User login
“Patchy” pneumonia
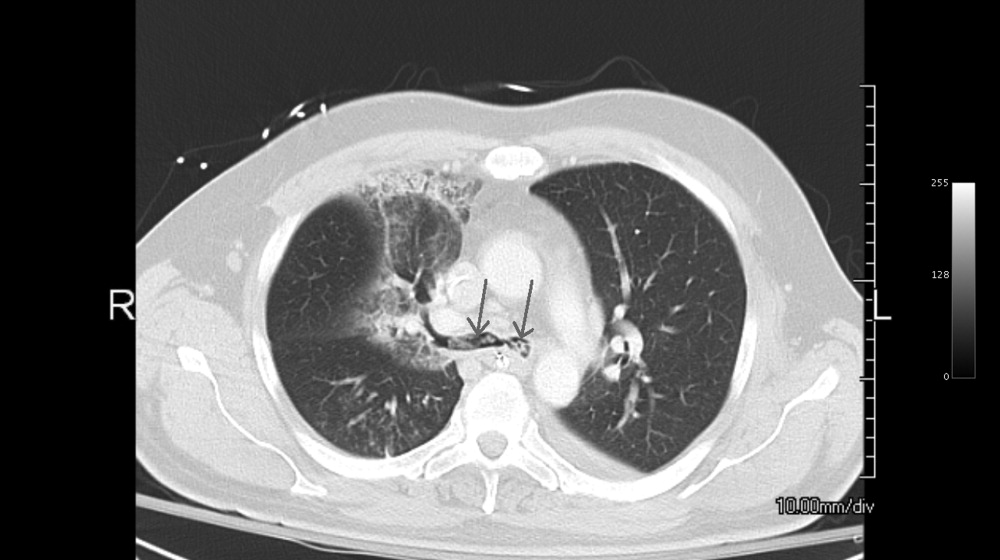
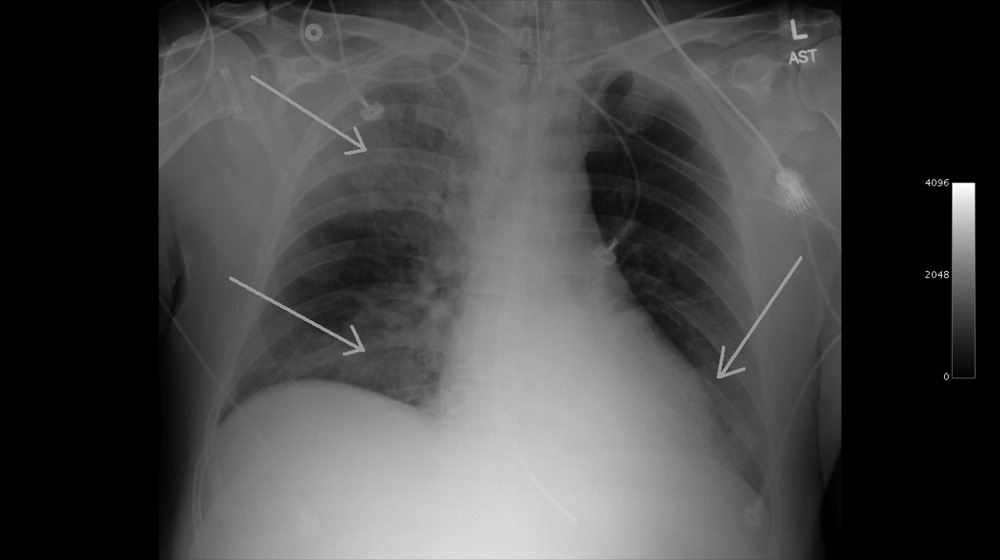
A 49‐year‐old retired air‐force officer presented with productive cough lasting 1 week. He was in good health except for back pain after a motor vehicle accident, 2 years ago, for which he took unspecified pain medications. His condition rapidly deteriorated necessitating mechanical ventilation. Chest x‐ray showed multilobar pneumonia (Figure 1). Blood and sputum cultures grew Serratia marcescens. Chest computed tomography (CT)‐scan showed multilobar involvement with debris in his airways that was thought to be respiratory secretions (Figure 2, arrows). He remained intubated for 2 weeks before his clinical status improved enough to permit extubation. Immediately following extubation, he coughed up a ball of crumpled, plastic material. His condition subsequently improved dramatically with complete radiological resolution of his pneumonia. On analyzing the foreign body, it turned out to be a fenestrated fentanyl patch (Figure 3). The patient then reported that he often cut‐up used fentanyl patches and sucked on them for an extra high. In retrospect, the endobronchial debris was actually the patch straddling the carina and had prevented rapid recovery. Aspiration of unusual foreign bodies have been reported in the literature. This foreign body masqueraded as respiratory secretions on imaging preventing early detection. This clinical encounter brings to light yet another innovative, but potentially deadly, form of drug abuse. It also emphasizes the importance of early bronchoscopy in nonresolving pneumonias.

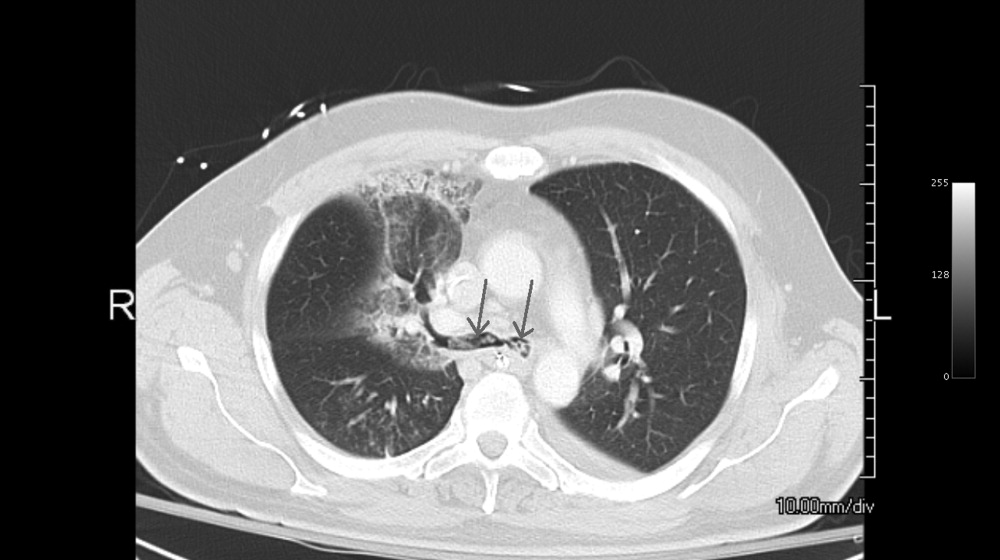
A 49‐year‐old retired air‐force officer presented with productive cough lasting 1 week. He was in good health except for back pain after a motor vehicle accident, 2 years ago, for which he took unspecified pain medications. His condition rapidly deteriorated necessitating mechanical ventilation. Chest x‐ray showed multilobar pneumonia (Figure 1). Blood and sputum cultures grew Serratia marcescens. Chest computed tomography (CT)‐scan showed multilobar involvement with debris in his airways that was thought to be respiratory secretions (Figure 2, arrows). He remained intubated for 2 weeks before his clinical status improved enough to permit extubation. Immediately following extubation, he coughed up a ball of crumpled, plastic material. His condition subsequently improved dramatically with complete radiological resolution of his pneumonia. On analyzing the foreign body, it turned out to be a fenestrated fentanyl patch (Figure 3). The patient then reported that he often cut‐up used fentanyl patches and sucked on them for an extra high. In retrospect, the endobronchial debris was actually the patch straddling the carina and had prevented rapid recovery. Aspiration of unusual foreign bodies have been reported in the literature. This foreign body masqueraded as respiratory secretions on imaging preventing early detection. This clinical encounter brings to light yet another innovative, but potentially deadly, form of drug abuse. It also emphasizes the importance of early bronchoscopy in nonresolving pneumonias.

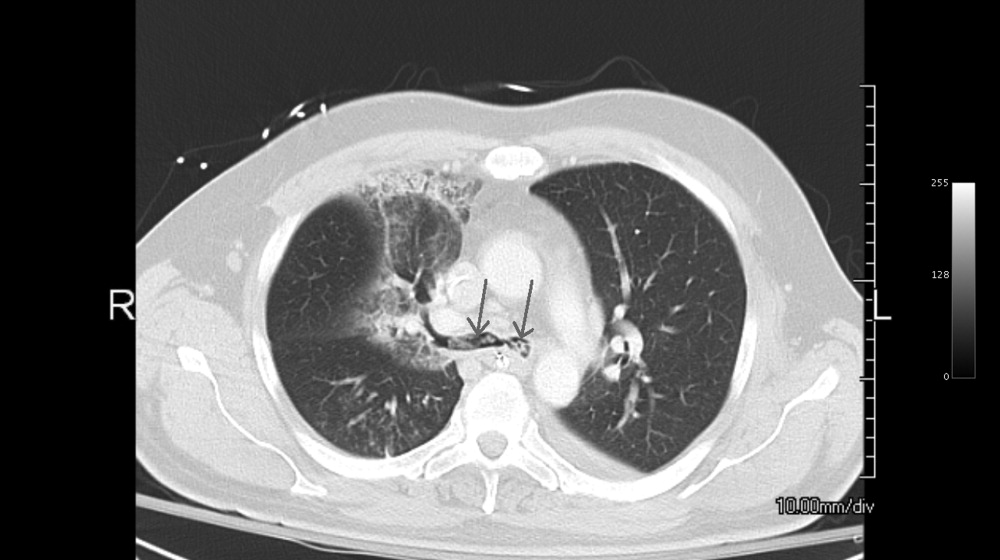
A 49‐year‐old retired air‐force officer presented with productive cough lasting 1 week. He was in good health except for back pain after a motor vehicle accident, 2 years ago, for which he took unspecified pain medications. His condition rapidly deteriorated necessitating mechanical ventilation. Chest x‐ray showed multilobar pneumonia (Figure 1). Blood and sputum cultures grew Serratia marcescens. Chest computed tomography (CT)‐scan showed multilobar involvement with debris in his airways that was thought to be respiratory secretions (Figure 2, arrows). He remained intubated for 2 weeks before his clinical status improved enough to permit extubation. Immediately following extubation, he coughed up a ball of crumpled, plastic material. His condition subsequently improved dramatically with complete radiological resolution of his pneumonia. On analyzing the foreign body, it turned out to be a fenestrated fentanyl patch (Figure 3). The patient then reported that he often cut‐up used fentanyl patches and sucked on them for an extra high. In retrospect, the endobronchial debris was actually the patch straddling the carina and had prevented rapid recovery. Aspiration of unusual foreign bodies have been reported in the literature. This foreign body masqueraded as respiratory secretions on imaging preventing early detection. This clinical encounter brings to light yet another innovative, but potentially deadly, form of drug abuse. It also emphasizes the importance of early bronchoscopy in nonresolving pneumonias.