User login
Evaluation and Treatment of the Adult Patient With Migraine
- The International Headache Society criteria provide a useful standardized way to diagnose migraine clinically.
- Neuroimaging is not necessary for patients who clearly meet clinical criteria for migraine and whose neurologic examination results are normal.
- Over-the-counter drugs (including aspirin, ibuprofen, and the combination of aspirin, acetaminophen, and caffeine) work well and are first-line treatments for mild migraine.
- Migraine-specific medications (including intranasal dihydroergotamine [DHE] and the triptans) are recommended for more severe migraine; little evidence exists to suggest one drug over another.
- Prophylaxis is recommended if patients find the severity or frequency of headaches bothersome enough to warrant preventive measures; amitriptyline, divalproex sodium, and propranolol are effective prophylaxes.
Migraine is a common and disabling condition. Among adults in the United States, approximately 18% of women and 6% of men report symptoms consistent with migraine1; less than half have been diagnosed by a physician or received prescription treatment from a physician.2 Migraine accounts for more than 2.8 million visits per year to US physicians and is the reason for encounter in about 1 visit per week to the typical family physician.3 Migraine is estimated to cost US employers more than $13 billion each year; direct medical costs exceed $1 billion annually.4
Pathophysiology
The exact pathophysiology of migraine is unknown. The prevailing theory is that a trigger (such as fatigue, stress, or certain foods) sets off a wave of brief neuronal activation, followed by a more sustained neuronal inhibition known as cortical spreading depression (CSD). At some point the trigeminovascular system is activated (possibly by CSD), releasing vasoactive neuropeptides that cause a painful inflammatory response in the meninges. Stimulation of presynaptic serotonin receptors inhibits release of the inflammatory neuropeptides; this is one possible explanation for the effectiveness of the triptans.5
Diagnosis
Migraine is a syndrome diagnosed by a certain combination of signs and symptoms. The International Headache Society (IHS) diagnostic criteria (Table 1) are widely accepted as the reference standard for the diagnosis of migraine, as well as that of other types of headache.6 Although they were originally intended to assist in the standardization of research subjects, the criteria for the most common headache disorders can be adapted for diagnosis in the clinical setting. Migraine diagnosis is based almost entirely on the history; the main role of the physical examination is to screen for life-threatening conditions, such as intracranial hemorrhage or tumors.
In some patients, migraine is difficult to distinguish from other primary or secondary headaches, especially tension-type headache. A recent meta-analysis demonstrated that the features most helpful to rule in migraine (compared with tension-type headache) are nausea (positive likelihood ratio [LR+] = 19.2), photophobia (LR+ = 5.8), and phonophobia (LR+ = 5.2). Table 2 provides additional information regarding these and other significant findings, including the post-test probabilities of migraine given the reported prevalence among adult men and women in the United States. The likelihood ratios are probably somewhat inflated, since many of these symptoms are also part of the criteria for the reference standard (“incorporation bias”). The IHS criteria for migraine without aura require nausea or the combination of photophobia and phonophobia to make the diagnosis; it is therefore not surprising that these findings would be the most specific.
While the presence of any single feature may not be sufficient to clinch the diagnosis, sequentially combining the post-test probabilities can prove useful in cases that are not straightforward. For example, a woman with a family history of migraine who complains of a unilateral headache accompanied by photophobia but no nausea has an approximately 80% post-test probability of migraine. This conclusion assumes statistical independence of these symptoms and thus may overestimate the probability somewhat.8
Migraine has no specific diagnostic findings on computed tomography (CT) or magnetic resonance imaging (MRI). The best evidence addressing the use of neuroimaging studies in migraine, as well as most other diagnostic and management issues, comes from the United States Headache Consortium (USHC), a panel of experts from several specialty societies and professional organizations, including the American Academy of Family Physicians. In April 2000, the USHC issued diagnosis and treatment guidelines based on rigorous evidence-based reviews of the medical literature.9 A USHC meta-analysis showed that the prevalence of significant abnormalities on head CT or MRI for migraine patients with a normal neurologic examination ranged from 0% to 3.1% with an overall prevalence of 0.18% (1 in 555).10 Therefore, the USHC does not recommend neuroimaging for patients with a normal neurologic examination who meet the IHS diagnostic criteria for migraine (level of evidence [LOE]: B, using the Centre for Evidence-Based Medicine classification scheme). Neuroimaging should be considered for patients for whom a diagnosis is less clear cut (LOE: C).
Further support for this recommendation is found in a well-designed retrospective study demonstrating that the rate of significant intracranial pathology (mass lesion or hemorrhage) in patients presenting to primary care practices with a new headache and no neurologic findings was only 0.35%.11 Some patients and physicians will find even this low risk unacceptable and will obtain neuroimaging studies for reasons (such as litigation fears, risk perception, and so forth) that likely are not amenable to statistical argument.
TABLE 1
DIAGNOSTIC CRITERIA FOR MIGRAINE
Migraine Without Aura
|
Migraine With Aura
|
| In both cases, the diagnosis of migraine cannot be made if the history or physical examination suggests another disorder unless that disorder has been ruled out by appropriate testing or the migraine attacks do not occur for the first time in close temporal relation to the disorder. |
| Adapted, with permission, from Headache Classification Committee of the International Headache Society. Diagnostic Criteria. Available at: http://www.i-h-s.org/ihsnew/guidelines/pdfs/diagnost.pdf. Accessed May 28, 2001. |
TABLE 2
DIAGNOSTIC FEATURES IN MIGRAINE
| Finding | Sensitivity (%) | Specificity (%) | LR+ | LR- | PV+% (M/F) | PV-% (M/F) |
|---|---|---|---|---|---|---|
| Versus Patients With Tension-Type Headache | ||||||
| Nausea | 81 | 96 | 19.2 | 0.20 | 56/82 | 1.2/4.2 |
| Photophobia | 79 | 86 | 5.8 | 0.25 | 26/55 | 1.5/5.1 |
| Phonophobia | 67 | 87 | 5.2 | 0.38 | 25/53 | 2.4/7.7 |
| Exacerbation by physical activity | 81 | 78 | 3.7 | 0.24 | 19/45 | 1.5/5.1 |
| Unilateral location | 65 | 82 | 3.7 | 0.43 | 19/44 | 2.7/8.6 |
| Throbbing or pulsating quality | 73 | 75 | 2.9 | 0.36 | 16/39 | 2.2/7.3 |
| Precipitated by chocolate | 33 | 95 | 7.1 | 0.70 | 30/59 | 4.3/13 |
| Versus Patients Without History of Headache | ||||||
| Family history of migraine | 58 | 88 | 5.0 | 0.47 | 24/51 | 3.0/10 |
| LR+ denotes positive likelihood ratio; LR-, negative likelihood ratio; PV+, probability of migraine given a positive finding; PV-, probability of migraine given a negative finding. | ||||||
| Prevalence of migraine in the US population is 6% for men (M) and 18% for women (F).1 | ||||||
| Adapted, with permission, from Smetana GW. The diagnostic value of historical features in primary headache syndromes: a comprehensive review. Arch Intern Med 2000; 160:2729-37. ©2000 American Medical Association. | ||||||
Treatment
General principles
Although the diagnostic criteria for migraine are relatively straightforward, the expression of these symptoms can be highly variable, both between patients and in any given patient between attacks. In addition, patients with migraine often experience intercurrent tension or other primary headaches, complicating both the diagnosis and the interpretation of response to a therapeutic trial. Consequently, finding the right medication for an individual is often challenging. The choice of treatment may be suggested or limited by coexisting conditions. The presence of severe nausea or vomiting during a migraine may require use of a medication that can be dosed other than by mouth.
Patient education and involvement in the development and evaluation of a migraine treatment plan is essential. Just as migraine sufferers differ in the type, frequency, and severity of their symptoms, they also differ in their treatment preferences and goals. Some are unable to tolerate certain side effects; others are more interested in rapid relief of pain. Discussions regarding expected responses to treatment can prevent patients’ disappointment and losing patients to follow-up. For example, a reduction in the frequency of headaches over the course of several months is a more realistic goal than immediate prevention of all headaches. A patient’s headache diary can aid the patient in identifying and possibly eliminating migraine triggers and greatly assist the physician in adjusting and refining a treatment plan.
Various treatments, both pharmacologic and nonpharmacologic, have been used to treat patients with migraine. This article examines treatments in 3 categories: abortive medications, prophylactic medications, and nonpharmacologic treatments.
Abortive medications
Table 3 lists over-the-counter (OTC) and prescription medications for acute migraine attacks. Until recently, little if any high-quality evidence existed to guide the physician in selecting the appropriate medication for a specific patient. The USHC issued a consensus recommendation that nonsteroidal antiinflammatory drugs (NSAIDs) and over-the-counter analgesics be considered first-line treatments, especially for mild migraine headaches, and that migraine-specific agents be used for patients with more severe episodes.12
Further support for this stratified-care approach to migraine treatment has since been provided by the Disability in Strategies of Care (DISC) Study. DISC demonstrated that patients whose treatment was chosen according to their Migraine Disability Assessment Scale (MIDAS) score (those with a score of I or II were treated with aspirin and metoclopramide; those with a score of III or IV were treated with zolmitriptan) had less disability and a significantly greater headache response at 2 hours than patients who were given zolmitriptan if their headaches failed to respond to aspirin and metoclopramide.13 The study supports the expert consensus that patients with a history of mild disability associated with migraine can be treated effectively with simple OTC analgesics, whereas patients with significant migraine-associated disability will have better outcomes if treated with migraine-specific medications (LOE: B).
Mild to moderate migraine can be treated effectively with an oral combination of aspirin, acetaminophen, and caffeine (Excedrin or generic substitutes) or aspirin plus metoclopramide (LOE: A). Patients who cannot take aspirin may respond to 1000 mg acetaminophen alone (LOE: B).
Triptans (5-hydroxytryptamine1B/1D receptor agonists) are the drugs of choice for the acute treatment of moderate to severe migraine (except hemiplegic or basilar migraine) (LOE: A). Contraindications include coronary artery disease, uncontrolled hypertension, pregnancy, and recent monoamine oxidase inhibitor or ergot alkaloid use. Little evidence exists to recommend one triptan over another. A few studies suggest that the newer oral triptans may be slightly more efficacious than oral sumatriptan, although the differences do not appear overwhelming.14-16
There have been no recent studies on isometheptene-containing compounds such as Midrin. Three randomized placebo-controlled trials in the mid-1970s found a modest but statistically significant effect on migraine pain.17-19 However, the lack of standardized inclusion criteria and outcome measures makes it difficult to draw firm, valid conclusions about the efficacy of isometheptene.20 These drugs should be considered second line in the acute treatment of migraine (LOE: B).
A number of randomized controlled studies have demonstrated the efficacy of acetaminophen–codeine combinations in the acute treatment of migraine.21-23 Some of these trials have used combinations that included other medications in addition to acetaminophen and codeine; no study has been done on the dose most readily available in the United States (ie, 300 mg acetaminophen plus 30 mg codeine). Concerns about abuse, tolerance, and rebound headache appropriately limit their use. In addition, there is no evidence that they are more effective than other abortive treatments; one study showed no difference between the acute migraine relief provided by 1000 mg plain aspirin versus 400 mg acetaminophen and 25 mg codeine.21 While acetaminophen plus codeine combinations probably are effective in migraine, they are second-line drugs (LOE: B).
No randomized, placebo-controlled trials have evaluated the efficacy of butalbital-containing agents for migraine. Because of concerns relating to dependence, withdrawal, and rebound headache, the USHC recommends that use of these agents “should be limited and carefully monitored” (LOE: D).12
In the emergency department setting, prochlorperazine (10 mg given intravenously [IV]) is a safe and effective treatment for migraine (LOE: A).24 Dihydroergotamine (DHE) given IV or intramuscularly (IM) in combination with antiemetics is at least as good as meperidine (IV or IM) in relieving the pain of migraine (LOE: A).25,26 Despite the widespread use of parenteral meperidine in this setting, there are no placebo-controlled studies documenting its effectiveness in the treatment of migraine headache.
TABLE 3
SELF-ADMINISTERED ACUTE TREATMENT OPTIONS IN MIGRAINE
| Strength of Recommendation | Treatment (Route of Administration) | Comments |
|---|---|---|
| A | Acetaminophen +aspirin + caffeine (PO) | NNT* 3.9 (3.2 to 4.9)51 |
| A | Aspirin (PO) | NNT range from 3.5 to 5.552 |
| A | Aspirin + metoclopramide (PO) | NNT 3.2 (2.6 to 4.0)53 |
| A | Butorphanol (IN) | Abuse/dependence and rebound headache potential |
| A | DHE (IN) | NNT 2.5 (1.9 to 3.7)54 |
| A | NSAIDs (PO) | NNT 7.5 (4.5 to 22) (for ibuprofen)55 |
| A | Triptans (PO) | NNT range from 2.7 to 5.456 |
| A | Sumatriptan (IN) | NNT 3.4 (2.9 to 4.1)56 |
| A | Sumatriptan (SC) | NNT 2.0 (1.8 to 2.2)56 |
| B | Acetaminophen (PO) | NNT 5.2 (3.3 to 13)57 |
| B | Acetaminophen + codeine (PO) | Abuse/dependence and rebound headache potential |
| B | Isometheptene compounds (PO) | Limited clinical trial data. |
| D | Butalbital compounds (PO) | No clinical trials; risk of rebound headache |
| D | Ergotamine (PO) | Conflicting evidence; increased risk of adverse effects |
| * Numbers needed to treat (NNT; 95% confidence interval) in this column are for headache response (reduction in headache severity from “severe” or “moderate” to “mild” or “none”) at 2 hours; included when available data permit. | ||
| IN denotes intranasal; PO, by mouth; SC, subcutaneous. | ||
Prophylactic medications
The USHC recommends that preventive treatment be considered for patients with migraine who desire a reduction in the frequency or severity of their headaches for any reason, including but not limited to frequent headaches that significantly interfere with daily activities despite acute treatment, unpleasant side effects associated with abortive medications, or the cost of abortive medications (LOE: D).27Table 4 lists medications available in the United States that are used in the prophylaxis of migraine.
Beta blockers, particularly propranolol, are commonly prescribed and are very effective in reducing the frequency of migraine (LOE: A).27-30 Most authorities consider them the migraine prophylactic of choice in patients with no contraindications (eg, asthma, congestive heart failure, or heart block).
Amitriptyline is the only antidepressant to demonstrate consistent efficacy in migraine prophylaxis.27,31,32 This medication may be especially useful in patients who suffer from both migraine and tension headaches.33 Divalproex sodium is another drug clearly shown effective against migraine prophylactically.27,30,34 The risk of significant hematologic and hepatic side effects requires laboratory monitoring and may limit its use in many patients.
Calcium channel blockers (CCBs), particularly verapamil, are widely used by both primary care physicians and neurologists for the prevention of migraine,35 and yet only 3 controlled trials of verapamil are reported in the English language literature. Two methodologically weak studies showed a small but significant effect from verapamil36,37; the third demonstrated no advantage over placebo.38 The only CCB consistently shown effective for migraine prophylaxis is flunarizine.27 Unfortunately, it is not available in the United States.
Besides use for acute treatment, NSAIDs are occasionally prescribed to prevent migraine. Naproxen sodium, the most frequently studied NSAID, shows a small but significant effect in overall improvement compared with placebo in several trials.39-41 Two of these studies showed a reduction in the number of severe headaches per week but no significant change in the total number of headaches per week.40,41
Some recent studies support the use of novel migraine prophylactics. One study of riboflavin (400 mg daily) showed a moderate reduction in migraine frequency.42 Achieving maximal therapeutic effect required 3 months of use. Another study found that 10 mg lisinopril daily can significantly reduce migraine frequency and severity when compared with placebo.43
TABLE 4
PROPHYLACTIC TREATMENT OPTIONS IN MIGRAINE
| Strength of Recommendation | Treatment | Comments |
|---|---|---|
| A | Amitriptyline | Evidence for no significant difference versus propranolol32, 33 |
| A | Divalproex sodium | NNT* range from 2.1 to 2.930, 34 |
| A | Propranolol | NNT range from 2.3 to 528-30 |
| B | Lisinopril | Based on 1 study (level 1b)43 |
| B | Naproxen sodium | Risk of rebound headache |
| B | Riboflavin | NNT 2.842 based on 1 study (level 1b) |
| D | Verapamil | Considered effective by many experts; limited, poor-quality clinical trials (see text) |
| * Numbers needed to treat (NNT) in this column are for a 50% reduction in headache frequency compared with baseline; reported when available data permit. | ||
Nonpharmacologic treatments
Although the data for nonpharmacologic migraine treatment are neither so extensive nor so rigorous as those for medications, some evidence is available. The Duke Center for Clinical Health Policy Research performed a comprehensive systematic review and meta-analysis of behavioral and physical treatments for migraine for the Agency for Healthcare Research and Quality.44 This review forms the evidence base for the USHC guideline in this area.45 The authors note that most studies were conducted on patients recruited at specialized headache centers; thus, caution should be exercised in generalizing the results to a primary care population.
The meta-analysis showed that cognitive–behavioral (including stress management) therapy, electromyelogram biofeedback, relaxation training, and thermal biofeedback combined with relaxation training are effective in migraine prophylaxis (LOE: B).44 An earlier meta-analysis concluded that the prophylactic benefit of combined relaxation and thermal biofeedback training was equivalent to the benefit obtained from propranolol.46 Because of limited or mixed evidence, no clear recommendations can be made with regard to acupuncture, cervical manipulation, hyperbaric oxygen, hypnosis, occlusal adjustment, or transcutaneous electronic nerve stimulation.45
Prognosis
Little evidence is available concerning the long-term prognosis of migraine, either with or without treatment. For many patients, migraine persists, but slowly decreases in frequency over a lifetime.47,48 For patients who respond well to prophylaxis, no data are available to help the clinician decide how long to continue using it. One small case series showed that while a few patients had a lasting reduction in the frequency of their migraines after stopping effective prophylactic medication, most experienced relapse.49
A subset of patients with migraine develops headaches of increasing frequency, often resulting in daily or continuous headaches. This syndrome has been known as transformed or malignant migraine. Many such patients use migraine medications on a daily basis. Although no controlled trials have been reported, the daily or near-daily use of most acute migraine medications (including acetaminophen, aspirin, dihydroergotamine, ergotamine, NSAIDs, opioids, and triptans) is believed capable of provoking medication-overuse headaches.50 Some of these patients can reduce the frequency of their headaches if they can break the cycle of medication use.47
Conclusions
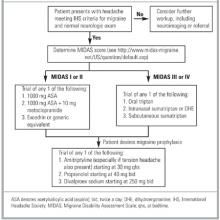
Migraine headache is a common and disabling condition. The diagnosis often can be made on the basis of key findings in the patient’s history. A classic history, in combination with a normal neurologic examination, obviates head imaging. Available evidence clearly shows that effective methods for both acute and prophylactic treatment of migraine exist. The Figure contains an algorithm summarizing such treatment. Wider implementation of the USHC evidence-based guidelines by primary care physicians treating those with migraine should result in decreased pain and increased productivity for many patients.
FIGURE
ALGORITHM FOR TREATMENT OF MIGRAINE
Acknowledgments
The author would like to thank John R. Holman, MD, MPH, for reviewing the manuscript and Anne J. O’Connor for her help in obtaining the references.
1. Stewart WF, Lipton RB, Celentano DD, Reed ML. Prevalence of migraine headache in the United States: relation to age, income, race and other sociodemographic factors. JAMA 1992;267:64-9.
2. Stewart WF, Lipton RB. Migraine headache: epidemiology and health care utilization. Cephalalgin 1993;13(suppl 12):41-6.
3. Schappert SM, Nelson C. National Ambulatory Medical Care Survey, 1995-1996 Summary. National Center for Health Statistics. Vital Health Stat 13(142). 1999.
4. Hu XH, Markson LE, Lipton RB, Stewart WF, Berger ML. Burden of migraine in the United States: disability and economic costs. Arch Intern Med 1999;159:813-8.
5. Goadsby PJ. Current concepts of the pathophysiology of migraine. Neurol Clin 1997;15:27-42.
6. Headache Classification Committee of the International Headache Society. Diagnostic criteria. Available at: www.i-h-s.org/ihsnew/guidelines/pdfs/diagnost.pdf/. Accessed May 28, 2001.
7. Smetana GW. The diagnostic value of historical features in primary headache syndromes: a comprehensive review. Arch Intern Med 2000;160:2729-37.
8. Diagnosing migraine. Available at: http://www.jr2.ox.ac.uk/bandolier/booth/Migraine/Diagmig.html/. Accessed November 6, 2001.
9. McCrory DC, Matchar DB, Rosenberg JH, Silberstein SD. Evidenced-based guidelines for migraine headache: overview of program description and methodology. Available at: www.aan.com/public/practiceguidelines/01.pdf/. Accessed November 29, 2001.
10. Frishberg BM, Rosenberg JH, Matchar DB, McCrory DC, Rozen TD, Silberstein SD. Evidence-based guidelines in the primary care setting: neuroimaging in patients with nonacute headache. Available at: www.aan.com/public/practiceguidelines/02.pdf/. Accessed November 29, 2001.
11. Becker LA, Green LA, Beaufait D, Kirk J, Froom J, Freeman WL. Detection of intracranial tumors, subarachnoid hemorrhages, and subdural hematomas in primary care patients: a report from ASPN, Part 2. J Fam Pract 1993;37:135-41.
12. Matchar DB, Young WB, Rosenberg JH, et al. Evidence-based guidelines for migraine headache in the primary care setting: pharmacological management of acute attacks. Available at: www.aan.com/public/practiceguidelines/03.pdf/. Accessed November 29, 2001.
13. Lipton RB, Stewart WF, Stone AM, Lainez MJA, Sawyer JPC. Stratified care vs step care strategies for migraine. The disability in strategies of care (DISC) study: a randomized trial. JAMA 2000;284:2599-605.
14. Tfelt-Hansen P, Teall J, Rodriguez F, et al. Oral rizatriptan versus oral sumatriptan: a direct comparative study in the acute treatment of migraine. Headache 1998;38:748-55.
15. Gallagher R, Dennish G, Spierings EL, Chitra R. A comparative trial of zolmitriptan and sumatriptan for the acute oral treatment of migraine. Headache 2000;40:119-28.
16. Gobel H, Winter P, Boswell D, Crisp A, Becker W, Hauge T, et al. Comparison of naratriptan and sumatriptan in recurrence-prone migraine patients. Clin Ther 2000;22:981-9.
17. Ryan RE. A study of Midrin in the symptomatic relief of migraine headache. Headache 1974;14:33-42.
18. Diamond S, Medina JL. Isometheptene-a non-ergot drug in the treatment of migraine. Headache 1975;15:211-3.
19. Diamond S. Treatment of migraine with isometheptene, acetaminophen, and dichloralphenazone combination: a double-blind, crossover trial. Headache 1976;15:282-7.
20. Isometheptene for acute migraine. Available at: http://www.jr2.ox.ac.uk/bandolier/booth/Migraine/IsomORacu.html/. Accessed November 9, 2001.
21. Boureau F, Joubert JM, Lasserre V, Prum B, Delecoeuillerie G. Double-blind comparison of an acetaminophen 400 mg-codeine 25 mg combination versus aspirin 1000 mg and placebo in acute migraine attack. Cephalalgia 1994;14:156-61.
22. Adam EI. A treatment for the acute migraine attack. J Int Med Res 1987;15:71-5.
23. Carasso RL, Yehuda S. The prevention and treatment of migraine with an analgesic combination. Br J Clin Pract 1984;38:25-7.
24. Coppola M, Yealy DM, Leibold RA. Randomized, placebo-controlled evaluation of prochlorperazine versus metoclopramide for emergency department treatment of migraine headache. Ann Emerg Med 1995;26:541-6.
25. Klapper JA, Stanton J. Current emergency treatment of severe migraine headaches. Headache 1993;33:560-2.
26. Carleton SC, Shesser RF, Pietrzak MP, et al. Double-blind, multicenter trial to compare the efficacy of intramuscular dihydroergotamine plus hydroxyzine versus intramuscular meperidine plus hydroxyzine for the emergency department treatment of acute migraine headache. Ann Emerg Med 1998;32:129-38.
27. Ramadan NM, Silberstein SD, Freitag FG, Gilbert TT, Frishberg BM. Evidence-based guidelines for migraine headache in the primary care setting: pharmacological management for the prevention of migraine. Available at: www.aan.com/public/practiceguidelines/05.pdf/. Accessed November 29, 2001.
28. Borgesen SE, Nielsen JL, Moller CE. Prophylactic treatment of migraine with propranolol: a clinical trial. Acta Neurol Scand 1974;50:651-6.
29. Tfelt-Hansen P, Standnes B, Kangasniemi P, Hakkarainen H, Olesen J. Timolol vs. propranolol vs. placebo in common migraine prophylaxis: a double-blind multicenter trial. Acta Neurol Scand 1984;69:1-8.
30. Kaniecki RG. A comparison of divalproex with propranolol and placebo for the prophylaxis of migraine without aura. Arch Neurol 1997;54:1141-5.
31. Couch JR, Hassanein RS. Amitriptyline in migraine prophylaxis. Arch Neurol 1979;36:695-9.
32. Ziegler DK, Hurwitz A, Hassanein RS, Kodanaz HA, Preskorn SH, Mason J. Migraine prophylaxis: a comparison of propranolol and amitriptyline. Arch Neurol 1987;44:486-9.
33. Mathew NT. Prophylaxis of migraine and mixed headache. A randomized controlled study. Headache 1981;21:105-9.
34. Mathew NT, Saper JR, Silberstein SD, et al. Migraine prophylaxis with divalproex. Arch Neurol 1995;52:281-6.
35. Ramadan NM, Schultz LL, Gilkey SJ. Migraine prophylactic drugs: proof of efficacy, utilization and cost. Cephalalgia 1997;17:73-80.
36. Solomon GD, Steel JG, Spaccavento LJ. Verapamil prophylaxis of migraine: a double-blind, placebo-controlled study. JAMA 1983;250:2500-2.
37. Markley HG, Cheronis JC, Piepho RW. Verapamil in prophylactic therapy of migraine. Neurology 1984;34:973-6.
38. Solomon GD. Verapamil and propranolol in migraine prophylaxis; a double-blind, cross-over study. Headache 1986;26:325.-
39. Ziegler DK, Ellis DJ. Naproxen in prophylaxis of migraine. Arch Neurol 1985;42:582-4.
40. Sargent J, Solbach P, Damasio H, et al. A comparison of naproxen sodium to propranolol hydrochloride and a placebo control for the prophylaxis of migraine headache. Headache 1985;25:320-4.
41. Welch KMA, Ellis DJ, Keenan PA. Successful migraine prophylaxis with naproxen sodium. Neurology 1985;35:1304-10.
42. Schoenen J, Jacquy J, Lenaerts M. Effectiveness of high-dose riboflavin in migraine prophylaxis: a randomized controlled trial. Neurology 1998;50:466-70.
43. Schrader H, Stoner LJ, Helde G, Sand T, Bovim G. Prophylactic treatment of migraine with angiotensin converting enzyme inhibitor (lisinopril): randomised, placebo controlled, crossover study. BMJ 2001;322:1-5.
44. Goslin RE, Gray RN, McCrory DC, Penzien D, Rains J, Hasselblad V. Behavioral and physical treatments for migraine headache. Technical review 2.2. February 1999. Prepared for the Agency for Health Care Policy and Research under Contract No. 290-94-2025. Available at: http://www.clinpol.mc.duke.edu./Pubs/Publications/Behavioral_Manuscript.pdf/. Accessed November 27, 2001.
45. Campbell JK, Penzien DB, Wall EM. Evidence-based guidelines for migraine headache: behavioral and physical treatments. Available at: www.aan.com/public/practiceguidelines/04.pdf/. Accessed November 29, 2001.
46. Holroyd KA, Penzien DB. Pharmacological versus non-pharmacological prophylaxis of recurrent migraine headache: a meta-analytic review of clinical trials. Pain 1990;42:1-13.
47. Silberstein SD, Lipton RB. Headache epidemiology. Emphasis on migraine. Neurol Clin 1996;14:421-34.
48. Silberstein SD, Young WB. Headache and facial pain. In: Goetz CG, Pappert EJ, eds. Textbook of clinical neurology. 1st ed. Philadelphia, Pa: Saunders; 1999:1095.
49. Wober C, Wober-Bingol C, Kock G, Wessely P. Long-term results of migraine prophylaxis with flunarazine and beta-blockers. Cephalalgia. 1991;11:251-6.
50. Diener HC, Dahlof CGH. Headache associated with chronic use of substances. In: Olesen J, Tfelt-Hansen P, Welch KMA, eds. The headaches. 2nd ed. Philadelphia, Pa: Lippincott, Williams & Wilkins; 2000:871-7.
51. Paracetamol, aspirin caffeine incombination (Excedrin) for acute migraine. Available at: http://www.jr2.ox.ac.uk/bandolier/booth/Migraine/Excedr.html/. Accessed November 9, 2001.
52. Aspirin for acute migraine. Available at: http://www.jr2.ox.ac.uk/bandolier/booth/Migraine/Aspacute.html/. Accessed November 9, 2001.
53. Aspirin plus metoclopramide for acute migraine. Available at: http://www.jr2.ox.ac.uk/bandolier/booth/Migraine/AsMcOacu.html/. Accessed November 9, 2001.
54. Intranasal dihydroergotamine for acute migraine Available at: http://www.jr2.ox.ac.uk/bandolier/booth/Migraine/DHEINacu.html/. Accessed November 9, 2001.
55. Ibuprofen for acute migraine (new RCT). Available at: http://www.jr2.ox.ac.uk/bandolier/booth/Migraine/ibu2.html/. Accessed November 9, 2001.
56. Migraine league table: acute treatments and two hour headache response. Available at: http://www.jr2.ox.ac.uk/bandolier/booth/Migraine/League.html/. Accessed November 9, 2001.
57. Lipton RB, Baggish JS, Stewart WF, Codispoti JR, Fu M. Efficacy and safety of acetaminophen in the treatment of migraine: results of a randomized, double-blind, placebo-controlled, population-based study. Arch Intern Med 2000;160:3486-92
- The International Headache Society criteria provide a useful standardized way to diagnose migraine clinically.
- Neuroimaging is not necessary for patients who clearly meet clinical criteria for migraine and whose neurologic examination results are normal.
- Over-the-counter drugs (including aspirin, ibuprofen, and the combination of aspirin, acetaminophen, and caffeine) work well and are first-line treatments for mild migraine.
- Migraine-specific medications (including intranasal dihydroergotamine [DHE] and the triptans) are recommended for more severe migraine; little evidence exists to suggest one drug over another.
- Prophylaxis is recommended if patients find the severity or frequency of headaches bothersome enough to warrant preventive measures; amitriptyline, divalproex sodium, and propranolol are effective prophylaxes.
Migraine is a common and disabling condition. Among adults in the United States, approximately 18% of women and 6% of men report symptoms consistent with migraine1; less than half have been diagnosed by a physician or received prescription treatment from a physician.2 Migraine accounts for more than 2.8 million visits per year to US physicians and is the reason for encounter in about 1 visit per week to the typical family physician.3 Migraine is estimated to cost US employers more than $13 billion each year; direct medical costs exceed $1 billion annually.4
Pathophysiology
The exact pathophysiology of migraine is unknown. The prevailing theory is that a trigger (such as fatigue, stress, or certain foods) sets off a wave of brief neuronal activation, followed by a more sustained neuronal inhibition known as cortical spreading depression (CSD). At some point the trigeminovascular system is activated (possibly by CSD), releasing vasoactive neuropeptides that cause a painful inflammatory response in the meninges. Stimulation of presynaptic serotonin receptors inhibits release of the inflammatory neuropeptides; this is one possible explanation for the effectiveness of the triptans.5
Diagnosis
Migraine is a syndrome diagnosed by a certain combination of signs and symptoms. The International Headache Society (IHS) diagnostic criteria (Table 1) are widely accepted as the reference standard for the diagnosis of migraine, as well as that of other types of headache.6 Although they were originally intended to assist in the standardization of research subjects, the criteria for the most common headache disorders can be adapted for diagnosis in the clinical setting. Migraine diagnosis is based almost entirely on the history; the main role of the physical examination is to screen for life-threatening conditions, such as intracranial hemorrhage or tumors.
In some patients, migraine is difficult to distinguish from other primary or secondary headaches, especially tension-type headache. A recent meta-analysis demonstrated that the features most helpful to rule in migraine (compared with tension-type headache) are nausea (positive likelihood ratio [LR+] = 19.2), photophobia (LR+ = 5.8), and phonophobia (LR+ = 5.2). Table 2 provides additional information regarding these and other significant findings, including the post-test probabilities of migraine given the reported prevalence among adult men and women in the United States. The likelihood ratios are probably somewhat inflated, since many of these symptoms are also part of the criteria for the reference standard (“incorporation bias”). The IHS criteria for migraine without aura require nausea or the combination of photophobia and phonophobia to make the diagnosis; it is therefore not surprising that these findings would be the most specific.
While the presence of any single feature may not be sufficient to clinch the diagnosis, sequentially combining the post-test probabilities can prove useful in cases that are not straightforward. For example, a woman with a family history of migraine who complains of a unilateral headache accompanied by photophobia but no nausea has an approximately 80% post-test probability of migraine. This conclusion assumes statistical independence of these symptoms and thus may overestimate the probability somewhat.8
Migraine has no specific diagnostic findings on computed tomography (CT) or magnetic resonance imaging (MRI). The best evidence addressing the use of neuroimaging studies in migraine, as well as most other diagnostic and management issues, comes from the United States Headache Consortium (USHC), a panel of experts from several specialty societies and professional organizations, including the American Academy of Family Physicians. In April 2000, the USHC issued diagnosis and treatment guidelines based on rigorous evidence-based reviews of the medical literature.9 A USHC meta-analysis showed that the prevalence of significant abnormalities on head CT or MRI for migraine patients with a normal neurologic examination ranged from 0% to 3.1% with an overall prevalence of 0.18% (1 in 555).10 Therefore, the USHC does not recommend neuroimaging for patients with a normal neurologic examination who meet the IHS diagnostic criteria for migraine (level of evidence [LOE]: B, using the Centre for Evidence-Based Medicine classification scheme). Neuroimaging should be considered for patients for whom a diagnosis is less clear cut (LOE: C).
Further support for this recommendation is found in a well-designed retrospective study demonstrating that the rate of significant intracranial pathology (mass lesion or hemorrhage) in patients presenting to primary care practices with a new headache and no neurologic findings was only 0.35%.11 Some patients and physicians will find even this low risk unacceptable and will obtain neuroimaging studies for reasons (such as litigation fears, risk perception, and so forth) that likely are not amenable to statistical argument.
TABLE 1
DIAGNOSTIC CRITERIA FOR MIGRAINE
Migraine Without Aura
|
Migraine With Aura
|
| In both cases, the diagnosis of migraine cannot be made if the history or physical examination suggests another disorder unless that disorder has been ruled out by appropriate testing or the migraine attacks do not occur for the first time in close temporal relation to the disorder. |
| Adapted, with permission, from Headache Classification Committee of the International Headache Society. Diagnostic Criteria. Available at: http://www.i-h-s.org/ihsnew/guidelines/pdfs/diagnost.pdf. Accessed May 28, 2001. |
TABLE 2
DIAGNOSTIC FEATURES IN MIGRAINE
| Finding | Sensitivity (%) | Specificity (%) | LR+ | LR- | PV+% (M/F) | PV-% (M/F) |
|---|---|---|---|---|---|---|
| Versus Patients With Tension-Type Headache | ||||||
| Nausea | 81 | 96 | 19.2 | 0.20 | 56/82 | 1.2/4.2 |
| Photophobia | 79 | 86 | 5.8 | 0.25 | 26/55 | 1.5/5.1 |
| Phonophobia | 67 | 87 | 5.2 | 0.38 | 25/53 | 2.4/7.7 |
| Exacerbation by physical activity | 81 | 78 | 3.7 | 0.24 | 19/45 | 1.5/5.1 |
| Unilateral location | 65 | 82 | 3.7 | 0.43 | 19/44 | 2.7/8.6 |
| Throbbing or pulsating quality | 73 | 75 | 2.9 | 0.36 | 16/39 | 2.2/7.3 |
| Precipitated by chocolate | 33 | 95 | 7.1 | 0.70 | 30/59 | 4.3/13 |
| Versus Patients Without History of Headache | ||||||
| Family history of migraine | 58 | 88 | 5.0 | 0.47 | 24/51 | 3.0/10 |
| LR+ denotes positive likelihood ratio; LR-, negative likelihood ratio; PV+, probability of migraine given a positive finding; PV-, probability of migraine given a negative finding. | ||||||
| Prevalence of migraine in the US population is 6% for men (M) and 18% for women (F).1 | ||||||
| Adapted, with permission, from Smetana GW. The diagnostic value of historical features in primary headache syndromes: a comprehensive review. Arch Intern Med 2000; 160:2729-37. ©2000 American Medical Association. | ||||||
Treatment
General principles
Although the diagnostic criteria for migraine are relatively straightforward, the expression of these symptoms can be highly variable, both between patients and in any given patient between attacks. In addition, patients with migraine often experience intercurrent tension or other primary headaches, complicating both the diagnosis and the interpretation of response to a therapeutic trial. Consequently, finding the right medication for an individual is often challenging. The choice of treatment may be suggested or limited by coexisting conditions. The presence of severe nausea or vomiting during a migraine may require use of a medication that can be dosed other than by mouth.
Patient education and involvement in the development and evaluation of a migraine treatment plan is essential. Just as migraine sufferers differ in the type, frequency, and severity of their symptoms, they also differ in their treatment preferences and goals. Some are unable to tolerate certain side effects; others are more interested in rapid relief of pain. Discussions regarding expected responses to treatment can prevent patients’ disappointment and losing patients to follow-up. For example, a reduction in the frequency of headaches over the course of several months is a more realistic goal than immediate prevention of all headaches. A patient’s headache diary can aid the patient in identifying and possibly eliminating migraine triggers and greatly assist the physician in adjusting and refining a treatment plan.
Various treatments, both pharmacologic and nonpharmacologic, have been used to treat patients with migraine. This article examines treatments in 3 categories: abortive medications, prophylactic medications, and nonpharmacologic treatments.
Abortive medications
Table 3 lists over-the-counter (OTC) and prescription medications for acute migraine attacks. Until recently, little if any high-quality evidence existed to guide the physician in selecting the appropriate medication for a specific patient. The USHC issued a consensus recommendation that nonsteroidal antiinflammatory drugs (NSAIDs) and over-the-counter analgesics be considered first-line treatments, especially for mild migraine headaches, and that migraine-specific agents be used for patients with more severe episodes.12
Further support for this stratified-care approach to migraine treatment has since been provided by the Disability in Strategies of Care (DISC) Study. DISC demonstrated that patients whose treatment was chosen according to their Migraine Disability Assessment Scale (MIDAS) score (those with a score of I or II were treated with aspirin and metoclopramide; those with a score of III or IV were treated with zolmitriptan) had less disability and a significantly greater headache response at 2 hours than patients who were given zolmitriptan if their headaches failed to respond to aspirin and metoclopramide.13 The study supports the expert consensus that patients with a history of mild disability associated with migraine can be treated effectively with simple OTC analgesics, whereas patients with significant migraine-associated disability will have better outcomes if treated with migraine-specific medications (LOE: B).
Mild to moderate migraine can be treated effectively with an oral combination of aspirin, acetaminophen, and caffeine (Excedrin or generic substitutes) or aspirin plus metoclopramide (LOE: A). Patients who cannot take aspirin may respond to 1000 mg acetaminophen alone (LOE: B).
Triptans (5-hydroxytryptamine1B/1D receptor agonists) are the drugs of choice for the acute treatment of moderate to severe migraine (except hemiplegic or basilar migraine) (LOE: A). Contraindications include coronary artery disease, uncontrolled hypertension, pregnancy, and recent monoamine oxidase inhibitor or ergot alkaloid use. Little evidence exists to recommend one triptan over another. A few studies suggest that the newer oral triptans may be slightly more efficacious than oral sumatriptan, although the differences do not appear overwhelming.14-16
There have been no recent studies on isometheptene-containing compounds such as Midrin. Three randomized placebo-controlled trials in the mid-1970s found a modest but statistically significant effect on migraine pain.17-19 However, the lack of standardized inclusion criteria and outcome measures makes it difficult to draw firm, valid conclusions about the efficacy of isometheptene.20 These drugs should be considered second line in the acute treatment of migraine (LOE: B).
A number of randomized controlled studies have demonstrated the efficacy of acetaminophen–codeine combinations in the acute treatment of migraine.21-23 Some of these trials have used combinations that included other medications in addition to acetaminophen and codeine; no study has been done on the dose most readily available in the United States (ie, 300 mg acetaminophen plus 30 mg codeine). Concerns about abuse, tolerance, and rebound headache appropriately limit their use. In addition, there is no evidence that they are more effective than other abortive treatments; one study showed no difference between the acute migraine relief provided by 1000 mg plain aspirin versus 400 mg acetaminophen and 25 mg codeine.21 While acetaminophen plus codeine combinations probably are effective in migraine, they are second-line drugs (LOE: B).
No randomized, placebo-controlled trials have evaluated the efficacy of butalbital-containing agents for migraine. Because of concerns relating to dependence, withdrawal, and rebound headache, the USHC recommends that use of these agents “should be limited and carefully monitored” (LOE: D).12
In the emergency department setting, prochlorperazine (10 mg given intravenously [IV]) is a safe and effective treatment for migraine (LOE: A).24 Dihydroergotamine (DHE) given IV or intramuscularly (IM) in combination with antiemetics is at least as good as meperidine (IV or IM) in relieving the pain of migraine (LOE: A).25,26 Despite the widespread use of parenteral meperidine in this setting, there are no placebo-controlled studies documenting its effectiveness in the treatment of migraine headache.
TABLE 3
SELF-ADMINISTERED ACUTE TREATMENT OPTIONS IN MIGRAINE
| Strength of Recommendation | Treatment (Route of Administration) | Comments |
|---|---|---|
| A | Acetaminophen +aspirin + caffeine (PO) | NNT* 3.9 (3.2 to 4.9)51 |
| A | Aspirin (PO) | NNT range from 3.5 to 5.552 |
| A | Aspirin + metoclopramide (PO) | NNT 3.2 (2.6 to 4.0)53 |
| A | Butorphanol (IN) | Abuse/dependence and rebound headache potential |
| A | DHE (IN) | NNT 2.5 (1.9 to 3.7)54 |
| A | NSAIDs (PO) | NNT 7.5 (4.5 to 22) (for ibuprofen)55 |
| A | Triptans (PO) | NNT range from 2.7 to 5.456 |
| A | Sumatriptan (IN) | NNT 3.4 (2.9 to 4.1)56 |
| A | Sumatriptan (SC) | NNT 2.0 (1.8 to 2.2)56 |
| B | Acetaminophen (PO) | NNT 5.2 (3.3 to 13)57 |
| B | Acetaminophen + codeine (PO) | Abuse/dependence and rebound headache potential |
| B | Isometheptene compounds (PO) | Limited clinical trial data. |
| D | Butalbital compounds (PO) | No clinical trials; risk of rebound headache |
| D | Ergotamine (PO) | Conflicting evidence; increased risk of adverse effects |
| * Numbers needed to treat (NNT; 95% confidence interval) in this column are for headache response (reduction in headache severity from “severe” or “moderate” to “mild” or “none”) at 2 hours; included when available data permit. | ||
| IN denotes intranasal; PO, by mouth; SC, subcutaneous. | ||
Prophylactic medications
The USHC recommends that preventive treatment be considered for patients with migraine who desire a reduction in the frequency or severity of their headaches for any reason, including but not limited to frequent headaches that significantly interfere with daily activities despite acute treatment, unpleasant side effects associated with abortive medications, or the cost of abortive medications (LOE: D).27Table 4 lists medications available in the United States that are used in the prophylaxis of migraine.
Beta blockers, particularly propranolol, are commonly prescribed and are very effective in reducing the frequency of migraine (LOE: A).27-30 Most authorities consider them the migraine prophylactic of choice in patients with no contraindications (eg, asthma, congestive heart failure, or heart block).
Amitriptyline is the only antidepressant to demonstrate consistent efficacy in migraine prophylaxis.27,31,32 This medication may be especially useful in patients who suffer from both migraine and tension headaches.33 Divalproex sodium is another drug clearly shown effective against migraine prophylactically.27,30,34 The risk of significant hematologic and hepatic side effects requires laboratory monitoring and may limit its use in many patients.
Calcium channel blockers (CCBs), particularly verapamil, are widely used by both primary care physicians and neurologists for the prevention of migraine,35 and yet only 3 controlled trials of verapamil are reported in the English language literature. Two methodologically weak studies showed a small but significant effect from verapamil36,37; the third demonstrated no advantage over placebo.38 The only CCB consistently shown effective for migraine prophylaxis is flunarizine.27 Unfortunately, it is not available in the United States.
Besides use for acute treatment, NSAIDs are occasionally prescribed to prevent migraine. Naproxen sodium, the most frequently studied NSAID, shows a small but significant effect in overall improvement compared with placebo in several trials.39-41 Two of these studies showed a reduction in the number of severe headaches per week but no significant change in the total number of headaches per week.40,41
Some recent studies support the use of novel migraine prophylactics. One study of riboflavin (400 mg daily) showed a moderate reduction in migraine frequency.42 Achieving maximal therapeutic effect required 3 months of use. Another study found that 10 mg lisinopril daily can significantly reduce migraine frequency and severity when compared with placebo.43
TABLE 4
PROPHYLACTIC TREATMENT OPTIONS IN MIGRAINE
| Strength of Recommendation | Treatment | Comments |
|---|---|---|
| A | Amitriptyline | Evidence for no significant difference versus propranolol32, 33 |
| A | Divalproex sodium | NNT* range from 2.1 to 2.930, 34 |
| A | Propranolol | NNT range from 2.3 to 528-30 |
| B | Lisinopril | Based on 1 study (level 1b)43 |
| B | Naproxen sodium | Risk of rebound headache |
| B | Riboflavin | NNT 2.842 based on 1 study (level 1b) |
| D | Verapamil | Considered effective by many experts; limited, poor-quality clinical trials (see text) |
| * Numbers needed to treat (NNT) in this column are for a 50% reduction in headache frequency compared with baseline; reported when available data permit. | ||
Nonpharmacologic treatments
Although the data for nonpharmacologic migraine treatment are neither so extensive nor so rigorous as those for medications, some evidence is available. The Duke Center for Clinical Health Policy Research performed a comprehensive systematic review and meta-analysis of behavioral and physical treatments for migraine for the Agency for Healthcare Research and Quality.44 This review forms the evidence base for the USHC guideline in this area.45 The authors note that most studies were conducted on patients recruited at specialized headache centers; thus, caution should be exercised in generalizing the results to a primary care population.
The meta-analysis showed that cognitive–behavioral (including stress management) therapy, electromyelogram biofeedback, relaxation training, and thermal biofeedback combined with relaxation training are effective in migraine prophylaxis (LOE: B).44 An earlier meta-analysis concluded that the prophylactic benefit of combined relaxation and thermal biofeedback training was equivalent to the benefit obtained from propranolol.46 Because of limited or mixed evidence, no clear recommendations can be made with regard to acupuncture, cervical manipulation, hyperbaric oxygen, hypnosis, occlusal adjustment, or transcutaneous electronic nerve stimulation.45
Prognosis
Little evidence is available concerning the long-term prognosis of migraine, either with or without treatment. For many patients, migraine persists, but slowly decreases in frequency over a lifetime.47,48 For patients who respond well to prophylaxis, no data are available to help the clinician decide how long to continue using it. One small case series showed that while a few patients had a lasting reduction in the frequency of their migraines after stopping effective prophylactic medication, most experienced relapse.49
A subset of patients with migraine develops headaches of increasing frequency, often resulting in daily or continuous headaches. This syndrome has been known as transformed or malignant migraine. Many such patients use migraine medications on a daily basis. Although no controlled trials have been reported, the daily or near-daily use of most acute migraine medications (including acetaminophen, aspirin, dihydroergotamine, ergotamine, NSAIDs, opioids, and triptans) is believed capable of provoking medication-overuse headaches.50 Some of these patients can reduce the frequency of their headaches if they can break the cycle of medication use.47
Conclusions
Migraine headache is a common and disabling condition. The diagnosis often can be made on the basis of key findings in the patient’s history. A classic history, in combination with a normal neurologic examination, obviates head imaging. Available evidence clearly shows that effective methods for both acute and prophylactic treatment of migraine exist. The Figure contains an algorithm summarizing such treatment. Wider implementation of the USHC evidence-based guidelines by primary care physicians treating those with migraine should result in decreased pain and increased productivity for many patients.
FIGURE
ALGORITHM FOR TREATMENT OF MIGRAINE
Acknowledgments
The author would like to thank John R. Holman, MD, MPH, for reviewing the manuscript and Anne J. O’Connor for her help in obtaining the references.
- The International Headache Society criteria provide a useful standardized way to diagnose migraine clinically.
- Neuroimaging is not necessary for patients who clearly meet clinical criteria for migraine and whose neurologic examination results are normal.
- Over-the-counter drugs (including aspirin, ibuprofen, and the combination of aspirin, acetaminophen, and caffeine) work well and are first-line treatments for mild migraine.
- Migraine-specific medications (including intranasal dihydroergotamine [DHE] and the triptans) are recommended for more severe migraine; little evidence exists to suggest one drug over another.
- Prophylaxis is recommended if patients find the severity or frequency of headaches bothersome enough to warrant preventive measures; amitriptyline, divalproex sodium, and propranolol are effective prophylaxes.
Migraine is a common and disabling condition. Among adults in the United States, approximately 18% of women and 6% of men report symptoms consistent with migraine1; less than half have been diagnosed by a physician or received prescription treatment from a physician.2 Migraine accounts for more than 2.8 million visits per year to US physicians and is the reason for encounter in about 1 visit per week to the typical family physician.3 Migraine is estimated to cost US employers more than $13 billion each year; direct medical costs exceed $1 billion annually.4
Pathophysiology
The exact pathophysiology of migraine is unknown. The prevailing theory is that a trigger (such as fatigue, stress, or certain foods) sets off a wave of brief neuronal activation, followed by a more sustained neuronal inhibition known as cortical spreading depression (CSD). At some point the trigeminovascular system is activated (possibly by CSD), releasing vasoactive neuropeptides that cause a painful inflammatory response in the meninges. Stimulation of presynaptic serotonin receptors inhibits release of the inflammatory neuropeptides; this is one possible explanation for the effectiveness of the triptans.5
Diagnosis
Migraine is a syndrome diagnosed by a certain combination of signs and symptoms. The International Headache Society (IHS) diagnostic criteria (Table 1) are widely accepted as the reference standard for the diagnosis of migraine, as well as that of other types of headache.6 Although they were originally intended to assist in the standardization of research subjects, the criteria for the most common headache disorders can be adapted for diagnosis in the clinical setting. Migraine diagnosis is based almost entirely on the history; the main role of the physical examination is to screen for life-threatening conditions, such as intracranial hemorrhage or tumors.
In some patients, migraine is difficult to distinguish from other primary or secondary headaches, especially tension-type headache. A recent meta-analysis demonstrated that the features most helpful to rule in migraine (compared with tension-type headache) are nausea (positive likelihood ratio [LR+] = 19.2), photophobia (LR+ = 5.8), and phonophobia (LR+ = 5.2). Table 2 provides additional information regarding these and other significant findings, including the post-test probabilities of migraine given the reported prevalence among adult men and women in the United States. The likelihood ratios are probably somewhat inflated, since many of these symptoms are also part of the criteria for the reference standard (“incorporation bias”). The IHS criteria for migraine without aura require nausea or the combination of photophobia and phonophobia to make the diagnosis; it is therefore not surprising that these findings would be the most specific.
While the presence of any single feature may not be sufficient to clinch the diagnosis, sequentially combining the post-test probabilities can prove useful in cases that are not straightforward. For example, a woman with a family history of migraine who complains of a unilateral headache accompanied by photophobia but no nausea has an approximately 80% post-test probability of migraine. This conclusion assumes statistical independence of these symptoms and thus may overestimate the probability somewhat.8
Migraine has no specific diagnostic findings on computed tomography (CT) or magnetic resonance imaging (MRI). The best evidence addressing the use of neuroimaging studies in migraine, as well as most other diagnostic and management issues, comes from the United States Headache Consortium (USHC), a panel of experts from several specialty societies and professional organizations, including the American Academy of Family Physicians. In April 2000, the USHC issued diagnosis and treatment guidelines based on rigorous evidence-based reviews of the medical literature.9 A USHC meta-analysis showed that the prevalence of significant abnormalities on head CT or MRI for migraine patients with a normal neurologic examination ranged from 0% to 3.1% with an overall prevalence of 0.18% (1 in 555).10 Therefore, the USHC does not recommend neuroimaging for patients with a normal neurologic examination who meet the IHS diagnostic criteria for migraine (level of evidence [LOE]: B, using the Centre for Evidence-Based Medicine classification scheme). Neuroimaging should be considered for patients for whom a diagnosis is less clear cut (LOE: C).
Further support for this recommendation is found in a well-designed retrospective study demonstrating that the rate of significant intracranial pathology (mass lesion or hemorrhage) in patients presenting to primary care practices with a new headache and no neurologic findings was only 0.35%.11 Some patients and physicians will find even this low risk unacceptable and will obtain neuroimaging studies for reasons (such as litigation fears, risk perception, and so forth) that likely are not amenable to statistical argument.
TABLE 1
DIAGNOSTIC CRITERIA FOR MIGRAINE
Migraine Without Aura
|
Migraine With Aura
|
| In both cases, the diagnosis of migraine cannot be made if the history or physical examination suggests another disorder unless that disorder has been ruled out by appropriate testing or the migraine attacks do not occur for the first time in close temporal relation to the disorder. |
| Adapted, with permission, from Headache Classification Committee of the International Headache Society. Diagnostic Criteria. Available at: http://www.i-h-s.org/ihsnew/guidelines/pdfs/diagnost.pdf. Accessed May 28, 2001. |
TABLE 2
DIAGNOSTIC FEATURES IN MIGRAINE
| Finding | Sensitivity (%) | Specificity (%) | LR+ | LR- | PV+% (M/F) | PV-% (M/F) |
|---|---|---|---|---|---|---|
| Versus Patients With Tension-Type Headache | ||||||
| Nausea | 81 | 96 | 19.2 | 0.20 | 56/82 | 1.2/4.2 |
| Photophobia | 79 | 86 | 5.8 | 0.25 | 26/55 | 1.5/5.1 |
| Phonophobia | 67 | 87 | 5.2 | 0.38 | 25/53 | 2.4/7.7 |
| Exacerbation by physical activity | 81 | 78 | 3.7 | 0.24 | 19/45 | 1.5/5.1 |
| Unilateral location | 65 | 82 | 3.7 | 0.43 | 19/44 | 2.7/8.6 |
| Throbbing or pulsating quality | 73 | 75 | 2.9 | 0.36 | 16/39 | 2.2/7.3 |
| Precipitated by chocolate | 33 | 95 | 7.1 | 0.70 | 30/59 | 4.3/13 |
| Versus Patients Without History of Headache | ||||||
| Family history of migraine | 58 | 88 | 5.0 | 0.47 | 24/51 | 3.0/10 |
| LR+ denotes positive likelihood ratio; LR-, negative likelihood ratio; PV+, probability of migraine given a positive finding; PV-, probability of migraine given a negative finding. | ||||||
| Prevalence of migraine in the US population is 6% for men (M) and 18% for women (F).1 | ||||||
| Adapted, with permission, from Smetana GW. The diagnostic value of historical features in primary headache syndromes: a comprehensive review. Arch Intern Med 2000; 160:2729-37. ©2000 American Medical Association. | ||||||
Treatment
General principles
Although the diagnostic criteria for migraine are relatively straightforward, the expression of these symptoms can be highly variable, both between patients and in any given patient between attacks. In addition, patients with migraine often experience intercurrent tension or other primary headaches, complicating both the diagnosis and the interpretation of response to a therapeutic trial. Consequently, finding the right medication for an individual is often challenging. The choice of treatment may be suggested or limited by coexisting conditions. The presence of severe nausea or vomiting during a migraine may require use of a medication that can be dosed other than by mouth.
Patient education and involvement in the development and evaluation of a migraine treatment plan is essential. Just as migraine sufferers differ in the type, frequency, and severity of their symptoms, they also differ in their treatment preferences and goals. Some are unable to tolerate certain side effects; others are more interested in rapid relief of pain. Discussions regarding expected responses to treatment can prevent patients’ disappointment and losing patients to follow-up. For example, a reduction in the frequency of headaches over the course of several months is a more realistic goal than immediate prevention of all headaches. A patient’s headache diary can aid the patient in identifying and possibly eliminating migraine triggers and greatly assist the physician in adjusting and refining a treatment plan.
Various treatments, both pharmacologic and nonpharmacologic, have been used to treat patients with migraine. This article examines treatments in 3 categories: abortive medications, prophylactic medications, and nonpharmacologic treatments.
Abortive medications
Table 3 lists over-the-counter (OTC) and prescription medications for acute migraine attacks. Until recently, little if any high-quality evidence existed to guide the physician in selecting the appropriate medication for a specific patient. The USHC issued a consensus recommendation that nonsteroidal antiinflammatory drugs (NSAIDs) and over-the-counter analgesics be considered first-line treatments, especially for mild migraine headaches, and that migraine-specific agents be used for patients with more severe episodes.12
Further support for this stratified-care approach to migraine treatment has since been provided by the Disability in Strategies of Care (DISC) Study. DISC demonstrated that patients whose treatment was chosen according to their Migraine Disability Assessment Scale (MIDAS) score (those with a score of I or II were treated with aspirin and metoclopramide; those with a score of III or IV were treated with zolmitriptan) had less disability and a significantly greater headache response at 2 hours than patients who were given zolmitriptan if their headaches failed to respond to aspirin and metoclopramide.13 The study supports the expert consensus that patients with a history of mild disability associated with migraine can be treated effectively with simple OTC analgesics, whereas patients with significant migraine-associated disability will have better outcomes if treated with migraine-specific medications (LOE: B).
Mild to moderate migraine can be treated effectively with an oral combination of aspirin, acetaminophen, and caffeine (Excedrin or generic substitutes) or aspirin plus metoclopramide (LOE: A). Patients who cannot take aspirin may respond to 1000 mg acetaminophen alone (LOE: B).
Triptans (5-hydroxytryptamine1B/1D receptor agonists) are the drugs of choice for the acute treatment of moderate to severe migraine (except hemiplegic or basilar migraine) (LOE: A). Contraindications include coronary artery disease, uncontrolled hypertension, pregnancy, and recent monoamine oxidase inhibitor or ergot alkaloid use. Little evidence exists to recommend one triptan over another. A few studies suggest that the newer oral triptans may be slightly more efficacious than oral sumatriptan, although the differences do not appear overwhelming.14-16
There have been no recent studies on isometheptene-containing compounds such as Midrin. Three randomized placebo-controlled trials in the mid-1970s found a modest but statistically significant effect on migraine pain.17-19 However, the lack of standardized inclusion criteria and outcome measures makes it difficult to draw firm, valid conclusions about the efficacy of isometheptene.20 These drugs should be considered second line in the acute treatment of migraine (LOE: B).
A number of randomized controlled studies have demonstrated the efficacy of acetaminophen–codeine combinations in the acute treatment of migraine.21-23 Some of these trials have used combinations that included other medications in addition to acetaminophen and codeine; no study has been done on the dose most readily available in the United States (ie, 300 mg acetaminophen plus 30 mg codeine). Concerns about abuse, tolerance, and rebound headache appropriately limit their use. In addition, there is no evidence that they are more effective than other abortive treatments; one study showed no difference between the acute migraine relief provided by 1000 mg plain aspirin versus 400 mg acetaminophen and 25 mg codeine.21 While acetaminophen plus codeine combinations probably are effective in migraine, they are second-line drugs (LOE: B).
No randomized, placebo-controlled trials have evaluated the efficacy of butalbital-containing agents for migraine. Because of concerns relating to dependence, withdrawal, and rebound headache, the USHC recommends that use of these agents “should be limited and carefully monitored” (LOE: D).12
In the emergency department setting, prochlorperazine (10 mg given intravenously [IV]) is a safe and effective treatment for migraine (LOE: A).24 Dihydroergotamine (DHE) given IV or intramuscularly (IM) in combination with antiemetics is at least as good as meperidine (IV or IM) in relieving the pain of migraine (LOE: A).25,26 Despite the widespread use of parenteral meperidine in this setting, there are no placebo-controlled studies documenting its effectiveness in the treatment of migraine headache.
TABLE 3
SELF-ADMINISTERED ACUTE TREATMENT OPTIONS IN MIGRAINE
| Strength of Recommendation | Treatment (Route of Administration) | Comments |
|---|---|---|
| A | Acetaminophen +aspirin + caffeine (PO) | NNT* 3.9 (3.2 to 4.9)51 |
| A | Aspirin (PO) | NNT range from 3.5 to 5.552 |
| A | Aspirin + metoclopramide (PO) | NNT 3.2 (2.6 to 4.0)53 |
| A | Butorphanol (IN) | Abuse/dependence and rebound headache potential |
| A | DHE (IN) | NNT 2.5 (1.9 to 3.7)54 |
| A | NSAIDs (PO) | NNT 7.5 (4.5 to 22) (for ibuprofen)55 |
| A | Triptans (PO) | NNT range from 2.7 to 5.456 |
| A | Sumatriptan (IN) | NNT 3.4 (2.9 to 4.1)56 |
| A | Sumatriptan (SC) | NNT 2.0 (1.8 to 2.2)56 |
| B | Acetaminophen (PO) | NNT 5.2 (3.3 to 13)57 |
| B | Acetaminophen + codeine (PO) | Abuse/dependence and rebound headache potential |
| B | Isometheptene compounds (PO) | Limited clinical trial data. |
| D | Butalbital compounds (PO) | No clinical trials; risk of rebound headache |
| D | Ergotamine (PO) | Conflicting evidence; increased risk of adverse effects |
| * Numbers needed to treat (NNT; 95% confidence interval) in this column are for headache response (reduction in headache severity from “severe” or “moderate” to “mild” or “none”) at 2 hours; included when available data permit. | ||
| IN denotes intranasal; PO, by mouth; SC, subcutaneous. | ||
Prophylactic medications
The USHC recommends that preventive treatment be considered for patients with migraine who desire a reduction in the frequency or severity of their headaches for any reason, including but not limited to frequent headaches that significantly interfere with daily activities despite acute treatment, unpleasant side effects associated with abortive medications, or the cost of abortive medications (LOE: D).27Table 4 lists medications available in the United States that are used in the prophylaxis of migraine.
Beta blockers, particularly propranolol, are commonly prescribed and are very effective in reducing the frequency of migraine (LOE: A).27-30 Most authorities consider them the migraine prophylactic of choice in patients with no contraindications (eg, asthma, congestive heart failure, or heart block).
Amitriptyline is the only antidepressant to demonstrate consistent efficacy in migraine prophylaxis.27,31,32 This medication may be especially useful in patients who suffer from both migraine and tension headaches.33 Divalproex sodium is another drug clearly shown effective against migraine prophylactically.27,30,34 The risk of significant hematologic and hepatic side effects requires laboratory monitoring and may limit its use in many patients.
Calcium channel blockers (CCBs), particularly verapamil, are widely used by both primary care physicians and neurologists for the prevention of migraine,35 and yet only 3 controlled trials of verapamil are reported in the English language literature. Two methodologically weak studies showed a small but significant effect from verapamil36,37; the third demonstrated no advantage over placebo.38 The only CCB consistently shown effective for migraine prophylaxis is flunarizine.27 Unfortunately, it is not available in the United States.
Besides use for acute treatment, NSAIDs are occasionally prescribed to prevent migraine. Naproxen sodium, the most frequently studied NSAID, shows a small but significant effect in overall improvement compared with placebo in several trials.39-41 Two of these studies showed a reduction in the number of severe headaches per week but no significant change in the total number of headaches per week.40,41
Some recent studies support the use of novel migraine prophylactics. One study of riboflavin (400 mg daily) showed a moderate reduction in migraine frequency.42 Achieving maximal therapeutic effect required 3 months of use. Another study found that 10 mg lisinopril daily can significantly reduce migraine frequency and severity when compared with placebo.43
TABLE 4
PROPHYLACTIC TREATMENT OPTIONS IN MIGRAINE
| Strength of Recommendation | Treatment | Comments |
|---|---|---|
| A | Amitriptyline | Evidence for no significant difference versus propranolol32, 33 |
| A | Divalproex sodium | NNT* range from 2.1 to 2.930, 34 |
| A | Propranolol | NNT range from 2.3 to 528-30 |
| B | Lisinopril | Based on 1 study (level 1b)43 |
| B | Naproxen sodium | Risk of rebound headache |
| B | Riboflavin | NNT 2.842 based on 1 study (level 1b) |
| D | Verapamil | Considered effective by many experts; limited, poor-quality clinical trials (see text) |
| * Numbers needed to treat (NNT) in this column are for a 50% reduction in headache frequency compared with baseline; reported when available data permit. | ||
Nonpharmacologic treatments
Although the data for nonpharmacologic migraine treatment are neither so extensive nor so rigorous as those for medications, some evidence is available. The Duke Center for Clinical Health Policy Research performed a comprehensive systematic review and meta-analysis of behavioral and physical treatments for migraine for the Agency for Healthcare Research and Quality.44 This review forms the evidence base for the USHC guideline in this area.45 The authors note that most studies were conducted on patients recruited at specialized headache centers; thus, caution should be exercised in generalizing the results to a primary care population.
The meta-analysis showed that cognitive–behavioral (including stress management) therapy, electromyelogram biofeedback, relaxation training, and thermal biofeedback combined with relaxation training are effective in migraine prophylaxis (LOE: B).44 An earlier meta-analysis concluded that the prophylactic benefit of combined relaxation and thermal biofeedback training was equivalent to the benefit obtained from propranolol.46 Because of limited or mixed evidence, no clear recommendations can be made with regard to acupuncture, cervical manipulation, hyperbaric oxygen, hypnosis, occlusal adjustment, or transcutaneous electronic nerve stimulation.45
Prognosis
Little evidence is available concerning the long-term prognosis of migraine, either with or without treatment. For many patients, migraine persists, but slowly decreases in frequency over a lifetime.47,48 For patients who respond well to prophylaxis, no data are available to help the clinician decide how long to continue using it. One small case series showed that while a few patients had a lasting reduction in the frequency of their migraines after stopping effective prophylactic medication, most experienced relapse.49
A subset of patients with migraine develops headaches of increasing frequency, often resulting in daily or continuous headaches. This syndrome has been known as transformed or malignant migraine. Many such patients use migraine medications on a daily basis. Although no controlled trials have been reported, the daily or near-daily use of most acute migraine medications (including acetaminophen, aspirin, dihydroergotamine, ergotamine, NSAIDs, opioids, and triptans) is believed capable of provoking medication-overuse headaches.50 Some of these patients can reduce the frequency of their headaches if they can break the cycle of medication use.47
Conclusions
Migraine headache is a common and disabling condition. The diagnosis often can be made on the basis of key findings in the patient’s history. A classic history, in combination with a normal neurologic examination, obviates head imaging. Available evidence clearly shows that effective methods for both acute and prophylactic treatment of migraine exist. The Figure contains an algorithm summarizing such treatment. Wider implementation of the USHC evidence-based guidelines by primary care physicians treating those with migraine should result in decreased pain and increased productivity for many patients.
FIGURE
ALGORITHM FOR TREATMENT OF MIGRAINE
Acknowledgments
The author would like to thank John R. Holman, MD, MPH, for reviewing the manuscript and Anne J. O’Connor for her help in obtaining the references.
1. Stewart WF, Lipton RB, Celentano DD, Reed ML. Prevalence of migraine headache in the United States: relation to age, income, race and other sociodemographic factors. JAMA 1992;267:64-9.
2. Stewart WF, Lipton RB. Migraine headache: epidemiology and health care utilization. Cephalalgin 1993;13(suppl 12):41-6.
3. Schappert SM, Nelson C. National Ambulatory Medical Care Survey, 1995-1996 Summary. National Center for Health Statistics. Vital Health Stat 13(142). 1999.
4. Hu XH, Markson LE, Lipton RB, Stewart WF, Berger ML. Burden of migraine in the United States: disability and economic costs. Arch Intern Med 1999;159:813-8.
5. Goadsby PJ. Current concepts of the pathophysiology of migraine. Neurol Clin 1997;15:27-42.
6. Headache Classification Committee of the International Headache Society. Diagnostic criteria. Available at: www.i-h-s.org/ihsnew/guidelines/pdfs/diagnost.pdf/. Accessed May 28, 2001.
7. Smetana GW. The diagnostic value of historical features in primary headache syndromes: a comprehensive review. Arch Intern Med 2000;160:2729-37.
8. Diagnosing migraine. Available at: http://www.jr2.ox.ac.uk/bandolier/booth/Migraine/Diagmig.html/. Accessed November 6, 2001.
9. McCrory DC, Matchar DB, Rosenberg JH, Silberstein SD. Evidenced-based guidelines for migraine headache: overview of program description and methodology. Available at: www.aan.com/public/practiceguidelines/01.pdf/. Accessed November 29, 2001.
10. Frishberg BM, Rosenberg JH, Matchar DB, McCrory DC, Rozen TD, Silberstein SD. Evidence-based guidelines in the primary care setting: neuroimaging in patients with nonacute headache. Available at: www.aan.com/public/practiceguidelines/02.pdf/. Accessed November 29, 2001.
11. Becker LA, Green LA, Beaufait D, Kirk J, Froom J, Freeman WL. Detection of intracranial tumors, subarachnoid hemorrhages, and subdural hematomas in primary care patients: a report from ASPN, Part 2. J Fam Pract 1993;37:135-41.
12. Matchar DB, Young WB, Rosenberg JH, et al. Evidence-based guidelines for migraine headache in the primary care setting: pharmacological management of acute attacks. Available at: www.aan.com/public/practiceguidelines/03.pdf/. Accessed November 29, 2001.
13. Lipton RB, Stewart WF, Stone AM, Lainez MJA, Sawyer JPC. Stratified care vs step care strategies for migraine. The disability in strategies of care (DISC) study: a randomized trial. JAMA 2000;284:2599-605.
14. Tfelt-Hansen P, Teall J, Rodriguez F, et al. Oral rizatriptan versus oral sumatriptan: a direct comparative study in the acute treatment of migraine. Headache 1998;38:748-55.
15. Gallagher R, Dennish G, Spierings EL, Chitra R. A comparative trial of zolmitriptan and sumatriptan for the acute oral treatment of migraine. Headache 2000;40:119-28.
16. Gobel H, Winter P, Boswell D, Crisp A, Becker W, Hauge T, et al. Comparison of naratriptan and sumatriptan in recurrence-prone migraine patients. Clin Ther 2000;22:981-9.
17. Ryan RE. A study of Midrin in the symptomatic relief of migraine headache. Headache 1974;14:33-42.
18. Diamond S, Medina JL. Isometheptene-a non-ergot drug in the treatment of migraine. Headache 1975;15:211-3.
19. Diamond S. Treatment of migraine with isometheptene, acetaminophen, and dichloralphenazone combination: a double-blind, crossover trial. Headache 1976;15:282-7.
20. Isometheptene for acute migraine. Available at: http://www.jr2.ox.ac.uk/bandolier/booth/Migraine/IsomORacu.html/. Accessed November 9, 2001.
21. Boureau F, Joubert JM, Lasserre V, Prum B, Delecoeuillerie G. Double-blind comparison of an acetaminophen 400 mg-codeine 25 mg combination versus aspirin 1000 mg and placebo in acute migraine attack. Cephalalgia 1994;14:156-61.
22. Adam EI. A treatment for the acute migraine attack. J Int Med Res 1987;15:71-5.
23. Carasso RL, Yehuda S. The prevention and treatment of migraine with an analgesic combination. Br J Clin Pract 1984;38:25-7.
24. Coppola M, Yealy DM, Leibold RA. Randomized, placebo-controlled evaluation of prochlorperazine versus metoclopramide for emergency department treatment of migraine headache. Ann Emerg Med 1995;26:541-6.
25. Klapper JA, Stanton J. Current emergency treatment of severe migraine headaches. Headache 1993;33:560-2.
26. Carleton SC, Shesser RF, Pietrzak MP, et al. Double-blind, multicenter trial to compare the efficacy of intramuscular dihydroergotamine plus hydroxyzine versus intramuscular meperidine plus hydroxyzine for the emergency department treatment of acute migraine headache. Ann Emerg Med 1998;32:129-38.
27. Ramadan NM, Silberstein SD, Freitag FG, Gilbert TT, Frishberg BM. Evidence-based guidelines for migraine headache in the primary care setting: pharmacological management for the prevention of migraine. Available at: www.aan.com/public/practiceguidelines/05.pdf/. Accessed November 29, 2001.
28. Borgesen SE, Nielsen JL, Moller CE. Prophylactic treatment of migraine with propranolol: a clinical trial. Acta Neurol Scand 1974;50:651-6.
29. Tfelt-Hansen P, Standnes B, Kangasniemi P, Hakkarainen H, Olesen J. Timolol vs. propranolol vs. placebo in common migraine prophylaxis: a double-blind multicenter trial. Acta Neurol Scand 1984;69:1-8.
30. Kaniecki RG. A comparison of divalproex with propranolol and placebo for the prophylaxis of migraine without aura. Arch Neurol 1997;54:1141-5.
31. Couch JR, Hassanein RS. Amitriptyline in migraine prophylaxis. Arch Neurol 1979;36:695-9.
32. Ziegler DK, Hurwitz A, Hassanein RS, Kodanaz HA, Preskorn SH, Mason J. Migraine prophylaxis: a comparison of propranolol and amitriptyline. Arch Neurol 1987;44:486-9.
33. Mathew NT. Prophylaxis of migraine and mixed headache. A randomized controlled study. Headache 1981;21:105-9.
34. Mathew NT, Saper JR, Silberstein SD, et al. Migraine prophylaxis with divalproex. Arch Neurol 1995;52:281-6.
35. Ramadan NM, Schultz LL, Gilkey SJ. Migraine prophylactic drugs: proof of efficacy, utilization and cost. Cephalalgia 1997;17:73-80.
36. Solomon GD, Steel JG, Spaccavento LJ. Verapamil prophylaxis of migraine: a double-blind, placebo-controlled study. JAMA 1983;250:2500-2.
37. Markley HG, Cheronis JC, Piepho RW. Verapamil in prophylactic therapy of migraine. Neurology 1984;34:973-6.
38. Solomon GD. Verapamil and propranolol in migraine prophylaxis; a double-blind, cross-over study. Headache 1986;26:325.-
39. Ziegler DK, Ellis DJ. Naproxen in prophylaxis of migraine. Arch Neurol 1985;42:582-4.
40. Sargent J, Solbach P, Damasio H, et al. A comparison of naproxen sodium to propranolol hydrochloride and a placebo control for the prophylaxis of migraine headache. Headache 1985;25:320-4.
41. Welch KMA, Ellis DJ, Keenan PA. Successful migraine prophylaxis with naproxen sodium. Neurology 1985;35:1304-10.
42. Schoenen J, Jacquy J, Lenaerts M. Effectiveness of high-dose riboflavin in migraine prophylaxis: a randomized controlled trial. Neurology 1998;50:466-70.
43. Schrader H, Stoner LJ, Helde G, Sand T, Bovim G. Prophylactic treatment of migraine with angiotensin converting enzyme inhibitor (lisinopril): randomised, placebo controlled, crossover study. BMJ 2001;322:1-5.
44. Goslin RE, Gray RN, McCrory DC, Penzien D, Rains J, Hasselblad V. Behavioral and physical treatments for migraine headache. Technical review 2.2. February 1999. Prepared for the Agency for Health Care Policy and Research under Contract No. 290-94-2025. Available at: http://www.clinpol.mc.duke.edu./Pubs/Publications/Behavioral_Manuscript.pdf/. Accessed November 27, 2001.
45. Campbell JK, Penzien DB, Wall EM. Evidence-based guidelines for migraine headache: behavioral and physical treatments. Available at: www.aan.com/public/practiceguidelines/04.pdf/. Accessed November 29, 2001.
46. Holroyd KA, Penzien DB. Pharmacological versus non-pharmacological prophylaxis of recurrent migraine headache: a meta-analytic review of clinical trials. Pain 1990;42:1-13.
47. Silberstein SD, Lipton RB. Headache epidemiology. Emphasis on migraine. Neurol Clin 1996;14:421-34.
48. Silberstein SD, Young WB. Headache and facial pain. In: Goetz CG, Pappert EJ, eds. Textbook of clinical neurology. 1st ed. Philadelphia, Pa: Saunders; 1999:1095.
49. Wober C, Wober-Bingol C, Kock G, Wessely P. Long-term results of migraine prophylaxis with flunarazine and beta-blockers. Cephalalgia. 1991;11:251-6.
50. Diener HC, Dahlof CGH. Headache associated with chronic use of substances. In: Olesen J, Tfelt-Hansen P, Welch KMA, eds. The headaches. 2nd ed. Philadelphia, Pa: Lippincott, Williams & Wilkins; 2000:871-7.
51. Paracetamol, aspirin caffeine incombination (Excedrin) for acute migraine. Available at: http://www.jr2.ox.ac.uk/bandolier/booth/Migraine/Excedr.html/. Accessed November 9, 2001.
52. Aspirin for acute migraine. Available at: http://www.jr2.ox.ac.uk/bandolier/booth/Migraine/Aspacute.html/. Accessed November 9, 2001.
53. Aspirin plus metoclopramide for acute migraine. Available at: http://www.jr2.ox.ac.uk/bandolier/booth/Migraine/AsMcOacu.html/. Accessed November 9, 2001.
54. Intranasal dihydroergotamine for acute migraine Available at: http://www.jr2.ox.ac.uk/bandolier/booth/Migraine/DHEINacu.html/. Accessed November 9, 2001.
55. Ibuprofen for acute migraine (new RCT). Available at: http://www.jr2.ox.ac.uk/bandolier/booth/Migraine/ibu2.html/. Accessed November 9, 2001.
56. Migraine league table: acute treatments and two hour headache response. Available at: http://www.jr2.ox.ac.uk/bandolier/booth/Migraine/League.html/. Accessed November 9, 2001.
57. Lipton RB, Baggish JS, Stewart WF, Codispoti JR, Fu M. Efficacy and safety of acetaminophen in the treatment of migraine: results of a randomized, double-blind, placebo-controlled, population-based study. Arch Intern Med 2000;160:3486-92
1. Stewart WF, Lipton RB, Celentano DD, Reed ML. Prevalence of migraine headache in the United States: relation to age, income, race and other sociodemographic factors. JAMA 1992;267:64-9.
2. Stewart WF, Lipton RB. Migraine headache: epidemiology and health care utilization. Cephalalgin 1993;13(suppl 12):41-6.
3. Schappert SM, Nelson C. National Ambulatory Medical Care Survey, 1995-1996 Summary. National Center for Health Statistics. Vital Health Stat 13(142). 1999.
4. Hu XH, Markson LE, Lipton RB, Stewart WF, Berger ML. Burden of migraine in the United States: disability and economic costs. Arch Intern Med 1999;159:813-8.
5. Goadsby PJ. Current concepts of the pathophysiology of migraine. Neurol Clin 1997;15:27-42.
6. Headache Classification Committee of the International Headache Society. Diagnostic criteria. Available at: www.i-h-s.org/ihsnew/guidelines/pdfs/diagnost.pdf/. Accessed May 28, 2001.
7. Smetana GW. The diagnostic value of historical features in primary headache syndromes: a comprehensive review. Arch Intern Med 2000;160:2729-37.
8. Diagnosing migraine. Available at: http://www.jr2.ox.ac.uk/bandolier/booth/Migraine/Diagmig.html/. Accessed November 6, 2001.
9. McCrory DC, Matchar DB, Rosenberg JH, Silberstein SD. Evidenced-based guidelines for migraine headache: overview of program description and methodology. Available at: www.aan.com/public/practiceguidelines/01.pdf/. Accessed November 29, 2001.
10. Frishberg BM, Rosenberg JH, Matchar DB, McCrory DC, Rozen TD, Silberstein SD. Evidence-based guidelines in the primary care setting: neuroimaging in patients with nonacute headache. Available at: www.aan.com/public/practiceguidelines/02.pdf/. Accessed November 29, 2001.
11. Becker LA, Green LA, Beaufait D, Kirk J, Froom J, Freeman WL. Detection of intracranial tumors, subarachnoid hemorrhages, and subdural hematomas in primary care patients: a report from ASPN, Part 2. J Fam Pract 1993;37:135-41.
12. Matchar DB, Young WB, Rosenberg JH, et al. Evidence-based guidelines for migraine headache in the primary care setting: pharmacological management of acute attacks. Available at: www.aan.com/public/practiceguidelines/03.pdf/. Accessed November 29, 2001.
13. Lipton RB, Stewart WF, Stone AM, Lainez MJA, Sawyer JPC. Stratified care vs step care strategies for migraine. The disability in strategies of care (DISC) study: a randomized trial. JAMA 2000;284:2599-605.
14. Tfelt-Hansen P, Teall J, Rodriguez F, et al. Oral rizatriptan versus oral sumatriptan: a direct comparative study in the acute treatment of migraine. Headache 1998;38:748-55.
15. Gallagher R, Dennish G, Spierings EL, Chitra R. A comparative trial of zolmitriptan and sumatriptan for the acute oral treatment of migraine. Headache 2000;40:119-28.
16. Gobel H, Winter P, Boswell D, Crisp A, Becker W, Hauge T, et al. Comparison of naratriptan and sumatriptan in recurrence-prone migraine patients. Clin Ther 2000;22:981-9.
17. Ryan RE. A study of Midrin in the symptomatic relief of migraine headache. Headache 1974;14:33-42.
18. Diamond S, Medina JL. Isometheptene-a non-ergot drug in the treatment of migraine. Headache 1975;15:211-3.
19. Diamond S. Treatment of migraine with isometheptene, acetaminophen, and dichloralphenazone combination: a double-blind, crossover trial. Headache 1976;15:282-7.
20. Isometheptene for acute migraine. Available at: http://www.jr2.ox.ac.uk/bandolier/booth/Migraine/IsomORacu.html/. Accessed November 9, 2001.
21. Boureau F, Joubert JM, Lasserre V, Prum B, Delecoeuillerie G. Double-blind comparison of an acetaminophen 400 mg-codeine 25 mg combination versus aspirin 1000 mg and placebo in acute migraine attack. Cephalalgia 1994;14:156-61.
22. Adam EI. A treatment for the acute migraine attack. J Int Med Res 1987;15:71-5.
23. Carasso RL, Yehuda S. The prevention and treatment of migraine with an analgesic combination. Br J Clin Pract 1984;38:25-7.
24. Coppola M, Yealy DM, Leibold RA. Randomized, placebo-controlled evaluation of prochlorperazine versus metoclopramide for emergency department treatment of migraine headache. Ann Emerg Med 1995;26:541-6.
25. Klapper JA, Stanton J. Current emergency treatment of severe migraine headaches. Headache 1993;33:560-2.
26. Carleton SC, Shesser RF, Pietrzak MP, et al. Double-blind, multicenter trial to compare the efficacy of intramuscular dihydroergotamine plus hydroxyzine versus intramuscular meperidine plus hydroxyzine for the emergency department treatment of acute migraine headache. Ann Emerg Med 1998;32:129-38.
27. Ramadan NM, Silberstein SD, Freitag FG, Gilbert TT, Frishberg BM. Evidence-based guidelines for migraine headache in the primary care setting: pharmacological management for the prevention of migraine. Available at: www.aan.com/public/practiceguidelines/05.pdf/. Accessed November 29, 2001.
28. Borgesen SE, Nielsen JL, Moller CE. Prophylactic treatment of migraine with propranolol: a clinical trial. Acta Neurol Scand 1974;50:651-6.
29. Tfelt-Hansen P, Standnes B, Kangasniemi P, Hakkarainen H, Olesen J. Timolol vs. propranolol vs. placebo in common migraine prophylaxis: a double-blind multicenter trial. Acta Neurol Scand 1984;69:1-8.
30. Kaniecki RG. A comparison of divalproex with propranolol and placebo for the prophylaxis of migraine without aura. Arch Neurol 1997;54:1141-5.
31. Couch JR, Hassanein RS. Amitriptyline in migraine prophylaxis. Arch Neurol 1979;36:695-9.
32. Ziegler DK, Hurwitz A, Hassanein RS, Kodanaz HA, Preskorn SH, Mason J. Migraine prophylaxis: a comparison of propranolol and amitriptyline. Arch Neurol 1987;44:486-9.
33. Mathew NT. Prophylaxis of migraine and mixed headache. A randomized controlled study. Headache 1981;21:105-9.
34. Mathew NT, Saper JR, Silberstein SD, et al. Migraine prophylaxis with divalproex. Arch Neurol 1995;52:281-6.
35. Ramadan NM, Schultz LL, Gilkey SJ. Migraine prophylactic drugs: proof of efficacy, utilization and cost. Cephalalgia 1997;17:73-80.
36. Solomon GD, Steel JG, Spaccavento LJ. Verapamil prophylaxis of migraine: a double-blind, placebo-controlled study. JAMA 1983;250:2500-2.
37. Markley HG, Cheronis JC, Piepho RW. Verapamil in prophylactic therapy of migraine. Neurology 1984;34:973-6.
38. Solomon GD. Verapamil and propranolol in migraine prophylaxis; a double-blind, cross-over study. Headache 1986;26:325.-
39. Ziegler DK, Ellis DJ. Naproxen in prophylaxis of migraine. Arch Neurol 1985;42:582-4.
40. Sargent J, Solbach P, Damasio H, et al. A comparison of naproxen sodium to propranolol hydrochloride and a placebo control for the prophylaxis of migraine headache. Headache 1985;25:320-4.
41. Welch KMA, Ellis DJ, Keenan PA. Successful migraine prophylaxis with naproxen sodium. Neurology 1985;35:1304-10.
42. Schoenen J, Jacquy J, Lenaerts M. Effectiveness of high-dose riboflavin in migraine prophylaxis: a randomized controlled trial. Neurology 1998;50:466-70.
43. Schrader H, Stoner LJ, Helde G, Sand T, Bovim G. Prophylactic treatment of migraine with angiotensin converting enzyme inhibitor (lisinopril): randomised, placebo controlled, crossover study. BMJ 2001;322:1-5.
44. Goslin RE, Gray RN, McCrory DC, Penzien D, Rains J, Hasselblad V. Behavioral and physical treatments for migraine headache. Technical review 2.2. February 1999. Prepared for the Agency for Health Care Policy and Research under Contract No. 290-94-2025. Available at: http://www.clinpol.mc.duke.edu./Pubs/Publications/Behavioral_Manuscript.pdf/. Accessed November 27, 2001.
45. Campbell JK, Penzien DB, Wall EM. Evidence-based guidelines for migraine headache: behavioral and physical treatments. Available at: www.aan.com/public/practiceguidelines/04.pdf/. Accessed November 29, 2001.
46. Holroyd KA, Penzien DB. Pharmacological versus non-pharmacological prophylaxis of recurrent migraine headache: a meta-analytic review of clinical trials. Pain 1990;42:1-13.
47. Silberstein SD, Lipton RB. Headache epidemiology. Emphasis on migraine. Neurol Clin 1996;14:421-34.
48. Silberstein SD, Young WB. Headache and facial pain. In: Goetz CG, Pappert EJ, eds. Textbook of clinical neurology. 1st ed. Philadelphia, Pa: Saunders; 1999:1095.
49. Wober C, Wober-Bingol C, Kock G, Wessely P. Long-term results of migraine prophylaxis with flunarazine and beta-blockers. Cephalalgia. 1991;11:251-6.
50. Diener HC, Dahlof CGH. Headache associated with chronic use of substances. In: Olesen J, Tfelt-Hansen P, Welch KMA, eds. The headaches. 2nd ed. Philadelphia, Pa: Lippincott, Williams & Wilkins; 2000:871-7.
51. Paracetamol, aspirin caffeine incombination (Excedrin) for acute migraine. Available at: http://www.jr2.ox.ac.uk/bandolier/booth/Migraine/Excedr.html/. Accessed November 9, 2001.
52. Aspirin for acute migraine. Available at: http://www.jr2.ox.ac.uk/bandolier/booth/Migraine/Aspacute.html/. Accessed November 9, 2001.
53. Aspirin plus metoclopramide for acute migraine. Available at: http://www.jr2.ox.ac.uk/bandolier/booth/Migraine/AsMcOacu.html/. Accessed November 9, 2001.
54. Intranasal dihydroergotamine for acute migraine Available at: http://www.jr2.ox.ac.uk/bandolier/booth/Migraine/DHEINacu.html/. Accessed November 9, 2001.
55. Ibuprofen for acute migraine (new RCT). Available at: http://www.jr2.ox.ac.uk/bandolier/booth/Migraine/ibu2.html/. Accessed November 9, 2001.
56. Migraine league table: acute treatments and two hour headache response. Available at: http://www.jr2.ox.ac.uk/bandolier/booth/Migraine/League.html/. Accessed November 9, 2001.
57. Lipton RB, Baggish JS, Stewart WF, Codispoti JR, Fu M. Efficacy and safety of acetaminophen in the treatment of migraine: results of a randomized, double-blind, placebo-controlled, population-based study. Arch Intern Med 2000;160:3486-92