User login
Depression and heart failure: An overview of what we know and don’t know
The relationship between depression and heart failure is not as obvious as the one between depression and coronary artery disease. Myriad questions on the subject are open to research:
- Does depression occur in heart failure at higher-than-expected rates?
- Does heart failure severity influence depression?
- Is depression a risk factor for heart failure? If so, why?
- How should we screen for depression in patients with heart failure?
- Do we have an evidence-based approach to treatment?
Part of the challenge in clarifying the relationship between depression and heart failure is that heart failure is a disease of chronically ill, elderly patients—a population in which adjustment disorder with depressed mood and major depression are also common diagnoses, with rates recently found to be 22.3% and 13.3%, respectively.1 Nevertheless, interest in examining the relationship between heart failure and depression is long-standing, and many clinical studies have examined this relationship.2–16 Unfortunately, measures are not standardized, so comparisons between studies are difficult.
DEPRESSION IS COMMON IN PATIENTS WITH HEART FAILURE
Many studies show that rates of depression among patients with heart failure are higher than expected among other elderly, chronically ill patients. Furthermore, depression has been linked to more severe heart failure symptoms and worse outcomes in some studies.
In a 2001 study, Jiang et al screened 374 hospitalized patients with heart failure using the Beck Depression Inventory score and found that 35% had scores of 10 or higher (indicative of at least mild depression).12 Further testing showed that 14% met criteria for major depression.
A 2006 meta-analysis of 27 studies by Rutledge et al found a 21% incidence of clinically significant depression in patients with heart failure.17 Rates of depression depended heavily on the rigor of screening criteria for classifying participants as depressed: rates were as high as 38% with the use of liberal criteria and as low as 14% with strict criteria. New York Heart Association (NYHA) functional status correlated strongly with the prevalence of depression, which increased steadily from 11% in patients with NYHA class I (mild) heart failure to 20% in those with class II, 38% in those with class III, and 42% in those with class IV (severe) heart failure.
In one of the studies included in the meta-analysis, Freedland et al found that the prevalence of major depression was strongly associated with age and functional status in hospitalized patients with heart failure.18 In patients younger than age 60 years, rates of major depression rose particularly sharply as heart failure symptoms worsened.
The Psychosocial Factors Outcome Study found that the prevalence of depression in patients with heart failure who participated in the community-based Sudden Cardiac Death in Heart Failure Trial (SCD-HeFT) was 36%, based on a score of 13 or greater on the Beck Depression Inventory-II.19 Similarly, unpublished preliminary data from the Heart Failure Adherence and Retention Trial (HART) show that about one-third of community-based patients with heart failure have depression.20
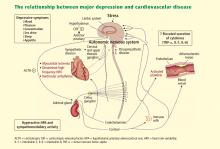
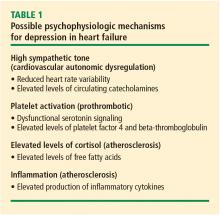
DEPRESSION AND HEART FAILURE ARE CLOSELY LINKED PHYSIOLOGICALLY
The evidence, therefore, strongly suggests a common pathway between heart failure and depression, and this evidence of a relationship favors a new paradigm that integrates the treatment of the two conditions.
BETA-BLOCKERS DO NOT RAISE RISK OF DEPRESSION
Pharmacotherapy is often implicated as a related factor in the development or exacerbation of depression in patients with heart failure, especially in those taking beta-blockers. Meta-analyses of the incidence of depression associated with various beta-blockers have been conducted in patients with hypertension, heart failure, and recent myocardial infarction. A 2002 meta-analysis of eight trials that randomized patients to treatment with a beta-blocker or placebo found no difference in the incidence of depressive symptoms between the active treatment and placebo groups, or between patients in the two groups who withdrew from the trial, presumably because of depression or other symptoms.24 An additional study not included in that meta-analysis found no differences in rates of depression among hypertensive patients according to the type of antihypertensive medication they were taking (ie, beta-blockers, diuretics, reserpine, or no drug therapy).25
Based on the evidence, I see no reason to avoid a trial of beta-blockers in patients who have depression at baseline or to be overly concerned that patients without depression will develop it as a result of beta-blocker treatment.
DEPRESSION LEADS TO WORSE OUTCOMES, HIGHER COSTS IN HEART FAILURE
Not only is depression prevalent in patients with heart failure, but depression adversely affects heart failure outcomes. One study of hospitalized patients older than 70 years found readmission rates to be 67% among heart failure patients with depression versus 44% among heart failure patients without depression.26 Patients in this study were three times as likely to die if they had heart failure than if they did not have heart failure, and they were twice as likely to die if they had depression than if they did not have depression. The mortality rate was 21% for patients with both heart failure and depression versus 15% for patients with heart failure without depression.26
Depressive symptoms also correlate with poorer quality of life in patients with heart failure. Gottlieb et al found that quality-of-life scores were significantly worse in heart failure patients if they had a diagnosis of depression on the basis of the Beck Depression Index.27
The 27-study meta-analysis by Rutledge et al discussed earlier found that the presence of depression in a patient with heart failure predicts worse outcomes in terms of hospital readmission rates, functional status, and walk times.17 This analysis also found twice the rate of death in heart failure patients with depression compared with heart failure patients without depression.
In a large community-based trial involving more than 48,000 patients with heart failure, Macchia et al found that survival was markedly reduced in patients who had a history of depression.28 This study also showed that depressed patients were less likely to adhere to medication regimens with angiotensin-converting enzyme inhibitors and beta-blockers, which may offer a potential explanation for the reduction in survival among depressed patients.
In a study of patients with coronary artery disease who had no diagnosis of depression or heart failure, May et al demonstrated that those who subsequently developed depression had more than four times the risk of also developing heart failure.29
The combination of heart failure and depression also is costly. In a 3-year retrospective study of community-based patients following a first hospitalization for heart failure, Sullivan et al found that annualized adjusted total costs were nearly 30% greater in patients diagnosed with depression and that inpatient and outpatient service utilization was also greater in those with depression.5
DIAGNOSIS AND TREATMENT
One simple question can effectively screen for depression
Numerous tools are available for the diagnosis of depression, but developing a tool that is readily useful to a busy clinician is challenging. Simply asking the single question, “Are you depressed?” has fairly high sensitivity (55%) and specificity (74%) for diagnosing depression in palliative care patients, a population even more seriously ill than heart failure patients.30 A variation on the question from British studies—“Do you feel that your life is empty?”—is considered to be a better screening question for elderly patients.31,32
Effect of depression therapy on heart failure still unclear
Unfortunately, evidence for the best treatment for depression in patients with heart failure is lacking. Some guidance may be gleaned from studies in patients with coronary artery disease. The Sertraline Antidepressant Heart Attack Randomized Trial (SADHART) was a multicenter, randomized, placebo-controlled study of the safety and efficacy of treating major depressive disorder with sertraline for 24 weeks in patients hospitalized for acute coronary syndrome.33,34 No significant differences were found between treatment groups in left ventricular ejection fraction, blood pressure, resting electrocardiogram, and cardiac arrhythmias. Although the trial was not powered to detect an effect of treatment on mortality, there were fewer deaths and severe cardiovascular adverse events in the active treatment group.
A later study was designed to evaluate 12 weeks of treatment with sertraline in patients with major depression and heart failure.35 Although symptoms of depression improved with treatment, no beneficial effect on heart failure was found.36 A nursing intervention that was included for both the treatment and placebo groups may have served to limit the impact of sertraline on heart failure surrogate end points.
The abovementioned HART study randomized patients with systolic or diastolic dysfunction and NYHA class II or III functional status to receive either heart failure education (comprising 18 American Heart Association tip sheets and 18 phone calls) or heart failure education plus self-management strategies (comprising the tip sheets, 18 group sessions, and problem-solving and self-management skills) following hospital discharge.37 Over 3 years, no difference between the two groups was found in the rates and timing of deaths or heart failure hospitalizations.
The best treatment strategies for depression in heart failure are still unclear, and more research is needed. Although guidelines exist for the management of depression in patients with coronary heart disease,38 no such guidelines have been issued for the management of depression in heart failure.
CONCLUSIONS
Although evidence is strong that treatment with medication or cognitive therapies improves symptoms of depression, evidence is lacking for a significant effect of such interventions on cardiac outcomes.39 Because depression and heart failure are so closely linked and appear to share a genetic and pathophysiologic basis, greater understanding of the relationship between these diseases across the stages of heart failure should be pursued.
Any patient with heart failure who is symptomatic has advanced disease, and is therefore closer to death than to health. The same is probably true of depression. Patients with heart failure and depression must be identified early, and interventions must be tried at these early stages of disease. Better depression screening tools and heightened awareness of the relationship between heart failure and depression are essential.
- Yazgan IC, Kuscu MK, Fistikci N, Keyvan A, Topcuoglu V. Geriatric psychiatry consultations in a Turkish university hospital. Int Psychogeriatr 2006; 18:327–333.
- Abramson J, Berger A, Krumholz HM, Vaccarino V. Depression and risk of heart failure among older persons with isolated systolic hypertension. Arch Intern Med 2001; 161:1725–1730.
- Williams SA, Kasl SV, Heiat A, Abramson JL, Krumholz HM, Vaccarino V. Depression and risk of heart failure among the elderly: a prospective community-based study. Psychosom Med 2002; 64:6–12.
- Himelhoch S, Weller WE, Wu AW, Anderson GF, Cooper LA. Chronic medical illness, depression, and use of acute medical services among Medicare beneficiaries. Med Care 2004; 42:512–521.
- Sullivan M, Simon G, Spertus J, Russo J. Depression-related costs in heart failure care. Arch Intern Med 2002; 162:1860–1866.
- Fulop G, Strain JJ, Stettin G. Congestive heart failure and depression in older adults: clinical course and health services use 6 months after hospitalization. Psychosomatics 2003; 44:367–373.
- Koenig HG. Depression in hospitalized older patients with congestive heart failure. Gen Hosp Psychiatry 1998; 20:29–43.
- Rumsfeld JS, Havranek E, Masoudi FA, et al Depressive symptoms are the strongest predictors of short-term declines in health status in patients with heart failure. J Am Coll Cardiol 2003; 42:1811–1817.
- de Denus S, Spinler SA, Jessup M, Kao A. History of depression as a predictor of adverse outcomes in patients hospitalized for decompensated heart failure. Pharmacotherapy 2004; 24:1306–1310.
- Faris R, Purcell H, Henein MY, Coats AJ. Clinical depression is common and significantly associated with reduced survival in patients with non-ischaemic heart failure. Eur J Heart Fail 2002; 4:541–551.
- Freedland KE, Carney RM, Rich MW, et al Depression in elderly patients with congestive heart failure. J Geriatr Psychiatry 1991; 24:59–71.
- Jiang W, Alexander J, Christopher E, et al Relationship of depression to increased risk of mortality and rehospitalization in patients with congestive heart failure. Arch Intern Med 2001; 161:1849–1856.
- Jünger J, Schellberg D, Müller-Tasch T, et al Depression increasingly predicts mortality in the course of congestive heart failure. Eur J Heart Fail 2005; 7:261–267.
- Murberg TA, Bru E, Svebak S, Tveterås R, Aarsland T. Depressed mood and subjective health symptoms as predictors of mortality in patients with congestive heart failure: a two-years follow-up study. Int J Psychiatry Med 1999; 29:311–326.
- Sullivan MD, Levy WC, Crane BA, Russo JE, Spertus JA. Usefulness of depression to predict time to combined end point of transplant or death for outpatients with advanced heart failure. Am J Cardiol 2004; 94:1577–1580.
- Vaccarino V, Kasl SV, Abramson J, Krumholz HM. Depressive symptoms and risk of functional decline and death in patients with heart failure. J Am Coll Cardiol 2001; 38:199–205.
- Rutledge T, Reis VA, Linke SE, Greenberg BH, Mills PJ. Depression in heart failure: a meta-analytic review of prevalence, intervention effects, and associations with clinical outcomes. J Am Coll Cardiol 2006; 48:1527–1537.
- Freedland KE, Rich MW, Skala JA, Carney RM, Dávila-Román VG, Jaffe AS. Prevalence of depression in hospitalized patients with congestive heart failure. Psychosom Med 2003; 65:119–128.
- Friedmann E, Thomas SA, Liu F, et al Relationship of depression, anxiety, and social isolation to chronic heart failure outpatient mortality. Am Heart J 2006; 152:940.e1–940.e8.
- de Leon CF, Grady KL, Eaton C, et al Quality of life in a diverse population of patients with heart failure: baseline findings from the Heart Failure Adherence and Retention trial (HART). J Cardiopulm Rehabil Prev 2009; 29:171–178.
- Musselman DL, Evans DL, Nemeroff CB. The relationship of depression to cardiovascular disease: epidemiology, biology, and treatment. Arch Gen Psychiatry 1998; 55:580–592.
- Caspi A, Sugden K, Moffitt TE, et al Influence of life stress on depression: moderation by a polymorphism in the 5-HTT gene. Science 2003; 301:386–389.
- Cohn JN, Levine TB, Olivari MT, et al Plasma norepinephrine as a guide to prognosis in patients with chronic congestive heart failure. N Engl J Med 1984; 311:819–823.
- Ko DT, Hebert PR, Coffey CS, Sedrakyan A, Curtis JP, Krumholz HM. β-blocker therapy and symptoms of depression, fatigue, and sexual dysfunction. JAMA 2002; 288:351–357.
- Prisant LM, Spruill WJ, Fincham JE, Wade WE, Carr AA, Adams MA. Depression associated with antihypertensive drugs. J Fam Pract 1991; 33:481–485.
- Rozzini R, Sabatini T, Frisoni GB, et al Depression and major outcomes in older patients with heart failure [letter]. Arch Intern Med 2002; 162:362–364.
- Gottlieb SS, Khatta M, Friedmann E, et al The influence of age, gender, and race on the prevalence of depression in heart failure patients. J Am Coll Cardiol 2004; 43:1542–1549.
- Macchia A, Monte S, Pellegrini F, et al Depression worsens outcomes in elderly patients with heart failure: an analysis of 48,117 patients in a community setting. Eur J Heart Fail 2008; 10:714–721.
- May HT, Horne BD, Carlquist JF, Sheng X, Joy E, Catinella AP. Depression after coronary artery disease is associated with heart failure. J Am Coll Cardiol 2009; 53:1440–1447.
- Lloyd-Williams M, Dennis M, Taylor F, Baker I. Is asking patients in palliative care, “Are you depressed?” appropriate? Prospective study. BMJ 2003; 327:372–373.
- Whelan PJ, Gaughran F, Walwyn R, Chatterton K, Macdonald A. ‘Do you feel that your life is empty?’ The clinical utility of a one-off question for detecting depression in elderly care home residents. Age Ageing 2008; 37:475–478.
- D’Ath P, Katona P, Mullan E, Evans S, Katona C. Screening, detection and management of depression in elderly primary care attenders. I: The acceptability and performance of the 15 item Geriatric Depression Scale (GDS15) and the development of short versions. Fam Pract 1994; 11:260–266.
- Glassman AH, O’Connor CM, Califf RM, et al., Sertraline Antidepressant Heart Attack Randomized Trial (SADHART) Group. Sertraline treatment of major depression in patients with acute MI or unstable angina. JAMA 2002; 288:701–709.
- Carney RM, Jaffe AS. Treatment of depression following acute myocardial infarction. JAMA 2002; 288:750–751.
- Jiang W, O’Connor C, Silva SG, et al., SADHART-CHF Investigators. Safety and efficacy of sertraline for depression in patients with CHF (SADHART-CHF): a randomized, double-blind, placebo-controlled trial of sertraline for major depression with congestive heart failure. Am Heart J 2008; 156:437–444.
- O’Connor CM, Wei J, Silva SG, et al., SADHART-CHF investigators. Safety and efficacy of sertraline plus nurse facilitated supportive intervention (NFSI) versus placebo plus nurse facilitated supportive intervention for depression in patients with CHF (SADHART-CHF). Presented at: 2008 Scientific Sessions of the Heart Failure Society of America; September 20–23, 2008; Toronto, ON, Canada.
- Powell LH, Calvin JE, Mendes de Leon CF, et al Impact of patient self-management skills training on death and hospitalization in patients with heart failure: results from the Heart Failure Adherence and Retention Trial. Circulation 2007; 116:2629. Abstract.
- Lichtman JH, Bigger JT, Blumenthal JA, et al Depression and coronary heart disease: recommendations for screening, referral, and treatment: a science advisory from the American Heart Association Prevention Committee of the Council on Cardiovascular Nursing, Council on Clinical Cardiology, Council on Epidemiology and Prevention, and Interdisciplinary Council on Quality of Care and Outcomes Research: endorsed by the American Psychiatric Association. Circulation 2008; 118:1768–1775.
- Thombs BD, de Jonge P, Coyne JC, et al Depression screening and patient outcomes in cardiovascular care: a systematic review. JAMA 2008; 300:2161–2171.
The relationship between depression and heart failure is not as obvious as the one between depression and coronary artery disease. Myriad questions on the subject are open to research:
- Does depression occur in heart failure at higher-than-expected rates?
- Does heart failure severity influence depression?
- Is depression a risk factor for heart failure? If so, why?
- How should we screen for depression in patients with heart failure?
- Do we have an evidence-based approach to treatment?
Part of the challenge in clarifying the relationship between depression and heart failure is that heart failure is a disease of chronically ill, elderly patients—a population in which adjustment disorder with depressed mood and major depression are also common diagnoses, with rates recently found to be 22.3% and 13.3%, respectively.1 Nevertheless, interest in examining the relationship between heart failure and depression is long-standing, and many clinical studies have examined this relationship.2–16 Unfortunately, measures are not standardized, so comparisons between studies are difficult.
DEPRESSION IS COMMON IN PATIENTS WITH HEART FAILURE
Many studies show that rates of depression among patients with heart failure are higher than expected among other elderly, chronically ill patients. Furthermore, depression has been linked to more severe heart failure symptoms and worse outcomes in some studies.
In a 2001 study, Jiang et al screened 374 hospitalized patients with heart failure using the Beck Depression Inventory score and found that 35% had scores of 10 or higher (indicative of at least mild depression).12 Further testing showed that 14% met criteria for major depression.
A 2006 meta-analysis of 27 studies by Rutledge et al found a 21% incidence of clinically significant depression in patients with heart failure.17 Rates of depression depended heavily on the rigor of screening criteria for classifying participants as depressed: rates were as high as 38% with the use of liberal criteria and as low as 14% with strict criteria. New York Heart Association (NYHA) functional status correlated strongly with the prevalence of depression, which increased steadily from 11% in patients with NYHA class I (mild) heart failure to 20% in those with class II, 38% in those with class III, and 42% in those with class IV (severe) heart failure.
In one of the studies included in the meta-analysis, Freedland et al found that the prevalence of major depression was strongly associated with age and functional status in hospitalized patients with heart failure.18 In patients younger than age 60 years, rates of major depression rose particularly sharply as heart failure symptoms worsened.
The Psychosocial Factors Outcome Study found that the prevalence of depression in patients with heart failure who participated in the community-based Sudden Cardiac Death in Heart Failure Trial (SCD-HeFT) was 36%, based on a score of 13 or greater on the Beck Depression Inventory-II.19 Similarly, unpublished preliminary data from the Heart Failure Adherence and Retention Trial (HART) show that about one-third of community-based patients with heart failure have depression.20
DEPRESSION AND HEART FAILURE ARE CLOSELY LINKED PHYSIOLOGICALLY
The evidence, therefore, strongly suggests a common pathway between heart failure and depression, and this evidence of a relationship favors a new paradigm that integrates the treatment of the two conditions.
BETA-BLOCKERS DO NOT RAISE RISK OF DEPRESSION
Pharmacotherapy is often implicated as a related factor in the development or exacerbation of depression in patients with heart failure, especially in those taking beta-blockers. Meta-analyses of the incidence of depression associated with various beta-blockers have been conducted in patients with hypertension, heart failure, and recent myocardial infarction. A 2002 meta-analysis of eight trials that randomized patients to treatment with a beta-blocker or placebo found no difference in the incidence of depressive symptoms between the active treatment and placebo groups, or between patients in the two groups who withdrew from the trial, presumably because of depression or other symptoms.24 An additional study not included in that meta-analysis found no differences in rates of depression among hypertensive patients according to the type of antihypertensive medication they were taking (ie, beta-blockers, diuretics, reserpine, or no drug therapy).25
Based on the evidence, I see no reason to avoid a trial of beta-blockers in patients who have depression at baseline or to be overly concerned that patients without depression will develop it as a result of beta-blocker treatment.
DEPRESSION LEADS TO WORSE OUTCOMES, HIGHER COSTS IN HEART FAILURE
Not only is depression prevalent in patients with heart failure, but depression adversely affects heart failure outcomes. One study of hospitalized patients older than 70 years found readmission rates to be 67% among heart failure patients with depression versus 44% among heart failure patients without depression.26 Patients in this study were three times as likely to die if they had heart failure than if they did not have heart failure, and they were twice as likely to die if they had depression than if they did not have depression. The mortality rate was 21% for patients with both heart failure and depression versus 15% for patients with heart failure without depression.26
Depressive symptoms also correlate with poorer quality of life in patients with heart failure. Gottlieb et al found that quality-of-life scores were significantly worse in heart failure patients if they had a diagnosis of depression on the basis of the Beck Depression Index.27
The 27-study meta-analysis by Rutledge et al discussed earlier found that the presence of depression in a patient with heart failure predicts worse outcomes in terms of hospital readmission rates, functional status, and walk times.17 This analysis also found twice the rate of death in heart failure patients with depression compared with heart failure patients without depression.
In a large community-based trial involving more than 48,000 patients with heart failure, Macchia et al found that survival was markedly reduced in patients who had a history of depression.28 This study also showed that depressed patients were less likely to adhere to medication regimens with angiotensin-converting enzyme inhibitors and beta-blockers, which may offer a potential explanation for the reduction in survival among depressed patients.
In a study of patients with coronary artery disease who had no diagnosis of depression or heart failure, May et al demonstrated that those who subsequently developed depression had more than four times the risk of also developing heart failure.29
The combination of heart failure and depression also is costly. In a 3-year retrospective study of community-based patients following a first hospitalization for heart failure, Sullivan et al found that annualized adjusted total costs were nearly 30% greater in patients diagnosed with depression and that inpatient and outpatient service utilization was also greater in those with depression.5
DIAGNOSIS AND TREATMENT
One simple question can effectively screen for depression
Numerous tools are available for the diagnosis of depression, but developing a tool that is readily useful to a busy clinician is challenging. Simply asking the single question, “Are you depressed?” has fairly high sensitivity (55%) and specificity (74%) for diagnosing depression in palliative care patients, a population even more seriously ill than heart failure patients.30 A variation on the question from British studies—“Do you feel that your life is empty?”—is considered to be a better screening question for elderly patients.31,32
Effect of depression therapy on heart failure still unclear
Unfortunately, evidence for the best treatment for depression in patients with heart failure is lacking. Some guidance may be gleaned from studies in patients with coronary artery disease. The Sertraline Antidepressant Heart Attack Randomized Trial (SADHART) was a multicenter, randomized, placebo-controlled study of the safety and efficacy of treating major depressive disorder with sertraline for 24 weeks in patients hospitalized for acute coronary syndrome.33,34 No significant differences were found between treatment groups in left ventricular ejection fraction, blood pressure, resting electrocardiogram, and cardiac arrhythmias. Although the trial was not powered to detect an effect of treatment on mortality, there were fewer deaths and severe cardiovascular adverse events in the active treatment group.
A later study was designed to evaluate 12 weeks of treatment with sertraline in patients with major depression and heart failure.35 Although symptoms of depression improved with treatment, no beneficial effect on heart failure was found.36 A nursing intervention that was included for both the treatment and placebo groups may have served to limit the impact of sertraline on heart failure surrogate end points.
The abovementioned HART study randomized patients with systolic or diastolic dysfunction and NYHA class II or III functional status to receive either heart failure education (comprising 18 American Heart Association tip sheets and 18 phone calls) or heart failure education plus self-management strategies (comprising the tip sheets, 18 group sessions, and problem-solving and self-management skills) following hospital discharge.37 Over 3 years, no difference between the two groups was found in the rates and timing of deaths or heart failure hospitalizations.
The best treatment strategies for depression in heart failure are still unclear, and more research is needed. Although guidelines exist for the management of depression in patients with coronary heart disease,38 no such guidelines have been issued for the management of depression in heart failure.
CONCLUSIONS
Although evidence is strong that treatment with medication or cognitive therapies improves symptoms of depression, evidence is lacking for a significant effect of such interventions on cardiac outcomes.39 Because depression and heart failure are so closely linked and appear to share a genetic and pathophysiologic basis, greater understanding of the relationship between these diseases across the stages of heart failure should be pursued.
Any patient with heart failure who is symptomatic has advanced disease, and is therefore closer to death than to health. The same is probably true of depression. Patients with heart failure and depression must be identified early, and interventions must be tried at these early stages of disease. Better depression screening tools and heightened awareness of the relationship between heart failure and depression are essential.
The relationship between depression and heart failure is not as obvious as the one between depression and coronary artery disease. Myriad questions on the subject are open to research:
- Does depression occur in heart failure at higher-than-expected rates?
- Does heart failure severity influence depression?
- Is depression a risk factor for heart failure? If so, why?
- How should we screen for depression in patients with heart failure?
- Do we have an evidence-based approach to treatment?
Part of the challenge in clarifying the relationship between depression and heart failure is that heart failure is a disease of chronically ill, elderly patients—a population in which adjustment disorder with depressed mood and major depression are also common diagnoses, with rates recently found to be 22.3% and 13.3%, respectively.1 Nevertheless, interest in examining the relationship between heart failure and depression is long-standing, and many clinical studies have examined this relationship.2–16 Unfortunately, measures are not standardized, so comparisons between studies are difficult.
DEPRESSION IS COMMON IN PATIENTS WITH HEART FAILURE
Many studies show that rates of depression among patients with heart failure are higher than expected among other elderly, chronically ill patients. Furthermore, depression has been linked to more severe heart failure symptoms and worse outcomes in some studies.
In a 2001 study, Jiang et al screened 374 hospitalized patients with heart failure using the Beck Depression Inventory score and found that 35% had scores of 10 or higher (indicative of at least mild depression).12 Further testing showed that 14% met criteria for major depression.
A 2006 meta-analysis of 27 studies by Rutledge et al found a 21% incidence of clinically significant depression in patients with heart failure.17 Rates of depression depended heavily on the rigor of screening criteria for classifying participants as depressed: rates were as high as 38% with the use of liberal criteria and as low as 14% with strict criteria. New York Heart Association (NYHA) functional status correlated strongly with the prevalence of depression, which increased steadily from 11% in patients with NYHA class I (mild) heart failure to 20% in those with class II, 38% in those with class III, and 42% in those with class IV (severe) heart failure.
In one of the studies included in the meta-analysis, Freedland et al found that the prevalence of major depression was strongly associated with age and functional status in hospitalized patients with heart failure.18 In patients younger than age 60 years, rates of major depression rose particularly sharply as heart failure symptoms worsened.
The Psychosocial Factors Outcome Study found that the prevalence of depression in patients with heart failure who participated in the community-based Sudden Cardiac Death in Heart Failure Trial (SCD-HeFT) was 36%, based on a score of 13 or greater on the Beck Depression Inventory-II.19 Similarly, unpublished preliminary data from the Heart Failure Adherence and Retention Trial (HART) show that about one-third of community-based patients with heart failure have depression.20
DEPRESSION AND HEART FAILURE ARE CLOSELY LINKED PHYSIOLOGICALLY
The evidence, therefore, strongly suggests a common pathway between heart failure and depression, and this evidence of a relationship favors a new paradigm that integrates the treatment of the two conditions.
BETA-BLOCKERS DO NOT RAISE RISK OF DEPRESSION
Pharmacotherapy is often implicated as a related factor in the development or exacerbation of depression in patients with heart failure, especially in those taking beta-blockers. Meta-analyses of the incidence of depression associated with various beta-blockers have been conducted in patients with hypertension, heart failure, and recent myocardial infarction. A 2002 meta-analysis of eight trials that randomized patients to treatment with a beta-blocker or placebo found no difference in the incidence of depressive symptoms between the active treatment and placebo groups, or between patients in the two groups who withdrew from the trial, presumably because of depression or other symptoms.24 An additional study not included in that meta-analysis found no differences in rates of depression among hypertensive patients according to the type of antihypertensive medication they were taking (ie, beta-blockers, diuretics, reserpine, or no drug therapy).25
Based on the evidence, I see no reason to avoid a trial of beta-blockers in patients who have depression at baseline or to be overly concerned that patients without depression will develop it as a result of beta-blocker treatment.
DEPRESSION LEADS TO WORSE OUTCOMES, HIGHER COSTS IN HEART FAILURE
Not only is depression prevalent in patients with heart failure, but depression adversely affects heart failure outcomes. One study of hospitalized patients older than 70 years found readmission rates to be 67% among heart failure patients with depression versus 44% among heart failure patients without depression.26 Patients in this study were three times as likely to die if they had heart failure than if they did not have heart failure, and they were twice as likely to die if they had depression than if they did not have depression. The mortality rate was 21% for patients with both heart failure and depression versus 15% for patients with heart failure without depression.26
Depressive symptoms also correlate with poorer quality of life in patients with heart failure. Gottlieb et al found that quality-of-life scores were significantly worse in heart failure patients if they had a diagnosis of depression on the basis of the Beck Depression Index.27
The 27-study meta-analysis by Rutledge et al discussed earlier found that the presence of depression in a patient with heart failure predicts worse outcomes in terms of hospital readmission rates, functional status, and walk times.17 This analysis also found twice the rate of death in heart failure patients with depression compared with heart failure patients without depression.
In a large community-based trial involving more than 48,000 patients with heart failure, Macchia et al found that survival was markedly reduced in patients who had a history of depression.28 This study also showed that depressed patients were less likely to adhere to medication regimens with angiotensin-converting enzyme inhibitors and beta-blockers, which may offer a potential explanation for the reduction in survival among depressed patients.
In a study of patients with coronary artery disease who had no diagnosis of depression or heart failure, May et al demonstrated that those who subsequently developed depression had more than four times the risk of also developing heart failure.29
The combination of heart failure and depression also is costly. In a 3-year retrospective study of community-based patients following a first hospitalization for heart failure, Sullivan et al found that annualized adjusted total costs were nearly 30% greater in patients diagnosed with depression and that inpatient and outpatient service utilization was also greater in those with depression.5
DIAGNOSIS AND TREATMENT
One simple question can effectively screen for depression
Numerous tools are available for the diagnosis of depression, but developing a tool that is readily useful to a busy clinician is challenging. Simply asking the single question, “Are you depressed?” has fairly high sensitivity (55%) and specificity (74%) for diagnosing depression in palliative care patients, a population even more seriously ill than heart failure patients.30 A variation on the question from British studies—“Do you feel that your life is empty?”—is considered to be a better screening question for elderly patients.31,32
Effect of depression therapy on heart failure still unclear
Unfortunately, evidence for the best treatment for depression in patients with heart failure is lacking. Some guidance may be gleaned from studies in patients with coronary artery disease. The Sertraline Antidepressant Heart Attack Randomized Trial (SADHART) was a multicenter, randomized, placebo-controlled study of the safety and efficacy of treating major depressive disorder with sertraline for 24 weeks in patients hospitalized for acute coronary syndrome.33,34 No significant differences were found between treatment groups in left ventricular ejection fraction, blood pressure, resting electrocardiogram, and cardiac arrhythmias. Although the trial was not powered to detect an effect of treatment on mortality, there were fewer deaths and severe cardiovascular adverse events in the active treatment group.
A later study was designed to evaluate 12 weeks of treatment with sertraline in patients with major depression and heart failure.35 Although symptoms of depression improved with treatment, no beneficial effect on heart failure was found.36 A nursing intervention that was included for both the treatment and placebo groups may have served to limit the impact of sertraline on heart failure surrogate end points.
The abovementioned HART study randomized patients with systolic or diastolic dysfunction and NYHA class II or III functional status to receive either heart failure education (comprising 18 American Heart Association tip sheets and 18 phone calls) or heart failure education plus self-management strategies (comprising the tip sheets, 18 group sessions, and problem-solving and self-management skills) following hospital discharge.37 Over 3 years, no difference between the two groups was found in the rates and timing of deaths or heart failure hospitalizations.
The best treatment strategies for depression in heart failure are still unclear, and more research is needed. Although guidelines exist for the management of depression in patients with coronary heart disease,38 no such guidelines have been issued for the management of depression in heart failure.
CONCLUSIONS
Although evidence is strong that treatment with medication or cognitive therapies improves symptoms of depression, evidence is lacking for a significant effect of such interventions on cardiac outcomes.39 Because depression and heart failure are so closely linked and appear to share a genetic and pathophysiologic basis, greater understanding of the relationship between these diseases across the stages of heart failure should be pursued.
Any patient with heart failure who is symptomatic has advanced disease, and is therefore closer to death than to health. The same is probably true of depression. Patients with heart failure and depression must be identified early, and interventions must be tried at these early stages of disease. Better depression screening tools and heightened awareness of the relationship between heart failure and depression are essential.
- Yazgan IC, Kuscu MK, Fistikci N, Keyvan A, Topcuoglu V. Geriatric psychiatry consultations in a Turkish university hospital. Int Psychogeriatr 2006; 18:327–333.
- Abramson J, Berger A, Krumholz HM, Vaccarino V. Depression and risk of heart failure among older persons with isolated systolic hypertension. Arch Intern Med 2001; 161:1725–1730.
- Williams SA, Kasl SV, Heiat A, Abramson JL, Krumholz HM, Vaccarino V. Depression and risk of heart failure among the elderly: a prospective community-based study. Psychosom Med 2002; 64:6–12.
- Himelhoch S, Weller WE, Wu AW, Anderson GF, Cooper LA. Chronic medical illness, depression, and use of acute medical services among Medicare beneficiaries. Med Care 2004; 42:512–521.
- Sullivan M, Simon G, Spertus J, Russo J. Depression-related costs in heart failure care. Arch Intern Med 2002; 162:1860–1866.
- Fulop G, Strain JJ, Stettin G. Congestive heart failure and depression in older adults: clinical course and health services use 6 months after hospitalization. Psychosomatics 2003; 44:367–373.
- Koenig HG. Depression in hospitalized older patients with congestive heart failure. Gen Hosp Psychiatry 1998; 20:29–43.
- Rumsfeld JS, Havranek E, Masoudi FA, et al Depressive symptoms are the strongest predictors of short-term declines in health status in patients with heart failure. J Am Coll Cardiol 2003; 42:1811–1817.
- de Denus S, Spinler SA, Jessup M, Kao A. History of depression as a predictor of adverse outcomes in patients hospitalized for decompensated heart failure. Pharmacotherapy 2004; 24:1306–1310.
- Faris R, Purcell H, Henein MY, Coats AJ. Clinical depression is common and significantly associated with reduced survival in patients with non-ischaemic heart failure. Eur J Heart Fail 2002; 4:541–551.
- Freedland KE, Carney RM, Rich MW, et al Depression in elderly patients with congestive heart failure. J Geriatr Psychiatry 1991; 24:59–71.
- Jiang W, Alexander J, Christopher E, et al Relationship of depression to increased risk of mortality and rehospitalization in patients with congestive heart failure. Arch Intern Med 2001; 161:1849–1856.
- Jünger J, Schellberg D, Müller-Tasch T, et al Depression increasingly predicts mortality in the course of congestive heart failure. Eur J Heart Fail 2005; 7:261–267.
- Murberg TA, Bru E, Svebak S, Tveterås R, Aarsland T. Depressed mood and subjective health symptoms as predictors of mortality in patients with congestive heart failure: a two-years follow-up study. Int J Psychiatry Med 1999; 29:311–326.
- Sullivan MD, Levy WC, Crane BA, Russo JE, Spertus JA. Usefulness of depression to predict time to combined end point of transplant or death for outpatients with advanced heart failure. Am J Cardiol 2004; 94:1577–1580.
- Vaccarino V, Kasl SV, Abramson J, Krumholz HM. Depressive symptoms and risk of functional decline and death in patients with heart failure. J Am Coll Cardiol 2001; 38:199–205.
- Rutledge T, Reis VA, Linke SE, Greenberg BH, Mills PJ. Depression in heart failure: a meta-analytic review of prevalence, intervention effects, and associations with clinical outcomes. J Am Coll Cardiol 2006; 48:1527–1537.
- Freedland KE, Rich MW, Skala JA, Carney RM, Dávila-Román VG, Jaffe AS. Prevalence of depression in hospitalized patients with congestive heart failure. Psychosom Med 2003; 65:119–128.
- Friedmann E, Thomas SA, Liu F, et al Relationship of depression, anxiety, and social isolation to chronic heart failure outpatient mortality. Am Heart J 2006; 152:940.e1–940.e8.
- de Leon CF, Grady KL, Eaton C, et al Quality of life in a diverse population of patients with heart failure: baseline findings from the Heart Failure Adherence and Retention trial (HART). J Cardiopulm Rehabil Prev 2009; 29:171–178.
- Musselman DL, Evans DL, Nemeroff CB. The relationship of depression to cardiovascular disease: epidemiology, biology, and treatment. Arch Gen Psychiatry 1998; 55:580–592.
- Caspi A, Sugden K, Moffitt TE, et al Influence of life stress on depression: moderation by a polymorphism in the 5-HTT gene. Science 2003; 301:386–389.
- Cohn JN, Levine TB, Olivari MT, et al Plasma norepinephrine as a guide to prognosis in patients with chronic congestive heart failure. N Engl J Med 1984; 311:819–823.
- Ko DT, Hebert PR, Coffey CS, Sedrakyan A, Curtis JP, Krumholz HM. β-blocker therapy and symptoms of depression, fatigue, and sexual dysfunction. JAMA 2002; 288:351–357.
- Prisant LM, Spruill WJ, Fincham JE, Wade WE, Carr AA, Adams MA. Depression associated with antihypertensive drugs. J Fam Pract 1991; 33:481–485.
- Rozzini R, Sabatini T, Frisoni GB, et al Depression and major outcomes in older patients with heart failure [letter]. Arch Intern Med 2002; 162:362–364.
- Gottlieb SS, Khatta M, Friedmann E, et al The influence of age, gender, and race on the prevalence of depression in heart failure patients. J Am Coll Cardiol 2004; 43:1542–1549.
- Macchia A, Monte S, Pellegrini F, et al Depression worsens outcomes in elderly patients with heart failure: an analysis of 48,117 patients in a community setting. Eur J Heart Fail 2008; 10:714–721.
- May HT, Horne BD, Carlquist JF, Sheng X, Joy E, Catinella AP. Depression after coronary artery disease is associated with heart failure. J Am Coll Cardiol 2009; 53:1440–1447.
- Lloyd-Williams M, Dennis M, Taylor F, Baker I. Is asking patients in palliative care, “Are you depressed?” appropriate? Prospective study. BMJ 2003; 327:372–373.
- Whelan PJ, Gaughran F, Walwyn R, Chatterton K, Macdonald A. ‘Do you feel that your life is empty?’ The clinical utility of a one-off question for detecting depression in elderly care home residents. Age Ageing 2008; 37:475–478.
- D’Ath P, Katona P, Mullan E, Evans S, Katona C. Screening, detection and management of depression in elderly primary care attenders. I: The acceptability and performance of the 15 item Geriatric Depression Scale (GDS15) and the development of short versions. Fam Pract 1994; 11:260–266.
- Glassman AH, O’Connor CM, Califf RM, et al., Sertraline Antidepressant Heart Attack Randomized Trial (SADHART) Group. Sertraline treatment of major depression in patients with acute MI or unstable angina. JAMA 2002; 288:701–709.
- Carney RM, Jaffe AS. Treatment of depression following acute myocardial infarction. JAMA 2002; 288:750–751.
- Jiang W, O’Connor C, Silva SG, et al., SADHART-CHF Investigators. Safety and efficacy of sertraline for depression in patients with CHF (SADHART-CHF): a randomized, double-blind, placebo-controlled trial of sertraline for major depression with congestive heart failure. Am Heart J 2008; 156:437–444.
- O’Connor CM, Wei J, Silva SG, et al., SADHART-CHF investigators. Safety and efficacy of sertraline plus nurse facilitated supportive intervention (NFSI) versus placebo plus nurse facilitated supportive intervention for depression in patients with CHF (SADHART-CHF). Presented at: 2008 Scientific Sessions of the Heart Failure Society of America; September 20–23, 2008; Toronto, ON, Canada.
- Powell LH, Calvin JE, Mendes de Leon CF, et al Impact of patient self-management skills training on death and hospitalization in patients with heart failure: results from the Heart Failure Adherence and Retention Trial. Circulation 2007; 116:2629. Abstract.
- Lichtman JH, Bigger JT, Blumenthal JA, et al Depression and coronary heart disease: recommendations for screening, referral, and treatment: a science advisory from the American Heart Association Prevention Committee of the Council on Cardiovascular Nursing, Council on Clinical Cardiology, Council on Epidemiology and Prevention, and Interdisciplinary Council on Quality of Care and Outcomes Research: endorsed by the American Psychiatric Association. Circulation 2008; 118:1768–1775.
- Thombs BD, de Jonge P, Coyne JC, et al Depression screening and patient outcomes in cardiovascular care: a systematic review. JAMA 2008; 300:2161–2171.
- Yazgan IC, Kuscu MK, Fistikci N, Keyvan A, Topcuoglu V. Geriatric psychiatry consultations in a Turkish university hospital. Int Psychogeriatr 2006; 18:327–333.
- Abramson J, Berger A, Krumholz HM, Vaccarino V. Depression and risk of heart failure among older persons with isolated systolic hypertension. Arch Intern Med 2001; 161:1725–1730.
- Williams SA, Kasl SV, Heiat A, Abramson JL, Krumholz HM, Vaccarino V. Depression and risk of heart failure among the elderly: a prospective community-based study. Psychosom Med 2002; 64:6–12.
- Himelhoch S, Weller WE, Wu AW, Anderson GF, Cooper LA. Chronic medical illness, depression, and use of acute medical services among Medicare beneficiaries. Med Care 2004; 42:512–521.
- Sullivan M, Simon G, Spertus J, Russo J. Depression-related costs in heart failure care. Arch Intern Med 2002; 162:1860–1866.
- Fulop G, Strain JJ, Stettin G. Congestive heart failure and depression in older adults: clinical course and health services use 6 months after hospitalization. Psychosomatics 2003; 44:367–373.
- Koenig HG. Depression in hospitalized older patients with congestive heart failure. Gen Hosp Psychiatry 1998; 20:29–43.
- Rumsfeld JS, Havranek E, Masoudi FA, et al Depressive symptoms are the strongest predictors of short-term declines in health status in patients with heart failure. J Am Coll Cardiol 2003; 42:1811–1817.
- de Denus S, Spinler SA, Jessup M, Kao A. History of depression as a predictor of adverse outcomes in patients hospitalized for decompensated heart failure. Pharmacotherapy 2004; 24:1306–1310.
- Faris R, Purcell H, Henein MY, Coats AJ. Clinical depression is common and significantly associated with reduced survival in patients with non-ischaemic heart failure. Eur J Heart Fail 2002; 4:541–551.
- Freedland KE, Carney RM, Rich MW, et al Depression in elderly patients with congestive heart failure. J Geriatr Psychiatry 1991; 24:59–71.
- Jiang W, Alexander J, Christopher E, et al Relationship of depression to increased risk of mortality and rehospitalization in patients with congestive heart failure. Arch Intern Med 2001; 161:1849–1856.
- Jünger J, Schellberg D, Müller-Tasch T, et al Depression increasingly predicts mortality in the course of congestive heart failure. Eur J Heart Fail 2005; 7:261–267.
- Murberg TA, Bru E, Svebak S, Tveterås R, Aarsland T. Depressed mood and subjective health symptoms as predictors of mortality in patients with congestive heart failure: a two-years follow-up study. Int J Psychiatry Med 1999; 29:311–326.
- Sullivan MD, Levy WC, Crane BA, Russo JE, Spertus JA. Usefulness of depression to predict time to combined end point of transplant or death for outpatients with advanced heart failure. Am J Cardiol 2004; 94:1577–1580.
- Vaccarino V, Kasl SV, Abramson J, Krumholz HM. Depressive symptoms and risk of functional decline and death in patients with heart failure. J Am Coll Cardiol 2001; 38:199–205.
- Rutledge T, Reis VA, Linke SE, Greenberg BH, Mills PJ. Depression in heart failure: a meta-analytic review of prevalence, intervention effects, and associations with clinical outcomes. J Am Coll Cardiol 2006; 48:1527–1537.
- Freedland KE, Rich MW, Skala JA, Carney RM, Dávila-Román VG, Jaffe AS. Prevalence of depression in hospitalized patients with congestive heart failure. Psychosom Med 2003; 65:119–128.
- Friedmann E, Thomas SA, Liu F, et al Relationship of depression, anxiety, and social isolation to chronic heart failure outpatient mortality. Am Heart J 2006; 152:940.e1–940.e8.
- de Leon CF, Grady KL, Eaton C, et al Quality of life in a diverse population of patients with heart failure: baseline findings from the Heart Failure Adherence and Retention trial (HART). J Cardiopulm Rehabil Prev 2009; 29:171–178.
- Musselman DL, Evans DL, Nemeroff CB. The relationship of depression to cardiovascular disease: epidemiology, biology, and treatment. Arch Gen Psychiatry 1998; 55:580–592.
- Caspi A, Sugden K, Moffitt TE, et al Influence of life stress on depression: moderation by a polymorphism in the 5-HTT gene. Science 2003; 301:386–389.
- Cohn JN, Levine TB, Olivari MT, et al Plasma norepinephrine as a guide to prognosis in patients with chronic congestive heart failure. N Engl J Med 1984; 311:819–823.
- Ko DT, Hebert PR, Coffey CS, Sedrakyan A, Curtis JP, Krumholz HM. β-blocker therapy and symptoms of depression, fatigue, and sexual dysfunction. JAMA 2002; 288:351–357.
- Prisant LM, Spruill WJ, Fincham JE, Wade WE, Carr AA, Adams MA. Depression associated with antihypertensive drugs. J Fam Pract 1991; 33:481–485.
- Rozzini R, Sabatini T, Frisoni GB, et al Depression and major outcomes in older patients with heart failure [letter]. Arch Intern Med 2002; 162:362–364.
- Gottlieb SS, Khatta M, Friedmann E, et al The influence of age, gender, and race on the prevalence of depression in heart failure patients. J Am Coll Cardiol 2004; 43:1542–1549.
- Macchia A, Monte S, Pellegrini F, et al Depression worsens outcomes in elderly patients with heart failure: an analysis of 48,117 patients in a community setting. Eur J Heart Fail 2008; 10:714–721.
- May HT, Horne BD, Carlquist JF, Sheng X, Joy E, Catinella AP. Depression after coronary artery disease is associated with heart failure. J Am Coll Cardiol 2009; 53:1440–1447.
- Lloyd-Williams M, Dennis M, Taylor F, Baker I. Is asking patients in palliative care, “Are you depressed?” appropriate? Prospective study. BMJ 2003; 327:372–373.
- Whelan PJ, Gaughran F, Walwyn R, Chatterton K, Macdonald A. ‘Do you feel that your life is empty?’ The clinical utility of a one-off question for detecting depression in elderly care home residents. Age Ageing 2008; 37:475–478.
- D’Ath P, Katona P, Mullan E, Evans S, Katona C. Screening, detection and management of depression in elderly primary care attenders. I: The acceptability and performance of the 15 item Geriatric Depression Scale (GDS15) and the development of short versions. Fam Pract 1994; 11:260–266.
- Glassman AH, O’Connor CM, Califf RM, et al., Sertraline Antidepressant Heart Attack Randomized Trial (SADHART) Group. Sertraline treatment of major depression in patients with acute MI or unstable angina. JAMA 2002; 288:701–709.
- Carney RM, Jaffe AS. Treatment of depression following acute myocardial infarction. JAMA 2002; 288:750–751.
- Jiang W, O’Connor C, Silva SG, et al., SADHART-CHF Investigators. Safety and efficacy of sertraline for depression in patients with CHF (SADHART-CHF): a randomized, double-blind, placebo-controlled trial of sertraline for major depression with congestive heart failure. Am Heart J 2008; 156:437–444.
- O’Connor CM, Wei J, Silva SG, et al., SADHART-CHF investigators. Safety and efficacy of sertraline plus nurse facilitated supportive intervention (NFSI) versus placebo plus nurse facilitated supportive intervention for depression in patients with CHF (SADHART-CHF). Presented at: 2008 Scientific Sessions of the Heart Failure Society of America; September 20–23, 2008; Toronto, ON, Canada.
- Powell LH, Calvin JE, Mendes de Leon CF, et al Impact of patient self-management skills training on death and hospitalization in patients with heart failure: results from the Heart Failure Adherence and Retention Trial. Circulation 2007; 116:2629. Abstract.
- Lichtman JH, Bigger JT, Blumenthal JA, et al Depression and coronary heart disease: recommendations for screening, referral, and treatment: a science advisory from the American Heart Association Prevention Committee of the Council on Cardiovascular Nursing, Council on Clinical Cardiology, Council on Epidemiology and Prevention, and Interdisciplinary Council on Quality of Care and Outcomes Research: endorsed by the American Psychiatric Association. Circulation 2008; 118:1768–1775.
- Thombs BD, de Jonge P, Coyne JC, et al Depression screening and patient outcomes in cardiovascular care: a systematic review. JAMA 2008; 300:2161–2171.