User login
Prescribing Error Education
Medication errors are an often preventable consequence of the medication use process. Multiple reviews, including the recent Preventing Medication Errors by the Institute of Medicine,1 have emphasized the need to curtail process‐related deficiencies in medication use. Among inpatients, medication errors account for about 20% of medical errors.2 Medication errors can occur at the point of prescribing, transcribing, dispensing, administration, and monitoring. Prescribing errors are the most common and account for 39% to 49% of medication errors among hospitalized patients.3, 4
The Joint Commission has mandated that healthcare institutions track and intervene within the medication use process to reduce errors.5 A number of complex and costly interventions have been forwarded with significant evidence bases, including computerized physician order entry (CPOE), clinical decision‐support systems, and pharmacist participation on rounding medical teams.1 However, little has been published on the effectiveness of providing education and feedback to institutional clinicians to reduce prescribing‐related errors.68
Providers often are already aware of classic medication order errors, but at most institutions, specific examples of prescribing errors are not regularly communicated from the pharmacy dispensary to prescribers. One exception occurs when a dispensary pharmacist contacts a prescriber to clarify an order. However, this usually takes place while that prescriber is focused on the care of another patient, and it is not a good educational setting to reduce future medication order errors.
We delivered a series of short educational sessions to internal medicine (IM) residents, providing repeated feedback on prescribing errors using examples specific to our institution. The sessions followed the effective pharmaceutical industry paradigms of detailing and repeatedly exposing physicians to an educational message to maintain its salience. This innovation report documents the effect of this pharmacist‐led program on prescribing errors made by IM residents.
METHODS
This study was deemed exempt by the institutional review board of the University of Toledo.
Study Design
This study used a prospective interrupted time series design. Study participants included all IM residents at the 320‐bed University of Toledo Medical Center.
Educational Intervention
In July 2006, the Department of Internal Medicine required all IM residents to participate in a weekly 3‐hour didactic training seminar series. The educational intervention occurred longitudinally during a portion of that weekly seminar series. Attendance was mandatory, but the level of participation varied across individual residents. No formal assessment or quiz was used for each resident during these discussions.
The intervention had 2 phases and was designed and executed by the primary author within his roles as an IM clinical pharmacist and faculty member. Phase 1 was an initial hour‐long didactic lecture on prescribing errors at the beginning of November 2006. This lecture focused on definitions and categories of medical errors and medication errors, Institute of Medicine reports, Joint Commission medication management requirements, and institutional medication order policies.
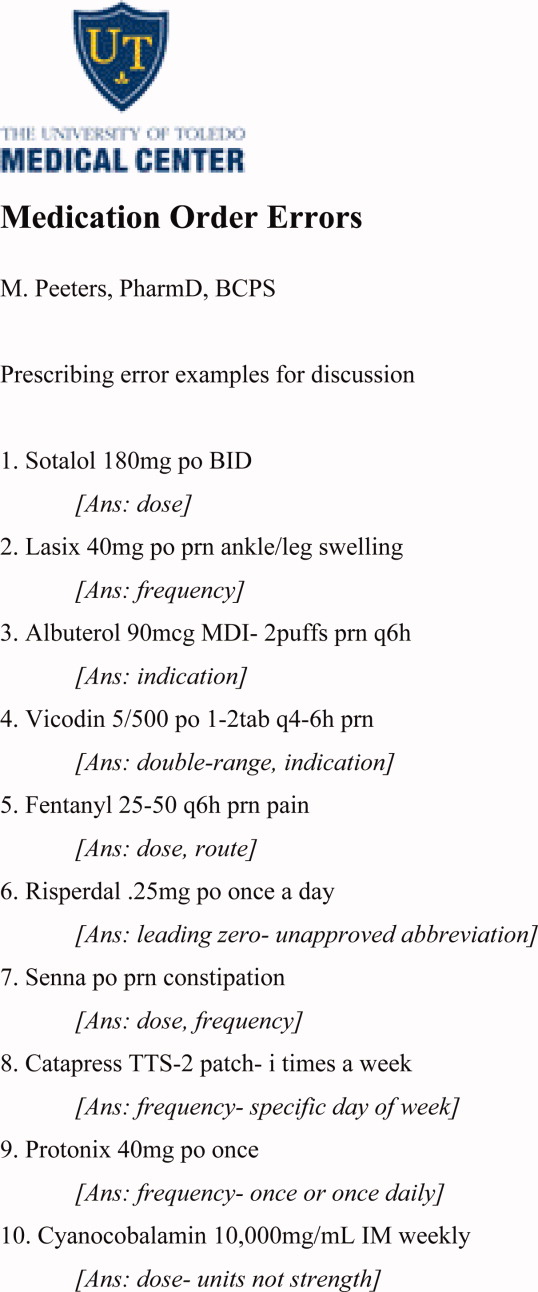
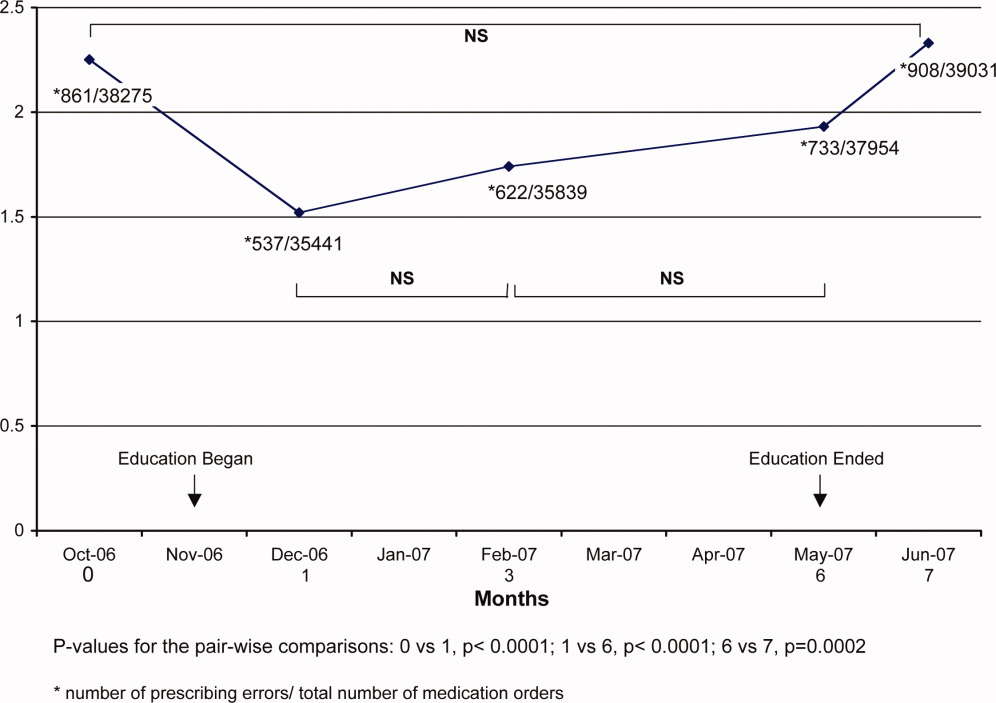
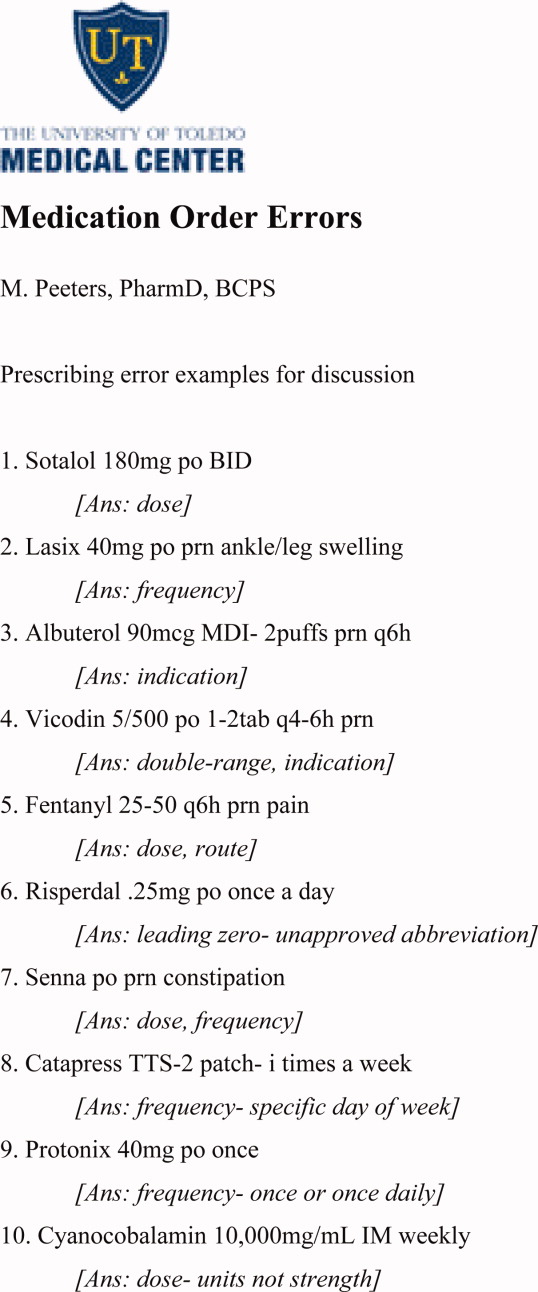
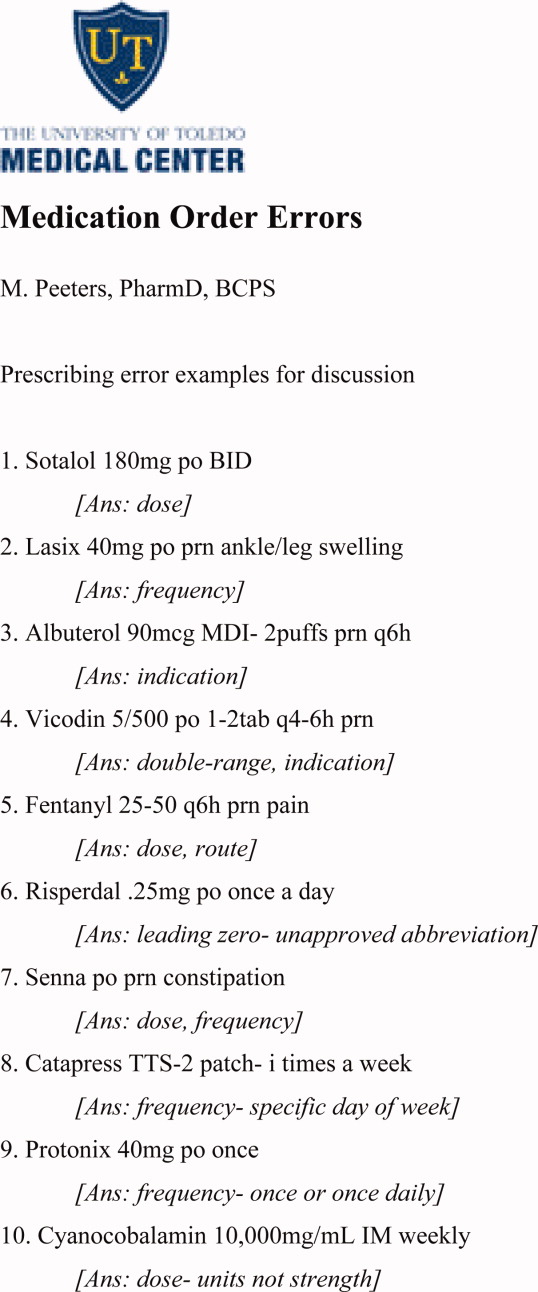
Phase 2 included a number of short, biweekly follow‐up discussion sessions in November and December 2006 and thereafter was modified to monthly discussions from January to May 2007. Discussions specifically addressed prescribing errors identified by the medication safety officer and primary author during the previous month. Sessions were approximately 15 minutes long and followed a handout that highlighted specific and commonly seen prescribing errors within the facility (Figure 1). Within these discussions, the error subtype was identified, and suggestions for properly writing the order were given.
Prescribing Error Definition and Subtypes
Prescribing error was defined as any error on a physician medication order form that was sent to the pharmacy as a dispensing request.
The subtypes of prescribing errors were as follows:
-
Orders containing unapproved abbreviations.
-
As‐needed orders without indication.
-
Resume home medications orders.
-
Double‐range orders (eg, 1‐2 Percocet q4‐6h prn headache).
-
Wrong drug.
-
Wrong dose.
-
Wrong route.
-
Wrong frequency.
-
Medication order for which the patient has a documented allergy.
-
Incomprehensible or illegible orders.
Data Collection
Prescribing errors were collected from October 2006 to June 2007 for 13 hospital units that had IM or subspecialty patients. During this time, a stable group of IM residents rotated on these units among various clinical services; no new residents entered or dropped out during the study period, except for times when they may have had an ambulatory rotation. Data collected in October 2006 established the preintervention baseline. Data were collected during the educational intervention at intervals of 1, 3, and 6 months (December, February, and May). Postintervention data were collected in June 2007.
During the study period, staff pharmacists continually screened medication orders for prescribing errors. Once identified, the incorrect orders were collected, transcribed, coded, and entered into a database by the medication safety officer. On a monthly basis, prescribing error rates were calculated by the division of the number of prescribing errors by the total number of medication orders within the facility.
Data Analysis
The experiment‐wise alpha for the main outcome was 0.05. The primary outcome was the frequency of prescribing errors across the preintervention (month 0), intervention (months 1, 3, and 6), and postintervention (month 7) periods. The primary analysis compared these 5 time periods with 10 Bonferroni‐adjusted chi‐square tests, reducing the pairwise alpha to 0.005.
RESULTS
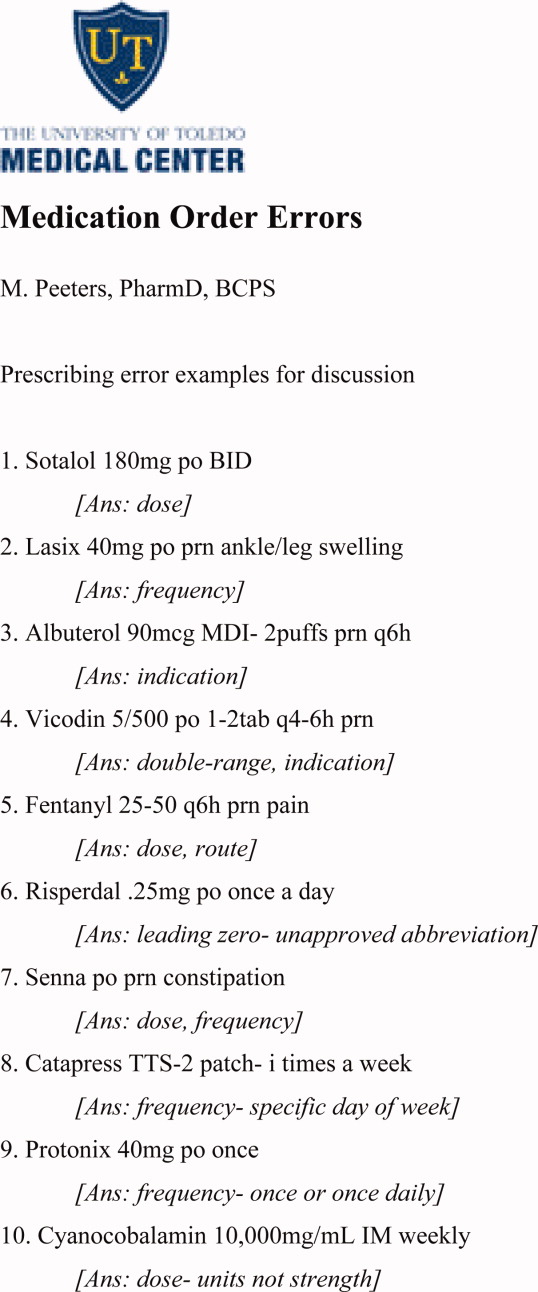
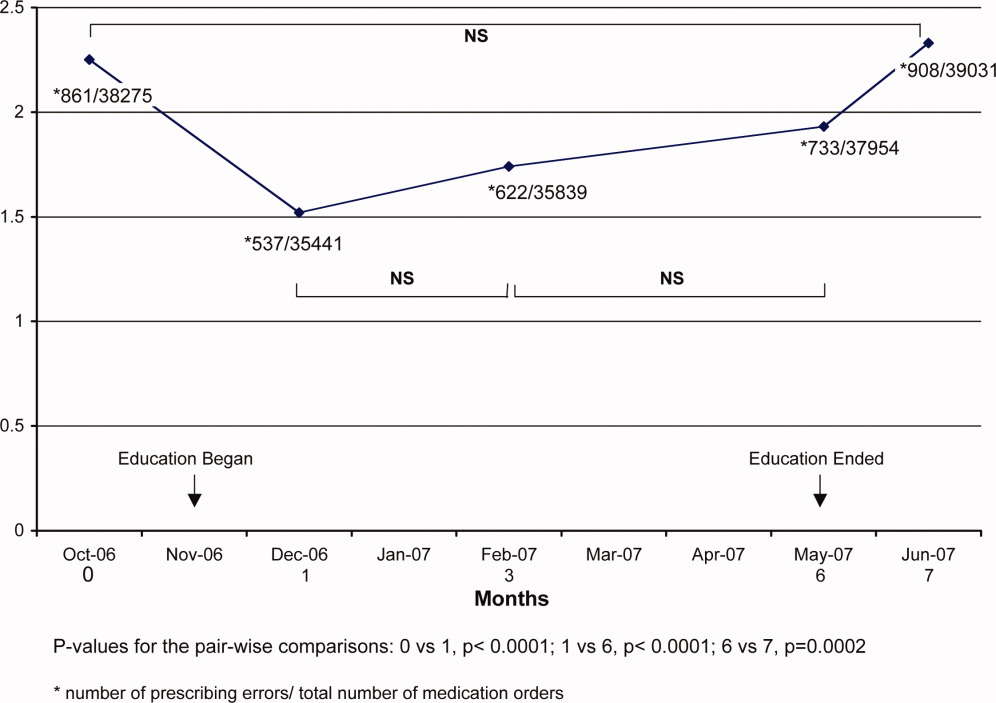
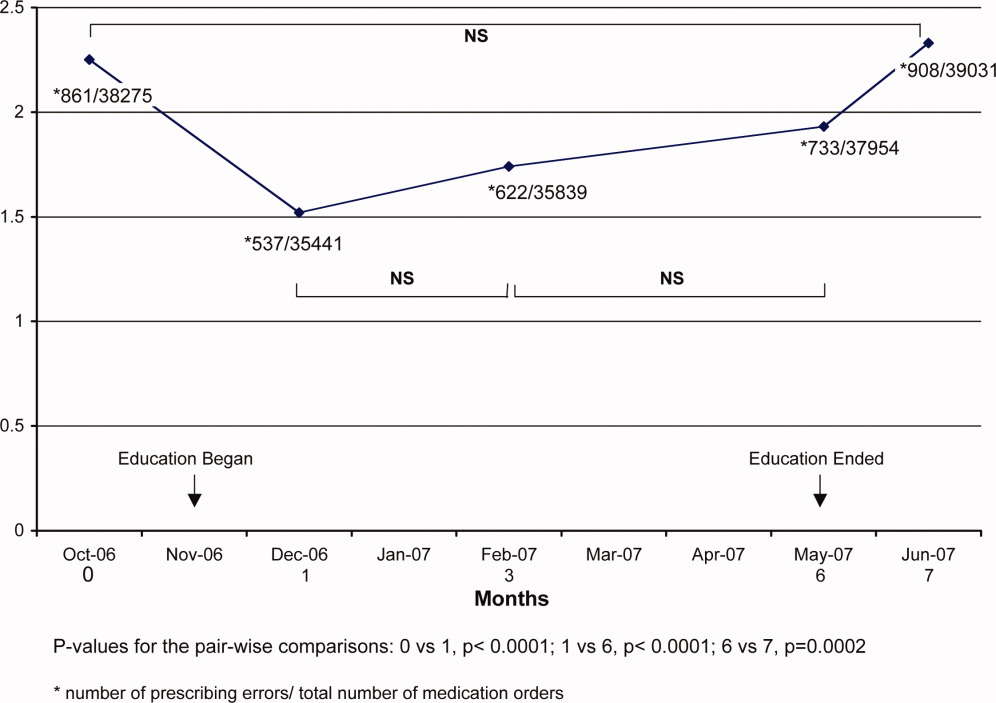
Forty‐two IM residents participated in this study. Prior to the educational intervention, prescribing errors affected 2.25% (861/38,275) of the institution's medication orders (Figure 2). Following phase 1 and early into phase 2 of the prescribing error education, the frequency dropped to 1.51% (P 0.001); that is, there was a 33% decline from the baseline. During the remainder of the intervention period, the frequency of prescribing errors fluctuated but remained lower than that observed pre‐intervention (P 0.001 for each pairwise comparison to the baseline). Post‐intervention, the frequency of prescribing errors rose to 2.33% and was similar to that observed at the baseline (P = 0.49).
DISCUSSION
An educational intervention that highlighted institution‐specific prescribing errors reduced such errors by 33% within the first month and resulted in a mean 26% reduction during the 6‐month intervention period. Without ongoing education, however, the frequency of prescribing errors returned to preintervention period levels.
Our findings compare favorably to results obtained by other more complex and costly methods used to reduce medication errors, namely, CPOE, clinical decision‐support software, and clinical pharmacists on medical rounds.1 For example, in 1 study, prescribing errors were reduced by 19% following the implementation of CPOE alone.9 In another report, CPOE with clinical decision‐support software led to a more dramatic reduction of 81%.10 Additionally, pharmacist involvement on medical rounds has reduced adverse drug events by 78%.11
The frequency of prescribing errors found in this study was similar to that found in previous literature, although the variation in the definitions limits this comparison somewhat.12 Interestingly, the frequency of errors increased as the overall number of medication orders for the facility increased (see the ratios in Figure 2). This suggests that errors may be more likely during busier time periods, which are defined by higher total order volumes. Others have made similar observations.13 On most occasions, the individual prescribing errors seemed obvious and most likely due to a physician's haste.
This study had some limitations, including its interrupted time series design, which limits the ability to define a causal relationship. However, a causal effect is suggested by the differences before and during intervention as well as the return to the preintervention error frequency after the intervention had concluded. Second, the reported frequencies represent all medication orders in the studied clinical areas, not only those orders written by medical residents who participated in the intervention, although they do account for a large portion of the prescribing at the study hospital. Third, we did not assess specific resident errors or compare changes in the types of errors over time. Fourth, generalizability is limited to IM residents at an academic institution. As trainees, the IM residents may have been both keener to participate in and more accessible for educational opportunities such as this study. Fifth, as noted previously, the IM residents in this study not only practiced in the inpatient areas but had outpatient clinic rotations as well. It is conceivable that the most error‐prone residents rotated on the inpatient units before and after the intervention period but not during it. This is not very likely but cannot be excluded.
CONCLUSIONS
Adverse drug events have an impact on patient safety and can commonly occur following prescribing errors. Therefore, reducing prescribing errors is extremely important. The longitudinal education of residents using a periodic educational intervention provides a successful and economically feasible prescribing error prevention strategy, although the effects are quickly reversed following cessation of the educational component. Therefore, supporting an ongoing commitment to trainee education and communication between pharmacy and prescribers about institution‐specific medication errors appears warranted.
Acknowledgements
The authors gratefully acknowledge Ziad Mattar, MD, the 2006‐2007 University of Toledo College of Medicine Internal Medicine Chief Resident, for his organizational influence regarding the educational sessions with internal medicine residents. In addition, the University of Toledo College of Medicine Medication Safety Officer, Ms. Jennifer Guy, provided great assistance in accumulating the data for this study.
- Institute of Medicine.Preventing Medication Errors: Quality Chasm Series.Washington, DC:National Academy Press;2007.
- ,,, et al.The nature of adverse events in hospitalized patients: results of the Harvard Medical Practice Study II.N Engl J Med.1991;324(6):377–384.
- ,,, et al.Incidence of adverse drug events and potential adverse drug events: implications for practice.JAMA.1995;274:29–34.
- ,,, et al.Systems analysis of adverse drug events.JAMA.1995;274:35–43.
- Comprehensive Accreditation Manual for Hospitals.Oakbrook Terrace, IL:Joint Commission on Accreditation of Healthcare Organizations;2004.
- .Education regarding medication order errors.CJHP.2007;60:130.
- ,,,,.Educational interventions to reduce use of unsafe abbreviations.Am J Health‐Syst Pharm.2007;64:1170–1173.
- ,,,,,.Error reduction: academic detailing as a method to reduce incorrect prescriptions.Eur J Clin Pharmacol.2003;59:697–699.
- ,,, et al.Effect of computerized physician order entry and a team intervention on prevention of serious medication errors.JAMA.1998;280:1311–1316.
- ,,, et al.The impact of computerized physician order entry on medication error prevention.J Am Med Inform Assoc.1999;6:313–321.
- ,,,.Pharmacists on rounding teams reduce preventable adverse drug events in hospital general medicine units.Arch Intern Med.2003;163:2014–2018.
- ,,,.The incidence of prescribing errors in hospital inpatients.Drug Saf.2005;28:891–900.
- ,,,,.A study of the quality of prescriptions issued in a busy pediatric emergency room.Public Health Rep.1975;90(5):402–408.
Medication errors are an often preventable consequence of the medication use process. Multiple reviews, including the recent Preventing Medication Errors by the Institute of Medicine,1 have emphasized the need to curtail process‐related deficiencies in medication use. Among inpatients, medication errors account for about 20% of medical errors.2 Medication errors can occur at the point of prescribing, transcribing, dispensing, administration, and monitoring. Prescribing errors are the most common and account for 39% to 49% of medication errors among hospitalized patients.3, 4
The Joint Commission has mandated that healthcare institutions track and intervene within the medication use process to reduce errors.5 A number of complex and costly interventions have been forwarded with significant evidence bases, including computerized physician order entry (CPOE), clinical decision‐support systems, and pharmacist participation on rounding medical teams.1 However, little has been published on the effectiveness of providing education and feedback to institutional clinicians to reduce prescribing‐related errors.68
Providers often are already aware of classic medication order errors, but at most institutions, specific examples of prescribing errors are not regularly communicated from the pharmacy dispensary to prescribers. One exception occurs when a dispensary pharmacist contacts a prescriber to clarify an order. However, this usually takes place while that prescriber is focused on the care of another patient, and it is not a good educational setting to reduce future medication order errors.
We delivered a series of short educational sessions to internal medicine (IM) residents, providing repeated feedback on prescribing errors using examples specific to our institution. The sessions followed the effective pharmaceutical industry paradigms of detailing and repeatedly exposing physicians to an educational message to maintain its salience. This innovation report documents the effect of this pharmacist‐led program on prescribing errors made by IM residents.
METHODS
This study was deemed exempt by the institutional review board of the University of Toledo.
Study Design
This study used a prospective interrupted time series design. Study participants included all IM residents at the 320‐bed University of Toledo Medical Center.
Educational Intervention
In July 2006, the Department of Internal Medicine required all IM residents to participate in a weekly 3‐hour didactic training seminar series. The educational intervention occurred longitudinally during a portion of that weekly seminar series. Attendance was mandatory, but the level of participation varied across individual residents. No formal assessment or quiz was used for each resident during these discussions.
The intervention had 2 phases and was designed and executed by the primary author within his roles as an IM clinical pharmacist and faculty member. Phase 1 was an initial hour‐long didactic lecture on prescribing errors at the beginning of November 2006. This lecture focused on definitions and categories of medical errors and medication errors, Institute of Medicine reports, Joint Commission medication management requirements, and institutional medication order policies.
Phase 2 included a number of short, biweekly follow‐up discussion sessions in November and December 2006 and thereafter was modified to monthly discussions from January to May 2007. Discussions specifically addressed prescribing errors identified by the medication safety officer and primary author during the previous month. Sessions were approximately 15 minutes long and followed a handout that highlighted specific and commonly seen prescribing errors within the facility (Figure 1). Within these discussions, the error subtype was identified, and suggestions for properly writing the order were given.
Prescribing Error Definition and Subtypes
Prescribing error was defined as any error on a physician medication order form that was sent to the pharmacy as a dispensing request.
The subtypes of prescribing errors were as follows:
-
Orders containing unapproved abbreviations.
-
As‐needed orders without indication.
-
Resume home medications orders.
-
Double‐range orders (eg, 1‐2 Percocet q4‐6h prn headache).
-
Wrong drug.
-
Wrong dose.
-
Wrong route.
-
Wrong frequency.
-
Medication order for which the patient has a documented allergy.
-
Incomprehensible or illegible orders.
Data Collection
Prescribing errors were collected from October 2006 to June 2007 for 13 hospital units that had IM or subspecialty patients. During this time, a stable group of IM residents rotated on these units among various clinical services; no new residents entered or dropped out during the study period, except for times when they may have had an ambulatory rotation. Data collected in October 2006 established the preintervention baseline. Data were collected during the educational intervention at intervals of 1, 3, and 6 months (December, February, and May). Postintervention data were collected in June 2007.
During the study period, staff pharmacists continually screened medication orders for prescribing errors. Once identified, the incorrect orders were collected, transcribed, coded, and entered into a database by the medication safety officer. On a monthly basis, prescribing error rates were calculated by the division of the number of prescribing errors by the total number of medication orders within the facility.
Data Analysis
The experiment‐wise alpha for the main outcome was 0.05. The primary outcome was the frequency of prescribing errors across the preintervention (month 0), intervention (months 1, 3, and 6), and postintervention (month 7) periods. The primary analysis compared these 5 time periods with 10 Bonferroni‐adjusted chi‐square tests, reducing the pairwise alpha to 0.005.
RESULTS
Forty‐two IM residents participated in this study. Prior to the educational intervention, prescribing errors affected 2.25% (861/38,275) of the institution's medication orders (Figure 2). Following phase 1 and early into phase 2 of the prescribing error education, the frequency dropped to 1.51% (P 0.001); that is, there was a 33% decline from the baseline. During the remainder of the intervention period, the frequency of prescribing errors fluctuated but remained lower than that observed pre‐intervention (P 0.001 for each pairwise comparison to the baseline). Post‐intervention, the frequency of prescribing errors rose to 2.33% and was similar to that observed at the baseline (P = 0.49).
DISCUSSION
An educational intervention that highlighted institution‐specific prescribing errors reduced such errors by 33% within the first month and resulted in a mean 26% reduction during the 6‐month intervention period. Without ongoing education, however, the frequency of prescribing errors returned to preintervention period levels.
Our findings compare favorably to results obtained by other more complex and costly methods used to reduce medication errors, namely, CPOE, clinical decision‐support software, and clinical pharmacists on medical rounds.1 For example, in 1 study, prescribing errors were reduced by 19% following the implementation of CPOE alone.9 In another report, CPOE with clinical decision‐support software led to a more dramatic reduction of 81%.10 Additionally, pharmacist involvement on medical rounds has reduced adverse drug events by 78%.11
The frequency of prescribing errors found in this study was similar to that found in previous literature, although the variation in the definitions limits this comparison somewhat.12 Interestingly, the frequency of errors increased as the overall number of medication orders for the facility increased (see the ratios in Figure 2). This suggests that errors may be more likely during busier time periods, which are defined by higher total order volumes. Others have made similar observations.13 On most occasions, the individual prescribing errors seemed obvious and most likely due to a physician's haste.
This study had some limitations, including its interrupted time series design, which limits the ability to define a causal relationship. However, a causal effect is suggested by the differences before and during intervention as well as the return to the preintervention error frequency after the intervention had concluded. Second, the reported frequencies represent all medication orders in the studied clinical areas, not only those orders written by medical residents who participated in the intervention, although they do account for a large portion of the prescribing at the study hospital. Third, we did not assess specific resident errors or compare changes in the types of errors over time. Fourth, generalizability is limited to IM residents at an academic institution. As trainees, the IM residents may have been both keener to participate in and more accessible for educational opportunities such as this study. Fifth, as noted previously, the IM residents in this study not only practiced in the inpatient areas but had outpatient clinic rotations as well. It is conceivable that the most error‐prone residents rotated on the inpatient units before and after the intervention period but not during it. This is not very likely but cannot be excluded.
CONCLUSIONS
Adverse drug events have an impact on patient safety and can commonly occur following prescribing errors. Therefore, reducing prescribing errors is extremely important. The longitudinal education of residents using a periodic educational intervention provides a successful and economically feasible prescribing error prevention strategy, although the effects are quickly reversed following cessation of the educational component. Therefore, supporting an ongoing commitment to trainee education and communication between pharmacy and prescribers about institution‐specific medication errors appears warranted.
Acknowledgements
The authors gratefully acknowledge Ziad Mattar, MD, the 2006‐2007 University of Toledo College of Medicine Internal Medicine Chief Resident, for his organizational influence regarding the educational sessions with internal medicine residents. In addition, the University of Toledo College of Medicine Medication Safety Officer, Ms. Jennifer Guy, provided great assistance in accumulating the data for this study.
Medication errors are an often preventable consequence of the medication use process. Multiple reviews, including the recent Preventing Medication Errors by the Institute of Medicine,1 have emphasized the need to curtail process‐related deficiencies in medication use. Among inpatients, medication errors account for about 20% of medical errors.2 Medication errors can occur at the point of prescribing, transcribing, dispensing, administration, and monitoring. Prescribing errors are the most common and account for 39% to 49% of medication errors among hospitalized patients.3, 4
The Joint Commission has mandated that healthcare institutions track and intervene within the medication use process to reduce errors.5 A number of complex and costly interventions have been forwarded with significant evidence bases, including computerized physician order entry (CPOE), clinical decision‐support systems, and pharmacist participation on rounding medical teams.1 However, little has been published on the effectiveness of providing education and feedback to institutional clinicians to reduce prescribing‐related errors.68
Providers often are already aware of classic medication order errors, but at most institutions, specific examples of prescribing errors are not regularly communicated from the pharmacy dispensary to prescribers. One exception occurs when a dispensary pharmacist contacts a prescriber to clarify an order. However, this usually takes place while that prescriber is focused on the care of another patient, and it is not a good educational setting to reduce future medication order errors.
We delivered a series of short educational sessions to internal medicine (IM) residents, providing repeated feedback on prescribing errors using examples specific to our institution. The sessions followed the effective pharmaceutical industry paradigms of detailing and repeatedly exposing physicians to an educational message to maintain its salience. This innovation report documents the effect of this pharmacist‐led program on prescribing errors made by IM residents.
METHODS
This study was deemed exempt by the institutional review board of the University of Toledo.
Study Design
This study used a prospective interrupted time series design. Study participants included all IM residents at the 320‐bed University of Toledo Medical Center.
Educational Intervention
In July 2006, the Department of Internal Medicine required all IM residents to participate in a weekly 3‐hour didactic training seminar series. The educational intervention occurred longitudinally during a portion of that weekly seminar series. Attendance was mandatory, but the level of participation varied across individual residents. No formal assessment or quiz was used for each resident during these discussions.
The intervention had 2 phases and was designed and executed by the primary author within his roles as an IM clinical pharmacist and faculty member. Phase 1 was an initial hour‐long didactic lecture on prescribing errors at the beginning of November 2006. This lecture focused on definitions and categories of medical errors and medication errors, Institute of Medicine reports, Joint Commission medication management requirements, and institutional medication order policies.
Phase 2 included a number of short, biweekly follow‐up discussion sessions in November and December 2006 and thereafter was modified to monthly discussions from January to May 2007. Discussions specifically addressed prescribing errors identified by the medication safety officer and primary author during the previous month. Sessions were approximately 15 minutes long and followed a handout that highlighted specific and commonly seen prescribing errors within the facility (Figure 1). Within these discussions, the error subtype was identified, and suggestions for properly writing the order were given.
Prescribing Error Definition and Subtypes
Prescribing error was defined as any error on a physician medication order form that was sent to the pharmacy as a dispensing request.
The subtypes of prescribing errors were as follows:
-
Orders containing unapproved abbreviations.
-
As‐needed orders without indication.
-
Resume home medications orders.
-
Double‐range orders (eg, 1‐2 Percocet q4‐6h prn headache).
-
Wrong drug.
-
Wrong dose.
-
Wrong route.
-
Wrong frequency.
-
Medication order for which the patient has a documented allergy.
-
Incomprehensible or illegible orders.
Data Collection
Prescribing errors were collected from October 2006 to June 2007 for 13 hospital units that had IM or subspecialty patients. During this time, a stable group of IM residents rotated on these units among various clinical services; no new residents entered or dropped out during the study period, except for times when they may have had an ambulatory rotation. Data collected in October 2006 established the preintervention baseline. Data were collected during the educational intervention at intervals of 1, 3, and 6 months (December, February, and May). Postintervention data were collected in June 2007.
During the study period, staff pharmacists continually screened medication orders for prescribing errors. Once identified, the incorrect orders were collected, transcribed, coded, and entered into a database by the medication safety officer. On a monthly basis, prescribing error rates were calculated by the division of the number of prescribing errors by the total number of medication orders within the facility.
Data Analysis
The experiment‐wise alpha for the main outcome was 0.05. The primary outcome was the frequency of prescribing errors across the preintervention (month 0), intervention (months 1, 3, and 6), and postintervention (month 7) periods. The primary analysis compared these 5 time periods with 10 Bonferroni‐adjusted chi‐square tests, reducing the pairwise alpha to 0.005.
RESULTS
Forty‐two IM residents participated in this study. Prior to the educational intervention, prescribing errors affected 2.25% (861/38,275) of the institution's medication orders (Figure 2). Following phase 1 and early into phase 2 of the prescribing error education, the frequency dropped to 1.51% (P 0.001); that is, there was a 33% decline from the baseline. During the remainder of the intervention period, the frequency of prescribing errors fluctuated but remained lower than that observed pre‐intervention (P 0.001 for each pairwise comparison to the baseline). Post‐intervention, the frequency of prescribing errors rose to 2.33% and was similar to that observed at the baseline (P = 0.49).
DISCUSSION
An educational intervention that highlighted institution‐specific prescribing errors reduced such errors by 33% within the first month and resulted in a mean 26% reduction during the 6‐month intervention period. Without ongoing education, however, the frequency of prescribing errors returned to preintervention period levels.
Our findings compare favorably to results obtained by other more complex and costly methods used to reduce medication errors, namely, CPOE, clinical decision‐support software, and clinical pharmacists on medical rounds.1 For example, in 1 study, prescribing errors were reduced by 19% following the implementation of CPOE alone.9 In another report, CPOE with clinical decision‐support software led to a more dramatic reduction of 81%.10 Additionally, pharmacist involvement on medical rounds has reduced adverse drug events by 78%.11
The frequency of prescribing errors found in this study was similar to that found in previous literature, although the variation in the definitions limits this comparison somewhat.12 Interestingly, the frequency of errors increased as the overall number of medication orders for the facility increased (see the ratios in Figure 2). This suggests that errors may be more likely during busier time periods, which are defined by higher total order volumes. Others have made similar observations.13 On most occasions, the individual prescribing errors seemed obvious and most likely due to a physician's haste.
This study had some limitations, including its interrupted time series design, which limits the ability to define a causal relationship. However, a causal effect is suggested by the differences before and during intervention as well as the return to the preintervention error frequency after the intervention had concluded. Second, the reported frequencies represent all medication orders in the studied clinical areas, not only those orders written by medical residents who participated in the intervention, although they do account for a large portion of the prescribing at the study hospital. Third, we did not assess specific resident errors or compare changes in the types of errors over time. Fourth, generalizability is limited to IM residents at an academic institution. As trainees, the IM residents may have been both keener to participate in and more accessible for educational opportunities such as this study. Fifth, as noted previously, the IM residents in this study not only practiced in the inpatient areas but had outpatient clinic rotations as well. It is conceivable that the most error‐prone residents rotated on the inpatient units before and after the intervention period but not during it. This is not very likely but cannot be excluded.
CONCLUSIONS
Adverse drug events have an impact on patient safety and can commonly occur following prescribing errors. Therefore, reducing prescribing errors is extremely important. The longitudinal education of residents using a periodic educational intervention provides a successful and economically feasible prescribing error prevention strategy, although the effects are quickly reversed following cessation of the educational component. Therefore, supporting an ongoing commitment to trainee education and communication between pharmacy and prescribers about institution‐specific medication errors appears warranted.
Acknowledgements
The authors gratefully acknowledge Ziad Mattar, MD, the 2006‐2007 University of Toledo College of Medicine Internal Medicine Chief Resident, for his organizational influence regarding the educational sessions with internal medicine residents. In addition, the University of Toledo College of Medicine Medication Safety Officer, Ms. Jennifer Guy, provided great assistance in accumulating the data for this study.
- Institute of Medicine.Preventing Medication Errors: Quality Chasm Series.Washington, DC:National Academy Press;2007.
- ,,, et al.The nature of adverse events in hospitalized patients: results of the Harvard Medical Practice Study II.N Engl J Med.1991;324(6):377–384.
- ,,, et al.Incidence of adverse drug events and potential adverse drug events: implications for practice.JAMA.1995;274:29–34.
- ,,, et al.Systems analysis of adverse drug events.JAMA.1995;274:35–43.
- Comprehensive Accreditation Manual for Hospitals.Oakbrook Terrace, IL:Joint Commission on Accreditation of Healthcare Organizations;2004.
- .Education regarding medication order errors.CJHP.2007;60:130.
- ,,,,.Educational interventions to reduce use of unsafe abbreviations.Am J Health‐Syst Pharm.2007;64:1170–1173.
- ,,,,,.Error reduction: academic detailing as a method to reduce incorrect prescriptions.Eur J Clin Pharmacol.2003;59:697–699.
- ,,, et al.Effect of computerized physician order entry and a team intervention on prevention of serious medication errors.JAMA.1998;280:1311–1316.
- ,,, et al.The impact of computerized physician order entry on medication error prevention.J Am Med Inform Assoc.1999;6:313–321.
- ,,,.Pharmacists on rounding teams reduce preventable adverse drug events in hospital general medicine units.Arch Intern Med.2003;163:2014–2018.
- ,,,.The incidence of prescribing errors in hospital inpatients.Drug Saf.2005;28:891–900.
- ,,,,.A study of the quality of prescriptions issued in a busy pediatric emergency room.Public Health Rep.1975;90(5):402–408.
- Institute of Medicine.Preventing Medication Errors: Quality Chasm Series.Washington, DC:National Academy Press;2007.
- ,,, et al.The nature of adverse events in hospitalized patients: results of the Harvard Medical Practice Study II.N Engl J Med.1991;324(6):377–384.
- ,,, et al.Incidence of adverse drug events and potential adverse drug events: implications for practice.JAMA.1995;274:29–34.
- ,,, et al.Systems analysis of adverse drug events.JAMA.1995;274:35–43.
- Comprehensive Accreditation Manual for Hospitals.Oakbrook Terrace, IL:Joint Commission on Accreditation of Healthcare Organizations;2004.
- .Education regarding medication order errors.CJHP.2007;60:130.
- ,,,,.Educational interventions to reduce use of unsafe abbreviations.Am J Health‐Syst Pharm.2007;64:1170–1173.
- ,,,,,.Error reduction: academic detailing as a method to reduce incorrect prescriptions.Eur J Clin Pharmacol.2003;59:697–699.
- ,,, et al.Effect of computerized physician order entry and a team intervention on prevention of serious medication errors.JAMA.1998;280:1311–1316.
- ,,, et al.The impact of computerized physician order entry on medication error prevention.J Am Med Inform Assoc.1999;6:313–321.
- ,,,.Pharmacists on rounding teams reduce preventable adverse drug events in hospital general medicine units.Arch Intern Med.2003;163:2014–2018.
- ,,,.The incidence of prescribing errors in hospital inpatients.Drug Saf.2005;28:891–900.
- ,,,,.A study of the quality of prescriptions issued in a busy pediatric emergency room.Public Health Rep.1975;90(5):402–408.