User login
The well-woman visit comes of age: What it offers, how we got here
When the Affordable Care Act (ACA) was passed in 2010, it represented an intended shift from reactive medicine, with its focus on acute and urgent needs, to a model focused on disease prevention.
OBG Management readers know about the important women’s health services ensured by the ACA, including well-woman care, as well as the key role played by the American Congress of Obstetricians and Gynecologists (ACOG) in winning this coverage. ACOG worked closely with the Institute of Medicine (IOM) to help define this set of services. And the ACA ensured that women have access to these services, often without copays and deductibles.
ACOG and the National Women’s Law Center (NWLC) work closely on many issues. At first independently and then together, the 2 organizations set out to explore some fundamental issues:
- How does a woman experience the new well-woman benefit when she visits her doctor?
- Does she receive a consistent care set?
- Do some patients have copays while patients in other clinics do not for the same services?
- What does well-woman care mean from one doctor to another, from an ObGyn to an internist to a family physician?
This article explores these issues.
2 initiatives focused on components of women’s health care
During her tenure as president of ACOG, Jeanne Conry, MD, PhD, decided to tackle clinical issues associated with well-woman care. She convened a Well-Woman Task Force, led by Haywood Brown, MD, and included the NWLC among other partner organizations (TABLE).
Table. Partipating organizations of the ACOG Well-Woman Task Force
• American Academy of Family Physicians
• American Academy of Pediatrics
• American Academy of Physician Assistants
• American College of Nurse–Midwives
• American College of Osteopathic Obstetricians and Gynecologists
• Association of Reproductive Health Professionals
• Association of Women’s Health, Obstetric, and Neonatal Nurses
• National Association of Nurse Practitioners in Women’s Health
• National Medical Association
• National Women’s Law Center
• Planned Parenthood Federation of America
• Society for Maternal-Fetal Medicine
• Society of Academic Specialists in General Obstetrics and Gynecology
• Society of Gynecologic Oncology
The NWLC and Brigham and Women’s Hospital also partnered with ACOG and others to help ensure a consistent patient experience. These 2 closely related initiatives were designed to work together to help patients and physicians understand and benefit from new coverage under the ACA.
1. How does a woman experience well-woman care?
Experts associated with these 2 initiatives recognized that well-woman care includes attention to the history, physical examination, counseling, and screening intended to maintain physical, mental, and social wellbeing and general health throughout a woman’s lifespan. Experts also recognized that the ACA guarantees coverage of at least one annual well-woman visit, although not all of the recommended components necessarily would be performed at the same visit or by the same provider.
For many women who have gained insurance coverage under the ACA, the well-woman visit represents their entry into the insured health care system. These women may have limited understanding of the services they should receive during this visit.
To address this issue, the NWLC invited ACOG to participate in its initiative with Brigham and Women’s Hospital to understand the well-woman visit from the patient’s point of view. This effort yielded patient education materials in English and Spanish that help women understand:
- that their health insurance now covers a well-woman visit
- what care is included in that visit
- that there is no deductible or copay for this visit
- how to prepare for this visit
- what questions to ask during the visit.
These materials help women understand that the purpose of the well-woman visit is to provide them with a chance to:
- “receive care and counseling that is appropriate, based on age, cognitive development, and life experience
- review their current health and risks to their health with their health care professional
- ask any questions they may have about their health or risk factors
- talk about what they can do to prevent future health problems
- build a trusting relationship with their health care provider, with an emphasis on confidentiality
- receive appropriate preventive screenings and immunizations and make sure they know which screenings and immunizations they should receive in the future
- review their reproductive plan and contraceptive choices.”1
The materials also advise patients that they may be asked about:
- current health concerns
- current medications, both prescription and over the counter
- family history on both the mother’s and father’s sides
- life management, including family relationships, work, and stress
- substance use habits, including alcohol and tobacco
- sexual activity
- eating habits and physical activity
- past reproductive health experience and any pregnancy complications
- any memory problems (older women)
- screening for depression, anxiety, substance use disorders, and interpersonal violence.
To view some of these materials, visit http://www.nwlc.org/sites/default/files/final_well-womanbrochure.pdf.
2. Does each woman receive consistent well-woman care?
ACOG’s Well-Woman Task Force was shaped by an awareness that many medical societies and government agencies provide recommendations and guidelines about the basic elements of women’s health. While these recommendations and guidelines all may be based on evidence and expert opinion, the recommendations vary. A goal of the task force was to work with providers across the women’s health spectrum to find consensus and provide guidance to women and clinicians with age-appropriate recommendations for a well-woman visit.
In the fall of 2015, the task force’s findings were published in an article entitled “Components of the well-woman visit” in the journal Obstetrics & Gynecology.2 Those findings outline a core set of well-woman care practices across a woman’s lifespan, from adolescence through the reproductive years and into maturity, and they are usable by any provider who cares for adolescent girls or women.
ACOG has summarized its well-woman recommendations, by age, on its website,3 at http://www.acog.org/About-ACOG/ACOG-Departments/Annual-Womens-Health-Care/Well-Woman-Recommendations.
3. Do all women have a copay for the well-woman visit?
Because research has revealed that any type of copay or deductible for preventive care significantly lessens the likelihood that patients will seek out such care, the ACA sought to make basic preventive care available without cost sharing.4
The US Department of Health and Human Services notes that: “The Affordable Care Act requires most health plans to cover recommended preventive services without cost sharing. In 2011 and 2012, 71 million Americans with private health insurance gained access to preventive services with no cost sharing because of the law.”4
Grandfathered plans (those created or sold before March 23, 2010) are exempt from this requirement, as are Medicare, TRICARE, and traditional Medicaid plans.
4. What does well-woman care mean from one doctor to another?
Under the ACA, well-woman care can be provided by a “wide range of providers, including family physicians, internists, nurse–midwives, nurse practitioners, obstetrician-gynecologists, pediatricians, and physician assistants,” depending on the age of the patient, her particular needs and preferences, and access to health services.2
The ACOG Well-Woman Task Force “focused on delineating the well-woman visit throughout the lifespan, across all providers and health plans.”2
In determining the components of well-woman care, ACOG’s task force compiled existing guidelines from many sources, including the Department of Health and Human Services, the IOM, the US Preventive Services Task Force, and each member organization.
Members categorized guidelines as:
- single source (eg, abdominal examination)
- no agreement (breast cancer/mammography screening)
- limited agreement (pelvic examination)
- general agreement (hypertension, osteoporosis)
- sound agreement (screening for sexually transmitted infections)
The task force also agreed that final recommendations would rely on evidence-based guidelines, evidence-informed guidelines, and uniform expert agreement. Recommendations were considered “strong” if they relied primarily on evidence-based or evidence-informed guidelines and “qualified” if they relied primarily on expert consensus.
Guidelines were further separated into age bands:
- adolescents (13–18 years)
- reproductive-aged women (19–45 years)
- mature women (46–64 years)
- women older than 64 years.
The task force recommended that, during the well-woman visit, health care professionals educate patients about:
- healthy eating habits and maintenance of healthy weight
- exercise and physical activity
- seat belt use
- risk factors for certain types of cancer
- heart health
- breast health
- bone health
- safer sex practices and prevention of sexually transmitted infections
- healthy interpersonal relationships
- prevention and management of chronic disease
- resources for the patient (online, written, community, patient groups)
- medication use
- fall prevention.
Health care providers also should counsel patients regarding:
- recommended preventive screenings and immunizations
- any concerns about mood, such as prolonged periods of sadness, a failure to enjoy what they usually find pleasant, or anxiety or irritability that seems out of proportion to events
- what to expect in terms of effects on mood and anxiety at reproductive life transitions, including menarche, pregnancy, the postpartum period, and perimenopause
- body image issues
- what to expect in terms of the menstrual cycle during perimenopause and menopause
- reproductive health or fertility concerns
- reproductive life planning (contraception appropriate for life stage, reproductive plans, and risk factors, including risk factors for breast and ovarian cancer and cardiovascular disease)
- pregnancy planning, including attaining and maintaining a healthy weight and managing any chronic conditions before or during pregnancy
- what to expect during menopause, including signs and symptoms and options for addressing symptoms (midlife and older women)
- symptoms of cardiovascular disease
- urinary incontinence.
The task force acknowledged that not all of these recommendations can be carried out at a single well-woman visit or by a single provider.
See, again, ACOG’s specific well-woman recommendations, by age range, at http://www.acog.org/About-ACOG/ACOG-Departments/Annual-Womens-Health-Care/Well-Woman-Recommendations.3
How to winnow a long list of recommendations to determine the most pressing issues for a specific patient
In an editorial accompanying the ACOG Well-Woman Task Force report, entitled “Re-envisioning the annual well-woman visit: the task forward,” George F. Sawaya, MD, of the University of California, San Francisco, devised a plan to determine the most pressing well-woman needs for a specific patient.1 He chose as an example a 41-year-old sexually active woman who does not smoke.
While Dr. Sawaya praised the Well-Woman Task Force recommendations for their “comprehensive scope,” he also noted that the sheer number of recommendations might be “overwhelming and difficult to navigate.”1 One tool for winnowing the recommendations comes from the Agency for Healthcare Research and Quality, which offers an Electronic Preventive Services Selector (http://epss.ahrq.gov/PDA/index.jsp), available both online and as a smartphone app. Once the clinician plugs in the patient’s age and a few risk factors, the tool generates a list of recommended preventive services. This list of services has been evaluated by the US Preventive Services Task Force, with each recommendation graded “A” through “D,” based on benefits versus harms.
Back to that 41-year-old sexually active woman: Using the Electronic Preventive Services Selector, a list of as many as 20 grade A and B recommendations would be generated. However, only 3 of them would be grade A (screening for cervical cancer, HIV, and high blood pressure). An additional 2 grade B recommendations might apply to an average-risk patient such as this: screening for alcohol misuse and depression. All 5 services fall within the Well-Woman Task Force’s recommendations. They also have “good face validity with clinicians as being important, so it seems reasonable that these be prioritized above the others, at least at the first visit,” Dr. Sawaya says.1
Clinicians can use a similar strategy for patients of various ages and risk factors.
Reference
1. Sawaya GF. Re-envisioning the annual well-woman visit: the task forward [editorial]. Obstet Gynecol. 2015;126(4):695–696.
The bottom line
By defining and implementing the foundational elements of women’s health, we can improve care for all women and ensure, as Dr. Conry emphasized during her tenure as ACOG president, “that every woman gets the care she needs, every time.”
Share your thoughts! Send your Letter to the Editor to [email protected]. Please include your name and the city and state in which you practice.
- National Women’s Law Center, Brigham and Women’s Hospital. Your Guide to Well-Woman Visits. http://www.nwlc.org/sites/default/files/final_well-womanbrochure.pdf. Accessed December 8, 2015.
- Conry JA, Brown H. Well-Woman Task Force: Components of the well-woman visit. Obstet Gynecol. 2015;126(4):697–701.
- American College of Obstetricians and Gynecologists. Well-Woman Recommendations. http://www.acog.org/About-ACOG/ACOG-Departments/Annual-Womens-Health-Care/Well-Woman-Recommendations. Accessed December 4, 2015.
- US Department of Health and Human Services. Affordable Care Act Rules on Expanding Access to Preventive Services for Women. http://www.hhs.gov/healthcare/facts-and-features/fact-sheets/aca-rules-on-expanding-access-to-preventive-services-for-women/index.html. Updated June 28, 2013. Accessed December 4, 2015.
When the Affordable Care Act (ACA) was passed in 2010, it represented an intended shift from reactive medicine, with its focus on acute and urgent needs, to a model focused on disease prevention.
OBG Management readers know about the important women’s health services ensured by the ACA, including well-woman care, as well as the key role played by the American Congress of Obstetricians and Gynecologists (ACOG) in winning this coverage. ACOG worked closely with the Institute of Medicine (IOM) to help define this set of services. And the ACA ensured that women have access to these services, often without copays and deductibles.
ACOG and the National Women’s Law Center (NWLC) work closely on many issues. At first independently and then together, the 2 organizations set out to explore some fundamental issues:
- How does a woman experience the new well-woman benefit when she visits her doctor?
- Does she receive a consistent care set?
- Do some patients have copays while patients in other clinics do not for the same services?
- What does well-woman care mean from one doctor to another, from an ObGyn to an internist to a family physician?
This article explores these issues.
2 initiatives focused on components of women’s health care
During her tenure as president of ACOG, Jeanne Conry, MD, PhD, decided to tackle clinical issues associated with well-woman care. She convened a Well-Woman Task Force, led by Haywood Brown, MD, and included the NWLC among other partner organizations (TABLE).
Table. Partipating organizations of the ACOG Well-Woman Task Force
• American Academy of Family Physicians
• American Academy of Pediatrics
• American Academy of Physician Assistants
• American College of Nurse–Midwives
• American College of Osteopathic Obstetricians and Gynecologists
• Association of Reproductive Health Professionals
• Association of Women’s Health, Obstetric, and Neonatal Nurses
• National Association of Nurse Practitioners in Women’s Health
• National Medical Association
• National Women’s Law Center
• Planned Parenthood Federation of America
• Society for Maternal-Fetal Medicine
• Society of Academic Specialists in General Obstetrics and Gynecology
• Society of Gynecologic Oncology
The NWLC and Brigham and Women’s Hospital also partnered with ACOG and others to help ensure a consistent patient experience. These 2 closely related initiatives were designed to work together to help patients and physicians understand and benefit from new coverage under the ACA.
1. How does a woman experience well-woman care?
Experts associated with these 2 initiatives recognized that well-woman care includes attention to the history, physical examination, counseling, and screening intended to maintain physical, mental, and social wellbeing and general health throughout a woman’s lifespan. Experts also recognized that the ACA guarantees coverage of at least one annual well-woman visit, although not all of the recommended components necessarily would be performed at the same visit or by the same provider.
For many women who have gained insurance coverage under the ACA, the well-woman visit represents their entry into the insured health care system. These women may have limited understanding of the services they should receive during this visit.
To address this issue, the NWLC invited ACOG to participate in its initiative with Brigham and Women’s Hospital to understand the well-woman visit from the patient’s point of view. This effort yielded patient education materials in English and Spanish that help women understand:
- that their health insurance now covers a well-woman visit
- what care is included in that visit
- that there is no deductible or copay for this visit
- how to prepare for this visit
- what questions to ask during the visit.
These materials help women understand that the purpose of the well-woman visit is to provide them with a chance to:
- “receive care and counseling that is appropriate, based on age, cognitive development, and life experience
- review their current health and risks to their health with their health care professional
- ask any questions they may have about their health or risk factors
- talk about what they can do to prevent future health problems
- build a trusting relationship with their health care provider, with an emphasis on confidentiality
- receive appropriate preventive screenings and immunizations and make sure they know which screenings and immunizations they should receive in the future
- review their reproductive plan and contraceptive choices.”1
The materials also advise patients that they may be asked about:
- current health concerns
- current medications, both prescription and over the counter
- family history on both the mother’s and father’s sides
- life management, including family relationships, work, and stress
- substance use habits, including alcohol and tobacco
- sexual activity
- eating habits and physical activity
- past reproductive health experience and any pregnancy complications
- any memory problems (older women)
- screening for depression, anxiety, substance use disorders, and interpersonal violence.
To view some of these materials, visit http://www.nwlc.org/sites/default/files/final_well-womanbrochure.pdf.
2. Does each woman receive consistent well-woman care?
ACOG’s Well-Woman Task Force was shaped by an awareness that many medical societies and government agencies provide recommendations and guidelines about the basic elements of women’s health. While these recommendations and guidelines all may be based on evidence and expert opinion, the recommendations vary. A goal of the task force was to work with providers across the women’s health spectrum to find consensus and provide guidance to women and clinicians with age-appropriate recommendations for a well-woman visit.
In the fall of 2015, the task force’s findings were published in an article entitled “Components of the well-woman visit” in the journal Obstetrics & Gynecology.2 Those findings outline a core set of well-woman care practices across a woman’s lifespan, from adolescence through the reproductive years and into maturity, and they are usable by any provider who cares for adolescent girls or women.
ACOG has summarized its well-woman recommendations, by age, on its website,3 at http://www.acog.org/About-ACOG/ACOG-Departments/Annual-Womens-Health-Care/Well-Woman-Recommendations.
3. Do all women have a copay for the well-woman visit?
Because research has revealed that any type of copay or deductible for preventive care significantly lessens the likelihood that patients will seek out such care, the ACA sought to make basic preventive care available without cost sharing.4
The US Department of Health and Human Services notes that: “The Affordable Care Act requires most health plans to cover recommended preventive services without cost sharing. In 2011 and 2012, 71 million Americans with private health insurance gained access to preventive services with no cost sharing because of the law.”4
Grandfathered plans (those created or sold before March 23, 2010) are exempt from this requirement, as are Medicare, TRICARE, and traditional Medicaid plans.
4. What does well-woman care mean from one doctor to another?
Under the ACA, well-woman care can be provided by a “wide range of providers, including family physicians, internists, nurse–midwives, nurse practitioners, obstetrician-gynecologists, pediatricians, and physician assistants,” depending on the age of the patient, her particular needs and preferences, and access to health services.2
The ACOG Well-Woman Task Force “focused on delineating the well-woman visit throughout the lifespan, across all providers and health plans.”2
In determining the components of well-woman care, ACOG’s task force compiled existing guidelines from many sources, including the Department of Health and Human Services, the IOM, the US Preventive Services Task Force, and each member organization.
Members categorized guidelines as:
- single source (eg, abdominal examination)
- no agreement (breast cancer/mammography screening)
- limited agreement (pelvic examination)
- general agreement (hypertension, osteoporosis)
- sound agreement (screening for sexually transmitted infections)
The task force also agreed that final recommendations would rely on evidence-based guidelines, evidence-informed guidelines, and uniform expert agreement. Recommendations were considered “strong” if they relied primarily on evidence-based or evidence-informed guidelines and “qualified” if they relied primarily on expert consensus.
Guidelines were further separated into age bands:
- adolescents (13–18 years)
- reproductive-aged women (19–45 years)
- mature women (46–64 years)
- women older than 64 years.
The task force recommended that, during the well-woman visit, health care professionals educate patients about:
- healthy eating habits and maintenance of healthy weight
- exercise and physical activity
- seat belt use
- risk factors for certain types of cancer
- heart health
- breast health
- bone health
- safer sex practices and prevention of sexually transmitted infections
- healthy interpersonal relationships
- prevention and management of chronic disease
- resources for the patient (online, written, community, patient groups)
- medication use
- fall prevention.
Health care providers also should counsel patients regarding:
- recommended preventive screenings and immunizations
- any concerns about mood, such as prolonged periods of sadness, a failure to enjoy what they usually find pleasant, or anxiety or irritability that seems out of proportion to events
- what to expect in terms of effects on mood and anxiety at reproductive life transitions, including menarche, pregnancy, the postpartum period, and perimenopause
- body image issues
- what to expect in terms of the menstrual cycle during perimenopause and menopause
- reproductive health or fertility concerns
- reproductive life planning (contraception appropriate for life stage, reproductive plans, and risk factors, including risk factors for breast and ovarian cancer and cardiovascular disease)
- pregnancy planning, including attaining and maintaining a healthy weight and managing any chronic conditions before or during pregnancy
- what to expect during menopause, including signs and symptoms and options for addressing symptoms (midlife and older women)
- symptoms of cardiovascular disease
- urinary incontinence.
The task force acknowledged that not all of these recommendations can be carried out at a single well-woman visit or by a single provider.
See, again, ACOG’s specific well-woman recommendations, by age range, at http://www.acog.org/About-ACOG/ACOG-Departments/Annual-Womens-Health-Care/Well-Woman-Recommendations.3
How to winnow a long list of recommendations to determine the most pressing issues for a specific patient
In an editorial accompanying the ACOG Well-Woman Task Force report, entitled “Re-envisioning the annual well-woman visit: the task forward,” George F. Sawaya, MD, of the University of California, San Francisco, devised a plan to determine the most pressing well-woman needs for a specific patient.1 He chose as an example a 41-year-old sexually active woman who does not smoke.
While Dr. Sawaya praised the Well-Woman Task Force recommendations for their “comprehensive scope,” he also noted that the sheer number of recommendations might be “overwhelming and difficult to navigate.”1 One tool for winnowing the recommendations comes from the Agency for Healthcare Research and Quality, which offers an Electronic Preventive Services Selector (http://epss.ahrq.gov/PDA/index.jsp), available both online and as a smartphone app. Once the clinician plugs in the patient’s age and a few risk factors, the tool generates a list of recommended preventive services. This list of services has been evaluated by the US Preventive Services Task Force, with each recommendation graded “A” through “D,” based on benefits versus harms.
Back to that 41-year-old sexually active woman: Using the Electronic Preventive Services Selector, a list of as many as 20 grade A and B recommendations would be generated. However, only 3 of them would be grade A (screening for cervical cancer, HIV, and high blood pressure). An additional 2 grade B recommendations might apply to an average-risk patient such as this: screening for alcohol misuse and depression. All 5 services fall within the Well-Woman Task Force’s recommendations. They also have “good face validity with clinicians as being important, so it seems reasonable that these be prioritized above the others, at least at the first visit,” Dr. Sawaya says.1
Clinicians can use a similar strategy for patients of various ages and risk factors.
Reference
1. Sawaya GF. Re-envisioning the annual well-woman visit: the task forward [editorial]. Obstet Gynecol. 2015;126(4):695–696.
The bottom line
By defining and implementing the foundational elements of women’s health, we can improve care for all women and ensure, as Dr. Conry emphasized during her tenure as ACOG president, “that every woman gets the care she needs, every time.”
Share your thoughts! Send your Letter to the Editor to [email protected]. Please include your name and the city and state in which you practice.
When the Affordable Care Act (ACA) was passed in 2010, it represented an intended shift from reactive medicine, with its focus on acute and urgent needs, to a model focused on disease prevention.
OBG Management readers know about the important women’s health services ensured by the ACA, including well-woman care, as well as the key role played by the American Congress of Obstetricians and Gynecologists (ACOG) in winning this coverage. ACOG worked closely with the Institute of Medicine (IOM) to help define this set of services. And the ACA ensured that women have access to these services, often without copays and deductibles.
ACOG and the National Women’s Law Center (NWLC) work closely on many issues. At first independently and then together, the 2 organizations set out to explore some fundamental issues:
- How does a woman experience the new well-woman benefit when she visits her doctor?
- Does she receive a consistent care set?
- Do some patients have copays while patients in other clinics do not for the same services?
- What does well-woman care mean from one doctor to another, from an ObGyn to an internist to a family physician?
This article explores these issues.
2 initiatives focused on components of women’s health care
During her tenure as president of ACOG, Jeanne Conry, MD, PhD, decided to tackle clinical issues associated with well-woman care. She convened a Well-Woman Task Force, led by Haywood Brown, MD, and included the NWLC among other partner organizations (TABLE).
Table. Partipating organizations of the ACOG Well-Woman Task Force
• American Academy of Family Physicians
• American Academy of Pediatrics
• American Academy of Physician Assistants
• American College of Nurse–Midwives
• American College of Osteopathic Obstetricians and Gynecologists
• Association of Reproductive Health Professionals
• Association of Women’s Health, Obstetric, and Neonatal Nurses
• National Association of Nurse Practitioners in Women’s Health
• National Medical Association
• National Women’s Law Center
• Planned Parenthood Federation of America
• Society for Maternal-Fetal Medicine
• Society of Academic Specialists in General Obstetrics and Gynecology
• Society of Gynecologic Oncology
The NWLC and Brigham and Women’s Hospital also partnered with ACOG and others to help ensure a consistent patient experience. These 2 closely related initiatives were designed to work together to help patients and physicians understand and benefit from new coverage under the ACA.
1. How does a woman experience well-woman care?
Experts associated with these 2 initiatives recognized that well-woman care includes attention to the history, physical examination, counseling, and screening intended to maintain physical, mental, and social wellbeing and general health throughout a woman’s lifespan. Experts also recognized that the ACA guarantees coverage of at least one annual well-woman visit, although not all of the recommended components necessarily would be performed at the same visit or by the same provider.
For many women who have gained insurance coverage under the ACA, the well-woman visit represents their entry into the insured health care system. These women may have limited understanding of the services they should receive during this visit.
To address this issue, the NWLC invited ACOG to participate in its initiative with Brigham and Women’s Hospital to understand the well-woman visit from the patient’s point of view. This effort yielded patient education materials in English and Spanish that help women understand:
- that their health insurance now covers a well-woman visit
- what care is included in that visit
- that there is no deductible or copay for this visit
- how to prepare for this visit
- what questions to ask during the visit.
These materials help women understand that the purpose of the well-woman visit is to provide them with a chance to:
- “receive care and counseling that is appropriate, based on age, cognitive development, and life experience
- review their current health and risks to their health with their health care professional
- ask any questions they may have about their health or risk factors
- talk about what they can do to prevent future health problems
- build a trusting relationship with their health care provider, with an emphasis on confidentiality
- receive appropriate preventive screenings and immunizations and make sure they know which screenings and immunizations they should receive in the future
- review their reproductive plan and contraceptive choices.”1
The materials also advise patients that they may be asked about:
- current health concerns
- current medications, both prescription and over the counter
- family history on both the mother’s and father’s sides
- life management, including family relationships, work, and stress
- substance use habits, including alcohol and tobacco
- sexual activity
- eating habits and physical activity
- past reproductive health experience and any pregnancy complications
- any memory problems (older women)
- screening for depression, anxiety, substance use disorders, and interpersonal violence.
To view some of these materials, visit http://www.nwlc.org/sites/default/files/final_well-womanbrochure.pdf.
2. Does each woman receive consistent well-woman care?
ACOG’s Well-Woman Task Force was shaped by an awareness that many medical societies and government agencies provide recommendations and guidelines about the basic elements of women’s health. While these recommendations and guidelines all may be based on evidence and expert opinion, the recommendations vary. A goal of the task force was to work with providers across the women’s health spectrum to find consensus and provide guidance to women and clinicians with age-appropriate recommendations for a well-woman visit.
In the fall of 2015, the task force’s findings were published in an article entitled “Components of the well-woman visit” in the journal Obstetrics & Gynecology.2 Those findings outline a core set of well-woman care practices across a woman’s lifespan, from adolescence through the reproductive years and into maturity, and they are usable by any provider who cares for adolescent girls or women.
ACOG has summarized its well-woman recommendations, by age, on its website,3 at http://www.acog.org/About-ACOG/ACOG-Departments/Annual-Womens-Health-Care/Well-Woman-Recommendations.
3. Do all women have a copay for the well-woman visit?
Because research has revealed that any type of copay or deductible for preventive care significantly lessens the likelihood that patients will seek out such care, the ACA sought to make basic preventive care available without cost sharing.4
The US Department of Health and Human Services notes that: “The Affordable Care Act requires most health plans to cover recommended preventive services without cost sharing. In 2011 and 2012, 71 million Americans with private health insurance gained access to preventive services with no cost sharing because of the law.”4
Grandfathered plans (those created or sold before March 23, 2010) are exempt from this requirement, as are Medicare, TRICARE, and traditional Medicaid plans.
4. What does well-woman care mean from one doctor to another?
Under the ACA, well-woman care can be provided by a “wide range of providers, including family physicians, internists, nurse–midwives, nurse practitioners, obstetrician-gynecologists, pediatricians, and physician assistants,” depending on the age of the patient, her particular needs and preferences, and access to health services.2
The ACOG Well-Woman Task Force “focused on delineating the well-woman visit throughout the lifespan, across all providers and health plans.”2
In determining the components of well-woman care, ACOG’s task force compiled existing guidelines from many sources, including the Department of Health and Human Services, the IOM, the US Preventive Services Task Force, and each member organization.
Members categorized guidelines as:
- single source (eg, abdominal examination)
- no agreement (breast cancer/mammography screening)
- limited agreement (pelvic examination)
- general agreement (hypertension, osteoporosis)
- sound agreement (screening for sexually transmitted infections)
The task force also agreed that final recommendations would rely on evidence-based guidelines, evidence-informed guidelines, and uniform expert agreement. Recommendations were considered “strong” if they relied primarily on evidence-based or evidence-informed guidelines and “qualified” if they relied primarily on expert consensus.
Guidelines were further separated into age bands:
- adolescents (13–18 years)
- reproductive-aged women (19–45 years)
- mature women (46–64 years)
- women older than 64 years.
The task force recommended that, during the well-woman visit, health care professionals educate patients about:
- healthy eating habits and maintenance of healthy weight
- exercise and physical activity
- seat belt use
- risk factors for certain types of cancer
- heart health
- breast health
- bone health
- safer sex practices and prevention of sexually transmitted infections
- healthy interpersonal relationships
- prevention and management of chronic disease
- resources for the patient (online, written, community, patient groups)
- medication use
- fall prevention.
Health care providers also should counsel patients regarding:
- recommended preventive screenings and immunizations
- any concerns about mood, such as prolonged periods of sadness, a failure to enjoy what they usually find pleasant, or anxiety or irritability that seems out of proportion to events
- what to expect in terms of effects on mood and anxiety at reproductive life transitions, including menarche, pregnancy, the postpartum period, and perimenopause
- body image issues
- what to expect in terms of the menstrual cycle during perimenopause and menopause
- reproductive health or fertility concerns
- reproductive life planning (contraception appropriate for life stage, reproductive plans, and risk factors, including risk factors for breast and ovarian cancer and cardiovascular disease)
- pregnancy planning, including attaining and maintaining a healthy weight and managing any chronic conditions before or during pregnancy
- what to expect during menopause, including signs and symptoms and options for addressing symptoms (midlife and older women)
- symptoms of cardiovascular disease
- urinary incontinence.
The task force acknowledged that not all of these recommendations can be carried out at a single well-woman visit or by a single provider.
See, again, ACOG’s specific well-woman recommendations, by age range, at http://www.acog.org/About-ACOG/ACOG-Departments/Annual-Womens-Health-Care/Well-Woman-Recommendations.3
How to winnow a long list of recommendations to determine the most pressing issues for a specific patient
In an editorial accompanying the ACOG Well-Woman Task Force report, entitled “Re-envisioning the annual well-woman visit: the task forward,” George F. Sawaya, MD, of the University of California, San Francisco, devised a plan to determine the most pressing well-woman needs for a specific patient.1 He chose as an example a 41-year-old sexually active woman who does not smoke.
While Dr. Sawaya praised the Well-Woman Task Force recommendations for their “comprehensive scope,” he also noted that the sheer number of recommendations might be “overwhelming and difficult to navigate.”1 One tool for winnowing the recommendations comes from the Agency for Healthcare Research and Quality, which offers an Electronic Preventive Services Selector (http://epss.ahrq.gov/PDA/index.jsp), available both online and as a smartphone app. Once the clinician plugs in the patient’s age and a few risk factors, the tool generates a list of recommended preventive services. This list of services has been evaluated by the US Preventive Services Task Force, with each recommendation graded “A” through “D,” based on benefits versus harms.
Back to that 41-year-old sexually active woman: Using the Electronic Preventive Services Selector, a list of as many as 20 grade A and B recommendations would be generated. However, only 3 of them would be grade A (screening for cervical cancer, HIV, and high blood pressure). An additional 2 grade B recommendations might apply to an average-risk patient such as this: screening for alcohol misuse and depression. All 5 services fall within the Well-Woman Task Force’s recommendations. They also have “good face validity with clinicians as being important, so it seems reasonable that these be prioritized above the others, at least at the first visit,” Dr. Sawaya says.1
Clinicians can use a similar strategy for patients of various ages and risk factors.
Reference
1. Sawaya GF. Re-envisioning the annual well-woman visit: the task forward [editorial]. Obstet Gynecol. 2015;126(4):695–696.
The bottom line
By defining and implementing the foundational elements of women’s health, we can improve care for all women and ensure, as Dr. Conry emphasized during her tenure as ACOG president, “that every woman gets the care she needs, every time.”
Share your thoughts! Send your Letter to the Editor to [email protected]. Please include your name and the city and state in which you practice.
- National Women’s Law Center, Brigham and Women’s Hospital. Your Guide to Well-Woman Visits. http://www.nwlc.org/sites/default/files/final_well-womanbrochure.pdf. Accessed December 8, 2015.
- Conry JA, Brown H. Well-Woman Task Force: Components of the well-woman visit. Obstet Gynecol. 2015;126(4):697–701.
- American College of Obstetricians and Gynecologists. Well-Woman Recommendations. http://www.acog.org/About-ACOG/ACOG-Departments/Annual-Womens-Health-Care/Well-Woman-Recommendations. Accessed December 4, 2015.
- US Department of Health and Human Services. Affordable Care Act Rules on Expanding Access to Preventive Services for Women. http://www.hhs.gov/healthcare/facts-and-features/fact-sheets/aca-rules-on-expanding-access-to-preventive-services-for-women/index.html. Updated June 28, 2013. Accessed December 4, 2015.
- National Women’s Law Center, Brigham and Women’s Hospital. Your Guide to Well-Woman Visits. http://www.nwlc.org/sites/default/files/final_well-womanbrochure.pdf. Accessed December 8, 2015.
- Conry JA, Brown H. Well-Woman Task Force: Components of the well-woman visit. Obstet Gynecol. 2015;126(4):697–701.
- American College of Obstetricians and Gynecologists. Well-Woman Recommendations. http://www.acog.org/About-ACOG/ACOG-Departments/Annual-Womens-Health-Care/Well-Woman-Recommendations. Accessed December 4, 2015.
- US Department of Health and Human Services. Affordable Care Act Rules on Expanding Access to Preventive Services for Women. http://www.hhs.gov/healthcare/facts-and-features/fact-sheets/aca-rules-on-expanding-access-to-preventive-services-for-women/index.html. Updated June 28, 2013. Accessed December 4, 2015.
ACOG plans consensus conference on uniform guidelines for breast cancer screening
The Susan G. Komen Foundation estimates that 84% of breast cancers are found through mammography.1 Clearly, the value of mammography is proven. But controversy and confusion abound on how much mammography, and beginning at what age, is best for women.
Currently, the United States Preventive Services Task Force (USPSTF), the American Cancer Society (ACS), and the American College of Obstetricians and Gynecologists (ACOG) all have differing recommendations about mammography and about the importance of clinical breast examinations. These inconsistencies largely are due to different interpretations of the same data, not the data itself, and tend to center on how harm is defined and measured. Importantly, these differences can wreak havoc on our patients’ confidence in our counsel and decision making, and can complicate women’s access to screening. Under the Affordable Care Act, women are guaranteed coverage of annual mammograms, but new USPSTF recommendations, due out soon, may undermine that guarantee.
On October 20, ACOG responded to the ACS’ new recommendations on breast cancer screening by emphasizing our continued advice that women should begin annual mammography screening at age 40, along with a clinical breast exam.2
Consensus conference plansIn an effort to address widespread confusion among patients, health care professionals, and payers, ACOG is convening a consensus conference in January 2016, with the goal of arriving at a consistent set of guidelines that can be agreed to, implemented clinically across the country, and hopefully adopted by insurers, as well. Major organizations and providers of women’s health care, including ACS, will gather to evaluate and interpret the data in greater detail and to consider the available data in the broader context of patient care.
Without doubt, guidelines and recommendations will need to evolve as new evidence emerges, but our hope is that scientific and medical organizations can look at the same evidence and speak with one voice on what is best for women’s health. Our patients would benefit from that alone.
ACOG’s recommendations, summarized
- Clinical breast examination every year for women aged 19 and older.
- Screening mammography every year for women aged 40 and older.
- Breast self-awareness has the potential to detect palpable breast cancer and can be recommended.2
Share your thoughts! Send your Letter to the Editor to [email protected]. Please include your name and the city and state in which you practice.
- Susan G. Komen Web site. Accuracy of mammograms. http://ww5.komen.org/BreastCancer/AccuracyofMammograms.html. Updated June 26, 2015. Accessed October 30, 2015.
- ACOG Statement on Revised American Cancer Society Recommendations on Breast Cancer Screening. American College of Obstetricians and Gynecologists Web site. http://www.acog.org/About-ACOG/News-Room/Statements/2015/ACOG-Statement-on-Recommendations-on-Breast-Cancer-Screening. Published October 20, 2015. Accessed October 30, 2015.
The Susan G. Komen Foundation estimates that 84% of breast cancers are found through mammography.1 Clearly, the value of mammography is proven. But controversy and confusion abound on how much mammography, and beginning at what age, is best for women.
Currently, the United States Preventive Services Task Force (USPSTF), the American Cancer Society (ACS), and the American College of Obstetricians and Gynecologists (ACOG) all have differing recommendations about mammography and about the importance of clinical breast examinations. These inconsistencies largely are due to different interpretations of the same data, not the data itself, and tend to center on how harm is defined and measured. Importantly, these differences can wreak havoc on our patients’ confidence in our counsel and decision making, and can complicate women’s access to screening. Under the Affordable Care Act, women are guaranteed coverage of annual mammograms, but new USPSTF recommendations, due out soon, may undermine that guarantee.
On October 20, ACOG responded to the ACS’ new recommendations on breast cancer screening by emphasizing our continued advice that women should begin annual mammography screening at age 40, along with a clinical breast exam.2
Consensus conference plansIn an effort to address widespread confusion among patients, health care professionals, and payers, ACOG is convening a consensus conference in January 2016, with the goal of arriving at a consistent set of guidelines that can be agreed to, implemented clinically across the country, and hopefully adopted by insurers, as well. Major organizations and providers of women’s health care, including ACS, will gather to evaluate and interpret the data in greater detail and to consider the available data in the broader context of patient care.
Without doubt, guidelines and recommendations will need to evolve as new evidence emerges, but our hope is that scientific and medical organizations can look at the same evidence and speak with one voice on what is best for women’s health. Our patients would benefit from that alone.
ACOG’s recommendations, summarized
- Clinical breast examination every year for women aged 19 and older.
- Screening mammography every year for women aged 40 and older.
- Breast self-awareness has the potential to detect palpable breast cancer and can be recommended.2
Share your thoughts! Send your Letter to the Editor to [email protected]. Please include your name and the city and state in which you practice.
The Susan G. Komen Foundation estimates that 84% of breast cancers are found through mammography.1 Clearly, the value of mammography is proven. But controversy and confusion abound on how much mammography, and beginning at what age, is best for women.
Currently, the United States Preventive Services Task Force (USPSTF), the American Cancer Society (ACS), and the American College of Obstetricians and Gynecologists (ACOG) all have differing recommendations about mammography and about the importance of clinical breast examinations. These inconsistencies largely are due to different interpretations of the same data, not the data itself, and tend to center on how harm is defined and measured. Importantly, these differences can wreak havoc on our patients’ confidence in our counsel and decision making, and can complicate women’s access to screening. Under the Affordable Care Act, women are guaranteed coverage of annual mammograms, but new USPSTF recommendations, due out soon, may undermine that guarantee.
On October 20, ACOG responded to the ACS’ new recommendations on breast cancer screening by emphasizing our continued advice that women should begin annual mammography screening at age 40, along with a clinical breast exam.2
Consensus conference plansIn an effort to address widespread confusion among patients, health care professionals, and payers, ACOG is convening a consensus conference in January 2016, with the goal of arriving at a consistent set of guidelines that can be agreed to, implemented clinically across the country, and hopefully adopted by insurers, as well. Major organizations and providers of women’s health care, including ACS, will gather to evaluate and interpret the data in greater detail and to consider the available data in the broader context of patient care.
Without doubt, guidelines and recommendations will need to evolve as new evidence emerges, but our hope is that scientific and medical organizations can look at the same evidence and speak with one voice on what is best for women’s health. Our patients would benefit from that alone.
ACOG’s recommendations, summarized
- Clinical breast examination every year for women aged 19 and older.
- Screening mammography every year for women aged 40 and older.
- Breast self-awareness has the potential to detect palpable breast cancer and can be recommended.2
Share your thoughts! Send your Letter to the Editor to [email protected]. Please include your name and the city and state in which you practice.
- Susan G. Komen Web site. Accuracy of mammograms. http://ww5.komen.org/BreastCancer/AccuracyofMammograms.html. Updated June 26, 2015. Accessed October 30, 2015.
- ACOG Statement on Revised American Cancer Society Recommendations on Breast Cancer Screening. American College of Obstetricians and Gynecologists Web site. http://www.acog.org/About-ACOG/News-Room/Statements/2015/ACOG-Statement-on-Recommendations-on-Breast-Cancer-Screening. Published October 20, 2015. Accessed October 30, 2015.
- Susan G. Komen Web site. Accuracy of mammograms. http://ww5.komen.org/BreastCancer/AccuracyofMammograms.html. Updated June 26, 2015. Accessed October 30, 2015.
- ACOG Statement on Revised American Cancer Society Recommendations on Breast Cancer Screening. American College of Obstetricians and Gynecologists Web site. http://www.acog.org/About-ACOG/News-Room/Statements/2015/ACOG-Statement-on-Recommendations-on-Breast-Cancer-Screening. Published October 20, 2015. Accessed October 30, 2015.
What the Supreme Court ruling in King v. Burwell means for women’s health
In a widely anticipated judgment on the Affordable Care Act (ACA), the US Supreme Court ruled 6-3 in favor of the law on June 26, 2015. The case at hand, King v. Burwell, challenged whether individuals purchasing health insurance through federal exchanges were eligible for federal premium subsidies. This ruling cemented the ACA into law and avoided a potential calamity in the private health insurance market. Let’s take a closer look.
What the case was about
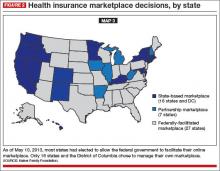
The ACA allows states to set up their own health insurance exchanges or participate in a federally run exchange. Although the drafters of the ACA had expected each state to set up its own exchange, two-thirds of the states declined to do so, many in opposition to the ACA. As a result, 7 million citizens in 34 states now purchase their health insurance through federally created exchanges.
The plaintiffs in King v. Burwell argued that, because the legislation refers to those enrolled “through an Exchange established by the State,” individuals in states with federally run exchanges are not eligible for subsidies.
The law states:
(A) the monthly premiums for such month for 1 or more qualified health plans offered in the individual market within a State which cover the taxpayer, the taxpayer’s spouse, or any dependent (as defined in section 152) of the taxpayer and which were enrolled in through an Exchange established by the State under 1311 of the Patient Protection and Affordable Care Act…[emphasis added].
The Supreme Court was asked to decide whether to adhere to those exact words or to honor Congress’ intent to allow individuals to purchase subsidized insurance on any type of exchange.
What might have happened
We’ve explored in previous articles the interconnectedness of many sections of the ACA. Nowhere is that interconnectedness more clearly demonstrated than here. In order to ensure that private health insurers provide better coverage, the law requires them to abide by important consumer protections, including the elimination of “preexisting condition” exclusions. In order to prevent adverse selection and keep insurers solvent under these new rules, all individuals are required to have health care coverage—the individual mandate. If everyone is required to purchase health insurance, it has to be affordable, so lower-income individuals were promised subsidies, paid for 100% by the federal government, to help them cover their premiums when insurance is purchased through an exchange. Take away the subsidies and the whole thing starts to unravel.
The Urban Institute estimated that a Supreme Court ruling in favor of King, which would have eliminated the subsidies in states using a federal exchange, would have reduced federal tax subsidies by $29 billion in 2016, making coverage unaffordable for many and increasing the ranks of the uninsured by 8.2 million people.1
Louise Sheiner and Brendan Mochoruk of the Brookings Institute speculated that healthy individuals would disproportionately leave the marketplace, triggering 35% increases in insurance premiums for those remaining, as well as significant increases in premiums for those who just lost their subsidies.2 Many observers, including these experts, forecast that insurance companies would exit the federal exchanges altogether, triggering a health insurance “death spiral”: As premiums rise, the healthiest customers leave the marketplace, causing premiums to rise more, causing more healthy people to leave, and so on.
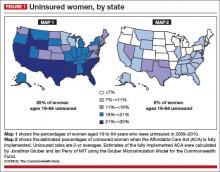
Clearly, this Supreme Court decision has had dramatic, long-term, real-world effects on millions of Americans. On the national level, 6,387,789 individuals were at risk of losing their tax credits if the Supreme Court had ruled in favor of King. That number represents more than $1.7 billion in total monthly tax credits. For a look at how a judgment in favor of King would have affected subsidies on a state-by-state basis, see TABLE 1.
What other commentators are saying about the King v. Burwell decision
In his majority opinion, Chief Justice John Roberts noted that the “meaning of the phrase ‘established by the State’ is not so clear.” And as Amy Howe articulated on SCOTUSblog: “if the phrase…is in fact not clear…then the next step is to look at the Affordable Care Act more broadly to determine what Congress meant by the phrase. And when you do that, the Court reasoned, it becomes apparent that Congress actually intended for the subsidies to be available to everyone who buys health insurance on an exchange, no matter who created it. If the subsidies weren’t available in the states with federal exchanges, the Court explained, the insurance markets in those states simply wouldn’t work properly: without the subsidies, almost all of the people who purchased insurance on the exchanges would no longer be required to purchase insurance because it would be too expensive. This would create a ‘death spiral’….”
—Amy Howe, SCOTUSblog3
“Additional court challenges to other ACA provisions are still possible, but King’s six-member majority shows little appetite for challenges threatening the Act’s core structure. Even Scalia’s dissent recognizes that the ACA may one day ‘attain the enduring status of the Social Security Act.’ Thus, the decision may usher in a new era of policy maturity, in which efforts to undermine the ACA diminish, as focus shifts to efforts to implement and improve it.”
—Mark A. Hall, JD, New England Journal of Medicine4
“With the Court upholding the administration’s interpretation of the law, the Obama administration has little reason to accede to
Republican proposals. The Court’s decision effectively puts the future of the ACA on hold until the 2016 elections, when the people will decide whether to stay the course or to chart a very different path.”
—Timothy Jost, Health Affairs5
“A case that 6 months ago seemed to offer the Court’s conservatives a low-risk opportunity to accomplish what they almost did in 2012—kill the Affordable Care Act—became suffused with danger, for the millions of newly insured Americans, of course, but also for the Supreme Court itself. Ideology came face to face with reality, and reality prevailed.”
—Linda Greenhouse, New York Times6
How premium subsidies work
Premium subsidies are actually tax credits. Individuals and families can qualify for them to purchase any type of health insurance offered on an exchange, except catastrophic coverage. To receive the premium tax credit for coverage starting in 2015, a marketplace enrollee must:
- have a household income that is 1 to4 times the federal poverty level. In 2015, the range of incomes that qualify for subsidies is $11,670 for an individual and $23,850 for a family of 4 at 100% of the federal poverty level. At 400% of the federal poverty level, it is $46,680 for an individual and $95,400 for a family of 4.
- lack access to affordable coverage through an employer (including a family member’s employer)
- be ineligible for coverage through Medicare, Medicaid, the Children’s Health Insurance Program, or other forms of public assistance
- have US citizenship or proof of legal residency
- file taxes jointly if married.
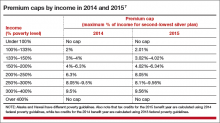
The premium tax credit caps the amount that an individual or family must spend on their monthly payments for health insurance. The cap depends on the family’s income; lower-income families have a lower cap. The amount of the tax credit remains the same, so a person who purchases a more expensive plan pays the cost difference (TABLE 2).
The ruling’s effect on women’s health
On June 26, American College of Obstetricians and Gynecologists President Mark S. DeFrancesco, MD, MBA, hailed the Supreme Court decision, saying, “Importantly, recent data have shown that newly insured adults under the ACA were more likely to be women. Those who did gain coverage through the ACA reported better access to health care and better financial security from medical costs.”
“Without question, many women enrollees were able to purchase health insurance coverage due, in part, to the ACA subsidies that helped make this purchase affordable. In fact, government data have suggested that roughly 85% of health exchange enrollees received subsidies,” Dr. DeFrancesco said.
“If the Supreme Court had overturned this important assistance, approximately 4.8 million women would have been unable to afford the coverage that they need. The impact also would have been widespread; as these women were forced to leave the insurance marketplace, it is likely that premiums throughout the marketplace would have risen dramatically,” he continued.
“Instead, patients—especially the low- and moderate-income American women who have particularly benefited from ACA subsidies—will continue to have the peace of mind that comes with insurance coverage.”
Share your thoughts! Send your Letter to the Editor to [email protected]. Please include your name and the city and state in which you practice.
1. Blumberg LJ, Buettgens M, Holahan J. The implications of a Supreme Court finding for the plaintiff in King v. Burwell: 8.2 million more uninsured and 35% higher premiums. Urban Institute. http://www.urban.org/research/publication/implications-supreme-court-finding-plaintiff-king-vs-burwell-82-million-more-uninsured-and-35-higher-premiums. Published January 8, 2015. Accessed July 2, 2015.
2. Sheiner L, Mochoruk B. King v. Burwell explained. Brookings Institute. http://www.brookings.edu/blogs/health360/posts/2015/03/03-king-v-burwell-explainer-sheiner. Published March 3, 2015. Accessed July 2, 2015.
3. Howe A. Court backs Obama administration on health care subsidies: In plain English. SCOTUSblog. http://www.scotusblog.com/2015/06/court-backs-obama-administration-on-health-care-subsidies-in-plain-english/. Published June 25, 2015. Accessed July 1, 2015.
4. Hall MA. King v. Burwell—ACA Armageddon averted. N Engl J Med. http://www.nejm.org/doi/full/10.1056/NEJMp1504077. Published July 1, 2015. Accessed July 2, 2015.
5. Jost T. Implementing health reform: The Supreme Court upholds tax credits in the federal exchange. Health Affairs blog. http://healthaffairs.org/blog/2015/06/25/implementing-health-reform-the-supreme-court-upholds-tax-credits-in-the-federal-exchange/. Published June 25, 2015. Accessed July 1, 2015.
6. Greenhouse L. The Roberts Court’s reality check. New York Times. http://www.nytimes.com/2015/06/26/opinion/the-roberts-courts-reality-check.html. Published June 25, 2015. Accessed July 1, 2015.
7. Henry J. Kaiser Family Foundation. Explaining health care reform: questions about health insurance subsidies. Table 2. http://kff.org/health-reform/issue-brief/explaining-health-care-reform-questions-about-health/. Published October 27, 2014. Accessed July 2, 2015.
In a widely anticipated judgment on the Affordable Care Act (ACA), the US Supreme Court ruled 6-3 in favor of the law on June 26, 2015. The case at hand, King v. Burwell, challenged whether individuals purchasing health insurance through federal exchanges were eligible for federal premium subsidies. This ruling cemented the ACA into law and avoided a potential calamity in the private health insurance market. Let’s take a closer look.
What the case was about
The ACA allows states to set up their own health insurance exchanges or participate in a federally run exchange. Although the drafters of the ACA had expected each state to set up its own exchange, two-thirds of the states declined to do so, many in opposition to the ACA. As a result, 7 million citizens in 34 states now purchase their health insurance through federally created exchanges.
The plaintiffs in King v. Burwell argued that, because the legislation refers to those enrolled “through an Exchange established by the State,” individuals in states with federally run exchanges are not eligible for subsidies.
The law states:
(A) the monthly premiums for such month for 1 or more qualified health plans offered in the individual market within a State which cover the taxpayer, the taxpayer’s spouse, or any dependent (as defined in section 152) of the taxpayer and which were enrolled in through an Exchange established by the State under 1311 of the Patient Protection and Affordable Care Act…[emphasis added].
The Supreme Court was asked to decide whether to adhere to those exact words or to honor Congress’ intent to allow individuals to purchase subsidized insurance on any type of exchange.
What might have happened
We’ve explored in previous articles the interconnectedness of many sections of the ACA. Nowhere is that interconnectedness more clearly demonstrated than here. In order to ensure that private health insurers provide better coverage, the law requires them to abide by important consumer protections, including the elimination of “preexisting condition” exclusions. In order to prevent adverse selection and keep insurers solvent under these new rules, all individuals are required to have health care coverage—the individual mandate. If everyone is required to purchase health insurance, it has to be affordable, so lower-income individuals were promised subsidies, paid for 100% by the federal government, to help them cover their premiums when insurance is purchased through an exchange. Take away the subsidies and the whole thing starts to unravel.
The Urban Institute estimated that a Supreme Court ruling in favor of King, which would have eliminated the subsidies in states using a federal exchange, would have reduced federal tax subsidies by $29 billion in 2016, making coverage unaffordable for many and increasing the ranks of the uninsured by 8.2 million people.1
Louise Sheiner and Brendan Mochoruk of the Brookings Institute speculated that healthy individuals would disproportionately leave the marketplace, triggering 35% increases in insurance premiums for those remaining, as well as significant increases in premiums for those who just lost their subsidies.2 Many observers, including these experts, forecast that insurance companies would exit the federal exchanges altogether, triggering a health insurance “death spiral”: As premiums rise, the healthiest customers leave the marketplace, causing premiums to rise more, causing more healthy people to leave, and so on.
Clearly, this Supreme Court decision has had dramatic, long-term, real-world effects on millions of Americans. On the national level, 6,387,789 individuals were at risk of losing their tax credits if the Supreme Court had ruled in favor of King. That number represents more than $1.7 billion in total monthly tax credits. For a look at how a judgment in favor of King would have affected subsidies on a state-by-state basis, see TABLE 1.
What other commentators are saying about the King v. Burwell decision
In his majority opinion, Chief Justice John Roberts noted that the “meaning of the phrase ‘established by the State’ is not so clear.” And as Amy Howe articulated on SCOTUSblog: “if the phrase…is in fact not clear…then the next step is to look at the Affordable Care Act more broadly to determine what Congress meant by the phrase. And when you do that, the Court reasoned, it becomes apparent that Congress actually intended for the subsidies to be available to everyone who buys health insurance on an exchange, no matter who created it. If the subsidies weren’t available in the states with federal exchanges, the Court explained, the insurance markets in those states simply wouldn’t work properly: without the subsidies, almost all of the people who purchased insurance on the exchanges would no longer be required to purchase insurance because it would be too expensive. This would create a ‘death spiral’….”
—Amy Howe, SCOTUSblog3
“Additional court challenges to other ACA provisions are still possible, but King’s six-member majority shows little appetite for challenges threatening the Act’s core structure. Even Scalia’s dissent recognizes that the ACA may one day ‘attain the enduring status of the Social Security Act.’ Thus, the decision may usher in a new era of policy maturity, in which efforts to undermine the ACA diminish, as focus shifts to efforts to implement and improve it.”
—Mark A. Hall, JD, New England Journal of Medicine4
“With the Court upholding the administration’s interpretation of the law, the Obama administration has little reason to accede to
Republican proposals. The Court’s decision effectively puts the future of the ACA on hold until the 2016 elections, when the people will decide whether to stay the course or to chart a very different path.”
—Timothy Jost, Health Affairs5
“A case that 6 months ago seemed to offer the Court’s conservatives a low-risk opportunity to accomplish what they almost did in 2012—kill the Affordable Care Act—became suffused with danger, for the millions of newly insured Americans, of course, but also for the Supreme Court itself. Ideology came face to face with reality, and reality prevailed.”
—Linda Greenhouse, New York Times6
How premium subsidies work
Premium subsidies are actually tax credits. Individuals and families can qualify for them to purchase any type of health insurance offered on an exchange, except catastrophic coverage. To receive the premium tax credit for coverage starting in 2015, a marketplace enrollee must:
- have a household income that is 1 to4 times the federal poverty level. In 2015, the range of incomes that qualify for subsidies is $11,670 for an individual and $23,850 for a family of 4 at 100% of the federal poverty level. At 400% of the federal poverty level, it is $46,680 for an individual and $95,400 for a family of 4.
- lack access to affordable coverage through an employer (including a family member’s employer)
- be ineligible for coverage through Medicare, Medicaid, the Children’s Health Insurance Program, or other forms of public assistance
- have US citizenship or proof of legal residency
- file taxes jointly if married.
The premium tax credit caps the amount that an individual or family must spend on their monthly payments for health insurance. The cap depends on the family’s income; lower-income families have a lower cap. The amount of the tax credit remains the same, so a person who purchases a more expensive plan pays the cost difference (TABLE 2).
The ruling’s effect on women’s health
On June 26, American College of Obstetricians and Gynecologists President Mark S. DeFrancesco, MD, MBA, hailed the Supreme Court decision, saying, “Importantly, recent data have shown that newly insured adults under the ACA were more likely to be women. Those who did gain coverage through the ACA reported better access to health care and better financial security from medical costs.”
“Without question, many women enrollees were able to purchase health insurance coverage due, in part, to the ACA subsidies that helped make this purchase affordable. In fact, government data have suggested that roughly 85% of health exchange enrollees received subsidies,” Dr. DeFrancesco said.
“If the Supreme Court had overturned this important assistance, approximately 4.8 million women would have been unable to afford the coverage that they need. The impact also would have been widespread; as these women were forced to leave the insurance marketplace, it is likely that premiums throughout the marketplace would have risen dramatically,” he continued.
“Instead, patients—especially the low- and moderate-income American women who have particularly benefited from ACA subsidies—will continue to have the peace of mind that comes with insurance coverage.”
Share your thoughts! Send your Letter to the Editor to [email protected]. Please include your name and the city and state in which you practice.
In a widely anticipated judgment on the Affordable Care Act (ACA), the US Supreme Court ruled 6-3 in favor of the law on June 26, 2015. The case at hand, King v. Burwell, challenged whether individuals purchasing health insurance through federal exchanges were eligible for federal premium subsidies. This ruling cemented the ACA into law and avoided a potential calamity in the private health insurance market. Let’s take a closer look.
What the case was about
The ACA allows states to set up their own health insurance exchanges or participate in a federally run exchange. Although the drafters of the ACA had expected each state to set up its own exchange, two-thirds of the states declined to do so, many in opposition to the ACA. As a result, 7 million citizens in 34 states now purchase their health insurance through federally created exchanges.
The plaintiffs in King v. Burwell argued that, because the legislation refers to those enrolled “through an Exchange established by the State,” individuals in states with federally run exchanges are not eligible for subsidies.
The law states:
(A) the monthly premiums for such month for 1 or more qualified health plans offered in the individual market within a State which cover the taxpayer, the taxpayer’s spouse, or any dependent (as defined in section 152) of the taxpayer and which were enrolled in through an Exchange established by the State under 1311 of the Patient Protection and Affordable Care Act…[emphasis added].
The Supreme Court was asked to decide whether to adhere to those exact words or to honor Congress’ intent to allow individuals to purchase subsidized insurance on any type of exchange.
What might have happened
We’ve explored in previous articles the interconnectedness of many sections of the ACA. Nowhere is that interconnectedness more clearly demonstrated than here. In order to ensure that private health insurers provide better coverage, the law requires them to abide by important consumer protections, including the elimination of “preexisting condition” exclusions. In order to prevent adverse selection and keep insurers solvent under these new rules, all individuals are required to have health care coverage—the individual mandate. If everyone is required to purchase health insurance, it has to be affordable, so lower-income individuals were promised subsidies, paid for 100% by the federal government, to help them cover their premiums when insurance is purchased through an exchange. Take away the subsidies and the whole thing starts to unravel.
The Urban Institute estimated that a Supreme Court ruling in favor of King, which would have eliminated the subsidies in states using a federal exchange, would have reduced federal tax subsidies by $29 billion in 2016, making coverage unaffordable for many and increasing the ranks of the uninsured by 8.2 million people.1
Louise Sheiner and Brendan Mochoruk of the Brookings Institute speculated that healthy individuals would disproportionately leave the marketplace, triggering 35% increases in insurance premiums for those remaining, as well as significant increases in premiums for those who just lost their subsidies.2 Many observers, including these experts, forecast that insurance companies would exit the federal exchanges altogether, triggering a health insurance “death spiral”: As premiums rise, the healthiest customers leave the marketplace, causing premiums to rise more, causing more healthy people to leave, and so on.
Clearly, this Supreme Court decision has had dramatic, long-term, real-world effects on millions of Americans. On the national level, 6,387,789 individuals were at risk of losing their tax credits if the Supreme Court had ruled in favor of King. That number represents more than $1.7 billion in total monthly tax credits. For a look at how a judgment in favor of King would have affected subsidies on a state-by-state basis, see TABLE 1.
What other commentators are saying about the King v. Burwell decision
In his majority opinion, Chief Justice John Roberts noted that the “meaning of the phrase ‘established by the State’ is not so clear.” And as Amy Howe articulated on SCOTUSblog: “if the phrase…is in fact not clear…then the next step is to look at the Affordable Care Act more broadly to determine what Congress meant by the phrase. And when you do that, the Court reasoned, it becomes apparent that Congress actually intended for the subsidies to be available to everyone who buys health insurance on an exchange, no matter who created it. If the subsidies weren’t available in the states with federal exchanges, the Court explained, the insurance markets in those states simply wouldn’t work properly: without the subsidies, almost all of the people who purchased insurance on the exchanges would no longer be required to purchase insurance because it would be too expensive. This would create a ‘death spiral’….”
—Amy Howe, SCOTUSblog3
“Additional court challenges to other ACA provisions are still possible, but King’s six-member majority shows little appetite for challenges threatening the Act’s core structure. Even Scalia’s dissent recognizes that the ACA may one day ‘attain the enduring status of the Social Security Act.’ Thus, the decision may usher in a new era of policy maturity, in which efforts to undermine the ACA diminish, as focus shifts to efforts to implement and improve it.”
—Mark A. Hall, JD, New England Journal of Medicine4
“With the Court upholding the administration’s interpretation of the law, the Obama administration has little reason to accede to
Republican proposals. The Court’s decision effectively puts the future of the ACA on hold until the 2016 elections, when the people will decide whether to stay the course or to chart a very different path.”
—Timothy Jost, Health Affairs5
“A case that 6 months ago seemed to offer the Court’s conservatives a low-risk opportunity to accomplish what they almost did in 2012—kill the Affordable Care Act—became suffused with danger, for the millions of newly insured Americans, of course, but also for the Supreme Court itself. Ideology came face to face with reality, and reality prevailed.”
—Linda Greenhouse, New York Times6
How premium subsidies work
Premium subsidies are actually tax credits. Individuals and families can qualify for them to purchase any type of health insurance offered on an exchange, except catastrophic coverage. To receive the premium tax credit for coverage starting in 2015, a marketplace enrollee must:
- have a household income that is 1 to4 times the federal poverty level. In 2015, the range of incomes that qualify for subsidies is $11,670 for an individual and $23,850 for a family of 4 at 100% of the federal poverty level. At 400% of the federal poverty level, it is $46,680 for an individual and $95,400 for a family of 4.
- lack access to affordable coverage through an employer (including a family member’s employer)
- be ineligible for coverage through Medicare, Medicaid, the Children’s Health Insurance Program, or other forms of public assistance
- have US citizenship or proof of legal residency
- file taxes jointly if married.
The premium tax credit caps the amount that an individual or family must spend on their monthly payments for health insurance. The cap depends on the family’s income; lower-income families have a lower cap. The amount of the tax credit remains the same, so a person who purchases a more expensive plan pays the cost difference (TABLE 2).
The ruling’s effect on women’s health
On June 26, American College of Obstetricians and Gynecologists President Mark S. DeFrancesco, MD, MBA, hailed the Supreme Court decision, saying, “Importantly, recent data have shown that newly insured adults under the ACA were more likely to be women. Those who did gain coverage through the ACA reported better access to health care and better financial security from medical costs.”
“Without question, many women enrollees were able to purchase health insurance coverage due, in part, to the ACA subsidies that helped make this purchase affordable. In fact, government data have suggested that roughly 85% of health exchange enrollees received subsidies,” Dr. DeFrancesco said.
“If the Supreme Court had overturned this important assistance, approximately 4.8 million women would have been unable to afford the coverage that they need. The impact also would have been widespread; as these women were forced to leave the insurance marketplace, it is likely that premiums throughout the marketplace would have risen dramatically,” he continued.
“Instead, patients—especially the low- and moderate-income American women who have particularly benefited from ACA subsidies—will continue to have the peace of mind that comes with insurance coverage.”
Share your thoughts! Send your Letter to the Editor to [email protected]. Please include your name and the city and state in which you practice.
1. Blumberg LJ, Buettgens M, Holahan J. The implications of a Supreme Court finding for the plaintiff in King v. Burwell: 8.2 million more uninsured and 35% higher premiums. Urban Institute. http://www.urban.org/research/publication/implications-supreme-court-finding-plaintiff-king-vs-burwell-82-million-more-uninsured-and-35-higher-premiums. Published January 8, 2015. Accessed July 2, 2015.
2. Sheiner L, Mochoruk B. King v. Burwell explained. Brookings Institute. http://www.brookings.edu/blogs/health360/posts/2015/03/03-king-v-burwell-explainer-sheiner. Published March 3, 2015. Accessed July 2, 2015.
3. Howe A. Court backs Obama administration on health care subsidies: In plain English. SCOTUSblog. http://www.scotusblog.com/2015/06/court-backs-obama-administration-on-health-care-subsidies-in-plain-english/. Published June 25, 2015. Accessed July 1, 2015.
4. Hall MA. King v. Burwell—ACA Armageddon averted. N Engl J Med. http://www.nejm.org/doi/full/10.1056/NEJMp1504077. Published July 1, 2015. Accessed July 2, 2015.
5. Jost T. Implementing health reform: The Supreme Court upholds tax credits in the federal exchange. Health Affairs blog. http://healthaffairs.org/blog/2015/06/25/implementing-health-reform-the-supreme-court-upholds-tax-credits-in-the-federal-exchange/. Published June 25, 2015. Accessed July 1, 2015.
6. Greenhouse L. The Roberts Court’s reality check. New York Times. http://www.nytimes.com/2015/06/26/opinion/the-roberts-courts-reality-check.html. Published June 25, 2015. Accessed July 1, 2015.
7. Henry J. Kaiser Family Foundation. Explaining health care reform: questions about health insurance subsidies. Table 2. http://kff.org/health-reform/issue-brief/explaining-health-care-reform-questions-about-health/. Published October 27, 2014. Accessed July 2, 2015.
1. Blumberg LJ, Buettgens M, Holahan J. The implications of a Supreme Court finding for the plaintiff in King v. Burwell: 8.2 million more uninsured and 35% higher premiums. Urban Institute. http://www.urban.org/research/publication/implications-supreme-court-finding-plaintiff-king-vs-burwell-82-million-more-uninsured-and-35-higher-premiums. Published January 8, 2015. Accessed July 2, 2015.
2. Sheiner L, Mochoruk B. King v. Burwell explained. Brookings Institute. http://www.brookings.edu/blogs/health360/posts/2015/03/03-king-v-burwell-explainer-sheiner. Published March 3, 2015. Accessed July 2, 2015.
3. Howe A. Court backs Obama administration on health care subsidies: In plain English. SCOTUSblog. http://www.scotusblog.com/2015/06/court-backs-obama-administration-on-health-care-subsidies-in-plain-english/. Published June 25, 2015. Accessed July 1, 2015.
4. Hall MA. King v. Burwell—ACA Armageddon averted. N Engl J Med. http://www.nejm.org/doi/full/10.1056/NEJMp1504077. Published July 1, 2015. Accessed July 2, 2015.
5. Jost T. Implementing health reform: The Supreme Court upholds tax credits in the federal exchange. Health Affairs blog. http://healthaffairs.org/blog/2015/06/25/implementing-health-reform-the-supreme-court-upholds-tax-credits-in-the-federal-exchange/. Published June 25, 2015. Accessed July 1, 2015.
6. Greenhouse L. The Roberts Court’s reality check. New York Times. http://www.nytimes.com/2015/06/26/opinion/the-roberts-courts-reality-check.html. Published June 25, 2015. Accessed July 1, 2015.
7. Henry J. Kaiser Family Foundation. Explaining health care reform: questions about health insurance subsidies. Table 2. http://kff.org/health-reform/issue-brief/explaining-health-care-reform-questions-about-health/. Published October 27, 2014. Accessed July 2, 2015.
The SGR is abolished! What comes next?
Congratulations, OBG Management readers! After years of hard work and collective advocacy on your part, the US Congress finally passed, and President Barack Obama quickly signed into law, a permanent repeal of the Medicare Sustainable Growth Rate (SGR) physician payment system. Yes, celebrations are in order.
The US House of Representatives passed the bill, HR 2, the Medicare Access and CHIP Reauthorization Act of 2015 (MACRA), sponsored by American College of Obstetricians and Gynecologists (ACOG) Fellow and US Rep. Michael Burgess (R-TX), on March 26, with 382 Republicans and Democrats voting “Yes.” The Senate followed, on April 14, and agreed with the House to repeal, forever, the Medicare SGR, passing the Burgess bill without amendment, on a bipartisan vote of 92–8. With only hours to go before the scheduled 21.2% cut took effect, the President signed the bill, now Public Law (PL) 114-10, on April 16. The President noted that he was “proud to sign the bill into law.” ACOG is proud to have been such an important part of this landmark moment.
SGR: the perennial nemesis of physicians
The SGR has wreaked havoc on medicine and patient care for 15 years or more. Approximately 30,000 ObGyns participate in Medicare, and many private health insurers use Medicare payment policies, as does TriCare, the nation’s health care coverage for military members and their families. The SGR’s effect was felt widely across medicine, making it nearly impossible for physician practices to invest in health information technology and other patient safety advances, or even to plan for the next year or continue accepting Medicare patients.
When it was introduced last year, HR 2 was supported by more than 600 national and state medical societies and specialty organizations, plus patient and provider organizations, policy think tanks, and advocacy groups across the political spectrum.
ACOG Fellows petitioned their members of Congress with incredible passion, perseverance, and commitment to put an end to the SGR wrecking ball. Hundreds flew into Washington, DC, sent thousands of emails, made phone calls, wrote letters, and personally lobbied at home and in the halls of Congress.
Special kudos, too, to our champions in Congress, and there are many, led by ACOG Fellows and US Reps. Dr. Burgess and Phil Roe, MD (R-TN). Burgess wrote the House bill and, together with Roe, pushed nonstop to get this bill over the finish line. It wouldn’t have happened without them.
ACOG worked tirelessly on its own and in coalition with the American Medical Association, surgical groups, and many other partners. We were able to win important provisions in the statute that we anticipate will greatly help ObGyns successfully transition to this new payment system.
PL114-10 replaces the SGR with a new payment system intended to promote care coordination and quality improvement and lead to better health for our nation’s seniors. Congress developed this new payment plan with the physician community, rather than imposing it on us. That’s why throughout the statute, we see repeated requirements that the Secretary of Health and Human Services must develop quality measures, alternative payment models, and a host of key aspects with input from and in consultation with physicians and the relevant medical specialties, ensuring that physicians retain their preeminent roles in these areas. Funding is provided for quality measure development at $15 million per year from 2015 to 2019.
This law will likely change physician practices more than the ACA ever will, and Congress agreed that physicians should be integral to its development to ensure that they can continue to thrive and provide high-quality care and access for their patients.
Let’s take a closer look at the new Medicare payment system—especially what it will mean for your practice.
What the new law does
Important provisions
- MACRA retains the fee-for-service payment model, now called the Merit-based Incentive Payment System, or MIPS. Physician participation in the Advanced Payment Models (APMs) is entirely voluntary. But physicians who participate in APMs and who score better each year will earn more.
- All physician types are treated equally. Congress didn’t pick specialty winners and losers.
- The new payment system rewards physicians for continuous improvement. You can determine how financially well you do.
- Beginning in 2019, Medicare physician payments will reflect each individual physician’s performance, based on a range of measures developed by the relevant medical specialty that will give individuals options that best reflect their practices.
- Individual physicians will receive confidential quarterly feedback on their performance.
- Technical support is provided for smaller practices, funded at $20 million per year from 2016 to 2020, to help them transition to MIPS and APMs. And physicians in small practices can opt to join a “virtual MIPS group,” associating with other practices or hospitals in the same geographic region or by specialty types.
- The law protects physicians from liability from federal or state standards of care. No health care guideline or other standard developed under federal or state requirements associated with this law may be used as a standard of care or duty of care owed by a health care professional to a patient in a medical liability lawsuit.
MACRA stabilizes the Medicare payment system by permanently repealing the SGR and scheduling payments into the future:
- through June 2015: Stable payments with no cuts
- July 2015–2019: 0.5% annual payment increases to all Medicare physicians
- 2020–2025: No automatic annual payment changes but opportunities for payment increases based on individual performance
- 2026 and beyond: 0.75% annual payment increases for qualifying APMs, 0.25% for MIPS providers, with opportunities in both systems for higher payments based on individual performance.
Top ACOG wins
Among the most meaningful accomplishments achieved by ACOG in its work to repeal the sustainable growth rate are:
- Reliable payment increases for the first 5 years. The law ensures a period of stability with modest Medicare payment in-
creases for 5 years and no cuts, with opportunity for payment increases for the next 5 years. This 5-year period gives physicians time to get ready for the new payment systems. - Protection for low-Medicare–volume physician practices. ObGyns and other physicians with a small Medicare patient population are exempt from many program requirements and penalties.
- Stops the Centers for Medicare and Medicaid Services (CMS) policy on global surgical codes, reinstating 10-day and 90-day global payment bundles for surgical services. This directly helps ObGyn subspecialists, including urogynecologists and gynecologic oncologists.
- Physician liability protections. The law ensures that federal quality measurements cannot be used to imply medical negligence and generate lawsuits.
- Protection for ultrasound. There are no cuts to ultrasound reimbursement.
- An end, in 2018, to penalties related to electronic health record (EHR) meaningful use, Physician Quality Reporting Systems, and the use of the value-based modifier.
- APM bonus payments. Bonus eligibility for Alternative Payment Model (APM) participation is based on patient volume, not just revenue, to make it easier for ObGyns to qualify.
- 2-year extension of the Children’s Health Insurance Program (CHIP), which provides comprehensive coverage to 8 million children, adolescents, and pregnant women across the country.
- Quality-measure development. The law helps professional organizations, such as ACOG, develop quality measures for the Merit-Based Incentive Payment System (MIPS) rather than allow these measures to be developed by a federal agency, ensuring that this new program works for physicians and our patients.
Two payment system options reward continuous quality improvement
Option 1: MIPS. MACRA consolidates and expands pay-for-performance incentives within the old SGR fee-for-service system, creating the new MIPS. Under MIPS, the Physician Quality Reporting System (PQRS), electronic health record (EHR) meaningful use incentive program, and physician value-based modifiers (VBMs) become a single program. In 2019, a physician’s individual score on these measures will be used to adjust his or her Medicare payments, and the penalties previously associated with these programs come to an end.
MACRA creates 4 categories of measures that are weighted to calculate an individual physician’s MIPS score:
- Quality (50% of total adjustment in 2019, shrinking to 30% of total adjustment in 2021). Quality measures currently in use in the PQRS, VBM, and EHR meaningful use programs will continue to be used. The Secretary of Health and Human Services must fund and work with specialty societies to develop any additional measures, and measures utilized in clinical data registries can be used for this category as well. Measures will be updated annually, and ACOG and other specialties can submit measures directly for approval, rather than rely on an outside entity.
- Resource use (10% of total adjustment in 2019, growing to 30% of total adjustment by 2021). Resource use measures are risk-adjusted and include those already used in the VBM program; others must be developed with physicians, reflecting both the physician’s role in treating the patient (eg, primary or specialty care) and the type of treatment (eg, chronic or acute).
- EHR use (25% of total adjustment). Current meaningful use systems will qualify for this category. The law also requires EHR interoperability by 2018 and prohibits the blocking of information sharing between EHR vendors.
- Clinical improvement (15% of total adjustment). This is a new component of physician measurement, intended to give physicians credit for working to improve their practices and help them participate in APMs, which have higher reimbursement potential. This menu of qualifying activities—including 24-hour availability, safety, and patient satisfaction—must be developed with physicians and must be attainable by all specialties and practice types, including small practices and those in rural and underserved areas. Maintenance of certification can be used to qual-ify for a high score.
Physicians will only be assessed on the categories, measures, and activities that apply to them. A physician’s composite score (0–100) will be compared with a performance threshold that reflects all physicians. Those who score above the threshold will receive increased payments; those who score below the threshold will receive reduced payments. Physicians will know these thresholds in advance and will know the score they must reach to avoid penalties and win higher reimbursements in each performance period.
As physicians as a whole improve their performance, the threshold will move with them. So each year, physicians will have the incentive to keep improving their quality, resource use, clinical improvement, and EHR use. A physician’s payment adjustment in one year will not affect his or her payment adjustment in the next year.
The range of potential payment adjustments based on MIPS performance measures increases each year through 2022. Providers who have high scores are rewarded with a 4% increase in 2019. By 2022, the reward is 9%. The program is budget-neutral, so total positive adjustments across all providers will equal total negative adjustments across all providers to poor performers. Separate funds are set aside to reward the highest performers, who will earn bonuses of up to 10% of their fee-for-service payment rate from 2019 through 2024, as well as to help low performers improve and qualify for increased payments from 2016 through 2020.
Help for physicians includes:
- flexibility to participate in a way that best reflects their practice, using risk-adjusted clinical outcome measures
- option to participate in a virtual MIPS group rather than go it alone
- technical assistance to practices with 15 or fewer professionals, $20 million annually from 2016 through 2020, with preference to practices with low MIPS scores and those in rural and underserved areas
- quarterly confidential feedback on performance in the quality and resource use categories
- advance notification to each physician of the score needed to reach higher payment levels
- exclusion from MIPS of physicians who treat few Medicare patients, as well as those who receive a significant portion of their revenues from APMs.
Option 2: APMs. Physicians can earn higher fees by opting out of MIPS fee for service and participating in APMs. The law defines qualifying APMs as those that require participating providers to take on “more than nominal” financial risk, report quality measures, and use certified EHR technology.
APMs will cover multiple services, show that they can limit the growth of spending, and use performance-based methods of compensation. These and other provisions will likely continue the trend away from physicians practicing in solo or small-group fee-for-service practices into risk-based multispecialty settings that are subject to increased management and oversight.
From 2019 to 2024, qualified APM physicians will receive a 5% annual lump sum bonus based on their prior year’s physician fee-schedule payments plus shared savings from participation. This bonus is based on patient volume, not just revenue, to make it easier for ObGyns to qualify. To make the bonus widely available, the Secretary of Health and Human Services must test APMs designed for specific specialties and physicians in small practices. As in MIPS, top APM performers will also receive an additional bonus.
To qualify, physicians must meet increasing thresholds for the percentage of their revenue that they receive through APMs. Those who are below but near the required level of APM revenue can be exempted from MIPS adjustments.
- 2019–2020: 25% of Medicare revenue must be received through APMs.
- 2021–2022: 50% of Medicare revenue or 50% of all-payer revenue along with 25% of Medicare revenue must be received through APMs.
- 2023 and beyond: 75% of Medicare revenue or 75% of all-payer revenue along with 25% of Medicare revenue must be received through APMs.
Who pays the bill?
Medicare beneficiaries pay more
The new law increases the percentage of Medicare Parts B and D premiums that high-income beneficiaries must pay beginning in 2018:
- Single seniors reporting income of more than $133,500 and married couples with income of more than $267,000 will see their share of premiums rise from 50% to 65%.
- Single seniors reporting income above $160,000 and married couples with income above $320,000 will see their premium share rise from 65% to 80%.
This change will affect about 2% of Medicare beneficiaries; half of all Medicare beneficiaries currently have annual incomes below $26,000.1
Medigap “first-dollar coverage” will end
Many Medigap plans on the market today provide “first-dollar coverage” for beneficiaries, which means that the plans pay the deductibles and copayments so that the beneficiaries have no out-of-pocket costs. Beginning in 2020, Medigap plans will only be available to cover costs above the Medicare Part B deductible, currently $147 per year, for new Medigap enrollees. Many lawmakers thought it was important for Medicare beneficiaries to have “skin in the game.”
The law cuts payments for some providers
To partially offset the cost of repealing the SGR, MACRA cuts Medicare payments to hospitals and postacute providers. It:
- delays Disproportionate Share Hospital (DSH) cuts scheduled to begin in 2017 by a year and extends them through 2025
- requires an increase in payments to hospitals scheduled for 2018 to instead be phased in over 6 years
- limits the 2018 payment update for post-acute providers to 1%.
The law extends many programs
These programs are vital to support the future ObGyn workforce and access to health care. Among these programs are:
- a halt to the Centers for Medicare and Medicaid Services (CMS) policy on global surgical codes. The law reinstates 10-day and 90-day global payment bundles for surgical services. This directly helps ObGyn subspecialists, such as urogynecologists and gynecologic oncologists.
- renewal of the Children’s Health Insurance Program (CHIP), which provides comprehensive coverage to 8 million children, adolescents, and pregnant women across the country
- establishment of a Medicaid/CHIP Pediatric Quality Measures Program, supporting the development and physician adoption of quality measures, including for prenatal and preconception care
- funding for the Maternal, Infant, and Early Childhood Home Visiting Program, helping at-risk pregnant women and their families to promote healthy births and early childhood development
- funding for community health centers, an important source of care for 13 million women and girls in all 50 states and the District of Columbia
- funding for the National Health Service Corps, bringing ObGyns and other primary care providers to underserved rural and urban areas through scholarships and loan repayment programs
- funding for the Teaching Health Center Graduate Medical Education Payment Program, enhancing training for ObGyns and other primary care providers in community-based settings
- extending the Medicare Geographic Practice Cost Index floor, helping ensure access to care for women in rural areas
- extending the Personal Responsibility Education Program to help prevent teen pregnancies and sexually transmitted infections.
Next steps
It’s very important that ObGyns and other physicians use these early years to understand and get ready for the new payment systems. ACOG is developing educational material for our members, and will work closely with our colleague medical organizations and the Department of Health and Human Services to develop key aspects of the law and ensure that it is properly implemented to work for physicians and patients.
Share your thoughts on this article! Send your Letter to the Editor to [email protected]. Please include your name and the city and state in which you practice.
Reference
1. Aaron HJ. Three cheers for log-rolling: The demise of the SGR. Brookings Health360. http://www.brookings.edu/blogs/health360/posts/2015/04/22-medicare-sgr-repeal-doc-fix-aaron. Published April 22, 2015. Accessed May 12, 2015.
Congratulations, OBG Management readers! After years of hard work and collective advocacy on your part, the US Congress finally passed, and President Barack Obama quickly signed into law, a permanent repeal of the Medicare Sustainable Growth Rate (SGR) physician payment system. Yes, celebrations are in order.
The US House of Representatives passed the bill, HR 2, the Medicare Access and CHIP Reauthorization Act of 2015 (MACRA), sponsored by American College of Obstetricians and Gynecologists (ACOG) Fellow and US Rep. Michael Burgess (R-TX), on March 26, with 382 Republicans and Democrats voting “Yes.” The Senate followed, on April 14, and agreed with the House to repeal, forever, the Medicare SGR, passing the Burgess bill without amendment, on a bipartisan vote of 92–8. With only hours to go before the scheduled 21.2% cut took effect, the President signed the bill, now Public Law (PL) 114-10, on April 16. The President noted that he was “proud to sign the bill into law.” ACOG is proud to have been such an important part of this landmark moment.
SGR: the perennial nemesis of physicians
The SGR has wreaked havoc on medicine and patient care for 15 years or more. Approximately 30,000 ObGyns participate in Medicare, and many private health insurers use Medicare payment policies, as does TriCare, the nation’s health care coverage for military members and their families. The SGR’s effect was felt widely across medicine, making it nearly impossible for physician practices to invest in health information technology and other patient safety advances, or even to plan for the next year or continue accepting Medicare patients.
When it was introduced last year, HR 2 was supported by more than 600 national and state medical societies and specialty organizations, plus patient and provider organizations, policy think tanks, and advocacy groups across the political spectrum.
ACOG Fellows petitioned their members of Congress with incredible passion, perseverance, and commitment to put an end to the SGR wrecking ball. Hundreds flew into Washington, DC, sent thousands of emails, made phone calls, wrote letters, and personally lobbied at home and in the halls of Congress.
Special kudos, too, to our champions in Congress, and there are many, led by ACOG Fellows and US Reps. Dr. Burgess and Phil Roe, MD (R-TN). Burgess wrote the House bill and, together with Roe, pushed nonstop to get this bill over the finish line. It wouldn’t have happened without them.
ACOG worked tirelessly on its own and in coalition with the American Medical Association, surgical groups, and many other partners. We were able to win important provisions in the statute that we anticipate will greatly help ObGyns successfully transition to this new payment system.
PL114-10 replaces the SGR with a new payment system intended to promote care coordination and quality improvement and lead to better health for our nation’s seniors. Congress developed this new payment plan with the physician community, rather than imposing it on us. That’s why throughout the statute, we see repeated requirements that the Secretary of Health and Human Services must develop quality measures, alternative payment models, and a host of key aspects with input from and in consultation with physicians and the relevant medical specialties, ensuring that physicians retain their preeminent roles in these areas. Funding is provided for quality measure development at $15 million per year from 2015 to 2019.
This law will likely change physician practices more than the ACA ever will, and Congress agreed that physicians should be integral to its development to ensure that they can continue to thrive and provide high-quality care and access for their patients.
Let’s take a closer look at the new Medicare payment system—especially what it will mean for your practice.
What the new law does
Important provisions
- MACRA retains the fee-for-service payment model, now called the Merit-based Incentive Payment System, or MIPS. Physician participation in the Advanced Payment Models (APMs) is entirely voluntary. But physicians who participate in APMs and who score better each year will earn more.
- All physician types are treated equally. Congress didn’t pick specialty winners and losers.
- The new payment system rewards physicians for continuous improvement. You can determine how financially well you do.
- Beginning in 2019, Medicare physician payments will reflect each individual physician’s performance, based on a range of measures developed by the relevant medical specialty that will give individuals options that best reflect their practices.
- Individual physicians will receive confidential quarterly feedback on their performance.
- Technical support is provided for smaller practices, funded at $20 million per year from 2016 to 2020, to help them transition to MIPS and APMs. And physicians in small practices can opt to join a “virtual MIPS group,” associating with other practices or hospitals in the same geographic region or by specialty types.
- The law protects physicians from liability from federal or state standards of care. No health care guideline or other standard developed under federal or state requirements associated with this law may be used as a standard of care or duty of care owed by a health care professional to a patient in a medical liability lawsuit.
MACRA stabilizes the Medicare payment system by permanently repealing the SGR and scheduling payments into the future:
- through June 2015: Stable payments with no cuts
- July 2015–2019: 0.5% annual payment increases to all Medicare physicians
- 2020–2025: No automatic annual payment changes but opportunities for payment increases based on individual performance
- 2026 and beyond: 0.75% annual payment increases for qualifying APMs, 0.25% for MIPS providers, with opportunities in both systems for higher payments based on individual performance.
Top ACOG wins
Among the most meaningful accomplishments achieved by ACOG in its work to repeal the sustainable growth rate are:
- Reliable payment increases for the first 5 years. The law ensures a period of stability with modest Medicare payment in-
creases for 5 years and no cuts, with opportunity for payment increases for the next 5 years. This 5-year period gives physicians time to get ready for the new payment systems. - Protection for low-Medicare–volume physician practices. ObGyns and other physicians with a small Medicare patient population are exempt from many program requirements and penalties.
- Stops the Centers for Medicare and Medicaid Services (CMS) policy on global surgical codes, reinstating 10-day and 90-day global payment bundles for surgical services. This directly helps ObGyn subspecialists, including urogynecologists and gynecologic oncologists.
- Physician liability protections. The law ensures that federal quality measurements cannot be used to imply medical negligence and generate lawsuits.
- Protection for ultrasound. There are no cuts to ultrasound reimbursement.
- An end, in 2018, to penalties related to electronic health record (EHR) meaningful use, Physician Quality Reporting Systems, and the use of the value-based modifier.
- APM bonus payments. Bonus eligibility for Alternative Payment Model (APM) participation is based on patient volume, not just revenue, to make it easier for ObGyns to qualify.
- 2-year extension of the Children’s Health Insurance Program (CHIP), which provides comprehensive coverage to 8 million children, adolescents, and pregnant women across the country.
- Quality-measure development. The law helps professional organizations, such as ACOG, develop quality measures for the Merit-Based Incentive Payment System (MIPS) rather than allow these measures to be developed by a federal agency, ensuring that this new program works for physicians and our patients.
Two payment system options reward continuous quality improvement
Option 1: MIPS. MACRA consolidates and expands pay-for-performance incentives within the old SGR fee-for-service system, creating the new MIPS. Under MIPS, the Physician Quality Reporting System (PQRS), electronic health record (EHR) meaningful use incentive program, and physician value-based modifiers (VBMs) become a single program. In 2019, a physician’s individual score on these measures will be used to adjust his or her Medicare payments, and the penalties previously associated with these programs come to an end.
MACRA creates 4 categories of measures that are weighted to calculate an individual physician’s MIPS score:
- Quality (50% of total adjustment in 2019, shrinking to 30% of total adjustment in 2021). Quality measures currently in use in the PQRS, VBM, and EHR meaningful use programs will continue to be used. The Secretary of Health and Human Services must fund and work with specialty societies to develop any additional measures, and measures utilized in clinical data registries can be used for this category as well. Measures will be updated annually, and ACOG and other specialties can submit measures directly for approval, rather than rely on an outside entity.
- Resource use (10% of total adjustment in 2019, growing to 30% of total adjustment by 2021). Resource use measures are risk-adjusted and include those already used in the VBM program; others must be developed with physicians, reflecting both the physician’s role in treating the patient (eg, primary or specialty care) and the type of treatment (eg, chronic or acute).
- EHR use (25% of total adjustment). Current meaningful use systems will qualify for this category. The law also requires EHR interoperability by 2018 and prohibits the blocking of information sharing between EHR vendors.
- Clinical improvement (15% of total adjustment). This is a new component of physician measurement, intended to give physicians credit for working to improve their practices and help them participate in APMs, which have higher reimbursement potential. This menu of qualifying activities—including 24-hour availability, safety, and patient satisfaction—must be developed with physicians and must be attainable by all specialties and practice types, including small practices and those in rural and underserved areas. Maintenance of certification can be used to qual-ify for a high score.
Physicians will only be assessed on the categories, measures, and activities that apply to them. A physician’s composite score (0–100) will be compared with a performance threshold that reflects all physicians. Those who score above the threshold will receive increased payments; those who score below the threshold will receive reduced payments. Physicians will know these thresholds in advance and will know the score they must reach to avoid penalties and win higher reimbursements in each performance period.
As physicians as a whole improve their performance, the threshold will move with them. So each year, physicians will have the incentive to keep improving their quality, resource use, clinical improvement, and EHR use. A physician’s payment adjustment in one year will not affect his or her payment adjustment in the next year.
The range of potential payment adjustments based on MIPS performance measures increases each year through 2022. Providers who have high scores are rewarded with a 4% increase in 2019. By 2022, the reward is 9%. The program is budget-neutral, so total positive adjustments across all providers will equal total negative adjustments across all providers to poor performers. Separate funds are set aside to reward the highest performers, who will earn bonuses of up to 10% of their fee-for-service payment rate from 2019 through 2024, as well as to help low performers improve and qualify for increased payments from 2016 through 2020.
Help for physicians includes:
- flexibility to participate in a way that best reflects their practice, using risk-adjusted clinical outcome measures
- option to participate in a virtual MIPS group rather than go it alone
- technical assistance to practices with 15 or fewer professionals, $20 million annually from 2016 through 2020, with preference to practices with low MIPS scores and those in rural and underserved areas
- quarterly confidential feedback on performance in the quality and resource use categories
- advance notification to each physician of the score needed to reach higher payment levels
- exclusion from MIPS of physicians who treat few Medicare patients, as well as those who receive a significant portion of their revenues from APMs.
Option 2: APMs. Physicians can earn higher fees by opting out of MIPS fee for service and participating in APMs. The law defines qualifying APMs as those that require participating providers to take on “more than nominal” financial risk, report quality measures, and use certified EHR technology.
APMs will cover multiple services, show that they can limit the growth of spending, and use performance-based methods of compensation. These and other provisions will likely continue the trend away from physicians practicing in solo or small-group fee-for-service practices into risk-based multispecialty settings that are subject to increased management and oversight.
From 2019 to 2024, qualified APM physicians will receive a 5% annual lump sum bonus based on their prior year’s physician fee-schedule payments plus shared savings from participation. This bonus is based on patient volume, not just revenue, to make it easier for ObGyns to qualify. To make the bonus widely available, the Secretary of Health and Human Services must test APMs designed for specific specialties and physicians in small practices. As in MIPS, top APM performers will also receive an additional bonus.
To qualify, physicians must meet increasing thresholds for the percentage of their revenue that they receive through APMs. Those who are below but near the required level of APM revenue can be exempted from MIPS adjustments.
- 2019–2020: 25% of Medicare revenue must be received through APMs.
- 2021–2022: 50% of Medicare revenue or 50% of all-payer revenue along with 25% of Medicare revenue must be received through APMs.
- 2023 and beyond: 75% of Medicare revenue or 75% of all-payer revenue along with 25% of Medicare revenue must be received through APMs.
Who pays the bill?
Medicare beneficiaries pay more
The new law increases the percentage of Medicare Parts B and D premiums that high-income beneficiaries must pay beginning in 2018:
- Single seniors reporting income of more than $133,500 and married couples with income of more than $267,000 will see their share of premiums rise from 50% to 65%.
- Single seniors reporting income above $160,000 and married couples with income above $320,000 will see their premium share rise from 65% to 80%.
This change will affect about 2% of Medicare beneficiaries; half of all Medicare beneficiaries currently have annual incomes below $26,000.1
Medigap “first-dollar coverage” will end
Many Medigap plans on the market today provide “first-dollar coverage” for beneficiaries, which means that the plans pay the deductibles and copayments so that the beneficiaries have no out-of-pocket costs. Beginning in 2020, Medigap plans will only be available to cover costs above the Medicare Part B deductible, currently $147 per year, for new Medigap enrollees. Many lawmakers thought it was important for Medicare beneficiaries to have “skin in the game.”
The law cuts payments for some providers
To partially offset the cost of repealing the SGR, MACRA cuts Medicare payments to hospitals and postacute providers. It:
- delays Disproportionate Share Hospital (DSH) cuts scheduled to begin in 2017 by a year and extends them through 2025
- requires an increase in payments to hospitals scheduled for 2018 to instead be phased in over 6 years
- limits the 2018 payment update for post-acute providers to 1%.
The law extends many programs
These programs are vital to support the future ObGyn workforce and access to health care. Among these programs are:
- a halt to the Centers for Medicare and Medicaid Services (CMS) policy on global surgical codes. The law reinstates 10-day and 90-day global payment bundles for surgical services. This directly helps ObGyn subspecialists, such as urogynecologists and gynecologic oncologists.
- renewal of the Children’s Health Insurance Program (CHIP), which provides comprehensive coverage to 8 million children, adolescents, and pregnant women across the country
- establishment of a Medicaid/CHIP Pediatric Quality Measures Program, supporting the development and physician adoption of quality measures, including for prenatal and preconception care
- funding for the Maternal, Infant, and Early Childhood Home Visiting Program, helping at-risk pregnant women and their families to promote healthy births and early childhood development
- funding for community health centers, an important source of care for 13 million women and girls in all 50 states and the District of Columbia
- funding for the National Health Service Corps, bringing ObGyns and other primary care providers to underserved rural and urban areas through scholarships and loan repayment programs
- funding for the Teaching Health Center Graduate Medical Education Payment Program, enhancing training for ObGyns and other primary care providers in community-based settings
- extending the Medicare Geographic Practice Cost Index floor, helping ensure access to care for women in rural areas
- extending the Personal Responsibility Education Program to help prevent teen pregnancies and sexually transmitted infections.
Next steps
It’s very important that ObGyns and other physicians use these early years to understand and get ready for the new payment systems. ACOG is developing educational material for our members, and will work closely with our colleague medical organizations and the Department of Health and Human Services to develop key aspects of the law and ensure that it is properly implemented to work for physicians and patients.
Share your thoughts on this article! Send your Letter to the Editor to [email protected]. Please include your name and the city and state in which you practice.
Congratulations, OBG Management readers! After years of hard work and collective advocacy on your part, the US Congress finally passed, and President Barack Obama quickly signed into law, a permanent repeal of the Medicare Sustainable Growth Rate (SGR) physician payment system. Yes, celebrations are in order.
The US House of Representatives passed the bill, HR 2, the Medicare Access and CHIP Reauthorization Act of 2015 (MACRA), sponsored by American College of Obstetricians and Gynecologists (ACOG) Fellow and US Rep. Michael Burgess (R-TX), on March 26, with 382 Republicans and Democrats voting “Yes.” The Senate followed, on April 14, and agreed with the House to repeal, forever, the Medicare SGR, passing the Burgess bill without amendment, on a bipartisan vote of 92–8. With only hours to go before the scheduled 21.2% cut took effect, the President signed the bill, now Public Law (PL) 114-10, on April 16. The President noted that he was “proud to sign the bill into law.” ACOG is proud to have been such an important part of this landmark moment.
SGR: the perennial nemesis of physicians
The SGR has wreaked havoc on medicine and patient care for 15 years or more. Approximately 30,000 ObGyns participate in Medicare, and many private health insurers use Medicare payment policies, as does TriCare, the nation’s health care coverage for military members and their families. The SGR’s effect was felt widely across medicine, making it nearly impossible for physician practices to invest in health information technology and other patient safety advances, or even to plan for the next year or continue accepting Medicare patients.
When it was introduced last year, HR 2 was supported by more than 600 national and state medical societies and specialty organizations, plus patient and provider organizations, policy think tanks, and advocacy groups across the political spectrum.
ACOG Fellows petitioned their members of Congress with incredible passion, perseverance, and commitment to put an end to the SGR wrecking ball. Hundreds flew into Washington, DC, sent thousands of emails, made phone calls, wrote letters, and personally lobbied at home and in the halls of Congress.
Special kudos, too, to our champions in Congress, and there are many, led by ACOG Fellows and US Reps. Dr. Burgess and Phil Roe, MD (R-TN). Burgess wrote the House bill and, together with Roe, pushed nonstop to get this bill over the finish line. It wouldn’t have happened without them.
ACOG worked tirelessly on its own and in coalition with the American Medical Association, surgical groups, and many other partners. We were able to win important provisions in the statute that we anticipate will greatly help ObGyns successfully transition to this new payment system.
PL114-10 replaces the SGR with a new payment system intended to promote care coordination and quality improvement and lead to better health for our nation’s seniors. Congress developed this new payment plan with the physician community, rather than imposing it on us. That’s why throughout the statute, we see repeated requirements that the Secretary of Health and Human Services must develop quality measures, alternative payment models, and a host of key aspects with input from and in consultation with physicians and the relevant medical specialties, ensuring that physicians retain their preeminent roles in these areas. Funding is provided for quality measure development at $15 million per year from 2015 to 2019.
This law will likely change physician practices more than the ACA ever will, and Congress agreed that physicians should be integral to its development to ensure that they can continue to thrive and provide high-quality care and access for their patients.
Let’s take a closer look at the new Medicare payment system—especially what it will mean for your practice.
What the new law does
Important provisions
- MACRA retains the fee-for-service payment model, now called the Merit-based Incentive Payment System, or MIPS. Physician participation in the Advanced Payment Models (APMs) is entirely voluntary. But physicians who participate in APMs and who score better each year will earn more.
- All physician types are treated equally. Congress didn’t pick specialty winners and losers.
- The new payment system rewards physicians for continuous improvement. You can determine how financially well you do.
- Beginning in 2019, Medicare physician payments will reflect each individual physician’s performance, based on a range of measures developed by the relevant medical specialty that will give individuals options that best reflect their practices.
- Individual physicians will receive confidential quarterly feedback on their performance.
- Technical support is provided for smaller practices, funded at $20 million per year from 2016 to 2020, to help them transition to MIPS and APMs. And physicians in small practices can opt to join a “virtual MIPS group,” associating with other practices or hospitals in the same geographic region or by specialty types.
- The law protects physicians from liability from federal or state standards of care. No health care guideline or other standard developed under federal or state requirements associated with this law may be used as a standard of care or duty of care owed by a health care professional to a patient in a medical liability lawsuit.
MACRA stabilizes the Medicare payment system by permanently repealing the SGR and scheduling payments into the future:
- through June 2015: Stable payments with no cuts
- July 2015–2019: 0.5% annual payment increases to all Medicare physicians
- 2020–2025: No automatic annual payment changes but opportunities for payment increases based on individual performance
- 2026 and beyond: 0.75% annual payment increases for qualifying APMs, 0.25% for MIPS providers, with opportunities in both systems for higher payments based on individual performance.
Top ACOG wins
Among the most meaningful accomplishments achieved by ACOG in its work to repeal the sustainable growth rate are:
- Reliable payment increases for the first 5 years. The law ensures a period of stability with modest Medicare payment in-
creases for 5 years and no cuts, with opportunity for payment increases for the next 5 years. This 5-year period gives physicians time to get ready for the new payment systems. - Protection for low-Medicare–volume physician practices. ObGyns and other physicians with a small Medicare patient population are exempt from many program requirements and penalties.
- Stops the Centers for Medicare and Medicaid Services (CMS) policy on global surgical codes, reinstating 10-day and 90-day global payment bundles for surgical services. This directly helps ObGyn subspecialists, including urogynecologists and gynecologic oncologists.
- Physician liability protections. The law ensures that federal quality measurements cannot be used to imply medical negligence and generate lawsuits.
- Protection for ultrasound. There are no cuts to ultrasound reimbursement.
- An end, in 2018, to penalties related to electronic health record (EHR) meaningful use, Physician Quality Reporting Systems, and the use of the value-based modifier.
- APM bonus payments. Bonus eligibility for Alternative Payment Model (APM) participation is based on patient volume, not just revenue, to make it easier for ObGyns to qualify.
- 2-year extension of the Children’s Health Insurance Program (CHIP), which provides comprehensive coverage to 8 million children, adolescents, and pregnant women across the country.
- Quality-measure development. The law helps professional organizations, such as ACOG, develop quality measures for the Merit-Based Incentive Payment System (MIPS) rather than allow these measures to be developed by a federal agency, ensuring that this new program works for physicians and our patients.
Two payment system options reward continuous quality improvement
Option 1: MIPS. MACRA consolidates and expands pay-for-performance incentives within the old SGR fee-for-service system, creating the new MIPS. Under MIPS, the Physician Quality Reporting System (PQRS), electronic health record (EHR) meaningful use incentive program, and physician value-based modifiers (VBMs) become a single program. In 2019, a physician’s individual score on these measures will be used to adjust his or her Medicare payments, and the penalties previously associated with these programs come to an end.
MACRA creates 4 categories of measures that are weighted to calculate an individual physician’s MIPS score:
- Quality (50% of total adjustment in 2019, shrinking to 30% of total adjustment in 2021). Quality measures currently in use in the PQRS, VBM, and EHR meaningful use programs will continue to be used. The Secretary of Health and Human Services must fund and work with specialty societies to develop any additional measures, and measures utilized in clinical data registries can be used for this category as well. Measures will be updated annually, and ACOG and other specialties can submit measures directly for approval, rather than rely on an outside entity.
- Resource use (10% of total adjustment in 2019, growing to 30% of total adjustment by 2021). Resource use measures are risk-adjusted and include those already used in the VBM program; others must be developed with physicians, reflecting both the physician’s role in treating the patient (eg, primary or specialty care) and the type of treatment (eg, chronic or acute).
- EHR use (25% of total adjustment). Current meaningful use systems will qualify for this category. The law also requires EHR interoperability by 2018 and prohibits the blocking of information sharing between EHR vendors.
- Clinical improvement (15% of total adjustment). This is a new component of physician measurement, intended to give physicians credit for working to improve their practices and help them participate in APMs, which have higher reimbursement potential. This menu of qualifying activities—including 24-hour availability, safety, and patient satisfaction—must be developed with physicians and must be attainable by all specialties and practice types, including small practices and those in rural and underserved areas. Maintenance of certification can be used to qual-ify for a high score.
Physicians will only be assessed on the categories, measures, and activities that apply to them. A physician’s composite score (0–100) will be compared with a performance threshold that reflects all physicians. Those who score above the threshold will receive increased payments; those who score below the threshold will receive reduced payments. Physicians will know these thresholds in advance and will know the score they must reach to avoid penalties and win higher reimbursements in each performance period.
As physicians as a whole improve their performance, the threshold will move with them. So each year, physicians will have the incentive to keep improving their quality, resource use, clinical improvement, and EHR use. A physician’s payment adjustment in one year will not affect his or her payment adjustment in the next year.
The range of potential payment adjustments based on MIPS performance measures increases each year through 2022. Providers who have high scores are rewarded with a 4% increase in 2019. By 2022, the reward is 9%. The program is budget-neutral, so total positive adjustments across all providers will equal total negative adjustments across all providers to poor performers. Separate funds are set aside to reward the highest performers, who will earn bonuses of up to 10% of their fee-for-service payment rate from 2019 through 2024, as well as to help low performers improve and qualify for increased payments from 2016 through 2020.
Help for physicians includes:
- flexibility to participate in a way that best reflects their practice, using risk-adjusted clinical outcome measures
- option to participate in a virtual MIPS group rather than go it alone
- technical assistance to practices with 15 or fewer professionals, $20 million annually from 2016 through 2020, with preference to practices with low MIPS scores and those in rural and underserved areas
- quarterly confidential feedback on performance in the quality and resource use categories
- advance notification to each physician of the score needed to reach higher payment levels
- exclusion from MIPS of physicians who treat few Medicare patients, as well as those who receive a significant portion of their revenues from APMs.
Option 2: APMs. Physicians can earn higher fees by opting out of MIPS fee for service and participating in APMs. The law defines qualifying APMs as those that require participating providers to take on “more than nominal” financial risk, report quality measures, and use certified EHR technology.
APMs will cover multiple services, show that they can limit the growth of spending, and use performance-based methods of compensation. These and other provisions will likely continue the trend away from physicians practicing in solo or small-group fee-for-service practices into risk-based multispecialty settings that are subject to increased management and oversight.
From 2019 to 2024, qualified APM physicians will receive a 5% annual lump sum bonus based on their prior year’s physician fee-schedule payments plus shared savings from participation. This bonus is based on patient volume, not just revenue, to make it easier for ObGyns to qualify. To make the bonus widely available, the Secretary of Health and Human Services must test APMs designed for specific specialties and physicians in small practices. As in MIPS, top APM performers will also receive an additional bonus.
To qualify, physicians must meet increasing thresholds for the percentage of their revenue that they receive through APMs. Those who are below but near the required level of APM revenue can be exempted from MIPS adjustments.
- 2019–2020: 25% of Medicare revenue must be received through APMs.
- 2021–2022: 50% of Medicare revenue or 50% of all-payer revenue along with 25% of Medicare revenue must be received through APMs.
- 2023 and beyond: 75% of Medicare revenue or 75% of all-payer revenue along with 25% of Medicare revenue must be received through APMs.
Who pays the bill?
Medicare beneficiaries pay more
The new law increases the percentage of Medicare Parts B and D premiums that high-income beneficiaries must pay beginning in 2018:
- Single seniors reporting income of more than $133,500 and married couples with income of more than $267,000 will see their share of premiums rise from 50% to 65%.
- Single seniors reporting income above $160,000 and married couples with income above $320,000 will see their premium share rise from 65% to 80%.
This change will affect about 2% of Medicare beneficiaries; half of all Medicare beneficiaries currently have annual incomes below $26,000.1
Medigap “first-dollar coverage” will end
Many Medigap plans on the market today provide “first-dollar coverage” for beneficiaries, which means that the plans pay the deductibles and copayments so that the beneficiaries have no out-of-pocket costs. Beginning in 2020, Medigap plans will only be available to cover costs above the Medicare Part B deductible, currently $147 per year, for new Medigap enrollees. Many lawmakers thought it was important for Medicare beneficiaries to have “skin in the game.”
The law cuts payments for some providers
To partially offset the cost of repealing the SGR, MACRA cuts Medicare payments to hospitals and postacute providers. It:
- delays Disproportionate Share Hospital (DSH) cuts scheduled to begin in 2017 by a year and extends them through 2025
- requires an increase in payments to hospitals scheduled for 2018 to instead be phased in over 6 years
- limits the 2018 payment update for post-acute providers to 1%.
The law extends many programs
These programs are vital to support the future ObGyn workforce and access to health care. Among these programs are:
- a halt to the Centers for Medicare and Medicaid Services (CMS) policy on global surgical codes. The law reinstates 10-day and 90-day global payment bundles for surgical services. This directly helps ObGyn subspecialists, such as urogynecologists and gynecologic oncologists.
- renewal of the Children’s Health Insurance Program (CHIP), which provides comprehensive coverage to 8 million children, adolescents, and pregnant women across the country
- establishment of a Medicaid/CHIP Pediatric Quality Measures Program, supporting the development and physician adoption of quality measures, including for prenatal and preconception care
- funding for the Maternal, Infant, and Early Childhood Home Visiting Program, helping at-risk pregnant women and their families to promote healthy births and early childhood development
- funding for community health centers, an important source of care for 13 million women and girls in all 50 states and the District of Columbia
- funding for the National Health Service Corps, bringing ObGyns and other primary care providers to underserved rural and urban areas through scholarships and loan repayment programs
- funding for the Teaching Health Center Graduate Medical Education Payment Program, enhancing training for ObGyns and other primary care providers in community-based settings
- extending the Medicare Geographic Practice Cost Index floor, helping ensure access to care for women in rural areas
- extending the Personal Responsibility Education Program to help prevent teen pregnancies and sexually transmitted infections.
Next steps
It’s very important that ObGyns and other physicians use these early years to understand and get ready for the new payment systems. ACOG is developing educational material for our members, and will work closely with our colleague medical organizations and the Department of Health and Human Services to develop key aspects of the law and ensure that it is properly implemented to work for physicians and patients.
Share your thoughts on this article! Send your Letter to the Editor to [email protected]. Please include your name and the city and state in which you practice.
Reference
1. Aaron HJ. Three cheers for log-rolling: The demise of the SGR. Brookings Health360. http://www.brookings.edu/blogs/health360/posts/2015/04/22-medicare-sgr-repeal-doc-fix-aaron. Published April 22, 2015. Accessed May 12, 2015.
Reference
1. Aaron HJ. Three cheers for log-rolling: The demise of the SGR. Brookings Health360. http://www.brookings.edu/blogs/health360/posts/2015/04/22-medicare-sgr-repeal-doc-fix-aaron. Published April 22, 2015. Accessed May 12, 2015.
Why CMS’ plan to unbundle global surgery periods should be scrapped
Sometimes it’s difficult to figure out which way is forward. For the past few years, private insurers and the federal government (through the Medicare program) have been experimenting with and putting in place different ways of paying physicians for the care they provide. Many alternatives are designed to increase value for our nation’s health care dollars and improve quality of care, often through care coordination. Most involve different ways of “bundling” care—paying a single sum for a patient’s episode of care rather than separate payments each time a physician encounters a patient.
For more than 20 years, Medicare has bundled most surgeries, paying 1 sum to the physician and requiring only 1 copayment from the beneficiary patient. In this way, when a patient needs surgery, Medicare pays the surgeon 1 payment for preparation the day before surgery, for the surgery itself, and for either 10 or 90 days of follow-up care, depending on the specific procedure involved (TABLE 1). Similarly the patient has had 1 copay for the entire episode of care. This bundling is called global surgical codes, and it applies to coding, billing, and reimbursement.
Table 1: CMS description of 10- and 90-day global codes Minor procedures: 10-day postoperative period
Major procedures: 90-day postoperative period
|
This approach may change soon—and not for the better. In this article, I describe how the federal Centers for Medicare and Medicaid Services (CMS) plan to eliminate global surgery bundling, as well as the efforts under way by the American Congress of Obstetricians and Gynecologists (ACOG) and other organizations to stop the proposed change.
The CMS plan to eliminate surgical bundling
In a significant twist from the trend toward bundling and care coordination, CMS finalized its proposed policy in its 2015 Medicare Physician Fee Schedule final rule to transition all 10- and 90-day global surgical codes to 0-day global surgical codes by 2017 and 2018, respectively. Beginning in 2017 for 10-day global codes and 2018 for 90-day codes, physicians will be paid separately for the day of surgery and for evaluation and management (E&M) provided on the day before and any days after. Patients will have copays for each physician intervention.
CMS has decided to move forward with this change despite overwhelming concern and opposition on the part of both patients and physicians. This change would affect more than 4,200 services on the Medicare Physician Fee Schedule—well over one-third of the 9,900 current procedural terminology (CPT) codes.
The new codes and increased paperwork and billing are daunting, and would result in an estimated 63 million additional claims per year to account for postsurgical E&M services. The cost to CMS alone for this huge new mountain of claims may be as high as $95 million per year. Moreover, under the new system, patients may not return for the full range of follow-up care needed if they get billed for every visit, possibly resulting in poorer outcomes.
CMS’ justification for unbundling
CMS argues that this change is needed because many surgeons are failing to provide as much care (as many E&M follow-up visits) as they’re paid to deliver under the 10- and 90-day codes. As evidence, CMS points to 3 reports published by the Department of Health and Human Services Office of Inspector General:
- An April 2009 report from the field of ocular surgery found that physicians provided fewer E&M services than were included in 201 of 300 examined global surgery fees. The cost of these undelivered services was approximately $97.6 million.1
- A May 2012 report from the field of cardiac surgery found that physicians provided fewer E&M services than were included in 132 global surgery fees of the 300 surgeries examined. The cost: $14.6 million.2
- Another May 2012 report, this one from the field of musculoskeletal surgery, found that physicians provided fewer E&M services than were included in 165 global surgery fees of the 300 surgeries examined. The cost for these undelivered services: $49 million.3
Based largely on these reports, CMS has determined that it cannot verify the number of visits, level of service, and relative costs of the services included in a global package, in large part because the current valuation methodology relies on survey data estimating the resources used in a typical case, instead of on actual data.
In each of these reports, the Inspector General also found smaller numbers of cases where surgeons provided more E&M care than was covered under the global payment. In each report, the Inspector General suggests that CMS should do more to identify and correctly value misvalued codes. ACOG Vice President for Health Policy Barbara Levy, MD, who is also chair of the Relative Value Scale Update Committee, or RUC, makes a compelling case that the RUC has identified and corrected many global surgical codes since these reports were issued and is in the process of revising more codes. She also argues that the RUC is the appropriate place to address these issues.
Policy analysis finds that total RVUs would decline
CMS has indicated that it intends to use a formula for converting the 10- and 90-day global services into 0-day services by simply reducing the work relative value units (RVUs) for the service by the number of work RVUs in the postoperative visits. The American College of Surgeons asked Health Policy Alternatives (HPA), a consulting firm, to analyze the CMS decision. HPA found that “systematically convert[ing] all global surgical codes to 0-day global codes by backing out of the bundled E&M services reduces the total RVUs and each component (work, practice expense, and malpractice) for surgical codes. Specifically, for surgical specialties, the impact of this transition on all Medicare reimbursed codes results in the following reductions:
- overall payment decrease of 1.8%
- payment decrease of 0.8% for work
- payment decrease of 2% for practice expense
- payment decrease of 9.2% for malpractice.
This modeling resulted in a total overall payment increase of 0.1% for generalists and a payment increase of 0.3% for medical specialists.”4
HPA’s findings related to the malpractice component are especially interesting for the ObGyn specialty. “Model results demonstrate that this policy results in significant redistribution of malpractice away from the main specialty provider of the surgical procedure into the entire group of providers (surgical and nonsurgical),” notes the HPA report.4 “Most impacted will be specialties with higher malpractice expenses, such as neurosurgeons and cardiac surgeons.”4 We could add ObGyns to that list.
ACOG cites numerous objections
ACOG is deeply involved in opposing this new CMS policy and preventing it from ever going into effect, working on our own, in coalition with our medical organization colleagues and patient organizations, and working closely with the US Congress.
ACOG and 28 other medical organizations, including the American Medical Association (AMA), summarized our opposition in a letter to US House and Senate Democratic and Republican leaders in December 2014, saying that this new policy:
Detracts from quality of care, impedes patient access, and complicates patient copays
- Patients will be responsible for copays on each service, including follow-up visits. This could considerably increase the administrative burden on patients. Worse, it could discourage them from returning for needed follow-up care.
- In the hospital critical care setting, the global payment structure allows the surgeon to oversee and coordinate care related to the patient’s recovery. Without the global structure, care will be fragmented and providers may compete to see patients and bill for the care they provide.
Undermines Medicare reform initiatives
- CMS initiatives for payment are all moving toward larger bundled payments. Deconstruction of the current payment structure for physicians is counterintuitive to the end goal of providing more comprehensive and coordinated care for the patient.
- Current bipartisan, bicameral legislation to repeal and replace the flawed sustainable growth rate formula calls for “a period of stability” in physician pay to allow physicians to transition to alternative payment models. The proposal to unbundle global surgical periods will add new complexities to an already flawed system and stymie progress.
Increases administrative burden
- The administrative burden on surgical practices and CMS (and its contractors) will be significant. Eliminating the global package will result in 63 million additional claims per year, adding unnecessary costs to our health care system.
Obstructs clinical registry data collection and quality improvement
- Surgeons will have less ability to collect information on patient outcomes in clinical registries, undermining many of the most meaningful quality improvement initiatives.5
Additional ACOG concerns
ACOG added these concerns to our opposition to the CMS plan:
- The change will not accurately account for physician work, practice expense, and malpractice risk for services performed.
- Thousands of new codes and/or values will need to be created for postoperative care because the supplies and equipment needed for postoperative care are not included in the E&M codes that will be used to report in-hospital and outpatient postoperative services (TABLE 2).
- Liability costs of a specific service should be derived from those of the performing specialties. Under the CMS plan, the liability costs associated with postoperative work would be removed from the primary service and artificially diluted by the wide mix of specialties performing all types of E&M services. Without global periods, a one-size-fits-all approach to professional liability insurance will be unsustainable and result in great disparities between the actual and realized malpractice costs for many physician specialties.
Table 2: Other postoperative care services currently bundled into global surgical packages
|
We have important allies
The American Association of Retired Persons (AARP) joined us in September 2014, when it formally asked CMS to abandon this new policy. In a letter to CMS Administrator Marilyn Tavenner, AARP noted that, “from a beneficiary perspective, we are concerned that this unbundling could produce considerable confusion and cause beneficiaries to receive multiple explanations of Medicare benefits (and incur separate cost-sharing obligations) related to a single surgical procedure….[G]iven the obvious methodological uncertainty and complexity involved in determining appropriate values for a very large number of ‘new’ 0-day global services, and the likely confusion surrounding the resulting increase in Medicare claims, AARP has serious doubts regarding the benefit of this unbundling proposal. We suggest [that] CMS consider other available alternatives, including the re-valuation of global services whose current values are believed to be incorrect.”6
Also in September, 27 Republican and Democratic members of Congress wrote a strong letter to CMS echoing the medical community’s concerns. The letter and many months of congressional leadership have been spearheaded by Representatives Larry Bucshon, MD, and Ami Bera, MD—demonstrating the value of having physicians in elective office. Other physician members of Congress who have provided outstanding leadership include ACOG Fellows and Representatives Michael Burgess, MD, and Phil Roe, MD, as well as Representatives Tom Price, MD; Andy Harris, MD; Joe Heck, DO; Charles Boustany, MD; Raul Ruiz, MD; and Dan Benishek, MD.
This important group of physician leaders, ACOG, AARP, and the surgical community are hard at work to derail or significantly delay what most physicians and policy analysts see as a very bad idea.
Congress takes action
In April 2015, Congress passed HR2, the Medicare Access and CHIP Reauthorization Bill, which most notably repealed the Medicare Sustainable Growth Rate formula. Included in this law is an important provision to halt implementation of CMS’ plan to unbundle all 10- and 90-day global codes.
Section 523 of that law requires CMS to periodically collect information on the services that surgeons furnish during these global periods, beginning no later than 2017, and use that information to ensure that the bundled payment amounts for surgical services are accurate. The Secretary of Health and Human Services is given the authority to withhold a portion of payment for services with a 10- or 90-day global period to incentivize the reporting of information. The Secretary can stop collecting this information from surgeons once the needed data can be obtained through other mechanisms, such as clinical data registries and electronic medical records.
Congressmen Bucshon and Bera championed this provision, along with nearly all physician members of the US House of Representatives. This change ensures a thorough, data-driven approach to appropriately valuing surgical services, including those provided by ObGyn subspecialists, such as urogynecologists and gynecologic oncologists.
Acknowledgment
The author thanks Barbara Levy, MD, ACOG Vice President for Health Policy, for her helpful comments.
Share your thoughts! Send your Letter to the Editor to [email protected]. Please include your name and the city and state in which you practice.
1. Department of Health and Human Services, Office of Inspector General. Nationwide Review of Evaluation and Management Services Included in Eye and Ocular Adnexa Global Surgery Fees for Calendar Year 2005. A-05-07-00077. Washington, DC: Department of Health and Human Services; April 2009.
2. Department of Health and Human Services, Office of Inspector General. Cardiovascular Global Surgery Fees Often Did Not Reflect the Number of Evaluation and Management Services Provided. A-05-09-00054. Washington, DC: Department of Health and Human Services; May 2012.
3. Department of Health and Human Services, Office of Inspector General. Musculoskeletal Global Surgery Fees Often Did Not Reflect the Number of Evaluation and Management Services Provided. A-05-09-00053. Washington, DC: Department of Health and Human Services; May 2012.
4. Summary of Initial Modeling Results of the CMS Policy to Transition 10- and 90-Day Global Surgery Codes to 0-Day Global Surgery Codes. Washington, DC: Health Policy Alternatives; January 9, 2015.
5. American Congress of Obstetricians and Gynecologists joint letter to Congress; December 2, 2014.
6. American Association of Retired Persons letter to Marilyn Tavenner, Administrator, Centers for Medicare and Medicaid Services; September 2, 2014.
Sometimes it’s difficult to figure out which way is forward. For the past few years, private insurers and the federal government (through the Medicare program) have been experimenting with and putting in place different ways of paying physicians for the care they provide. Many alternatives are designed to increase value for our nation’s health care dollars and improve quality of care, often through care coordination. Most involve different ways of “bundling” care—paying a single sum for a patient’s episode of care rather than separate payments each time a physician encounters a patient.
For more than 20 years, Medicare has bundled most surgeries, paying 1 sum to the physician and requiring only 1 copayment from the beneficiary patient. In this way, when a patient needs surgery, Medicare pays the surgeon 1 payment for preparation the day before surgery, for the surgery itself, and for either 10 or 90 days of follow-up care, depending on the specific procedure involved (TABLE 1). Similarly the patient has had 1 copay for the entire episode of care. This bundling is called global surgical codes, and it applies to coding, billing, and reimbursement.
Table 1: CMS description of 10- and 90-day global codes Minor procedures: 10-day postoperative period
Major procedures: 90-day postoperative period
|
This approach may change soon—and not for the better. In this article, I describe how the federal Centers for Medicare and Medicaid Services (CMS) plan to eliminate global surgery bundling, as well as the efforts under way by the American Congress of Obstetricians and Gynecologists (ACOG) and other organizations to stop the proposed change.
The CMS plan to eliminate surgical bundling
In a significant twist from the trend toward bundling and care coordination, CMS finalized its proposed policy in its 2015 Medicare Physician Fee Schedule final rule to transition all 10- and 90-day global surgical codes to 0-day global surgical codes by 2017 and 2018, respectively. Beginning in 2017 for 10-day global codes and 2018 for 90-day codes, physicians will be paid separately for the day of surgery and for evaluation and management (E&M) provided on the day before and any days after. Patients will have copays for each physician intervention.
CMS has decided to move forward with this change despite overwhelming concern and opposition on the part of both patients and physicians. This change would affect more than 4,200 services on the Medicare Physician Fee Schedule—well over one-third of the 9,900 current procedural terminology (CPT) codes.
The new codes and increased paperwork and billing are daunting, and would result in an estimated 63 million additional claims per year to account for postsurgical E&M services. The cost to CMS alone for this huge new mountain of claims may be as high as $95 million per year. Moreover, under the new system, patients may not return for the full range of follow-up care needed if they get billed for every visit, possibly resulting in poorer outcomes.
CMS’ justification for unbundling
CMS argues that this change is needed because many surgeons are failing to provide as much care (as many E&M follow-up visits) as they’re paid to deliver under the 10- and 90-day codes. As evidence, CMS points to 3 reports published by the Department of Health and Human Services Office of Inspector General:
- An April 2009 report from the field of ocular surgery found that physicians provided fewer E&M services than were included in 201 of 300 examined global surgery fees. The cost of these undelivered services was approximately $97.6 million.1
- A May 2012 report from the field of cardiac surgery found that physicians provided fewer E&M services than were included in 132 global surgery fees of the 300 surgeries examined. The cost: $14.6 million.2
- Another May 2012 report, this one from the field of musculoskeletal surgery, found that physicians provided fewer E&M services than were included in 165 global surgery fees of the 300 surgeries examined. The cost for these undelivered services: $49 million.3
Based largely on these reports, CMS has determined that it cannot verify the number of visits, level of service, and relative costs of the services included in a global package, in large part because the current valuation methodology relies on survey data estimating the resources used in a typical case, instead of on actual data.
In each of these reports, the Inspector General also found smaller numbers of cases where surgeons provided more E&M care than was covered under the global payment. In each report, the Inspector General suggests that CMS should do more to identify and correctly value misvalued codes. ACOG Vice President for Health Policy Barbara Levy, MD, who is also chair of the Relative Value Scale Update Committee, or RUC, makes a compelling case that the RUC has identified and corrected many global surgical codes since these reports were issued and is in the process of revising more codes. She also argues that the RUC is the appropriate place to address these issues.
Policy analysis finds that total RVUs would decline
CMS has indicated that it intends to use a formula for converting the 10- and 90-day global services into 0-day services by simply reducing the work relative value units (RVUs) for the service by the number of work RVUs in the postoperative visits. The American College of Surgeons asked Health Policy Alternatives (HPA), a consulting firm, to analyze the CMS decision. HPA found that “systematically convert[ing] all global surgical codes to 0-day global codes by backing out of the bundled E&M services reduces the total RVUs and each component (work, practice expense, and malpractice) for surgical codes. Specifically, for surgical specialties, the impact of this transition on all Medicare reimbursed codes results in the following reductions:
- overall payment decrease of 1.8%
- payment decrease of 0.8% for work
- payment decrease of 2% for practice expense
- payment decrease of 9.2% for malpractice.
This modeling resulted in a total overall payment increase of 0.1% for generalists and a payment increase of 0.3% for medical specialists.”4
HPA’s findings related to the malpractice component are especially interesting for the ObGyn specialty. “Model results demonstrate that this policy results in significant redistribution of malpractice away from the main specialty provider of the surgical procedure into the entire group of providers (surgical and nonsurgical),” notes the HPA report.4 “Most impacted will be specialties with higher malpractice expenses, such as neurosurgeons and cardiac surgeons.”4 We could add ObGyns to that list.
ACOG cites numerous objections
ACOG is deeply involved in opposing this new CMS policy and preventing it from ever going into effect, working on our own, in coalition with our medical organization colleagues and patient organizations, and working closely with the US Congress.
ACOG and 28 other medical organizations, including the American Medical Association (AMA), summarized our opposition in a letter to US House and Senate Democratic and Republican leaders in December 2014, saying that this new policy:
Detracts from quality of care, impedes patient access, and complicates patient copays
- Patients will be responsible for copays on each service, including follow-up visits. This could considerably increase the administrative burden on patients. Worse, it could discourage them from returning for needed follow-up care.
- In the hospital critical care setting, the global payment structure allows the surgeon to oversee and coordinate care related to the patient’s recovery. Without the global structure, care will be fragmented and providers may compete to see patients and bill for the care they provide.
Undermines Medicare reform initiatives
- CMS initiatives for payment are all moving toward larger bundled payments. Deconstruction of the current payment structure for physicians is counterintuitive to the end goal of providing more comprehensive and coordinated care for the patient.
- Current bipartisan, bicameral legislation to repeal and replace the flawed sustainable growth rate formula calls for “a period of stability” in physician pay to allow physicians to transition to alternative payment models. The proposal to unbundle global surgical periods will add new complexities to an already flawed system and stymie progress.
Increases administrative burden
- The administrative burden on surgical practices and CMS (and its contractors) will be significant. Eliminating the global package will result in 63 million additional claims per year, adding unnecessary costs to our health care system.
Obstructs clinical registry data collection and quality improvement
- Surgeons will have less ability to collect information on patient outcomes in clinical registries, undermining many of the most meaningful quality improvement initiatives.5
Additional ACOG concerns
ACOG added these concerns to our opposition to the CMS plan:
- The change will not accurately account for physician work, practice expense, and malpractice risk for services performed.
- Thousands of new codes and/or values will need to be created for postoperative care because the supplies and equipment needed for postoperative care are not included in the E&M codes that will be used to report in-hospital and outpatient postoperative services (TABLE 2).
- Liability costs of a specific service should be derived from those of the performing specialties. Under the CMS plan, the liability costs associated with postoperative work would be removed from the primary service and artificially diluted by the wide mix of specialties performing all types of E&M services. Without global periods, a one-size-fits-all approach to professional liability insurance will be unsustainable and result in great disparities between the actual and realized malpractice costs for many physician specialties.
Table 2: Other postoperative care services currently bundled into global surgical packages
|
We have important allies
The American Association of Retired Persons (AARP) joined us in September 2014, when it formally asked CMS to abandon this new policy. In a letter to CMS Administrator Marilyn Tavenner, AARP noted that, “from a beneficiary perspective, we are concerned that this unbundling could produce considerable confusion and cause beneficiaries to receive multiple explanations of Medicare benefits (and incur separate cost-sharing obligations) related to a single surgical procedure….[G]iven the obvious methodological uncertainty and complexity involved in determining appropriate values for a very large number of ‘new’ 0-day global services, and the likely confusion surrounding the resulting increase in Medicare claims, AARP has serious doubts regarding the benefit of this unbundling proposal. We suggest [that] CMS consider other available alternatives, including the re-valuation of global services whose current values are believed to be incorrect.”6
Also in September, 27 Republican and Democratic members of Congress wrote a strong letter to CMS echoing the medical community’s concerns. The letter and many months of congressional leadership have been spearheaded by Representatives Larry Bucshon, MD, and Ami Bera, MD—demonstrating the value of having physicians in elective office. Other physician members of Congress who have provided outstanding leadership include ACOG Fellows and Representatives Michael Burgess, MD, and Phil Roe, MD, as well as Representatives Tom Price, MD; Andy Harris, MD; Joe Heck, DO; Charles Boustany, MD; Raul Ruiz, MD; and Dan Benishek, MD.
This important group of physician leaders, ACOG, AARP, and the surgical community are hard at work to derail or significantly delay what most physicians and policy analysts see as a very bad idea.
Congress takes action
In April 2015, Congress passed HR2, the Medicare Access and CHIP Reauthorization Bill, which most notably repealed the Medicare Sustainable Growth Rate formula. Included in this law is an important provision to halt implementation of CMS’ plan to unbundle all 10- and 90-day global codes.
Section 523 of that law requires CMS to periodically collect information on the services that surgeons furnish during these global periods, beginning no later than 2017, and use that information to ensure that the bundled payment amounts for surgical services are accurate. The Secretary of Health and Human Services is given the authority to withhold a portion of payment for services with a 10- or 90-day global period to incentivize the reporting of information. The Secretary can stop collecting this information from surgeons once the needed data can be obtained through other mechanisms, such as clinical data registries and electronic medical records.
Congressmen Bucshon and Bera championed this provision, along with nearly all physician members of the US House of Representatives. This change ensures a thorough, data-driven approach to appropriately valuing surgical services, including those provided by ObGyn subspecialists, such as urogynecologists and gynecologic oncologists.
Acknowledgment
The author thanks Barbara Levy, MD, ACOG Vice President for Health Policy, for her helpful comments.
Share your thoughts! Send your Letter to the Editor to [email protected]. Please include your name and the city and state in which you practice.
Sometimes it’s difficult to figure out which way is forward. For the past few years, private insurers and the federal government (through the Medicare program) have been experimenting with and putting in place different ways of paying physicians for the care they provide. Many alternatives are designed to increase value for our nation’s health care dollars and improve quality of care, often through care coordination. Most involve different ways of “bundling” care—paying a single sum for a patient’s episode of care rather than separate payments each time a physician encounters a patient.
For more than 20 years, Medicare has bundled most surgeries, paying 1 sum to the physician and requiring only 1 copayment from the beneficiary patient. In this way, when a patient needs surgery, Medicare pays the surgeon 1 payment for preparation the day before surgery, for the surgery itself, and for either 10 or 90 days of follow-up care, depending on the specific procedure involved (TABLE 1). Similarly the patient has had 1 copay for the entire episode of care. This bundling is called global surgical codes, and it applies to coding, billing, and reimbursement.
Table 1: CMS description of 10- and 90-day global codes Minor procedures: 10-day postoperative period
Major procedures: 90-day postoperative period
|
This approach may change soon—and not for the better. In this article, I describe how the federal Centers for Medicare and Medicaid Services (CMS) plan to eliminate global surgery bundling, as well as the efforts under way by the American Congress of Obstetricians and Gynecologists (ACOG) and other organizations to stop the proposed change.
The CMS plan to eliminate surgical bundling
In a significant twist from the trend toward bundling and care coordination, CMS finalized its proposed policy in its 2015 Medicare Physician Fee Schedule final rule to transition all 10- and 90-day global surgical codes to 0-day global surgical codes by 2017 and 2018, respectively. Beginning in 2017 for 10-day global codes and 2018 for 90-day codes, physicians will be paid separately for the day of surgery and for evaluation and management (E&M) provided on the day before and any days after. Patients will have copays for each physician intervention.
CMS has decided to move forward with this change despite overwhelming concern and opposition on the part of both patients and physicians. This change would affect more than 4,200 services on the Medicare Physician Fee Schedule—well over one-third of the 9,900 current procedural terminology (CPT) codes.
The new codes and increased paperwork and billing are daunting, and would result in an estimated 63 million additional claims per year to account for postsurgical E&M services. The cost to CMS alone for this huge new mountain of claims may be as high as $95 million per year. Moreover, under the new system, patients may not return for the full range of follow-up care needed if they get billed for every visit, possibly resulting in poorer outcomes.
CMS’ justification for unbundling
CMS argues that this change is needed because many surgeons are failing to provide as much care (as many E&M follow-up visits) as they’re paid to deliver under the 10- and 90-day codes. As evidence, CMS points to 3 reports published by the Department of Health and Human Services Office of Inspector General:
- An April 2009 report from the field of ocular surgery found that physicians provided fewer E&M services than were included in 201 of 300 examined global surgery fees. The cost of these undelivered services was approximately $97.6 million.1
- A May 2012 report from the field of cardiac surgery found that physicians provided fewer E&M services than were included in 132 global surgery fees of the 300 surgeries examined. The cost: $14.6 million.2
- Another May 2012 report, this one from the field of musculoskeletal surgery, found that physicians provided fewer E&M services than were included in 165 global surgery fees of the 300 surgeries examined. The cost for these undelivered services: $49 million.3
Based largely on these reports, CMS has determined that it cannot verify the number of visits, level of service, and relative costs of the services included in a global package, in large part because the current valuation methodology relies on survey data estimating the resources used in a typical case, instead of on actual data.
In each of these reports, the Inspector General also found smaller numbers of cases where surgeons provided more E&M care than was covered under the global payment. In each report, the Inspector General suggests that CMS should do more to identify and correctly value misvalued codes. ACOG Vice President for Health Policy Barbara Levy, MD, who is also chair of the Relative Value Scale Update Committee, or RUC, makes a compelling case that the RUC has identified and corrected many global surgical codes since these reports were issued and is in the process of revising more codes. She also argues that the RUC is the appropriate place to address these issues.
Policy analysis finds that total RVUs would decline
CMS has indicated that it intends to use a formula for converting the 10- and 90-day global services into 0-day services by simply reducing the work relative value units (RVUs) for the service by the number of work RVUs in the postoperative visits. The American College of Surgeons asked Health Policy Alternatives (HPA), a consulting firm, to analyze the CMS decision. HPA found that “systematically convert[ing] all global surgical codes to 0-day global codes by backing out of the bundled E&M services reduces the total RVUs and each component (work, practice expense, and malpractice) for surgical codes. Specifically, for surgical specialties, the impact of this transition on all Medicare reimbursed codes results in the following reductions:
- overall payment decrease of 1.8%
- payment decrease of 0.8% for work
- payment decrease of 2% for practice expense
- payment decrease of 9.2% for malpractice.
This modeling resulted in a total overall payment increase of 0.1% for generalists and a payment increase of 0.3% for medical specialists.”4
HPA’s findings related to the malpractice component are especially interesting for the ObGyn specialty. “Model results demonstrate that this policy results in significant redistribution of malpractice away from the main specialty provider of the surgical procedure into the entire group of providers (surgical and nonsurgical),” notes the HPA report.4 “Most impacted will be specialties with higher malpractice expenses, such as neurosurgeons and cardiac surgeons.”4 We could add ObGyns to that list.
ACOG cites numerous objections
ACOG is deeply involved in opposing this new CMS policy and preventing it from ever going into effect, working on our own, in coalition with our medical organization colleagues and patient organizations, and working closely with the US Congress.
ACOG and 28 other medical organizations, including the American Medical Association (AMA), summarized our opposition in a letter to US House and Senate Democratic and Republican leaders in December 2014, saying that this new policy:
Detracts from quality of care, impedes patient access, and complicates patient copays
- Patients will be responsible for copays on each service, including follow-up visits. This could considerably increase the administrative burden on patients. Worse, it could discourage them from returning for needed follow-up care.
- In the hospital critical care setting, the global payment structure allows the surgeon to oversee and coordinate care related to the patient’s recovery. Without the global structure, care will be fragmented and providers may compete to see patients and bill for the care they provide.
Undermines Medicare reform initiatives
- CMS initiatives for payment are all moving toward larger bundled payments. Deconstruction of the current payment structure for physicians is counterintuitive to the end goal of providing more comprehensive and coordinated care for the patient.
- Current bipartisan, bicameral legislation to repeal and replace the flawed sustainable growth rate formula calls for “a period of stability” in physician pay to allow physicians to transition to alternative payment models. The proposal to unbundle global surgical periods will add new complexities to an already flawed system and stymie progress.
Increases administrative burden
- The administrative burden on surgical practices and CMS (and its contractors) will be significant. Eliminating the global package will result in 63 million additional claims per year, adding unnecessary costs to our health care system.
Obstructs clinical registry data collection and quality improvement
- Surgeons will have less ability to collect information on patient outcomes in clinical registries, undermining many of the most meaningful quality improvement initiatives.5
Additional ACOG concerns
ACOG added these concerns to our opposition to the CMS plan:
- The change will not accurately account for physician work, practice expense, and malpractice risk for services performed.
- Thousands of new codes and/or values will need to be created for postoperative care because the supplies and equipment needed for postoperative care are not included in the E&M codes that will be used to report in-hospital and outpatient postoperative services (TABLE 2).
- Liability costs of a specific service should be derived from those of the performing specialties. Under the CMS plan, the liability costs associated with postoperative work would be removed from the primary service and artificially diluted by the wide mix of specialties performing all types of E&M services. Without global periods, a one-size-fits-all approach to professional liability insurance will be unsustainable and result in great disparities between the actual and realized malpractice costs for many physician specialties.
Table 2: Other postoperative care services currently bundled into global surgical packages
|
We have important allies
The American Association of Retired Persons (AARP) joined us in September 2014, when it formally asked CMS to abandon this new policy. In a letter to CMS Administrator Marilyn Tavenner, AARP noted that, “from a beneficiary perspective, we are concerned that this unbundling could produce considerable confusion and cause beneficiaries to receive multiple explanations of Medicare benefits (and incur separate cost-sharing obligations) related to a single surgical procedure….[G]iven the obvious methodological uncertainty and complexity involved in determining appropriate values for a very large number of ‘new’ 0-day global services, and the likely confusion surrounding the resulting increase in Medicare claims, AARP has serious doubts regarding the benefit of this unbundling proposal. We suggest [that] CMS consider other available alternatives, including the re-valuation of global services whose current values are believed to be incorrect.”6
Also in September, 27 Republican and Democratic members of Congress wrote a strong letter to CMS echoing the medical community’s concerns. The letter and many months of congressional leadership have been spearheaded by Representatives Larry Bucshon, MD, and Ami Bera, MD—demonstrating the value of having physicians in elective office. Other physician members of Congress who have provided outstanding leadership include ACOG Fellows and Representatives Michael Burgess, MD, and Phil Roe, MD, as well as Representatives Tom Price, MD; Andy Harris, MD; Joe Heck, DO; Charles Boustany, MD; Raul Ruiz, MD; and Dan Benishek, MD.
This important group of physician leaders, ACOG, AARP, and the surgical community are hard at work to derail or significantly delay what most physicians and policy analysts see as a very bad idea.
Congress takes action
In April 2015, Congress passed HR2, the Medicare Access and CHIP Reauthorization Bill, which most notably repealed the Medicare Sustainable Growth Rate formula. Included in this law is an important provision to halt implementation of CMS’ plan to unbundle all 10- and 90-day global codes.
Section 523 of that law requires CMS to periodically collect information on the services that surgeons furnish during these global periods, beginning no later than 2017, and use that information to ensure that the bundled payment amounts for surgical services are accurate. The Secretary of Health and Human Services is given the authority to withhold a portion of payment for services with a 10- or 90-day global period to incentivize the reporting of information. The Secretary can stop collecting this information from surgeons once the needed data can be obtained through other mechanisms, such as clinical data registries and electronic medical records.
Congressmen Bucshon and Bera championed this provision, along with nearly all physician members of the US House of Representatives. This change ensures a thorough, data-driven approach to appropriately valuing surgical services, including those provided by ObGyn subspecialists, such as urogynecologists and gynecologic oncologists.
Acknowledgment
The author thanks Barbara Levy, MD, ACOG Vice President for Health Policy, for her helpful comments.
Share your thoughts! Send your Letter to the Editor to [email protected]. Please include your name and the city and state in which you practice.
1. Department of Health and Human Services, Office of Inspector General. Nationwide Review of Evaluation and Management Services Included in Eye and Ocular Adnexa Global Surgery Fees for Calendar Year 2005. A-05-07-00077. Washington, DC: Department of Health and Human Services; April 2009.
2. Department of Health and Human Services, Office of Inspector General. Cardiovascular Global Surgery Fees Often Did Not Reflect the Number of Evaluation and Management Services Provided. A-05-09-00054. Washington, DC: Department of Health and Human Services; May 2012.
3. Department of Health and Human Services, Office of Inspector General. Musculoskeletal Global Surgery Fees Often Did Not Reflect the Number of Evaluation and Management Services Provided. A-05-09-00053. Washington, DC: Department of Health and Human Services; May 2012.
4. Summary of Initial Modeling Results of the CMS Policy to Transition 10- and 90-Day Global Surgery Codes to 0-Day Global Surgery Codes. Washington, DC: Health Policy Alternatives; January 9, 2015.
5. American Congress of Obstetricians and Gynecologists joint letter to Congress; December 2, 2014.
6. American Association of Retired Persons letter to Marilyn Tavenner, Administrator, Centers for Medicare and Medicaid Services; September 2, 2014.
1. Department of Health and Human Services, Office of Inspector General. Nationwide Review of Evaluation and Management Services Included in Eye and Ocular Adnexa Global Surgery Fees for Calendar Year 2005. A-05-07-00077. Washington, DC: Department of Health and Human Services; April 2009.
2. Department of Health and Human Services, Office of Inspector General. Cardiovascular Global Surgery Fees Often Did Not Reflect the Number of Evaluation and Management Services Provided. A-05-09-00054. Washington, DC: Department of Health and Human Services; May 2012.
3. Department of Health and Human Services, Office of Inspector General. Musculoskeletal Global Surgery Fees Often Did Not Reflect the Number of Evaluation and Management Services Provided. A-05-09-00053. Washington, DC: Department of Health and Human Services; May 2012.
4. Summary of Initial Modeling Results of the CMS Policy to Transition 10- and 90-Day Global Surgery Codes to 0-Day Global Surgery Codes. Washington, DC: Health Policy Alternatives; January 9, 2015.
5. American Congress of Obstetricians and Gynecologists joint letter to Congress; December 2, 2014.
6. American Association of Retired Persons letter to Marilyn Tavenner, Administrator, Centers for Medicare and Medicaid Services; September 2, 2014.
Are ObGyns getting “bumped” out of deserved Medicaid reimbursement?
With enactment of the Affordable Care Act (ACA) came a number of significant changes to federal and state Medicaid programs to increase access to care for low-income individuals. One landmark change, which became a state option after a ruling by the US Supreme Court, is the expansion of eligibility to all adults who have an income at or below 138% of the federal poverty line, which was $16,105 annually for an individual or $32,913 for a family of four in 2014.
Pregnancy is no longer a criterion for eligibility for low-income women in states with expanded Medicaid programs—a real game changer for millions of women in need of care.
As of this writing, 27 states, including the District of Columbia, have expanded their Medicaid program. Data from the Centers for Medicare and Medicaid Services (CMS) show that total enrollment in the Children’s Health Insurance Program (CHIP) and Medicaid increased by more than 4.8 million people (from 58.9 million to 63.7 million) between July 2013 and March 2014, in the 47 states reporting data for both periods. Nearly all of this growth occurred in Medicaid expansion states.1,2 More recent data show that 7.9 million more people were enrolled in Medicaid in July 2014 than in the previous year.3,4
Is Medicaid a losing proposition for ObGyns?
In many states, it costs ObGyns more than Medicaid pays to provide primary care to Medicaid patients. Nationally, providers receive 41% less in Medicaid reimbursement than they get with Medicare for primary care services.5 In 2012, the worst offender was Rhode Island’s Medicaid program, which paid physicians only 33% of the Medicare reimbursement rates for primary care.5
The rate of Medicaid reimbursement affects a physician’s willingness to accept new Medicaid patients. Only 50% of physicians are willing to accept new Medicaid patients, compared with 70% who are willing to accept new Medicare or privately insured patients. Twenty-three percent of female Medicaid beneficiaries report a problem finding a new doctor, compared with 7% of Medicare beneficiaries and 13% of privately insured women. The main reason: low Medicaid payment rates.6
In 2007, 38% of all ObGyns accepted Medicaid gynecology patients, and 44% accepted Medicaid obstetric patients, with Medicaid accounting for 18% of revenue for the average ObGyn practice. In its 2013 survey of members, ACOG found that while 63.2% accept all Medicare patients, only 44.4% accept all Medicaid gynecology patients, and 48.7% accept all Medicaid obstetric patients, up from 2007. The percentage of ObGyns who don’t see Medicaid gynecology or obstetric patients was 22.7% and 16.3%, respectively. Only 8.2% of ObGyns see no Medicare patients.7
According to a 2014 survey, 34% of physicians report an increase in Medicaid patients; 41% of those report an increase of 11% or more.3
The American Medical Association – The AMA considers the ObGyn specialty one of four specialties that provide primary care.
Tricare – The health-care program for uniformed service members (active, Guard/Reserve, retired) and their families around the world designates ObGyns as among primary care case managers.
Community Health Teams – A grant program to support primary care practices and patient-centered medical homes includes ObGyns as primary care providers.
Medicaid – Thirty-four states and the District of Columbia define ObGyns as primary care providers.
Medicaid Health Homes – Authorized under federal law to coordinate care for Medicaid enrollees with chronic conditions, health home providers coordinate all primary care, acute, behavioral health, and long-term services and supports to treat the whole person. ObGyns are eligible home health providers.
Health Resources Services Administration – This agency delineates health professional shortage areas, providing bonuses for physicians serving in these areas. It includes ObGyns as one of four primary care specialties.
National Health Service Corps – This organization offers loan repayments and scholarships to primary care providers working in underserved communities and recognizes ObGyns as primary care physicians.
Teaching Health Center Graduate Medical Education – This program supports community-based primary care residency programs to increase the number of primary care residents and dentists trained in geographically isolated or economically or medically vulnerable
communities.
Congress addresses the discrepancy
The ACA Medicaid primary care “bump,” as it’s called, was designed to help ensure access to primary care for the huge new group of individuals covered by Medicaid. It raised Medicaid payment rates for primary care services to Medicare fee levels in 2013 and 2014, an overall average increase of 73% in Medicaid payment rates for Evaluation and Management (E/M) codes 99201–99499, and for vaccine administration codes 90461 and 90471–90474 (FIGURES 1–3).8
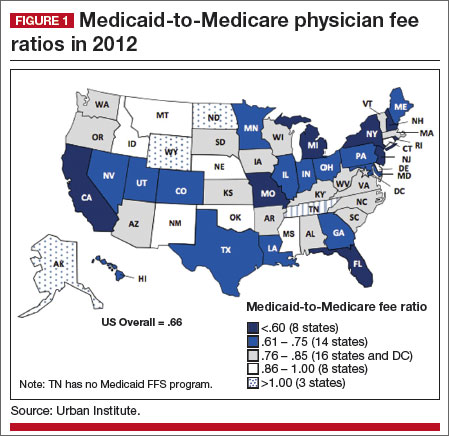
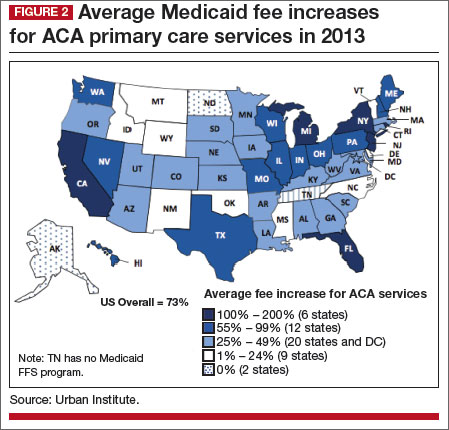
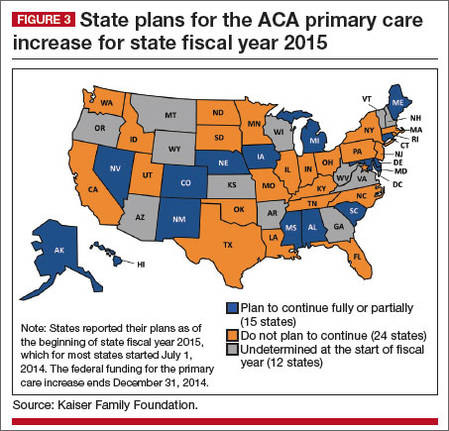
|
The catch? The bump only applies to internists, family medicine physicians, and pediatricians. The House-passed bill included ObGyns—women’s primary care providers—but the Senate bill did not, and the Senate bill was the version ultimately enacted into law.
To qualify for these additional payments, physicians must self-attest to the state Medicaid agency that she or he meets one of the following criteria:
- board certification in family medicine, general internal medicine, or pediatric medicine or a subspecialty recognized by the American Board of Medical Specialties, the American Board of Physician Specialties, or the American Osteopathic Association
- 60% of Medicaid billing involves the specified E/M and vaccine administration codes.
For newly eligible physicians, the previous month’s billing is used to determine eligibility.
What about women’s health?
In speaking with ACOG Fellows, here’s what ACOG President John Jennings, MD, had to say about the omission of ObGyns from the primary care rate bump:
This federal program, which expires at the end of this year, was designed to increase access to needed primary care services for low-income individuals. But as the program stands right now, it leaves out women’s health.
That’s just not right. And we have before us a chance to fix it.
ObGyns deliver primary and preventive care services to women; an ObGyn often is the only doctor a woman sees on a regular basis. Thirty-five state Medicaid programs classify ObGyns as primary care providers.9 Twelve percent of women aged 18 to 64 years rely on Medicaid for their health coverage, and more than 68% of adult Medicaid beneficiaries are women.10
Seeing an opportunity to expand the primary care reimbursement bump to include ObGyns, ACOG recently briefed Congress on the long and deep tradition of primary care in obstetrics and gynecology—a tradition that begins in residency. We provided Congress with ObGyn resident training requirements, as outlined by the Council on Resident Education in Obstetrics and Gynecology (CREOG).11
How ObGyns provide primary care
According to CREOG, “ObGyns provide primary health-care services to their patients both within and outside the traditional purview of reproductive medicine. As primary care physicians, ObGyns establish relationships with their patients that transcend the disease spectrum and extend to routine assessments, preventive care, early intervention, and management of medical disorders.”11
Among the services they provide are age-appropriate screening for substance use, sexual and reproductive health, sexually transmitted infection, psychosocial risks, breast disorders, cancer, and cardiovascular disease. ObGyns routinely counsel patients about diet, exercise, contraception, dental health, osteoporosis, and sexual health. And they provide front-line immunizations against such diseases as influenza, human papillomavirus, rubella, measles, meningitis, hepatitis A and B, and pneumonia.11
Certification in obstetrics and gynecology requires written and oral examinations in office practice and women’s health as a primary care content area. In fact, fully one-third of the board certification test taken by 97% of the ObGyns in this country tests their knowledge and training in primary care.11
How women view their ObGyn
A 2014 survey of women found that ObGyns play a critical role in providing primary care in the United States. Almost six in 10 women (58%) report that they see an ObGyn on a regular basis, and one-third of women (35%) view their ObGyn as their main source of care.12
Low-income women and women of color report that their ObGyn plays an even greater role in their health care. Latinas are far more likely (47%) to report that their ObGyn is their main source of care, compared with 35% of women overall. Sixty-four percent of African-American women say they see an ObGyn regularly, compared with 58% of women overall.12
Other survey findings:
- ObGyn providers are the first providers women choose as adults. They move from a pediatrician to an ObGyn.
- ObGyn providers are the “usual” providers for young women—the ones women see most frequently. They see internal medicine physicians and other providers infrequently during this period of their life.
- The ObGyn-patient relationship is intimate, comfortable, trusting, and confidential, and ObGyns often are considered “a friend.” Patients discuss issues with their ObGyns that are not raised with other providers.
- The care women receive from their -ObGyn provider is broad, ranging from an annual exam and breast exam to prenatal care, immunizations, a review of medications, blood pressure checks, and more.
- Women say their ObGyn does a better job than their family practice and internal medicine providers in providing a range of care and services.12
ObGyns may see relief in 2015
Congress has before it legislation to extend the primary care bump program into the future and expand it to include ObGyns and other women’s health clinicians. A proposal to that effect was introduced in the Senate by Patty Murray (D-WA) and Sherrod Brown (D-OH) and in the House by Reps. Frank Pallone (D-NJ) and Henry Waxman (D-CA).
At press time, ACOG was doing everything in its power to get this legislation passed in the lame duck session of Congress. We scored a big win at the November assembly of the American Medical Association (AMA) House of Delegates, when, with the support of the American Academy of Pediatricians (AAP) and the American College of Physicians, the House of Delegates overwhelmingly approved AMA policy to support extension of the program, including broadening it to include ObGyns.
ACOG also has enlisted the support of national women’s advocacy groups, including Planned Parenthood, the National Partnership for Families and Children, and the National Women’s Law Center. ACOG President Jennings led 35 ACOG leaders from across the country to Washington, DC, in November 2014, to urge members of Congress to pass this important legislation. They were joined by Thomas McInerney, MD, immediate past president of the AAP, and a number of leaders from Planned Parenthood.
Our message to Congress is clear: Not without women!
Share your thoughts on this article! Send your Letter to the Editor to [email protected]. Please include your name and the city and state in which you practice.
1. Kaiser Family Foundation. Implementing the ACA: Medicaid Spending & Enrollment Growth for FY 2014 and FY 2015. http://kff.org/medicaid/issue-brief/implementing-the-aca-medicaid-spending-enrollment-growth-for-fy-2014-and-fy-2015/. Published October 14, 2014. Accessed December 15, 2014.
2. Center for Medicare and Medicaid Services. Medicaid and CHIP: March 2014 Monthly Applications, Eligibility Determinations, and Enrollment Report. http://www.medicaid.gov/AffordableCareAct/Medicaid-Moving-Forward-2014/Downloads/March-2014-Enrollment-Report.pdf. May 1, 2014. Accessed December 17, 2014.
3. Kane L, Peckham C. Insurer Ratings Report 2014. Medscape. http://www.medscape.com/features/slideshow /public/insurerratingsreport2014. Published October 21, 2014. Accessed December 15, 2014.
4. Kenney GM, Zuckerman S, Dubay L, et al. Opting in to the Medicaid expansion under the ACA: who are the uninsured adults who could gain health insurance coverage? Timely Analysis of Immediate Health Policy Issues. Urban Institute. http://www.urban.org/uploadedpdf/412630-opting-in-medicaid.pdf. Published August 2012. Accessed December 15, 2014.
5. Kaiser Family Foundation. Medicaid-to-Medicare Fee Index. http://kff.org/medicaid/state-indicator/medicaid-to-medicare-fee-index/. Updated November 11, 2014. Accessed December 15, 2014.
6. Kaiser Family Foundation. Women and Health Care: A National Profile. Key Findings from the Kaiser Women’s Health Survey. http://kaiserfamilyfoundation.files.wordpress.com/2013/01/women-and-health-care-a-national-profile-key-findings-from-the-kaiser-women-s-health-survey.pdf. Published July 2005. Accessed December 15, 2014.
7. ACOG 2013 survey of members. http://www.acog.org/~/media/Departments/Practice-Management-and-Managed-Care/2013SocioeconomicSurvey.pdf. Accessed December 17, 2014.
8. Zuckerman S, Goin D, Kaiser Family Foundation. How much will Medicaid physician fees for primary care rise in 2013? Evidence from a 2012 survey of Medicaid physician fees. http://kff.org/medicaid/issue-brief/how-much-will-medicaid-physician-fees-for/. Published December 13, 2012. Accessed December 15, 2014.
9. Based on an ACOG review of state Medicaid regulations, statutes, and provider manuals.
10. National Women’s Law Center. Battles over Medicaid Funding and Eligibility: What’s at Stake for Women. http://nwlc.org/sites/default/files/pdfs/national.pdf. Published June 2011. Accessed December 15, 2014.
11. Carey JC, Blanchard MH, Adams KE, et al; Education Committee of the Council on Resident Education in Obstetrics and Gynecology (CREOG). CREOG Educational Objectives: Core Curriculum in Obstetrics and Gynecology, 10th ed. American Congress of Obstetricians and Gynecologists. http://www.acog.org/About-ACOG/ACOG-Departments/CREOG/CREOG-Search/CREOG-Educational-Objectives. Published 2013. Accessed December 15, 2014.
12. Montefiore Investigators to Present Data at American Congress of Obstetricians and Gynecologists Annual Meeting [news release]. April 25, 2014. http://www.montefiore.org/body.cfm?id=1738&action=detail&ref=1142. Accessed December 17, 2014.
With enactment of the Affordable Care Act (ACA) came a number of significant changes to federal and state Medicaid programs to increase access to care for low-income individuals. One landmark change, which became a state option after a ruling by the US Supreme Court, is the expansion of eligibility to all adults who have an income at or below 138% of the federal poverty line, which was $16,105 annually for an individual or $32,913 for a family of four in 2014.
Pregnancy is no longer a criterion for eligibility for low-income women in states with expanded Medicaid programs—a real game changer for millions of women in need of care.
As of this writing, 27 states, including the District of Columbia, have expanded their Medicaid program. Data from the Centers for Medicare and Medicaid Services (CMS) show that total enrollment in the Children’s Health Insurance Program (CHIP) and Medicaid increased by more than 4.8 million people (from 58.9 million to 63.7 million) between July 2013 and March 2014, in the 47 states reporting data for both periods. Nearly all of this growth occurred in Medicaid expansion states.1,2 More recent data show that 7.9 million more people were enrolled in Medicaid in July 2014 than in the previous year.3,4
Is Medicaid a losing proposition for ObGyns?
In many states, it costs ObGyns more than Medicaid pays to provide primary care to Medicaid patients. Nationally, providers receive 41% less in Medicaid reimbursement than they get with Medicare for primary care services.5 In 2012, the worst offender was Rhode Island’s Medicaid program, which paid physicians only 33% of the Medicare reimbursement rates for primary care.5
The rate of Medicaid reimbursement affects a physician’s willingness to accept new Medicaid patients. Only 50% of physicians are willing to accept new Medicaid patients, compared with 70% who are willing to accept new Medicare or privately insured patients. Twenty-three percent of female Medicaid beneficiaries report a problem finding a new doctor, compared with 7% of Medicare beneficiaries and 13% of privately insured women. The main reason: low Medicaid payment rates.6
In 2007, 38% of all ObGyns accepted Medicaid gynecology patients, and 44% accepted Medicaid obstetric patients, with Medicaid accounting for 18% of revenue for the average ObGyn practice. In its 2013 survey of members, ACOG found that while 63.2% accept all Medicare patients, only 44.4% accept all Medicaid gynecology patients, and 48.7% accept all Medicaid obstetric patients, up from 2007. The percentage of ObGyns who don’t see Medicaid gynecology or obstetric patients was 22.7% and 16.3%, respectively. Only 8.2% of ObGyns see no Medicare patients.7
According to a 2014 survey, 34% of physicians report an increase in Medicaid patients; 41% of those report an increase of 11% or more.3
The American Medical Association – The AMA considers the ObGyn specialty one of four specialties that provide primary care.
Tricare – The health-care program for uniformed service members (active, Guard/Reserve, retired) and their families around the world designates ObGyns as among primary care case managers.
Community Health Teams – A grant program to support primary care practices and patient-centered medical homes includes ObGyns as primary care providers.
Medicaid – Thirty-four states and the District of Columbia define ObGyns as primary care providers.
Medicaid Health Homes – Authorized under federal law to coordinate care for Medicaid enrollees with chronic conditions, health home providers coordinate all primary care, acute, behavioral health, and long-term services and supports to treat the whole person. ObGyns are eligible home health providers.
Health Resources Services Administration – This agency delineates health professional shortage areas, providing bonuses for physicians serving in these areas. It includes ObGyns as one of four primary care specialties.
National Health Service Corps – This organization offers loan repayments and scholarships to primary care providers working in underserved communities and recognizes ObGyns as primary care physicians.
Teaching Health Center Graduate Medical Education – This program supports community-based primary care residency programs to increase the number of primary care residents and dentists trained in geographically isolated or economically or medically vulnerable
communities.
Congress addresses the discrepancy
The ACA Medicaid primary care “bump,” as it’s called, was designed to help ensure access to primary care for the huge new group of individuals covered by Medicaid. It raised Medicaid payment rates for primary care services to Medicare fee levels in 2013 and 2014, an overall average increase of 73% in Medicaid payment rates for Evaluation and Management (E/M) codes 99201–99499, and for vaccine administration codes 90461 and 90471–90474 (FIGURES 1–3).8
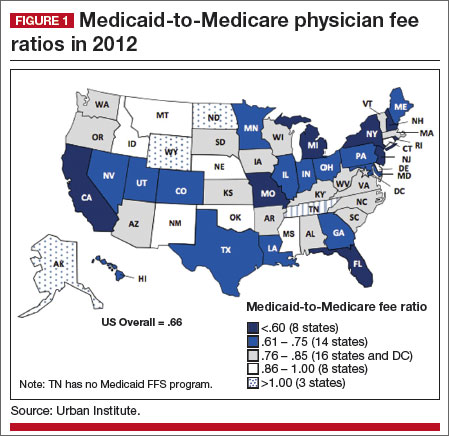
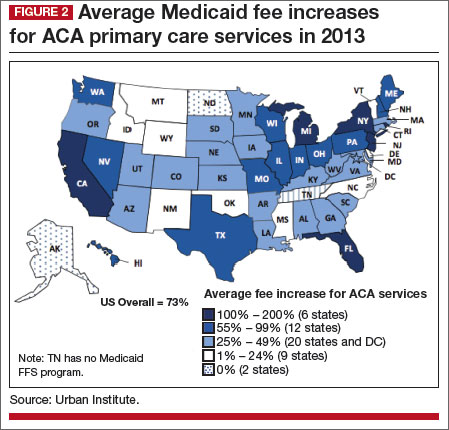
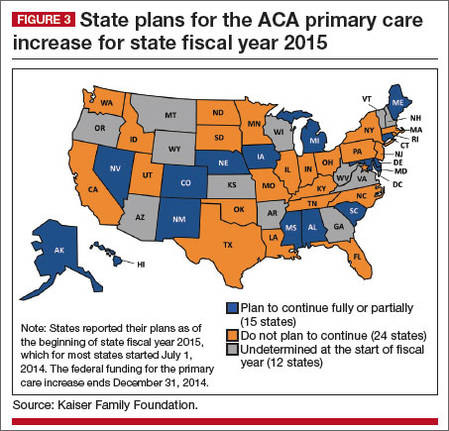
|
The catch? The bump only applies to internists, family medicine physicians, and pediatricians. The House-passed bill included ObGyns—women’s primary care providers—but the Senate bill did not, and the Senate bill was the version ultimately enacted into law.
To qualify for these additional payments, physicians must self-attest to the state Medicaid agency that she or he meets one of the following criteria:
- board certification in family medicine, general internal medicine, or pediatric medicine or a subspecialty recognized by the American Board of Medical Specialties, the American Board of Physician Specialties, or the American Osteopathic Association
- 60% of Medicaid billing involves the specified E/M and vaccine administration codes.
For newly eligible physicians, the previous month’s billing is used to determine eligibility.
What about women’s health?
In speaking with ACOG Fellows, here’s what ACOG President John Jennings, MD, had to say about the omission of ObGyns from the primary care rate bump:
This federal program, which expires at the end of this year, was designed to increase access to needed primary care services for low-income individuals. But as the program stands right now, it leaves out women’s health.
That’s just not right. And we have before us a chance to fix it.
ObGyns deliver primary and preventive care services to women; an ObGyn often is the only doctor a woman sees on a regular basis. Thirty-five state Medicaid programs classify ObGyns as primary care providers.9 Twelve percent of women aged 18 to 64 years rely on Medicaid for their health coverage, and more than 68% of adult Medicaid beneficiaries are women.10
Seeing an opportunity to expand the primary care reimbursement bump to include ObGyns, ACOG recently briefed Congress on the long and deep tradition of primary care in obstetrics and gynecology—a tradition that begins in residency. We provided Congress with ObGyn resident training requirements, as outlined by the Council on Resident Education in Obstetrics and Gynecology (CREOG).11
How ObGyns provide primary care
According to CREOG, “ObGyns provide primary health-care services to their patients both within and outside the traditional purview of reproductive medicine. As primary care physicians, ObGyns establish relationships with their patients that transcend the disease spectrum and extend to routine assessments, preventive care, early intervention, and management of medical disorders.”11
Among the services they provide are age-appropriate screening for substance use, sexual and reproductive health, sexually transmitted infection, psychosocial risks, breast disorders, cancer, and cardiovascular disease. ObGyns routinely counsel patients about diet, exercise, contraception, dental health, osteoporosis, and sexual health. And they provide front-line immunizations against such diseases as influenza, human papillomavirus, rubella, measles, meningitis, hepatitis A and B, and pneumonia.11
Certification in obstetrics and gynecology requires written and oral examinations in office practice and women’s health as a primary care content area. In fact, fully one-third of the board certification test taken by 97% of the ObGyns in this country tests their knowledge and training in primary care.11
How women view their ObGyn
A 2014 survey of women found that ObGyns play a critical role in providing primary care in the United States. Almost six in 10 women (58%) report that they see an ObGyn on a regular basis, and one-third of women (35%) view their ObGyn as their main source of care.12
Low-income women and women of color report that their ObGyn plays an even greater role in their health care. Latinas are far more likely (47%) to report that their ObGyn is their main source of care, compared with 35% of women overall. Sixty-four percent of African-American women say they see an ObGyn regularly, compared with 58% of women overall.12
Other survey findings:
- ObGyn providers are the first providers women choose as adults. They move from a pediatrician to an ObGyn.
- ObGyn providers are the “usual” providers for young women—the ones women see most frequently. They see internal medicine physicians and other providers infrequently during this period of their life.
- The ObGyn-patient relationship is intimate, comfortable, trusting, and confidential, and ObGyns often are considered “a friend.” Patients discuss issues with their ObGyns that are not raised with other providers.
- The care women receive from their -ObGyn provider is broad, ranging from an annual exam and breast exam to prenatal care, immunizations, a review of medications, blood pressure checks, and more.
- Women say their ObGyn does a better job than their family practice and internal medicine providers in providing a range of care and services.12
ObGyns may see relief in 2015
Congress has before it legislation to extend the primary care bump program into the future and expand it to include ObGyns and other women’s health clinicians. A proposal to that effect was introduced in the Senate by Patty Murray (D-WA) and Sherrod Brown (D-OH) and in the House by Reps. Frank Pallone (D-NJ) and Henry Waxman (D-CA).
At press time, ACOG was doing everything in its power to get this legislation passed in the lame duck session of Congress. We scored a big win at the November assembly of the American Medical Association (AMA) House of Delegates, when, with the support of the American Academy of Pediatricians (AAP) and the American College of Physicians, the House of Delegates overwhelmingly approved AMA policy to support extension of the program, including broadening it to include ObGyns.
ACOG also has enlisted the support of national women’s advocacy groups, including Planned Parenthood, the National Partnership for Families and Children, and the National Women’s Law Center. ACOG President Jennings led 35 ACOG leaders from across the country to Washington, DC, in November 2014, to urge members of Congress to pass this important legislation. They were joined by Thomas McInerney, MD, immediate past president of the AAP, and a number of leaders from Planned Parenthood.
Our message to Congress is clear: Not without women!
Share your thoughts on this article! Send your Letter to the Editor to [email protected]. Please include your name and the city and state in which you practice.
With enactment of the Affordable Care Act (ACA) came a number of significant changes to federal and state Medicaid programs to increase access to care for low-income individuals. One landmark change, which became a state option after a ruling by the US Supreme Court, is the expansion of eligibility to all adults who have an income at or below 138% of the federal poverty line, which was $16,105 annually for an individual or $32,913 for a family of four in 2014.
Pregnancy is no longer a criterion for eligibility for low-income women in states with expanded Medicaid programs—a real game changer for millions of women in need of care.
As of this writing, 27 states, including the District of Columbia, have expanded their Medicaid program. Data from the Centers for Medicare and Medicaid Services (CMS) show that total enrollment in the Children’s Health Insurance Program (CHIP) and Medicaid increased by more than 4.8 million people (from 58.9 million to 63.7 million) between July 2013 and March 2014, in the 47 states reporting data for both periods. Nearly all of this growth occurred in Medicaid expansion states.1,2 More recent data show that 7.9 million more people were enrolled in Medicaid in July 2014 than in the previous year.3,4
Is Medicaid a losing proposition for ObGyns?
In many states, it costs ObGyns more than Medicaid pays to provide primary care to Medicaid patients. Nationally, providers receive 41% less in Medicaid reimbursement than they get with Medicare for primary care services.5 In 2012, the worst offender was Rhode Island’s Medicaid program, which paid physicians only 33% of the Medicare reimbursement rates for primary care.5
The rate of Medicaid reimbursement affects a physician’s willingness to accept new Medicaid patients. Only 50% of physicians are willing to accept new Medicaid patients, compared with 70% who are willing to accept new Medicare or privately insured patients. Twenty-three percent of female Medicaid beneficiaries report a problem finding a new doctor, compared with 7% of Medicare beneficiaries and 13% of privately insured women. The main reason: low Medicaid payment rates.6
In 2007, 38% of all ObGyns accepted Medicaid gynecology patients, and 44% accepted Medicaid obstetric patients, with Medicaid accounting for 18% of revenue for the average ObGyn practice. In its 2013 survey of members, ACOG found that while 63.2% accept all Medicare patients, only 44.4% accept all Medicaid gynecology patients, and 48.7% accept all Medicaid obstetric patients, up from 2007. The percentage of ObGyns who don’t see Medicaid gynecology or obstetric patients was 22.7% and 16.3%, respectively. Only 8.2% of ObGyns see no Medicare patients.7
According to a 2014 survey, 34% of physicians report an increase in Medicaid patients; 41% of those report an increase of 11% or more.3
The American Medical Association – The AMA considers the ObGyn specialty one of four specialties that provide primary care.
Tricare – The health-care program for uniformed service members (active, Guard/Reserve, retired) and their families around the world designates ObGyns as among primary care case managers.
Community Health Teams – A grant program to support primary care practices and patient-centered medical homes includes ObGyns as primary care providers.
Medicaid – Thirty-four states and the District of Columbia define ObGyns as primary care providers.
Medicaid Health Homes – Authorized under federal law to coordinate care for Medicaid enrollees with chronic conditions, health home providers coordinate all primary care, acute, behavioral health, and long-term services and supports to treat the whole person. ObGyns are eligible home health providers.
Health Resources Services Administration – This agency delineates health professional shortage areas, providing bonuses for physicians serving in these areas. It includes ObGyns as one of four primary care specialties.
National Health Service Corps – This organization offers loan repayments and scholarships to primary care providers working in underserved communities and recognizes ObGyns as primary care physicians.
Teaching Health Center Graduate Medical Education – This program supports community-based primary care residency programs to increase the number of primary care residents and dentists trained in geographically isolated or economically or medically vulnerable
communities.
Congress addresses the discrepancy
The ACA Medicaid primary care “bump,” as it’s called, was designed to help ensure access to primary care for the huge new group of individuals covered by Medicaid. It raised Medicaid payment rates for primary care services to Medicare fee levels in 2013 and 2014, an overall average increase of 73% in Medicaid payment rates for Evaluation and Management (E/M) codes 99201–99499, and for vaccine administration codes 90461 and 90471–90474 (FIGURES 1–3).8
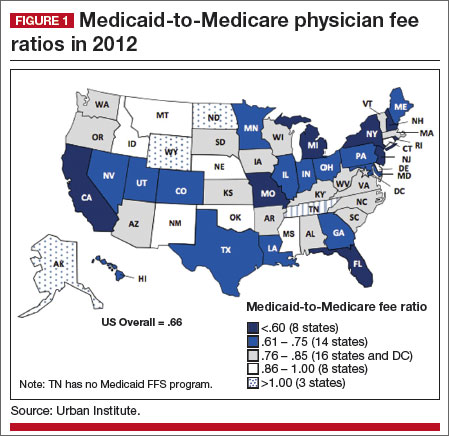
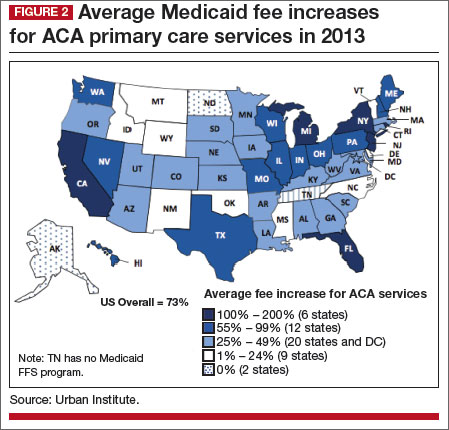
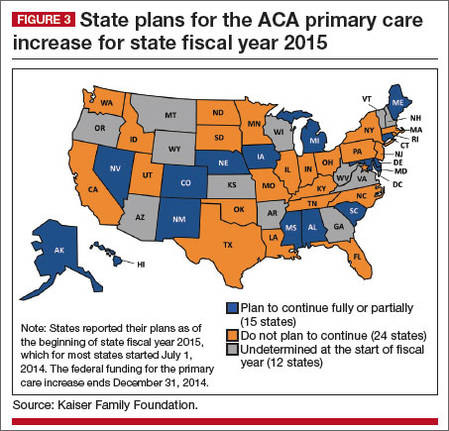
|
The catch? The bump only applies to internists, family medicine physicians, and pediatricians. The House-passed bill included ObGyns—women’s primary care providers—but the Senate bill did not, and the Senate bill was the version ultimately enacted into law.
To qualify for these additional payments, physicians must self-attest to the state Medicaid agency that she or he meets one of the following criteria:
- board certification in family medicine, general internal medicine, or pediatric medicine or a subspecialty recognized by the American Board of Medical Specialties, the American Board of Physician Specialties, or the American Osteopathic Association
- 60% of Medicaid billing involves the specified E/M and vaccine administration codes.
For newly eligible physicians, the previous month’s billing is used to determine eligibility.
What about women’s health?
In speaking with ACOG Fellows, here’s what ACOG President John Jennings, MD, had to say about the omission of ObGyns from the primary care rate bump:
This federal program, which expires at the end of this year, was designed to increase access to needed primary care services for low-income individuals. But as the program stands right now, it leaves out women’s health.
That’s just not right. And we have before us a chance to fix it.
ObGyns deliver primary and preventive care services to women; an ObGyn often is the only doctor a woman sees on a regular basis. Thirty-five state Medicaid programs classify ObGyns as primary care providers.9 Twelve percent of women aged 18 to 64 years rely on Medicaid for their health coverage, and more than 68% of adult Medicaid beneficiaries are women.10
Seeing an opportunity to expand the primary care reimbursement bump to include ObGyns, ACOG recently briefed Congress on the long and deep tradition of primary care in obstetrics and gynecology—a tradition that begins in residency. We provided Congress with ObGyn resident training requirements, as outlined by the Council on Resident Education in Obstetrics and Gynecology (CREOG).11
How ObGyns provide primary care
According to CREOG, “ObGyns provide primary health-care services to their patients both within and outside the traditional purview of reproductive medicine. As primary care physicians, ObGyns establish relationships with their patients that transcend the disease spectrum and extend to routine assessments, preventive care, early intervention, and management of medical disorders.”11
Among the services they provide are age-appropriate screening for substance use, sexual and reproductive health, sexually transmitted infection, psychosocial risks, breast disorders, cancer, and cardiovascular disease. ObGyns routinely counsel patients about diet, exercise, contraception, dental health, osteoporosis, and sexual health. And they provide front-line immunizations against such diseases as influenza, human papillomavirus, rubella, measles, meningitis, hepatitis A and B, and pneumonia.11
Certification in obstetrics and gynecology requires written and oral examinations in office practice and women’s health as a primary care content area. In fact, fully one-third of the board certification test taken by 97% of the ObGyns in this country tests their knowledge and training in primary care.11
How women view their ObGyn
A 2014 survey of women found that ObGyns play a critical role in providing primary care in the United States. Almost six in 10 women (58%) report that they see an ObGyn on a regular basis, and one-third of women (35%) view their ObGyn as their main source of care.12
Low-income women and women of color report that their ObGyn plays an even greater role in their health care. Latinas are far more likely (47%) to report that their ObGyn is their main source of care, compared with 35% of women overall. Sixty-four percent of African-American women say they see an ObGyn regularly, compared with 58% of women overall.12
Other survey findings:
- ObGyn providers are the first providers women choose as adults. They move from a pediatrician to an ObGyn.
- ObGyn providers are the “usual” providers for young women—the ones women see most frequently. They see internal medicine physicians and other providers infrequently during this period of their life.
- The ObGyn-patient relationship is intimate, comfortable, trusting, and confidential, and ObGyns often are considered “a friend.” Patients discuss issues with their ObGyns that are not raised with other providers.
- The care women receive from their -ObGyn provider is broad, ranging from an annual exam and breast exam to prenatal care, immunizations, a review of medications, blood pressure checks, and more.
- Women say their ObGyn does a better job than their family practice and internal medicine providers in providing a range of care and services.12
ObGyns may see relief in 2015
Congress has before it legislation to extend the primary care bump program into the future and expand it to include ObGyns and other women’s health clinicians. A proposal to that effect was introduced in the Senate by Patty Murray (D-WA) and Sherrod Brown (D-OH) and in the House by Reps. Frank Pallone (D-NJ) and Henry Waxman (D-CA).
At press time, ACOG was doing everything in its power to get this legislation passed in the lame duck session of Congress. We scored a big win at the November assembly of the American Medical Association (AMA) House of Delegates, when, with the support of the American Academy of Pediatricians (AAP) and the American College of Physicians, the House of Delegates overwhelmingly approved AMA policy to support extension of the program, including broadening it to include ObGyns.
ACOG also has enlisted the support of national women’s advocacy groups, including Planned Parenthood, the National Partnership for Families and Children, and the National Women’s Law Center. ACOG President Jennings led 35 ACOG leaders from across the country to Washington, DC, in November 2014, to urge members of Congress to pass this important legislation. They were joined by Thomas McInerney, MD, immediate past president of the AAP, and a number of leaders from Planned Parenthood.
Our message to Congress is clear: Not without women!
Share your thoughts on this article! Send your Letter to the Editor to [email protected]. Please include your name and the city and state in which you practice.
1. Kaiser Family Foundation. Implementing the ACA: Medicaid Spending & Enrollment Growth for FY 2014 and FY 2015. http://kff.org/medicaid/issue-brief/implementing-the-aca-medicaid-spending-enrollment-growth-for-fy-2014-and-fy-2015/. Published October 14, 2014. Accessed December 15, 2014.
2. Center for Medicare and Medicaid Services. Medicaid and CHIP: March 2014 Monthly Applications, Eligibility Determinations, and Enrollment Report. http://www.medicaid.gov/AffordableCareAct/Medicaid-Moving-Forward-2014/Downloads/March-2014-Enrollment-Report.pdf. May 1, 2014. Accessed December 17, 2014.
3. Kane L, Peckham C. Insurer Ratings Report 2014. Medscape. http://www.medscape.com/features/slideshow /public/insurerratingsreport2014. Published October 21, 2014. Accessed December 15, 2014.
4. Kenney GM, Zuckerman S, Dubay L, et al. Opting in to the Medicaid expansion under the ACA: who are the uninsured adults who could gain health insurance coverage? Timely Analysis of Immediate Health Policy Issues. Urban Institute. http://www.urban.org/uploadedpdf/412630-opting-in-medicaid.pdf. Published August 2012. Accessed December 15, 2014.
5. Kaiser Family Foundation. Medicaid-to-Medicare Fee Index. http://kff.org/medicaid/state-indicator/medicaid-to-medicare-fee-index/. Updated November 11, 2014. Accessed December 15, 2014.
6. Kaiser Family Foundation. Women and Health Care: A National Profile. Key Findings from the Kaiser Women’s Health Survey. http://kaiserfamilyfoundation.files.wordpress.com/2013/01/women-and-health-care-a-national-profile-key-findings-from-the-kaiser-women-s-health-survey.pdf. Published July 2005. Accessed December 15, 2014.
7. ACOG 2013 survey of members. http://www.acog.org/~/media/Departments/Practice-Management-and-Managed-Care/2013SocioeconomicSurvey.pdf. Accessed December 17, 2014.
8. Zuckerman S, Goin D, Kaiser Family Foundation. How much will Medicaid physician fees for primary care rise in 2013? Evidence from a 2012 survey of Medicaid physician fees. http://kff.org/medicaid/issue-brief/how-much-will-medicaid-physician-fees-for/. Published December 13, 2012. Accessed December 15, 2014.
9. Based on an ACOG review of state Medicaid regulations, statutes, and provider manuals.
10. National Women’s Law Center. Battles over Medicaid Funding and Eligibility: What’s at Stake for Women. http://nwlc.org/sites/default/files/pdfs/national.pdf. Published June 2011. Accessed December 15, 2014.
11. Carey JC, Blanchard MH, Adams KE, et al; Education Committee of the Council on Resident Education in Obstetrics and Gynecology (CREOG). CREOG Educational Objectives: Core Curriculum in Obstetrics and Gynecology, 10th ed. American Congress of Obstetricians and Gynecologists. http://www.acog.org/About-ACOG/ACOG-Departments/CREOG/CREOG-Search/CREOG-Educational-Objectives. Published 2013. Accessed December 15, 2014.
12. Montefiore Investigators to Present Data at American Congress of Obstetricians and Gynecologists Annual Meeting [news release]. April 25, 2014. http://www.montefiore.org/body.cfm?id=1738&action=detail&ref=1142. Accessed December 17, 2014.
1. Kaiser Family Foundation. Implementing the ACA: Medicaid Spending & Enrollment Growth for FY 2014 and FY 2015. http://kff.org/medicaid/issue-brief/implementing-the-aca-medicaid-spending-enrollment-growth-for-fy-2014-and-fy-2015/. Published October 14, 2014. Accessed December 15, 2014.
2. Center for Medicare and Medicaid Services. Medicaid and CHIP: March 2014 Monthly Applications, Eligibility Determinations, and Enrollment Report. http://www.medicaid.gov/AffordableCareAct/Medicaid-Moving-Forward-2014/Downloads/March-2014-Enrollment-Report.pdf. May 1, 2014. Accessed December 17, 2014.
3. Kane L, Peckham C. Insurer Ratings Report 2014. Medscape. http://www.medscape.com/features/slideshow /public/insurerratingsreport2014. Published October 21, 2014. Accessed December 15, 2014.
4. Kenney GM, Zuckerman S, Dubay L, et al. Opting in to the Medicaid expansion under the ACA: who are the uninsured adults who could gain health insurance coverage? Timely Analysis of Immediate Health Policy Issues. Urban Institute. http://www.urban.org/uploadedpdf/412630-opting-in-medicaid.pdf. Published August 2012. Accessed December 15, 2014.
5. Kaiser Family Foundation. Medicaid-to-Medicare Fee Index. http://kff.org/medicaid/state-indicator/medicaid-to-medicare-fee-index/. Updated November 11, 2014. Accessed December 15, 2014.
6. Kaiser Family Foundation. Women and Health Care: A National Profile. Key Findings from the Kaiser Women’s Health Survey. http://kaiserfamilyfoundation.files.wordpress.com/2013/01/women-and-health-care-a-national-profile-key-findings-from-the-kaiser-women-s-health-survey.pdf. Published July 2005. Accessed December 15, 2014.
7. ACOG 2013 survey of members. http://www.acog.org/~/media/Departments/Practice-Management-and-Managed-Care/2013SocioeconomicSurvey.pdf. Accessed December 17, 2014.
8. Zuckerman S, Goin D, Kaiser Family Foundation. How much will Medicaid physician fees for primary care rise in 2013? Evidence from a 2012 survey of Medicaid physician fees. http://kff.org/medicaid/issue-brief/how-much-will-medicaid-physician-fees-for/. Published December 13, 2012. Accessed December 15, 2014.
9. Based on an ACOG review of state Medicaid regulations, statutes, and provider manuals.
10. National Women’s Law Center. Battles over Medicaid Funding and Eligibility: What’s at Stake for Women. http://nwlc.org/sites/default/files/pdfs/national.pdf. Published June 2011. Accessed December 15, 2014.
11. Carey JC, Blanchard MH, Adams KE, et al; Education Committee of the Council on Resident Education in Obstetrics and Gynecology (CREOG). CREOG Educational Objectives: Core Curriculum in Obstetrics and Gynecology, 10th ed. American Congress of Obstetricians and Gynecologists. http://www.acog.org/About-ACOG/ACOG-Departments/CREOG/CREOG-Search/CREOG-Educational-Objectives. Published 2013. Accessed December 15, 2014.
12. Montefiore Investigators to Present Data at American Congress of Obstetricians and Gynecologists Annual Meeting [news release]. April 25, 2014. http://www.montefiore.org/body.cfm?id=1738&action=detail&ref=1142. Accessed December 17, 2014.
It’s a Republican majority following midterm election results. How will that affect the ACA and women’s health?
The Affordable Care Act: What’s the latest?
mmmm
When I last wrote about the Affordable Care Act (ACA), in May 2014, I focused on the contraception issue. Since then, the US Supreme Court ruled, in Burwell v. Hobby Lobby, that closely held, for-profit companies with religious objections to covering birth control can opt out of the requirement to provide contraceptive coverage to their employees.
In this article, I explore that decision and what it means for women’s health. I also present data on the uninsured rate in the United States, which has dropped significantly since enactment of the ACA, and I discuss one increasingly common barrier to access to care—the use of narrow networks by insurers.
A corporation now can hold a religious belief
The Supreme Court’s majority 5-4 ruling recognized, for the first time, that a for-profit corporation can hold a religious belief, but the Court limited this claim to closely held corporations. The Court also decided that the ACA placed a substantial burden on the corporations’ religious beliefs and concluded that there are less burdensome ways to accomplish the law’s intent, rendering the contraceptive coverage provision in the ACA in violation of the Religious Freedom Restoration Act (RFRA). The Court limited its ruling to the contraceptive coverage requirement, essentially turning the requirement into an option for many employers.
Are contraceptives abortifacients?
The religious belief at the center of Burwell v. Hobby Lobby was that life begins at conception, which the Green family—the owners of Hobby Lobby—equate to fertilization. Hobby Lobby’s attorneys also asserted that four contraceptives approved by the US Food and Drug Administration and included in the ACA mandate may prevent implantation of a fertilized egg, thereby constituting abortion.
Although there is no scientific answer as to when life begins, ACOG and the medical community agree that pregnancy begins at implantation. In its amicus brief to the US Supreme Court, ACOG asserted the medical community’s consensus that the four contraceptives prevent pregnancy rather than end it, and are not abortifacients:
- emergency contraceptive pills: levonorgestrel (Plan B) and its generic equivalents and ulipristal acetate (ella)
- the copper IUD (ParaGard)
- levonorgestrel-releasing intrauterine systems (Mirena, Skyla).
What is a closely held corporation?
In general, according to the Pew Research Center, a closely held corporation is a private company (not publicly traded) with a limited number of shareholders. The Internal Revenue Service (IRS), an important source, defines a closely held corporation as one in which more than half of the stock is owned (directly or indirectly) by five or fewer individuals at any time in the second half of the year.
“S” corporations are also considered closely held. These are corporations with 100 or fewer shareholders, with all members of the same family counted as one shareholder. “S” corporations don’t pay income tax; their shareholders pay tax on their personal returns, based on the corporations’ profits and losses.
Hobby Lobby is organized as an “S” corporation. According to the IRS, in 2011, there were 4,158,572 “S” corporations, 99.4% of them with 10 or fewer shareholders.1
The US Census Bureau estimates that, in 2012, about 2.9 million “S” corporations employed more than 29 million people. Many closely held corporations are quite large.2 According to the Pew Research Center, family-owned Cargill employs 140,000 people and had $136.7 billion in revenue in fiscal 2013. Hobby Lobby has estimated revenues of $3.3 billion and 23,000 employees.2
What’s next?
ACOG helped secure coverage of contraceptives in the ACA and is working with the US Congress and our women’s health partners to restore this important care. Days after the Supreme Court decision, Senator Patty Murray (D-WA) introduced the Protect Women’s Health from Corporate Interference Act, S. 2578, with 46 cosponsors as of this writing. ACOG fully supports this bill, also known as the “Not My Boss’ Business Bill,” which would reestablish the contraceptive coverage mandate as well as other care required by federal law. This bill still maintains the exemption from contraceptive coverage for houses of worship and the accommodation for religious nonprofits.
In introducing her bill, Senator Murray pointed out that “the contraceptive coverage requirement has already made a tremendous difference in women’s lives—24 million more prescriptions for oral contraceptives were filled with no copay in 2013 than in 2012, and women have saved $483 million in out-of-pocket costs for oral contraceptives.”3
Uninsured rate is declining
The Commonwealth Fund shows that, from July–September 2013 to April–June 2014, the nation’s uninsured rate fell from 20% to 15%, resulting in 9.5 million fewer uninsured adults.4 The biggest drop occurred among young adults, with the uninsured rate falling from 28% to 18%, and in states that adopted the Medicaid expansion, where uninsured rates fell from 28% to 17%.4
States that didn’t expand their Medicaid program didn’t show any noticeable change, with the uninsured rate declining only two points, from 38% to 36%.4
Coverage resulted in access to care for the majority of the newly covered. Sixty percent of people with new coverage visited a provider or hospital or paid for a prescription. Sixty-two percent of these individuals said they wouldn’t have been able to access this care before getting this coverage. Eighty-one percent of people with new coverage said they were better off now than before.4
ACA works better in some states than others
The Kaiser Family Foundation looked at four successful states—Colorado, Connecticut, Kentucky, and Washington state—to see what lessons can be learned. Important commonalities include the fact that the states run their own marketplace, adopted the Medi-caid expansion, and conducted extensive outreach and public education, including engaging providers in patient outreach and enrollment.5
Other tools of success were developing good marketing and branding, providing consumer-friendly assistance, and attention to systems and operations.5
How the Hobby Lobby decision affects individual states
Because the Supreme Court’s decision concerned interpretation of a federal law—the Religious Freedom Restoration Act (RFRA)—it does not supersede state laws that mandate coverage of contraceptives.
Twenty-eight states have laws or rulings requiring insurers to cover contraceptives, most of them dating from the 1990s and providing some exemption for religious insurers or plans. Only Illinois allows an exemption for secular bodies.
Although these state laws remain in effect, state officials may opt to stop enforcing them with regard to certain companies. For example, after the Hobby Lobby decision, Wisconsin officials announced that they no longer will enforce contraceptive coverage when a company has a religious objection.
For companies that self-fund or self-insure worker health coverage, the state coverage laws don’t apply—only federal law does. These companies do not have to adhere to state insurance mandates.
Some states have their own version of the RFRA. See the chart at right for details on a state-by-state basis.
The Supreme Court ruling also has no effect on state laws that guarantee access to emergency contraception in hospital emergency departments and that require pharmacists to dispense contraceptives.
| State | Contraceptive equity law? | Employer/insurer exemption to equity law? | Religious freedom law? |
| Alabama | ✔ | ||
| Alaska | |||
| Arizona | ✔ | ✔ | ✔ |
| Arkansas | ✔ | ✔ | |
| California | ✔ | ✔ | |
| Colorado | ✔ | ||
| Connecticut | ✔ | ✔ | ✔ |
| Delaware | ✔ | ✔ | |
| Florida | ✔ | ||
| Georgia | ✔ | ||
| Hawaii | ✔ | ✔ | |
| Idaho | ✔ | ||
| Illinois | ✔ | ✔ | ✔ |
| Indiana | |||
| Iowa | ✔ | ||
| Kansas | |||
| Kentucky | ✔ | ||
| Louisiana | ✔ | ||
| Maine | ✔ | ✔ | |
| Maryland | ✔ | ✔ | |
| Massachusetts | ✔ | ✔ | |
| Michigan | ✔ | ✔ | |
| Minnesota | |||
| Mississippi | ✔ | ||
| Missouri | ✔ | ✔ | ✔ |
| Montana | ✔ | ||
| Nebraska | |||
| Nevada | ✔ | ✔ | |
| New Hampshire | ✔ | ||
| New Jersey | ✔ | ✔ | |
| New Mexico | ✔ | ✔ | ✔ |
| New York | ✔ | ✔ | |
| North Carolina | ✔ | ✔ | |
| North Dakota | |||
| Ohio | |||
| Oklahoma | ✔ | ||
| Oregon | ✔ | ✔ | |
| Pennsylvania | ✔ | ||
| Rhode Island | ✔ | ✔ | ✔ |
| South Carolina | ✔ | ||
| South Dakota | |||
| Tennessee | ✔ | ||
| Texas | ✔ | ||
| Utah | |||
| Vermont | ✔ | ||
| Virginia | ✔ | ||
| Washington | ✔ | ||
| West Virginia | ✔ | ✔ | |
| Wisconsin | ✔ | ||
| Wyoming | |||
| TOTAL | 28 | 20 | 18 |
Narrow networks limit access to care
Huge concerns abound regarding implementation and real-life experiences related to the ACA. A number of them—high deductibles, low payment rates, limited access to physicians, long drive and wait times—can be related to “narrow networks.” Insurers exclude certain providers and offer all providers lower payment rates (which leads some physicians to drop out of the plan); they also create tiers (charging consumers lower copays and deductibles for using inner-tier preferred providers and high out-of-pocket costs for using other providers, even though they may be in the network).
Narrow networks work for insurers as an effective tool for lowering provider payment rates to keep premiums low and gain market share. The narrower the network, the lower are physician payments and premiums.
The ACA promises expanded access to high-quality, affordable health care for millions of Americans—a promise being compromised in many areas of the country through narrow networks. In these instances, insurers offering new plans in a health-care marketplace limit patient access to the numbers, types, and locations of physicians and hospitals covered under certain plans. Insurers typically offer patients low premiums, offer selected providers a high volume of patients at low payment levels, and exclude other providers whom the insurer deems to be high-cost.
Narrow networks aren’t new
As with so many elements of the ACA, narrow networks aren’t a new phenomenon. Many of us remember the public relations price that HMOs paid in the 1980s and 1990s for exceedingly limiting patients’ access to care while charging low premiums. The consumer outcry led the National Association of Insurance Commissioners to urge states to require managed-care plans to maintain adequate networks, the approach adopted by the federal government in the ACA.6
The pendulum swung in the next decade to broader networks in which consumers had much greater access, but premiums increased by an average of 11% per year.6 Employers then pushed insurers to reduce premium costs, leading back to narrow networks in the years just before the ACA. Narrow network plans accounted for 23% of all employer-sponsored plans in 2012, up from 15% in 2007.6
Increasing consolidation contributes to narrow networks
The trend toward narrower networks is also linked to increasing consolidation in health care. As health systems grow and individual or small group practices disappear, insurers rely on being able to credibly threaten to exclude systems and big groups from their networks as leverage in payment negotiations. By restricting the choice of providers in a plan, the insurer can promise more customers for the doctors and hospitals that are included, and negotiate lower payments to those providers.
The downside for physicians is clear:
- low payment rates
- exclusion from networks and coverage
- inability to refer patients to providers the physician determines to be best for that patient’s needs.
- The downside for patients:
- If they have to go out of network to get needed care, they may end up paying high out-of-pocket costs
- If they delay or forego care, their health may suffer significantly.
The insurance industry’s position is that patients have choices. Plans with access to more hospitals and specialists are available but usually at a higher price.
Narrow networks are one way to achieve low premiums
In the months leading up to ACA enactment, insurers got to work developing plans designed to be sold on the exchanges that would attract consumers through low-cost premiums and still maximize profits, especially now that insurers, under the ACA, are barred from excluding sick enrollees or increasing premiums for women, in addition to other important protections.
In previous articles, we’ve explored these landmark protections. Insurers in the individual market used to be able to keep premiums relatively low, and profits up, through use of preexisting coverage exclusions, benefit exclusions including noncoverage for maternity care or prescription drugs, and high cost sharing. Not anymore.
Since enactment of the ACA, narrow networks seem to be the preferred, and most effective, payment negotiation tool of many insurers offering plans through the exchanges, reflecting the trend we’re already seeing in the private health insurance marketplace.
NPR spotlights the difficulty of finding a specialist
The consumer and provider problems of narrow networks have been gaining attention in the media. In July, the National Public Radio (NPR) Web site carried an article entitled, “Patients with low-cost insurance struggle to find specialists,” with a key subtitle: “So you found an exchange plan. But can you find a provider?”7
In the NPR article, author Carrie Feibel reported on the situation in a majority-immigrant area of southwest Houston.
There, many patients at the local clinic have health insurance coverage for the first time, an important step toward healthier lives for themselves and their families. But many people in need of a specialist are learning that their insurance card doesn’t guarantee them access to a needed surgeon or hospital. They’ve purchased a narrow-network insurance plan, with a low premium but few specialists who accept that insurance.7
The two largest hospital chains in Houston—Houston Methodist and Memorial Hermann—as well as Houston’s MD Anderson Cancer Center, don’t participate in the Blue Cross Blue Shield HMO Silver plan, a plan popular with low-income consumers because of its low premium.7
Will the government take action?
The ACA actually guards against overly narrow networks and established the first national standard for network adequacy—a standard that needs fuller development, for sure. Plans sold on the exchanges are required to establish networks that include, among other providers, essential community providers, who typically care for mostly low-income and medically underserved populations. Networks also must include sufficient numbers and types of providers, including “providers that specialize in mental health and substance abuse services, to assure that all services will be accessible without unreasonable delay.”8
Insurers also must provide people who are considering purchasing their products with an accurate directory—both online and a hard copy—identifying providers not accepting new patients in the network. And plans are prohibited from charging out-of-network cost-sharing for emergency services.
Much of the oversight and many of the details—how much is adequate? what is unreasonable?—are left to the states, many of which have years of experience grappling with the downsides and delicate balance of networks.
The Urban Institute points out that Vermont and Delaware set standards for maximum geographic distance and drive times for primary care services. In California, plans must make it easy for consumers to reach urban providers on public transportation.6
Professional societies are taking note
Today, the misuse of narrow networks by exchange plans also has gotten the attention of the American Medical Association, ACOG, and many other national medical specialty societies, in addition to the states and federal government.
The trick, many health-care policy experts agree, is to find the right balance. How broad can the network be before premiums soar? Most agree that consumers must be able to choose between plans with confidence, without any cost or access surprises, meaning much better transparency. And many agree that provider quality, in addition to cost, has to find its way into the equation.
This year, the Center for Consumer Information and Insurance Oversight, a part of the federal Department of Health and Human Services created by the ACA to investigate these kinds of issues, is investigating access to hospital systems, mental health services, oncology, and primary care providers and is developing time, distance, and other standards that insurers will have to adhere to.
Employer groups oppose strong standards or limits on narrow networks. Recently, representatives of the US Chamber of Commerce, the National Retail Federation, and others warned Congress to stay out of this fight. They understand that more generous networks mean higher premiums. These employer representative groups prefer to strengthen consumer protections like directories and keep low the cost of health insurance that they provide for their employees.
Acknowledgment
The author acknowledges the work and expertise of ACOG's state government affairs team for the state analysis—Kathryn Moore, Director, and Kate Vlach, Senior Manager—as well as advocacy partners.
Share your thoughts on this article! Send your Letter to the Editor to [email protected]. Please include your name and the city and state in which you practice.
1. Internal Revenue Service. SOI Tax States, Table 1, Returns of Active Corporations, Form 1120S. http://www.irs.gov/uac/SOI-Tax-Stats-Table-1-Returns-of-Active-Corporations,-Form-1120S. Updated June 27, 2014. Accessed September 4, 2014.
2. DeSilver D. What is a ‘closely held corporation,’ anyway, and how many are there? Pew Research Center: Fact Tank. http://www.pewresearch.org/fact-tank/2014/07/07/what-is-a-closely-held-corporation-anyway-and-how-many-are-there/. Published July 7, 2014. Accessed September 4, 2014.
3. Murray P. Protect Women’s Health From Corporate Interference Act: Summary. http://www.murray.senate.gov/public/_cache/files/30554052-0f84-485a-babc-ccc04af85bb6/protect-women-s-health-from-corporate-interference-act---one-page-summary---final.pdf. Accessed September 4, 2014.
4. The Commonwealth Fund. New Survey: After First ACA Enrollment Period, Uninsured Rate Dropped from 20% to 15%; Largest Declines Among Young Adults, Latinos, and Low-Income People. http://www.commonwealthfund.org/publications/press-releases/2014/jul/after-first-aca -enrollment-period. Published July 10,2014. Accessed September 4, 2014.
5. Artiga S, Stephens J, Rudowitz R, Perry M. What Worked and What’s Next? Strategies in Four States Leading ACA Enrollment Efforts. Kaiser Family Foundation. http://kff.org/health-reform/issue-brief/what-worked-and-whats-next-strategies-in-four-states-leading-aca-enrollment-efforts/. Published July 16, 2014. Accessed September 4, 2014.
6. Corlette S, Volk J. Narrow Provider Networks in New Health Plans: Balancing Affordability with Access to Quality Care. Urban Institute: Georgetown University Center on Health Insurance Reforms. http://www.urban.org/UploadedPDF/413135-New-Provider-Networks-in-New-Health-Plans.pdf. Published May 2014. Accessed September 4, 2014.
7. Feibel C. Patients With Low-Cost Insurance Struggle to Find Specialists. National Public Radio. http://www.npr.org/blogs/health/2014/07/16/331419293/patients-with-low-cost-insurance-struggle-to-find-specialists. Published July 16, 2014. Accessed September 4, 2014.
8. Patient Protection and Affordable Care Act: Preexisting Condition Exclusions, Lifetime and Annual Limits, Rescissions, and Patient Protections. US Department of Health and Human Services. http://www.regulations.go/#!documentDetail;D=HHS-OS-2010-0014-0001. Published June 28, 2010. Accessed September 9, 2014.
mmmm
When I last wrote about the Affordable Care Act (ACA), in May 2014, I focused on the contraception issue. Since then, the US Supreme Court ruled, in Burwell v. Hobby Lobby, that closely held, for-profit companies with religious objections to covering birth control can opt out of the requirement to provide contraceptive coverage to their employees.
In this article, I explore that decision and what it means for women’s health. I also present data on the uninsured rate in the United States, which has dropped significantly since enactment of the ACA, and I discuss one increasingly common barrier to access to care—the use of narrow networks by insurers.
A corporation now can hold a religious belief
The Supreme Court’s majority 5-4 ruling recognized, for the first time, that a for-profit corporation can hold a religious belief, but the Court limited this claim to closely held corporations. The Court also decided that the ACA placed a substantial burden on the corporations’ religious beliefs and concluded that there are less burdensome ways to accomplish the law’s intent, rendering the contraceptive coverage provision in the ACA in violation of the Religious Freedom Restoration Act (RFRA). The Court limited its ruling to the contraceptive coverage requirement, essentially turning the requirement into an option for many employers.
Are contraceptives abortifacients?
The religious belief at the center of Burwell v. Hobby Lobby was that life begins at conception, which the Green family—the owners of Hobby Lobby—equate to fertilization. Hobby Lobby’s attorneys also asserted that four contraceptives approved by the US Food and Drug Administration and included in the ACA mandate may prevent implantation of a fertilized egg, thereby constituting abortion.
Although there is no scientific answer as to when life begins, ACOG and the medical community agree that pregnancy begins at implantation. In its amicus brief to the US Supreme Court, ACOG asserted the medical community’s consensus that the four contraceptives prevent pregnancy rather than end it, and are not abortifacients:
- emergency contraceptive pills: levonorgestrel (Plan B) and its generic equivalents and ulipristal acetate (ella)
- the copper IUD (ParaGard)
- levonorgestrel-releasing intrauterine systems (Mirena, Skyla).
What is a closely held corporation?
In general, according to the Pew Research Center, a closely held corporation is a private company (not publicly traded) with a limited number of shareholders. The Internal Revenue Service (IRS), an important source, defines a closely held corporation as one in which more than half of the stock is owned (directly or indirectly) by five or fewer individuals at any time in the second half of the year.
“S” corporations are also considered closely held. These are corporations with 100 or fewer shareholders, with all members of the same family counted as one shareholder. “S” corporations don’t pay income tax; their shareholders pay tax on their personal returns, based on the corporations’ profits and losses.
Hobby Lobby is organized as an “S” corporation. According to the IRS, in 2011, there were 4,158,572 “S” corporations, 99.4% of them with 10 or fewer shareholders.1
The US Census Bureau estimates that, in 2012, about 2.9 million “S” corporations employed more than 29 million people. Many closely held corporations are quite large.2 According to the Pew Research Center, family-owned Cargill employs 140,000 people and had $136.7 billion in revenue in fiscal 2013. Hobby Lobby has estimated revenues of $3.3 billion and 23,000 employees.2
What’s next?
ACOG helped secure coverage of contraceptives in the ACA and is working with the US Congress and our women’s health partners to restore this important care. Days after the Supreme Court decision, Senator Patty Murray (D-WA) introduced the Protect Women’s Health from Corporate Interference Act, S. 2578, with 46 cosponsors as of this writing. ACOG fully supports this bill, also known as the “Not My Boss’ Business Bill,” which would reestablish the contraceptive coverage mandate as well as other care required by federal law. This bill still maintains the exemption from contraceptive coverage for houses of worship and the accommodation for religious nonprofits.
In introducing her bill, Senator Murray pointed out that “the contraceptive coverage requirement has already made a tremendous difference in women’s lives—24 million more prescriptions for oral contraceptives were filled with no copay in 2013 than in 2012, and women have saved $483 million in out-of-pocket costs for oral contraceptives.”3
Uninsured rate is declining
The Commonwealth Fund shows that, from July–September 2013 to April–June 2014, the nation’s uninsured rate fell from 20% to 15%, resulting in 9.5 million fewer uninsured adults.4 The biggest drop occurred among young adults, with the uninsured rate falling from 28% to 18%, and in states that adopted the Medicaid expansion, where uninsured rates fell from 28% to 17%.4
States that didn’t expand their Medicaid program didn’t show any noticeable change, with the uninsured rate declining only two points, from 38% to 36%.4
Coverage resulted in access to care for the majority of the newly covered. Sixty percent of people with new coverage visited a provider or hospital or paid for a prescription. Sixty-two percent of these individuals said they wouldn’t have been able to access this care before getting this coverage. Eighty-one percent of people with new coverage said they were better off now than before.4
ACA works better in some states than others
The Kaiser Family Foundation looked at four successful states—Colorado, Connecticut, Kentucky, and Washington state—to see what lessons can be learned. Important commonalities include the fact that the states run their own marketplace, adopted the Medi-caid expansion, and conducted extensive outreach and public education, including engaging providers in patient outreach and enrollment.5
Other tools of success were developing good marketing and branding, providing consumer-friendly assistance, and attention to systems and operations.5
How the Hobby Lobby decision affects individual states
Because the Supreme Court’s decision concerned interpretation of a federal law—the Religious Freedom Restoration Act (RFRA)—it does not supersede state laws that mandate coverage of contraceptives.
Twenty-eight states have laws or rulings requiring insurers to cover contraceptives, most of them dating from the 1990s and providing some exemption for religious insurers or plans. Only Illinois allows an exemption for secular bodies.
Although these state laws remain in effect, state officials may opt to stop enforcing them with regard to certain companies. For example, after the Hobby Lobby decision, Wisconsin officials announced that they no longer will enforce contraceptive coverage when a company has a religious objection.
For companies that self-fund or self-insure worker health coverage, the state coverage laws don’t apply—only federal law does. These companies do not have to adhere to state insurance mandates.
Some states have their own version of the RFRA. See the chart at right for details on a state-by-state basis.
The Supreme Court ruling also has no effect on state laws that guarantee access to emergency contraception in hospital emergency departments and that require pharmacists to dispense contraceptives.
| State | Contraceptive equity law? | Employer/insurer exemption to equity law? | Religious freedom law? |
| Alabama | ✔ | ||
| Alaska | |||
| Arizona | ✔ | ✔ | ✔ |
| Arkansas | ✔ | ✔ | |
| California | ✔ | ✔ | |
| Colorado | ✔ | ||
| Connecticut | ✔ | ✔ | ✔ |
| Delaware | ✔ | ✔ | |
| Florida | ✔ | ||
| Georgia | ✔ | ||
| Hawaii | ✔ | ✔ | |
| Idaho | ✔ | ||
| Illinois | ✔ | ✔ | ✔ |
| Indiana | |||
| Iowa | ✔ | ||
| Kansas | |||
| Kentucky | ✔ | ||
| Louisiana | ✔ | ||
| Maine | ✔ | ✔ | |
| Maryland | ✔ | ✔ | |
| Massachusetts | ✔ | ✔ | |
| Michigan | ✔ | ✔ | |
| Minnesota | |||
| Mississippi | ✔ | ||
| Missouri | ✔ | ✔ | ✔ |
| Montana | ✔ | ||
| Nebraska | |||
| Nevada | ✔ | ✔ | |
| New Hampshire | ✔ | ||
| New Jersey | ✔ | ✔ | |
| New Mexico | ✔ | ✔ | ✔ |
| New York | ✔ | ✔ | |
| North Carolina | ✔ | ✔ | |
| North Dakota | |||
| Ohio | |||
| Oklahoma | ✔ | ||
| Oregon | ✔ | ✔ | |
| Pennsylvania | ✔ | ||
| Rhode Island | ✔ | ✔ | ✔ |
| South Carolina | ✔ | ||
| South Dakota | |||
| Tennessee | ✔ | ||
| Texas | ✔ | ||
| Utah | |||
| Vermont | ✔ | ||
| Virginia | ✔ | ||
| Washington | ✔ | ||
| West Virginia | ✔ | ✔ | |
| Wisconsin | ✔ | ||
| Wyoming | |||
| TOTAL | 28 | 20 | 18 |
Narrow networks limit access to care
Huge concerns abound regarding implementation and real-life experiences related to the ACA. A number of them—high deductibles, low payment rates, limited access to physicians, long drive and wait times—can be related to “narrow networks.” Insurers exclude certain providers and offer all providers lower payment rates (which leads some physicians to drop out of the plan); they also create tiers (charging consumers lower copays and deductibles for using inner-tier preferred providers and high out-of-pocket costs for using other providers, even though they may be in the network).
Narrow networks work for insurers as an effective tool for lowering provider payment rates to keep premiums low and gain market share. The narrower the network, the lower are physician payments and premiums.
The ACA promises expanded access to high-quality, affordable health care for millions of Americans—a promise being compromised in many areas of the country through narrow networks. In these instances, insurers offering new plans in a health-care marketplace limit patient access to the numbers, types, and locations of physicians and hospitals covered under certain plans. Insurers typically offer patients low premiums, offer selected providers a high volume of patients at low payment levels, and exclude other providers whom the insurer deems to be high-cost.
Narrow networks aren’t new
As with so many elements of the ACA, narrow networks aren’t a new phenomenon. Many of us remember the public relations price that HMOs paid in the 1980s and 1990s for exceedingly limiting patients’ access to care while charging low premiums. The consumer outcry led the National Association of Insurance Commissioners to urge states to require managed-care plans to maintain adequate networks, the approach adopted by the federal government in the ACA.6
The pendulum swung in the next decade to broader networks in which consumers had much greater access, but premiums increased by an average of 11% per year.6 Employers then pushed insurers to reduce premium costs, leading back to narrow networks in the years just before the ACA. Narrow network plans accounted for 23% of all employer-sponsored plans in 2012, up from 15% in 2007.6
Increasing consolidation contributes to narrow networks
The trend toward narrower networks is also linked to increasing consolidation in health care. As health systems grow and individual or small group practices disappear, insurers rely on being able to credibly threaten to exclude systems and big groups from their networks as leverage in payment negotiations. By restricting the choice of providers in a plan, the insurer can promise more customers for the doctors and hospitals that are included, and negotiate lower payments to those providers.
The downside for physicians is clear:
- low payment rates
- exclusion from networks and coverage
- inability to refer patients to providers the physician determines to be best for that patient’s needs.
- The downside for patients:
- If they have to go out of network to get needed care, they may end up paying high out-of-pocket costs
- If they delay or forego care, their health may suffer significantly.
The insurance industry’s position is that patients have choices. Plans with access to more hospitals and specialists are available but usually at a higher price.
Narrow networks are one way to achieve low premiums
In the months leading up to ACA enactment, insurers got to work developing plans designed to be sold on the exchanges that would attract consumers through low-cost premiums and still maximize profits, especially now that insurers, under the ACA, are barred from excluding sick enrollees or increasing premiums for women, in addition to other important protections.
In previous articles, we’ve explored these landmark protections. Insurers in the individual market used to be able to keep premiums relatively low, and profits up, through use of preexisting coverage exclusions, benefit exclusions including noncoverage for maternity care or prescription drugs, and high cost sharing. Not anymore.
Since enactment of the ACA, narrow networks seem to be the preferred, and most effective, payment negotiation tool of many insurers offering plans through the exchanges, reflecting the trend we’re already seeing in the private health insurance marketplace.
NPR spotlights the difficulty of finding a specialist
The consumer and provider problems of narrow networks have been gaining attention in the media. In July, the National Public Radio (NPR) Web site carried an article entitled, “Patients with low-cost insurance struggle to find specialists,” with a key subtitle: “So you found an exchange plan. But can you find a provider?”7
In the NPR article, author Carrie Feibel reported on the situation in a majority-immigrant area of southwest Houston.
There, many patients at the local clinic have health insurance coverage for the first time, an important step toward healthier lives for themselves and their families. But many people in need of a specialist are learning that their insurance card doesn’t guarantee them access to a needed surgeon or hospital. They’ve purchased a narrow-network insurance plan, with a low premium but few specialists who accept that insurance.7
The two largest hospital chains in Houston—Houston Methodist and Memorial Hermann—as well as Houston’s MD Anderson Cancer Center, don’t participate in the Blue Cross Blue Shield HMO Silver plan, a plan popular with low-income consumers because of its low premium.7
Will the government take action?
The ACA actually guards against overly narrow networks and established the first national standard for network adequacy—a standard that needs fuller development, for sure. Plans sold on the exchanges are required to establish networks that include, among other providers, essential community providers, who typically care for mostly low-income and medically underserved populations. Networks also must include sufficient numbers and types of providers, including “providers that specialize in mental health and substance abuse services, to assure that all services will be accessible without unreasonable delay.”8
Insurers also must provide people who are considering purchasing their products with an accurate directory—both online and a hard copy—identifying providers not accepting new patients in the network. And plans are prohibited from charging out-of-network cost-sharing for emergency services.
Much of the oversight and many of the details—how much is adequate? what is unreasonable?—are left to the states, many of which have years of experience grappling with the downsides and delicate balance of networks.
The Urban Institute points out that Vermont and Delaware set standards for maximum geographic distance and drive times for primary care services. In California, plans must make it easy for consumers to reach urban providers on public transportation.6
Professional societies are taking note
Today, the misuse of narrow networks by exchange plans also has gotten the attention of the American Medical Association, ACOG, and many other national medical specialty societies, in addition to the states and federal government.
The trick, many health-care policy experts agree, is to find the right balance. How broad can the network be before premiums soar? Most agree that consumers must be able to choose between plans with confidence, without any cost or access surprises, meaning much better transparency. And many agree that provider quality, in addition to cost, has to find its way into the equation.
This year, the Center for Consumer Information and Insurance Oversight, a part of the federal Department of Health and Human Services created by the ACA to investigate these kinds of issues, is investigating access to hospital systems, mental health services, oncology, and primary care providers and is developing time, distance, and other standards that insurers will have to adhere to.
Employer groups oppose strong standards or limits on narrow networks. Recently, representatives of the US Chamber of Commerce, the National Retail Federation, and others warned Congress to stay out of this fight. They understand that more generous networks mean higher premiums. These employer representative groups prefer to strengthen consumer protections like directories and keep low the cost of health insurance that they provide for their employees.
Acknowledgment
The author acknowledges the work and expertise of ACOG's state government affairs team for the state analysis—Kathryn Moore, Director, and Kate Vlach, Senior Manager—as well as advocacy partners.
Share your thoughts on this article! Send your Letter to the Editor to [email protected]. Please include your name and the city and state in which you practice.
mmmm
When I last wrote about the Affordable Care Act (ACA), in May 2014, I focused on the contraception issue. Since then, the US Supreme Court ruled, in Burwell v. Hobby Lobby, that closely held, for-profit companies with religious objections to covering birth control can opt out of the requirement to provide contraceptive coverage to their employees.
In this article, I explore that decision and what it means for women’s health. I also present data on the uninsured rate in the United States, which has dropped significantly since enactment of the ACA, and I discuss one increasingly common barrier to access to care—the use of narrow networks by insurers.
A corporation now can hold a religious belief
The Supreme Court’s majority 5-4 ruling recognized, for the first time, that a for-profit corporation can hold a religious belief, but the Court limited this claim to closely held corporations. The Court also decided that the ACA placed a substantial burden on the corporations’ religious beliefs and concluded that there are less burdensome ways to accomplish the law’s intent, rendering the contraceptive coverage provision in the ACA in violation of the Religious Freedom Restoration Act (RFRA). The Court limited its ruling to the contraceptive coverage requirement, essentially turning the requirement into an option for many employers.
Are contraceptives abortifacients?
The religious belief at the center of Burwell v. Hobby Lobby was that life begins at conception, which the Green family—the owners of Hobby Lobby—equate to fertilization. Hobby Lobby’s attorneys also asserted that four contraceptives approved by the US Food and Drug Administration and included in the ACA mandate may prevent implantation of a fertilized egg, thereby constituting abortion.
Although there is no scientific answer as to when life begins, ACOG and the medical community agree that pregnancy begins at implantation. In its amicus brief to the US Supreme Court, ACOG asserted the medical community’s consensus that the four contraceptives prevent pregnancy rather than end it, and are not abortifacients:
- emergency contraceptive pills: levonorgestrel (Plan B) and its generic equivalents and ulipristal acetate (ella)
- the copper IUD (ParaGard)
- levonorgestrel-releasing intrauterine systems (Mirena, Skyla).
What is a closely held corporation?
In general, according to the Pew Research Center, a closely held corporation is a private company (not publicly traded) with a limited number of shareholders. The Internal Revenue Service (IRS), an important source, defines a closely held corporation as one in which more than half of the stock is owned (directly or indirectly) by five or fewer individuals at any time in the second half of the year.
“S” corporations are also considered closely held. These are corporations with 100 or fewer shareholders, with all members of the same family counted as one shareholder. “S” corporations don’t pay income tax; their shareholders pay tax on their personal returns, based on the corporations’ profits and losses.
Hobby Lobby is organized as an “S” corporation. According to the IRS, in 2011, there were 4,158,572 “S” corporations, 99.4% of them with 10 or fewer shareholders.1
The US Census Bureau estimates that, in 2012, about 2.9 million “S” corporations employed more than 29 million people. Many closely held corporations are quite large.2 According to the Pew Research Center, family-owned Cargill employs 140,000 people and had $136.7 billion in revenue in fiscal 2013. Hobby Lobby has estimated revenues of $3.3 billion and 23,000 employees.2
What’s next?
ACOG helped secure coverage of contraceptives in the ACA and is working with the US Congress and our women’s health partners to restore this important care. Days after the Supreme Court decision, Senator Patty Murray (D-WA) introduced the Protect Women’s Health from Corporate Interference Act, S. 2578, with 46 cosponsors as of this writing. ACOG fully supports this bill, also known as the “Not My Boss’ Business Bill,” which would reestablish the contraceptive coverage mandate as well as other care required by federal law. This bill still maintains the exemption from contraceptive coverage for houses of worship and the accommodation for religious nonprofits.
In introducing her bill, Senator Murray pointed out that “the contraceptive coverage requirement has already made a tremendous difference in women’s lives—24 million more prescriptions for oral contraceptives were filled with no copay in 2013 than in 2012, and women have saved $483 million in out-of-pocket costs for oral contraceptives.”3
Uninsured rate is declining
The Commonwealth Fund shows that, from July–September 2013 to April–June 2014, the nation’s uninsured rate fell from 20% to 15%, resulting in 9.5 million fewer uninsured adults.4 The biggest drop occurred among young adults, with the uninsured rate falling from 28% to 18%, and in states that adopted the Medicaid expansion, where uninsured rates fell from 28% to 17%.4
States that didn’t expand their Medicaid program didn’t show any noticeable change, with the uninsured rate declining only two points, from 38% to 36%.4
Coverage resulted in access to care for the majority of the newly covered. Sixty percent of people with new coverage visited a provider or hospital or paid for a prescription. Sixty-two percent of these individuals said they wouldn’t have been able to access this care before getting this coverage. Eighty-one percent of people with new coverage said they were better off now than before.4
ACA works better in some states than others
The Kaiser Family Foundation looked at four successful states—Colorado, Connecticut, Kentucky, and Washington state—to see what lessons can be learned. Important commonalities include the fact that the states run their own marketplace, adopted the Medi-caid expansion, and conducted extensive outreach and public education, including engaging providers in patient outreach and enrollment.5
Other tools of success were developing good marketing and branding, providing consumer-friendly assistance, and attention to systems and operations.5
How the Hobby Lobby decision affects individual states
Because the Supreme Court’s decision concerned interpretation of a federal law—the Religious Freedom Restoration Act (RFRA)—it does not supersede state laws that mandate coverage of contraceptives.
Twenty-eight states have laws or rulings requiring insurers to cover contraceptives, most of them dating from the 1990s and providing some exemption for religious insurers or plans. Only Illinois allows an exemption for secular bodies.
Although these state laws remain in effect, state officials may opt to stop enforcing them with regard to certain companies. For example, after the Hobby Lobby decision, Wisconsin officials announced that they no longer will enforce contraceptive coverage when a company has a religious objection.
For companies that self-fund or self-insure worker health coverage, the state coverage laws don’t apply—only federal law does. These companies do not have to adhere to state insurance mandates.
Some states have their own version of the RFRA. See the chart at right for details on a state-by-state basis.
The Supreme Court ruling also has no effect on state laws that guarantee access to emergency contraception in hospital emergency departments and that require pharmacists to dispense contraceptives.
| State | Contraceptive equity law? | Employer/insurer exemption to equity law? | Religious freedom law? |
| Alabama | ✔ | ||
| Alaska | |||
| Arizona | ✔ | ✔ | ✔ |
| Arkansas | ✔ | ✔ | |
| California | ✔ | ✔ | |
| Colorado | ✔ | ||
| Connecticut | ✔ | ✔ | ✔ |
| Delaware | ✔ | ✔ | |
| Florida | ✔ | ||
| Georgia | ✔ | ||
| Hawaii | ✔ | ✔ | |
| Idaho | ✔ | ||
| Illinois | ✔ | ✔ | ✔ |
| Indiana | |||
| Iowa | ✔ | ||
| Kansas | |||
| Kentucky | ✔ | ||
| Louisiana | ✔ | ||
| Maine | ✔ | ✔ | |
| Maryland | ✔ | ✔ | |
| Massachusetts | ✔ | ✔ | |
| Michigan | ✔ | ✔ | |
| Minnesota | |||
| Mississippi | ✔ | ||
| Missouri | ✔ | ✔ | ✔ |
| Montana | ✔ | ||
| Nebraska | |||
| Nevada | ✔ | ✔ | |
| New Hampshire | ✔ | ||
| New Jersey | ✔ | ✔ | |
| New Mexico | ✔ | ✔ | ✔ |
| New York | ✔ | ✔ | |
| North Carolina | ✔ | ✔ | |
| North Dakota | |||
| Ohio | |||
| Oklahoma | ✔ | ||
| Oregon | ✔ | ✔ | |
| Pennsylvania | ✔ | ||
| Rhode Island | ✔ | ✔ | ✔ |
| South Carolina | ✔ | ||
| South Dakota | |||
| Tennessee | ✔ | ||
| Texas | ✔ | ||
| Utah | |||
| Vermont | ✔ | ||
| Virginia | ✔ | ||
| Washington | ✔ | ||
| West Virginia | ✔ | ✔ | |
| Wisconsin | ✔ | ||
| Wyoming | |||
| TOTAL | 28 | 20 | 18 |
Narrow networks limit access to care
Huge concerns abound regarding implementation and real-life experiences related to the ACA. A number of them—high deductibles, low payment rates, limited access to physicians, long drive and wait times—can be related to “narrow networks.” Insurers exclude certain providers and offer all providers lower payment rates (which leads some physicians to drop out of the plan); they also create tiers (charging consumers lower copays and deductibles for using inner-tier preferred providers and high out-of-pocket costs for using other providers, even though they may be in the network).
Narrow networks work for insurers as an effective tool for lowering provider payment rates to keep premiums low and gain market share. The narrower the network, the lower are physician payments and premiums.
The ACA promises expanded access to high-quality, affordable health care for millions of Americans—a promise being compromised in many areas of the country through narrow networks. In these instances, insurers offering new plans in a health-care marketplace limit patient access to the numbers, types, and locations of physicians and hospitals covered under certain plans. Insurers typically offer patients low premiums, offer selected providers a high volume of patients at low payment levels, and exclude other providers whom the insurer deems to be high-cost.
Narrow networks aren’t new
As with so many elements of the ACA, narrow networks aren’t a new phenomenon. Many of us remember the public relations price that HMOs paid in the 1980s and 1990s for exceedingly limiting patients’ access to care while charging low premiums. The consumer outcry led the National Association of Insurance Commissioners to urge states to require managed-care plans to maintain adequate networks, the approach adopted by the federal government in the ACA.6
The pendulum swung in the next decade to broader networks in which consumers had much greater access, but premiums increased by an average of 11% per year.6 Employers then pushed insurers to reduce premium costs, leading back to narrow networks in the years just before the ACA. Narrow network plans accounted for 23% of all employer-sponsored plans in 2012, up from 15% in 2007.6
Increasing consolidation contributes to narrow networks
The trend toward narrower networks is also linked to increasing consolidation in health care. As health systems grow and individual or small group practices disappear, insurers rely on being able to credibly threaten to exclude systems and big groups from their networks as leverage in payment negotiations. By restricting the choice of providers in a plan, the insurer can promise more customers for the doctors and hospitals that are included, and negotiate lower payments to those providers.
The downside for physicians is clear:
- low payment rates
- exclusion from networks and coverage
- inability to refer patients to providers the physician determines to be best for that patient’s needs.
- The downside for patients:
- If they have to go out of network to get needed care, they may end up paying high out-of-pocket costs
- If they delay or forego care, their health may suffer significantly.
The insurance industry’s position is that patients have choices. Plans with access to more hospitals and specialists are available but usually at a higher price.
Narrow networks are one way to achieve low premiums
In the months leading up to ACA enactment, insurers got to work developing plans designed to be sold on the exchanges that would attract consumers through low-cost premiums and still maximize profits, especially now that insurers, under the ACA, are barred from excluding sick enrollees or increasing premiums for women, in addition to other important protections.
In previous articles, we’ve explored these landmark protections. Insurers in the individual market used to be able to keep premiums relatively low, and profits up, through use of preexisting coverage exclusions, benefit exclusions including noncoverage for maternity care or prescription drugs, and high cost sharing. Not anymore.
Since enactment of the ACA, narrow networks seem to be the preferred, and most effective, payment negotiation tool of many insurers offering plans through the exchanges, reflecting the trend we’re already seeing in the private health insurance marketplace.
NPR spotlights the difficulty of finding a specialist
The consumer and provider problems of narrow networks have been gaining attention in the media. In July, the National Public Radio (NPR) Web site carried an article entitled, “Patients with low-cost insurance struggle to find specialists,” with a key subtitle: “So you found an exchange plan. But can you find a provider?”7
In the NPR article, author Carrie Feibel reported on the situation in a majority-immigrant area of southwest Houston.
There, many patients at the local clinic have health insurance coverage for the first time, an important step toward healthier lives for themselves and their families. But many people in need of a specialist are learning that their insurance card doesn’t guarantee them access to a needed surgeon or hospital. They’ve purchased a narrow-network insurance plan, with a low premium but few specialists who accept that insurance.7
The two largest hospital chains in Houston—Houston Methodist and Memorial Hermann—as well as Houston’s MD Anderson Cancer Center, don’t participate in the Blue Cross Blue Shield HMO Silver plan, a plan popular with low-income consumers because of its low premium.7
Will the government take action?
The ACA actually guards against overly narrow networks and established the first national standard for network adequacy—a standard that needs fuller development, for sure. Plans sold on the exchanges are required to establish networks that include, among other providers, essential community providers, who typically care for mostly low-income and medically underserved populations. Networks also must include sufficient numbers and types of providers, including “providers that specialize in mental health and substance abuse services, to assure that all services will be accessible without unreasonable delay.”8
Insurers also must provide people who are considering purchasing their products with an accurate directory—both online and a hard copy—identifying providers not accepting new patients in the network. And plans are prohibited from charging out-of-network cost-sharing for emergency services.
Much of the oversight and many of the details—how much is adequate? what is unreasonable?—are left to the states, many of which have years of experience grappling with the downsides and delicate balance of networks.
The Urban Institute points out that Vermont and Delaware set standards for maximum geographic distance and drive times for primary care services. In California, plans must make it easy for consumers to reach urban providers on public transportation.6
Professional societies are taking note
Today, the misuse of narrow networks by exchange plans also has gotten the attention of the American Medical Association, ACOG, and many other national medical specialty societies, in addition to the states and federal government.
The trick, many health-care policy experts agree, is to find the right balance. How broad can the network be before premiums soar? Most agree that consumers must be able to choose between plans with confidence, without any cost or access surprises, meaning much better transparency. And many agree that provider quality, in addition to cost, has to find its way into the equation.
This year, the Center for Consumer Information and Insurance Oversight, a part of the federal Department of Health and Human Services created by the ACA to investigate these kinds of issues, is investigating access to hospital systems, mental health services, oncology, and primary care providers and is developing time, distance, and other standards that insurers will have to adhere to.
Employer groups oppose strong standards or limits on narrow networks. Recently, representatives of the US Chamber of Commerce, the National Retail Federation, and others warned Congress to stay out of this fight. They understand that more generous networks mean higher premiums. These employer representative groups prefer to strengthen consumer protections like directories and keep low the cost of health insurance that they provide for their employees.
Acknowledgment
The author acknowledges the work and expertise of ACOG's state government affairs team for the state analysis—Kathryn Moore, Director, and Kate Vlach, Senior Manager—as well as advocacy partners.
Share your thoughts on this article! Send your Letter to the Editor to [email protected]. Please include your name and the city and state in which you practice.
1. Internal Revenue Service. SOI Tax States, Table 1, Returns of Active Corporations, Form 1120S. http://www.irs.gov/uac/SOI-Tax-Stats-Table-1-Returns-of-Active-Corporations,-Form-1120S. Updated June 27, 2014. Accessed September 4, 2014.
2. DeSilver D. What is a ‘closely held corporation,’ anyway, and how many are there? Pew Research Center: Fact Tank. http://www.pewresearch.org/fact-tank/2014/07/07/what-is-a-closely-held-corporation-anyway-and-how-many-are-there/. Published July 7, 2014. Accessed September 4, 2014.
3. Murray P. Protect Women’s Health From Corporate Interference Act: Summary. http://www.murray.senate.gov/public/_cache/files/30554052-0f84-485a-babc-ccc04af85bb6/protect-women-s-health-from-corporate-interference-act---one-page-summary---final.pdf. Accessed September 4, 2014.
4. The Commonwealth Fund. New Survey: After First ACA Enrollment Period, Uninsured Rate Dropped from 20% to 15%; Largest Declines Among Young Adults, Latinos, and Low-Income People. http://www.commonwealthfund.org/publications/press-releases/2014/jul/after-first-aca -enrollment-period. Published July 10,2014. Accessed September 4, 2014.
5. Artiga S, Stephens J, Rudowitz R, Perry M. What Worked and What’s Next? Strategies in Four States Leading ACA Enrollment Efforts. Kaiser Family Foundation. http://kff.org/health-reform/issue-brief/what-worked-and-whats-next-strategies-in-four-states-leading-aca-enrollment-efforts/. Published July 16, 2014. Accessed September 4, 2014.
6. Corlette S, Volk J. Narrow Provider Networks in New Health Plans: Balancing Affordability with Access to Quality Care. Urban Institute: Georgetown University Center on Health Insurance Reforms. http://www.urban.org/UploadedPDF/413135-New-Provider-Networks-in-New-Health-Plans.pdf. Published May 2014. Accessed September 4, 2014.
7. Feibel C. Patients With Low-Cost Insurance Struggle to Find Specialists. National Public Radio. http://www.npr.org/blogs/health/2014/07/16/331419293/patients-with-low-cost-insurance-struggle-to-find-specialists. Published July 16, 2014. Accessed September 4, 2014.
8. Patient Protection and Affordable Care Act: Preexisting Condition Exclusions, Lifetime and Annual Limits, Rescissions, and Patient Protections. US Department of Health and Human Services. http://www.regulations.go/#!documentDetail;D=HHS-OS-2010-0014-0001. Published June 28, 2010. Accessed September 9, 2014.
1. Internal Revenue Service. SOI Tax States, Table 1, Returns of Active Corporations, Form 1120S. http://www.irs.gov/uac/SOI-Tax-Stats-Table-1-Returns-of-Active-Corporations,-Form-1120S. Updated June 27, 2014. Accessed September 4, 2014.
2. DeSilver D. What is a ‘closely held corporation,’ anyway, and how many are there? Pew Research Center: Fact Tank. http://www.pewresearch.org/fact-tank/2014/07/07/what-is-a-closely-held-corporation-anyway-and-how-many-are-there/. Published July 7, 2014. Accessed September 4, 2014.
3. Murray P. Protect Women’s Health From Corporate Interference Act: Summary. http://www.murray.senate.gov/public/_cache/files/30554052-0f84-485a-babc-ccc04af85bb6/protect-women-s-health-from-corporate-interference-act---one-page-summary---final.pdf. Accessed September 4, 2014.
4. The Commonwealth Fund. New Survey: After First ACA Enrollment Period, Uninsured Rate Dropped from 20% to 15%; Largest Declines Among Young Adults, Latinos, and Low-Income People. http://www.commonwealthfund.org/publications/press-releases/2014/jul/after-first-aca -enrollment-period. Published July 10,2014. Accessed September 4, 2014.
5. Artiga S, Stephens J, Rudowitz R, Perry M. What Worked and What’s Next? Strategies in Four States Leading ACA Enrollment Efforts. Kaiser Family Foundation. http://kff.org/health-reform/issue-brief/what-worked-and-whats-next-strategies-in-four-states-leading-aca-enrollment-efforts/. Published July 16, 2014. Accessed September 4, 2014.
6. Corlette S, Volk J. Narrow Provider Networks in New Health Plans: Balancing Affordability with Access to Quality Care. Urban Institute: Georgetown University Center on Health Insurance Reforms. http://www.urban.org/UploadedPDF/413135-New-Provider-Networks-in-New-Health-Plans.pdf. Published May 2014. Accessed September 4, 2014.
7. Feibel C. Patients With Low-Cost Insurance Struggle to Find Specialists. National Public Radio. http://www.npr.org/blogs/health/2014/07/16/331419293/patients-with-low-cost-insurance-struggle-to-find-specialists. Published July 16, 2014. Accessed September 4, 2014.
8. Patient Protection and Affordable Care Act: Preexisting Condition Exclusions, Lifetime and Annual Limits, Rescissions, and Patient Protections. US Department of Health and Human Services. http://www.regulations.go/#!documentDetail;D=HHS-OS-2010-0014-0001. Published June 28, 2010. Accessed September 9, 2014.
Inside the article:
Are contraceptives abortifacients?
How the Hobby Lobby decision affects individual states
Narrow networks limit access to care
The Affordable Care Act and contraception: Is it covered, or not?
Our specialty sees contraception as a basic element of women’s preventive care. It helps women determine and space their pregnancies; helps ensure healthier pregnancies; and helps many women with health-care concerns not related to pregnancy to better manage their symptoms and stay healthy.
The drafters of the Affordable Care Act (ACA) recognized the importance of contraception to women’s health when they guaranteed coverage of prescription contraceptives and services, including all methods approved by the US Food and Drug Administration, without deductibles or copays, to millions of women through their private health insurance. This policy was vetted and approved by the Institute of Medicine (IOM) and US Department of Health and Human Services (HHS).
The American Congress of Obstetricians and Gynecologists (ACOG) was central to these discussions. ACOG Executive Vice President and CEO Hal C. Lawrence III, MD, offered our women’s health guidelines and guidance to the IOM, the entity designated by the Secretary of HHS to recommend exactly what coverage and services should fall within the category of women’s preventive care. ACOG’s recommendations were broadly accepted by IOM and HHS and are now required coverage for women across the nation.
Related Article: ACOG to legislators: Partnership, not interference Lucia DiVenere, MA (April 2013)
So, why the confusion and controversy?
Let’s clear up the confusion first.
We’ve heard that private health plans now are required to cover contraceptives without cost sharing. But it’s a little more complicated than that.
CONTRACEPTIVE MANDATE AFFECTS NEW PLANS ONLY
It’s true that the ACA requires new private plans to cover a broad range of preventive services:
- evidence-based screenings and counseling
- routine immunizations
- childhood preventive services
- preventive services for women.
Did you catch the word “new” in that sentence?
Health plans that existed before March 23, 2010—the date the ACA was signed into law—and that haven’t changed in ways that substantially cut benefits or increase costs for consumers are considered “grandfathered plans” and are not required to abide by these and other requirements in the law.
There are two types of grandfathered plans:
- job-based plans—health insurance plans administered through employers can continue to enroll people as long as no significant changes are made to coverage
- individual plans—a grandfathered plan purchased by an individual cannot expand coverage beyond that individual.
Any insurer can cancel a grandfathered plan as long as it provides 90-day notice to the plan’s enrollees and offers other coverage options. Because grandfathered plans are exempt from a number of ACA benefits and protections, these plans are required to disclose their status to their enrollees.
The number of people enrolled in grandfathered plans is steadily decreasing. In 2013, 36% of people covered through their jobs were enrolled in a grandfathered health plan, down from 48% in 2012 and 56% in 2011, according to the Kaiser Family Foundation.1 Here’s a quick look at the consumer protections that do and do not apply to grandfathered plans.
All health plans must:
- end lifetime limits on coverage
- end arbitrary cancellations of health coverage
- cover adult children up to age 26
- provide a Summary of Benefits and Coverage, a short, easy-to-understand summary of what a plan covers and costs
- spend revenue from premiums on health care, not on administrative costs and bonuses.
Grandfathered plans don’t have to:
- cover preventive care for free, including contraceptives
- guarantee your right to appeal
- protect your choice of doctors and access to emergency care
- be held accountable through Rate Review for excessive premium increases.
Nor do grandfathered individual plans (the kind you buy yourself, not the kind you get from an employer) have to end yearly limits on coverage or cover a preexisting health condition.
Right away, then, we have a situation in which some patients may have 100% coverage for contraceptives while others don’t, especially if their plans were in effect before the ACA became law.
Nonprofits with religious ties are exempted, too
There’s a second segment of your patient population that may not have full contraceptive coverage: those who are covered through employment with a religiously affiliated nonprofit. Initially, in August 2011, only health insurance provided through employment with houses of worship was exempted from the requirement to cover contraceptives. In July 2013, this exemption was expanded to address concerns from other religious affiliates, including universities and hospitals.
This “accommodation,” as it’s known, exempts religiously affiliated nonprofits with religious objections from contracting, arranging, paying for, or referring for contraceptive coverage for their employees. Instead, their insurers are required to provide this coverage free of charge to the employer or employees—an attempt to ensure that all women have the same access to care, regardless of their employment setting. This accommodation is available only to organizations that:
- oppose the mandate to provide contraceptive coverage because of religious beliefs
- are nonprofit
- hold themselves out as religious organizations AND
- self-certify that they meet the just-stated requirements of 1–3.
Related article: As the Affordable Care Act comes of age, a look behind the headlines Lucia DiVenere, MA (January 2014)
The rule for small companies
There’s a third group that doesn’t have to provide contraceptive coverage to employees: for-profit companies with fewer than 50 workers. Under the law, these employers have two options:
- Provide no health care: This option carries no penalty but, rather, is an attempt to help small businesses, now that individuals can buy coverage on the exchanges
- Offer health care: If small businesses choose this option, their coverage must include contraceptive care.
So when your patient approaches your front desk to pay her bill, or picks up her contraceptive prescription at the pharmacy, her bill will vary, depending on the age of her plan, her employer’s religious status, and the size of the business she works for. It’s important that you check her coverage with her policy.
Now, on to the controversy.
FOR-PROFIT COMPANIES ALSO SEEK EXEMPTION
Houses of worship are exempted and religiously affiliated nonprofit organizations are offered an accommodation to avoid direct involvement with the contraceptive coverage mandate. More than 40 religiously affiliated nonprofit corporations are currently challenging the mandate, asserting that the accommodation still burdens their religious rights.
What happens when owners of a for-profit corporation claim a religious right to not offer contraceptive coverage to their employees? That’s the question currently before the US Supreme Court. As of this writing, the Court heard arguments on March 25, 2014, and is likely to hand down its decision in two cases in June. The two corporations involved are Conestoga Wood Specialties and Hobby Lobby Stores.
Under the ACA, for-profit employers do not qualify for religious exemptions or accommodations from the contraceptive coverage mandate. As we saw earlier, the mandate varies in its application to these employers by employer size. All for-profit employers with 50 or more employees must provide coverage, unless their coverage is through a grandfathered plan. Employers with fewer than 50 workers have two options. They’re not penalized if they don’t offer any health-care coverage to their employees—but if they do, that coverage must include contraception.
Both Conestoga and Hobby Lobby are major employers. Conestoga Wood has 950 full-time employees. Hobby Lobby operates 514 stores in 41 states, with more than 13,000 employees.
Lower court rulings have been conflicting
The Supreme Court agreed to review and rule on these cases largely to settle widely divergent rulings at lower court levels. As of this writing, more than 40 for-profit businesses have challenged the coverage mandate in federal court. The Conestoga and Hobby Lobby owners, like the owners of other businesses challenging the law, say that because they are religious families—Mennonite and Protestant, respectively—and they run their businesses according to their faiths, their religious views extend to their businesses. They claim that the ACA mandate violates their First Amendment right to protection of free exercise of religion as well as their rights under the 1993 Religious Freedom Restoration Act (RFRA), a law enacted to protect individuals from laws that substantially burden their exercise of religion. They are left, they assert, with a choice of providing objectionable coverage or paying a fine, a substantial burden on their freedom of religion.
The key issue before the Court is whether secular for-profit corporations can avoid complying with the legal mandates of the ACA based on the religious beliefs of their owners. To date, five federal circuit courts have ruled on the RFRA claim. Some have determined that corporations have no religious rights. Others have found the opposite. The Supreme Court will attempt to set the path for lower courts to follow.
The outcome of these cases will have a profound effect on women’s health, and may be felt much more broadly in our health-care system. If a business owner can opt out of one sort of coverage based on his or her religious beliefs, then wouldn’t that rule apply to other areas of health care? Employers might choose not to cover childhood immunizations, blood transfusions, or maternity care for single workers. Allowing employers to pick and choose can be risky business.
ACOG joins an amicus brief
ACOG partnered with a number of other preeminent health-care organizations, including the American Academy of Pediatrics, the American College of Nurse-Midwives, the American Society for Reproductive Medicine, the Society for Maternal-Fetal Medicine, Physicians for Reproductive Health, and the International Association of Forensic Nurses, to prepare an amicus brief to the Court on these cases.
The arguments we and our colleagues put forward centered on two points:
- Employers should not be allowed to interfere in the provider-patient relationship
- Allowing employers to veto coverage based on their own religious beliefs has broad and troubling public health implications.
Contraception is an essential component of women’s health care. The Supreme Court could unravel this important new guarantee or protect it for today’s and future generations.
Acknowledgment
The author thanks and acknowledges Sara Needleman Kline, JD, Deputy General Counsel, ACOG, for her helpful review and comments.
WE WANT TO HEAR FROM YOU!
Share your thoughts on this article or on any topic relevant to ObGyns and women’s health practitioners. Tell us which topics you’d like to see covered in future issues, and what challenges you face in daily practice. We will consider publishing your letter in a future issue. Send your letter to: [email protected] Please include the city and state in which you practice. Stay in touch! Your feedback is important to us!
- Kaiser Family Foundation. 2013 Employer Health Benefits Survey. http://kff.org/private-insurance/report/2013-employer-health-benefits/. Published August 20, 2013. Accessed March 27, 2014.
- Office of the US Federal Register. Definition of Grandfathered Health Plan Coverage in Paragraph (a) of 26 CFR 54.9815-1251T, 29 CFR 2590.715-1251, and 45 CFR 147.140 of These Interim Final Regulations. https://www.federalregister.gov/articles/2010/06/17/2010-14488/interim-final-rules-for-group-health-plans-and-health-insurance-coverage-relating-to-status-as-a#h-11. Published June 17, 2010. Accessed March 25, 2014.
Our specialty sees contraception as a basic element of women’s preventive care. It helps women determine and space their pregnancies; helps ensure healthier pregnancies; and helps many women with health-care concerns not related to pregnancy to better manage their symptoms and stay healthy.
The drafters of the Affordable Care Act (ACA) recognized the importance of contraception to women’s health when they guaranteed coverage of prescription contraceptives and services, including all methods approved by the US Food and Drug Administration, without deductibles or copays, to millions of women through their private health insurance. This policy was vetted and approved by the Institute of Medicine (IOM) and US Department of Health and Human Services (HHS).
The American Congress of Obstetricians and Gynecologists (ACOG) was central to these discussions. ACOG Executive Vice President and CEO Hal C. Lawrence III, MD, offered our women’s health guidelines and guidance to the IOM, the entity designated by the Secretary of HHS to recommend exactly what coverage and services should fall within the category of women’s preventive care. ACOG’s recommendations were broadly accepted by IOM and HHS and are now required coverage for women across the nation.
Related Article: ACOG to legislators: Partnership, not interference Lucia DiVenere, MA (April 2013)
So, why the confusion and controversy?
Let’s clear up the confusion first.
We’ve heard that private health plans now are required to cover contraceptives without cost sharing. But it’s a little more complicated than that.
CONTRACEPTIVE MANDATE AFFECTS NEW PLANS ONLY
It’s true that the ACA requires new private plans to cover a broad range of preventive services:
- evidence-based screenings and counseling
- routine immunizations
- childhood preventive services
- preventive services for women.
Did you catch the word “new” in that sentence?
Health plans that existed before March 23, 2010—the date the ACA was signed into law—and that haven’t changed in ways that substantially cut benefits or increase costs for consumers are considered “grandfathered plans” and are not required to abide by these and other requirements in the law.
There are two types of grandfathered plans:
- job-based plans—health insurance plans administered through employers can continue to enroll people as long as no significant changes are made to coverage
- individual plans—a grandfathered plan purchased by an individual cannot expand coverage beyond that individual.
Any insurer can cancel a grandfathered plan as long as it provides 90-day notice to the plan’s enrollees and offers other coverage options. Because grandfathered plans are exempt from a number of ACA benefits and protections, these plans are required to disclose their status to their enrollees.
The number of people enrolled in grandfathered plans is steadily decreasing. In 2013, 36% of people covered through their jobs were enrolled in a grandfathered health plan, down from 48% in 2012 and 56% in 2011, according to the Kaiser Family Foundation.1 Here’s a quick look at the consumer protections that do and do not apply to grandfathered plans.
All health plans must:
- end lifetime limits on coverage
- end arbitrary cancellations of health coverage
- cover adult children up to age 26
- provide a Summary of Benefits and Coverage, a short, easy-to-understand summary of what a plan covers and costs
- spend revenue from premiums on health care, not on administrative costs and bonuses.
Grandfathered plans don’t have to:
- cover preventive care for free, including contraceptives
- guarantee your right to appeal
- protect your choice of doctors and access to emergency care
- be held accountable through Rate Review for excessive premium increases.
Nor do grandfathered individual plans (the kind you buy yourself, not the kind you get from an employer) have to end yearly limits on coverage or cover a preexisting health condition.
Right away, then, we have a situation in which some patients may have 100% coverage for contraceptives while others don’t, especially if their plans were in effect before the ACA became law.
Nonprofits with religious ties are exempted, too
There’s a second segment of your patient population that may not have full contraceptive coverage: those who are covered through employment with a religiously affiliated nonprofit. Initially, in August 2011, only health insurance provided through employment with houses of worship was exempted from the requirement to cover contraceptives. In July 2013, this exemption was expanded to address concerns from other religious affiliates, including universities and hospitals.
This “accommodation,” as it’s known, exempts religiously affiliated nonprofits with religious objections from contracting, arranging, paying for, or referring for contraceptive coverage for their employees. Instead, their insurers are required to provide this coverage free of charge to the employer or employees—an attempt to ensure that all women have the same access to care, regardless of their employment setting. This accommodation is available only to organizations that:
- oppose the mandate to provide contraceptive coverage because of religious beliefs
- are nonprofit
- hold themselves out as religious organizations AND
- self-certify that they meet the just-stated requirements of 1–3.
Related article: As the Affordable Care Act comes of age, a look behind the headlines Lucia DiVenere, MA (January 2014)
The rule for small companies
There’s a third group that doesn’t have to provide contraceptive coverage to employees: for-profit companies with fewer than 50 workers. Under the law, these employers have two options:
- Provide no health care: This option carries no penalty but, rather, is an attempt to help small businesses, now that individuals can buy coverage on the exchanges
- Offer health care: If small businesses choose this option, their coverage must include contraceptive care.
So when your patient approaches your front desk to pay her bill, or picks up her contraceptive prescription at the pharmacy, her bill will vary, depending on the age of her plan, her employer’s religious status, and the size of the business she works for. It’s important that you check her coverage with her policy.
Now, on to the controversy.
FOR-PROFIT COMPANIES ALSO SEEK EXEMPTION
Houses of worship are exempted and religiously affiliated nonprofit organizations are offered an accommodation to avoid direct involvement with the contraceptive coverage mandate. More than 40 religiously affiliated nonprofit corporations are currently challenging the mandate, asserting that the accommodation still burdens their religious rights.
What happens when owners of a for-profit corporation claim a religious right to not offer contraceptive coverage to their employees? That’s the question currently before the US Supreme Court. As of this writing, the Court heard arguments on March 25, 2014, and is likely to hand down its decision in two cases in June. The two corporations involved are Conestoga Wood Specialties and Hobby Lobby Stores.
Under the ACA, for-profit employers do not qualify for religious exemptions or accommodations from the contraceptive coverage mandate. As we saw earlier, the mandate varies in its application to these employers by employer size. All for-profit employers with 50 or more employees must provide coverage, unless their coverage is through a grandfathered plan. Employers with fewer than 50 workers have two options. They’re not penalized if they don’t offer any health-care coverage to their employees—but if they do, that coverage must include contraception.
Both Conestoga and Hobby Lobby are major employers. Conestoga Wood has 950 full-time employees. Hobby Lobby operates 514 stores in 41 states, with more than 13,000 employees.
Lower court rulings have been conflicting
The Supreme Court agreed to review and rule on these cases largely to settle widely divergent rulings at lower court levels. As of this writing, more than 40 for-profit businesses have challenged the coverage mandate in federal court. The Conestoga and Hobby Lobby owners, like the owners of other businesses challenging the law, say that because they are religious families—Mennonite and Protestant, respectively—and they run their businesses according to their faiths, their religious views extend to their businesses. They claim that the ACA mandate violates their First Amendment right to protection of free exercise of religion as well as their rights under the 1993 Religious Freedom Restoration Act (RFRA), a law enacted to protect individuals from laws that substantially burden their exercise of religion. They are left, they assert, with a choice of providing objectionable coverage or paying a fine, a substantial burden on their freedom of religion.
The key issue before the Court is whether secular for-profit corporations can avoid complying with the legal mandates of the ACA based on the religious beliefs of their owners. To date, five federal circuit courts have ruled on the RFRA claim. Some have determined that corporations have no religious rights. Others have found the opposite. The Supreme Court will attempt to set the path for lower courts to follow.
The outcome of these cases will have a profound effect on women’s health, and may be felt much more broadly in our health-care system. If a business owner can opt out of one sort of coverage based on his or her religious beliefs, then wouldn’t that rule apply to other areas of health care? Employers might choose not to cover childhood immunizations, blood transfusions, or maternity care for single workers. Allowing employers to pick and choose can be risky business.
ACOG joins an amicus brief
ACOG partnered with a number of other preeminent health-care organizations, including the American Academy of Pediatrics, the American College of Nurse-Midwives, the American Society for Reproductive Medicine, the Society for Maternal-Fetal Medicine, Physicians for Reproductive Health, and the International Association of Forensic Nurses, to prepare an amicus brief to the Court on these cases.
The arguments we and our colleagues put forward centered on two points:
- Employers should not be allowed to interfere in the provider-patient relationship
- Allowing employers to veto coverage based on their own religious beliefs has broad and troubling public health implications.
Contraception is an essential component of women’s health care. The Supreme Court could unravel this important new guarantee or protect it for today’s and future generations.
Acknowledgment
The author thanks and acknowledges Sara Needleman Kline, JD, Deputy General Counsel, ACOG, for her helpful review and comments.
WE WANT TO HEAR FROM YOU!
Share your thoughts on this article or on any topic relevant to ObGyns and women’s health practitioners. Tell us which topics you’d like to see covered in future issues, and what challenges you face in daily practice. We will consider publishing your letter in a future issue. Send your letter to: [email protected] Please include the city and state in which you practice. Stay in touch! Your feedback is important to us!
Our specialty sees contraception as a basic element of women’s preventive care. It helps women determine and space their pregnancies; helps ensure healthier pregnancies; and helps many women with health-care concerns not related to pregnancy to better manage their symptoms and stay healthy.
The drafters of the Affordable Care Act (ACA) recognized the importance of contraception to women’s health when they guaranteed coverage of prescription contraceptives and services, including all methods approved by the US Food and Drug Administration, without deductibles or copays, to millions of women through their private health insurance. This policy was vetted and approved by the Institute of Medicine (IOM) and US Department of Health and Human Services (HHS).
The American Congress of Obstetricians and Gynecologists (ACOG) was central to these discussions. ACOG Executive Vice President and CEO Hal C. Lawrence III, MD, offered our women’s health guidelines and guidance to the IOM, the entity designated by the Secretary of HHS to recommend exactly what coverage and services should fall within the category of women’s preventive care. ACOG’s recommendations were broadly accepted by IOM and HHS and are now required coverage for women across the nation.
Related Article: ACOG to legislators: Partnership, not interference Lucia DiVenere, MA (April 2013)
So, why the confusion and controversy?
Let’s clear up the confusion first.
We’ve heard that private health plans now are required to cover contraceptives without cost sharing. But it’s a little more complicated than that.
CONTRACEPTIVE MANDATE AFFECTS NEW PLANS ONLY
It’s true that the ACA requires new private plans to cover a broad range of preventive services:
- evidence-based screenings and counseling
- routine immunizations
- childhood preventive services
- preventive services for women.
Did you catch the word “new” in that sentence?
Health plans that existed before March 23, 2010—the date the ACA was signed into law—and that haven’t changed in ways that substantially cut benefits or increase costs for consumers are considered “grandfathered plans” and are not required to abide by these and other requirements in the law.
There are two types of grandfathered plans:
- job-based plans—health insurance plans administered through employers can continue to enroll people as long as no significant changes are made to coverage
- individual plans—a grandfathered plan purchased by an individual cannot expand coverage beyond that individual.
Any insurer can cancel a grandfathered plan as long as it provides 90-day notice to the plan’s enrollees and offers other coverage options. Because grandfathered plans are exempt from a number of ACA benefits and protections, these plans are required to disclose their status to their enrollees.
The number of people enrolled in grandfathered plans is steadily decreasing. In 2013, 36% of people covered through their jobs were enrolled in a grandfathered health plan, down from 48% in 2012 and 56% in 2011, according to the Kaiser Family Foundation.1 Here’s a quick look at the consumer protections that do and do not apply to grandfathered plans.
All health plans must:
- end lifetime limits on coverage
- end arbitrary cancellations of health coverage
- cover adult children up to age 26
- provide a Summary of Benefits and Coverage, a short, easy-to-understand summary of what a plan covers and costs
- spend revenue from premiums on health care, not on administrative costs and bonuses.
Grandfathered plans don’t have to:
- cover preventive care for free, including contraceptives
- guarantee your right to appeal
- protect your choice of doctors and access to emergency care
- be held accountable through Rate Review for excessive premium increases.
Nor do grandfathered individual plans (the kind you buy yourself, not the kind you get from an employer) have to end yearly limits on coverage or cover a preexisting health condition.
Right away, then, we have a situation in which some patients may have 100% coverage for contraceptives while others don’t, especially if their plans were in effect before the ACA became law.
Nonprofits with religious ties are exempted, too
There’s a second segment of your patient population that may not have full contraceptive coverage: those who are covered through employment with a religiously affiliated nonprofit. Initially, in August 2011, only health insurance provided through employment with houses of worship was exempted from the requirement to cover contraceptives. In July 2013, this exemption was expanded to address concerns from other religious affiliates, including universities and hospitals.
This “accommodation,” as it’s known, exempts religiously affiliated nonprofits with religious objections from contracting, arranging, paying for, or referring for contraceptive coverage for their employees. Instead, their insurers are required to provide this coverage free of charge to the employer or employees—an attempt to ensure that all women have the same access to care, regardless of their employment setting. This accommodation is available only to organizations that:
- oppose the mandate to provide contraceptive coverage because of religious beliefs
- are nonprofit
- hold themselves out as religious organizations AND
- self-certify that they meet the just-stated requirements of 1–3.
Related article: As the Affordable Care Act comes of age, a look behind the headlines Lucia DiVenere, MA (January 2014)
The rule for small companies
There’s a third group that doesn’t have to provide contraceptive coverage to employees: for-profit companies with fewer than 50 workers. Under the law, these employers have two options:
- Provide no health care: This option carries no penalty but, rather, is an attempt to help small businesses, now that individuals can buy coverage on the exchanges
- Offer health care: If small businesses choose this option, their coverage must include contraceptive care.
So when your patient approaches your front desk to pay her bill, or picks up her contraceptive prescription at the pharmacy, her bill will vary, depending on the age of her plan, her employer’s religious status, and the size of the business she works for. It’s important that you check her coverage with her policy.
Now, on to the controversy.
FOR-PROFIT COMPANIES ALSO SEEK EXEMPTION
Houses of worship are exempted and religiously affiliated nonprofit organizations are offered an accommodation to avoid direct involvement with the contraceptive coverage mandate. More than 40 religiously affiliated nonprofit corporations are currently challenging the mandate, asserting that the accommodation still burdens their religious rights.
What happens when owners of a for-profit corporation claim a religious right to not offer contraceptive coverage to their employees? That’s the question currently before the US Supreme Court. As of this writing, the Court heard arguments on March 25, 2014, and is likely to hand down its decision in two cases in June. The two corporations involved are Conestoga Wood Specialties and Hobby Lobby Stores.
Under the ACA, for-profit employers do not qualify for religious exemptions or accommodations from the contraceptive coverage mandate. As we saw earlier, the mandate varies in its application to these employers by employer size. All for-profit employers with 50 or more employees must provide coverage, unless their coverage is through a grandfathered plan. Employers with fewer than 50 workers have two options. They’re not penalized if they don’t offer any health-care coverage to their employees—but if they do, that coverage must include contraception.
Both Conestoga and Hobby Lobby are major employers. Conestoga Wood has 950 full-time employees. Hobby Lobby operates 514 stores in 41 states, with more than 13,000 employees.
Lower court rulings have been conflicting
The Supreme Court agreed to review and rule on these cases largely to settle widely divergent rulings at lower court levels. As of this writing, more than 40 for-profit businesses have challenged the coverage mandate in federal court. The Conestoga and Hobby Lobby owners, like the owners of other businesses challenging the law, say that because they are religious families—Mennonite and Protestant, respectively—and they run their businesses according to their faiths, their religious views extend to their businesses. They claim that the ACA mandate violates their First Amendment right to protection of free exercise of religion as well as their rights under the 1993 Religious Freedom Restoration Act (RFRA), a law enacted to protect individuals from laws that substantially burden their exercise of religion. They are left, they assert, with a choice of providing objectionable coverage or paying a fine, a substantial burden on their freedom of religion.
The key issue before the Court is whether secular for-profit corporations can avoid complying with the legal mandates of the ACA based on the religious beliefs of their owners. To date, five federal circuit courts have ruled on the RFRA claim. Some have determined that corporations have no religious rights. Others have found the opposite. The Supreme Court will attempt to set the path for lower courts to follow.
The outcome of these cases will have a profound effect on women’s health, and may be felt much more broadly in our health-care system. If a business owner can opt out of one sort of coverage based on his or her religious beliefs, then wouldn’t that rule apply to other areas of health care? Employers might choose not to cover childhood immunizations, blood transfusions, or maternity care for single workers. Allowing employers to pick and choose can be risky business.
ACOG joins an amicus brief
ACOG partnered with a number of other preeminent health-care organizations, including the American Academy of Pediatrics, the American College of Nurse-Midwives, the American Society for Reproductive Medicine, the Society for Maternal-Fetal Medicine, Physicians for Reproductive Health, and the International Association of Forensic Nurses, to prepare an amicus brief to the Court on these cases.
The arguments we and our colleagues put forward centered on two points:
- Employers should not be allowed to interfere in the provider-patient relationship
- Allowing employers to veto coverage based on their own religious beliefs has broad and troubling public health implications.
Contraception is an essential component of women’s health care. The Supreme Court could unravel this important new guarantee or protect it for today’s and future generations.
Acknowledgment
The author thanks and acknowledges Sara Needleman Kline, JD, Deputy General Counsel, ACOG, for her helpful review and comments.
WE WANT TO HEAR FROM YOU!
Share your thoughts on this article or on any topic relevant to ObGyns and women’s health practitioners. Tell us which topics you’d like to see covered in future issues, and what challenges you face in daily practice. We will consider publishing your letter in a future issue. Send your letter to: [email protected] Please include the city and state in which you practice. Stay in touch! Your feedback is important to us!
- Kaiser Family Foundation. 2013 Employer Health Benefits Survey. http://kff.org/private-insurance/report/2013-employer-health-benefits/. Published August 20, 2013. Accessed March 27, 2014.
- Office of the US Federal Register. Definition of Grandfathered Health Plan Coverage in Paragraph (a) of 26 CFR 54.9815-1251T, 29 CFR 2590.715-1251, and 45 CFR 147.140 of These Interim Final Regulations. https://www.federalregister.gov/articles/2010/06/17/2010-14488/interim-final-rules-for-group-health-plans-and-health-insurance-coverage-relating-to-status-as-a#h-11. Published June 17, 2010. Accessed March 25, 2014.
- Kaiser Family Foundation. 2013 Employer Health Benefits Survey. http://kff.org/private-insurance/report/2013-employer-health-benefits/. Published August 20, 2013. Accessed March 27, 2014.
- Office of the US Federal Register. Definition of Grandfathered Health Plan Coverage in Paragraph (a) of 26 CFR 54.9815-1251T, 29 CFR 2590.715-1251, and 45 CFR 147.140 of These Interim Final Regulations. https://www.federalregister.gov/articles/2010/06/17/2010-14488/interim-final-rules-for-group-health-plans-and-health-insurance-coverage-relating-to-status-as-a#h-11. Published June 17, 2010. Accessed March 25, 2014.
As the Affordable Care Act comes of age, a look behind the headlines
The Affordable Care Act (ACA) faced—and failed—an important test on October 1, 2013, when open enrollment began in the new health-care marketplaces. Plenty has been written about Web site crashes, technical glitches, and what seems to be general mismanagement of this crucial aspect of implementation.
Let’s look behind the headlines to see which aspects of the ACA are working, and which aren’t, and why.
KNOWING THE FACTS CAN HELP YOU HELP YOUR PATIENTS
ObGyns are scientists. As a scientist, you know the importance of facts. In your research and clinical care, you seek out and rely on scientific facts and evidence. You leave aside unsubstantiated thinking.
It’s imperative that we take the same approach with this subject. Far too many misleading and unsubstantiated claims and headlines are crowding out reliable factual information, seriously hindering physicians’ ability to understand this important health-care system change and respond to it appropriately on behalf of patients. As much as we all love Facebook, for example, it may not be the most accurate source of information on the ACA.
Plenty of reliable, factual, unbiased sources of information about the ACA exist, such as “Understanding Obamacare, Politico’s Guide to the Affordable Care Act” (http://www.politico.com/obamacare-guide/). Other helpful sources of ACA outreach and enrollment information:
HealthCare.gov is the federal government’s main portal for information on the Affordable Care Act. A Spanish version of this site can be accessed at www.CuidadoDeSalud.gov.
“FAQ: What you need to know about the new online marketplaces” features questions and answers from Kaiser Health News at http://www.kaiserhealthnews.org/stories/2013/september/17/marketplace-faq-insurance-exchange-obamacare-aca.aspx.
“Fact sheets: Why the Affordable Care Act matters for women” offers links to summaries of ACA provisions; information on health care for pregnant, low-income and older women; preventive care; and more from the National Partnership for Women and Families at http://go.nationalpartnership.org/site/PageServer?pagename=issues_health_reform_anniversary.
Webinars, speakers, FAQs, and more from Doctors for America at http://www.drsforamerica.org/take-action/get-people-covered.
Reports, blog posts, and links to information on enrollment from Enroll America at www.enrollamerica.org.
An informative video on coverage decisions from the Kaiser Family Foundation at http://kff.org/health-reform/video/youtoons-obamacare-video/.
A REVIEW OF THE CHANGES UNDER ACA
Let’s start with one key fact: The ACA offers a lot of good for women’s health care. Many of these improvements hinge on individuals’ ability to enroll in private health insurance policies sold in the marketplaces.
Each state’s marketplace is similar to the system used by the Federal Employees Health Benefits Program (FEHBP), the insurance marketplace used nationwide by federal employees, including members of Congress. Private plans, such as Blue Cross Blue Shield, Aetna, and United Healthcare, offer health insurance on the FEHBP marketplace to the millions of federal employees each year.
In state marketplaces, private health insurers will offer plans to potentially millions of previously under- or uninsured individuals and families. In exchange for access to this huge new group of consumers, private insurers must abide by a number of important consumer protections in order to be eligible to sell their policies in a state marketplace:
Insurers must agree to abide by the 80/20 rule. Under this game-changer, insurers agree to return the actuarial value of 80% of an enrollee’s premium to health care, keeping only a maximum of 20% for profits and other non-health-care categories.
Insurers must agree to cover 10 essential benefits, including maternity care.
Insurers must agree to cover key preventive services, without copays or deductibles, helping our patients stay healthy.
Insurers must abide by significant insurance protections. They can’t, for example, deny a woman coverage because she has a preexisting condition, was once the victim of domestic violence, or once had a cesarean delivery.
Essential benefits and preventive services
All private health insurance plans sold in the state marketplaces must cover the 10 essential health benefits:
ambulatory patient services
emergency services
hospitalization
maternity and newborn care
mental health and substance use disorder services, including behavioral health treatment
prescription drugs
rehabilitative and habilitative services and devices
laboratory services
preventive and wellness services and chronic disease management
pediatric services, including oral and vision care.
These insurers also must cover—with no charge to the patient—preventive services:
well-woman visits (one or more)
all FDA-approved contraceptive methods and contraception counseling
gestational diabetes screening
mammograms
Pap tests
HIV and other sexually transmitted infection screening and counseling
breastfeeding support, supplies, and counseling
domestic violence screening and counseling.
Related Article: Your age-based guide to comprehensive well-woman care Robert L. Barbieri, MD (October 2012)
In addition, private insurers must offer additional preventive services, although they can charge copays for them:
anemia screening on a routine basis for pregnant women
screening for urinary tract or other infection for pregnant women
counseling about genetic testing for a BRCA mutation for women at higher risk
counseling about chemoprevention of breast cancer for women at higher risk
cervical cancer screening for sexually active women
folic acid supplementation for women who may become pregnant
osteoporosis screening for women over age 60, depending on risk factors
screening for Rh incompatibility for all pregnant women and follow-up testing for women at higher risk
tobacco use screening and interventions for all women, and expanded counseling for pregnant users of tobacco.
An end to preexisting-condition exclusions and other harmful practices
Insurers offering plans in the state marketplaces also must abide by important insurance reforms:
They must eliminate exclusions for preexisting conditions. Insurers cannot deny individuals coverage because they already have a condition that requires medical care, including pregnancy. Before this ACA rule, private insurers often rejected applicants who needed care, as well as those who accessed health care in the past. Insurers regularly denied coverage to women who had had a cesarean delivery or had once been a victim of domestic violence.
They cannot charge women more than men for the same coverage. Before the ACA, women seeking health-care coverage often faced higher premiums than men for identical coverage. This made private coverage less affordable for our patients.
They cannot impose a 9-month waiting period. (Need I say more?)
They must eliminate any annual lifetime limits on coverage. Insurers selling policies in the marketplaces cannot end coverage after a certain dollar amount has been reached, a common practice before the ACA. This change is good news for you and your patients. A patient needing long or expensive care won’t lose coverage when the cost of her care hits an arbitrary ceiling.
They cannot rescind coverage unless fraud is proven. Before the ACA, private health insurers would often drop an individual if he or she started racking up high health-care costs. Patients in the middle of expensive cancer treatments, for example, would find themselves suddenly without health insurance. This won’t happen for policies sold in marketplaces unless the patient lied on her enrollment forms or failed to keep up her premium payments.
What these changes mean, in real numbers
These protections are critically important to your ability to care for your patients. Here’s what they mean in real life:
Health-care coverage for about 10,000 insured women is no longer subject to an annual lifetime coverage limit.
Private insurers can’t drop coverage, a change that will affect about 5.5 million insured women.
Insurance companies cannot deny coverage for preexisting conditions, which will help insure about 100,000 women.
Each state marketplace offers four types of plans, the idea being to help people compare policies side by side. All plans sold in the marketplaces must abide by the consumer protections I just reviewed. Each tier is differentiated by the average percentage of an enrollee’s health-care expenses paid by the insurer. The more an enrollee agrees to pay out of pocket, the lower his or her premium.
The tiers are:
Bronze – The insurer covers 60% of health-care costs, and the insured covers 40%. This tier offers the cheapest premiums.
Silver – The insurer covers 70% of costs.
Gold – The insurer covers 80% of costs.
Platinum – The insurer covers 90% of costs.
WHAT WENT WRONG
If everything had gone according to plan, women’s access to health insurance would have increased dramatically nationwide, including in the dark blue states in FIGURE 1 (Map 1)—states that rank lowest in access to care. You’ll notice that many of the states that are dark blue in Map 1 shift to light blue in Map 2. Take a careful look at those dark blue states and see what colors they are in the next two maps (FIGURES 1 and 2). Hint: There’s a pattern.
Problem 1 – Strains on Healthcare.gov
When the ACA was signed into law, most states were expected to build and run their own online marketplaces. The federal government offered to run a state exchange if a state didn’t. Few ACA engineers anticipated that the federal government would have to run the marketplaces in more than half the states—politics-fueled decisions in many states. Now you can see that many of the states that are dark blue in Map 1 are gray in Map 3 (FIGURE 2). Many states whose populations have the greatest need left it to the federal government to run the marketplaces.
Data indicate that state-run marketplaces are doing pretty well—a fact not often caught in frenzied headlines. If we look at the percentage of the target population actually enrolled in marketplace insurance plans during the first month, we see that the lowest state marketplace enrollment was in Washington State, with 30% of its target population enrolled. The highest target-population enrollment was achieved in Connecticut, with 191%.
Compare these numbers to the rates of target-population enrollment in states with marketplaces run by the federal government, which range from 3% to 20% (FIGURE 2). During the first month, federal and state-run marketplaces together enrolled 106,000 individuals into new coverage, 21% of the national target.
The news media have focused on the federal online enrollment debacle. Easier enrollment options are available to people who live in federally run marketplace states, including direct enrollment. Strongly supported by America’s health insurance industry, direct enrollment lets potential enrollees purchase coverage directly from insurance companies participating in the marketplaces.
Problem 2: People lost their current coverage
This is a problem worth exploring—one that affects people who previously bought insurance on the individual insurance market. This is the market that offers people comparatively limited coverage, usually with no maternity care coverage, for comparatively high premiums.
So why are these individuals losing coverage?
They are losing coverage because, as of January 2014, new individual plans must abide by the 80/20 rule, abide by insurance protections, and cover 10 essential services with no cost sharing.
You may recall that, in August 2009, Americans were demanding that they be able to keep the health-care coverage they currently had, and President Barack Obama promised that they would be able to. Consequently, health insurance policies in effect before March 2010, when the ACA was signed into law, were exempted—“grandfathered”—from most ACA requirements. If people liked their old policies, they could keep them.
Grandfathered plans are exempt from:
the requirement to cover the 10 essential health benefits
the requirement that plans must provide preventive services with no patient cost sharing
state or federal review of insurance premium increases of 10% or more for non-group and small business plans
a rule allowing consumers to appeal denials of claims to a third-party reviewer.
Most ACA requirements apply to new policies—those offered after March 2010 and those that have been changed significantly by the insurance companies. Some examples of changes in coverage that would cause a plan to lose grandfathering include:
the elimination of benefits to diagnose or treat a particular condition
an increase in the up-front deductible patients must pay before coverage kicks in by more than the cumulative growth in medical inflation since March 2010 plus 15%
a reduction in the share of the premium that the employer pays by more than 5% since March 2010.
How many people are we talking about? Not the 40% of Americans who have employer-based coverage or the 20% of Americans on Medicare, Medicaid, or Tricare. This provision affects about 5% of the insured, as many as 15 million people—many with plans that offer little coverage for high premiums.
The ACA intention was that many people previously covered in the individual insurance market would find better and cheaper coverage in their state marketplaces. That may be a good option for people in states that have chosen to run their own marketplaces, and a good option for people in other states, too, as federal online enrollment issues get fixed.
Problem 3: Medicaid expansion became a state option
When the US Supreme Court upheld the constitutionality of the ACA’s individual mandate, it also effectively turned the ACA Medicaid expansion into a state option.
Think of the Medicaid expansion as Medicaid Part 2. Regular Medicaid remains largely unchanged, with the same eligibility rules and coverage requirements.
The ACA included a provision under which every state would add a new part to its Medicaid program. Beginning in 2014, this part—the expansion—would cover individuals in each state with incomes under 138% of the federal poverty line—about $32,000 for a family of four in 2014. Medicaid expansion coverage is based only on income eligibility, a major change for women, many of whom currently qualify for Medicaid only if they’re pregnant.
Who would pay for the new coverage?
In 2014, 2015, and 2016, the federal government pays 100% of the cost of care for Medicaid expansion. From 2017 to 2020, the federal share gradually drops to 90%.
Medicaid expansion is an integral part of reducing the number of uninsured under the ACA and is expected to reduce the uninsured rate by almost 30% if adopted by every state. Medicaid expansion plus the ACA marketplaces were expected to cut our uninsured rate almost in half.
FIGURE 3 shows how states responded when the Supreme Court effectively converted the Medicaid expansion into an option, leaving us, again, with coverage gaps. Many of the states that have opted not to expand Medicaid are the same states that declined to operate their own state marketplaces, the same states with highest percentages of the uninsured.
The ACA has many interdependent parts. Make the Medicaid expansion a state option, and you end up with higher than expected rates of uninsured. Trigger big changes in the individual market when there are still bugs in the system, and people are left in the lurch.
Related Article: ACOG to legislators: Partnership, not interference Lucia DiVenere, MA (April 2013)
What’s happening now
As this article is going to press, enrollment in the marketplaces is getting easier, with Web site fixes and useful alternatives to Web-based enrollment. Small changes are being made to some deadlines to help people who have gotten stuck in the process. We’ll likely continue to see steps forward and back over the next many months.
Two things remain important:
We need to stick with the facts. If you see something in the news that seems too crazy to be real, your hunch may be right.
Your patients can benefit significantly from the ACA. An ACOG Fellow recently told me about one of his patients who has a severe health condition, no insurance, and needs expensive treatment. The ACA, with its marketplace rules outlawing exclusions for preexisting conditions and offering premium assistance, may be a lifesaver to her. But first she needs to enroll.
As your patients’ trusted physician, you can help point them in the right direction, possibly toward coverage that they never had before.
That’s good for all of us.
WE WANT TO HEAR FROM YOU!
Drop us a line and let us know what you think about current articles, which topics you'd like to see covered in future issues, and what challenges you face in daily practice. Tell us what you think by emailing us at: [email protected]
The Affordable Care Act (ACA) faced—and failed—an important test on October 1, 2013, when open enrollment began in the new health-care marketplaces. Plenty has been written about Web site crashes, technical glitches, and what seems to be general mismanagement of this crucial aspect of implementation.
Let’s look behind the headlines to see which aspects of the ACA are working, and which aren’t, and why.
KNOWING THE FACTS CAN HELP YOU HELP YOUR PATIENTS
ObGyns are scientists. As a scientist, you know the importance of facts. In your research and clinical care, you seek out and rely on scientific facts and evidence. You leave aside unsubstantiated thinking.
It’s imperative that we take the same approach with this subject. Far too many misleading and unsubstantiated claims and headlines are crowding out reliable factual information, seriously hindering physicians’ ability to understand this important health-care system change and respond to it appropriately on behalf of patients. As much as we all love Facebook, for example, it may not be the most accurate source of information on the ACA.
Plenty of reliable, factual, unbiased sources of information about the ACA exist, such as “Understanding Obamacare, Politico’s Guide to the Affordable Care Act” (http://www.politico.com/obamacare-guide/). Other helpful sources of ACA outreach and enrollment information:
HealthCare.gov is the federal government’s main portal for information on the Affordable Care Act. A Spanish version of this site can be accessed at www.CuidadoDeSalud.gov.
“FAQ: What you need to know about the new online marketplaces” features questions and answers from Kaiser Health News at http://www.kaiserhealthnews.org/stories/2013/september/17/marketplace-faq-insurance-exchange-obamacare-aca.aspx.
“Fact sheets: Why the Affordable Care Act matters for women” offers links to summaries of ACA provisions; information on health care for pregnant, low-income and older women; preventive care; and more from the National Partnership for Women and Families at http://go.nationalpartnership.org/site/PageServer?pagename=issues_health_reform_anniversary.
Webinars, speakers, FAQs, and more from Doctors for America at http://www.drsforamerica.org/take-action/get-people-covered.
Reports, blog posts, and links to information on enrollment from Enroll America at www.enrollamerica.org.
An informative video on coverage decisions from the Kaiser Family Foundation at http://kff.org/health-reform/video/youtoons-obamacare-video/.
A REVIEW OF THE CHANGES UNDER ACA
Let’s start with one key fact: The ACA offers a lot of good for women’s health care. Many of these improvements hinge on individuals’ ability to enroll in private health insurance policies sold in the marketplaces.
Each state’s marketplace is similar to the system used by the Federal Employees Health Benefits Program (FEHBP), the insurance marketplace used nationwide by federal employees, including members of Congress. Private plans, such as Blue Cross Blue Shield, Aetna, and United Healthcare, offer health insurance on the FEHBP marketplace to the millions of federal employees each year.
In state marketplaces, private health insurers will offer plans to potentially millions of previously under- or uninsured individuals and families. In exchange for access to this huge new group of consumers, private insurers must abide by a number of important consumer protections in order to be eligible to sell their policies in a state marketplace:
Insurers must agree to abide by the 80/20 rule. Under this game-changer, insurers agree to return the actuarial value of 80% of an enrollee’s premium to health care, keeping only a maximum of 20% for profits and other non-health-care categories.
Insurers must agree to cover 10 essential benefits, including maternity care.
Insurers must agree to cover key preventive services, without copays or deductibles, helping our patients stay healthy.
Insurers must abide by significant insurance protections. They can’t, for example, deny a woman coverage because she has a preexisting condition, was once the victim of domestic violence, or once had a cesarean delivery.
Essential benefits and preventive services
All private health insurance plans sold in the state marketplaces must cover the 10 essential health benefits:
ambulatory patient services
emergency services
hospitalization
maternity and newborn care
mental health and substance use disorder services, including behavioral health treatment
prescription drugs
rehabilitative and habilitative services and devices
laboratory services
preventive and wellness services and chronic disease management
pediatric services, including oral and vision care.
These insurers also must cover—with no charge to the patient—preventive services:
well-woman visits (one or more)
all FDA-approved contraceptive methods and contraception counseling
gestational diabetes screening
mammograms
Pap tests
HIV and other sexually transmitted infection screening and counseling
breastfeeding support, supplies, and counseling
domestic violence screening and counseling.
Related Article: Your age-based guide to comprehensive well-woman care Robert L. Barbieri, MD (October 2012)
In addition, private insurers must offer additional preventive services, although they can charge copays for them:
anemia screening on a routine basis for pregnant women
screening for urinary tract or other infection for pregnant women
counseling about genetic testing for a BRCA mutation for women at higher risk
counseling about chemoprevention of breast cancer for women at higher risk
cervical cancer screening for sexually active women
folic acid supplementation for women who may become pregnant
osteoporosis screening for women over age 60, depending on risk factors
screening for Rh incompatibility for all pregnant women and follow-up testing for women at higher risk
tobacco use screening and interventions for all women, and expanded counseling for pregnant users of tobacco.
An end to preexisting-condition exclusions and other harmful practices
Insurers offering plans in the state marketplaces also must abide by important insurance reforms:
They must eliminate exclusions for preexisting conditions. Insurers cannot deny individuals coverage because they already have a condition that requires medical care, including pregnancy. Before this ACA rule, private insurers often rejected applicants who needed care, as well as those who accessed health care in the past. Insurers regularly denied coverage to women who had had a cesarean delivery or had once been a victim of domestic violence.
They cannot charge women more than men for the same coverage. Before the ACA, women seeking health-care coverage often faced higher premiums than men for identical coverage. This made private coverage less affordable for our patients.
They cannot impose a 9-month waiting period. (Need I say more?)
They must eliminate any annual lifetime limits on coverage. Insurers selling policies in the marketplaces cannot end coverage after a certain dollar amount has been reached, a common practice before the ACA. This change is good news for you and your patients. A patient needing long or expensive care won’t lose coverage when the cost of her care hits an arbitrary ceiling.
They cannot rescind coverage unless fraud is proven. Before the ACA, private health insurers would often drop an individual if he or she started racking up high health-care costs. Patients in the middle of expensive cancer treatments, for example, would find themselves suddenly without health insurance. This won’t happen for policies sold in marketplaces unless the patient lied on her enrollment forms or failed to keep up her premium payments.
What these changes mean, in real numbers
These protections are critically important to your ability to care for your patients. Here’s what they mean in real life:
Health-care coverage for about 10,000 insured women is no longer subject to an annual lifetime coverage limit.
Private insurers can’t drop coverage, a change that will affect about 5.5 million insured women.
Insurance companies cannot deny coverage for preexisting conditions, which will help insure about 100,000 women.
Each state marketplace offers four types of plans, the idea being to help people compare policies side by side. All plans sold in the marketplaces must abide by the consumer protections I just reviewed. Each tier is differentiated by the average percentage of an enrollee’s health-care expenses paid by the insurer. The more an enrollee agrees to pay out of pocket, the lower his or her premium.
The tiers are:
Bronze – The insurer covers 60% of health-care costs, and the insured covers 40%. This tier offers the cheapest premiums.
Silver – The insurer covers 70% of costs.
Gold – The insurer covers 80% of costs.
Platinum – The insurer covers 90% of costs.
WHAT WENT WRONG
If everything had gone according to plan, women’s access to health insurance would have increased dramatically nationwide, including in the dark blue states in FIGURE 1 (Map 1)—states that rank lowest in access to care. You’ll notice that many of the states that are dark blue in Map 1 shift to light blue in Map 2. Take a careful look at those dark blue states and see what colors they are in the next two maps (FIGURES 1 and 2). Hint: There’s a pattern.
Problem 1 – Strains on Healthcare.gov
When the ACA was signed into law, most states were expected to build and run their own online marketplaces. The federal government offered to run a state exchange if a state didn’t. Few ACA engineers anticipated that the federal government would have to run the marketplaces in more than half the states—politics-fueled decisions in many states. Now you can see that many of the states that are dark blue in Map 1 are gray in Map 3 (FIGURE 2). Many states whose populations have the greatest need left it to the federal government to run the marketplaces.
Data indicate that state-run marketplaces are doing pretty well—a fact not often caught in frenzied headlines. If we look at the percentage of the target population actually enrolled in marketplace insurance plans during the first month, we see that the lowest state marketplace enrollment was in Washington State, with 30% of its target population enrolled. The highest target-population enrollment was achieved in Connecticut, with 191%.
Compare these numbers to the rates of target-population enrollment in states with marketplaces run by the federal government, which range from 3% to 20% (FIGURE 2). During the first month, federal and state-run marketplaces together enrolled 106,000 individuals into new coverage, 21% of the national target.
The news media have focused on the federal online enrollment debacle. Easier enrollment options are available to people who live in federally run marketplace states, including direct enrollment. Strongly supported by America’s health insurance industry, direct enrollment lets potential enrollees purchase coverage directly from insurance companies participating in the marketplaces.
Problem 2: People lost their current coverage
This is a problem worth exploring—one that affects people who previously bought insurance on the individual insurance market. This is the market that offers people comparatively limited coverage, usually with no maternity care coverage, for comparatively high premiums.
So why are these individuals losing coverage?
They are losing coverage because, as of January 2014, new individual plans must abide by the 80/20 rule, abide by insurance protections, and cover 10 essential services with no cost sharing.
You may recall that, in August 2009, Americans were demanding that they be able to keep the health-care coverage they currently had, and President Barack Obama promised that they would be able to. Consequently, health insurance policies in effect before March 2010, when the ACA was signed into law, were exempted—“grandfathered”—from most ACA requirements. If people liked their old policies, they could keep them.
Grandfathered plans are exempt from:
the requirement to cover the 10 essential health benefits
the requirement that plans must provide preventive services with no patient cost sharing
state or federal review of insurance premium increases of 10% or more for non-group and small business plans
a rule allowing consumers to appeal denials of claims to a third-party reviewer.
Most ACA requirements apply to new policies—those offered after March 2010 and those that have been changed significantly by the insurance companies. Some examples of changes in coverage that would cause a plan to lose grandfathering include:
the elimination of benefits to diagnose or treat a particular condition
an increase in the up-front deductible patients must pay before coverage kicks in by more than the cumulative growth in medical inflation since March 2010 plus 15%
a reduction in the share of the premium that the employer pays by more than 5% since March 2010.
How many people are we talking about? Not the 40% of Americans who have employer-based coverage or the 20% of Americans on Medicare, Medicaid, or Tricare. This provision affects about 5% of the insured, as many as 15 million people—many with plans that offer little coverage for high premiums.
The ACA intention was that many people previously covered in the individual insurance market would find better and cheaper coverage in their state marketplaces. That may be a good option for people in states that have chosen to run their own marketplaces, and a good option for people in other states, too, as federal online enrollment issues get fixed.
Problem 3: Medicaid expansion became a state option
When the US Supreme Court upheld the constitutionality of the ACA’s individual mandate, it also effectively turned the ACA Medicaid expansion into a state option.
Think of the Medicaid expansion as Medicaid Part 2. Regular Medicaid remains largely unchanged, with the same eligibility rules and coverage requirements.
The ACA included a provision under which every state would add a new part to its Medicaid program. Beginning in 2014, this part—the expansion—would cover individuals in each state with incomes under 138% of the federal poverty line—about $32,000 for a family of four in 2014. Medicaid expansion coverage is based only on income eligibility, a major change for women, many of whom currently qualify for Medicaid only if they’re pregnant.
Who would pay for the new coverage?
In 2014, 2015, and 2016, the federal government pays 100% of the cost of care for Medicaid expansion. From 2017 to 2020, the federal share gradually drops to 90%.
Medicaid expansion is an integral part of reducing the number of uninsured under the ACA and is expected to reduce the uninsured rate by almost 30% if adopted by every state. Medicaid expansion plus the ACA marketplaces were expected to cut our uninsured rate almost in half.
FIGURE 3 shows how states responded when the Supreme Court effectively converted the Medicaid expansion into an option, leaving us, again, with coverage gaps. Many of the states that have opted not to expand Medicaid are the same states that declined to operate their own state marketplaces, the same states with highest percentages of the uninsured.
The ACA has many interdependent parts. Make the Medicaid expansion a state option, and you end up with higher than expected rates of uninsured. Trigger big changes in the individual market when there are still bugs in the system, and people are left in the lurch.
Related Article: ACOG to legislators: Partnership, not interference Lucia DiVenere, MA (April 2013)
What’s happening now
As this article is going to press, enrollment in the marketplaces is getting easier, with Web site fixes and useful alternatives to Web-based enrollment. Small changes are being made to some deadlines to help people who have gotten stuck in the process. We’ll likely continue to see steps forward and back over the next many months.
Two things remain important:
We need to stick with the facts. If you see something in the news that seems too crazy to be real, your hunch may be right.
Your patients can benefit significantly from the ACA. An ACOG Fellow recently told me about one of his patients who has a severe health condition, no insurance, and needs expensive treatment. The ACA, with its marketplace rules outlawing exclusions for preexisting conditions and offering premium assistance, may be a lifesaver to her. But first she needs to enroll.
As your patients’ trusted physician, you can help point them in the right direction, possibly toward coverage that they never had before.
That’s good for all of us.
WE WANT TO HEAR FROM YOU!
Drop us a line and let us know what you think about current articles, which topics you'd like to see covered in future issues, and what challenges you face in daily practice. Tell us what you think by emailing us at: [email protected]
The Affordable Care Act (ACA) faced—and failed—an important test on October 1, 2013, when open enrollment began in the new health-care marketplaces. Plenty has been written about Web site crashes, technical glitches, and what seems to be general mismanagement of this crucial aspect of implementation.
Let’s look behind the headlines to see which aspects of the ACA are working, and which aren’t, and why.
KNOWING THE FACTS CAN HELP YOU HELP YOUR PATIENTS
ObGyns are scientists. As a scientist, you know the importance of facts. In your research and clinical care, you seek out and rely on scientific facts and evidence. You leave aside unsubstantiated thinking.
It’s imperative that we take the same approach with this subject. Far too many misleading and unsubstantiated claims and headlines are crowding out reliable factual information, seriously hindering physicians’ ability to understand this important health-care system change and respond to it appropriately on behalf of patients. As much as we all love Facebook, for example, it may not be the most accurate source of information on the ACA.
Plenty of reliable, factual, unbiased sources of information about the ACA exist, such as “Understanding Obamacare, Politico’s Guide to the Affordable Care Act” (http://www.politico.com/obamacare-guide/). Other helpful sources of ACA outreach and enrollment information:
HealthCare.gov is the federal government’s main portal for information on the Affordable Care Act. A Spanish version of this site can be accessed at www.CuidadoDeSalud.gov.
“FAQ: What you need to know about the new online marketplaces” features questions and answers from Kaiser Health News at http://www.kaiserhealthnews.org/stories/2013/september/17/marketplace-faq-insurance-exchange-obamacare-aca.aspx.
“Fact sheets: Why the Affordable Care Act matters for women” offers links to summaries of ACA provisions; information on health care for pregnant, low-income and older women; preventive care; and more from the National Partnership for Women and Families at http://go.nationalpartnership.org/site/PageServer?pagename=issues_health_reform_anniversary.
Webinars, speakers, FAQs, and more from Doctors for America at http://www.drsforamerica.org/take-action/get-people-covered.
Reports, blog posts, and links to information on enrollment from Enroll America at www.enrollamerica.org.
An informative video on coverage decisions from the Kaiser Family Foundation at http://kff.org/health-reform/video/youtoons-obamacare-video/.
A REVIEW OF THE CHANGES UNDER ACA
Let’s start with one key fact: The ACA offers a lot of good for women’s health care. Many of these improvements hinge on individuals’ ability to enroll in private health insurance policies sold in the marketplaces.
Each state’s marketplace is similar to the system used by the Federal Employees Health Benefits Program (FEHBP), the insurance marketplace used nationwide by federal employees, including members of Congress. Private plans, such as Blue Cross Blue Shield, Aetna, and United Healthcare, offer health insurance on the FEHBP marketplace to the millions of federal employees each year.
In state marketplaces, private health insurers will offer plans to potentially millions of previously under- or uninsured individuals and families. In exchange for access to this huge new group of consumers, private insurers must abide by a number of important consumer protections in order to be eligible to sell their policies in a state marketplace:
Insurers must agree to abide by the 80/20 rule. Under this game-changer, insurers agree to return the actuarial value of 80% of an enrollee’s premium to health care, keeping only a maximum of 20% for profits and other non-health-care categories.
Insurers must agree to cover 10 essential benefits, including maternity care.
Insurers must agree to cover key preventive services, without copays or deductibles, helping our patients stay healthy.
Insurers must abide by significant insurance protections. They can’t, for example, deny a woman coverage because she has a preexisting condition, was once the victim of domestic violence, or once had a cesarean delivery.
Essential benefits and preventive services
All private health insurance plans sold in the state marketplaces must cover the 10 essential health benefits:
ambulatory patient services
emergency services
hospitalization
maternity and newborn care
mental health and substance use disorder services, including behavioral health treatment
prescription drugs
rehabilitative and habilitative services and devices
laboratory services
preventive and wellness services and chronic disease management
pediatric services, including oral and vision care.
These insurers also must cover—with no charge to the patient—preventive services:
well-woman visits (one or more)
all FDA-approved contraceptive methods and contraception counseling
gestational diabetes screening
mammograms
Pap tests
HIV and other sexually transmitted infection screening and counseling
breastfeeding support, supplies, and counseling
domestic violence screening and counseling.
Related Article: Your age-based guide to comprehensive well-woman care Robert L. Barbieri, MD (October 2012)
In addition, private insurers must offer additional preventive services, although they can charge copays for them:
anemia screening on a routine basis for pregnant women
screening for urinary tract or other infection for pregnant women
counseling about genetic testing for a BRCA mutation for women at higher risk
counseling about chemoprevention of breast cancer for women at higher risk
cervical cancer screening for sexually active women
folic acid supplementation for women who may become pregnant
osteoporosis screening for women over age 60, depending on risk factors
screening for Rh incompatibility for all pregnant women and follow-up testing for women at higher risk
tobacco use screening and interventions for all women, and expanded counseling for pregnant users of tobacco.
An end to preexisting-condition exclusions and other harmful practices
Insurers offering plans in the state marketplaces also must abide by important insurance reforms:
They must eliminate exclusions for preexisting conditions. Insurers cannot deny individuals coverage because they already have a condition that requires medical care, including pregnancy. Before this ACA rule, private insurers often rejected applicants who needed care, as well as those who accessed health care in the past. Insurers regularly denied coverage to women who had had a cesarean delivery or had once been a victim of domestic violence.
They cannot charge women more than men for the same coverage. Before the ACA, women seeking health-care coverage often faced higher premiums than men for identical coverage. This made private coverage less affordable for our patients.
They cannot impose a 9-month waiting period. (Need I say more?)
They must eliminate any annual lifetime limits on coverage. Insurers selling policies in the marketplaces cannot end coverage after a certain dollar amount has been reached, a common practice before the ACA. This change is good news for you and your patients. A patient needing long or expensive care won’t lose coverage when the cost of her care hits an arbitrary ceiling.
They cannot rescind coverage unless fraud is proven. Before the ACA, private health insurers would often drop an individual if he or she started racking up high health-care costs. Patients in the middle of expensive cancer treatments, for example, would find themselves suddenly without health insurance. This won’t happen for policies sold in marketplaces unless the patient lied on her enrollment forms or failed to keep up her premium payments.
What these changes mean, in real numbers
These protections are critically important to your ability to care for your patients. Here’s what they mean in real life:
Health-care coverage for about 10,000 insured women is no longer subject to an annual lifetime coverage limit.
Private insurers can’t drop coverage, a change that will affect about 5.5 million insured women.
Insurance companies cannot deny coverage for preexisting conditions, which will help insure about 100,000 women.
Each state marketplace offers four types of plans, the idea being to help people compare policies side by side. All plans sold in the marketplaces must abide by the consumer protections I just reviewed. Each tier is differentiated by the average percentage of an enrollee’s health-care expenses paid by the insurer. The more an enrollee agrees to pay out of pocket, the lower his or her premium.
The tiers are:
Bronze – The insurer covers 60% of health-care costs, and the insured covers 40%. This tier offers the cheapest premiums.
Silver – The insurer covers 70% of costs.
Gold – The insurer covers 80% of costs.
Platinum – The insurer covers 90% of costs.
WHAT WENT WRONG
If everything had gone according to plan, women’s access to health insurance would have increased dramatically nationwide, including in the dark blue states in FIGURE 1 (Map 1)—states that rank lowest in access to care. You’ll notice that many of the states that are dark blue in Map 1 shift to light blue in Map 2. Take a careful look at those dark blue states and see what colors they are in the next two maps (FIGURES 1 and 2). Hint: There’s a pattern.
Problem 1 – Strains on Healthcare.gov
When the ACA was signed into law, most states were expected to build and run their own online marketplaces. The federal government offered to run a state exchange if a state didn’t. Few ACA engineers anticipated that the federal government would have to run the marketplaces in more than half the states—politics-fueled decisions in many states. Now you can see that many of the states that are dark blue in Map 1 are gray in Map 3 (FIGURE 2). Many states whose populations have the greatest need left it to the federal government to run the marketplaces.
Data indicate that state-run marketplaces are doing pretty well—a fact not often caught in frenzied headlines. If we look at the percentage of the target population actually enrolled in marketplace insurance plans during the first month, we see that the lowest state marketplace enrollment was in Washington State, with 30% of its target population enrolled. The highest target-population enrollment was achieved in Connecticut, with 191%.
Compare these numbers to the rates of target-population enrollment in states with marketplaces run by the federal government, which range from 3% to 20% (FIGURE 2). During the first month, federal and state-run marketplaces together enrolled 106,000 individuals into new coverage, 21% of the national target.
The news media have focused on the federal online enrollment debacle. Easier enrollment options are available to people who live in federally run marketplace states, including direct enrollment. Strongly supported by America’s health insurance industry, direct enrollment lets potential enrollees purchase coverage directly from insurance companies participating in the marketplaces.
Problem 2: People lost their current coverage
This is a problem worth exploring—one that affects people who previously bought insurance on the individual insurance market. This is the market that offers people comparatively limited coverage, usually with no maternity care coverage, for comparatively high premiums.
So why are these individuals losing coverage?
They are losing coverage because, as of January 2014, new individual plans must abide by the 80/20 rule, abide by insurance protections, and cover 10 essential services with no cost sharing.
You may recall that, in August 2009, Americans were demanding that they be able to keep the health-care coverage they currently had, and President Barack Obama promised that they would be able to. Consequently, health insurance policies in effect before March 2010, when the ACA was signed into law, were exempted—“grandfathered”—from most ACA requirements. If people liked their old policies, they could keep them.
Grandfathered plans are exempt from:
the requirement to cover the 10 essential health benefits
the requirement that plans must provide preventive services with no patient cost sharing
state or federal review of insurance premium increases of 10% or more for non-group and small business plans
a rule allowing consumers to appeal denials of claims to a third-party reviewer.
Most ACA requirements apply to new policies—those offered after March 2010 and those that have been changed significantly by the insurance companies. Some examples of changes in coverage that would cause a plan to lose grandfathering include:
the elimination of benefits to diagnose or treat a particular condition
an increase in the up-front deductible patients must pay before coverage kicks in by more than the cumulative growth in medical inflation since March 2010 plus 15%
a reduction in the share of the premium that the employer pays by more than 5% since March 2010.
How many people are we talking about? Not the 40% of Americans who have employer-based coverage or the 20% of Americans on Medicare, Medicaid, or Tricare. This provision affects about 5% of the insured, as many as 15 million people—many with plans that offer little coverage for high premiums.
The ACA intention was that many people previously covered in the individual insurance market would find better and cheaper coverage in their state marketplaces. That may be a good option for people in states that have chosen to run their own marketplaces, and a good option for people in other states, too, as federal online enrollment issues get fixed.
Problem 3: Medicaid expansion became a state option
When the US Supreme Court upheld the constitutionality of the ACA’s individual mandate, it also effectively turned the ACA Medicaid expansion into a state option.
Think of the Medicaid expansion as Medicaid Part 2. Regular Medicaid remains largely unchanged, with the same eligibility rules and coverage requirements.
The ACA included a provision under which every state would add a new part to its Medicaid program. Beginning in 2014, this part—the expansion—would cover individuals in each state with incomes under 138% of the federal poverty line—about $32,000 for a family of four in 2014. Medicaid expansion coverage is based only on income eligibility, a major change for women, many of whom currently qualify for Medicaid only if they’re pregnant.
Who would pay for the new coverage?
In 2014, 2015, and 2016, the federal government pays 100% of the cost of care for Medicaid expansion. From 2017 to 2020, the federal share gradually drops to 90%.
Medicaid expansion is an integral part of reducing the number of uninsured under the ACA and is expected to reduce the uninsured rate by almost 30% if adopted by every state. Medicaid expansion plus the ACA marketplaces were expected to cut our uninsured rate almost in half.
FIGURE 3 shows how states responded when the Supreme Court effectively converted the Medicaid expansion into an option, leaving us, again, with coverage gaps. Many of the states that have opted not to expand Medicaid are the same states that declined to operate their own state marketplaces, the same states with highest percentages of the uninsured.
The ACA has many interdependent parts. Make the Medicaid expansion a state option, and you end up with higher than expected rates of uninsured. Trigger big changes in the individual market when there are still bugs in the system, and people are left in the lurch.
Related Article: ACOG to legislators: Partnership, not interference Lucia DiVenere, MA (April 2013)
What’s happening now
As this article is going to press, enrollment in the marketplaces is getting easier, with Web site fixes and useful alternatives to Web-based enrollment. Small changes are being made to some deadlines to help people who have gotten stuck in the process. We’ll likely continue to see steps forward and back over the next many months.
Two things remain important:
We need to stick with the facts. If you see something in the news that seems too crazy to be real, your hunch may be right.
Your patients can benefit significantly from the ACA. An ACOG Fellow recently told me about one of his patients who has a severe health condition, no insurance, and needs expensive treatment. The ACA, with its marketplace rules outlawing exclusions for preexisting conditions and offering premium assistance, may be a lifesaver to her. But first she needs to enroll.
As your patients’ trusted physician, you can help point them in the right direction, possibly toward coverage that they never had before.
That’s good for all of us.
WE WANT TO HEAR FROM YOU!
Drop us a line and let us know what you think about current articles, which topics you'd like to see covered in future issues, and what challenges you face in daily practice. Tell us what you think by emailing us at: [email protected]