a statutory organization that manages the compensation plan used to pay for the care of infants born with certain neurological injuries. This plan is available to eligible families statewide without litigation. By eliminating costly legal proceedings, and through professional management of its disbursements, NICA ensures that birth-injured infants receive the care they need while reducing the financial burden on medical providers and families. Defensive work continues on the NICA Board and trial bar.
HB 7015, expert witness. Status: March 28, 2013, the House Justice Appropriations Subcommittee reported favorably. This bill would adopt the Daubert standard for expert witness testimony. It provides that a witness qualified as an expert by knowledge, skill, experience, training, or education may testify in the form of an opinion as to the facts at issue in a case.
Georgia
HB 499, Provider Shield Act. Georgia is the first state to introduce legislation based on the American Medical Association’s model bill, “The Provider Shield Act,” which clarifies language in the Affordable Care Act by providing that a physician’s failure to comply with, or a breach of, any federal statute, regulation, program, guideline, or other provision shall not: (1) be admissible; (2) be used to determine the standard of care; or (3) be the legal basis for a presumption of negligence.
Status: Enacted May 6, 2013. The law prohibits the use of payer guidelines and quality criteria outlined in federal law as a legal basis for negligence or standard of care in determining medical liability. Physicians are concerned that without such protections, the medical profession could be exposed to charges of negligence that aren’t based on clinical standards or the patient’s unique medical needs. Implementation of any guideline by any public or private payor, or the establishment of any payment standard or reimbursement criteria under any federal laws or regulations related to health care, shall not be construed, without competent expert testimony establishing the appropriate standard of care, to establish a legal basis for negligence or the standard of care or duty of care owed by a health-care provider to a patient in any civil action for medical malpractice or product liability.
This first-of-its-kind legislation reinforces the concept that medical decisions should be based on a patient’s unique medical needs. HB 499 makes it clear that federal standards or guidelines designed to enhance access to high-quality health care cannot be used to invent new legal actions against physicians.
Hawaii
SB 1308, health-care provider benevolent gesture legislation.
Illinois
On March 22, 2013, several pieces of tort-reform legislation were re-referred to the House Committee on Rules, effectively killing the bills for the session. The House Speaker would have to choose to “release” any of the bills in order for them to move again; this is highly unlikely.
HB 138 would have deleted existing-venue language providing that an action may commence in any county if all defendants are nonresidents of the state, and replaced it with language providing that, if no defendants that are joined in good faith and with probable cause for the purpose of obtaining a judgment against them are residents of the state, an action may be commenced only in the county in which the transaction or some part thereof occurred out of which the cause of action arose.
HB 2220 and HB 2222 provided that, with respect to certain types of actions, for any defendant whose fault is less than 25% of the total fault attributable to the plaintiff, the defendants sued by the plaintiff, and any third-party defendant who could have been sued by the plaintiff (instead of any third-party defendant except the plaintiff’s employer), shall be severally liable for all other damages. In addition, these bills provided that, for any defendant whose fault is 25% or greater of the total fault attributable to the plaintiff, the defendants sued by the plaintiff, and any third-party defendants who could have been sued by the plaintiff (instead of any third-party defendants except the plaintiff’s employer), shall be jointly and severally liable for all other damages.
HB 2221 created requirements regarding qualifications, testimony, disclosure and compensation of expert testimony and standards for reviewing courts to follow in ruling on the admissibility of expert testimony.
Iowa
SSB 1054 and HSB 36, expert’s certificate of merit affidavit and noneconomic cap. These bills provide that in any medical liability action, the plaintiff is required, within 180 days of the defendant’s answer, to serve the defendant with an expert’s certificate of merit affidavit for each expert scheduled to testify. They also would limit noneconomic damage awards in medical liability cases to $1 million.
Missouri
HJR 6 proposes a constitutional amendment allowing the legislature to cap noneconomic damages in medical liability cases.
SJR 1 grants the legislature the power to limit, by statute, jury awards for noneconomic damages.
SB 64 changes the evidentiary standard in medical liability cases to “clear and convincing” for noneconomic damages.
Oregon
SB 483, early discussion and resolution. Status: Passed by the legislature. This bill establishes an early discussion and resolution (EDC) process within the Oregon Patient Safety Commission. This voluntary process is intended to facilitate open communication about all outcomes of care, including serious events, between the provider, health-care facility, and the patient. When an adverse health-care incident occurs, the patient, health-care provider or health-care facility where the incident occurred may file a notice of adverse health-care incident with the Commission. This notice triggers discussion of the health-care incident and, if appropriate, an offer of compensation. If discussion does not result in the resolution of the claim, the bill gives the parties the option of participating in Commission-facilitated mediation. The entire process is voluntary.
SJR 30, proposed amendment to constitution, $1 million limit on noneconomic awards in medical liability cases. Slated for next general election.
Rhode Island
HB 5380, apology bill. Status: Heard in House Judiciary Committee on March 27, 2013; no action was taken. This bill provides that statements by a health-care provider to a patient or to the patient’s family regarding the outcome of such patient’s medical care and treatment, such as an apology or expression of sympathy, shall be inadmissible as evidence or an admission of liability in any claim or action against the provider.
Tennessee
Joint and several liability. Status: On March 26, 2013, the House Civil Justice Subcommittee reported favorably. This bill would codify current state law by providing that if multiple defendants are found liable in a civil action governed by comparative fault, a defendant shall only be severally liable for the percentage of damages for which fault is attributed to such defendant by the trier of fact, and no defendant shall be held jointly liable for any damages.
SB 274, medical liability expert witness reform.
Utah
HB 135, rules, arbitration. Status: March 21, 2013, sent to Governor Gary Herbert for his approval. HB 135 provides that a party in a medical liability action or arbitration may not attempt to allocate fault to any health-care provider unless a certificate of compliance has been issued. HB 135 also requires that evidence from a medical review panel remain unreportable to a health-care facility or health insurance plan.
Summing up
Medical liability reform—the obvious need for it, the good reasons to do it, and the fact that it remains beyond reach—is a constant source of frustration among many ObGyns. Maybe Captain Sully can save the day.
How medical liability affects the ObGyn specialty
ACOG’s 2012 Survey on Professional Liability, our 11th survey since 1983, assessed the effects of professional liability litigation and insurance issues on the practice of obstetrics and gynecology.6 The survey, conducted under the direction of ACOG’s Vice President for Fellowship and Deputy Executive Vice President Albert Strunk, MD, JD, included segments on demographics, patient care, liability claims experience, and practice changes associated with the cost of liability insurance and the fear of litigation. The survey went to 32,238 Fellows and Junior Fellows. Of these, 9,006 completed the questionnaire. Here are major findings.
Provider profiles
A total of 72.5% of respondents provided both obstetric and gynecologic care, slightly lower than the percentage identified in the 2009 survey, which was 74.3%. Fewer than 7% of respondents provided obstetric care only; 19.8% provided gynecologic care only. Of those restricting their services to gynecology, 88.9% had previously offered obstetric care. The average age at which these physicians stopped practicing obstetrics was 49 years.
Cost of liability insurance
ObGyns spent an average of 12.4% of their gross income on liability insurance premiums in 2012, down from 18% in 2009.
How liability issues affected practice
Since the previous survey in 2009, 57.9% of respondents made one or more changes to their practice to mitigate the risk or fear of professional liability claims or litigation.
Obstetric practice. Among respondents who made changes to their obstetric practice, 27.4% decreased the number of high-risk patients they see, 23.8% increased the number of cesarean deliveries they perform, 18.9% stopped offering and performing vaginal birth after cesarean (VBAC), 11.5% reduced the total number of deliveries, and 6.2% stopped practicing obstetrics altogether.
Gynecologic practice. Respondents who changed their gynecologic practice cut back on surgical procedures (18.9%), stopped performing major gynecologic surgery (6.7%), and stopped performing all surgery (1.8%).
Other changes. Medical liability issues contributed to the decisions of 12.3% of respondents to choose salaried employment with a hospital, government, or other institution.
Claims experience
Obstetric claims were likely to involve a neurologically impaired infant (28.8%) as the primary allegation, followed by stillbirth or neonatal death (14.4%).
Other variables involved in obstetric claims included electronic fetal monitoring (20.9%), shoulder dystocia and/or brachial plexus injury (15.5%), and actions of ObGyn residents (11.4%).
Gynecologic claims. Survey respondents reported a total of 1,496 gynecologic claims. Major injury to the patient was the primary allegation of 29.1% of these claims. A delay in diagnosis or failure to diagnose was the second most common primary allegation (22.1%), followed by minor injury to the patient (20.7%).Of the claims involving a delayed or missed diagnosis, 41.8% involved cancer. Of these, breast cancer was the most frequent type of cancer (39.1%), followed by uterine cancer (20.3%), ovarian cancer (14.5%), and cervical cancer (10.9%).
Many gynecologic claims (44.4%) involved surgical complications arising from hysterectomy (28.7%) and laparoscopic procedures (14.6%).
Claims outcomes. A total of 43.9% of claims were dropped or settled without any payment on behalf of the ObGyn. Of these, 29.0% were dropped by the plaintiff, 11.2% were dismissed by the court, and 3.7% were settled without payment on behalf of the ObGyn.The average for all paid claims was $510,473.
The average payment for claims involving a neurologically impaired infant was $982,051. Other average payments for obstetric claims include $364,794 for “other infant injury–major” and $271,149 for stillbirth or neonatal death.
Average payments for gynecologic claims include $407,500 for a failure to diagnose breast cancer and $315,633 for “patient injury–major.”
Most challenging locales. It will come as no surprise to many readers that average medical liability payouts are especially high in six states:
New York - $677,866,050
Pennsylvania - $319,710,250
Illinois - $242,108,800
New Jersey - $221,170,750
Florida - $218,123,050
California - $215,519,200.
Fifty-eight percent of payouts nationwide were for female patients.7
Tell us what you think, at [email protected]. Please include your name and city and state.
It’s a conundrum. There seems to be no doubt about the need for medical liability reform—in fact, there is wide-spread support for it. And yet....
Four years after Captain Chesley “Sully” Sullenberger saved a planeload of passengers during an emergency landing—the “miracle on the Hudson”—he’s become a national champion of medical liability reform. In a recent interview with Politico, Sullenberger equated the 200,000 lives estimated to be lost each year due to medical errors to “20 jetliners crashing per week,” a situation he insists would close airports and ground flights until the problem was solved. But these 200,000 deaths cause little more than a ripple of concern, he claims.1
Among the solutions he proposes is “a whole different approach to reviewing medical errors, figuring out what’s behind them, not just blaming doctors and nurses.”1
Captain Sullenberger is discovering the difficult reality we’ve experienced for too many years: Solutions just don’t come very fast to medical liability reform, despite wide-spread support for it.
At the American Congress of Obstetricians and Gynecologists (ACOG), our campaign for medical liability reform has focused, as always, on patients, using the campaign line: “Who will delivery my baby?” ACOG supports caps on noneconomic damages and other reforms, such as those contained in the California Medical Injury Compensation Reform Act (MICRA), the gold standard for medical liability reform. We will continue to push for national MICRA reform until we’ve won that important protection for all ObGyns and their patients.
Until we reach that goal, we’re working to accomplish meaningful steps to liability reform where we can, including testing state alternatives. And our colleague organizations? Many of them, once insisting on federal adoption of MICRA or nothing at all, now actively support meaningful alternatives, too.
What do we want?
Proposals for tort reform, based on California’s MICRA statute, include:
- mandatory periodic payments of all future damages exceeding $100,000
- a $250,000 ceiling on noneconomic damage awards
- a requirement that claims must be filed within 2 years of the date by which the alleged injury reasonably should have been discovered but in no event more than 4 years from the time of the alleged injury. In the case of alleged injury to children under 4 years of age, claims must be filed by the child’s 8th birthday.
- limits on punitive damages, with 50% of punitive damage awards going to a state disciplinary fund
- limits on attorney contingency fees
- reductions in awards based on the amount paid from another source, such as health or disability insurance
- a requirement for “clear and convincing evidence” rather than the usual “preponderance of evidence” when a health-care professional who provided delivery services but not prenatal care is sued
- alternative systems for dispute resolution.
10 alternative reforms
Good ideas include:
1. Require a certificate of merit from the plaintiff
This proposal would require the plaintiff to file an affidavit with the court to demonstrate that the case has merit before the complaint can move forward. Certificates would necessitate the written opinion of a legally qualified health-care provider affirming that the defendant failed to meet the care standards that would be followed by a reasonably prudent health-care provider—and that this failure caused or directly contributed to the damages claimed.
2. Facilitate early settlement offers
Under this idea, a physician or hospital would be allowed to offer economic damages to an injured party without involving the courts. This offer would not constitute an admission of liability and would be inadmissible if a lawsuit were later filed in the case. Physicians would have an incentive to make a good-faith offer as early as possible after the injury is discovered, and patients would have an incentive to accept legitimate offers of compensation. Early-offer programs would require the injured party to meet a higher burden of proof for alleged negligence if that party chooses to reject the offer and file a lawsuit.
3. Create health-care courts
Health-care courts would allow for a bench or jury trial presided over by a specially trained judge to exclusively hear medical liability cases. Such courts have the potential to correct severe deficiencies in the current medical justice system and to reduce health-system errors and improve patient safety.
4. Allow a physician to say, “I’m sorry”
This proposal would encourage physicians to directly discuss errors and injuries with patients, to apologize and outline corrective action. Such discussions would be inadmissible if a patient later files a lawsuit.
5. Establish medical review panels
Any claim against a physician would be reviewed by a panel of experts who would provide an opinion on whether the physician failed to act within the relevant standards of care.
6. Require a claim to be screened and mediated
A plaintiff ’s claim would have to be evaluated by a screening panel before it could proceed to litigation. The panel would identify claims hat merit compensation and encourage early resolution of those claims. It also would encourage withdrawal or dismissal of non-meritorious claims.
7. Protect physicians who follow evidence-based guidelines
Health-care providers who follow guidelines based on solid evidence, and those who have legitimate justifications for departing from guidelines, would be protected from liability claims.
8. Allow the voluntary resolution of disputes
This proposal would motivate states to encourage the creation of other innovative systems to compensate individuals who are injured in the course of receiving health-care services.
9. Require expert witnesses to meet certain standards
This alternative would limit expert-witness standing to individuals who:
- are licensed and trained in the same specialty as the defendant
- have particular expertise in the disease process or procedure performed in the case
- have been in active medical practice in the same specialty as the defendant within 5 years of the claim or who have been taught at an accredited medical school on the care and type of treatment at issue.
10. Create catastrophic injury systems
These systems would establish a fund for individuals who have experienced bad outcomes. Birth injury funds are an example of this model.
Who’s on our side?
Congressional policy wonks give liability reform a thumbs up
In early 2010, the Medicare Payment Advisory Commission (MedPAC), a nonpartisan advisory counsel to the US Congress, identified three important ways that our current malpractice system harms the Medicare program and Medicare beneficiaries, the aged, and disabled:
- Medicare payments to providers include some liability costs (folded into hospital diagnosis-related group [DRG] payments; factored into physician fee schedule calculation)
- Defensive medicine drives up costs for Medicare
- Malpractice impairs the quality and safety of care to beneficiaries. That is, the current system does not improve patient safety.
MedPAC staff recommended that the commissioners urge Congress to pass government-subsidized malpractice reinsurance for providers who meet certain safety criteria or create a federal administrative adjudication process. The commissioners expressed an interest in alternatives to address the costs of medical malpractice, including ways to encourage states and providers to address medical malpractice in a manner most appropriate for them. However, when MedPAC returned to this topic at its next meeting later the same year, the commissioners mentioned medical liability only to dismiss it as an incidental issue in opening remarks.
The Congressional Budget Office (CBO) estimates that medical malpractice costs our health-care system $35 billion in direct costs, with billions more as a result of defensive medicine.
CBO has scored these medical liability reform proposals as providing significant savings to our federal budget:
- a $250,000 cap on subjective, noneconomic damages (with no limit on economic damages)
- collateral source rule allowing evidence of outside payments to be submitted in court
- a ban on subrogation by certain collateral sources
- caps on attorney contingency fees
- periodic payments of future damages
- a reasonable statute of limitations.
In addition, in 2011, CBO scored comprehensive medical liability reform as saving the federal government $62.4 billion over 10 years. As longtime Illinois Senator Everett Dirksen was known to say, “A billion here, a billion there, and pretty soon you’re talking real money.”
Many Republican congressional leaders “walk the walk”
Republicans have long claimed medical liability reform as their issue. And they walk the walk.
Representative Phil Gingrey, MD, of Georgia, an ACOG Fellow, has led the medical liability reform fight on Capitol Hill for a number of years. His bill, the Protecting Access to Healthcare Act (HR 5), which would have brought MICRA to the national level, was repeatedly passed by the Republican majority of the House of Representatives, only to be ignored by the Democrats controlling the Senate.
Again this year, Dr. Gingrey introduced legislation to protect physicians from unexpected liability. His Standard of Care Protection Act (HR 1473) would ensure that provisions of the Affordable Care Act (ACA) cannot be used to create new causes of action against medical professionals. HR 1473 would ensure that Medicare, Medicaid, and other federal programs that establish government standards and guidelines for health-care providers cannot be used to create new causes of action.
Federal health-care programs are changing to ensure that payment reflects quality of care. As a result, new payment rules, guidelines, and standards are being written into federal laws and regulations. HR 1473 would make clear that these cannot be used to define the applicable standard of care or duty of care in a medical liability lawsuit.
ACOG supports Dr. Gingrey’s bill, as well as a second, companion approach that would ensure that ObGyns who follow guidelines and standards of care developed by their medical society are protected from liability, with sensible exceptions for egregious harm and negligence.
Representative Charlie Dent, Republican of Pennsylvania, also has introduced ACOG-supported medical liability legislation. The Health Care Safety Net Enhancement Act (HR 36) would provide federal liability protection for physicians providing care under the Emergency Medical Treatment and Active Labor Act (EMTALA). HR 36 is commonly referred to as Good Samaritan legislation, intended to protect doctors who rush to the aid of a sick individual. The likelihood of any of these bills getting enacted into law is slim. Even some conservative Republicans oppose federal liability reform as an intrusion into states’ rights.
Some Democrats have said good things
In his proposed budget for fiscal year 2012, President Barack Obama asked Congress for funding to address medical liability issues.
He proposed “to restrain health-care costs” through “a more aggressive effort to reform our medical malpractice system to reduce defensive medicine, promote patient safety, and improve patient outcomes.” He encouraged Republicans to work constructively with him on medical malpractice as part of an overall effort to restrain health-care costs.2
The President asked Congress for “$250 million in grants to states to reform the way they resolve medical malpractice disputes,” including health courts, safe harbors, early disclosure and offer, and other legal reforms such as joint and several liability and collateral source rules.2
Congress never funded the President’s request.
President Obama repeated his request in his fiscal year 2013 budget proposal. Congress didn’t fund it then, either.
Earlier, in March 2009, in remarks to the Business Roundtable, President Obama noted that “the cost issue is the thing that we actually think is the big driver in this whole debate...things like comparative effectiveness, health IT, prevention, figuring out how our reimbursement structures are designed under Medicare and Medicaid. Medical liability issues—I think all those things have to be on the table.”3
In an interview the same month, Senator Ron Wyden, Democrat of Oregon, said, “I think [medical liability reform is] an essential piece for there to be enduring reform, reform that will stick and will get a significant bipar-tisan vote in the United States Senate.”4
Senator Wyden’s Healthy Americans Act (S 391) included incentives to get states to enact malpractice reforms as a key to overhauling the health-care system.
Also in March 2009, Representative Rob Andrews, Democrat of New Jersey, Chairman of the House Education and Labor, Health Subcommittee, pointed to the need for medical liability reform.
“It’s hard for me to imagine a [health-care reform] result that gets to the president’s desk that doesn’t deal with the medical mal-practice issue in some way.”4
And Senator Max Baucus, Democrat of Montana, Chairman of the Senate Finance Committee, proposed providing states grant money to develop alternative litigation models, such as encouraging disclosure and compensation in the case of error, and establishing health courts whose judges have health-care expertise.
As early as May 2006, President Obama (then a Senator from Illinois) and Senator Hillary Rodham Clinton, Democrat of New York, urged a focus on patient safety.
“Instead of focusing on the few areas of intense disagreement,” they wrote in the New England Journal of Medicine, “such as the possibility of mandating caps on the financial damages awarded to patients, we believe that the discussion should center on a more fundamental issue: the need to improve patient safety....”
“To improve both patient safety and the medical liability climate, the tort system must achieve four goals: reduce the rates of preventable patient injuries, promote open communication between physicians and patients, ensure patients access to fair compensation for legitimate medical injuries, and reduce liability insurance premiums for health-care providers. Addressing just one of these issues is not sufficient.”5
And then there are the trial lawyers
Readers of OBG Management know all too well that the role of trial lawyers in medical liability reform has been to block meaningful reforms from passing and to repeal reforms currently in place. The Association of Trial Lawyers of America, now known as the American Association for Justice, tries to portray itself as defending vulnerable patients against a few bad apples. Its Web site (www.justice.org) points to recent National Practitioner Data Bank (NPDB) figures indicating that “just 6% of doctors are responsible for 58% of all negligence incidents. The civil justice system seeks to weed out those few doctors whose actions have such devastating impact on patients.”
The Web site includes these bullet points:
- 6% of doctors have been responsible for 58% of all malpractice payments since 1991
- 2% of doctors having three or more mal-practice payments were responsible for 33% of all payments
- 1% of doctors having four or more malprac-tice payments were responsible for 20% of all payments
- 82% of doctors have never had a medical malpractice payment.
Tell that to ObGyns, who, in 2012, paid an average of 12.4% of their gross income for liability insurance premiums in 2012, and nearly 60% of whom changed their practices based on the risk or fear of professional liability claims or litigation. And this despite the fact that 43.9% of claims were dropped or settled without any payment on behalf of the ObGyn.
Action at the state level
We need a federal solution, but since that isn’t within reach, we’re looking to the states for action. And there’s a lot of action in some states, including Connecticut, Florida, Georgia, Hawaii, Illinois, Iowa, Missouri, Oregon, Rhode Island, Tennessee, and Utah.
Advocates in these states are trying a number of different approaches, hoping that some type of meaningful reform will be signed into law. Here’s a sampling of what’s under way.
Connecticut
HB 6687, amend certificates of merit in medical liability actions. Status: April 1, 2013: Joint Committee on Judiciary hearing. The bill would eliminate the need for a detailed basis for the formation of an opinion and replace it with a lower threshold stating the appearance of one or more specific breaches of the prevailing professional standard of care.
In addition, HB 6687 would allow any expert who may testify in court to satisfy the certificate of merit requirement, but at trial the “expert,” in order to testify, needs to have the court determine him or her to be qualified to testify based on discovery and evidentiary issues that are decided at trial. This expert then could sign a certificate of merit but have the court determine that he or she is indeed not an expert for that case. HB 6687 delays the challenging of qualifications of an expert only after the completion of discovery, adding substantial time and cost to defending meritless suits. Finally, the bill allows for a second bite of the apple for cases that did not meet this watered down standard for certificate of merit and would eliminate the automatic dismissal of cases filed with inadequate certificates that did not meet the rules of the court.
SB 1154, amend Connecticut’s failure of suit statute to allow a plaintiff whose lawsuit was dismissed due to a failure to file a certificate of good faith as required by statute, to commence a new action.
HB 5229, limit noneconomic damages in medical liability cases to $250,000 for each health-care provider and institution per event, and $750,000 overall for each event.
HB 5270, establish peer-review panels in medical liability actions. The panels would consist of physicians, medical professionals, and individuals outside the medical profession who would review claims of alleged negligence and determine whether there is probable cause that the medical liability claims have been made in good faith prior to the action being referred to mandatory mediation.
SB 97, extend the statute of limitations in medical liability cases, allowing for an action to be brought no more than 10 years from the date of the act or omission that serves as the basis for the claim.
Florida
The Birth-Related Neurological Injury Compensation Association (NICA). NICA is a statutory organization that manages the compensation plan used to pay for the care of infants born with certain neurological injuries. This plan is available to eligible families statewide without litigation. By eliminating costly legal proceedings, and through professional management of its disbursements, NICA ensures that birth-injured infants receive the care they need while reducing the financial burden on medical providers and families. Defensive work continues on the NICA Board and trial bar.
HB 7015, expert witness. Status: March 28, 2013, the House Justice Appropriations Subcommittee reported favorably. This bill would adopt the Daubert standard for expert witness testimony. It provides that a witness qualified as an expert by knowledge, skill, experience, training, or education may testify in the form of an opinion as to the facts at issue in a case.
Georgia
HB 499, Provider Shield Act. Georgia is the first state to introduce legislation based on the American Medical Association’s model bill, “The Provider Shield Act,” which clarifies language in the Affordable Care Act by providing that a physician’s failure to comply with, or a breach of, any federal statute, regulation, program, guideline, or other provision shall not: (1) be admissible; (2) be used to determine the standard of care; or (3) be the legal basis for a presumption of negligence.
Status: Enacted May 6, 2013. The law prohibits the use of payer guidelines and quality criteria outlined in federal law as a legal basis for negligence or standard of care in determining medical liability. Physicians are concerned that without such protections, the medical profession could be exposed to charges of negligence that aren’t based on clinical standards or the patient’s unique medical needs. Implementation of any guideline by any public or private payor, or the establishment of any payment standard or reimbursement criteria under any federal laws or regulations related to health care, shall not be construed, without competent expert testimony establishing the appropriate standard of care, to establish a legal basis for negligence or the standard of care or duty of care owed by a health-care provider to a patient in any civil action for medical malpractice or product liability.
This first-of-its-kind legislation reinforces the concept that medical decisions should be based on a patient’s unique medical needs. HB 499 makes it clear that federal standards or guidelines designed to enhance access to high-quality health care cannot be used to invent new legal actions against physicians.
Hawaii
SB 1308, health-care provider benevolent gesture legislation.
Illinois
On March 22, 2013, several pieces of tort-reform legislation were re-referred to the House Committee on Rules, effectively killing the bills for the session. The House Speaker would have to choose to “release” any of the bills in order for them to move again; this is highly unlikely.
HB 138 would have deleted existing-venue language providing that an action may commence in any county if all defendants are nonresidents of the state, and replaced it with language providing that, if no defendants that are joined in good faith and with probable cause for the purpose of obtaining a judgment against them are residents of the state, an action may be commenced only in the county in which the transaction or some part thereof occurred out of which the cause of action arose.
HB 2220 and HB 2222 provided that, with respect to certain types of actions, for any defendant whose fault is less than 25% of the total fault attributable to the plaintiff, the defendants sued by the plaintiff, and any third-party defendant who could have been sued by the plaintiff (instead of any third-party defendant except the plaintiff’s employer), shall be severally liable for all other damages. In addition, these bills provided that, for any defendant whose fault is 25% or greater of the total fault attributable to the plaintiff, the defendants sued by the plaintiff, and any third-party defendants who could have been sued by the plaintiff (instead of any third-party defendants except the plaintiff’s employer), shall be jointly and severally liable for all other damages.
HB 2221 created requirements regarding qualifications, testimony, disclosure and compensation of expert testimony and standards for reviewing courts to follow in ruling on the admissibility of expert testimony.
Iowa
SSB 1054 and HSB 36, expert’s certificate of merit affidavit and noneconomic cap. These bills provide that in any medical liability action, the plaintiff is required, within 180 days of the defendant’s answer, to serve the defendant with an expert’s certificate of merit affidavit for each expert scheduled to testify. They also would limit noneconomic damage awards in medical liability cases to $1 million.
Missouri
HJR 6 proposes a constitutional amendment allowing the legislature to cap noneconomic damages in medical liability cases.
SJR 1 grants the legislature the power to limit, by statute, jury awards for noneconomic damages.
SB 64 changes the evidentiary standard in medical liability cases to “clear and convincing” for noneconomic damages.
Oregon
SB 483, early discussion and resolution. Status: Passed by the legislature. This bill establishes an early discussion and resolution (EDC) process within the Oregon Patient Safety Commission. This voluntary process is intended to facilitate open communication about all outcomes of care, including serious events, between the provider, health-care facility, and the patient. When an adverse health-care incident occurs, the patient, health-care provider or health-care facility where the incident occurred may file a notice of adverse health-care incident with the Commission. This notice triggers discussion of the health-care incident and, if appropriate, an offer of compensation. If discussion does not result in the resolution of the claim, the bill gives the parties the option of participating in Commission-facilitated mediation. The entire process is voluntary.
SJR 30, proposed amendment to constitution, $1 million limit on noneconomic awards in medical liability cases. Slated for next general election.
Rhode Island
HB 5380, apology bill. Status: Heard in House Judiciary Committee on March 27, 2013; no action was taken. This bill provides that statements by a health-care provider to a patient or to the patient’s family regarding the outcome of such patient’s medical care and treatment, such as an apology or expression of sympathy, shall be inadmissible as evidence or an admission of liability in any claim or action against the provider.
Tennessee
Joint and several liability. Status: On March 26, 2013, the House Civil Justice Subcommittee reported favorably. This bill would codify current state law by providing that if multiple defendants are found liable in a civil action governed by comparative fault, a defendant shall only be severally liable for the percentage of damages for which fault is attributed to such defendant by the trier of fact, and no defendant shall be held jointly liable for any damages.
SB 274, medical liability expert witness reform.
Utah
HB 135, rules, arbitration. Status: March 21, 2013, sent to Governor Gary Herbert for his approval. HB 135 provides that a party in a medical liability action or arbitration may not attempt to allocate fault to any health-care provider unless a certificate of compliance has been issued. HB 135 also requires that evidence from a medical review panel remain unreportable to a health-care facility or health insurance plan.
Summing up
Medical liability reform—the obvious need for it, the good reasons to do it, and the fact that it remains beyond reach—is a constant source of frustration among many ObGyns. Maybe Captain Sully can save the day.
How medical liability affects the ObGyn specialty
ACOG’s 2012 Survey on Professional Liability, our 11th survey since 1983, assessed the effects of professional liability litigation and insurance issues on the practice of obstetrics and gynecology.6 The survey, conducted under the direction of ACOG’s Vice President for Fellowship and Deputy Executive Vice President Albert Strunk, MD, JD, included segments on demographics, patient care, liability claims experience, and practice changes associated with the cost of liability insurance and the fear of litigation. The survey went to 32,238 Fellows and Junior Fellows. Of these, 9,006 completed the questionnaire. Here are major findings.
Provider profiles
A total of 72.5% of respondents provided both obstetric and gynecologic care, slightly lower than the percentage identified in the 2009 survey, which was 74.3%. Fewer than 7% of respondents provided obstetric care only; 19.8% provided gynecologic care only. Of those restricting their services to gynecology, 88.9% had previously offered obstetric care. The average age at which these physicians stopped practicing obstetrics was 49 years.
Cost of liability insurance
ObGyns spent an average of 12.4% of their gross income on liability insurance premiums in 2012, down from 18% in 2009.
How liability issues affected practice
Since the previous survey in 2009, 57.9% of respondents made one or more changes to their practice to mitigate the risk or fear of professional liability claims or litigation.
Obstetric practice. Among respondents who made changes to their obstetric practice, 27.4% decreased the number of high-risk patients they see, 23.8% increased the number of cesarean deliveries they perform, 18.9% stopped offering and performing vaginal birth after cesarean (VBAC), 11.5% reduced the total number of deliveries, and 6.2% stopped practicing obstetrics altogether.
Gynecologic practice. Respondents who changed their gynecologic practice cut back on surgical procedures (18.9%), stopped performing major gynecologic surgery (6.7%), and stopped performing all surgery (1.8%).
Other changes. Medical liability issues contributed to the decisions of 12.3% of respondents to choose salaried employment with a hospital, government, or other institution.
Claims experience
Obstetric claims were likely to involve a neurologically impaired infant (28.8%) as the primary allegation, followed by stillbirth or neonatal death (14.4%).
Other variables involved in obstetric claims included electronic fetal monitoring (20.9%), shoulder dystocia and/or brachial plexus injury (15.5%), and actions of ObGyn residents (11.4%).
Gynecologic claims. Survey respondents reported a total of 1,496 gynecologic claims. Major injury to the patient was the primary allegation of 29.1% of these claims. A delay in diagnosis or failure to diagnose was the second most common primary allegation (22.1%), followed by minor injury to the patient (20.7%).Of the claims involving a delayed or missed diagnosis, 41.8% involved cancer. Of these, breast cancer was the most frequent type of cancer (39.1%), followed by uterine cancer (20.3%), ovarian cancer (14.5%), and cervical cancer (10.9%).
Many gynecologic claims (44.4%) involved surgical complications arising from hysterectomy (28.7%) and laparoscopic procedures (14.6%).
Claims outcomes. A total of 43.9% of claims were dropped or settled without any payment on behalf of the ObGyn. Of these, 29.0% were dropped by the plaintiff, 11.2% were dismissed by the court, and 3.7% were settled without payment on behalf of the ObGyn.The average for all paid claims was $510,473.
The average payment for claims involving a neurologically impaired infant was $982,051. Other average payments for obstetric claims include $364,794 for “other infant injury–major” and $271,149 for stillbirth or neonatal death.
Average payments for gynecologic claims include $407,500 for a failure to diagnose breast cancer and $315,633 for “patient injury–major.”
Most challenging locales. It will come as no surprise to many readers that average medical liability payouts are especially high in six states:
New York - $677,866,050
Pennsylvania - $319,710,250
Illinois - $242,108,800
New Jersey - $221,170,750
Florida - $218,123,050
California - $215,519,200.
Fifty-eight percent of payouts nationwide were for female patients.7
Tell us what you think, at [email protected]. Please include your name and city and state.
1.Cheney K. ‘Miracle’ pilot on mission against medical errors. Politico.com. August 1, 2013. http://www.politico.com/story/2013/08/sully-sullenberger-mission-medical-erros-95009.html. Accessed August 6, 2013.
2.Office of Management and Budget. Fiscal Year 2012 Budget of the US Government. http://www.whitehouse.gov/files/documents/budget_2012.pdf. Accessed August 8, 2013.
3.Obama’s remarks to the Business Roundtable, March 12, 2009. Wall Street Journal: Washington Wire. http://blogs.wsj.com/washwire/2009/03/12/obamas-remarks-to-the-business-roundtable/. Accessed August 8, 2013.
4.Werner E. Health debate could spur malpractice changes. Salt Lake Tribune. March 17, 2009. http://www.sltrib.com/ci_11933162. Accessed August 8, 2013.
5.Clinton HR, Obama B. Perspective: Making patient safety the centerpiece of medical liability reform. N Engl J Med. 2006;354(21):2205–2208.
6.American Congress of Obstetricians and Gynecologists. Survey on Professional Liability. 2012 Survey Results. http://www.acog.org/About_ACOG/ACOG_Departments/Professional_Liability/2012_Survey_Results. Accessed August 7, 2013.
7. Latner AW. Six states account for 50% of malpractice payouts. Clinical Advisor. April 17, 2012. http://www.clinicaladvisor.com/six-states-account-for-50-of-malpractice-payouts/article/236931. Accessed August 7, 2013.
1.Cheney K. ‘Miracle’ pilot on mission against medical errors. Politico.com. August 1, 2013. http://www.politico.com/story/2013/08/sully-sullenberger-mission-medical-erros-95009.html. Accessed August 6, 2013.
2.Office of Management and Budget. Fiscal Year 2012 Budget of the US Government. http://www.whitehouse.gov/files/documents/budget_2012.pdf. Accessed August 8, 2013.
3.Obama’s remarks to the Business Roundtable, March 12, 2009. Wall Street Journal: Washington Wire. http://blogs.wsj.com/washwire/2009/03/12/obamas-remarks-to-the-business-roundtable/. Accessed August 8, 2013.
4.Werner E. Health debate could spur malpractice changes. Salt Lake Tribune. March 17, 2009. http://www.sltrib.com/ci_11933162. Accessed August 8, 2013.
5.Clinton HR, Obama B. Perspective: Making patient safety the centerpiece of medical liability reform. N Engl J Med. 2006;354(21):2205–2208.
6.American Congress of Obstetricians and Gynecologists. Survey on Professional Liability. 2012 Survey Results. http://www.acog.org/About_ACOG/ACOG_Departments/Professional_Liability/2012_Survey_Results. Accessed August 7, 2013.
7. Latner AW. Six states account for 50% of malpractice payouts. Clinical Advisor. April 17, 2012. http://www.clinicaladvisor.com/six-states-account-for-50-of-malpractice-payouts/article/236931. Accessed August 7, 2013.
- ACOG proposals for reform
- Action at the state level
- How medical liability affects the ObGyn specialty
ACOG to legislators: Partnership, not interference
Who’s in charge here?
It’s a legitimate question being asked by more physicians in all areas of the country as they struggle to provide good quality care. Yes, physicians face longstanding payment and coverage issues, regulations, and the insurance bureaucracy. But more and more often, physicians are struggling to care for their patients in the face of legislative interference that reaches right into their exam rooms. Who’s in charge here, indeed?
In this article, I detail several examples of legislative interference and describe the response of the American Congress of Obstetricians and Gynecologists (ACOG). I also detail a very healthy partnership ACOG has undertaken with the US Department of Health and Human Services (HHS) and the March of Dimes to end early elective deliveries before 39 weeks of gestation.
Physician gag law passes in Florida
State lawmakers in Florida have decided that physicians should no longer ask about guns in the home when performing a child wellness exam. The use of bike helmets and exposure to secondhand smoke are childhood health concerns worth mentioning, but the importance of keeping guns unloaded and locked away is not.
Under the Firearm Owners’ Privacy Act, enacted in 2011, physicians in Florida could be fined or imprisoned for initiating this conversation, and could be charged with a third-degree felony punishable by a fine of up to $5 million. Thanks to public pushback, the law was amended to remove the criminal penalty. Instead, patients who feel “harassed” by their physicians’ questions about gun safety can complain to the Florida Board of Medicine, which can take disciplinary action against an offending physician.
In November 2012, ACOG joined an amicus brief in the case of Wollschlaeger v the State of Florida, asking the court to overturn the Florida bill, now known as the “physician gag law,” challenging, in part, the government’s right to interfere with a physician’s freedom of speech.
In another example of legislative interference, energy production politics gets in the way of doctors sharing relevant medical information with their patients. Four states—Colorado, Ohio, Pennsylvania, and Texas—prohibit physicians from disclosing information about exposure to chemicals used in hydraulic fracturing, or fracking. Scientific evidence shows that exposure to the chemicals used in fracking can result in a spectrum of health-care problems, from headaches to cancer. Can doctors talk about this with their patients? Not in these states.
While some states are trying to gag physicians by limiting what they can talk about with their patients, legislators in other states are considering requiring physicians to read, or offer to read, scripts to all patients who might have a terminal illness about end-of-life care options. Laws were enacted in California (2008) and New York (2011) to do just that. ObGyns are too familiar with legislatively mandated scripts; we know how inappropriate they are.
According to the Guttmacher Institute, in 2013, a number of states require abortion providers to read a script or provide written materials to patients seeking abortions; often these scripts contain medically inaccurate information. Twelve states require the physician to “inform” the patient about the ability of the fetus to feel pain, five states require the physician to claim that personhood begins at conception, and five states require doctors to say that abortion increases the risk of breast cancer. Six states require inaccurate information on the effects of abortion on future fertility.1
Serious penalties usually accompany these laws—financial fines, loss of licensure, and jail time. These and other legislative efforts infringe on physicians’ freedom of speech and force physicians to make terrible choices: Do you risk criminal prosecution or do you give your patient scientifically accurate and complete information? Do you adhere to your professional obligation to your patients, and risk putting your professional career on the line?
CLICK HERE to read other insightful articles by Ms. DiVenere.
Women’s reproductive health in the firing line
Nowhere is legislative interference more rampant than in the world of women’s health care. Over the past 2 years, an unprecedented number of bills have been introduced in the US Congress and statehouses restricting access to care for women and placing inappropriate requirements on physicians. The year 2011 was record-breaking in terms of abortion restrictions in the states, with 92 restrictions enacted.
In 2012, 42 states and the District of Columbia enacted 122 reproductive health provisions, one-third of them related to abortion restrictions. Forty-three new laws in 19 states were passed that restrict access to abortion. More than half of these new laws came from six states: Arizona was first with seven anti-abortion restrictions. Kansas, Louisiana, Oklahoma, South Dakota, and Wisconsin all had at least three.
In 2013, there have already been bills introduced in the US Congress and in the states that would:
- prohibit Title X family planning funds from going to clinics that provide abortions or prohibit funds from going to other entities that perform abortions (US Congress)
- repeal the Affordable Care Act, including the insurance protections and preventive services provisions that ACOG supports (US Congress)
- ban medical abortion (Mississippi)
- require women to undergo transvaginal ultrasound before having an abortion (Michigan)
- prohibit abortion after detection of a fetal heartbeat (at least three states: Arkansas, North Dakota, and Wyoming).
Few, if any, of these proposals are based on medical science. In fact, many of them run contrary to science and good patient-care principles. And although most of these efforts focus on reducing access to reproductive health care, including abortions, legislative interference is an issue of concern to physicians of all specialties, regardless of individual positions on life and choice.
What the medical community is doing
The American Medical Association (AMA) has made clear, consistent with the direction of its House of Delegates, that it fully opposes political interference in the patient-physician relationship. In 2012, the AMA unveiled its “Protect the sanctity of the patient-physician relationship” campaign with a panel that included Dr. Erin Tracy, chair of the Massachusetts Section of ACOG; Dr. Tim Bartholow, chief medical officer of the Wisconsin Medical Society; and Dr. H. Garry Gardner, chair of the American Academy of Pediatrics’ (AAP) Council on Injury, Violence, and Poison Prevention Executive Committee.
The AMA’s campaign is designed to educate physicians and to work with state medical societies and specialties to “articulate a compelling and comprehensive legal foundation to oppose legislation that encroaches on the sanctity of the patient-physician relationship.”
ACOG’s leadership has directly and forcefully pushed back on legislative encroachment. In 2012, ACOG Executive Vice President Hal C. Lawrence III, MD, and the executive leadership of the American Academy of Family Physicians (AAFP), AAP, the American College of Physicians, and the American College of Surgeons issued a joint statement that was published in the New England Journal of Medicine against legislative interference in the exam room.2
In addition, ACOG President James T. Breeden, MD, has written eight oped pieces, letters to the editor, and other public statements in venues with far and important reach, including the New York Times, USA Today, and Capitol Hill dailies (see the box). ACOG has also issued “Rapid Responses” to counter inaccurate statements about women’s health made in the media or on the campaign trail by state or national politicians.
In a paid ad message to the National Conference on State Legislatures (NCSL), which the NCSL refused to run, Dr. Breeden said, in part:
- Because we stand firmly for access to needed care, we also stand firmly against legislative interference with the patient-physician relationship. There’s only room for two people in our exam rooms: the patient and the caregiver. Lawmakers get in the way of good patient care when they try to force women to undergo transvaginal ultrasounds or other unnecessary medical procedures; when they try to close health clinics for specious reasons; or when they try to tell women that legislators know best.
Lawmakers can and do play a vitally productive and important role in ensuring public health. Lawmakers should not, however, attempt to define, mandate, or prohibit medical practices or require doctors to read a government script to their patients.
As ObGyns visit with state and federal legislators this year, our message is simple: Partnership with lawmakers, yes. Legislative interference, no.
Our campaign makes the point that there are a number of legitimate roles that state and federal governments play in public health. We welcome opportunities to partner with legislators on important women’s health-care needs. We draw the line at legislative interference of all stripes.
Here are just a few examples of ACOG’s many statements on behalf of women’s reproductive health
USA Today – Letter to the editor – May 21, 2012
“Politicians should not be legislating the practice of medicine or the doctor-patient relationship. We all need to speak up and take action when legislators pretend they know what’s best for women and their physicians.” —ACOG President James T. Breeden, MD
New York Times – Letter to the editor – June 4, 2012
“Politicians were not elected to, nor should they, legislate the practice of medicine or dictate the parameters of the doctor-patient relationship. Our message to politicians is unequivocal: Get out of our exam rooms.” —ACOG President James T. Breeden, MD
“Universal access to contraception could be a lifesaver” – Las Vegas Review Journal – July 22, 2012
“Contraception is a basic and essential element of women’s preventive health care and a basic public health necessity.” —ACOG President James T. Breeden, MD
ACOG Rapid Response to Rep. Todd Akin’s August 19, 2012 statement on “legitimate rape” – Issued August 20, 2012
“Absolutely no veracity to the claim … A woman who is raped has no control over ovulation, fertilization, or implantation of a fertilized egg. To suggest otherwise contradicts basic biological truths.”
ACOG Rapid Response to Rep. Joe Walsh’s October 18, 2012, statement that “Technology has advanced to the point that abortions are never needed to save the health or life of a mother” – Issued October 19, 2012
“Abortions are necessary in a number of circumstances to save the life of a woman or to preserve her health.”
A meaningful partnership: Strong Start
ACOG was invited to partner with the HHS and the March of Dimes on an initiative designed to bring about a meaningful and lasting improvement in maternity care: ending early elective deliveries before 39 weeks’ gestation. At the press conference announcing this partnership on the Strong Start initiative, Dr. Lawrence stood with HHS Secretary Kathleen Sebelius and said, in part:
- An ObGyn’s job is one of the most rewarding jobs on the planet, bringing little babies into the world. This job carries enormous responsibilities, too, ensuring the highest levels of health and safety for every mom and baby.
- The American College of Obstetricians and Gynecologists is proud to partner with the Department of Health and Human Services and the March of Dimes on one of the most certain ways of helping babies get a good start in life: Babies should not be delivered earlier than 39 weeks, unless pregnancy complications require otherwise to keep mother and child safe.
- Such a simple change, but one that can tremendously benefit children, families, our health system, and our society.
- Our joint initiative will help bring this important information to women and physicians across the nation, and has enormous potential to make a real and lasting change in how we care for expectant moms, and more importantly, how expectant moms expect us to care for them.
The Strong Start initiative is an all-too-rare example of a wonderful partnership between government, medicine, and the public to lead and create important change. This initiative goes far beyond the original press conference. Dr. Lawrence and other leaders have participated in webinars and interviews to spread the word. ACOG has developed patient education materials tailored to the message of no early elective deliveries before 39 weeks unless there is a maternal or fetal medical indication. Strong Start has provided funding to innovative maternity care models, including centering and pregnancy medical homes.
Earlier this year, Dr. Lawrence convened a Strong Start summit of the heads of the American Hospital Association, AAFP, AAP, the American Women’s Health and Neonatal Nurses Association, the American College of Nurse Midwives, the March of Dimes, and our federal partners, the Centers for Medicare and Medicaid Services and the Center for Medicare and Medicaid Innovation.
This one-day summit had a clear goal: gain unanimous agreement and commitment from the maternal care community to move our clinical knowledge into practice, ending nonmedically indicated early elective deliveries before 39 weeks.
Since 1979, ACOG has emphasized that labor should be induced “when the benefits of delivery to the fetus or the mother exceed the benefits of continuing the pregnancy,” and that pregnancies should be maintained until at least 39 weeks unless medical indications make early delivery necessary. This guidance was based on sound clinical knowledge in 1979, and today’s data are only more compelling. Somehow, however, early elective deliveries are still common and, for a variety of reasons, usually not related to infant or maternal health. This Strong Start summit is our specialty’s way of leading through partnership to encourage every maternity hospital in America to have in place a practice policy supporting no nonmedically indicated early elective deliveries before 39 weeks.
In many important ways, Strong Start is an example of the best that partnership with government and our colleagues has to offer.
The difference between partnership and interference is easy to see. That’s why we say: Partnership, yes. Interference, no.
We want to hear from you! Tell us what you think.
1. Guttmacher Institute. State Policies in Brief: Counseling and Waiting Period for Abortion. New York, NY, and Washington, DC: Guttmacher Institute; 2013.
2. Weinberger SE, Lawrence HC, III, Henley DE, et al. Legislative interference with the patient-physician relationship. N Engl J Med. 2012;367(16):1557-1559.
Who’s in charge here?
It’s a legitimate question being asked by more physicians in all areas of the country as they struggle to provide good quality care. Yes, physicians face longstanding payment and coverage issues, regulations, and the insurance bureaucracy. But more and more often, physicians are struggling to care for their patients in the face of legislative interference that reaches right into their exam rooms. Who’s in charge here, indeed?
In this article, I detail several examples of legislative interference and describe the response of the American Congress of Obstetricians and Gynecologists (ACOG). I also detail a very healthy partnership ACOG has undertaken with the US Department of Health and Human Services (HHS) and the March of Dimes to end early elective deliveries before 39 weeks of gestation.
Physician gag law passes in Florida
State lawmakers in Florida have decided that physicians should no longer ask about guns in the home when performing a child wellness exam. The use of bike helmets and exposure to secondhand smoke are childhood health concerns worth mentioning, but the importance of keeping guns unloaded and locked away is not.
Under the Firearm Owners’ Privacy Act, enacted in 2011, physicians in Florida could be fined or imprisoned for initiating this conversation, and could be charged with a third-degree felony punishable by a fine of up to $5 million. Thanks to public pushback, the law was amended to remove the criminal penalty. Instead, patients who feel “harassed” by their physicians’ questions about gun safety can complain to the Florida Board of Medicine, which can take disciplinary action against an offending physician.
In November 2012, ACOG joined an amicus brief in the case of Wollschlaeger v the State of Florida, asking the court to overturn the Florida bill, now known as the “physician gag law,” challenging, in part, the government’s right to interfere with a physician’s freedom of speech.
In another example of legislative interference, energy production politics gets in the way of doctors sharing relevant medical information with their patients. Four states—Colorado, Ohio, Pennsylvania, and Texas—prohibit physicians from disclosing information about exposure to chemicals used in hydraulic fracturing, or fracking. Scientific evidence shows that exposure to the chemicals used in fracking can result in a spectrum of health-care problems, from headaches to cancer. Can doctors talk about this with their patients? Not in these states.
While some states are trying to gag physicians by limiting what they can talk about with their patients, legislators in other states are considering requiring physicians to read, or offer to read, scripts to all patients who might have a terminal illness about end-of-life care options. Laws were enacted in California (2008) and New York (2011) to do just that. ObGyns are too familiar with legislatively mandated scripts; we know how inappropriate they are.
According to the Guttmacher Institute, in 2013, a number of states require abortion providers to read a script or provide written materials to patients seeking abortions; often these scripts contain medically inaccurate information. Twelve states require the physician to “inform” the patient about the ability of the fetus to feel pain, five states require the physician to claim that personhood begins at conception, and five states require doctors to say that abortion increases the risk of breast cancer. Six states require inaccurate information on the effects of abortion on future fertility.1
Serious penalties usually accompany these laws—financial fines, loss of licensure, and jail time. These and other legislative efforts infringe on physicians’ freedom of speech and force physicians to make terrible choices: Do you risk criminal prosecution or do you give your patient scientifically accurate and complete information? Do you adhere to your professional obligation to your patients, and risk putting your professional career on the line?
CLICK HERE to read other insightful articles by Ms. DiVenere.
Women’s reproductive health in the firing line
Nowhere is legislative interference more rampant than in the world of women’s health care. Over the past 2 years, an unprecedented number of bills have been introduced in the US Congress and statehouses restricting access to care for women and placing inappropriate requirements on physicians. The year 2011 was record-breaking in terms of abortion restrictions in the states, with 92 restrictions enacted.
In 2012, 42 states and the District of Columbia enacted 122 reproductive health provisions, one-third of them related to abortion restrictions. Forty-three new laws in 19 states were passed that restrict access to abortion. More than half of these new laws came from six states: Arizona was first with seven anti-abortion restrictions. Kansas, Louisiana, Oklahoma, South Dakota, and Wisconsin all had at least three.
In 2013, there have already been bills introduced in the US Congress and in the states that would:
- prohibit Title X family planning funds from going to clinics that provide abortions or prohibit funds from going to other entities that perform abortions (US Congress)
- repeal the Affordable Care Act, including the insurance protections and preventive services provisions that ACOG supports (US Congress)
- ban medical abortion (Mississippi)
- require women to undergo transvaginal ultrasound before having an abortion (Michigan)
- prohibit abortion after detection of a fetal heartbeat (at least three states: Arkansas, North Dakota, and Wyoming).
Few, if any, of these proposals are based on medical science. In fact, many of them run contrary to science and good patient-care principles. And although most of these efforts focus on reducing access to reproductive health care, including abortions, legislative interference is an issue of concern to physicians of all specialties, regardless of individual positions on life and choice.
What the medical community is doing
The American Medical Association (AMA) has made clear, consistent with the direction of its House of Delegates, that it fully opposes political interference in the patient-physician relationship. In 2012, the AMA unveiled its “Protect the sanctity of the patient-physician relationship” campaign with a panel that included Dr. Erin Tracy, chair of the Massachusetts Section of ACOG; Dr. Tim Bartholow, chief medical officer of the Wisconsin Medical Society; and Dr. H. Garry Gardner, chair of the American Academy of Pediatrics’ (AAP) Council on Injury, Violence, and Poison Prevention Executive Committee.
The AMA’s campaign is designed to educate physicians and to work with state medical societies and specialties to “articulate a compelling and comprehensive legal foundation to oppose legislation that encroaches on the sanctity of the patient-physician relationship.”
ACOG’s leadership has directly and forcefully pushed back on legislative encroachment. In 2012, ACOG Executive Vice President Hal C. Lawrence III, MD, and the executive leadership of the American Academy of Family Physicians (AAFP), AAP, the American College of Physicians, and the American College of Surgeons issued a joint statement that was published in the New England Journal of Medicine against legislative interference in the exam room.2
In addition, ACOG President James T. Breeden, MD, has written eight oped pieces, letters to the editor, and other public statements in venues with far and important reach, including the New York Times, USA Today, and Capitol Hill dailies (see the box). ACOG has also issued “Rapid Responses” to counter inaccurate statements about women’s health made in the media or on the campaign trail by state or national politicians.
In a paid ad message to the National Conference on State Legislatures (NCSL), which the NCSL refused to run, Dr. Breeden said, in part:
- Because we stand firmly for access to needed care, we also stand firmly against legislative interference with the patient-physician relationship. There’s only room for two people in our exam rooms: the patient and the caregiver. Lawmakers get in the way of good patient care when they try to force women to undergo transvaginal ultrasounds or other unnecessary medical procedures; when they try to close health clinics for specious reasons; or when they try to tell women that legislators know best.
Lawmakers can and do play a vitally productive and important role in ensuring public health. Lawmakers should not, however, attempt to define, mandate, or prohibit medical practices or require doctors to read a government script to their patients.
As ObGyns visit with state and federal legislators this year, our message is simple: Partnership with lawmakers, yes. Legislative interference, no.
Our campaign makes the point that there are a number of legitimate roles that state and federal governments play in public health. We welcome opportunities to partner with legislators on important women’s health-care needs. We draw the line at legislative interference of all stripes.
Here are just a few examples of ACOG’s many statements on behalf of women’s reproductive health
USA Today – Letter to the editor – May 21, 2012
“Politicians should not be legislating the practice of medicine or the doctor-patient relationship. We all need to speak up and take action when legislators pretend they know what’s best for women and their physicians.” —ACOG President James T. Breeden, MD
New York Times – Letter to the editor – June 4, 2012
“Politicians were not elected to, nor should they, legislate the practice of medicine or dictate the parameters of the doctor-patient relationship. Our message to politicians is unequivocal: Get out of our exam rooms.” —ACOG President James T. Breeden, MD
“Universal access to contraception could be a lifesaver” – Las Vegas Review Journal – July 22, 2012
“Contraception is a basic and essential element of women’s preventive health care and a basic public health necessity.” —ACOG President James T. Breeden, MD
ACOG Rapid Response to Rep. Todd Akin’s August 19, 2012 statement on “legitimate rape” – Issued August 20, 2012
“Absolutely no veracity to the claim … A woman who is raped has no control over ovulation, fertilization, or implantation of a fertilized egg. To suggest otherwise contradicts basic biological truths.”
ACOG Rapid Response to Rep. Joe Walsh’s October 18, 2012, statement that “Technology has advanced to the point that abortions are never needed to save the health or life of a mother” – Issued October 19, 2012
“Abortions are necessary in a number of circumstances to save the life of a woman or to preserve her health.”
A meaningful partnership: Strong Start
ACOG was invited to partner with the HHS and the March of Dimes on an initiative designed to bring about a meaningful and lasting improvement in maternity care: ending early elective deliveries before 39 weeks’ gestation. At the press conference announcing this partnership on the Strong Start initiative, Dr. Lawrence stood with HHS Secretary Kathleen Sebelius and said, in part:
- An ObGyn’s job is one of the most rewarding jobs on the planet, bringing little babies into the world. This job carries enormous responsibilities, too, ensuring the highest levels of health and safety for every mom and baby.
- The American College of Obstetricians and Gynecologists is proud to partner with the Department of Health and Human Services and the March of Dimes on one of the most certain ways of helping babies get a good start in life: Babies should not be delivered earlier than 39 weeks, unless pregnancy complications require otherwise to keep mother and child safe.
- Such a simple change, but one that can tremendously benefit children, families, our health system, and our society.
- Our joint initiative will help bring this important information to women and physicians across the nation, and has enormous potential to make a real and lasting change in how we care for expectant moms, and more importantly, how expectant moms expect us to care for them.
The Strong Start initiative is an all-too-rare example of a wonderful partnership between government, medicine, and the public to lead and create important change. This initiative goes far beyond the original press conference. Dr. Lawrence and other leaders have participated in webinars and interviews to spread the word. ACOG has developed patient education materials tailored to the message of no early elective deliveries before 39 weeks unless there is a maternal or fetal medical indication. Strong Start has provided funding to innovative maternity care models, including centering and pregnancy medical homes.
Earlier this year, Dr. Lawrence convened a Strong Start summit of the heads of the American Hospital Association, AAFP, AAP, the American Women’s Health and Neonatal Nurses Association, the American College of Nurse Midwives, the March of Dimes, and our federal partners, the Centers for Medicare and Medicaid Services and the Center for Medicare and Medicaid Innovation.
This one-day summit had a clear goal: gain unanimous agreement and commitment from the maternal care community to move our clinical knowledge into practice, ending nonmedically indicated early elective deliveries before 39 weeks.
Since 1979, ACOG has emphasized that labor should be induced “when the benefits of delivery to the fetus or the mother exceed the benefits of continuing the pregnancy,” and that pregnancies should be maintained until at least 39 weeks unless medical indications make early delivery necessary. This guidance was based on sound clinical knowledge in 1979, and today’s data are only more compelling. Somehow, however, early elective deliveries are still common and, for a variety of reasons, usually not related to infant or maternal health. This Strong Start summit is our specialty’s way of leading through partnership to encourage every maternity hospital in America to have in place a practice policy supporting no nonmedically indicated early elective deliveries before 39 weeks.
In many important ways, Strong Start is an example of the best that partnership with government and our colleagues has to offer.
The difference between partnership and interference is easy to see. That’s why we say: Partnership, yes. Interference, no.
We want to hear from you! Tell us what you think.
Who’s in charge here?
It’s a legitimate question being asked by more physicians in all areas of the country as they struggle to provide good quality care. Yes, physicians face longstanding payment and coverage issues, regulations, and the insurance bureaucracy. But more and more often, physicians are struggling to care for their patients in the face of legislative interference that reaches right into their exam rooms. Who’s in charge here, indeed?
In this article, I detail several examples of legislative interference and describe the response of the American Congress of Obstetricians and Gynecologists (ACOG). I also detail a very healthy partnership ACOG has undertaken with the US Department of Health and Human Services (HHS) and the March of Dimes to end early elective deliveries before 39 weeks of gestation.
Physician gag law passes in Florida
State lawmakers in Florida have decided that physicians should no longer ask about guns in the home when performing a child wellness exam. The use of bike helmets and exposure to secondhand smoke are childhood health concerns worth mentioning, but the importance of keeping guns unloaded and locked away is not.
Under the Firearm Owners’ Privacy Act, enacted in 2011, physicians in Florida could be fined or imprisoned for initiating this conversation, and could be charged with a third-degree felony punishable by a fine of up to $5 million. Thanks to public pushback, the law was amended to remove the criminal penalty. Instead, patients who feel “harassed” by their physicians’ questions about gun safety can complain to the Florida Board of Medicine, which can take disciplinary action against an offending physician.
In November 2012, ACOG joined an amicus brief in the case of Wollschlaeger v the State of Florida, asking the court to overturn the Florida bill, now known as the “physician gag law,” challenging, in part, the government’s right to interfere with a physician’s freedom of speech.
In another example of legislative interference, energy production politics gets in the way of doctors sharing relevant medical information with their patients. Four states—Colorado, Ohio, Pennsylvania, and Texas—prohibit physicians from disclosing information about exposure to chemicals used in hydraulic fracturing, or fracking. Scientific evidence shows that exposure to the chemicals used in fracking can result in a spectrum of health-care problems, from headaches to cancer. Can doctors talk about this with their patients? Not in these states.
While some states are trying to gag physicians by limiting what they can talk about with their patients, legislators in other states are considering requiring physicians to read, or offer to read, scripts to all patients who might have a terminal illness about end-of-life care options. Laws were enacted in California (2008) and New York (2011) to do just that. ObGyns are too familiar with legislatively mandated scripts; we know how inappropriate they are.
According to the Guttmacher Institute, in 2013, a number of states require abortion providers to read a script or provide written materials to patients seeking abortions; often these scripts contain medically inaccurate information. Twelve states require the physician to “inform” the patient about the ability of the fetus to feel pain, five states require the physician to claim that personhood begins at conception, and five states require doctors to say that abortion increases the risk of breast cancer. Six states require inaccurate information on the effects of abortion on future fertility.1
Serious penalties usually accompany these laws—financial fines, loss of licensure, and jail time. These and other legislative efforts infringe on physicians’ freedom of speech and force physicians to make terrible choices: Do you risk criminal prosecution or do you give your patient scientifically accurate and complete information? Do you adhere to your professional obligation to your patients, and risk putting your professional career on the line?
CLICK HERE to read other insightful articles by Ms. DiVenere.
Women’s reproductive health in the firing line
Nowhere is legislative interference more rampant than in the world of women’s health care. Over the past 2 years, an unprecedented number of bills have been introduced in the US Congress and statehouses restricting access to care for women and placing inappropriate requirements on physicians. The year 2011 was record-breaking in terms of abortion restrictions in the states, with 92 restrictions enacted.
In 2012, 42 states and the District of Columbia enacted 122 reproductive health provisions, one-third of them related to abortion restrictions. Forty-three new laws in 19 states were passed that restrict access to abortion. More than half of these new laws came from six states: Arizona was first with seven anti-abortion restrictions. Kansas, Louisiana, Oklahoma, South Dakota, and Wisconsin all had at least three.
In 2013, there have already been bills introduced in the US Congress and in the states that would:
- prohibit Title X family planning funds from going to clinics that provide abortions or prohibit funds from going to other entities that perform abortions (US Congress)
- repeal the Affordable Care Act, including the insurance protections and preventive services provisions that ACOG supports (US Congress)
- ban medical abortion (Mississippi)
- require women to undergo transvaginal ultrasound before having an abortion (Michigan)
- prohibit abortion after detection of a fetal heartbeat (at least three states: Arkansas, North Dakota, and Wyoming).
Few, if any, of these proposals are based on medical science. In fact, many of them run contrary to science and good patient-care principles. And although most of these efforts focus on reducing access to reproductive health care, including abortions, legislative interference is an issue of concern to physicians of all specialties, regardless of individual positions on life and choice.
What the medical community is doing
The American Medical Association (AMA) has made clear, consistent with the direction of its House of Delegates, that it fully opposes political interference in the patient-physician relationship. In 2012, the AMA unveiled its “Protect the sanctity of the patient-physician relationship” campaign with a panel that included Dr. Erin Tracy, chair of the Massachusetts Section of ACOG; Dr. Tim Bartholow, chief medical officer of the Wisconsin Medical Society; and Dr. H. Garry Gardner, chair of the American Academy of Pediatrics’ (AAP) Council on Injury, Violence, and Poison Prevention Executive Committee.
The AMA’s campaign is designed to educate physicians and to work with state medical societies and specialties to “articulate a compelling and comprehensive legal foundation to oppose legislation that encroaches on the sanctity of the patient-physician relationship.”
ACOG’s leadership has directly and forcefully pushed back on legislative encroachment. In 2012, ACOG Executive Vice President Hal C. Lawrence III, MD, and the executive leadership of the American Academy of Family Physicians (AAFP), AAP, the American College of Physicians, and the American College of Surgeons issued a joint statement that was published in the New England Journal of Medicine against legislative interference in the exam room.2
In addition, ACOG President James T. Breeden, MD, has written eight oped pieces, letters to the editor, and other public statements in venues with far and important reach, including the New York Times, USA Today, and Capitol Hill dailies (see the box). ACOG has also issued “Rapid Responses” to counter inaccurate statements about women’s health made in the media or on the campaign trail by state or national politicians.
In a paid ad message to the National Conference on State Legislatures (NCSL), which the NCSL refused to run, Dr. Breeden said, in part:
- Because we stand firmly for access to needed care, we also stand firmly against legislative interference with the patient-physician relationship. There’s only room for two people in our exam rooms: the patient and the caregiver. Lawmakers get in the way of good patient care when they try to force women to undergo transvaginal ultrasounds or other unnecessary medical procedures; when they try to close health clinics for specious reasons; or when they try to tell women that legislators know best.
Lawmakers can and do play a vitally productive and important role in ensuring public health. Lawmakers should not, however, attempt to define, mandate, or prohibit medical practices or require doctors to read a government script to their patients.
As ObGyns visit with state and federal legislators this year, our message is simple: Partnership with lawmakers, yes. Legislative interference, no.
Our campaign makes the point that there are a number of legitimate roles that state and federal governments play in public health. We welcome opportunities to partner with legislators on important women’s health-care needs. We draw the line at legislative interference of all stripes.
Here are just a few examples of ACOG’s many statements on behalf of women’s reproductive health
USA Today – Letter to the editor – May 21, 2012
“Politicians should not be legislating the practice of medicine or the doctor-patient relationship. We all need to speak up and take action when legislators pretend they know what’s best for women and their physicians.” —ACOG President James T. Breeden, MD
New York Times – Letter to the editor – June 4, 2012
“Politicians were not elected to, nor should they, legislate the practice of medicine or dictate the parameters of the doctor-patient relationship. Our message to politicians is unequivocal: Get out of our exam rooms.” —ACOG President James T. Breeden, MD
“Universal access to contraception could be a lifesaver” – Las Vegas Review Journal – July 22, 2012
“Contraception is a basic and essential element of women’s preventive health care and a basic public health necessity.” —ACOG President James T. Breeden, MD
ACOG Rapid Response to Rep. Todd Akin’s August 19, 2012 statement on “legitimate rape” – Issued August 20, 2012
“Absolutely no veracity to the claim … A woman who is raped has no control over ovulation, fertilization, or implantation of a fertilized egg. To suggest otherwise contradicts basic biological truths.”
ACOG Rapid Response to Rep. Joe Walsh’s October 18, 2012, statement that “Technology has advanced to the point that abortions are never needed to save the health or life of a mother” – Issued October 19, 2012
“Abortions are necessary in a number of circumstances to save the life of a woman or to preserve her health.”
A meaningful partnership: Strong Start
ACOG was invited to partner with the HHS and the March of Dimes on an initiative designed to bring about a meaningful and lasting improvement in maternity care: ending early elective deliveries before 39 weeks’ gestation. At the press conference announcing this partnership on the Strong Start initiative, Dr. Lawrence stood with HHS Secretary Kathleen Sebelius and said, in part:
- An ObGyn’s job is one of the most rewarding jobs on the planet, bringing little babies into the world. This job carries enormous responsibilities, too, ensuring the highest levels of health and safety for every mom and baby.
- The American College of Obstetricians and Gynecologists is proud to partner with the Department of Health and Human Services and the March of Dimes on one of the most certain ways of helping babies get a good start in life: Babies should not be delivered earlier than 39 weeks, unless pregnancy complications require otherwise to keep mother and child safe.
- Such a simple change, but one that can tremendously benefit children, families, our health system, and our society.
- Our joint initiative will help bring this important information to women and physicians across the nation, and has enormous potential to make a real and lasting change in how we care for expectant moms, and more importantly, how expectant moms expect us to care for them.
The Strong Start initiative is an all-too-rare example of a wonderful partnership between government, medicine, and the public to lead and create important change. This initiative goes far beyond the original press conference. Dr. Lawrence and other leaders have participated in webinars and interviews to spread the word. ACOG has developed patient education materials tailored to the message of no early elective deliveries before 39 weeks unless there is a maternal or fetal medical indication. Strong Start has provided funding to innovative maternity care models, including centering and pregnancy medical homes.
Earlier this year, Dr. Lawrence convened a Strong Start summit of the heads of the American Hospital Association, AAFP, AAP, the American Women’s Health and Neonatal Nurses Association, the American College of Nurse Midwives, the March of Dimes, and our federal partners, the Centers for Medicare and Medicaid Services and the Center for Medicare and Medicaid Innovation.
This one-day summit had a clear goal: gain unanimous agreement and commitment from the maternal care community to move our clinical knowledge into practice, ending nonmedically indicated early elective deliveries before 39 weeks.
Since 1979, ACOG has emphasized that labor should be induced “when the benefits of delivery to the fetus or the mother exceed the benefits of continuing the pregnancy,” and that pregnancies should be maintained until at least 39 weeks unless medical indications make early delivery necessary. This guidance was based on sound clinical knowledge in 1979, and today’s data are only more compelling. Somehow, however, early elective deliveries are still common and, for a variety of reasons, usually not related to infant or maternal health. This Strong Start summit is our specialty’s way of leading through partnership to encourage every maternity hospital in America to have in place a practice policy supporting no nonmedically indicated early elective deliveries before 39 weeks.
In many important ways, Strong Start is an example of the best that partnership with government and our colleagues has to offer.
The difference between partnership and interference is easy to see. That’s why we say: Partnership, yes. Interference, no.
We want to hear from you! Tell us what you think.
1. Guttmacher Institute. State Policies in Brief: Counseling and Waiting Period for Abortion. New York, NY, and Washington, DC: Guttmacher Institute; 2013.
2. Weinberger SE, Lawrence HC, III, Henley DE, et al. Legislative interference with the patient-physician relationship. N Engl J Med. 2012;367(16):1557-1559.
1. Guttmacher Institute. State Policies in Brief: Counseling and Waiting Period for Abortion. New York, NY, and Washington, DC: Guttmacher Institute; 2013.
2. Weinberger SE, Lawrence HC, III, Henley DE, et al. Legislative interference with the patient-physician relationship. N Engl J Med. 2012;367(16):1557-1559.
Why (and how) we must repeal the sustainable growth rate
Imagine this: Your 20-year-old daughter tells you she wants to attend an expensive school for 5 years of intensive postgraduate training, amassing tens of thousands of dollars of debt, to provide expert services to the US population. There is no good substitute for the services she hopes to provide, and they are vitally needed. The services also carry risk. Despite this, she tells you that her salary will not increase every year in tandem with the cost of living; in fact, she expects her salary to be cut by nearly one-third each year. Compensation in her chosen field hasn’t increased in real dollars for many years.
Sound like a good plan?
By now you have recognized this as your own story, at least if you’re among the 92% of ObGyns who participate in Medicare.
ObGyn participation in the Medicare program reflects ObGyn training and commitment to serve as lifelong principal care physicians for women of all ages, including women with disabilities. Fifty-six percent of all Medicare beneficiaries are women. With continuing shortages of primary care physicians and the transitioning of the Baby Boomer generation to Medicare, it is likely that ObGyns will become more involved in delivering health care to this population.
Medicare physician payments matter to ObGyns in other ways, too, because TRICARE and private payers often follow Medicare payment and coverage policies. Clearly, the Medicare program is a pretty big gorilla in every exam room. We all have much at stake in ensuring a stable Medicare system for years to come, starting with an improved physician payment system.
In 2011, Medicare paid $68 billion for physician care provided to nearly 50 million elderly and disabled individuals—about 12% of total Medicare spending—covering just over 1 billion distinct physician services. Physicians received a 10-month reprieve from a 27% cut in Medicare payments that had been scheduled for March 1, 2011, extending current payment rates through the end of this year. The agreement is part of a deal to extend a payroll tax cut and unemployment benefits. It is the 14th short-term patch to the sustainable growth rate (SGR) in the past 10 years. On January 1, 2013, we now face a 26.5% cut that Congress will have to find $245 billion to eliminate altogether.
How did we get here?
In 1997, Congress passed the Balanced Budget Act (BBA), at a time when many members of Congress were frustrated by continued increases in Medicare costs, fueled on the physician side, in part, by increases in the number of visits, tests, and procedures. To control these costs, Congress included in the BBA a complicated formula to peg Medicare physician payments to an economic growth target—the SGR. For the first few years, Medicare expenditures stayed within the target, and doctors received modest pay increases. But in 2002, expenditures rose faster than the SGR, and doctors were slated for a 4.8% pay cut.
Every year since, the SGR has signaled physician pay cuts, and every year, Congress has stopped the cuts from taking effect. But each deferral just made the next cut bigger and increased the price tag of stopping each pay cut. Today, the price of eliminating the SGR is $245 billion over the next 10 years. In these days of sequestration and deficit reduction, $245 billion is hard to find.
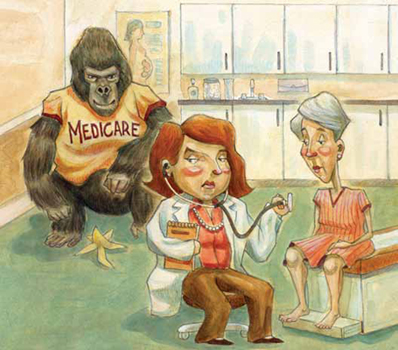
What now?
The good news is that support for eliminating the SGR is bicameral and bipartisan, rare in these hyperpartisan political days. Both Republicans and Democrats in the US House and Senate agree: The SGR has got to go. It’s a topic of conversation that wore out its welcome long ago.
The bad news? The $245 billion price tag. Remember, the SGR is in statute, so it requires an Act of Congress, signed by the President, to repeal it—and every Act is scored by the Congressional Budget Office.
The likeliest scenario is one we’ve seen many times before: Congress returns from a difficult election for a short, lame-duck session, during which it will have to address the cut before January 1. A real solution won’t be within reach, so Congress will likely kick that well-dented can a few more yards down the road, delaying the cut for yet another legislative cliffhanger.
In October 2012, the American Congress of Obstetricians and Gynecologists (ACOG) joined the American Medical Association (AMA) and 110 state and national medical societies in providing the US Congress with a clear and definitive document—Driving Principles and Core Elements—that describes a way to transition to a Medicare payment system that will endure and ensure high-quality care for the individuals who rely on that program, and for many millions more whose care is linked to Medicare payment policies.
This document is unique in many ways, perhaps especially in the unity it demonstrates among all physician organizations. It echoes ACOG’s earlier guidance to the US Congress on essential elements for a Medicare payment system that benefits women’s health. Among ACOG’s recommendations:
Make the new system simple, coordinated, and transparent. A new Medicare physician payment system should coordinate closely with other health-care programs; ensure that information technology is interoperable; and guarantee that quality-measurement programs are the same across all payers and rely on high-quality, risk-adjusted data.
Maintain the global obstetric care package. Medicare currently uses this package to reimburse for pregnancy. It works well and may be a model for global payment options for care provided by other physician types. The global obstetric care payment covers 10 months of care, from the first antepartum visit through the final postdelivery office visit.
Global payments allow a physician to manage costs and care for a patient’s course of treatment, rather than for a patient’s individual medical encounters.
Maintain fee for service for women’s health physicians who have small Medicare populations. Depending on the practice mix, type, and area, ObGyns and ObGyn subspecialists could see relatively few Medicare patients; unique Medicare requirements can pose significant administrative challenges and create inefficiencies with participation. Physicians who have small numbers of Medicare patients must be accommodated—and not penalized—in a new payment system.
Ensure that payment fairly and accurately reflects the cost of care. Medicare payments to obstetricians are already well below the cost of maternity care; no further cuts should be allowed for this care.
Support innovative care models, including a women’s medical home. These models should recognize the dual role that ObGyns may play as primary care and specialty care physicians.
Repeal the Independent Medicare Payment Advisory Board. Leaving Medicare payment decisions in the hands of an unelected, unaccountable body with minimal Congressional oversight is just a bad idea.
Pass medical liability reform. Congress must enact meaningful medical liability reform, which the Congressional Budget Office says could save $40 billion—enough for a small downpayment on SGR repeal.
A continuing promise
Rest assured that ACOG’s work to ensure appropriate Medicare payments to physicians, and to ensure that your patients have access to needed care, won’t stop until the job is done.
ACOG, AMA, and 110 state and national medical societies think so, and prescribe driving principles and core elements for the transition
In their letter to Congressional leaders, ACOG, AMA, and other societies acknowledged the “profound change” sweeping through the US health-care system, noting that it offers a “unique opportunity to improve and restructure how we deliver and pay for care.” When it comes to the SGR, however, these organizations conclude that it is “an enormous impediment to successful health-care delivery and payment reforms that can improve the quality of patient care while lowering growth in costs. Physicians facing the constant specter of severe cuts under the SGR cannot invest their time, energy, and resources in care redesign. The first step in moving to a higher-performing Medicare program must be the elimination of the SGR formula,” they write, based on the following principles, values, and key reforms.
Driving principles
- Successful delivery reform is an essential foundation for transitioning to a high-performing Medicare program that provides patient choice and meets the health-care needs of a diverse patient population.
- The Medicare program must invest in and support physician infrastructure that provides the platform for delivery and payment reform.
- Medicare payment updates should reflect the cost of providing services as well as efforts and progress on quality improvements and managing costs.
Core elements of reform
- Reflect the diversity of physician practices and provide opportunities for physicians to choose payment models that work for their patients, practice, specialty, and region.
- Encourage incremental changes with positive incentives and rewards during a defined timetable instead of using penalties to order abrupt changes in the delivery of care.
- Provide a way to measure progress and show policymakers that physicians are taking accountability for quality and costs.
Recommended structural improvements
- Reward physicians for savings achieved across the health-care spectrum.
- Enhance prospects for physicians adopting new models to achieve positive updates.
- Tie incentives to physicians’ own actions, rather than the actions of others or variables beyond their influence.
- Enhance prospects to harmonize measures and alter incentives in current law.
- Encourage systems of care, regional collaborative efforts, and primary care and specialist cooperation while preserving patient choice.
- Allow specialty and state society initiatives to be credited as delivering improvements (deeming authority) and recognize the central role of the profession in determining and measuring quality.
- Provide exemptions and alternative pathways for physicians in practice situations in which making or recovering the investments that may be needed to improve care delivery would constitute a hardship.
We want to hear from you! Tell us what you think.
Women’s health under the Affordable Care Act: What is covered?
(September 2012)
Lay midwives and the ObGyn: Is collaboration risky?
(May 2012)
How state budget crises are putting the squeeze on Medicaid (and you)
(February 2012)
Is private ObGyn practice on its way out?
(October 2011)
14 questions (and answers) about health reform and you
with Janelle Yates, Senior Editor (August 2010)
Imagine this: Your 20-year-old daughter tells you she wants to attend an expensive school for 5 years of intensive postgraduate training, amassing tens of thousands of dollars of debt, to provide expert services to the US population. There is no good substitute for the services she hopes to provide, and they are vitally needed. The services also carry risk. Despite this, she tells you that her salary will not increase every year in tandem with the cost of living; in fact, she expects her salary to be cut by nearly one-third each year. Compensation in her chosen field hasn’t increased in real dollars for many years.
Sound like a good plan?
By now you have recognized this as your own story, at least if you’re among the 92% of ObGyns who participate in Medicare.
ObGyn participation in the Medicare program reflects ObGyn training and commitment to serve as lifelong principal care physicians for women of all ages, including women with disabilities. Fifty-six percent of all Medicare beneficiaries are women. With continuing shortages of primary care physicians and the transitioning of the Baby Boomer generation to Medicare, it is likely that ObGyns will become more involved in delivering health care to this population.
Medicare physician payments matter to ObGyns in other ways, too, because TRICARE and private payers often follow Medicare payment and coverage policies. Clearly, the Medicare program is a pretty big gorilla in every exam room. We all have much at stake in ensuring a stable Medicare system for years to come, starting with an improved physician payment system.
In 2011, Medicare paid $68 billion for physician care provided to nearly 50 million elderly and disabled individuals—about 12% of total Medicare spending—covering just over 1 billion distinct physician services. Physicians received a 10-month reprieve from a 27% cut in Medicare payments that had been scheduled for March 1, 2011, extending current payment rates through the end of this year. The agreement is part of a deal to extend a payroll tax cut and unemployment benefits. It is the 14th short-term patch to the sustainable growth rate (SGR) in the past 10 years. On January 1, 2013, we now face a 26.5% cut that Congress will have to find $245 billion to eliminate altogether.
How did we get here?
In 1997, Congress passed the Balanced Budget Act (BBA), at a time when many members of Congress were frustrated by continued increases in Medicare costs, fueled on the physician side, in part, by increases in the number of visits, tests, and procedures. To control these costs, Congress included in the BBA a complicated formula to peg Medicare physician payments to an economic growth target—the SGR. For the first few years, Medicare expenditures stayed within the target, and doctors received modest pay increases. But in 2002, expenditures rose faster than the SGR, and doctors were slated for a 4.8% pay cut.
Every year since, the SGR has signaled physician pay cuts, and every year, Congress has stopped the cuts from taking effect. But each deferral just made the next cut bigger and increased the price tag of stopping each pay cut. Today, the price of eliminating the SGR is $245 billion over the next 10 years. In these days of sequestration and deficit reduction, $245 billion is hard to find.
What now?
The good news is that support for eliminating the SGR is bicameral and bipartisan, rare in these hyperpartisan political days. Both Republicans and Democrats in the US House and Senate agree: The SGR has got to go. It’s a topic of conversation that wore out its welcome long ago.
The bad news? The $245 billion price tag. Remember, the SGR is in statute, so it requires an Act of Congress, signed by the President, to repeal it—and every Act is scored by the Congressional Budget Office.
The likeliest scenario is one we’ve seen many times before: Congress returns from a difficult election for a short, lame-duck session, during which it will have to address the cut before January 1. A real solution won’t be within reach, so Congress will likely kick that well-dented can a few more yards down the road, delaying the cut for yet another legislative cliffhanger.
In October 2012, the American Congress of Obstetricians and Gynecologists (ACOG) joined the American Medical Association (AMA) and 110 state and national medical societies in providing the US Congress with a clear and definitive document—Driving Principles and Core Elements—that describes a way to transition to a Medicare payment system that will endure and ensure high-quality care for the individuals who rely on that program, and for many millions more whose care is linked to Medicare payment policies.
This document is unique in many ways, perhaps especially in the unity it demonstrates among all physician organizations. It echoes ACOG’s earlier guidance to the US Congress on essential elements for a Medicare payment system that benefits women’s health. Among ACOG’s recommendations:
Make the new system simple, coordinated, and transparent. A new Medicare physician payment system should coordinate closely with other health-care programs; ensure that information technology is interoperable; and guarantee that quality-measurement programs are the same across all payers and rely on high-quality, risk-adjusted data.
Maintain the global obstetric care package. Medicare currently uses this package to reimburse for pregnancy. It works well and may be a model for global payment options for care provided by other physician types. The global obstetric care payment covers 10 months of care, from the first antepartum visit through the final postdelivery office visit.
Global payments allow a physician to manage costs and care for a patient’s course of treatment, rather than for a patient’s individual medical encounters.
Maintain fee for service for women’s health physicians who have small Medicare populations. Depending on the practice mix, type, and area, ObGyns and ObGyn subspecialists could see relatively few Medicare patients; unique Medicare requirements can pose significant administrative challenges and create inefficiencies with participation. Physicians who have small numbers of Medicare patients must be accommodated—and not penalized—in a new payment system.
Ensure that payment fairly and accurately reflects the cost of care. Medicare payments to obstetricians are already well below the cost of maternity care; no further cuts should be allowed for this care.
Support innovative care models, including a women’s medical home. These models should recognize the dual role that ObGyns may play as primary care and specialty care physicians.
Repeal the Independent Medicare Payment Advisory Board. Leaving Medicare payment decisions in the hands of an unelected, unaccountable body with minimal Congressional oversight is just a bad idea.
Pass medical liability reform. Congress must enact meaningful medical liability reform, which the Congressional Budget Office says could save $40 billion—enough for a small downpayment on SGR repeal.
A continuing promise
Rest assured that ACOG’s work to ensure appropriate Medicare payments to physicians, and to ensure that your patients have access to needed care, won’t stop until the job is done.
ACOG, AMA, and 110 state and national medical societies think so, and prescribe driving principles and core elements for the transition
In their letter to Congressional leaders, ACOG, AMA, and other societies acknowledged the “profound change” sweeping through the US health-care system, noting that it offers a “unique opportunity to improve and restructure how we deliver and pay for care.” When it comes to the SGR, however, these organizations conclude that it is “an enormous impediment to successful health-care delivery and payment reforms that can improve the quality of patient care while lowering growth in costs. Physicians facing the constant specter of severe cuts under the SGR cannot invest their time, energy, and resources in care redesign. The first step in moving to a higher-performing Medicare program must be the elimination of the SGR formula,” they write, based on the following principles, values, and key reforms.
Driving principles
- Successful delivery reform is an essential foundation for transitioning to a high-performing Medicare program that provides patient choice and meets the health-care needs of a diverse patient population.
- The Medicare program must invest in and support physician infrastructure that provides the platform for delivery and payment reform.
- Medicare payment updates should reflect the cost of providing services as well as efforts and progress on quality improvements and managing costs.
Core elements of reform
- Reflect the diversity of physician practices and provide opportunities for physicians to choose payment models that work for their patients, practice, specialty, and region.
- Encourage incremental changes with positive incentives and rewards during a defined timetable instead of using penalties to order abrupt changes in the delivery of care.
- Provide a way to measure progress and show policymakers that physicians are taking accountability for quality and costs.
Recommended structural improvements
- Reward physicians for savings achieved across the health-care spectrum.
- Enhance prospects for physicians adopting new models to achieve positive updates.
- Tie incentives to physicians’ own actions, rather than the actions of others or variables beyond their influence.
- Enhance prospects to harmonize measures and alter incentives in current law.
- Encourage systems of care, regional collaborative efforts, and primary care and specialist cooperation while preserving patient choice.
- Allow specialty and state society initiatives to be credited as delivering improvements (deeming authority) and recognize the central role of the profession in determining and measuring quality.
- Provide exemptions and alternative pathways for physicians in practice situations in which making or recovering the investments that may be needed to improve care delivery would constitute a hardship.
We want to hear from you! Tell us what you think.
Women’s health under the Affordable Care Act: What is covered?
(September 2012)
Lay midwives and the ObGyn: Is collaboration risky?
(May 2012)
How state budget crises are putting the squeeze on Medicaid (and you)
(February 2012)
Is private ObGyn practice on its way out?
(October 2011)
14 questions (and answers) about health reform and you
with Janelle Yates, Senior Editor (August 2010)
Imagine this: Your 20-year-old daughter tells you she wants to attend an expensive school for 5 years of intensive postgraduate training, amassing tens of thousands of dollars of debt, to provide expert services to the US population. There is no good substitute for the services she hopes to provide, and they are vitally needed. The services also carry risk. Despite this, she tells you that her salary will not increase every year in tandem with the cost of living; in fact, she expects her salary to be cut by nearly one-third each year. Compensation in her chosen field hasn’t increased in real dollars for many years.
Sound like a good plan?
By now you have recognized this as your own story, at least if you’re among the 92% of ObGyns who participate in Medicare.
ObGyn participation in the Medicare program reflects ObGyn training and commitment to serve as lifelong principal care physicians for women of all ages, including women with disabilities. Fifty-six percent of all Medicare beneficiaries are women. With continuing shortages of primary care physicians and the transitioning of the Baby Boomer generation to Medicare, it is likely that ObGyns will become more involved in delivering health care to this population.
Medicare physician payments matter to ObGyns in other ways, too, because TRICARE and private payers often follow Medicare payment and coverage policies. Clearly, the Medicare program is a pretty big gorilla in every exam room. We all have much at stake in ensuring a stable Medicare system for years to come, starting with an improved physician payment system.
In 2011, Medicare paid $68 billion for physician care provided to nearly 50 million elderly and disabled individuals—about 12% of total Medicare spending—covering just over 1 billion distinct physician services. Physicians received a 10-month reprieve from a 27% cut in Medicare payments that had been scheduled for March 1, 2011, extending current payment rates through the end of this year. The agreement is part of a deal to extend a payroll tax cut and unemployment benefits. It is the 14th short-term patch to the sustainable growth rate (SGR) in the past 10 years. On January 1, 2013, we now face a 26.5% cut that Congress will have to find $245 billion to eliminate altogether.
How did we get here?
In 1997, Congress passed the Balanced Budget Act (BBA), at a time when many members of Congress were frustrated by continued increases in Medicare costs, fueled on the physician side, in part, by increases in the number of visits, tests, and procedures. To control these costs, Congress included in the BBA a complicated formula to peg Medicare physician payments to an economic growth target—the SGR. For the first few years, Medicare expenditures stayed within the target, and doctors received modest pay increases. But in 2002, expenditures rose faster than the SGR, and doctors were slated for a 4.8% pay cut.
Every year since, the SGR has signaled physician pay cuts, and every year, Congress has stopped the cuts from taking effect. But each deferral just made the next cut bigger and increased the price tag of stopping each pay cut. Today, the price of eliminating the SGR is $245 billion over the next 10 years. In these days of sequestration and deficit reduction, $245 billion is hard to find.
What now?
The good news is that support for eliminating the SGR is bicameral and bipartisan, rare in these hyperpartisan political days. Both Republicans and Democrats in the US House and Senate agree: The SGR has got to go. It’s a topic of conversation that wore out its welcome long ago.
The bad news? The $245 billion price tag. Remember, the SGR is in statute, so it requires an Act of Congress, signed by the President, to repeal it—and every Act is scored by the Congressional Budget Office.
The likeliest scenario is one we’ve seen many times before: Congress returns from a difficult election for a short, lame-duck session, during which it will have to address the cut before January 1. A real solution won’t be within reach, so Congress will likely kick that well-dented can a few more yards down the road, delaying the cut for yet another legislative cliffhanger.
In October 2012, the American Congress of Obstetricians and Gynecologists (ACOG) joined the American Medical Association (AMA) and 110 state and national medical societies in providing the US Congress with a clear and definitive document—Driving Principles and Core Elements—that describes a way to transition to a Medicare payment system that will endure and ensure high-quality care for the individuals who rely on that program, and for many millions more whose care is linked to Medicare payment policies.
This document is unique in many ways, perhaps especially in the unity it demonstrates among all physician organizations. It echoes ACOG’s earlier guidance to the US Congress on essential elements for a Medicare payment system that benefits women’s health. Among ACOG’s recommendations:
Make the new system simple, coordinated, and transparent. A new Medicare physician payment system should coordinate closely with other health-care programs; ensure that information technology is interoperable; and guarantee that quality-measurement programs are the same across all payers and rely on high-quality, risk-adjusted data.
Maintain the global obstetric care package. Medicare currently uses this package to reimburse for pregnancy. It works well and may be a model for global payment options for care provided by other physician types. The global obstetric care payment covers 10 months of care, from the first antepartum visit through the final postdelivery office visit.
Global payments allow a physician to manage costs and care for a patient’s course of treatment, rather than for a patient’s individual medical encounters.
Maintain fee for service for women’s health physicians who have small Medicare populations. Depending on the practice mix, type, and area, ObGyns and ObGyn subspecialists could see relatively few Medicare patients; unique Medicare requirements can pose significant administrative challenges and create inefficiencies with participation. Physicians who have small numbers of Medicare patients must be accommodated—and not penalized—in a new payment system.
Ensure that payment fairly and accurately reflects the cost of care. Medicare payments to obstetricians are already well below the cost of maternity care; no further cuts should be allowed for this care.
Support innovative care models, including a women’s medical home. These models should recognize the dual role that ObGyns may play as primary care and specialty care physicians.
Repeal the Independent Medicare Payment Advisory Board. Leaving Medicare payment decisions in the hands of an unelected, unaccountable body with minimal Congressional oversight is just a bad idea.
Pass medical liability reform. Congress must enact meaningful medical liability reform, which the Congressional Budget Office says could save $40 billion—enough for a small downpayment on SGR repeal.
A continuing promise
Rest assured that ACOG’s work to ensure appropriate Medicare payments to physicians, and to ensure that your patients have access to needed care, won’t stop until the job is done.
ACOG, AMA, and 110 state and national medical societies think so, and prescribe driving principles and core elements for the transition
In their letter to Congressional leaders, ACOG, AMA, and other societies acknowledged the “profound change” sweeping through the US health-care system, noting that it offers a “unique opportunity to improve and restructure how we deliver and pay for care.” When it comes to the SGR, however, these organizations conclude that it is “an enormous impediment to successful health-care delivery and payment reforms that can improve the quality of patient care while lowering growth in costs. Physicians facing the constant specter of severe cuts under the SGR cannot invest their time, energy, and resources in care redesign. The first step in moving to a higher-performing Medicare program must be the elimination of the SGR formula,” they write, based on the following principles, values, and key reforms.
Driving principles
- Successful delivery reform is an essential foundation for transitioning to a high-performing Medicare program that provides patient choice and meets the health-care needs of a diverse patient population.
- The Medicare program must invest in and support physician infrastructure that provides the platform for delivery and payment reform.
- Medicare payment updates should reflect the cost of providing services as well as efforts and progress on quality improvements and managing costs.
Core elements of reform
- Reflect the diversity of physician practices and provide opportunities for physicians to choose payment models that work for their patients, practice, specialty, and region.
- Encourage incremental changes with positive incentives and rewards during a defined timetable instead of using penalties to order abrupt changes in the delivery of care.
- Provide a way to measure progress and show policymakers that physicians are taking accountability for quality and costs.
Recommended structural improvements
- Reward physicians for savings achieved across the health-care spectrum.
- Enhance prospects for physicians adopting new models to achieve positive updates.
- Tie incentives to physicians’ own actions, rather than the actions of others or variables beyond their influence.
- Enhance prospects to harmonize measures and alter incentives in current law.
- Encourage systems of care, regional collaborative efforts, and primary care and specialist cooperation while preserving patient choice.
- Allow specialty and state society initiatives to be credited as delivering improvements (deeming authority) and recognize the central role of the profession in determining and measuring quality.
- Provide exemptions and alternative pathways for physicians in practice situations in which making or recovering the investments that may be needed to improve care delivery would constitute a hardship.
We want to hear from you! Tell us what you think.
Women’s health under the Affordable Care Act: What is covered?
(September 2012)
Lay midwives and the ObGyn: Is collaboration risky?
(May 2012)
How state budget crises are putting the squeeze on Medicaid (and you)
(February 2012)
Is private ObGyn practice on its way out?
(October 2011)
14 questions (and answers) about health reform and you
with Janelle Yates, Senior Editor (August 2010)
Women’s health under the Affordable Care Act: What is covered?
Lay midwives and the ObGyn: Is collaboration risky?
(May 2012)
How state budget crises are putting the squeeze on Medicaid (and you)
(February 2012)
Is private ObGyn practice on its way out?
(October 2011)
14 questions (and answers) about health reform and you
with Janelle Yates, Senior Editor (August 2010)
For the first half of 2012, the big question was: Will anything be covered under the Affordable Care Act (ACA)? After considering constitutional challenges to the Act that had the potential to invalidate the entire law, the US Supreme Court ruled, on June 28, that the ACA met constitutional muster in National Federation of Independent Business v. Sebelius (2012).
Now that the Court has upheld the ACA, let’s review the major women’s health services included under the law. This Web version incorporates 10 more women's health provisions from the ACA, from smoking cessation to young women’s breast cancer, that were not in the print version.

Preventive services guaranteed without copays
A major component of the health reform law went into effect August 1, 2012; it requires most health plans to cover women’s preventive services without requiring enrollees to pay a copay or deductibles. This provision reflects Congress’ understanding that women have a longer life expectancy and bear a greater burden of chronic disease, disability, and reproductive and gender-specific conditions. In addition, women often have a different response to treatment than men do.
The federal Department of Health and Human Services (HHS) estimates that Americans use preventive services at only about half of the recommended rate. By 2013, as many as 73 million individuals will benefit from preventive care offered under the law.
The American Congress of Obstetricians and Gynecologists (ACOG) worked with the Institute of Medicine (IOM)—which was charged with advising HHS—to encourage the inclusion of women’s preventive services specified in ACOG guidelines to ensure women’s health and well-being. As ACOG Executive Vice President Hal C. Lawrence, MD, told the IOM in January 2011:
- The College’s clinical guidelines…offer an excellent resource…and encompass the entire field of women’s preventive care. Our guidance is based on the best available evidence and is developed by committees with expertise reflecting the breadth of women’s health care and subject to a rigorous conflict of interest policy.
Dr. Lawrence further urged the IOM “to recommend coverage of the following services and products without cost-sharing”:
- well-woman visits
- preconception care
- family planning counseling and services
- HIV screening (for women at average risk)
- screening for intimate partner violence
- testing for human papillomavirus (HPV) as part of cervical cancer screening.
ACOG’s recommendations were approved by the IOM and, subsequently, by HHS. As a result, all private health plans that began on or after September 30, 2010, are required to cover these services at no out-of-pocket cost to patients (TABLE).
Women’s preventive services guaranteed under ACA*
| Service | Frequency | HHS guidelines for health insurance coverage |
|---|---|---|
| Well-woman visit | Annual for adult women, although HHS recognizes that several visits may be needed to obtain all necessary recommended preventive services, depending on a woman’s health status, health needs, and other risk factors** | The visit should focus on preventive services that are appropriate for the patient’s age and development, including preconception and prenatal care. This visit should, where appropriate, include other preventive services listed in this set of guidelines, as well as others referenced in section 2713 |
| Screening for gestational diabetes | Between 24 and 28 weeks of gestation and at the first prenatal visit for pregnant women identified to be at high risk for diabetes | |
| Testing for human papillomavirus (HPV) | At age 30 and older, no more frequently than every 3 years | High-risk HPV DNA testing in women who have normal cervical cytology |
| Counseling about sexually transmitted infection (STI) | Annual | All sexually active women |
| Counseling about and screening for HIV | Annual | All sexually active women |
| Counseling about and provision of contraception† | As prescribed | All FDA-approved contraceptive methods and sterilization procedures. Counseling for all women with reproductive capacity |
| Breastfeeding support, supplies, and counseling | In conjunction with each birth | Comprehensive lactation support and counseling by a trained provider during pregnancy or postpartum (or both), as well as costs for renting breastfeeding equipment |
| Screening for and counseling about interpersonal and domestic violence | Annual | |
| HHS = Health and Human Services * HHS guidelines are effective August 1, 2011. Nongrandfathered plans and insurers are required to provide coverage without cost-sharing consistent with HHS guidelines in the first plan year (in the individual market, policy year) that begins on or after August 1, 2012. ** The July 2011 Institute of Medicine report titled “Clinical preventive services for women: closing the gap” lists recommendations on individual preventive services that may be obtained during a well-woman preventive service visit. † Group health plans sponsored by certain religious employers, and group health insurance coverage in connection with such plans, are exempt from the requirement to cover contraceptive services. SOURCE: Adapted from Healthcare.gov. Affordable Care Act Expands Prevention Coverage for Women’s Health and Well-Being. http://www.hrsa.gov/womensguidelines/. Accessed August 8, 2012. | ||
Contraceptive mandate triggers a firestorm
On February 10, 2012, under pressure from religious groups, the Obama Administration offered a religious exemption to the contraception mandate for certain employers and group health plans. Under this “accommodation,” certain religious employers are exempt from the requirement to cover contraceptive services in their group health plans. An employer qualifies for this exemption if it:
- has the inculcation of religious values as one of its purposes
- primarily employs individuals who share its religious tenets
- primarily serves individuals who share its religious tenets, and
- qualifies for nonprofit status under
Internal Revenue Service (IRS) rules. At the same time that the Obama Administration wanted to accommodate employers’ religious beliefs, it also wanted to ensure that every woman would have access to free preventive care, including contraceptive services, regardless of where she works. And so while the Administration requires insurers to offer group health plan coverage without contraceptive coverage to religious-affiliated organizations, it also requires insurers to provide contraceptive coverage directly to individuals covered under the organization’s group health plan with no cost sharing.
This contraceptive mandate—even with the accommodation—has set off a firestorm on Capitol Hill that will eventually be settled in the courts.
Medicaid expansion falls short of original goal
In National Federation of Independent Business v. Sebelius, the plaintiffs asked the Supreme Court to rule on the federal government’s authority to require states to expand their Medicaid programs. Medicaid costs are typically shared by the federal and state governments. Under the ACA, state Medicaid programs were required to cover nearly all individuals who have incomes below 133% of the federal poverty level—$30,656 for a family of four in 2012—paid entirely by the federal government from 2014 through 2016. After that, the federal share gradually declines to, and then stays at, 90%. States that did not expand their Medicaid programs risked losing all federal Medicaid funding.
The Court ruled that the federal government can expand Medicaid but can’t penalize states that don’t accept the expansion mandate—effectively turning the mandate into a state option. States will receive the additional federal funds if they expand coverage, but states that don’t expand will not be penalized by losing existing federal funds for other parts of the program.
Since the ruling, a number of governors have announced that they will not expand their Medicaid programs, including governors of Florida and Louisiana. Those two states alone are home to 20% of all individuals intended to be covered under the Medicaid expansion.
This part of the ACA is particularly important to women because it strikes, for the first time, the requirement that a low-income woman must be pregnant to receive Medicaid coverage.
The figure below shows the dramatic potential improvement in coverage for women if all states fully implement the Medicaid expansion. Time, court decisions, elections, and state budget fights will determine how much of this change is realized for women’s health.
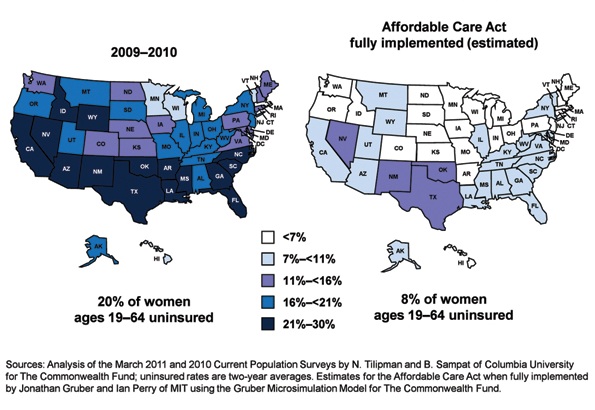
Percentage of insured women will increase under ACA
Percentage of women aged 19 to 64 years who were uninsured in 2009–2012 and under the Affordable Care Act when fully implemented.
SOURCE: Commonwealth Fund. Analysis of the March 2011 and 2010 Current Population Surveys by N. Tilipman and B. Sampat of Columbia University.
Women gain direct access to ObGyns
The ACA guarantees women in all states and all plans direct access to their ObGyns. Before the ACA, women in nine states lacked this guarantee, and women in 16 other states had only limited direct access. Now, a woman can go directly to her ObGyn without having to get a referral from her primary care physician or insurer.
Direct access is especially important because the ACA establishes new delivery systems, such as medical homes and accountable care organizations, designed to capture patients to maximize savings. An ObGyn does not have to be the patient’s primary care provider, and the patient’s access to her ObGyn cannot be limited to a certain number of visits or types of services.
ACA encourages states to cover family-planning services
Under the ACA, states have an easier time covering family-planning services, up to the same eligibility levels as pregnant women. Family planning is still an optional service that a state can choose to extend to women who have incomes above the Medicaid income eligibility level but, before the ACA was enacted, states had to apply to HHS for permission to waive the federal rules, often a very cumbersome process.
Prior to the ACA, 27 states had family planning waivers to provide services to nonpregnant women who had incomes above the Medicaid eligibility level—most at or near 200% of poverty. Now, states can provide family planning services to this population without federal approval.
Don’t miss Dr. Robert L. Barbieri’s October article titled “Gynecologic care across a woman’s life”
Insurance reforms end lifetime limits on coverage
Insurance reforms are important to us and our patients. The better the private health insurance system works—allowing us to provide our best possible care to patients and making sure they can see us when they need our care—the less our nation relies on the public safety net.
Beginning in 2010, the ACA eliminated all lifetime limits on how much insurance companies would cover when beneficiaries get sick; it also bans insurance companies from dropping people from coverage when they get sick. So if your patient has private health insurance and has faithfully paid her premiums and hasn’t committed fraud, her insurer cannot drop her or impose a limit on her coverage once she claims benefits.
This may be especially important for patients who need the most care, such as those who have cancer or another long-term, expensive, and unforeseen diagnosis. Because of this provision, you will not have to worry about your patient losing coverage in the middle of a long course of treatment.
The insurance practice of charging women more than men for equivalent policies ended on January 1, 2011, making insurance more affordable for our patients. Insurers in the individual and small group markets are allowed to vary premiums only for age, geographic location, family size, and tobacco use, not for gender—another important aspect of the law.
2014 is a key year in health reform
Exchanges begin
In 2014, under the ACA, state health insurance exchanges become reality.
An exchange is a marketplace where people can shop for health insurance; private health insurers can market their insurance products in state and multistate exchanges if they comply with new federal insurance reforms established in the ACA and offer the minimum benefits packages established by each state. Exchanges are intended to offer patients a choice of health insurance plans that are affordable, comprehensive, and easy to compare. Low-income individuals will be able to purchase private insurance in the exchanges with the federal premium subsidies or tax credits.
Insurers wanting to market their policies in an exchange may not deny coverage for preexisting conditions, including pregnancy, domestic violence, and previous cesarean delivery. They can’t deny coverage on the basis of an individual’s medical history, health status, genetic information, or disability. And they can’t impose waiting periods longer than 90 days before coverage takes effect, including 9-month waiting periods before maternity coverage.
Essential benefits are established
The ACA sets a minimum standard of health-care coverage that must be included in nearly every private insurance policy. The intent is that every person in the United States, regardless of where they live, who employs them, and what their income is, should have access to the same basic care.
Effective January 1, 2014, all insurance plans, except plans that existed before the ACA was enacted on March 23, 2010, must offer an “essential health benefits” (EHB) package, which must include:
- ambulatory patient services
- emergency services
- hospitalization
- maternity and newborn care
- mental health and substance use disorder services
- prescription drugs
- rehabilitative and habilitative services and devices
- laboratory services
- women’s preventive and wellness services and chronic disease management
- pediatric services, including oral and vision care.
Last December, HHS surprised many by giving states flexibility to design their own EHB packages, as long as the packages included each service on the list.
To choose its EHB package, a state must select a “benchmark” plan from the top- selling plans in four markets: federal and state public employee plans, commercial HMO plans, and small business plans. If a state doesn’t select a benchmark plan, the EHB defaults to the largest small-group market plan in the state. Each state must also choose an EHB package for its Medicaid program using the same 10 benefit categories.
State EHB plans must follow ACA requirements on annual and lifetime dollar limits but may impose limits on the scope and duration of coverage.
As for state-mandated benefits, if a state selects an EHB package that does not include a benefit already mandated by the state, the state must fund coverage for that service on its own—a decision HHS has promised to revisit in 2016.
Abortion decisions reside with the states
ACA requirements regarding abortion coverage 1) take effect in 2014 and 2) apply only to private health insurance plans marketed in the state exchanges that 3) cover abortions beyond those eligible for Medicaid coverage now, which are those that involve cases of rape or incest or that are necessary to save the life of the mother. Medicaid coverage for these categories of abortion is allowed under the Hyde Amendment.
Each insurer marketing a health plan in an exchange can determine whether or not its plan will cover abortion and, if it does, whether coverage will be limited to or go beyond those allowed under the Hyde Amendment. No federal tax or premium subsidies may be used to pay for abortions beyond those permitted by the Hyde Amendment.
The Secretary of HHS must ensure that at least one plan in each state exchange covers abortion, and that at least one plan either covers no abortions or limits abortions to those allowed under the Hyde Amendment. Insurers who offer abortion coverage beyond Hyde have to comply with a number of administrative requirements.
Congress was clear that the ultimate decisions about abortion should be made at the state rather than the federal level, and it gave states the ultimate trump card: Any state can pass legislation that prohibits any plan from offering abortion coverage of any kind within that state’s exchange. Any state can prohibit insurers offering plans within that state’s exchange from including any abortion coverage.
10 additional health provisions under the ACA
1. Creation of women's medical homes
The law points the way for creation of medical homes for women in the Medicare and Medicaid programs. The bill establishes an Innovation Center within the Centers for Medicare and Medicaid Services that has broad authority to evaluate, test, and adopt systems that foster patient-centered care, improve quality, and contain costs under Medicare, Medicaid, and the Children’s Health Insurance Program (CHIP)—and this includes patient-centered medical homes that address women’s unique health needs. ObGyn practices are eligible to participate and to receive additional reimbursement if they do.
2. Smoking-cessation counseling in pregnancy
The framers of the ACA recognized the large negative impact that smoking has on health, especially during pregnancy. Studies suggest that the intervention of a physician—most notably, counseling of the patient to quit smoking—has strong potential to modify this behavior. The new law provides reimbursement for this intervention. There are no copays or deductibles for patients, and smoking-cessation services can include diagnostic, therapeutic, and counseling modalities in addition to prescription of pharmacotherapy.
Before this bill became law, only 24 state Medicaid programs paid ObGyns or other physicians for smoking-cessation counseling of pregnant patients, and five states provided no coverage at all. Now, all pregnant Medicaid patients can get this counseling, and you’ll be paid for this important service.
3. Payments to nonphysician providers in freestanding birth centers
Before the ACA became law, Medicaid was authorized to pay hospitals and other facilities operated by and under the supervision of a physician; no payments were authorized for services of an ambulatory center operated by other health professionals. The ACA authorizes Medicaid payments to state-recognized freestanding birth centers not operated by or under the supervision of a physician. A state that doesn’t currently license birth centers must pass legislation and license these centers before the centers can receive these payments.
Medicaid will also reimburse providers who practice in state-recognized freestanding birth centers, as long as the individuals are practicing within their state’s scope of practice laws and regulations. Because the type of provider is not specified but instead left up to each state’s scope of practice laws and regulations, this provision could allow for separate provider payments for physicians, certified nurse midwives, certified professional midwives, and doulas.
4. Immigrant coverage
Legal immigrants are bound by the individual coverage mandate and must purchase health insurance. These individuals are eligible for income-related premium credits and subsidies for insurance purchased through an exchange. Legal immigrants who are barred from Medicaid during their first 5 years in the United States (by earlier law) are eligible for premium credits only.
Undocumented immigrants are not eligible for Medicaid, premium credits, or subsidies and are barred from purchasing insurance in the exchange, even with their own money.
5. Postpartum depression
Health reform will help bring perinatal and postpartum depression out of the shadows by providing federal funds for research, patient education, and clinical treatment. For example, the federal Department of Health and Human Services (HHS) will:
- conduct research into the causes of, and treatments for, postpartum conditions
- create a national public awareness campaign to increase awareness and knowledge of postpartum depression and psychosis
- provide grants to study the benefits of screening for postpartum depression and psychosis
- establish grants to deliver or enhance outpatient, inpatient, and home-based health and support services, including case management and comprehensive treatment services for individuals with, or at risk for, postpartum conditions.
The National Institute of Mental Health is encouraged to conduct a 10-year longitudinal study on the mental health consequences of pregnancy. This study is intended to focus on perinatal depression.
Community health centers will be eligible for grants in 2012 (as they were in 2011) to the tune of $3 million for inpatient and outpatient counseling and services.
And a federal public awareness campaign will educate the public through radio and television ads.
These endeavors point to the need for ObGyns to familiarize themselves with postpartum depression—if they aren’t already well versed in the subject—because patients are likely to become more aware of this issue and look to their ObGyns for answers.
6. Maternal home visits
Congress established a new Maternal, Infant, and Early Childhood Home Visiting program to improve maternal and fetal health in underserved areas of our country. This program will provide funds to states, tribes, and territories to develop and implement evidence-based home-visitation models to reduce infant and maternal mortality and its causes by producing improvements in:
- prenatal, maternal, and newborn health
- child health and development
- parenting skills
- school readiness
- juvenile delinquency
- family economic self-sufficiency.
These programs will have to demonstrate effectiveness and improved outcomes. HHS recently requested suggestions on ways of demonstrating the effectiveness of home-visiting program models for pregnant women, expectant fathers, and caregivers of children from birth through entry into kindergarten.
The law appropriates $350 million to this program in 2012 and $400 million in both 2013 and 2014.
7. Assistance for pregnant students
A new Pregnancy Assistance Fund—$25 million annually over 10 years (fiscal years 2010–2019)—requires the Secretary of HHS (in collaboration with the Secretary of Education) to establish a state grant program to help pregnant and parenting teens and young women. The aim of this program is to help teens who become pregnant and who choose to bring their pregnancies to term or keep their babies, or both, to stay in school. Grants will go to institutions of higher education, high schools and community service centers, as well as state attorneys general.
Institutions that receive grants must work with providers to meet specific practical needs of pregnant or parenting students:
- housing
- childcare
- parenting education
- postpartum counseling
- assistance in finding and accessing needed services
- referrals for prenatal care and delivery, infant or foster care, or adoption.
Funds to attorneys general will be used to combat domestic violence among pregnant teens.
8. Young women's breast cancer
A new program is intended to help educate young women about the importance of breast health and screening, in two ways:
- The National Institutes of Health (NIH) will conduct research to develop and test screening measures for prevention and early detection of breast cancer in women 15 to 44 years old.
- The US Department of HHS will create a national awareness campaign, with $9 million in funding each year from 2010 to 2014, to encourage young women to talk with their doctors about breast cancer and early detection.
ObGyns can expect to see more interest and questions about breast health among young women and their mothers. It pays to be prepared with good information for these important conversations.
9. Personal responsibility education
From 2010 through 2014, each state will receive funds for personal responsibility education programs aimed at reducing pregnancy in youths. Funds are $75 million for each fiscal year, allocated to each state depending on the size of its youth population but not intended to be less than $250,000 per state.
Educational programs eligible for federal funds must include both abstinence and contraception information for prevention of teenage pregnancy and sexually transmitted infections, including HIV/AIDS, as well as three or more adulthood-preparation subjects.
10. Community-based support of Patient-Centered Medical Homes
Federal funding is available to states for the development of community-based health teams to support medical homes run by primary care practices. These teams may include specialists, nurses, pharmacists, nutritionists, dieticians, social workers, behavioral and mental health providers, and physician assistants. Primary care practices in this program function as medical homes and are responsible for addressing a patient’s personal health-care needs. The team links the medical home to community support services for its patients.
Eligible ObGyn practices can qualify as primary care practices, and ObGyns are eligible to serve as specialist members of the community-based health team.
ACA is a mixed bag for ObGyns
Women have much to gain from the provisions of the ACA. It’s also true that many parts of the law are terrible for practicing ObGyns, including the Independent Payment Advisory Board (IPAB) and the absence of meaningful medical liability reform. For more on these issues, see “Is private ObGyn practice on its way out?” which appears in the October 2011 issue of OBG Management (available in the archive at obgmanagement.com). ACOG is committed to working with Congress to repeal or remedy those aspects of the law.
A recent study reveals that almost one-third of physicians are no longer accepting Medicaid patients
If all states expanded Medicaid to cover people with incomes at or below 138% of the federal poverty level in 2014, as the Affordable Care Act (ACA) proposes, 23 million people would become eligible for the program.1
That statistic prompts important questions:
- Would the health-care workforce be able to meet the demand of caring for all these new patients?
- Would it be willing?
A recent analysis of data from 4,326 office-based physicians suggests that the answer to both questions is “No”: Almost one-third of these providers were already declining to accept new Medicaid patients in 2011.2
Although 96% of physicians in the analysis accepted new patients in 2011, the percentage of physicians accepting new patients covered by Medicaid was lower (69%), as was the percentage accepting new self-paying patients (91.7%), patients covered by Medicare (83%), and patients with private insurance (82%).2
Physicians who were in solo practice were 23.5% less likely to accept new Medicaid patients, compared with those who practiced in an office with 10 or more other physicians.2
The data from this study come from the 2011 National Ambulatory Medical Care Survey Electronic Medical Records Supplement, a survey conducted by the Centers for Disease Control and Prevention National Center for Health Statistics. The survey included questions exploring whether physicians were accepting new patients.2
Earlier studies have found that the low reimbursement levels for care delivered through Medicaid has deterred many physicians from accepting patients.3
The view in the ObGyn specialty
The findings of this analysis were not broken down by specialty—only by primary care versus non–primary care. To get an idea of conditions in the ObGyn specialty, OBG Management surveyed the members of its Virtual Board of Editors (VBE). Of the 117 members contacted, 61 responded—a response rate of 52.1%. Roughly three-quarters (75.4%) reported that they currently treat patients covered by Medicaid, but only 60.7% are accepting new patients covered by Medicaid. Twenty-one percent of respondents reported that they have not and will not accept patients covered by Medicaid.
When asked to comment on their level of satisfaction with Medicaid, the most common response among VBE members was dissatisfaction due to “insufficient reimbursement.”
“I am not satisfied with Medicaid,” commented one VBE member. “The reimbursement is terrible….I have certainly thought of stopping care for Medicaid patients and, if Congress ever allows the big cuts to reimbursement that are threatened every year, I think I would stop.”
Another VBE member reported extreme dissatisfaction with Medicaid because of “lousy” reimbursement. He also pointed to “all the paperwork and crazy regulations that require inordinate time and additional personnel just to handle….and then [the claim] gets denied for reasons beyond reason.” He added that physicians who do accept Medicaid “are on the fast track to sainthood.”
Other reasons for refusing to accept patients with Medicaid (or, if Medicaid was accepted, for high levels of aggravation with the program):
- payment rejections
- too many different categories of coverage “that patients are completely uninformed about”
- difficulty finding a specialist who will manage high-risk patients covered by Medicaid
- red tape
- the complex health problems that Medicaid patients tend to have, compared with patients who have other types of coverage.
One VBE member summed up his feelings in one word: “Phooey.”
Several VBE members suggested that health reform should focus on the Medicaid program.
“These plans are just sucking up the state’s money and paying docs peanuts and their administrators big bucks!” wrote Mary Vanko, MD, of Munster, Indiana.
“I’m tired of how much Medicaid is being abused by people,” commented another VBE member. “People using other people’s cards, people with regular insurance getting Medicaid to cover their copays. The whole system needs reform!”
Some physicians were satisfied with Medicaid
Among the respondents were several who reported being satisfied with the program, including one who called the experience “good” and another who reported being “shielded from the reimbursement issues.”
“I have no problems with Medicaid,” wrote another.
—Janelle Yates, Senior Editor
References
1. Kenney GM, Dubay L, Zuckerman S, Huntress M. Making the Medicaid Expansion an ACA Option: How Many Low-Income Americans Could Remain Uninsured? Washington, DC: Urban Institute Health Policy Center; June 29, 2012. http://www.urban.org/UploadedPDF/412606-Making-the-Medicaid-Expansion-an-ACA-Option.pdf. Accessed August 18, 2012.
2. Decker SL. In 2011 nearly one-third of physicians said they would not accept new Medicaid patients, but rising fees may help. Health Affairs. 2012;31(8):1673–1679.
3. Centers for Disease Control and Prevention. QuickStats: percentage of office-based physicians accepting new patients, by types of payment accepted—United States, 1999–2000 and 2008–2009. MMWR Morb Mortal Wkly Rep. 2011;60(27):928.
We want to hear from you! Tell us what you think.
Lay midwives and the ObGyn: Is collaboration risky?
(May 2012)
How state budget crises are putting the squeeze on Medicaid (and you)
(February 2012)
Is private ObGyn practice on its way out?
(October 2011)
14 questions (and answers) about health reform and you
with Janelle Yates, Senior Editor (August 2010)
For the first half of 2012, the big question was: Will anything be covered under the Affordable Care Act (ACA)? After considering constitutional challenges to the Act that had the potential to invalidate the entire law, the US Supreme Court ruled, on June 28, that the ACA met constitutional muster in National Federation of Independent Business v. Sebelius (2012).
Now that the Court has upheld the ACA, let’s review the major women’s health services included under the law. This Web version incorporates 10 more women's health provisions from the ACA, from smoking cessation to young women’s breast cancer, that were not in the print version.

Preventive services guaranteed without copays
A major component of the health reform law went into effect August 1, 2012; it requires most health plans to cover women’s preventive services without requiring enrollees to pay a copay or deductibles. This provision reflects Congress’ understanding that women have a longer life expectancy and bear a greater burden of chronic disease, disability, and reproductive and gender-specific conditions. In addition, women often have a different response to treatment than men do.
The federal Department of Health and Human Services (HHS) estimates that Americans use preventive services at only about half of the recommended rate. By 2013, as many as 73 million individuals will benefit from preventive care offered under the law.
The American Congress of Obstetricians and Gynecologists (ACOG) worked with the Institute of Medicine (IOM)—which was charged with advising HHS—to encourage the inclusion of women’s preventive services specified in ACOG guidelines to ensure women’s health and well-being. As ACOG Executive Vice President Hal C. Lawrence, MD, told the IOM in January 2011:
- The College’s clinical guidelines…offer an excellent resource…and encompass the entire field of women’s preventive care. Our guidance is based on the best available evidence and is developed by committees with expertise reflecting the breadth of women’s health care and subject to a rigorous conflict of interest policy.
Dr. Lawrence further urged the IOM “to recommend coverage of the following services and products without cost-sharing”:
- well-woman visits
- preconception care
- family planning counseling and services
- HIV screening (for women at average risk)
- screening for intimate partner violence
- testing for human papillomavirus (HPV) as part of cervical cancer screening.
ACOG’s recommendations were approved by the IOM and, subsequently, by HHS. As a result, all private health plans that began on or after September 30, 2010, are required to cover these services at no out-of-pocket cost to patients (TABLE).
Women’s preventive services guaranteed under ACA*
| Service | Frequency | HHS guidelines for health insurance coverage |
|---|---|---|
| Well-woman visit | Annual for adult women, although HHS recognizes that several visits may be needed to obtain all necessary recommended preventive services, depending on a woman’s health status, health needs, and other risk factors** | The visit should focus on preventive services that are appropriate for the patient’s age and development, including preconception and prenatal care. This visit should, where appropriate, include other preventive services listed in this set of guidelines, as well as others referenced in section 2713 |
| Screening for gestational diabetes | Between 24 and 28 weeks of gestation and at the first prenatal visit for pregnant women identified to be at high risk for diabetes | |
| Testing for human papillomavirus (HPV) | At age 30 and older, no more frequently than every 3 years | High-risk HPV DNA testing in women who have normal cervical cytology |
| Counseling about sexually transmitted infection (STI) | Annual | All sexually active women |
| Counseling about and screening for HIV | Annual | All sexually active women |
| Counseling about and provision of contraception† | As prescribed | All FDA-approved contraceptive methods and sterilization procedures. Counseling for all women with reproductive capacity |
| Breastfeeding support, supplies, and counseling | In conjunction with each birth | Comprehensive lactation support and counseling by a trained provider during pregnancy or postpartum (or both), as well as costs for renting breastfeeding equipment |
| Screening for and counseling about interpersonal and domestic violence | Annual | |
| HHS = Health and Human Services * HHS guidelines are effective August 1, 2011. Nongrandfathered plans and insurers are required to provide coverage without cost-sharing consistent with HHS guidelines in the first plan year (in the individual market, policy year) that begins on or after August 1, 2012. ** The July 2011 Institute of Medicine report titled “Clinical preventive services for women: closing the gap” lists recommendations on individual preventive services that may be obtained during a well-woman preventive service visit. † Group health plans sponsored by certain religious employers, and group health insurance coverage in connection with such plans, are exempt from the requirement to cover contraceptive services. SOURCE: Adapted from Healthcare.gov. Affordable Care Act Expands Prevention Coverage for Women’s Health and Well-Being. http://www.hrsa.gov/womensguidelines/. Accessed August 8, 2012. | ||
Contraceptive mandate triggers a firestorm
On February 10, 2012, under pressure from religious groups, the Obama Administration offered a religious exemption to the contraception mandate for certain employers and group health plans. Under this “accommodation,” certain religious employers are exempt from the requirement to cover contraceptive services in their group health plans. An employer qualifies for this exemption if it:
- has the inculcation of religious values as one of its purposes
- primarily employs individuals who share its religious tenets
- primarily serves individuals who share its religious tenets, and
- qualifies for nonprofit status under
Internal Revenue Service (IRS) rules. At the same time that the Obama Administration wanted to accommodate employers’ religious beliefs, it also wanted to ensure that every woman would have access to free preventive care, including contraceptive services, regardless of where she works. And so while the Administration requires insurers to offer group health plan coverage without contraceptive coverage to religious-affiliated organizations, it also requires insurers to provide contraceptive coverage directly to individuals covered under the organization’s group health plan with no cost sharing.
This contraceptive mandate—even with the accommodation—has set off a firestorm on Capitol Hill that will eventually be settled in the courts.
Medicaid expansion falls short of original goal
In National Federation of Independent Business v. Sebelius, the plaintiffs asked the Supreme Court to rule on the federal government’s authority to require states to expand their Medicaid programs. Medicaid costs are typically shared by the federal and state governments. Under the ACA, state Medicaid programs were required to cover nearly all individuals who have incomes below 133% of the federal poverty level—$30,656 for a family of four in 2012—paid entirely by the federal government from 2014 through 2016. After that, the federal share gradually declines to, and then stays at, 90%. States that did not expand their Medicaid programs risked losing all federal Medicaid funding.
The Court ruled that the federal government can expand Medicaid but can’t penalize states that don’t accept the expansion mandate—effectively turning the mandate into a state option. States will receive the additional federal funds if they expand coverage, but states that don’t expand will not be penalized by losing existing federal funds for other parts of the program.
Since the ruling, a number of governors have announced that they will not expand their Medicaid programs, including governors of Florida and Louisiana. Those two states alone are home to 20% of all individuals intended to be covered under the Medicaid expansion.
This part of the ACA is particularly important to women because it strikes, for the first time, the requirement that a low-income woman must be pregnant to receive Medicaid coverage.
The figure below shows the dramatic potential improvement in coverage for women if all states fully implement the Medicaid expansion. Time, court decisions, elections, and state budget fights will determine how much of this change is realized for women’s health.
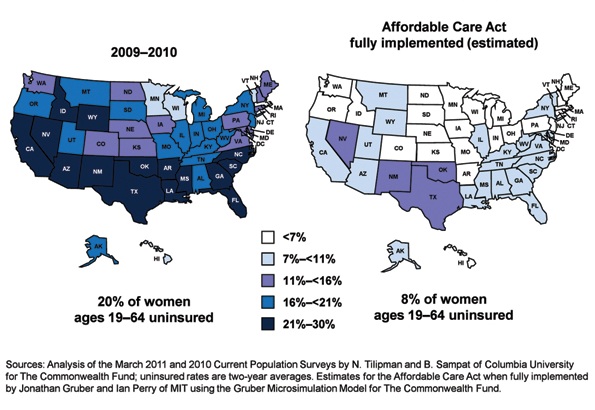
Percentage of insured women will increase under ACA
Percentage of women aged 19 to 64 years who were uninsured in 2009–2012 and under the Affordable Care Act when fully implemented.
SOURCE: Commonwealth Fund. Analysis of the March 2011 and 2010 Current Population Surveys by N. Tilipman and B. Sampat of Columbia University.
Women gain direct access to ObGyns
The ACA guarantees women in all states and all plans direct access to their ObGyns. Before the ACA, women in nine states lacked this guarantee, and women in 16 other states had only limited direct access. Now, a woman can go directly to her ObGyn without having to get a referral from her primary care physician or insurer.
Direct access is especially important because the ACA establishes new delivery systems, such as medical homes and accountable care organizations, designed to capture patients to maximize savings. An ObGyn does not have to be the patient’s primary care provider, and the patient’s access to her ObGyn cannot be limited to a certain number of visits or types of services.
ACA encourages states to cover family-planning services
Under the ACA, states have an easier time covering family-planning services, up to the same eligibility levels as pregnant women. Family planning is still an optional service that a state can choose to extend to women who have incomes above the Medicaid income eligibility level but, before the ACA was enacted, states had to apply to HHS for permission to waive the federal rules, often a very cumbersome process.
Prior to the ACA, 27 states had family planning waivers to provide services to nonpregnant women who had incomes above the Medicaid eligibility level—most at or near 200% of poverty. Now, states can provide family planning services to this population without federal approval.
Don’t miss Dr. Robert L. Barbieri’s October article titled “Gynecologic care across a woman’s life”
Insurance reforms end lifetime limits on coverage
Insurance reforms are important to us and our patients. The better the private health insurance system works—allowing us to provide our best possible care to patients and making sure they can see us when they need our care—the less our nation relies on the public safety net.
Beginning in 2010, the ACA eliminated all lifetime limits on how much insurance companies would cover when beneficiaries get sick; it also bans insurance companies from dropping people from coverage when they get sick. So if your patient has private health insurance and has faithfully paid her premiums and hasn’t committed fraud, her insurer cannot drop her or impose a limit on her coverage once she claims benefits.
This may be especially important for patients who need the most care, such as those who have cancer or another long-term, expensive, and unforeseen diagnosis. Because of this provision, you will not have to worry about your patient losing coverage in the middle of a long course of treatment.
The insurance practice of charging women more than men for equivalent policies ended on January 1, 2011, making insurance more affordable for our patients. Insurers in the individual and small group markets are allowed to vary premiums only for age, geographic location, family size, and tobacco use, not for gender—another important aspect of the law.
2014 is a key year in health reform
Exchanges begin
In 2014, under the ACA, state health insurance exchanges become reality.
An exchange is a marketplace where people can shop for health insurance; private health insurers can market their insurance products in state and multistate exchanges if they comply with new federal insurance reforms established in the ACA and offer the minimum benefits packages established by each state. Exchanges are intended to offer patients a choice of health insurance plans that are affordable, comprehensive, and easy to compare. Low-income individuals will be able to purchase private insurance in the exchanges with the federal premium subsidies or tax credits.
Insurers wanting to market their policies in an exchange may not deny coverage for preexisting conditions, including pregnancy, domestic violence, and previous cesarean delivery. They can’t deny coverage on the basis of an individual’s medical history, health status, genetic information, or disability. And they can’t impose waiting periods longer than 90 days before coverage takes effect, including 9-month waiting periods before maternity coverage.
Essential benefits are established
The ACA sets a minimum standard of health-care coverage that must be included in nearly every private insurance policy. The intent is that every person in the United States, regardless of where they live, who employs them, and what their income is, should have access to the same basic care.
Effective January 1, 2014, all insurance plans, except plans that existed before the ACA was enacted on March 23, 2010, must offer an “essential health benefits” (EHB) package, which must include:
- ambulatory patient services
- emergency services
- hospitalization
- maternity and newborn care
- mental health and substance use disorder services
- prescription drugs
- rehabilitative and habilitative services and devices
- laboratory services
- women’s preventive and wellness services and chronic disease management
- pediatric services, including oral and vision care.
Last December, HHS surprised many by giving states flexibility to design their own EHB packages, as long as the packages included each service on the list.
To choose its EHB package, a state must select a “benchmark” plan from the top- selling plans in four markets: federal and state public employee plans, commercial HMO plans, and small business plans. If a state doesn’t select a benchmark plan, the EHB defaults to the largest small-group market plan in the state. Each state must also choose an EHB package for its Medicaid program using the same 10 benefit categories.
State EHB plans must follow ACA requirements on annual and lifetime dollar limits but may impose limits on the scope and duration of coverage.
As for state-mandated benefits, if a state selects an EHB package that does not include a benefit already mandated by the state, the state must fund coverage for that service on its own—a decision HHS has promised to revisit in 2016.
Abortion decisions reside with the states
ACA requirements regarding abortion coverage 1) take effect in 2014 and 2) apply only to private health insurance plans marketed in the state exchanges that 3) cover abortions beyond those eligible for Medicaid coverage now, which are those that involve cases of rape or incest or that are necessary to save the life of the mother. Medicaid coverage for these categories of abortion is allowed under the Hyde Amendment.
Each insurer marketing a health plan in an exchange can determine whether or not its plan will cover abortion and, if it does, whether coverage will be limited to or go beyond those allowed under the Hyde Amendment. No federal tax or premium subsidies may be used to pay for abortions beyond those permitted by the Hyde Amendment.
The Secretary of HHS must ensure that at least one plan in each state exchange covers abortion, and that at least one plan either covers no abortions or limits abortions to those allowed under the Hyde Amendment. Insurers who offer abortion coverage beyond Hyde have to comply with a number of administrative requirements.
Congress was clear that the ultimate decisions about abortion should be made at the state rather than the federal level, and it gave states the ultimate trump card: Any state can pass legislation that prohibits any plan from offering abortion coverage of any kind within that state’s exchange. Any state can prohibit insurers offering plans within that state’s exchange from including any abortion coverage.
10 additional health provisions under the ACA
1. Creation of women's medical homes
The law points the way for creation of medical homes for women in the Medicare and Medicaid programs. The bill establishes an Innovation Center within the Centers for Medicare and Medicaid Services that has broad authority to evaluate, test, and adopt systems that foster patient-centered care, improve quality, and contain costs under Medicare, Medicaid, and the Children’s Health Insurance Program (CHIP)—and this includes patient-centered medical homes that address women’s unique health needs. ObGyn practices are eligible to participate and to receive additional reimbursement if they do.
2. Smoking-cessation counseling in pregnancy
The framers of the ACA recognized the large negative impact that smoking has on health, especially during pregnancy. Studies suggest that the intervention of a physician—most notably, counseling of the patient to quit smoking—has strong potential to modify this behavior. The new law provides reimbursement for this intervention. There are no copays or deductibles for patients, and smoking-cessation services can include diagnostic, therapeutic, and counseling modalities in addition to prescription of pharmacotherapy.
Before this bill became law, only 24 state Medicaid programs paid ObGyns or other physicians for smoking-cessation counseling of pregnant patients, and five states provided no coverage at all. Now, all pregnant Medicaid patients can get this counseling, and you’ll be paid for this important service.
3. Payments to nonphysician providers in freestanding birth centers
Before the ACA became law, Medicaid was authorized to pay hospitals and other facilities operated by and under the supervision of a physician; no payments were authorized for services of an ambulatory center operated by other health professionals. The ACA authorizes Medicaid payments to state-recognized freestanding birth centers not operated by or under the supervision of a physician. A state that doesn’t currently license birth centers must pass legislation and license these centers before the centers can receive these payments.
Medicaid will also reimburse providers who practice in state-recognized freestanding birth centers, as long as the individuals are practicing within their state’s scope of practice laws and regulations. Because the type of provider is not specified but instead left up to each state’s scope of practice laws and regulations, this provision could allow for separate provider payments for physicians, certified nurse midwives, certified professional midwives, and doulas.
4. Immigrant coverage
Legal immigrants are bound by the individual coverage mandate and must purchase health insurance. These individuals are eligible for income-related premium credits and subsidies for insurance purchased through an exchange. Legal immigrants who are barred from Medicaid during their first 5 years in the United States (by earlier law) are eligible for premium credits only.
Undocumented immigrants are not eligible for Medicaid, premium credits, or subsidies and are barred from purchasing insurance in the exchange, even with their own money.
5. Postpartum depression
Health reform will help bring perinatal and postpartum depression out of the shadows by providing federal funds for research, patient education, and clinical treatment. For example, the federal Department of Health and Human Services (HHS) will:
- conduct research into the causes of, and treatments for, postpartum conditions
- create a national public awareness campaign to increase awareness and knowledge of postpartum depression and psychosis
- provide grants to study the benefits of screening for postpartum depression and psychosis
- establish grants to deliver or enhance outpatient, inpatient, and home-based health and support services, including case management and comprehensive treatment services for individuals with, or at risk for, postpartum conditions.
The National Institute of Mental Health is encouraged to conduct a 10-year longitudinal study on the mental health consequences of pregnancy. This study is intended to focus on perinatal depression.
Community health centers will be eligible for grants in 2012 (as they were in 2011) to the tune of $3 million for inpatient and outpatient counseling and services.
And a federal public awareness campaign will educate the public through radio and television ads.
These endeavors point to the need for ObGyns to familiarize themselves with postpartum depression—if they aren’t already well versed in the subject—because patients are likely to become more aware of this issue and look to their ObGyns for answers.
6. Maternal home visits
Congress established a new Maternal, Infant, and Early Childhood Home Visiting program to improve maternal and fetal health in underserved areas of our country. This program will provide funds to states, tribes, and territories to develop and implement evidence-based home-visitation models to reduce infant and maternal mortality and its causes by producing improvements in:
- prenatal, maternal, and newborn health
- child health and development
- parenting skills
- school readiness
- juvenile delinquency
- family economic self-sufficiency.
These programs will have to demonstrate effectiveness and improved outcomes. HHS recently requested suggestions on ways of demonstrating the effectiveness of home-visiting program models for pregnant women, expectant fathers, and caregivers of children from birth through entry into kindergarten.
The law appropriates $350 million to this program in 2012 and $400 million in both 2013 and 2014.
7. Assistance for pregnant students
A new Pregnancy Assistance Fund—$25 million annually over 10 years (fiscal years 2010–2019)—requires the Secretary of HHS (in collaboration with the Secretary of Education) to establish a state grant program to help pregnant and parenting teens and young women. The aim of this program is to help teens who become pregnant and who choose to bring their pregnancies to term or keep their babies, or both, to stay in school. Grants will go to institutions of higher education, high schools and community service centers, as well as state attorneys general.
Institutions that receive grants must work with providers to meet specific practical needs of pregnant or parenting students:
- housing
- childcare
- parenting education
- postpartum counseling
- assistance in finding and accessing needed services
- referrals for prenatal care and delivery, infant or foster care, or adoption.
Funds to attorneys general will be used to combat domestic violence among pregnant teens.
8. Young women's breast cancer
A new program is intended to help educate young women about the importance of breast health and screening, in two ways:
- The National Institutes of Health (NIH) will conduct research to develop and test screening measures for prevention and early detection of breast cancer in women 15 to 44 years old.
- The US Department of HHS will create a national awareness campaign, with $9 million in funding each year from 2010 to 2014, to encourage young women to talk with their doctors about breast cancer and early detection.
ObGyns can expect to see more interest and questions about breast health among young women and their mothers. It pays to be prepared with good information for these important conversations.
9. Personal responsibility education
From 2010 through 2014, each state will receive funds for personal responsibility education programs aimed at reducing pregnancy in youths. Funds are $75 million for each fiscal year, allocated to each state depending on the size of its youth population but not intended to be less than $250,000 per state.
Educational programs eligible for federal funds must include both abstinence and contraception information for prevention of teenage pregnancy and sexually transmitted infections, including HIV/AIDS, as well as three or more adulthood-preparation subjects.
10. Community-based support of Patient-Centered Medical Homes
Federal funding is available to states for the development of community-based health teams to support medical homes run by primary care practices. These teams may include specialists, nurses, pharmacists, nutritionists, dieticians, social workers, behavioral and mental health providers, and physician assistants. Primary care practices in this program function as medical homes and are responsible for addressing a patient’s personal health-care needs. The team links the medical home to community support services for its patients.
Eligible ObGyn practices can qualify as primary care practices, and ObGyns are eligible to serve as specialist members of the community-based health team.
ACA is a mixed bag for ObGyns
Women have much to gain from the provisions of the ACA. It’s also true that many parts of the law are terrible for practicing ObGyns, including the Independent Payment Advisory Board (IPAB) and the absence of meaningful medical liability reform. For more on these issues, see “Is private ObGyn practice on its way out?” which appears in the October 2011 issue of OBG Management (available in the archive at obgmanagement.com). ACOG is committed to working with Congress to repeal or remedy those aspects of the law.
A recent study reveals that almost one-third of physicians are no longer accepting Medicaid patients
If all states expanded Medicaid to cover people with incomes at or below 138% of the federal poverty level in 2014, as the Affordable Care Act (ACA) proposes, 23 million people would become eligible for the program.1
That statistic prompts important questions:
- Would the health-care workforce be able to meet the demand of caring for all these new patients?
- Would it be willing?
A recent analysis of data from 4,326 office-based physicians suggests that the answer to both questions is “No”: Almost one-third of these providers were already declining to accept new Medicaid patients in 2011.2
Although 96% of physicians in the analysis accepted new patients in 2011, the percentage of physicians accepting new patients covered by Medicaid was lower (69%), as was the percentage accepting new self-paying patients (91.7%), patients covered by Medicare (83%), and patients with private insurance (82%).2
Physicians who were in solo practice were 23.5% less likely to accept new Medicaid patients, compared with those who practiced in an office with 10 or more other physicians.2
The data from this study come from the 2011 National Ambulatory Medical Care Survey Electronic Medical Records Supplement, a survey conducted by the Centers for Disease Control and Prevention National Center for Health Statistics. The survey included questions exploring whether physicians were accepting new patients.2
Earlier studies have found that the low reimbursement levels for care delivered through Medicaid has deterred many physicians from accepting patients.3
The view in the ObGyn specialty
The findings of this analysis were not broken down by specialty—only by primary care versus non–primary care. To get an idea of conditions in the ObGyn specialty, OBG Management surveyed the members of its Virtual Board of Editors (VBE). Of the 117 members contacted, 61 responded—a response rate of 52.1%. Roughly three-quarters (75.4%) reported that they currently treat patients covered by Medicaid, but only 60.7% are accepting new patients covered by Medicaid. Twenty-one percent of respondents reported that they have not and will not accept patients covered by Medicaid.
When asked to comment on their level of satisfaction with Medicaid, the most common response among VBE members was dissatisfaction due to “insufficient reimbursement.”
“I am not satisfied with Medicaid,” commented one VBE member. “The reimbursement is terrible….I have certainly thought of stopping care for Medicaid patients and, if Congress ever allows the big cuts to reimbursement that are threatened every year, I think I would stop.”
Another VBE member reported extreme dissatisfaction with Medicaid because of “lousy” reimbursement. He also pointed to “all the paperwork and crazy regulations that require inordinate time and additional personnel just to handle….and then [the claim] gets denied for reasons beyond reason.” He added that physicians who do accept Medicaid “are on the fast track to sainthood.”
Other reasons for refusing to accept patients with Medicaid (or, if Medicaid was accepted, for high levels of aggravation with the program):
- payment rejections
- too many different categories of coverage “that patients are completely uninformed about”
- difficulty finding a specialist who will manage high-risk patients covered by Medicaid
- red tape
- the complex health problems that Medicaid patients tend to have, compared with patients who have other types of coverage.
One VBE member summed up his feelings in one word: “Phooey.”
Several VBE members suggested that health reform should focus on the Medicaid program.
“These plans are just sucking up the state’s money and paying docs peanuts and their administrators big bucks!” wrote Mary Vanko, MD, of Munster, Indiana.
“I’m tired of how much Medicaid is being abused by people,” commented another VBE member. “People using other people’s cards, people with regular insurance getting Medicaid to cover their copays. The whole system needs reform!”
Some physicians were satisfied with Medicaid
Among the respondents were several who reported being satisfied with the program, including one who called the experience “good” and another who reported being “shielded from the reimbursement issues.”
“I have no problems with Medicaid,” wrote another.
—Janelle Yates, Senior Editor
References
1. Kenney GM, Dubay L, Zuckerman S, Huntress M. Making the Medicaid Expansion an ACA Option: How Many Low-Income Americans Could Remain Uninsured? Washington, DC: Urban Institute Health Policy Center; June 29, 2012. http://www.urban.org/UploadedPDF/412606-Making-the-Medicaid-Expansion-an-ACA-Option.pdf. Accessed August 18, 2012.
2. Decker SL. In 2011 nearly one-third of physicians said they would not accept new Medicaid patients, but rising fees may help. Health Affairs. 2012;31(8):1673–1679.
3. Centers for Disease Control and Prevention. QuickStats: percentage of office-based physicians accepting new patients, by types of payment accepted—United States, 1999–2000 and 2008–2009. MMWR Morb Mortal Wkly Rep. 2011;60(27):928.
We want to hear from you! Tell us what you think.
Lay midwives and the ObGyn: Is collaboration risky?
(May 2012)
How state budget crises are putting the squeeze on Medicaid (and you)
(February 2012)
Is private ObGyn practice on its way out?
(October 2011)
14 questions (and answers) about health reform and you
with Janelle Yates, Senior Editor (August 2010)
For the first half of 2012, the big question was: Will anything be covered under the Affordable Care Act (ACA)? After considering constitutional challenges to the Act that had the potential to invalidate the entire law, the US Supreme Court ruled, on June 28, that the ACA met constitutional muster in National Federation of Independent Business v. Sebelius (2012).
Now that the Court has upheld the ACA, let’s review the major women’s health services included under the law. This Web version incorporates 10 more women's health provisions from the ACA, from smoking cessation to young women’s breast cancer, that were not in the print version.

Preventive services guaranteed without copays
A major component of the health reform law went into effect August 1, 2012; it requires most health plans to cover women’s preventive services without requiring enrollees to pay a copay or deductibles. This provision reflects Congress’ understanding that women have a longer life expectancy and bear a greater burden of chronic disease, disability, and reproductive and gender-specific conditions. In addition, women often have a different response to treatment than men do.
The federal Department of Health and Human Services (HHS) estimates that Americans use preventive services at only about half of the recommended rate. By 2013, as many as 73 million individuals will benefit from preventive care offered under the law.
The American Congress of Obstetricians and Gynecologists (ACOG) worked with the Institute of Medicine (IOM)—which was charged with advising HHS—to encourage the inclusion of women’s preventive services specified in ACOG guidelines to ensure women’s health and well-being. As ACOG Executive Vice President Hal C. Lawrence, MD, told the IOM in January 2011:
- The College’s clinical guidelines…offer an excellent resource…and encompass the entire field of women’s preventive care. Our guidance is based on the best available evidence and is developed by committees with expertise reflecting the breadth of women’s health care and subject to a rigorous conflict of interest policy.
Dr. Lawrence further urged the IOM “to recommend coverage of the following services and products without cost-sharing”:
- well-woman visits
- preconception care
- family planning counseling and services
- HIV screening (for women at average risk)
- screening for intimate partner violence
- testing for human papillomavirus (HPV) as part of cervical cancer screening.
ACOG’s recommendations were approved by the IOM and, subsequently, by HHS. As a result, all private health plans that began on or after September 30, 2010, are required to cover these services at no out-of-pocket cost to patients (TABLE).
Women’s preventive services guaranteed under ACA*
| Service | Frequency | HHS guidelines for health insurance coverage |
|---|---|---|
| Well-woman visit | Annual for adult women, although HHS recognizes that several visits may be needed to obtain all necessary recommended preventive services, depending on a woman’s health status, health needs, and other risk factors** | The visit should focus on preventive services that are appropriate for the patient’s age and development, including preconception and prenatal care. This visit should, where appropriate, include other preventive services listed in this set of guidelines, as well as others referenced in section 2713 |
| Screening for gestational diabetes | Between 24 and 28 weeks of gestation and at the first prenatal visit for pregnant women identified to be at high risk for diabetes | |
| Testing for human papillomavirus (HPV) | At age 30 and older, no more frequently than every 3 years | High-risk HPV DNA testing in women who have normal cervical cytology |
| Counseling about sexually transmitted infection (STI) | Annual | All sexually active women |
| Counseling about and screening for HIV | Annual | All sexually active women |
| Counseling about and provision of contraception† | As prescribed | All FDA-approved contraceptive methods and sterilization procedures. Counseling for all women with reproductive capacity |
| Breastfeeding support, supplies, and counseling | In conjunction with each birth | Comprehensive lactation support and counseling by a trained provider during pregnancy or postpartum (or both), as well as costs for renting breastfeeding equipment |
| Screening for and counseling about interpersonal and domestic violence | Annual | |
| HHS = Health and Human Services * HHS guidelines are effective August 1, 2011. Nongrandfathered plans and insurers are required to provide coverage without cost-sharing consistent with HHS guidelines in the first plan year (in the individual market, policy year) that begins on or after August 1, 2012. ** The July 2011 Institute of Medicine report titled “Clinical preventive services for women: closing the gap” lists recommendations on individual preventive services that may be obtained during a well-woman preventive service visit. † Group health plans sponsored by certain religious employers, and group health insurance coverage in connection with such plans, are exempt from the requirement to cover contraceptive services. SOURCE: Adapted from Healthcare.gov. Affordable Care Act Expands Prevention Coverage for Women’s Health and Well-Being. http://www.hrsa.gov/womensguidelines/. Accessed August 8, 2012. | ||
Contraceptive mandate triggers a firestorm
On February 10, 2012, under pressure from religious groups, the Obama Administration offered a religious exemption to the contraception mandate for certain employers and group health plans. Under this “accommodation,” certain religious employers are exempt from the requirement to cover contraceptive services in their group health plans. An employer qualifies for this exemption if it:
- has the inculcation of religious values as one of its purposes
- primarily employs individuals who share its religious tenets
- primarily serves individuals who share its religious tenets, and
- qualifies for nonprofit status under
Internal Revenue Service (IRS) rules. At the same time that the Obama Administration wanted to accommodate employers’ religious beliefs, it also wanted to ensure that every woman would have access to free preventive care, including contraceptive services, regardless of where she works. And so while the Administration requires insurers to offer group health plan coverage without contraceptive coverage to religious-affiliated organizations, it also requires insurers to provide contraceptive coverage directly to individuals covered under the organization’s group health plan with no cost sharing.
This contraceptive mandate—even with the accommodation—has set off a firestorm on Capitol Hill that will eventually be settled in the courts.
Medicaid expansion falls short of original goal
In National Federation of Independent Business v. Sebelius, the plaintiffs asked the Supreme Court to rule on the federal government’s authority to require states to expand their Medicaid programs. Medicaid costs are typically shared by the federal and state governments. Under the ACA, state Medicaid programs were required to cover nearly all individuals who have incomes below 133% of the federal poverty level—$30,656 for a family of four in 2012—paid entirely by the federal government from 2014 through 2016. After that, the federal share gradually declines to, and then stays at, 90%. States that did not expand their Medicaid programs risked losing all federal Medicaid funding.
The Court ruled that the federal government can expand Medicaid but can’t penalize states that don’t accept the expansion mandate—effectively turning the mandate into a state option. States will receive the additional federal funds if they expand coverage, but states that don’t expand will not be penalized by losing existing federal funds for other parts of the program.
Since the ruling, a number of governors have announced that they will not expand their Medicaid programs, including governors of Florida and Louisiana. Those two states alone are home to 20% of all individuals intended to be covered under the Medicaid expansion.
This part of the ACA is particularly important to women because it strikes, for the first time, the requirement that a low-income woman must be pregnant to receive Medicaid coverage.
The figure below shows the dramatic potential improvement in coverage for women if all states fully implement the Medicaid expansion. Time, court decisions, elections, and state budget fights will determine how much of this change is realized for women’s health.
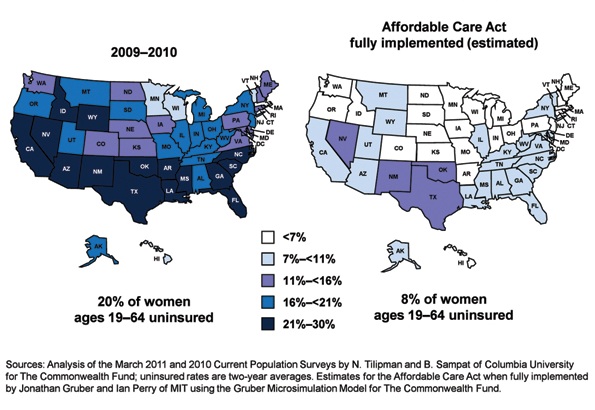
Percentage of insured women will increase under ACA
Percentage of women aged 19 to 64 years who were uninsured in 2009–2012 and under the Affordable Care Act when fully implemented.
SOURCE: Commonwealth Fund. Analysis of the March 2011 and 2010 Current Population Surveys by N. Tilipman and B. Sampat of Columbia University.
Women gain direct access to ObGyns
The ACA guarantees women in all states and all plans direct access to their ObGyns. Before the ACA, women in nine states lacked this guarantee, and women in 16 other states had only limited direct access. Now, a woman can go directly to her ObGyn without having to get a referral from her primary care physician or insurer.
Direct access is especially important because the ACA establishes new delivery systems, such as medical homes and accountable care organizations, designed to capture patients to maximize savings. An ObGyn does not have to be the patient’s primary care provider, and the patient’s access to her ObGyn cannot be limited to a certain number of visits or types of services.
ACA encourages states to cover family-planning services
Under the ACA, states have an easier time covering family-planning services, up to the same eligibility levels as pregnant women. Family planning is still an optional service that a state can choose to extend to women who have incomes above the Medicaid income eligibility level but, before the ACA was enacted, states had to apply to HHS for permission to waive the federal rules, often a very cumbersome process.
Prior to the ACA, 27 states had family planning waivers to provide services to nonpregnant women who had incomes above the Medicaid eligibility level—most at or near 200% of poverty. Now, states can provide family planning services to this population without federal approval.
Don’t miss Dr. Robert L. Barbieri’s October article titled “Gynecologic care across a woman’s life”
Insurance reforms end lifetime limits on coverage
Insurance reforms are important to us and our patients. The better the private health insurance system works—allowing us to provide our best possible care to patients and making sure they can see us when they need our care—the less our nation relies on the public safety net.
Beginning in 2010, the ACA eliminated all lifetime limits on how much insurance companies would cover when beneficiaries get sick; it also bans insurance companies from dropping people from coverage when they get sick. So if your patient has private health insurance and has faithfully paid her premiums and hasn’t committed fraud, her insurer cannot drop her or impose a limit on her coverage once she claims benefits.
This may be especially important for patients who need the most care, such as those who have cancer or another long-term, expensive, and unforeseen diagnosis. Because of this provision, you will not have to worry about your patient losing coverage in the middle of a long course of treatment.
The insurance practice of charging women more than men for equivalent policies ended on January 1, 2011, making insurance more affordable for our patients. Insurers in the individual and small group markets are allowed to vary premiums only for age, geographic location, family size, and tobacco use, not for gender—another important aspect of the law.
2014 is a key year in health reform
Exchanges begin
In 2014, under the ACA, state health insurance exchanges become reality.
An exchange is a marketplace where people can shop for health insurance; private health insurers can market their insurance products in state and multistate exchanges if they comply with new federal insurance reforms established in the ACA and offer the minimum benefits packages established by each state. Exchanges are intended to offer patients a choice of health insurance plans that are affordable, comprehensive, and easy to compare. Low-income individuals will be able to purchase private insurance in the exchanges with the federal premium subsidies or tax credits.
Insurers wanting to market their policies in an exchange may not deny coverage for preexisting conditions, including pregnancy, domestic violence, and previous cesarean delivery. They can’t deny coverage on the basis of an individual’s medical history, health status, genetic information, or disability. And they can’t impose waiting periods longer than 90 days before coverage takes effect, including 9-month waiting periods before maternity coverage.
Essential benefits are established
The ACA sets a minimum standard of health-care coverage that must be included in nearly every private insurance policy. The intent is that every person in the United States, regardless of where they live, who employs them, and what their income is, should have access to the same basic care.
Effective January 1, 2014, all insurance plans, except plans that existed before the ACA was enacted on March 23, 2010, must offer an “essential health benefits” (EHB) package, which must include:
- ambulatory patient services
- emergency services
- hospitalization
- maternity and newborn care
- mental health and substance use disorder services
- prescription drugs
- rehabilitative and habilitative services and devices
- laboratory services
- women’s preventive and wellness services and chronic disease management
- pediatric services, including oral and vision care.
Last December, HHS surprised many by giving states flexibility to design their own EHB packages, as long as the packages included each service on the list.
To choose its EHB package, a state must select a “benchmark” plan from the top- selling plans in four markets: federal and state public employee plans, commercial HMO plans, and small business plans. If a state doesn’t select a benchmark plan, the EHB defaults to the largest small-group market plan in the state. Each state must also choose an EHB package for its Medicaid program using the same 10 benefit categories.
State EHB plans must follow ACA requirements on annual and lifetime dollar limits but may impose limits on the scope and duration of coverage.
As for state-mandated benefits, if a state selects an EHB package that does not include a benefit already mandated by the state, the state must fund coverage for that service on its own—a decision HHS has promised to revisit in 2016.
Abortion decisions reside with the states
ACA requirements regarding abortion coverage 1) take effect in 2014 and 2) apply only to private health insurance plans marketed in the state exchanges that 3) cover abortions beyond those eligible for Medicaid coverage now, which are those that involve cases of rape or incest or that are necessary to save the life of the mother. Medicaid coverage for these categories of abortion is allowed under the Hyde Amendment.
Each insurer marketing a health plan in an exchange can determine whether or not its plan will cover abortion and, if it does, whether coverage will be limited to or go beyond those allowed under the Hyde Amendment. No federal tax or premium subsidies may be used to pay for abortions beyond those permitted by the Hyde Amendment.
The Secretary of HHS must ensure that at least one plan in each state exchange covers abortion, and that at least one plan either covers no abortions or limits abortions to those allowed under the Hyde Amendment. Insurers who offer abortion coverage beyond Hyde have to comply with a number of administrative requirements.
Congress was clear that the ultimate decisions about abortion should be made at the state rather than the federal level, and it gave states the ultimate trump card: Any state can pass legislation that prohibits any plan from offering abortion coverage of any kind within that state’s exchange. Any state can prohibit insurers offering plans within that state’s exchange from including any abortion coverage.
10 additional health provisions under the ACA
1. Creation of women's medical homes
The law points the way for creation of medical homes for women in the Medicare and Medicaid programs. The bill establishes an Innovation Center within the Centers for Medicare and Medicaid Services that has broad authority to evaluate, test, and adopt systems that foster patient-centered care, improve quality, and contain costs under Medicare, Medicaid, and the Children’s Health Insurance Program (CHIP)—and this includes patient-centered medical homes that address women’s unique health needs. ObGyn practices are eligible to participate and to receive additional reimbursement if they do.
2. Smoking-cessation counseling in pregnancy
The framers of the ACA recognized the large negative impact that smoking has on health, especially during pregnancy. Studies suggest that the intervention of a physician—most notably, counseling of the patient to quit smoking—has strong potential to modify this behavior. The new law provides reimbursement for this intervention. There are no copays or deductibles for patients, and smoking-cessation services can include diagnostic, therapeutic, and counseling modalities in addition to prescription of pharmacotherapy.
Before this bill became law, only 24 state Medicaid programs paid ObGyns or other physicians for smoking-cessation counseling of pregnant patients, and five states provided no coverage at all. Now, all pregnant Medicaid patients can get this counseling, and you’ll be paid for this important service.
3. Payments to nonphysician providers in freestanding birth centers
Before the ACA became law, Medicaid was authorized to pay hospitals and other facilities operated by and under the supervision of a physician; no payments were authorized for services of an ambulatory center operated by other health professionals. The ACA authorizes Medicaid payments to state-recognized freestanding birth centers not operated by or under the supervision of a physician. A state that doesn’t currently license birth centers must pass legislation and license these centers before the centers can receive these payments.
Medicaid will also reimburse providers who practice in state-recognized freestanding birth centers, as long as the individuals are practicing within their state’s scope of practice laws and regulations. Because the type of provider is not specified but instead left up to each state’s scope of practice laws and regulations, this provision could allow for separate provider payments for physicians, certified nurse midwives, certified professional midwives, and doulas.
4. Immigrant coverage
Legal immigrants are bound by the individual coverage mandate and must purchase health insurance. These individuals are eligible for income-related premium credits and subsidies for insurance purchased through an exchange. Legal immigrants who are barred from Medicaid during their first 5 years in the United States (by earlier law) are eligible for premium credits only.
Undocumented immigrants are not eligible for Medicaid, premium credits, or subsidies and are barred from purchasing insurance in the exchange, even with their own money.
5. Postpartum depression
Health reform will help bring perinatal and postpartum depression out of the shadows by providing federal funds for research, patient education, and clinical treatment. For example, the federal Department of Health and Human Services (HHS) will:
- conduct research into the causes of, and treatments for, postpartum conditions
- create a national public awareness campaign to increase awareness and knowledge of postpartum depression and psychosis
- provide grants to study the benefits of screening for postpartum depression and psychosis
- establish grants to deliver or enhance outpatient, inpatient, and home-based health and support services, including case management and comprehensive treatment services for individuals with, or at risk for, postpartum conditions.
The National Institute of Mental Health is encouraged to conduct a 10-year longitudinal study on the mental health consequences of pregnancy. This study is intended to focus on perinatal depression.
Community health centers will be eligible for grants in 2012 (as they were in 2011) to the tune of $3 million for inpatient and outpatient counseling and services.
And a federal public awareness campaign will educate the public through radio and television ads.
These endeavors point to the need for ObGyns to familiarize themselves with postpartum depression—if they aren’t already well versed in the subject—because patients are likely to become more aware of this issue and look to their ObGyns for answers.
6. Maternal home visits
Congress established a new Maternal, Infant, and Early Childhood Home Visiting program to improve maternal and fetal health in underserved areas of our country. This program will provide funds to states, tribes, and territories to develop and implement evidence-based home-visitation models to reduce infant and maternal mortality and its causes by producing improvements in:
- prenatal, maternal, and newborn health
- child health and development
- parenting skills
- school readiness
- juvenile delinquency
- family economic self-sufficiency.
These programs will have to demonstrate effectiveness and improved outcomes. HHS recently requested suggestions on ways of demonstrating the effectiveness of home-visiting program models for pregnant women, expectant fathers, and caregivers of children from birth through entry into kindergarten.
The law appropriates $350 million to this program in 2012 and $400 million in both 2013 and 2014.
7. Assistance for pregnant students
A new Pregnancy Assistance Fund—$25 million annually over 10 years (fiscal years 2010–2019)—requires the Secretary of HHS (in collaboration with the Secretary of Education) to establish a state grant program to help pregnant and parenting teens and young women. The aim of this program is to help teens who become pregnant and who choose to bring their pregnancies to term or keep their babies, or both, to stay in school. Grants will go to institutions of higher education, high schools and community service centers, as well as state attorneys general.
Institutions that receive grants must work with providers to meet specific practical needs of pregnant or parenting students:
- housing
- childcare
- parenting education
- postpartum counseling
- assistance in finding and accessing needed services
- referrals for prenatal care and delivery, infant or foster care, or adoption.
Funds to attorneys general will be used to combat domestic violence among pregnant teens.
8. Young women's breast cancer
A new program is intended to help educate young women about the importance of breast health and screening, in two ways:
- The National Institutes of Health (NIH) will conduct research to develop and test screening measures for prevention and early detection of breast cancer in women 15 to 44 years old.
- The US Department of HHS will create a national awareness campaign, with $9 million in funding each year from 2010 to 2014, to encourage young women to talk with their doctors about breast cancer and early detection.
ObGyns can expect to see more interest and questions about breast health among young women and their mothers. It pays to be prepared with good information for these important conversations.
9. Personal responsibility education
From 2010 through 2014, each state will receive funds for personal responsibility education programs aimed at reducing pregnancy in youths. Funds are $75 million for each fiscal year, allocated to each state depending on the size of its youth population but not intended to be less than $250,000 per state.
Educational programs eligible for federal funds must include both abstinence and contraception information for prevention of teenage pregnancy and sexually transmitted infections, including HIV/AIDS, as well as three or more adulthood-preparation subjects.
10. Community-based support of Patient-Centered Medical Homes
Federal funding is available to states for the development of community-based health teams to support medical homes run by primary care practices. These teams may include specialists, nurses, pharmacists, nutritionists, dieticians, social workers, behavioral and mental health providers, and physician assistants. Primary care practices in this program function as medical homes and are responsible for addressing a patient’s personal health-care needs. The team links the medical home to community support services for its patients.
Eligible ObGyn practices can qualify as primary care practices, and ObGyns are eligible to serve as specialist members of the community-based health team.
ACA is a mixed bag for ObGyns
Women have much to gain from the provisions of the ACA. It’s also true that many parts of the law are terrible for practicing ObGyns, including the Independent Payment Advisory Board (IPAB) and the absence of meaningful medical liability reform. For more on these issues, see “Is private ObGyn practice on its way out?” which appears in the October 2011 issue of OBG Management (available in the archive at obgmanagement.com). ACOG is committed to working with Congress to repeal or remedy those aspects of the law.
A recent study reveals that almost one-third of physicians are no longer accepting Medicaid patients
If all states expanded Medicaid to cover people with incomes at or below 138% of the federal poverty level in 2014, as the Affordable Care Act (ACA) proposes, 23 million people would become eligible for the program.1
That statistic prompts important questions:
- Would the health-care workforce be able to meet the demand of caring for all these new patients?
- Would it be willing?
A recent analysis of data from 4,326 office-based physicians suggests that the answer to both questions is “No”: Almost one-third of these providers were already declining to accept new Medicaid patients in 2011.2
Although 96% of physicians in the analysis accepted new patients in 2011, the percentage of physicians accepting new patients covered by Medicaid was lower (69%), as was the percentage accepting new self-paying patients (91.7%), patients covered by Medicare (83%), and patients with private insurance (82%).2
Physicians who were in solo practice were 23.5% less likely to accept new Medicaid patients, compared with those who practiced in an office with 10 or more other physicians.2
The data from this study come from the 2011 National Ambulatory Medical Care Survey Electronic Medical Records Supplement, a survey conducted by the Centers for Disease Control and Prevention National Center for Health Statistics. The survey included questions exploring whether physicians were accepting new patients.2
Earlier studies have found that the low reimbursement levels for care delivered through Medicaid has deterred many physicians from accepting patients.3
The view in the ObGyn specialty
The findings of this analysis were not broken down by specialty—only by primary care versus non–primary care. To get an idea of conditions in the ObGyn specialty, OBG Management surveyed the members of its Virtual Board of Editors (VBE). Of the 117 members contacted, 61 responded—a response rate of 52.1%. Roughly three-quarters (75.4%) reported that they currently treat patients covered by Medicaid, but only 60.7% are accepting new patients covered by Medicaid. Twenty-one percent of respondents reported that they have not and will not accept patients covered by Medicaid.
When asked to comment on their level of satisfaction with Medicaid, the most common response among VBE members was dissatisfaction due to “insufficient reimbursement.”
“I am not satisfied with Medicaid,” commented one VBE member. “The reimbursement is terrible….I have certainly thought of stopping care for Medicaid patients and, if Congress ever allows the big cuts to reimbursement that are threatened every year, I think I would stop.”
Another VBE member reported extreme dissatisfaction with Medicaid because of “lousy” reimbursement. He also pointed to “all the paperwork and crazy regulations that require inordinate time and additional personnel just to handle….and then [the claim] gets denied for reasons beyond reason.” He added that physicians who do accept Medicaid “are on the fast track to sainthood.”
Other reasons for refusing to accept patients with Medicaid (or, if Medicaid was accepted, for high levels of aggravation with the program):
- payment rejections
- too many different categories of coverage “that patients are completely uninformed about”
- difficulty finding a specialist who will manage high-risk patients covered by Medicaid
- red tape
- the complex health problems that Medicaid patients tend to have, compared with patients who have other types of coverage.
One VBE member summed up his feelings in one word: “Phooey.”
Several VBE members suggested that health reform should focus on the Medicaid program.
“These plans are just sucking up the state’s money and paying docs peanuts and their administrators big bucks!” wrote Mary Vanko, MD, of Munster, Indiana.
“I’m tired of how much Medicaid is being abused by people,” commented another VBE member. “People using other people’s cards, people with regular insurance getting Medicaid to cover their copays. The whole system needs reform!”
Some physicians were satisfied with Medicaid
Among the respondents were several who reported being satisfied with the program, including one who called the experience “good” and another who reported being “shielded from the reimbursement issues.”
“I have no problems with Medicaid,” wrote another.
—Janelle Yates, Senior Editor
References
1. Kenney GM, Dubay L, Zuckerman S, Huntress M. Making the Medicaid Expansion an ACA Option: How Many Low-Income Americans Could Remain Uninsured? Washington, DC: Urban Institute Health Policy Center; June 29, 2012. http://www.urban.org/UploadedPDF/412606-Making-the-Medicaid-Expansion-an-ACA-Option.pdf. Accessed August 18, 2012.
2. Decker SL. In 2011 nearly one-third of physicians said they would not accept new Medicaid patients, but rising fees may help. Health Affairs. 2012;31(8):1673–1679.
3. Centers for Disease Control and Prevention. QuickStats: percentage of office-based physicians accepting new patients, by types of payment accepted—United States, 1999–2000 and 2008–2009. MMWR Morb Mortal Wkly Rep. 2011;60(27):928.
We want to hear from you! Tell us what you think.
Lay midwives and the ObGyn: Is collaboration risky?
“We have indeed in America medical practitioners not inferior to the best elsewhere; but there is probably no other country in the world in which there is so great a distance and so fatal a difference between the best, the average, and the worst.”
—Flexner report from 19101
ObGyn is a risky specialty, with no guarantee of a perfect outcome, even with the best education, training, and skills. Does collaboration make it riskier? Or can collaboration help you deliver high-quality care to your patients?
This article explores these questions as they relate to provision of health care in collaboration with midwives—specifically, certified nurse midwives (CNMs), who are approved by the American Midwifery Certification Board, and certified professional midwives (CPMs), who are not. (See thebox for a more detailed discussion of different types of midwives in practice today.)
Got acronym fatigue? Here’s a rundown of the various credentials and certifying organizations.
The American College of Nurse-Midwives (ACNM) is a professional organization established in 1955 for certified nurse midwives and certified midwives. ACNM sets standards for academic preparation and clinical practice. For more information, visit http://www.midwife.org.
The American Midwifery Certification Board (AMCB) is the certification organization affiliated with ACNM. This board was formerly called the ACNM Certification Council (ACC). Certification by AMCB is equivalent to certification by ACC.
In 1997, AMCB opened its national certification exam to non-nurse graduates of midwifery education programs and issued the first certified midwife credential. Since 2010, a graduate degree has been required for entry into clinical practice for both certified nurse midwives and certified midwives. http://www.amcbmidwife.org
Certified midwife (CM). In 1996, the ACNM adopted standards for the certification of direct-entry midwives. These midwives undergo the same certification process as certified nurse midwives, but their training does not include education in nursing. CMs must pass the same certification exam as CNMs and must have a master’s degree.
CMs are licensed in only three states: New Jersey, New York, and Rhode Island. New York had the first CM training program and was the first state to recognize the CM credential. It is the only state that has one unified framework for licensing all midwives—both CNMs and CMs.
Certified nurse midwife (CNM). A midwife who has training in both nursing and midwifery. A master’s degree is required for certification. These midwives typically have prescriptive authority for most drugs; are eligible for third-party reimbursement, including Medicaid; and practice independently or in collaborative practice with physicians.
Certified professional midwife (CPM). In the mid 1990s, the CPM credential was developed jointly by the Midwives Alliance of North America (MANA), the North American Registry of Midwives (NARM), and the Midwifery Education Accreditation Council (MEAC). There is no single standard for education; both apprentice-only–trained midwives and midwives who undergo university-affiliated training use the title CPM.
A CPM can learn through a structured program, through apprenticeship, or through self-study. Another route to the credential is current legal recognition to practice in the United Kingdom. CPMs must pass a written and practical exam for certification.
According to MANA, 24 states recognize the CPM credential as the basis for licensure or use the NARM written exam. Some of these states use a different nomenclature. For example, licensed midwife (LM) is used in California, Idaho, Oregon, and Washington; licensed direct-entry midwife (LDM) is used in Utah; and registered midwife (RM) is used in Colorado.
SOURCE: ACOG10
Moving away from a physician-oriented system
Like it or not, change is under way. Subtle but important shifts are taking place in the way maternity care is provided in your community.
The challenges facing our specialty? Ensuring that the highest levels of patient safety and quality care are maintained. And educating federal and state lawmakers, insurers, and the public accordingly.
Free-standing birth centers are gaining prominence
The Patient Protection and Affordable Care Act (ACA) establishes alternative pathways for maternity care. Congress, state lawmakers, and insurers want to know: Can access to quality maternity care be provided at lower cost outside of hospitals or by nonphysicians? The answer isn’t clear.
Under the ACA, free-standing birth centers are a Medicaid maternity-care choice for low-income women. Birth centers appeal to lawmakers and insurers because of their lower cost. For example, in 2008, the average facility cost for a vaginal delivery in a hospital, with no complications and no newborn charges, was $8,920. In 2010, the average facility cost for a similar delivery at a birth center was $2,277.2,3
We know that dollars alone don’t tell the full story—but they’re easy listening to lawmakers’ ears.
Since 2010, Medicaid payments are allowed to go to state-licensed, free-standing birth centers even if they are not operated by or under the supervision of a physician. Before the ACA became law, Medicaid paid only for services provided in ambulatory centers under the supervision or oversight of a physician.
Another important change: Medicaid now reimburses for the services of any provider who practices in a state-licensed, free-standing birth center as long as that provider is practicing within the state’s scope of practice laws and regulations. That means that if a state allows doulas or lay midwives to provide childbirth care in free-standing birth centers, the federal and state Medicaid programs will pay for this care. This policy is consistent with “any willing provider” rules found elsewhere in Medicaid.
There are 215 birth centers in the United States, with more in development. The number of birth centers has increased more than 20% over the past 5 years; they are regulated in 41 states.4
ACOG’s Guidelines for Perinatal Care asserts: “The hospital, including a birthing center within a hospital complex, or free-standing birthing centers that meet the standards of the Accreditation Association of Birth Centers, provide the safest setting for labor, delivery, and the postpartum period.”5
Reimbursements for nonphysicians are increasing
Beginning in 2011, the Medicare program began reimbursing CNMs, the most highly trained midwives, at 100% of the physician payment rate for obstetric services. Until 2011, CNMs were paid at 65% of the physician’s rate for the same billed services.
In addition, from 2011 through 2015, CNMs whose primary care services account for at least 60% of their Medicare-allowed charges will receive Medicare bonus payments of 10%, reflecting Congress’ concern that our nation faces a serious shortage of primary care providers.
Another important provision goes into effect in 2014: All health plans offered in a state insurance exchange must accept and pay any provider recognized under state law for services covered by that plan. CPMs, some of whom are among the least highly trained providers, are licensed to provide maternity care in 24 states. This provision may put pressure on health insurers to pay for maternity care provided by CPMs, regardless of their training and certification, even if the insurer doesn’t contract with these providers.
“Even a normal pregnancy can become high-risk”
In 2008, the Massachusetts legislature debated expanding childbirth care to encompass less highly trained providers. ACOG President Kenneth L. Noller, MD, MS, cautioned them about the move, saying: “Even a normal pregnancy can become high-risk with little or no warning, and serious, sometimes life-threatening complications may arise for the woman and her fetus.”
He noted that shoulder dystocia occurs in one in every 200 births and listed the frequency of other complications:
- prolapsed umbilical cord: 1 in every 200 births
- life-threatening maternal hemorrhage: 1 in 250
- eclamptic seizures: 1 in 500
- uterine inversion: 1 in 700
- Apgar score of 0–3 at 5 minutes: 1 in 100 to 200.
Three years later, ACOG President Richard A. Waldman, MD, and American College of Nurse Midwives (ACNM) President Holly Powell Kennedy, CNM, PhD, wrote: “Collaborative practice [is] the provision of health care by an interdisciplinary team of professionals who collaborate to accomplish a common goal, and is associated with increased efficiency, improved clinical outcomes, and enhanced provider satisfaction.”5
These messages demonstrate the importance of careful use of collaboration to manage risk and maintain the highest standards of patient care. The questions for ObGyns who are considering collaborative practice:
- What is careful use?
- How do you collaborate carefully, without increasing the risks faced by your patients and your practice?
- How do you make collaboration a success?
- ACOG has taken on these questions and offers sound practical advice.

ACOG recommends high standards and clear practice agreements
ObGyns have a long history of collaboration with our nurse-midwife colleagues—possibly one of the strongest collaborative traditions in medicine. ACOG supports the practice and licensure of trained midwives credentialed by the ACNM. CNMs are well-educated, highly trained, and well-integrated into the health-care system.
In addition to the ACNM standards, ACOG supports the “global standards for midwifery education” established by the International Confederation of Midwives (ICM) in 2010:
- The minimum entry level of students is completion of secondary education
- The minimum length of a direct-entry midwifery education program is 3 years
- The minimum length of a post-nursing/health-care provider program is 18 months
- Standards are congruent with current core ICM documents and position statements.
ACOG strongly encourages that in no case should the professional standards of any maternity provider be less than the standards established or accepted by ACOG or the ACNM.
Effective collaboration depends on clear practice agreements between physicians and CNMs, consistent use of shared practice guidelines, and malpractice insurance coverage of all parties. A collaborative agreement that clearly spells out the mechanism for consultation, collaboration, and referral is essential to assure the best care.
The picture gets a little trickier—and riskier—when we look at less-trained maternity providers.
A majority of CPMs lack adequate training
Few of the nation’s 1,400 CPMs in practice today meet the educational and training standards accepted by ACOG and the ACNM. The educational background of CPMs—known in some states as direct entry or lay midwives—varies widely across the nation. Unlike CNMs, CPMs are not required to have a nursing background. They practice primarily in out-of-hospital settings, including birthing centers and private homes. Many CPMs have no formal academic education or medical training, and their training requirements fall short of internationally established standards for midwives and traditional birth attendants.
Other relevant points:
- A person without a high school degree could be licensed as a CPM if he or she passed the certifying exam, observed 20 deliveries, and participated as the primary attendant in 10
- As a group, CPMs have not adopted home-birth patient-selection criteria that are based on generally accepted medical evidence or public safety
- The curriculum, clinical skills training, and experience of CPMs have not been approved by the American Midwifery Certification Board. Nor are they reviewed by the American Board of Obstetrics and Gynecology or the American Board of Family Medicine—recognized authorities in the certification of knowledge and skills associated with the practice of obstetrics.
- The North American Registry of Midwives’ Portfolio Evaluation Process requires midwives to be the primary care provider during 50 home births and to have 3 years’ experience. The average ObGyn resident gets this much experience in 1 month.
CPMs who lack a high school diploma and are apprentice-trained only (without core curriculum training and formal academic experience) clearly do not meet ACOG standards. Therefore, ACOG cautions its Fellows and the public that, for quality and safety reasons, it “does not support the provision of care by … midwives who are not certified by the American Midwifery Certification Board” [ACNM’s accreditation body]. Certification by this board, then, is a good indication of skill.
Requirements for successful collaborative practice
Where can you look for examples of collaboration that work, and for data on the effects of collaboration on health-care outcomes? Four articles in the September 2011 issue of Obstetrics and Gynecology highlight successful models of collaboration between ObGyns and CNMs in very different, well-established maternity programs.6-9 In each article, the authors describe their collaborative practice model in some detail, offering guidance to others interested in successful collaboration. Common threads run through these narratives:
- trust
- communication
- mutual respect
- administrative support for continuing medical education
- consensus meetings
- common adherence to accepted guidelines
- an established support network for back-up and transfer.
The benefits to ObGyns include greater job satisfaction. Benefits to patients include improved health outcomes, as demonstrated, for example, in a model from Washington State: a high rate of vaginal delivery, low rate of cesarean birth, high rate of successful vaginal birth after cesarean (VBAC), and low rate of repeat cesarean delivery.7
ACOG’s policy on collaborative practice finds its origins just over 100 years ago in the Flexner report, quoted at the beginning of this article, which emphasized the need to ensure that medical care in the United States is of no less quality than in other parts of the world.1
Medical education and quality of care have improved dramatically over the past century. ACOG is working to ensure the highest standards of care for pregnant women, standards no lower than for the rest of the population.
Collaboration is a time-honored tradition in ObGyn. Doing it right is key to patient safety.
- How state budget crises are putting the squeeze on Medicaid (and you)
(February 2012) - Is private ObGyn practice on its way out?
with Janelle Yates (October 2011) - 14 questions (and answers) about health reform and you
with Janelle Yates (August 2010)
Acknowledgment
The author acknowledges and thanks ACOG Executive Vice President Hal C. Lawrence III, MD, for his helpful review and comments
We want to hear from you! Tell us what you think.
1. Flexner A. Medical Education in the United States and Canada. A Report to the Carnegie Foundation for the Advancement of Teaching. Bulletin No. 4. 1910. Boston Mass: D. B. Updike, Merrymount Press; 1972.
2. American Association of Birth Centers Uniform Data Set. 2010 Data. Perkiomenville Pa: ASBC; 2011.
3. Facts and Figures 2008. Healthcare Cost and Utilization Project (HCUP). October 2010. Agency for Healthcare Research and Quality Rockville, MD. www.hcup-us.ahrq.gov/reports/factsandfigures/2008/TOC_2008.jsp. Accessed March 30, 2012.
4. American Association of Birth Centers. http://www.birthcenters.org.Accessed March 30, 2012.
5. Waldman RN, Kennedy HP. Collaborative practice between obstetricians and midwives. Obstet Gynecol. 2011;118(3):503-504.
6. Shaw-Battista J, Fineberg A, Boehler B, Skubic B, Woolley D, Tilton Z. Obstetrician and nurse-midwife collaboration: successful public health and private practice partnership. Obstet Gynecol. 2011;118(3):663-672.
7. Darlington A, McBroom K, Warwick S. A Northwest collaborative practice model. Obstet Gynecol. 2011;118(3):673-677.
8. Hutchison MS, Ennis L, Shaw-Battista J, et al. Great minds don’t think alike: collaborative maternity care at San Francisco General Hospital. Obstet Gynecol. 2011;118(3):678-682.
9. DeJoy S, Burkman RT, Graves BW, et al. Making it work: successful collaborative practice. Obstet Gynecol. 2011;118(3):683-686.
10. American Congress of Obstetricians and Gynecologists Glossary of Midwifery Organizations and Terms. Washington DC; 2010.
“We have indeed in America medical practitioners not inferior to the best elsewhere; but there is probably no other country in the world in which there is so great a distance and so fatal a difference between the best, the average, and the worst.”
—Flexner report from 19101
ObGyn is a risky specialty, with no guarantee of a perfect outcome, even with the best education, training, and skills. Does collaboration make it riskier? Or can collaboration help you deliver high-quality care to your patients?
This article explores these questions as they relate to provision of health care in collaboration with midwives—specifically, certified nurse midwives (CNMs), who are approved by the American Midwifery Certification Board, and certified professional midwives (CPMs), who are not. (See thebox for a more detailed discussion of different types of midwives in practice today.)
Got acronym fatigue? Here’s a rundown of the various credentials and certifying organizations.
The American College of Nurse-Midwives (ACNM) is a professional organization established in 1955 for certified nurse midwives and certified midwives. ACNM sets standards for academic preparation and clinical practice. For more information, visit http://www.midwife.org.
The American Midwifery Certification Board (AMCB) is the certification organization affiliated with ACNM. This board was formerly called the ACNM Certification Council (ACC). Certification by AMCB is equivalent to certification by ACC.
In 1997, AMCB opened its national certification exam to non-nurse graduates of midwifery education programs and issued the first certified midwife credential. Since 2010, a graduate degree has been required for entry into clinical practice for both certified nurse midwives and certified midwives. http://www.amcbmidwife.org
Certified midwife (CM). In 1996, the ACNM adopted standards for the certification of direct-entry midwives. These midwives undergo the same certification process as certified nurse midwives, but their training does not include education in nursing. CMs must pass the same certification exam as CNMs and must have a master’s degree.
CMs are licensed in only three states: New Jersey, New York, and Rhode Island. New York had the first CM training program and was the first state to recognize the CM credential. It is the only state that has one unified framework for licensing all midwives—both CNMs and CMs.
Certified nurse midwife (CNM). A midwife who has training in both nursing and midwifery. A master’s degree is required for certification. These midwives typically have prescriptive authority for most drugs; are eligible for third-party reimbursement, including Medicaid; and practice independently or in collaborative practice with physicians.
Certified professional midwife (CPM). In the mid 1990s, the CPM credential was developed jointly by the Midwives Alliance of North America (MANA), the North American Registry of Midwives (NARM), and the Midwifery Education Accreditation Council (MEAC). There is no single standard for education; both apprentice-only–trained midwives and midwives who undergo university-affiliated training use the title CPM.
A CPM can learn through a structured program, through apprenticeship, or through self-study. Another route to the credential is current legal recognition to practice in the United Kingdom. CPMs must pass a written and practical exam for certification.
According to MANA, 24 states recognize the CPM credential as the basis for licensure or use the NARM written exam. Some of these states use a different nomenclature. For example, licensed midwife (LM) is used in California, Idaho, Oregon, and Washington; licensed direct-entry midwife (LDM) is used in Utah; and registered midwife (RM) is used in Colorado.
SOURCE: ACOG10
Moving away from a physician-oriented system
Like it or not, change is under way. Subtle but important shifts are taking place in the way maternity care is provided in your community.
The challenges facing our specialty? Ensuring that the highest levels of patient safety and quality care are maintained. And educating federal and state lawmakers, insurers, and the public accordingly.
Free-standing birth centers are gaining prominence
The Patient Protection and Affordable Care Act (ACA) establishes alternative pathways for maternity care. Congress, state lawmakers, and insurers want to know: Can access to quality maternity care be provided at lower cost outside of hospitals or by nonphysicians? The answer isn’t clear.
Under the ACA, free-standing birth centers are a Medicaid maternity-care choice for low-income women. Birth centers appeal to lawmakers and insurers because of their lower cost. For example, in 2008, the average facility cost for a vaginal delivery in a hospital, with no complications and no newborn charges, was $8,920. In 2010, the average facility cost for a similar delivery at a birth center was $2,277.2,3
We know that dollars alone don’t tell the full story—but they’re easy listening to lawmakers’ ears.
Since 2010, Medicaid payments are allowed to go to state-licensed, free-standing birth centers even if they are not operated by or under the supervision of a physician. Before the ACA became law, Medicaid paid only for services provided in ambulatory centers under the supervision or oversight of a physician.
Another important change: Medicaid now reimburses for the services of any provider who practices in a state-licensed, free-standing birth center as long as that provider is practicing within the state’s scope of practice laws and regulations. That means that if a state allows doulas or lay midwives to provide childbirth care in free-standing birth centers, the federal and state Medicaid programs will pay for this care. This policy is consistent with “any willing provider” rules found elsewhere in Medicaid.
There are 215 birth centers in the United States, with more in development. The number of birth centers has increased more than 20% over the past 5 years; they are regulated in 41 states.4
ACOG’s Guidelines for Perinatal Care asserts: “The hospital, including a birthing center within a hospital complex, or free-standing birthing centers that meet the standards of the Accreditation Association of Birth Centers, provide the safest setting for labor, delivery, and the postpartum period.”5
Reimbursements for nonphysicians are increasing
Beginning in 2011, the Medicare program began reimbursing CNMs, the most highly trained midwives, at 100% of the physician payment rate for obstetric services. Until 2011, CNMs were paid at 65% of the physician’s rate for the same billed services.
In addition, from 2011 through 2015, CNMs whose primary care services account for at least 60% of their Medicare-allowed charges will receive Medicare bonus payments of 10%, reflecting Congress’ concern that our nation faces a serious shortage of primary care providers.
Another important provision goes into effect in 2014: All health plans offered in a state insurance exchange must accept and pay any provider recognized under state law for services covered by that plan. CPMs, some of whom are among the least highly trained providers, are licensed to provide maternity care in 24 states. This provision may put pressure on health insurers to pay for maternity care provided by CPMs, regardless of their training and certification, even if the insurer doesn’t contract with these providers.
“Even a normal pregnancy can become high-risk”
In 2008, the Massachusetts legislature debated expanding childbirth care to encompass less highly trained providers. ACOG President Kenneth L. Noller, MD, MS, cautioned them about the move, saying: “Even a normal pregnancy can become high-risk with little or no warning, and serious, sometimes life-threatening complications may arise for the woman and her fetus.”
He noted that shoulder dystocia occurs in one in every 200 births and listed the frequency of other complications:
- prolapsed umbilical cord: 1 in every 200 births
- life-threatening maternal hemorrhage: 1 in 250
- eclamptic seizures: 1 in 500
- uterine inversion: 1 in 700
- Apgar score of 0–3 at 5 minutes: 1 in 100 to 200.
Three years later, ACOG President Richard A. Waldman, MD, and American College of Nurse Midwives (ACNM) President Holly Powell Kennedy, CNM, PhD, wrote: “Collaborative practice [is] the provision of health care by an interdisciplinary team of professionals who collaborate to accomplish a common goal, and is associated with increased efficiency, improved clinical outcomes, and enhanced provider satisfaction.”5
These messages demonstrate the importance of careful use of collaboration to manage risk and maintain the highest standards of patient care. The questions for ObGyns who are considering collaborative practice:
- What is careful use?
- How do you collaborate carefully, without increasing the risks faced by your patients and your practice?
- How do you make collaboration a success?
- ACOG has taken on these questions and offers sound practical advice.

ACOG recommends high standards and clear practice agreements
ObGyns have a long history of collaboration with our nurse-midwife colleagues—possibly one of the strongest collaborative traditions in medicine. ACOG supports the practice and licensure of trained midwives credentialed by the ACNM. CNMs are well-educated, highly trained, and well-integrated into the health-care system.
In addition to the ACNM standards, ACOG supports the “global standards for midwifery education” established by the International Confederation of Midwives (ICM) in 2010:
- The minimum entry level of students is completion of secondary education
- The minimum length of a direct-entry midwifery education program is 3 years
- The minimum length of a post-nursing/health-care provider program is 18 months
- Standards are congruent with current core ICM documents and position statements.
ACOG strongly encourages that in no case should the professional standards of any maternity provider be less than the standards established or accepted by ACOG or the ACNM.
Effective collaboration depends on clear practice agreements between physicians and CNMs, consistent use of shared practice guidelines, and malpractice insurance coverage of all parties. A collaborative agreement that clearly spells out the mechanism for consultation, collaboration, and referral is essential to assure the best care.
The picture gets a little trickier—and riskier—when we look at less-trained maternity providers.
A majority of CPMs lack adequate training
Few of the nation’s 1,400 CPMs in practice today meet the educational and training standards accepted by ACOG and the ACNM. The educational background of CPMs—known in some states as direct entry or lay midwives—varies widely across the nation. Unlike CNMs, CPMs are not required to have a nursing background. They practice primarily in out-of-hospital settings, including birthing centers and private homes. Many CPMs have no formal academic education or medical training, and their training requirements fall short of internationally established standards for midwives and traditional birth attendants.
Other relevant points:
- A person without a high school degree could be licensed as a CPM if he or she passed the certifying exam, observed 20 deliveries, and participated as the primary attendant in 10
- As a group, CPMs have not adopted home-birth patient-selection criteria that are based on generally accepted medical evidence or public safety
- The curriculum, clinical skills training, and experience of CPMs have not been approved by the American Midwifery Certification Board. Nor are they reviewed by the American Board of Obstetrics and Gynecology or the American Board of Family Medicine—recognized authorities in the certification of knowledge and skills associated with the practice of obstetrics.
- The North American Registry of Midwives’ Portfolio Evaluation Process requires midwives to be the primary care provider during 50 home births and to have 3 years’ experience. The average ObGyn resident gets this much experience in 1 month.
CPMs who lack a high school diploma and are apprentice-trained only (without core curriculum training and formal academic experience) clearly do not meet ACOG standards. Therefore, ACOG cautions its Fellows and the public that, for quality and safety reasons, it “does not support the provision of care by … midwives who are not certified by the American Midwifery Certification Board” [ACNM’s accreditation body]. Certification by this board, then, is a good indication of skill.
Requirements for successful collaborative practice
Where can you look for examples of collaboration that work, and for data on the effects of collaboration on health-care outcomes? Four articles in the September 2011 issue of Obstetrics and Gynecology highlight successful models of collaboration between ObGyns and CNMs in very different, well-established maternity programs.6-9 In each article, the authors describe their collaborative practice model in some detail, offering guidance to others interested in successful collaboration. Common threads run through these narratives:
- trust
- communication
- mutual respect
- administrative support for continuing medical education
- consensus meetings
- common adherence to accepted guidelines
- an established support network for back-up and transfer.
The benefits to ObGyns include greater job satisfaction. Benefits to patients include improved health outcomes, as demonstrated, for example, in a model from Washington State: a high rate of vaginal delivery, low rate of cesarean birth, high rate of successful vaginal birth after cesarean (VBAC), and low rate of repeat cesarean delivery.7
ACOG’s policy on collaborative practice finds its origins just over 100 years ago in the Flexner report, quoted at the beginning of this article, which emphasized the need to ensure that medical care in the United States is of no less quality than in other parts of the world.1
Medical education and quality of care have improved dramatically over the past century. ACOG is working to ensure the highest standards of care for pregnant women, standards no lower than for the rest of the population.
Collaboration is a time-honored tradition in ObGyn. Doing it right is key to patient safety.
- How state budget crises are putting the squeeze on Medicaid (and you)
(February 2012) - Is private ObGyn practice on its way out?
with Janelle Yates (October 2011) - 14 questions (and answers) about health reform and you
with Janelle Yates (August 2010)
Acknowledgment
The author acknowledges and thanks ACOG Executive Vice President Hal C. Lawrence III, MD, for his helpful review and comments
We want to hear from you! Tell us what you think.
“We have indeed in America medical practitioners not inferior to the best elsewhere; but there is probably no other country in the world in which there is so great a distance and so fatal a difference between the best, the average, and the worst.”
—Flexner report from 19101
ObGyn is a risky specialty, with no guarantee of a perfect outcome, even with the best education, training, and skills. Does collaboration make it riskier? Or can collaboration help you deliver high-quality care to your patients?
This article explores these questions as they relate to provision of health care in collaboration with midwives—specifically, certified nurse midwives (CNMs), who are approved by the American Midwifery Certification Board, and certified professional midwives (CPMs), who are not. (See thebox for a more detailed discussion of different types of midwives in practice today.)
Got acronym fatigue? Here’s a rundown of the various credentials and certifying organizations.
The American College of Nurse-Midwives (ACNM) is a professional organization established in 1955 for certified nurse midwives and certified midwives. ACNM sets standards for academic preparation and clinical practice. For more information, visit http://www.midwife.org.
The American Midwifery Certification Board (AMCB) is the certification organization affiliated with ACNM. This board was formerly called the ACNM Certification Council (ACC). Certification by AMCB is equivalent to certification by ACC.
In 1997, AMCB opened its national certification exam to non-nurse graduates of midwifery education programs and issued the first certified midwife credential. Since 2010, a graduate degree has been required for entry into clinical practice for both certified nurse midwives and certified midwives. http://www.amcbmidwife.org
Certified midwife (CM). In 1996, the ACNM adopted standards for the certification of direct-entry midwives. These midwives undergo the same certification process as certified nurse midwives, but their training does not include education in nursing. CMs must pass the same certification exam as CNMs and must have a master’s degree.
CMs are licensed in only three states: New Jersey, New York, and Rhode Island. New York had the first CM training program and was the first state to recognize the CM credential. It is the only state that has one unified framework for licensing all midwives—both CNMs and CMs.
Certified nurse midwife (CNM). A midwife who has training in both nursing and midwifery. A master’s degree is required for certification. These midwives typically have prescriptive authority for most drugs; are eligible for third-party reimbursement, including Medicaid; and practice independently or in collaborative practice with physicians.
Certified professional midwife (CPM). In the mid 1990s, the CPM credential was developed jointly by the Midwives Alliance of North America (MANA), the North American Registry of Midwives (NARM), and the Midwifery Education Accreditation Council (MEAC). There is no single standard for education; both apprentice-only–trained midwives and midwives who undergo university-affiliated training use the title CPM.
A CPM can learn through a structured program, through apprenticeship, or through self-study. Another route to the credential is current legal recognition to practice in the United Kingdom. CPMs must pass a written and practical exam for certification.
According to MANA, 24 states recognize the CPM credential as the basis for licensure or use the NARM written exam. Some of these states use a different nomenclature. For example, licensed midwife (LM) is used in California, Idaho, Oregon, and Washington; licensed direct-entry midwife (LDM) is used in Utah; and registered midwife (RM) is used in Colorado.
SOURCE: ACOG10
Moving away from a physician-oriented system
Like it or not, change is under way. Subtle but important shifts are taking place in the way maternity care is provided in your community.
The challenges facing our specialty? Ensuring that the highest levels of patient safety and quality care are maintained. And educating federal and state lawmakers, insurers, and the public accordingly.
Free-standing birth centers are gaining prominence
The Patient Protection and Affordable Care Act (ACA) establishes alternative pathways for maternity care. Congress, state lawmakers, and insurers want to know: Can access to quality maternity care be provided at lower cost outside of hospitals or by nonphysicians? The answer isn’t clear.
Under the ACA, free-standing birth centers are a Medicaid maternity-care choice for low-income women. Birth centers appeal to lawmakers and insurers because of their lower cost. For example, in 2008, the average facility cost for a vaginal delivery in a hospital, with no complications and no newborn charges, was $8,920. In 2010, the average facility cost for a similar delivery at a birth center was $2,277.2,3
We know that dollars alone don’t tell the full story—but they’re easy listening to lawmakers’ ears.
Since 2010, Medicaid payments are allowed to go to state-licensed, free-standing birth centers even if they are not operated by or under the supervision of a physician. Before the ACA became law, Medicaid paid only for services provided in ambulatory centers under the supervision or oversight of a physician.
Another important change: Medicaid now reimburses for the services of any provider who practices in a state-licensed, free-standing birth center as long as that provider is practicing within the state’s scope of practice laws and regulations. That means that if a state allows doulas or lay midwives to provide childbirth care in free-standing birth centers, the federal and state Medicaid programs will pay for this care. This policy is consistent with “any willing provider” rules found elsewhere in Medicaid.
There are 215 birth centers in the United States, with more in development. The number of birth centers has increased more than 20% over the past 5 years; they are regulated in 41 states.4
ACOG’s Guidelines for Perinatal Care asserts: “The hospital, including a birthing center within a hospital complex, or free-standing birthing centers that meet the standards of the Accreditation Association of Birth Centers, provide the safest setting for labor, delivery, and the postpartum period.”5
Reimbursements for nonphysicians are increasing
Beginning in 2011, the Medicare program began reimbursing CNMs, the most highly trained midwives, at 100% of the physician payment rate for obstetric services. Until 2011, CNMs were paid at 65% of the physician’s rate for the same billed services.
In addition, from 2011 through 2015, CNMs whose primary care services account for at least 60% of their Medicare-allowed charges will receive Medicare bonus payments of 10%, reflecting Congress’ concern that our nation faces a serious shortage of primary care providers.
Another important provision goes into effect in 2014: All health plans offered in a state insurance exchange must accept and pay any provider recognized under state law for services covered by that plan. CPMs, some of whom are among the least highly trained providers, are licensed to provide maternity care in 24 states. This provision may put pressure on health insurers to pay for maternity care provided by CPMs, regardless of their training and certification, even if the insurer doesn’t contract with these providers.
“Even a normal pregnancy can become high-risk”
In 2008, the Massachusetts legislature debated expanding childbirth care to encompass less highly trained providers. ACOG President Kenneth L. Noller, MD, MS, cautioned them about the move, saying: “Even a normal pregnancy can become high-risk with little or no warning, and serious, sometimes life-threatening complications may arise for the woman and her fetus.”
He noted that shoulder dystocia occurs in one in every 200 births and listed the frequency of other complications:
- prolapsed umbilical cord: 1 in every 200 births
- life-threatening maternal hemorrhage: 1 in 250
- eclamptic seizures: 1 in 500
- uterine inversion: 1 in 700
- Apgar score of 0–3 at 5 minutes: 1 in 100 to 200.
Three years later, ACOG President Richard A. Waldman, MD, and American College of Nurse Midwives (ACNM) President Holly Powell Kennedy, CNM, PhD, wrote: “Collaborative practice [is] the provision of health care by an interdisciplinary team of professionals who collaborate to accomplish a common goal, and is associated with increased efficiency, improved clinical outcomes, and enhanced provider satisfaction.”5
These messages demonstrate the importance of careful use of collaboration to manage risk and maintain the highest standards of patient care. The questions for ObGyns who are considering collaborative practice:
- What is careful use?
- How do you collaborate carefully, without increasing the risks faced by your patients and your practice?
- How do you make collaboration a success?
- ACOG has taken on these questions and offers sound practical advice.

ACOG recommends high standards and clear practice agreements
ObGyns have a long history of collaboration with our nurse-midwife colleagues—possibly one of the strongest collaborative traditions in medicine. ACOG supports the practice and licensure of trained midwives credentialed by the ACNM. CNMs are well-educated, highly trained, and well-integrated into the health-care system.
In addition to the ACNM standards, ACOG supports the “global standards for midwifery education” established by the International Confederation of Midwives (ICM) in 2010:
- The minimum entry level of students is completion of secondary education
- The minimum length of a direct-entry midwifery education program is 3 years
- The minimum length of a post-nursing/health-care provider program is 18 months
- Standards are congruent with current core ICM documents and position statements.
ACOG strongly encourages that in no case should the professional standards of any maternity provider be less than the standards established or accepted by ACOG or the ACNM.
Effective collaboration depends on clear practice agreements between physicians and CNMs, consistent use of shared practice guidelines, and malpractice insurance coverage of all parties. A collaborative agreement that clearly spells out the mechanism for consultation, collaboration, and referral is essential to assure the best care.
The picture gets a little trickier—and riskier—when we look at less-trained maternity providers.
A majority of CPMs lack adequate training
Few of the nation’s 1,400 CPMs in practice today meet the educational and training standards accepted by ACOG and the ACNM. The educational background of CPMs—known in some states as direct entry or lay midwives—varies widely across the nation. Unlike CNMs, CPMs are not required to have a nursing background. They practice primarily in out-of-hospital settings, including birthing centers and private homes. Many CPMs have no formal academic education or medical training, and their training requirements fall short of internationally established standards for midwives and traditional birth attendants.
Other relevant points:
- A person without a high school degree could be licensed as a CPM if he or she passed the certifying exam, observed 20 deliveries, and participated as the primary attendant in 10
- As a group, CPMs have not adopted home-birth patient-selection criteria that are based on generally accepted medical evidence or public safety
- The curriculum, clinical skills training, and experience of CPMs have not been approved by the American Midwifery Certification Board. Nor are they reviewed by the American Board of Obstetrics and Gynecology or the American Board of Family Medicine—recognized authorities in the certification of knowledge and skills associated with the practice of obstetrics.
- The North American Registry of Midwives’ Portfolio Evaluation Process requires midwives to be the primary care provider during 50 home births and to have 3 years’ experience. The average ObGyn resident gets this much experience in 1 month.
CPMs who lack a high school diploma and are apprentice-trained only (without core curriculum training and formal academic experience) clearly do not meet ACOG standards. Therefore, ACOG cautions its Fellows and the public that, for quality and safety reasons, it “does not support the provision of care by … midwives who are not certified by the American Midwifery Certification Board” [ACNM’s accreditation body]. Certification by this board, then, is a good indication of skill.
Requirements for successful collaborative practice
Where can you look for examples of collaboration that work, and for data on the effects of collaboration on health-care outcomes? Four articles in the September 2011 issue of Obstetrics and Gynecology highlight successful models of collaboration between ObGyns and CNMs in very different, well-established maternity programs.6-9 In each article, the authors describe their collaborative practice model in some detail, offering guidance to others interested in successful collaboration. Common threads run through these narratives:
- trust
- communication
- mutual respect
- administrative support for continuing medical education
- consensus meetings
- common adherence to accepted guidelines
- an established support network for back-up and transfer.
The benefits to ObGyns include greater job satisfaction. Benefits to patients include improved health outcomes, as demonstrated, for example, in a model from Washington State: a high rate of vaginal delivery, low rate of cesarean birth, high rate of successful vaginal birth after cesarean (VBAC), and low rate of repeat cesarean delivery.7
ACOG’s policy on collaborative practice finds its origins just over 100 years ago in the Flexner report, quoted at the beginning of this article, which emphasized the need to ensure that medical care in the United States is of no less quality than in other parts of the world.1
Medical education and quality of care have improved dramatically over the past century. ACOG is working to ensure the highest standards of care for pregnant women, standards no lower than for the rest of the population.
Collaboration is a time-honored tradition in ObGyn. Doing it right is key to patient safety.
- How state budget crises are putting the squeeze on Medicaid (and you)
(February 2012) - Is private ObGyn practice on its way out?
with Janelle Yates (October 2011) - 14 questions (and answers) about health reform and you
with Janelle Yates (August 2010)
Acknowledgment
The author acknowledges and thanks ACOG Executive Vice President Hal C. Lawrence III, MD, for his helpful review and comments
We want to hear from you! Tell us what you think.
1. Flexner A. Medical Education in the United States and Canada. A Report to the Carnegie Foundation for the Advancement of Teaching. Bulletin No. 4. 1910. Boston Mass: D. B. Updike, Merrymount Press; 1972.
2. American Association of Birth Centers Uniform Data Set. 2010 Data. Perkiomenville Pa: ASBC; 2011.
3. Facts and Figures 2008. Healthcare Cost and Utilization Project (HCUP). October 2010. Agency for Healthcare Research and Quality Rockville, MD. www.hcup-us.ahrq.gov/reports/factsandfigures/2008/TOC_2008.jsp. Accessed March 30, 2012.
4. American Association of Birth Centers. http://www.birthcenters.org.Accessed March 30, 2012.
5. Waldman RN, Kennedy HP. Collaborative practice between obstetricians and midwives. Obstet Gynecol. 2011;118(3):503-504.
6. Shaw-Battista J, Fineberg A, Boehler B, Skubic B, Woolley D, Tilton Z. Obstetrician and nurse-midwife collaboration: successful public health and private practice partnership. Obstet Gynecol. 2011;118(3):663-672.
7. Darlington A, McBroom K, Warwick S. A Northwest collaborative practice model. Obstet Gynecol. 2011;118(3):673-677.
8. Hutchison MS, Ennis L, Shaw-Battista J, et al. Great minds don’t think alike: collaborative maternity care at San Francisco General Hospital. Obstet Gynecol. 2011;118(3):678-682.
9. DeJoy S, Burkman RT, Graves BW, et al. Making it work: successful collaborative practice. Obstet Gynecol. 2011;118(3):683-686.
10. American Congress of Obstetricians and Gynecologists Glossary of Midwifery Organizations and Terms. Washington DC; 2010.
1. Flexner A. Medical Education in the United States and Canada. A Report to the Carnegie Foundation for the Advancement of Teaching. Bulletin No. 4. 1910. Boston Mass: D. B. Updike, Merrymount Press; 1972.
2. American Association of Birth Centers Uniform Data Set. 2010 Data. Perkiomenville Pa: ASBC; 2011.
3. Facts and Figures 2008. Healthcare Cost and Utilization Project (HCUP). October 2010. Agency for Healthcare Research and Quality Rockville, MD. www.hcup-us.ahrq.gov/reports/factsandfigures/2008/TOC_2008.jsp. Accessed March 30, 2012.
4. American Association of Birth Centers. http://www.birthcenters.org.Accessed March 30, 2012.
5. Waldman RN, Kennedy HP. Collaborative practice between obstetricians and midwives. Obstet Gynecol. 2011;118(3):503-504.
6. Shaw-Battista J, Fineberg A, Boehler B, Skubic B, Woolley D, Tilton Z. Obstetrician and nurse-midwife collaboration: successful public health and private practice partnership. Obstet Gynecol. 2011;118(3):663-672.
7. Darlington A, McBroom K, Warwick S. A Northwest collaborative practice model. Obstet Gynecol. 2011;118(3):673-677.
8. Hutchison MS, Ennis L, Shaw-Battista J, et al. Great minds don’t think alike: collaborative maternity care at San Francisco General Hospital. Obstet Gynecol. 2011;118(3):678-682.
9. DeJoy S, Burkman RT, Graves BW, et al. Making it work: successful collaborative practice. Obstet Gynecol. 2011;118(3):683-686.
10. American Congress of Obstetricians and Gynecologists Glossary of Midwifery Organizations and Terms. Washington DC; 2010.




