User login
PELVIC SURGERY
The authors report no financial relationships relevant to this article.
The use of transvaginal mesh—with or without trocar placement—is surrounded by controversy. A number of minimally invasive vaginal mesh kits are commercially available for the repair of pelvic organ prolapse, and new kits are entering the market rapidly. The challenge is determining whether these new techniques are as effective and safe as traditional prolapse repairs.
Although the use of permanent mesh to repair prolapse has been explored in retrospective and prospective studies, no rigorous controlled trials have compared these new procedures with abdominal sacrocolpopexy or uterosacral ligament suspension, for example. The current body of literature does suggest a high rate of recurrent prolapse after traditional anterior or posterior colporrhaphy, and the use of allograft material has not been shown to improve outcomes. Surgeons are now turning their attention to permanent polypropylene mesh as a possible alternative. In addition, repair of the vaginal apex at the time of anterior and posterior vaginal wall repair is being explored as a way to increase durability of the repair. The new trocar-delivered mesh kits address this issue by suspending the vaginal vault while providing support to the vaginal walls.
This article highlights three recent studies that focus on a new trocar-delivered, protected, low-weight polypropylene mesh (Ugytex, distributed by Bard as Pelvitex) and three trocar-delivered mesh kits (Prolift, Apogee, and Perigee).
One-year outcomes encouraging for low-weight polypropylene mesh
De Tayrac R, Devoldere G, Renaudie J, Villard P, Guilbaud O, Eglin G. Prolapse repair by vaginal route using a new protected low-weight polypropylene mesh: 1-year functional and anatomical outcome in a prospective multicentre study. Int Urogynecol J Pelvic Floor Dysfunct. 2007;18:251–256.
This study evaluated functional and anatomic outcomes after placement for prolapse repair of low-weight polypropylene mesh protected by absorbable hydrophilic film. The film, a combination of atelocollagen, polyethylene glycol, and glycerol, is designed to protect pelvic organs from acute inflammation during healing. In a separate investigation of unprotected, heavyweight polypropylene mesh in prolapse repair, the anatomic success rate ranged from 75% to 100%, but the rate of mesh erosion (13%) and dyspareunia (69%) seemed unacceptably high.1
Rigorous preoperative assessment
In this trial, 230 women with symptomatic vaginal wall prolapse were recruited at 13 centers in a consecutive fashion. At enrollment, all patients were measured using the pelvic organ prolapse quantitative staging system (POP-Q). They also completed the validated Pelvic Floor Distress Inventory and Pelvic Floor Impact Questionnaire. The presence and severity of dyspareunia were also recorded, as well as the Urinary Dysfunction Measurement Scale. All participants had prolapse equal to or exceeding stage II.
Surgeons used trocars to percutaneously place a low-weight (38 g/m2) and highly porous polypropylene monofilament mesh (Ugytex/Pelvitex) for vaginal repair and performed any concomitant procedures. Perioperative and postoperative complications were recorded. Patients were evaluated at 6 weeks, 6 months, and 1 year. The first 143 patients with at least 10 months of follow-up were analyzed, with a mean follow-up of 13±2 months (range: 10–19). Anatomic cure was defined as no prolapse greater than or equal to stage II.
Patient satisfaction was high
The anatomic cure rate was 92.3%, with a 6.8% recurrence of anterior vaginal wall prolapse and 2.6% recurrence of posterior vaginal wall prolapse. Only one patient with recurrence was symptomatic.
Six of 143 patients (4.2%) sustained an intraoperative complication: three bladder injuries, one rectal injury, one uterine artery hemorrhage (during hysterectomy), and one vaginal sulcus perforation (during transobturator tape placement). The most significant postoperative complication related to the vaginal mesh kit was vaginal hematoma; one of the two cases required reoperation and partial removal of the mesh.
Nine patients developed mesh erosion in the first 3 months, for an erosion rate of 6.3%. Six required partial excision of the mesh. Overall, symptoms and quality of life improved significantly, with an overall satisfaction rate at follow-up of 96.5%. No significant difference was noted between pre- and postoperative rates of dyspareunia.
Further evaluation is warranted
The authors are already conducting a randomized trial to compare anterior vaginal wall repair using this low-weight polypropylene mesh with traditional anterior colporrhaphy to confirm and explore these results.
Note: Bard now offers a kit called Avaulta Plus that uses the same mesh material with a trocar delivery system, previously lacking (although investigators used trocars in this study).
Perioperative complications were uncommon with Prolift system
Altman D, Falconer C. Perioperative morbidity using transvaginal mesh in pelvic organ prolapse repair. Obstet Gynecol. 2007;109:303–308.
This study explored the frequency and characteristics of perioperative complications associated with the use of Prolift, a transvaginal mesh system for the repair of pelvic organ prolapse (FIGURE). Twenty-five centers participated by registering a standardized safety protocol form for 248 women who underwent surgery using the system over a 6-month period. The form included information about perioperative complications, adverse intraoperative events, and the associated hospital stay, as well as obstetric and gynecologic medical history and previous pelvic surgery.
Pelvic organ perforation (lower urinary tract or anorectal injury) and blood loss greater than 1,000 mL were recorded as major complications, and any other adverse events related to the hospital stay were documented as minor complications. Most of the cohort had already undergone prolapse repair, and prolapse had recurred in the same vaginal compartment.
One author was an educational adviser for Gynecare Sweden AB, and the other an adviser for Johnson & Johnson. Although the study was funded entirely by university-administered research funds, pretrial scientific meetings were paid for by Gynecare Sweden AB.
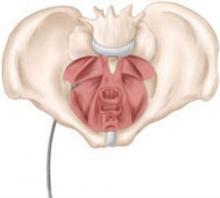
FIGURE: Mesh support of pelvic organs
Prolift mesh in final position, with extension arms passed through the sacrospinous ligaments and the obturator foramen bilaterally.
4.4% rate of serious complications
Serious complications occurred in 4.4% (11 of 248) of cases (95% confidence interval [CI], 2.5–7.8). The predominant complication was visceral injury, which included bladder, urethral, and rectal perforation. One patient had blood loss exceeding 1,000 mL.
Minor complications occurred in 44 patients (18%). The most common minor complication was urinary tract infection. Adverse events included urinary retention requiring catheterization, anemia, transfusion, fever, groin and buttock pain, and vaginal hematoma, among others.
Concurrent pelvic floor surgery increased the risk for minor complications (odds ratio, 2.8; 95% CI, 1.1–6.9). Concurrent procedures included vaginal hysterectomy, sling procedure with tension-free vaginal tape or transobturator tension-free tape, sacrospinal fixation, repair of vaginal enterocele, and bilateral salpingo-oophorectomy. This risk analysis identified no other predictors of outcome.
Posterior/apical repair
- Adequately infiltrate the vaginal epithelium with diluted epinephrine solution, especially toward the lateral apices, to facilitate hemostasis and dissection
- Be thorough in lateral dissection toward the ischial spine and stay in the proper surgical plane to create a thick vaginal epithelial flap
- Palpate the ischial spine, with the preoperatively packed rectum retracted medially
- During passage of the trocar, place an index finger along the vaginal dissection to palpate the trocar in the ischiorectal fossa and deep to the levator ani muscles until the tip is palpated at the level of the ischial spine
- Pass the trocar through the arcus tendineus/levator fascia at the level of the ischial spine, as shown below:
- Do not apply excess tension to the straps of the graft material
- Do not trim the vaginal epithelium
Anterior wall (obturator foramen trocar passage)
- Same key points as posterior wall technique, but in anterior repair, there are two passes through the obturator foramen
- The first trocar is inserted into the inferior obturator foramen, rotated, and guided with the surgeon’s finger inserted into and held in the vaginal dissection, as shown below:
- The superior passage exits close to the bladder neck, and the inferior passage approximates the ischial spine. Penetrate along the arcus tendineus approximately 1 cm from the ischial spine
Caution! Keep summary points in context
These key points are not intended as formal medical training, but as general information only. Continued research into these techniques is needed to assess long-term outcomes.
Short-term outcomes data only
Because this study focused on immediate complications, no long-term data on such complications as persistent pain, mesh erosion, or infection were collected.
All surgeons underwent hands-on training with the transvaginal repair system before patients were enrolled in the study. Nevertheless, the authors observe that many repair procedures were performed at the beginning of the physicians’ learning curve, with a higher number of complications than would be expected from more experienced surgeons.
The data may also have been affected by selection bias (ie, toward more complicated cases), given that most patients had already undergone prolapse repair.
Two systems yield excellent short-term results in women with recurrent prolapse
Gauruder-Burmester A, Koutouzidou P, Rohne J, Gronewold M, Tunn R. Follow-up after polypropylene mesh repair of anterior and posterior compartments in patients with recurrent prolapse. Int Urogynecol J Pelvic Floor Dysfunct. 2007;18:1059–1064.
This retrospective study involved women who had already undergone one or more prolapse repairs. These patients then underwent reoperation with mesh-reinforced repair. The authors hypothesized that recurrent prolapse represents poor tissue quality, necessitating the use of mesh in subsequent repairs. Both pre- and postoperative symptoms and functional changes were analyzed, with a special focus on mesh erosion and sexual function.
Details of the study
Of 145 women who underwent repair with the Apogee (apical posterior) or Perigee (anterior wall) system during a 1-year period, 120 were included in the analysis. The other 25 patients were excluded because they did not return for follow-up, were missing urodynamic data, or had inaccurate POP-Q staging. All patients had recurrent stage III posterior or anterior vaginal wall prolapse. Forty percent of patients had an apical posterior repair, and 60% had anterior wall repair. None had both procedures performed simultaneously.
All patients had undergone hysterectomy and received vaginal estrogen before and after surgery. Urinary incontinence was treated in a two-step fashion; that is, it was not addressed until 3 months after repair of the prolapse. Routine follow-up occurred at 1 month and 1 year after surgery.
One-year cure rate was 93%
No perioperative or intraoperative complications occurred, and mean operative time was 35±4.5 minutes. Mesh erosion occurred in four patients (3%) and involved anterior mesh placement only. No mesh infections were noted.
At 1 year, 93% of women were anatomically cured of prolapse (ie, they had less than stage II prolapse). Prolapse recurred in eight women; all cases involved the anterior compartment.
No dyspareunia was associated with the repair. In fact, prolapse-associated dyspareunia resolved in all 15 women who reported this symptom before surgery. In addition, questionnaires about quality of life and satisfaction revealed significant improvement after mesh placement (P=.023).
The authors attribute the positive results to the fact that both surgeons involved in the study used the technique on 15 patients before operating on study participants, minimizing the effect of the learning curve. The authors were also careful about patient selection.
Results merit cautious optimism
The authors propose that the low erosion rate and lack of new-onset dyspareunia after surgery may be misleading because long-term results have not yet been obtained. We also speculate that precise dissection in the proper surgical plane likely minimized early erosions.
Reference
1. Milani R, Salvatore S, Soligo M, Pifarotti P, Meschia M, Cortese M. Functional and anatomical outcome of anterior and posterior vaginal prolapse repair with prolene mesh. Br J Obstet Gynaecol. 2004;111:1-5.
The authors report no financial relationships relevant to this article.
The use of transvaginal mesh—with or without trocar placement—is surrounded by controversy. A number of minimally invasive vaginal mesh kits are commercially available for the repair of pelvic organ prolapse, and new kits are entering the market rapidly. The challenge is determining whether these new techniques are as effective and safe as traditional prolapse repairs.
Although the use of permanent mesh to repair prolapse has been explored in retrospective and prospective studies, no rigorous controlled trials have compared these new procedures with abdominal sacrocolpopexy or uterosacral ligament suspension, for example. The current body of literature does suggest a high rate of recurrent prolapse after traditional anterior or posterior colporrhaphy, and the use of allograft material has not been shown to improve outcomes. Surgeons are now turning their attention to permanent polypropylene mesh as a possible alternative. In addition, repair of the vaginal apex at the time of anterior and posterior vaginal wall repair is being explored as a way to increase durability of the repair. The new trocar-delivered mesh kits address this issue by suspending the vaginal vault while providing support to the vaginal walls.
This article highlights three recent studies that focus on a new trocar-delivered, protected, low-weight polypropylene mesh (Ugytex, distributed by Bard as Pelvitex) and three trocar-delivered mesh kits (Prolift, Apogee, and Perigee).
One-year outcomes encouraging for low-weight polypropylene mesh
De Tayrac R, Devoldere G, Renaudie J, Villard P, Guilbaud O, Eglin G. Prolapse repair by vaginal route using a new protected low-weight polypropylene mesh: 1-year functional and anatomical outcome in a prospective multicentre study. Int Urogynecol J Pelvic Floor Dysfunct. 2007;18:251–256.
This study evaluated functional and anatomic outcomes after placement for prolapse repair of low-weight polypropylene mesh protected by absorbable hydrophilic film. The film, a combination of atelocollagen, polyethylene glycol, and glycerol, is designed to protect pelvic organs from acute inflammation during healing. In a separate investigation of unprotected, heavyweight polypropylene mesh in prolapse repair, the anatomic success rate ranged from 75% to 100%, but the rate of mesh erosion (13%) and dyspareunia (69%) seemed unacceptably high.1
Rigorous preoperative assessment
In this trial, 230 women with symptomatic vaginal wall prolapse were recruited at 13 centers in a consecutive fashion. At enrollment, all patients were measured using the pelvic organ prolapse quantitative staging system (POP-Q). They also completed the validated Pelvic Floor Distress Inventory and Pelvic Floor Impact Questionnaire. The presence and severity of dyspareunia were also recorded, as well as the Urinary Dysfunction Measurement Scale. All participants had prolapse equal to or exceeding stage II.
Surgeons used trocars to percutaneously place a low-weight (38 g/m2) and highly porous polypropylene monofilament mesh (Ugytex/Pelvitex) for vaginal repair and performed any concomitant procedures. Perioperative and postoperative complications were recorded. Patients were evaluated at 6 weeks, 6 months, and 1 year. The first 143 patients with at least 10 months of follow-up were analyzed, with a mean follow-up of 13±2 months (range: 10–19). Anatomic cure was defined as no prolapse greater than or equal to stage II.
Patient satisfaction was high
The anatomic cure rate was 92.3%, with a 6.8% recurrence of anterior vaginal wall prolapse and 2.6% recurrence of posterior vaginal wall prolapse. Only one patient with recurrence was symptomatic.
Six of 143 patients (4.2%) sustained an intraoperative complication: three bladder injuries, one rectal injury, one uterine artery hemorrhage (during hysterectomy), and one vaginal sulcus perforation (during transobturator tape placement). The most significant postoperative complication related to the vaginal mesh kit was vaginal hematoma; one of the two cases required reoperation and partial removal of the mesh.
Nine patients developed mesh erosion in the first 3 months, for an erosion rate of 6.3%. Six required partial excision of the mesh. Overall, symptoms and quality of life improved significantly, with an overall satisfaction rate at follow-up of 96.5%. No significant difference was noted between pre- and postoperative rates of dyspareunia.
Further evaluation is warranted
The authors are already conducting a randomized trial to compare anterior vaginal wall repair using this low-weight polypropylene mesh with traditional anterior colporrhaphy to confirm and explore these results.
Note: Bard now offers a kit called Avaulta Plus that uses the same mesh material with a trocar delivery system, previously lacking (although investigators used trocars in this study).
Perioperative complications were uncommon with Prolift system
Altman D, Falconer C. Perioperative morbidity using transvaginal mesh in pelvic organ prolapse repair. Obstet Gynecol. 2007;109:303–308.
This study explored the frequency and characteristics of perioperative complications associated with the use of Prolift, a transvaginal mesh system for the repair of pelvic organ prolapse (FIGURE). Twenty-five centers participated by registering a standardized safety protocol form for 248 women who underwent surgery using the system over a 6-month period. The form included information about perioperative complications, adverse intraoperative events, and the associated hospital stay, as well as obstetric and gynecologic medical history and previous pelvic surgery.
Pelvic organ perforation (lower urinary tract or anorectal injury) and blood loss greater than 1,000 mL were recorded as major complications, and any other adverse events related to the hospital stay were documented as minor complications. Most of the cohort had already undergone prolapse repair, and prolapse had recurred in the same vaginal compartment.
One author was an educational adviser for Gynecare Sweden AB, and the other an adviser for Johnson & Johnson. Although the study was funded entirely by university-administered research funds, pretrial scientific meetings were paid for by Gynecare Sweden AB.
FIGURE: Mesh support of pelvic organs
Prolift mesh in final position, with extension arms passed through the sacrospinous ligaments and the obturator foramen bilaterally.
4.4% rate of serious complications
Serious complications occurred in 4.4% (11 of 248) of cases (95% confidence interval [CI], 2.5–7.8). The predominant complication was visceral injury, which included bladder, urethral, and rectal perforation. One patient had blood loss exceeding 1,000 mL.
Minor complications occurred in 44 patients (18%). The most common minor complication was urinary tract infection. Adverse events included urinary retention requiring catheterization, anemia, transfusion, fever, groin and buttock pain, and vaginal hematoma, among others.
Concurrent pelvic floor surgery increased the risk for minor complications (odds ratio, 2.8; 95% CI, 1.1–6.9). Concurrent procedures included vaginal hysterectomy, sling procedure with tension-free vaginal tape or transobturator tension-free tape, sacrospinal fixation, repair of vaginal enterocele, and bilateral salpingo-oophorectomy. This risk analysis identified no other predictors of outcome.
Posterior/apical repair
- Adequately infiltrate the vaginal epithelium with diluted epinephrine solution, especially toward the lateral apices, to facilitate hemostasis and dissection
- Be thorough in lateral dissection toward the ischial spine and stay in the proper surgical plane to create a thick vaginal epithelial flap
- Palpate the ischial spine, with the preoperatively packed rectum retracted medially
- During passage of the trocar, place an index finger along the vaginal dissection to palpate the trocar in the ischiorectal fossa and deep to the levator ani muscles until the tip is palpated at the level of the ischial spine
- Pass the trocar through the arcus tendineus/levator fascia at the level of the ischial spine, as shown below:
- Do not apply excess tension to the straps of the graft material
- Do not trim the vaginal epithelium
Anterior wall (obturator foramen trocar passage)
- Same key points as posterior wall technique, but in anterior repair, there are two passes through the obturator foramen
- The first trocar is inserted into the inferior obturator foramen, rotated, and guided with the surgeon’s finger inserted into and held in the vaginal dissection, as shown below:
- The superior passage exits close to the bladder neck, and the inferior passage approximates the ischial spine. Penetrate along the arcus tendineus approximately 1 cm from the ischial spine
Caution! Keep summary points in context
These key points are not intended as formal medical training, but as general information only. Continued research into these techniques is needed to assess long-term outcomes.
Short-term outcomes data only
Because this study focused on immediate complications, no long-term data on such complications as persistent pain, mesh erosion, or infection were collected.
All surgeons underwent hands-on training with the transvaginal repair system before patients were enrolled in the study. Nevertheless, the authors observe that many repair procedures were performed at the beginning of the physicians’ learning curve, with a higher number of complications than would be expected from more experienced surgeons.
The data may also have been affected by selection bias (ie, toward more complicated cases), given that most patients had already undergone prolapse repair.
Two systems yield excellent short-term results in women with recurrent prolapse
Gauruder-Burmester A, Koutouzidou P, Rohne J, Gronewold M, Tunn R. Follow-up after polypropylene mesh repair of anterior and posterior compartments in patients with recurrent prolapse. Int Urogynecol J Pelvic Floor Dysfunct. 2007;18:1059–1064.
This retrospective study involved women who had already undergone one or more prolapse repairs. These patients then underwent reoperation with mesh-reinforced repair. The authors hypothesized that recurrent prolapse represents poor tissue quality, necessitating the use of mesh in subsequent repairs. Both pre- and postoperative symptoms and functional changes were analyzed, with a special focus on mesh erosion and sexual function.
Details of the study
Of 145 women who underwent repair with the Apogee (apical posterior) or Perigee (anterior wall) system during a 1-year period, 120 were included in the analysis. The other 25 patients were excluded because they did not return for follow-up, were missing urodynamic data, or had inaccurate POP-Q staging. All patients had recurrent stage III posterior or anterior vaginal wall prolapse. Forty percent of patients had an apical posterior repair, and 60% had anterior wall repair. None had both procedures performed simultaneously.
All patients had undergone hysterectomy and received vaginal estrogen before and after surgery. Urinary incontinence was treated in a two-step fashion; that is, it was not addressed until 3 months after repair of the prolapse. Routine follow-up occurred at 1 month and 1 year after surgery.
One-year cure rate was 93%
No perioperative or intraoperative complications occurred, and mean operative time was 35±4.5 minutes. Mesh erosion occurred in four patients (3%) and involved anterior mesh placement only. No mesh infections were noted.
At 1 year, 93% of women were anatomically cured of prolapse (ie, they had less than stage II prolapse). Prolapse recurred in eight women; all cases involved the anterior compartment.
No dyspareunia was associated with the repair. In fact, prolapse-associated dyspareunia resolved in all 15 women who reported this symptom before surgery. In addition, questionnaires about quality of life and satisfaction revealed significant improvement after mesh placement (P=.023).
The authors attribute the positive results to the fact that both surgeons involved in the study used the technique on 15 patients before operating on study participants, minimizing the effect of the learning curve. The authors were also careful about patient selection.
Results merit cautious optimism
The authors propose that the low erosion rate and lack of new-onset dyspareunia after surgery may be misleading because long-term results have not yet been obtained. We also speculate that precise dissection in the proper surgical plane likely minimized early erosions.
The authors report no financial relationships relevant to this article.
The use of transvaginal mesh—with or without trocar placement—is surrounded by controversy. A number of minimally invasive vaginal mesh kits are commercially available for the repair of pelvic organ prolapse, and new kits are entering the market rapidly. The challenge is determining whether these new techniques are as effective and safe as traditional prolapse repairs.
Although the use of permanent mesh to repair prolapse has been explored in retrospective and prospective studies, no rigorous controlled trials have compared these new procedures with abdominal sacrocolpopexy or uterosacral ligament suspension, for example. The current body of literature does suggest a high rate of recurrent prolapse after traditional anterior or posterior colporrhaphy, and the use of allograft material has not been shown to improve outcomes. Surgeons are now turning their attention to permanent polypropylene mesh as a possible alternative. In addition, repair of the vaginal apex at the time of anterior and posterior vaginal wall repair is being explored as a way to increase durability of the repair. The new trocar-delivered mesh kits address this issue by suspending the vaginal vault while providing support to the vaginal walls.
This article highlights three recent studies that focus on a new trocar-delivered, protected, low-weight polypropylene mesh (Ugytex, distributed by Bard as Pelvitex) and three trocar-delivered mesh kits (Prolift, Apogee, and Perigee).
One-year outcomes encouraging for low-weight polypropylene mesh
De Tayrac R, Devoldere G, Renaudie J, Villard P, Guilbaud O, Eglin G. Prolapse repair by vaginal route using a new protected low-weight polypropylene mesh: 1-year functional and anatomical outcome in a prospective multicentre study. Int Urogynecol J Pelvic Floor Dysfunct. 2007;18:251–256.
This study evaluated functional and anatomic outcomes after placement for prolapse repair of low-weight polypropylene mesh protected by absorbable hydrophilic film. The film, a combination of atelocollagen, polyethylene glycol, and glycerol, is designed to protect pelvic organs from acute inflammation during healing. In a separate investigation of unprotected, heavyweight polypropylene mesh in prolapse repair, the anatomic success rate ranged from 75% to 100%, but the rate of mesh erosion (13%) and dyspareunia (69%) seemed unacceptably high.1
Rigorous preoperative assessment
In this trial, 230 women with symptomatic vaginal wall prolapse were recruited at 13 centers in a consecutive fashion. At enrollment, all patients were measured using the pelvic organ prolapse quantitative staging system (POP-Q). They also completed the validated Pelvic Floor Distress Inventory and Pelvic Floor Impact Questionnaire. The presence and severity of dyspareunia were also recorded, as well as the Urinary Dysfunction Measurement Scale. All participants had prolapse equal to or exceeding stage II.
Surgeons used trocars to percutaneously place a low-weight (38 g/m2) and highly porous polypropylene monofilament mesh (Ugytex/Pelvitex) for vaginal repair and performed any concomitant procedures. Perioperative and postoperative complications were recorded. Patients were evaluated at 6 weeks, 6 months, and 1 year. The first 143 patients with at least 10 months of follow-up were analyzed, with a mean follow-up of 13±2 months (range: 10–19). Anatomic cure was defined as no prolapse greater than or equal to stage II.
Patient satisfaction was high
The anatomic cure rate was 92.3%, with a 6.8% recurrence of anterior vaginal wall prolapse and 2.6% recurrence of posterior vaginal wall prolapse. Only one patient with recurrence was symptomatic.
Six of 143 patients (4.2%) sustained an intraoperative complication: three bladder injuries, one rectal injury, one uterine artery hemorrhage (during hysterectomy), and one vaginal sulcus perforation (during transobturator tape placement). The most significant postoperative complication related to the vaginal mesh kit was vaginal hematoma; one of the two cases required reoperation and partial removal of the mesh.
Nine patients developed mesh erosion in the first 3 months, for an erosion rate of 6.3%. Six required partial excision of the mesh. Overall, symptoms and quality of life improved significantly, with an overall satisfaction rate at follow-up of 96.5%. No significant difference was noted between pre- and postoperative rates of dyspareunia.
Further evaluation is warranted
The authors are already conducting a randomized trial to compare anterior vaginal wall repair using this low-weight polypropylene mesh with traditional anterior colporrhaphy to confirm and explore these results.
Note: Bard now offers a kit called Avaulta Plus that uses the same mesh material with a trocar delivery system, previously lacking (although investigators used trocars in this study).
Perioperative complications were uncommon with Prolift system
Altman D, Falconer C. Perioperative morbidity using transvaginal mesh in pelvic organ prolapse repair. Obstet Gynecol. 2007;109:303–308.
This study explored the frequency and characteristics of perioperative complications associated with the use of Prolift, a transvaginal mesh system for the repair of pelvic organ prolapse (FIGURE). Twenty-five centers participated by registering a standardized safety protocol form for 248 women who underwent surgery using the system over a 6-month period. The form included information about perioperative complications, adverse intraoperative events, and the associated hospital stay, as well as obstetric and gynecologic medical history and previous pelvic surgery.
Pelvic organ perforation (lower urinary tract or anorectal injury) and blood loss greater than 1,000 mL were recorded as major complications, and any other adverse events related to the hospital stay were documented as minor complications. Most of the cohort had already undergone prolapse repair, and prolapse had recurred in the same vaginal compartment.
One author was an educational adviser for Gynecare Sweden AB, and the other an adviser for Johnson & Johnson. Although the study was funded entirely by university-administered research funds, pretrial scientific meetings were paid for by Gynecare Sweden AB.
FIGURE: Mesh support of pelvic organs
Prolift mesh in final position, with extension arms passed through the sacrospinous ligaments and the obturator foramen bilaterally.
4.4% rate of serious complications
Serious complications occurred in 4.4% (11 of 248) of cases (95% confidence interval [CI], 2.5–7.8). The predominant complication was visceral injury, which included bladder, urethral, and rectal perforation. One patient had blood loss exceeding 1,000 mL.
Minor complications occurred in 44 patients (18%). The most common minor complication was urinary tract infection. Adverse events included urinary retention requiring catheterization, anemia, transfusion, fever, groin and buttock pain, and vaginal hematoma, among others.
Concurrent pelvic floor surgery increased the risk for minor complications (odds ratio, 2.8; 95% CI, 1.1–6.9). Concurrent procedures included vaginal hysterectomy, sling procedure with tension-free vaginal tape or transobturator tension-free tape, sacrospinal fixation, repair of vaginal enterocele, and bilateral salpingo-oophorectomy. This risk analysis identified no other predictors of outcome.
Posterior/apical repair
- Adequately infiltrate the vaginal epithelium with diluted epinephrine solution, especially toward the lateral apices, to facilitate hemostasis and dissection
- Be thorough in lateral dissection toward the ischial spine and stay in the proper surgical plane to create a thick vaginal epithelial flap
- Palpate the ischial spine, with the preoperatively packed rectum retracted medially
- During passage of the trocar, place an index finger along the vaginal dissection to palpate the trocar in the ischiorectal fossa and deep to the levator ani muscles until the tip is palpated at the level of the ischial spine
- Pass the trocar through the arcus tendineus/levator fascia at the level of the ischial spine, as shown below:
- Do not apply excess tension to the straps of the graft material
- Do not trim the vaginal epithelium
Anterior wall (obturator foramen trocar passage)
- Same key points as posterior wall technique, but in anterior repair, there are two passes through the obturator foramen
- The first trocar is inserted into the inferior obturator foramen, rotated, and guided with the surgeon’s finger inserted into and held in the vaginal dissection, as shown below:
- The superior passage exits close to the bladder neck, and the inferior passage approximates the ischial spine. Penetrate along the arcus tendineus approximately 1 cm from the ischial spine
Caution! Keep summary points in context
These key points are not intended as formal medical training, but as general information only. Continued research into these techniques is needed to assess long-term outcomes.
Short-term outcomes data only
Because this study focused on immediate complications, no long-term data on such complications as persistent pain, mesh erosion, or infection were collected.
All surgeons underwent hands-on training with the transvaginal repair system before patients were enrolled in the study. Nevertheless, the authors observe that many repair procedures were performed at the beginning of the physicians’ learning curve, with a higher number of complications than would be expected from more experienced surgeons.
The data may also have been affected by selection bias (ie, toward more complicated cases), given that most patients had already undergone prolapse repair.
Two systems yield excellent short-term results in women with recurrent prolapse
Gauruder-Burmester A, Koutouzidou P, Rohne J, Gronewold M, Tunn R. Follow-up after polypropylene mesh repair of anterior and posterior compartments in patients with recurrent prolapse. Int Urogynecol J Pelvic Floor Dysfunct. 2007;18:1059–1064.
This retrospective study involved women who had already undergone one or more prolapse repairs. These patients then underwent reoperation with mesh-reinforced repair. The authors hypothesized that recurrent prolapse represents poor tissue quality, necessitating the use of mesh in subsequent repairs. Both pre- and postoperative symptoms and functional changes were analyzed, with a special focus on mesh erosion and sexual function.
Details of the study
Of 145 women who underwent repair with the Apogee (apical posterior) or Perigee (anterior wall) system during a 1-year period, 120 were included in the analysis. The other 25 patients were excluded because they did not return for follow-up, were missing urodynamic data, or had inaccurate POP-Q staging. All patients had recurrent stage III posterior or anterior vaginal wall prolapse. Forty percent of patients had an apical posterior repair, and 60% had anterior wall repair. None had both procedures performed simultaneously.
All patients had undergone hysterectomy and received vaginal estrogen before and after surgery. Urinary incontinence was treated in a two-step fashion; that is, it was not addressed until 3 months after repair of the prolapse. Routine follow-up occurred at 1 month and 1 year after surgery.
One-year cure rate was 93%
No perioperative or intraoperative complications occurred, and mean operative time was 35±4.5 minutes. Mesh erosion occurred in four patients (3%) and involved anterior mesh placement only. No mesh infections were noted.
At 1 year, 93% of women were anatomically cured of prolapse (ie, they had less than stage II prolapse). Prolapse recurred in eight women; all cases involved the anterior compartment.
No dyspareunia was associated with the repair. In fact, prolapse-associated dyspareunia resolved in all 15 women who reported this symptom before surgery. In addition, questionnaires about quality of life and satisfaction revealed significant improvement after mesh placement (P=.023).
The authors attribute the positive results to the fact that both surgeons involved in the study used the technique on 15 patients before operating on study participants, minimizing the effect of the learning curve. The authors were also careful about patient selection.
Results merit cautious optimism
The authors propose that the low erosion rate and lack of new-onset dyspareunia after surgery may be misleading because long-term results have not yet been obtained. We also speculate that precise dissection in the proper surgical plane likely minimized early erosions.
Reference
1. Milani R, Salvatore S, Soligo M, Pifarotti P, Meschia M, Cortese M. Functional and anatomical outcome of anterior and posterior vaginal prolapse repair with prolene mesh. Br J Obstet Gynaecol. 2004;111:1-5.
Reference
1. Milani R, Salvatore S, Soligo M, Pifarotti P, Meschia M, Cortese M. Functional and anatomical outcome of anterior and posterior vaginal prolapse repair with prolene mesh. Br J Obstet Gynaecol. 2004;111:1-5.