User login
Stressors associated with drug misuse
How to prevent misuse of psychotropics among college students
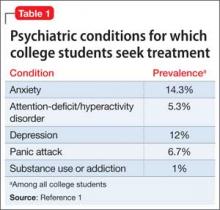
Many college students suffer from mental illness (Table 1),1 which can have a negative impact on academic performance. Although psychotropic medications are an important part of treatment for many college students, the potential for misuse always is present. Drug misuse occurs when patients use medications for reasons inconsistent with legal or medical guidelines.2 For example, patients may take a medication that has not been prescribed for them or in a manner that is inconsistent with the prescriber’s instructions, including administration with other substances.3
Misuse of psychotropic drugs is prevalent among college students. A study of 14,175 students from 26 campuses reported that 14.7% of students taking a psychotropic are doing so without a prescription, including stimulants (52.6%), anxiolytics (38.4%), and antidepressants (17.4%).4 Another study states that more than one-third of responders reported misuse of >1 class of medication.5
Psychotropic misuse is concerning because it increases the risk of adverse events. Nearly one-half of medication errors are associated with writing and dispensing the prescription, which means that prescribers can work to reduce these errors.6 However, nonadherence, prescription misuse, and failure to disclose use of over-the-counter drugs, illicit drugs, and herbal products makes preventing most adverse events difficult, if not impossible, for prescribers.7,8
Psychotropic drug misuse among college students is highly variable and unpredictable. Students misuse medications, including stimulants, benzodiazepines, and antidepressants, for a variety of reasons, such as study enhancement, experimentation, intoxication, self-medication, relaxation, and stress management.8 One survey reported that >70% of students taking a psychotropic medication took it with alcohol or another illicit drug.9
However, <20% of those using a psychotropic medication with alcohol or other illicit drugs told their health care provider(s),9 making it impossible for clinicians to predict a patient’s risk of drug− drug interactions and subsequent adverse events. Additionally, additive effects could occur10 and changes in a patient’s presentation could be caused by a reaction to a combination of medications, rather than a new symptom of mental illness.
This article will examine common issues associated with drug misuse among college-age students and review prevention strategies (Table 2).
Stimulants
Stimulants have the highest rate of diversion; 61.7% of college students prescribed stimulants have shared or sold their medication.11 A survey of 115 students from 2 universities reported that the most common reason for stimulant misuse was to enhance academic performance.12 The same survey showed that some students take stimulants with Cannabis (17%) and alcohol (30%).12 As a result, in addition to lowering grade point average (GPA) and other academic difficulties,13 students misusing stimulants are at risk of drug interactions.14
It is critical to ascertain the route of drug administration, because non-oral routes, including crushing then snorting or injecting, are associated with additional health concerns, such as accidental death or blood-borne illnesses.15,16 Cardiac adverse effects of stimulants include hypertension, vasospasm, tachycardia, and dysrhythmia; psychiatric and other effects include serotonin syndrome, hallucinations, anxiety, paranoia, seizures, tics, hyperthermia, and tremor.17 Health care providers prescribing or caring for people taking a stimulant should monitor for these potential effects.
The risk of switch to mania might not be apparent to those who prescribe stimulants or to young people who take non-prescribed stimulants for academic enhancement or to achieve medication-induced euphoria. Adolescent stimulant use is associated with symptoms of early-onset bipolar disorder in patients who have attention-deficit/ hyperactivity disorder (ADHD) and undiagnosed bipolarity.18
The cardiovascular risk associated with stimulant use is debatable. Although several studies have been conducted,19-21 methodological factors limit their applicability. To minimize potential risks, several precautions should be taken before prescribing a stimulant to treat ADHD.
First, obtain a detailed personal and family medical history, asking about possible cardiovascular disease. Second, carefully scrutinize the patient’s cardiovascular system during the physical exam. Third, consider additional testing, such as an electrocardiogram, if the patient’s history or physical exam indicates possible risk.22
As a prescriber, you should be aware of the prevalence of stimulant use among students with and without ADHD, including those who could be feigning ADHD symptoms.15 Diversion could occur through sharing medications or selling them to friends and family.11 It also is possible that these medications may be used with other illicit substances, such as Cannabis, ecstasy, cocaine, and opiates.23 Students also could misuse stimulants by taking more than the prescribed dosage.24
Risk factors for misuse of stimulants include: heavy alcohol use, previous illicit drug use, white race, fraternity or sorority membership, low GPA, increased hyperactivity symptoms, and attendance at a competitive college or university.25-27
Benzodiazepines
Misuse of benzodiazepine is a significant component of prescription drug abuse and often occurs with other medications and alcohol.28 Additional methods of misuse include increased dosage and non-oral routes of administration.29
A 2001 national survey reported that 7.8% of college students have misused benzodiazepines.23 Common characteristics of benzodiazepine abusers include young age, male sex, personality characteristics of impulsivity and hopelessness, and abuse of other drugs, including cocaine and methadone.28,29
Benzodiazepines are prescribed for their anxiolytic and hypnotic properties and students could use these drugs with other agents to augment the euphoric effects or diminish withdrawal symptoms.30 Patients taking benzodiazepines for anxiety might self-medicate with alcohol, which increases sedation and depression, and can contribute to the risk for respiratory depression.10 Misuse of benzodiazepines can result in cognitive and psychomotor impairment and increase the risk of accidents and overdose.29,31
Although overdose with monotherapy is rare, the risk increases when a benzodiazepine is used with alcohol10 or another respiratory depressants, such as opioids, because combination use can produce additive effects.28 You should therefore avoid prescribing benzodiazepines to patients who have a history of significant substance abuse and consider using alternative, non-addictive agents, such as selective serotonin reuptake inhibitors, or non-pharmaceutical treatment when such patients present with an anxiety disorder. The risk of adverse effects of benzodiazepines can be reduced by limiting the dosing and the duration of the treatment, and by using longer-acting rather than the more addictive, shorter-acting, agents.
Antidepressants
Health care providers should be aware that, despite the relative absence of physically addictive properties, antidepressants from most classes are abusable agents sought by young people for non-medical use. In particular, the literature highlights monoamine oxidase inhibitors (MAOIs), tricyclic antidepressants, serotonin-norepinephrine reuptake inhibitors, and bupropion as the antidepressants most likely to be misused for their amphetamine-like euphoric effects or serotonin-induced dissociative effects.32 However, compared with other drug classes discussed in this article, the rate of antidepressant misuse is relatively low among college students.
Regardless of the antidepressant selected, clinicians should be concerned about alcohol use among college-age patients. Persons with depression are at increased risk of alcoholism compared with the general population.33 This combination can increase depressive symptoms and sedation, and decrease coordination, judgment, and reaction time.33
Excessive alcohol use can increase the risk of seizures in patients taking antidepressants such as buproprion.34 Employ caution when prescribing bupropion to patients who have a predisposing clinical factor that increases seizure risk, such as excessive alcohol use and abrupt cessation, use of other medications that may lower seizure threshold (eg, theophylline, amphetamines, phenothiazines), and a history of head trauma.34
To minimize the risk of seizures with bupropion, titrate up the dosage slowly. Furthermore, using a low dosage during dual therapy for antidepressant augmentation further decreases the risk of seizure.35 For these reasons, we recommend that you avoid bupropion in patients who are at risk of binge drinking, and give careful consideration to providing alternative therapies for them.
Prescribers and patients should also keep in mind that hypertensive crisis could occur if MAOIs are combined with certain types of alcoholic beverages containing tyramine, including some wines and draft beer.33
How you can identify and prevent misuse
Careful communication between health care provider and patient that is necessary to minimize the risk of adverse drug events with psychotropic medications often is lacking. For example, 24% of study college-age participants did not remember if their physician provided a diagnosis and 28.8% could not recall being informed about side effects and, perhaps as a result, many students did not take their medications as prescribed.9
Further, prescribers should ask college-age patients who are undergoing stimulant treatment if they believe that they are being adequately treated. They should inquire about how they are taking their medications.11 These questions can lead to discussion of the need for these medications and reevaluation of their perceived indication.11
Remind patients to take their medication only as directed.36 Highlight the need to:
• store medications in a discreet location
• properly dispose of unused medications
• keep tabs on the quantity of pills
• know how to resist requests for diversion from peers.
The Substance Abuse and Mental Health Services Administration offers additional useful strategies,37 and pharmacists also can be partners in substance use education and prevention.38 These are examples of how health care providers can take an active role in providing patients with a thorough and detailed understanding of (1) their conditions and (2) their prescribed medications to improve efficacy and safety while preventing misuse.8
A study found that the most common method of obtaining these medications without a prescription is acquiring them from peers; 54% of undergraduate patients with stimulant prescriptions have been approached by peers to give, trade, or sell their drugs.25 Other methods include purchasing medications online or faking prescriptions.39 Health care providers should remind patients of the legal ramifications of sharing or selling their prescribed medications. Finally, providers must be vigilant for students who may feign symptoms to obtain a prescription:
• be wary if symptom presentation sounds too “textbook”
• seek collateral history from family. Adults with ADHD should have shown symptoms during childhood
• use external verification such as neuropsychological testing for ADHD. A neuropsychologist can detect deception by analyzing the pattern of responses to questions.
Patient assessment is a key step to in preventing abuse of psychotropic medications. Gentle inquiry about school-related stress and other risk factors for misuse can help practitioners determine if students are at risk of diversion and if additional screening is necessary.
In response to these issues, Stone and Merlo8 have suggested that, in addition to the educational programs held on college campuses on alcohol, illicit drugs, and prescription painkillers, patients should be better informed on the appropriate use of prescription psychiatric medications, instructed to avoid sharing with family and friends, and assessed for abuse risk at regular intervals.
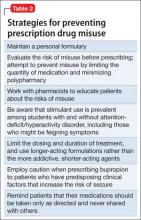
To further protect patients from adverse outcomes during treatment, you can employ conservative and safe prescribing techniques. One strategy might be to keep a personal formulary that lists key medications you use in everyday practice, including knowledge about each drug’s dosage, potential adverse effects, key warnings, and drug−drug interactions.40
Furthermore, maintain healthy caution about newly approved medications and carefully consider how they measure up to existing agents—in other words, practice evidence-based medicine, particularly when students request a particular agent.40,41 Prescribers should evaluate the risk of abuse before prescribing and attempt to prevent misuse by limiting quantities and minimizing polypharmacy.
Last, pharmacists can be key allies for consultation and appropriate medication selection.
Bottom Line
Psychotropic medications are necessary to treat the variety of conditions—anxiety, attention-deficit/hyperactivity disorder, depression, and panic disorder—common among college students. However, students are at risk of combining their prescribed medications with other medications, drugs, and alcohol or could sell or share their medication with peers. Proper counseling and identification of risk factors can be important tools for preventing such events.
Related Resources
• American College Health Association-National College Health Assessment. www.acha-ncha.org.
• Schwartz VI. College mental health: How to provide care for students in need. Current Psychiatry. 2011;10(12):22-29.
Drug Brand Names
Bupropion • Wellbutrin, Zyban
Methadone • Methadose, Dolophine
Theophylline • Theo-24, Theolair, Uniphyl
Disclosures
The authors report no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
1. American College Health Association. American College Health Association-National College Health Assessment II: Reference Group Executive Summary Spring 2014. http://www.acha-ncha.org/docs/ACHA-NCHA-II_ReferenceGroup_ExecutiveSummary_ Spring2014.pdf. Published 2014. Accessed January 13, 2015.
2. World Health Organization. Management of substance abuse. http://www.who.int/substance_abuse/terminology/ abuse/en. Accessed June 4, 2015.
3. U.S. Food and Drug Administration. Combating misuse and abuse of prescription drugs: Q&A with Michael Klein, PhD. http://www.fda.gov/ForConsumers/ConsumerUpdates/ ucm220112.htm. Published July 28, 2010. Accessed June 18, 2014.
4. Eisenberg D, Hunt J, Speer N, et al. Mental health service utilization among college students in the United States. J Nerv Ment Dis. 2011;199(5):301-308.
5. Peralta RL, Steele JL. Nonmedical prescription drug use among US college students at a Midwest university: a partial test of social learning theory. Subst Use Misuse. 2010;45(6):865-887.
6. Agency for Healthcare Research and Quality. Reducing and preventing adverse drug events to decrease hospital costs: Research in action. http://www.ahrq.gov/research/ findings/factsheets/errors-safety/aderia/index.html. Updated March 2001. Accessed June 21, 2014.
7. Procyshyn RM, Barr AM, Brickell T, et al. Medication errors in psychiatry: a comprehensive review. CNS Drugs. 2010;24(7):595-609.
8. Stone AM, Merlo LJ. Attitudes of college students toward mental illness stigma and the misuse of psychiatric medications. J Clin Psychiatry. 2011;72(2):134-139.
9. Oberleitner LM, Tzilos GK, Zumberg KM, et al. Psychotropic drug use among college students: patterns of use, misuse, and medical monitoring. J Am Coll Health. 2011;59(7):658-661.
10. Linnoila MI. Benzodiazepines and alcohol. J Psychiatr Res. 1990;24(suppl 2):121-127.
11. Garnier LM, Arria AM, Caldeira KM, et al. Sharing and selling of prescription medications in a college student sample. J Clin Psychiatry. 2010;71(3):262-269.
12. Rabiner DL, Anastopoulos AD, Costello EJ, et al. The misuse and diversion of prescribed ADHD medications by college students. J Atten Disord. 2009;13(2):144-153.
13. Arria AM. Nonmedical use of prescription stimulants and analgesics: associations with social and academic behaviors among college students. J Drug Issues. 2008; 38(4):1045-1060.
14. Arria AM, Caldeira KM, O’Grady KE, et al. Nonmedical use of prescription stimulants among college students: associations with attention-deficit-hyperactivity disorder and polydrug use. Pharmacotherapy. 2008;28(2):156-169.
15. Rabiner DL. Stimulant prescription cautions: addressing misuse, diversion and malingering. Curr Psychiatry Rep. 2013;15(7):375.
16. Sepúlveda DR, Thomas LM, McCabe SE, et al. Misuse of prescribed stimulant medication for ADHD and associated patterns of substance use: preliminary analysis among college students. J Pharm Pract. 2011;24(6):551-560.
17. Greydanus DE. Stimulant misuse: strategies to manage a growing problem. http://www.acha.org/Continuing_ Education/docs/ACHA_Use_Misuse_of_Stimulants_ Article2.pdf. Accessed June 29, 2015.
18. Vergne D, Whitham E, Barroilhet S, et al. Adult ADHD and amphetamines: a new paradigm. Neuropsychiatry. 2011;1(6):591-598.
19. Habel LA, Cooper WO, Sox CM, et al. ADHD medications and risk of serious cardiovascular events in young and middle-aged adults. JAMA. 2011;306(24):2673-2683.
20. Cooper WO, Habel LA, Sox CM, et al. ADHD drugs and serious cardiovascular events in children and young adults. N Engl J Med. 2011;365(20):1896-1904.
21. Schelleman H, Bilker WB, Kimmel SE, et al. Methylphenidate and risk of serious cardiovascular events in adults. Am J Psychiatry. 2012;169(2):178-185.
22. U.S. Food and Drug Administration. Communication about an ongoing safety review of stimulant medications used in children with attention-deficit/hyperactivity disorder (ADHD). http://www.fda.gov/Drugs/Drug Safety/PostmarketDrugSafetyInformationforPatients andProviders/DrugSafetyInformationforHeathcare Professionals/ucm165858.htm. Updated August 15, 2013. Accessed June 25, 2014.
23. McCabe SE, Knight JR, Teter CJ, et al. Non-medical use of prescription stimulants among US college students: prevalence and correlates from a national survey. Addiction. 2005;100(1):96-106.
24. McNiel AD, Muzzin KB, DeWald JP, et al. The nonmedical use of prescription stimulants among dental and dental hygiene students. J Dent Educ. 2011;75(3):365-376.
25. McCabe SE, Teter CJ, Boyd CJ. Medical use, illicit use and diversion of prescription stimulant medication. J Psychoactive Drugs. 2006;38(1):43-56.
26. Arria AM, Garnier-Dykstra LM, Caldeira KM, et al. Persistent nonmedical use of prescription stimulants among college students: possible association with ADHD symptoms. J Atten Disord. 2011;15(5):347-356.
27. Teter CJ, McCabe SE, Boyd CJ, et al. Illicit methylphenidate use in an undergraduate student sample: prevalence and risk factors. Pharmacotherapy. 2003;23(5):609-617.
28. Hernandez SH, Nelson LS. Prescription drug abuse: insight into the epidemic. Clin Pharmacol Ther. 2010; 88(3):307-317.
29. McLarnon ME, Monaghan TL, Stewart SH, et al. Drug misuse and diversion in adults prescribed anxiolytics and sedatives. Pharmacotherapy. 2011;31(3):262-272.
30. Woods JH, Katz JL, Winger G. Benzodiazepines: use, abuse, and consequences. Pharmacol Rev. 1992;44(2):151-347.
31. Buffett-Jerrott SE, Stewart SH. Cognitive and sedative effects of benzodiazepine use. Curr Pharm Des. 2002;8(1):45-58.
32. Evans EA, Sullivan MA. Abuse and misuse of antidepressants. Subst Abuse Rehabil. 2014;5:107-120.
33. Hall-Flavin DK. Why is it bad to mix antidepressants and alcohol? http://www.mayoclinic.com/health/antidepressants-and-alcohol/AN01653. Updated June 12, 2014. Accessed June 20, 2014.
34. Wellbutrin [package insert]. Research Triangle Park, NC: GlaxoSmithKline LLC; 2014.
35. Davidson J. Seizures and bupropion: a review. J Clin Psychiatry. 1989;50(7):256-261.
36. Maddox JC, Levi M, Thompson C. The compliance with antidepressants in general practice. J Psychopharmacol. 1994;8(1):48-52.
37. Substance Abuse and Mental Health Services Administration. You’re in control: using prescription medication responsibly. http://store.samhsa.gov/shin/content/SMA12-4678B3/SMA12-4678B3.pdf. Accessed June 5, 2015.
38. ASHP statement on the pharmacist’s role in substance abuse prevention, education, and assistance. Am J Health Syst Pharm. 2014;71(3):243-246.
39. Inciardi JA, Surratt HL, Cicero TJ, et al. Prescription drugs purchased through the internet: who are the end users? Drug Alcohol Depend. 2010;110(1-2):21-29.
40. Preskorn SH, Flockhart D. 2006 Guide to psychiatric drug interactions. Primary Psychiatry. 2006;13(4):35-64.
41. Schiff GD, Galanter WL, Duhig J, et al. Principles of conservative prescribing. Arch Intern Med. 2011;171(16): 1433-1440.
Many college students suffer from mental illness (Table 1),1 which can have a negative impact on academic performance. Although psychotropic medications are an important part of treatment for many college students, the potential for misuse always is present. Drug misuse occurs when patients use medications for reasons inconsistent with legal or medical guidelines.2 For example, patients may take a medication that has not been prescribed for them or in a manner that is inconsistent with the prescriber’s instructions, including administration with other substances.3
Misuse of psychotropic drugs is prevalent among college students. A study of 14,175 students from 26 campuses reported that 14.7% of students taking a psychotropic are doing so without a prescription, including stimulants (52.6%), anxiolytics (38.4%), and antidepressants (17.4%).4 Another study states that more than one-third of responders reported misuse of >1 class of medication.5
Psychotropic misuse is concerning because it increases the risk of adverse events. Nearly one-half of medication errors are associated with writing and dispensing the prescription, which means that prescribers can work to reduce these errors.6 However, nonadherence, prescription misuse, and failure to disclose use of over-the-counter drugs, illicit drugs, and herbal products makes preventing most adverse events difficult, if not impossible, for prescribers.7,8
Psychotropic drug misuse among college students is highly variable and unpredictable. Students misuse medications, including stimulants, benzodiazepines, and antidepressants, for a variety of reasons, such as study enhancement, experimentation, intoxication, self-medication, relaxation, and stress management.8 One survey reported that >70% of students taking a psychotropic medication took it with alcohol or another illicit drug.9
However, <20% of those using a psychotropic medication with alcohol or other illicit drugs told their health care provider(s),9 making it impossible for clinicians to predict a patient’s risk of drug− drug interactions and subsequent adverse events. Additionally, additive effects could occur10 and changes in a patient’s presentation could be caused by a reaction to a combination of medications, rather than a new symptom of mental illness.
This article will examine common issues associated with drug misuse among college-age students and review prevention strategies (Table 2).
Stimulants
Stimulants have the highest rate of diversion; 61.7% of college students prescribed stimulants have shared or sold their medication.11 A survey of 115 students from 2 universities reported that the most common reason for stimulant misuse was to enhance academic performance.12 The same survey showed that some students take stimulants with Cannabis (17%) and alcohol (30%).12 As a result, in addition to lowering grade point average (GPA) and other academic difficulties,13 students misusing stimulants are at risk of drug interactions.14
It is critical to ascertain the route of drug administration, because non-oral routes, including crushing then snorting or injecting, are associated with additional health concerns, such as accidental death or blood-borne illnesses.15,16 Cardiac adverse effects of stimulants include hypertension, vasospasm, tachycardia, and dysrhythmia; psychiatric and other effects include serotonin syndrome, hallucinations, anxiety, paranoia, seizures, tics, hyperthermia, and tremor.17 Health care providers prescribing or caring for people taking a stimulant should monitor for these potential effects.
The risk of switch to mania might not be apparent to those who prescribe stimulants or to young people who take non-prescribed stimulants for academic enhancement or to achieve medication-induced euphoria. Adolescent stimulant use is associated with symptoms of early-onset bipolar disorder in patients who have attention-deficit/ hyperactivity disorder (ADHD) and undiagnosed bipolarity.18
The cardiovascular risk associated with stimulant use is debatable. Although several studies have been conducted,19-21 methodological factors limit their applicability. To minimize potential risks, several precautions should be taken before prescribing a stimulant to treat ADHD.
First, obtain a detailed personal and family medical history, asking about possible cardiovascular disease. Second, carefully scrutinize the patient’s cardiovascular system during the physical exam. Third, consider additional testing, such as an electrocardiogram, if the patient’s history or physical exam indicates possible risk.22
As a prescriber, you should be aware of the prevalence of stimulant use among students with and without ADHD, including those who could be feigning ADHD symptoms.15 Diversion could occur through sharing medications or selling them to friends and family.11 It also is possible that these medications may be used with other illicit substances, such as Cannabis, ecstasy, cocaine, and opiates.23 Students also could misuse stimulants by taking more than the prescribed dosage.24
Risk factors for misuse of stimulants include: heavy alcohol use, previous illicit drug use, white race, fraternity or sorority membership, low GPA, increased hyperactivity symptoms, and attendance at a competitive college or university.25-27
Benzodiazepines
Misuse of benzodiazepine is a significant component of prescription drug abuse and often occurs with other medications and alcohol.28 Additional methods of misuse include increased dosage and non-oral routes of administration.29
A 2001 national survey reported that 7.8% of college students have misused benzodiazepines.23 Common characteristics of benzodiazepine abusers include young age, male sex, personality characteristics of impulsivity and hopelessness, and abuse of other drugs, including cocaine and methadone.28,29
Benzodiazepines are prescribed for their anxiolytic and hypnotic properties and students could use these drugs with other agents to augment the euphoric effects or diminish withdrawal symptoms.30 Patients taking benzodiazepines for anxiety might self-medicate with alcohol, which increases sedation and depression, and can contribute to the risk for respiratory depression.10 Misuse of benzodiazepines can result in cognitive and psychomotor impairment and increase the risk of accidents and overdose.29,31
Although overdose with monotherapy is rare, the risk increases when a benzodiazepine is used with alcohol10 or another respiratory depressants, such as opioids, because combination use can produce additive effects.28 You should therefore avoid prescribing benzodiazepines to patients who have a history of significant substance abuse and consider using alternative, non-addictive agents, such as selective serotonin reuptake inhibitors, or non-pharmaceutical treatment when such patients present with an anxiety disorder. The risk of adverse effects of benzodiazepines can be reduced by limiting the dosing and the duration of the treatment, and by using longer-acting rather than the more addictive, shorter-acting, agents.
Antidepressants
Health care providers should be aware that, despite the relative absence of physically addictive properties, antidepressants from most classes are abusable agents sought by young people for non-medical use. In particular, the literature highlights monoamine oxidase inhibitors (MAOIs), tricyclic antidepressants, serotonin-norepinephrine reuptake inhibitors, and bupropion as the antidepressants most likely to be misused for their amphetamine-like euphoric effects or serotonin-induced dissociative effects.32 However, compared with other drug classes discussed in this article, the rate of antidepressant misuse is relatively low among college students.
Regardless of the antidepressant selected, clinicians should be concerned about alcohol use among college-age patients. Persons with depression are at increased risk of alcoholism compared with the general population.33 This combination can increase depressive symptoms and sedation, and decrease coordination, judgment, and reaction time.33
Excessive alcohol use can increase the risk of seizures in patients taking antidepressants such as buproprion.34 Employ caution when prescribing bupropion to patients who have a predisposing clinical factor that increases seizure risk, such as excessive alcohol use and abrupt cessation, use of other medications that may lower seizure threshold (eg, theophylline, amphetamines, phenothiazines), and a history of head trauma.34
To minimize the risk of seizures with bupropion, titrate up the dosage slowly. Furthermore, using a low dosage during dual therapy for antidepressant augmentation further decreases the risk of seizure.35 For these reasons, we recommend that you avoid bupropion in patients who are at risk of binge drinking, and give careful consideration to providing alternative therapies for them.
Prescribers and patients should also keep in mind that hypertensive crisis could occur if MAOIs are combined with certain types of alcoholic beverages containing tyramine, including some wines and draft beer.33
How you can identify and prevent misuse
Careful communication between health care provider and patient that is necessary to minimize the risk of adverse drug events with psychotropic medications often is lacking. For example, 24% of study college-age participants did not remember if their physician provided a diagnosis and 28.8% could not recall being informed about side effects and, perhaps as a result, many students did not take their medications as prescribed.9
Further, prescribers should ask college-age patients who are undergoing stimulant treatment if they believe that they are being adequately treated. They should inquire about how they are taking their medications.11 These questions can lead to discussion of the need for these medications and reevaluation of their perceived indication.11
Remind patients to take their medication only as directed.36 Highlight the need to:
• store medications in a discreet location
• properly dispose of unused medications
• keep tabs on the quantity of pills
• know how to resist requests for diversion from peers.
The Substance Abuse and Mental Health Services Administration offers additional useful strategies,37 and pharmacists also can be partners in substance use education and prevention.38 These are examples of how health care providers can take an active role in providing patients with a thorough and detailed understanding of (1) their conditions and (2) their prescribed medications to improve efficacy and safety while preventing misuse.8
A study found that the most common method of obtaining these medications without a prescription is acquiring them from peers; 54% of undergraduate patients with stimulant prescriptions have been approached by peers to give, trade, or sell their drugs.25 Other methods include purchasing medications online or faking prescriptions.39 Health care providers should remind patients of the legal ramifications of sharing or selling their prescribed medications. Finally, providers must be vigilant for students who may feign symptoms to obtain a prescription:
• be wary if symptom presentation sounds too “textbook”
• seek collateral history from family. Adults with ADHD should have shown symptoms during childhood
• use external verification such as neuropsychological testing for ADHD. A neuropsychologist can detect deception by analyzing the pattern of responses to questions.
Patient assessment is a key step to in preventing abuse of psychotropic medications. Gentle inquiry about school-related stress and other risk factors for misuse can help practitioners determine if students are at risk of diversion and if additional screening is necessary.
In response to these issues, Stone and Merlo8 have suggested that, in addition to the educational programs held on college campuses on alcohol, illicit drugs, and prescription painkillers, patients should be better informed on the appropriate use of prescription psychiatric medications, instructed to avoid sharing with family and friends, and assessed for abuse risk at regular intervals.
To further protect patients from adverse outcomes during treatment, you can employ conservative and safe prescribing techniques. One strategy might be to keep a personal formulary that lists key medications you use in everyday practice, including knowledge about each drug’s dosage, potential adverse effects, key warnings, and drug−drug interactions.40
Furthermore, maintain healthy caution about newly approved medications and carefully consider how they measure up to existing agents—in other words, practice evidence-based medicine, particularly when students request a particular agent.40,41 Prescribers should evaluate the risk of abuse before prescribing and attempt to prevent misuse by limiting quantities and minimizing polypharmacy.
Last, pharmacists can be key allies for consultation and appropriate medication selection.
Bottom Line
Psychotropic medications are necessary to treat the variety of conditions—anxiety, attention-deficit/hyperactivity disorder, depression, and panic disorder—common among college students. However, students are at risk of combining their prescribed medications with other medications, drugs, and alcohol or could sell or share their medication with peers. Proper counseling and identification of risk factors can be important tools for preventing such events.
Related Resources
• American College Health Association-National College Health Assessment. www.acha-ncha.org.
• Schwartz VI. College mental health: How to provide care for students in need. Current Psychiatry. 2011;10(12):22-29.
Drug Brand Names
Bupropion • Wellbutrin, Zyban
Methadone • Methadose, Dolophine
Theophylline • Theo-24, Theolair, Uniphyl
Disclosures
The authors report no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
Many college students suffer from mental illness (Table 1),1 which can have a negative impact on academic performance. Although psychotropic medications are an important part of treatment for many college students, the potential for misuse always is present. Drug misuse occurs when patients use medications for reasons inconsistent with legal or medical guidelines.2 For example, patients may take a medication that has not been prescribed for them or in a manner that is inconsistent with the prescriber’s instructions, including administration with other substances.3
Misuse of psychotropic drugs is prevalent among college students. A study of 14,175 students from 26 campuses reported that 14.7% of students taking a psychotropic are doing so without a prescription, including stimulants (52.6%), anxiolytics (38.4%), and antidepressants (17.4%).4 Another study states that more than one-third of responders reported misuse of >1 class of medication.5
Psychotropic misuse is concerning because it increases the risk of adverse events. Nearly one-half of medication errors are associated with writing and dispensing the prescription, which means that prescribers can work to reduce these errors.6 However, nonadherence, prescription misuse, and failure to disclose use of over-the-counter drugs, illicit drugs, and herbal products makes preventing most adverse events difficult, if not impossible, for prescribers.7,8
Psychotropic drug misuse among college students is highly variable and unpredictable. Students misuse medications, including stimulants, benzodiazepines, and antidepressants, for a variety of reasons, such as study enhancement, experimentation, intoxication, self-medication, relaxation, and stress management.8 One survey reported that >70% of students taking a psychotropic medication took it with alcohol or another illicit drug.9
However, <20% of those using a psychotropic medication with alcohol or other illicit drugs told their health care provider(s),9 making it impossible for clinicians to predict a patient’s risk of drug− drug interactions and subsequent adverse events. Additionally, additive effects could occur10 and changes in a patient’s presentation could be caused by a reaction to a combination of medications, rather than a new symptom of mental illness.
This article will examine common issues associated with drug misuse among college-age students and review prevention strategies (Table 2).
Stimulants
Stimulants have the highest rate of diversion; 61.7% of college students prescribed stimulants have shared or sold their medication.11 A survey of 115 students from 2 universities reported that the most common reason for stimulant misuse was to enhance academic performance.12 The same survey showed that some students take stimulants with Cannabis (17%) and alcohol (30%).12 As a result, in addition to lowering grade point average (GPA) and other academic difficulties,13 students misusing stimulants are at risk of drug interactions.14
It is critical to ascertain the route of drug administration, because non-oral routes, including crushing then snorting or injecting, are associated with additional health concerns, such as accidental death or blood-borne illnesses.15,16 Cardiac adverse effects of stimulants include hypertension, vasospasm, tachycardia, and dysrhythmia; psychiatric and other effects include serotonin syndrome, hallucinations, anxiety, paranoia, seizures, tics, hyperthermia, and tremor.17 Health care providers prescribing or caring for people taking a stimulant should monitor for these potential effects.
The risk of switch to mania might not be apparent to those who prescribe stimulants or to young people who take non-prescribed stimulants for academic enhancement or to achieve medication-induced euphoria. Adolescent stimulant use is associated with symptoms of early-onset bipolar disorder in patients who have attention-deficit/ hyperactivity disorder (ADHD) and undiagnosed bipolarity.18
The cardiovascular risk associated with stimulant use is debatable. Although several studies have been conducted,19-21 methodological factors limit their applicability. To minimize potential risks, several precautions should be taken before prescribing a stimulant to treat ADHD.
First, obtain a detailed personal and family medical history, asking about possible cardiovascular disease. Second, carefully scrutinize the patient’s cardiovascular system during the physical exam. Third, consider additional testing, such as an electrocardiogram, if the patient’s history or physical exam indicates possible risk.22
As a prescriber, you should be aware of the prevalence of stimulant use among students with and without ADHD, including those who could be feigning ADHD symptoms.15 Diversion could occur through sharing medications or selling them to friends and family.11 It also is possible that these medications may be used with other illicit substances, such as Cannabis, ecstasy, cocaine, and opiates.23 Students also could misuse stimulants by taking more than the prescribed dosage.24
Risk factors for misuse of stimulants include: heavy alcohol use, previous illicit drug use, white race, fraternity or sorority membership, low GPA, increased hyperactivity symptoms, and attendance at a competitive college or university.25-27
Benzodiazepines
Misuse of benzodiazepine is a significant component of prescription drug abuse and often occurs with other medications and alcohol.28 Additional methods of misuse include increased dosage and non-oral routes of administration.29
A 2001 national survey reported that 7.8% of college students have misused benzodiazepines.23 Common characteristics of benzodiazepine abusers include young age, male sex, personality characteristics of impulsivity and hopelessness, and abuse of other drugs, including cocaine and methadone.28,29
Benzodiazepines are prescribed for their anxiolytic and hypnotic properties and students could use these drugs with other agents to augment the euphoric effects or diminish withdrawal symptoms.30 Patients taking benzodiazepines for anxiety might self-medicate with alcohol, which increases sedation and depression, and can contribute to the risk for respiratory depression.10 Misuse of benzodiazepines can result in cognitive and psychomotor impairment and increase the risk of accidents and overdose.29,31
Although overdose with monotherapy is rare, the risk increases when a benzodiazepine is used with alcohol10 or another respiratory depressants, such as opioids, because combination use can produce additive effects.28 You should therefore avoid prescribing benzodiazepines to patients who have a history of significant substance abuse and consider using alternative, non-addictive agents, such as selective serotonin reuptake inhibitors, or non-pharmaceutical treatment when such patients present with an anxiety disorder. The risk of adverse effects of benzodiazepines can be reduced by limiting the dosing and the duration of the treatment, and by using longer-acting rather than the more addictive, shorter-acting, agents.
Antidepressants
Health care providers should be aware that, despite the relative absence of physically addictive properties, antidepressants from most classes are abusable agents sought by young people for non-medical use. In particular, the literature highlights monoamine oxidase inhibitors (MAOIs), tricyclic antidepressants, serotonin-norepinephrine reuptake inhibitors, and bupropion as the antidepressants most likely to be misused for their amphetamine-like euphoric effects or serotonin-induced dissociative effects.32 However, compared with other drug classes discussed in this article, the rate of antidepressant misuse is relatively low among college students.
Regardless of the antidepressant selected, clinicians should be concerned about alcohol use among college-age patients. Persons with depression are at increased risk of alcoholism compared with the general population.33 This combination can increase depressive symptoms and sedation, and decrease coordination, judgment, and reaction time.33
Excessive alcohol use can increase the risk of seizures in patients taking antidepressants such as buproprion.34 Employ caution when prescribing bupropion to patients who have a predisposing clinical factor that increases seizure risk, such as excessive alcohol use and abrupt cessation, use of other medications that may lower seizure threshold (eg, theophylline, amphetamines, phenothiazines), and a history of head trauma.34
To minimize the risk of seizures with bupropion, titrate up the dosage slowly. Furthermore, using a low dosage during dual therapy for antidepressant augmentation further decreases the risk of seizure.35 For these reasons, we recommend that you avoid bupropion in patients who are at risk of binge drinking, and give careful consideration to providing alternative therapies for them.
Prescribers and patients should also keep in mind that hypertensive crisis could occur if MAOIs are combined with certain types of alcoholic beverages containing tyramine, including some wines and draft beer.33
How you can identify and prevent misuse
Careful communication between health care provider and patient that is necessary to minimize the risk of adverse drug events with psychotropic medications often is lacking. For example, 24% of study college-age participants did not remember if their physician provided a diagnosis and 28.8% could not recall being informed about side effects and, perhaps as a result, many students did not take their medications as prescribed.9
Further, prescribers should ask college-age patients who are undergoing stimulant treatment if they believe that they are being adequately treated. They should inquire about how they are taking their medications.11 These questions can lead to discussion of the need for these medications and reevaluation of their perceived indication.11
Remind patients to take their medication only as directed.36 Highlight the need to:
• store medications in a discreet location
• properly dispose of unused medications
• keep tabs on the quantity of pills
• know how to resist requests for diversion from peers.
The Substance Abuse and Mental Health Services Administration offers additional useful strategies,37 and pharmacists also can be partners in substance use education and prevention.38 These are examples of how health care providers can take an active role in providing patients with a thorough and detailed understanding of (1) their conditions and (2) their prescribed medications to improve efficacy and safety while preventing misuse.8
A study found that the most common method of obtaining these medications without a prescription is acquiring them from peers; 54% of undergraduate patients with stimulant prescriptions have been approached by peers to give, trade, or sell their drugs.25 Other methods include purchasing medications online or faking prescriptions.39 Health care providers should remind patients of the legal ramifications of sharing or selling their prescribed medications. Finally, providers must be vigilant for students who may feign symptoms to obtain a prescription:
• be wary if symptom presentation sounds too “textbook”
• seek collateral history from family. Adults with ADHD should have shown symptoms during childhood
• use external verification such as neuropsychological testing for ADHD. A neuropsychologist can detect deception by analyzing the pattern of responses to questions.
Patient assessment is a key step to in preventing abuse of psychotropic medications. Gentle inquiry about school-related stress and other risk factors for misuse can help practitioners determine if students are at risk of diversion and if additional screening is necessary.
In response to these issues, Stone and Merlo8 have suggested that, in addition to the educational programs held on college campuses on alcohol, illicit drugs, and prescription painkillers, patients should be better informed on the appropriate use of prescription psychiatric medications, instructed to avoid sharing with family and friends, and assessed for abuse risk at regular intervals.
To further protect patients from adverse outcomes during treatment, you can employ conservative and safe prescribing techniques. One strategy might be to keep a personal formulary that lists key medications you use in everyday practice, including knowledge about each drug’s dosage, potential adverse effects, key warnings, and drug−drug interactions.40
Furthermore, maintain healthy caution about newly approved medications and carefully consider how they measure up to existing agents—in other words, practice evidence-based medicine, particularly when students request a particular agent.40,41 Prescribers should evaluate the risk of abuse before prescribing and attempt to prevent misuse by limiting quantities and minimizing polypharmacy.
Last, pharmacists can be key allies for consultation and appropriate medication selection.
Bottom Line
Psychotropic medications are necessary to treat the variety of conditions—anxiety, attention-deficit/hyperactivity disorder, depression, and panic disorder—common among college students. However, students are at risk of combining their prescribed medications with other medications, drugs, and alcohol or could sell or share their medication with peers. Proper counseling and identification of risk factors can be important tools for preventing such events.
Related Resources
• American College Health Association-National College Health Assessment. www.acha-ncha.org.
• Schwartz VI. College mental health: How to provide care for students in need. Current Psychiatry. 2011;10(12):22-29.
Drug Brand Names
Bupropion • Wellbutrin, Zyban
Methadone • Methadose, Dolophine
Theophylline • Theo-24, Theolair, Uniphyl
Disclosures
The authors report no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
1. American College Health Association. American College Health Association-National College Health Assessment II: Reference Group Executive Summary Spring 2014. http://www.acha-ncha.org/docs/ACHA-NCHA-II_ReferenceGroup_ExecutiveSummary_ Spring2014.pdf. Published 2014. Accessed January 13, 2015.
2. World Health Organization. Management of substance abuse. http://www.who.int/substance_abuse/terminology/ abuse/en. Accessed June 4, 2015.
3. U.S. Food and Drug Administration. Combating misuse and abuse of prescription drugs: Q&A with Michael Klein, PhD. http://www.fda.gov/ForConsumers/ConsumerUpdates/ ucm220112.htm. Published July 28, 2010. Accessed June 18, 2014.
4. Eisenberg D, Hunt J, Speer N, et al. Mental health service utilization among college students in the United States. J Nerv Ment Dis. 2011;199(5):301-308.
5. Peralta RL, Steele JL. Nonmedical prescription drug use among US college students at a Midwest university: a partial test of social learning theory. Subst Use Misuse. 2010;45(6):865-887.
6. Agency for Healthcare Research and Quality. Reducing and preventing adverse drug events to decrease hospital costs: Research in action. http://www.ahrq.gov/research/ findings/factsheets/errors-safety/aderia/index.html. Updated March 2001. Accessed June 21, 2014.
7. Procyshyn RM, Barr AM, Brickell T, et al. Medication errors in psychiatry: a comprehensive review. CNS Drugs. 2010;24(7):595-609.
8. Stone AM, Merlo LJ. Attitudes of college students toward mental illness stigma and the misuse of psychiatric medications. J Clin Psychiatry. 2011;72(2):134-139.
9. Oberleitner LM, Tzilos GK, Zumberg KM, et al. Psychotropic drug use among college students: patterns of use, misuse, and medical monitoring. J Am Coll Health. 2011;59(7):658-661.
10. Linnoila MI. Benzodiazepines and alcohol. J Psychiatr Res. 1990;24(suppl 2):121-127.
11. Garnier LM, Arria AM, Caldeira KM, et al. Sharing and selling of prescription medications in a college student sample. J Clin Psychiatry. 2010;71(3):262-269.
12. Rabiner DL, Anastopoulos AD, Costello EJ, et al. The misuse and diversion of prescribed ADHD medications by college students. J Atten Disord. 2009;13(2):144-153.
13. Arria AM. Nonmedical use of prescription stimulants and analgesics: associations with social and academic behaviors among college students. J Drug Issues. 2008; 38(4):1045-1060.
14. Arria AM, Caldeira KM, O’Grady KE, et al. Nonmedical use of prescription stimulants among college students: associations with attention-deficit-hyperactivity disorder and polydrug use. Pharmacotherapy. 2008;28(2):156-169.
15. Rabiner DL. Stimulant prescription cautions: addressing misuse, diversion and malingering. Curr Psychiatry Rep. 2013;15(7):375.
16. Sepúlveda DR, Thomas LM, McCabe SE, et al. Misuse of prescribed stimulant medication for ADHD and associated patterns of substance use: preliminary analysis among college students. J Pharm Pract. 2011;24(6):551-560.
17. Greydanus DE. Stimulant misuse: strategies to manage a growing problem. http://www.acha.org/Continuing_ Education/docs/ACHA_Use_Misuse_of_Stimulants_ Article2.pdf. Accessed June 29, 2015.
18. Vergne D, Whitham E, Barroilhet S, et al. Adult ADHD and amphetamines: a new paradigm. Neuropsychiatry. 2011;1(6):591-598.
19. Habel LA, Cooper WO, Sox CM, et al. ADHD medications and risk of serious cardiovascular events in young and middle-aged adults. JAMA. 2011;306(24):2673-2683.
20. Cooper WO, Habel LA, Sox CM, et al. ADHD drugs and serious cardiovascular events in children and young adults. N Engl J Med. 2011;365(20):1896-1904.
21. Schelleman H, Bilker WB, Kimmel SE, et al. Methylphenidate and risk of serious cardiovascular events in adults. Am J Psychiatry. 2012;169(2):178-185.
22. U.S. Food and Drug Administration. Communication about an ongoing safety review of stimulant medications used in children with attention-deficit/hyperactivity disorder (ADHD). http://www.fda.gov/Drugs/Drug Safety/PostmarketDrugSafetyInformationforPatients andProviders/DrugSafetyInformationforHeathcare Professionals/ucm165858.htm. Updated August 15, 2013. Accessed June 25, 2014.
23. McCabe SE, Knight JR, Teter CJ, et al. Non-medical use of prescription stimulants among US college students: prevalence and correlates from a national survey. Addiction. 2005;100(1):96-106.
24. McNiel AD, Muzzin KB, DeWald JP, et al. The nonmedical use of prescription stimulants among dental and dental hygiene students. J Dent Educ. 2011;75(3):365-376.
25. McCabe SE, Teter CJ, Boyd CJ. Medical use, illicit use and diversion of prescription stimulant medication. J Psychoactive Drugs. 2006;38(1):43-56.
26. Arria AM, Garnier-Dykstra LM, Caldeira KM, et al. Persistent nonmedical use of prescription stimulants among college students: possible association with ADHD symptoms. J Atten Disord. 2011;15(5):347-356.
27. Teter CJ, McCabe SE, Boyd CJ, et al. Illicit methylphenidate use in an undergraduate student sample: prevalence and risk factors. Pharmacotherapy. 2003;23(5):609-617.
28. Hernandez SH, Nelson LS. Prescription drug abuse: insight into the epidemic. Clin Pharmacol Ther. 2010; 88(3):307-317.
29. McLarnon ME, Monaghan TL, Stewart SH, et al. Drug misuse and diversion in adults prescribed anxiolytics and sedatives. Pharmacotherapy. 2011;31(3):262-272.
30. Woods JH, Katz JL, Winger G. Benzodiazepines: use, abuse, and consequences. Pharmacol Rev. 1992;44(2):151-347.
31. Buffett-Jerrott SE, Stewart SH. Cognitive and sedative effects of benzodiazepine use. Curr Pharm Des. 2002;8(1):45-58.
32. Evans EA, Sullivan MA. Abuse and misuse of antidepressants. Subst Abuse Rehabil. 2014;5:107-120.
33. Hall-Flavin DK. Why is it bad to mix antidepressants and alcohol? http://www.mayoclinic.com/health/antidepressants-and-alcohol/AN01653. Updated June 12, 2014. Accessed June 20, 2014.
34. Wellbutrin [package insert]. Research Triangle Park, NC: GlaxoSmithKline LLC; 2014.
35. Davidson J. Seizures and bupropion: a review. J Clin Psychiatry. 1989;50(7):256-261.
36. Maddox JC, Levi M, Thompson C. The compliance with antidepressants in general practice. J Psychopharmacol. 1994;8(1):48-52.
37. Substance Abuse and Mental Health Services Administration. You’re in control: using prescription medication responsibly. http://store.samhsa.gov/shin/content/SMA12-4678B3/SMA12-4678B3.pdf. Accessed June 5, 2015.
38. ASHP statement on the pharmacist’s role in substance abuse prevention, education, and assistance. Am J Health Syst Pharm. 2014;71(3):243-246.
39. Inciardi JA, Surratt HL, Cicero TJ, et al. Prescription drugs purchased through the internet: who are the end users? Drug Alcohol Depend. 2010;110(1-2):21-29.
40. Preskorn SH, Flockhart D. 2006 Guide to psychiatric drug interactions. Primary Psychiatry. 2006;13(4):35-64.
41. Schiff GD, Galanter WL, Duhig J, et al. Principles of conservative prescribing. Arch Intern Med. 2011;171(16): 1433-1440.
1. American College Health Association. American College Health Association-National College Health Assessment II: Reference Group Executive Summary Spring 2014. http://www.acha-ncha.org/docs/ACHA-NCHA-II_ReferenceGroup_ExecutiveSummary_ Spring2014.pdf. Published 2014. Accessed January 13, 2015.
2. World Health Organization. Management of substance abuse. http://www.who.int/substance_abuse/terminology/ abuse/en. Accessed June 4, 2015.
3. U.S. Food and Drug Administration. Combating misuse and abuse of prescription drugs: Q&A with Michael Klein, PhD. http://www.fda.gov/ForConsumers/ConsumerUpdates/ ucm220112.htm. Published July 28, 2010. Accessed June 18, 2014.
4. Eisenberg D, Hunt J, Speer N, et al. Mental health service utilization among college students in the United States. J Nerv Ment Dis. 2011;199(5):301-308.
5. Peralta RL, Steele JL. Nonmedical prescription drug use among US college students at a Midwest university: a partial test of social learning theory. Subst Use Misuse. 2010;45(6):865-887.
6. Agency for Healthcare Research and Quality. Reducing and preventing adverse drug events to decrease hospital costs: Research in action. http://www.ahrq.gov/research/ findings/factsheets/errors-safety/aderia/index.html. Updated March 2001. Accessed June 21, 2014.
7. Procyshyn RM, Barr AM, Brickell T, et al. Medication errors in psychiatry: a comprehensive review. CNS Drugs. 2010;24(7):595-609.
8. Stone AM, Merlo LJ. Attitudes of college students toward mental illness stigma and the misuse of psychiatric medications. J Clin Psychiatry. 2011;72(2):134-139.
9. Oberleitner LM, Tzilos GK, Zumberg KM, et al. Psychotropic drug use among college students: patterns of use, misuse, and medical monitoring. J Am Coll Health. 2011;59(7):658-661.
10. Linnoila MI. Benzodiazepines and alcohol. J Psychiatr Res. 1990;24(suppl 2):121-127.
11. Garnier LM, Arria AM, Caldeira KM, et al. Sharing and selling of prescription medications in a college student sample. J Clin Psychiatry. 2010;71(3):262-269.
12. Rabiner DL, Anastopoulos AD, Costello EJ, et al. The misuse and diversion of prescribed ADHD medications by college students. J Atten Disord. 2009;13(2):144-153.
13. Arria AM. Nonmedical use of prescription stimulants and analgesics: associations with social and academic behaviors among college students. J Drug Issues. 2008; 38(4):1045-1060.
14. Arria AM, Caldeira KM, O’Grady KE, et al. Nonmedical use of prescription stimulants among college students: associations with attention-deficit-hyperactivity disorder and polydrug use. Pharmacotherapy. 2008;28(2):156-169.
15. Rabiner DL. Stimulant prescription cautions: addressing misuse, diversion and malingering. Curr Psychiatry Rep. 2013;15(7):375.
16. Sepúlveda DR, Thomas LM, McCabe SE, et al. Misuse of prescribed stimulant medication for ADHD and associated patterns of substance use: preliminary analysis among college students. J Pharm Pract. 2011;24(6):551-560.
17. Greydanus DE. Stimulant misuse: strategies to manage a growing problem. http://www.acha.org/Continuing_ Education/docs/ACHA_Use_Misuse_of_Stimulants_ Article2.pdf. Accessed June 29, 2015.
18. Vergne D, Whitham E, Barroilhet S, et al. Adult ADHD and amphetamines: a new paradigm. Neuropsychiatry. 2011;1(6):591-598.
19. Habel LA, Cooper WO, Sox CM, et al. ADHD medications and risk of serious cardiovascular events in young and middle-aged adults. JAMA. 2011;306(24):2673-2683.
20. Cooper WO, Habel LA, Sox CM, et al. ADHD drugs and serious cardiovascular events in children and young adults. N Engl J Med. 2011;365(20):1896-1904.
21. Schelleman H, Bilker WB, Kimmel SE, et al. Methylphenidate and risk of serious cardiovascular events in adults. Am J Psychiatry. 2012;169(2):178-185.
22. U.S. Food and Drug Administration. Communication about an ongoing safety review of stimulant medications used in children with attention-deficit/hyperactivity disorder (ADHD). http://www.fda.gov/Drugs/Drug Safety/PostmarketDrugSafetyInformationforPatients andProviders/DrugSafetyInformationforHeathcare Professionals/ucm165858.htm. Updated August 15, 2013. Accessed June 25, 2014.
23. McCabe SE, Knight JR, Teter CJ, et al. Non-medical use of prescription stimulants among US college students: prevalence and correlates from a national survey. Addiction. 2005;100(1):96-106.
24. McNiel AD, Muzzin KB, DeWald JP, et al. The nonmedical use of prescription stimulants among dental and dental hygiene students. J Dent Educ. 2011;75(3):365-376.
25. McCabe SE, Teter CJ, Boyd CJ. Medical use, illicit use and diversion of prescription stimulant medication. J Psychoactive Drugs. 2006;38(1):43-56.
26. Arria AM, Garnier-Dykstra LM, Caldeira KM, et al. Persistent nonmedical use of prescription stimulants among college students: possible association with ADHD symptoms. J Atten Disord. 2011;15(5):347-356.
27. Teter CJ, McCabe SE, Boyd CJ, et al. Illicit methylphenidate use in an undergraduate student sample: prevalence and risk factors. Pharmacotherapy. 2003;23(5):609-617.
28. Hernandez SH, Nelson LS. Prescription drug abuse: insight into the epidemic. Clin Pharmacol Ther. 2010; 88(3):307-317.
29. McLarnon ME, Monaghan TL, Stewart SH, et al. Drug misuse and diversion in adults prescribed anxiolytics and sedatives. Pharmacotherapy. 2011;31(3):262-272.
30. Woods JH, Katz JL, Winger G. Benzodiazepines: use, abuse, and consequences. Pharmacol Rev. 1992;44(2):151-347.
31. Buffett-Jerrott SE, Stewart SH. Cognitive and sedative effects of benzodiazepine use. Curr Pharm Des. 2002;8(1):45-58.
32. Evans EA, Sullivan MA. Abuse and misuse of antidepressants. Subst Abuse Rehabil. 2014;5:107-120.
33. Hall-Flavin DK. Why is it bad to mix antidepressants and alcohol? http://www.mayoclinic.com/health/antidepressants-and-alcohol/AN01653. Updated June 12, 2014. Accessed June 20, 2014.
34. Wellbutrin [package insert]. Research Triangle Park, NC: GlaxoSmithKline LLC; 2014.
35. Davidson J. Seizures and bupropion: a review. J Clin Psychiatry. 1989;50(7):256-261.
36. Maddox JC, Levi M, Thompson C. The compliance with antidepressants in general practice. J Psychopharmacol. 1994;8(1):48-52.
37. Substance Abuse and Mental Health Services Administration. You’re in control: using prescription medication responsibly. http://store.samhsa.gov/shin/content/SMA12-4678B3/SMA12-4678B3.pdf. Accessed June 5, 2015.
38. ASHP statement on the pharmacist’s role in substance abuse prevention, education, and assistance. Am J Health Syst Pharm. 2014;71(3):243-246.
39. Inciardi JA, Surratt HL, Cicero TJ, et al. Prescription drugs purchased through the internet: who are the end users? Drug Alcohol Depend. 2010;110(1-2):21-29.
40. Preskorn SH, Flockhart D. 2006 Guide to psychiatric drug interactions. Primary Psychiatry. 2006;13(4):35-64.
41. Schiff GD, Galanter WL, Duhig J, et al. Principles of conservative prescribing. Arch Intern Med. 2011;171(16): 1433-1440.
How to collaborate effectively with psychiatric nurse practitioners
Discuss this article at www.facebook.com/CurrentPsychiatry
Psychiatrists who are accustomed to working with “med/surg” or psychiatric nurses may be less familiar with how to collaborate with more specialized psychiatric-mental health nurse practitioners (PMHNPs). These clinicians play an important role in delivering mental health services, which is likely to continue because of the physician shortage in the United States1 and increasing mental health care needs from passage of the Affordable Health Care Act and the Mental Health Parity Act.2 These specialty trained, master’s level nurses work with psychiatrists in outpatient clinics, hospital consultation and liaison services, psychiatric emergency services, inpatient units, and geropsychiatric consultation.3-5 PMHNPs can fill gaps of coverage in underserved areas, supplement and complement busy and overburdened psychiatrists, and add an important dimension of holistic care.
This article reviews issues related to a successful psychiatrist-PMHNP collaboration, including:
- PMHNP’s training and scope of practice
- their skill and competency development in inpatient and outpatient settings
- the principles and dynamics of collaboration, hindrances to cooperation, and keys to relationship-building for PMHNPs and psychiatrists.
Rigorous requirements
PMHNPs enroll in an accredited graduate nursing program that takes 16 to 24 months to complete and builds on the competencies of their undergraduate nursing education and clinical experience. All programs meet standards set by national nursing accrediting agencies. The typical graduate-level curriculum for a PMHNP includes core bio-behavioral theory, research courses, advanced physiology and pathophysiology, advanced physical and psychiatric health assessment, pharmacologic and nonpharmacologic interventions, and managing health care delivery systems. For graduation and certification, PMHNPs must complete 500 supervised clinical hours focused on psychiatric and mental health care.
- comprehensive psychiatric evaluation
- formulation of a differential diagnosis
- ordering and interpreting diagnostic tests
- prescribing pharmacologic agents
- conducting individual, couple, group, or family psychotherapy using evidence-based approaches.
PMHNPs also are responsible for recognizing the limits of their knowledge and experience, planning for situations beyond their expertise, and providing appropriate referral to other health care providers when indicated.8
Successful collaborative practice requires a clear definition and understanding of roles.9 This is particularly important for collaborating psychiatrists and PMHNPs because there has been confusion among physicians and the general public related to the nurse practitioner’s role. Psychiatrists who work with PMHNPs need to be familiar with state regulations that govern levels of physician supervision and prescriptive authority for nurse practitioners. Eleven states and the District of Columbia allow nurse practitioners to prescribe independently, including controlled substances. Most states require physician collaboration for prescribing medications, but the language can be ambiguous, with restrictions on certain formularies or drug schedules—eg, Michigan nurse practitioners may prescribe schedule II through V controlled substances, but schedule II medications are limited to nurse practitioners who work in hospitals, surgical outpatient settings, or hospices.10
Competencies and development
New PMHNPs see patients and prescribe medication, but their work needs close supervision. Postgraduate clinical experience combined with supervision gradually allows the PMHNP greater independence. A PMHNP who provides care in a busy outpatient clinic, inpatient unit, or psychiatric emergency department is likely to master the treatment philosophy and ancillary competencies related to that particular clinical site—including favored pharmacologic approaches, electronic documentation and ordering functions, and admission and discharge facilitation—at a level exceeding that of psychiatric residents, who rotate on and off a service as part of their training.
It’s helpful for new PMHNPs to have a time frame for their development over several years. The Table11 outlines general graded competency areas PMHNPs may focus on in their development. See this article at CurrentPsychiatry.com for Tables that provide examples of detailed competencies for third-year PMHNPs in inpatient and outpatient settings.
Table
PMHNP development: General graded competency areas
| Psychiatric evaluation and diagnosis |
| Psychiatric treatments, including medications and psychotherapies |
| Maintenance of the therapeutic alliance, including monitoring the PMHNP’s emotional responses to patients |
| Participation in an interdisciplinary team |
| Understanding comorbid medical conditions, integrating laboratory and other tests into the treatment plan, and recognizing the need for consultation with the medical team |
| Documentation, such as initial evaluations, progress notes, and discharge summaries |
| Assessment for suicide and violence potential |
| Teaching |
| Patient and family psychoeducation |
| Use of feedback and supervision |
| PMHNP: psychiatric-mental health nurse practitioner Source: Reference 11 |
Table 1
Competencies for third-year PMHNPs in an outpatient clinic
| Recognize clinical presentations of complex psychiatric disorders, variants, and comorbidities |
| Firm knowledge of diagnostic criteria, and skills for independent comprehensive assessment and diagnosis |
| Firm knowledge of evidence-based outpatient treatments for disorders, with mastery of ≥1 nonpharmacologic modality in addition to prescribing and managing medications |
| Use and provide feedback in comprehensive case formulations and treatment plans |
| Assist in clinical education of trainees in psychiatric nursing, social work, psychiatric residency, and psychology |
| Participate and collaborate in educational events and initiatives |
| Knowledge of internal and external health system and resources, and facilitating patient access to these networks |
| Incorporate mental health and behavioral and psychiatric nursing research into patient care |
| PMHNP: psychiatric-mental health nurse practitioner |
Competencies for third-year PMHNPs on an inpatient psychiatric unit
| Refinement of assessment section in evaluations, progress notes, and discharge summaries |
| Understanding indications for neuropsychological testing, and integrating findings into the treatment plan |
| Assessment of readiness for discharge in patients with a history of suicidality or violence |
| Developing a sophisticated and detailed discharge or follow-up plan |
| Understanding treatment resistance in mood and psychotic disorders, and implementing treatment |
| More detailed knowledge of types of illness treated on an inpatient unit |
| Ability to orient and train PMHNPs and other inpatient unit trainees |
| Ability to gather and use articles and other literature pertaining to inpatient care |
| Increasing competence in short-term, crisis-based therapeutic techniques, including familiarity with DBT, CBT, and IPT |
| Understanding family systems and impact on patient care |
| CBT: cognitive-behavioral therapy; DBT: dialectical behavior therapy; IPT: interpersonal therapy; PMHNP: psychiatric-mental health nurse practitioner |
Principles of practice
Studies have demonstrated the importance of understanding how to effectively implement collaborative care across medical disciplines.12 See the Box12 for a discussion of 3 key determinants for successful clinical collaborations.
San Martín-Rodríguez et al12 recognized 3 key factors that may help develop successful collaborative clinical relationships.
Interactional factors include a mutual willingness to collaborate, a commitment to collaborate, a belief in the benefits of collaborating, and sharing common objectives. Trust in the partnering clinician’s competency contributes to a successful collaboration. Strong communication skills—including the ability to convey what each clinician can contribute to achieving goals—also strengthens collaboration. Learning and understanding skills in conflict management and dialogue are key. Mutual respect also is essential.
Organizational factors include a shift from a traditional hierarchical structure to a more horizontal structure, and a work climate that supports openness, risk taking—ie, a willingness to disagree with a colleague if it is in a patient’s best interest or to develop a new and innovative method of providing care—integrity, and trust. Administrative structures and supports that convey the importance of collaboration also are key components of a strong collaborative environment. Teamwork and shared decision-making are important elements; teamwork should include time to discuss patient issues and develop strong interpersonal relationships. A commitment to professional development is another key factor.
Systemic factors include a social system that supports collegial relationships and professionalism that respects and accepts other professions. This includes decreased focus on protecting professional territory and increased recognition of overlaps among professions.
Enhancing collaboration
Psychiatrists who work with PMHNPs develop trust based on observing each PMHNP’s work, including their relationship with patients, ability to conceptualize a case and develop a treatment plan, and the skill with which they function within a team. The psychiatrist’s comfort level also is related to his or her awareness of the comprehensiveness of the PMHNP’s training and the competencies gained from clinical experience. Respect for the PMHNP’s educational and professional background is the foundation for what is often—at least in the collaborative relationship’s initial stages—a combined cooperative and supervisory relationship with the PMHNP. As such, the PMHNP gradually will absorb certain “intangibles” to supplement the training and work experiences that preceded his or her position. This may include assimilating the psychiatrist’s or clinic’s philosophy and treatment practice, including expertise in dealing with specialized psychiatric populations (eg, developmental disabilities, acute psychosis, or treatment-resistant depression).
The patient’s comfort level
Collaborating PMHNPs and psychiatrists need to be prepared for a patient who expresses disappointment with being treated by a PMHNP or a preference to see “a doctor.” Psychiatrists who have not worked through their own ambivalence about the collaboration or who lack confidence in the PMHNP’s abilities may find themselves consciously or unconsciously aligning with the patient’s stance. They may neglect to explore the basis and meaning of the patient’s preference, which may be related to the patient’s lack of knowledge about the PMHNP’s role and training. The PMHNP who encounters such a patient has a more challenging task—namely, how to calmly address the patient’s concern while the patient is challenging the PMHNP’s competence. Both the PMHNP and psychiatrist need to be alert to the possibility of “splitting” in the treatment of axis II-disordered patients.
Barriers to collaboration
From the PMHNP perspective, barriers to a collaborative relationship include referring to PMHNPs by a less preferred term or title, instead of a nurse practitioner or APN, which can hinder the relationship. Although physician assistants and NPs have been grouped together under the term “mid-level providers,” the American Academy of Nurse Practitioners notes that this term suggests a lower level of care or service is being provided.18 “Physician extender” is another term that fails to recognize the PMHNP’s separate and unique role and the PMHNP’s view of their role as complementary to medicine, rather than an extension of a physician’s practice.
Territorial issues can impede collaborative relationships. Psychiatrists who resist collaborating will be less effective than those who welcome a PMHNP and readily delegate specific tasks and portions of the workload, whereas psychiatrists who value the help will be more likely to build a collaborative partnership, leading to better patient care.
Autonomy is a critical determinant of professional satisfaction for PMHNPs. A PMHNP’s autonomy can be impeded by organizational constraints and physician perceptions.19 PMHNPs require autonomy to self-direct patient diagnosis and treatment within the scope of their practice, and many find this relative independence essential to delivering high quality patient care. Lack of autonomy can lead to breaks in workflow in the outpatient setting and increased length of stay for hospitalized patients. In addition, an autonomously functioning, experienced PMHNP can increase efficiency in hospital settings where psychiatrists can be in short supply, preoccupied with administrative matters, or require help on weekends.
Related Resources
- American Psychiatric Nurses Association. www.apna.org.
- International Society of Psychiatric-Mental Health Nurses. www.ispn-psych.org.
- American Nurses Association. www.nursingworld.org.
Dr. Casher is a speaker for Sunovion Pharmaceuticals and receives royalties from Cambridge University Press.
Ms. Kuebler, Ms. Bastida, and Ms. Chipps report no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
1. Sataline S, Wang SS. Medical schools can’t keep up. Wall Street Journal. April 12 2010. http://online.wsj.com/article/SB10001424052702304506904575180331528424238.html. Accessed August 21, 2012.
2. U.S. Department of Health and Human Services. The health care law & you. http://www.healthcare.gov/law/index.html. Accessed August 21, 2012.
3. Wand T, Fisher J. The mental health nurse practitioner in the emergency department: an Australian experience. Int J Ment Health Nurs. 2006;15(3):201-208.
4. Eisch JS, Brozovic B, Colling K, et al. Nurse practitioner geropsychiatric consultation service to nursing homes. Geriatr Nurs. 2000;21(3):150-155.
5. Baker N. Exploring the mental health nurse practitioner scope of practice in youth early psychosis: an anecdotal account. Contemp Nurse. 2010;34(2):211-220.
6. International Society of Psychiatric-Mental Health Nurses. Psychiatric mental health nursing scope & standards. http://www.ispn-psych.org/docs/standards/scope-standards-draft.pdf. Updated 2006. Accessed August 21, 2012.
7. Centers for Medicare and Medicaid Services. HHS finalizes new rules to cut regulations for hospitals and health care providers saving more than $5 billion. http://www.cms.gov/apps/media/press/release.asp?Counter=4362. Published May 9, 2012. Accessed August 21, 2012.
8. APRN Consensus Work Group, National Council of State Boards of Nursing APRN Advisory Committee. Consensus model for regulation: licensure accreditation, certification & education. https://www.ncsbn.org/Consensus_Model_for_APRN_Regulation_July_2008.pdf. Published July 7, 2008. Accessed August 21, 2012.
9. Legault F, Humbert J, Amos S, et al. Difficulties encountered in collaborative care: logistics trumps desire. J Am Board Fam Med. 2012;25(2):168-176.
10. Michigan Council of Nurse Practitioners. Michigan’s rules and regulations for prescriptive authority. http://micnp.org/displaycommon.cfm?an=1&subarticlenbr=109. Accessed August 21, 2012.
11. Wheeler K, Haber J. Development of psychiatric-mental health nurse practitioner competencies: opportunities for the 21st century. J Am Psychiatr Nurses Assoc. 2004;10(3):129-138.
12. San Martín-Rodríguez L, Beaulieu MD, D’Amour D, et al. The determinants of successful collaboration: a review of theoretical and empirical studies. J Interprof Care. 2005;19(suppl 1):132-147.
13. Suter E, Arndt J, Arthur N, et al. Role understanding and effective communication as core competencies for collaborative practice. J Interprof Care. 2009;23(1):41-51.
14. Horrocks S, Anderson E, Salisbury C. Systematic review of whether nurse practitioners working in primary care can provide equivalent care to doctors. BMJ. 2002;324(7341):819-823.
15. Byrne G, Richardson M, Brunsdon J, et al. Patient satisfaction with emergency nurse practitioners in A & E. J Clin Nurs. 2000;9(1):83-92.
16. McCann TV, Clark E. Attitudes of patients towards mental health nurse prescribing of antipsychotic agents. Int J Nurs Pract. 2008;14(2):115-121.
17. Wortans J, Happell B, Johnstone H. The role of the nurse practitioner in psychiatric/mental health nursing: exploring consumer satisfaction. J Psychiatr Ment Health Nurs. 2006;13(1):78-84.
18. Frellick M. The nurse practitioner will see you now. Advanced practice providers fill the physician gap. Hosp Health Netw. 2011;85(7):44-46, 48–49.
19. Maylone MM, Ranieri L, Quinn Griffin MT, et al. Collaboration and autonomy: perceptions among nurse practitioners. J Am Acad Nurse Pract. 2011;23(1):51-57.
Discuss this article at www.facebook.com/CurrentPsychiatry
Psychiatrists who are accustomed to working with “med/surg” or psychiatric nurses may be less familiar with how to collaborate with more specialized psychiatric-mental health nurse practitioners (PMHNPs). These clinicians play an important role in delivering mental health services, which is likely to continue because of the physician shortage in the United States1 and increasing mental health care needs from passage of the Affordable Health Care Act and the Mental Health Parity Act.2 These specialty trained, master’s level nurses work with psychiatrists in outpatient clinics, hospital consultation and liaison services, psychiatric emergency services, inpatient units, and geropsychiatric consultation.3-5 PMHNPs can fill gaps of coverage in underserved areas, supplement and complement busy and overburdened psychiatrists, and add an important dimension of holistic care.
This article reviews issues related to a successful psychiatrist-PMHNP collaboration, including:
- PMHNP’s training and scope of practice
- their skill and competency development in inpatient and outpatient settings
- the principles and dynamics of collaboration, hindrances to cooperation, and keys to relationship-building for PMHNPs and psychiatrists.
Rigorous requirements
PMHNPs enroll in an accredited graduate nursing program that takes 16 to 24 months to complete and builds on the competencies of their undergraduate nursing education and clinical experience. All programs meet standards set by national nursing accrediting agencies. The typical graduate-level curriculum for a PMHNP includes core bio-behavioral theory, research courses, advanced physiology and pathophysiology, advanced physical and psychiatric health assessment, pharmacologic and nonpharmacologic interventions, and managing health care delivery systems. For graduation and certification, PMHNPs must complete 500 supervised clinical hours focused on psychiatric and mental health care.
- comprehensive psychiatric evaluation
- formulation of a differential diagnosis
- ordering and interpreting diagnostic tests
- prescribing pharmacologic agents
- conducting individual, couple, group, or family psychotherapy using evidence-based approaches.
PMHNPs also are responsible for recognizing the limits of their knowledge and experience, planning for situations beyond their expertise, and providing appropriate referral to other health care providers when indicated.8
Successful collaborative practice requires a clear definition and understanding of roles.9 This is particularly important for collaborating psychiatrists and PMHNPs because there has been confusion among physicians and the general public related to the nurse practitioner’s role. Psychiatrists who work with PMHNPs need to be familiar with state regulations that govern levels of physician supervision and prescriptive authority for nurse practitioners. Eleven states and the District of Columbia allow nurse practitioners to prescribe independently, including controlled substances. Most states require physician collaboration for prescribing medications, but the language can be ambiguous, with restrictions on certain formularies or drug schedules—eg, Michigan nurse practitioners may prescribe schedule II through V controlled substances, but schedule II medications are limited to nurse practitioners who work in hospitals, surgical outpatient settings, or hospices.10
Competencies and development
New PMHNPs see patients and prescribe medication, but their work needs close supervision. Postgraduate clinical experience combined with supervision gradually allows the PMHNP greater independence. A PMHNP who provides care in a busy outpatient clinic, inpatient unit, or psychiatric emergency department is likely to master the treatment philosophy and ancillary competencies related to that particular clinical site—including favored pharmacologic approaches, electronic documentation and ordering functions, and admission and discharge facilitation—at a level exceeding that of psychiatric residents, who rotate on and off a service as part of their training.
It’s helpful for new PMHNPs to have a time frame for their development over several years. The Table11 outlines general graded competency areas PMHNPs may focus on in their development. See this article at CurrentPsychiatry.com for Tables that provide examples of detailed competencies for third-year PMHNPs in inpatient and outpatient settings.
Table
PMHNP development: General graded competency areas
| Psychiatric evaluation and diagnosis |
| Psychiatric treatments, including medications and psychotherapies |
| Maintenance of the therapeutic alliance, including monitoring the PMHNP’s emotional responses to patients |
| Participation in an interdisciplinary team |
| Understanding comorbid medical conditions, integrating laboratory and other tests into the treatment plan, and recognizing the need for consultation with the medical team |
| Documentation, such as initial evaluations, progress notes, and discharge summaries |
| Assessment for suicide and violence potential |
| Teaching |
| Patient and family psychoeducation |
| Use of feedback and supervision |
| PMHNP: psychiatric-mental health nurse practitioner Source: Reference 11 |
Table 1
Competencies for third-year PMHNPs in an outpatient clinic
| Recognize clinical presentations of complex psychiatric disorders, variants, and comorbidities |
| Firm knowledge of diagnostic criteria, and skills for independent comprehensive assessment and diagnosis |
| Firm knowledge of evidence-based outpatient treatments for disorders, with mastery of ≥1 nonpharmacologic modality in addition to prescribing and managing medications |
| Use and provide feedback in comprehensive case formulations and treatment plans |
| Assist in clinical education of trainees in psychiatric nursing, social work, psychiatric residency, and psychology |
| Participate and collaborate in educational events and initiatives |
| Knowledge of internal and external health system and resources, and facilitating patient access to these networks |
| Incorporate mental health and behavioral and psychiatric nursing research into patient care |
| PMHNP: psychiatric-mental health nurse practitioner |
Competencies for third-year PMHNPs on an inpatient psychiatric unit
| Refinement of assessment section in evaluations, progress notes, and discharge summaries |
| Understanding indications for neuropsychological testing, and integrating findings into the treatment plan |
| Assessment of readiness for discharge in patients with a history of suicidality or violence |
| Developing a sophisticated and detailed discharge or follow-up plan |
| Understanding treatment resistance in mood and psychotic disorders, and implementing treatment |
| More detailed knowledge of types of illness treated on an inpatient unit |
| Ability to orient and train PMHNPs and other inpatient unit trainees |
| Ability to gather and use articles and other literature pertaining to inpatient care |
| Increasing competence in short-term, crisis-based therapeutic techniques, including familiarity with DBT, CBT, and IPT |
| Understanding family systems and impact on patient care |
| CBT: cognitive-behavioral therapy; DBT: dialectical behavior therapy; IPT: interpersonal therapy; PMHNP: psychiatric-mental health nurse practitioner |
Principles of practice
Studies have demonstrated the importance of understanding how to effectively implement collaborative care across medical disciplines.12 See the Box12 for a discussion of 3 key determinants for successful clinical collaborations.
San Martín-Rodríguez et al12 recognized 3 key factors that may help develop successful collaborative clinical relationships.
Interactional factors include a mutual willingness to collaborate, a commitment to collaborate, a belief in the benefits of collaborating, and sharing common objectives. Trust in the partnering clinician’s competency contributes to a successful collaboration. Strong communication skills—including the ability to convey what each clinician can contribute to achieving goals—also strengthens collaboration. Learning and understanding skills in conflict management and dialogue are key. Mutual respect also is essential.
Organizational factors include a shift from a traditional hierarchical structure to a more horizontal structure, and a work climate that supports openness, risk taking—ie, a willingness to disagree with a colleague if it is in a patient’s best interest or to develop a new and innovative method of providing care—integrity, and trust. Administrative structures and supports that convey the importance of collaboration also are key components of a strong collaborative environment. Teamwork and shared decision-making are important elements; teamwork should include time to discuss patient issues and develop strong interpersonal relationships. A commitment to professional development is another key factor.
Systemic factors include a social system that supports collegial relationships and professionalism that respects and accepts other professions. This includes decreased focus on protecting professional territory and increased recognition of overlaps among professions.
Enhancing collaboration
Psychiatrists who work with PMHNPs develop trust based on observing each PMHNP’s work, including their relationship with patients, ability to conceptualize a case and develop a treatment plan, and the skill with which they function within a team. The psychiatrist’s comfort level also is related to his or her awareness of the comprehensiveness of the PMHNP’s training and the competencies gained from clinical experience. Respect for the PMHNP’s educational and professional background is the foundation for what is often—at least in the collaborative relationship’s initial stages—a combined cooperative and supervisory relationship with the PMHNP. As such, the PMHNP gradually will absorb certain “intangibles” to supplement the training and work experiences that preceded his or her position. This may include assimilating the psychiatrist’s or clinic’s philosophy and treatment practice, including expertise in dealing with specialized psychiatric populations (eg, developmental disabilities, acute psychosis, or treatment-resistant depression).
The patient’s comfort level
Collaborating PMHNPs and psychiatrists need to be prepared for a patient who expresses disappointment with being treated by a PMHNP or a preference to see “a doctor.” Psychiatrists who have not worked through their own ambivalence about the collaboration or who lack confidence in the PMHNP’s abilities may find themselves consciously or unconsciously aligning with the patient’s stance. They may neglect to explore the basis and meaning of the patient’s preference, which may be related to the patient’s lack of knowledge about the PMHNP’s role and training. The PMHNP who encounters such a patient has a more challenging task—namely, how to calmly address the patient’s concern while the patient is challenging the PMHNP’s competence. Both the PMHNP and psychiatrist need to be alert to the possibility of “splitting” in the treatment of axis II-disordered patients.
Barriers to collaboration
From the PMHNP perspective, barriers to a collaborative relationship include referring to PMHNPs by a less preferred term or title, instead of a nurse practitioner or APN, which can hinder the relationship. Although physician assistants and NPs have been grouped together under the term “mid-level providers,” the American Academy of Nurse Practitioners notes that this term suggests a lower level of care or service is being provided.18 “Physician extender” is another term that fails to recognize the PMHNP’s separate and unique role and the PMHNP’s view of their role as complementary to medicine, rather than an extension of a physician’s practice.
Territorial issues can impede collaborative relationships. Psychiatrists who resist collaborating will be less effective than those who welcome a PMHNP and readily delegate specific tasks and portions of the workload, whereas psychiatrists who value the help will be more likely to build a collaborative partnership, leading to better patient care.
Autonomy is a critical determinant of professional satisfaction for PMHNPs. A PMHNP’s autonomy can be impeded by organizational constraints and physician perceptions.19 PMHNPs require autonomy to self-direct patient diagnosis and treatment within the scope of their practice, and many find this relative independence essential to delivering high quality patient care. Lack of autonomy can lead to breaks in workflow in the outpatient setting and increased length of stay for hospitalized patients. In addition, an autonomously functioning, experienced PMHNP can increase efficiency in hospital settings where psychiatrists can be in short supply, preoccupied with administrative matters, or require help on weekends.
Related Resources
- American Psychiatric Nurses Association. www.apna.org.
- International Society of Psychiatric-Mental Health Nurses. www.ispn-psych.org.
- American Nurses Association. www.nursingworld.org.
Dr. Casher is a speaker for Sunovion Pharmaceuticals and receives royalties from Cambridge University Press.
Ms. Kuebler, Ms. Bastida, and Ms. Chipps report no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
Discuss this article at www.facebook.com/CurrentPsychiatry
Psychiatrists who are accustomed to working with “med/surg” or psychiatric nurses may be less familiar with how to collaborate with more specialized psychiatric-mental health nurse practitioners (PMHNPs). These clinicians play an important role in delivering mental health services, which is likely to continue because of the physician shortage in the United States1 and increasing mental health care needs from passage of the Affordable Health Care Act and the Mental Health Parity Act.2 These specialty trained, master’s level nurses work with psychiatrists in outpatient clinics, hospital consultation and liaison services, psychiatric emergency services, inpatient units, and geropsychiatric consultation.3-5 PMHNPs can fill gaps of coverage in underserved areas, supplement and complement busy and overburdened psychiatrists, and add an important dimension of holistic care.
This article reviews issues related to a successful psychiatrist-PMHNP collaboration, including:
- PMHNP’s training and scope of practice
- their skill and competency development in inpatient and outpatient settings
- the principles and dynamics of collaboration, hindrances to cooperation, and keys to relationship-building for PMHNPs and psychiatrists.
Rigorous requirements
PMHNPs enroll in an accredited graduate nursing program that takes 16 to 24 months to complete and builds on the competencies of their undergraduate nursing education and clinical experience. All programs meet standards set by national nursing accrediting agencies. The typical graduate-level curriculum for a PMHNP includes core bio-behavioral theory, research courses, advanced physiology and pathophysiology, advanced physical and psychiatric health assessment, pharmacologic and nonpharmacologic interventions, and managing health care delivery systems. For graduation and certification, PMHNPs must complete 500 supervised clinical hours focused on psychiatric and mental health care.
- comprehensive psychiatric evaluation
- formulation of a differential diagnosis
- ordering and interpreting diagnostic tests
- prescribing pharmacologic agents
- conducting individual, couple, group, or family psychotherapy using evidence-based approaches.
PMHNPs also are responsible for recognizing the limits of their knowledge and experience, planning for situations beyond their expertise, and providing appropriate referral to other health care providers when indicated.8
Successful collaborative practice requires a clear definition and understanding of roles.9 This is particularly important for collaborating psychiatrists and PMHNPs because there has been confusion among physicians and the general public related to the nurse practitioner’s role. Psychiatrists who work with PMHNPs need to be familiar with state regulations that govern levels of physician supervision and prescriptive authority for nurse practitioners. Eleven states and the District of Columbia allow nurse practitioners to prescribe independently, including controlled substances. Most states require physician collaboration for prescribing medications, but the language can be ambiguous, with restrictions on certain formularies or drug schedules—eg, Michigan nurse practitioners may prescribe schedule II through V controlled substances, but schedule II medications are limited to nurse practitioners who work in hospitals, surgical outpatient settings, or hospices.10
Competencies and development
New PMHNPs see patients and prescribe medication, but their work needs close supervision. Postgraduate clinical experience combined with supervision gradually allows the PMHNP greater independence. A PMHNP who provides care in a busy outpatient clinic, inpatient unit, or psychiatric emergency department is likely to master the treatment philosophy and ancillary competencies related to that particular clinical site—including favored pharmacologic approaches, electronic documentation and ordering functions, and admission and discharge facilitation—at a level exceeding that of psychiatric residents, who rotate on and off a service as part of their training.
It’s helpful for new PMHNPs to have a time frame for their development over several years. The Table11 outlines general graded competency areas PMHNPs may focus on in their development. See this article at CurrentPsychiatry.com for Tables that provide examples of detailed competencies for third-year PMHNPs in inpatient and outpatient settings.
Table
PMHNP development: General graded competency areas
| Psychiatric evaluation and diagnosis |
| Psychiatric treatments, including medications and psychotherapies |
| Maintenance of the therapeutic alliance, including monitoring the PMHNP’s emotional responses to patients |
| Participation in an interdisciplinary team |
| Understanding comorbid medical conditions, integrating laboratory and other tests into the treatment plan, and recognizing the need for consultation with the medical team |
| Documentation, such as initial evaluations, progress notes, and discharge summaries |
| Assessment for suicide and violence potential |
| Teaching |
| Patient and family psychoeducation |
| Use of feedback and supervision |
| PMHNP: psychiatric-mental health nurse practitioner Source: Reference 11 |
Table 1
Competencies for third-year PMHNPs in an outpatient clinic
| Recognize clinical presentations of complex psychiatric disorders, variants, and comorbidities |
| Firm knowledge of diagnostic criteria, and skills for independent comprehensive assessment and diagnosis |
| Firm knowledge of evidence-based outpatient treatments for disorders, with mastery of ≥1 nonpharmacologic modality in addition to prescribing and managing medications |
| Use and provide feedback in comprehensive case formulations and treatment plans |
| Assist in clinical education of trainees in psychiatric nursing, social work, psychiatric residency, and psychology |
| Participate and collaborate in educational events and initiatives |
| Knowledge of internal and external health system and resources, and facilitating patient access to these networks |
| Incorporate mental health and behavioral and psychiatric nursing research into patient care |
| PMHNP: psychiatric-mental health nurse practitioner |
Competencies for third-year PMHNPs on an inpatient psychiatric unit
| Refinement of assessment section in evaluations, progress notes, and discharge summaries |
| Understanding indications for neuropsychological testing, and integrating findings into the treatment plan |
| Assessment of readiness for discharge in patients with a history of suicidality or violence |
| Developing a sophisticated and detailed discharge or follow-up plan |
| Understanding treatment resistance in mood and psychotic disorders, and implementing treatment |
| More detailed knowledge of types of illness treated on an inpatient unit |
| Ability to orient and train PMHNPs and other inpatient unit trainees |
| Ability to gather and use articles and other literature pertaining to inpatient care |
| Increasing competence in short-term, crisis-based therapeutic techniques, including familiarity with DBT, CBT, and IPT |
| Understanding family systems and impact on patient care |
| CBT: cognitive-behavioral therapy; DBT: dialectical behavior therapy; IPT: interpersonal therapy; PMHNP: psychiatric-mental health nurse practitioner |
Principles of practice
Studies have demonstrated the importance of understanding how to effectively implement collaborative care across medical disciplines.12 See the Box12 for a discussion of 3 key determinants for successful clinical collaborations.
San Martín-Rodríguez et al12 recognized 3 key factors that may help develop successful collaborative clinical relationships.
Interactional factors include a mutual willingness to collaborate, a commitment to collaborate, a belief in the benefits of collaborating, and sharing common objectives. Trust in the partnering clinician’s competency contributes to a successful collaboration. Strong communication skills—including the ability to convey what each clinician can contribute to achieving goals—also strengthens collaboration. Learning and understanding skills in conflict management and dialogue are key. Mutual respect also is essential.
Organizational factors include a shift from a traditional hierarchical structure to a more horizontal structure, and a work climate that supports openness, risk taking—ie, a willingness to disagree with a colleague if it is in a patient’s best interest or to develop a new and innovative method of providing care—integrity, and trust. Administrative structures and supports that convey the importance of collaboration also are key components of a strong collaborative environment. Teamwork and shared decision-making are important elements; teamwork should include time to discuss patient issues and develop strong interpersonal relationships. A commitment to professional development is another key factor.
Systemic factors include a social system that supports collegial relationships and professionalism that respects and accepts other professions. This includes decreased focus on protecting professional territory and increased recognition of overlaps among professions.
Enhancing collaboration
Psychiatrists who work with PMHNPs develop trust based on observing each PMHNP’s work, including their relationship with patients, ability to conceptualize a case and develop a treatment plan, and the skill with which they function within a team. The psychiatrist’s comfort level also is related to his or her awareness of the comprehensiveness of the PMHNP’s training and the competencies gained from clinical experience. Respect for the PMHNP’s educational and professional background is the foundation for what is often—at least in the collaborative relationship’s initial stages—a combined cooperative and supervisory relationship with the PMHNP. As such, the PMHNP gradually will absorb certain “intangibles” to supplement the training and work experiences that preceded his or her position. This may include assimilating the psychiatrist’s or clinic’s philosophy and treatment practice, including expertise in dealing with specialized psychiatric populations (eg, developmental disabilities, acute psychosis, or treatment-resistant depression).
The patient’s comfort level
Collaborating PMHNPs and psychiatrists need to be prepared for a patient who expresses disappointment with being treated by a PMHNP or a preference to see “a doctor.” Psychiatrists who have not worked through their own ambivalence about the collaboration or who lack confidence in the PMHNP’s abilities may find themselves consciously or unconsciously aligning with the patient’s stance. They may neglect to explore the basis and meaning of the patient’s preference, which may be related to the patient’s lack of knowledge about the PMHNP’s role and training. The PMHNP who encounters such a patient has a more challenging task—namely, how to calmly address the patient’s concern while the patient is challenging the PMHNP’s competence. Both the PMHNP and psychiatrist need to be alert to the possibility of “splitting” in the treatment of axis II-disordered patients.
Barriers to collaboration
From the PMHNP perspective, barriers to a collaborative relationship include referring to PMHNPs by a less preferred term or title, instead of a nurse practitioner or APN, which can hinder the relationship. Although physician assistants and NPs have been grouped together under the term “mid-level providers,” the American Academy of Nurse Practitioners notes that this term suggests a lower level of care or service is being provided.18 “Physician extender” is another term that fails to recognize the PMHNP’s separate and unique role and the PMHNP’s view of their role as complementary to medicine, rather than an extension of a physician’s practice.
Territorial issues can impede collaborative relationships. Psychiatrists who resist collaborating will be less effective than those who welcome a PMHNP and readily delegate specific tasks and portions of the workload, whereas psychiatrists who value the help will be more likely to build a collaborative partnership, leading to better patient care.
Autonomy is a critical determinant of professional satisfaction for PMHNPs. A PMHNP’s autonomy can be impeded by organizational constraints and physician perceptions.19 PMHNPs require autonomy to self-direct patient diagnosis and treatment within the scope of their practice, and many find this relative independence essential to delivering high quality patient care. Lack of autonomy can lead to breaks in workflow in the outpatient setting and increased length of stay for hospitalized patients. In addition, an autonomously functioning, experienced PMHNP can increase efficiency in hospital settings where psychiatrists can be in short supply, preoccupied with administrative matters, or require help on weekends.
Related Resources
- American Psychiatric Nurses Association. www.apna.org.
- International Society of Psychiatric-Mental Health Nurses. www.ispn-psych.org.
- American Nurses Association. www.nursingworld.org.
Dr. Casher is a speaker for Sunovion Pharmaceuticals and receives royalties from Cambridge University Press.
Ms. Kuebler, Ms. Bastida, and Ms. Chipps report no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
1. Sataline S, Wang SS. Medical schools can’t keep up. Wall Street Journal. April 12 2010. http://online.wsj.com/article/SB10001424052702304506904575180331528424238.html. Accessed August 21, 2012.
2. U.S. Department of Health and Human Services. The health care law & you. http://www.healthcare.gov/law/index.html. Accessed August 21, 2012.
3. Wand T, Fisher J. The mental health nurse practitioner in the emergency department: an Australian experience. Int J Ment Health Nurs. 2006;15(3):201-208.
4. Eisch JS, Brozovic B, Colling K, et al. Nurse practitioner geropsychiatric consultation service to nursing homes. Geriatr Nurs. 2000;21(3):150-155.
5. Baker N. Exploring the mental health nurse practitioner scope of practice in youth early psychosis: an anecdotal account. Contemp Nurse. 2010;34(2):211-220.
6. International Society of Psychiatric-Mental Health Nurses. Psychiatric mental health nursing scope & standards. http://www.ispn-psych.org/docs/standards/scope-standards-draft.pdf. Updated 2006. Accessed August 21, 2012.
7. Centers for Medicare and Medicaid Services. HHS finalizes new rules to cut regulations for hospitals and health care providers saving more than $5 billion. http://www.cms.gov/apps/media/press/release.asp?Counter=4362. Published May 9, 2012. Accessed August 21, 2012.
8. APRN Consensus Work Group, National Council of State Boards of Nursing APRN Advisory Committee. Consensus model for regulation: licensure accreditation, certification & education. https://www.ncsbn.org/Consensus_Model_for_APRN_Regulation_July_2008.pdf. Published July 7, 2008. Accessed August 21, 2012.
9. Legault F, Humbert J, Amos S, et al. Difficulties encountered in collaborative care: logistics trumps desire. J Am Board Fam Med. 2012;25(2):168-176.
10. Michigan Council of Nurse Practitioners. Michigan’s rules and regulations for prescriptive authority. http://micnp.org/displaycommon.cfm?an=1&subarticlenbr=109. Accessed August 21, 2012.
11. Wheeler K, Haber J. Development of psychiatric-mental health nurse practitioner competencies: opportunities for the 21st century. J Am Psychiatr Nurses Assoc. 2004;10(3):129-138.
12. San Martín-Rodríguez L, Beaulieu MD, D’Amour D, et al. The determinants of successful collaboration: a review of theoretical and empirical studies. J Interprof Care. 2005;19(suppl 1):132-147.
13. Suter E, Arndt J, Arthur N, et al. Role understanding and effective communication as core competencies for collaborative practice. J Interprof Care. 2009;23(1):41-51.
14. Horrocks S, Anderson E, Salisbury C. Systematic review of whether nurse practitioners working in primary care can provide equivalent care to doctors. BMJ. 2002;324(7341):819-823.
15. Byrne G, Richardson M, Brunsdon J, et al. Patient satisfaction with emergency nurse practitioners in A & E. J Clin Nurs. 2000;9(1):83-92.
16. McCann TV, Clark E. Attitudes of patients towards mental health nurse prescribing of antipsychotic agents. Int J Nurs Pract. 2008;14(2):115-121.
17. Wortans J, Happell B, Johnstone H. The role of the nurse practitioner in psychiatric/mental health nursing: exploring consumer satisfaction. J Psychiatr Ment Health Nurs. 2006;13(1):78-84.
18. Frellick M. The nurse practitioner will see you now. Advanced practice providers fill the physician gap. Hosp Health Netw. 2011;85(7):44-46, 48–49.
19. Maylone MM, Ranieri L, Quinn Griffin MT, et al. Collaboration and autonomy: perceptions among nurse practitioners. J Am Acad Nurse Pract. 2011;23(1):51-57.
1. Sataline S, Wang SS. Medical schools can’t keep up. Wall Street Journal. April 12 2010. http://online.wsj.com/article/SB10001424052702304506904575180331528424238.html. Accessed August 21, 2012.
2. U.S. Department of Health and Human Services. The health care law & you. http://www.healthcare.gov/law/index.html. Accessed August 21, 2012.
3. Wand T, Fisher J. The mental health nurse practitioner in the emergency department: an Australian experience. Int J Ment Health Nurs. 2006;15(3):201-208.
4. Eisch JS, Brozovic B, Colling K, et al. Nurse practitioner geropsychiatric consultation service to nursing homes. Geriatr Nurs. 2000;21(3):150-155.
5. Baker N. Exploring the mental health nurse practitioner scope of practice in youth early psychosis: an anecdotal account. Contemp Nurse. 2010;34(2):211-220.
6. International Society of Psychiatric-Mental Health Nurses. Psychiatric mental health nursing scope & standards. http://www.ispn-psych.org/docs/standards/scope-standards-draft.pdf. Updated 2006. Accessed August 21, 2012.
7. Centers for Medicare and Medicaid Services. HHS finalizes new rules to cut regulations for hospitals and health care providers saving more than $5 billion. http://www.cms.gov/apps/media/press/release.asp?Counter=4362. Published May 9, 2012. Accessed August 21, 2012.
8. APRN Consensus Work Group, National Council of State Boards of Nursing APRN Advisory Committee. Consensus model for regulation: licensure accreditation, certification & education. https://www.ncsbn.org/Consensus_Model_for_APRN_Regulation_July_2008.pdf. Published July 7, 2008. Accessed August 21, 2012.
9. Legault F, Humbert J, Amos S, et al. Difficulties encountered in collaborative care: logistics trumps desire. J Am Board Fam Med. 2012;25(2):168-176.
10. Michigan Council of Nurse Practitioners. Michigan’s rules and regulations for prescriptive authority. http://micnp.org/displaycommon.cfm?an=1&subarticlenbr=109. Accessed August 21, 2012.
11. Wheeler K, Haber J. Development of psychiatric-mental health nurse practitioner competencies: opportunities for the 21st century. J Am Psychiatr Nurses Assoc. 2004;10(3):129-138.
12. San Martín-Rodríguez L, Beaulieu MD, D’Amour D, et al. The determinants of successful collaboration: a review of theoretical and empirical studies. J Interprof Care. 2005;19(suppl 1):132-147.
13. Suter E, Arndt J, Arthur N, et al. Role understanding and effective communication as core competencies for collaborative practice. J Interprof Care. 2009;23(1):41-51.
14. Horrocks S, Anderson E, Salisbury C. Systematic review of whether nurse practitioners working in primary care can provide equivalent care to doctors. BMJ. 2002;324(7341):819-823.
15. Byrne G, Richardson M, Brunsdon J, et al. Patient satisfaction with emergency nurse practitioners in A & E. J Clin Nurs. 2000;9(1):83-92.
16. McCann TV, Clark E. Attitudes of patients towards mental health nurse prescribing of antipsychotic agents. Int J Nurs Pract. 2008;14(2):115-121.
17. Wortans J, Happell B, Johnstone H. The role of the nurse practitioner in psychiatric/mental health nursing: exploring consumer satisfaction. J Psychiatr Ment Health Nurs. 2006;13(1):78-84.
18. Frellick M. The nurse practitioner will see you now. Advanced practice providers fill the physician gap. Hosp Health Netw. 2011;85(7):44-46, 48–49.
19. Maylone MM, Ranieri L, Quinn Griffin MT, et al. Collaboration and autonomy: perceptions among nurse practitioners. J Am Acad Nurse Pract. 2011;23(1):51-57.
Benzodiazepines: A versatile clinical tool
How to prevent adverse drug events
Medication errors due to system-, provider-, or patient-related factors contribute significantly to increased costs, adverse drug events (ADEs), and morbidity and mortality.1 One study found >60% of ADEs that led to hospitalization could have been prevented by strategies such as adequate monitoring or appropriate prescribing.2 Psychiatrists have an opportunity to reduce rates of ADEs; however, the possibility of disease symptoms overlapping with these adverse events is 1 of many obstacles prescribing clinicians face.1 Prescribers also must contend with adverse effects of polypharmacy, which are common among psychiatric patients. Patient-related factors of concern include:
- seeing multiple prescribers
- medication nonadherence
- failure to communicate use of herbal or over-the-counter products
- lack of insight
- comorbid medical and psychiatric diagnoses, such as dementia.1
This article highlights potential ADEs and major medication safety concerns that may contribute to morbidity and mortality among patients taking psychotropics. Although many factors are beyond the prescribing clinician’s control—such as medication dispensing and administration errors—psychiatrists can substantially reduce ADEs. We will cover potential adverse events associated with key medications or medication classes, drug interactions with potentially devastating consequences, and strategies to minimize risks of ADEs, including enhanced awareness and monitoring (Table 1).
Table 1
How to avoid ADEs with psychotropics
| Establish a collaborative practice among physicians, pharmacists, nurses, and social workers to enhance patient care and reduce the risk of medication errors and negative outcomes |
| Educate patients to increase their understanding of psychiatric diseases and medications and increase compliance with therapy. This may lead the patient to self-monitor drug efficacy and adverse effects |
| Be aware of psychotropic medications’ ‘black-box’ warnings that guide their safe use |
| Pay particular attention to drugs with a narrow therapeutic index, such as lithium and tricyclic antidepressants, which have small safety margins and are lethal in overdose |
| Avoid using 1 drug to treat the side effects of another. Minimizing polypharmacy can reduce medication errors, DDIs, and ADEs |
| Remain vigilant for DDIs, which can be serious and life-threatening. Examples include sudden cardiac death from additive QTc prolongation effects and NMS. Early detection of NMS and discontinuing the offending agent(s) can help prevent patient morbidity and mortality |
| Stay up-to-date on literature and drug warnings to employ best practices and avoid potentially serious adverse and/or lethal outcomes |
| Encourage patients to disclose any prescription drugs, over-the-counter medications, and herbal therapies they are taking |
| Develop strategies to prevent ADEs, such as personal formularies, suicide assessments, prescribing limited quantities, ‘eyes on’ medication administration, therapeutic drug monitoring, utilizing databases and resources for drug information, and patient education |
| ADEs: adverse drug events; DDIs: drug-drug interactions; NMS: neuroleptic malignant syndrome |
Prescription drug overdose
Each year, unintentional drug overdoses account for >20,000 deaths in the United States.3 Prescription medications, particularly opioid analgesics, have contributed to the doubling of overdose mortality rates in recent years. A recent study reported that nearly 50% of unintentional drug overdose deaths were associated with psychotropics and one-third of these deaths were associated with benzodiazepines, many of which were not prescribed to the individual.4
The risk of mortality from intentional drug overdose also must be assessed. Tricyclic antidepressants (TCAs) are a particularly lethal class of medications in suicide attempts and may result in arrhythmias, coma, seizures, respiratory failure, and death.5 Venlafaxine and mirtazapine are associated with greater risk of death and toxicity in overdose, respectively, than selective serotonin reuptake inhibitors (SSRIs).6 Lithium toxicity in overdose may lead to bradycardia, seizure, coma, hyperventilation, serotonin syndrome, respiratory failure, or death.5 The risk of death with lithium or benzodiazepine monotherapy is low when these agents are taken as prescribed. However, prescribers must exercise caution when these agents are used in combination. Interactions involving drugs with a narrow therapeutic index—such as lithium and TCAs—are more likely to be clinically significant because small increases in drug concentration can lead to serious adverse effects or death. See Related Resources for a review article on appropriate use and monitoring of lithium.
Drug-drug interactions
Many Americans take multiple prescription and nonprescription drugs, and psychiatric patients are more likely than other individuals to have more complex medication regimens.7 This can result in polypharmacy and drug-drug interactions (DDIs), which can lead to undesired medication effects and serious, potentially fatal ADEs.
Pharmacokinetic interactions typically affect drug concentrations and occur when 1 drug interferes with the absorption, distribution, metabolism, or excretion of another drug. Many common pharmacokinetic interactions involve the liver cytochrome P450 (CYP) system, which is responsible for metabolizing many medications.8 DDIs can occur when CYP enzymes are modified by inhibitors or inducers, which can decrease or increase drug clearance, respectively. Table 2 5,7,9 provides examples of common CYP450 substrates, inhibitors, and inducers. Polymorphisms in the pharmacogenetics of CYP450 also can affect overall drug clearance and the impact of DDIs.8
Pharmacodynamic interactions are caused by additive or competing effects of multiple drugs. The most serious of these involve medications that increase a patient’s risk of serotonin syndrome or neuroleptic malignant syndrome (NMS); both are medical emergencies that require immediate hospitalization.
Although any medication with serotonergic activity can induce serotonin syndrome, combinations of serotonergic drugs in particular are associated with increased risk.10 Serotonin syndrome is characterized by hyperthermia, altered muscle tone, altered mental status, and autonomic instability; rhabdomyolysis and disseminated intravascular coagulation are potential lethal complications.10 A high index of suspicion can help clinicians rapidly detect serotonin syndrome, discontinue offending agents, and initiate supportive treatments.
NMS is a life-threatening complication of antipsychotics characterized by fever, delirium, muscle rigidity, autonomic instability, and abnormal laboratory findings that include elevated white blood count and increased creatinine kinase from muscle injury. In early stages, NMS may be mistaken for extrapyramidal symptoms. Although NMS can occur with any antipsychotic as monotherapy, additive antidopaminergic effects increase the risk. Patients with a compromised CNS as a result of mental retardation, traumatic brain injury, or metabolic abnormalities also are at increased risk of developing NMS.11
Other pharmacodynamic interactions involve medications that may have additive effects on prolonging QTc intervals. For example, TCAs are pro-arrhythmic and have quinidine-like effects, which can cause cardiac conduction abnormalities and prolonged PR and QTc intervals.12 Employ routine ECG monitoring when prescribing multiple medications known to cause QTc prolongation, such as TCAs (Table 3).13,14 The Arizona Center for Education and Research on Therapeutics (www.azcert.org) provides a searchable list of QT-prolonging drugs (see Related Resources).
Medications also can interact with food, disease states, and herbal supplements. Alcohol interacts with many CNS-active medications, including many psychotropics. Patients taking benzodiazepines may experience oversedation and respiratory depression from alcohol’s additive sedating effects.5 Advise patients to limit their alcohol intake while taking CNS-depressing psychotropics such as benzodiazepines, antipsychotics, and some antidepressants. Monoamine oxidase inhibitors (MAOIs) and tyramine-containing food—such as cheese, beer, preserved meat, and soy sauce—can lead to a dangerous hypertensive crisis that requires immediate medical intervention to prevent life-threatening complications.5 Hypertensive crisis may be more significant in patients who have pre-existing hypertension. Finally, herbal supplements also can interact with medications. Patients who take St. John’s wort for depressive symptoms might not realize that it can reduce the efficacy of other drugs or increase their risk of serotonin syndrome.9
Table 2
Cytochrome P450 substrates, inhibitors, and inducers
| 3A4 | 2D6 | 2C9 | 2C19 | 1A2 | |
|---|---|---|---|---|---|
| Substrates | Carbamazepine Citalopram Fluoxetine Haloperidol Mirtazapine Oxcarbazepine Quetiapine Sertraline Ziprasidone | Aripiprazole Citalopram Duloxetine Fluoxetine Haloperidol Mirtazapine Paroxetine Risperidone Sertraline Venlafaxine TCAs | Amitriptyline Carbamazepine Sertraline Valproic acid | Citalopram Clomipramine Sertraline Valproic acid | Carbamazepine Clozapine Olanzapine |
| Inhibitors | Amiodarone Aprepitant Azole antifungals Carbamazepine Cimetidine Diltiazem Erythromycin Fluoxetine (norfloxetine) Grapefruit juice Imatinib Paroxetine Ritonavir Sertraline Verapamil | Amiodarone Bupropion Cimetidine Duloxetine Fluoxetine Methadone Paroxetine Ritonavir Sertraline | Amiodarone Fluconazole Isoniazid Sertraline Trimethoprim-sulfamethoxazole Valproic acid | Cimetidine Fluoxetine Ketoconazole Omeprazole Sertraline Valproic acid | Amiodarone Cimetidine Fluoroquinolones |
| Inducers | Carbamazepine Phenobarbital Phenytoin Rifampin St. John’s wort | Rifampin | Phenobarbital Rifampin | Carbamazepine Rifampin | Nafcillin Phenobarbital Rifampin Smoking |
| TCAs: tricyclic antidepressants Source: References 5,7,9 | |||||
Table 3
Psychotropics associated with QT prolongation
| Class | Agents |
|---|---|
| Antidepressants | Mirtazapine, SNRIs (desvenlafaxine, venlafaxine), SSRIs (citalopram, fluoxetine, paroxetine, sertraline), TCAs (amitriptyline, clomipramine, desipramine, doxepin, imipramine, protriptyline, trimipramine), trazodone |
| Typical antipsychotics | Chlorpromazine, fluphenazine, haloperidol, perphenazine, thioridazine, trifluoperazine |
| Atypical antipsychotics | Aripiprazole, asenapine, clozapine, iloperidone, paliperidone, quetiapine, risperidone, ziprasidone |
| Mood stabilizers | Lithium |
| Miscellaneous agents | Amantadine, atomoxetine, chloral hydrate, diphenhydramine, galantamine |
| Stimulants | Amphetamine/dextroamphetamine products, methylphenidate/dexmethylphenidate |
| SNRIs: serotonin-norepinephrine reuptake inhibitors; SSRIs: selective serotonin reuptake inhibitors; TCAs: tricyclic antidepressants Source: Adapted from references 13,14 | |
“Black-box” warnings issued by the FDA are included in the package insert to highlight a medication’s risks of dangerous and potentially lethal adverse effects. Table 4 highlights current black-box warnings for various psychotropics.5,14-16
Antidepressants and suicide. All medications with antidepressant indications carry a black-box warning for risk of suicidal ideation and behavior in children, adolescents, and young adults during the early months of medication therapy. This includes not only SSRIs and serotonin-norepinephrine reuptake inhibitors, but also anticonvulsants and atypical antipsychotics indicated for treating mood disorders. Monitor young patients carefully and advise family members to alert clinicians of any signs of suicidality or unusual behavior.
Lamotrigine and aseptic meningitis. Aseptic meningitis—inflammation of the meninges that is not caused by bacteria—is a rare but serious adverse effect of lamotrigine. Symptoms include headache, fever, stiff neck, nausea and vomiting, delirium, rash, and sensitivity to light.5 Forty cases of aseptic meningitis in children and adults were reported over 15 years, representing <.01% of all lamotrigine prescriptions.5 Most of these patients required hospitalization, but symptoms resolved after lamotrigine was discontinued. Prompt identification and management of aseptic meningitis are necessary to prevent permanent brain damage and death. Other complications of aseptic meningitis include long-term neurologic sequelae such as cognitive impairment, seizure disorders, and behavioral disturbances.
Table 4
Which psychotropics carry ‘black-box’ warnings?
| Warning | Class or medication affected | Comments |
|---|---|---|
| Suicidality | Antidepressants Antipsychotics indicated for mood disorders Anticonvulsants | See ‘Black-box warnings’ |
| Serious, life-threatening rashes such as Stevens-Johnson syndrome or toxic epidermal necrolysis | Lamotrigine Carbamazepine | Lamotrigine’s risk of severe dermatologic reactions necessitates slow titration during drug initiation Carbamazepine warning includes a recommendation for genetic screening in Asian patients because Stevens-Johnson syndrome is associated with the HLA-B*1502 allele found primarily in the Asian population |
| Increased mortality in elderly patients with dementia-related psychosis | Antipsychotics | A study of >10,000 geriatric patients with dementia showed mortality rates of 22.6% to 29.1% among those who took antipsychotics compared with 14.6% for patients taking other psychiatric medications. When antipsychotics are used in older adults, well-documented informed consent from the patient or substitute decision-maker is required |
| Other effects | Clozapine | Agranulocytosis occurs in 1% to 2% of clozapine patients, necessitating WBC/ANC monitoring Clozapine-induced myocarditis, generally accompanied by peripheral eosinophilia, usually occurs within the first 2 months of treatment, and can result in significant mortality from resultant cardiomyopathy. Early warning signs of fever, fatigue, and tachycardia are easily mistaken for the more benign effects of clozapine titration Seizures are more likely with higher doses. Cautious use is advised with patients who have an underlying seizure disorder Other cardiovascular and respiratory effects: Hypotension has been associated with rapid initial titration. Cardiac and respiratory arrest and circulatory collapse have occurred rarely. Respiratory complications are more likely when clozapine is used in combination with benzodiazepines |
| ANC: absolute neutrophil count; WBC: white blood cell Source: References 5,14-16 | ||
Other complications
Hematologic effects. All classes of psychotropics carry a risk (1 to 2 cases per year per 100,00 patients) of serious hematologic complications, including neutropenia, agranulocytosis, eosinophilia, thrombocytopenia, purpura, and anemia.17 Agranulocytosis has been associated most commonly with clozapine, carbamazepine, and typical antipsychotics.17 SSRIs, which are widely prescribed, are associated with increased risk of bruising and bleeding. Patients with bleeding or platelet disorders are at an increased risk for these complications.17
Seizures. Several classes of psychotropics are associated with an increased risk of seizures. Among antipsychotics, clozapine and chlorpromazine are the most seizurogenic.18 Among antidepressants, bupropion and clomipramine are most likely to lower seizure thresholds.18 Psychotropics’ seizure-inducing effects are dose-related. Vulnerability to seizures while taking psychotropics is related to having a history of epilepsy or brain injury.18 Seizures also can occur when benzodiazepines or anticonvulsants are withdrawn too quickly.
Heat stroke. Although a rare occurrence, psychotropics with anticholinergic side effects can contribute to heat stroke. Older patients are particularly vulnerable to the risk of body temperature dysregulation.19
Ketoacidosis and hyperosmolar coma. Medication-related deaths have occurred as a result of ketoacidosis and hyperosmolar coma associated with atypical antipsychotics. These hyperglycemia-related fatalities are most likely with clozapine and olanzapine.20
Hip fractures and falls. Geriatric patients are vulnerable to falls and resultant hip fractures related to use of TCAs, SSRIs, benzodiazepines, and antipsychotics. This is not a trivial matter; hip fractures increase the mortality rate by 12% to 20% in the year after the injury.21 The risk of falls is related to sedation, orthostatic hypotension, arrhythmias, and confusion associated with psychotropics.21,22
Akathisia and suicide. Unrecognized or undertreated akathisia is most commonly associated with antipsychotics, but also can occur with SSRIs. Although akathisia is commonly thought of as a motor syndrome of restlessness, patients may find the less-recognized psychic symptoms of increased inner turmoil and hallucinations just as distressing. This complex of symptoms is associated with an increased risk of suicide.23 If discontinuing the offending agent is not feasible, akathisia can be treated with beta blockers, benzodiazepines, or anticholinergics.24
Hepatotoxicity. Hepatotoxicity from psychotropics occurs in only a small percentage of patients, and can range from transient elevations in liver enzymes to fulminant liver failure. Adverse hepatic effects may be a manifestation of a hypersensitivity reaction accompanied by rash and eosinophilia.25 MAOIs and TCAs can cause cholestatic liver injury, whereas nefazodone has been associated with fulminant liver failure. Other psychotropics—including SSRIs, antipsychotics, benzodiazepines, and older antiepileptics—can cause negative hepatic effects but rarely are associated with acute liver failure.25,26 Although few medications can cause complete liver failure on their own, hepatotoxicity from medications may precipitate severe, potentially fatal outcomes in patients with underlying liver diseases such as hepatitis and cirrhosis. Additive hepatotoxicity from multiple medications also can be problematic. Although psychotropic-induced hepatotoxicity is rare, assess psychotropic doses in patients with liver dysfunction, because drug clearance may be altered, which increases the risk for other serious adverse events.25
Suicide assessment is key
Ongoing monitoring for current or developing suicidal ideation is an important strategy to prevent medication-related mortality in patients vulnerable to self-harm. Initial assessments and follow-up appointments should include a detailed inquiry about suicidal ideations, plans, and behaviors. Patients taking medications that carry black-box warnings for suicide risk should be seen frequently during the first few months of treatment. Patients receiving medications that are lethal in overdose (eg, lithium and TCAs) should be carefully screened for suicide risk. Prescribe medications in limited quantities or arrange for a family member to monitor the patient if necessary. Patients with a history of suicide attempts and current suicide plans may require close observation and initiating medications while hospitalized.
Other prevention strategies
Prescribing psychotropics in a manner that promotes mental well being while minimizing negative outcomes can be challenging. By developing a personal formulary of drugs commonly encountered and prescribed in their practice, psychiatrists can increase their awareness of serious safety concerns, potential DDIs, and appropriate use based on available literature.7,27
Medication histories and drug reconciliation—comparing a patient’s medication orders to all of the medications the patient has been taking—can help clinicians avoid making inappropriate dose adjustments, duplicating therapy, or prescribing medications patients previously have failed or did not tolerate. Establishing a collaborative practice environment with physicians, pharmacists, nurses, and social workers can minimize medication errors and risk of adverse outcomes by increasing communication regarding the patient’s treatment.7
Computerized drug databases and other electronic resources and consultation with pharmacists can help prescribers identify, avoid, and manage clinically significant DDIs.27 Medications could interact with other drugs as long as their effects persist in the body, which could be days to months after the drug is discontinued. Future research may lead to tools to identify patient pharmacogenetic profiles.
Recognizing psychotropic DDIs and adverse effects remains a challenge because of the complexity of the affected organ, the brain. Clinicians should be vigilant to changes in a patient’s presentation because they may be a manifestation of a medication side effect.7 Appropriate therapeutic drug monitoring should occur on a routine, scheduled basis. Closer monitoring may be necessary with dose changes, potential DDIs, signs and symptoms of toxicity/efficacy failure, and renal or hepatic function changes.
Lastly, patients’ education and involvement in their health care may increase their awareness, responsibility, and medication adherence. For challenging patients, family involvement and “eyes on” medication administration can increase adherence and prevent psychotropic misuse.
- Arizona Center for Education and Research on Therapeutics. Drugs that prolong the QT interval and/or induce Torsades de Pointes ventricular arrhythmia. www.azcert.org/medical-pros/drug-lists/drug-lists.cfm.
- Cates ME, Sims PJ. Therapeutic drug management of lithium. Am J Pharm Educ. 2005;69(5):88.
- Wren P, Frizzell LA, Keltner NL, et al. Three potentially fatal adverse effects of psychotropic medications. Perspect Psychiatr Care. 2003;39(2):75-81.
- Bishop JR, Bishop DL. How to prevent serotonin syndrome from drug-drug interactions. Current Psychiatry. 2011;10(3):81-83.
Drug Brand Names
- Amantadine • Symmetrel
- Amiodarone • Cordarone, Pacerone
- Amitriptyline • Elavil
- Amphetamine/dextroamphetamine • Adderall, others
- Aprepitant • Emend
- Aripiprazole • Abilify
- Asenapine • Saphris
- Atomoxetine • Strattera
- Bupropion • Wellbutrin, Zyban
- Carbamazepine • Tegretol, others
- Chloral hydrate • Somnote
- Chlorpromazine • Thorazine
- Cimetidine • Tagamet
- Citalopram • Celexa
- Clomipramine • Anafranil
- Clozapine • Clozaril
- Desipramine • Norpramin
- Desvenlafaxine • Pristiq
- Diltiazem • Cardia, others
- Diphenhydramine • Benadryl, others
- Doxepin • Sinequan, Silenor
- Duloxetine • Cymbalta
- Erythromycin • Ery-Tab, others
- Fluconazole • Diflucan
- Fluoxetine • Prozac
- Fluphenazine • Prolixin
- Galantamine • Razadyne
- Haloperidol • Haldol
- Iloperidone • Fanapt
- Imatinib • Gleevec
- Imipramine • Tofranil
- Isoniazid • Nydrazid, others
- Ketoconazole • Nizoral, others
- Lamotrigine • Lamictal
- Lithium • Eskalith, others
- Methadone • Dolophine, Methadose
- Methylphenidate/ dexmethylphenidate • Ritalin, others
- Mirtazapine • Remeron
- Nafcillin • Nafcil, others
- Nefazodone • Serzone
- Olanzapine • Zyprexa
- Omeprazole • Prilosec
- Oxcarbazepine • Trileptal
- Paliperidone • Invega
- Paroxetine • Paxil
- Perphenazine • Trilafon
- Phenobarbital • Luminal, others
- Phenytoin • Dilantin
- Protriptyline • Vivactil
- Quetiapine • Seroquel
- Rifampin • Rifadin, others
- Risperidone • Risperdal
- Ritonavir • Norvir
- Sertraline • Zoloft
- Thioridazine • Mellaril
- Trazodone • Desyrel, Oleptro
- Trifluoperazine • Stelazine
- Trimethoprim/Sulfamethoxazole • Bactrim, Septra
- Trimipramine • Surmontil
- Valproic acid • Depakote, others
- Venlafaxine • Effexor
- Verapamil • Calan, others
- Ziprasidone • Geodon
Disclosure
Drs. Yu and Bostwick report no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
Dr. Casher is a speaker for AstraZeneca, Pfizer Inc, and Sunovion Pharmaceuticals.
1. Procyshyn RM, Barr AM, Brickell T, et al. Medication errors in psychiatry: a comprehensive review. CNS Drugs. 2004;24(7):595-609.
2. McDonnell PJ, Jacobs MR. Hospital admissions resulting from preventable adverse drug reactions. Ann Pharmacother. 2002;36(9):1331-1336.
3. Centers for Disease Control and Prevention. Prescription drug overdose: state health agencies respond. 2008. Available at: http://www.cdc.gov/HomeandRecreationalSafety/pubs/RXReport_web-a.pdf. Accessed February 15 2011.
4. Toblin RL, Paulozzi LJ, Logan JE, et al. Mental illness and psychotropic drug use among prescription drug overdose deaths: a medical examiner chart review. J Clin Psychiatry. 2010;71(4):491-496.
5. Micromedex Healthcare Series (electronic version). 2011. Available at: http://www.micromedex.com. Accessed February 15 2011.
6. Hawton K, Bergen H, Simkin S, et al. Toxicity of antidepressants: rates of suicide relative to prescribing and non-fatal overdose. Br J Psychiatry. 2010;196(5):354-358.
7. Preskorn SH, Flockhart D. 2010 guide to psychiatric drug interactions. Primary Psychiatry. 2009;16(12):45-74.
8. Lin JH, Lu AY. Inhibition and induction of cytochrome P450 and the clinical implications. Clin Pharmacokinet. 1998;35(5):361-390.
9. Kutscher EC, Alexander B. A review of drug interactions with psychiatric medicines for the pharmacy practitioner. J Pharm Pract. 2007;20(4):327-333.
10. Wren P, Frizzell LA, Keltner NL, et al. Three potentially fatal adverse effects of psychotropic medications. Perspect Psychiatr Care. 2003;39(2):75-81.
11. Dave M, Miceli K, Modha P. Psychiatric medicine. The psychiatrist’s guide to the treatment of common medical illnesses. Philadelphia PA: Lippincott Williams & Wilkins; 2007.
12. Mir S, Taylor D. The adverse effects of antidepressants. Curr Opin Psychiatry. 1997;10(2):88-94.
13. Drug-induced long QT interval. Pharmacist’s Letter/Prescriber’s Letter. 2010;26(4):260421.-
14. Drug-induced prolongation of the QT interval and torsades de pointes. 2011. Available at: http://online.factsandcomparisons.com. Accessed February 15 2011.
15. Kales HC, Valenstein M, Kim HM, et al. Mortality risk in patients with dementia treated with antipsychotics versus other psychiatric medications. Am J Psychiatry. 2007;164(10):1568-1576; quiz 1623.
16. Merrill DB, Ahmari SE, Bradford JM, et al. Myocarditis during clozapine treatment. Am J Psychiatry. 2006;163(2):204-208.
17. Oyesanmi O, Kunkel EJ, Monti DA, et al. Hematologic side effects of psychotropics. Psychosomatics. 1999;40(5):414-421.
18. Pisani F, Oteri G, Costa C, et al. Effects of psychotropic drugs on seizure threshold. Drug Saf. 2002;25(2):91-110.
19. Martin-Latry K, Goumy M, Latry P, et al. Psychotropic drugs use and risk of heat-related hospitalization. Eur Psychiatry. 2007;22:335-338.
20. Melkersson K, Dahl ML. Adverse metabolic effects associated with atypical antipsychotics: literature review and clinical implications. Drugs. 2004;64(7):701-723.
21. Liu B, Anderson G, Mittmann N, et al. Use of selective serotonin-reuptake inhibitors or tricyclic antidepressants and risk of hip fractures in elderly people. Lancet. 1998;351(9112):1303-1307.
22. Cumming RG, Le Couteur DG. Benzodiazepines and risk of hip fractures in older people: a review of the evidence. CNS Drugs. 2003;17(11):825-837.
23. Hirose S. The causes of underdiagnosing akathisia. Schizophr Bull. 2003;29(3):547-558.
24. Kane JM, Fleischhacker WW, Hansen L, et al. Akathisia: an updated review focusing on second-generation antipsychotics. J Clin Psychiatry. 2009;70(5):627-643.
25. Selim K, Kaplowitz N. Hepatotoxicity of psychotropic drugs. Hepatology. 1999;29(5):1347-1351.
26. Chitturi S, George J. Hepatotoxicity of commonly used drugs: nonsteroidal anti-inflammatory drugs antihypertensives, antidiabetic agents, anticonvulsants, lipid-lowering agents, psychotropic drugs. Semin Liver Dis. 2002;22(2):169-183.
27. Sandson NB, Armstrong SC, Cozza KL. An overview of psychotropic drug-drug interactions. Psychosomatics. 2005;46(5):464-494.
Medication errors due to system-, provider-, or patient-related factors contribute significantly to increased costs, adverse drug events (ADEs), and morbidity and mortality.1 One study found >60% of ADEs that led to hospitalization could have been prevented by strategies such as adequate monitoring or appropriate prescribing.2 Psychiatrists have an opportunity to reduce rates of ADEs; however, the possibility of disease symptoms overlapping with these adverse events is 1 of many obstacles prescribing clinicians face.1 Prescribers also must contend with adverse effects of polypharmacy, which are common among psychiatric patients. Patient-related factors of concern include:
- seeing multiple prescribers
- medication nonadherence
- failure to communicate use of herbal or over-the-counter products
- lack of insight
- comorbid medical and psychiatric diagnoses, such as dementia.1
This article highlights potential ADEs and major medication safety concerns that may contribute to morbidity and mortality among patients taking psychotropics. Although many factors are beyond the prescribing clinician’s control—such as medication dispensing and administration errors—psychiatrists can substantially reduce ADEs. We will cover potential adverse events associated with key medications or medication classes, drug interactions with potentially devastating consequences, and strategies to minimize risks of ADEs, including enhanced awareness and monitoring (Table 1).
Table 1
How to avoid ADEs with psychotropics
| Establish a collaborative practice among physicians, pharmacists, nurses, and social workers to enhance patient care and reduce the risk of medication errors and negative outcomes |
| Educate patients to increase their understanding of psychiatric diseases and medications and increase compliance with therapy. This may lead the patient to self-monitor drug efficacy and adverse effects |
| Be aware of psychotropic medications’ ‘black-box’ warnings that guide their safe use |
| Pay particular attention to drugs with a narrow therapeutic index, such as lithium and tricyclic antidepressants, which have small safety margins and are lethal in overdose |
| Avoid using 1 drug to treat the side effects of another. Minimizing polypharmacy can reduce medication errors, DDIs, and ADEs |
| Remain vigilant for DDIs, which can be serious and life-threatening. Examples include sudden cardiac death from additive QTc prolongation effects and NMS. Early detection of NMS and discontinuing the offending agent(s) can help prevent patient morbidity and mortality |
| Stay up-to-date on literature and drug warnings to employ best practices and avoid potentially serious adverse and/or lethal outcomes |
| Encourage patients to disclose any prescription drugs, over-the-counter medications, and herbal therapies they are taking |
| Develop strategies to prevent ADEs, such as personal formularies, suicide assessments, prescribing limited quantities, ‘eyes on’ medication administration, therapeutic drug monitoring, utilizing databases and resources for drug information, and patient education |
| ADEs: adverse drug events; DDIs: drug-drug interactions; NMS: neuroleptic malignant syndrome |
Prescription drug overdose
Each year, unintentional drug overdoses account for >20,000 deaths in the United States.3 Prescription medications, particularly opioid analgesics, have contributed to the doubling of overdose mortality rates in recent years. A recent study reported that nearly 50% of unintentional drug overdose deaths were associated with psychotropics and one-third of these deaths were associated with benzodiazepines, many of which were not prescribed to the individual.4
The risk of mortality from intentional drug overdose also must be assessed. Tricyclic antidepressants (TCAs) are a particularly lethal class of medications in suicide attempts and may result in arrhythmias, coma, seizures, respiratory failure, and death.5 Venlafaxine and mirtazapine are associated with greater risk of death and toxicity in overdose, respectively, than selective serotonin reuptake inhibitors (SSRIs).6 Lithium toxicity in overdose may lead to bradycardia, seizure, coma, hyperventilation, serotonin syndrome, respiratory failure, or death.5 The risk of death with lithium or benzodiazepine monotherapy is low when these agents are taken as prescribed. However, prescribers must exercise caution when these agents are used in combination. Interactions involving drugs with a narrow therapeutic index—such as lithium and TCAs—are more likely to be clinically significant because small increases in drug concentration can lead to serious adverse effects or death. See Related Resources for a review article on appropriate use and monitoring of lithium.
Drug-drug interactions
Many Americans take multiple prescription and nonprescription drugs, and psychiatric patients are more likely than other individuals to have more complex medication regimens.7 This can result in polypharmacy and drug-drug interactions (DDIs), which can lead to undesired medication effects and serious, potentially fatal ADEs.
Pharmacokinetic interactions typically affect drug concentrations and occur when 1 drug interferes with the absorption, distribution, metabolism, or excretion of another drug. Many common pharmacokinetic interactions involve the liver cytochrome P450 (CYP) system, which is responsible for metabolizing many medications.8 DDIs can occur when CYP enzymes are modified by inhibitors or inducers, which can decrease or increase drug clearance, respectively. Table 2 5,7,9 provides examples of common CYP450 substrates, inhibitors, and inducers. Polymorphisms in the pharmacogenetics of CYP450 also can affect overall drug clearance and the impact of DDIs.8
Pharmacodynamic interactions are caused by additive or competing effects of multiple drugs. The most serious of these involve medications that increase a patient’s risk of serotonin syndrome or neuroleptic malignant syndrome (NMS); both are medical emergencies that require immediate hospitalization.
Although any medication with serotonergic activity can induce serotonin syndrome, combinations of serotonergic drugs in particular are associated with increased risk.10 Serotonin syndrome is characterized by hyperthermia, altered muscle tone, altered mental status, and autonomic instability; rhabdomyolysis and disseminated intravascular coagulation are potential lethal complications.10 A high index of suspicion can help clinicians rapidly detect serotonin syndrome, discontinue offending agents, and initiate supportive treatments.
NMS is a life-threatening complication of antipsychotics characterized by fever, delirium, muscle rigidity, autonomic instability, and abnormal laboratory findings that include elevated white blood count and increased creatinine kinase from muscle injury. In early stages, NMS may be mistaken for extrapyramidal symptoms. Although NMS can occur with any antipsychotic as monotherapy, additive antidopaminergic effects increase the risk. Patients with a compromised CNS as a result of mental retardation, traumatic brain injury, or metabolic abnormalities also are at increased risk of developing NMS.11
Other pharmacodynamic interactions involve medications that may have additive effects on prolonging QTc intervals. For example, TCAs are pro-arrhythmic and have quinidine-like effects, which can cause cardiac conduction abnormalities and prolonged PR and QTc intervals.12 Employ routine ECG monitoring when prescribing multiple medications known to cause QTc prolongation, such as TCAs (Table 3).13,14 The Arizona Center for Education and Research on Therapeutics (www.azcert.org) provides a searchable list of QT-prolonging drugs (see Related Resources).
Medications also can interact with food, disease states, and herbal supplements. Alcohol interacts with many CNS-active medications, including many psychotropics. Patients taking benzodiazepines may experience oversedation and respiratory depression from alcohol’s additive sedating effects.5 Advise patients to limit their alcohol intake while taking CNS-depressing psychotropics such as benzodiazepines, antipsychotics, and some antidepressants. Monoamine oxidase inhibitors (MAOIs) and tyramine-containing food—such as cheese, beer, preserved meat, and soy sauce—can lead to a dangerous hypertensive crisis that requires immediate medical intervention to prevent life-threatening complications.5 Hypertensive crisis may be more significant in patients who have pre-existing hypertension. Finally, herbal supplements also can interact with medications. Patients who take St. John’s wort for depressive symptoms might not realize that it can reduce the efficacy of other drugs or increase their risk of serotonin syndrome.9
Table 2
Cytochrome P450 substrates, inhibitors, and inducers
| 3A4 | 2D6 | 2C9 | 2C19 | 1A2 | |
|---|---|---|---|---|---|
| Substrates | Carbamazepine Citalopram Fluoxetine Haloperidol Mirtazapine Oxcarbazepine Quetiapine Sertraline Ziprasidone | Aripiprazole Citalopram Duloxetine Fluoxetine Haloperidol Mirtazapine Paroxetine Risperidone Sertraline Venlafaxine TCAs | Amitriptyline Carbamazepine Sertraline Valproic acid | Citalopram Clomipramine Sertraline Valproic acid | Carbamazepine Clozapine Olanzapine |
| Inhibitors | Amiodarone Aprepitant Azole antifungals Carbamazepine Cimetidine Diltiazem Erythromycin Fluoxetine (norfloxetine) Grapefruit juice Imatinib Paroxetine Ritonavir Sertraline Verapamil | Amiodarone Bupropion Cimetidine Duloxetine Fluoxetine Methadone Paroxetine Ritonavir Sertraline | Amiodarone Fluconazole Isoniazid Sertraline Trimethoprim-sulfamethoxazole Valproic acid | Cimetidine Fluoxetine Ketoconazole Omeprazole Sertraline Valproic acid | Amiodarone Cimetidine Fluoroquinolones |
| Inducers | Carbamazepine Phenobarbital Phenytoin Rifampin St. John’s wort | Rifampin | Phenobarbital Rifampin | Carbamazepine Rifampin | Nafcillin Phenobarbital Rifampin Smoking |
| TCAs: tricyclic antidepressants Source: References 5,7,9 | |||||
Table 3
Psychotropics associated with QT prolongation
| Class | Agents |
|---|---|
| Antidepressants | Mirtazapine, SNRIs (desvenlafaxine, venlafaxine), SSRIs (citalopram, fluoxetine, paroxetine, sertraline), TCAs (amitriptyline, clomipramine, desipramine, doxepin, imipramine, protriptyline, trimipramine), trazodone |
| Typical antipsychotics | Chlorpromazine, fluphenazine, haloperidol, perphenazine, thioridazine, trifluoperazine |
| Atypical antipsychotics | Aripiprazole, asenapine, clozapine, iloperidone, paliperidone, quetiapine, risperidone, ziprasidone |
| Mood stabilizers | Lithium |
| Miscellaneous agents | Amantadine, atomoxetine, chloral hydrate, diphenhydramine, galantamine |
| Stimulants | Amphetamine/dextroamphetamine products, methylphenidate/dexmethylphenidate |
| SNRIs: serotonin-norepinephrine reuptake inhibitors; SSRIs: selective serotonin reuptake inhibitors; TCAs: tricyclic antidepressants Source: Adapted from references 13,14 | |
“Black-box” warnings issued by the FDA are included in the package insert to highlight a medication’s risks of dangerous and potentially lethal adverse effects. Table 4 highlights current black-box warnings for various psychotropics.5,14-16
Antidepressants and suicide. All medications with antidepressant indications carry a black-box warning for risk of suicidal ideation and behavior in children, adolescents, and young adults during the early months of medication therapy. This includes not only SSRIs and serotonin-norepinephrine reuptake inhibitors, but also anticonvulsants and atypical antipsychotics indicated for treating mood disorders. Monitor young patients carefully and advise family members to alert clinicians of any signs of suicidality or unusual behavior.
Lamotrigine and aseptic meningitis. Aseptic meningitis—inflammation of the meninges that is not caused by bacteria—is a rare but serious adverse effect of lamotrigine. Symptoms include headache, fever, stiff neck, nausea and vomiting, delirium, rash, and sensitivity to light.5 Forty cases of aseptic meningitis in children and adults were reported over 15 years, representing <.01% of all lamotrigine prescriptions.5 Most of these patients required hospitalization, but symptoms resolved after lamotrigine was discontinued. Prompt identification and management of aseptic meningitis are necessary to prevent permanent brain damage and death. Other complications of aseptic meningitis include long-term neurologic sequelae such as cognitive impairment, seizure disorders, and behavioral disturbances.
Table 4
Which psychotropics carry ‘black-box’ warnings?
| Warning | Class or medication affected | Comments |
|---|---|---|
| Suicidality | Antidepressants Antipsychotics indicated for mood disorders Anticonvulsants | See ‘Black-box warnings’ |
| Serious, life-threatening rashes such as Stevens-Johnson syndrome or toxic epidermal necrolysis | Lamotrigine Carbamazepine | Lamotrigine’s risk of severe dermatologic reactions necessitates slow titration during drug initiation Carbamazepine warning includes a recommendation for genetic screening in Asian patients because Stevens-Johnson syndrome is associated with the HLA-B*1502 allele found primarily in the Asian population |
| Increased mortality in elderly patients with dementia-related psychosis | Antipsychotics | A study of >10,000 geriatric patients with dementia showed mortality rates of 22.6% to 29.1% among those who took antipsychotics compared with 14.6% for patients taking other psychiatric medications. When antipsychotics are used in older adults, well-documented informed consent from the patient or substitute decision-maker is required |
| Other effects | Clozapine | Agranulocytosis occurs in 1% to 2% of clozapine patients, necessitating WBC/ANC monitoring Clozapine-induced myocarditis, generally accompanied by peripheral eosinophilia, usually occurs within the first 2 months of treatment, and can result in significant mortality from resultant cardiomyopathy. Early warning signs of fever, fatigue, and tachycardia are easily mistaken for the more benign effects of clozapine titration Seizures are more likely with higher doses. Cautious use is advised with patients who have an underlying seizure disorder Other cardiovascular and respiratory effects: Hypotension has been associated with rapid initial titration. Cardiac and respiratory arrest and circulatory collapse have occurred rarely. Respiratory complications are more likely when clozapine is used in combination with benzodiazepines |
| ANC: absolute neutrophil count; WBC: white blood cell Source: References 5,14-16 | ||
Other complications
Hematologic effects. All classes of psychotropics carry a risk (1 to 2 cases per year per 100,00 patients) of serious hematologic complications, including neutropenia, agranulocytosis, eosinophilia, thrombocytopenia, purpura, and anemia.17 Agranulocytosis has been associated most commonly with clozapine, carbamazepine, and typical antipsychotics.17 SSRIs, which are widely prescribed, are associated with increased risk of bruising and bleeding. Patients with bleeding or platelet disorders are at an increased risk for these complications.17
Seizures. Several classes of psychotropics are associated with an increased risk of seizures. Among antipsychotics, clozapine and chlorpromazine are the most seizurogenic.18 Among antidepressants, bupropion and clomipramine are most likely to lower seizure thresholds.18 Psychotropics’ seizure-inducing effects are dose-related. Vulnerability to seizures while taking psychotropics is related to having a history of epilepsy or brain injury.18 Seizures also can occur when benzodiazepines or anticonvulsants are withdrawn too quickly.
Heat stroke. Although a rare occurrence, psychotropics with anticholinergic side effects can contribute to heat stroke. Older patients are particularly vulnerable to the risk of body temperature dysregulation.19
Ketoacidosis and hyperosmolar coma. Medication-related deaths have occurred as a result of ketoacidosis and hyperosmolar coma associated with atypical antipsychotics. These hyperglycemia-related fatalities are most likely with clozapine and olanzapine.20
Hip fractures and falls. Geriatric patients are vulnerable to falls and resultant hip fractures related to use of TCAs, SSRIs, benzodiazepines, and antipsychotics. This is not a trivial matter; hip fractures increase the mortality rate by 12% to 20% in the year after the injury.21 The risk of falls is related to sedation, orthostatic hypotension, arrhythmias, and confusion associated with psychotropics.21,22
Akathisia and suicide. Unrecognized or undertreated akathisia is most commonly associated with antipsychotics, but also can occur with SSRIs. Although akathisia is commonly thought of as a motor syndrome of restlessness, patients may find the less-recognized psychic symptoms of increased inner turmoil and hallucinations just as distressing. This complex of symptoms is associated with an increased risk of suicide.23 If discontinuing the offending agent is not feasible, akathisia can be treated with beta blockers, benzodiazepines, or anticholinergics.24
Hepatotoxicity. Hepatotoxicity from psychotropics occurs in only a small percentage of patients, and can range from transient elevations in liver enzymes to fulminant liver failure. Adverse hepatic effects may be a manifestation of a hypersensitivity reaction accompanied by rash and eosinophilia.25 MAOIs and TCAs can cause cholestatic liver injury, whereas nefazodone has been associated with fulminant liver failure. Other psychotropics—including SSRIs, antipsychotics, benzodiazepines, and older antiepileptics—can cause negative hepatic effects but rarely are associated with acute liver failure.25,26 Although few medications can cause complete liver failure on their own, hepatotoxicity from medications may precipitate severe, potentially fatal outcomes in patients with underlying liver diseases such as hepatitis and cirrhosis. Additive hepatotoxicity from multiple medications also can be problematic. Although psychotropic-induced hepatotoxicity is rare, assess psychotropic doses in patients with liver dysfunction, because drug clearance may be altered, which increases the risk for other serious adverse events.25
Suicide assessment is key
Ongoing monitoring for current or developing suicidal ideation is an important strategy to prevent medication-related mortality in patients vulnerable to self-harm. Initial assessments and follow-up appointments should include a detailed inquiry about suicidal ideations, plans, and behaviors. Patients taking medications that carry black-box warnings for suicide risk should be seen frequently during the first few months of treatment. Patients receiving medications that are lethal in overdose (eg, lithium and TCAs) should be carefully screened for suicide risk. Prescribe medications in limited quantities or arrange for a family member to monitor the patient if necessary. Patients with a history of suicide attempts and current suicide plans may require close observation and initiating medications while hospitalized.
Other prevention strategies
Prescribing psychotropics in a manner that promotes mental well being while minimizing negative outcomes can be challenging. By developing a personal formulary of drugs commonly encountered and prescribed in their practice, psychiatrists can increase their awareness of serious safety concerns, potential DDIs, and appropriate use based on available literature.7,27
Medication histories and drug reconciliation—comparing a patient’s medication orders to all of the medications the patient has been taking—can help clinicians avoid making inappropriate dose adjustments, duplicating therapy, or prescribing medications patients previously have failed or did not tolerate. Establishing a collaborative practice environment with physicians, pharmacists, nurses, and social workers can minimize medication errors and risk of adverse outcomes by increasing communication regarding the patient’s treatment.7
Computerized drug databases and other electronic resources and consultation with pharmacists can help prescribers identify, avoid, and manage clinically significant DDIs.27 Medications could interact with other drugs as long as their effects persist in the body, which could be days to months after the drug is discontinued. Future research may lead to tools to identify patient pharmacogenetic profiles.
Recognizing psychotropic DDIs and adverse effects remains a challenge because of the complexity of the affected organ, the brain. Clinicians should be vigilant to changes in a patient’s presentation because they may be a manifestation of a medication side effect.7 Appropriate therapeutic drug monitoring should occur on a routine, scheduled basis. Closer monitoring may be necessary with dose changes, potential DDIs, signs and symptoms of toxicity/efficacy failure, and renal or hepatic function changes.
Lastly, patients’ education and involvement in their health care may increase their awareness, responsibility, and medication adherence. For challenging patients, family involvement and “eyes on” medication administration can increase adherence and prevent psychotropic misuse.
- Arizona Center for Education and Research on Therapeutics. Drugs that prolong the QT interval and/or induce Torsades de Pointes ventricular arrhythmia. www.azcert.org/medical-pros/drug-lists/drug-lists.cfm.
- Cates ME, Sims PJ. Therapeutic drug management of lithium. Am J Pharm Educ. 2005;69(5):88.
- Wren P, Frizzell LA, Keltner NL, et al. Three potentially fatal adverse effects of psychotropic medications. Perspect Psychiatr Care. 2003;39(2):75-81.
- Bishop JR, Bishop DL. How to prevent serotonin syndrome from drug-drug interactions. Current Psychiatry. 2011;10(3):81-83.
Drug Brand Names
- Amantadine • Symmetrel
- Amiodarone • Cordarone, Pacerone
- Amitriptyline • Elavil
- Amphetamine/dextroamphetamine • Adderall, others
- Aprepitant • Emend
- Aripiprazole • Abilify
- Asenapine • Saphris
- Atomoxetine • Strattera
- Bupropion • Wellbutrin, Zyban
- Carbamazepine • Tegretol, others
- Chloral hydrate • Somnote
- Chlorpromazine • Thorazine
- Cimetidine • Tagamet
- Citalopram • Celexa
- Clomipramine • Anafranil
- Clozapine • Clozaril
- Desipramine • Norpramin
- Desvenlafaxine • Pristiq
- Diltiazem • Cardia, others
- Diphenhydramine • Benadryl, others
- Doxepin • Sinequan, Silenor
- Duloxetine • Cymbalta
- Erythromycin • Ery-Tab, others
- Fluconazole • Diflucan
- Fluoxetine • Prozac
- Fluphenazine • Prolixin
- Galantamine • Razadyne
- Haloperidol • Haldol
- Iloperidone • Fanapt
- Imatinib • Gleevec
- Imipramine • Tofranil
- Isoniazid • Nydrazid, others
- Ketoconazole • Nizoral, others
- Lamotrigine • Lamictal
- Lithium • Eskalith, others
- Methadone • Dolophine, Methadose
- Methylphenidate/ dexmethylphenidate • Ritalin, others
- Mirtazapine • Remeron
- Nafcillin • Nafcil, others
- Nefazodone • Serzone
- Olanzapine • Zyprexa
- Omeprazole • Prilosec
- Oxcarbazepine • Trileptal
- Paliperidone • Invega
- Paroxetine • Paxil
- Perphenazine • Trilafon
- Phenobarbital • Luminal, others
- Phenytoin • Dilantin
- Protriptyline • Vivactil
- Quetiapine • Seroquel
- Rifampin • Rifadin, others
- Risperidone • Risperdal
- Ritonavir • Norvir
- Sertraline • Zoloft
- Thioridazine • Mellaril
- Trazodone • Desyrel, Oleptro
- Trifluoperazine • Stelazine
- Trimethoprim/Sulfamethoxazole • Bactrim, Septra
- Trimipramine • Surmontil
- Valproic acid • Depakote, others
- Venlafaxine • Effexor
- Verapamil • Calan, others
- Ziprasidone • Geodon
Disclosure
Drs. Yu and Bostwick report no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
Dr. Casher is a speaker for AstraZeneca, Pfizer Inc, and Sunovion Pharmaceuticals.
Medication errors due to system-, provider-, or patient-related factors contribute significantly to increased costs, adverse drug events (ADEs), and morbidity and mortality.1 One study found >60% of ADEs that led to hospitalization could have been prevented by strategies such as adequate monitoring or appropriate prescribing.2 Psychiatrists have an opportunity to reduce rates of ADEs; however, the possibility of disease symptoms overlapping with these adverse events is 1 of many obstacles prescribing clinicians face.1 Prescribers also must contend with adverse effects of polypharmacy, which are common among psychiatric patients. Patient-related factors of concern include:
- seeing multiple prescribers
- medication nonadherence
- failure to communicate use of herbal or over-the-counter products
- lack of insight
- comorbid medical and psychiatric diagnoses, such as dementia.1
This article highlights potential ADEs and major medication safety concerns that may contribute to morbidity and mortality among patients taking psychotropics. Although many factors are beyond the prescribing clinician’s control—such as medication dispensing and administration errors—psychiatrists can substantially reduce ADEs. We will cover potential adverse events associated with key medications or medication classes, drug interactions with potentially devastating consequences, and strategies to minimize risks of ADEs, including enhanced awareness and monitoring (Table 1).
Table 1
How to avoid ADEs with psychotropics
| Establish a collaborative practice among physicians, pharmacists, nurses, and social workers to enhance patient care and reduce the risk of medication errors and negative outcomes |
| Educate patients to increase their understanding of psychiatric diseases and medications and increase compliance with therapy. This may lead the patient to self-monitor drug efficacy and adverse effects |
| Be aware of psychotropic medications’ ‘black-box’ warnings that guide their safe use |
| Pay particular attention to drugs with a narrow therapeutic index, such as lithium and tricyclic antidepressants, which have small safety margins and are lethal in overdose |
| Avoid using 1 drug to treat the side effects of another. Minimizing polypharmacy can reduce medication errors, DDIs, and ADEs |
| Remain vigilant for DDIs, which can be serious and life-threatening. Examples include sudden cardiac death from additive QTc prolongation effects and NMS. Early detection of NMS and discontinuing the offending agent(s) can help prevent patient morbidity and mortality |
| Stay up-to-date on literature and drug warnings to employ best practices and avoid potentially serious adverse and/or lethal outcomes |
| Encourage patients to disclose any prescription drugs, over-the-counter medications, and herbal therapies they are taking |
| Develop strategies to prevent ADEs, such as personal formularies, suicide assessments, prescribing limited quantities, ‘eyes on’ medication administration, therapeutic drug monitoring, utilizing databases and resources for drug information, and patient education |
| ADEs: adverse drug events; DDIs: drug-drug interactions; NMS: neuroleptic malignant syndrome |
Prescription drug overdose
Each year, unintentional drug overdoses account for >20,000 deaths in the United States.3 Prescription medications, particularly opioid analgesics, have contributed to the doubling of overdose mortality rates in recent years. A recent study reported that nearly 50% of unintentional drug overdose deaths were associated with psychotropics and one-third of these deaths were associated with benzodiazepines, many of which were not prescribed to the individual.4
The risk of mortality from intentional drug overdose also must be assessed. Tricyclic antidepressants (TCAs) are a particularly lethal class of medications in suicide attempts and may result in arrhythmias, coma, seizures, respiratory failure, and death.5 Venlafaxine and mirtazapine are associated with greater risk of death and toxicity in overdose, respectively, than selective serotonin reuptake inhibitors (SSRIs).6 Lithium toxicity in overdose may lead to bradycardia, seizure, coma, hyperventilation, serotonin syndrome, respiratory failure, or death.5 The risk of death with lithium or benzodiazepine monotherapy is low when these agents are taken as prescribed. However, prescribers must exercise caution when these agents are used in combination. Interactions involving drugs with a narrow therapeutic index—such as lithium and TCAs—are more likely to be clinically significant because small increases in drug concentration can lead to serious adverse effects or death. See Related Resources for a review article on appropriate use and monitoring of lithium.
Drug-drug interactions
Many Americans take multiple prescription and nonprescription drugs, and psychiatric patients are more likely than other individuals to have more complex medication regimens.7 This can result in polypharmacy and drug-drug interactions (DDIs), which can lead to undesired medication effects and serious, potentially fatal ADEs.
Pharmacokinetic interactions typically affect drug concentrations and occur when 1 drug interferes with the absorption, distribution, metabolism, or excretion of another drug. Many common pharmacokinetic interactions involve the liver cytochrome P450 (CYP) system, which is responsible for metabolizing many medications.8 DDIs can occur when CYP enzymes are modified by inhibitors or inducers, which can decrease or increase drug clearance, respectively. Table 2 5,7,9 provides examples of common CYP450 substrates, inhibitors, and inducers. Polymorphisms in the pharmacogenetics of CYP450 also can affect overall drug clearance and the impact of DDIs.8
Pharmacodynamic interactions are caused by additive or competing effects of multiple drugs. The most serious of these involve medications that increase a patient’s risk of serotonin syndrome or neuroleptic malignant syndrome (NMS); both are medical emergencies that require immediate hospitalization.
Although any medication with serotonergic activity can induce serotonin syndrome, combinations of serotonergic drugs in particular are associated with increased risk.10 Serotonin syndrome is characterized by hyperthermia, altered muscle tone, altered mental status, and autonomic instability; rhabdomyolysis and disseminated intravascular coagulation are potential lethal complications.10 A high index of suspicion can help clinicians rapidly detect serotonin syndrome, discontinue offending agents, and initiate supportive treatments.
NMS is a life-threatening complication of antipsychotics characterized by fever, delirium, muscle rigidity, autonomic instability, and abnormal laboratory findings that include elevated white blood count and increased creatinine kinase from muscle injury. In early stages, NMS may be mistaken for extrapyramidal symptoms. Although NMS can occur with any antipsychotic as monotherapy, additive antidopaminergic effects increase the risk. Patients with a compromised CNS as a result of mental retardation, traumatic brain injury, or metabolic abnormalities also are at increased risk of developing NMS.11
Other pharmacodynamic interactions involve medications that may have additive effects on prolonging QTc intervals. For example, TCAs are pro-arrhythmic and have quinidine-like effects, which can cause cardiac conduction abnormalities and prolonged PR and QTc intervals.12 Employ routine ECG monitoring when prescribing multiple medications known to cause QTc prolongation, such as TCAs (Table 3).13,14 The Arizona Center for Education and Research on Therapeutics (www.azcert.org) provides a searchable list of QT-prolonging drugs (see Related Resources).
Medications also can interact with food, disease states, and herbal supplements. Alcohol interacts with many CNS-active medications, including many psychotropics. Patients taking benzodiazepines may experience oversedation and respiratory depression from alcohol’s additive sedating effects.5 Advise patients to limit their alcohol intake while taking CNS-depressing psychotropics such as benzodiazepines, antipsychotics, and some antidepressants. Monoamine oxidase inhibitors (MAOIs) and tyramine-containing food—such as cheese, beer, preserved meat, and soy sauce—can lead to a dangerous hypertensive crisis that requires immediate medical intervention to prevent life-threatening complications.5 Hypertensive crisis may be more significant in patients who have pre-existing hypertension. Finally, herbal supplements also can interact with medications. Patients who take St. John’s wort for depressive symptoms might not realize that it can reduce the efficacy of other drugs or increase their risk of serotonin syndrome.9
Table 2
Cytochrome P450 substrates, inhibitors, and inducers
| 3A4 | 2D6 | 2C9 | 2C19 | 1A2 | |
|---|---|---|---|---|---|
| Substrates | Carbamazepine Citalopram Fluoxetine Haloperidol Mirtazapine Oxcarbazepine Quetiapine Sertraline Ziprasidone | Aripiprazole Citalopram Duloxetine Fluoxetine Haloperidol Mirtazapine Paroxetine Risperidone Sertraline Venlafaxine TCAs | Amitriptyline Carbamazepine Sertraline Valproic acid | Citalopram Clomipramine Sertraline Valproic acid | Carbamazepine Clozapine Olanzapine |
| Inhibitors | Amiodarone Aprepitant Azole antifungals Carbamazepine Cimetidine Diltiazem Erythromycin Fluoxetine (norfloxetine) Grapefruit juice Imatinib Paroxetine Ritonavir Sertraline Verapamil | Amiodarone Bupropion Cimetidine Duloxetine Fluoxetine Methadone Paroxetine Ritonavir Sertraline | Amiodarone Fluconazole Isoniazid Sertraline Trimethoprim-sulfamethoxazole Valproic acid | Cimetidine Fluoxetine Ketoconazole Omeprazole Sertraline Valproic acid | Amiodarone Cimetidine Fluoroquinolones |
| Inducers | Carbamazepine Phenobarbital Phenytoin Rifampin St. John’s wort | Rifampin | Phenobarbital Rifampin | Carbamazepine Rifampin | Nafcillin Phenobarbital Rifampin Smoking |
| TCAs: tricyclic antidepressants Source: References 5,7,9 | |||||
Table 3
Psychotropics associated with QT prolongation
| Class | Agents |
|---|---|
| Antidepressants | Mirtazapine, SNRIs (desvenlafaxine, venlafaxine), SSRIs (citalopram, fluoxetine, paroxetine, sertraline), TCAs (amitriptyline, clomipramine, desipramine, doxepin, imipramine, protriptyline, trimipramine), trazodone |
| Typical antipsychotics | Chlorpromazine, fluphenazine, haloperidol, perphenazine, thioridazine, trifluoperazine |
| Atypical antipsychotics | Aripiprazole, asenapine, clozapine, iloperidone, paliperidone, quetiapine, risperidone, ziprasidone |
| Mood stabilizers | Lithium |
| Miscellaneous agents | Amantadine, atomoxetine, chloral hydrate, diphenhydramine, galantamine |
| Stimulants | Amphetamine/dextroamphetamine products, methylphenidate/dexmethylphenidate |
| SNRIs: serotonin-norepinephrine reuptake inhibitors; SSRIs: selective serotonin reuptake inhibitors; TCAs: tricyclic antidepressants Source: Adapted from references 13,14 | |
“Black-box” warnings issued by the FDA are included in the package insert to highlight a medication’s risks of dangerous and potentially lethal adverse effects. Table 4 highlights current black-box warnings for various psychotropics.5,14-16
Antidepressants and suicide. All medications with antidepressant indications carry a black-box warning for risk of suicidal ideation and behavior in children, adolescents, and young adults during the early months of medication therapy. This includes not only SSRIs and serotonin-norepinephrine reuptake inhibitors, but also anticonvulsants and atypical antipsychotics indicated for treating mood disorders. Monitor young patients carefully and advise family members to alert clinicians of any signs of suicidality or unusual behavior.
Lamotrigine and aseptic meningitis. Aseptic meningitis—inflammation of the meninges that is not caused by bacteria—is a rare but serious adverse effect of lamotrigine. Symptoms include headache, fever, stiff neck, nausea and vomiting, delirium, rash, and sensitivity to light.5 Forty cases of aseptic meningitis in children and adults were reported over 15 years, representing <.01% of all lamotrigine prescriptions.5 Most of these patients required hospitalization, but symptoms resolved after lamotrigine was discontinued. Prompt identification and management of aseptic meningitis are necessary to prevent permanent brain damage and death. Other complications of aseptic meningitis include long-term neurologic sequelae such as cognitive impairment, seizure disorders, and behavioral disturbances.
Table 4
Which psychotropics carry ‘black-box’ warnings?
| Warning | Class or medication affected | Comments |
|---|---|---|
| Suicidality | Antidepressants Antipsychotics indicated for mood disorders Anticonvulsants | See ‘Black-box warnings’ |
| Serious, life-threatening rashes such as Stevens-Johnson syndrome or toxic epidermal necrolysis | Lamotrigine Carbamazepine | Lamotrigine’s risk of severe dermatologic reactions necessitates slow titration during drug initiation Carbamazepine warning includes a recommendation for genetic screening in Asian patients because Stevens-Johnson syndrome is associated with the HLA-B*1502 allele found primarily in the Asian population |
| Increased mortality in elderly patients with dementia-related psychosis | Antipsychotics | A study of >10,000 geriatric patients with dementia showed mortality rates of 22.6% to 29.1% among those who took antipsychotics compared with 14.6% for patients taking other psychiatric medications. When antipsychotics are used in older adults, well-documented informed consent from the patient or substitute decision-maker is required |
| Other effects | Clozapine | Agranulocytosis occurs in 1% to 2% of clozapine patients, necessitating WBC/ANC monitoring Clozapine-induced myocarditis, generally accompanied by peripheral eosinophilia, usually occurs within the first 2 months of treatment, and can result in significant mortality from resultant cardiomyopathy. Early warning signs of fever, fatigue, and tachycardia are easily mistaken for the more benign effects of clozapine titration Seizures are more likely with higher doses. Cautious use is advised with patients who have an underlying seizure disorder Other cardiovascular and respiratory effects: Hypotension has been associated with rapid initial titration. Cardiac and respiratory arrest and circulatory collapse have occurred rarely. Respiratory complications are more likely when clozapine is used in combination with benzodiazepines |
| ANC: absolute neutrophil count; WBC: white blood cell Source: References 5,14-16 | ||
Other complications
Hematologic effects. All classes of psychotropics carry a risk (1 to 2 cases per year per 100,00 patients) of serious hematologic complications, including neutropenia, agranulocytosis, eosinophilia, thrombocytopenia, purpura, and anemia.17 Agranulocytosis has been associated most commonly with clozapine, carbamazepine, and typical antipsychotics.17 SSRIs, which are widely prescribed, are associated with increased risk of bruising and bleeding. Patients with bleeding or platelet disorders are at an increased risk for these complications.17
Seizures. Several classes of psychotropics are associated with an increased risk of seizures. Among antipsychotics, clozapine and chlorpromazine are the most seizurogenic.18 Among antidepressants, bupropion and clomipramine are most likely to lower seizure thresholds.18 Psychotropics’ seizure-inducing effects are dose-related. Vulnerability to seizures while taking psychotropics is related to having a history of epilepsy or brain injury.18 Seizures also can occur when benzodiazepines or anticonvulsants are withdrawn too quickly.
Heat stroke. Although a rare occurrence, psychotropics with anticholinergic side effects can contribute to heat stroke. Older patients are particularly vulnerable to the risk of body temperature dysregulation.19
Ketoacidosis and hyperosmolar coma. Medication-related deaths have occurred as a result of ketoacidosis and hyperosmolar coma associated with atypical antipsychotics. These hyperglycemia-related fatalities are most likely with clozapine and olanzapine.20
Hip fractures and falls. Geriatric patients are vulnerable to falls and resultant hip fractures related to use of TCAs, SSRIs, benzodiazepines, and antipsychotics. This is not a trivial matter; hip fractures increase the mortality rate by 12% to 20% in the year after the injury.21 The risk of falls is related to sedation, orthostatic hypotension, arrhythmias, and confusion associated with psychotropics.21,22
Akathisia and suicide. Unrecognized or undertreated akathisia is most commonly associated with antipsychotics, but also can occur with SSRIs. Although akathisia is commonly thought of as a motor syndrome of restlessness, patients may find the less-recognized psychic symptoms of increased inner turmoil and hallucinations just as distressing. This complex of symptoms is associated with an increased risk of suicide.23 If discontinuing the offending agent is not feasible, akathisia can be treated with beta blockers, benzodiazepines, or anticholinergics.24
Hepatotoxicity. Hepatotoxicity from psychotropics occurs in only a small percentage of patients, and can range from transient elevations in liver enzymes to fulminant liver failure. Adverse hepatic effects may be a manifestation of a hypersensitivity reaction accompanied by rash and eosinophilia.25 MAOIs and TCAs can cause cholestatic liver injury, whereas nefazodone has been associated with fulminant liver failure. Other psychotropics—including SSRIs, antipsychotics, benzodiazepines, and older antiepileptics—can cause negative hepatic effects but rarely are associated with acute liver failure.25,26 Although few medications can cause complete liver failure on their own, hepatotoxicity from medications may precipitate severe, potentially fatal outcomes in patients with underlying liver diseases such as hepatitis and cirrhosis. Additive hepatotoxicity from multiple medications also can be problematic. Although psychotropic-induced hepatotoxicity is rare, assess psychotropic doses in patients with liver dysfunction, because drug clearance may be altered, which increases the risk for other serious adverse events.25
Suicide assessment is key
Ongoing monitoring for current or developing suicidal ideation is an important strategy to prevent medication-related mortality in patients vulnerable to self-harm. Initial assessments and follow-up appointments should include a detailed inquiry about suicidal ideations, plans, and behaviors. Patients taking medications that carry black-box warnings for suicide risk should be seen frequently during the first few months of treatment. Patients receiving medications that are lethal in overdose (eg, lithium and TCAs) should be carefully screened for suicide risk. Prescribe medications in limited quantities or arrange for a family member to monitor the patient if necessary. Patients with a history of suicide attempts and current suicide plans may require close observation and initiating medications while hospitalized.
Other prevention strategies
Prescribing psychotropics in a manner that promotes mental well being while minimizing negative outcomes can be challenging. By developing a personal formulary of drugs commonly encountered and prescribed in their practice, psychiatrists can increase their awareness of serious safety concerns, potential DDIs, and appropriate use based on available literature.7,27
Medication histories and drug reconciliation—comparing a patient’s medication orders to all of the medications the patient has been taking—can help clinicians avoid making inappropriate dose adjustments, duplicating therapy, or prescribing medications patients previously have failed or did not tolerate. Establishing a collaborative practice environment with physicians, pharmacists, nurses, and social workers can minimize medication errors and risk of adverse outcomes by increasing communication regarding the patient’s treatment.7
Computerized drug databases and other electronic resources and consultation with pharmacists can help prescribers identify, avoid, and manage clinically significant DDIs.27 Medications could interact with other drugs as long as their effects persist in the body, which could be days to months after the drug is discontinued. Future research may lead to tools to identify patient pharmacogenetic profiles.
Recognizing psychotropic DDIs and adverse effects remains a challenge because of the complexity of the affected organ, the brain. Clinicians should be vigilant to changes in a patient’s presentation because they may be a manifestation of a medication side effect.7 Appropriate therapeutic drug monitoring should occur on a routine, scheduled basis. Closer monitoring may be necessary with dose changes, potential DDIs, signs and symptoms of toxicity/efficacy failure, and renal or hepatic function changes.
Lastly, patients’ education and involvement in their health care may increase their awareness, responsibility, and medication adherence. For challenging patients, family involvement and “eyes on” medication administration can increase adherence and prevent psychotropic misuse.
- Arizona Center for Education and Research on Therapeutics. Drugs that prolong the QT interval and/or induce Torsades de Pointes ventricular arrhythmia. www.azcert.org/medical-pros/drug-lists/drug-lists.cfm.
- Cates ME, Sims PJ. Therapeutic drug management of lithium. Am J Pharm Educ. 2005;69(5):88.
- Wren P, Frizzell LA, Keltner NL, et al. Three potentially fatal adverse effects of psychotropic medications. Perspect Psychiatr Care. 2003;39(2):75-81.
- Bishop JR, Bishop DL. How to prevent serotonin syndrome from drug-drug interactions. Current Psychiatry. 2011;10(3):81-83.
Drug Brand Names
- Amantadine • Symmetrel
- Amiodarone • Cordarone, Pacerone
- Amitriptyline • Elavil
- Amphetamine/dextroamphetamine • Adderall, others
- Aprepitant • Emend
- Aripiprazole • Abilify
- Asenapine • Saphris
- Atomoxetine • Strattera
- Bupropion • Wellbutrin, Zyban
- Carbamazepine • Tegretol, others
- Chloral hydrate • Somnote
- Chlorpromazine • Thorazine
- Cimetidine • Tagamet
- Citalopram • Celexa
- Clomipramine • Anafranil
- Clozapine • Clozaril
- Desipramine • Norpramin
- Desvenlafaxine • Pristiq
- Diltiazem • Cardia, others
- Diphenhydramine • Benadryl, others
- Doxepin • Sinequan, Silenor
- Duloxetine • Cymbalta
- Erythromycin • Ery-Tab, others
- Fluconazole • Diflucan
- Fluoxetine • Prozac
- Fluphenazine • Prolixin
- Galantamine • Razadyne
- Haloperidol • Haldol
- Iloperidone • Fanapt
- Imatinib • Gleevec
- Imipramine • Tofranil
- Isoniazid • Nydrazid, others
- Ketoconazole • Nizoral, others
- Lamotrigine • Lamictal
- Lithium • Eskalith, others
- Methadone • Dolophine, Methadose
- Methylphenidate/ dexmethylphenidate • Ritalin, others
- Mirtazapine • Remeron
- Nafcillin • Nafcil, others
- Nefazodone • Serzone
- Olanzapine • Zyprexa
- Omeprazole • Prilosec
- Oxcarbazepine • Trileptal
- Paliperidone • Invega
- Paroxetine • Paxil
- Perphenazine • Trilafon
- Phenobarbital • Luminal, others
- Phenytoin • Dilantin
- Protriptyline • Vivactil
- Quetiapine • Seroquel
- Rifampin • Rifadin, others
- Risperidone • Risperdal
- Ritonavir • Norvir
- Sertraline • Zoloft
- Thioridazine • Mellaril
- Trazodone • Desyrel, Oleptro
- Trifluoperazine • Stelazine
- Trimethoprim/Sulfamethoxazole • Bactrim, Septra
- Trimipramine • Surmontil
- Valproic acid • Depakote, others
- Venlafaxine • Effexor
- Verapamil • Calan, others
- Ziprasidone • Geodon
Disclosure
Drs. Yu and Bostwick report no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
Dr. Casher is a speaker for AstraZeneca, Pfizer Inc, and Sunovion Pharmaceuticals.
1. Procyshyn RM, Barr AM, Brickell T, et al. Medication errors in psychiatry: a comprehensive review. CNS Drugs. 2004;24(7):595-609.
2. McDonnell PJ, Jacobs MR. Hospital admissions resulting from preventable adverse drug reactions. Ann Pharmacother. 2002;36(9):1331-1336.
3. Centers for Disease Control and Prevention. Prescription drug overdose: state health agencies respond. 2008. Available at: http://www.cdc.gov/HomeandRecreationalSafety/pubs/RXReport_web-a.pdf. Accessed February 15 2011.
4. Toblin RL, Paulozzi LJ, Logan JE, et al. Mental illness and psychotropic drug use among prescription drug overdose deaths: a medical examiner chart review. J Clin Psychiatry. 2010;71(4):491-496.
5. Micromedex Healthcare Series (electronic version). 2011. Available at: http://www.micromedex.com. Accessed February 15 2011.
6. Hawton K, Bergen H, Simkin S, et al. Toxicity of antidepressants: rates of suicide relative to prescribing and non-fatal overdose. Br J Psychiatry. 2010;196(5):354-358.
7. Preskorn SH, Flockhart D. 2010 guide to psychiatric drug interactions. Primary Psychiatry. 2009;16(12):45-74.
8. Lin JH, Lu AY. Inhibition and induction of cytochrome P450 and the clinical implications. Clin Pharmacokinet. 1998;35(5):361-390.
9. Kutscher EC, Alexander B. A review of drug interactions with psychiatric medicines for the pharmacy practitioner. J Pharm Pract. 2007;20(4):327-333.
10. Wren P, Frizzell LA, Keltner NL, et al. Three potentially fatal adverse effects of psychotropic medications. Perspect Psychiatr Care. 2003;39(2):75-81.
11. Dave M, Miceli K, Modha P. Psychiatric medicine. The psychiatrist’s guide to the treatment of common medical illnesses. Philadelphia PA: Lippincott Williams & Wilkins; 2007.
12. Mir S, Taylor D. The adverse effects of antidepressants. Curr Opin Psychiatry. 1997;10(2):88-94.
13. Drug-induced long QT interval. Pharmacist’s Letter/Prescriber’s Letter. 2010;26(4):260421.-
14. Drug-induced prolongation of the QT interval and torsades de pointes. 2011. Available at: http://online.factsandcomparisons.com. Accessed February 15 2011.
15. Kales HC, Valenstein M, Kim HM, et al. Mortality risk in patients with dementia treated with antipsychotics versus other psychiatric medications. Am J Psychiatry. 2007;164(10):1568-1576; quiz 1623.
16. Merrill DB, Ahmari SE, Bradford JM, et al. Myocarditis during clozapine treatment. Am J Psychiatry. 2006;163(2):204-208.
17. Oyesanmi O, Kunkel EJ, Monti DA, et al. Hematologic side effects of psychotropics. Psychosomatics. 1999;40(5):414-421.
18. Pisani F, Oteri G, Costa C, et al. Effects of psychotropic drugs on seizure threshold. Drug Saf. 2002;25(2):91-110.
19. Martin-Latry K, Goumy M, Latry P, et al. Psychotropic drugs use and risk of heat-related hospitalization. Eur Psychiatry. 2007;22:335-338.
20. Melkersson K, Dahl ML. Adverse metabolic effects associated with atypical antipsychotics: literature review and clinical implications. Drugs. 2004;64(7):701-723.
21. Liu B, Anderson G, Mittmann N, et al. Use of selective serotonin-reuptake inhibitors or tricyclic antidepressants and risk of hip fractures in elderly people. Lancet. 1998;351(9112):1303-1307.
22. Cumming RG, Le Couteur DG. Benzodiazepines and risk of hip fractures in older people: a review of the evidence. CNS Drugs. 2003;17(11):825-837.
23. Hirose S. The causes of underdiagnosing akathisia. Schizophr Bull. 2003;29(3):547-558.
24. Kane JM, Fleischhacker WW, Hansen L, et al. Akathisia: an updated review focusing on second-generation antipsychotics. J Clin Psychiatry. 2009;70(5):627-643.
25. Selim K, Kaplowitz N. Hepatotoxicity of psychotropic drugs. Hepatology. 1999;29(5):1347-1351.
26. Chitturi S, George J. Hepatotoxicity of commonly used drugs: nonsteroidal anti-inflammatory drugs antihypertensives, antidiabetic agents, anticonvulsants, lipid-lowering agents, psychotropic drugs. Semin Liver Dis. 2002;22(2):169-183.
27. Sandson NB, Armstrong SC, Cozza KL. An overview of psychotropic drug-drug interactions. Psychosomatics. 2005;46(5):464-494.
1. Procyshyn RM, Barr AM, Brickell T, et al. Medication errors in psychiatry: a comprehensive review. CNS Drugs. 2004;24(7):595-609.
2. McDonnell PJ, Jacobs MR. Hospital admissions resulting from preventable adverse drug reactions. Ann Pharmacother. 2002;36(9):1331-1336.
3. Centers for Disease Control and Prevention. Prescription drug overdose: state health agencies respond. 2008. Available at: http://www.cdc.gov/HomeandRecreationalSafety/pubs/RXReport_web-a.pdf. Accessed February 15 2011.
4. Toblin RL, Paulozzi LJ, Logan JE, et al. Mental illness and psychotropic drug use among prescription drug overdose deaths: a medical examiner chart review. J Clin Psychiatry. 2010;71(4):491-496.
5. Micromedex Healthcare Series (electronic version). 2011. Available at: http://www.micromedex.com. Accessed February 15 2011.
6. Hawton K, Bergen H, Simkin S, et al. Toxicity of antidepressants: rates of suicide relative to prescribing and non-fatal overdose. Br J Psychiatry. 2010;196(5):354-358.
7. Preskorn SH, Flockhart D. 2010 guide to psychiatric drug interactions. Primary Psychiatry. 2009;16(12):45-74.
8. Lin JH, Lu AY. Inhibition and induction of cytochrome P450 and the clinical implications. Clin Pharmacokinet. 1998;35(5):361-390.
9. Kutscher EC, Alexander B. A review of drug interactions with psychiatric medicines for the pharmacy practitioner. J Pharm Pract. 2007;20(4):327-333.
10. Wren P, Frizzell LA, Keltner NL, et al. Three potentially fatal adverse effects of psychotropic medications. Perspect Psychiatr Care. 2003;39(2):75-81.
11. Dave M, Miceli K, Modha P. Psychiatric medicine. The psychiatrist’s guide to the treatment of common medical illnesses. Philadelphia PA: Lippincott Williams & Wilkins; 2007.
12. Mir S, Taylor D. The adverse effects of antidepressants. Curr Opin Psychiatry. 1997;10(2):88-94.
13. Drug-induced long QT interval. Pharmacist’s Letter/Prescriber’s Letter. 2010;26(4):260421.-
14. Drug-induced prolongation of the QT interval and torsades de pointes. 2011. Available at: http://online.factsandcomparisons.com. Accessed February 15 2011.
15. Kales HC, Valenstein M, Kim HM, et al. Mortality risk in patients with dementia treated with antipsychotics versus other psychiatric medications. Am J Psychiatry. 2007;164(10):1568-1576; quiz 1623.
16. Merrill DB, Ahmari SE, Bradford JM, et al. Myocarditis during clozapine treatment. Am J Psychiatry. 2006;163(2):204-208.
17. Oyesanmi O, Kunkel EJ, Monti DA, et al. Hematologic side effects of psychotropics. Psychosomatics. 1999;40(5):414-421.
18. Pisani F, Oteri G, Costa C, et al. Effects of psychotropic drugs on seizure threshold. Drug Saf. 2002;25(2):91-110.
19. Martin-Latry K, Goumy M, Latry P, et al. Psychotropic drugs use and risk of heat-related hospitalization. Eur Psychiatry. 2007;22:335-338.
20. Melkersson K, Dahl ML. Adverse metabolic effects associated with atypical antipsychotics: literature review and clinical implications. Drugs. 2004;64(7):701-723.
21. Liu B, Anderson G, Mittmann N, et al. Use of selective serotonin-reuptake inhibitors or tricyclic antidepressants and risk of hip fractures in elderly people. Lancet. 1998;351(9112):1303-1307.
22. Cumming RG, Le Couteur DG. Benzodiazepines and risk of hip fractures in older people: a review of the evidence. CNS Drugs. 2003;17(11):825-837.
23. Hirose S. The causes of underdiagnosing akathisia. Schizophr Bull. 2003;29(3):547-558.
24. Kane JM, Fleischhacker WW, Hansen L, et al. Akathisia: an updated review focusing on second-generation antipsychotics. J Clin Psychiatry. 2009;70(5):627-643.
25. Selim K, Kaplowitz N. Hepatotoxicity of psychotropic drugs. Hepatology. 1999;29(5):1347-1351.
26. Chitturi S, George J. Hepatotoxicity of commonly used drugs: nonsteroidal anti-inflammatory drugs antihypertensives, antidiabetic agents, anticonvulsants, lipid-lowering agents, psychotropic drugs. Semin Liver Dis. 2002;22(2):169-183.
27. Sandson NB, Armstrong SC, Cozza KL. An overview of psychotropic drug-drug interactions. Psychosomatics. 2005;46(5):464-494.
Benzodiazepines and stimulants for patients with substance use disorders
Although benzodiazepines and stimulants have well-documented efficacy for numerous psychiatric disorders, psychiatrists hesitate to prescribe these medications to patients with substance use disorders (SUDs)—even to those with a comorbid condition that likely would respond to a benzodiazepine or stimulant—because of risk of abuse or dependence. Conventional practice typically has focused on treating active substance use first rather than using simultaneous treatments. Prejudice, fear, and misinformation can influence this decision.
We believe these cases lie on a continuum. At one extreme, ignoring a past or present SUD may lead a remitted patient toward relapse, or further delay recovery for an active user. At the other end, psychiatrists who overreact to a remote history of substance use may deprive patients of legitimate pharmacologic symptom relief. Most cases lie somewhere in the middle.
A literature review does not support the assertion that the use of these medications leads to future substance use or worsens active use, especially for stimulants. In fact, stepwise—as opposed to concurrent—treatment for both conditions actually may delay recovery and increase patients’ risk for morbidity.
We outline issues involved in these complex clinical situations, point out controversies, review relevant research data, and offer guidelines for treatment.
CASE 1 Panic disorder in sobriety
Since he was a teen, Mr. A, age 51, drank heavily, which cost him jobs and relationships. After being convicted for driving under the influence, he was court-ordered to attend a rehabilitation facility, where, as he describes it, he “finally turned [his] life around.” He followed up residential treatment with regular attendance at Alcoholics Anonymous meetings.
After 1 year of sobriety, Mr. A develops increasingly frequent episodes of intense anxiety with sweating, nausea, chest pain, and hyperventilation and is diagnosed with panic disorder. His internist prescribes alprazolam, 0.5 mg 3 times a day, which provides some symptom relief, and refers him for follow-up psychiatric care. At his first visit, Mr. A confides to his psychiatrist that he is taking much more than the prescribed dosage of alprazolam, even when he is not experiencing anxiety, and is contemplating “buying it on the street” if his dosage is not raised to “at least 3 mg 3 times a day.”
CASE 2 Anxiety in controlled psychosis
Ms. B, age 40, had her first psychotic break at age 18 and was diagnosed with schizophrenia. Since then, she has had multiple psychiatric hospitalizations, usually presenting with auditory hallucinations and a recurring delusion that the person who calls herself Ms. B’s mother is really an actress “playing” her mother. At times this delusion has led Ms. B to attack her “imposter” mother. Over several years Ms. B began to drink heavily, but recently achieved a few months of sobriety by attending dual-diagnosis groups at her local community mental health center and individual psychotherapy sessions with her case manager. Fortunately, Ms. B’s psychosis has been stabilized with risperidone long-acting injection, 25 mg every 2 weeks, which she tolerates well.
When her beloved calico cat passes away, Ms. B experiences intense anxiety. Ms. B’s friend tells her she “needs some Valium,” but her psychiatrist, case manager, and the other patients in her dual-diagnosis group are not sure this is a good idea.
Benzodiazepines
Pros. There are multiple legitimate uses of benzodiazepines in general medicine and psychiatric practice, based upon their considerable sedative/hypnotic, anxiolytic, anticonvulsant, and muscle-relaxant properties (Table 1).1
Recommendations regarding benzodiazepine use for anxious patients with a history of SUD are not clear-cut. First, it often is difficult to determine whether the patient truly has an anxiety disorder or is suffering anxiety symptoms secondary to substance use and/or withdrawal. In addition, even if a diagnosis of a separate anxiety disorder is established, psychiatrists debate how to treat such patients. Some clinicians maintain that benzodiazepines should be used only for acute detoxification, and that ongoing benzodiazepine use will lead to relapse or benzodiazepine dependence. However, in a prospective study of 545 alcohol use disorder (AUD) patients receiving benzodiazepines for anxiety disorders, Mueller et al2 found no association—at 12 months or at 12 years—between benzodiazepine use and AUD recurrence. Furthermore, there was no difference in benzodiazepine usage when comparing patients with and without an AUD.3
Table 1
Clinical uses of benzodiazepines
| Insomnia |
| Anxiety disorders (eg, generalized anxiety disorder, panic disorder, posttraumatic stress disorder, social phobia, and obsessive-compulsive disorder) |
| Side effects of other psychiatric medications (eg, akathisia with antipsychotics or tremor with lithium) |
| Alcohol or benzodiazepine withdrawal |
| Acute agitation states, either as monotherapy or as adjuncts to antipsychotics or mood stabilizers |
| Catatonia |
| Source: Reference 1 |
Cons. Although widely prescribed—and despite their efficacy in numerous conditions— both acute or long-term benzodiazepine use frequently causes adverse effects.4 Patients may develop tolerance, which can lead to escalating dosages and/or to withdrawal symptoms when patients attempt to cut back. Benzodiazepines eventually become ineffective for sleep, and continued use can cause rebound insomnia. Also, with many patients taking benzodiazepines long-term, clinicians struggle to differentiate between “real” anxiety symptoms and subtle states of withdrawal from fluctuating benzodiazepine blood levels.5
Geriatric patients who take benzodiazepines are at risk for falls and hip fractures.4 Although older dementia patients are at particular risk for cognitive problems— including frank delirium—secondary to benzodiazepine use, patients of all ages are susceptible to these medications’ deleterious neurocognitive effects.
Benzodiazepines can lead to excessive sedation, thereby impairing performance at work or school, and have been implicated as a cause of motor vehicle accidents.6 Finally, a serious drawback to benzodiazepine use is possible lethality in overdose, especially when combined with alcohol.
Benzodiazepine prescribing should not be taken lightly. Always analyze the difference between benzodiazepines’ well-documented efficacy and their adverse effect profile. This risk-benefit analysis becomes much more complex for patients with SUDs.
Special considerations. Patients at higher risk for benzodiazepine abuse include those with:
- severe alcohol dependence (ie, long-term use, drinking since a young age [“Type II”])
- intravenous drug use
- comorbid alcoholism and antisocial personality disorder.7,8
Exercise special caution when considering benzodiazepines for patients with severe psychiatric illness such as schizophrenia-spectrum disorders, bipolar disorder, or severe depression. Patients with schizophrenia have high rates of alcohol, cocaine, cannabis, and benzodiazepine abuse.9,10 Bipolar disorder patients show similar vulnerability—up to 56% of patients screen positive for substance abuse or dependence.11 Vulnerability to addiction in severely ill psychiatric patients is thought to be related to several factors, including:
- use of drugs as self-medication
- genetic predisposition
- environment/lifestyle that supports substance abuse
- neurobiologic deficits that lead to lack of inhibition of reward-seeking behaviors.11
Bipolar disorder patients in particular score high on measures of sensation seeking, which leaves them vulnerable to abusing all classes of substances.12
In a 6-year study of 203 patients with severe psychiatric illnesses and SUDs, Brunette et al13 found that these patients were 2.5 times more likely than patients with severe psychiatric illness alone to abuse prescribed benzodiazepines. In an analysis of Medicaid records, Clark et al14 found similar vulnerability in patients with major depressive disorder (MDD) and SUD. Not only did these patients show a higher rate of benzodiazepine use than patients with MDD without SUD, but the dual-diagnosis group also gravitated toward more addictive high-potency/fast-acting benzodiazepines, such as alprazolam, estazolam, or triazolam.
Case discussion/suggestions. Initially, Mr. A may seem to be an appropriate candidate for closely monitored benzodiazepine use. However, he shows a pattern of misuse, likely related to his history of severe alcohol dependence and alprazolam use. This benzodiazepine is fast-acting and has a short half-life, and thus is highly reinforcing.
Similarly, Ms. B might benefit from benzodiazepine treatment. However, her history of schizophrenia and alcohol abuse makes her a risky candidate, and alternative treatments for anxiety symptoms should be considered. If prescribed at all, a benzodiazepine should be used only short-term (eg, 1 to 2 weeks).
In general, avoid prescribing benzodiazepines to most patients who have an ongoing or past SUD.15 Consider making an exception for SUD patients with comorbid anxiety disorders, with close monitoring of their benzodiazepine use. Clonazepam, chlordiazepoxide, clorazepate, and oxazepam may be less reinforcing for SUD patients than diazepam, lorazepam, alprazolam, estazolam, or triazolam.7,16 The drawbacks of benzodiazepines, especially in the situations described above, point to the need to find alternative treatments (Table 2).17 Keep in mind nonpharmacologic options, which completely avoid the risks of medication misuse and diversion. Cognitive-behavioral therapy (CBT), for instance, has well-documented efficacy in treating insomnia and anxiety disorders.18,19
Table 2
Alternatives to benzodiazepines for anxiety and/or insomnia
| Treatment option | Comments |
|---|---|
| CBT, relaxation techniques, sleep hygiene counseling | Many advantages to nonpharmacologic interventions (eg, fewer side effects, no risk of substance dependence) |
| Antihistamines (eg, diphenhydramine, 25 to 50 mg at bedtime* for sleep, or 2 to 3 times a day for anxiety) | Can be used for anxiety or insomnia; can cause confusion in older patients |
| Atypical antipsychotics | Off-label use; many agents in this class have metabolic side effects |
| SSRIs/SNRIs | First-line for many anxiety disorders, including panic disorder, GAD; possible weight gain and sexual side effects |
| Mirtazapine (7.5 to 30 mg at bedtime*) | Sedation side effect helps with sleep; weight gain and oversedation limit use |
| Trazodone (25 to 100 mg at bedtime*) | Commonly used off-label as a sleep aid |
| Monoamine oxidase inhibitors | May be useful for social phobia; dietary restrictions and side effects limit use |
| Doxepin (3 to 6 mg at bedtime) | Minimal anticholinergic and alpha-blockade side effects at this dose; FDA-approved for insomnia |
| Gabapentin (300 to 2,000 mg/d* in divided doses) | Off-label use, mild anxiolytic and sedative properties, relatively weight neutral |
| Beta blockers (eg, propranolol, 20 to 80 mg twice a day*) | Useful for peripheral manifestations of anxiety; may be effective for social phobias |
| Pregabalin (50 to 200 mg 3 times a day*) | Off-label use; industry-sponsored studies show comparable to SNRIs for anxiety |
| Non-benzodiazepine GABAA receptor modulators | Short-term option for primary insomnia, some abuse potential |
| Melatonin (1 to 3 mg at bedtime*) | Mild and ‘natural’ but not always an effective sleep aid |
| *Off-label approximate doses based on the authors’ clinical experience and consensus of the literature; agents listed may require slow titration and close monitoring for adverse effects CBT: cognitive-behavioral therapy; GABA: gamma-aminobutyric acid; GAD: generalized anxiety disorder; SNRI: serotoninnorepinephrine reuptake inhibitor; SSRI: selective serotonin reuptake inhibitor Source: Reference 17 | |
CASE 3 Adult ADHD and marijuana use
Mr. C, age 30, presents to a psychiatrist with ongoing complaints of inattention, fatigue, and difficulty staying organized. A self-report screen yields symptoms consistent with adult attention-deficit/hyperactivity disorder (ADHD). Mr. C’s school and job history and collateral history from his wife appear to corroborate his assertion that his symptoms have been lifelong. He later admits to regular marijuana use. After further discussion and full evaluation of his substance use, Mr. C is started on bupropion, titrated to 300 mg/d. After 2 months, despite faithful attendance at appointments and openness about his continued marijuana use, Mr. C’s symptoms remain unchanged. He asks about atomoxetine.
Stimulants
Pros. Despite many clinicians’ hesitance to prescribe controlled substances to patients with SUDs, psychostimulants should be considered in a variety of scenarios. Although nonstimulant options are available, stimulants consistently have demonstrated superior efficacy over other treatments and remain first-line agents for adult ADHD.20 Methylphenidate, mixed amphetamine salts, lisdexamfetamine, and atomoxetine are FDA-approved for adult ADHD. Both stimulant classes (methylphenidate and amphetamine-based products) are equally effective for ADHD. In addition, stimulants are used to treat narcolepsy, cognitive disorders such as traumatic brain injury, and as augmentation to antidepressants for MDD.
ADHD affects 5% to 12% of children, and >60% of patients remain symptomatic into adulthood and require continued treatment.21 In particular, problematic inattention may persist throughout adulthood. ADHD does not appear to be an independent risk factor for SUDs in children and adolescents.22 However, substance use increases sharply as ADHD patients enter late adolescence and adulthood, and eventually becomes a problem for 20% of adolescents and adults with ADHD. Conversely, 17% to 50% of patients with alcohol, cocaine, or opioid dependence have co-occurring ADHD.23
Withholding ADHD treatment based on concerns about future or increased current substance abuse is unfounded. A meta-analysis of 6 studies that included 674 medicated and 360 unmedicated patients with ADHD who were followed at least 4 years demonstrated that childhood treatment of ADHD with stimulants reduces the risk of developing alcohol and other drug disorders in adulthood.24 Regarding the effect stimulants have on active substance use, a 12-week, double-blind, randomized controlled trial of 48 cocaine-dependent adults with ADHD showed methylphenidate did not change cocaine abuse or craving, but did improve ADHD symptoms.25
Clinicians also must assess whether untreated ADHD symptoms impair patients’ work or other activities. Driving is a particular concern because ADHD is associated with risky driving habits, motor vehicle accidents, traffic violations, and driving license suspensions.26 In a study that administered cognitive tests to 27 adults with ADHD, methylphenidate treatment improved cognitive performance related to driving (eg, better visual-motor coordination under high-stress conditions, improved visual orientation, and sustained visual attention).27 It is likely this effect could be generalized to other activities where safety is important. Finally, appropriate stimulant treatment may improve participation in rehabilitative programs.
Cons. Despite their positive effects, stimulants can have adverse effects and consequences.28 In routinely prescribed dosages, methylphenidate and amphetamines can cause symptoms related to sympathetic activation, including anxiety, tics, anorexia/ weight loss, and sleep disturbance. A 5-year study of 79 school-age children prescribed methylphenidate, dextroamphetamine, or pemoline, which is no longer available in the United States, showed a significant association between adherence to stimulants and persistence of physiological (eg, headaches, insomnia, anorexia) and mood-related (eg, irritability, dysphoria) side effects.29 Stimulants’ sympathomimetic properties also can lead to dangerous drug-drug interactions with monoamine oxidase inhibitors. For both methylphenidate and amphetamines, overdose can lead to seizures, cardiac toxicity, dysrhythmias, and hyperthermia. All stimulants carry an FDA “black-box” warning that lists increased risk of cardiac complications, sudden death, and psychiatric complications such as psychosis or mania.30
Special considerations. All stimulants have potential for diversion or abuse. Pay close attention to these issues, especially in vulnerable populations and situations where rates of abuse and diversion are elevated. Among college students, white patients, fraternity/sorority members, and individuals with lower grade point averages may be at higher risk for nonmedical stimulant use.31 Adults who misuse or divert stimulants commonly have a history of substance abuse and conduct disorder.32 Short-acting stimulants are abused 4 times more often than extended-release preparations.33
If your ADHD patient has active substance use, be clear that continued substance use is likely to limit stimulants’ effectiveness. In patients who are actively using substances, it will be difficult to disentangle apparent nonresponse to stimulants from the negative cognitive effects of substance use.
Case discussion/suggestions. As Mr. C’s case illustrates, there are alternatives to stimulants for ADHD. For example, atomoxetine, a selective norepinephrine reuptake inhibitor, may be considered a first-line agent in patients with mostly inattentive ADHD symptoms and comorbid stimulant abuse, or for those in whom stimulants cause adverse effects such as mood lability or tics.34 Other alternatives to stimulants are listed in Table 3.35
Because Mr. C did not respond to bupropion, which presumably was tried first because of his ongoing substance use, he asked about atomoxetine. This agent is not addictive and there is no evidence that it leads to or exacerbates substance use. Depending on Mr. C’s symptom profile, atomoxetine might be a good choice. Continued monitoring of his marijuana use and frequent assessment of his motivation to quit are necessary. Psychoeducation about the cognitive effects of marijuana, including inattention and poor concentration, is important.
If Mr. C does not respond to atomoxetine, his psychiatrist will face a difficult decision. Setting Mr. C’s marijuana use aside, symptoms that do not respond to atomoxetine or a second-line agent are likely to respond to a stimulant. However, several issues must be addressed. If Mr. C’s motivation to stop using marijuana is low, how motivated is he to improve his ADHD symptoms? Next, would marijuana’s depressive/blunting effects counteract the anticipated benefit of a stimulant? Also, what is the risk that Mr. C might sell or exchange his stimulants to obtain marijuana? Assessing these complicated questions is key. Another important factor in Mr. C’s case is his wife’s involvement. Does she monitor his marijuana use? Would she be willing to supervise Mr. C’s stimulant use, and would he allow it?
Past or present SUDs are not an absolute contraindication to stimulant use. You should affirm the diagnosis and identify target symptoms. Consider nonstimulant alternatives if appropriate.
Table 3
Alternatives to stimulants for ADHD
| Treatment option | Comments |
|---|---|
| Atomoxetine | Effectiveness may be limited to inattentive type |
| Modafinil | Well-tolerated but expensive, limited evidence, no FDA indication; may be a consideration in ADHD + SUD |
| α2-adrenergic agonist (eg, clonidine or guanfacine) | Useful when hyperactivity/impulsivity symptoms predominate, or when stimulant-induced insomnia occurs |
| Bupropion | Some evidence of mild efficacy, especially useful if nicotine dependence also is a target for treatment |
| Psychotherapy | Can be useful as adjunctive treatment, but as monotherapy it is of little benefit in ADHD |
| ADHD: attention-deficit/hyperactivity disorder; SUD: substance abuse disorder Source: Reference 35 | |
Legal liabilities
Being aware of the medicolegal issues of benzodiazepine and/or stimulant prescribing is crucial because a court may find a psychiatrist liable for negative outcomes (eg, suicide) when controlled substances are prescribed to a patient with a history of addiction.36 The most prudent course is to weigh the pros and cons for each patient individually, taking into consideration the factors described above.8 This is consistent with guidelines from the American Psychiatric Association and the British Association for Psychopharmacology,37 both of which call for extreme caution in these cases.
Educate patients and caregivers about the risks of taking a controlled substance, including misuse, diversion, and theft. Provide and document explicit instructions that the patient will receive stimulants from only a single provider. Remind patients that state and federal authorities closely track controlled medications. Finally, a “stimulant contract” or “benzodiazepine contract,” similar to a pain or narcotic contact, may be useful to formally document discussions about appropriate medication use.
Related Resources
- National Institute on Drug Abuse. Prescription drugs: abuse and addiction. Research Report Series, 2005. http://drugabuse.gov/ResearchReports/Prescription/Prescription.html.
- Galanter M, Kleber HD. The American Psychiatric Publishing textbook of substance abuse treatment. 4th ed. Arlington, VA: American Psychiatric Publishing, Inc; 2008.
Drug Brand Names
- Alprazolam • Xanax
- Atomoxetine • Strattera
- Bupropion • Wellbutrin, others
- Chlordiazepoxide • Librium
- Clonazepam • Klonopin
- Clonidine • Catapres
- Clorazepate • Tranxene
- Dextroamphetamine • Dexedrine
- Diazepam • Valium
- Diphenhydramine • Benadryl, others
- Doxepin • Silenor
- Estazolam • ProSom
- Gabapentin • Neurontin
- Guanfacine • Tenex, Intuniv
- Lisdexamfetamine • Vyvanse
- Lithium • Eskalith, Lithobid
- Lorazepam • Ativan
- Methylphenidate • Ritalin, Concerta, others
- Mirtazapine • Remeron
- Mixed amphetamine salts • Adderall
- Modafinil • Provigil
- Oxazepam • Serax
- Pemoline • Cylert
- Propranolol • Inderal
- Trazodone • Desyrel, Oleptro
- Triazolam • Halcion
Disclosures
Dr. Casher is a speaker for AstraZeneca and Pfizer Inc.
Drs. Gih and Bess report no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
1. Ashton H. Guidelines for the rational use of benzodiazepines. When and what to use. Drugs. 1994;48(1):25.-
2. Mueller TI, Pagano ME, Rodriguez BF, et al. Long-term use of benzodiazepines in participants with comorbid anxiety and alcohol use disorders. Alcohol Clin Exp Res. 2005;29(8):1411-1418.
3. Mueller TI, Goldenberg IM, Gordon AL, et al. Benzodiazepine use in anxiety disordered patients with and without a history of alcoholism. J Clin Psychiatry. 1996;57(2):83-89.
4. Ashton H. The diagnosis and management of benzodiazepine dependence. Curr Opin Psychiatry. 2005;(18):249-255.
5. Back SE, Brady KT. Anxiety disorders with comorbid substance use disorders: diagnostic and treatment considerations. Psychiatric Annals. 2008;38(11):724-729.
6. Walsh JM, Flegel R, Cangianelli LA, et al. Epidemiology of alcohol and other drug use among motor vehicle crash victims admitted to a trauma center. Traffic Inj Prev. 2004;5(3):254-260.
7. Ciraulo DA, Nace EP. Benzodiazepine treatment of anxiety or insomnia in substance abuse patients. Am J Addict. 2000;9(4):276-279;discussion 280–284.
8. Sattar S, Bhatia S. Benzodiazepines for substance abusers. Current Psychiatry. 2003;2(5):25-34.
9. Regier DA, Farmer ME, Rae DS, et al. Comorbidity of mental disorders with alcohol and other drug abuse. Results from the Epidemiologic Catchment Area (ECA) Study. JAMA. 1990;264(19):2511-2518.
10. Kendler KS, Gallagher TJ, Abelson JM, et al. Lifetime prevalence, demographic risk factors, and diagnostic validity of nonaffective psychosis as assessed in a US community sample. The National Comorbidity Survey. Arch Gen Psychiatry. 1996;53(11):1022-1031
11. Buckley PF. Prevalence and consequences of the dual diagnosis of substance abuse and severe mental illness. J Clin Psychiatry. 2006;67(suppl 7):5-9.
12. Bizzarri JV, Sbrana A, Rucci P, et al. The spectrum of substance abuse in bipolar disorder: reasons for use, sensation seeking and substance sensitivity. Bipolar Disord. 2007;9(3):213-220.
13. Brunette MF, Noordsy DL, Xie H, et al. Benzodiazepine use and abuse among patients with severe mental illness and co-occurring substance use disorders. Psychiatr Serv. 2003;54(10):1395-1401.
14. Clark RE, Xie H, Brunette MF, et al. Benzodiazepine prescription practices and substance abuse in persons with severe mental illness. J Clin Psychiatry. 2004;65(2):151-155.
15. Longo LP. Addiction: part I. Benzodiazepines—side effects abuse risk and alternatives. Am Fam Physician. 2000;61(7):2121-2128.
16. Ciraulo DA, Barnhill JG, Ciraulo AM, et al. Alterations in pharmacodynamics of anxiolytics in abstinent alcoholic men: subjective responses, abuse liability, and electroencephalographic effects of alprazolam, diazepam, and buspirone. J Clin Pharmacol. 1997;37(1):64-73.
17. Casher MI, Bess JD. Manual of inpatient psychiatry. Cambridge United Kingdom: Cambridge University Press; 2010.
18. Hofmann S, Smits JA. Cognitive-behavioral therapy for adult anxiety disorders: a meta-analysis of randomized placebo-controlled trials. J Clin Psychiatry. 2008;69(4):621-632.
19. Morgenthaler T, Kramer M, Alessi C, et al. Practice parameters for the psychological and behavioral treatment of insomnia: an update. An American Academy of Sleep Medicine report. Sleep. 2006;29(11):1415-1419.
20. Wilens TE. Drug therapy for adults with attention-deficit hyperactivity disorder. Drugs. 2003;63(22):2395-2411.
21. Faraone SV, Biederman J, Mick E. The age-dependent decline of attention deficit hyperactivity disorder: a meta-analysis of follow-up studies. Psychol Med. 2006;36(2):159-165.
22. Biederman J, Wilens T, Mick E, et al. Is ADHD a risk factor for psychoactive substance use disorders? Findings from a four-year prospective follow-up study. J Am Acad Child Adolesc Psychiatry. 1997;36(1):21-29.
23. Waid L, Johnson D, Anton R. Attention-deficit hyperactivity disorder and substance abuse. In: Kranzler HR Rounsaville BJ, eds. Dual diagnosis and treatment: substance abuse and comorbid medical and psychiatric disorders. vol 8. New York, NY: Marcel Dekker; 1998:393–425.
24. Wilens TE, Faraone SV, Biederman J, et al. Does stimulant therapy of attention-deficit/hyperactivity disorder beget later substance abuse? A meta-analytic review of the literature. Pediatrics. 2003;111(1):179-185.
25. Schubiner H, Saules KK, Arfken CL, et al. Double-blind placebo-controlled trial of methylphenidate in the treatment of adult ADHD patients with comorbid cocaine dependence. Exp Clin Psychopharmacol. 2002;10(3):286-294.
26. Barkley RA, Murphy KR, Kwasnik D. Motor vehicle driving competencies and risks in teens and young adults with attention deficit hyperactivity disorder. Pediatrics. 1996;98(6 Pt 1):1089-1095.
27. Sobanski E, Sabljic D, Alm B, et al. Driving-related risks and impact of methylphenidate treatment on driving in adults with attention-deficit/hyperactivity disorder (ADHD). J Neural Transm. 2008;115(2):347-356.
28. Leonard BE, McCartan D, White J, et al. Methylphenidate: a review of its neuropharmacological, neuropsychological and adverse clinical effects. Hum Psychopharmacol. 2004;19(3):151-180.
29. Charach A, Ickowicz A, Schachar R. Stimulant treatment over five years: adherence effectiveness, and adverse effects. J Am Acad Child Adolesc Psychiatry. 2004;43(5):559-567.
30. Schatzberg AF, Nemeroff CB. The American Psychiatric Publishing textbook of psychopharmacology. 4th ed. Arlington VA: American Psychiatric Publishing, Inc; 2009.
31. Wilens TE, Adler LA, Adams J, et al. Misuse and diversion of stimulants prescribed for ADHD: a systematic review of the literature. J Am Acad Child Adolesc Psychiatry. 2008;47(1):21-31.
32. Wilens TE, Gignac M, Swezey A, et al. Characteristics of adolescents and young adults with ADHD who divert or misuse their prescribed medications. J Am Acad Child Adolesc Psychiatry. 2006;45(4):408-414.
33. Bright GM. Abuse of medications employed for the treatment of ADHD: results from a large-scale community survey. Medscape J Med. 2008;10(5):111.-
34. Biederman J, Spencer T, Wilens T. Evidence-based pharmacotherapy for attention-deficit hyperactivity disorder. Int J Neuropsychopharmacol. 2004;7(1):77-97.
35. Mann N, Bitsios P. Modafinil treatment of amphetamine abuse in adult ADHD. J Psychopharmacol. 2009;23(4):468-471.
36. Grant JE. Prudent prescribing for patients with addictions. Current Psychiatry. 2006;5(10):99-102.
37. Lingford-Hughes AR, Welch S, Nutt DJ. and the British Association for Psychopharmacology. Evidence-based guidelines for the pharmacological management of substance misuse addiction and comorbidity: recommendations from the British Association for Psychopharmacology. J Psychopharmacol. 2004;18(3):293-335.
Although benzodiazepines and stimulants have well-documented efficacy for numerous psychiatric disorders, psychiatrists hesitate to prescribe these medications to patients with substance use disorders (SUDs)—even to those with a comorbid condition that likely would respond to a benzodiazepine or stimulant—because of risk of abuse or dependence. Conventional practice typically has focused on treating active substance use first rather than using simultaneous treatments. Prejudice, fear, and misinformation can influence this decision.
We believe these cases lie on a continuum. At one extreme, ignoring a past or present SUD may lead a remitted patient toward relapse, or further delay recovery for an active user. At the other end, psychiatrists who overreact to a remote history of substance use may deprive patients of legitimate pharmacologic symptom relief. Most cases lie somewhere in the middle.
A literature review does not support the assertion that the use of these medications leads to future substance use or worsens active use, especially for stimulants. In fact, stepwise—as opposed to concurrent—treatment for both conditions actually may delay recovery and increase patients’ risk for morbidity.
We outline issues involved in these complex clinical situations, point out controversies, review relevant research data, and offer guidelines for treatment.
CASE 1 Panic disorder in sobriety
Since he was a teen, Mr. A, age 51, drank heavily, which cost him jobs and relationships. After being convicted for driving under the influence, he was court-ordered to attend a rehabilitation facility, where, as he describes it, he “finally turned [his] life around.” He followed up residential treatment with regular attendance at Alcoholics Anonymous meetings.
After 1 year of sobriety, Mr. A develops increasingly frequent episodes of intense anxiety with sweating, nausea, chest pain, and hyperventilation and is diagnosed with panic disorder. His internist prescribes alprazolam, 0.5 mg 3 times a day, which provides some symptom relief, and refers him for follow-up psychiatric care. At his first visit, Mr. A confides to his psychiatrist that he is taking much more than the prescribed dosage of alprazolam, even when he is not experiencing anxiety, and is contemplating “buying it on the street” if his dosage is not raised to “at least 3 mg 3 times a day.”
CASE 2 Anxiety in controlled psychosis
Ms. B, age 40, had her first psychotic break at age 18 and was diagnosed with schizophrenia. Since then, she has had multiple psychiatric hospitalizations, usually presenting with auditory hallucinations and a recurring delusion that the person who calls herself Ms. B’s mother is really an actress “playing” her mother. At times this delusion has led Ms. B to attack her “imposter” mother. Over several years Ms. B began to drink heavily, but recently achieved a few months of sobriety by attending dual-diagnosis groups at her local community mental health center and individual psychotherapy sessions with her case manager. Fortunately, Ms. B’s psychosis has been stabilized with risperidone long-acting injection, 25 mg every 2 weeks, which she tolerates well.
When her beloved calico cat passes away, Ms. B experiences intense anxiety. Ms. B’s friend tells her she “needs some Valium,” but her psychiatrist, case manager, and the other patients in her dual-diagnosis group are not sure this is a good idea.
Benzodiazepines
Pros. There are multiple legitimate uses of benzodiazepines in general medicine and psychiatric practice, based upon their considerable sedative/hypnotic, anxiolytic, anticonvulsant, and muscle-relaxant properties (Table 1).1
Recommendations regarding benzodiazepine use for anxious patients with a history of SUD are not clear-cut. First, it often is difficult to determine whether the patient truly has an anxiety disorder or is suffering anxiety symptoms secondary to substance use and/or withdrawal. In addition, even if a diagnosis of a separate anxiety disorder is established, psychiatrists debate how to treat such patients. Some clinicians maintain that benzodiazepines should be used only for acute detoxification, and that ongoing benzodiazepine use will lead to relapse or benzodiazepine dependence. However, in a prospective study of 545 alcohol use disorder (AUD) patients receiving benzodiazepines for anxiety disorders, Mueller et al2 found no association—at 12 months or at 12 years—between benzodiazepine use and AUD recurrence. Furthermore, there was no difference in benzodiazepine usage when comparing patients with and without an AUD.3
Table 1
Clinical uses of benzodiazepines
| Insomnia |
| Anxiety disorders (eg, generalized anxiety disorder, panic disorder, posttraumatic stress disorder, social phobia, and obsessive-compulsive disorder) |
| Side effects of other psychiatric medications (eg, akathisia with antipsychotics or tremor with lithium) |
| Alcohol or benzodiazepine withdrawal |
| Acute agitation states, either as monotherapy or as adjuncts to antipsychotics or mood stabilizers |
| Catatonia |
| Source: Reference 1 |
Cons. Although widely prescribed—and despite their efficacy in numerous conditions— both acute or long-term benzodiazepine use frequently causes adverse effects.4 Patients may develop tolerance, which can lead to escalating dosages and/or to withdrawal symptoms when patients attempt to cut back. Benzodiazepines eventually become ineffective for sleep, and continued use can cause rebound insomnia. Also, with many patients taking benzodiazepines long-term, clinicians struggle to differentiate between “real” anxiety symptoms and subtle states of withdrawal from fluctuating benzodiazepine blood levels.5
Geriatric patients who take benzodiazepines are at risk for falls and hip fractures.4 Although older dementia patients are at particular risk for cognitive problems— including frank delirium—secondary to benzodiazepine use, patients of all ages are susceptible to these medications’ deleterious neurocognitive effects.
Benzodiazepines can lead to excessive sedation, thereby impairing performance at work or school, and have been implicated as a cause of motor vehicle accidents.6 Finally, a serious drawback to benzodiazepine use is possible lethality in overdose, especially when combined with alcohol.
Benzodiazepine prescribing should not be taken lightly. Always analyze the difference between benzodiazepines’ well-documented efficacy and their adverse effect profile. This risk-benefit analysis becomes much more complex for patients with SUDs.
Special considerations. Patients at higher risk for benzodiazepine abuse include those with:
- severe alcohol dependence (ie, long-term use, drinking since a young age [“Type II”])
- intravenous drug use
- comorbid alcoholism and antisocial personality disorder.7,8
Exercise special caution when considering benzodiazepines for patients with severe psychiatric illness such as schizophrenia-spectrum disorders, bipolar disorder, or severe depression. Patients with schizophrenia have high rates of alcohol, cocaine, cannabis, and benzodiazepine abuse.9,10 Bipolar disorder patients show similar vulnerability—up to 56% of patients screen positive for substance abuse or dependence.11 Vulnerability to addiction in severely ill psychiatric patients is thought to be related to several factors, including:
- use of drugs as self-medication
- genetic predisposition
- environment/lifestyle that supports substance abuse
- neurobiologic deficits that lead to lack of inhibition of reward-seeking behaviors.11
Bipolar disorder patients in particular score high on measures of sensation seeking, which leaves them vulnerable to abusing all classes of substances.12
In a 6-year study of 203 patients with severe psychiatric illnesses and SUDs, Brunette et al13 found that these patients were 2.5 times more likely than patients with severe psychiatric illness alone to abuse prescribed benzodiazepines. In an analysis of Medicaid records, Clark et al14 found similar vulnerability in patients with major depressive disorder (MDD) and SUD. Not only did these patients show a higher rate of benzodiazepine use than patients with MDD without SUD, but the dual-diagnosis group also gravitated toward more addictive high-potency/fast-acting benzodiazepines, such as alprazolam, estazolam, or triazolam.
Case discussion/suggestions. Initially, Mr. A may seem to be an appropriate candidate for closely monitored benzodiazepine use. However, he shows a pattern of misuse, likely related to his history of severe alcohol dependence and alprazolam use. This benzodiazepine is fast-acting and has a short half-life, and thus is highly reinforcing.
Similarly, Ms. B might benefit from benzodiazepine treatment. However, her history of schizophrenia and alcohol abuse makes her a risky candidate, and alternative treatments for anxiety symptoms should be considered. If prescribed at all, a benzodiazepine should be used only short-term (eg, 1 to 2 weeks).
In general, avoid prescribing benzodiazepines to most patients who have an ongoing or past SUD.15 Consider making an exception for SUD patients with comorbid anxiety disorders, with close monitoring of their benzodiazepine use. Clonazepam, chlordiazepoxide, clorazepate, and oxazepam may be less reinforcing for SUD patients than diazepam, lorazepam, alprazolam, estazolam, or triazolam.7,16 The drawbacks of benzodiazepines, especially in the situations described above, point to the need to find alternative treatments (Table 2).17 Keep in mind nonpharmacologic options, which completely avoid the risks of medication misuse and diversion. Cognitive-behavioral therapy (CBT), for instance, has well-documented efficacy in treating insomnia and anxiety disorders.18,19
Table 2
Alternatives to benzodiazepines for anxiety and/or insomnia
| Treatment option | Comments |
|---|---|
| CBT, relaxation techniques, sleep hygiene counseling | Many advantages to nonpharmacologic interventions (eg, fewer side effects, no risk of substance dependence) |
| Antihistamines (eg, diphenhydramine, 25 to 50 mg at bedtime* for sleep, or 2 to 3 times a day for anxiety) | Can be used for anxiety or insomnia; can cause confusion in older patients |
| Atypical antipsychotics | Off-label use; many agents in this class have metabolic side effects |
| SSRIs/SNRIs | First-line for many anxiety disorders, including panic disorder, GAD; possible weight gain and sexual side effects |
| Mirtazapine (7.5 to 30 mg at bedtime*) | Sedation side effect helps with sleep; weight gain and oversedation limit use |
| Trazodone (25 to 100 mg at bedtime*) | Commonly used off-label as a sleep aid |
| Monoamine oxidase inhibitors | May be useful for social phobia; dietary restrictions and side effects limit use |
| Doxepin (3 to 6 mg at bedtime) | Minimal anticholinergic and alpha-blockade side effects at this dose; FDA-approved for insomnia |
| Gabapentin (300 to 2,000 mg/d* in divided doses) | Off-label use, mild anxiolytic and sedative properties, relatively weight neutral |
| Beta blockers (eg, propranolol, 20 to 80 mg twice a day*) | Useful for peripheral manifestations of anxiety; may be effective for social phobias |
| Pregabalin (50 to 200 mg 3 times a day*) | Off-label use; industry-sponsored studies show comparable to SNRIs for anxiety |
| Non-benzodiazepine GABAA receptor modulators | Short-term option for primary insomnia, some abuse potential |
| Melatonin (1 to 3 mg at bedtime*) | Mild and ‘natural’ but not always an effective sleep aid |
| *Off-label approximate doses based on the authors’ clinical experience and consensus of the literature; agents listed may require slow titration and close monitoring for adverse effects CBT: cognitive-behavioral therapy; GABA: gamma-aminobutyric acid; GAD: generalized anxiety disorder; SNRI: serotoninnorepinephrine reuptake inhibitor; SSRI: selective serotonin reuptake inhibitor Source: Reference 17 | |
CASE 3 Adult ADHD and marijuana use
Mr. C, age 30, presents to a psychiatrist with ongoing complaints of inattention, fatigue, and difficulty staying organized. A self-report screen yields symptoms consistent with adult attention-deficit/hyperactivity disorder (ADHD). Mr. C’s school and job history and collateral history from his wife appear to corroborate his assertion that his symptoms have been lifelong. He later admits to regular marijuana use. After further discussion and full evaluation of his substance use, Mr. C is started on bupropion, titrated to 300 mg/d. After 2 months, despite faithful attendance at appointments and openness about his continued marijuana use, Mr. C’s symptoms remain unchanged. He asks about atomoxetine.
Stimulants
Pros. Despite many clinicians’ hesitance to prescribe controlled substances to patients with SUDs, psychostimulants should be considered in a variety of scenarios. Although nonstimulant options are available, stimulants consistently have demonstrated superior efficacy over other treatments and remain first-line agents for adult ADHD.20 Methylphenidate, mixed amphetamine salts, lisdexamfetamine, and atomoxetine are FDA-approved for adult ADHD. Both stimulant classes (methylphenidate and amphetamine-based products) are equally effective for ADHD. In addition, stimulants are used to treat narcolepsy, cognitive disorders such as traumatic brain injury, and as augmentation to antidepressants for MDD.
ADHD affects 5% to 12% of children, and >60% of patients remain symptomatic into adulthood and require continued treatment.21 In particular, problematic inattention may persist throughout adulthood. ADHD does not appear to be an independent risk factor for SUDs in children and adolescents.22 However, substance use increases sharply as ADHD patients enter late adolescence and adulthood, and eventually becomes a problem for 20% of adolescents and adults with ADHD. Conversely, 17% to 50% of patients with alcohol, cocaine, or opioid dependence have co-occurring ADHD.23
Withholding ADHD treatment based on concerns about future or increased current substance abuse is unfounded. A meta-analysis of 6 studies that included 674 medicated and 360 unmedicated patients with ADHD who were followed at least 4 years demonstrated that childhood treatment of ADHD with stimulants reduces the risk of developing alcohol and other drug disorders in adulthood.24 Regarding the effect stimulants have on active substance use, a 12-week, double-blind, randomized controlled trial of 48 cocaine-dependent adults with ADHD showed methylphenidate did not change cocaine abuse or craving, but did improve ADHD symptoms.25
Clinicians also must assess whether untreated ADHD symptoms impair patients’ work or other activities. Driving is a particular concern because ADHD is associated with risky driving habits, motor vehicle accidents, traffic violations, and driving license suspensions.26 In a study that administered cognitive tests to 27 adults with ADHD, methylphenidate treatment improved cognitive performance related to driving (eg, better visual-motor coordination under high-stress conditions, improved visual orientation, and sustained visual attention).27 It is likely this effect could be generalized to other activities where safety is important. Finally, appropriate stimulant treatment may improve participation in rehabilitative programs.
Cons. Despite their positive effects, stimulants can have adverse effects and consequences.28 In routinely prescribed dosages, methylphenidate and amphetamines can cause symptoms related to sympathetic activation, including anxiety, tics, anorexia/ weight loss, and sleep disturbance. A 5-year study of 79 school-age children prescribed methylphenidate, dextroamphetamine, or pemoline, which is no longer available in the United States, showed a significant association between adherence to stimulants and persistence of physiological (eg, headaches, insomnia, anorexia) and mood-related (eg, irritability, dysphoria) side effects.29 Stimulants’ sympathomimetic properties also can lead to dangerous drug-drug interactions with monoamine oxidase inhibitors. For both methylphenidate and amphetamines, overdose can lead to seizures, cardiac toxicity, dysrhythmias, and hyperthermia. All stimulants carry an FDA “black-box” warning that lists increased risk of cardiac complications, sudden death, and psychiatric complications such as psychosis or mania.30
Special considerations. All stimulants have potential for diversion or abuse. Pay close attention to these issues, especially in vulnerable populations and situations where rates of abuse and diversion are elevated. Among college students, white patients, fraternity/sorority members, and individuals with lower grade point averages may be at higher risk for nonmedical stimulant use.31 Adults who misuse or divert stimulants commonly have a history of substance abuse and conduct disorder.32 Short-acting stimulants are abused 4 times more often than extended-release preparations.33
If your ADHD patient has active substance use, be clear that continued substance use is likely to limit stimulants’ effectiveness. In patients who are actively using substances, it will be difficult to disentangle apparent nonresponse to stimulants from the negative cognitive effects of substance use.
Case discussion/suggestions. As Mr. C’s case illustrates, there are alternatives to stimulants for ADHD. For example, atomoxetine, a selective norepinephrine reuptake inhibitor, may be considered a first-line agent in patients with mostly inattentive ADHD symptoms and comorbid stimulant abuse, or for those in whom stimulants cause adverse effects such as mood lability or tics.34 Other alternatives to stimulants are listed in Table 3.35
Because Mr. C did not respond to bupropion, which presumably was tried first because of his ongoing substance use, he asked about atomoxetine. This agent is not addictive and there is no evidence that it leads to or exacerbates substance use. Depending on Mr. C’s symptom profile, atomoxetine might be a good choice. Continued monitoring of his marijuana use and frequent assessment of his motivation to quit are necessary. Psychoeducation about the cognitive effects of marijuana, including inattention and poor concentration, is important.
If Mr. C does not respond to atomoxetine, his psychiatrist will face a difficult decision. Setting Mr. C’s marijuana use aside, symptoms that do not respond to atomoxetine or a second-line agent are likely to respond to a stimulant. However, several issues must be addressed. If Mr. C’s motivation to stop using marijuana is low, how motivated is he to improve his ADHD symptoms? Next, would marijuana’s depressive/blunting effects counteract the anticipated benefit of a stimulant? Also, what is the risk that Mr. C might sell or exchange his stimulants to obtain marijuana? Assessing these complicated questions is key. Another important factor in Mr. C’s case is his wife’s involvement. Does she monitor his marijuana use? Would she be willing to supervise Mr. C’s stimulant use, and would he allow it?
Past or present SUDs are not an absolute contraindication to stimulant use. You should affirm the diagnosis and identify target symptoms. Consider nonstimulant alternatives if appropriate.
Table 3
Alternatives to stimulants for ADHD
| Treatment option | Comments |
|---|---|
| Atomoxetine | Effectiveness may be limited to inattentive type |
| Modafinil | Well-tolerated but expensive, limited evidence, no FDA indication; may be a consideration in ADHD + SUD |
| α2-adrenergic agonist (eg, clonidine or guanfacine) | Useful when hyperactivity/impulsivity symptoms predominate, or when stimulant-induced insomnia occurs |
| Bupropion | Some evidence of mild efficacy, especially useful if nicotine dependence also is a target for treatment |
| Psychotherapy | Can be useful as adjunctive treatment, but as monotherapy it is of little benefit in ADHD |
| ADHD: attention-deficit/hyperactivity disorder; SUD: substance abuse disorder Source: Reference 35 | |
Legal liabilities
Being aware of the medicolegal issues of benzodiazepine and/or stimulant prescribing is crucial because a court may find a psychiatrist liable for negative outcomes (eg, suicide) when controlled substances are prescribed to a patient with a history of addiction.36 The most prudent course is to weigh the pros and cons for each patient individually, taking into consideration the factors described above.8 This is consistent with guidelines from the American Psychiatric Association and the British Association for Psychopharmacology,37 both of which call for extreme caution in these cases.
Educate patients and caregivers about the risks of taking a controlled substance, including misuse, diversion, and theft. Provide and document explicit instructions that the patient will receive stimulants from only a single provider. Remind patients that state and federal authorities closely track controlled medications. Finally, a “stimulant contract” or “benzodiazepine contract,” similar to a pain or narcotic contact, may be useful to formally document discussions about appropriate medication use.
Related Resources
- National Institute on Drug Abuse. Prescription drugs: abuse and addiction. Research Report Series, 2005. http://drugabuse.gov/ResearchReports/Prescription/Prescription.html.
- Galanter M, Kleber HD. The American Psychiatric Publishing textbook of substance abuse treatment. 4th ed. Arlington, VA: American Psychiatric Publishing, Inc; 2008.
Drug Brand Names
- Alprazolam • Xanax
- Atomoxetine • Strattera
- Bupropion • Wellbutrin, others
- Chlordiazepoxide • Librium
- Clonazepam • Klonopin
- Clonidine • Catapres
- Clorazepate • Tranxene
- Dextroamphetamine • Dexedrine
- Diazepam • Valium
- Diphenhydramine • Benadryl, others
- Doxepin • Silenor
- Estazolam • ProSom
- Gabapentin • Neurontin
- Guanfacine • Tenex, Intuniv
- Lisdexamfetamine • Vyvanse
- Lithium • Eskalith, Lithobid
- Lorazepam • Ativan
- Methylphenidate • Ritalin, Concerta, others
- Mirtazapine • Remeron
- Mixed amphetamine salts • Adderall
- Modafinil • Provigil
- Oxazepam • Serax
- Pemoline • Cylert
- Propranolol • Inderal
- Trazodone • Desyrel, Oleptro
- Triazolam • Halcion
Disclosures
Dr. Casher is a speaker for AstraZeneca and Pfizer Inc.
Drs. Gih and Bess report no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
Although benzodiazepines and stimulants have well-documented efficacy for numerous psychiatric disorders, psychiatrists hesitate to prescribe these medications to patients with substance use disorders (SUDs)—even to those with a comorbid condition that likely would respond to a benzodiazepine or stimulant—because of risk of abuse or dependence. Conventional practice typically has focused on treating active substance use first rather than using simultaneous treatments. Prejudice, fear, and misinformation can influence this decision.
We believe these cases lie on a continuum. At one extreme, ignoring a past or present SUD may lead a remitted patient toward relapse, or further delay recovery for an active user. At the other end, psychiatrists who overreact to a remote history of substance use may deprive patients of legitimate pharmacologic symptom relief. Most cases lie somewhere in the middle.
A literature review does not support the assertion that the use of these medications leads to future substance use or worsens active use, especially for stimulants. In fact, stepwise—as opposed to concurrent—treatment for both conditions actually may delay recovery and increase patients’ risk for morbidity.
We outline issues involved in these complex clinical situations, point out controversies, review relevant research data, and offer guidelines for treatment.
CASE 1 Panic disorder in sobriety
Since he was a teen, Mr. A, age 51, drank heavily, which cost him jobs and relationships. After being convicted for driving under the influence, he was court-ordered to attend a rehabilitation facility, where, as he describes it, he “finally turned [his] life around.” He followed up residential treatment with regular attendance at Alcoholics Anonymous meetings.
After 1 year of sobriety, Mr. A develops increasingly frequent episodes of intense anxiety with sweating, nausea, chest pain, and hyperventilation and is diagnosed with panic disorder. His internist prescribes alprazolam, 0.5 mg 3 times a day, which provides some symptom relief, and refers him for follow-up psychiatric care. At his first visit, Mr. A confides to his psychiatrist that he is taking much more than the prescribed dosage of alprazolam, even when he is not experiencing anxiety, and is contemplating “buying it on the street” if his dosage is not raised to “at least 3 mg 3 times a day.”
CASE 2 Anxiety in controlled psychosis
Ms. B, age 40, had her first psychotic break at age 18 and was diagnosed with schizophrenia. Since then, she has had multiple psychiatric hospitalizations, usually presenting with auditory hallucinations and a recurring delusion that the person who calls herself Ms. B’s mother is really an actress “playing” her mother. At times this delusion has led Ms. B to attack her “imposter” mother. Over several years Ms. B began to drink heavily, but recently achieved a few months of sobriety by attending dual-diagnosis groups at her local community mental health center and individual psychotherapy sessions with her case manager. Fortunately, Ms. B’s psychosis has been stabilized with risperidone long-acting injection, 25 mg every 2 weeks, which she tolerates well.
When her beloved calico cat passes away, Ms. B experiences intense anxiety. Ms. B’s friend tells her she “needs some Valium,” but her psychiatrist, case manager, and the other patients in her dual-diagnosis group are not sure this is a good idea.
Benzodiazepines
Pros. There are multiple legitimate uses of benzodiazepines in general medicine and psychiatric practice, based upon their considerable sedative/hypnotic, anxiolytic, anticonvulsant, and muscle-relaxant properties (Table 1).1
Recommendations regarding benzodiazepine use for anxious patients with a history of SUD are not clear-cut. First, it often is difficult to determine whether the patient truly has an anxiety disorder or is suffering anxiety symptoms secondary to substance use and/or withdrawal. In addition, even if a diagnosis of a separate anxiety disorder is established, psychiatrists debate how to treat such patients. Some clinicians maintain that benzodiazepines should be used only for acute detoxification, and that ongoing benzodiazepine use will lead to relapse or benzodiazepine dependence. However, in a prospective study of 545 alcohol use disorder (AUD) patients receiving benzodiazepines for anxiety disorders, Mueller et al2 found no association—at 12 months or at 12 years—between benzodiazepine use and AUD recurrence. Furthermore, there was no difference in benzodiazepine usage when comparing patients with and without an AUD.3
Table 1
Clinical uses of benzodiazepines
| Insomnia |
| Anxiety disorders (eg, generalized anxiety disorder, panic disorder, posttraumatic stress disorder, social phobia, and obsessive-compulsive disorder) |
| Side effects of other psychiatric medications (eg, akathisia with antipsychotics or tremor with lithium) |
| Alcohol or benzodiazepine withdrawal |
| Acute agitation states, either as monotherapy or as adjuncts to antipsychotics or mood stabilizers |
| Catatonia |
| Source: Reference 1 |
Cons. Although widely prescribed—and despite their efficacy in numerous conditions— both acute or long-term benzodiazepine use frequently causes adverse effects.4 Patients may develop tolerance, which can lead to escalating dosages and/or to withdrawal symptoms when patients attempt to cut back. Benzodiazepines eventually become ineffective for sleep, and continued use can cause rebound insomnia. Also, with many patients taking benzodiazepines long-term, clinicians struggle to differentiate between “real” anxiety symptoms and subtle states of withdrawal from fluctuating benzodiazepine blood levels.5
Geriatric patients who take benzodiazepines are at risk for falls and hip fractures.4 Although older dementia patients are at particular risk for cognitive problems— including frank delirium—secondary to benzodiazepine use, patients of all ages are susceptible to these medications’ deleterious neurocognitive effects.
Benzodiazepines can lead to excessive sedation, thereby impairing performance at work or school, and have been implicated as a cause of motor vehicle accidents.6 Finally, a serious drawback to benzodiazepine use is possible lethality in overdose, especially when combined with alcohol.
Benzodiazepine prescribing should not be taken lightly. Always analyze the difference between benzodiazepines’ well-documented efficacy and their adverse effect profile. This risk-benefit analysis becomes much more complex for patients with SUDs.
Special considerations. Patients at higher risk for benzodiazepine abuse include those with:
- severe alcohol dependence (ie, long-term use, drinking since a young age [“Type II”])
- intravenous drug use
- comorbid alcoholism and antisocial personality disorder.7,8
Exercise special caution when considering benzodiazepines for patients with severe psychiatric illness such as schizophrenia-spectrum disorders, bipolar disorder, or severe depression. Patients with schizophrenia have high rates of alcohol, cocaine, cannabis, and benzodiazepine abuse.9,10 Bipolar disorder patients show similar vulnerability—up to 56% of patients screen positive for substance abuse or dependence.11 Vulnerability to addiction in severely ill psychiatric patients is thought to be related to several factors, including:
- use of drugs as self-medication
- genetic predisposition
- environment/lifestyle that supports substance abuse
- neurobiologic deficits that lead to lack of inhibition of reward-seeking behaviors.11
Bipolar disorder patients in particular score high on measures of sensation seeking, which leaves them vulnerable to abusing all classes of substances.12
In a 6-year study of 203 patients with severe psychiatric illnesses and SUDs, Brunette et al13 found that these patients were 2.5 times more likely than patients with severe psychiatric illness alone to abuse prescribed benzodiazepines. In an analysis of Medicaid records, Clark et al14 found similar vulnerability in patients with major depressive disorder (MDD) and SUD. Not only did these patients show a higher rate of benzodiazepine use than patients with MDD without SUD, but the dual-diagnosis group also gravitated toward more addictive high-potency/fast-acting benzodiazepines, such as alprazolam, estazolam, or triazolam.
Case discussion/suggestions. Initially, Mr. A may seem to be an appropriate candidate for closely monitored benzodiazepine use. However, he shows a pattern of misuse, likely related to his history of severe alcohol dependence and alprazolam use. This benzodiazepine is fast-acting and has a short half-life, and thus is highly reinforcing.
Similarly, Ms. B might benefit from benzodiazepine treatment. However, her history of schizophrenia and alcohol abuse makes her a risky candidate, and alternative treatments for anxiety symptoms should be considered. If prescribed at all, a benzodiazepine should be used only short-term (eg, 1 to 2 weeks).
In general, avoid prescribing benzodiazepines to most patients who have an ongoing or past SUD.15 Consider making an exception for SUD patients with comorbid anxiety disorders, with close monitoring of their benzodiazepine use. Clonazepam, chlordiazepoxide, clorazepate, and oxazepam may be less reinforcing for SUD patients than diazepam, lorazepam, alprazolam, estazolam, or triazolam.7,16 The drawbacks of benzodiazepines, especially in the situations described above, point to the need to find alternative treatments (Table 2).17 Keep in mind nonpharmacologic options, which completely avoid the risks of medication misuse and diversion. Cognitive-behavioral therapy (CBT), for instance, has well-documented efficacy in treating insomnia and anxiety disorders.18,19
Table 2
Alternatives to benzodiazepines for anxiety and/or insomnia
| Treatment option | Comments |
|---|---|
| CBT, relaxation techniques, sleep hygiene counseling | Many advantages to nonpharmacologic interventions (eg, fewer side effects, no risk of substance dependence) |
| Antihistamines (eg, diphenhydramine, 25 to 50 mg at bedtime* for sleep, or 2 to 3 times a day for anxiety) | Can be used for anxiety or insomnia; can cause confusion in older patients |
| Atypical antipsychotics | Off-label use; many agents in this class have metabolic side effects |
| SSRIs/SNRIs | First-line for many anxiety disorders, including panic disorder, GAD; possible weight gain and sexual side effects |
| Mirtazapine (7.5 to 30 mg at bedtime*) | Sedation side effect helps with sleep; weight gain and oversedation limit use |
| Trazodone (25 to 100 mg at bedtime*) | Commonly used off-label as a sleep aid |
| Monoamine oxidase inhibitors | May be useful for social phobia; dietary restrictions and side effects limit use |
| Doxepin (3 to 6 mg at bedtime) | Minimal anticholinergic and alpha-blockade side effects at this dose; FDA-approved for insomnia |
| Gabapentin (300 to 2,000 mg/d* in divided doses) | Off-label use, mild anxiolytic and sedative properties, relatively weight neutral |
| Beta blockers (eg, propranolol, 20 to 80 mg twice a day*) | Useful for peripheral manifestations of anxiety; may be effective for social phobias |
| Pregabalin (50 to 200 mg 3 times a day*) | Off-label use; industry-sponsored studies show comparable to SNRIs for anxiety |
| Non-benzodiazepine GABAA receptor modulators | Short-term option for primary insomnia, some abuse potential |
| Melatonin (1 to 3 mg at bedtime*) | Mild and ‘natural’ but not always an effective sleep aid |
| *Off-label approximate doses based on the authors’ clinical experience and consensus of the literature; agents listed may require slow titration and close monitoring for adverse effects CBT: cognitive-behavioral therapy; GABA: gamma-aminobutyric acid; GAD: generalized anxiety disorder; SNRI: serotoninnorepinephrine reuptake inhibitor; SSRI: selective serotonin reuptake inhibitor Source: Reference 17 | |
CASE 3 Adult ADHD and marijuana use
Mr. C, age 30, presents to a psychiatrist with ongoing complaints of inattention, fatigue, and difficulty staying organized. A self-report screen yields symptoms consistent with adult attention-deficit/hyperactivity disorder (ADHD). Mr. C’s school and job history and collateral history from his wife appear to corroborate his assertion that his symptoms have been lifelong. He later admits to regular marijuana use. After further discussion and full evaluation of his substance use, Mr. C is started on bupropion, titrated to 300 mg/d. After 2 months, despite faithful attendance at appointments and openness about his continued marijuana use, Mr. C’s symptoms remain unchanged. He asks about atomoxetine.
Stimulants
Pros. Despite many clinicians’ hesitance to prescribe controlled substances to patients with SUDs, psychostimulants should be considered in a variety of scenarios. Although nonstimulant options are available, stimulants consistently have demonstrated superior efficacy over other treatments and remain first-line agents for adult ADHD.20 Methylphenidate, mixed amphetamine salts, lisdexamfetamine, and atomoxetine are FDA-approved for adult ADHD. Both stimulant classes (methylphenidate and amphetamine-based products) are equally effective for ADHD. In addition, stimulants are used to treat narcolepsy, cognitive disorders such as traumatic brain injury, and as augmentation to antidepressants for MDD.
ADHD affects 5% to 12% of children, and >60% of patients remain symptomatic into adulthood and require continued treatment.21 In particular, problematic inattention may persist throughout adulthood. ADHD does not appear to be an independent risk factor for SUDs in children and adolescents.22 However, substance use increases sharply as ADHD patients enter late adolescence and adulthood, and eventually becomes a problem for 20% of adolescents and adults with ADHD. Conversely, 17% to 50% of patients with alcohol, cocaine, or opioid dependence have co-occurring ADHD.23
Withholding ADHD treatment based on concerns about future or increased current substance abuse is unfounded. A meta-analysis of 6 studies that included 674 medicated and 360 unmedicated patients with ADHD who were followed at least 4 years demonstrated that childhood treatment of ADHD with stimulants reduces the risk of developing alcohol and other drug disorders in adulthood.24 Regarding the effect stimulants have on active substance use, a 12-week, double-blind, randomized controlled trial of 48 cocaine-dependent adults with ADHD showed methylphenidate did not change cocaine abuse or craving, but did improve ADHD symptoms.25
Clinicians also must assess whether untreated ADHD symptoms impair patients’ work or other activities. Driving is a particular concern because ADHD is associated with risky driving habits, motor vehicle accidents, traffic violations, and driving license suspensions.26 In a study that administered cognitive tests to 27 adults with ADHD, methylphenidate treatment improved cognitive performance related to driving (eg, better visual-motor coordination under high-stress conditions, improved visual orientation, and sustained visual attention).27 It is likely this effect could be generalized to other activities where safety is important. Finally, appropriate stimulant treatment may improve participation in rehabilitative programs.
Cons. Despite their positive effects, stimulants can have adverse effects and consequences.28 In routinely prescribed dosages, methylphenidate and amphetamines can cause symptoms related to sympathetic activation, including anxiety, tics, anorexia/ weight loss, and sleep disturbance. A 5-year study of 79 school-age children prescribed methylphenidate, dextroamphetamine, or pemoline, which is no longer available in the United States, showed a significant association between adherence to stimulants and persistence of physiological (eg, headaches, insomnia, anorexia) and mood-related (eg, irritability, dysphoria) side effects.29 Stimulants’ sympathomimetic properties also can lead to dangerous drug-drug interactions with monoamine oxidase inhibitors. For both methylphenidate and amphetamines, overdose can lead to seizures, cardiac toxicity, dysrhythmias, and hyperthermia. All stimulants carry an FDA “black-box” warning that lists increased risk of cardiac complications, sudden death, and psychiatric complications such as psychosis or mania.30
Special considerations. All stimulants have potential for diversion or abuse. Pay close attention to these issues, especially in vulnerable populations and situations where rates of abuse and diversion are elevated. Among college students, white patients, fraternity/sorority members, and individuals with lower grade point averages may be at higher risk for nonmedical stimulant use.31 Adults who misuse or divert stimulants commonly have a history of substance abuse and conduct disorder.32 Short-acting stimulants are abused 4 times more often than extended-release preparations.33
If your ADHD patient has active substance use, be clear that continued substance use is likely to limit stimulants’ effectiveness. In patients who are actively using substances, it will be difficult to disentangle apparent nonresponse to stimulants from the negative cognitive effects of substance use.
Case discussion/suggestions. As Mr. C’s case illustrates, there are alternatives to stimulants for ADHD. For example, atomoxetine, a selective norepinephrine reuptake inhibitor, may be considered a first-line agent in patients with mostly inattentive ADHD symptoms and comorbid stimulant abuse, or for those in whom stimulants cause adverse effects such as mood lability or tics.34 Other alternatives to stimulants are listed in Table 3.35
Because Mr. C did not respond to bupropion, which presumably was tried first because of his ongoing substance use, he asked about atomoxetine. This agent is not addictive and there is no evidence that it leads to or exacerbates substance use. Depending on Mr. C’s symptom profile, atomoxetine might be a good choice. Continued monitoring of his marijuana use and frequent assessment of his motivation to quit are necessary. Psychoeducation about the cognitive effects of marijuana, including inattention and poor concentration, is important.
If Mr. C does not respond to atomoxetine, his psychiatrist will face a difficult decision. Setting Mr. C’s marijuana use aside, symptoms that do not respond to atomoxetine or a second-line agent are likely to respond to a stimulant. However, several issues must be addressed. If Mr. C’s motivation to stop using marijuana is low, how motivated is he to improve his ADHD symptoms? Next, would marijuana’s depressive/blunting effects counteract the anticipated benefit of a stimulant? Also, what is the risk that Mr. C might sell or exchange his stimulants to obtain marijuana? Assessing these complicated questions is key. Another important factor in Mr. C’s case is his wife’s involvement. Does she monitor his marijuana use? Would she be willing to supervise Mr. C’s stimulant use, and would he allow it?
Past or present SUDs are not an absolute contraindication to stimulant use. You should affirm the diagnosis and identify target symptoms. Consider nonstimulant alternatives if appropriate.
Table 3
Alternatives to stimulants for ADHD
| Treatment option | Comments |
|---|---|
| Atomoxetine | Effectiveness may be limited to inattentive type |
| Modafinil | Well-tolerated but expensive, limited evidence, no FDA indication; may be a consideration in ADHD + SUD |
| α2-adrenergic agonist (eg, clonidine or guanfacine) | Useful when hyperactivity/impulsivity symptoms predominate, or when stimulant-induced insomnia occurs |
| Bupropion | Some evidence of mild efficacy, especially useful if nicotine dependence also is a target for treatment |
| Psychotherapy | Can be useful as adjunctive treatment, but as monotherapy it is of little benefit in ADHD |
| ADHD: attention-deficit/hyperactivity disorder; SUD: substance abuse disorder Source: Reference 35 | |
Legal liabilities
Being aware of the medicolegal issues of benzodiazepine and/or stimulant prescribing is crucial because a court may find a psychiatrist liable for negative outcomes (eg, suicide) when controlled substances are prescribed to a patient with a history of addiction.36 The most prudent course is to weigh the pros and cons for each patient individually, taking into consideration the factors described above.8 This is consistent with guidelines from the American Psychiatric Association and the British Association for Psychopharmacology,37 both of which call for extreme caution in these cases.
Educate patients and caregivers about the risks of taking a controlled substance, including misuse, diversion, and theft. Provide and document explicit instructions that the patient will receive stimulants from only a single provider. Remind patients that state and federal authorities closely track controlled medications. Finally, a “stimulant contract” or “benzodiazepine contract,” similar to a pain or narcotic contact, may be useful to formally document discussions about appropriate medication use.
Related Resources
- National Institute on Drug Abuse. Prescription drugs: abuse and addiction. Research Report Series, 2005. http://drugabuse.gov/ResearchReports/Prescription/Prescription.html.
- Galanter M, Kleber HD. The American Psychiatric Publishing textbook of substance abuse treatment. 4th ed. Arlington, VA: American Psychiatric Publishing, Inc; 2008.
Drug Brand Names
- Alprazolam • Xanax
- Atomoxetine • Strattera
- Bupropion • Wellbutrin, others
- Chlordiazepoxide • Librium
- Clonazepam • Klonopin
- Clonidine • Catapres
- Clorazepate • Tranxene
- Dextroamphetamine • Dexedrine
- Diazepam • Valium
- Diphenhydramine • Benadryl, others
- Doxepin • Silenor
- Estazolam • ProSom
- Gabapentin • Neurontin
- Guanfacine • Tenex, Intuniv
- Lisdexamfetamine • Vyvanse
- Lithium • Eskalith, Lithobid
- Lorazepam • Ativan
- Methylphenidate • Ritalin, Concerta, others
- Mirtazapine • Remeron
- Mixed amphetamine salts • Adderall
- Modafinil • Provigil
- Oxazepam • Serax
- Pemoline • Cylert
- Propranolol • Inderal
- Trazodone • Desyrel, Oleptro
- Triazolam • Halcion
Disclosures
Dr. Casher is a speaker for AstraZeneca and Pfizer Inc.
Drs. Gih and Bess report no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
1. Ashton H. Guidelines for the rational use of benzodiazepines. When and what to use. Drugs. 1994;48(1):25.-
2. Mueller TI, Pagano ME, Rodriguez BF, et al. Long-term use of benzodiazepines in participants with comorbid anxiety and alcohol use disorders. Alcohol Clin Exp Res. 2005;29(8):1411-1418.
3. Mueller TI, Goldenberg IM, Gordon AL, et al. Benzodiazepine use in anxiety disordered patients with and without a history of alcoholism. J Clin Psychiatry. 1996;57(2):83-89.
4. Ashton H. The diagnosis and management of benzodiazepine dependence. Curr Opin Psychiatry. 2005;(18):249-255.
5. Back SE, Brady KT. Anxiety disorders with comorbid substance use disorders: diagnostic and treatment considerations. Psychiatric Annals. 2008;38(11):724-729.
6. Walsh JM, Flegel R, Cangianelli LA, et al. Epidemiology of alcohol and other drug use among motor vehicle crash victims admitted to a trauma center. Traffic Inj Prev. 2004;5(3):254-260.
7. Ciraulo DA, Nace EP. Benzodiazepine treatment of anxiety or insomnia in substance abuse patients. Am J Addict. 2000;9(4):276-279;discussion 280–284.
8. Sattar S, Bhatia S. Benzodiazepines for substance abusers. Current Psychiatry. 2003;2(5):25-34.
9. Regier DA, Farmer ME, Rae DS, et al. Comorbidity of mental disorders with alcohol and other drug abuse. Results from the Epidemiologic Catchment Area (ECA) Study. JAMA. 1990;264(19):2511-2518.
10. Kendler KS, Gallagher TJ, Abelson JM, et al. Lifetime prevalence, demographic risk factors, and diagnostic validity of nonaffective psychosis as assessed in a US community sample. The National Comorbidity Survey. Arch Gen Psychiatry. 1996;53(11):1022-1031
11. Buckley PF. Prevalence and consequences of the dual diagnosis of substance abuse and severe mental illness. J Clin Psychiatry. 2006;67(suppl 7):5-9.
12. Bizzarri JV, Sbrana A, Rucci P, et al. The spectrum of substance abuse in bipolar disorder: reasons for use, sensation seeking and substance sensitivity. Bipolar Disord. 2007;9(3):213-220.
13. Brunette MF, Noordsy DL, Xie H, et al. Benzodiazepine use and abuse among patients with severe mental illness and co-occurring substance use disorders. Psychiatr Serv. 2003;54(10):1395-1401.
14. Clark RE, Xie H, Brunette MF, et al. Benzodiazepine prescription practices and substance abuse in persons with severe mental illness. J Clin Psychiatry. 2004;65(2):151-155.
15. Longo LP. Addiction: part I. Benzodiazepines—side effects abuse risk and alternatives. Am Fam Physician. 2000;61(7):2121-2128.
16. Ciraulo DA, Barnhill JG, Ciraulo AM, et al. Alterations in pharmacodynamics of anxiolytics in abstinent alcoholic men: subjective responses, abuse liability, and electroencephalographic effects of alprazolam, diazepam, and buspirone. J Clin Pharmacol. 1997;37(1):64-73.
17. Casher MI, Bess JD. Manual of inpatient psychiatry. Cambridge United Kingdom: Cambridge University Press; 2010.
18. Hofmann S, Smits JA. Cognitive-behavioral therapy for adult anxiety disorders: a meta-analysis of randomized placebo-controlled trials. J Clin Psychiatry. 2008;69(4):621-632.
19. Morgenthaler T, Kramer M, Alessi C, et al. Practice parameters for the psychological and behavioral treatment of insomnia: an update. An American Academy of Sleep Medicine report. Sleep. 2006;29(11):1415-1419.
20. Wilens TE. Drug therapy for adults with attention-deficit hyperactivity disorder. Drugs. 2003;63(22):2395-2411.
21. Faraone SV, Biederman J, Mick E. The age-dependent decline of attention deficit hyperactivity disorder: a meta-analysis of follow-up studies. Psychol Med. 2006;36(2):159-165.
22. Biederman J, Wilens T, Mick E, et al. Is ADHD a risk factor for psychoactive substance use disorders? Findings from a four-year prospective follow-up study. J Am Acad Child Adolesc Psychiatry. 1997;36(1):21-29.
23. Waid L, Johnson D, Anton R. Attention-deficit hyperactivity disorder and substance abuse. In: Kranzler HR Rounsaville BJ, eds. Dual diagnosis and treatment: substance abuse and comorbid medical and psychiatric disorders. vol 8. New York, NY: Marcel Dekker; 1998:393–425.
24. Wilens TE, Faraone SV, Biederman J, et al. Does stimulant therapy of attention-deficit/hyperactivity disorder beget later substance abuse? A meta-analytic review of the literature. Pediatrics. 2003;111(1):179-185.
25. Schubiner H, Saules KK, Arfken CL, et al. Double-blind placebo-controlled trial of methylphenidate in the treatment of adult ADHD patients with comorbid cocaine dependence. Exp Clin Psychopharmacol. 2002;10(3):286-294.
26. Barkley RA, Murphy KR, Kwasnik D. Motor vehicle driving competencies and risks in teens and young adults with attention deficit hyperactivity disorder. Pediatrics. 1996;98(6 Pt 1):1089-1095.
27. Sobanski E, Sabljic D, Alm B, et al. Driving-related risks and impact of methylphenidate treatment on driving in adults with attention-deficit/hyperactivity disorder (ADHD). J Neural Transm. 2008;115(2):347-356.
28. Leonard BE, McCartan D, White J, et al. Methylphenidate: a review of its neuropharmacological, neuropsychological and adverse clinical effects. Hum Psychopharmacol. 2004;19(3):151-180.
29. Charach A, Ickowicz A, Schachar R. Stimulant treatment over five years: adherence effectiveness, and adverse effects. J Am Acad Child Adolesc Psychiatry. 2004;43(5):559-567.
30. Schatzberg AF, Nemeroff CB. The American Psychiatric Publishing textbook of psychopharmacology. 4th ed. Arlington VA: American Psychiatric Publishing, Inc; 2009.
31. Wilens TE, Adler LA, Adams J, et al. Misuse and diversion of stimulants prescribed for ADHD: a systematic review of the literature. J Am Acad Child Adolesc Psychiatry. 2008;47(1):21-31.
32. Wilens TE, Gignac M, Swezey A, et al. Characteristics of adolescents and young adults with ADHD who divert or misuse their prescribed medications. J Am Acad Child Adolesc Psychiatry. 2006;45(4):408-414.
33. Bright GM. Abuse of medications employed for the treatment of ADHD: results from a large-scale community survey. Medscape J Med. 2008;10(5):111.-
34. Biederman J, Spencer T, Wilens T. Evidence-based pharmacotherapy for attention-deficit hyperactivity disorder. Int J Neuropsychopharmacol. 2004;7(1):77-97.
35. Mann N, Bitsios P. Modafinil treatment of amphetamine abuse in adult ADHD. J Psychopharmacol. 2009;23(4):468-471.
36. Grant JE. Prudent prescribing for patients with addictions. Current Psychiatry. 2006;5(10):99-102.
37. Lingford-Hughes AR, Welch S, Nutt DJ. and the British Association for Psychopharmacology. Evidence-based guidelines for the pharmacological management of substance misuse addiction and comorbidity: recommendations from the British Association for Psychopharmacology. J Psychopharmacol. 2004;18(3):293-335.
1. Ashton H. Guidelines for the rational use of benzodiazepines. When and what to use. Drugs. 1994;48(1):25.-
2. Mueller TI, Pagano ME, Rodriguez BF, et al. Long-term use of benzodiazepines in participants with comorbid anxiety and alcohol use disorders. Alcohol Clin Exp Res. 2005;29(8):1411-1418.
3. Mueller TI, Goldenberg IM, Gordon AL, et al. Benzodiazepine use in anxiety disordered patients with and without a history of alcoholism. J Clin Psychiatry. 1996;57(2):83-89.
4. Ashton H. The diagnosis and management of benzodiazepine dependence. Curr Opin Psychiatry. 2005;(18):249-255.
5. Back SE, Brady KT. Anxiety disorders with comorbid substance use disorders: diagnostic and treatment considerations. Psychiatric Annals. 2008;38(11):724-729.
6. Walsh JM, Flegel R, Cangianelli LA, et al. Epidemiology of alcohol and other drug use among motor vehicle crash victims admitted to a trauma center. Traffic Inj Prev. 2004;5(3):254-260.
7. Ciraulo DA, Nace EP. Benzodiazepine treatment of anxiety or insomnia in substance abuse patients. Am J Addict. 2000;9(4):276-279;discussion 280–284.
8. Sattar S, Bhatia S. Benzodiazepines for substance abusers. Current Psychiatry. 2003;2(5):25-34.
9. Regier DA, Farmer ME, Rae DS, et al. Comorbidity of mental disorders with alcohol and other drug abuse. Results from the Epidemiologic Catchment Area (ECA) Study. JAMA. 1990;264(19):2511-2518.
10. Kendler KS, Gallagher TJ, Abelson JM, et al. Lifetime prevalence, demographic risk factors, and diagnostic validity of nonaffective psychosis as assessed in a US community sample. The National Comorbidity Survey. Arch Gen Psychiatry. 1996;53(11):1022-1031
11. Buckley PF. Prevalence and consequences of the dual diagnosis of substance abuse and severe mental illness. J Clin Psychiatry. 2006;67(suppl 7):5-9.
12. Bizzarri JV, Sbrana A, Rucci P, et al. The spectrum of substance abuse in bipolar disorder: reasons for use, sensation seeking and substance sensitivity. Bipolar Disord. 2007;9(3):213-220.
13. Brunette MF, Noordsy DL, Xie H, et al. Benzodiazepine use and abuse among patients with severe mental illness and co-occurring substance use disorders. Psychiatr Serv. 2003;54(10):1395-1401.
14. Clark RE, Xie H, Brunette MF, et al. Benzodiazepine prescription practices and substance abuse in persons with severe mental illness. J Clin Psychiatry. 2004;65(2):151-155.
15. Longo LP. Addiction: part I. Benzodiazepines—side effects abuse risk and alternatives. Am Fam Physician. 2000;61(7):2121-2128.
16. Ciraulo DA, Barnhill JG, Ciraulo AM, et al. Alterations in pharmacodynamics of anxiolytics in abstinent alcoholic men: subjective responses, abuse liability, and electroencephalographic effects of alprazolam, diazepam, and buspirone. J Clin Pharmacol. 1997;37(1):64-73.
17. Casher MI, Bess JD. Manual of inpatient psychiatry. Cambridge United Kingdom: Cambridge University Press; 2010.
18. Hofmann S, Smits JA. Cognitive-behavioral therapy for adult anxiety disorders: a meta-analysis of randomized placebo-controlled trials. J Clin Psychiatry. 2008;69(4):621-632.
19. Morgenthaler T, Kramer M, Alessi C, et al. Practice parameters for the psychological and behavioral treatment of insomnia: an update. An American Academy of Sleep Medicine report. Sleep. 2006;29(11):1415-1419.
20. Wilens TE. Drug therapy for adults with attention-deficit hyperactivity disorder. Drugs. 2003;63(22):2395-2411.
21. Faraone SV, Biederman J, Mick E. The age-dependent decline of attention deficit hyperactivity disorder: a meta-analysis of follow-up studies. Psychol Med. 2006;36(2):159-165.
22. Biederman J, Wilens T, Mick E, et al. Is ADHD a risk factor for psychoactive substance use disorders? Findings from a four-year prospective follow-up study. J Am Acad Child Adolesc Psychiatry. 1997;36(1):21-29.
23. Waid L, Johnson D, Anton R. Attention-deficit hyperactivity disorder and substance abuse. In: Kranzler HR Rounsaville BJ, eds. Dual diagnosis and treatment: substance abuse and comorbid medical and psychiatric disorders. vol 8. New York, NY: Marcel Dekker; 1998:393–425.
24. Wilens TE, Faraone SV, Biederman J, et al. Does stimulant therapy of attention-deficit/hyperactivity disorder beget later substance abuse? A meta-analytic review of the literature. Pediatrics. 2003;111(1):179-185.
25. Schubiner H, Saules KK, Arfken CL, et al. Double-blind placebo-controlled trial of methylphenidate in the treatment of adult ADHD patients with comorbid cocaine dependence. Exp Clin Psychopharmacol. 2002;10(3):286-294.
26. Barkley RA, Murphy KR, Kwasnik D. Motor vehicle driving competencies and risks in teens and young adults with attention deficit hyperactivity disorder. Pediatrics. 1996;98(6 Pt 1):1089-1095.
27. Sobanski E, Sabljic D, Alm B, et al. Driving-related risks and impact of methylphenidate treatment on driving in adults with attention-deficit/hyperactivity disorder (ADHD). J Neural Transm. 2008;115(2):347-356.
28. Leonard BE, McCartan D, White J, et al. Methylphenidate: a review of its neuropharmacological, neuropsychological and adverse clinical effects. Hum Psychopharmacol. 2004;19(3):151-180.
29. Charach A, Ickowicz A, Schachar R. Stimulant treatment over five years: adherence effectiveness, and adverse effects. J Am Acad Child Adolesc Psychiatry. 2004;43(5):559-567.
30. Schatzberg AF, Nemeroff CB. The American Psychiatric Publishing textbook of psychopharmacology. 4th ed. Arlington VA: American Psychiatric Publishing, Inc; 2009.
31. Wilens TE, Adler LA, Adams J, et al. Misuse and diversion of stimulants prescribed for ADHD: a systematic review of the literature. J Am Acad Child Adolesc Psychiatry. 2008;47(1):21-31.
32. Wilens TE, Gignac M, Swezey A, et al. Characteristics of adolescents and young adults with ADHD who divert or misuse their prescribed medications. J Am Acad Child Adolesc Psychiatry. 2006;45(4):408-414.
33. Bright GM. Abuse of medications employed for the treatment of ADHD: results from a large-scale community survey. Medscape J Med. 2008;10(5):111.-
34. Biederman J, Spencer T, Wilens T. Evidence-based pharmacotherapy for attention-deficit hyperactivity disorder. Int J Neuropsychopharmacol. 2004;7(1):77-97.
35. Mann N, Bitsios P. Modafinil treatment of amphetamine abuse in adult ADHD. J Psychopharmacol. 2009;23(4):468-471.
36. Grant JE. Prudent prescribing for patients with addictions. Current Psychiatry. 2006;5(10):99-102.
37. Lingford-Hughes AR, Welch S, Nutt DJ. and the British Association for Psychopharmacology. Evidence-based guidelines for the pharmacological management of substance misuse addiction and comorbidity: recommendations from the British Association for Psychopharmacology. J Psychopharmacol. 2004;18(3):293-335.