User login
Update on pelvic surgery
The authors report no financial relationships relevant to this article.
Over the past 10 years, the midurethral sling has replaced the Burch urethropexy as the most common surgical procedure for correcting stress urinary incontinence (SUI). In this “Update” on midurethral slings, we highlight three recently published studies that compare popular surgical approaches to SUI:
- the original tension-free vaginal tape (TVT) technique (FIGURE [“A”])
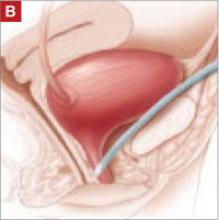
- the suprapubic urethral support sling (SPARC) (FIGURE [“B”])
- the transobturator tape (TOT) technique (FIGURE [“C”])
- the traditional pubovaginal sling (PVS), placed at the bladder neck (FIGURE [“D”]).
FIGURE [“A”] Four options for a midurethral sling to correct stress urinary incontinence: Tension-free vaginal tape (TVT) technique
FIGURE [“B”] Four options for a midurethral sling to correct stress urinary incontinence: Suprapubic urethral support sling (SPARC)
FIGURE [“C”] Four options for a midurethral sling to correct stress urinary incontinence: Transobturator tape (TOT) technique
FIGURE [“D”] Four options for a midurethral sling to correct stress urinary incontinence: Pubovaginal sling (PVS)
We’ve had a decade-plus of experience with the sling
The midurethral sling, first introduced as the tension-free vaginal tape, or TVT (Gynecare), was quick to be adopted because:
- it offers a minimally invasive approach
- it is highly efficacious
- serious adverse events are rare.
TVT utilizes a 5-mm trocar that is passed from the vagina through the retropubic space, exiting via small suprapubic incisions. A strip of permanent polypropylene mesh attached to these trocars is placed under the midportion of the urethra (FIGURE [“A”]).
We now have 11 years of follow-up data to support the use of the TVT midurethral sling for SUI.1
As TVT gained popularity, surgical equipment manufacturers developed various “kits,” so to speak, for placing a midurethral sling. Many have included innovations that have theoretical advantages over traditional TVT. Some place smaller, 3-mm trocars in a similar “bottom-up” fashion, as the TVT sling does; others utilize smaller trocars that are placed “top down” through the retropubic space into the vagina.
A later generation of slings uses the transobturator approach, to avoid blind passage of trocars through the retropubic space. These slings can be placed “in to out” or “out to in,” and rest in a slightly different orientation under the midurethra.
In an effort to make the procedure even more minimally invasive, some manufacturers now offer slings that are placed through one vaginal incision, thereby avoiding additional suprapubic or groin incisions. Other kits have made alterations to the polypropylene mesh by heat-sealing the material or applying a coating.
Such modifications haven’t always been improvements—some sling kits carried a higher incidence of mesh-related complications, and certain ones were removed from the market. And, although the number of commercially available midurethral sling kits has exploded, we’ve seen scant data published that compare the traditional TVT method with alternative approaches. Those alternatives may be considered midurethral slings, but we haven’t known whether minor variations in technique, or in the instrumentation, translate to improvements in long-term efficacy.
More readjustments for retention are needed after SPARC (vs. TVT)
Lord HE, Taylor JD, Finn JC, et al. A randomized controlled equivalence trial of short-term complications and efficacy of tension-free vaginal tape and suprapubic urethral support sling for treating stress incontinence. BJU Int. 2006;98:367–376.
This randomized, controlled trial compared TVT with SPARC to treat SUI. The study was designed as an equivalence trial: the investigators sought to determine if the “newer” intervention of the two (SPARC) is therapeutically equivalent to the existing intervention (TVT)—not whether one is superior. They therefore looked to see if patients who underwent TVT and those who underwent SPARC had the same rate (within a 5% margin) of bladder injury and other secondary outcomes.
Subjects were eligible to participate if they had SUI on the basis of urodynamic or clinical parameters. They were unaware of their assigned treatment, underwent TVT or SPARC, and were reevaluated 6 weeks postoperatively. Intraoperative, postoperative, and 6-week follow-up data were recorded by the study surgeon.
Three hundred and one patients were enrolled; 147 underwent TVT and 154 underwent SPARC. The groups were similar in regard to all baseline characteristics.
No significant difference was noted between the groups in the primary outcome, which was the rate of bladder perforation (TVT, 0.7%; SPARC, 1.9% [p=.62]). This effect remained after controlling for age, parity, prior urinary incontinence surgery, other concomitant surgery, and the surgeon’s level of experience. There were no intergroup differences in perioperative blood loss, urgency, or objective cure of SUI (defined as negative cough stress test) 6 weeks after surgery.
Subjects who underwent SPARC were more likely to experience urinary retention that required surgical readjustment of the sling (SPARC, 10 of 154; TVT, none [p=.002]). Although the objective cure rate was similar across groups, the subjective cure rate was significantly different (TVT, 87.1%; SPARC, 76.5% [p=.03]).
Regression analysis revealed that subjects who had prior surgery for urinary incontinence and those whose surgery was performed by a comparatively less experienced physician were more likely to report persistence of SUI symptoms.
This study reflects general clinical practice, in that it was conducted across a heterogeneous sample of subjects who had both primary and recurrent stress incontinence. Although the rate of bladder perforation was equivalent across groups, more patients who underwent SPARC required loosening of the sling postoperatively to relieve urinary retention.
These data suggest that the SPARC sling may be more difficult to adjust correctly even though it is designed with a tensioning suture. The difficulty may be a consequence of 1) smaller-caliber trocar tunnels or 2) the “top-down” approach less accurately locating the sling at the midportion of the urethra.
This study would have been more rigorous and the results, stronger, if postoperative assessment was made by a blinded examiner. An exceptional positive aspect of study design was that the investigators considered the surgeon’s level of experience—a variable that can certainly affect outcome.
Barber MD, Kleeman S, Karram MM, et al. Transobturator tape compared with tension-free vaginal tape for the treatment of stress urinary incontinence. Obstet Gynecol. 2008;111:611–621.
This randomized, controlled trial compared the efficacy of TVT with the transobturator tape (TOT) technique. Like Lord and colleagues’ study just discussed, it was conducted as an equivalence trial—to determine whether TOT is equivalent to TVT.
The primary outcome was abnormal bladder function 12 months after surgery, defined as the presence of any of the following:
- incontinence symptoms
- positive cough stress test
- retreatment for SUI
- treatment for postoperative urinary retention.
Women who had urodynamic stress incontinence were recruited from three academic centers; excluded were women who had detrusor overactivity, postvoid residual volume >100 mL, prior sling surgery, or contraindications to a midurethral sling.
For the retropubic approach, TVT was used. For the transobturator approach, the Monarc Subfascial Hammock (American Medical Systems) was used. Here, the tape is placed in an “outside-in” fashion.
Subjects completed a baseline bladder diary and a series of validated questionnaires. Postoperatively, subjects were followed for 2 years. Follow-up data included validated questionnaires, bladder diary, pelvic organ prolapse quantification, cough stress test, and postvoid residual volume determination. It was not possible to blind subjects or surgeons, but all postoperative assessments and exams were performed by a blinded nurse.
The investigators sought to determine if TVT and TOT yielded an equivalent (within a 15% margin) rate of abnormal bladder function.
Eventually, 170 patients underwent randomization and surgery (88, TVT; 82, TOT). Baseline demographic, clinical, and incontinence severity data were similar across groups.
Bladder perforation was more common with TVT than with TOT (7% and 0, respectively [p=.02]). Abnormal bladder function was noted in 46.6% of TVT subjects and in 42.7% of TOT subjects, with a noninferiority test demonstrating equivalence (p=.006). One year after surgery, 79% of patients in the TVT group and 82% of patients in the TOT group reported that bladder symptoms were “much better” or “very much better” (p=.88). No significant difference was noted between groups in any of the questionnaire responses after surgery.
This study has many strengths, including rigorous assessments, use of a blinded nurse-examiner to collect postoperative data, and a battery of validated questionnaires used throughout the study. In addition, the primary outcome measure, abnormal bladder function, is defined by stringent criteria that combine subjective and objective components, efficacy, and adverse events.
It will be interesting to see if the efficacy of TOT is maintained over time. The authors of the article point out that several transobturator sling kits are available, utilizing various trocar shapes, different approaches (i.e., “in to out”), and different types of mesh; this may mean variable rates of complications and different degrees of efficacy from one kit to the next.
Also notable in this study is that subjects had relatively high Valsalva leak-point pressures (approaching 100 cm H2O) in both groups.
Which technique is best for SUI with intrinsic sphincter deficiency?
Jeon MJ, Jung HJ, Chung SM, et al. Comparison of the treatment outcome of pubovaginal sling, tension-free vaginal tape, and transobturator tape for stress urinary incontinence with intrinsic sphincter deficiency. Am J Obstet Gynecol. 2008;199:76.e1–76.e4.
This retrospective cohort study was designed to evaluate techniques for treating severe SUI. Researchers were mainly interested in patients who had intrinsic sphincter deficiency (ISD), defined as a Valsalva leak-point pressure <60 cm H2O or maximal urethral closure pressure <20 cm H2O.
The pubovaginal (bladder neck) sling (PVS) has been considered the gold standard therapeutic option for patients who have ISD. Recently, however, data have shown satisfactory outcomes using TVT in this setting.2,3 The aim of this study, therefore, was to compare PVS, TVT, and TOT for treating SUI in patients who had ISD. (Note: The researchers used Uratape [Mentor-Purgès] for the transobturator sling.)
The study included 253 subjects who had ISD and who underwent surgical intervention (87, PVS; 94, TVT; 92, TOT); women who had detrusor overactivity and voiding dysfunction were excluded. Follow-up assessments were performed at 1, 3, 6, and 12 months and annually thereafter. Outcomes studied included complications and rates of cure; the latter was defined as 1) the absence of subjective complaints of leakage and 2) a negative cough stress test.
Median follow-up was 36, 24, and 12 months in the PVS, TVT, and TOT groups, respectively. All groups were similar in regard to baseline clinical and demographic characteristics. Bladder perforation was rare (PVS, 1; TVT and TOT, 0). No significant difference was noted across techniques in the rate of de novo urgency, voiding dysfunction, reoperation for urinary retention, and recurrent urinary tract infection.
Two years after surgery, the cure rate for the three procedures differed significantly: PVS and TVT, 87% each; TOT, 35% (p<.0001). A Cox proportional hazards regression model revealed that the risk of treatment failure with PVS was no different than it was for TVT. However, this model demonstrated that the risk of failure was 4.6 times higher for TOT compared with PVS (p<.0001).
This study is subject to the limitations of any retrospective study. It is unique, however, in that investigators focused on a more severe sample of subjects with ISD. In addition, the authors of the study used the appropriate statistical techniques to attempt to control for potential confounders.
Although the rate of cure was higher with TVT than with TOT, the rate of voiding dysfunction (i.e., the need for catheterization longer than 1 month after surgery) and de novo urgency was higher with TVT as well. This finding suggests that TVT provides more compressive force around the urethra than TOT does; on the other hand, it is possible instead that the difference arises in the method of tensioning of various types of sling.
Last, the study surgeon conducted the postoperative evaluations and was not blinded. This may have introduced bias into the assessments.
As more long-term data become available about different approaches to placing a midurethral sling, it’s likely that we will learn that not all techniques are equal. A customized approach—one that takes into account the individual patient’s clinical parameters—may be necessary to yield long-term efficacy with a sling.
Although, as the authors of this Update discuss, there are several surgical approaches to stress urinary incontinence (tension-free vaginal tape, suprapubic urethral support sling, transobturator tape, pubovaginal sling placed at the bladder neck), coding for the procedure is limited to a single Current Procedural Terminology (CPT) code when surgery is performed via a vaginal approach. CPT code 57288 ( Sling operation for stress incontinence [e.g., fascia or synthetic] ) has been assigned 21.59 relative value units in 2008 and should be reported no matter what type of sling is placed or what method is used to place it.
Failed placement
On occasion, sling material erodes or creates other problems for the patient, such that it must be removed or revised. To report correction of this adverse outcome, bill with 57287 (Removal or revision of sling for stress incontinence [e.g., fascia or synthetic]). If revision must be performed within the global period for the original procedure by the surgeon who placed the sling, append modifier -78 (Unplanned return to the operating/procedure room by the same physician following initial procedure for a related procedure during the postoperative period) to the revision code.
Minimally invasive placement
If you perform a sling procedure laparoscopically, report 51992 (Laparoscopy, surgical; sling operation for stress incontinence [e.g., fascia or synthetic]) instead. No corresponding code exists for laparoscopic revision of a sling procedure; under CPT rules, your only course is to report 51999 (Unlisted laparoscopy procedure, bladder).—MELANIE WITT, RN, CPC-OBGYN, MA
1. Nilsson CG, Palva K, Rezapour M, Falconer C. Eleven years prospective follow-up of the tension-free vaginal tape procedure for treatment of stress urinary incontinence. Int Urygynecol J Pelvic Floor Dysfunct. 2008;19:1043-1047.
2. Rezapour M, Falconer C, Ulmsten U. Tension-free vaginal tape (TVT) in stress incontinent women with intrinsic sphincter deficiency (ISD)—a long-term follow-up. Int Urogynecol J Pelvic Floor Dysfunct. 2001;12(Suppl 2):S12-S14.
3. Meschia M, Pifarotti P, Buonaguidi A, Gattei U, Spennacchio M. Tension-free vaginal tape (TVT) for treatment of stress urinary incontinence in women with low-pressure urethra. Eur J Obstet Gynecol Reprod Biol. 2005;122:118-121.
The authors report no financial relationships relevant to this article.
Over the past 10 years, the midurethral sling has replaced the Burch urethropexy as the most common surgical procedure for correcting stress urinary incontinence (SUI). In this “Update” on midurethral slings, we highlight three recently published studies that compare popular surgical approaches to SUI:
- the original tension-free vaginal tape (TVT) technique (FIGURE [“A”])
- the suprapubic urethral support sling (SPARC) (FIGURE [“B”])
- the transobturator tape (TOT) technique (FIGURE [“C”])
- the traditional pubovaginal sling (PVS), placed at the bladder neck (FIGURE [“D”]).
FIGURE [“A”] Four options for a midurethral sling to correct stress urinary incontinence: Tension-free vaginal tape (TVT) technique
FIGURE [“B”] Four options for a midurethral sling to correct stress urinary incontinence: Suprapubic urethral support sling (SPARC)
FIGURE [“C”] Four options for a midurethral sling to correct stress urinary incontinence: Transobturator tape (TOT) technique
FIGURE [“D”] Four options for a midurethral sling to correct stress urinary incontinence: Pubovaginal sling (PVS)
We’ve had a decade-plus of experience with the sling
The midurethral sling, first introduced as the tension-free vaginal tape, or TVT (Gynecare), was quick to be adopted because:
- it offers a minimally invasive approach
- it is highly efficacious
- serious adverse events are rare.
TVT utilizes a 5-mm trocar that is passed from the vagina through the retropubic space, exiting via small suprapubic incisions. A strip of permanent polypropylene mesh attached to these trocars is placed under the midportion of the urethra (FIGURE [“A”]).
We now have 11 years of follow-up data to support the use of the TVT midurethral sling for SUI.1
As TVT gained popularity, surgical equipment manufacturers developed various “kits,” so to speak, for placing a midurethral sling. Many have included innovations that have theoretical advantages over traditional TVT. Some place smaller, 3-mm trocars in a similar “bottom-up” fashion, as the TVT sling does; others utilize smaller trocars that are placed “top down” through the retropubic space into the vagina.
A later generation of slings uses the transobturator approach, to avoid blind passage of trocars through the retropubic space. These slings can be placed “in to out” or “out to in,” and rest in a slightly different orientation under the midurethra.
In an effort to make the procedure even more minimally invasive, some manufacturers now offer slings that are placed through one vaginal incision, thereby avoiding additional suprapubic or groin incisions. Other kits have made alterations to the polypropylene mesh by heat-sealing the material or applying a coating.
Such modifications haven’t always been improvements—some sling kits carried a higher incidence of mesh-related complications, and certain ones were removed from the market. And, although the number of commercially available midurethral sling kits has exploded, we’ve seen scant data published that compare the traditional TVT method with alternative approaches. Those alternatives may be considered midurethral slings, but we haven’t known whether minor variations in technique, or in the instrumentation, translate to improvements in long-term efficacy.
More readjustments for retention are needed after SPARC (vs. TVT)
Lord HE, Taylor JD, Finn JC, et al. A randomized controlled equivalence trial of short-term complications and efficacy of tension-free vaginal tape and suprapubic urethral support sling for treating stress incontinence. BJU Int. 2006;98:367–376.
This randomized, controlled trial compared TVT with SPARC to treat SUI. The study was designed as an equivalence trial: the investigators sought to determine if the “newer” intervention of the two (SPARC) is therapeutically equivalent to the existing intervention (TVT)—not whether one is superior. They therefore looked to see if patients who underwent TVT and those who underwent SPARC had the same rate (within a 5% margin) of bladder injury and other secondary outcomes.
Subjects were eligible to participate if they had SUI on the basis of urodynamic or clinical parameters. They were unaware of their assigned treatment, underwent TVT or SPARC, and were reevaluated 6 weeks postoperatively. Intraoperative, postoperative, and 6-week follow-up data were recorded by the study surgeon.
Three hundred and one patients were enrolled; 147 underwent TVT and 154 underwent SPARC. The groups were similar in regard to all baseline characteristics.
No significant difference was noted between the groups in the primary outcome, which was the rate of bladder perforation (TVT, 0.7%; SPARC, 1.9% [p=.62]). This effect remained after controlling for age, parity, prior urinary incontinence surgery, other concomitant surgery, and the surgeon’s level of experience. There were no intergroup differences in perioperative blood loss, urgency, or objective cure of SUI (defined as negative cough stress test) 6 weeks after surgery.
Subjects who underwent SPARC were more likely to experience urinary retention that required surgical readjustment of the sling (SPARC, 10 of 154; TVT, none [p=.002]). Although the objective cure rate was similar across groups, the subjective cure rate was significantly different (TVT, 87.1%; SPARC, 76.5% [p=.03]).
Regression analysis revealed that subjects who had prior surgery for urinary incontinence and those whose surgery was performed by a comparatively less experienced physician were more likely to report persistence of SUI symptoms.
This study reflects general clinical practice, in that it was conducted across a heterogeneous sample of subjects who had both primary and recurrent stress incontinence. Although the rate of bladder perforation was equivalent across groups, more patients who underwent SPARC required loosening of the sling postoperatively to relieve urinary retention.
These data suggest that the SPARC sling may be more difficult to adjust correctly even though it is designed with a tensioning suture. The difficulty may be a consequence of 1) smaller-caliber trocar tunnels or 2) the “top-down” approach less accurately locating the sling at the midportion of the urethra.
This study would have been more rigorous and the results, stronger, if postoperative assessment was made by a blinded examiner. An exceptional positive aspect of study design was that the investigators considered the surgeon’s level of experience—a variable that can certainly affect outcome.
Barber MD, Kleeman S, Karram MM, et al. Transobturator tape compared with tension-free vaginal tape for the treatment of stress urinary incontinence. Obstet Gynecol. 2008;111:611–621.
This randomized, controlled trial compared the efficacy of TVT with the transobturator tape (TOT) technique. Like Lord and colleagues’ study just discussed, it was conducted as an equivalence trial—to determine whether TOT is equivalent to TVT.
The primary outcome was abnormal bladder function 12 months after surgery, defined as the presence of any of the following:
- incontinence symptoms
- positive cough stress test
- retreatment for SUI
- treatment for postoperative urinary retention.
Women who had urodynamic stress incontinence were recruited from three academic centers; excluded were women who had detrusor overactivity, postvoid residual volume >100 mL, prior sling surgery, or contraindications to a midurethral sling.
For the retropubic approach, TVT was used. For the transobturator approach, the Monarc Subfascial Hammock (American Medical Systems) was used. Here, the tape is placed in an “outside-in” fashion.
Subjects completed a baseline bladder diary and a series of validated questionnaires. Postoperatively, subjects were followed for 2 years. Follow-up data included validated questionnaires, bladder diary, pelvic organ prolapse quantification, cough stress test, and postvoid residual volume determination. It was not possible to blind subjects or surgeons, but all postoperative assessments and exams were performed by a blinded nurse.
The investigators sought to determine if TVT and TOT yielded an equivalent (within a 15% margin) rate of abnormal bladder function.
Eventually, 170 patients underwent randomization and surgery (88, TVT; 82, TOT). Baseline demographic, clinical, and incontinence severity data were similar across groups.
Bladder perforation was more common with TVT than with TOT (7% and 0, respectively [p=.02]). Abnormal bladder function was noted in 46.6% of TVT subjects and in 42.7% of TOT subjects, with a noninferiority test demonstrating equivalence (p=.006). One year after surgery, 79% of patients in the TVT group and 82% of patients in the TOT group reported that bladder symptoms were “much better” or “very much better” (p=.88). No significant difference was noted between groups in any of the questionnaire responses after surgery.
This study has many strengths, including rigorous assessments, use of a blinded nurse-examiner to collect postoperative data, and a battery of validated questionnaires used throughout the study. In addition, the primary outcome measure, abnormal bladder function, is defined by stringent criteria that combine subjective and objective components, efficacy, and adverse events.
It will be interesting to see if the efficacy of TOT is maintained over time. The authors of the article point out that several transobturator sling kits are available, utilizing various trocar shapes, different approaches (i.e., “in to out”), and different types of mesh; this may mean variable rates of complications and different degrees of efficacy from one kit to the next.
Also notable in this study is that subjects had relatively high Valsalva leak-point pressures (approaching 100 cm H2O) in both groups.
Which technique is best for SUI with intrinsic sphincter deficiency?
Jeon MJ, Jung HJ, Chung SM, et al. Comparison of the treatment outcome of pubovaginal sling, tension-free vaginal tape, and transobturator tape for stress urinary incontinence with intrinsic sphincter deficiency. Am J Obstet Gynecol. 2008;199:76.e1–76.e4.
This retrospective cohort study was designed to evaluate techniques for treating severe SUI. Researchers were mainly interested in patients who had intrinsic sphincter deficiency (ISD), defined as a Valsalva leak-point pressure <60 cm H2O or maximal urethral closure pressure <20 cm H2O.
The pubovaginal (bladder neck) sling (PVS) has been considered the gold standard therapeutic option for patients who have ISD. Recently, however, data have shown satisfactory outcomes using TVT in this setting.2,3 The aim of this study, therefore, was to compare PVS, TVT, and TOT for treating SUI in patients who had ISD. (Note: The researchers used Uratape [Mentor-Purgès] for the transobturator sling.)
The study included 253 subjects who had ISD and who underwent surgical intervention (87, PVS; 94, TVT; 92, TOT); women who had detrusor overactivity and voiding dysfunction were excluded. Follow-up assessments were performed at 1, 3, 6, and 12 months and annually thereafter. Outcomes studied included complications and rates of cure; the latter was defined as 1) the absence of subjective complaints of leakage and 2) a negative cough stress test.
Median follow-up was 36, 24, and 12 months in the PVS, TVT, and TOT groups, respectively. All groups were similar in regard to baseline clinical and demographic characteristics. Bladder perforation was rare (PVS, 1; TVT and TOT, 0). No significant difference was noted across techniques in the rate of de novo urgency, voiding dysfunction, reoperation for urinary retention, and recurrent urinary tract infection.
Two years after surgery, the cure rate for the three procedures differed significantly: PVS and TVT, 87% each; TOT, 35% (p<.0001). A Cox proportional hazards regression model revealed that the risk of treatment failure with PVS was no different than it was for TVT. However, this model demonstrated that the risk of failure was 4.6 times higher for TOT compared with PVS (p<.0001).
This study is subject to the limitations of any retrospective study. It is unique, however, in that investigators focused on a more severe sample of subjects with ISD. In addition, the authors of the study used the appropriate statistical techniques to attempt to control for potential confounders.
Although the rate of cure was higher with TVT than with TOT, the rate of voiding dysfunction (i.e., the need for catheterization longer than 1 month after surgery) and de novo urgency was higher with TVT as well. This finding suggests that TVT provides more compressive force around the urethra than TOT does; on the other hand, it is possible instead that the difference arises in the method of tensioning of various types of sling.
Last, the study surgeon conducted the postoperative evaluations and was not blinded. This may have introduced bias into the assessments.
As more long-term data become available about different approaches to placing a midurethral sling, it’s likely that we will learn that not all techniques are equal. A customized approach—one that takes into account the individual patient’s clinical parameters—may be necessary to yield long-term efficacy with a sling.
Although, as the authors of this Update discuss, there are several surgical approaches to stress urinary incontinence (tension-free vaginal tape, suprapubic urethral support sling, transobturator tape, pubovaginal sling placed at the bladder neck), coding for the procedure is limited to a single Current Procedural Terminology (CPT) code when surgery is performed via a vaginal approach. CPT code 57288 ( Sling operation for stress incontinence [e.g., fascia or synthetic] ) has been assigned 21.59 relative value units in 2008 and should be reported no matter what type of sling is placed or what method is used to place it.
Failed placement
On occasion, sling material erodes or creates other problems for the patient, such that it must be removed or revised. To report correction of this adverse outcome, bill with 57287 (Removal or revision of sling for stress incontinence [e.g., fascia or synthetic]). If revision must be performed within the global period for the original procedure by the surgeon who placed the sling, append modifier -78 (Unplanned return to the operating/procedure room by the same physician following initial procedure for a related procedure during the postoperative period) to the revision code.
Minimally invasive placement
If you perform a sling procedure laparoscopically, report 51992 (Laparoscopy, surgical; sling operation for stress incontinence [e.g., fascia or synthetic]) instead. No corresponding code exists for laparoscopic revision of a sling procedure; under CPT rules, your only course is to report 51999 (Unlisted laparoscopy procedure, bladder).—MELANIE WITT, RN, CPC-OBGYN, MA
The authors report no financial relationships relevant to this article.
Over the past 10 years, the midurethral sling has replaced the Burch urethropexy as the most common surgical procedure for correcting stress urinary incontinence (SUI). In this “Update” on midurethral slings, we highlight three recently published studies that compare popular surgical approaches to SUI:
- the original tension-free vaginal tape (TVT) technique (FIGURE [“A”])
- the suprapubic urethral support sling (SPARC) (FIGURE [“B”])
- the transobturator tape (TOT) technique (FIGURE [“C”])
- the traditional pubovaginal sling (PVS), placed at the bladder neck (FIGURE [“D”]).
FIGURE [“A”] Four options for a midurethral sling to correct stress urinary incontinence: Tension-free vaginal tape (TVT) technique
FIGURE [“B”] Four options for a midurethral sling to correct stress urinary incontinence: Suprapubic urethral support sling (SPARC)
FIGURE [“C”] Four options for a midurethral sling to correct stress urinary incontinence: Transobturator tape (TOT) technique
FIGURE [“D”] Four options for a midurethral sling to correct stress urinary incontinence: Pubovaginal sling (PVS)
We’ve had a decade-plus of experience with the sling
The midurethral sling, first introduced as the tension-free vaginal tape, or TVT (Gynecare), was quick to be adopted because:
- it offers a minimally invasive approach
- it is highly efficacious
- serious adverse events are rare.
TVT utilizes a 5-mm trocar that is passed from the vagina through the retropubic space, exiting via small suprapubic incisions. A strip of permanent polypropylene mesh attached to these trocars is placed under the midportion of the urethra (FIGURE [“A”]).
We now have 11 years of follow-up data to support the use of the TVT midurethral sling for SUI.1
As TVT gained popularity, surgical equipment manufacturers developed various “kits,” so to speak, for placing a midurethral sling. Many have included innovations that have theoretical advantages over traditional TVT. Some place smaller, 3-mm trocars in a similar “bottom-up” fashion, as the TVT sling does; others utilize smaller trocars that are placed “top down” through the retropubic space into the vagina.
A later generation of slings uses the transobturator approach, to avoid blind passage of trocars through the retropubic space. These slings can be placed “in to out” or “out to in,” and rest in a slightly different orientation under the midurethra.
In an effort to make the procedure even more minimally invasive, some manufacturers now offer slings that are placed through one vaginal incision, thereby avoiding additional suprapubic or groin incisions. Other kits have made alterations to the polypropylene mesh by heat-sealing the material or applying a coating.
Such modifications haven’t always been improvements—some sling kits carried a higher incidence of mesh-related complications, and certain ones were removed from the market. And, although the number of commercially available midurethral sling kits has exploded, we’ve seen scant data published that compare the traditional TVT method with alternative approaches. Those alternatives may be considered midurethral slings, but we haven’t known whether minor variations in technique, or in the instrumentation, translate to improvements in long-term efficacy.
More readjustments for retention are needed after SPARC (vs. TVT)
Lord HE, Taylor JD, Finn JC, et al. A randomized controlled equivalence trial of short-term complications and efficacy of tension-free vaginal tape and suprapubic urethral support sling for treating stress incontinence. BJU Int. 2006;98:367–376.
This randomized, controlled trial compared TVT with SPARC to treat SUI. The study was designed as an equivalence trial: the investigators sought to determine if the “newer” intervention of the two (SPARC) is therapeutically equivalent to the existing intervention (TVT)—not whether one is superior. They therefore looked to see if patients who underwent TVT and those who underwent SPARC had the same rate (within a 5% margin) of bladder injury and other secondary outcomes.
Subjects were eligible to participate if they had SUI on the basis of urodynamic or clinical parameters. They were unaware of their assigned treatment, underwent TVT or SPARC, and were reevaluated 6 weeks postoperatively. Intraoperative, postoperative, and 6-week follow-up data were recorded by the study surgeon.
Three hundred and one patients were enrolled; 147 underwent TVT and 154 underwent SPARC. The groups were similar in regard to all baseline characteristics.
No significant difference was noted between the groups in the primary outcome, which was the rate of bladder perforation (TVT, 0.7%; SPARC, 1.9% [p=.62]). This effect remained after controlling for age, parity, prior urinary incontinence surgery, other concomitant surgery, and the surgeon’s level of experience. There were no intergroup differences in perioperative blood loss, urgency, or objective cure of SUI (defined as negative cough stress test) 6 weeks after surgery.
Subjects who underwent SPARC were more likely to experience urinary retention that required surgical readjustment of the sling (SPARC, 10 of 154; TVT, none [p=.002]). Although the objective cure rate was similar across groups, the subjective cure rate was significantly different (TVT, 87.1%; SPARC, 76.5% [p=.03]).
Regression analysis revealed that subjects who had prior surgery for urinary incontinence and those whose surgery was performed by a comparatively less experienced physician were more likely to report persistence of SUI symptoms.
This study reflects general clinical practice, in that it was conducted across a heterogeneous sample of subjects who had both primary and recurrent stress incontinence. Although the rate of bladder perforation was equivalent across groups, more patients who underwent SPARC required loosening of the sling postoperatively to relieve urinary retention.
These data suggest that the SPARC sling may be more difficult to adjust correctly even though it is designed with a tensioning suture. The difficulty may be a consequence of 1) smaller-caliber trocar tunnels or 2) the “top-down” approach less accurately locating the sling at the midportion of the urethra.
This study would have been more rigorous and the results, stronger, if postoperative assessment was made by a blinded examiner. An exceptional positive aspect of study design was that the investigators considered the surgeon’s level of experience—a variable that can certainly affect outcome.
Barber MD, Kleeman S, Karram MM, et al. Transobturator tape compared with tension-free vaginal tape for the treatment of stress urinary incontinence. Obstet Gynecol. 2008;111:611–621.
This randomized, controlled trial compared the efficacy of TVT with the transobturator tape (TOT) technique. Like Lord and colleagues’ study just discussed, it was conducted as an equivalence trial—to determine whether TOT is equivalent to TVT.
The primary outcome was abnormal bladder function 12 months after surgery, defined as the presence of any of the following:
- incontinence symptoms
- positive cough stress test
- retreatment for SUI
- treatment for postoperative urinary retention.
Women who had urodynamic stress incontinence were recruited from three academic centers; excluded were women who had detrusor overactivity, postvoid residual volume >100 mL, prior sling surgery, or contraindications to a midurethral sling.
For the retropubic approach, TVT was used. For the transobturator approach, the Monarc Subfascial Hammock (American Medical Systems) was used. Here, the tape is placed in an “outside-in” fashion.
Subjects completed a baseline bladder diary and a series of validated questionnaires. Postoperatively, subjects were followed for 2 years. Follow-up data included validated questionnaires, bladder diary, pelvic organ prolapse quantification, cough stress test, and postvoid residual volume determination. It was not possible to blind subjects or surgeons, but all postoperative assessments and exams were performed by a blinded nurse.
The investigators sought to determine if TVT and TOT yielded an equivalent (within a 15% margin) rate of abnormal bladder function.
Eventually, 170 patients underwent randomization and surgery (88, TVT; 82, TOT). Baseline demographic, clinical, and incontinence severity data were similar across groups.
Bladder perforation was more common with TVT than with TOT (7% and 0, respectively [p=.02]). Abnormal bladder function was noted in 46.6% of TVT subjects and in 42.7% of TOT subjects, with a noninferiority test demonstrating equivalence (p=.006). One year after surgery, 79% of patients in the TVT group and 82% of patients in the TOT group reported that bladder symptoms were “much better” or “very much better” (p=.88). No significant difference was noted between groups in any of the questionnaire responses after surgery.
This study has many strengths, including rigorous assessments, use of a blinded nurse-examiner to collect postoperative data, and a battery of validated questionnaires used throughout the study. In addition, the primary outcome measure, abnormal bladder function, is defined by stringent criteria that combine subjective and objective components, efficacy, and adverse events.
It will be interesting to see if the efficacy of TOT is maintained over time. The authors of the article point out that several transobturator sling kits are available, utilizing various trocar shapes, different approaches (i.e., “in to out”), and different types of mesh; this may mean variable rates of complications and different degrees of efficacy from one kit to the next.
Also notable in this study is that subjects had relatively high Valsalva leak-point pressures (approaching 100 cm H2O) in both groups.
Which technique is best for SUI with intrinsic sphincter deficiency?
Jeon MJ, Jung HJ, Chung SM, et al. Comparison of the treatment outcome of pubovaginal sling, tension-free vaginal tape, and transobturator tape for stress urinary incontinence with intrinsic sphincter deficiency. Am J Obstet Gynecol. 2008;199:76.e1–76.e4.
This retrospective cohort study was designed to evaluate techniques for treating severe SUI. Researchers were mainly interested in patients who had intrinsic sphincter deficiency (ISD), defined as a Valsalva leak-point pressure <60 cm H2O or maximal urethral closure pressure <20 cm H2O.
The pubovaginal (bladder neck) sling (PVS) has been considered the gold standard therapeutic option for patients who have ISD. Recently, however, data have shown satisfactory outcomes using TVT in this setting.2,3 The aim of this study, therefore, was to compare PVS, TVT, and TOT for treating SUI in patients who had ISD. (Note: The researchers used Uratape [Mentor-Purgès] for the transobturator sling.)
The study included 253 subjects who had ISD and who underwent surgical intervention (87, PVS; 94, TVT; 92, TOT); women who had detrusor overactivity and voiding dysfunction were excluded. Follow-up assessments were performed at 1, 3, 6, and 12 months and annually thereafter. Outcomes studied included complications and rates of cure; the latter was defined as 1) the absence of subjective complaints of leakage and 2) a negative cough stress test.
Median follow-up was 36, 24, and 12 months in the PVS, TVT, and TOT groups, respectively. All groups were similar in regard to baseline clinical and demographic characteristics. Bladder perforation was rare (PVS, 1; TVT and TOT, 0). No significant difference was noted across techniques in the rate of de novo urgency, voiding dysfunction, reoperation for urinary retention, and recurrent urinary tract infection.
Two years after surgery, the cure rate for the three procedures differed significantly: PVS and TVT, 87% each; TOT, 35% (p<.0001). A Cox proportional hazards regression model revealed that the risk of treatment failure with PVS was no different than it was for TVT. However, this model demonstrated that the risk of failure was 4.6 times higher for TOT compared with PVS (p<.0001).
This study is subject to the limitations of any retrospective study. It is unique, however, in that investigators focused on a more severe sample of subjects with ISD. In addition, the authors of the study used the appropriate statistical techniques to attempt to control for potential confounders.
Although the rate of cure was higher with TVT than with TOT, the rate of voiding dysfunction (i.e., the need for catheterization longer than 1 month after surgery) and de novo urgency was higher with TVT as well. This finding suggests that TVT provides more compressive force around the urethra than TOT does; on the other hand, it is possible instead that the difference arises in the method of tensioning of various types of sling.
Last, the study surgeon conducted the postoperative evaluations and was not blinded. This may have introduced bias into the assessments.
As more long-term data become available about different approaches to placing a midurethral sling, it’s likely that we will learn that not all techniques are equal. A customized approach—one that takes into account the individual patient’s clinical parameters—may be necessary to yield long-term efficacy with a sling.
Although, as the authors of this Update discuss, there are several surgical approaches to stress urinary incontinence (tension-free vaginal tape, suprapubic urethral support sling, transobturator tape, pubovaginal sling placed at the bladder neck), coding for the procedure is limited to a single Current Procedural Terminology (CPT) code when surgery is performed via a vaginal approach. CPT code 57288 ( Sling operation for stress incontinence [e.g., fascia or synthetic] ) has been assigned 21.59 relative value units in 2008 and should be reported no matter what type of sling is placed or what method is used to place it.
Failed placement
On occasion, sling material erodes or creates other problems for the patient, such that it must be removed or revised. To report correction of this adverse outcome, bill with 57287 (Removal or revision of sling for stress incontinence [e.g., fascia or synthetic]). If revision must be performed within the global period for the original procedure by the surgeon who placed the sling, append modifier -78 (Unplanned return to the operating/procedure room by the same physician following initial procedure for a related procedure during the postoperative period) to the revision code.
Minimally invasive placement
If you perform a sling procedure laparoscopically, report 51992 (Laparoscopy, surgical; sling operation for stress incontinence [e.g., fascia or synthetic]) instead. No corresponding code exists for laparoscopic revision of a sling procedure; under CPT rules, your only course is to report 51999 (Unlisted laparoscopy procedure, bladder).—MELANIE WITT, RN, CPC-OBGYN, MA
1. Nilsson CG, Palva K, Rezapour M, Falconer C. Eleven years prospective follow-up of the tension-free vaginal tape procedure for treatment of stress urinary incontinence. Int Urygynecol J Pelvic Floor Dysfunct. 2008;19:1043-1047.
2. Rezapour M, Falconer C, Ulmsten U. Tension-free vaginal tape (TVT) in stress incontinent women with intrinsic sphincter deficiency (ISD)—a long-term follow-up. Int Urogynecol J Pelvic Floor Dysfunct. 2001;12(Suppl 2):S12-S14.
3. Meschia M, Pifarotti P, Buonaguidi A, Gattei U, Spennacchio M. Tension-free vaginal tape (TVT) for treatment of stress urinary incontinence in women with low-pressure urethra. Eur J Obstet Gynecol Reprod Biol. 2005;122:118-121.
1. Nilsson CG, Palva K, Rezapour M, Falconer C. Eleven years prospective follow-up of the tension-free vaginal tape procedure for treatment of stress urinary incontinence. Int Urygynecol J Pelvic Floor Dysfunct. 2008;19:1043-1047.
2. Rezapour M, Falconer C, Ulmsten U. Tension-free vaginal tape (TVT) in stress incontinent women with intrinsic sphincter deficiency (ISD)—a long-term follow-up. Int Urogynecol J Pelvic Floor Dysfunct. 2001;12(Suppl 2):S12-S14.
3. Meschia M, Pifarotti P, Buonaguidi A, Gattei U, Spennacchio M. Tension-free vaginal tape (TVT) for treatment of stress urinary incontinence in women with low-pressure urethra. Eur J Obstet Gynecol Reprod Biol. 2005;122:118-121.